Session 2007/2008
Third Report
The Committee for Health, Social Services and Public Safety
Report on the Inquiry into
the Prevention of Suicide
and Self Harm
Volume Two
WRITEEN SUBMISSIONS, OTHER EVIDENCE AND LIST OF WITNESSES
RELATING TO THE REPORT
Ordered by The Committee for Health, Social Services and Public Safety
to be printed 1 May 2008
Report: 27/07/08R Committee for Health, Social Services and Public Safety
This document is available in a range of alternative formats.
For more information please contact the
Northern Ireland Assembly, Printed Paper Office,
Parliament Buildings, Stormont, Belfast, BT4 3XX
Tel: 028 9052 1078
Committee for Health, Social Services
and Public Safety
Membership and Powers
The Committee for Health, Social Services and Public Safety is a Statutory Departmental Committee established in accordance with paragraphs 8 and 9 of the Belfast Agreement, section 29 of the Northern Ireland Act 1998 and under Standing Order 46.
The Committee has power to:
- Consider and advise on Departmental budgets and annual plans in the context of the overall budget allocation;
- Consider relevant secondary legislation and take the Committee stage of primary legislation;
- Call for persons and papers;
- Initiate inquires and make reports; and
- Consider and advise on any matters brought to the Committee by the Minister for Health, Social Services and Public Safety
The Committee has 11 members including a Chairperson and Deputy Chairperson and a quorum of 5.
The membership of the Committee since 9 May 2007 has been as follows:
Mrs Iris Robinson MP (Chairperson)
Ms Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Mrs Carmel Hanna
Rev Dr Robert Coulter
Mr John McCallister
Dr Kieran Deeny
Ms Carál Ní Chuilín
Mr Alex Easton Ms Sue Ramsey
Mr Tommy Gallagher
Table of Contents
Volume One
Volume Two
Written Submissions
Other Evidence Considered by the Committee
List of Witnesses who Gave Oral Evidence to the Committee
Appendix 3
Written Submissions
Age Concern Northern Ireland
Introduction:
Age Concern Northern Ireland (ACNI) is a major voluntary organisation committed through campaigning and service provision to promoting the rights of all older people as active, involved and equal citizens. We act as a Northern Ireland-wide campaigning body and support a network of local Age Concern Groups operating throughout Northern Ireland.
We offer policy advice on a range of issues which impact on the lives of older people. These policies are based on:
- the expressed views of older people throughout Northern Ireland based on on-going contact and research;
- a knowledge of older people and an ageing society.
In 2003 Age Concern and the Mental Health Foundation launched the UK Inquiry into Mental Health and Well-Being in Later Life. This was because of a shared concern that mental health in later life is a neglected area with gaps between policies and services for mental health and those for older people. ACNI was represented on the Advisory Group which contributed to the
Inquiry. The Inquiry’s second report published by in August 2007– www.mhilli.org- reviews the services available to older people with mental health problems . We commend the Inquiry report to the Committee as a valuable source of information and guidance
The Northern Ireland Suicide Prevention Strategy 2006-2011-Protect Life: A shared Vision has, and rightly so, focused on children and young people. However suicide and self-harm is also an issue in later life, with suicide rates across the UK remaining high for both older men and women, especially those aged 75 and over. Depression in older people is under-diagnosed and, even in diagnosed cases, under treated. In our view the Committee inquiry in examining the current strategic approach to the prevention of suicide and self harm should consider what can be done to improve levels of services and support for those aged 65 and over. Older people should be identified and included as a priority group within the scope of the strategy.
Suicide in Later Life.
Depression is the leading cause of suicide in older people. Between 71% and 95% of older people who die by suicide have a diagnosable mental health problem at the time of death (Beeston 2006 quoted in Improving Services for Older With Mental Health Problems) Risk factors for depression are therefore also risk factors for suicide. Better detection, prevention and treatment of depression will have the most effect on preventing suicides in older people. Other risk factors include sleep problems such as insomnia, and alcohol consumption, particularly in men.
Suicide in later life is marked by certain distinct characteristics
- Although older people make fewer suicide attempts than young people they are more likely to be successful in taking their own lives.
- Older people , especially men, use more lethal methods such as firearms and hanging. Older women often die by drug overdose.
- Older people are less likely to recover from a suicide attempt and are less likely to have someone intervene.
- Nearly half of older people who take their own lives visit their GP in the month before suicide.
Preventing Suicide.
There is a need to raise the profile of older people within mental health strategy and service provision so that suicide in later life will be recognised as the serious problem that it is.
Public education campaigns are needed to raise general awareness about suicide risk in later life. These should target family, friends and frontline workers in health and social care and others who have regular contact with older people.
Prevention strategy needs to give high priority to community based initiatives that reduce social isolation amongst older people. This could include telephone help-lines that target isolated and disabled older people.
Follow up services are needed for older people who have attempted suicide and those who deliberately self harm.
Reducing access to lethal means for men and prescription drugs (benzodiazepines and other sedatives) for women would have a positive impact.
David Savage
Policy Officer
Age Concern Northern Ireland
9th October 2007.
The Royal College of Psychiatrists
The Royal College of Psychiatrists is the statutory body responsible for the supervision of the training and accreditation of psychiatrists in Britain and Ireland and for providing guidelines and advice regarding the treatment, care and prevention of mental and behavioural disorders.
The College welcomes the Assembly Health Committee’s inquiry to examine the current strategy to prevent suicide and self harm, and is grateful for the opportunity to contribute to this.
Consultant psychiatrists lead multidisciplinary teams that are at the heart of the service in every locality in Northern Ireland, and as such work with people at risk of suicide on a daily basis.[1]
The College has 230 members in Northern Ireland, as well as younger doctors in training. These doctors provide the backbone of the local psychiatric service, offering inpatient, day patient and outpatient treatment, as well as specialist care and consultation across a large range of settings.
Every day throughout their professional lives psychiatrists assess suicidal risk; this is an integral part of the basic psychiatric assessment. Consultant psychiatrists will have spent up to 10 years in training in the full range of physical, psychological and social therapeutic techniques and are well placed to manage the most complex cases. Our contact with large numbers of patients gives an overview of many of the background factors that affect suicide and suicidal behaviour.
Suicide is a final act which always arises as a consequence of a great complexity of issues. It can be related firstly to severe mental illness such as schizophrenia, bipolar disorder or severe depression. Secondly, it may be associated with abuse of alcohol or drugs, personality difficulties or social problems. Often these are not easily remedied by direct medical intervention, although longer-term work may be of benefit to the person. Thirdly, suicide is also significantly linked to prevailing social and cultural issues within society, for example easy access to a means of suicide or a local suicide cluster.
About 50% of people have suicidal thoughts at some time, but each year just 0.01% (one in 10,000) die by suicide. It is clear that there is no single answer to dealing with our suicide problem; the only approach is for all of us, professionals, the voluntary sector, politicians, local communities, families and individuals as citizens to work together to provide a range of interventions.
The College has identified key areas that we believe are essential to tackling the problem of suicide. These are:
- Psychiatric services in general hospitals for those who have self-harmed, and the availability of specialist advice to hospitals for adolescents who are suicidal;
- The urgent need for more ‘talking therapies’; and
- A stronger societal response to alcohol misuse.
In addition, there is an overarching need to develop a mentally healthy society and to identify opportunities for real partnership between the statutory and voluntary sectors. The role of the media in overcoming stigma surrounding mental health and responsibly reporting on suicide cannot be underestimated.
Psychiatric services in general hospitals for those who have self harmed
Recent research suggests that full assessment of self harm[2] cases is possibly the most important suicide prevention measure that can be taken.[3]
Of those who self harm, 1% are likely to complete suicide within the next year[4], an increase in risk of 100 times. This is clearly an easily identifiable group of people who are at risk and who can and should be offered thorough assessment and, if necessary, follow up.
Research indicates that when a person who has self harmed is assessed by a trained mental heath professional, the likelihood of repetition is reduced by 50% (NICE – The National Institute of Clinical Excellence 2004). Local audit has noted that a thorough professional assessment improves the outcome by a factor of 4. The NICE Guidelines (2004) demand that every patient is given a full psychosocial assessment after self–harm.[5]
Approximately 10% of those who present to A&E Departments with self harm are adolescents. The committee will be aware of the continuing difficulties in developing a comprehensive adolescent service which can provide expert advice to all Emergency Departments.
Ideally, each Emergency Department should be able to call on a rota of adolescent mental health professionals.
Unfortunately it seems unlikely that this will happen in the near future, particularly given continuing recruitment problems.
The Department of Social Development has recently funded a Self – Harm Service for North and West Belfast based at the Mater Hospital in Belfast to run until April 2008.
Under the leadership of Dr. O’ Kane, this team with specialist skills offers a comprehensive assessment and treatment to people who have self-harmed. This model is based upon best practice developed throughout the UK and North America and is the only service of its type in Ireland. Early results have been encouraging and a full audit of the service is being carried out.
On the basis of knowledge and skills particularly developed since 2004, the team runs a twice weekly, 16 week psychotherapy group for people who repeatedly self harm, often suffering from Emotionally Unstable Personality Disorder. Middle aged females with this diagnosis are recognised as being at particular risk of suicide.
The Mater Emergency Department has reported a significant reduction in the attendance of such individuals with self–harming behaviour as a result. For the most complex patients there is an 18-month group. Early indicators of improved social and psychological functioning have been very positive.
This is currently only a temporary project. The College would strongly encourage the Committee to consider how this type of service can be more permanently made available.
The need for more ‘Talking Therapies’
Surveys often report that patients and the public in general would like more access to ‘Talking Therapies’ including psychotherapy and counselling.[6] There is a common perception that doctors are overly reliant upon medication. The reality is that Psychiatrists and GPs are as frustrated as the public at the lack of availability of psychotherapies. All psychiatrists have training and experience in psychotherapy, a number have specialised in specific therapies and others are local leaders in psychotherapy. However all too often the demands of providing a 24-hour service for all psychiatric illness within a defined geographical area means there is insufficient time for psychiatrists to offer more psychotherapeutic treatments.
Many of those who present to Emergency Departments having harmed themselves, particularly younger people, have problems related to interpersonal, social and personality difficulties rather than primary psychiatric illness. For these individuals it is much more fruitful to adopt a psychosocial approach. Such an approach requires both time and training.
The World Federation for Mental Health has said[7] : ‘A series of psychotherapies has been shown to reduce suicidal behaviour including cognitive behavioural therapy (CBT) , interpersonal psychotherapy (IPT), dialectic behaviour therapy (DBT), psychodynamic / analytic psychotherapy and some forms of problem solving therapy (PST)’. The Federation went on to say that action was needed to improve treatment methods and facilities for suicidal individuals through psychotherapeutic interventions. It also called for more research into psychotherapy and counselling for those who have self-harmed.
The College reiterates its view that there is a real dearth of psychotherapeutic interventions for patients in N. Ireland, and calls for a real effort to address this.
The problem of Alcohol Misuse
Alcohol and drug abuse contribute significantly to suicide and self-harm behaviour. They often lead to depression, they can cause multiple social and financial problems, and they often lead to impulsive and risky behaviour. Every psychiatrist who sees patients in general hospitals is keenly aware that alcohol is a factor in over 50% of self– harm cases, and that people who are intoxicated and harm themselves in many cases would not have done so had they been sober.
In Northern Ireland there are well-developed addiction services, although more needs to be done.
The College takes the view that this is an area where public health and indeed public policy has a major role to play. Our cultural tradition is of relatively heavy binge drinking, particularly at weekends. This leads not just to an increase in self-harm but to high levels of aggression and violence.
It will be very difficult to change long-established patterns of behaviour in this area, but we must persist. The College believes that we must carefully review the issue of advertising on television. The sponsorship of sports by the alcohol industry is particularly alarming, given the high suicide rate in young men, the key target group of the advertising.
There is evidence that alcohol consumption is related to price and availability. While recognising that these are complex and politicised issues the College recommends, given our current suicide problem, that we look at the whole range of possible public health approaches to alcohol misuse.
Underpinning issues
The College welcomes the £3 million funding made available by the Minister to implement the recommendations of the Suicide Taskforce and warmly commends the commitment of a wide range of voluntary and community groups, as well certain highly dedicated individuals, who have contributed right across Northern Ireland to raising the profile of mental illness and its consequences.
The College was represented on the initial Suicide Taskforce and responded to the consultation. We have concerns however that there is sometimes a lack of communication between all the main stakeholders. We hope that the development of five large Trusts with coherent Mental Health leadership will enable real partnership working between the professionals and the voluntary sector.
To have a lasting reduction in the rate of suicide in Northern Ireland, we must start building a more mentally healthy society. This means working in schools to raise awareness of mental well-being, so that the next generation will have stronger emotional resilience and a better understanding of mental ill health. To be effective, this will require genuine cross-government working between the Departments responsible for health, schools, further education, training and employment. Mental health must be put on the school curriculum, with parents and teachers also given information on supporting a young person with a mental health problem. The Royal College of Psychiatrists has a range of free materials that can be downloaded from our internet site.[8]
There is an abundance of international evidence that shows the role the media has in combating the stigma of mental health problems, but also the risk of triggering suicide through irresponsible reporting or portrayal. Stigma prevents people from getting help early, or in some cases at all. We are aware that the Minister’s team is working with the media to promote safe reporting, and hope this will continue. We commend the Health Promotion Agency’s awareness campaign, and hope to see further marketing approaches to combating stigma.
Conclusion
The College is keen to assure the Committee that its members remain deeply committed to doing everything within their power, at the clinical and the policy level, to provide the best care possible for the mentally ill and particularly those at risk of suicide.
Appendix One (Glossary)
Self – Harm
A deliberate non-fatal act, including overdosing, cutting and attempted hanging, done in the knowledge that it is potentially harmful. It can be conceptualised as a non-verbal externalised communication.
Psychotherapy
A talking technique through which the therapist helps patients find relief from emotional distress. Its success depends upon the therapist’s ability to understand the patient and the patient’s use of the therapist.
Cognitive Behaviour Therapy (Cbt).
This treatment is based upon the premise that the way the patient thinks (‘negative automatic thoughts’) can lead to depression and other problems. The therapist helps the patient identify and change the negative thoughts.
Interpersonal Psychotherapy
A therapy based on the premise that problems in interpersonal relationships including bereavement, disputes and life changes can lead to depression. The therapist helps the patient to improve their interpersonal communication and to develop new attachments.
Dynamic Psychotherapy
A treatment in which the therapist helps the patient to understand and deal with current problems in the context of what has happened in the past.
Multidisciplinary Teams
In the community psychiatric care is delivered by a team of professionals working closely together, including psychiatrists, community psychiatric nurses, mental health social workers, occupational therapists and sometimes psychologists.
APPENDIX 2
The Self Harm Service North and West Belfast
The Self Harm Service for North and West Belfast is based at the Mater Hospital. It has been funded by the Department of Social Development through the Renewing Protestant Working Class Communities Initiative until April 2008. It currently consists of a consultant psychiatrist in psychotherapy /adult psychiatry, 3 mental health nurse therapists, trained in the range of psychotherapies, a part-time psychoanalytic psychotherapist (10 hrs per week) and administrative support.
Across the Mater and RVH A&E departments there are currently up to 50 presentations for mental health reasons, 90% of whom present with self harm per week. There is one full time psychiatric liaison nurse based at the RVH (mon-fri 8.30-4.30pm) and 1.4 psychiatric liaison nurses based at the Mater (8.30-4.30pm daily). This provision is regarded universally as being wholly inadequate, particularly at times when annual leave has to be covered.
The Self Harm Service interfaces with the Psychiatric liaison services at the Mater and RVH sites. It provides rapid follow up to people discharged from A&E assessed as at increased risk of self harm and suicide, through short-term one to one interventions.
Where longer term work is required, particularly for those who repeatedly self harm and present with other challenging behaviours, an initial twice weekly 16 week self harm programme is offered, and where required, a longer term group for those with emotionally unstable personality disorder, where repeated self harm is a constant feature of the disorder.
In addition, through government agencies such as the Health Action Zone, the Team works in partnership with users, carers, community and voluntary sector representatives.
The Team leads the “Better Services for People who Self Harm “audit in North and West Belfast run by the Royal College of Psychiatrists in collaboration with the Royal College of Nursing, College of Emergency Medicine, LAMP and the Ambulance Service Northern Ireland.
The Self Harm Team has been trained by experts from England and North America. In addition, it now provides expert trainings (such as STORM) to other professional groups. Within the framework of the Protect Life Strategy in conjunction with the Health Promotion Agency, we are developing a regional Self Harm and Suicide Prevention training strategy for North and West Belfast to be considered for Northern Ireland.
In addition we have organised a number of User led initiatives and conferences.
Aims
1) To provide a rapid and comprehensive follow-up to those people who have attended A&E following an episode of self-harm. In collaboration with existing Psychiatric Liaison Nursing Services (PLN) at the Mater and the RVH sites, the Self Harm Team targets a group of people who traditionally would not receive a rapid follow-up service, who are at an increased risk of completed suicide (Hawton and Fagg 1992, Nordentoft et al 1993 and Powell et al 2000).
2) To provide ongoing treatment and support, particularly group interventions, to those people who have a history of repeated self harm.
3) To participate in local and regional Audit and research of Self Harm Services
4) To provide advice and teaching and training to others involved in the provision of services to people who self harm
5) To liaise and where appropriate to work with all relevant statutory and non-statutory organisations, locally, regionally and nationally.
6) To develop and maintain effective working relationships with all stakeholders involved in the delivery of mental health services to provide, where possible, a seamless service within the community.
7) To promote partnerships among practitioners, service users and carers.
The Profile of the Service Users
Of those who attend the service because of repeated self harm, a profile has begun to emerge. The age range is 18-66 years.
23% have been in care as children
72% have been in contact with the criminal justice system, usually for minor offences
60% have a history of drug and alcohol misuse
60% have a history of childhood sexual abuse
35% have a history of teenage pregnancy
50% have young children
65% have history of social services involvement
100% are on state benefits
100% have a history of failed employment
100% have a history of repeated broken relationships
100% have received psychiatric inpatient care in the past
82% have a diagnosis of Emotionally Unstable Personality Disorder
30% have a history of eating disorders
30% have been on the peripheries of paramilitary activity
Following Contact with Services, Outcomes to date:
90% have consistently reduced their self harming behaviours
The usage of the overall percentage of A&E services has dropped from 25% of all attendances to <5%
25% have completed NVQs, HNDs or begun Third Level Education
10% have begun part-time paid employment
Hospital Admission has dropped with fewer than 10% now using psychiatric hospital admission, and now on a respite or severe crisis basis only
[1] Appendix 1 explains the roles within the multidisciplinary team.
[2] Self harm is explained in Appendix 1
[3] Professor David Owens of Leeds University and Dr Navneet Kapur of the Manchester Centre for Suicide Prevention (British Journal of Psychiatry 2005)
[4] Keith Hawton (2000)
[5] Clinical Guideline 16, Self Harm, NICE 2004
[6] For more information on Talking Therapies, see Appendix 1
[7] World Federation for Mental Health (2006)
[8] http://www.rcpsych.ac.uk/mentalhealthinformation/mentalhealthandgrowingup.aspx
The Health and Safety Executive for Northern Ireland
1. The Committee is invited to note that the role of the Health and Safety Executive for Northern Ireland (HSENI) is prescribed by the Health and Safety at Work (Northern Ireland) Order 1978 as amended by the Health and Safety at Work ( Amendment) ( Northern Ireland ) Order 1998.
2. This limits HSENI’s role to one of regulating health and safety within the context of the workplace. HSENI therefore works to try to encourage preventative workplace strategies based around promoting good mental health and well being that in the long run may mitigate the stressors that arise from work that might contribute to someone self harming or committing suicide.
3. HSENI has concentrated on preventive strategies aimed at particular work sectors such as the health sector where work related stress has been identified as a causal factor in sickness absence. These interventions are aimed at delivering a positive effect on the health and mental well-being of people within organisations through the adoption of good stress management practices.
4. HSENI is working with the Northern Ireland Civil Service Occupational Health Service to study the causes of sickness absence and in terms of mental health HSENI is working with the Department of Finance and Personnel Central Personnel Group helping it adopt the UK stress management toolkit for the workplace, known as the Stress Management Standards.
5. In addition HSENI has worked with other public sector employers such as the District Councils and further education colleges encouraging them to identify and begin to manage stress related issues and to encourage the use of the toolkit. This work has been piloted under the banner of “Workpositive” and will be further extended during 2007/08 with new work sectors being challenged.
6. In the current year HSENI will challenge the education sector to tackle the issue of stress related ill health amongst teachers. HSENI has already participated in the NASUWT conference held in Belfast, with an advisory stand for the teacher delegates.
7. At a strategic level, HSENI will be engaging with other stakeholders through the further implementation of the long term Northern Ireland Working for Health Strategy. This second phase of this strategy which embraces all work related health issues including mental health will commence in October 2007. How great an impact the strategy will make will be dependent on the outcome of the Comprehensive Spending Review.
8. In addition HSENI is proposing an initiative called “Safestart-NI” which is aimed at school leavers in the 15 to 18 year old age group with the intent of providing knowledge and skills for young people entering work for the first time. This programme will build capacity and self esteem amongst the very young people who unfortunately account for increasing numbers of suicides. This is also subject to successfully obtaining funding under CSR07.
9. In conclusion HSENI is not in the front line when it comes to tackling the issues of suicide and self harm. However the work that it can do within a workplace setting may well lessen or reduce the likelihood of employees going on to self harm or suicide if they enjoy a working environment that fosters well being.
Kevin Toner
Deputy Chief Executive
HSENI
11th October 2007
Professor Kevin Malone, MD, FRCPI, FRCPsych.
Thank you for your invitation to submit memoranda in relation to the Committee Inquiry into the prevention of suicide and self-harm. I come to the problem of suicide in Ireland following 20 years of research in suicidal behaviour including suicide in the US in the 1990s, and having been appointed as Professor of Psychiatry in the School of Medicine and Medical Science in UCD since 2002.
Research
Since my return to Ireland in 1998 I have established a North-South Suicide Research Programme called the Ireland North-South Urban Rural Epidemiologic Collaborative Study of Suicidal Behaviour and Major Psychiatric Disorders (the INSURE Project). Over the past six years this project has interviewed over 1000 sufferers from mental illness with varying degrees of suicidialty affiliated with their condition. These clinical interviews took place both in outpatient clinics (Study 1), as well as in emergency departments (Study 2) in six locations on the island of Ireland, including Dublin, the Midlands, Ballinasloe, Letterkenny, Omagh and Belfast. This project was collaboratively designed with Queen’s University Belfast (Prof. Roy McClelland, Dr Chris Kelly and Dr Tom Foster). Study 3 of the INSURE study has taken place in the south of Ireland focussing exclusively on a psychological autopsy study of Lives Lost to Suicide in Ireland in the past three years. We have currently interviewed the families and friends of fifty suicide deaths since our project started in earnest in January 2007, and we anticipate that we will have interviewed seventy families by the end of the year.
UCD Research
The Suicide Research Programme we have developed here at University College Dublin in collaboration with other institutions nationally and internationally includes three major strands:
i. Clinical and Applied Neuroscience, including molecular genetics and functional brain imaging. This strand focuses on neurobiological studies of suicidal depression, understanding brain pathways and genetic regulation of impulsivity and restraint and with impact on mood disorders and the emergence of suicidal behaviour.
ii. Clinical epidemiology, randomised control trials and health economics: this strand focuses on many of the aspects of the INSURE Project. As well on the clinical epidemiology side we have completed a study of all drownings in Ireland in the past five years, as well as all railway suicide deaths in Ireland in the past twenty years. Preliminary findings from these projects were presented at the recent IASP Conference in Killarney and further information will be provided on request.
Continuing with epidemiology we have a link with the DETECT Project, First Episode Psychosis, which is being led by Prof. Eadbhard O’Callaghan. This study is of a group at obvious increased risk for suicide in the first episode of their psychotic illness.
Health Economics is an under-researched area in relation to the problem of suicide and we have linked up with our economic colleagues in the Geary Institute at University College Dublin (Prof. Cecily Kelleher and Dr Liam Delaney) to study economic factors associated with suicide in modern Ireland.
iii. Strand three is Community and Humanity. This strand focuses on the impact of suicide on communities and one of the foci of the Suicide in Ireland Survey. The unique additional component to this Suicide in Ireland Survey is the carrying out of the first ever Visual Arts Autopsy in parallel with the psychological autopsy enquiry. This has the added bonus of combining clinical science with arts and humanities research, and all the families we have interviewed have warmly welcomed it. The other unique possibility associated with the Suicide in Ireland Survey is the platform to study the occurrence of clusters and even in our first forty-six cases we have identified an additional forty-seven cases that more than likely were associated with cluster effects. Again, these preliminary data were published and presented at the IASP meeting in Killarney and can be shared in greater detail at your request.
PhD Programme in Suicide Studies
UCD is the first university in Ireland to put together a PhD Programme in Suicide Studies. We appointed our first PhD student in September 06 and we will be taking on a further two PhD students in January 2008. These three students are looking at very different components of suicide in Ireland and they will make a unique contribution to fourth level education in this regard. I believe this is one of the ways forward with regard to attracting new and talented researchers into the field.
All Island Approach
It has been my opinion since my return to Ireland in 1998 that an all island approach was required to the research of the problem of suicide and deliberate self-harm in Ireland, and particularly the problem of suicide. It was for this purpose that I established the INSURE Project. This project has a wealth of data, which unfortunately we have not had the funds to properly analyse. We presented the first poster on the Year 1 data from this project at the IASP Conference in Killarney and this can be provided to your Committee, if it is desired. The advantage of the INSURE Project is that our research areas straddle the border counties and also urban and rural sites in both Northern Ireland and in the Republic, and also include areas of significant deprivation such as the border, midlands and west. The major drawback to not being in a stronger position with regard to new knowledge from these projects has been the lack of resources and also lack of sustained resources over time so that properly planned studies can be implemented.
Northern Ireland Research
Dr Tom Foster in Northern Ireland conducted a psychological autopsy study in 1994 of all suicide deaths in Northern Ireland. Whilst that is only twelve years ago things have changed dramatically on the island since that time and I believe there is significant merit in considering an all island psychological autopsy study, particularly of young suicide deaths under the age of twenty-five. Dr Tom Foster is ideally placed, and trained from an expertise point of view, to lead this study in Northern Ireland and I would be happy to continue leading this study in the South. However, I firmly believe if a research programme is to be successful it requires guaranteed resources for a specific period of time, rather than wondering from one year to the next whether or not funding will be sustained. These studies are labour-intensive, they are hugely rich in terms of the data they can provide, and I have adopted a case control designed to my protocol, as recommended by the International Association for Suicide Research in New York in 2006, and this strengthens the methodology considerably.
DSH
I am sure you will have had input from the National Suicide Research Foundation in Cork and their experiences with the National Parasuicide Register, which obviously is providing new data on deliberate self-harm more so than of suicide. Nevertheless, it is a valuable resource that probably should be extended on an all island basis. There are some problems with that Register that may require ironing out before it would be considered compatible for the entire island.
Mental Illness
All the international studies clearly demonstrate that a significant component of suicide deaths are associated with varying degrees of mental illness. To my knowledge in the Republic, there has been no proper audit to date in terms of exactly what statutory and voluntary services are available for (a) people (especially young people) with emerging mental illness and (b) particularly those in suicidal crisis. Whilst documents like “Vision for Change” and “Reach Out” are government policy documents here in the Republic, there is no sound, solid foundation to say “here is our starting point, this is what we have, this is what we do not have, this is what is available, this is what is not available, and here is what is available in part of the country A versus part of the country B”. Nor is there any real meaningful client feedback services or data, which is a real shortcoming in health strategy.
International Lessons
Much can be learned from the response to suicide statistics in other countries. For example, Finland has experienced a significant reduction in suicide deaths over the past fifteen years. Their approach was extremely methodical and focused particularly on early recognition of treatment of depression and alcohol problems, as the major planks of their strategy.
Schools
Much has been written and spoken about “going into schools” despite any robust data to indicate that this may be effective. I hosted a two-day Dublin International Workshop on Youth Suicide on 25 and 26 August 07 in the Royal College of Physicians where over twenty leading youth suicide experts presented their findings from around the world. We are currently writing up the proceedings of this Workshop and hope to publish it in a major international journal. One of the sessions, however, was on school-based interventions and Prof. David Schafer from Columbia University New York had very little confidence in the effectiveness of school-based intervention, as opposed to case finding studies in schools, which is a very different approach.
NOSP
I am an advisory board member to the National Office of Suicide Prevention and I am aware that your office in Northern Ireland has been in close consultation with the national office here so I will not cover that territory in this submission.
Large Scale Intervention Projects
An all island approach will also be necessary for large-scale intervention projects designed to demonstrate effectiveness in reducing suicide rates. Such studies have been effective in other countries such as Hungary. Further information can be provided on this if necessary.
Advocacy
In 2002 I co-founded the charity, 3Ts (Turn the Tide of Suicide) with Irish businessman, Mr. Noel Smyth. Over the past five years we have aimed to increase awareness of the problem of suicide and also to raise funding to support existing voluntary agencies on the ground around the country who are involved in suicide intervention, prevention and postvention. As you are probably aware, there are at least three hundred voluntary organisations dedicated to various suicide awareness and prevention projects in the Republic. The 3Ts has aimed to pull many of these charities and voluntary organisations together under a united umbrella, The Action on Suicide Alliance, and so I have forwarded your correspondence to the Chairman of the 3Ts, Mr. Noel Smyth to provide feedback to you on the activities of this charity.
Summary
I do believe, in summary, and based on what I have outlined above that we have a unique opportunity to build an all island research education, intervention and prevention programme right across the communities that will be inclusive as opposed to exclusive, and that with sufficient and sustained resources and planning we could emulate the success of our neighbours in Finland and Denmark, for example, who have seen their suicide rates decline between 20% to 40% in the last two decades through targeted, dedicated, and well-resourced strategies, programmes and projects led from within communities and facilitated by devoted national leadership.
Young at Art
We have received information about the inquiry via the Youth Council for Northern Ireland and would submit the following for consideration.
It is our organisation’s mission to make the lives of children and young people as creative as possible through engagement with the arts. As such we are committed to supporting and protecting children and young people and support the NI Assembly and its committees in pursuing any cross-departmental strategy that reduces suicide and self-harm.
In our experience over ten years of working with children and young people across Northern Ireland, we feel that the success of any future strategy is dependent on cooperation between all departments. We also believe that coherent structures for communicating that strategy to and between grassroots organisations are vital.
We would strongly advocate investment in existing resources and structures to tackle the causes of suicide and selfharm – low self esteem, lack of opportunity, limited education and employment opportunities, limited access to mental health support, lack of communication and interpersonal skills, sectarianism and bullying. We would advocate planned and negotiated longterm investment with existing structures over and above the creation of shortterm posts to address this issue.
As an arts organisation, we believe that creative activities have a key role to play in supporting personal skills development and promoting the issues around suicide and self-harm. Key strengths of the arts in tackling these topics are:
- The ability to explore sensitive issues at a safe distance through drama, performance, literature, film and the visual arts
- The ability to engage with young people in ways that interest them – through music, design and live events
- The opportunities to articulate one’s feelings in ways other than speaking – projecting them visually and non-verbally
- The opportunity to build social support networks through arts activities and groups, filling a gap that often opens in young people’s lives when they are experiencing any mental trauma.
The arts have been proven in supporting the rehabilitation of young people following trauma both in Northern Ireland and across the world. Live theatre and film have been used in an educational context to examine and raise awareness of a range of personal health and emotional wellbeing issues among young people with very positive results. As such we would request that consideration be given to creative and cultural activities as a part of the framework for tackling the ongoing difficulties experienced by young people in Northern Ireland.
Specific examples are the work undertaken by our organisation with Amnesty International to both raise awareness of children’s rights and support alcohol free activities for 16 – 18 year olds and our work to promote physical health among parents of very young children; the work of Replay Productions in collaboration with the Health Promotion Agency, DHSSPS and RoSPA to develop touring theatre programmes on personal safety, sexual health, suicide and anger management and drug awareness; the work of Belfast Community Circus with young offenders since the 1980s; the work of Wheelworks in a range of disadvantaged communities to address anti-social behaviour, sectarianism, racism and to support the needs of Section 75 groups.
We welcome the opportunity to contribute to any further consultations.
Ali FitzGibbon
Director
Mr Chris Smallwoods, Regional Manager, The NEXUS Institute
Suicide is indeed an emotive and sensitive subject and from the experiences of The NEXUS Institute in relation to our specific client base the reasons for attempting or successfully carrying out the act would likely be very much related to the suffering which may have been caused by the individual having been subjected to prolonged childhood sexual abuse or even rape/violent sexual attack.
In relation to the implementation of effective interventions the NEXUS Institute has carried out research into the value of counselling services in dealing with the impacts of childhood sexual abuse and rape. Sixty three clients participated in the study and completed a questionnaire during 20 / 30 minute telephone interviews conducted with Nexus counsellors.
The biographical profile of participants was 92% (58) of the sample were female and 8% (5) were male. What is worthy of note in terms of this related subject was that 59% (17) of cases, related to mental health issues.
The personal aims which clients had for undergoing counselling included feeling better, greater understanding, learning to cope, reclaim their lives, and increase their self confidence and esteem.
The two most common goals were “to feel better” (21%) and to achieve “greater understanding” of the reasons why they were victimised and how this had affected their lives. (19%). Thirteen people stated that they wanted to feel better, particularly from depression or suicidal ideation.
It did become apparent that the majority of respondents were struggling to cope with the emotional, cognitive and social sequelae of their abusive experiences. Eleven percent (7) stated that they were depressed to varying degrees, i.e. some stated that they were seriously depressed and two people reported having attempted suicide and another experienced panic attacks. The inability to cope with their emotions such as feelings of guilt or shame, along with intrusive memories was a common problem.
Overall, whilst many perceived themselves to have experienced high levels of difficulties prior to counselling, they also felt that having undergone counselling, they observed significant improvements immediately after and at 6 months after counselling. Arguably, the most worrying statistic is that prior to counselling, 66% (29) of all of the individuals who participated in the research felt suicidal before receiving any help at Nexus. Fifty percent (29) strongly agreed with this statement and 11% (5) agreed, with another 11% (5) undecided. Immediately after counselling, only 2%, which represents one person still considered themselves to be at high risk of committing suicide. However, another 16% (7) agreed with this statement and therefore were still at risk of ending their own lives. However, six months after completing their counselling with Nexus, 14% of clients experienced a desire (14%, 5) to commit suicide. It is encouraging to note that none of the clients expressed a very strong desire to commit suicide, which would suggest that the intervention of counselling was successful in helping to reduce or in some cases eliminate suicidal ideation.
They also reported a decrease in the reliance of potentially risky coping tools such as the consumption of alcohol, self harming and even suicide. There was also an increase in the use of more positive strategies, such as reframing negative thoughts and emotions through talking about it to a supportive person, which were taught as part of their counselling courses. Many clients also attributed their difficulties to their poor health or specific health problems and a few commented that since undergoing counselling their mental and emotional health had improved. One individual commented that the progress they had made was “remarkable” and it was imperative to their mental health.
However for counselling to be effective it cannot be taken as a ‘stand alone’ intervention where there are serious mental health concerns but should be supported by meaningful mental health professional back up, particularly so when the client has entered into the counselling process and it is highly probable that many traumatic and frightening memories will re-emerge and thus impacting on the overall state of that clients vulnerability and mental health. In terms of my project there have been instances when clients have had to be denied access to counselling because those resources could not be put in place by the mental health teams of the region, which I was advised was due to a lack of resources (CPN’s). However a model of good practice does exist in one outreach site where there is a solid and effective working relationship between the counsellor, client and mental health resource which works very effectively.
From the experiences of both the agency and our client base what does stand out is the recognised need for an increase in awareness for men about the many obvious benefits of ‘Therapies for Men’ in terms of the counselling intervention. There is clear evidence to indicate that men suffer from emotional distress and that they will seek counselling only half as often as women which is particularly the case within the areas of male sexual abuse and rape. Our own statistics highlight a gender delivery of 82% female and 18% male, these figures would not be representative of reported abuse and rape incidents but it would be fair to say that the comparison of those seeking help against the likely levels of reported and unreported abuse would indicate that there is a definite reticence amongst males to come forward and seek counselling help.
In relation to training and development within our specific work area all our counselling staff are qualified and if not already in receipt would be working towards accreditation of an approved body such as BACP. It is also our intention that all counsellors and secretarial staff (first point of contact for clients) would have attended the well advertised and available ASIST courses.
Whilst The NEXUS Institute is both established and recognised as the leading agency in terms of providing support and being an accessible part of a support network in local communities for those who have suffered sexual abuse or rape there continues to be instability and uncertainty around the issues of both appropriate and secure funding and it is felt that this needs to be resolved as a priority.
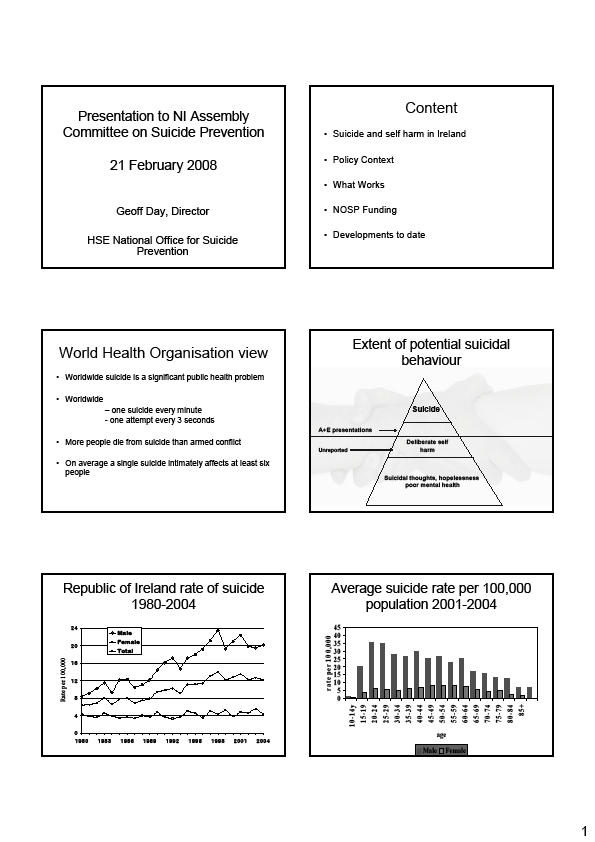
National Office for Suicide Prevention
Evidence to the Committee for Health, Social Services and Public Safety – Northern Ireland Assembly – Committee Inquiry into the Prevention of Suicide and Self Harm
1. Background:
Reach Out the National Strategy for Action on Suicide Prevention in the Republic of Ireland was launched by the Minister for Health and Children, Mary Harney TD in September 2005. The report followed extensive public and organisational consultation and was approved by both the Department of Health and Children and the Health Service Executive jointly.
Reach Out has 26 Action areas and 96 actions to be taken over the 10 year span of the strategy. Dividing the actions into General population and specific targeted areas follows the World Health Organisation suggested approach and this is noted in other countries strategy documents.
In order to provide a focus for implementation the HSE established the National Office for Suicide Prevention (NOSP) within the Population Health Directorate in September 2005. This Office has national director and currently 5 staff members. The Office has established a national advisory group of people with expertise in the field of self harm and suicide and an annual forum of all interested parties. The office has its own web site www.nosp.ie and links to the HSE web site and those of the key voluntary organisations.
The HSE is required by legislation, the Health (Miscellaneous) Provisions Act 2001, to submit to the Houses of the Oireachtas, an annual report on the actions taken in the previous year to prevent suicide. A copy of the report is enclosed and will also be available soon on our web site.
2. General Response:
Protect Life – The NI Suicide Prevention Strategy has taken a similar approach to our own strategy and therefore many of the actions are compatible in terms of implementation. Funding to deliver the elements of the strategy is key. In our experience such investment needs to be significant, targeted and sustained over time.
The National Office has worked with colleagues in the DHSSPSNI and the HPA to agree an all island action plan on suicide prevention. This plan is the basis for joint actions across the island. A copy is attached. Most significant has been the work around awareness campaigns in the media, the most recent being the launch of a new TV/radio advertisement in both jurisdictions.
There are substantial advantages to joint working not least the cost effectiveness of combining resources and not re inventing actions already taken. We can learn from each others experience of implementation, indeed we can and are learning from our UK and world wide colleagues. The successful joint funding of the recent World Congress on suicide prevention held in Killarney has enabled us to achieve jointly a high profile for suicide prevention in Ireland.
Additionally we have established a 5 nation’s strategy group comprising Northern Ireland, Republic of Ireland, Wales, Scotland and England
a) Assess the scope and appropriateness of the Department’s Strategy – Protect Life
The Strategy is set for a period of 5 years which in our view is sufficient for implementation and monitoring of progress to establish if a reduction in suicide levels can be achieved. Ongoing evaluation of individual programmes is necessary and all NOSP projects are asked to establish evaluations the intensity of these being related to the sum of funding involved and the capacity of the organisation concerned. Reachout has been in place for just over 2 years and we are now about to commission an independent evaluation of progress so far with the strategy and the operation of NOSP. We would recommend that Protect Life adopts a similar approach.
Protect Life sets clear targets for reducing suicide levels. While we originally did not set targets due to concerns over the reliability of data we have now done so even though the recording of suicide data is still a concern. We have taken the view that a target does allow us all to focus our efforts and be accountable for actions taken. As well as setting a target recently for reduction in suicide we have also set a target for the reduction in the rate of repitition of self harm
b) Examine the level of stakeholder involvement
A central part of the work of NOSP has been the engagement with other stakeholders namely, those bereaved through suicide, voluntary organisations at local and national level working in this area, professional bodies, and statutory organisations. We use a national forum every year to meet with all those on our extensive mailing list who have an interest in this area. The Forum is designed to provide information about the work of the NOSP, discuss recent evidence based initiatives and consult with stakeholders on future direction.
We have been impressed by the work of the Families Forum in NI and whilst we have similar families groups in the South they do not yet meet together as a national grouping. There is an opportunity in the future to establish an all island network of bereaved families
c) Examine the level of services and support
Whilst it is difficult to comment on individual services in NI we would state that it is important to develop services and supports across the spectrum of the strategy, from health promotion to postvention. We have tried to use our limited additional resources in this way although it does often mean that service development can be constrained and slow to progress.
We have been encouraged by the willingness in NI to take some of the initiatives already underway in the South e.g. self harm registry data collection, media watch, to develop all island coverage. We have worked together on mental health awareness campaigns and the world congress on suicide prevention. We will be further examining initiatives in NI which we can adopt in the South
d) Consider what further action is required
Cross border co operation to date has been effective with good working relationships with both the DHSSPSNI and the HPA. It would be helpful if there was similar organisation to the NOSP in NI as this would allow for one contact point for this office. Also in our experience the establishment of the office has provided a national focus for all our initiatives as well as a central coordination role. For government it provides a single channel through which Dept of Health and Children funding and policy monitoring can take place. We would urge you to establish a team within the health/ social care statutory set up to undertake this work. The objectives of the NOSP team are
- oversee the implementation of ReachOut
- commission appropriate research
- coordinate suicide prevention activity
- consult widely and regularly with interested organisations
Additionally we have found that the statutory obligation on the HSE (through NOSP) to report to the Houses of the Oireachtas on suicide prevention activities in the previous year has been helpful in focussing our efforts. We produce an annual report for this purpose which is available on our website (hard copy enclosed)
We would support the extension of the current all island suicide prevention action plan for the delivery of practical actions to prevent suicide. In our view there is no need to change the current strategies north and south, but it is important that we continue to work together and evaluate, jointly if possible, the impact of the actions/recommendations set out in the two documents.
Geoff Day
Director
HSE National Office for Suicide Prevention
15.10.07
All-Ireland Suicide Prevention Action Plan – Position Paper
1. Training
2. ROs and Coordinators meetings
3. MediaWatch/Volunteers/Guidelines
4. Men’s Health Forum
5. Registry of Self Harm
6. Suicide Data Collection Arrangements
7. Awareness campaign
8. CAWT
9. Implementation Groups
10. XXIV Biennial Congress of the International Association of Suicide Prevention
1. Training
Awareness Training
Opportunity: A basic awareness training programme in suicide prevention has been developed jointly by the HSE Resource Officers for Suicide Prevention and Suicide Awareness Coordinators in Northern Ireland. An opportunity now exists to assess the suitability for the roll-out of this awareness training to community groups throughout Ireland, north and south.
Delivery Partners: National Training Officer of the HSE NOSP (appointment is due) and possible designation of Awareness Coordinator in Northern Ireland.
Timeframe: November 2006 – ongoing.
Outcome: Common standardised awareness training delivery to communities north and south
Skills-based Training
Opportunity: Both jurisdictions have a number of trainers in the ASIST (Applied Suicide Intervention Skills Training) Programme and an evaluation tool is currently being developed. It is recommended that a common evaluation tool is utilised for all ASIST workshops throughout Ireland.
Delivery Partners: NOSP Assistant Research and Resource Officer and designated ASIST Training coordinator in Northern Ireland.
Timeframe: November 2006 – ongoing.
Outcome: Programme evaluation to inform future skills-based training needs.
2. Resource Officers and Awareness Coordinators meetings
Opportunity: The third cross-border meeting of Resource Officers for Suicide Prevention and their Northern Ireland counterparts took place in Monaghan in April, 2005. It is recommended that this meeting be continued as an information-sharing meeting.
Delivery Partners: HSE Resource Officers and NI Suicide Awareness Coordinators with the support of the Department of Health, Social Services and Public Safety, and the National Office for Suicide Prevention of the Health Service Executive.
Timeframe: March 2007 and annually thereafter.
Outcome: Economies of scale in suicide prevention practices and programmes, information sharing and a cross-border peer support network.
3. Media Monitoring / Volunteer Programme / Media Training
Opportunity: A new media monitoring campaign, Headline, has just been launched as a partnership project between the NOSP and an alliance of voluntary mental health organisations in the south. Furthermore, as part of the implementation of the Reach Out strategy the NOSP plans to develop a panel of volunteers who have been affected by mental health issues and/or suicidal behaviour to respond to the media on these issues following training and with ongoing support. It is envisaged that the development of such a network of volunteers, both in NI and ROI, will facilitate access to media training courses and provide an incentive to editors and sub-editors to develop links with the NOSP, DHSSPS and other partner organisations. It is proposed that the development of the campaign, the network and the media training should adopt an all-island approach as far as possible / practical.
Delivery Partners: Headline, NOSP, HPA, DHSSPS, NUJ, Association of Editors
Timeframe: Headline campaign - October 2006. Volunteer Programme and Media Training – June 2007.
Outcome: common messages and standardised safe reporting practices in relation to suicidal behaviour.
4. Men’s Health Forum
Opportunity: both Reach Out and Protect Life highlight male suicide as an area of particular concern, requiring dedicated and specific actions for prevention. The Men’s Health Forum in Ireland provides a unique vehicle to develop and implement such actions on an all-island basis. The Men’s Health Forum in Ireland (MHFI) is a voluntary network of individuals and organisations proactively highlighting and addressing key men’s health issues in Ireland, including mental health and suicide. It is proposed that we should consider appointing a mental health promotion and suicide prevention officer to coordinate suicide prevention activities for men throughout Ireland.
Delivery Partners: NOSP, DHSSPS and Men’s Health Forum.
Timeframe: March 2007 – ongoing.
Outcome: coordinated suicide prevention activities for men through a dedicated post.
5. Registry of Self-Harm
Opportunity: the National Registry of Deliberate Self-Harm was established in 2001 and reached full coverage of Accident and Emergency Departments throughout the south of Ireland by 2005. The Registry reports annually on the number and rate of presentations for deliberate self-harm in each hospital according to age, gender, method and type of care received. Service planning is informed by the Registry report. It is proposed that the Registry should be piloted, and then rolled out on a phased basis in Northern Ireland providing all-island data on self-harm.
Delivery Partners: National Suicide Research Foundation, NOSP and DHSSPS.
Timeframe: October 2006 (planning meeting), pilot site in Northern Ireland from January 2007.
Outcome: Comparative all-island data on self-harm to assist in evaluating current service provision models and plan future service developments.
6. Suicide Data Collection Arrangements
Opportunity: It is anticipated that the successful implementation of both Strategies will result in reduced stigma surrounding the issue of suicide, and this in turn will likely lead to an increased number of deaths being officially recorded as suicide. Such increases, while being an inevitable outworking of a successful implementation process, would make it difficult to report objectively on the achievements of our respective Strategies. The development of standardised recording arrangements would therefore provide us with the opportunity to make accurate and meaningful statistical comparisons with a neighbouring jurisdiction. The establishment of an Island wide confidential enquiry into deaths by suicide may provide us with the method for achieving this harmonisation.
Delivery Partners: DHSSPS, NOSP, NI Coroners Office, National Suicide Research Foundation.
Timeframe: November 2006 - Ongoing
Outcome: Standardised suicide recording throughout the Island of Ireland.
7. Awareness Campaign
Opportunity: Both Strategies highlight the need to develop major information campaigns which aim to de-stigmatise and promote positive mental health. The Health promotion Agency (HPA) in Northern Ireland has recently published details of extensive research into this issue, and it is intended that these findings will provide the basis for the forthcoming campaign in Northern Ireland. As both jurisdictions have a similar delivery timescale for their campaigns, an opportunity exists to share the research findings with NOSP and HSE with a view to developing a joint awareness campaign
Delivery Partners: DHSSPS, HPA, NOSP, and HSE
Timeframe: November 2006 – March 2007
Outcome: An agreed message being delivered across the many shared media outlets in both jurisdictions
8. Co-operation and Working Together (CAWT)
Opportunity: CAWT is a cross border body formed in 1992, and it currently operates within the North Western/Eastern HSE (ROI) and the Western and Southern HSSB’s (NI) boundaries. CAWT is dedicated to realising the full potential of cross border co-operation in Health and Social Care in order to improve the well-being of the resident population. The potential therefore exists to expand the number of projects managed by CAWT and to enhance its Health and Social Care co-ordination role in the border regions, and potentially further afield.
Delivery Partners: SSIB, CAWT, NOSP, HSE and DHSSPS
Timeframe: November 2006 – Ongoing
Outcome: The provision of standardised and seamless Health and Social Care services in the border regions, and potentially further afield.
9. Implementation Groups
Opportunity: Implementation of the “Reach Out” and “Protect Life – A Shared Vision” Strategies is at a similar stage, and close co-operation and information sharing already takes place between the respective implementation bodies in both jurisdictions. The opportunity exists to formalise this co-operation by offering reciprocal membership of the Suicide Strategy Implementation Body (NI) and the National Advisory Group (ROI) to the NOSP and the DHSSPS respectively. .
Delivery Partners: DHSSPS, NOSP, SSIB, and National Advisory Group.
Timeframe: October 2006 – Ongoing
Outcome: Enhanced information sharing in relation to the implementation of the respective Suicide Prevention Strategies.
10. XXIV Biennial Congress of the International Association of Suicide Prevention
Opportunity: The XXIV Biennial Congress is being hosted by the Irish Association of Suicidology (IAS) in Killarney, from 28 August 2007 to 1 September 2007. The congress is a major international event and it is anticipated that it will attract between 400-500 delegates. There will be a major symposium on Suicide Prevention in Ireland, North and South, during the congress, and this will allow us the opportunity to showcase the implementation of both Strategies to an international audience.
Delivery Partners: IAS, NOSP, DHSSPS, HPA.
Timeframe: November 2006 – September 2007
Outcome: Evaluation and testing of the implementation process for both the “Reach Out” and “Protect Life” Strategies against an international audience.
Ulidia Integrated College
Before I begin, I wish to ask for clarification concerning ‘Protect Life: A Shared Vision’ – Preventing Suicide Actions in the Promoting Mental Health Strategy and Action Plan, Annex 1, Page 67.
I quote,
“Action 21: DE and DEL in partnership with Education and Library Boards, Schools, Youth Council for NI, HPA and HSS Boards will implement programmes on awareness of suicide for teachers and youth leaders.
Target Date: April 2004
Objective: Achieved.”
I am at a loss - as a teacher - to know what Action 21 is or what it accomplished. I would like to discover how many teachers know anything about it. Certainly everything I have learned in relation to suicide, I have learned through my own initiative. How has this Action been “achieved”?
My Response
I wish to respond to the committee in two sections:
- Counselling in Schools
- Effective Teaching concerning Mental Health Issues in the Classroom
I fully support improved links between education and health. The Health professionals I have met are very approachable, such as Colm Donaghy, Chief Executive of the Southern Area Trust and Head of the Taskforce into Prevention of Suicide, in Northern Ireland. However, the Department of Education remains aloof and bureaucratic.
I think the approach to Mental Health in schools needs to change dramatically. The Department of Education needs to speak with principals and teachers rather than be cut off from schools and unresponsive. Whilst great things may be afoot behind closed doors concerning this issue, schools are not made aware of them, nor are teachers included in the process.
Counselling
All schools have a Pastoral Care System; some are more effective than others. The Pastoral Care Coordinator is usually at Vice Principal or Senior Teacher level. These senior teachers administer the pastoral care system and ensure that the procedures are followed. However, they are not and should not be counsellors. A pupil cannot be expected to bare his soul to someone who may have to teach him the next day and perhaps reprimand him for not having a homework done. Counsellors should be independent, and should have a different and very productive relationship with pupils, which is wholly pastoral.
This year, commencing September, 2007, Contact Youth has been awarded a contract to offer counselling in schools. Many people not involved in education greeted this news with delight. Counsellors in every school! Wonderful! However the reality is very different. This is at most a token gesture.
It is my understanding that some schools may have a Contact Youth counsellor for one – three hours, at most once a week. Other schools have NSPCC counsellors who work part-time in schools, for a few afternoons /mornings and have had these counsellors for some years. A very few schools have full-time counsellors.
The fact is all schools need a counsellor present, every day, solely responsible to the pupils in that school.
The cost of such counselling would be worthwhile on two counts:
- the human right to a healthy, happy life
- the resulting reduction in mental health problems among the adult population in the NHS.
When pupils experience problems, these should not be deferred until a counsellor happens to come into the school, if one does come. Problems need dealt with as these arise. Problems which are not addressed grow and cause great unhappiness in adulthood and can profoundly affect the next generation of children, born to a parent with a mental health problem.
‘Protect Life: A Shared Vision’ – Annex 4, page 79 - states that “Research has shown that a psychiatric disorder is present in around 90% of suicide victims.” (Cavanagh et al 2003).
I believe that young people often lack the strategies to cope with situations such as death, broken relationships, et cetera, and that if their problems are not resolved or if they do not get help, they can become more deeply depressed. Many distressing problems can arise from poor parental skills and these can have devastating effects on the children. I would like to see more research done about psychiatric disorders and whether these result from long-term depression, arising from lack of coping strategies. Often a counsellor can advise pupils how to cope with the difficulties they encounter if she is accessible when the pupils need her.
I hope the provision of a few counsellors in some schools for a few hours does not lead to the Department of Education ticking the box ‘counselling in schools - done’ and forgetting to expand and improve the system.
The target should be to employ a counsellor in every school, primary and secondary, during term times only.
Moreover, effective research needs to be carried out, costing done and projections made on the savings counselling would bring in relation to the NHS and expenditure on mental health issues.
I would like assurance that this research will be done urgently, if it is not already underway.
It is also my understanding that when the provision for Contact Youth counsellors was introduced, the counsellors reported directly to their supervisors and not to the Headmaster or Child Protection Officer in the school. I think this has been redressed but why was it not foreseen? All counsellors should have to report to the Headmaster/Child Protection Officer where a pupil has disclosed self-harm, abuse or where suicidal thoughts have been expressed. No pupils should be allowed to leave school without their safety being safe-guarded by a responsible adult.
Counsellors in schools often have limited access to senior management and can work on the periphery of school life; they can be hidden away if the principal stigmatises Mental Health, and their counselling rooms can be very small and barren. Such attitudes and conditions must be redressed urgently. Tokenism will not suffice to bring about the changes in attitude and provision necessary to secure a high standard of mental health care in Northern Ireland.
Pastoral Care and Counselling in Ulidia Integrated College –
A Model of Excellence
In my school, Ulidia Integrated College, in Carrickfergus, we have a full-time counsellor paid for by the college. She works from 8.50 am – 4.00 pm, or later if the need arises.
Our counsellor dislikes the term ‘counsellor’ and she is known as the ‘Student Support Officer’ as this enables pupils to realise that their visits to her can be about little issues, not just a major crisis in their lives. Pupils can drop in for a chat at break time or over lunch time or arrange appointments during class time for 35 minutes on a one-to-one basis, weekly or fortnightly depending on their need.
The room used by the Student Support Officer is known as the Group Room. It is warm, bright and colourful, with posters and leaflets on the wall about counselling issues and help-lines/organisations. There are books and leaflets available about organisations that can assist pupils. There are plants in the room, a carpet and three green leather settees; the blinds on the windows allow pupils to see out but not into the room. The Group Room is situated opposite the Resource Centre and the foyer the rooms share has comfortable chairs and bright, colourful posters on the walls.
It is an area of the school that is safe, quiet and well used. Few pupils mind anyone seeing them talking with our Student Support Officer because it is the norm to do so.
Our Student Support Officer is well qualified and extremely well respected by the teaching staff. She has a key role in the college and meets regularly with the Pastoral Care Coordinator and the Heads of Year. She is the designated Deputy Child Protection Officer in the school. (The Vice Principal is the designated Child Protection Officer.) She attends Senior Management Meetings and has input into management decisions as she is the person with most knowledge concerning the welfare of the 530 pupils in the college. This involvement at management level is probably unique and illustrates the importance attached to her role by the Headmaster.
‘Protect Life – A Shared Vision’ – page 42 – states that all schools should protect children from bullying and Health and Social Services’ Trusts should have a buddying/mentoring type scheme in place by 2008.
Our Student Support Officer has trained and worked with Childline. She has introduced a Mentor Scheme into Years 13 and 14 and these pupils receive training from Childline. They are able to mentor Year 8 and 9 pupils and help them resolve the difficulties they face or else direct these pupils to seek appropriate assistance from staff or parents. The Sixth Form pupils love being mentors and see it as a badge of honour; it is not available to all Sixth Formers. Pupils must be appropriate in their attitudes and dedication to others. The Student Support Officer picks the mentors. They are trained (as are all teachers and staff in schools in Northern Ireland), in Child Protection and they know that a pupil cannot be offered confidentiality when they could be at risk of harm from themselves or from others. They report directly to the Student Support Officer if a pupil discloses something of concern - as do all staff.
The Headmaster, the Pastoral Care Coordinator, the Student Support Officer and the staff and pupils at Ulidia Integrated College have created a whole school ethos which is anti-bullying and every class room displays an anti-bullying poster created by the pupils. This gives pupils ownership of the ethos and, as we are an integrated college, all pupils are aware of avoiding terminology that is racist or bigoted. Our mission statement is: ‘Educating together, Catholics and Protestants and those of other religions, or none, in an atmosphere of understanding and tolerance to the highest academic standards.’ This whole-school ethos is essential in every school. It is fostered by discussing issues openly in an atmosphere of tolerance. Too many schools avoid discussing controversial issues, thus restricting pupils’ ability to expand their thinking.
At Ulidia, the Headmaster takes the four Year 8 classes for ‘Ulidia Studies’ and they discuss issues that are in the news or which arise naturally and interest them. On one occasion a Year 8 pupil was speaking with the late Mo Mowlam while she visited the school, and he told her that he had discussed disarmament in Northern Ireland in Ulidia Studies. She was most impressed! Of course, the point is that pupils who feel that their opinions are valued and respected don’t bully or tolerate bullying behaviour in others. All pupils in Ulidia know that any signs of bullying will be dealt with and never ignored.
The Education and Training Inspectorate said of the college in 2007,
“There are significant strengths in many aspects of the arrangements for pastoral care and child protection, which include:
- the well resourced and high quality counselling service;
- the effective Students’ Council;
- the well-embedded anti-bullying programme; and
- the effective mentoring system.”
Some of the college’s teachers and the Student Support Officer have been involved with Drugs’ Awareness days with the PSNI and our pupils designed the Hate Crime leaflet used by the PSNI. These links foster respect and cooperation with the police and the counsellor also liaises with various external bodies regularly, such as CAMHS, NEXUS, NSPCC, Childline, social workers, hospitals, local GPs and Clinical Psychologists.
Our Student Support Officer attends the Year 8 Residential which welcomes Year 8 pupils to the school. She gets to know these pupils well and can anticipate difficulties that could arise, often preventing these occurring. Pupils find her friendly and approachable and trust her. It is her accessibility and the bond of trust that makes having a full-time counsellor so important. Many parents also find solace talking with her when she meets with them to discuss difficulties their children are facing.
The college has produced three leaflets in liaison with the Student Support Officer: ‘SPLAT’; ‘Need 2 Talk’ and ‘Need 2 Talk: Self-Harm and Suicide’.
The ‘SPLAT’ leaflet is about the activities which take place in the afternoon club known as SPLAT. This is a fun club organised by the Mentors for Years 8 and 9. Pupils can also do home works at this club.
The ‘Need 2 Talk’ leaflet is for all pupils and it explains the importance of discussing worries before these overwhelm the pupil and it gives contact web sites and telephone numbers of help lines. It also gives the Student Support Officer’s E-mail address for pupils who do not want face-to-face contact.
‘The Need 2 Talk: Self-Harm and Suicide’ leaflet is given to those in need and gives helpful websites and telephone help-lines. It also gives the Student Support Officer’s E-mail address, and she would keep in close contact with any student at risk.
It is definitely the case that where the Student Support Officer has been made aware that a pupil is self-harming or that a pupil has had suicidal thoughts she has made a positive contribution to the pupil’s welfare and has definitely deterred pupils from ending their lives. Unfortunately it is not always possible to save every life, but schools have a duty to try, as does the whole of society. Our Student Support Officer is keen to set up a PIPS Project in our area to help prevent suicides as five children that we know of have taken their lives in the NE Antrim area in the last two years.
Ulidia Integrated College was very pleased to learn of the strategies the Ulster Hospital has in place for those who are suicidal and we have had Alan McIntosh (in charge of the 24/7 Crisis response Unit at the Ulster Hospital), to our college. The strategies available at the Ulster Hospital’s A&E for those self-harming or at risk of taking their own lives has led to the inclusion of suicide prevention strategies in
A&E departments in the workbooks I have introduced into Year 11. (More about this will be discussed in the next section under Education concerning Mental Health Issues in the Classroom.)
The Student Support Officer and I have attended ASIST Training in suicide prevention which was most informative and I believe strongly that every school should have at least two representatives who have undergone such training.
We strongly support the training of GPs in this area and the attendance of more teachers at conferences discussing issues such as Sexual Violence, Women’s Aid, Suicide and Self-Harm Prevention; et cetera. It is very sad that there are many workshops on mental health in England and on other issues of interest to teachers, but these are not held in Northern Ireland. This should also be redressed.
We are aware that some schools believe they have no need for a counsellor and I can only feel deep disappointment for the lack of support they must offer their pupils. With increasing family break-up and increasing pressure on families, with both parents working or a single parent working, and with increasing mental health issues in society, the need for counselling will surely escalate.
Effective Teaching concerning Mental Health Issues in the Classroom
I teach GCSE Home Economics Child Development which includes:
- Contraception
- Conception
- Pregnancy
- The Role of the Father
- The Birth
- Caring for the Baby for the First Five Years
- Parenting Skills
I find this to be an invaluable subject for the pupils and I wish all pupils had an opportunity to study this subject.
I also teach the new GCSE called ‘Learning for Life and Work’. I teach the strand called ‘Personal Development’ which is now compulsory for Year 11 pupils, though not necessarily as a GCSE examination subject. At present, ‘Personal Development’ at GCSE level does not incorporate parenting skills which would be immensely valuable to many pupils who have poor role models, if any role model.
It does incorporate:
- “Self awareness which provides opportunities to consider the importance of self-confidence and self-esteem to physical and emotional/mental health;
- Personal health which provides opportunities to understand the importance of recognising and managing factors that may influence physical and emotional/mental health;
- Relationships which provides opportunities to understand the importance of forming and maintaining relationships to physical and emotional/mental health.”
This is quoted from an excellent CCEA document: ‘Guidance for Coordinators and Teachers of Personal Development’ and it also states that “More than any other institution, with the exception of family, school has the potential to shape and nurture the skills, well being and potential of our young people in Northern Ireland.”
I thoroughly agree with this statement.
I am delighted that Mental Health has been introduced into schools. However, the emphasis is on self-esteem, and the issues of self-harm and suicide prevention have not been high-lighted.
I am teaching this subject to Year 11, including prevention of suicide and self-harm, (despite time restraints), because these issues are too important to ignore. I believe that these elements of Mental Health should be taught in all schools to Year 11 pupils and be mandatory. Only teachers who are committed to delivering such a message without stigma or prejudice should undertake to do so. Training in the ASIST programme would be superb for these teachers.
My pupils have responded very well to the lessons and they have learned a few key facts that could potentially save lives in the future:
- How to recognise trauma and how to access help
- Why people self-harm
- Causes of depression
- How to respond to someone who is depressed
- What can lead people to consider suicide
- How to access help
- Agencies that can help
- Hospital A&E procedure for those who are suicidal
- Asking the person at risk if he is considering taking his own life
- Asking whether he has a plan in place
- Never keeping disclosures of suicidal thoughts confidential
- Always accessing help on the person’s behalf (as the person is no longer able to do so)
Such simple knowledge could be invaluable to the pupils at any stage in their lives, and it could assist them to assist others.
I finish this submission with an invitation to the committee to visit Ulidia Integrated College and see the Student Support Officer’s room and meet with her, and to see the counselling and pastoral care system in action. The Headmaster would make you most welcome.
The Northern Ireland Commissioner for Children and Young People
1.0 Background
1.1 The Northern Ireland Commissioner for Children and Young People (NICCY) was established in 2003 under legislation of the same name. The primary aim of NICCY is to safeguard and promote the rights and best interests of children and young people.
1.2 Nigel Williams, Northern Ireland’s first Commissioner for Children and Young People, who died on 28th March, 2006, was vociferous in expressing his concerns about young people’s mental health needs not being adequately provided for in Northern Ireland. In February, 2005, NICCY hosted a conference which highlighted the issue of self harm and suicide and also displayed best practice in the area of prevention. Patricia Lewsley, appointed to the post of Commissioner in January 2007, has forcefully taken up this issue with the relevant government departments, and remains concerned about inadequate service provision for children and young people at risk of self harm and suicide.
1.3 In Autumn, 2005, NICCY ran a campaign entitled “Message to the Minister” whereby young people were invited to place messages on the NICCY website to be relayed to the Minister for Health, detailing views on how self harm and suicide could be dealt with. In February, 2006, a report of the findings was delivered to Minister Shaun Woodward, and a copy was forwarded to the Taskforce. We believe it is worth re-stating here, the difficulties that the young people highlighted with regards to the current arrangements for self harm and suicide prevention.
In the “Message to the Minister” exercise, the following issues were suggested by young people as significant aspects of developing a suicide prevention strategy:
- Consultation with children and young people regarding their needs and wishes.
- More counseling/support services that are accessible to, and appropriate for, young people. Particular reference was made to the need for localised and school based provision, the need for a 24/7 ‘crisis response’ service and the importance of professional and experienced staff working within these. Reference was also made to the benefits of peer-support and to the wisdom of utilising a number of different mediums for delivering information and services, including those of email and the internet.
- Increased public education and preventative initiatives.
- More mental health clinics, particularly those catering specifically for children and adolescents.
- Increased funding of both statutory and voluntary services.
- An overarching comprehensive strategy, which addresses need at the individual, family, community and societal level.
- A holistic approach that integrates families, communities, the voluntary and statutory sectors and those whose lives have previously been impacted by suicide.
- Uniform access to services across NI, in both rural and urban areas.
- Recognition of the good work that some organisations are currently undertaking within the field and the benefit of supporting and promoting such good practice.
- Difficulties identifying appropriate sources of advice and support.
- Unacceptable delays in accessing services.
- Inappropriate placement of adolescents in adult mental health units.
- Inappropriate incarceration of young people with mental health needs.
- Insufficient needs-focused training and education amongst professionals.
- Inappropriate responses from professionals approached for help.
- Continued stigma/negative societal attitudes.
- Under-funding of services resulting in continued insufficient service provision across the fields of education, health and social services.
1.4 NICCY submitted a response to the consultation document on the draft Strategy “Protect Life, A shared Vision”. The comments forwarded in that response are contained in this paper.
2.0 Context
2.1 NICCY is acutely aware of the complexity of issues surrounding young people who self harm and take their lives by suicide. It is important in our opinion to understand the context of the wider mental health issues in Northern Ireland as part of the challenge of developing a suicide prevention strategy. NICCY acknowledges that the strategy contained in Protect Life, could only be broad-brush in its approach and that the detail under each of the objectives would be significant in tackling the issues of self harm and suicide. However, having said that, if the underlying causes of self harm and suicide are not addressed, then the strategy will fail in reaching its target of suicide reduction.
2.2 NICCY responded to the CAMHS report as part of Professor Bamford’s Review, and highlighted the following areas for further consideration:
- Identification of the gaps in services is critical before remedial action can be taken. NICCY would welcome an exercise which plots needs with current service delivery. Clearly need is a changing occurrence, and a geo-mapping exercise of this nature could assist with prioritising planning of service delivery.
- While supportive of the 4-tiered approach suggested in the report, NICCY believes that there needs to be, in the first instance, leadership at Government level which would drive the development of a CAMH strategy. We believe this should be a key priority for the incoming Mental Health Tsar. NICCY is mindful of a number of key strategies being developed currently and sees the need to link a CAMH strategy with some of those key strategies, in particular The Children and Young People’s Strategy – which makes some reference to a prevention of suicide strategy; and a prevention/Family Support Strategy, which although not yet developed should have major consequences for children and young people’s mental health.
- NICCY also believes that an outcomes approach should be adopted in developing a CAMHs strategy which has measurable objectives.
- There is limited reference in the draft report to the resourcing of a comprehensive strategy. NICCY would suggest that prior to the final report a costings exercise is undertaken so that appropriate financial and staffing resources can be allocated to ensure the delivery of the strategy.
- NICCY has expressed particular concerns about delays in assessment and appropriate therapy for children and young people with mental health needs. There is no reference to developing acceptable Standards and targets, akin to those detailed in the Service Framework for Mental Health and Psychological Well-Being of Children and Young People in England and Wales. There is much to be recommended in those standards and NICCY commends them to the Committee for inclusion in any final strategy.
2.3 NICCY would like to emphasise at this point, our disappointment that the findings of Bamford have not been implemented in full. We believe that the recommendations provide a sound blueprint for action and would strongly urge these are actionned as a matter of urgency.
2.4 In research conducted by QUB for NICCY in 2004 on Children’s Rights in Northern Ireland[1], it was highlighted that more than 20% of children and young people in Northern Ireland suffer from mental health problems. The research found that children here experience higher levels of abuse and suicide than those in the rest of the UK and the problem of substance abuse is also continuing to grow. Despite this fact, support and therapy services are unable to provide an efficient and coherent service for all those who need to access it. Some professionals who were interviewed during this research commented that;
The research reiterates this point emphasising that although children and young people (18 years and under) represent 25% of the Northern Ireland population, less than 5% of the mental health budget is spent on child and adolescent services.
3.0 Views on Suicide Prevention Strategy
NICCY recognises that the Suicide Prevention Strategy is targeted at all ages, however for the purposes of this response we will concentrate our comments on issues which affect children and young people. We offer the follow comments:
3.1 Based on the context outlined above, NICCY would strongly recommend that the Suicide Prevention Strategy is based on a comprehensive mental health strategy for young people. We would recommend that the Taskforce meets the chair of the CAMHS working group to ensure that this strategy flows from the CAMHS strategy and that detailed timetables for implementation of both strategies are agreed.
3.2 Coroners Office
NICCY would suggest that “The regional death review protocol” needs to be referred to in the suicide prevention strategy, as death by suicide of a young person under 18 (or 21 if they have been in care or are disabled) should be reviewed through the new arrangements.
3.3 Analysis of Self-Harm in Northern Ireland
NICCY supports the recommendation to monitor self harm attendances at A&E in Northern Ireland. We would further recommend that Health and Social Services Trusts similarly set up a mechanism for key workers to identify young people who self harm in order to ensure a consistent, timely and appropriate response.
3.4 Review of Evidence Base
NICCY is concerned that the strategy should pay particular emphasis to some of the more fundamental causes of mental health problems, such as abuse in early childhood. We would recommend that reference needs to be made to the requirement to provide post abuse therapy, and develop prevention programmes as part of effective intervention in self harm and suicide.
3.5 Training and Development
We would also recommend a further area, which is the need to develop self esteem and confidence building programmes in schools, particularly in relation to young males who may find it difficult to articulate and deal with their feelings. NICCY would strongly advocate for counselling services to be made available in all schools, it is essential however that any service is developed in consultation with children and young people to ensure that the service is designed to meet their needs.
3.6 Overall target
While NICCY accepts that reducing the suicide rate will be very difficult, it is our view that a 10% reduction is too low, and would suggest a target rate of 33%.
3.7 Action Plan – Children and Young People (Chapter 5)
NICCY would strongly recommend the development of a much more detailed Action plan which seeks to address the fundamental underlying causes of self harm and suicide: low self esteem, consequences of abuse, drug and alcohol misuse, impact of paramilitary control etc.
3.8 Health and Social Services
NICCY suggests that there needs to be clear links made by Health and Social Services between the suicide prevention strategy and other key strategies – Children and Young People’s Strategy, CAMHS Strategy, Children’s Services Plans etc. It is essential that this strategy is implemented in line with other relevant policies.
3.9 Police and Emergency Services
NICCY has been concerned that a number of young people who present at A&E departments with self-harming or suicidal behaviour have been dismissed without the requisite follow-up support as they have nothing “physically wrong”. NICCY recommends the inclusion of training for staff in A&E Departments with regards to establishing a greater understanding of the emotional needs of these young people.
NICCY has heard considerable anecdotal information about poor outcomes for young people presenting at A&E departments: Lack of follow-up by specialist agencies, lack of access to adolescent psychiatric services, unacceptably long waiting lists for referral to child and adolescent psychiatrists etc. NICCY therefore recommends an urgent review of the outcomes of referrals made to A&E departments as part of a process of ensuring appropriate and timely follow-up for young people who present with self-harming and/or suicidal behaviour.
A 24 hour crisis care and suicide intervention must be available through a network of services across Northern Ireland, including the out of hours doctors provision.
4.0 Consultation with Children and Young People
NICCY recommends that children and young people should be represented on an Advisory Group to the Taskforce, including those who are most vulnerable and marginalised, and that their views on the proposed strategy should be sought in a direct and meaningful way.
Conclusion
The views detailed in this response are based on NICCY’s involvement over a three year period with young people and representative organisations concerned about mental health provision, self harm and suicide in Northern Ireland. We have also reviewed our own research on Children’s Rights in Northern Ireland, which we carried out in 2003/4, and unpublished research we have just completed with over 2000 children and young people on the current state of rights in Northern Ireland in 2007.
NICCY supports the overall thrust of the Strategy, but as highlighted above, believes that it needs to be set in the context of a comprehensive Child and Adolescent Mental Health Strategy. Both of the Strategies need to be suitably costed and funded, with a clear, detailed timeframe for actions.
NICCY would strongly urge the committee to ensure the recommendations of the Bamford Review are implemented in full.
[1] Kilkelly et al, 2004:88
STEER Mental Health
Background to STEER
STEER exists to promote the social recovery of people who experience mental health difficulties. In addition, STEER lobbies for improvements in the care and treatment of people who use mental health services. STEER is an acronym for Support, Training, Education, Employment and Research, some of the essential components of recovery.
Protect Life: A Shared Vision
In principle, STEER welcomes ‘The Northern Ireland Suicide Prevention Strategy and Action Plan 2006-2011.’ All means of preserving life that would otherwise be lost to suicide must surely be welcomed by all rational thinking people in Northern Ireland.
In relation to the prevention strategy, STEER would make the following points:
- Suicide rates are an unknown quantity and an accurate system for recording suicide statistics must be developed as a priority so that the overall aim of the strategy: “To reduce the suicide rate in Northern Ireland’, can be measured.
- If suicide prevention is to be recognised as a priority by all relevant Government Departments, the Suicide Strategy Implementation Body should be located within the Department of The First and The Deputy First Minister.
- As outlined in paragraph 3.12 development of suitable tools to measure progress and outcomes should be compiled as soon as possible. In addition, the key people who are responsible for ensuring that targets are met and the person or persons who will take full responsibility if the implementation does not meet set targets should be clearly indicated. Accountability and transparency should have a strong bearing on the implementation of the strategy.
- The budget for implementing the strategy must be realistic and not merely tokenism. It would it appear that the current budget would not be sufficient to implement all actions detailed in the strategy
- Health and social care voluntary sector organisations should be adequately resourced to ensure that the strategy will be fully implemented.
Stakeholder Involvement
The term ‘stakeholder involvement’ needs to be clearly and officially defined. A toolkit should be devised that can measure the extent of stakeholder involvement. At present STEER believes that stakeholder involvement is merely a ‘box ticking’ exercise by some agencies.
Services and Support.
Each Health Trust area should appoint a dedicated ‘Service Coordinator’ who will map all statutory, voluntary and related service provision within his/her designated area. The appointed person would liase with stakeholders, service providers and ‘gatekeepers’ to ensure that referral agents have the required information to make referrals to the appropriate service provider. There is a general lack of knowledge amongst key referral agents of what services exist within their own area. In addition there is a need to measure the quality of the services that providers offer. A uniform charter mark system should be used to identify the best performers and appropriate resources should be given for sustainability. Evidence of compliance with existing quality management systems such as Investor in People and ISO 9001 could contribute towards organisations securing charter mark status.
Colin Community Counselling
History
Colin Community Counselling is a community counselling organisation founded in 2003 to serve the people of Twinbrook, Poleglass, Lagmore.
The Project was initiated as a result of concerns in the Colin Community at the level of deaths by suicide and the lack of local community resources to offer emotional health support.
Through a good working partnership, with the then, Down & Lisburn Trust, local community and church representatives, politicians and Probation Board Colin Community Counselling was started.
The Project offers individual counselling and workshops on a range of issues.
Initial set up funding of £5,000.00 was provided by PBNI and £50,000.00 through slippage from Down & Lisburn Trust contributed to maintain the Project.
Down & Lisburn Trust provided accommodation in the Colin Family Centre, Poleglass. Counselling is also offered in other venues throughout the area.
Vision
That the people of the Colin Area will have access to a Counselling Service that supports their emotional health and well being and contributes to enabling them to develop their full potential.
Mission
Colin Community Counselling offers a Counselling Service that enables clients to explore issues impacting on their lives and to discover ways of living more effectively
The service offered will be accessible and sensitive to the needs of the clients
It will be delivered by professionally qualified counsellors supported and managed
in accordance with recognised codes of practice and working in partnership with other service providers.
Governance
The Project:
- Is a constituted organisation and is registered with the Charities commission.
- Maintains Professional Indemnity and Public Liability Insurance.
- Is overseen by a Management Committee composed of representatives from the South Eastern Trust, community organisations and is currently chaired by Mr Jim Deeds, Barnados. [Copy of Management Committee attached]
- Accounts are audited annually by professional accountants
Counselling:
- All Counsellors have a minimum qualification of Diploma Counselling
- All are POCVA checked
- All work within recognised code practice [BACP / IACP ]
- All have contract re terms / conditions and must work within Code of Ethics for this Project
- All must engage in Clinical Supervision ratio as recommended
- All engage in regular line management with Clinical Coordinator
- Clients complete individual evaluations
- Policy Handbook maintained and updated
Staff:
- Clinical Co-ordinator [part time 25 hours]
- Administrative assistant [part time 20 hours]
- 1 Part-time counsellor employed through European Fund for Peace / Reconciliation through Lisburn Partnership [22.5 hours] ceases 2008]
- 8 Professional Counsellors working on sessional basis
Remit
The service:
- is currently open to adults, male & female, aged eighteen years and over
- offers counselling on a range of generic issues
- engages in partnership working with other agencies in the Colin Area; Surestart; Domestic Violence Forum; Colin Suicide Task Group; Colin Health for All
Referrals to Project:
- Self referral;
- GP’s
- Social workers
- Community groups
- Lagan Valley Assessment Centre
- Health Visitors.
Developments 2006/7
Peace 2 Funding secured for period of eighteen months to employ part time Counsellor to work specifically within the Twinbrook area and Old Warren, Lisburn.
This is successful to date.
Consultations are ongoing with South Eastern Trust, Investing for Health re offering service to persons below eighteen years.
Workshops on Anger Management & Anxiety Management
Achievements
Highly Commended in Chairman’s Prize, Down & Lisburn Trust 2006
Funding
- Current £50,00.00 per year from Trust [no uplift in 4 years]
- Total £26,000.00 x eighteen months from Peace 2 through Lisburn Partnership
- Small Grants from Community Relations Council for IT Update
- Accommodation in Colin Family Centre
Statistics
- see attached information on client group and issues presented.
Summary
I have presented the above facts to demonstrate how Colin Counselling working with a very restricted budget is generating effective mental and emotional support at community level.
Our statistics show that clients are engaging with the local service;
The Project is recognised by both statutory and community agencies as providing an effective service
We are building a reputable Project and gaining a reputation for professional and quality service provision
We are working towards the targets of the local Colin Health for All Priorities
We are engaged in the prevention, intervention and post-vention aspects of suicide
We are providing a valuable service within a community making it easier for people to access the help they need when they need it
Statistics
Year April 2006 – March 2007
Contacts to Project |
188 |
Assessments Completed |
106 |
New Clients Attended |
81 |
Ongoing Counselling Sessions attended |
932 |
Total sessions attended |
1119 |
Anne Mc Larnon
Co-ordinator
North Down YMCA
Committee Inquiry into the Prevention of Suicide and Self Harm
1. Introduction
My involvement with the issue of suicide and self-harm is as a member of our local Mental Health and Emotional Wellbeing “Community of Interest”[1] in the North Down & Ards area (developed through the implementation of the Investing for Health Strategy) and through my day to day work with my organisation (North DownYMCA) in providing support and services to young people (age range 5 -25).
The following information has been gathered from my knowledge as a member of the local Community of Interest (COI) and representative for the COI on the Eastern Area SSIB Sub-Group and Regional SSIB. I have also had discussions with some members of the local group in preparing this response.
2. Background
The North Down & Ards Community of Interest (COI) on Promoting Mental Health and Emotional Wellbeing began in September 2003 when approximately 40 organisations attended a workshop in Newtownards.
Member organisations include:
| Action Mental
Health Age Concern Citizens Advice Bureau Autism NI Barnardos Fountain Centre (vol. Organisation) Belfast Central Mission Cruse The Link Family & Community Centre North Down YMCA North Down LSP Ards & North Down Borough Councils Samaritans Holywood Family Trust |
Peninsula Healthy Living Initiative |
Since that date the group have met on a number of occasions taking forward collective action in the local area and a local Action Plan was developed in April 2005 for a period of 3 years.
In 2006, the group established 4 sub-groups to focus on specific issues and drive forward action. One of these sub groups was established to concentrate on the issue of Suicide and Self Harm.
3. Suicide and Self Harm
Official statistics for suicide in the North Down & Ards area show a decreasing trend from 2000 (19 no.) to 2004 (11). In 2006 the numbers have increased to 13, however it will take time to tell whether this is an in-year increase or an upward trend.
Notwithstanding the above, each suicide is a tragedy for the individual, their family and the local community. The local COI welcomed the Protect Life: Suicide Strategy in 2006 as it gave focus to the issue of suicide prevention. The Strategy stresses the fact that “suicide is everyone’s business” and this is perhaps reflected in the large number of actions (62 no in total) and the range of delivery partners identified.
There have been queries raised on issues such as -
(a) how progress can be made on so many actions, given that “lead” partners are not clearly identified and much of the responsibility for driving action lies with the DHSSPS;
(b) No identification of organisations in the community and voluntary sector who could have a contribution to make;
(c) Danger of services being driven via DHSSPS and the potential therefore to “medicalise” the solutions to the issue.
1.1 Stakeholder Involvement
In the development of the Protect Life Strategy local people were encouraged to attend the consultation sessions and bring forward their views. The “open door” policy of the local COI enables engagement on suicide prevention from any individual, group or organisation.
The “Community Support Package” element of the resources under the Protect Life Strategy is targeting funding to providers in the community & voluntary sector. This would appear to have been driven by the engagement of community & voluntary organisations at the regional strategic level. This has ensured that resources channelled via HSSB’s and the IfH (COIs) have been made available to community/voluntary organisations at a very local level.
The high profile of the Strategy in the media etc., the establishment of a local sub-group, the delivery of training and the new resources available has enabled more people to become involved through debate and discussion across a range of local partnerships and within various community organisations.
There is limited engagement at present locally from families bereaved by suicide and this may take time to develop.
3.2 Existing Services
It is important to take time to assess the impact of the existing programmes/projects that are taking place. For example, programmes such as “developing coping skills of young people” are cited as being effective in improving their mental health. Many of the personal development programmes in schools and youth organisations have been in operation for a number of years and their contribution to the suicide prevention agenda should be assessed.
Services and support made available under the Protect Life resources have only been in place for a short time and will need time to become established and for any assessment to take place of their effectiveness.
3.3 Further Action
It is difficult to determine what further action might need to take place at this early stage. One of the key issues highlighted on a regular basis is the fact that those actions that are being put in place require “recurrent” resources to have any lasting effect. Short term, in year resource often have limited impact.
The establishment of good local networks as an “early warning system” and also as an effective, efficient support system in response to a crisis is seen as a key action.
[1] A “Community of Interest” is defined as a group of people who come together because they have an interest in an issue, either from an individual, group or organisational perspective.
Zest
In response to your terms of reference outlined I would report as follows:-
I welcome the department’s pro-active approach in the development of a Suicide Strategy for Northern Ireland and in particular to the “Protect Life: A Shared Vision” document.
I also welcome the department’s decision to carry out this inquiry and would respond as on behalf of Zest follows:-.
In assessing the scope and appropriateness of the strategy document this appears to have been achieved, in part, through the consultation process where all key stakeholders had the opportunity to actively get involved in making suicide prevention possible through the setting up of committees to implement the strategy. As a result of this process and the information contained within the strategy document it has been successful in identifying, highlighting and targeting areas of need through effectively beginning to work towards reducing the numbers of suicides and self-harm in Northern Ireland. However, in consciously raising awareness it has resulted in an increase in the demand for accessible services which the strategy fails to effectively address based on the long term needs of individuals who self-harm or attempted suicide together with family members or friends affected by the impact of self-harm and suicide.
On examining the level of stakeholder involvement this has changed during the process. From a community perspective there are concerns in relation to equal partnership and, in particular, equality in the decision-making process. This has been expressed from members of the community and voluntary sector in that the decision making does not always appear transparent. Should the lack of confidence in the decision making process continue to grow it will have consequences for the implementation of the strategy. In addition, it is evident that the short time-frames between consultation and allocation of monies is not helpful as monies may be allocated based on the principle it has to be spent before a certain time-frame.
This practice runs the risk that it may not be the best allocation of monies that will make a long term difference to people lives in accordance with the aims and objective of the strategy.
In terms of the level of services and support to promote good mental health. This target has been partly achieved. It appears that a considerable amount of monies and time has been allocated to the delivery and promotion of a wide range of awareness programmes and less on actual provision of psychological services which has been identified through a number of consultation processes. In actively delivering awareness programmes we create an increase in demand for services. This gap has also been identified in the recent Bamford Mental Health Review, Camelot “Truth Hurts” Report and NHSS report on young people’s emotional well-being.
It would appear if the suicide strategy document is implemented in isolation of the findings within the above reports there is a possibility we may fail in the long-term to effectively address the needs of individuals who self-harm or are suicidal and families affected by the impact of self-harm and suicide.
The question we ask but still fail to answer and respond to is - “if you were suicidal what might you need”. I feel this question highlights clearly the need for psychological services throughout Northern Ireland delivered by both statutory and voluntary services working in partnership to addressing the alarming rates of self-harm and suicides in Northern Ireland.
I hope this information is of value. Zest is committed to actively working to implement the suicide strategy and ensure the delivery of accessible effective services in partnership with the statutory services.
Noella McConnellogue
Service Manager
Gerard and Carol McCartan
We lost our son Danny to suicide on 11th April 2005 he was 18yr old.
As you our all probably aware we had an independant review into the treatment and care of him by 3 health trusts. There was recommendations made and also it highlighted the failings of the health service while our son was in there care. We would like the health committee to read the report as im sure you all have done and make sure no family has to suffer the way we did. We know this is only a short note but we feel everything you need to know is in the report. Thank you for writing to us and I hope we can be of help to you.
National Union of Students
- Union of Students in Ireland
The initiation of an inquiry into suicide prevention by the Health Committee is one we see as timely and incredibly important in light of the recent increasing numbers of people who have taken their own lives.
For our part, NUS-USI, as an organisation, represents over 185,000 students across Northern Ireland and is finding that, as a result of the pressures associated with student life, suicide prevention and awareness of the factors surrounding it are becoming ever important.
Can we also note, for the attention of the Committee, NUS-USI has recently launched a project entitled ‘Open Your Mind’ that deals with mental health issues among students and, as a result, looks at confronting the issue of suicide awareness and prevention amongst the student population. See appendix 1.
As has been laid out in the Committee’s press release (HSSPS 13/07), we will make our response based on the four areas you seek to address.
1. Scope and Appropriateness of ‘Protect Life: A Shared Vision’ strategy
The Department’s strategy earmarked £3 million per annum, £15 million over five years, towards the implementation of its strategy[1].
We welcome this allocation of resources and the Department’s attempts to confront the issues that have arisen; however, we have some reservations over the current package.
During Health Oral Answers in the Assembly on 1st October[2] the Minister noted the four hundred mental health nursing vacancies in Northern Ireland. He further indicated that fifty-three places would soon be taken up by new graduates. We believe that here there is scope for action.
There should be much more promotion of the need for such nurses in light of the current climate. Without them the entire strategy of the Department must be called into question as a result of under-staffing.
We also note that in the strategy there was provision made for the training of GPs in suicide prevention methods and techniques. As noted in a BBC Online article in early September[3], up to 80% of local doctors still do not have ‘specialist training in suicide prevention’. The article further noted that, ‘80% of people who took their own lives had visited their GPs in the previous six months’.
There is a need for a statutory duty to provide adequate and appropriate treatment.
Considering the recent upsurge of suicide rates in Northern Ireland we do indeed believe that the Department’s strategy was timely.
2. Level of stakeholder involvement
As an organisation which represents the students of Northern Ireland, it is our belief that there is not enough dialogue between those who formulate policy, those who act on it and the student body.
We note that, as a result of the pressures of student life, there is an increasing issue of those in tertiary education becoming susceptible to the problems arising.
With regard to the ‘Protect Life: A Shared Vision’ strategy, NUS-USI believes that the joined-up thinking which was promised has not been seen as pro-active as is necessary.
We urge a greater collaboration between professionals, policy makers and students in order to highlight the specific needs of such a wide section of the population and in order to cut the risks that currently exist and are developing further.
Students may be becoming more vulnerable to the increasing trend that has been identified but we want to help to solve the issues and again urge greater participation and dialogue amongst all stakeholders.
As an example, we believe those students who are already carers for family members can be under incredible pressure, and fear that they are not receiving adequate support which can have directly negative consequences.
3. The level of services and support currently available
Here, we note the work carried out through the Applied Suicide Intervention Skills Training (ASIST) and urge that such training be provided to those who currently work in medical and counselling services throughout our universities and colleges.
Other examples of such good work in the field come via the Public Initiative for the Prevention of Suicide (PIPS) and the activities of the Samaritans. NUS-USI would like to take the opportunity to congratulate these groups on their activities with regard to suicide prevention and awareness but note with caution the relatively small amount of groups who are currently pro-actively engaged in such work.
The position of university tutors and staff must also not be overlooked. For many students, advisors of study become people with which regular contact becomes imperative. Training in suicide awareness techniques amongst these groups may also be beneficial in order to further entrench the required action to counter the issue.
We are aware of the recent pilot at Queen’s University’s health centre of an online CBT programme and note our support for their efforts to roll this out across all colleges and universities in Northern Ireland with the active involvement of those institutions.
Akin to the sexual health drop-in centres that presently exist at Belfast Metropolitan College, we would like to see the establishment of mental health awareness contact/information points at our universities and colleges. These could provide a facility for students to confidentially discuss issues of concern and would potentially minimise the development of mental health conditions within the student population.
4. Further Action required
As we indicated earlier we urge the Committee to advocate a more joined-up approach in how policy is formulated and delivered, perhaps by developing the role of the Mental Health Review Tribunal into a decision-making body as per the Mental Health Tribunal for Scotland.
Too much time and too many resources are spent in constantly reviewing the subject and in formulating never ending plans to its resolution.
We accept that there is excellent treatment available, however, are concerned about the lack of awareness of this amongst the groups that most need it. The evidence gap which currently exists in diagnosis must be filled with a great deal of urgency.
Recently we have seen counselling services being set-up for post-primary pupils in order to counter problems specific to their age-groups. Such procedures, amongst others, should now be driven forward for those in tertiary level education in Northern Ireland.
More funding should be provided to organisations like PIPS who currently have only two paid full-time staff. Their services should be available to families and not just those who suffer.
We would also like to see greater promotion of days such as World Mental Health Day and Suicide Prevention Day. The public are largely oblivious to the issues at hand without public promotion. If we are to take seriously the level of the problem then awareness must be a major priority.
Katie Morgan
President NUS-USI
Appendix 1
Note on NUS-USI’s ‘Open Your Mind’ project
Background
Open Your Mind is a five-year peer-led mental health project which has been funded by the Big Lottery Fund. NUS-USI and Rethink NI jointly manage the project.
Volunteers will be recruited from the student body on an annual basis. The volunteers will then be trained in a number of courses and will develop and lead the campaigns.
Aims
We aim to promote awareness of mental health issues amongst students aged 16-25 across Northern Ireland and reduce the risk factors related to mental illness through awareness raising.
Why?
A lack of consistent positive mental health services for those who need it most in the student population has led us to formulate the project launched on 10th October at Queen’s University.
Student issues which contribute to problems
- Transition from school to university and a different level of work
- Financial difficulties
- Moving away from friends and family
- Sharing accommodation
- Basic housekeeping
- Doing wrong subject/choosing wrong career
- Pressure of drugs, alcohol, risky sexual behaviour and irregular sleeping patterns
- For those who have a mental illness and going into FE/HE may have to deal with the daily stigma and discrimination that is associated with it
Objectives
As the project will run for five years we hope it will allow us to achieve something more long-term for students across Northern Ireland. There will also be an opportunity to evaluate the project at key stages over its life; the evaluations largely being shaped by students themselves.
Final Remarks
We would like to thank the Committee again for initiating this inquiry and look forward to participating in its further development after the closing date for written submissions.
[1] Department of Health, Social Services and Public Safety; ‘Protect Life: A Shared Vision’, October 2006
[2] See link; http://archive.niassembly.gov.uk/record/reports2007/071001.htm#6
[3] See link; http://news.bbc.co.uk/1/hi/northern_ireland/6980845.stm
Aware Defeat Depression
At Aware Defeat Depression we welcome this initiative taken by the Committee and the opportunity to feed our experience into the process.
Background
Aware Defeat Depression has been operating in Northern Ireland for over10 years. Our vision is of a society where people affected by depression are enabled to seek and find the help they need in order to recover. Estimates suggest that of every 4 people suffering from depression only 2 will seek help and only 1 will get the support and/or treatment they need for this disabling and potentially fatal condition.
We support people experiencing, or at risk of, depression and their carers through the provision of information, promotion of self help, support for research and by working for positive changes in public attitudes and health care provision.
We recognise that positive mental well being is more than just the absence of illness and we holistically promote the importance of self management skills, self awareness, warm relationships, social support and physical fitness.
Our core services are based on self help and health promotion models and include:
- a depression helpline
- 20 self help support groups in local communities across N. Ireland
- the provision of a range of publications providing factual information
- an annual series of free public talks
- ‘Mood Matters’ - depression awareness programme for young people in schools and other appropriate settings.
The majority of our services are provided by trained volunteers (around 100 in total), most of whom have personal experience of depression. They are supported by a small staff team of 10 people. We estimate that our services currently reach around 15,000 people per year and that there is much more we need to do to extend the reach of our services. Suicide has been an ever present theme raised by our service users throughout our history.(The Clinical Standards Advisory Group (2000) estimated that 1 in 6 people with enduring depression would eventually commit suicide).
We welcomed, therefore, the recognition in the Protect Life Strategy of depression as a key risk factor in suicide and have supported the need to develop a range of actions to prevent depression as well as enabling people to cope with and recover from it. We are particularly keen to see action which supports people experiencing, or at risk of, depression and their carers through the provision of information, promotion of self help, support for research and by working for positive changes in public attitudes and health care provision. We are convinced that the broad range of coherent and co-ordinated actions in this regard set out in the strategy has the potential to make a significant impact on suicide rates over the long term.
Protect Life Strategy
Aware Defeat Depression has been involved in a number of key areas in the implementation of the strategy to date including:
The development and roll out of the Depression Awareness Training Programme for GPs and other primary care professionals. As the majority of people experiencing depression are dealt with at primary care level we view the sustainability of this programme and the potential to develop the ‘whole practice’ approach as a crucial long term goal. The regional nature of the programme to date (supporting local action) led by the Health Promotion Agency has enabled us to participate effectively and bring to bear our expertise in the field of self help and the user perspective.
The Mind your Head public information campaign. A number of our service users were involved in the consultation on the media campaign and we believe that it has also brought our work to the attention of new users. Our service users tell us that stigma is a primary reason why they do not seek help because of the potential loss of esteem. We regard the continuation of campaigns of this nature to be a crucial long term under-pinning element in the strategy to promote help seeking behaviour.
As a stakeholder we have been involved in the Suicide Strategy Implementation Body at N.Ireland level as well in the Western and Eastern Board areas, including on sub groups and locality groups. We acknowledge that for the strategy to be effective it must reach into and respond to local needs. At the same time the number of structures which exist for engagement and they way in which these differ from area to area presents significant challenges to smaller regional organisations like our in terms of available human resources to engage and communicate effectively. In some areas we have simply not had the capacity to keep fully abreast of developments.
We have successfully achieved modest amounts of funding for some of our work, particularly our schools and youth programme. This is always welcome in our quest for stable income streams for work which has been positively evaluated. We have some concerns about the level of bureaucracy involved in the bidding process and the variation in processes across areas. Again this is very challenging for smaller organisations with dispersed services and can have a negative impact on the resources available to put into frontline services. The availability of some regional funding streams for non-statutory projects would be an aspiration we would hold for the future development of the strategy, likewise the need for stable recurrent funding to maximize both planning and impact.
Conclusion
We look forward to supporting the development of policy in this crucial area. We are fully committed to the broad direction of cross departmental and cross sectoral working which recognizes the complex determinants of mental health as well as understanding the often very simple needs of people with depression who have lost hope to the extent that suicide presents as an option.
Sharon Sinclair
Chief Executive
Northern Ireland Human Rights Commission
Further to previous discussions regarding your call for submissions to the Committee’s Inquiry, the Human Rights Commission is not in a position to submit evidence but wishes to express its keen interest in the subject, to commend the Committee for addressing it, and to inform the Inquiry of its own planned work in relation to suicide in children and young people.
This issue was discussed by the Commission’s Policy Committee earlier this week, and approval was given for a short piece of policy development work that may in time lead to a more substantial piece of research or an investigation, the eventual design of which is likely to be greatly assisted by the outcomes of your Inquiry.
For the present, the scope of our work is limited to planning an expert colloquium in the late spring of 2008 on the basis of independent academic research on which Dr Angela O’Rawe from CAMS (a consultant pediatrician with an LLM in human rights) is currently working. This will focus on the case for, and a possible model for, a regional strategy for the prevention of suicides and self-harm among children and adolescents. From the Commission’s perspective, our focus will be on effective responses to this issue as an expression of the positive obligation on the state to protect life, as an element of Article 2 of the European Convention on Human Rights. Consideration will also be given to publishing a paper from the colloquium, perhaps in the form of a summary of Dr O’Rawe’s recommendations and short responses from some of the experts taking part.
We hope that the Inquiry will take note of this work and that its sessions will help to inform our own policy development around the protection of the right to life including this specific issue of a regional strategy.
Should you have any further queries please do not hesitate to contact me.
Virginia McVea
Solicitor
Action Mental Health
Thank you for the invitation to comment on the preventative work going on in relation to suicide and self harm under the Protect Life – A Shared Vision strategy.
The scope of the strategy in its targeted and population approach is ambitious and far reaching, as it needs to be. Continuous efforts are necessary to ensure that the issue of suicide and self harm remain important and high priority across government departments, statutory, voluntary and community sectors and throughout communities. What is equally important is how the document is translated in to the action plans of each respective Health Board/Health & Social Care Trust, and subsequent support for all people affected by suicide and self harm and how involved people in need feel in this process for the outcome to be beneficial. Although difficult to achieve, the effort involved is worthwhile as the effect is often much more meaningful and lasting for beneficiaries.
Concerning the appropriateness of the strategy, what is encouraging is the planned annual review in to the progress made against targets by the Suicide Strategy Implementation Body (SSIB). This should see targets change as others are met and sustained, ensuring that the strategy remains fluid and responsive. What will be important is that future targets are informed by research and mindful of emerging needs from the genuine consultation of all key stakeholders.
I am aware of and involved in the efforts being made within the Southern Area Trust to engage all stakeholders in the prevention of suicide and self harm. Whereas some of this work is still developing there are established groups at Board and Trust level with voluntary, community, church, PSNI representation and an ‘open door’ policy for other interested parties to become involved in this work. Although true and commendable, confusion particularly at community level is apparent and communication needs to be clearer across all sectors so that information and support is quickly understood and effective. Another key stakeholder, the Media should be used to better effect throughout NI in their reporting of suicide, self harm and mental health.
Mental Health should receive constant coverage from the point of well being, awareness raising and the identification of sources of support rather than the present sensationalist headlines. I know that media guidelines do exist and these are welcomed, but concerted effort is required at regional and local level to nurture relationships with the media for this to be achieved. Similarly, in respect of the level of GP interest and action in relation to suicide and self harm further work is necessary regarding training and awareness of presenting mental health problems and sources of support.
In your scoping exercise to examine the level of services and support available to promote good mental health, to prevent suicide and self harm and to support those affected by suicide you will discover examples of good working practice across sectors and specific areas better served with such services than others. What will be required here is a more coordinated approach in meeting the diverse needs of individuals and local communities. Even where services exist, access can be a problem due to lack of awareness, stigma and referral procedures. Notable gaps in services that should emerge are good, targeted mental health promotion approaches for all people, comprehensive community based services for people with mental health & learning disability needs, support for new communities now residing in NI and people affected by suicide and self harm.
I note also that the focus of such work should consider more the need and benefit in preventative measures that encourage early help seeking behaviour concerning mental health, suicide and self harm.
Action Mental Health (AMH) in serving people with mental health and learning disability needs advocate better future services and opportunities for people wherein they feel valued and empowered to achieve their full potential. AMH echo the recent statement by Mr Colm Donaghy, Chair of the Suicide Strategy Implementation Body, for additional funding for already under funded mental health services and the implementation of the recommendations of the Bamford Review of Mental Health & Learning Disability Services. When achieved the needs of one of the highest identified groups at risk from suicide and self harm, people with mental health needs, will begin to be appropriately addressed.
In conclusion, I again thank you for this opportunity to comment on the strategy and confirm AMH’s interest, commitment and cooperation in working with others in respect of Protect Life – A Shared Vision.
Colin Loughran
Service Manager
TMR Health Professionals
The Niamh Louise Foundation
The Niamh Louise Foundation was established on the 2nd February 2006 on what would have been Niamh Mc Kees 16th birthday.
Niamh died by suicide on the 21st of November 2005 at the age of 15. Her death shocked not only her family but also the small rural community of Clonmore. Niamh was actively involved in all events held within the community, she played ladies Gaelic football, sang with Clonmore choir for five years and eagerly participated in any arts or drama held in the local hall.
No one knew how to help her family or the community so Niamhs mother and stepfather turned to other organisations in Belfast for support and enlightenment as to why their child died by suicide.
With grief heavily weighing on their shoulders they realised that they needed support locally as they could not continue to travel the distance to Belfast and they desired the comfort from people in their own rural area who could relate to the thinking and living within a small rural community.
There was no support and suicide was heavily stigmatised in rural mid Ulster so determined to create awareness for the local rural communities Niamhs family established the foundation.
Since its formation the suicide “ Protect Life Strategy ” was introduced to Northern Ireland and the foundation participated in all the consultation events held within the Southern Area Board.
The Foundation was able to reply and make comments before the Southern Area Action Plan was completed.
As a result of the foundations close involvement of the implementation of the Strategy Catherine Mc Bennett (community development worker for the foundation) sits on the SSIB, the Southern Area Protect Life Steering group and the Protect Life Implementation group in the southern area.
To help the foundation achieve all aims and objectives it has recently partnered with Breakthru in Dungannon. Breakthru are a drug and alcohol awareness organisation with an on site suicide counsellor and are passionate about aiding the foundation in reducing the rates of suicide especially which the foundation makes
Population approach
It is the foundations belief that there is a need for a resource centre in mid Ulster to meet the needs of the people living in rural areas. The vision of the foundation is to provide a centre that is not labelled suicide awareness, as stigma is still high in rural areas, but to provide a centre that has the qualities of a village where people can make use of a drop in facility. The resource centre would have a coffee shop or tearoom available to the general public, a library with awareness literature on suicide and self-harm amongst the self-help categories and craft or gift shop to help in the sustainability of the centre.
The idea is to have a centre that is open to the public with all the awareness and signposting information available on site. The foundation would have an office within the centre so that anyone can seek help without worrying about stigma associated with suicide so everyone can avail of the proper help.
The centre would also host the suicide bereavement support groups that are currently being facilitated by the foundation at the Breakthru offices in Dungannon and the Niamh Louise Foundation youth forum, which meets twice a month.
The Resource centre would also follow the aims and objections of the Niamh Louise Foundation to create awareness on suicide and self-harm on prevention, intervention and postvention. Therefore the centre would also be seen as a research and training facility as well as a support and signposting facility.
At present no monies have been allocated to the foundation to provide such a centre but monies have been allocated for a community worker and satellite resource centres in the southern area. It is the foundations aim to provide one centre, as stated, so a high level of standard can be maintained through out all areas in regard suicide and self-harm prevention, intervention and postvention and one centre of evaluation rather than satellite centres at present where communication is lacking and the general public don’t know who to turn to for help.
Communication is very poor with regards public bodies and the work being done on ground level by community organisations such as the Niamh Louise Foundation. As mentioned the foundation was set up to meet the needs of the rural areas in mid Ulster, the catchments areas of the foundation being Tyrone and Armagh.
Even though the foundation has strong link with P.I.P.S in Belfast, Newry and with the West Belfast support group, it seems that the N. Ireland Assembly has forgotten the needs of the rural people as the only reference made to any community organisation publicly is to P.I.P.S.
While the foundation commends the good work being done to date by P.I.P.S it is important to stress that what may work well within the cities in regards suicide awareness does not always work well in rural areas.
The foundation was established for such reasons and it is crucial that the needs of the people living in rural areas be addressed and highlighted.
The foundation would like to propose that this does not seem to have been included in the development of the strategy and the principal that one method works well in all areas should be readdressed and special attention given to how to create awareness and response mechanisms in the aftermath of a suicide in our rural areas.
It is essential we think of this when developing packages for our schools, hospitals and crisis response teams.
Although the pilot telephone help line is currently being used successfully in Belfast it is important to rethink how it can be rolled out in the rural areas and how the advertising and follow up procedures are addressed.
ASIST
Although an evaluation has been undertaken in the southern area regarding the ASIST training it is the foundations belief that this training should be available to all members of the community and not just professionals. Over 500 people have been ASIST trained within the southern area but the foundation doesn’t have access to those trained with a view to help the foundation when an intervention is required.
It has been suggested that more T4T training is required but the foundation would question how fully utilised are the people already T4T trained and the suitability of those chosen to do the training. It seems that with all the training being given it is still the few dedicated people within the foundation that is called when an intervention is required.
Having consulted with the southern area health promotion department on this matter it is both the foundation and SAHPD belief that T4T ASIST training was offered primarily to statutory bodies and then voluntary organisations with the view to role out ASIST training in the southern area. But it has since been evaluated that managers will only allow certain individuals to train once a year so it is essential that T4T training will only be offered to those dedicated to its implementation.
The foundation would therefore propose that training is only made available to those who intend to do interventions within the work place and the local community and everyone should offer a couple of hours every few months to a community organisation such as the foundation when an intervention is required or additional help is needed.
The foundation is aware that Michelle mc Masters HPD is currently compiling information regarding all training currently being used and we await her findings in due course but still feel the training problems regarding ASIST should be dealt with sooner rather than later.
Targeted Approach
The foundation is aware that time will help create awareness for young males and females who have suicidal thoughts or have been self-harming to seek the help they need but improvement within the health system regarding mental health care and availability of resources is of the up most importance.
It is distressing that GPs are unwilling to avail of the training made available to them at present especially when they are the gatekeepers from the community to the mental health care system. The stigma is still very high in rural areas regarding approaching a GP for help even for mild depression as the general belief from the community in rural areas is that GPs are under pressure, have no time to listen, have no empathy for some one suffering form suicidal thoughts or self-harm. and lack the knowledge and again empathy for families bereaved from suicide often distressing the families further.
The foundation having being ASIST trained with two members T4T ASIST trained and have undertaken the Mental Health First Aid Course would like to offer our services any way possible in helping GPs become more aware of the need to improve their training in relation to mental health prevention, intervention and postvention in the rural areas of Tyrone and Armagh.
It is the foundations ambition not only to help create awareness to GPS but to schools, colleges and everyone in the rural areas of Tyrone and Armagh.
Department for Social Development
Introduction
1. Three areas of responsibility within the Department for Social Development have particular relevance to the ongoing implementation of the Suicide Prevention Strategy. Their impact and links are detailed below.
Neighbourhood Renewal
2. Neighbourhood Renewal represents Government’s key vehicle to tackle disadvantage and deprivation. It is an area based strategy focused on those neighbourhoods suffering the worst levels of multiple deprivation as measured using the Noble Index of Multiple Deprivation.
3. Whilst the strategy is led by the Department for Social Development, due to its lead role in addressing social need and social exclusion including community development and urban regeneration, it is a cross cutting Government strategy. As such it provides the link and means to integrate, at local neighbourhood level, all major Government strategies and policies such as the NI Suicide Prevention strategy, Lifetime Opportunities – the Government’s Anti-Poverty and Social Inclusion strategy, Shared Future, Investing for Health, Community Safety, and strategies for Skills, Employability and Sustainability.
4. In all, 36 Neighbourhood Renewal areas have been identified, these are all urban areas suffering the highest levels of deprivation ( 15 in Belfast, 15 in towns and cities across Northern Ireland and 6 in the North West, details are set out in Annex 1). Approximately 1 person in 6 of the population in Northern Ireland is being targeted. This equates to approx 280,000 people.
5. As Neighbourhood Renewal is targeted at areas with high levels of deprivation and, many of these areas have suffered the worst rigours of the troubles, the link between the Suicide Prevention Strategy and Neighbourhood Renewal is very strong.
6. In each of these neighbourhoods, Partnerships representative of the key community, voluntary, statutory, political and private sectors in the area have been established. Their role is to develop a long term vision for the area, (7 to 10 years) and agree 3 year rolling Action Plans to detail the programmes and/or initiatives required to improve life and life chances in each of the areas. Contact details for each Neighbourhood Partnership have been shared with Health and Social Services Board representatives to support the development of improved linkages between the Suicide Strategy and Neighbourhood Renewal and relevant information is exchanged on a regular basis.
Neighbourhood Renewal Action Plans
7. In determining and agreeing local priorities and proposed Action Plans in each area, Neighbourhood Partnerships are working to tackle the specific needs of disadvantage. Through this process Neighbourhood Renewal is seeking to ensure that the substantial amount of public money available is spent in a co-ordinated and effective way to ensure it has the greatest impact. The vast majority of Neighbourhood Renewal Action Plans have identified suicide, self harm and mental health as key issues which affect their areas; they have also identified specific actions to address these issues, working closely with statutory bodies where possible. Regional Neighbourhood Renewal targets to measure the impact of the strategy overall have been determined and agreed with Ministers across respective Departments, this includes a specific target to reduce the higher rate of suicide in Neighbourhood Renewal areas.
Neighbourhood Renewal in the Community
North West
8. The North West Development Office (NWDO), which is responsible for the delivery of Neighbourhood Renewal in the North West works closely with Western Health and Social Services Board (WHSSB) and the Foyle Health and Social Services Trust, now known as the Western Health Social Care Trust, both of which have representatives on the Neighbourhood Renewal Programme Group, the overarching statutory structure for Neighbourhood Renewal in that area. The WHSSB is represented by the Investing for Health manager.
9. NWDO, through the Neighbourhood Renewal Investment Fund is funding various projects such as Foyle Search and Rescue, Mencap, Greater Shantallow Area Partnership and a number of other projects brought forward by the WHSSB aimed at addressing issues associated with suicide prevention and support for families of suicide victims, supporting people with mental health problems and dealing with drugs and alcohol related problems.
10. The Neighbourhood Partnerships in the North West have developed Action Plans for their respective areas and the following action is included in the Outer North Neighbourhood Action Plan:
“Support the roll-out of the Northern Ireland Suicide Prevention Action Plan within the area - Intervention Programmes initiated”.
Belfast
11. In the Greater Belfast area the Belfast Regeneration Office currently supports a number of initiatives which contribute to the ongoing implementation of the Suicide Prevention Strategy through the funding of strategic posts and capital costs. These include salaries for key centre managers/ Directors with responsibility for the co –ordination, management and development of training and counselling services including suicide awareness elements. The counselling services also deal with issues of bereavement, guilt and anger of those affected by suicide. The details are as follows:
Corpus Christi Services provides counselling services to residents throughout the Upper Springfield Whiterock Neighbourhood Renewal Area. The programme is funded through the Department for Social Development’s Belfast Regeneration Office, Neighbourhood Renewal Investment Fund.
Ballymurphy Women’s Centre provides counselling and complementary therapies to women fro the Upper Springfield/Whiterock Neighbourhood Renewal Area. The project receives funding from Department for Social Developments’ Belfast Regeneration Office, Neighbourhood Renewal Investment Fund.
Colin Neighbourhood Partnership has established the Colin Suicide Prevention Task Group that draws representation from community, voluntary and public sector. Suicide prevention has been identified as a priority under Health within the local Action Plan agreed for the Colin area in June 2007. The Task Group are developing mechanisms for the coordination of work by local agencies to improve and ensure that support mechanisms available within the area are promoted including ASIST (Applied Suicide Intervention Skills Training).
Footprints Women’s Centre provides counselling services, and through the Assist Training programme staff have participated in training specifically focused on suicide awareness and prevention and have also hosted 2 conferences on the subject to promote awareness and disseminate information. This programme makes referrals as necessary and provides a confidential local resource that would not be possible without BRO’s support of the management posts. The programme is funded through South & East Health and Social Care Trust
Cloona Oasis Centre also provides similar counselling services as Footprints for Men the Men at Risk Support Group; this includes a variety of workshops designed around issues of depression, suicide, drug / alcohol and substance abuse all of which are conditions associated with suicide. D & L Trust directly supports the programme through the Pharmacy project and referrals.
Upper Andersonstown Community Forum - through their services in conjunction with Social Services runs a specific programme that focuses on issues of depression and suicide prevention through counselling, referrals and volunteering. They have run a specific programme for local youth promoting suicide awareness and prevention.
Forum for Action on Substance Abuse (FASA) was set up in 1997 as a community response to the problems of drug and alcohol abuse in the Greater Shankill area and the often associated issues of self harm and suicide risk. Over the past decade it has established its reputation as a quality service provider, supporting sufferers and their families through a range of interventions. Programmes delivered by FASA include counselling, drug awareness, complementary therapies, anger management, family intervention and skills based training for users. The majority of their work is in the Greater Shankill area but they also work on a cross community basis in other areas of north and west Belfast. FASA manages the Health Trust-funded suicide action group for the Shankill, RAYS and recently hosted a high profile suicide awareness event with Health Minister Michael McGimpsey as guest speaker.
New Life Counselling Service – North Belfast
Belfast Regeneration Office has provided funding through the Neighbourhood Renewal Investment Fund to support 4 key posts of Project Manager, Therapeutic Co coordinator, a Youth Counsellor and Adult Counsellor for New Life Counselling Service (NLCS).
NLCS provides a counselling and information service for children, young people and adults receiving referrals from a range of sources i.e. parents/guardians, schools youth clubs, social services, probation, clergy, doctors, local hospitals, social workers, education welfare officers and others. The main aims and objectives of NLCS are to deliver an accessible community based counselling service to meet the health needs of local communities in the Crumlin/Ardoyne NRA.
NLCS is a unique community based counselling service and is the only one of its kind in North Belfast. This uniqueness allows the organisation to provide counselling at the doorstep of communities that are continually in crises and in many instances NLCS provides a life line for local people as they struggle with emerging issues such as self harming and suicidal thoughts and behaviours.
Voluntary & Community Unit
12. The Voluntary and Community Unit (VCU) within DSD is working to support the development of enhanced links between churches/religious bodies and the local community support networks and is currently leading a cross-Departmental review of how Government engages with the faith sector across a number of policy areas. This overall objective of the work, which is funded through the Renewing Communities initiative, is to create conditions in which faith based organisations can make a maximum contribution to civic society in Northern Ireland through, for example, the provision of services (such as support services), representing community interests etc. Building on Good Faith Conference, bringing together representatives of the sector, was held on 30 April 2007 and in advance of this, all Departments were asked to consider the current and potential contribution of faith based organisations to their policy areas. Research findings on Christian, non Christian and Inter-faith group’s contribution to engagement with and barriers to engagement with Government were presented at the conference. The ultimate output of the work will be a policy framework for engagement with consideration given to any changes in approach needed to facilitate this. VCU officials have met with the Inter-faith Liaison Officer in Scotland and will also be meeting representatives from Taoiseach’s Office to discuss their current dialogue with faith based organisations.
13. This work will make a significant contribution to the area action specifically related to the churches and religious bodies.
14. Through VCU, DSD has overall responsibility for volunteering issues across Government. An extensive range of voluntary organisations provides practical support and counselling services for people across Northern Ireland. A number of these organisations are funded by VCU under the Community Volunteering Scheme. Volunteering can also give individuals a sense of purpose, involvement in the local community and a range of skills and experiences. Under the Volunteer Bureau Initiative, VCU also funds 15 local Volunteer Centres to promote volunteering and develop volunteering opportunities, to enable individuals to make a contribution to improving the quality of life in their communities.
15. VCU also supports numerous organisations and initiatives through a range of funding programmes. The support provided through these programmes ensures that Voluntary and Community organisations have the ability to provide valuable activities and services to communities. A large number of regional and sub-regional support organisations are assisted through these programmes. The range of programmes is at Annex 2.
Social Security Agency (SSA) & Child Support Agency (CSA)
16. DSD’s Permanent Secretary and the two Chief Executives of Social Security Agency and the Child Support Agency are co-signatories along with others to the Northern Ireland Prison Service’s resettlement strategy which was published in 2004. They provide universal services which target the most needy. A supporting Implementation Plan was subsequently launched by Ministers in the spring of 2005. The purpose of this strategy and implementation plan is to prevent re-offending by prisoners following their release from custody. The SSA has membership on a multi Agency steering group set up to oversee the implementation of the recommendations within the strategy. In conjunction with Prisons Resettlement Branch, NIACRO and the three main prisons we have implemented a number of practical measures supporting the overall strategy – these include:
- The identification of barriers to prisoners and their dependents in accessing the benefits system on entering or leaving prison and the simplification and speed of that process;
- The provision of awareness and training to staff in NIACRO and the three prisons on the range of benefits available to prisoners, conditions of entitlement and how to help prisoners complete claim forms prior to or on release to ensure they have access to funds;
- The provision of part funding of a benefits advice service across all three main prison establishments for the 07/08 year to enable benefit queries to be resolved, and;
- The agreement of a mechanism for monitoring and review against resettlement targets with partners in the strategy.
17. Although not specifically linked to the work of the Suicide Prevention Strategy, anything that can prevent an individual (particularly vulnerable ones) to contemplate suicide through lack of access of financial resources needs to be encouraged. Again this work will contribute significantly towards the actions identified under Prisoners within the Strategy’s Action Plan and the SSA and CSA are open to receiving the advice of SSIB to help in further improvement of services and access to services.
Annex 1
The 36 Neighbourhood Renewal Areas
Belfast Regeneration Office Neighbourhood Renewal Areas
1 |
Andersonstown |
Andersonstown |
2 |
Colin |
Poleglass, Twinbrook |
3 |
Crumlin/Ardoyne |
Ardoyne, Lower Oldpark, Cliftonville. |
4 |
Falls/Clonard |
Divis / Hamill / John Streets, Roden St Estate, Clonard/ Falls, Cavendish, Fort/ Forest Streets, Beechmount, Donegal Road (North), Iveagh , Broadway. |
5 |
Greater Shankill |
Lower Shankill, Mid Shankill / Woodvale, Upper Shankill , Ainsworth, Glencairn, Ballygomartin Road |
6 |
Inner East Belfast |
Short Strand, Lower Newtownards Rd Albertbridge Road, Albertbridge / Beersbridge, The Mount, Woodstock Road , Lower Ravenhill Road, |
7 |
Inner North Belfast |
Duncairn, Limestone Road, Mountcollyer, New Lodge, Unity/Carrick Hill |
8 |
Inner South Belfast |
Markets, Donegall Pass, Lower Ormeau |
9 |
Ligoniel |
Ligoniel |
10 |
Outer West Belfast |
Lenadoon, Glencolin Estate |
11 |
Rathcoole |
part of Rathcoole Estate, Carmeen Drive / Rathmore Drive |
12 |
South West Belfast |
Sandy Row, Lower Donegall Road, The Village, Roden St. |
13 |
Tullycarnet |
Kinross, Melfort, Vionville |
14 |
Upper Ardoyne / Ballysillan |
Silverstream, Wheatfield, Glenbryn |
15 |
Upper Springfield / Whiterock |
Ballymurphy, Springhill, Whiterock ‘Rock’ Streets, Turf Lodge, New Barnsley, Dermot Hill, Moyard, Springfield Park. |
North West Development Office Neighbourhood Renewal Areas
16 |
Cityside |
Bogside, Brandywell, Creggan and the Fountain |
17 |
Outer North |
Greater Shantallow |
18 |
Outer West |
Ballymagroarty, Hazelbank, The Glen and Rosemount |
19 |
Waterside |
Top of the Hill, Irish Street, Clooney, Tullyally, Curryneirin, Bond Street, The Triangle and Caw |
20 |
Limavady |
The Neighbourhood Renewal Area will be on the western side of Limavady and will include the Hospital Lane, Greystone Park and Roeview Park areas |
21 |
Strabane |
The main part of this Neighbourhood Renewal Area will take in the Fountain, Springhill Park and Ballycolman estates. |
Regional Development Office Neighbourhood Renewal Areas
22 |
Armagh |
The Neighbourhood Renewal Area will be on the western side of Armagh City and will include the Callanbridge Park, Mullacreevie and Drumarg estates. |
23 |
Ballyclare |
The Neighbourhood Renewal Area will cover the Grange and Thornhill estates in the northern part of Ballyclare. |
24 |
Ballymena |
The Neighbourhood Renewal Area will be based around the Ballykeel and Ballee estates. |
25 |
Bangor |
The Neighbourhood Renewal Area will be on the south western outskirts of the town, centred on the Kilcooley estate. |
26 |
Brownlow |
The Neighbourhood Renewal Area will cover a number of estates that are part of the Brownlow development. |
27 |
Churchlands |
This Neighbourhood Renewal Area will be based on Churchland ward on the western side of Coleraine, which includes the Heights and Killowen housing estates. |
28 |
Coalisland |
The Square; South of Mourne Avenue; Newtownkelly; Part of Gortgonis Road; Part of Annagher Road; Inishmore Park. |
29 |
Coleraine (East) |
This Neighbourhood Renewal Area will be based around the Ballysally and Millburn estates on the eastern side of Coleraine. |
30 |
Downpatrick |
The Neighbourhood Renewal Area will be based around the Flying Horse ward and will take in the Model Farm, New Model Farm and Flying Horse estates and some other parts of the town. |
31 |
Dungannon |
The Neighbourhood Renewal Area will be to the south and west of Dungannon town centre and will include the Ballygawley Road estate. |
32 |
Enniskillen |
The Island and Derrychara Link; Windmill Heights/Windmill Drive; Rossory Church Road; Willoughby Place/The Brook; Cornagrade and Kilmacormick 1 |
33 |
Lurgan |
The Neighbourhood Renewal Area will be on the western side of Lurgan and will include areas such as Edward Street, Hill Street and Russell Drive. |
34 |
Newry |
The Neighbourhood Renewal Area will take in a large part of the central and western areas of Newry. It will include the Derrybeg, Carnagat, Daisy Hill and Mourneview Park estates and a number of other areas. |
35 |
North West Portadown |
The Neighbourhood Renewal Area will be on the north western side of Portadown and will take in the Obins Street, King Street, Churchill Park and Woodside areas. |
36 |
Omagh |
The Neighbourhood Renewal Area will be in the centre of Omagh and will take in the Gallows Hill and Campsie Road areas. |
Annex 2
Voluntary and Community Unit Programmes
Programme |
|
1. |
Areas at Risk |
2. |
Community Support Programme |
3. |
Community Volunteer Scheme |
4. |
Comunity Investment Fund |
5. |
Interreg 3.1 |
6. |
Modernisation Fund Revenue |
7. |
Modernisation Fund Capital |
8. |
Regional Infrastructure Programme |
9. |
Renewing Communities (various) |
10. |
Volunteer Bureau Initiative |
11. |
Local Community Fund |
Royal College of Nursing Northern Ireland
Introduction
1 RCN Northern Ireland welcomes this opportunity to submit evidence to the Committee on the issue of the prevention of suicide in Northern Ireland and wishes to convey our gratitude for the opportunity to do so. We hope that our comments will prove helpful to the Committee in its Inquiry and we commend the Committee for its attention to this issue.
2 The primary focus of our submission is the four key themes identified by the Committee in its call for evidence. As the largest professional group within health and social care, and the practitioners that spend the greatest amount of their professional lives in direct contact with patients and clients, nurses are central to the delivery of effective strategies to prevent suicide in Northern Ireland.
3 It is not our intention to seek to outline in this submission the extent, nature and causes of suicide in Northern Ireland. The Committee will already be familiar with the essential information and this is, in any event, more than adequately documented in chapters 1 and 2 of Protect life: a shared vision, the Northern Ireland suicide prevention strategy and action plan.
4 RCN Northern Ireland welcomes the considerable political and media attention that has been focused upon the issue of suicide prevention over the last two years, most significantly by the current Minister for Health, Social Services and Public Safety and also by his two immediate direct rule predecessors. We also welcome the fact that all the major Northern Ireland political parties referred to the need to address suicide and appropriately fund related health and social care services in their manifesto commitments prior to the March 2007 Assembly election. The cross-party and cross-community consensus that exists in relation to the importance of tackling this issue is an indispensable basis upon which progress can be made.
The scope and appropriateness of the Department’s strategy Protect life: a shared vision, the Northern Ireland suicide prevention strategy and action plan
5 RCN Northern Ireland commented favourably upon the draft strategy and, eighteen months later, we believe that it remains a credible document. Its strengths lie in its recognition that there are no simple and immediate solutions that can somehow be enacted unilaterally by government. Tackling suicide is a complex issue that can only be pursued incrementally and in partnership with a wide range of stakeholders, organisations and individuals. RCN Northern Ireland also welcomes the strategy’s inherent link between suicide prevention and wider mental health service provision, its analysis of the merits of mental health promotion and the de-stigmatisation of mental ill health, and its recognition that suicide affects a broad range of marginalised, disadvantaged, abused and, in Northern Ireland, terrorised individuals and social groups. Media and popular stereotyping of the ‘typical’ suicide victim is unhelpful in this regard, for reasons elaborated upon at paragraph 15 below.
6 We would urge the Committee to note that the DHSSPS strategy seeks to address the issue of self-harm as well as suicide. The two issues are broadly linked but not necessarily mutually inter-dependent.
7 In summary, whilst any strategy document of this nature and complexity should regularly be reviewed, revised and updated, RCN Northern Ireland believes that its analysis of the issues and associated action plan are inherently sound. What needs to be addressed is its further implementation and associated resourcing. The Committee, we believe, can play a significant role in helping to guide this process.
The level of stakeholder involvement
8 The strategy itself derives from widely-publicised direct discussions between a former direct rule health minister and the relatives of suicide victims. It also displays strong evidence of involvement and input from a wide range of organisations, individuals and communities. Chapter three, particularly at paragraph 3.9, clearly references the need for close co-operation between different government departments, public sector organisations, and communities, organisations and the voluntary sector. In this respect, the strategy’s commitment to stakeholder involvement can not be faulted.
9 What is less clear, however, is the extent to which this co-operation is manifesting itself in the implementation of the strategy. RCN Northern Ireland believes that the leadership and personal commitment being shown on this issue by the Minister for Health, Social Services and Public Safety is exemplary. We also welcome the support for the strategy, and for parallel initiatives at an All-Ireland level, that have been articulated by a range of individual Assembly Members. However, and despite the fact that the broader issue of suicide arguably touches upon the responsibilities of every single Stormont department, there is no discernible evidence of the inter-departmental commitment that the strategy envisages. It is difficult to avoid the conclusion that the Northern Ireland Executive appears to regard suicide and suicide prevention solely as a health issue, when it is in fact far broader. RCN Northern Ireland would like to see this re-dressed in the forthcoming Programme for Government and recommends that the Committee may wish to press the case for a far more visible and productive level of inter-departmental and inter-ministerial partnership working in this respect.
10 We also note the recent comments made by Colm Donaghy of the Northern Ireland Suicide Prevention Taskforce in relation to the lack of training undertaken by general practitioners on suicide prevention. This echoes one of the key recommendations in the strategy’s associated action plan in relation to health and social care staff training. It would not be appropriate for the RCN to comment upon an issue relating to another health profession but, in relation to our own nursing and health care assistant membership, we would draw the Committee’s attention to the fact that, during times of financial challenge, one of the initial reactions of the health service is routinely to curtail staff in-service training. It is essential that such training takes place on a multi-disciplinary basis and equally important that it is appropriately resourced, evaluated and reviewed.
Services and support available to promote good mental health, to prevent suicide and self-harm and to support those affected by suicide
11 RCN Northern Ireland believes that this is the key issue requiring attention if the strategy is successfully to be delivered. The Minister has committed time, attention and departmental resources (estimated at £3 million for the current financial year alone) and it is right that this should be acknowledged and welcomed. However, the Minister himself has only this week drawn attention to the gross under-funding of health and social care services, and particularly mental health services, in Northern Ireland. The fact is that there are nowhere near enough mental health nurses to ensure that the suicide prevention strategy, the associated DHSSPS Promoting mental health strategy and action plan, or the various recommendations of the Bamford Review, are delivered. The most recent DHSSPS workforce census confirms, for example, that there are 367 community psychiatric nurses, of whom 42 work part-time, covering the whole of Northern Ireland. This is hopelessly inadequate.
12 The DHSSPS has recognised this problem and is about to launch, with the support of RCN Northern Ireland and others, a recruitment campaign for mental health nursing that will seek to address the large number of vacant mental health nursing training place that are currently available and the large number of unfilled mental health nurse vacancies that exist within the health and social care services. Without significant levels of renewed and enhanced investment, however, recruiting more nurses (and other practitioners) to what the Minister himself has described as “a Cinderella service” will fail to address the underlying problems. There is substantial political, professional and social consensus across all sections of Northern Ireland society on the need to enhance the funding and support of services for these most vulnerable members of our community. RCN Northern Ireland urges the Committee to address, as a matter of urgency given the imminent budgetary announcements and consultation, with the Assembly, the Department of Finance and Personnel, and ultimately with the full Northern Ireland Executive, the need to secure and maintain appropriate levels of investment in mental health and suicide prevention services.
Consider what further action is required, taking account, as appropriate, of experience elsewhere
13 Separate suicide strategies already exist in England and Scotland but in many respects these simply reflect the same aims and objectives set out in Protect life: a shared vision, the Northern Ireland suicide prevention strategy and action plan. We would also draw the attention of the Committee to guidance on suicide prevention published by the World Health organisation [WHO]. This emphasises the value of effective interventions, whereby strategies involving the restriction of access to common methods of suicide have proven to be effective in reducing suicide rates. They also emphasise the need to adopt multi-sectoral approaches involving other levels of intervention and activities, such as crisis centres.
14 The WHO also stresses that there is compelling evidence to indicate that adequate prevention and treatment of depression, alcohol and substance abuse can reduce suicide rates. Finally, school-based interventions involving crisis management, self-esteem enhancement and the development of coping skills and healthy decision-making have been demonstrated to reduce the risk of suicide among young people.
15 Partly as a consequence of media coverage of the suicide issue, a popular stereotype has emerged of the ‘typical’ suicide victim. Whilst RCN Northern Ireland welcomes strategies designed to support all suicide victims and potential victims, we believe that this stereotyping had led to a tendency to neglect those who are victims or potential victims for medical, as opposed to social, reasons. Primarily this would comprise people with severe and persistent mental health problems and also elderly people with depression and other mental health problems. In simple terms, suicide is not always a social issue; it may also be a health issue.
16 With those for whom suicide or suicidal tendencies are founded in social alienation of one form or another, the problems and solutions are often complex, multi-faceted and necessitate inter-professional and inter-agency working. For client groups in whom suicide or suicidal tendencies are more closely associated with their ill-health, the solutions may be more tangible and this is where nursing has a key role to play in the assessment, treatment and recovery process. RCN Northern Ireland believes that, although Protect life: a shared vision, the Northern Ireland suicide prevention strategy and action plan recognises the link between suicide and mental ill health, insufficient attention is currently being paid towards supporting the nursing and other health care professionals that are best placed to provide the necessary assessment, treatment and support for these vulnerable client groups.
Summary
17 The key recommendations made by RCN Northern Ireland to the Committee are summarised as follows.
- Protect life: a shared vision, the Northern Ireland suicide prevention strategy and action plan provides an appropriate template for addressing the issues.
- The strategy and action plan need to be appropriately resourced and the Committee should play a leading role in helping to lobby for this funding.
- The levels of stakeholder involvement are appropriate but there is little evidence of the necessary inter-departmental commitment, co-operation and leadership at an Executive level. The Committee could and should play a leading role in helping to secure this.
- The implementation of the strategy is being hampered by a severe shortage of mental health nurses, particularly those practising within community settings.
- The funding of mental health and learning disability services in Northern Ireland is, as the Minister has recently observed, wholly inadequate. Again, we believe that the Committee can play a leading role in helping to ensure that this is addressed in a sustainable manner at an Assembly and Executive level.
- Investment should be targeted at effective intervention strategies, particularly through crisis centres, mental health and addiction services and through communicating effectively with children and young people. RCN Northern Ireland believes that school nursing could play a significant role in this regard in partnership with other stakeholders and organisations.
- Service provision must be developed and maintained for all potential victims, whether the underlying causes are social, medical or a combination of the two.
- The unique contribution that nurses can make to the assessment, treatment, support and recovery of potential suicide victims should be more widely recognised and appropriately resourced.
Conclusion and further information
18 RCN Northern Ireland reiterates our gratitude to the Committee for inviting this submission and we hope that our comments will prove helpful to the Committee in the conduct of its Inquiry.
19 For further information about the work of the RCN in support of nurses and patient services in Northern Ireland, please contact Dr John Knape, RCN Northern Ireland Head of Communications and Policy, at john.knape@rcn.org.uk or by telephone on 028 90 384 600.
October 2007
Retrieve Foundation Mental Health Forum
Thank you for inviting our comments on the Department’s strategy
“ Protect life: a shared vision.
As a member of the Retrieve Foundation Mental Health Forum and with the Bean Feasa na hEireann and a number of other Retrieve members I met Mr. Maxwell at Castle Buildings on 14th September 2007.
Mr Maxwell gave us background information to the Suicide Prevention Strategy and how the Government had responded to the alarming increase in suicide rates.
Our group highlighted the lack of spiritual healing available to young people who feel different and suffer from depression, and our hope for an all Ireland suicide prevention strategy.
A helpful exchange of information followed and Mr Maxwell suggested our group meet with the National Office for suicide prevention ( Southern Government ) with Mr Geoff Day as a contact person. Mr Maxwell indicated his willingness to attend.
The Retrieve Foundation recognises the elements covered by the task force and the work of the Commission to date.
It is just recently that we have been approached and asked to associate with the Commission as we share the same overall aim which is to reduce the suicide rate in Ireland.
Retrieve Foundation.
The Retrieve Foundation was founded by Bean Feasa na hEireann, Margaret Connolly, about 20 years ago with aims to educate by providing a programme of activities to enhance the development of the social and cultural needs of the people of this land and “ to create a safe place for people to reconnect with their own innate nature. Our own indigenous ways have been activated over the past 13 years throughout Ireland both North and South “ Retrieve.
The Foundation strives to teach ethical practices and to enlighten young people in many areas of life that could not be achieved through other education systems. It also aims to support families in a time of changing family structure.
The Foundation’s Mental Health Forum is based on deep concern about the high incidence of suicide, depression and self harming behaviour among young people.
All groups in our society are affected by it. Anyone can develop a mental health problem and become suicidal. This is a national problem.
At Retrieve we understand that our human nature is predisposed to be happy and peaceful and our programmes are organised to achieve this for those who come seeking healing.
Department’s strategy.
The strategic approach has resulted in obtaining valuable information.
Working together to obtain support from counterparts in the Republic of Ireland and Great Britain was most appropriate, as was the approach in engaging with the public, bereaved families, local churches, coroners, prison service, police service and the Northern Ireland Commissioner for Children and Young People.
The twelve week public consultation period and workshops and consultations with health professionals in both the voluntary and statutory sector were also most appropriate.
The analysis of suicide and self harm provided data over a five year period which will be available for comparisons with subsequent periods.
Intervention.
The report found limited evidence available in relation to the effectiveness of reducing the risk of suicide and self harm.
Some studies produced conflicting results.
We believe that the manner in which people with psychiatric problems are diagnosed and labelled must change to a more holistic approach. It is recognised in the report that the Strategy’s key aim cannot be met by Health and Social Services alone and that the onus is on all interested and responsible members of our society.
At Retrieve we agree with this and have adopted a programme which is Holistic in approach (Mind, Body, Spirit,)
This programme offers a safe place for individuals to connect with their own innate Devine Natural Ability.
It has been our experience that confusion arises in some young people, especially within the 14 – mid twenties age group due to their inability to articulate their Spiritual experiences in a safe place and this often leads to despair.
The most difficult pain in which to live is the pain of Soul loss and this is often compounded by an uncaring family. Soul loss often first presents in alcohol and drug misuse.
Mockery in dismissal in families contributes in no small measure to a person’s despair.
Retrieve Foundation holds that the Women of Ireland are the key to Healing as they carry indigenous traditional knowledge.
Women’s place in society was diminished resulting in the indigenous ways being removed in the consciousness and therefore creating an imbalance, loss of value and innate worth as a holistic person.
The challenge today is to Retrieve the National soul loss – hence the name Retrieve – and connect and correct the imbalance through restoring the indigenous ways.
Our aim is to raise awareness of ancestral healing which according to Retrieve’s founder, Bean Feasa na hEireann is “ a hands on tradition transmitted through presence”
The Report’s Action Plan.
We agree that the action plan in chapter four will play a central role in aiming to reduce death by suicide, and we recognise that a reduction by Health and Social Services cannot be achieved.
There are groups in many communities in Ireland engaging at various levels with bereaved families and young people with self harm tendencies.
This is helpful in many situations but we believe that the medical model within which young people are treated presents problems.
This model labels them and increases the likelihood considering themselves patients and abdicating taking responsibility for themselves instead as seeing themselves as gifted holistic people.
Training has been made available for general practitoners who treat these people and according to the findings of the report a small number attended.
Even where there is a willingness on the part of the general practitoners to undertake specialist training in the area of suicide prevention have they really got time in a busy practice to implement their new training?
We suggest that more practitoners and not specialist groups, as this will further the problem of stigma already present in the current treatment model.
Services
We welcome the approach of various timescales to be used in the promotion of Mental Health – short term, medium/long term and ongoing.
Suicide awareness has been raised in many communities due to the establishment of small groups set up often by families of suicide victims.
It is time now for Social Services and medical personnel to work with voluntary and community groups to provide support and professionalism with an aim to have a “non stigmatising service” available.
We welcome the action plan to take care of school children in promoting positive mental health in an atmosphere in society where children are encouraged to talk and to know that their voice will be heard weather they are victims of abuse at home or in the community or bullying at school.
At Retrieve we believe that there is a need for teachers and parents to have a greater understanding of Spiritually gifted children, and in this context, “people see others, only at the level of their own enlightenment and understanding.” Bean Feasa, M.Connolly.
Retrieve practitoners have undergone an inner Spiritual journey to reconnect with and to heal their own Divine Natural Ability.
This greater depth enables them to relate at a deeper level with love, empathy and respect.
“It takes one instant to hurt, it can take one instant to heal”
Retrieve Foundation is involved in programmes for educating for a peaceful community. Bean Feasa and Retrieve members have contributed to many such programmes in USA, India and South Africa with the Indigenous Spiritual leaders and their respective communities.
The following Programmes are for Teachers.
T.E.A.M. (Teachers of Experimental and Adventure Mythology)
Programme. Leadership within and Leadership without.
Exploring the concept of Leadership.
RAINBOW HOOPS for the NINE GENERATIONS.
Experience useful and practical Healing practices, involving art, dance & storytelling. Encompassing ethnic diversity and environmental awareness. Teachers leave with a valuable tool to help students integrate their Outer world with Inner Peace.
Building and Sustaining Inclusive Organisations.
This emotionally engaging centred programme focuses on the personal and organisational Shifts and Steps necessary towards creating an organisation with teams that are inclusive of all people based on gender, physical ability, religious affiliation, sexual orientation, ethic diversity and age.
Funtime.
No Props, No Problem!
This activity is hands on adventure, a great programme for all ages.
Discovering your DNA (Divine Natural Ability)
The following programmes are for Carers.
“You choose to be the change you wish to see in the World!” Bean Feasa.
This Inner journey is a process of Self-Discovery.
Children don’t care how much I know until they know how much I care.
Is my Destiny my Job or is my Job my Destiny?
This programme is aimed at Carers, to alienate the stress that impedes the caring process.
Birthing.
The greatest act of Creativity and Sacredness in the world is giving Birth.
In midwifing the Baby, we also midwife the Spirit.
How is my energy as a midwife/doctor?
“What is in my Heart, transmits though my touch.”
What print have I left on this new-born Baby?
Death is Transformation.
Midwifing the Spirit back home.
Holding of Sacred Space.
This is an insight into One’s own Sacred Space.
“All creation starts with a single Thought”
“Are my attachments to the outcome interfering with the Spiritual Process?”
John Greenleaf Whittier’s Poem – The Mystery.
“No clue of memory laid me on”
“But well the way I Knew”
“A feeling of familiar things”
“With every footstep grew”
These are questions sometimes asked and answered by the Bean Feasa.
“I don’t know how to become a self-aware person?”
“Is there a practical technique I can practice?”
ANS. Take note of every strong impression you see in yourself during the day. Only the stronger ones, the more emotional ones. Before bedtime, review the passing pictures of the events you observed.
This makes you aware of the contents of consciousness that change you.
Q. I want to help others.
ANS. Please do not go around trying to save the world, get to know your own True self.
“When you know yourself, you know the world, when you heal yourself, you heal the world”
Bean Feasa.
There are many roads to finding your own innate nature. The wisdom of our Grandmothers is all around us, if only we become receptive. When I speak of Receptivity, it is not merely reading about Spiritual ideas. It is not attending lectures, taking courses or teaching others. Many people do these activities for years, yet never change a single thing in themselves.
They are unconsciously trapped by the delusion THAT DOING IS THE SAME AS BEING, but it is NOT, as their daily irritations, nervousness and fears testify.
Receptivity is something entirely different. It is an Inner process that changes your Values and uplifts your Spirit. It is a state of mind that is beginning to Love facts more than falsehoods. It is a total acceptance of one’s self exactly as I am at this present moment in time. It is an Inner Secret process. Don’t take the difficult as impossible, courageously abandon your fixed ideas.
We may observe throughout history how society has tried to treat social problems by legislative action, warfare, market manipulation, laws & prohibitions and manifestations of force, only to see these problems to persist or re-occur despite their treatment.
The motivation of Retrieve, knowing the distinction between Force and True Power, knowing this is most important for the purpose to heal the ills of suicide and self-harm on our land.
We should remember, wherever Force meets Power, Force is eventually defeated, as is the difference between Treating and Healing.
Love is knowledge, wisdom and compassion and when we give with love it is accepted and we are endeavouring to share this aspect with the committee.
Force versus Power.
Where there is force there is violence either action, word or thought.
When an individual is forced into a category or labelled this can result in depression as it is a violation of someone’s right to have choice.
Power equates knowledge to correct at all levels the events which cause the distress/illness and maybe historical or ancestral.
The essence of healing is removing energy from events which cause the illness so it no longer exists.
We live in an age of science, but the extraordinary success of science carry with them the danger of thinking that only science is verifiable knowledge, that scientific proof is the only kind of proof that is conclusive, and indeed that science is the only kind of rational knowledge.
Outside of science it is claimed that there is only irrational belief, including Spiritual.
The French philosopher Maurice Merleau-Pony said that the philosophical mission of the twentieth century is to “explain the irrational” and to “integrate it into an enlarged reason”
Retrieve Foundation was founded by Bean Feasa na hEireann, Margaret Connolly with a similar philosophy.
Thanks again for the opportunity to be included and we hope that our comments will be of assistance to your Committee.
Anne Murphy.
Northern Health and Social Services Board
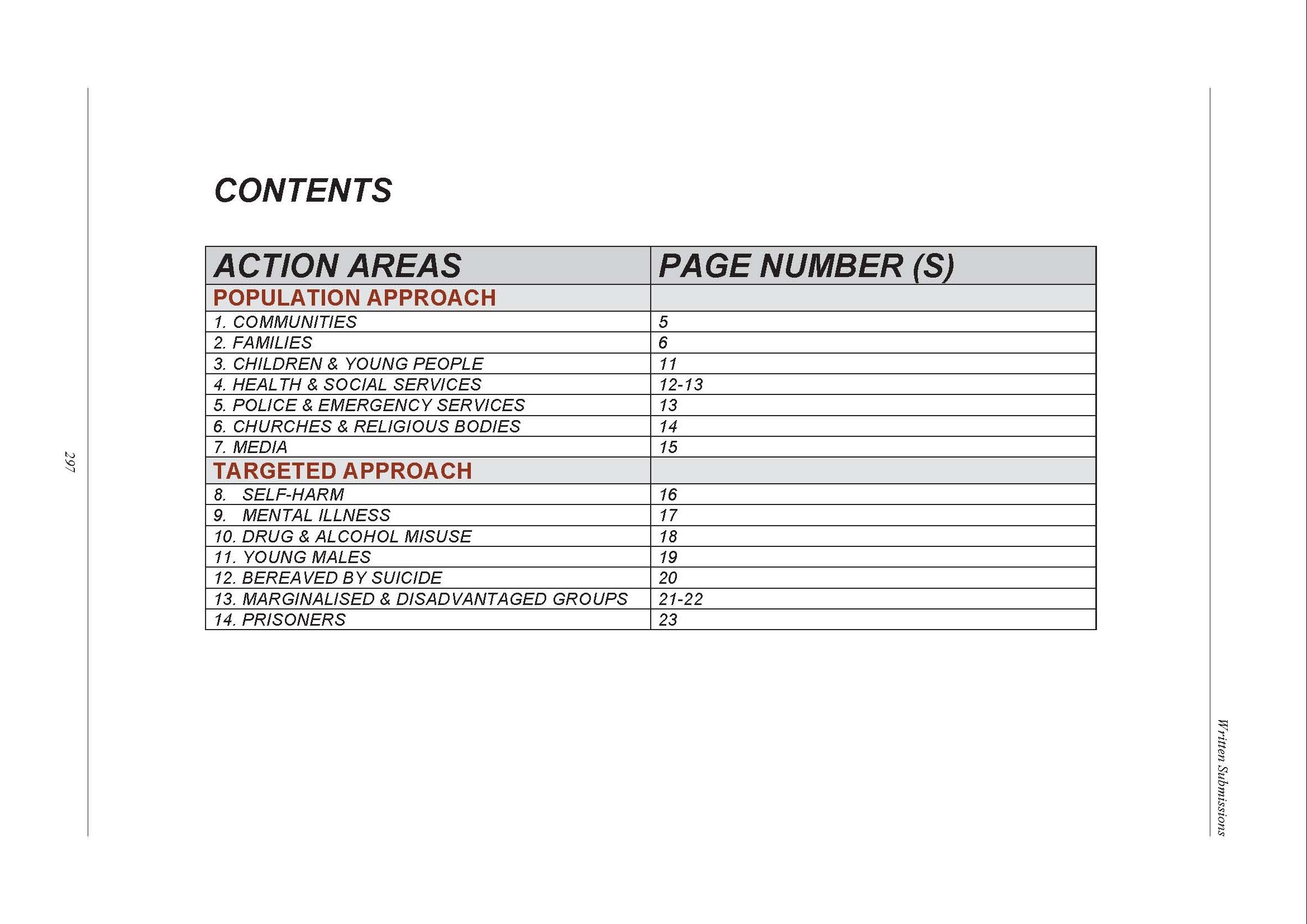

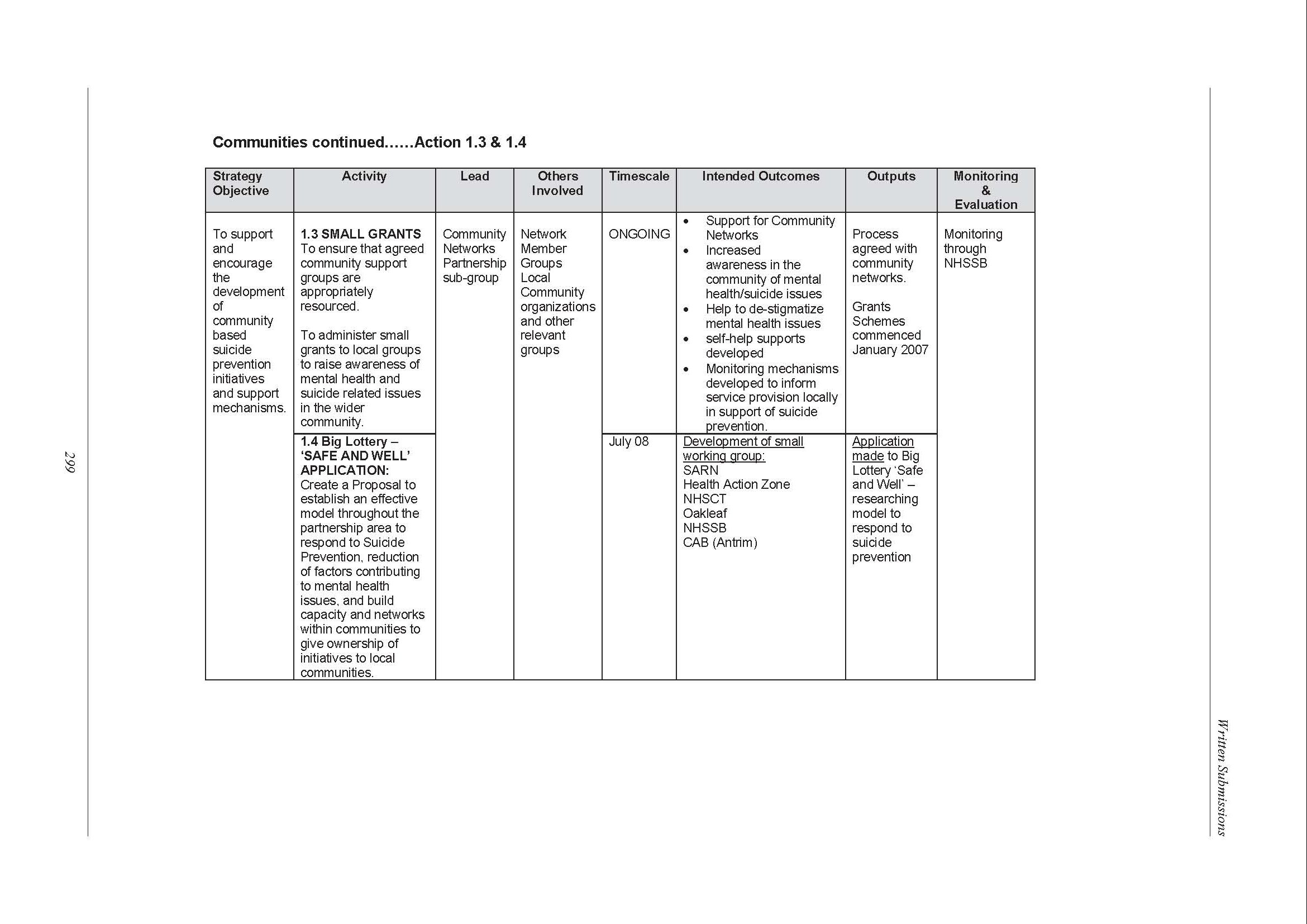
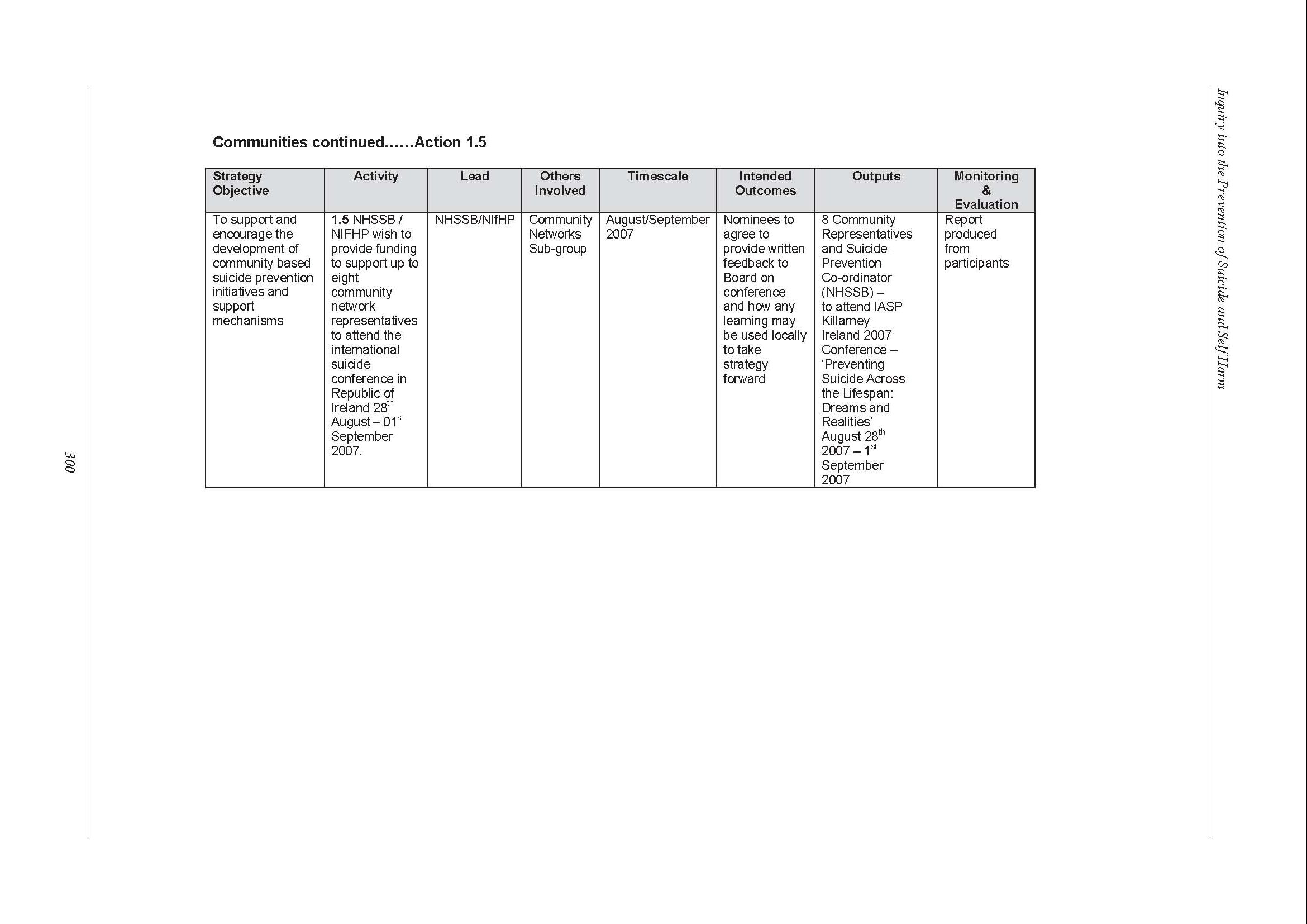
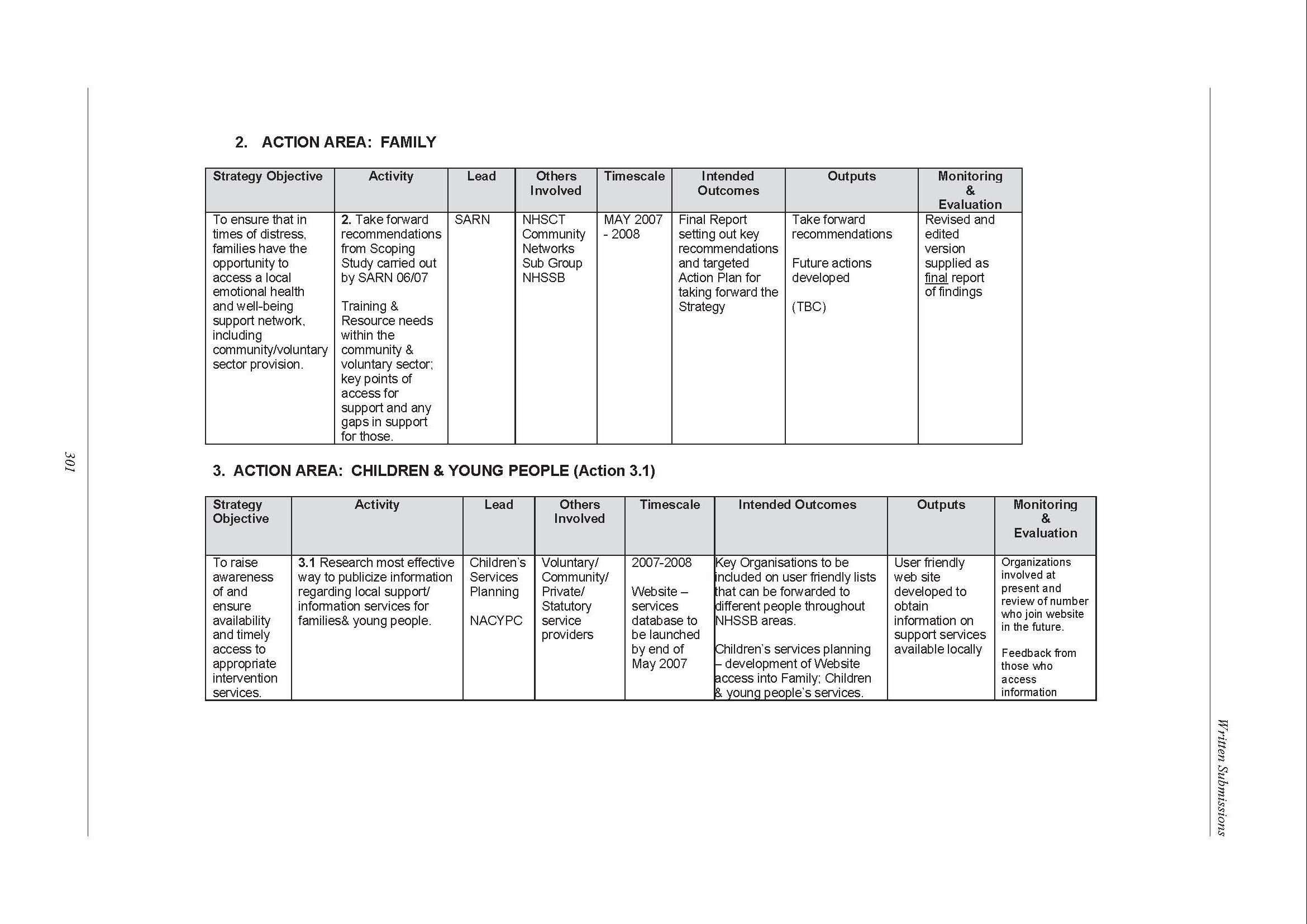
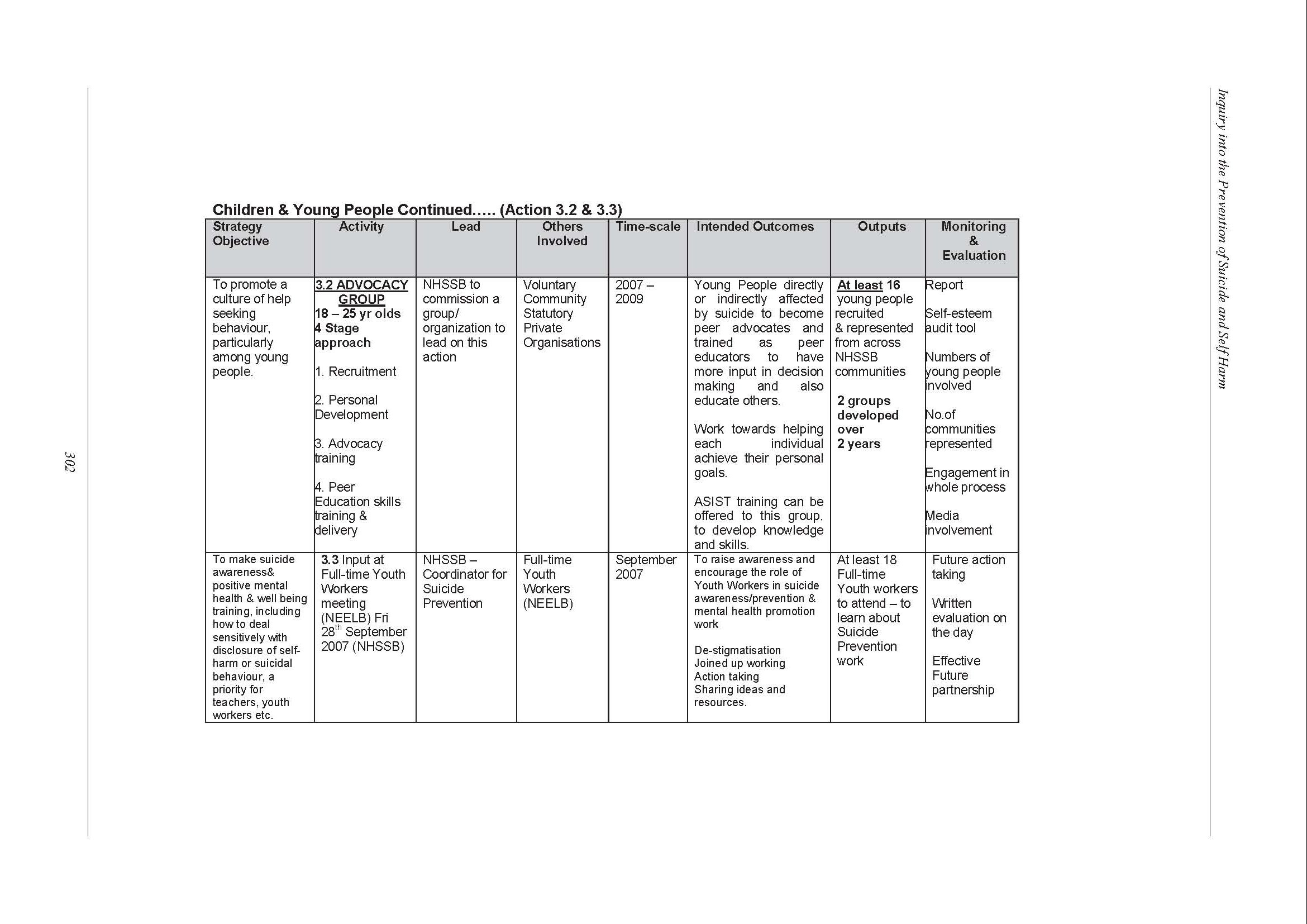
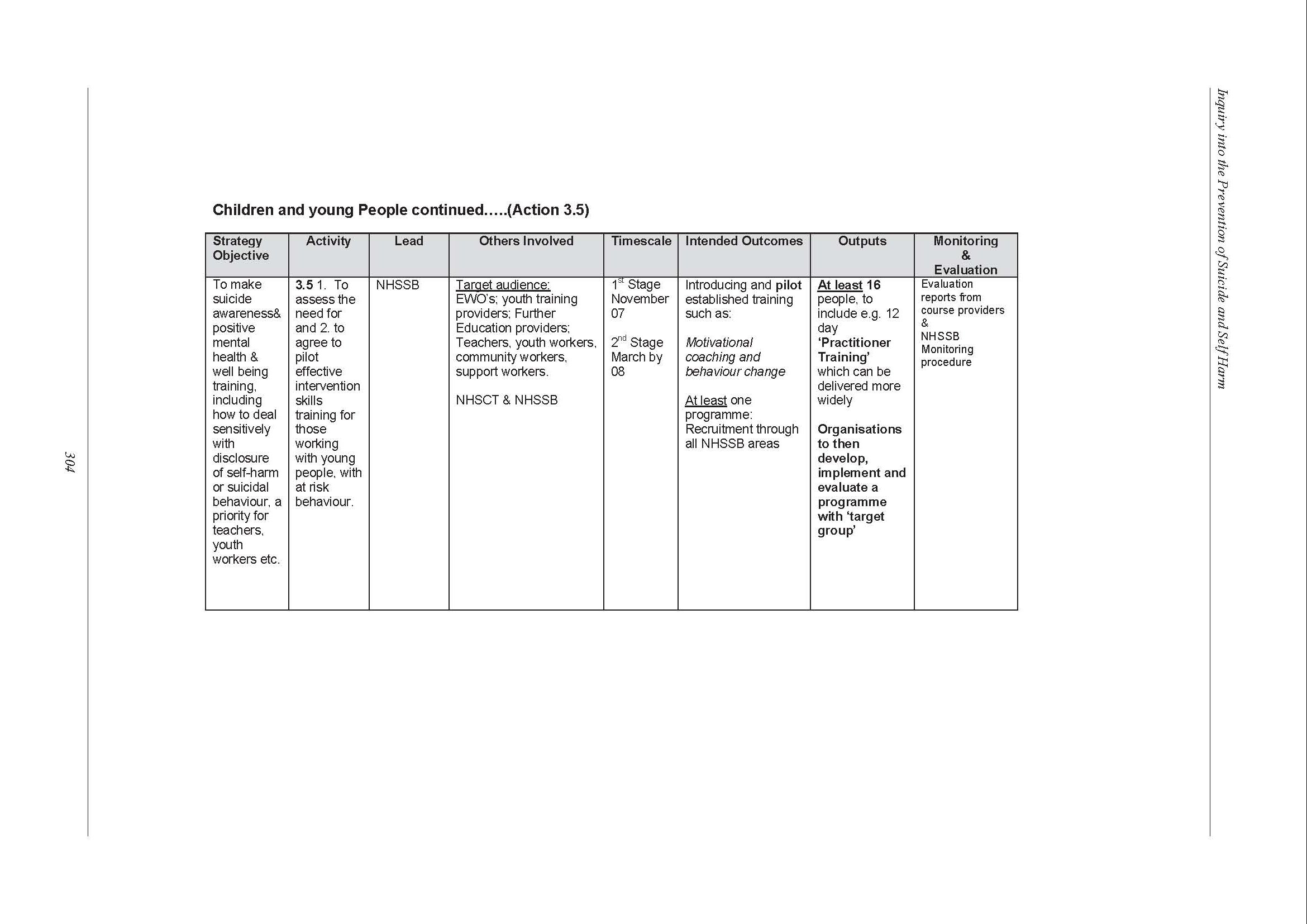

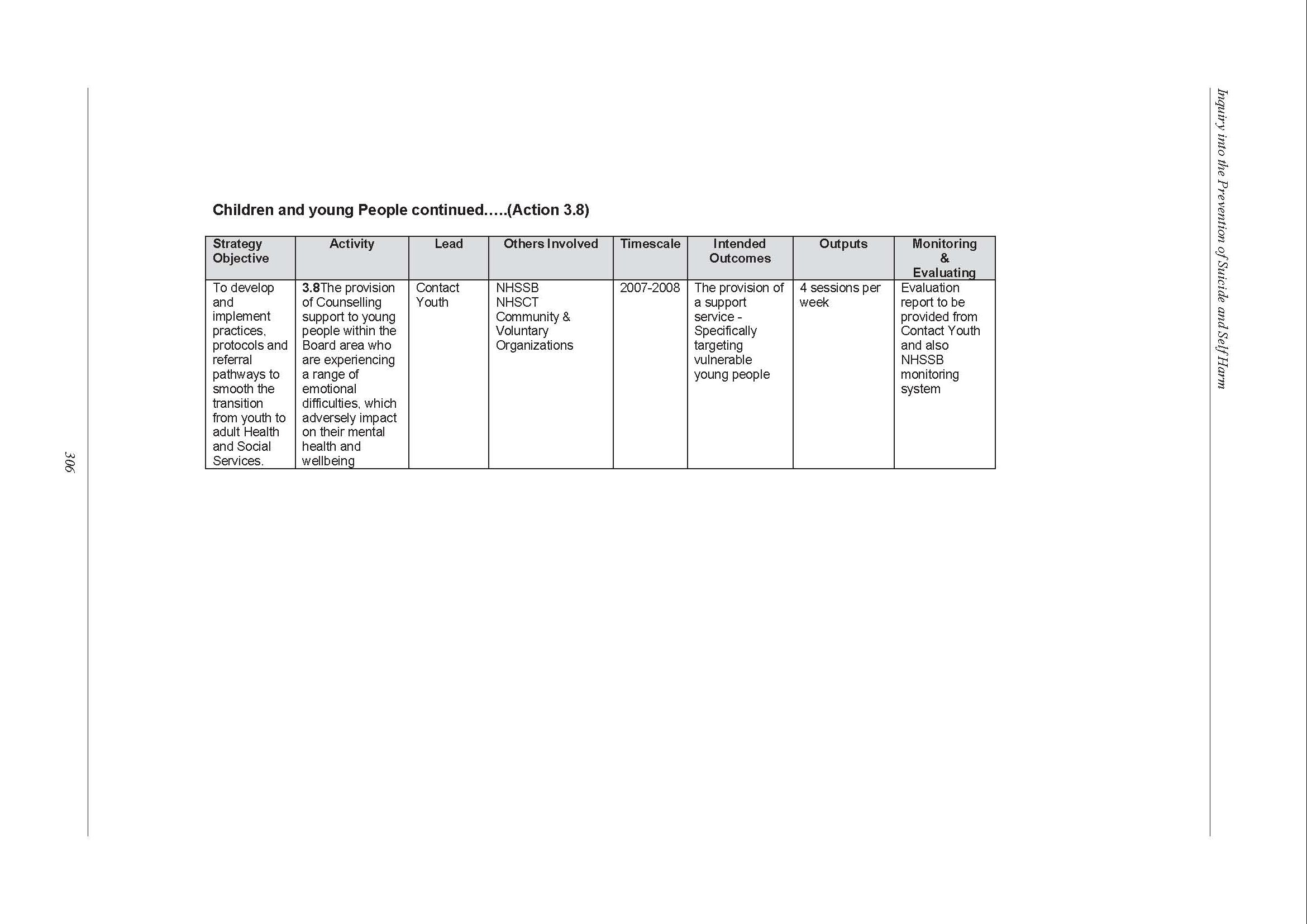
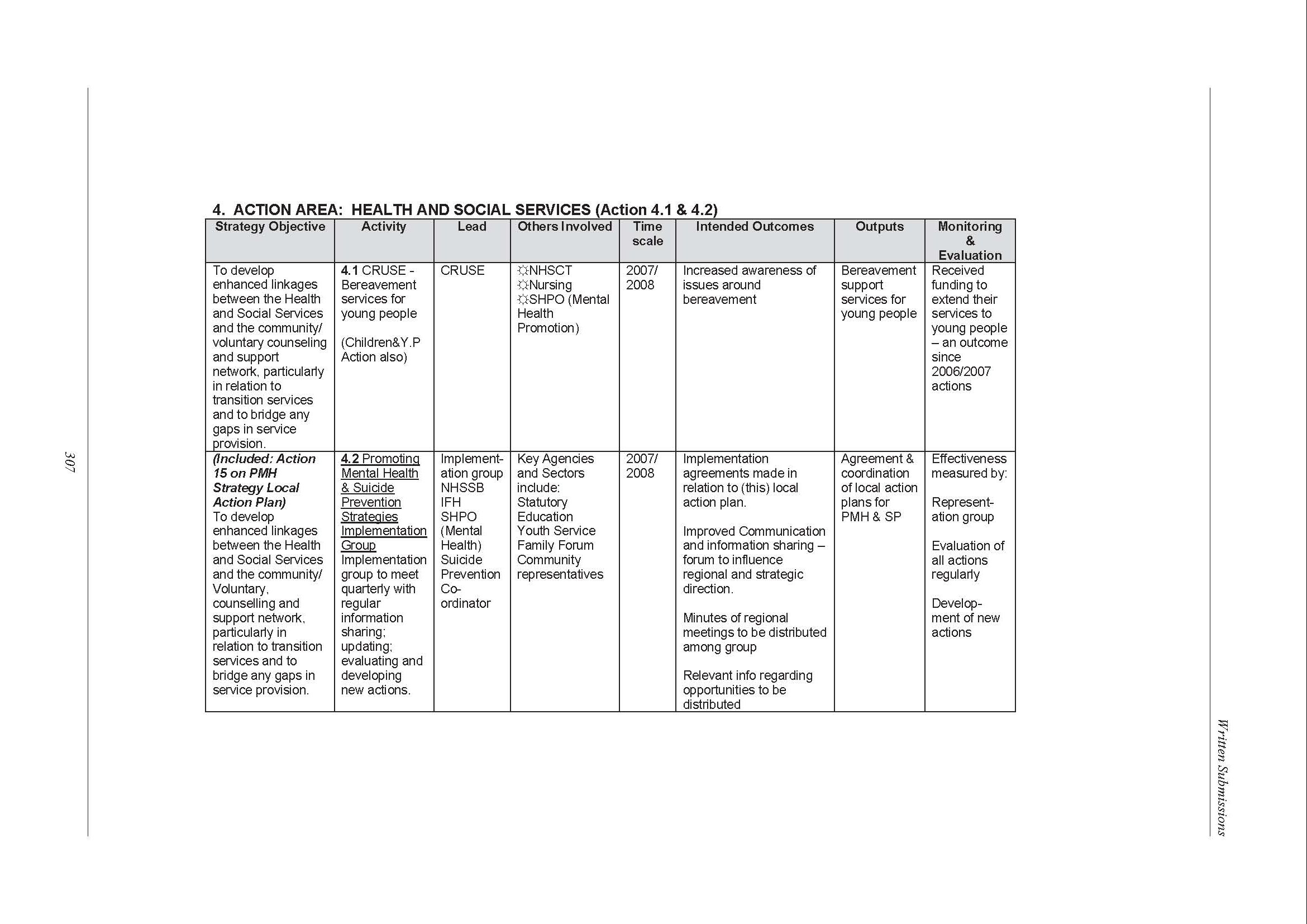
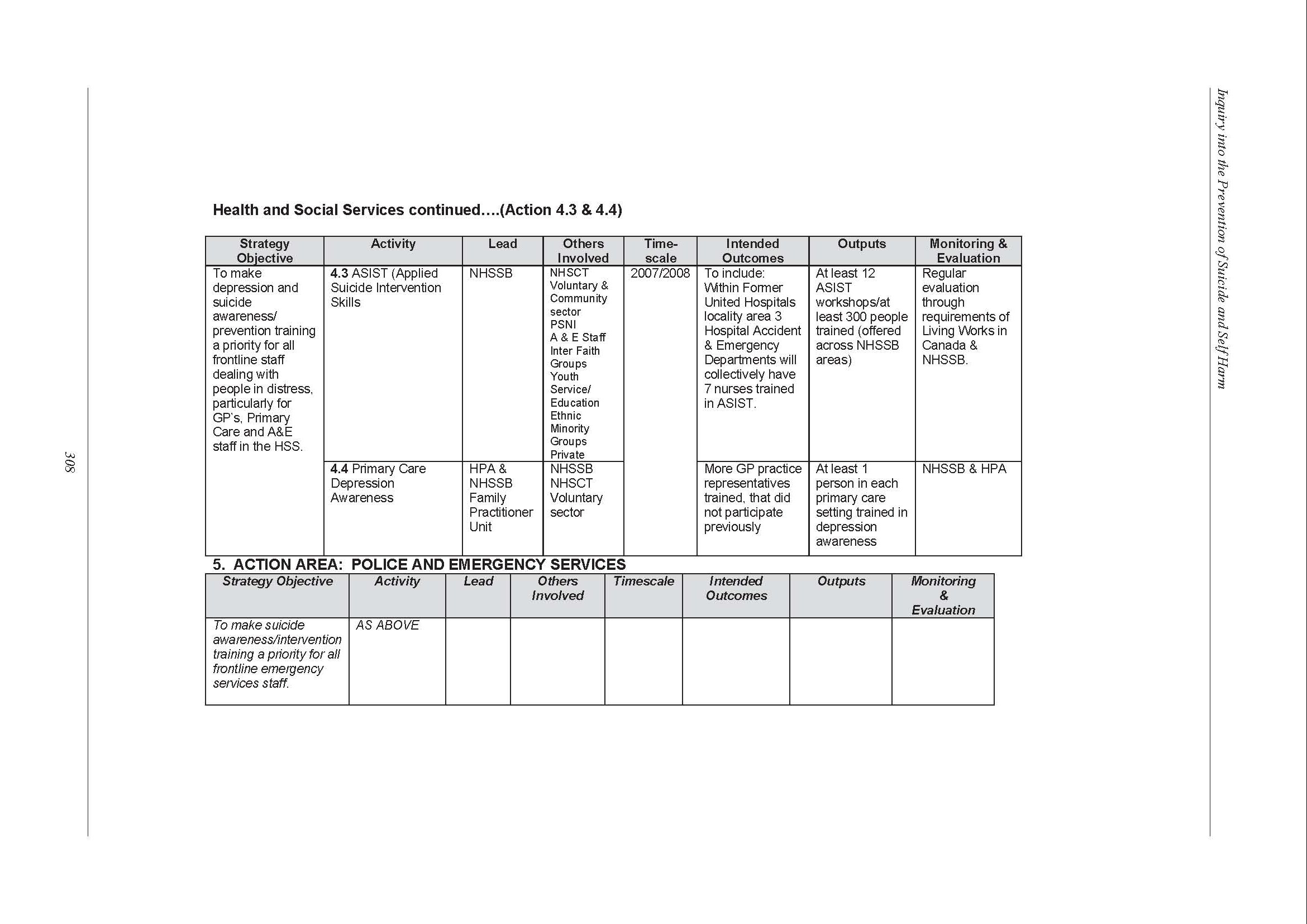
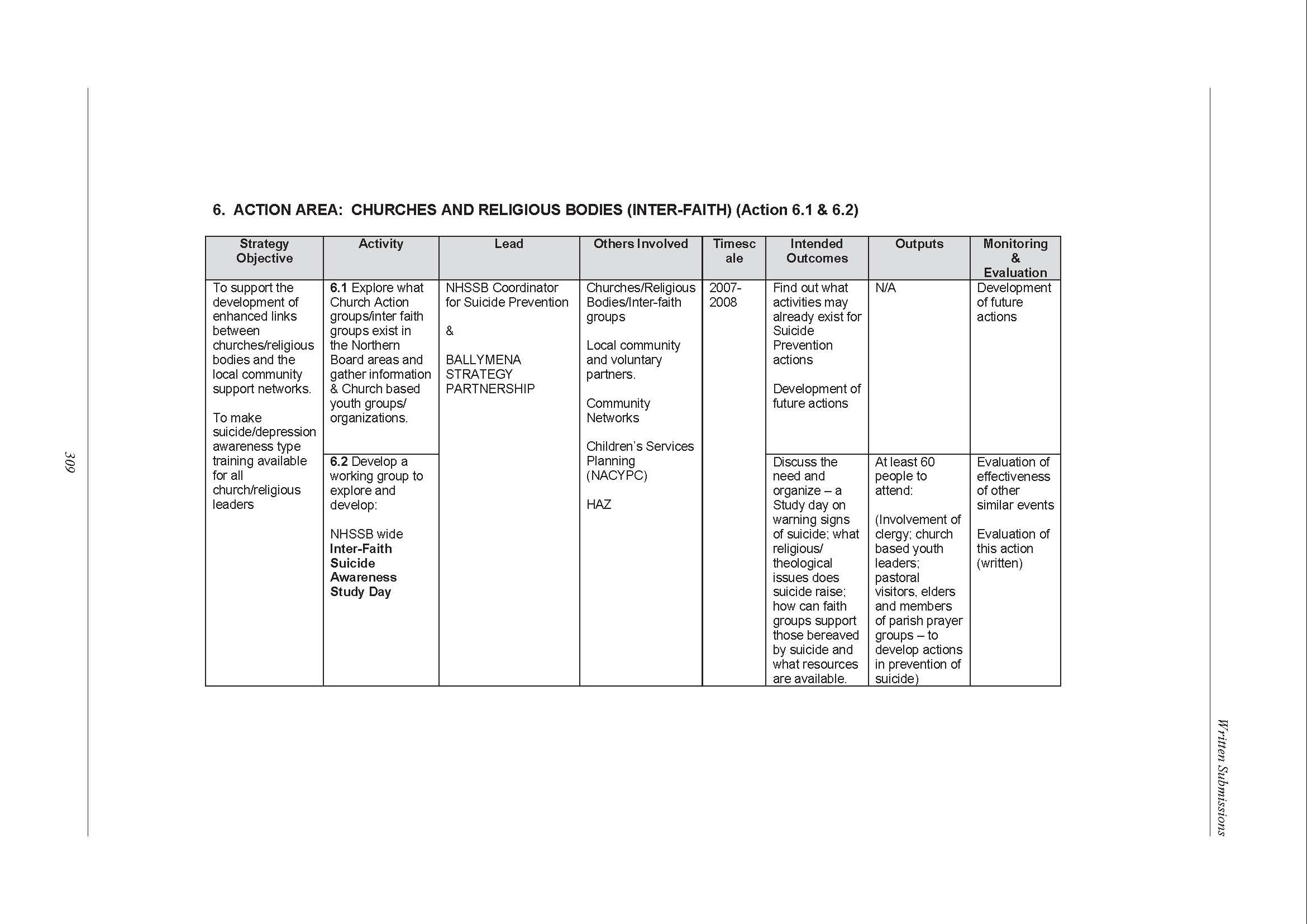
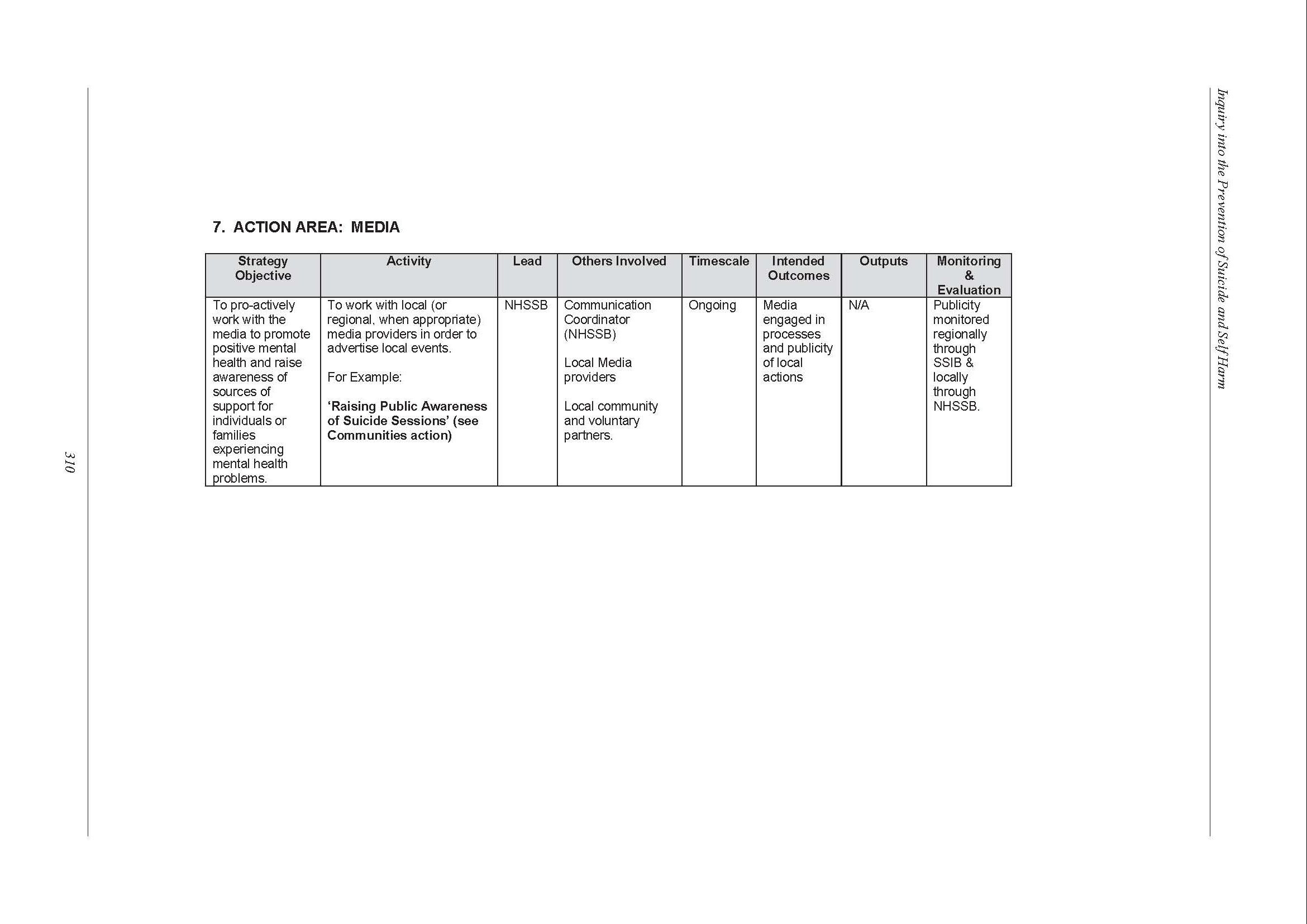
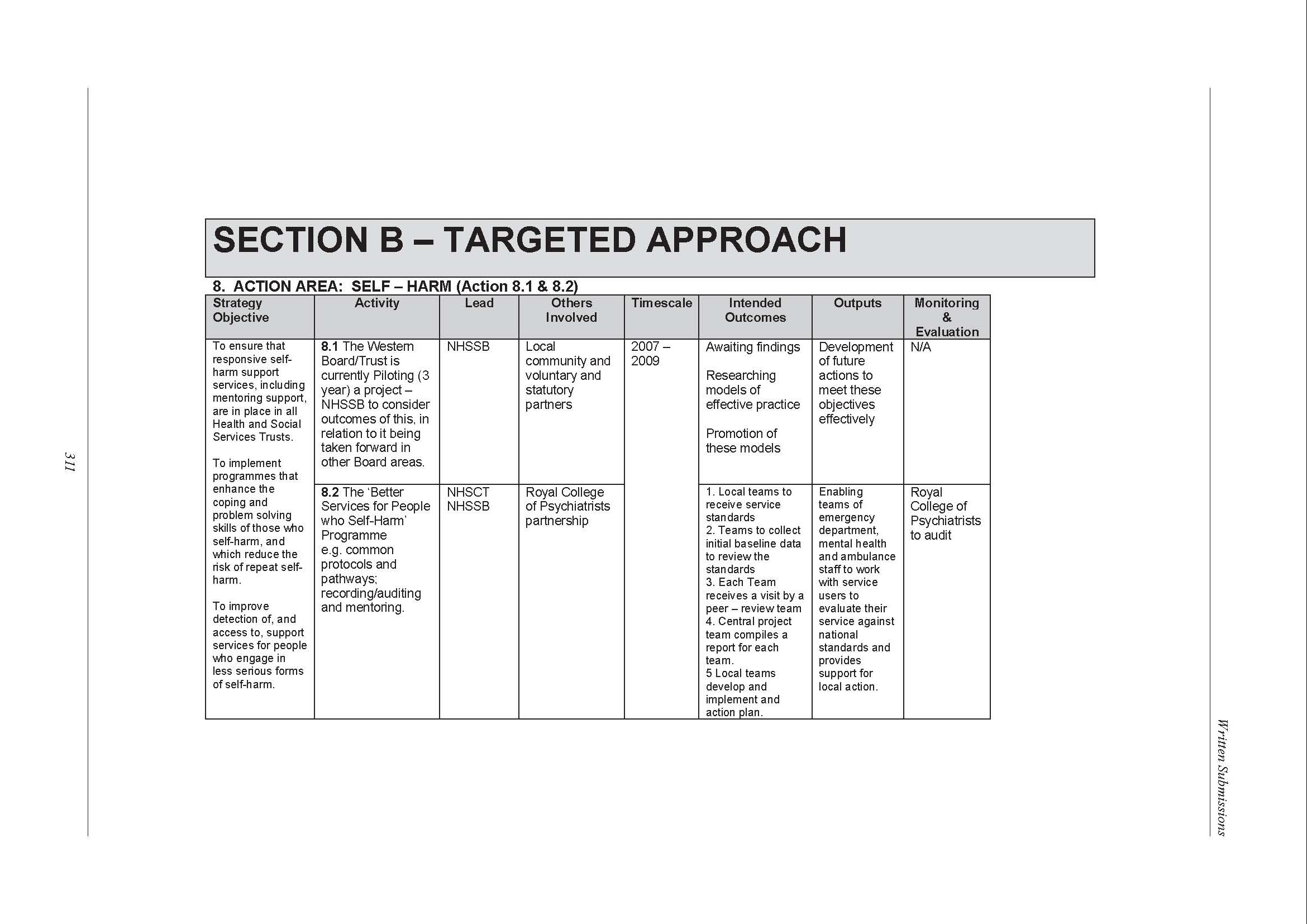
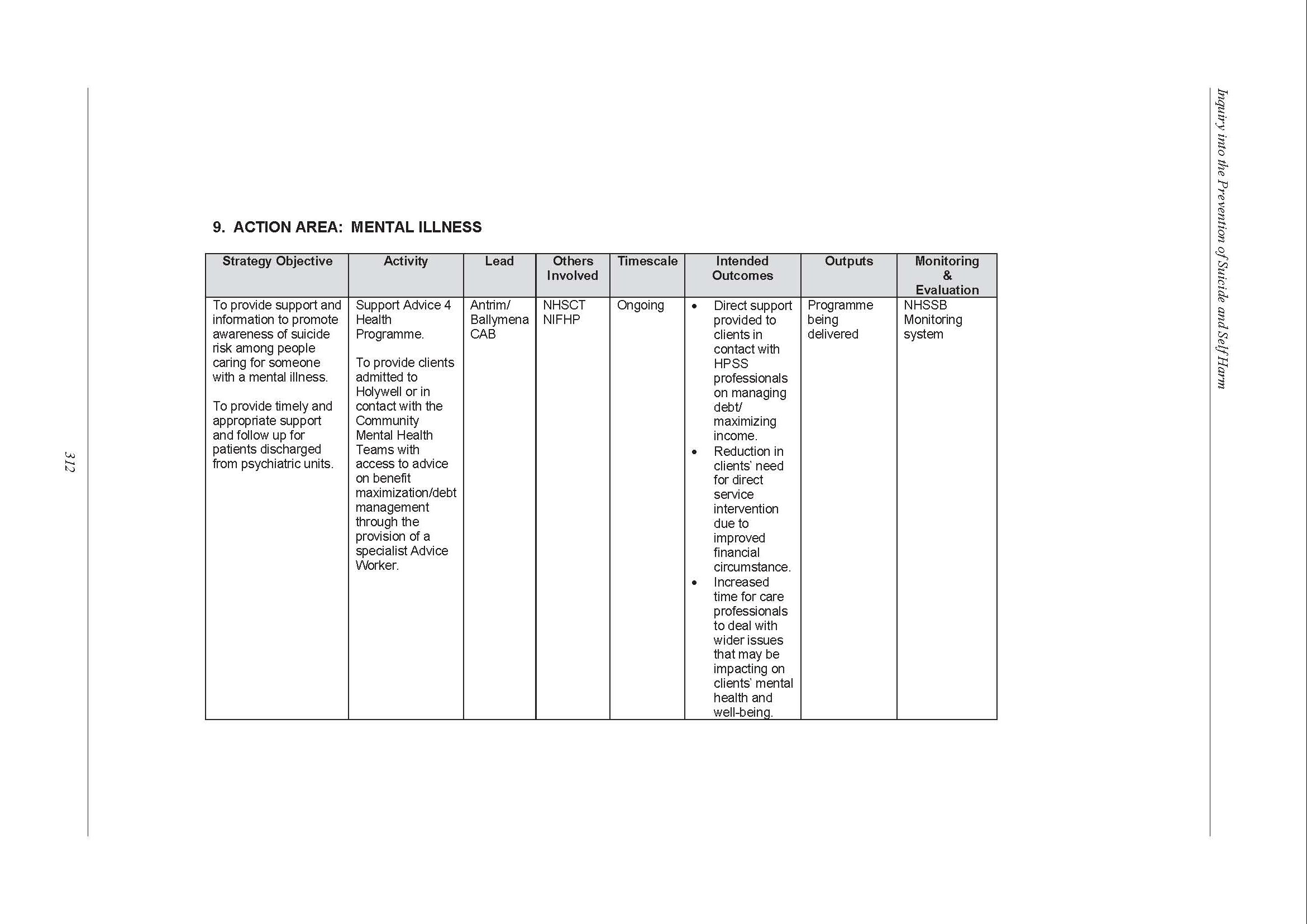
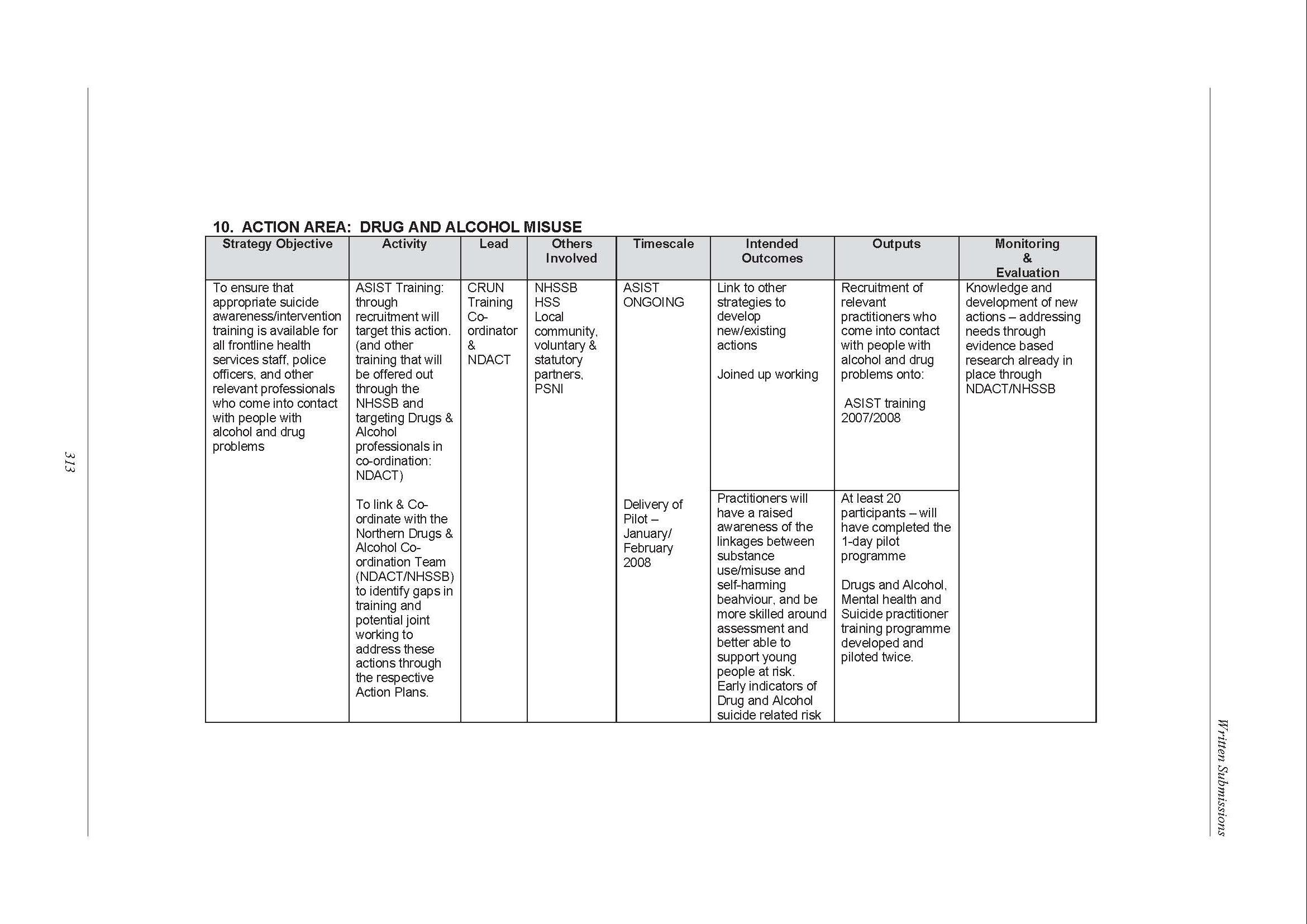
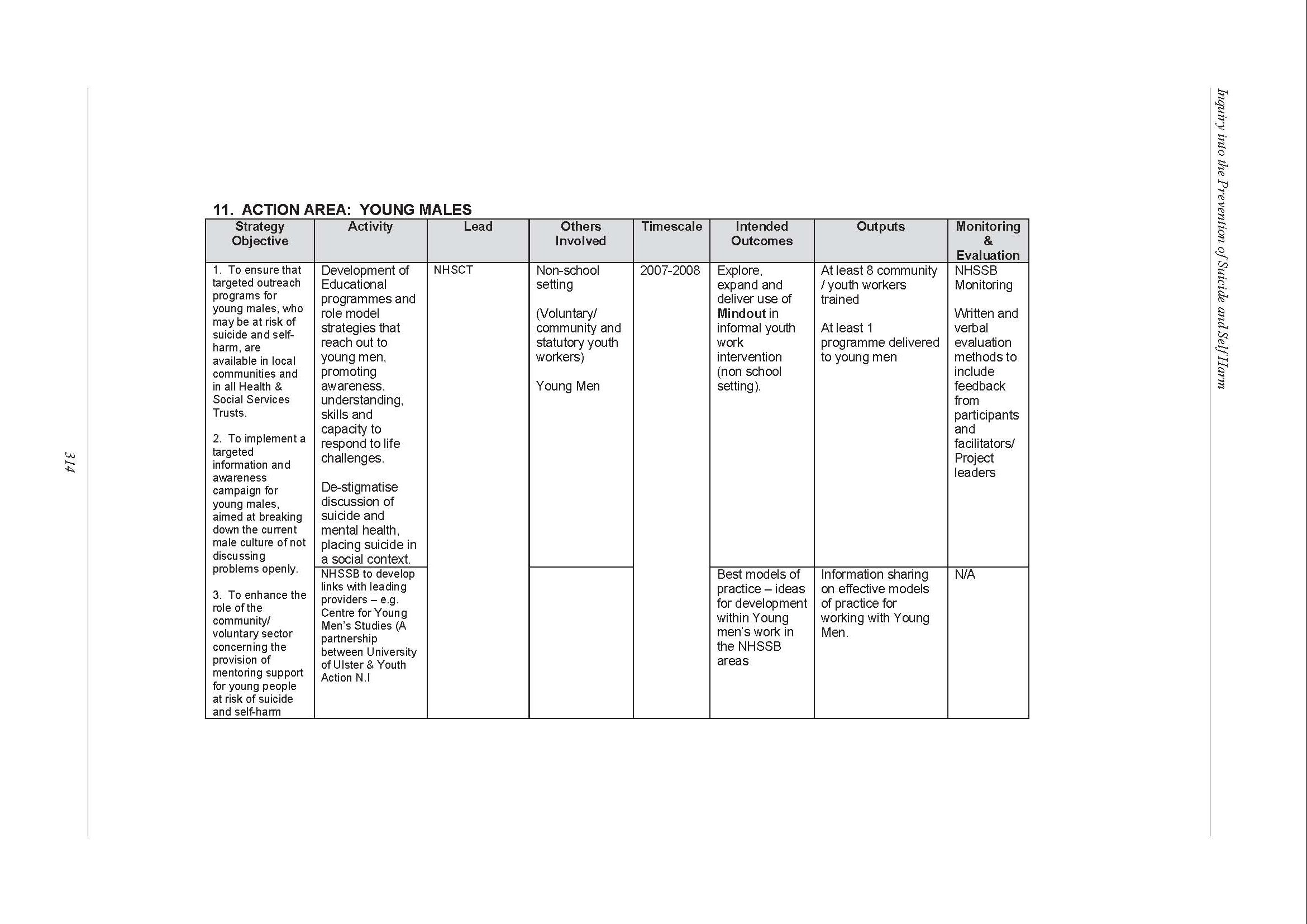
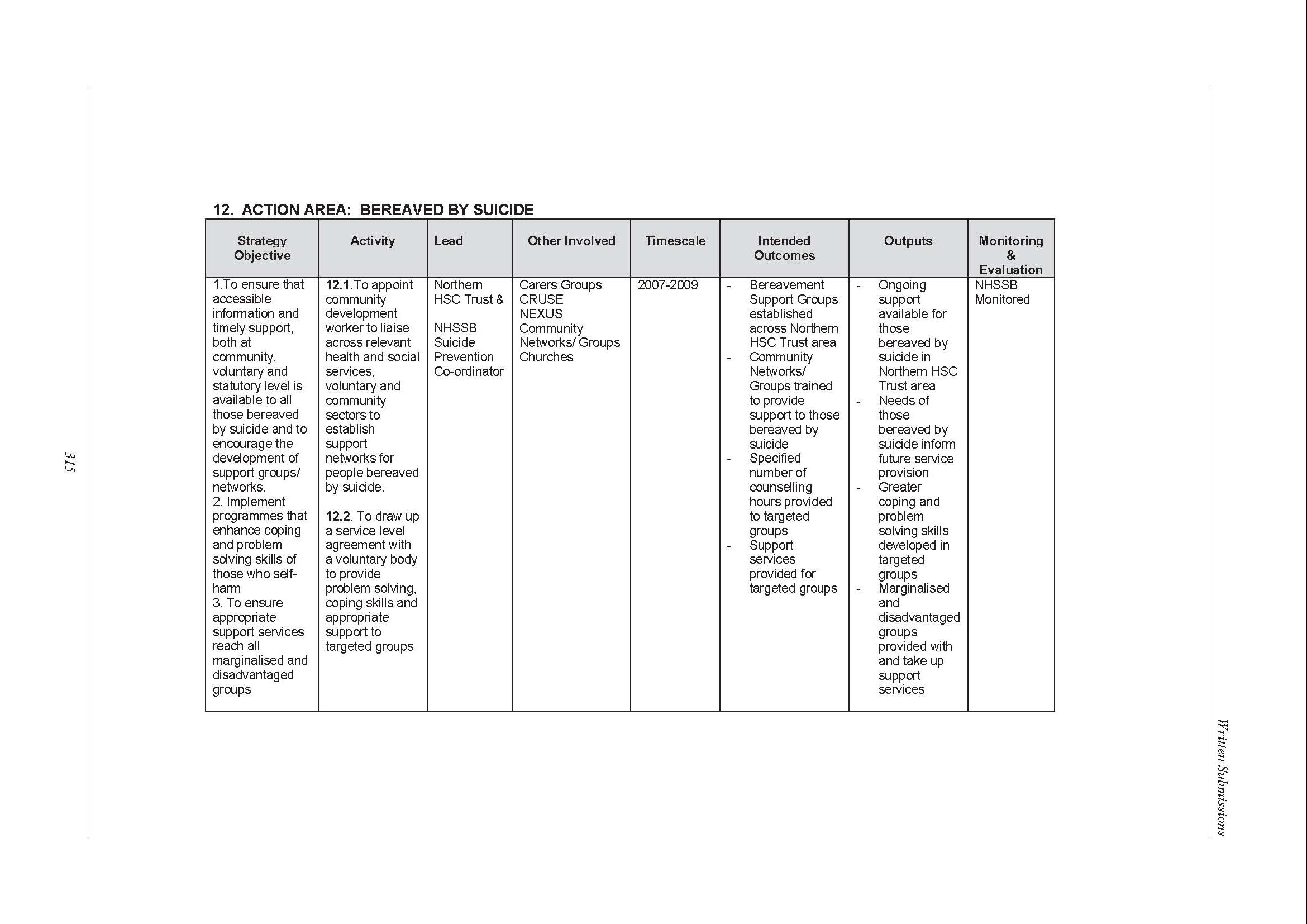
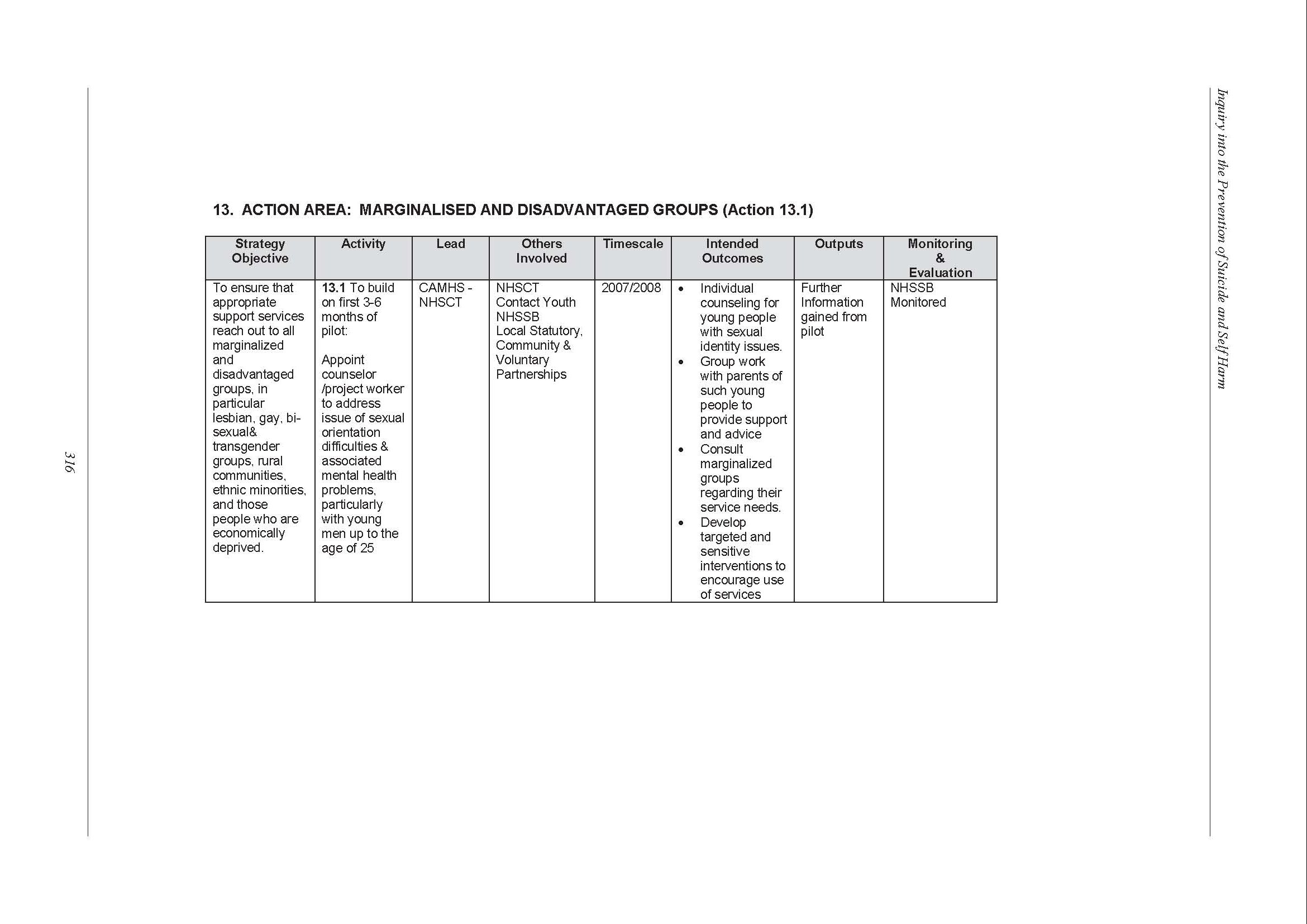
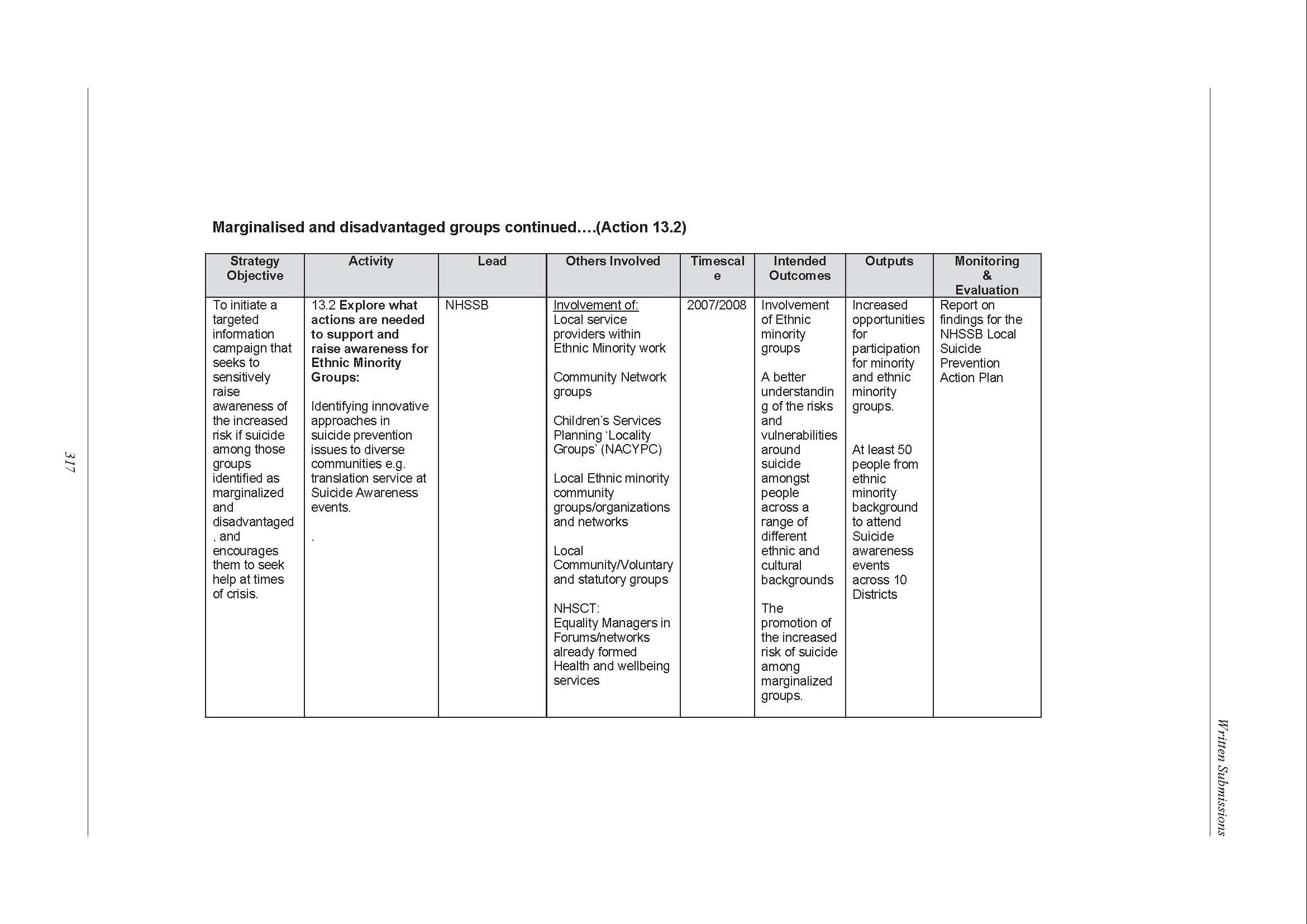

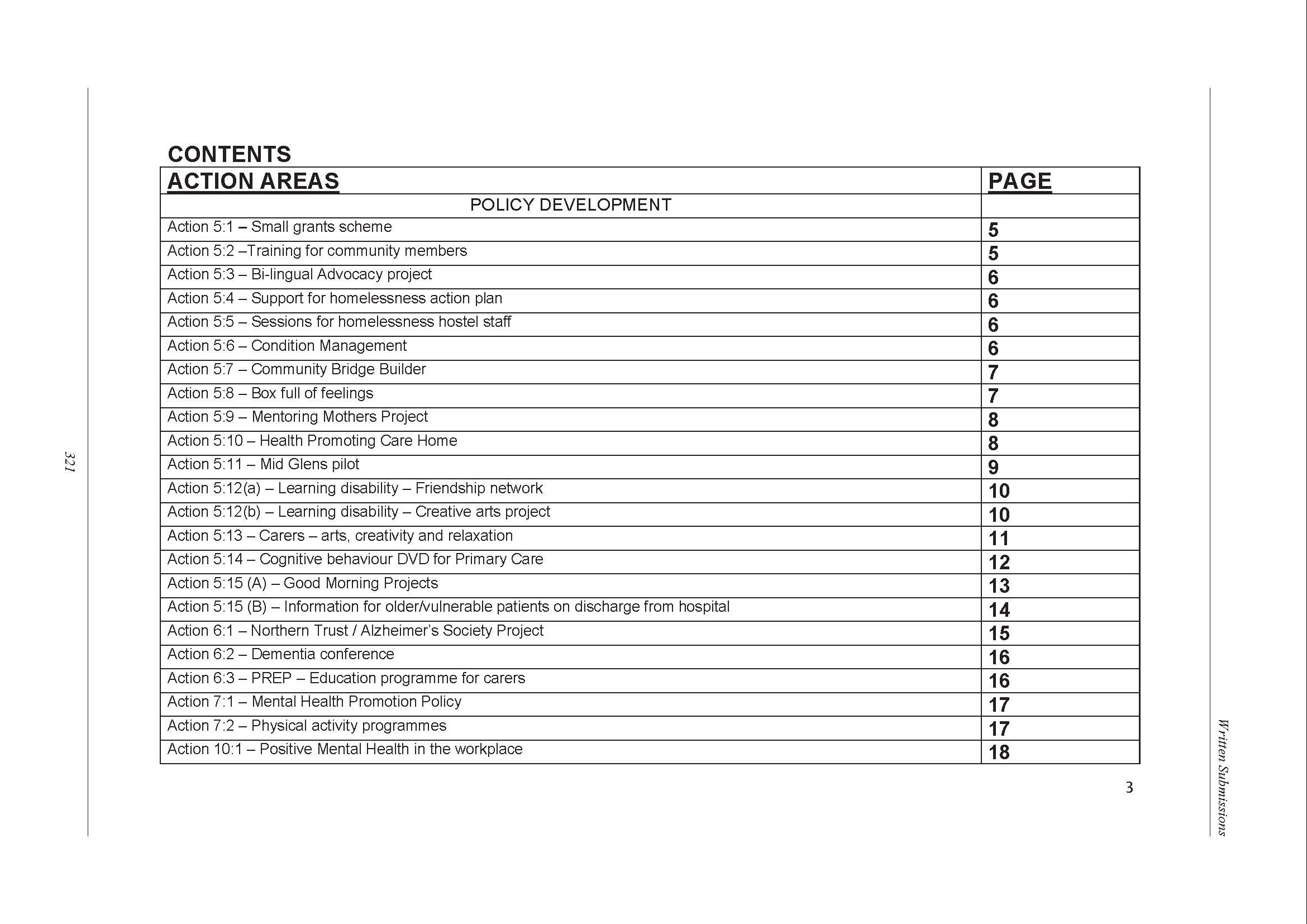
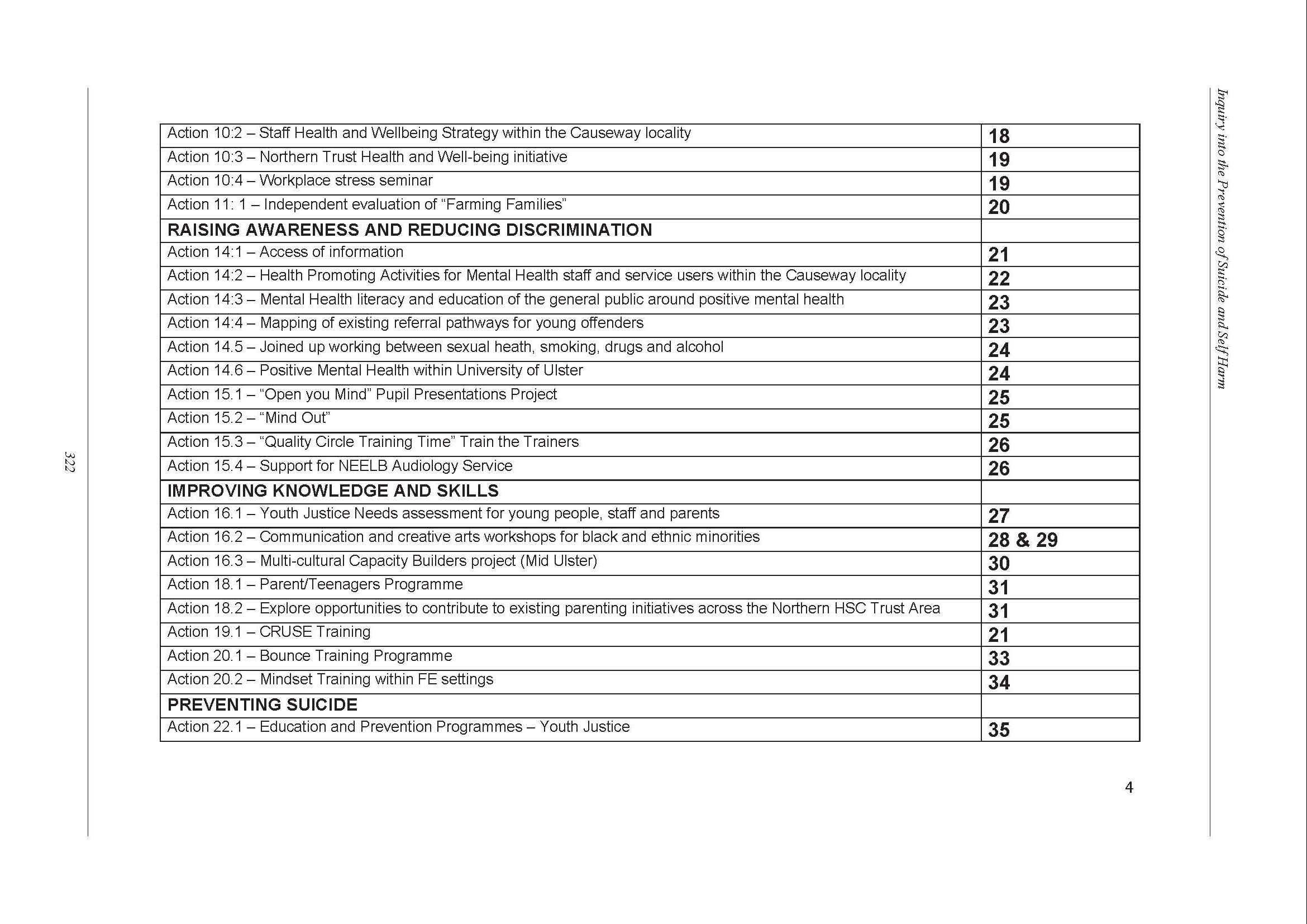
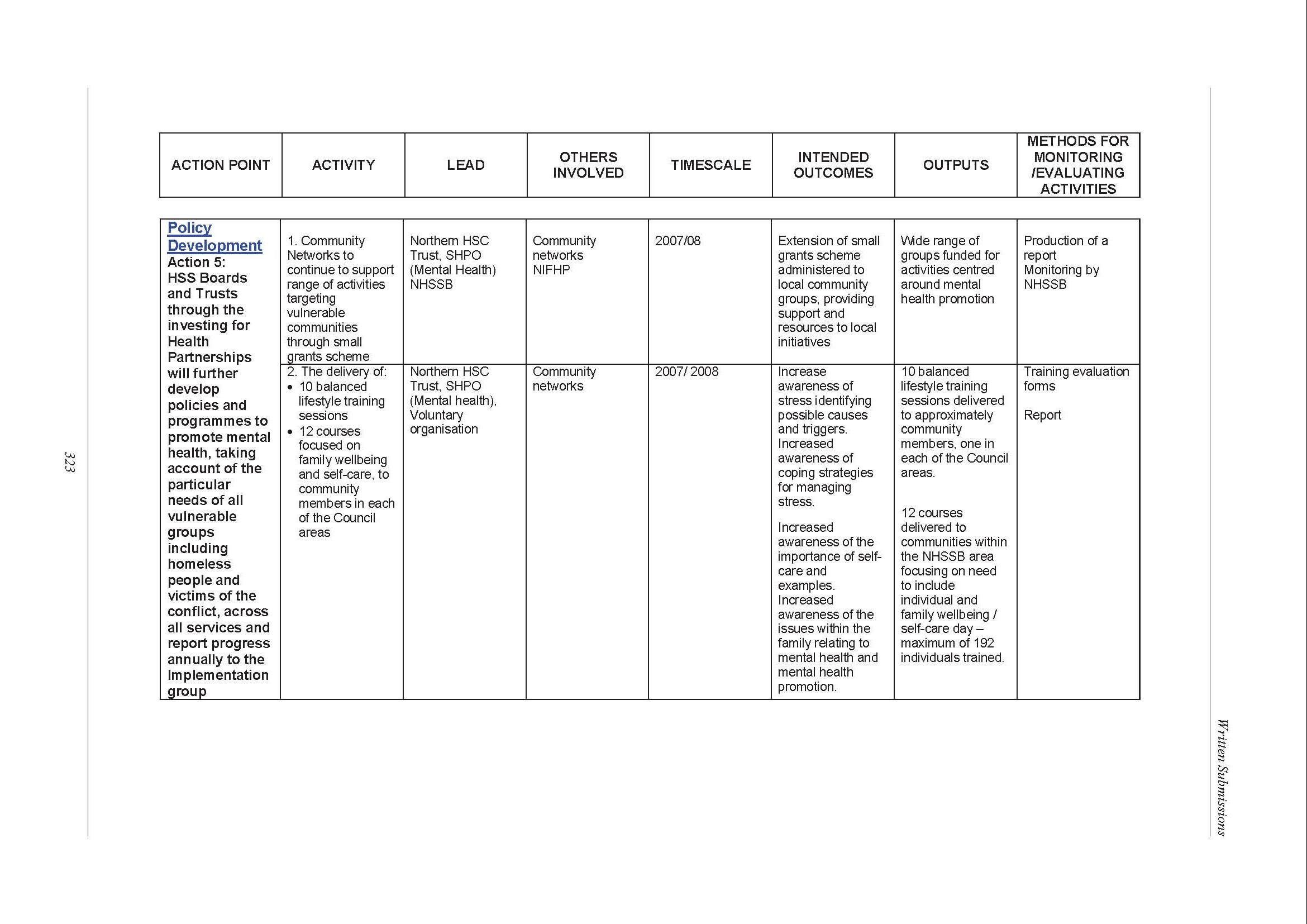
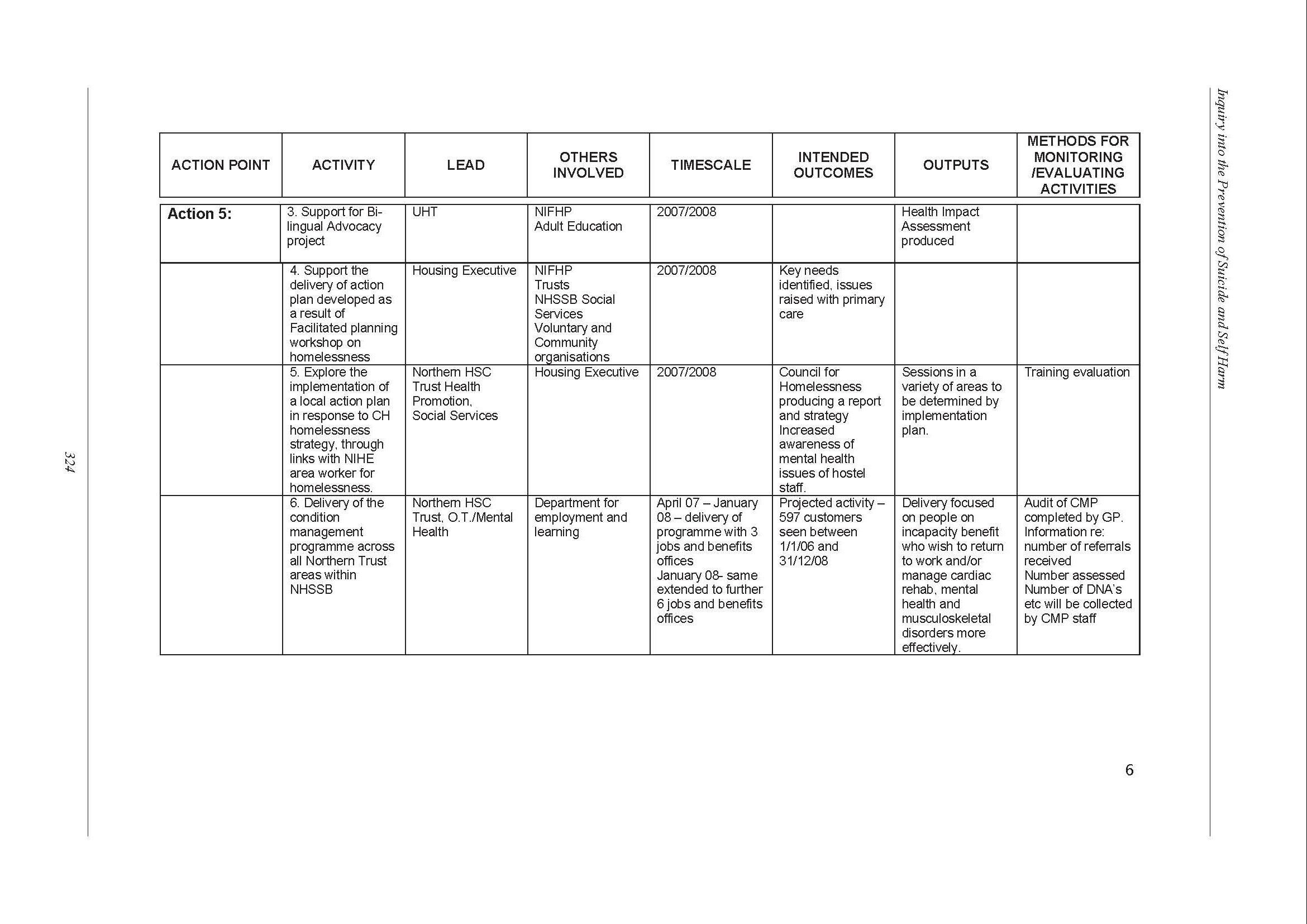
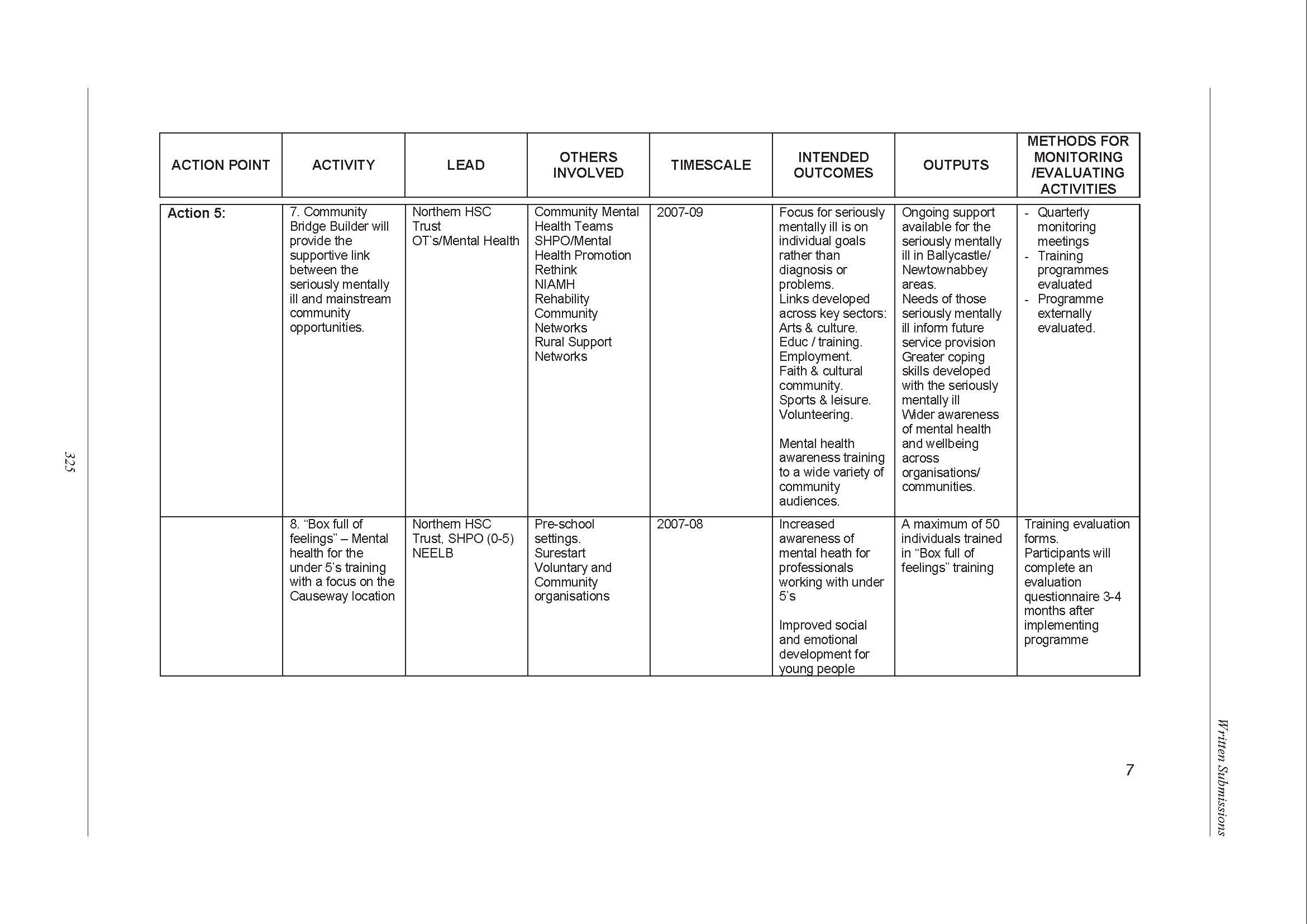
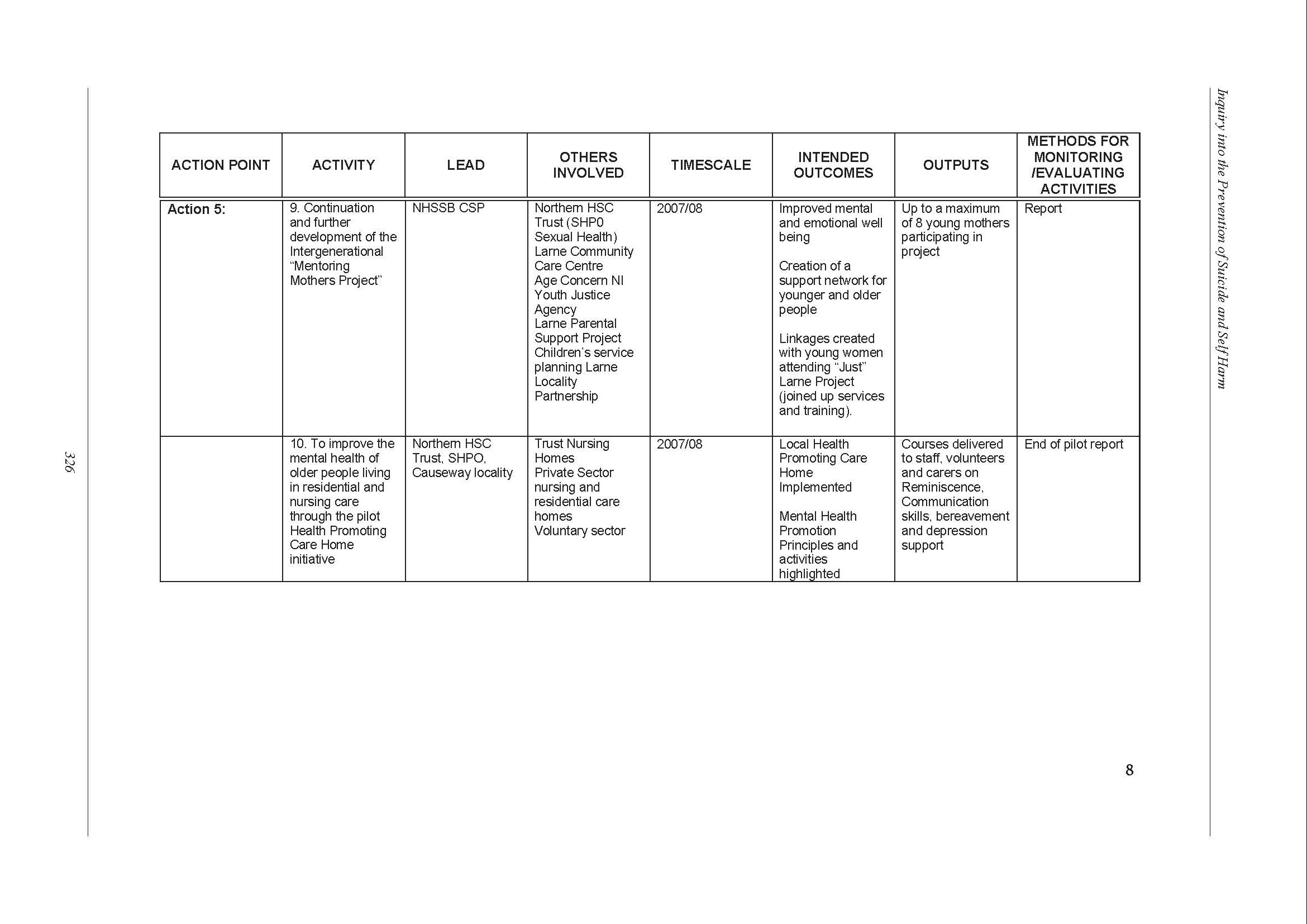
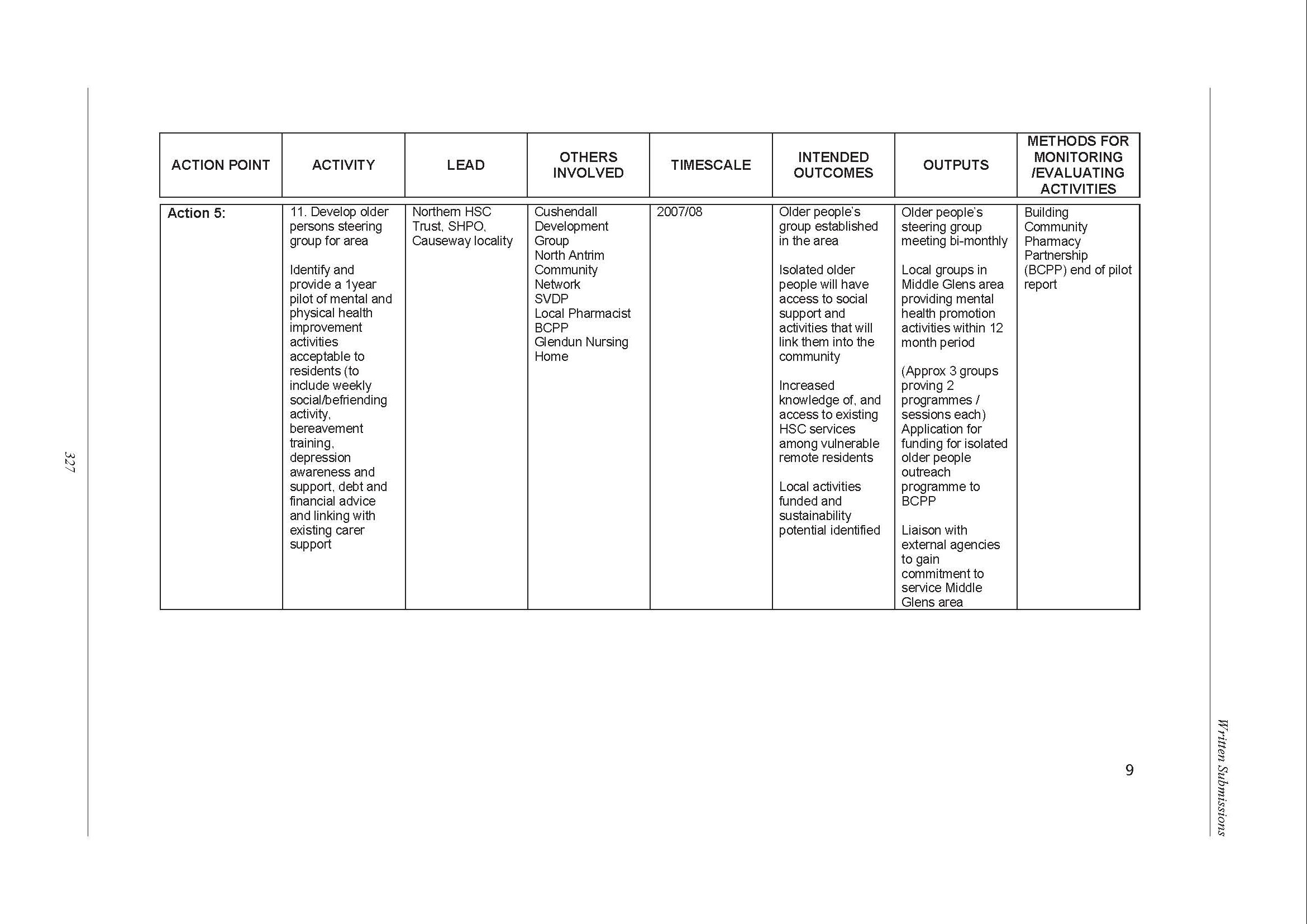
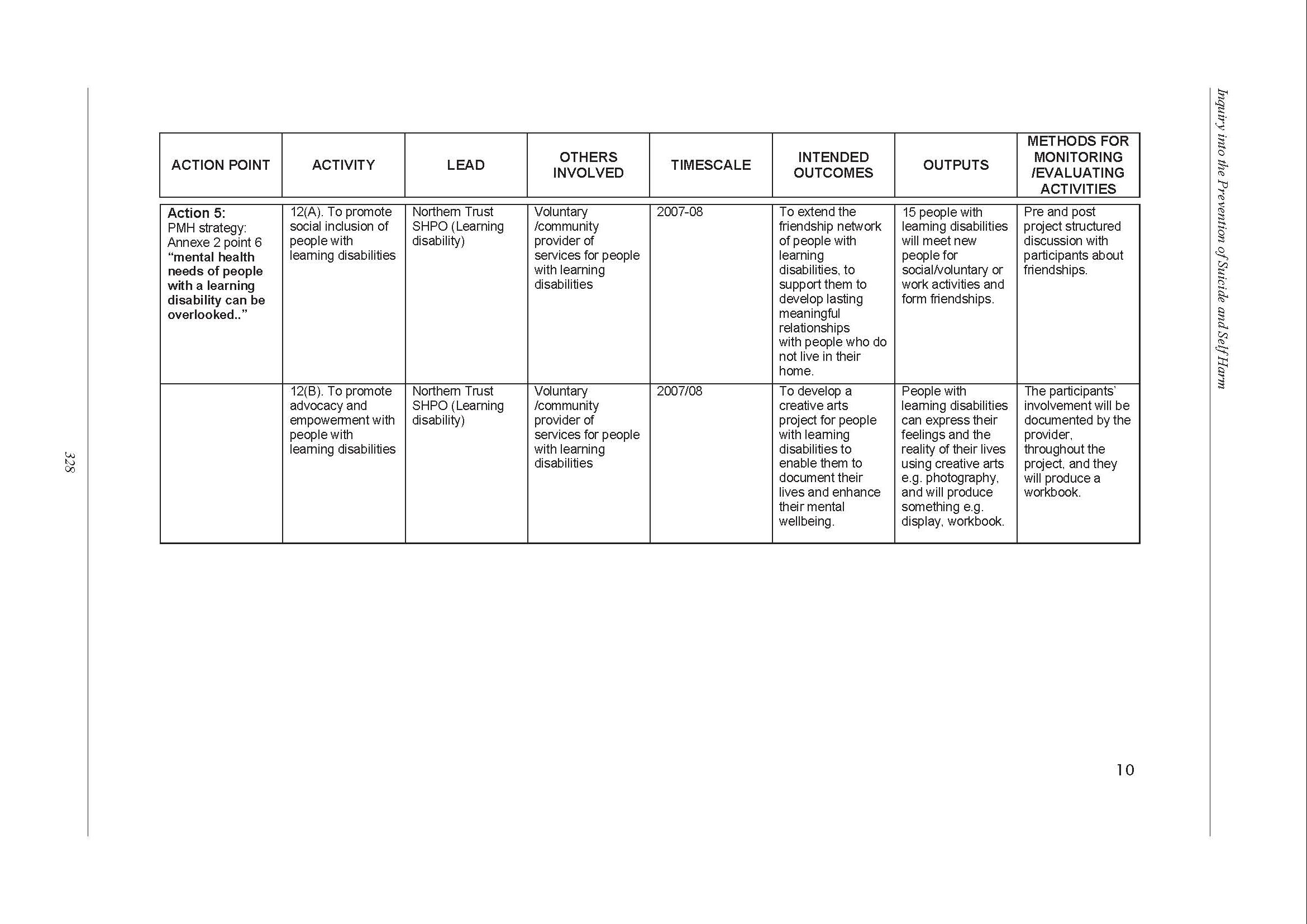
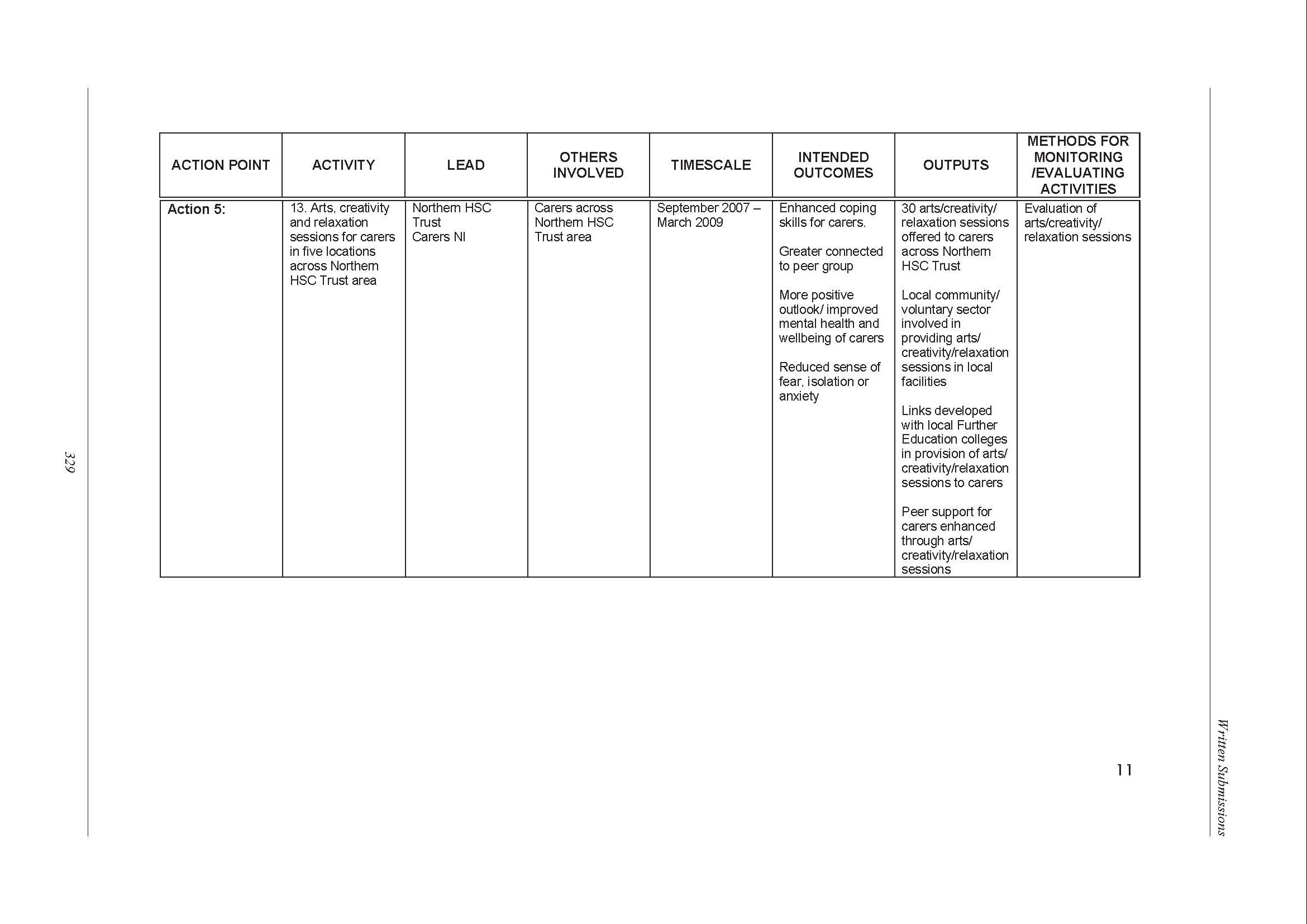
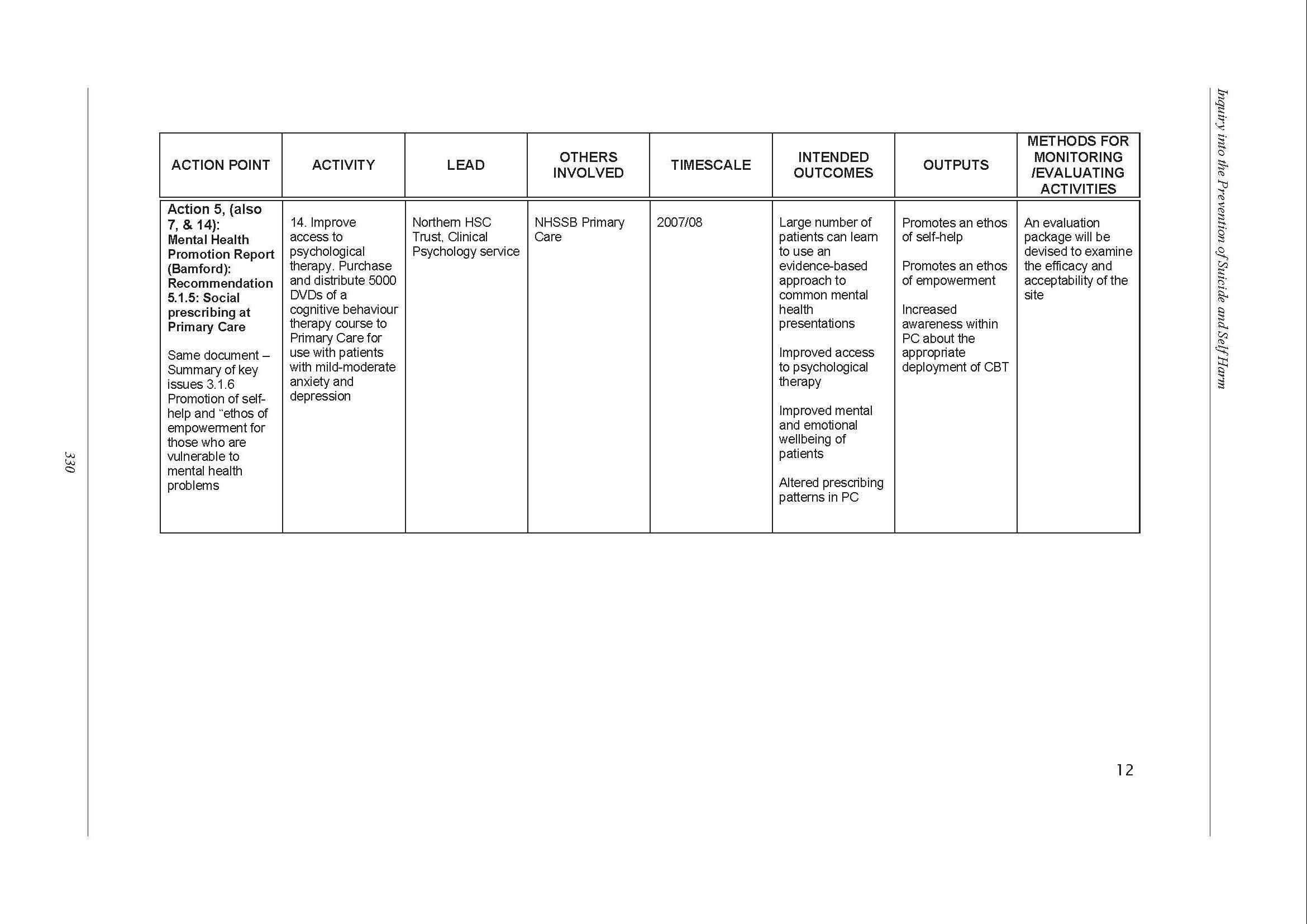
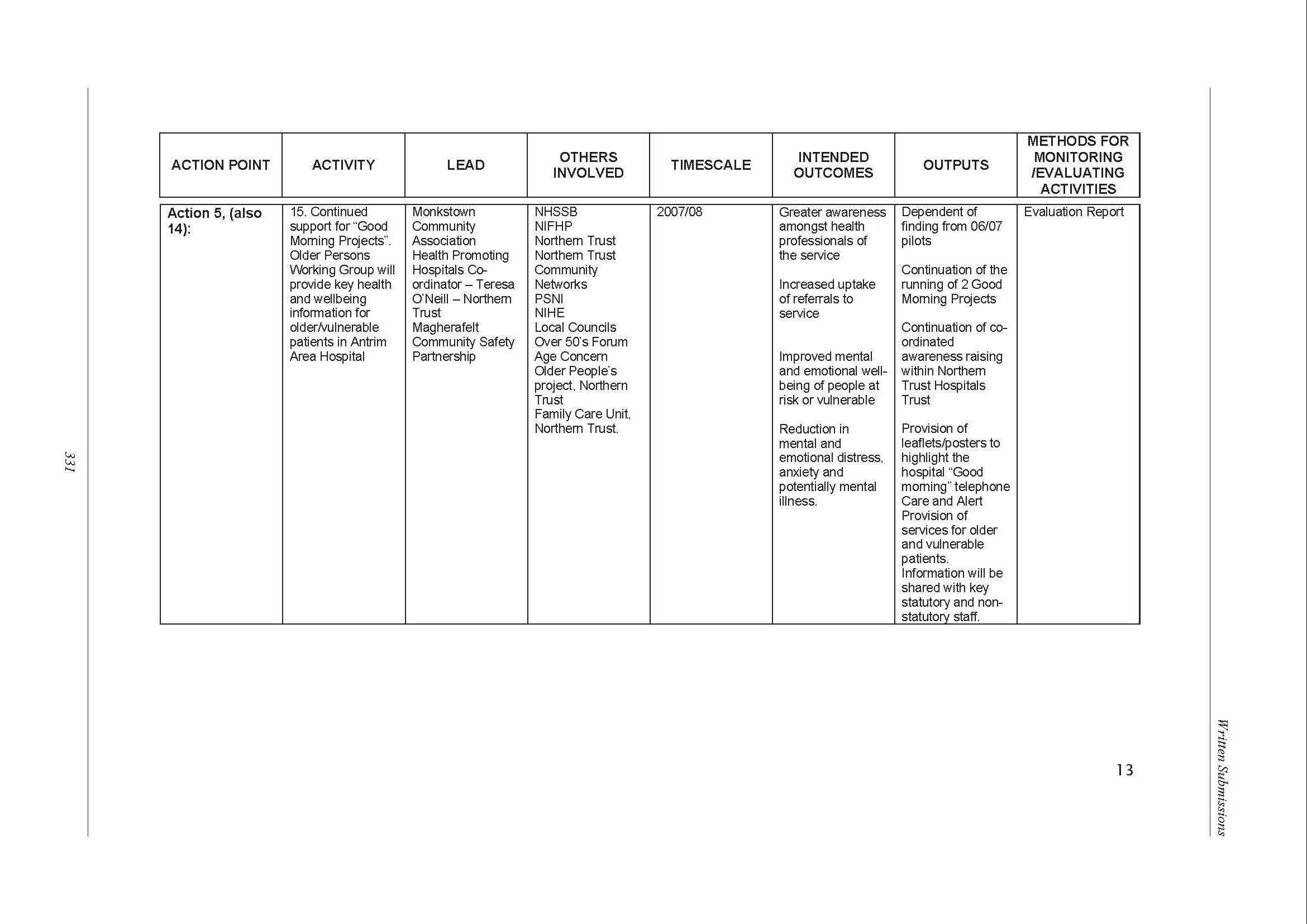
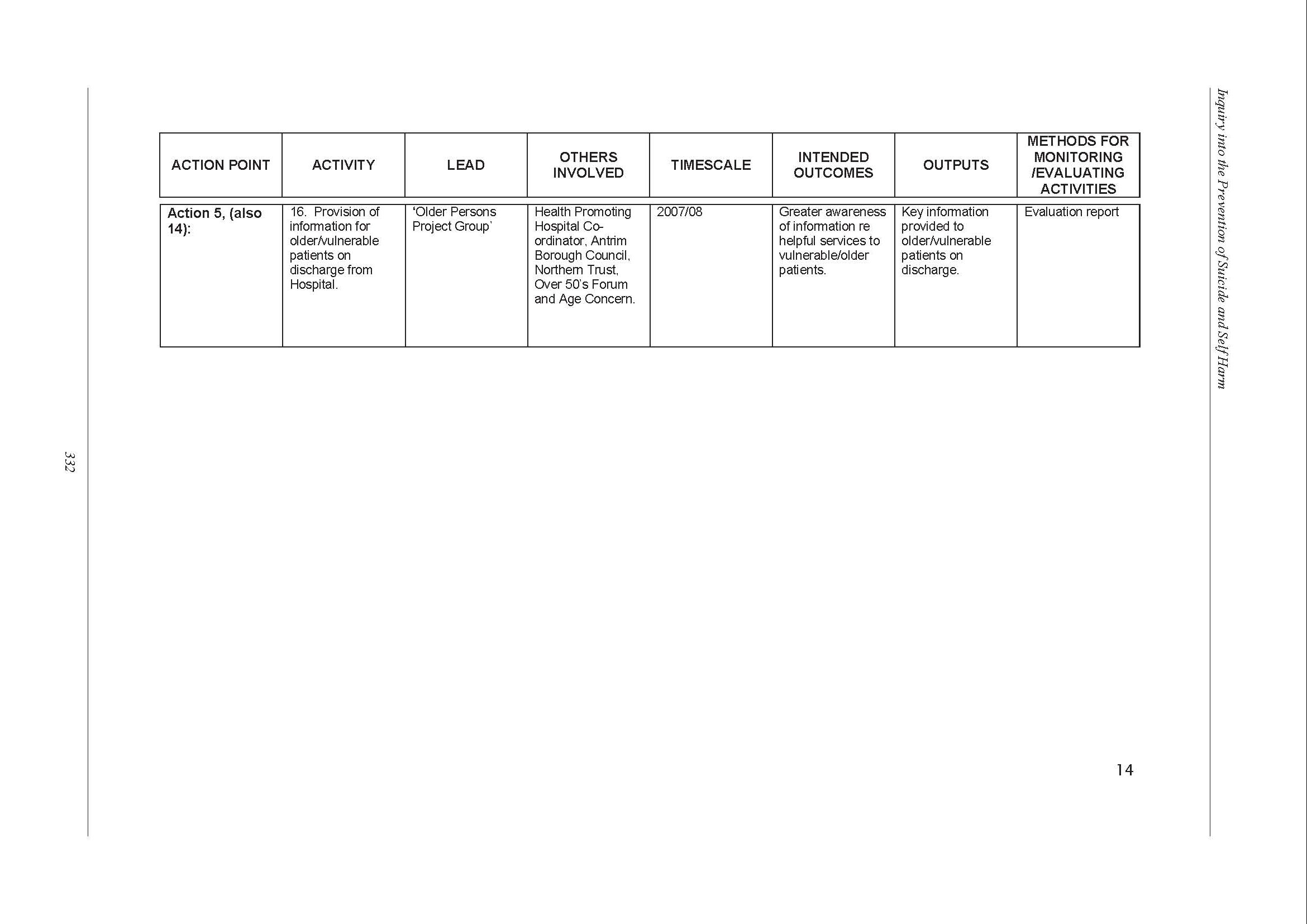
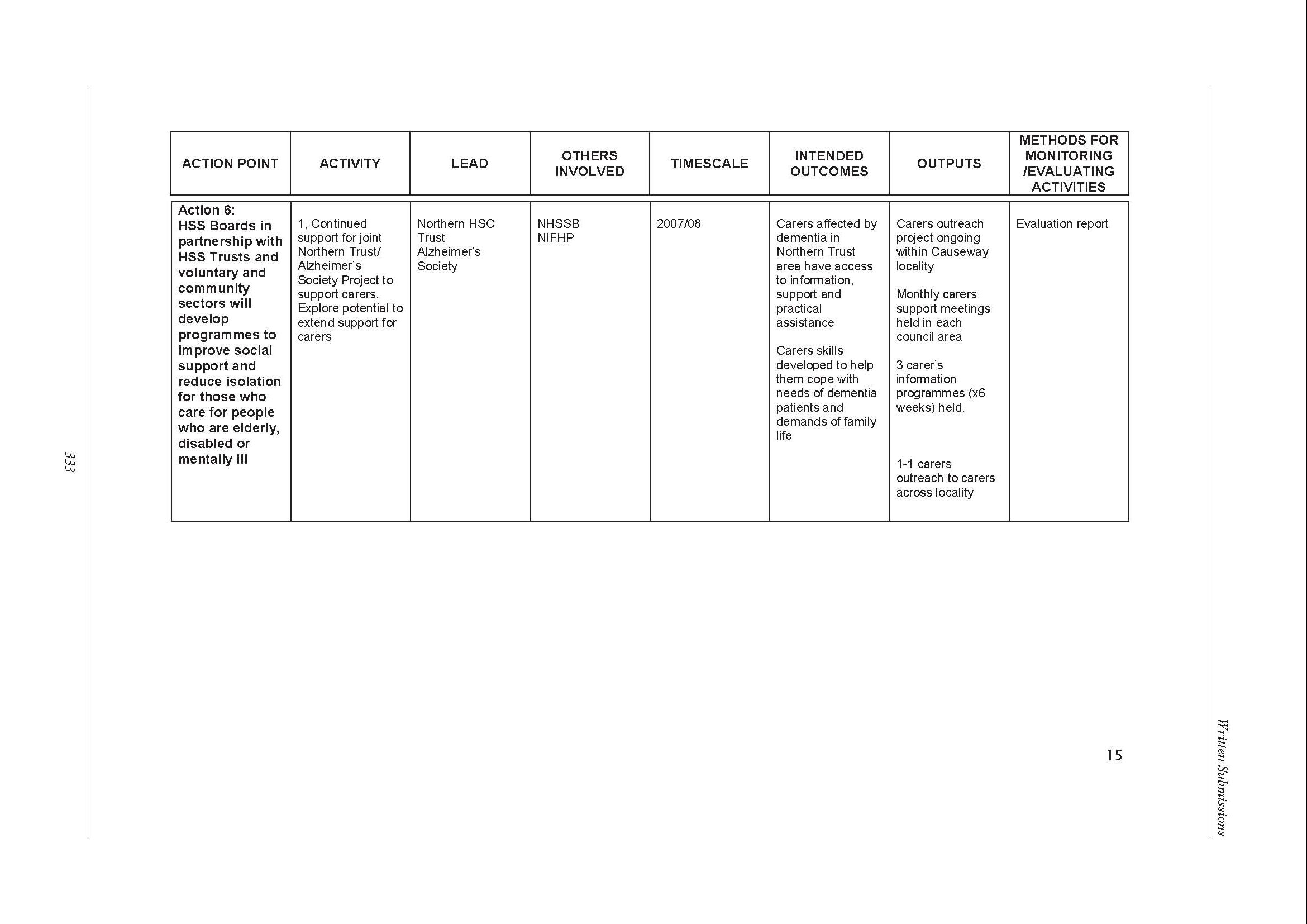
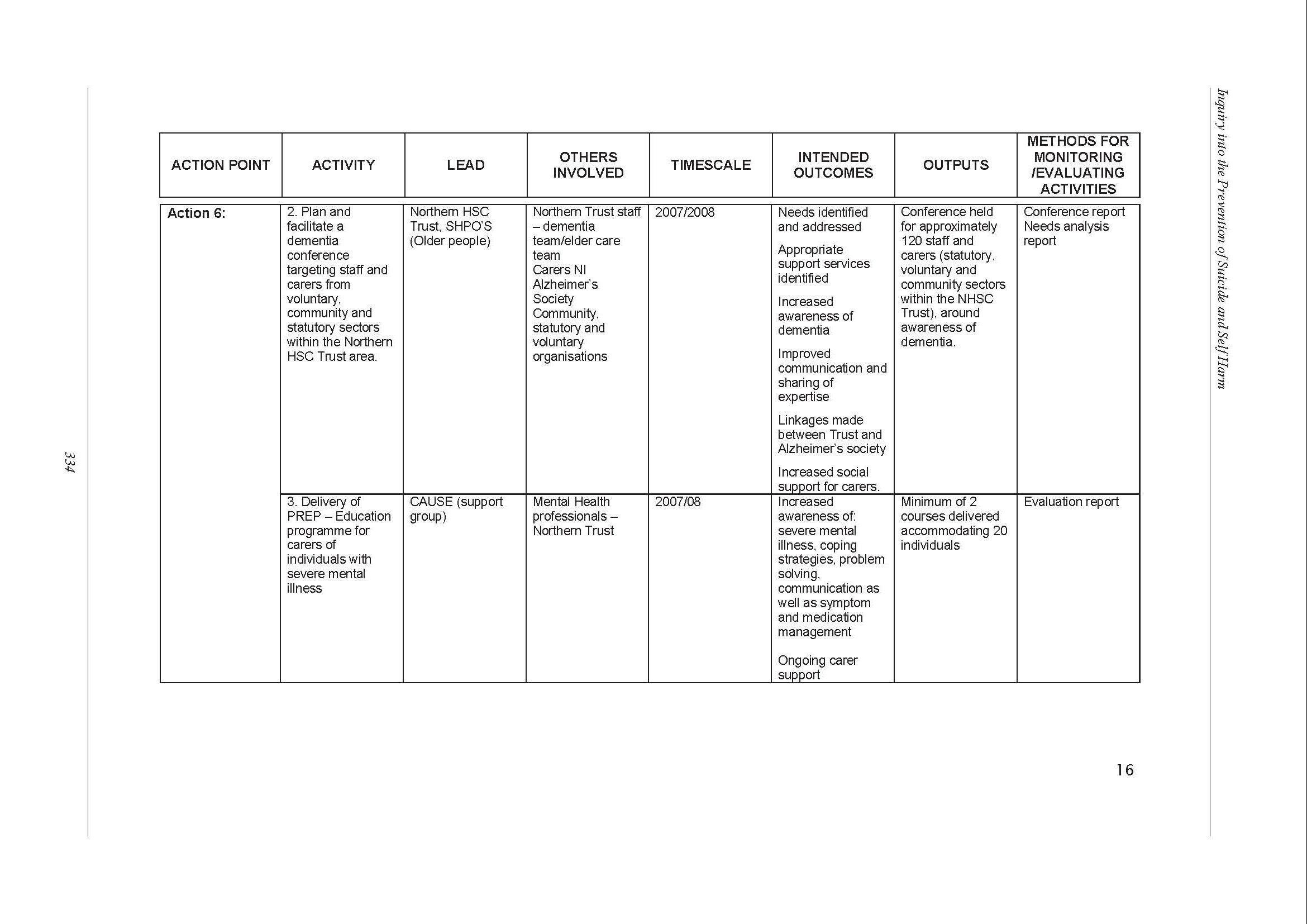
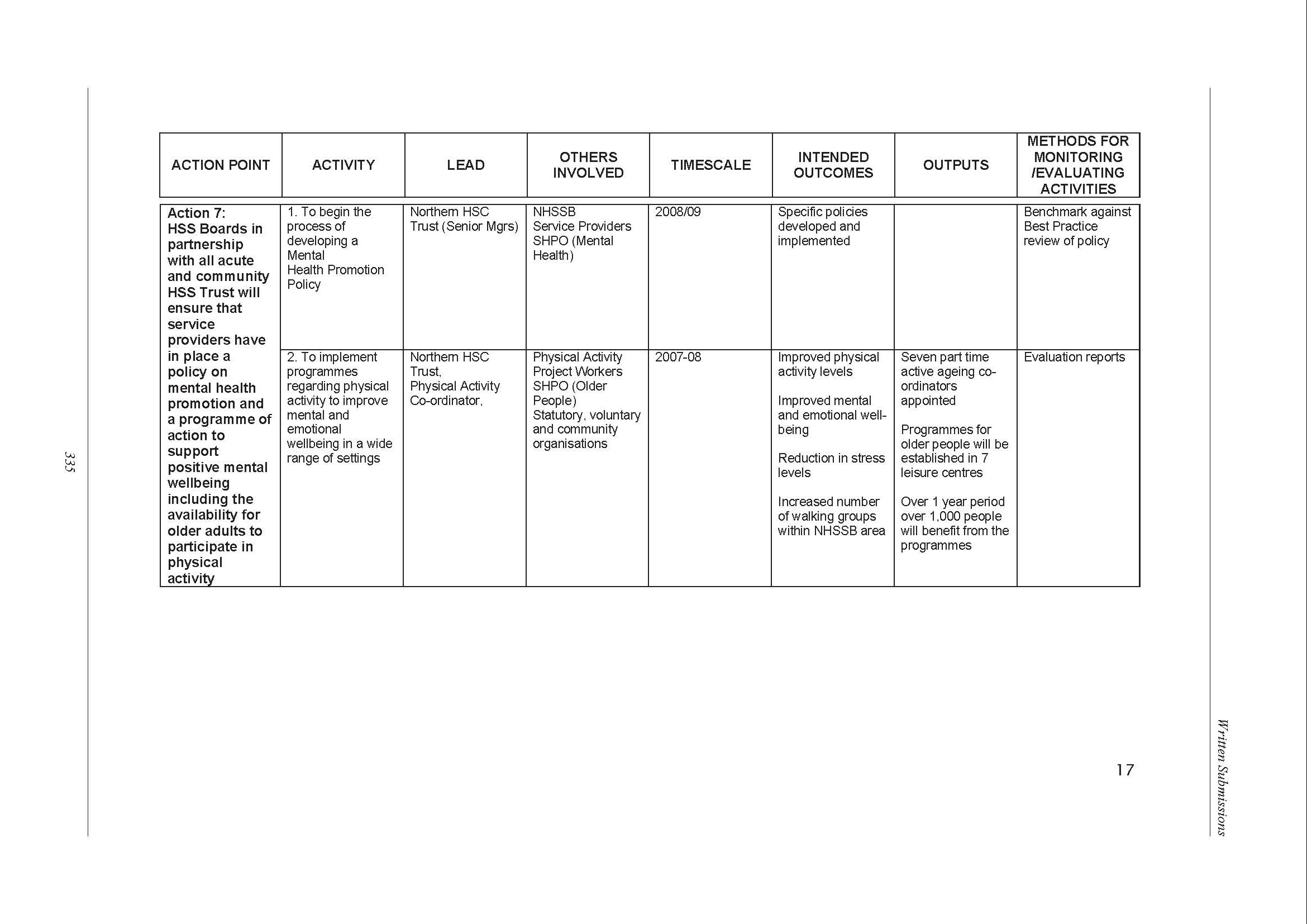
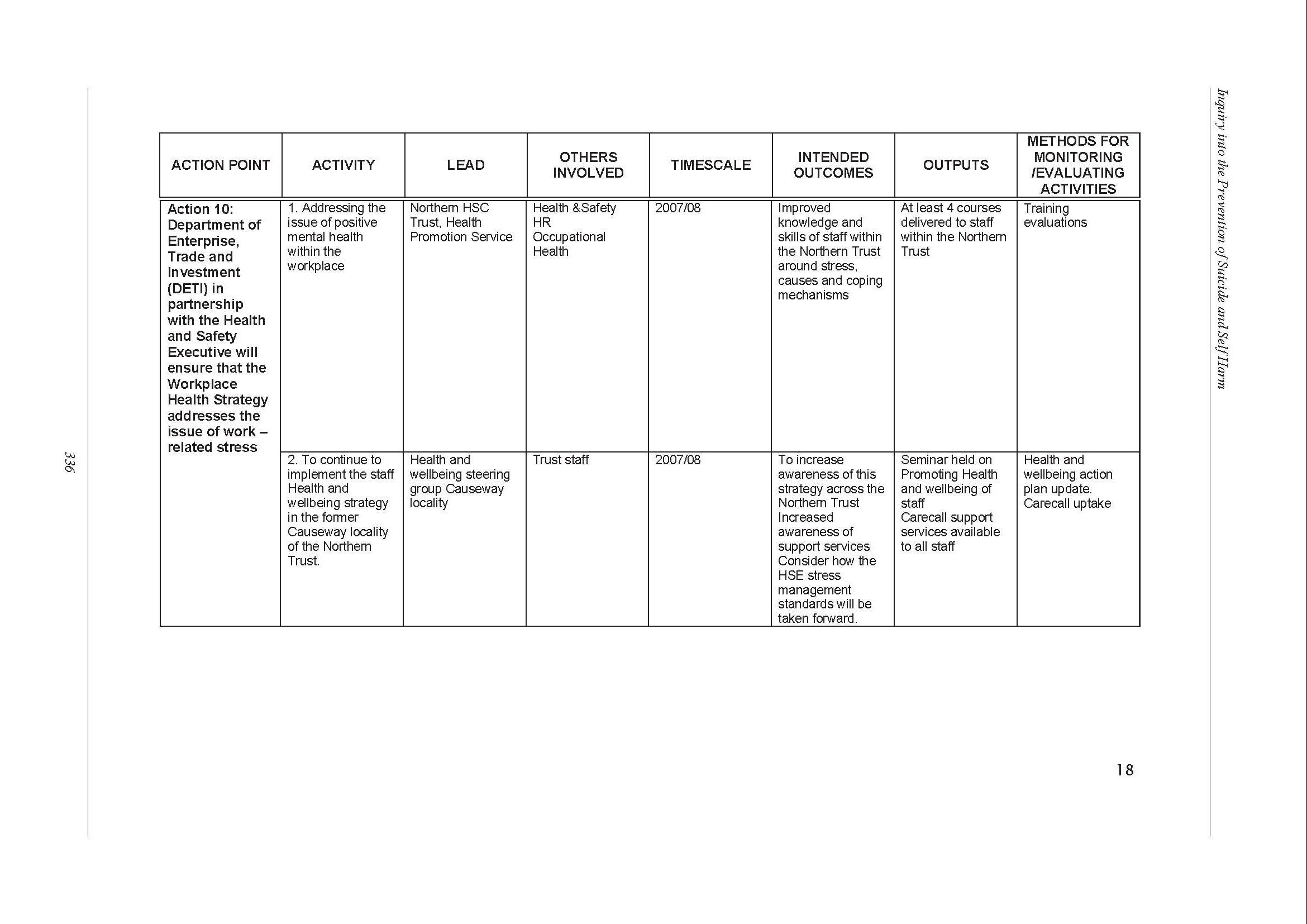
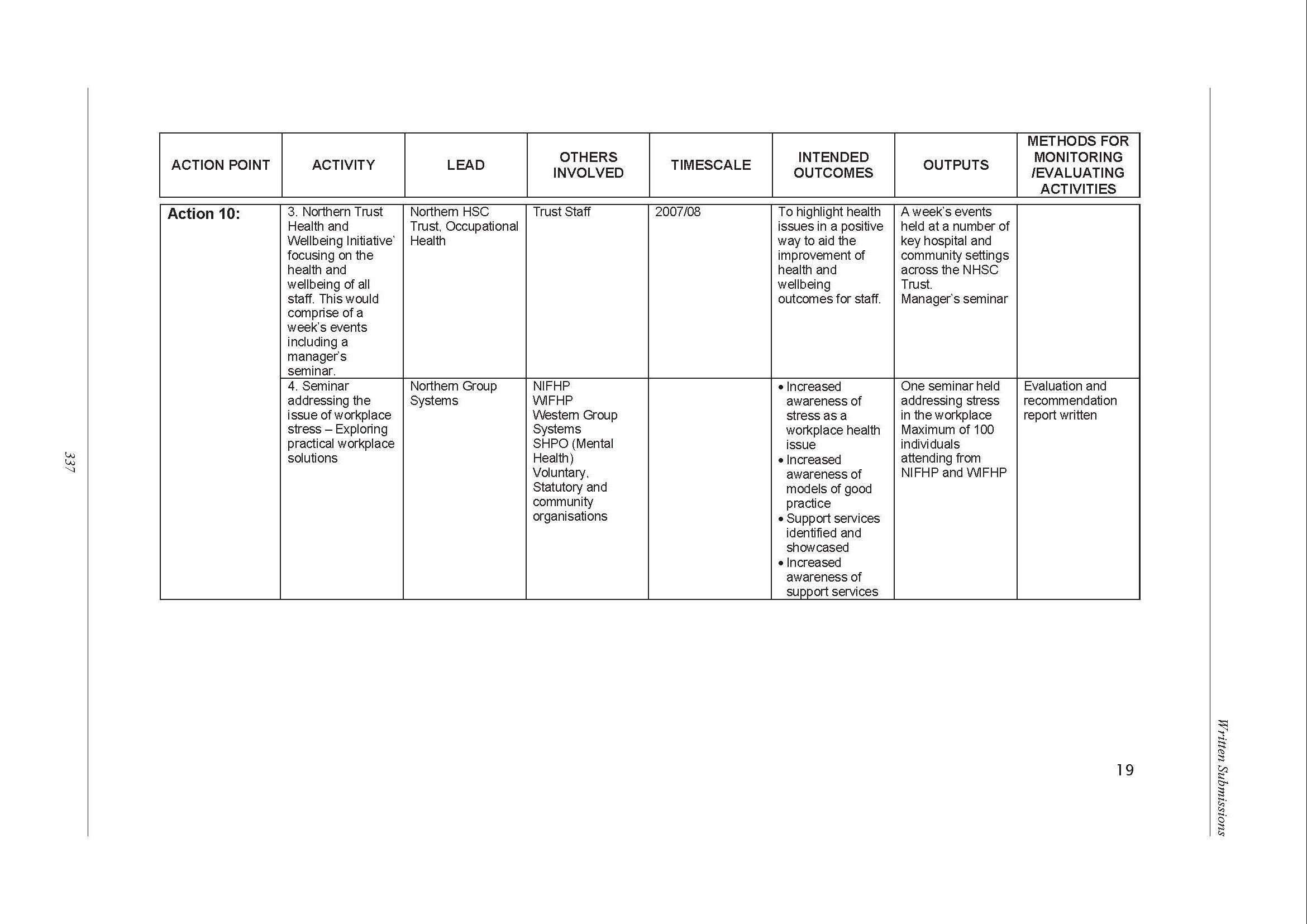
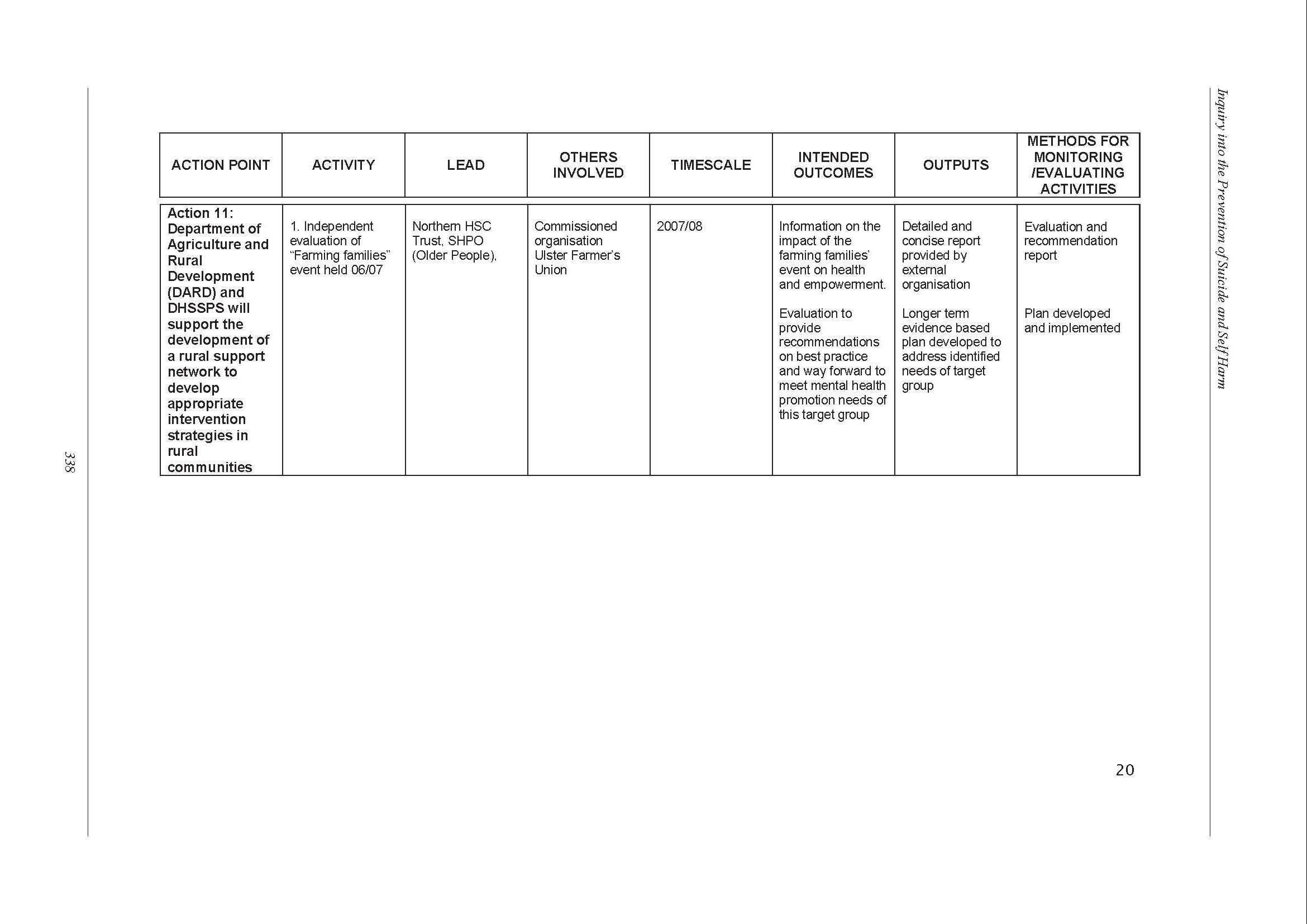
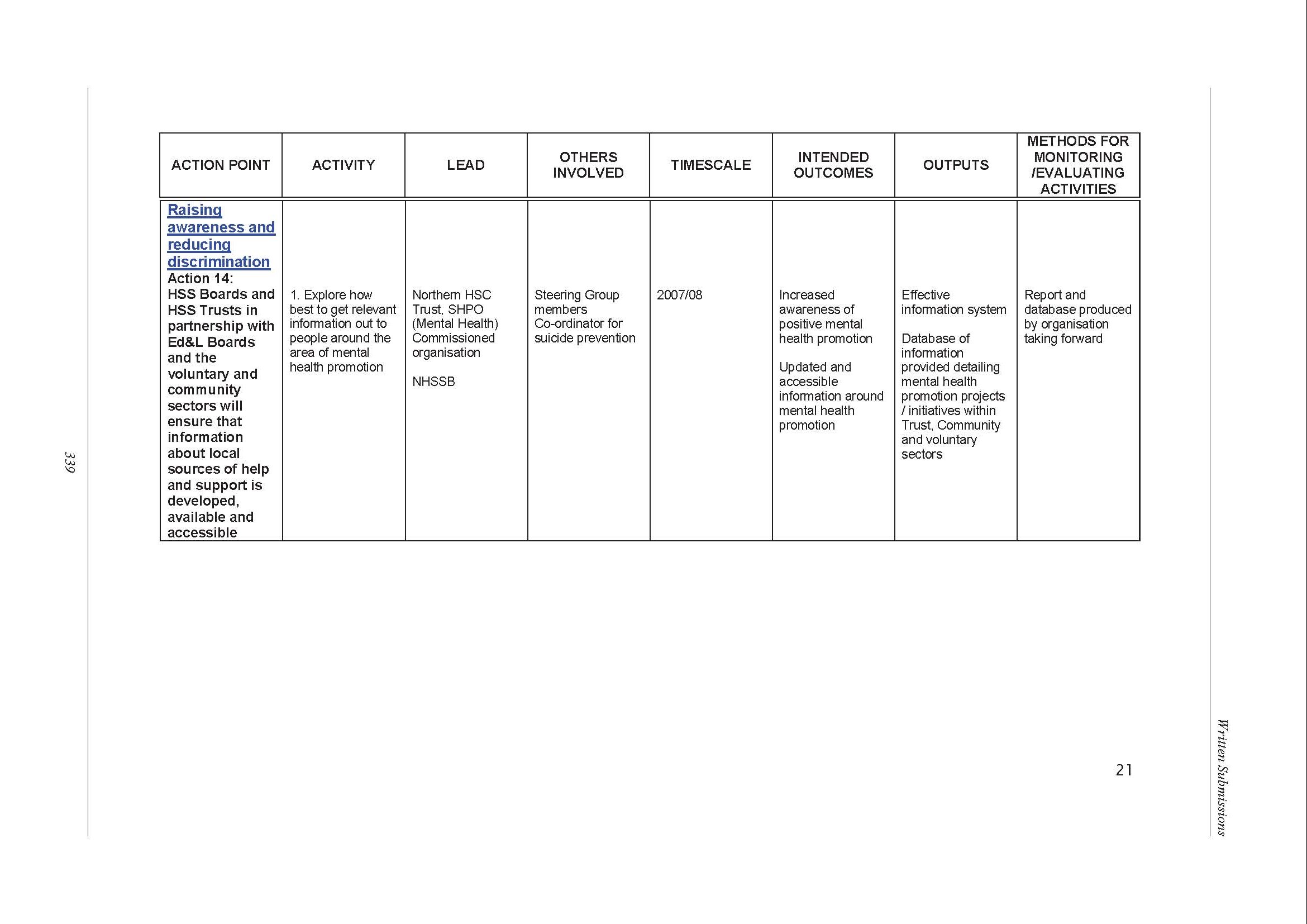
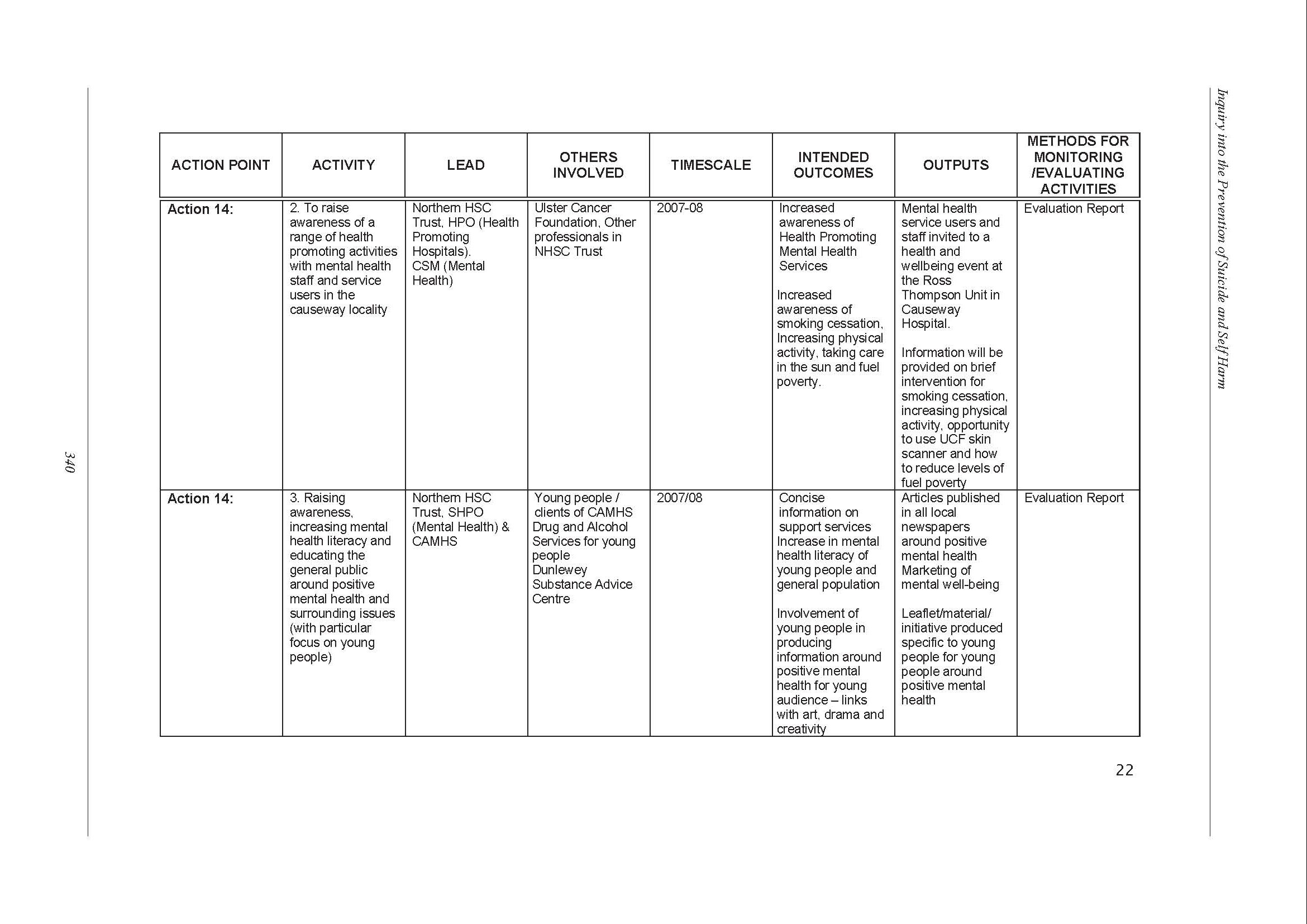
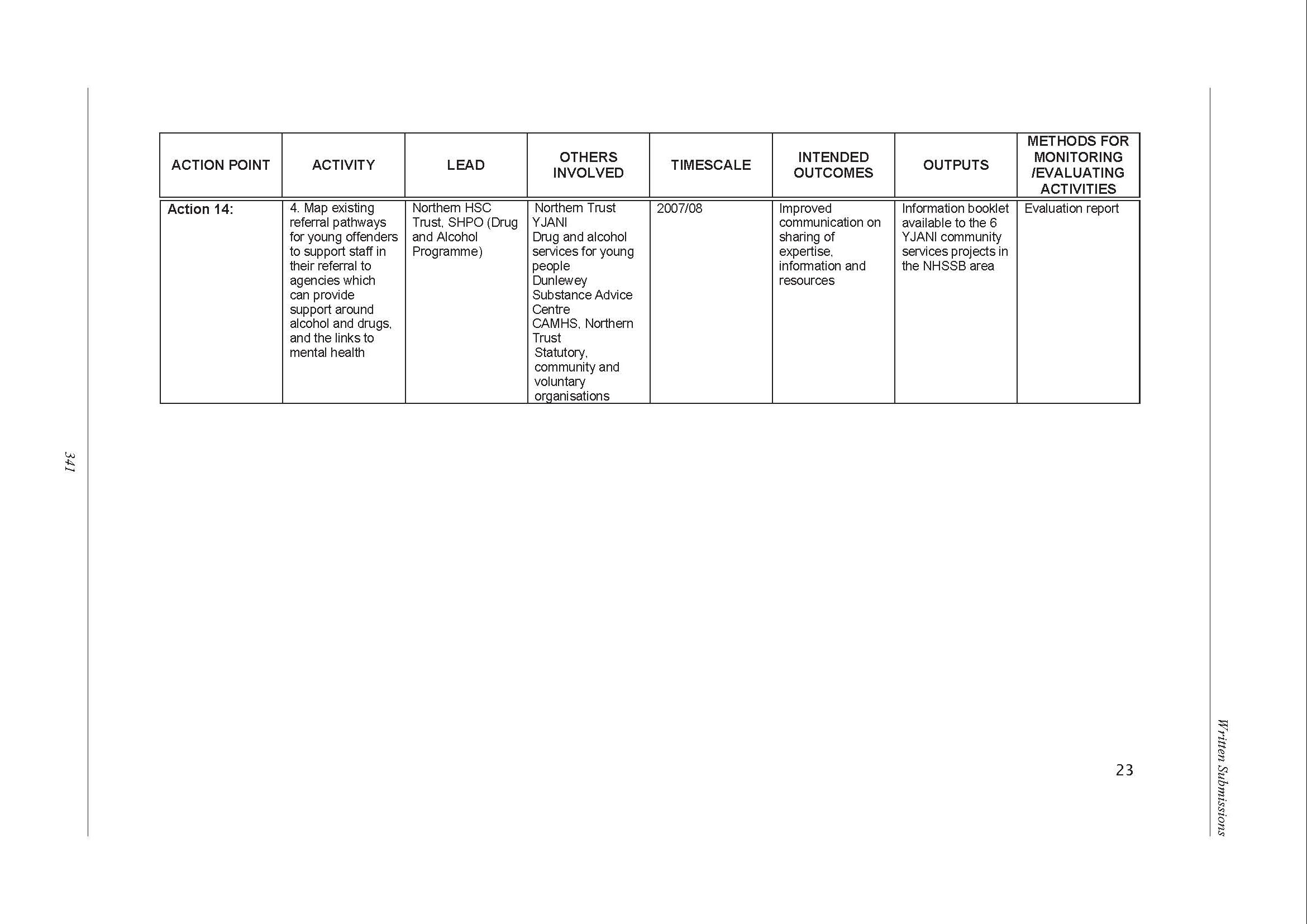
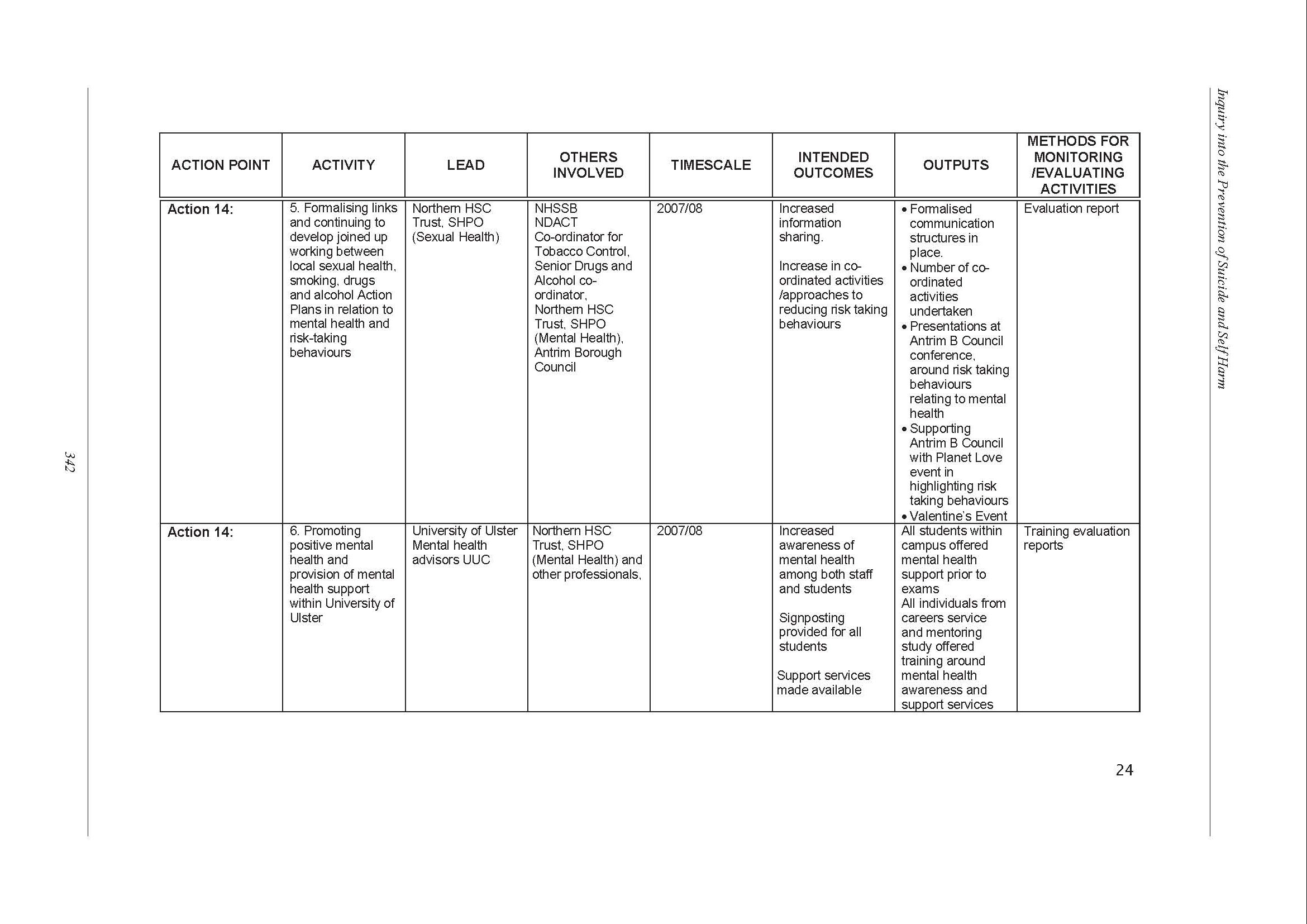

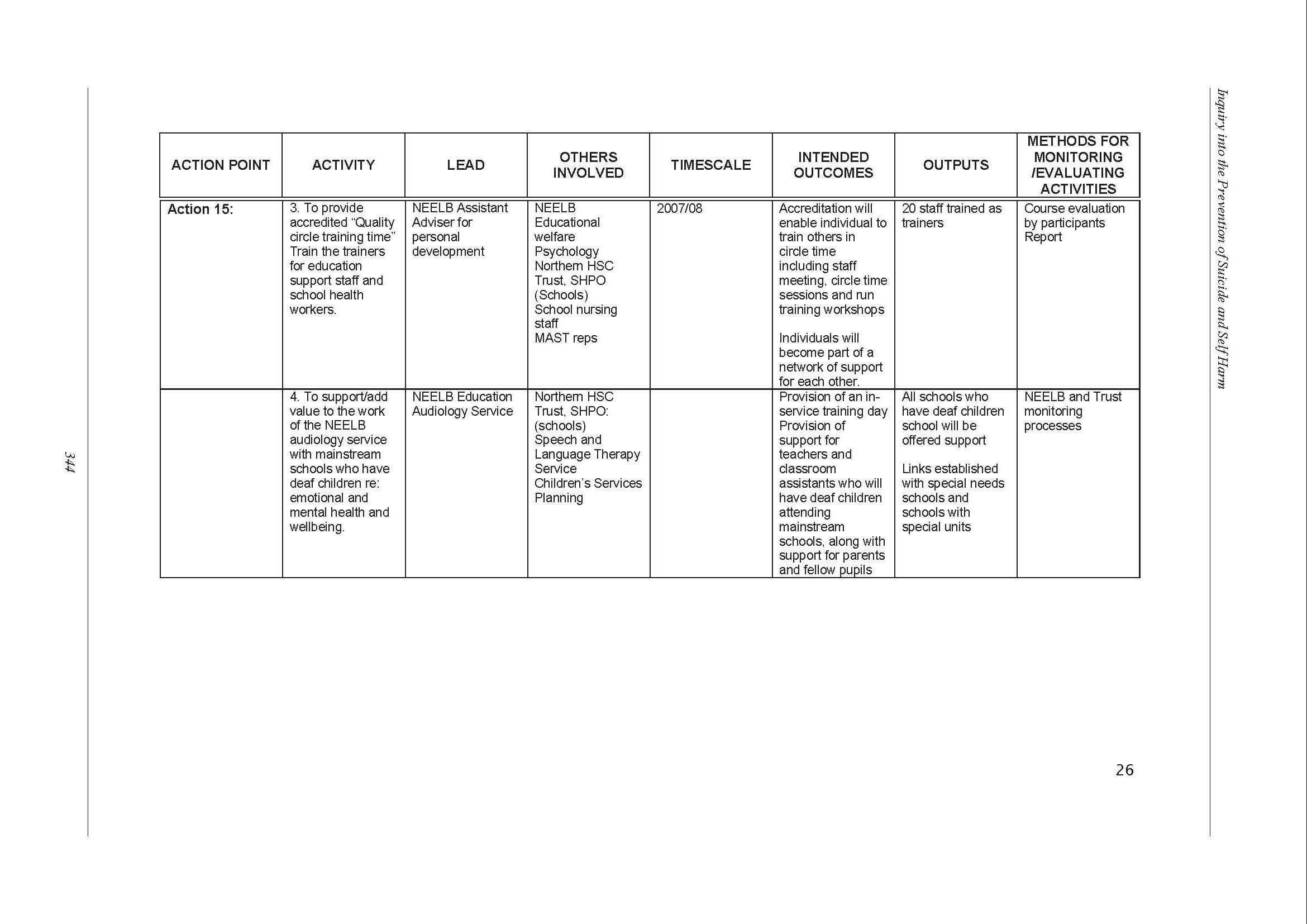
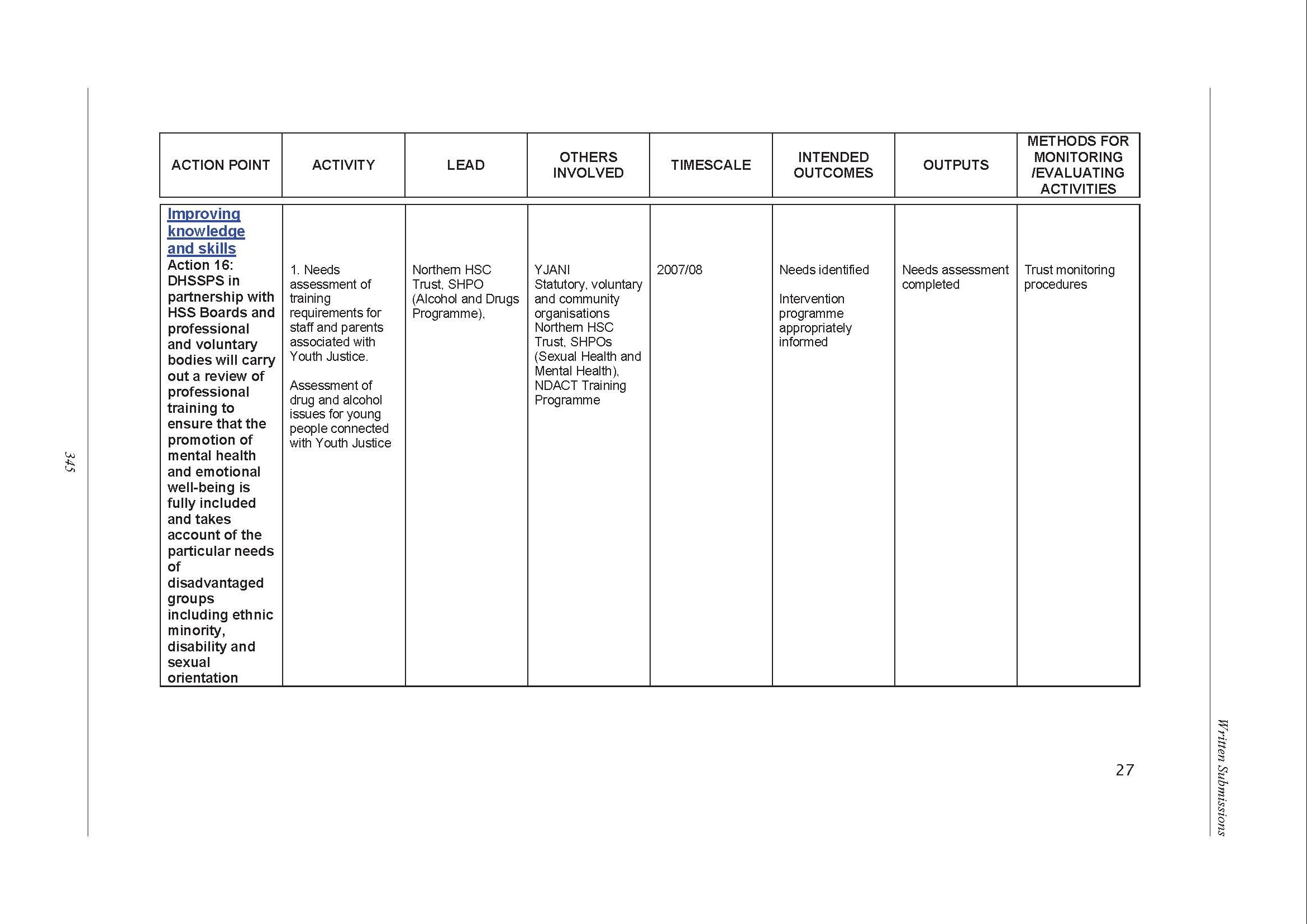
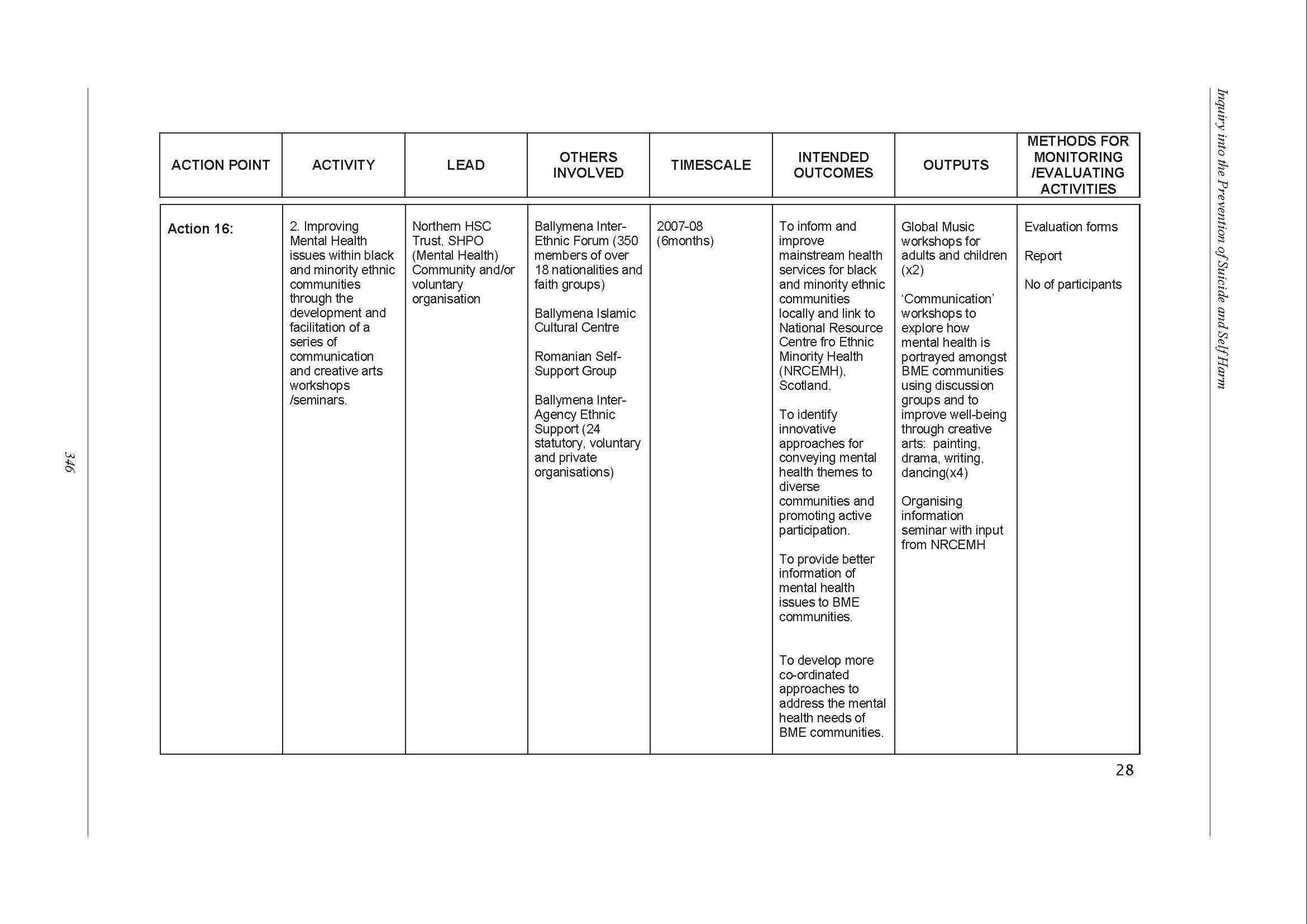
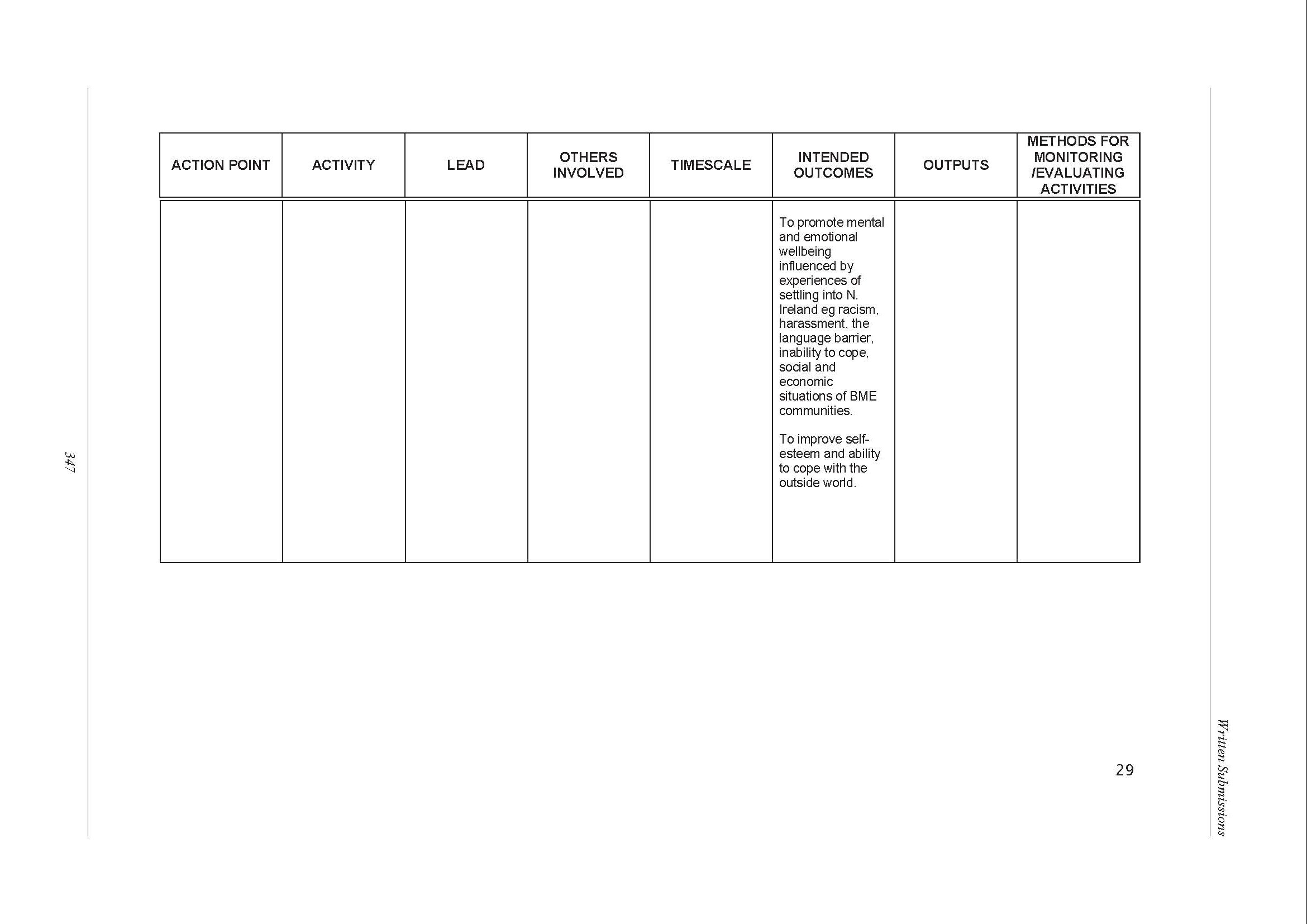
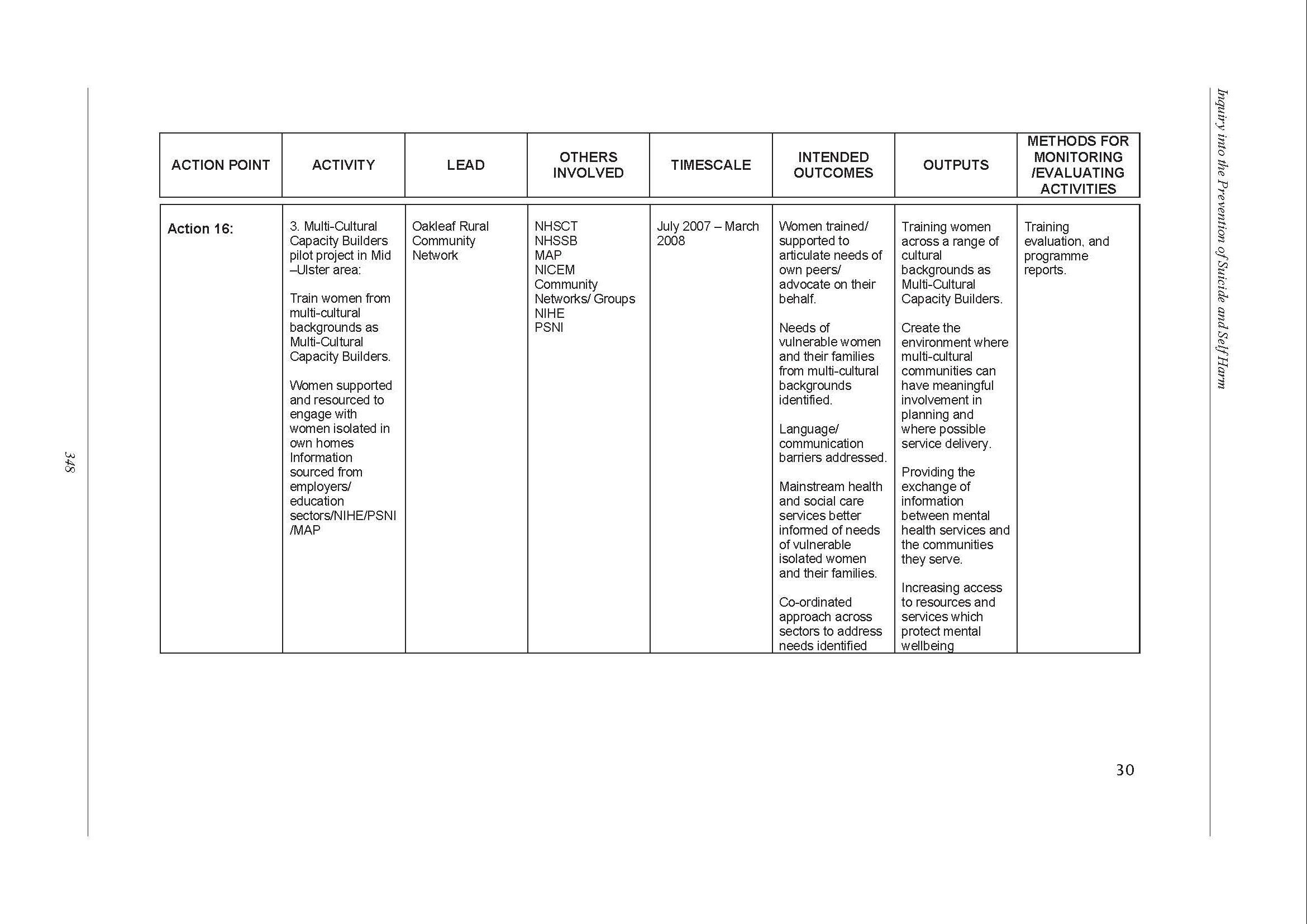
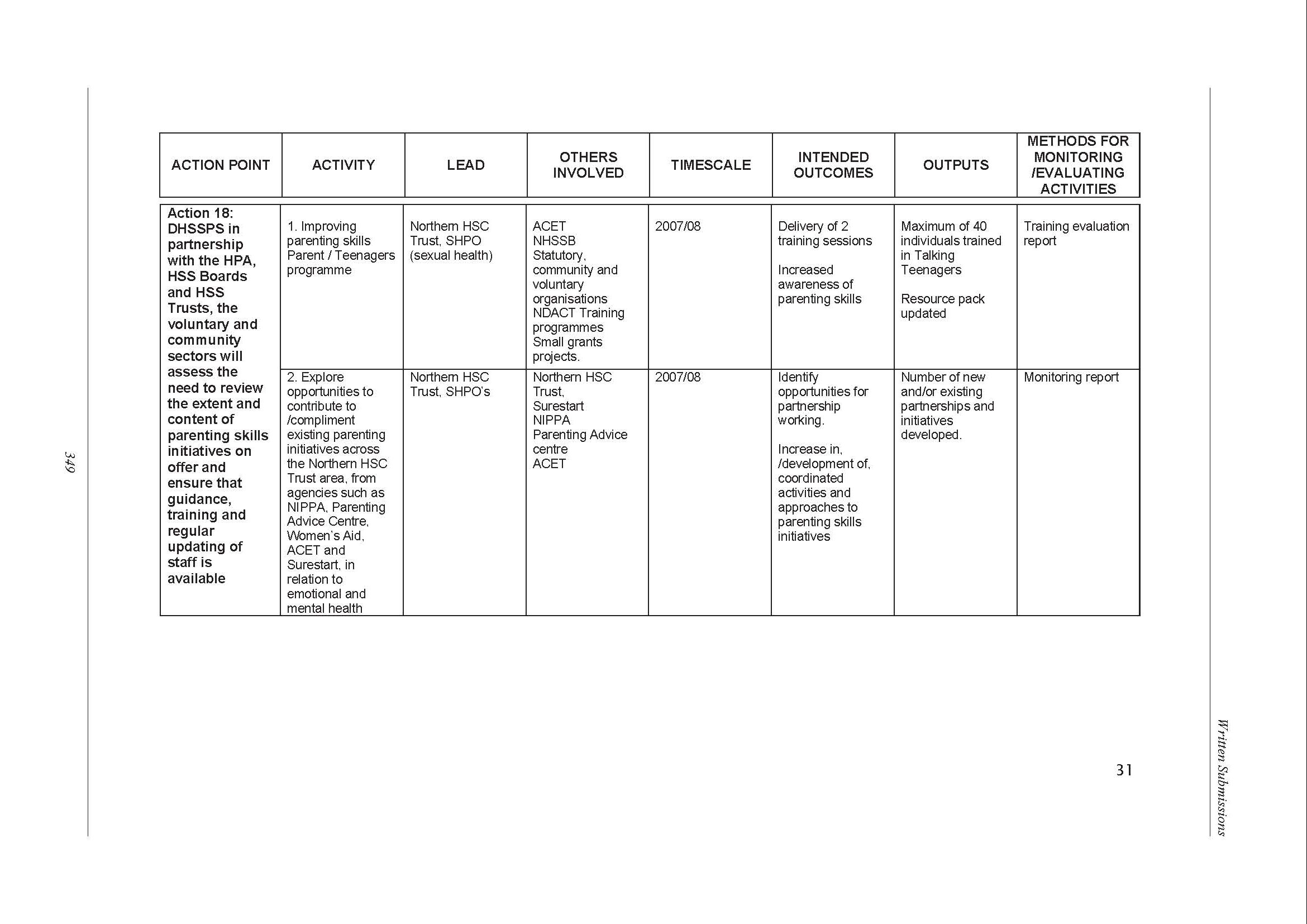
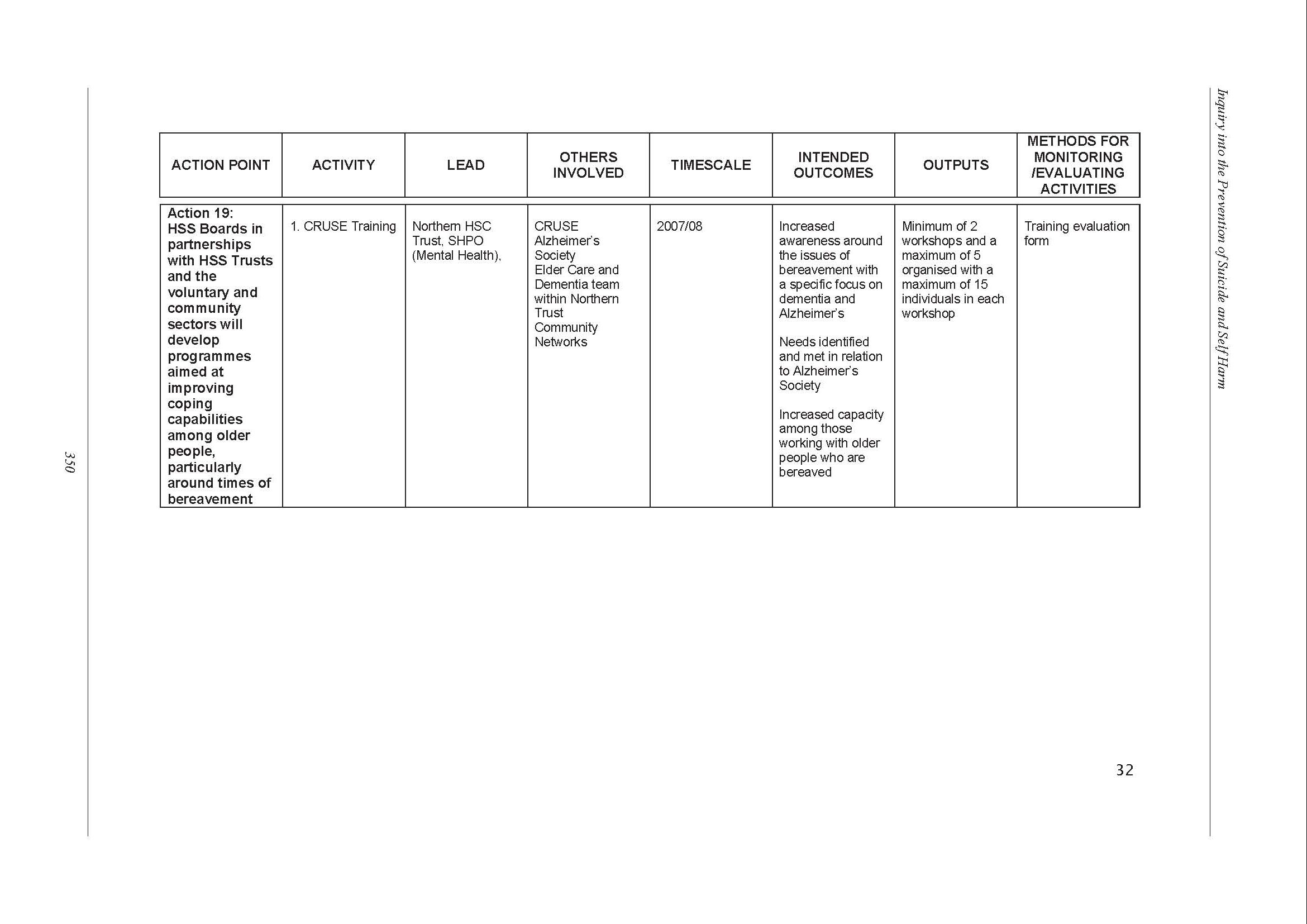
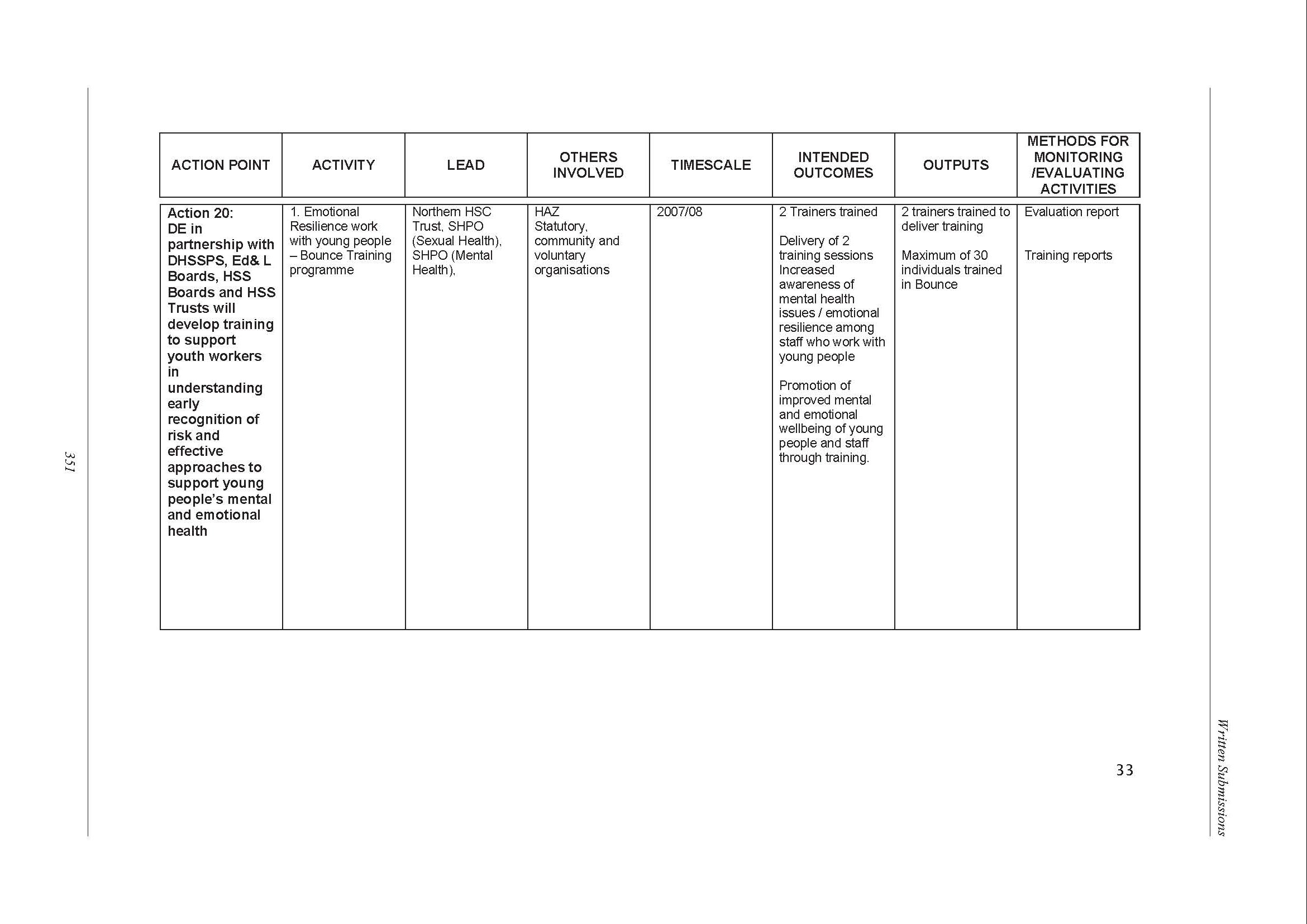
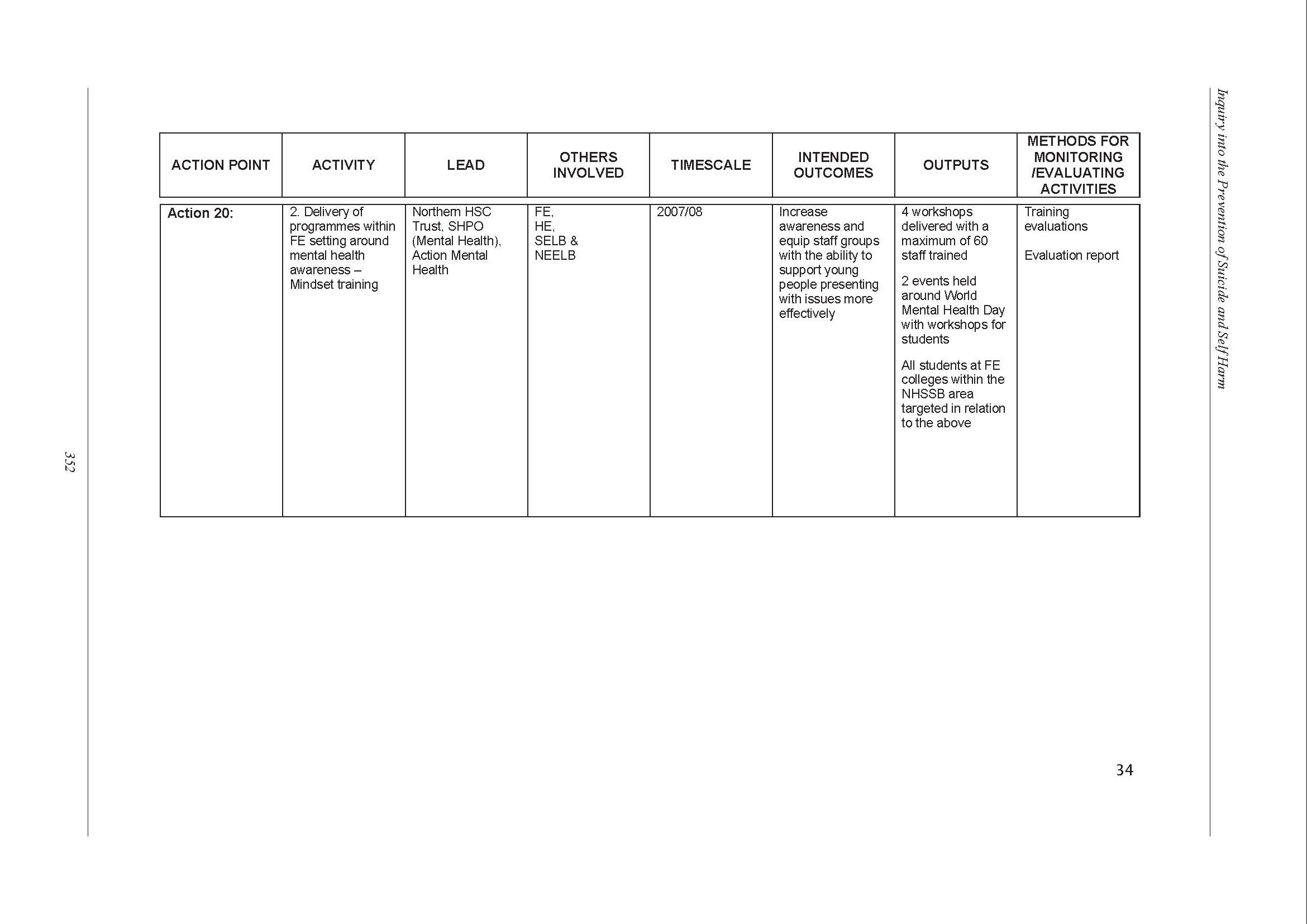
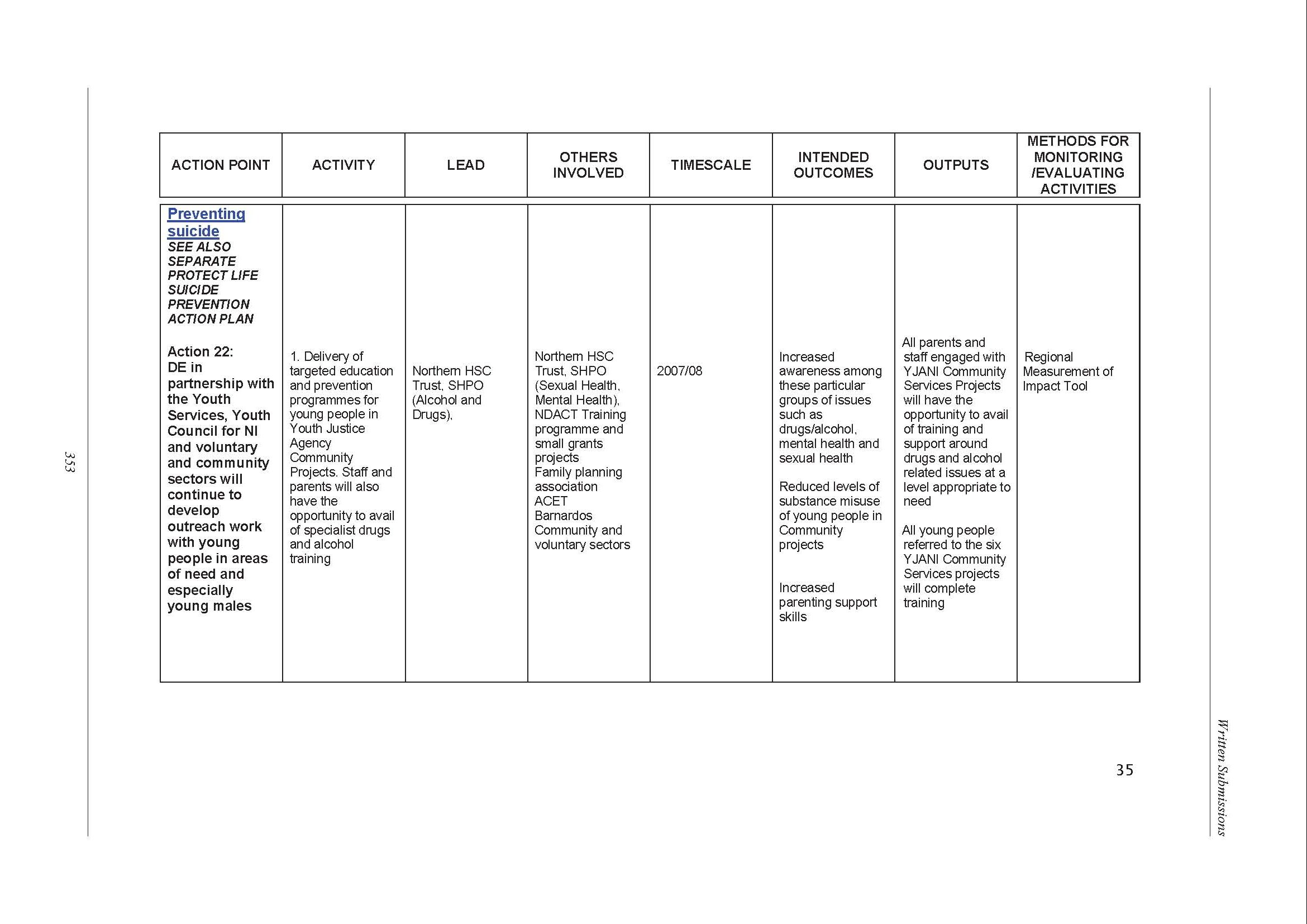
Voice of Young People in Care
Introduction
Voice Of Young People In Care, VOYPIC, is an independent regional voice that seeks to empower and enable children and young people with an experience of care to participate fully in decisions affecting their lives. Our aim is to improve their life chances through working in partnership with children, young people, staff, managers, agencies and government. We do this through listening, learning and facilitating change which impacts on and influences legislation, policy and practice.
VOYPIC works across five project areas, advocacy, mentoring, policy, participation and research. All of these areas focus on issues that are important to children and young people who have an experience of care.
Issues re mental health and emotional well being
Many young people who have an experience of care, that is have been removed from their families for a period of time and have been “looked after” by local Health and Social Care Trusts, are vulnerable to poor outcomes. This has been well documented across education, employment, housing and health, including mental health and emotional well being.
VOYPIC has been very aware of the difficulties that many of these young people have in relation to mental health and emotional well being and in response to this carried out research on the issue, in partnership with the EHSSB and Down and Lisburn Health and Social Services Trust. This research was known as the Caspar project and involved individual interviews with 51 young people aged 12-21 years who were living in a range of care settings, residential, foster care, aftercare, across the Eastern Health Board. These young people were randomly selected and had not been identified as having mental health or emotional well being needs. The research outcomes, which are documented in the research report “Don’t be so Formal, I’m normal” clearly indicated that there were significant issues experienced by young people, which compromised their mental health and emotional well-being and 17 strategic recommendations were drawn up based on these. A copy of the recommendations is attached in appendix 1.
Issues raised by young people re suicide
On 15th June 2006 a consultation was carried out with five young people on the draft suicide strategy. The consultation looked at the areas in the draft strategy that were most relevant to the group, that is, young people with a care experience. It was agreed, before the session, that the consultation would focus on the section on “children and young people” page 42 and 43 of the strategy document. The views expressed and the words used in the next section of this response document are those of the group members.
How the session was designed
To make sure that all the information was easy to understand VOYPIC staff designed appropriate exercises that would support the group to give their views on the strategy.
Instead of asking the group to give their views on the objective and each target a general discussion on suicide was facilitated. From this it was clear that all group members felt that suicide was a very important issue and that the government needed to take it seriously and do something to help young people.
To help the group identify the issues that they felt were most important we designed an ‘issue wall’. This gave the group the opportunity to talk about what was important to them and to other young people with a care experience.
The final stage of the consultation involved young people ranking the issues in order of importance; examining each issue; and highlighting what needed to happen in order to help young people with the issue.
What young people said
The group highlighted the following issues as being of importance and concern to young people with an experience of care in relation to the suicide strategy.
1. Bullying- this could occur in the work place, school or where person is living.
2. Alcohol and drugs, this could be use by parents or self.
3. Stigma – included mental health and being seen as different because of clothes, music, sexuality.
4. No family contact
5. Low self esteem
6. Lonliness
7. People letting young people down about important things, e.g. parents, social workers and other professionals
8. Depression
9. Bereavement
10. Staff in residential units not understanding young people’s issues and responding in an unhelpful way.
11. Having no hope.
12. Having difficulties with relationships, finding it hard to trust people. Professionals and others.
13. Leaving care, having to take on responsibility for self, having nowhere to live, having problems with finance.
Young people’s recommendations
The group selected three issues and made recommendations in relation to how each could be addressed in a more positive and effective way.
Bullying
- Information services should be made more readily available to all young people. There should be free helplines.
- People need to be taught about bullying, about what it is. The stigma of bullying needs to be broken.
- Young people who come forward to report bullying need to be able to remain anonymous.
- The police need to set up a service for people who are being bullied. The police or schools need to take more control of bullies and need to provide more support to those people who are being bullied.
- There should be a government representative to act as an independent body for complaints.
- There should be better training for teachers on dealing with bullying. They should take responsibility for dealing with bullying and accept that it is happening.
- Free helplines should be available in schools
- Better counselling services should be available in schools.
- An outside person should be employed to deal with more difficult bullying situations.
Leaving Care
- Young people leaving care should be made aware of their rights, they should also know how to make a complaint.
- Young people should have support to gain and maintain employment, maybe through a tutor. They should be able to get careers advice.
- Young people should have ensured weekly income and get help to budget.
- Young people should be able to have pre-planned medical appointments and have help to set these up.
- Young people should know how to use the Housing Executive.
- Young people should be given suitable placements/places to live which meet their needs
- Young people should be helped to link into social groups.
- Young people should be helped to keep contact with family and friends.
- Young people should have someone to talk to in confidence about their feelings.
- Young people should be helped to build confidence and self esteem.
Bereavement
- Young people should have access to free helplines.
- There should be ads on TV and leaflets and posters advertising and providing information about agencies that can help with bereavement.
- Counselling should be available.
- Young people should be taught about coping mechanisms.
- Other people should be sensitive to the young person and give them space if they need it.
- Support should be available to the young person whenever they need it. This could be from family and friends or staff. There needs to be flexibility from staff.
- There should be services available for the young person to help them concentrate on positive things, this could be through mentoring.
Conclusion
The evidence that has been provided through the Caspar Research Report “Don’t be so formal, I’m Normal” and the consultation on the draft suicide strategy strongly indicates that there are significant issues which young people have to deal with on a daily basis which impact on their levels of mental health and emotional well being. Young people are very clear about the difficulties which they experience and rely on the adults around them to listen and act on the information which they are giving to them. It is our duty as a community to listen to what young people are telling us and to invest now so that they can have a decent future both for themselves, their children and the community of which they are a part. Bearing this in mind VOYPIC would like to draw the attention of the committee to the following three recommendations from the Caspar project.
1. To implement the following recommendations and improve the emotional health and well-being of Looked After Children requires a Ministerial Champion supported by a taskforce to drive forward an agenda for change in this time of administrative and political restructuring.
2. Northern Ireland requires a local centralised body of expertise and knowledge focusing on Looked After Children.
3. Currently in Northern Ireland CAMHS services are hugely fragmented. This research supports the Bamford, (2006), recommendation 30, outlining the need to develop a model for LAC.
a. A cornerstone of the model must be close collaboration between social services and the networks surrounding the child.
b. The present CAMHS Tier 3 & 4 are not fully responsive to the needs of young people in relation to contact, placement issues, coping with new placements and talking about feelings. Further investment to Tier 1 & 2 is required to develop and enhance preventative work. It is also important that young people are able to access services at the time of need.
c. Training for staff across the different levels of provision within the LAC continuum is required to ensure the effectiveness of a preventative model.
Appendix 1
1. To implement the following recommendations and improve the emotional health and well-being of Looked After Children requires a Ministerial Champion supported by a taskforce to drive forward an agenda for change in this time of administrative and political restructuring.
2. Northern Ireland requires a local centralised body of expertise and knowledge focusing on Looked After Children.
3. Children experience a risk-adverse care system. There are distinct tensions between bureaucracy and a child-centred approach. Children engaged in a therapeutic process, coming to terms with their issues should be afforded confidentiality unless the child or another child is deemed in immediate risk. The tensions between statutory functions versus children’s needs must be explored through the facilitation of a high level cross-sectoral debate.
4. Where a child lives, may not dictate who they are but the attitudes of others can influence who they believe they could be. A public information campaign is required to dispel the negative images and myths about children in care, thereby directly reducing the stigma and discrimination faced by them.
5. Every child entering the care system experiences huge trauma and distress. This should be recognised and action taken to support the child to make sense of their experience and understand how and why they feel as they do. The provision of age appropriate information and communication is a critical factor in developing sound relationships with children and young people who experience severe disorientation when entering care. A training strategy is required to support staff and carers to have the skills, and resources to take responsibility for this critical aspect of the work.
6. The high levels of instability experienced by children in the care system contribute to mental ill-health. This instability results from lack of contact with family, placement moves, change of workers, change of school and friendship networks. Further research is required to identify how to minimise the negative impact of growing up in care.
7. Care experienced children and young people need assistance through the development of Positive Health Promotion Programmes to have an understanding and language which empower them to take more control of their emotional health and well being.
8. In managing emotional health and well-being, the culture of “referring young people on to specialist services” needs to be challenged. The value of the key relationships in the young person’s life are currently not adequately recognised. These key relationships should be identified, connected into a network of professional advice and guidance and supported in a process of capacity-building to enable them to address and assist the young person to manage their issues.
9. Children move out of families and risky situations into care and experience the stress of new cultures, new families and substantial change. This change presents different risks to their emotional health and well being and has implications for policy and practice:
a. Emotional well-being needs to be a central concept in placement planning.
b. The assessment process needs to be child-centered with specific focus on emotional health and well being; understanding the impact of past experience and the potential impact of each placement.
c. To ensure the effectiveness of the assessment process, training is required by staff and carers to understand the impact of loss, stigma, change and new family cultures.
d. Child friendly tools need to be developed, which support this holistic approach, and mainstreamed into the current assessment process throughout a child’s life in care.
10. Contact with parents, siblings and significant members of the extended family remains a critical factor in determining the emotional health and wellbeing of the child and young person. This needs to be recognised, resourced and integrated fully into all care plans and supported by key professional in the child or young person’s life.
11. Continuity of social worker, thereby developing strong, sound relationships and having time outside crisis situations was identified as a key protective factor by children. This requires staff having dedicated and sufficient time, through smaller case loads, to build relationships with children in distress. A training and development strategy promoting one-to-one individual work skills with children will ensure effective implementation.
12. The decision-making process, particularly the LAC Review, is viewed by children as procedurally driven and not child centred. Children need to be active participants, have more control and be empowered to come to terms with decisions.
a. A small core group of decision makers needs to be wrapped around the child and mandated to assess and manage risk, providing ongoing and immediate decisions based upon the best therapeutic outcome for the child.
b. A Departmental Review of care planning procedures needs to be carried out with a view to devising a range of models that meets both statutory requirements, but also facilitates young people’s participation, taking account of current circumstances. Such a review should address:
- Preparation and planning
- LAC forms
- Procedures
- Social Work Report
- Content and process of reviews
- Contents of Plans
- Timescales
- Young people’s engagement
13. Respite care presents a range of competing needs, that is the Foster carers need for a break, the child’s need to feel part of the family and the systems need to support the placement. Children require an open and honest discussion from the outset to explain respite care and address the impact on the child. It is critical that the child retains a sense of belonging, stability and emotional security.
14. Education, training and employment provide children and young people with a range of protective factors. The findings of the Caspar Project need to be presented to and integrated into current initiatives:
a. Implementation of the Children Leaving Care Act, with particular reference to the training strategy for Pathway Planning and Personal Advisors.
b. The Regional LACE Project. Particular issues to be addressed will include:
I. Awareness raising in schools through Citizenship Educations and PSE
II. Anti-bullying strategies
III. Managing personal information
IV. Designated teachers
V. Personal development
15. Engaging in leisure activities presents the greatest challenge for residential care and work is required to increase children and young people’s confidence and ability to participate. Leisure should be promoted in the individual care plan and supported by a well-funded leisure strategy.
16. Transition to adulthood presents particular emotional issues for young people and there is often a need for ongoing support:
a. Protocols need to be developed with Adult Mental Health to ensure continuity of the provision of mental health services.
b. There needs to be training for frontline workers in Adult Mental Health services, including Accident and Emergency Services, about the particular emotional and mental health needs of young adults who have an experience of care.
c. There needs to be some flexibility for those young people who are approaching the age of 18, but are still engaged in therapeutic work with CAMHS , to allow them to complete this work.
d. A mental health professional should be attached to Leaving Care teams to provide ongoing support to those young people who require it, until the age of 21.
17. Currently in Northern Ireland CAMHS services are hugely fragmented. This research supports the Bamford, (2006), recommendation 30, outlining the need to develop a model for LAC.
A cornerstone of the model must be close collaboration between social services and the networks surrounding the child.
The present CAMHS Tier 3 & 4 are not fully responsive to the needs of young people in relation to contact, placement issues, coping with new placements and talking about feelings. Further investment to Tier 1 & 2 is required to develop and enhance preventative work. It is also important that young people are able to access services at the time of need.
Training for staff across the different levels of provision within the LAC continuum is required to ensure the effectiveness of a preventative model.
British Medical Association
University of Ulster
Thank you for asking the University to respond to this important consultation. We welcome the opportunity to contribute to the strategic direction and operational guidelines on the prevention and care of those affected by suicide.
Probably the most important document that has been produced in recent times in Northern Ireland is: Protect Life: A shared vision, which was published in October 2006. This document has a number of well made points with regard to suicide. Its proposed strategy of targeting vulnerable populations is to be commended. It identifies young males and those bereaved by suicide as being particularly vulnerable. Recent developments within Northern Ireland, particularly PIPS in Belfast and the recent ‘Buddying’ contract awarded to Zest – Healing the Hurt are prime examples where the strategy is being operationalised. In addition, recent changes within statutory services such as the development of ‘Psychological Therapy’ are to be commended. While the proposed opening times until 1.00am are an improvement, there is a need for 24-hour support as there is evidence that many people feel at their lowest in the earliest hours of the morning.
Suicide Related Behaviour and Mental Health Nursing
Successive government enquiries have shown that suicide following discharge from hospital is high among patients experiencing mental health difficulties. Therefore, more could be done whilst people are inpatients in mental health facilities. The most important group in the delivery of inpatient care are Mental Health Nurses and so are in a prime position to help inpatients who may have suicidal ideation.
Interventions in Attempted Suicide and Self Harm
In recent years there have been reports that psychopharmacological interventions may be less effective than was previously thought. Certainly the link between Seroxat and suicide in young people has been highlighted. In addition, some authors have questioned the effectiveness of the SSRI and SNRI group of medications in the treatment of attempted suicide and self harming behaviour.
Recently, the National Institute for Clinical Excellence and the Sainsbury Centre for Mental Health have indicated that ‘talking therapies’ such as Cognitive Behavioural Therapy (CBT) offer a way forward. CBT is an effective counselling / psychotherapeutic intervention treatment and the academic research literature supports its use in the prevention of suicide. However, the empirical evidence suggests that people in crisis are not always seeking solutions. Frequently they are trying to understand themselves and what is going on in their lives. Other therapies such as ‘Patient Centred Therapy’, ‘Family Systems Therapy’, ‘Gestalt Therapy’ and ‘Psychodynamic Therapy’ can also offer effective interventions. Nonetheless, it is not about matching the person to the therapy, it is about matching the therapy to the person. In Northern Ireland there is a need for mental health teams whose members are competent in the delivery of specific ‘Talking Therapies’. An analysis of the skills and the skill mix required in front line mental health carers is urgently required if we are to provide appropriate care for people following self harm or attempted suicide.
The prevention of suicide and related behaviour
Unfortunately, many eminent researchers will agree that preventing suicide in its totality is near impossible. Nonetheless, many will also agree that the reduction of suicide and other related behaviour such as self harm can be achieved. This type of thinking requires a mind shift by Government. Much of the current research focuses too much on causative factors and how people commit or attempt suicide. There is a need to focus on factors that have helped people to regain their will to live. Indeed, research that identifies what has helped people to refocus their suicidal thoughts towards a life orientation is of the utmost importance and should have a higher funding priority than investigations into why people attempt or commit suicide.
Suicide and self harm are much commoner in younger people (15 – 24) than in other age groups. As alluded to above, this age group has been identified in the ‘Protect Life’ strategy. Issues such as bullying, sexual orientation and difficulty in relationships frequently are often at the roots of suicide and other related behaviour. The empirical literature suggests that young people have difficulty with problem solving or coming to terms with complex issues in life. This has implications for both research and practice. Currently, such research is being undertaken in a joint Research and Development Office funded Project between the University of Ulster and Queens University Belfast (McKenna, Jordan).
In addition, The University of Ulster has in the last academic year completed a preliminary study into the aetiology of suicide based on cases recorded in the Greater Londonderry area between 2000 and 2005 (Moore). This research has used the contemporaneous notes of the Forensic Medical Examiner called out to investigate the death of the victim and also the official forms completed by the Police Investigating Officer. Such combined information presented a unique opportunity to elucidate the historical background of the victims, to record details of methods used and other possible causative factors relating to the suicide. The detailed analyses of these data have been rapidly accepted for publication in the Journal of Forensic and Legal Medicine and should be available nationally before the end of 2007.
The main findings have highlighted the upward trend in the occurrence of suicides in the North West, particularly among young males in their late teens and twenties. These results mirror the results of other studies that have been officially published elsewhere and reports in the local news media concerning suicides in other regions of Northern Ireland.
The preliminary UU report, published in July 2007, concluded with a call to local policy makers to enhance the level of services available to potential suicide victims. Additionally, it has called for increasing attention to be paid to the control and possible prevention of malicious websites dedicated to the encouragement and promotion of suicide. This call was also highlighted by the recent UTV Insight programme to which the UU contributed.
We recommend that the opportunity be taken to support locally-developed scientific research on the causes of suicide attempts in those areas where there has been a huge rise, such as North and West Belfast and the Banbridge area. One project has been underway to validate the use of hair and saliva sampling to track down the long-suspected link with antidepressant use in these young people. A research team at UU has published three papers on state-of-the-art analytical chemistry (Smyth). They demonstrated the effectiveness of hair and saliva sampling in the detection of antidepressant and other drug use.
Scope and appropriateness of the Protect Life: A Shared Vision
From our point of view, the ‘Protect Life Strategy’ adopts a very narrow focus with the main thrust being on the impact that mental health and psychiatric disorder can have on a person, perhaps leading them toward suicide. There are a number of important issues arising from the strategy:
1. The ‘Troubles’
The impact of the ‘Troubles’ on the social and emotional well-being of the population as a whole and on individuals is not really addressed. As part of the strategy a review of literature was published in July 2007 into the impact of the ‘Troubles’. However, this again maintained the narrow focus on mental disorder.
What is missing is any discussion, or comment, on the social impact of the ‘Troubles’. For example, inward economic investment was low during the conflict; does this under investment have a role to play in suicide today? Low skilled, temporary or unstable employment can be viewed as risk factors for suicide. Other social factors associated with suicide including educational attainment and marital status and these may have been affected by the ‘Troubles’.
Similarly, the psychological aspects of a person do not really seem to be considered. In 2005, colleagues in UU published findings from a study suggesting that the ‘Troubles’ afforded some social cohesion and a sense of identity (McGowan). As we move toward normalisation, where do people get their identity from and how do they identify themselves? Again, these are well established risk factors for suicide, yet do not seem to be considered in the strategy. The University of Ulster is currently engaged in developing a programme of research with colleagues across many European countries to address these issues (McGowan).
2. Vulnerable Groups
Suicide and self harm are complex human phenomena, have multi-faceted aetiologies and permeate all groups in society. The incidence of female suicides is much lower than that of males but, paradoxically, the incidence of female self harm is higher. Additionally, the University of Ulster is taking forward international collaborations on suicide and self harm in pregnancy and the first post-partum year. This is a much under rated problem that can have serious consequences for the individuals, their off spring and the families (Sinclair).
It has been shown, for example that NI and Poland are the only two countries globally in which the suicide rate in the older population is lower than other age groups. Why is this so? Also, recent evidence suggests that there is a slight increase in the suicide rates in the over 65’s. As the population grows older this is an area that requires further consideration. A pre emptive approach to older suicide is needed. Therefore, the reduction / prevention of suicide and self harm should be perceived in the broad context that includes both sexes and all age groups. Any five year strategy needs to take into account of changing demographics and other factors. Subsequently, the absence of these may suggest that the current strategy is no more than a reaction to current issues, with little thought for future problems.
3. Suicide & Self harm in one strategy
There is a brief acknowledgement in the strategy on the differences between self harm and suicide. However, the link between them is not emphasised. Indeed, researchers within the University of Ulster have recently published in this field and offered clarity to health care professionals (McLaughlin). While suicide and attempted suicide are death orientated behaviours, self harm is a life orientated. Accepting this, it is well documented that those who have a history of self harm are at higher risk of eventual suicide than any other group. Many of the well known interventions address suicide but few, with exception of the current programme run by Zest, offer assistance to those who self harm or those who have attempted suicide.
The aim of the strategy is “To reduce suicide in Northern Ireland” and the majority of interventions address this. Self harm where there is no lethal intent doesn’t seem to fit in this strategy. Comments such as “less serious self harm” as a generality are dangerous and arguably increase the stigma of self harm.
4. Dissemination
Northern Ireland is unique in that it appears to be the only country that is in conflict or coming out of conflict to have a suicide prevention plan or strategy. In the UU work with colleagues in Bosnia, Kosovo and Israel it is apparent that they expect an increase in suicide as ‘normality’ returns (McGowan). Notwithstanding the above, the population and targeted model of suicide prevention is good, and there needs for international dissemination of good practice and innovative research to help these countries address what they expect to be a rise in suicide.
Level of Stakeholder Involvement
It is notable that there was no local academic input into the Taskforce’s deliberations. While, some eminent academics were included in the QA group, none have any recent direct experience of suicide in Northern Ireland. The evidence base of social, psychological and biological factors influencing suicide, from a Northern Ireland context, does not appear to have been taken into account.
Level of services and support available
The strategy acknowledges correctly that no universally effective treatment or intervention has been found. Subsequently, we need to be innovative in our approach to suicide and self harm prevention. At a policy level the development of a co-ordinated regional service offering consistent individualised care (and where required, treatment) should be considered.
Further action
As with the service development there needs to be a structure in place that allows for academia, service providers and users and other interested parties to co-ordinate and plan an innovative programme of work. We would argue that this should be placed in a University setting where there is the expertise, experience and networks to assess the need, plan the intervention, deliver it in partnership with our clinical colleagues, evaluate and disseminate the findings regionally, nationally and internationally.
We would call on the Committee of Inquiry to recommend that the research that has been ongoing in UU on the prevention of suicide, and the support, care and treatment of families and suicide survivors be continued and expanded. This would facilitate the establishment of a database of information in order to enhance our understanding of the motivations for suicides that have led to the upward trend in its occurrence. The research would also enable policy makers to monitor and assess the accuracy of any measures subsequently undertaken for its future prevention and control.
Specific areas needing urgent attention;
- The prevalence and demographics of people that self harm;
- Research that identifies what has helped people to refocus their suicidal thoughts towards a life orientation;
- Improvement and innovation in understanding suicide (e.g. case studies, non linear dynamics, sociological autopsy, through the arts);
- The social and psychological impact of losing a person to suicide;
- Establishing what suicidal people want from the services;
- Establishment of a Centre for Suicide/ Self Harm Research & Development;
- Establishment of a central register of self harm and attempted suicide presentations at A&E departments;
- An exploration of how health and social care professionals respond to suicidal behaviour;
- A commitment to long term funding for any suicide prevention strategy whether it be clinically or research focussed or both;
Once again, the University of Ulster are pleased to see that this important issue is getting the attention of politicians and policy makers and we would like to thank the Committee of Inquiry for seeking our views. We would be pleased to supply further information and publications on the studies referred to in this response.
Professor Hugh McKenna, Dean, Faculty of Life & Health Sciences: with input from:
Professor Julian Leslie (Psychology)
Dr Franklin Smyth (Biomedical Sciences)
Professor Marlene Sinclair (Midwifery)
Dr Tara Moore (Biomedical Science)
Dr Columba McLaughlin (Nursing)
Dr Sinead Keeney (Nursing)
Mr Iain McGowan (Nursing)
Queens University Belfast
1. This submission is based on research carried out recently for the Department of Health, Social Services and Public Safety under Northern Ireland’s Suicide Prevention Strategy. The Strategy calls for initial research on suicide, including finding out what, if any, relationship exists between the legacies of ‘the troubles’ and current suicide trends.
2. The research took the form of a systematic literature review to assess the evidence of the effects of the Northern Ireland conflict on mental health and well-being, with special reference to suicide. Evidence was gathered from all over the world, with a particular focus on studies of countries and regions in conflict. The report is called The Trouble with Suicide – Mental Health, Suicide and the Northern Ireland Conflict: A Review of the Evidence, and is available at http://www.investingforhealthni.gov.uk/
3. The report includes an examination of suicide trends from the 1960s to the present and shows how these trends break down by age and gender. In global terms, Northern Ireland has a low-to-medium suicide rate. However, the rate appears to be rising and this is against the trend of most countries and regions of the European Union, with the exception of some Eastern European countries and the Irish Republic which saw a steady increase in the 1990s (and a slight decline since).
4. The report also looked at available evidence of self-harming. Knowledge of this issue in Northern Ireland is derived from hospital presentations but most self-harming does not come to the attention of health and social care professionals. This is a known issue and progress is needed as a matter of priority so that the ways in which anxiety, distress and depression are being experienced and expressed by younger people can be better understood and supported.
5. Recent increases in registered suicides in Northern Ireland are largely accounted for by men in younger age groups, especially under 35 year olds. The suicide rate for 25-34 year old men doubled between 1995 and 2000. This age group saw a three-fold increase in the rate of suicides amongst women over the same period, but from a much lower base and smaller numbers.
6. The highest suicide rates for women in recent years are in the 45-54 year old age group, followed by the 25-34 year old group. For men, the highest rate in any year tends to be for the 25-34 year old group followed by 15-24 year olds. These are fairly recent trends as the highest suicides rates are traditionally found amongst older people, a pattern reflected in many countries with stable or declining suicide rates.
7. There has been an erratic upward trend in the number of suicides among the under 25s, with peaks of 42 in 1988 and 45 in 2000. Taking all the deaths for this age group, ‘transport accidents’ and suicides typically account for a half or more, with the former as the leading cause of death. Suicides account for about one fifth of the deaths in this age group in any year. But this has not always been the case. Going back to pre-conflict 1967, suicides account for just under 5 per cent of all deaths among 10-24 year olds.
8. The youngest group represented in the published suicide data is those aged 10-14. While the numbers involved are very small, there is a discernible increase in recent years. In the two years 1967 and 1968, three children aged 14 or younger killed themselves according to the official record, but from 1969 to 1980 only one suicide occurred in this age group. Over twenty years from 1967 there was less than one death every two years in this age group. The average since 1997 is now 1.1 a year.
9. The number of male suicides recorded in any year in Northern Ireland is typically 3.5 times the number of female suicides. That ratio appears to have come down slightly over the last decade. In most parts of the world more men than women take their own lives and in some countries the ratio is as high as 6 to 1 (eg in the Russian Federation). Rural China and parts of India provide exceptions to the gender rule.
10. There is a class profile to suicides. For men aged 20-64 in social class V, the risk of suicide was seven times that for men in social class 1 (based on men in Northern Ireland 1991-93).
11. Scotland has the highest suicide rate of all countries in the UK and Ireland. This was 17.6 suicides per 100,000 population (age standardized) in 2002, the year that a suicide prevention policy was introduced. It has since fallen to 14.7. Northern Ireland’s overall rate was between 9 and 11 over the last decade but rose to 12 in 2005 compared to England’s rate of 9. Scotland’s rate for men is 22 compared to Northern Ireland’s rate of 20 and the Republic’s rate of 17. Although not too much reliance should be placed on a single year’s figures (for reasons explained below) it is clear that Northern Ireland is poised to become the worst area for suicide on these islands.
12. Before 1998, no parliamentary constituency in Northern Ireland came anywhere near Scotland which had fourteen of the top twenty worst areas for suicides in the UK. But after 1998, North Belfast had gone from 319th to 11th place, with a suicide rate of 35.4 for men (1998-2004), and West Belfast from 259th to 13th, with a male suicide rate of 34.2.
13. Over the period 1999 to 2003 Banbridge had the highest suicide rate of all the district council areas. Belfast, Omagh, Newry and Mourne and Strabane were all above average.
14. According to the official figures, there were 291 registered suicides in Northern Ireland in 2006. In 2004 the figure was 146. At first glance this is an alarming increase over a short period. The official figures, however, are difficult to assess over a short period as there are considerable time delays before a suicide comes to be registered as such. For the period 2002-04, for example, the three year rolling average of registered suicides was 158 (per year), but the suicides that occurred each year over that period averaged 184. Another way of looking at this is to observe that only 72 of the 291 suicides registered in 2006 actually occurred that year.
15. The discrepancy between suicide occurrence and registration is an issue that needs to be addressed. This involves reviewing the procedures governing death certification, post-mortems, inquests and the coronial system.
16. Experts are divided over the impact of the years of conflict on Northern Ireland’s mental health. Population based surveys have produced evidence of a strong association between direct conflict experience and poor mental health. Those who experienced most violence have significantly higher rates of depression than those with little or no experience. There is also evidence that people whose areas had been heavily affected by violence had very high rates of depression.
17. Only a minority of people who kill themselves have been in contact with mental health services in the previous twelve months (less than 30%). Since 1996, the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness at Manchester University has been gathering data on all suicides in the UK. Northern Ireland participates in the NCI but the most recent report on the last five years (April 2000 to December 2004) covers only England and Wales. Valuable data on the situation and treatment of a substantial number of suicides has been collected but not analysed.
18. Northern Ireland’s legacy of poor mental health is reflected in other observations such as the Bamford Report’s statement that the prevalence of mental health problems is ‘at least 25% higher than in England’. The proportion of people in receipt of Disability Allowance for mental health reasons is three times the figure in Britain. 22 per cent of the population in Northern Ireland have used prescribed sedatives, tranquillisers and anti-depressants compared to 12 per cent in the Irish Republic. From 1989-1999, there was a 5.7 fold increase in the volume of prescribed anti-depressants. By 2005, 1.4 million anti-depressant prescription items were issued in Northern Ireland, or .78 prescription items per head. The proportion of those drinking ‘above sensible levels’ rose from 9% (1986) to 19% (2000) for men and from 3% to 9% for women. 9% of males drink at ‘dangerous’ levels.
19. Some studies have shown that anti-depressant prescribing is associated with lower suicide rates for some age groups. On the other hand such medication is involved in up to one fifth of suicides. Because of possible links to suicide, there are now official warnings against the use of selective serotonin re-uptake inhibitors for children, even backed up by manufacturers themselves.
20. Alongside the increased use of prescription drugs, there is evidence that the use of illicit drugs has risen sharply since the mid-1990s.
21. Such patterns indicate that over the past decade in Northern Ireland key risk factors traditionally associated with suicide at the individual level – depression, alcohol and drugs problems – have all increased. These trends present major challenges to the suicide prevention strategy.
22. How these risk factors relate to past patterns of conflict is poorly understood. There is little systematic evidence concerning suicides amongst those occupational and other groups who were in the frontline of conflict. Although specific risk groups have been defined in the suicide prevention strategy, the evidence base appears to be weak. A number of small research projects need to be carried out with specific groups, including ex-prisoners, to provide better evidence of mental health needs and suicide risk. There is also the suggestion that the particular stresses of frontline activity have led to higher rates of physical illness and premature death. Again, this ought to be investigated.
23. There is a lack of knowledge about how families and local communities cope with depression, self-harming and suicide, and how knowledge of, and attitudes towards potential sources of help vary. Funding community-based projects allows local experience and knowledge to be developed and consolidated in conjunction with those working in public services such as teachers, GPs, social workers, and mental health professionals.
24. Suicide prevention policies can only succeed in the long-term if they are based on a proper appreciation of the economic and social changes that contribute to social isolation and greater levels of anxiety.
Mike Tomlinson
School of Sociology, Social Policy and Social Work
East Belfast Mission
Overview of our Service
Hosford House is a homeless hostel providing accommodation for single people aged 18 to 65. Our aim is to ensure that people who are homeless, or at risk of homelessness have an effective response to their needs. One of our objectives is to facilitate access to appropriate health and care support services for those engaged with EBM homelessness services. Our Staff have a variety of experience from throughout the care field. None are qualified Social Workers or mental health professionals. On the job training is provided for everyone to deal with medium support needs and what resources are available in specialised fields.
We have built professional, mutually respectful relationships with most of the healthcare agencies we use regularly and can rely on them for support and advice when required. There are a number of services we can access to gain support for our Service Users including Multi-Disciplinary Homeless Support Team, our local GP and the mental health team at Woodstock Lodge. We also have a pastoral team and limited counselling within our parent organisation (East Belfast Mission/ EBM).
What we have found overall is that waiting time for psychiatric assessments in the community is too long. This can often take months and by then someone’s circumstances can have deteriorated significantly. What has happened regularly is that SUs go to their GP who prescribes anti-depressants and/or sleeping tablets. There is a lack of services for training professionals in dealing with self-harm and helping SUs prevent and deal with self-harm.
In our collective experience of 5 years at Hosford House we know of one person who was referred to Cognitive Behavioural Therapy. This person was in his fifties and had been diagnosed with OCD thirty years ago and had been abusing his medication regularly.
We have asked psychiatrists to refer our SUs to CBT in the past and they have refused stating that it would not be of benefit to the SU.
In the majority of cases where a SU has self-harmed or attempted suicide, they have suffered sexual abuse. Referral to the only agency in NI that specifically provides counselling with survivors of sexual abuse has a waiting list of up to 2 years.
Experience of support services
Below is a few of our experiences of dealing with suicide attempts and self-harm. This covers some of the more serious incidents we have dealt with in the past year or so and what support we or our SUs have or have not received from healthcare services.
December 2004 to January 2006
Cathy has a history of alcohol and drug abuse, sexual abuse, dysfunctional family, violent behaviour. She had been taking overdoses and cutting herself since her early teens. She has a conviction for stabbing an ex-partner and served 3 years in prison.
She presented to staff as having audio hallucinations telling her to kill herself and the member of staff on duty. She said she had been having the hallucinations for some weeks but they were becoming out of her control. She had a clear plan of how she would kill both the staff member and herself and was in possession of a knife. Staff managed to persuade her to hand over the knife after an hour of negotiation. PSNI and emergency medical services were called. Crisis Response Team said that she presented as no immediate threat to anyone and that they would not be doing any work with her. They left without recommendation or referral to any support service and Cathy with the member of staff she had threatened to kill.
August 2006
Betty had a history of being abused physically, psychologically and sexually by a number of people in her life. She had lived in several foster homes and short-term accommodation services. She had support from Social Services to have access to her children who were in foster placement, a SW from the learning disability team, EBM counsellor and a Floating Support Worker from the Aftercare team. She had a history of self harm, overdosing and cutting herself. She never received specialist counselling or therapy for any of the abuse she had suffered despite the number of agencies involved with her.
She was a Service User with us while two other young people with a history of self-harm were also staying here. The three of them found it difficult to deal with incidents involving each other one cutting them self led to another doing the same on a number of occasions.
June 2007
Anne, an ex SU, contacted us by phone to say she had taken an overdose of alcohol and tablets.
An ambulance crew went to Anne’s house; however she refused treatment so they left. Staff contacted her doctor’s surgery and spoke to a locum who said he would not make her a priority and told staff, “I don’t want to feed her behaviour for the next 20 years”. Staff told him they had been speaking to her over the past hour and she was starting to get sleepy since the tablets were starting to take effect and we thought it was a priority to get her medical treatment to save her life, at which point he said, “I’ll see what I can do”. He then called to say he had been to see her and she told him she hadn’t taken anything and to go away, which he did! We telephoned the practice manager and emphasised our concern. He responded by calling to see Anne and calling an ambulance and taking her to hospital. This action could have and should have been taken an hour earlier.
This person was then supported by CRT in the community for 1 week after being discharged from hospital. They refused to engage with her when she presented as under the influence of alcohol. She has a history of self-harm, cutting and overdosing. She has no long-term psychiatric care. She had an admission to Knockbracken Hospital for 2 weeks in Feb 2007 and was discharged with no mental health support services in place.
August 2007
Tom made an attempt on his life by trying to choke himself with a belt. When he was found he was almost unconscious. When the ambulance crew arrived they gave Tom the option of going to the hospital. He refused at first and after negotiation with staff on duty agreed to go. He was taken to hospital by ambulance and discharged by the doctor on duty with no follow-up care an hour later. The doctor on duty refused to discuss anything with hostel staff. Tom was advised to see his GP. The following day a doctor from casualty called to see how he was doing and expressed her concern and surprise that her colleague had discharged him without psychiatric assessment and no referral to psychiatric services. She then said Tom could call there anytime if he needed support.
This was the second time Tom had tried to commit suicide. During a previous stay at Hosford House he had tried to hang himself with a belt but was found by another SU. He had written a suicide note on that occasion. He was referred to the EBM counselling service who met with him the following day, and he saw his GP who referred him to the mental health team. Crisis Response Team saw Tom that day and said he was an inappropriate referral due to him not having a mental health problem but being under stress. They recommended he be given anti-depressants despite a long history of prescription drug abuse.
Another SU who had been involved in the incident with Tom has previously lost three friends to suicide. He had never received any type of counselling or support to help him cope with this. We arranged for him to see a counsellor at CRUSE (bereavement care) and his GP.
October 2007
One of our current SUs John has been cutting himself and has done so on 6 occasions within a 10 day period. On-call doctor and GP have been called on each occasion and they have said that he does not need to be admitted to hospital. The Crisis Response Team was called and was slow to respond. They told us his support needs were outside their remit, but were reluctant to tell us what their client criterion actually is. An emergency referral was made to Triage CPN via the SU’s GP who in turn made a referral to a Psychiatrist for assessment and to a specialist Psychiatrist.
Throughout this period the professionals involved fed back to the staff on every aspect of the John’s behaviour, assessment and work to be carried out. They listened to our input and were willing to take into consideration our limitations when formulating a care plan.
May 2006 to present
Twenty year old David has been staying with us on and off for the past 2 years. He has a history of being sexually abused and abusing medication and cutting himself. His family (parents and siblings) have a history of alcohol and drug abuse and involvement with the Child Protection Team at Social Services. On at least 7 occasions during his stays at Hosford House he has cut himself and needed emergency medical treatment. He has had no adequate follow up support after any of these incidents. What has happened is that he has gone to his GP and been prescribed sleeping tablets and over the years different anti-depressants.
It is obvious in this case that prescription drugs are not an effective solution without additional support.
He has also taken overdoses and is presently in ICU after taking an overdose 5 days ago. He was on a life support machine for 12 hours and has done long term liver and kidney damage.
Recommendations
- Supported housing should have fast-track referral to psychiatric services – with interim referral to Triage CPN. This would facilitate those in immediate need to be assessed when they are most in need
- Psychiatric team in community can make referrals to Hosford House or Floating Support. Floating Support would help prevent people having to leave their tenancies and provide them with support in their own home. If someone cannot manage to remain living on their own, mental health services can make a referral to Hosford House and provide support in conjunction
- Clinic at Hosford House every month with Triage CPN to feedback to Psychiatrist for assessment purposes.
- Funding should be made available for services that specialise in providing support for those affected by self-harm both personally and professionally.
- Increased availability of psychological therapies rather than prescribed psychiatric medication, particularly in cases where the SU has a history of medication abuse. Research has shown that addiction to anti-depressants and ‘benzos’ is common.
Caroline Cushenan
Senior Project Worker
The Rainbow Project
The Rainbow Project welcomes this opportunity to submit written evidence on the issue of suicide and self harm to The Committee for Health, Social Services and Public Safety.
The Rainbow project was set up in 1994 with the aim of addressing the physical, mental and emotional health needs of gay and bi-sexual men in Northern Ireland and has offices in both Belfast and L’Derry.
In 2006 The Rainbow Project published research on the mental health of young same-sex attracted men. The report aimed:
“To investigate the perceived and expressed mental health needs of young same-sex attracted men in Northern Ireland; moreover to explore how young same-sex attracted men’s mental health has been affected by society’s attitudes to people of a non-heterosexual orientation.”
The following are the main findings of the research (1):
The findings from the questionnaire show that almost one third (32.4 per cent) of the respondents had a potential psychiatric disorder (as measured by the GHQ 12 score) and over one third (34.4 per cent) of the respondents had been diagnosed with a mental illness at some time in their lives. The findings also showed in total 37.9 per cent of respondents received professional help and a further 3.2 per cent had been referred for professional help and did not follow it through. Of those who received professional help, almost two thirds said it was related to their same-sex attraction.
The impact of negativity when coming out, isolation, difficulties in school and work related to sexual orientation and homophobia in society where analysed. Combined, all had an impact upon mental health. However, the key factor which predicted whether the respondent showed signs of a potential mental health difficulty (GHQ of four or more) was the absence of someone to talk to. When all factors were taken into account, this was also the only significant factor that explained lower self-esteem on the self-esteem scale.
Over one quarter (27.1per cent) of the respondents had attempted suicide and over two thirds (71.3 per cent) of respondents had thought about taking their own life. Four out of five (80.5 per cent) of the respondents who had suicidal thoughts indicated that the suicidal thoughts were related to their same-sex attraction. Within the survey, 30.7 per cent of the respondents had self harmed. One fifth (20.6 per cent) of the respondents had self harmed more than once and 11.1 per cent had self harmed once. Two-thirds (64.4 per cent) of those who had self harmed indicated that the self-harming was related to their same-sex attraction.
As with mental health in the survey, it was a combination of different factors that contributed to suicidal thoughts, attempts and self-harm. In particular, homo-negative experiences in school had a crucial impact on suicide and self-harm. Experience of bullying was a key factor in predicting whether the respondent had attempted suicide, while homophobia from other pupils was a key factor in whether the respondent had considered suicide. Homophobia from neighbours or other tenants was also a key predictor for suicidal thoughts, attempts and self-harm. Those interviewed, who had attempted suicide, contributed their suicide attempts, in part, to difficulties surrounding their sexual orientation
It was apparent in the interviews that some of the young men held negative beliefs about their sexual orientation and had a fear of society’s attitudes to people of a non-heterosexual orientation. These factors were measured in the survey by the internalised homophobia scale. Those respondents who had a higher score on the internalised homophobia scale were more likely to have lower self-esteem, show signs of a mental health difficulty (GHQ12 above four) and consider suicide.
These quantitative findings were verified in the interviews. The young men spoke of different factors which affected their mental health. These factors were: difficulties accepting their sexuality, a shortage of people that understood what they going through and homophobia in school, at home and in society. Loneliness and isolation were subjects that also took great prominence in the interviews. It materialised that there was an absence of people interviewees felt they could talk to who understood issues surrounding sexual orientation.
Another common topic was the attitudes of family members to non-heterosexual orientations. Some interviewees described the blatant homophobia on their family’s part due to this unappreciative perception of what it is to be gay. It led to one young interviewee leaving the family home. Moreover, in the questionnaire, two fifths of the respondents moved out of home because of negative attitudes to their sexual orientation. Leaving home because of negative attitudes to sexual orientation was a key predictor for suicidal thoughts.
Those interviewed acknowledged that tensions with family members improved over time and that their families grew to accept their sexual orientation. Although, it transpired that this was often superficial. This was primarily connected to family members’ aversion of the subject. Family members did not candidly express disapproval of non-heterosexual orientations but for some, their son’s life as a gay man was never discussed and his sexual orientation was kept silent to extended family and family friends. The feeling of isolation remained with the young men and the inclusion that was so vehemently sought did not always happen.
It was confirmed through the survey and the interviews that most young men realise their sexual orientation while at school. Nearly two-thirds (65.3 per cent) experienced some difficulties in school related to sexual orientation. Most common were homophobia from other pupils (51.9 per cent) and bullying (44.7 per cent). Respondents who were bullied in school were more likely to have been diagnosed with a mental health problem, been referred for professional help, have a lower self-esteem, have self-harmed, have considered suicide and have attempted suicide. Additionally, homophobia from teaching staff was a key factor which explained higher GHQ score and referral for professional help.
It was clear to see in the interviews that the endemic homophobic pejoratives in school can have a negative impact on a young gay man’s acceptance of his sexuality. This was coupled with a lack of teaching on non-heterosexual orientations. Two thirds (66.3 per cent) of the respondents stated they would like more training in schools. The young men’s narratives also provided an overwhelming conviction that sexuality needs to be covered in the education system and some form of confidential and non-judgemental support needs to be available to students.
The survey and the narratives illustrate that homo-negative and heterosexist attitudes are widespread in Northern Ireland. Over one-third (33.9 per cent) of the respondents experienced negative attitudes at work because of their sexual orientation. Outside school, the most common place to experience homophobia was in an open place (44.2 per cent). However, two-fifths (41.1 per cent) experienced homophobia while receiving goods, facilities or services and 16.3 per cent were subject to homophobia from their neighbours or other tenants. An analysis of the findings and the narratives confirmed that homophobic incidents had an affect on the young men’s emotional wellbeing.
It appears that it is not just one instance of homophobia that affected the young men, rather, it is repeated instances of homophobia that had a negative affect on their mental health.
The needs of young same-sex attracted men are currently not being met. Although support groups for young same-sex attracted men exist, over half (55.3 per cent) of respondents had not used their services. There were practical reasons for this, such as the distant location of the groups or lack of knowledge of the existence of certain groups. Other difficulties also arose, namely that the young men were too anxious to attend by themselves. As limited support was available in school and family settings, the young men had no choice but to seek out other means to meet young LGB people. Most commonly, this was through the use of the internet and the gay scene. These avenues were invaluable to some of the young men. However, the research showed these avenues often do nothing to discourage self-destructive behaviours, such as alcohol or drug misuse or unsafe sex and they may not provide a supportive milieu for a young man who is lacking in self-confidence.
These collective factors have a bearing upon the mental health of young same-sex attracted men. It is therefore not a straightforward task to address the mental health needs of this population. A number of different elements will have to be addressed. LGB youth groups, personal development courses and individual counselling all have parts to play. However, changes need to be made to the psyche of our culture. Despite the welcomed changes to legislation which protect LGB people, there are still many facets of society that are heterosexist and homophobic.
The mental health needs of young same-sex attracted men must be addressed by everyone who works with young people. The needs of this population must be included in the strategic planning of organisations that work with young people, accompanied by inclusive policies which address the needs of LGB people and staff training. It is only when all sectors begin to be inclusive of LGB people that this acceptance and can filter through to the rest of society.
Recommendations
1. Central Government funded specific training and resources on different sexual orientations should be provided to all professionals working with young people. This should not only include those in the field of mental health, but also teachers, youth workers and health and social services professionals.
2. Current Government Strategies and Action Plans such as the Mental Health Strategy, the Suicide Prevention Strategy and upcoming strategies such as the Sexual Orientation Strategy should take on board the findings of this report.
3. The Department of Education needs to make schools aware that there are non-heterosexual students in their schools and ensure that non-heterosexual students are provided with the relevant protection and education.
Schools should be designated fully for the purposes of Section 75 of the Northern Ireland Act1998.
4. Government funding for specific LGB youth groups in Northern Ireland or an LGB element of an existing youth group, preferably for areas outside Belfast or Derry/Londonderry.
5. Additionally Northern Ireland specific resources for young people on sexual orientation need to be developed. These should be disseminated widely in schools and the youth service.
6. Government support for personal development courses for gay and bisexual men.
7. Resources should be made available by the Government and other funding bodies for parents and families of same-sex attracted men. Materials should be widely available for example, in GP surgeries, social work offices and public libraries.
8. Government should provide complete financial backing to the Equality Commission for Northern Ireland to ensure the full implementation of the new anti-discrimination legislation covering Goods, Facilities and Services for people of differing sexual orientation. This legislation is due to be introduced later this year. (Note: This report was published 2006)
9. Further research into this topic should be supported by Government and/or other funding bodies in the next five years.
10. Specific research should be conducted by the Department for Social Development and/or Northern Ireland Housing Executive and/or Housing Associations into the needs of LGB people who access housing.
(1) McNamee, H. (2006) Out on Your Own – An Examination of the Mental Health of Young Same-Sex Attracted Men, The Rainbow Project
Mirjam Bader
The Rural Community Network
The Rural Community Network [RCN] is a regional voluntary organisation established by community groups from rural areas in 1991 to articulate the voice of rural communities on issues relating to poverty, disadvantage and equality. RCN is part of the Rural Community Development Networking Infrastructure, a Northern Ireland wide networking infrastructure that includes RCN and twelve sub-regional Rural Support Networks [RSNs] with a collective membership of more than 600 members. A number of the Rural Support Networks such as Cookstown and Western Shores Network, North Antrim Community Network, Oakleaf, South Antrim Rural Network, Strabane and District Community Network and East Down Network have been involved in mental health promotion and suicide awareness work.
North Antrim Community Network is currently with the Northern Health and Social Services Board and the Northern Investing for Health Partnership in delivering a small grants programme “Promoting Mental Health and Suicide Prevention Programme”.
The RSNs and RCN welcome the opportunity to respond to the Inquiry into the Prevention of Suicide and Self Harm. Our response highlights the specific rural issues with regards to mental health and suicide and we would fully support the submission of the Niamh Louise Foundation in this regard. We would also refer the Committee to Fact Sheet by Mind with regards their Fact Sheet on Rural Issues. [http://www.mind.org.uk/Information/Factsheets/Rural+issues+in+mental+health.htm] which this submission has drawn upon.
Poverty and disadvantage in rural communities
Poverty and disadvantage are realities for many across rural communities in Northern Ireland. However, those living in poverty are less geographically concentrated as they might be in more urban areas. Rural dwellers living on low incomes may often be scattered across less populated areas, often living next to more affluent members of the community. This means that their poverty is less visible to policy makers and those delivering services, who use ‘indicators of deprivation’ that are more suited to the higher concentrations of poverty found in towns and cities.
Rural dwellers face other difficulties such as accessing and the availability of quality services, affordable housing, poor public transport and the impact of significant social and economic changes within rural areas with key points of reference disappearing such as farming, rural schools, and post offices. These issues have a significant impact on the health of individuals and families with the particular mental health issues of farmers and farm families increasingly well documented through organisations such as Rural Support in the wake of BSE and Foot and Mouth disease.
Stigma around mental health and suicide
The Niamh Louise Foundation would argue that there is often a higher degree of stigma in many rural communities with regards to mental health problems. It can be harder to acknowledge issues personally, to speak out, and to seek support. In many rural areas, there would be strong culture of self-reliance and keeping problems within the family. There is a greater concern in remaining anonymous and keeping issues confidential and due to smaller population sizes and more stable communities greater pressures in doing so.
The consequences of stigma can have a serious effect on a person’s willingness to access mental health services or confide in potentially supportive individuals and agencies. Consequently the approaches support agencies develop in rural areas need to take these issues into account.
Provision of and access to mental health care and support services
Population density and consequently economies of scale mean that historically most services are either located or have their headquarters in urban areas. Extra resources are often required to extend services into rural areas.
Where services might exist, they are likely to be at some distance from a patient’s home requiring easy access to a car due to poor public transport. This has time and cost implications and adds another barrier in making that choice to accessing help. Those who might be most affected by poor transport are often those most in need: older people, young people, women (often young mothers) living in one-car households, people living on low incomes and those with physical or mental health problems.
Given the stigma attached to suicide/self harm in rural areas it is imperative that when a GP is approached in the first instance he is able to refer the patient quickly and more importantly secure the necessary specialised help. There may be a time lag if it has taken time for the person to pluck up the courage to seek help. Unfortunately there are cases where help has not been available in time to prevent suicide.
It is also worth mentioning the ASSIST suicide prevention training which is an invaluable resource and is available in most towns.
Accessing information
“Access to reliable, high quality information has a profound effect on mental health and wellbeing. It enables us, as individuals and as social groups, to make the most of our lives, fully aware of our rights and the resources available to us. This applies to local and national community information in general, as well as to information specifically about health.” [Mind Fact Sheet - www.mind.org.uk/Information/Factsheets]
Distributing and accessing information in rural areas poses different challenges than in urban areas with single information points often not the answer. Key information points such as GP surgeries, libraries, post offices, local shops are more dispersed or disappearing. Information is often through word of mouth and existing networks and relationships; this creates extra difficulties for those newly arrived or don’t belong to networks such as new citizens, minority ethnic communities. There is also the added difficulty for those who don’t have English as their first language who again are at a higher degree of isolation in rural communities.
High risk groups in rural areas
As the Mind Fact Sheet states, while anyone can develop a mental health problem, certain groups in rural communities are particularly vulnerable.
Farmers and farm workers
Restructuring of farming, crises such as BSE and Foot and Mouth have placed immense strain on farmers and farm families struggling to make ends meet. Farmers and farm workers have been identified as a high risk group for stress, depression and suicide and the work of Rural Support provides important information and support.
Black and minority ethnic (BME) populations
Key issues for black and minority ethnic people living in rural areas, as identified by many organisations including ANIMATE, STEP and in the Equality Impact Assessment Consultation Report by the Department of Agricullture and Rural Development:
- Invisibility, loneliness and isolation;
- Difficulties in accessing interpreters;
- Limited social opportunities;
- Transport;
- Lack of English classes;
- Less opportunities for training in areas of employment;
- Prejudice and discrimination.
Children and young people
Rural areas are becoming older with young people (those aged between 16 to 29) a declining population. Work by Youth Action in rural areas has highlighted the specific challenges facing young people such as a more limited range of education, training and employment opportunities, limited access to recreational, advice and counselling services and a shortage of affordable housing meaning that young people are staying longer with their families placing increased strain on family relationships.
Young males in rural areas are at particular risk. There is a lack of activities to channel their energies that can often lead to frustration. In a small community any difficulty faced by a young person may be well known leading to embarassement and an already vulnerable person may just be tipped over the edge.
Women with children
Women with children are often very isolated with particular issues for women who have moved into an area, have limited social networks and whose partner might be away working with the car. Poor public transport, lack of services, limited access to childcare and difficult access to information present challenges this group with greater risk of mental health problems.
Again, problems such as financial concerns, domestic violence, other stresses might be kept hidden and stay within the family. Farmers’ wives have the additional strain of providing care and support to husbands who work in a highly stressful occupation.
Lesbian, Gay, Bisexual and Transgender Populations
Around 10% of the population is lesbian, gay, bisexual and transgender (LGBT). They make up minorities in many parts of Northern Ireland They make up even smaller minorities in the countryside. Negative attitudes towards LGBT people, reported across rural Northern Ireland, are not tackled effectively, mainly because the groups affected are so small that they cannot easily build strong local support networks and have poor access to peer support.
Often, those who plan services do not believe that members of LGBT populations live in rural areas. This is not the case. As these populations tend to be small and isolated, individuals can suffer doubly from being visible within their local community but invisible to those who plan services. For the most part, LGBT people don’t come forward asking for support and the need therefore isn’t apparent.
Older people
Rural areas are becoming older. For example, in 10 years time 1 in 4 people in Fermanagh will be over 60. The Northern Ireland average is 1 in 5. Essential services for older people continue to be under threat or downgraded such as post-offices and public transport.
Due to changing family structures and changing life-styles, older people in rural areas are less likely than their urban counterparts to have relatives nearby to support them and are more likely to live alone. Housing and employment pressures mean that children have to move away, often at some distance from their parents. These factors can lead to feelings of isolation. Studies have also shown that older people make up the largest group of people living in poverty in rural areas which, combined with the higher cost of living in the countryside, can cause considerable stress.
Travellers
Members of the Travelling community take place within a distinct set of problems. These include:
- The higher birth rate as well as higher death rates among Travellers as compared with the Settled population. Life expectancy of Travellers is around 20% lower than that of the general population
- 10% of the population is over 40 years of age and 1% is over 65;
- High infant mortality and high death rates among children due to disease, poor diet, poor hygiene and lack of access to health services. There is a mortality rate for Traveller children up to the age of 10 ten times that for the population as a whole
- High levels of disability among children due to genetic diseases and little access to or use of primary health care during pregnancy;
Travellers face huge barriers in their access to health and related services, such as social care and education. This is largely because they are subject to frequent evictions from unauthorised sites. As temporary residents in a health authority’s catchment area and lacking a fixed abode, it can be difficult for Travellers to register with a GP. This can also make it difficult for them to receive long-term treatment provided by a health authority.
Migrant workers
Many Northern Ireland farmers depend on migrant workers to perform a range of seasonal tasks and increasingly many rural businesses. With the expansion of the European Union, the number of eastern European migrant workers has increased sharply, many living and working in rural areas. Some migrant workers are in the UK illegally and this group is at particular risk of exploitation and abuse. Some are from further afield such as South Korean workers working in fishing fleets.
The mental health of migrant workers, and especially illegal migrant workers, presents particular challenges to service providers. Workers may speak little or no English.They may find mental health services difficult to understand and even threatening, particularly if they have received hostile treatment from settled local communities. If employed in seasonal work, a migrant worker may not be resident in a NHS Trust catchment area long enough to receive the treatment they need.
Ways of working in rural areas
There is no single rural area or type with different areas facing different planning, economic and social issues. However, it is also possible to identify shared issues around pressures of changes in agriculture, declining services and difficulties around access, changes in population and a culture of self-reliance and keeping problems within the family.
This context means that there might need to be different ways of working with mental health issues and suicide prevention appropriate to different rural community needs. Stigma around mental health and suicide is sometimes very high requiring a light and gentle tread, with interventions based on request and word of mouth rather than high profile publicity.
On behalf of the Rural Community Development Networking Infrastructure
Michael Hughes [Rural Community Network]
COSTA
Cookstown and Western Shores Network
East Down Network
North Antrim Community Network
Omagh Forum for Rural Associations
ROMAL
Strabane and District Community Network
Southern Health and Social Care Trust
Protect Life Strategy
1. Introduction
This paper reflects the views of the Southern Health and Social Care Trust to the current development and implementation of the Protect Life Suicide Prevention Strategy. The paper firstly explores a number of relevant issues pertaining to the outworking of the strategy and then provides a brief overview of what is currently underway within the Southern Trust Area to realise the Goals, Objectives and Key Actions of the Strategy.
2. Views on the Current and Future Development of the Strategy
The Trust has welcomed and embraced the Protect Life Strategy on a number of grounds. It has provided a significant and much needed focus to the issue of suicide within Northern Ireland. It has created an opportunity to openly discuss and address an issue which hitherto was largely unspoken and therefore unaddressed. The Strategy has given legitimacy to what is a highly sensitive issue and one in which many of those who have suffered as a result of a suicide of a close friend or family member felt largely unsupported. It has generated a momentum across community, statutory and voluntary partners to work together to find more appropriate ways of responding to the needs experienced by individuals, families and communities.
The focus of the strategy on the three key dimensions of prevention, intervention and postvention is welcomed. This has ensured a balance between the need to address the issue of suicide or self harm if and when it occurs with the needs to maximise the opportunities that exist to prevent the incidence of suicide and self harm through targeted interventions that seek to build resilience, self help and support. The maintenance of this holistic approach is vital in any future development of the strategy.
The locating of the strategy within the wider context of Mental Health Promotion is also welcomed as it maintains a balance both in terms of focus and priority but also recognises that much of what is undertaken in the context of good practice in Mental Health Promotion contributes to the prevention of suicide and self harm.
From the outset the Protect Life Strategy has sought to embrace the needs and priorities of individuals, families and communities. The Trust has welcomed this approach and sought to maintain this focus in the development of its work across the Southern area and in the development of its Action Plan (as detailed below). Involving those who have been affected by suicide and self harm is a vital element of effective service design, development and delivery.
The rollout of the Strategy through the N.I. Investing for Health Partnership infrastructure has sought to ensure that its implementation is founded on effective partnership working across the sectors. This has allowed the strategy to benefit from the expertise that multi-sectoral and multidisciplinary structures bring to addressing local need and as a result has ensured that there has been an effective community, statutory and voluntary partnership approach to the outworking of the strategy.
Given the multi-sectoral nature of the strategy at regional, area and local levels, coordination is vital. The infrastructure that has been established through the Regional SSIB group, the Board Implementation Group and the local Trust Implementation Group has sought to ensure coordination and collaborative working both across and between levels. Representation on these groups by service providers, commissioners, individuals and communities is critical in ensuring firstly that responses are targeted at addressing the needs of those who have experienced first hand the effects of suicide and self harm and secondly that these responses are multifaceted in nature thus ensuring a holistic response to need.
The Trust has identified the need to ensure effective coordination mechanisms are established across the area as a means of developing comprehensive and collaborative action by partners. The value of working together across the community, statutory and voluntary sectors is essential if we are to ensure the development of a seamless model of service provision that is both effective and efficient in responding to the needs of individuals, families and communities. Any future development of the strategy needs to give sufficient recognition to this dimension.
The pilot schemes that have been developed under the current outworking of the strategy need to be evaluated to assess their roll-out position Northern Ireland wide. There is a need to ensure that services such as the “Helpline” are more widely targeted at addressing the needs of all communities across the province and not just those within one specific geographical area. In addition it is essential that these services establish more effective links with local service providers thus improving their ability to signpost those in need to appropriate, locally based services.
The outcome of the General Practitioner Training programme provided through the Health Promotion Agency is as yet unclear. There is a need to assess the relevance, appropriateness and therefore uptake of the current training provision and to explore more fully if it is indeed addressing the real needs of General Practitioners. It is vital that General Practitioners are made more aware of what services are currently available in their respective communities and as a result encouraged to make referrals to these services for more sustained and longer term support.
In any future strategy development it is essential to embrace the fact that other members of the Primary Care Team as well as community, statutory and voluntary partners often constitute part of the first line response in a wider multi-sectoral health service model. It is therefore essential not just to focus on the training needs of one specific discipline i.e. the General Practitioner, but to fully embrace a wider model of primary care provision and as a result address the needs of all those who are engaged in the provision of “front line” services.
The current regional media campaign has focused on a Mental Health Promotion message rather than directly addressing the issue of suicide. Whilst it is acknowledged that there is a need to avoid a sensationalist and “scare mongering” approach there is a need to balance this with an ability to begin a direct debate and dialogue about suicide within our wider community.
In establishing local service provision the need to reduce competitiveness and single organisation service provision has been evident. Both Board and Trust have sought to ensure a culture of collaboration and partnership working. This is essential not just in ensuring effective, efficient and value for money based approaches but more importantly in creating a model of service provision in which the needs of the individual are paramount and where partners refer across the boundaries of organisations to ensure that the most appropriate response to individual need is achieved.
As consideration is given to the ongoing development of the Strategy it is essential to consider the development of agreed quality standards in relation to the commissioning and resourcing of future services such as a first line response, family support and counselling provision. These standards need to be accepted across the region and applied across all sectors.
Addressing suicide and self harm cannot by its very nature be regarded as a short term “quick fix” approach. It is essential to recognise the need for sustained resource and support over the medium to long term. Much remains to be learned as to the nature and extent of services required by individuals, families and communities in addressing this public health issue. In addition current training programmes are as yet not fully evidence-based and a research focus needs to be developed in this regard.
3. Current Progress on Implementation within the Southern Trust Area
The Southern Health & Social Care Trust is actively engaged in implementing the Protect Life Strategy across the Southern Area. This process has involved bringing together a broad range of community, statutory and voluntary partners, with the Trust providing overall coordination and support. It has established a Protect Life Implementation Group to oversee the outworking of the area action plan, chaired by the Director of Mental Health Services for the Trust. The group currently has representation from key Trust staff, Police Service Northern Ireland, Southern Education & Library Board, Council representatives, Southern Health & Social Services Board, Northern Ireland Housing Executive and a range of Community and Voluntary sector partners.
In line with the Goals, Objectives and Actions in the Regional Strategy the Trust has led the development of an Action Plan which targets a coordinated multi-sectoral range of actions addressing prevention, intervention and postvention approaches. Within this context the need has been identified to establish a lead worker to facilitate this area of work across the area and the Trust is currently working with the SHSSB to resource this post. The Trust is also a member of the Southern Area Investing for Health Partnership and Protect Life Implementation Group and is committed to ensuring that there is synergy across respective action plans and to delivering its obligations with regard to suicide and self harm. Key areas of activity across the Southern Trust area to date have included:
- Engaging with individuals, families and communities to ascertain need and develop appropriate actions;
- Providing an initial crisis response in the immediate aftermath of local deaths by suicide;
- Developing locally sensitive cross sectoral actions including parental support, youth provision, resource development , information sharing and fast-tracking to Children’s and Mental Health Services;
- Increasing access to information and education;
- Establishing a comprehensive interagency training strategy and delivering training for key workers and stakeholder organisations;
- Increasing the profile and priority of suicide and self-harm;
- Establishing Community Worker posts and locality based Resource Centres, managed by Voluntary partners;
- Commissioning additional counselling services from the voluntary sector to meet expressed and identified need;
- Establishing relationships with both PIPS groups and the Niamh Louise Foundation in the locality to enable effective collaborative working;
- Liaising with the private sector who are interested in coordinating a community response to suicide and self harm;
- Developing a coordinated and consensus based approach.
The ongoing development of the action plan will ensure that sustainable mechanisms are in place to further these agendas and target appropriate actions and responses to address the needs of local communities.
Department of Culture, Arts and Leisure
Youth Action Northern Ireland
Youth Action Northern Ireland is a regional voluntary youth work organisation with bases in Armagh, Ballygawley, Belfast, Newry and the North West. We engage with young people to support them as active and equal citizens whose voices are heard, respected and valued.
We focus on working with urban and rural young people aged between 10 to 25 years. We target social need, working in partnership with those young people who are most deprived of and excluded from resources.
We base our strategy and practice upon research and evaluation into the needs and issues most critical to young people.
We disseminate our research findings and practice models through training and publications.
The agency welcomes the opportunity to respond to the strategy. With the ever increasing pressures on young people, it is vital that they are provided with the resources and services to enable them to deal with the issues that they experience in their lives.
More opportunities need to be created to discuss with stakeholders from across all the sectors engaging with young people. YouthAction Northern Ireland attended a number of different initial consultation initiatives at the start of the process and then completed a response to the consultation. There was no follow up after this point to engage with us as an agency and how the strategy was being implemented on the ground. Opportunities to do this would have been useful as it would help us see how the work that we are doing can link to and complement the Protect Life strategy. Involvement of all stakeholders is key to the success of the strategy and more needs to be done to share the learning and experiences from other projects to ensure that we are all helping with developing preventive strategies for young people at risk of suicide and self harm.
Considering that the Protect Life Strategy highlights young people as a key target group, there is a need for more training and support for those working with young people. Earlier interventions with young people through the Youth Sector will assist with helping to increasing awareness, developing stress management skills, preventive techniques and strategies to help young people make positive choices about their lives.
Those engaging with young people need to have the skills; knowledge and develop the confidence to enable them to do work more effectively on the specific issues that are having a detrimental impact on their lives. More resources need to be created to enable this to take place and shared across the education, health and community sectors working with young people on the ground.
The “It’s always in the back of your mind” (YouthAction NI 2006) research indicates that mental health and positive emotional well being are significant factors impacting upon young people’s development but that there is often a lack of understanding around mental health (as opposed to mental illness) and not focussing on the positive elements of it.
- “Mental health is only discussed or addressed when something goes wrong- this should be talked about in a positive way.” (practitioner)
- “In Northern Ireland we are not positive to one another…our sense of humour is negative…and we have some emotional literacy issues where we cant say thanks to one another…this is magnified for young men…as workers we need to understand young men’s behaviour and the reason behind it, rather than blaming them.” (practitioner)
- “I often think about how others who seem completely normal and carefree may have problems deep down.” (young person)
Strategies need to be developed to enable those engaging with young people to address these issues and feel that they are supported to do so
Young Men
The health consultation carried out by YouthAction NI and Armagh Dungannon HAZ, Some Men Do; Some Men Don’t (2004) which took place with urban and rural young men in Armagh and Tyrone documented how young men viewed issues and services around their health. While young men had an awareness of what health services such as doctors, dentists and chemists provided, they had limited knowledge of other services. On services such as family planning, drug and alcohol advisors, counselors etc. young men had this to say:
“I don’t have a clue what it is”; “I don’t know where to go”; “No need to use a counselor, I don’t have any problems”
Other things the young men that participated on the project said was:
“You don’t really think about emotional health and all that in the same way as you think about general health – it’s different”; “What causes depression – what kicks it off?”; “I wouldn’t go to a doctor about my sexual health – I’d be embarrassed”
Young men who participated in the ‘Check these Out - Young Men’s Health Events ‘ (2006) discussed how getting access to information relevant to their health was important:
“There’s nowhere to get information (about your health and well being) but at least this helped”
“I have never accessed services but would like to”
“I got loads of information on relevant issues concerning looking after your Health”
“I got loads of information from very helpful people”
“There was lots of interaction with the young men. Things were active, they could ask questions about issues they didn’t know about” (Practitioner)
Young men aged 15-18 years are extremely vulnerable and it is in the period that they may begin to experience the stress, bullying, confusion, pressure etc which impacts on their later decision to attempt suicide or self harm. Preventative models of practice need to be developed with young men in local communities to help young men deal with the pressure that they are under in their everyday lives and that there is somewhere to turn if they feel down or depressed.
YouthAction Northern Ireland has engaged young men on a number of local community based initiatives and they have said the following:
“This group has been really good for me. I usually avoid talking about these issues but listening to others has made me realise that other people are worse off than I am”
“You need to talk about the things that bother you and express yourself sometimes. It can relieve your anger and stop you exploding”
“There aren’t many opportunities for men to talk about their problems but there should be”
“I learnt about ways of calming myself down or staying calm and thought about feelings you get after you get angry or crack up”
“I was never any good at school, so I didn’t really learn. You feel wick when everything goes over your head. But if you tell them you don’t understand, they just keep going on with the subjects and you fall further behind. It makes you feel like shit like, cause schools supposed to be a place where you learn.”
“I have learnt more during this project than I ever did at school. We got the chance to talk about stuff and look at things that we are interested in.”
“I think that we are seen as wasters. It’s hard trying to keep up with something if you don’t understand. I’d rather be doing something that would help me with getting a job.”
“School causes stress, extra pressure at exam time sometimes causes people to get medication.”
“I’d rather take or give a thump rather than have to answer a question.”
Young Women
YouthAction NI carried out research into the needs and issues facing young women aged 18-25 years, Still Waiting (2006) Many stressful events were highly individualised (e.g. the birth of a child, bereavement, ‘coming out’) while others related to education and exam pressure, the general stress of everyday life and/or the interaction of a number of factors. There were also clear examples of young women lacking self-esteem, putting themselves down, blaming themselves for things which were outside their control and putting great pressures on themselves. Failure to get good grades in school, the job they wanted etc. was often individualised with little recognition of the unequal structures in society or a lack of good quality support or advice.
“I’d be more somebody who would bottle it up more than talkin’ about it” (Young woman aged 20)
“I think men put it to the back of their heads and forget about it but women would be more ‘I wanna talk about this, I wanna talk about this’” (Young woman aged 18)
“I was looking after me, him [her dad], my wee brother, trying to do all my school work, cooking, cleaning, you name it I was doing it. See by the time it came to sit down and do my homework, I was shattered …” (Young woman aged 17)
There is potential to link with the Youth Sector in developing specific projects with young women and young men in addressing issues such as self esteem, violence, relationships, bullying, suicide, gender roles, sexual orientation etc. and how these link with mental health. It needs to be highlighted the importance for different strategies and approaches be used for engaging with young men and young women due to there different and varied issues.
Again the Emotional and Mental Health Needs of Young People Research Report specifies programmes focusing on “social needs, gender and other relevant issues.” It is vital that male practitioners in particular are supported to be positive male mentors to young men in helping them to overcome the restrictions often imposed by masculinity in suppressing and internalising feelings and emotions.
Preventative strategies need to be developed for those that workers such as Detached Youth Workers and Street Youth workers – support mechanisms and strategies devised for those that work with young people at times when they are most at risk of suicide or self harm
Opportunities need to be created for young people to explore issues that affect their future such as life skills, gender expectations and preparation for the working and adult life.
Links to other strategies
There should be recognition of other strategies and alliances such as A Gender Equality Strategy for Northern Ireland 2006 – 2016; The Youth Work Strategy for N.I.; The Equality Strategy; Rural Strategy 2007 - 2013 and RPA implementation etc.
Within RPA there is the opportunity to inform community planners of the need for pro-active interventions in working with young people within the new 7 council areas.
Consideration to LGBT specific issues through the Shout initiative and LGBT consortium.
Joined up practice and practical partnerships at local level need to be developed and implemented and good practice shared across the sectors engaging with young people.
Southern Health and Social Services Board
The Southern Health and Social Services Board welcomes the Health, Social Services and Public Safety Statutory Committee inquiry into suicide and self harm prevention. The Board’s response is provided below and follows the headings set out within the Inquiry’s Terms of Reference:
The Appropriateness of DHSSPS strategy - ‘Protect Life: A Shared Vision’
The Board is satisfied, in general, with the content and recommendations outlined within the regional Protect Life strategy.
The strategy is based upon a robust review of the worldwide literature in this field. In this respect, the Committee will appreciate the complexity of the overall issue. The Committee will undoubtedly appreciate that there are many social pressures, especially for young people, that create stress and each person reacts differently to those pressures. There are also the wider societal issues of decreasing family support structures, general social pressures, the impact of alcohol and drugs and general deprivation factors. This emphasises the need for a multi-agency/multi-sectoral response to self harm and suicide, i.e. the impact of Health and
Social Services working alone will be limited. The Board is working with a range of agencies locally and it is noted that the Committee is working on a cross government basis.
While the gravity of the current situation regarding suicide/self harm is clearly apparent, the underlying evidence base to guide the response of services and agencies is uncertain. It should be noted that the impact of potential initiatives is often not significant. As outlined within the review of literature published within the strategy document, only a limited number of areas/initiatives have been shown to be firmly evidence based. Furthermore, even when an intervention has been shown to be evidence based, the actual impact of such actions/initiatives is sometimes unclear and may only be limited. This emphases the need to ensure that regional and local Action Plans are based upon the available evidence in terms of what is likely to work in practice.
With regard to the wider strategy document and associated recommendations, the dual ‘Population’ and ‘Targeted’ focus of the strategy is supported including the specific actions area highlighted across the report. The Board strongly supports the tiered approach advocated, with a regional strategy and specific targets, to then be taken forward at Board level through partnership approaches such as the Southern Investing for Health Partnership (SIHP) which locally has facilitated a particular focus upon community based actions and interventions.
Stakeholder Involvement
The Committee will be aware that at an overall regional level a wide range of sectors, agencies and community groups/representatives have been involved in both the development of the strategy and its subsequent implementation.
From the publication of the draft strategy, the Southern area has been fully committed and indeed exemplary in engaging stakeholders in the development of a Southern area response to this issue.
Initially, 10 Community Consultation events were held (2006) across the Southern area to highlight the Protect Life Strategy, current work to address it and most importantly to seek local views in how best to plan and co-ordinate a focused response to it. Three further community workshops were held (2007) to draw together these thoughts into an action plan document and a final event agreed a Southern Area Action Plan for 2007 – 08.
Details of all these consultation events, workshops and a copy of the final Southern Area Protect Life Action Plan can be downloaded at: http://www.southernifh.com/suicide.cfm
To ensure that this level of Community and Voluntary sector involvement and engagement continues, the Southern Area Protect Life Steering Group has been established, which has representatives from all key stakeholders (details of representatives on this Group, Role and Remit and minutes of their meetings can be found at the website referenced above).
In addition, it was felt vital that local communities had an opportunity to share and discuss issues related to the Protect Life Strategy and so a ‘Community Forum’ has been established and is beginning the process of identifying a meaningful role and remit for it.
Services to Promote Good Mental Health
Regional priorities for mental health promotion are set out in the DHSSPS (2003) Promoting Mental Health Strategy and Action Plan 2002 – 2008, which aims to improve mental and emotional wellbeing and to prevent or reduce the impact of mental illness. The strategy combines an approach encompassing the need to address life circumstances and developing life skills and is based on three principles i.e. holistic approach, empowerment and respect for personal dignity.
The Southern Board has been responsible for overseeing the implementation of this strategy locally and has established a robust infrastructure encompassing 60 stakeholders from the voluntary, community, private and public sectors with particular emphasis on the involvement of service users. In addition, a multi-agency steering group, a Mental Health Forum for older people and a network for BME workers has been established to promote good communication.
An annual Action Plan is developed through consultation events where stakeholders have identified key themes to be address as a priority. They include policy development, raising awareness/reducing discrimination, improving knowledge and skills and preventing suicide.
With regard to implementation of the Strategy, it should be noted that only limited resources were made available regionally. Locally, it has only been possible to establish a relatively limited practitioner resource to support the ‘Promoting Mental Health Strategy’ during its timescale: two specialist Mental Health Promotion officer posts have been established to co-ordinate activities across the Southern area. Successful initiatives undertaken to date include the ‘Open Your Mind’ public speaking competition for schools, the development of ‘Bounce’ a resilience and self esteem programme for young people, a Bibliotherapy Project involving General Practitioners and Librarians, as well as training and development programmes for vulnerable groups.
Further Action
As outlined within the ‘Bamford’ regional review of Mental Health and Learning Disability, the Committee will be aware of the need to strengthen Mental Health services within Northern Ireland. For example, it is well established that the level of community mental health infrastructure is considerably less here than that available elsewhere, such as within England and Wales.
A more robust/comprehensive mental health service working in tandem with, for example, primary care, Accident and Emergency services and the voluntary/community sectors would undoubtedly provide a stronger foundation to provide services with capacity to intervene in crisis situations on a 24/7 basis. The need for robust mental health services was highlighted within the Protect Life strategy report and I understand that DHSSPS will be providing its response to the Bamford Review in the near future. The Committee will no doubt be aware of the substantial investment required to develop mental health services in general across Northern Ireland.
I trust the above will be of assistance and look forward to reading the report that I anticipate will follow the Committees Inquiry.
Sean McKeever
Acting Chief Executive
R.A.Y.S Crisis Centre and the greater Shankill Bereaved families
The greater Shankill Bereaved families meet @ RAYS Crisis Centre on a weekly basis to provide support to each other, and to receive advice and practical support from the staff at the centre.
The Centre was set up in October 2006 in response to the increasing numbers of suicides across the area. The RAYS project was funded from the Renewing Communities Fund until March 2008 to date recurrent funding has been identified. The aim of the centre was to provide support to bereaved families who had felt that until this particular point in time the wider community had little or nothing offer to people who where suffering as a result of bereavement through suicide. The concept was to provide support through good post-vention services, support people in crisis and raise awareness through prevantative measures which would impact on reducing the numbers of suicides and, act as a catylist to reduce the stigma associated with suicide. To give practical support and services to carers often left alone to cope in difficult, demanding and exhausting situations.
The families involved from the outset had originally lobbied and campaigned at local and government levels with friends from North and West belfast to strengthen their voice and add weight to their concerns at the lack of services and resources to adequately address the issue of suicide and self harm. These families believe that even though suicide is a complex issue, many of their loved ones deaths could have been prevented had adequate services been available. It is this belief that drives the families on into each new day in the hope that their experiences and subject knowledge may just prevent somone else suffering the anguish and pain they carry.
The greater Shankill Bereaved Families have felt that funding provision and localised campaigns have enabled the local community to find out more about suicide this hopfully is the beginning of a concept that this community will embrace and, begin to reduce stigma. Through the consultation process at the outset of the strategy and resulting from the taskforce report the bereaved families generally felt that they had been listened too, and that their oponions experiences and concerns had been taken on board. However the families felt that a significant number of issues had been ommitted from the draft version of the strategy and that the final document was merely to appease people – and the final draft had selectively been cut in half. The Families had been informed but feel they have had no real consultation: as their ideas and inputs where not included in forming the final outcomesof the strategy, no real user involvement about what shape services should look like. e.g. What was this all about?
Families had expressed concerns at the lack of sensitivy to support families dealing with the death from clergy, PSNI the Coroner’s Office and Registrars. They feel that little has changed, recently bereaved families relay the same stories.
It is unclear as to the budget funding stream for suicide, self harm and mental health. £1.9m in 2006 was inadequate. The current funding of £3m has highlighted issues around suicide and self harm at a localised level. While their may be a strategy to 2011 it has not been transferable beyond March 2008 with effectively no strategy or vision for funding provision of existing services delivering at a local level post March 08.
There has been an improvement in community support but no real tangible difference in statutory services. Clients and community users feel that although the community is more aware of the issue of suicide and self harm, but when trying to access statutory services there has been no change – the same difficulties still apply in trying to access help. RAYS staff still have difficulties accessing statutory support services which are timely and appropriate to people in crisis. The centre deals with an average of 2.5 people in Crisis a week. Up to 18 bereaved family members a week and up to 20 carers a week. The staff experience a lack of co-ordinated and adequately resources services to tackle the level of suicide, and often there are conflicting stories about how services may be accessed. A clear response pathway should be actioned informing the community about what services are available and how to access them.
The Health Promotion Agency media campaigns have been oriented towards mental health instead of suicide and self harm – money has been taken from the Suicide and Self Harm budget and used for advertising mental health only. This has lead to an ineffective advertising campaign. The advertising campaign needs to have ‘impact’ to begin to address the area of suicide and self harm. Services for self harm specifically have become even more scant than the crisis services. It seems that self harm has not even been acknowledged as an issue.
Families genuinely believed that the strategy would end their lobbying and campaigning however this is not so, and they feel the need to “keep the pressure on” . Issues have shifted from a lack of beds to a lack of staff to oversee the patients using the new beds. New adolescent unit beds have been put back until 2009. Ongoing inadequate management of people presenting in crisis e.g. clients are put in with other mixed mental health adults before/without being diagnosed as having mental health issues themselves. This introduces new risk factors to the client. It also stereotypes ALL those in crisis as having mental health issues. We are told that not everyone in crisis needs to be hospitalised and indeed we all agree many people would progress much better a home. However sending people home without any suppports and expecting families to bear the burden of suicide watch is adding undue pressure to vulnerable families. The statutory agencies have admonished their duty of care and neglected the individuals right to services for health and wellbeing.
The GP education and training pogramme to increase detection of depression seems to be inadequate when it comes to GPs. Many GPs have been resistant to the ASIST training. The staff team have experienced that training and support services for carers goes widely unacknowledged.
Follow-up appointments for patients who have been hospitalised are still not routinely processed and the staff spend quite a high proportion of time tracking patient appointments. Patients are being discharged with inadequate support services in place. Some have gone on to complete suicide.
The families believe that many interventions which have implemented have not been effectively evaluated to determine their effectiveness or the need to make changes.
This report has been compiled by Roberta Coates Co-ordinator RAYS Crisis Centre in consultation with the Greater Shankill Beraved Families
Please feel free to consult us at
RAYS Crisis Centre 16 Woodvale Road BT 13 3BS 02890 319333
www.rays.org.uk for further information about our services
The Committee for Social Development
The Committee for Social Development welcomes the Committee for Health, Social Services and Public Safety’s Inquiry into the prevention of suicide and self-harm and is grateful for the opportunity to respond. It is clear that there is no single solution to the prevention of suicide and self-harm therefore the Committee would wish to comment on a range of issues/interventions, some of which fall outside the remit of the Department for Social Development.
Risk factors
1. Research has told us that there are many suicide risk factors including depression, alcohol and drug misuse, personality disorder, hopelessness, low self-esteem, bereavement, break-up of a relationship and social isolation. The Committee would wish to see all identified risk factors addressed as part of a strategic approach to promoting mental health and well-being, and in particular, the full implementation of the Bamford recommendations.
Poverty and social exclusion and other strategies
2. Historically, research has shown that in deprived areas the suicide rate is much higher than in non-deprived areas and when focusing solely on economic deprivation, the suicide rate gap increases even further in economically deprived areas compared to the rate in non-economically deprived areas.
3. Lifetime Opportunities, the Government’s strategy to tackle poverty and social exclusion, would appear to be the best vehicle to address deprivation. However it is imperative that there are strong links between all relevant strategies, for example the Department for Social Development’s strategies that deal with housing and homelessness, neighbourhood renewal, urban regeneration, fuel poverty, benefit uptake, child support, and funding for the community and voluntary sector.
Training
4. The Committee would wish to see the development of a training strategy linked to the prevention strategy that has the commitment of all the relevant statutory and voluntary bodies. The Committee would envisage a strategy that focuses on attitudes and beliefs as well as information and procedures.
5. Training should be provided to all who come into contact with those at risk of suicide and self-harm – from professionals to front of house staff. Front of house staff should include those who work in Social Security offices; the Child Support Agency; Housing Executive; Tax offices etc.
6. Training should be tailored to meet the needs of different levels of staff i.e. matched to the level of involvement of the staff concerned. In addition, the Committee believes that mandatory risk assessment training for health professionals should be introduced at the earliest opportunity.
Inter-agency and multi-agency working
7. Good inter-agency and multi-agency working is essential to deal effectively with those who present with suicidal or self-harm tendencies. This might mean the co-ordination or, in some instances, the integration of services.
Psychiatric services and psychotherapeutic treatments
8. The Committee is predominantly concerned about lack of access to psychiatric services including psychotherapeutic treatments and the unacceptably long waiting lists for referral to psychiatrists - in particular waiting lists for child and adolescent psychiatrists. Real efforts need to be made to address the inadequate provision of psychiatric services including the lack of psychiatric beds throughout Northern Ireland.
Voluntary and community sector
9. In light of the lack of psychotherapeutic treatments being offered by psychiatrists, the Committee would wish to see the enhancement of the role played by the voluntary and community sector matched with adequate funding.
Media/ public education campaigns
10. The Committee is aware that the Department for Health, Social Services and Public Safety is working closely with the media on mental health and suicide/self-harm issues and is in favour of a rolling high profile media campaign to raise awareness and promote safe reporting.
11. The Committee would wish to see greater efforts being made to educate the public, and in particular our young people, about mental health, suicide and self-harm. The Committee recognises that other departments and agencies should be involved in education campaigns, particularly the Department of Education and the Department for Employment and Learning, and would encourage strong cross-departmental working. As with all media/education campaigns, any information produced should be accessible to all.
Faith communities
12. Faith leaders are in a key position to provide guidance to those who present with suicide and self-harm tendencies and influence societal attitudes. The Committee would recommend that guidance for Faith leaders be developed to include information on how to respond effectively to members of their congregations who present with suicidal or self-harm tendencies, or their families and friends. The Guide should also include advice to help leaders dispel the stigma and raise awareness about the issue.
Helpline and mentoring schemes
13. The Committee would recommend that the pilot schemes established to assist with the strategy’s implementation, including a telephone helpline and mentoring schemes for those in crisis, should be extended throughout Northern Ireland as a matter of urgency.
Recording
14. To deal with the issue of suicide it is vital that there are accurate statistics available to assess the full scale of the problem. Suicide rates in Northern Ireland are inaccurate as a result of an inconsistent recording system and the Committee would recommend that a robust system for recording suicide statistics is developed as a priority. The Committee also believes that the way in which coroners present their findings and the way in which a death is coded by the General Register Office should be examined. Bereaved families have expressed concern that the coding of deaths by other causes than suicide may be masking the real extent of the problem.
Resources
15. The Committee would urge the Department for Health and Social Services and Public Safety to allocate adequate funding to implement its Protect Life - Suicide Prevention Strategy and Action Plan in full. The Committee would also wish to see serious consideration being given to the submission of joint bids by departments on aspects of the Strategy/Action Plan that are cross-departmental.
Eastern Health and Social Services Board
1. Introduction
Research has highlighted the differing psychological motivation associated with self-harm and suicide ideation. Most people who commit self-harm are not seeking to take their own lives, but rather to find some relief from an unbearable psychological pain. Research suggests that approximately 30-40% of people who do self-harm have suicidal ideation. Whilst there are a range of factors which give rise to an increased risk to suicide which, amongst others, include deprivation, depression, physical and sexual abuse and alcohol or drug misuse, the single greatest predictor of future suicide is previous suicide attempts.
Work is being undertaken to better understand some of the psychological aspects of suicide to identify why some individuals who share some of the risk factors go on to make serious suicide attempts and others do not. A number of themes are beginning to emerge, not least the impact on the individual of issues such as bullying and confusion about sexual orientation.
Just as suicide is recognised as being everyone’s business, so the sound emotional and psychological development of children, which is a precursor to good mental health should also be regarded as everyone’s business. Health and Social Services, by themselves, cannot significantly ameliorate the damage to the individual and community caused by poor early development.
It will be seen from the above, that the Board strongly favours a multi-agency, early interventionist approach which is built upon greater co-ordination between the institutions of Health and Social Services, Education and Justice.
In this paper the Board will:
- Report on incidence of deliberate self harm in the Board’s area;
- Comment on stakeholder involvement;
- Report on services provided with funding from the “Protect Life” strategy; and
- Report on the current capacity of mental health services to meet this demand.
2. Incidence of self harm
The Committee will be aware that an initiative was launched recently in the Western Board area to collect data regarding self harm in a way that is consistent with the National Register of Deliberate Self Harm in the Republic of Ireland.
In response to the recently launched McCartan Report and the possible need for a 24/7 crisis service, data was extracted from our hospital information systems to better understand presentations to hospital A&E departments and admissions to hospital, as a result of self-harm. This work, which focuses on young people aged 10 to 24 and is broken down into age bands of 10-17 years and 18-24 years.
Care must be taken with this data for a variety of reasons. Firstly it is a manual exercise. Secondly it is not clinically coded data but a proxy derived from triage text. And thirdly, for the Mater Hospital, only 6 months data was available.
The following findings may be of interest to the Committee.
(i) A&E attendances and hospital admissions for self harm, of people aged 10 to 24, in EHSSB in 2005-2006.
The analysis to date has highlighted the following:
- 1,310 attendances at A&E department, relating to self harm were identified. Of these, 474 were aged 10-17 years and 836 were aged 18-24 years.
For the same period, in the whole of the Republic of Ireland, there were 2,990 presentations to A&E. The population in the Republic of 10-24 year olds is roughly 6 times that of the Eastern Board. The Eastern Board therefore has a rate of 852 per 100,000 of population as opposed to the Republic of Ireland rate of 326 per 100,000 (The Board would urge some caution as it has no means of verifying the completeness of the Republic of Ireland’ figures. However, these have been taken from the Republic of Ireland’s official documentation on self harm.)
- Females in both age categories were the greater service. The highest number of attendances was for teenage females with overdoses.
- The reasons for attending were:
- Overdoses 78%
- Cutting 9%
- Hanging 6%
- Other 7%
- Nearly 40% of attendances resulted in hospital admission. The precursors to admission were:
- Overdoses 44%
- Cutting 16%
- Hanging 16%
- Other 41%
- Some 9% of individuals presented to an A&E department with self harm on more than one occasion. Most people used the same hospital each time. Interestingly, this is lower than the repeat figure for the Republic of Ireland.
(ii) Hospital admissions for self harm, in Northern Ireland, in 2005-2006 and 2006-2007.
The analysis to date has highlighted the following:
- In EHSSB, 2005-2006, there were 585 hospital admissions as a result of self harm, 542 of which were Eastern Board residents.
- Of the 585 admissions, 185 were young people aged 10-17 and 400 were aged 18-24.
- The provisional 2006/7 data shows 612 admissions to EHSSB hospitals, 567 of whom were EHSSB residents.
- Within the EHSSB this represents 1 to 2 people aged 10-24 being admitted to hospital each day.
- As methods of self harm; cutting and hanging were more common in males than females. This is consistent with the data from the National Registry of Self Harm in the Republic of Ireland.
- Two thirds of all admissions were discharged the same or next day (72% of those aged 10 to 24 years)
- There is a marked difference in gender in the age profile of admissions. For females most admissions are by those aged 14 to 21. For males most admissions are by those aged 19 to 24.
(iii) Information from the Pilot Helpline run by the Belfast Trust for young people at risk of suicide
The above level of self-harm needs to be considered alongside early expressions of demand arising from the 24/7 helpline run by the Belfast Trust.
In July 2007 the helpline took 1,921 calls of which approximately 1,000 were “hang-ups” or “silent calls”. It is unclear what the motivation for these calls was, some may have been prank calls, but it might suggest that some callers were in need of help but not yet prepared to speak about their difficulties. There were 159 new callers in this month. The top ten reasons for calls are as follows:
% |
|
Information |
16 |
Suicide |
14 |
Self Harm |
13 |
Depression |
11 |
Family conflict |
9 |
Mental health |
8 |
Relationships |
8 |
Anger |
7 |
Bereavement |
7 |
Physical health |
7 |
Total |
100 |
It should be noted that calls were received from all parts of the Province and not solely the Belfast area.
3. Stakeholder involvement
Within the Board’s area stakeholder involvement takes place at two levels – locality and Board.
As part of the Investing for Health strategy a mental Health and Emotional wellbeing Community of Interest (COI) has been established in each of the four localities:
- North and West Belfast;
- South and East Belfast and Castlereagh;
- North Down and Ards; and
- Down and Lisburn.
The COI in North and West Belfast works closely with the local Suicide Prevention Task Force.
The Communities of interest consist of those individuals and organisations that identify themselves as being concerned about mental health issues. The Board used the COIs as the main consultative process for developing services funded by the Protecting Life strategy (see section 3, below).
The Board has established a Board-level sub-group of SSIB that has representatives of statutory, voluntary and community organisations and from Family Voices. The contribution made by the families themselves and the community sector is particularly strong within the Eastern Board area.
The sub-group’s primary role is to develop local priorities to assist in the implementation of the Protect Life Strategy. Another major objective is to ensure a consistency of approach by developing common pathways as to how individuals and families, who are at risk of suicide or where suicide has occurred, should be managed.
4. Services provided under the Protect Life strategy
In 2006-2007, £393,000 was spent in the Board’s area on services to prevent suicide and to help bereaved families to cope with its consequences. These services included:
- Mentoring support for young people at risk
- Counselling for young people
- ASIST suicide awareness training
- Mental Health First Aid training
- Early response service for families bereaved by suicide
- “Mood Matters” depression awareness for post primary pupils
- “Mind Out” teacher training
- Complimentary therapies
The Board’s Investing for Health Managers drew up the following assessment of the effectiveness of the services commissioned under the categories of prevention, intervention and post-vention initiatives.
(i) Prevention
Included under this heading are:
a. Information sessions for community groups/organisations/ schools
b. Production of materials and resources e.g. leaflets, directories of services, good practice guidelines, suicide awareness packs etc.
c. Education and training programmes e.g. ASIST, Mental Health First Aid, Mind Out for Teachers, Mood Matters, Mental Health Self Help Project).
What worked?
All of these initiatives were well received. There has been a very significant increase in awareness and understanding of individual partner/organisation work; a more cohesive and co-ordinated approach emerging across sectors and localities; and a greater consensus on focus and priority for investment in extending and developing new services.
We need to develop a common language around mental health & suicide prevention that promotes understanding of the issues. Printed material and resources are essential. However we need to avoid duplication or differing presentations of core messages while still providing local contacts/telephone numbers, etc.
The education and training programmes have already established waiting lists e.g. ASIST courses and Mental Health First Aid. These courses meet an obvious need for information, knowledge and skills.
What needs improved?
The challenge will be in ensuring that we have sufficient trainers to meet the demand. In addition, there is a need to maintain and support the development of consistency of information and training.
(ii) Intervention
A broad range of intervention services have been provided that include: counselling sessions, complementary therapies, peer education/mentoring programmes, diversionary and social activities for young people. Partners have been commissioned with dedicated staff teams to drive this agenda forward.
What worked?
There has been a gradual uptake of these programmes to the point where waiting lists are beginning to emerge. The locality approach enabled the identification of existing services and facilitated increased access and uptake.
What needs improved?
The Community of Interest model has proved a vital first step in identifying and anticipating real demand, but this is a complex issue that will take time to assess and stabilise. Dialogue is needed with other commissioning partners outside of HPSS to produce an evidence base for how in particular counselling based approaches can be more effectively and efficiently delivered.
(iii) Post-vention
A range of services have been developed and extended that seek to support those bereaved by suicide - information, counselling, support groups, complementary therapies and post treatment therapeutic support (for families as well as individuals).
What worked?
The counselling service for families offering a mix of one-to-one and group support have been well received with actual reported cases of how this service has prevented further suicides taking place. The local availability of these services has been important increasing profile, access and uptake.
What needs improved?
Some families bereaved by suicide find support in groups most helpful, but this is not available in all areas. There is the need to maintain the support and profile of these services and look at the longer term needs of those who have experienced bereavement from suicide.
General Comment
The Board believe that the initiatives undertaken by the voluntary and community sector, and in particular PIPS, have been very significant in highlighting the distress of individuals who self-harm and families bereaved by suicide. This has the effect of raising public awareness and facilitating the uptake of counselling and support.
5. The current capacity of Mental Health Services to meet Need
It has long been recognised that mental health services are under-funded within Northern Ireland. The high incidence of self-harm and suicide within the Board’s area has created a major challenge for services.
One illustration of this is in the field of Child and Adolescent Mental Health Services (CAMHS).
The Royal College of Psychiatrists, in their paper “Building and Sustaining Specialist CAMHS”, recommend as a minimum standard, excluding in-patient care, that there should be 15 clinicians per 100,000 population in non-teaching areas and that this should rise to 20 clinicians per 100,000 in teaching areas. These figures are for population up to their 16th birthday. In Northern Ireland, CAMHS are provided for young people up to their 18th birthday. These recommendations have been accepted by The English National Service Framework and the Bamford Review. In the Eastern Board, to meet this standard, would require approximately 120 clinical staff. At present the Board has 52 staff albeit that these numbers could be marginally boosted by realigning and retraining some staff who primarily work in the area of Adolescent Services but who would not recognise themselves as CAMHS professionals.
The Eastern Board has sought to compare its adult mental health services with other major industrial cities in the United Kingdom, most notably Manchester, Liverpool and Newcastle. The Board has done this by benchmarking its provisions with the national data collected by the University of Durham. There is an annual requirement on Trusts providing mental health services within England and Wales to report on a variety of measures including staffing.
The figures for the Eastern Board show that we are broadly comparable, albeit we have slightly less inpatient beds than our English counterparts. However, there is a marked difference in terms of community manpower and community services, with the Eastern Board having less than half the service provision of cities such as Liverpool, Manchester and Newcastle.
The consequence of this is that within the Eastern Board we have a much higher reliance on in-patient treatment, largely because of the dearth of alternatives. In recent years the Board has developed adult Crisis Response and Home Treatment services which have been effective in reducing the number of people coming in to hospital, but which struggle to meet the need for early assessment of individuals who self-harm. Work continues to try to improve this interface.
The Board is very conscious of the need to seek to ensure that wherever possible, people, be they children, adolescents or adults, are managed, as far as possible, within community settings. For this to be effective, specialist clinicians need to work alongside others such as GPs and teachers to ensure the latter’s capacity to effectively manage those with minor to moderate disorders is increased, whilst also achieving a greater consistency in the early identification of those with severe disorders who need more specialist intervention.
The Board believes that suicide and self-harm should be a priority for the Assembly. The Board believes that there is significant evidence of the damaging effects which poor mental health in childhood and adolescence will have in adulthood. The Board favours a co-ordinated early intervention approach. Such an approach requires coordination between the statutory, voluntary and community sectors. In particular it requires a strong Ministerial lead in relation to Health and Social Services, Education and Youth Justice to achieve a more timely and co-ordinated model of service delivery.
Department of Enterprise, Trade and Investment
New Life Counselling
Mission Statement:
New Life Counselling Service is a dynamic voluntary counselling service that is committed to meeting the emotional and psychological needs of children, young people, adults and families. It supports, guides and enables them in their journey to reach their full potential.
Background to New Life Counselling
Established in 1993, New Life Counselling is a small to medium sized company limited by guarantee, recognised as a charity by the Inland Revenue, located in north Belfast and serving the diverse communities of north and west Belfast. Services are being extended during 2008 to increase access across the Eastern Health Board area, in response to demands from referring agencies and partners.
This cross-community, non-political organisation employs a team of 30 paid, self-employed and volunteer counsellors to offer a therapy-based counselling service to all ages, through four distinct projects:-
- Child Project (5-11yr olds)
- Youth Project (11-25yr olds)
- Adult Project (25 yrs plus)
- Family Project (all ages and sizes)
Many of the team are already accredited practitioners, some are qualified to Masters level and PhD level in their specialist fields and therefore offer access to a wealth of knowledge and expertise for these communities of need.
The organisation is unique in that it is the only voluntary sector organisation offering a multi-modal response to the needs of some of the most vulnerable people in society.
The organisation has established a reputation for the provision of high quality, cost effective and efficient service delivery in partnership with statutory and voluntary agencies in the context of health and wellbeing, education, social inclusion, good relations and rehabilitation of offenders
The organisation welcomes this opportunity to share our experience of service delivery in north and west Belfast. Please refer to Appendix 1 for further information.
Scope and appropriateness of the Department’s strategy
New Life Counselling (NLC) welcomes the strategy and was actively involved in the work of the Health Action Zone (HAZ) Taskforce leading up to its publication.
Colm Donaghy, spoke to the strategy at our AGM in June 2006 and acknowledged the work of the agency in responding to local needs.
Recommendation
Medium to long term resource investment
It is noted that the resources secured to March 2008 from Protect Life (through the Belfast Trust) are most welcome in contributing to the work in this area.
However: -
- we only secured funds to work with children in August 2007
- we are still not funded by this route to work with adults, who suffer greatly in relation to this context.
Funding on an annual basis doesn’t facilitate medium or long term planning to respond to needs and doesn’t facilitate staff retention. If we are to respond effectively to the complex needs of vulnerable groups, we need to invest in securing the services of a professional team who are, in turn, secure in themselves that their role is not at ongoing risk of redundancy. Losing good people means we lose their expertise, knowledge and developed understanding of the need and how best to meet that need.
Therefore it is recommended that future funds are offered on a multi-annual basis rather than an annual basis.
Level of stakeholder involvement
Action areas: Mental Illness, Drug and Alcohol misuse and Prisoners and Health and Social Services.
The organisation has long established relationships with local GPs, health professionals, Hospitals, Trusts and community groups.
It is the view of New Life that the strategy was developed with effective engagement with key stakeholder groups. It is to be commended for its efforts in ensuring that the views of community groups on the ground and, in particular, the bereaved families, were heard.
It is the experience of the agency that GPs and Health Professionals rely heavily on our services and we welcome this ‘caring in partnership’ model of response. However, on occasion, inappropriate referrals have been made to the agency for individuals whose needs cannot be met by a voluntary community based counselling agency. In a small number of occasions these referrals were individuals at serious risk to themselves. It is due to the professionalism of the team at New Life that practitioners such s Dr. Marie Coyle, have the background and professional training to recognise, offer some diagnosis and advocate on behalf of the individual to ensure that the appropriate services intervene. This is extremely resource intensive to New Life and is not what we are funded to do.
Recommendations
1. It is recommended that resources are made available to enable New Life to facilitate training with key referral agencies to support development of understanding about these issues, effective responses, appropriate referral routes and partnerships locally with statutory partners (particularly PBNI and GPs), to protect the most at risk cases and reduce the risk of this recurring.
2. It is also recommended that statutory services are better resourced to respond to acute cases, to reduce the risk of people ‘slipping through the net’.
Level of services available to: -
- promote good mental health
- prevent suicide and self harm
- support those affected by suicide
- consider further action required
The agency has developed a unique multi-modal response to the complex needs of local families. The therapy team at New Life employs the services of almost 30 paid and voluntary counsellors and most have already achieved accreditation with BACP. Several have Masters level qualifications and some have PhD level qualifications, offering a wealth of knowledge and experience to local communities.
During 2006, the agency responded to ongoing and emerging needs as illustrated in Table 1 below
Table 1 –
Mental health and wellbeing Needs analysis of service users, north & west Belfast
Presenting issues/ risk factors |
Children |
Youth |
Adults |
Families |
Family breakdown |
√ |
√ |
√ |
√ |
Domestic violence |
√ |
√ |
√ |
√ |
Abuse (sexual, physical, emotional neglect) |
√ |
√ |
√ |
|
School and peer difficulties |
√ |
√ |
√ |
|
Difficulties with children |
√ |
√ |
√ |
|
Trauma related to the NI conflict |
√ |
√ |
√ |
√ |
Bereavement |
√ |
√ |
√ |
√ |
Bullying |
√ |
√ |
√ |
|
self harming behaviours and suicidal ideation and attempted suicide |
√(emerging need since 2006) |
√(ongoing since 1993. Increasing referral rates since 2005) |
√ |
√ |
Depression/anxiety |
√ |
√ |
√ |
√ |
Substance misuse |
√ |
√ |
√ |
|
Relationship difficulties |
√ |
√ |
√ |
√ |
Work related problems |
√ |
√ |
√ |
|
Family illness |
√ |
√ |
√ |
|
Separation/divorce |
√ |
√ |
√ |
√ |
Sleeping difficulties |
√ |
√ |
√ |
Source: NLCS service user presenting issues data, 2006
Promote good mental health
Action area: Communities, Children and Young People, Young Males, Marginalised and Disadvantaged Groups, Survivors of Sexual, Physical and Emotional Abuse
Dr. Marie Coyle, one of our youth counsellors, has delivered a series of innovative pilot health promotion or health education interventions in local communities in partnership with local schools and community groups. The model of mini conferencing and café style workshops has been evaluated by Dr. Coyle and was found to be an effective mechanism for awareness raising and mental health promotion amongst young people.
The evaluation also found that de-stigmatising mental health issues and possible helping responses (such as counselling) as well as promoting help seeking behaviours, was offering the young people more healthy options to consider when they are experiencing difficulty, as opposed to unhealthy options such as self harming behaviours.
A review of current research has confirmed that this model is new thinking and therefore we are happy to share our evaluation with you more fully, at your request. This model was supported for a one off pilot and is not currently funded by Protect Life.
The organisation developed a model of reaching young males at risk of suicide or self harm, in partnership with Challenge for Youth. The model supports young males to cope beyond survival in modern world. The model of partnership was held up as an example of good practice by the Big Lottery. Target group included those with suicidal ideation. Unfortunately there are no funds at present to resource the continuation of this model.
Recommendations
It is recommended that these innovative new modal responses to promoting good mental health are resourced to roll-out across the Eastern Board area to make support accessible to rural as well as urban localities.
Prevent suicide and self harm
Action areas: Children and Young People and Families
Protect Life has resourced a timely access to appropriate needs of local people and we welcome this. Prior to the strategy, New Life had a waiting list of approximately 30 individual cases in each of the child and youth projects. Sadly the lives of each of these individuals had been touched by suicide or self harm. Therefore the strategy has had a direct impact on improving the accessibility of services for at-risk groups.
However, the agency continues to receive demand for our unique multi-modal approach far beyond our capability to deliver. Therefore, on occasion we cannot offer support for those at- risk of self harm or suicide.
Furthermore children as young as ten yrs. have contemplated or attempted suicide. Recently a six year old child was reported to say he wanted to kill himself to be with his Dad. (Whilst children of this age normally play with the idea of being dead and killing, the reason stated behind this child’s words brings it into the realm of a harsh reality. Daddy had taken his own life and following in his footsteps was seen to be a possible way of connecting with him again). In an eight month period, c90% of referrals to one child practitioner (working with 5 – 11year olds) were related to suicide. These are shocking statistics. Suicide seems to have become a cultural option or life choice for children in the community within which New Life practices. There was a time when someone who was considering taking his/her own life would present in a way that might alert one to this possibility i.e. that someone was outwardly very distressed and self-harming. There were signs of desperation and suicide was the last choice for making change. Now suicide seems to be considered sooner as a solution to an experience of difficulty. It is as if there is less value for life.
New Life Counselling’s response to a suicide-related referral differs with each case in the child project. The following are some of the approaches taken:
- crisis intervention;
- self-care contract and risk management;
- prevention – investigating and promoting alternative actions
- education – the normality of traumatic and grief responses
- support network and community resources promotion
- advocacy; making links with wider system – family, school, GP, social services, child and family clinic
- bereavement work
These approaches are facilitated through ‘phone consultation as well as face-to-face work with children and or their carers. A direct cognitive approach may go alongside a more free, ‘processing’ approach where a child’s play, art, music and story-making is the primary vehicle for emotional expression and communication.
Please refer to Appendix 2 for an example of how we respond to a suicide-related referral.
Recommendations
1. A greater resource investment would be recommended to enable the agency to roll-out this unique model of practice across targeted communities of need in Belfast
Support those affected by suicide
Action areas: Children and Young People, Families, Self Harm and Bereaved by Suicide
All practitioners within the child therapy project continue to work with children (aged 5-11yrs) who have been referred because they have either been bereaved through suicide, usually of a parent, or they have contemplated or attempted suicide.
The youngest child referred who has attempted suicide is ten years old.
The youngest child referred to New Life for counselling, because of loss of a parent through suicide, is four.
When parents take their own life it raises many questions for children about, not just the value of life itself, but the value of the child in someone else’s life.
It stirs up normal feelings of confusion, anger, loss and sadness as well as a sense of vulnerability and fear related to sudden traumatic death. In our experience children who are thinking about taking their own life often present with low affect but may send out warning signals by writing letters or making pictures to be found in the home. Those who are bereaved through suicide may threaten to take their own life.
This can be a dramatic response to a traumatic death in an attempt to find escape from the flood of emotion, the search for understanding and the desire for things to be different.
The Child therapy team at New Life Counselling Service is a unique service in north and west Belfast and we are thankful that this emerging need was heard by the local team in Belfast Trust and that on response, the resources were provided to enable us to respond. Sadly, the team continues to struggle with a growing waiting list, as there is a dearth of provision for this age group. There is also a lack of practitioners with the specialist training required to work with this age group.
Recommendations
Therefore it is recommended that Protect Life releases resource to enable New Life to invest in the development and delivery of specialist training for practitioners in the region to increase the level of resource to this community of need.
Appendix 1
Origins of the organisation
The organisation was first established in 1993, to respond to the findings of a local research project into the needs of women in Ardoyne, Ardoyne Women’s Research Project (1990:29). At that time, there were no counselling services or statutory health services located in the area. The nearest health centre was approximately 2 miles away from this densely populated community of 7,000 residents living in overcrowded housing in an environment of chronic socio-economic deprivation, high security force presence, paramilitary activity, lack of green space, no outdoor play facilities and sanitation problems. The following was reported
- 73% often feel tense
- 58% often feel depressed
- 42% have felt suicidal
- 37% know a child or adult who has been sexually abused
- 36% have suffered as a family due to the troubles
- 30% are affected by domestic violence
- 27% said violence affects their lives
… the most frequently mentioned health concerns expressed were cancer, depression and stress. When asked how they coped with stress and depression in their lives all said that they tried not to think about it, or smoked, or used alcohol.
In north and west, over 25% of working age people are classed as having long term limiting illness or disability (2004). People in these communities are more likely to experience feelings of hopelessness that may lead to inappropriate or unsafe behaviour (such as smoking, alcohol related harm, drug misuse) A Healthier Future (2004).
Priority needs identified
- Improving mental health and wellbeing across all ages.
- Risk reduction intervention. Empowering individuals to manage / cope with or reduce the emotional and mental distress, feelings of hopelessness, impulsive and/or aggressive tendencies or harmful behaviours; the underlying causes of depression, stress, anxiety, dependency on alcohol, drugs (prescribed or illegal), smoking and other unhealthy coping mechanisms that, for some individuals, may contribute to the development of more acute health conditions such as clinical depression, acute mental health problems, self harming behaviours ,suicidal behaviours, heart problems, cancer and so on.
Increase good mental health awareness. Offer psycho-educational initiatives in partnership with statutory services, local primary and secondary schools and community groups, with children, parents, families and young people to create forums for discussion, sharing and learning about issues affecting them; to de-stigmatise counselling, increase knowledge of current issues such as suicide and self harm, managing emotions, problem solving, coping mechanisms and healthier alternatives to coping with difficult or stressful situations as well as reduce risk of trans-generational traumas / behavioural patterns developing.
Evidence-based need
Since 2000, these needs have been validated from a range of sources including data collected at regional and city level in relation to government departments’ strategic and policy planning; area based needs analysis and data collation by the organisation itself. Some examples of sources are noted below
Area based needs analysis
The organisation supports and makes use of findings from local surveys and research carried out by community based partners. For example
- Ardoyne Women’s Research Project (1990)
- A Statement of Need for North Belfast, NBPB (2002)
- The Early Years Feasability Study, Ardoyne Marrowbone Youth Providers Forum (2005), of which we are a member.
- Ardoyne Marrowbone CEP
- HAZ North & West Belfast Taskforce on Suicide Prevention (2006), in which we co-chaired one sub-group.
- Wellnet Health improvement plan N&W Belfast
Agency based research and analysis
Furthermore, New Life Counselling Service (NLCS) completes their own research and needs analysis (or commission these) based on the target groups availing of services and key stakeholders such as schools, community groups and statutory agencies in the locality. For example
- Justice Associates (2004) Networking and Programme Development Proposal for reaching young males 16-24 years old.
- Justice Associates (2005) Evaluation report on ‘Beyond Survival’ – An Experimental Partnership between New Life Counselling Service and Challenge for Youth.
- Diversity Works (2006) Diversity Needs Analysis/Action Plan NLCS
- CENI (2006) External evaluation of New Life Counselling Services.
- NLCS (2006) Survey of the needs of 11-18 year olds in north Belfast.
- NLCS (2006) Survey of the needs of 5-11 year olds in north Belfast
- NLCS (2006) Youth Focus group analysis of the needs of vulnerable young people in West Belfast
Regular needs analysis of target groups using services
New Life Counselling Service (NLCS) regularly analyses the nature of the needs presented on referral forms when local children, young people, adults and families refer themselves, or are referred by other agencies to NLCS, and these have been identified as follows: -
Appendix 2
New Life Counselling Service
Example response to suicide or self harm in the local community
It’s Friday.
A mother rings anxious and upset. Her ex-husband has taken his own life. Their 10 year-old son is threatening to kill or harm himself in the aftermath to the death. He is also asking questions about the suicide which she is not sure how to answer.
The level of risk is assessed as is the scope of support available to Mom (so she can support her son). She is advised that his dramatic response is normal and is probably a quest for understanding as well as being related to anger about the event. It is suggested that she talk with him honestly about the death so that he knows the truth (if he’s asking for it) and hears it from her (not from people on the street). This promotes his sense of trust and connection with his surviving parent. Mom is further advised of the importance of maintaining routine so there is a sense of control over some aspects of life.
There is an invitation to see the child on Monday and the offer of ongoing support to Mom. The child attends his appointment. He spends the whole time talking about his father and how he died. He makes something to put on the graveside.
He had the opportunity to think, feel and talk freely about his response to the suicide. He knew the practitioner didn’t need protected from the awful truth. He knew she was there to hear and support him. He continues to attend. His Mom knows that therapeutic support is available for her if she ever feels she needs it in her own right. In the meantime the practitioner connects with her and the school in the interest of supporting him.
As practitioners we have the unique opportunity to invite children to be curious about death, to consider the value of life and to be informed about options in life when the going gets tough. It is our responsibility to the children and their families to help them think about how to find happiness and strength within themselves so they know they can live through the challenges of growing up.
Pat McGreevy,
South Eastern Health and Social Care Trust
Scope and Appropriateness
The strategy is a comprehensive document which suicide prevention activists and families bereaved by suicide campaigned for and is in keeping with similar national strategies.
Looking at the key objectives:
To raise awareness of mental health and wellbeing issues
More needs to be done to raise awareness about suicide specifically and the potential to prevent it. We know that the majority of suicides are preventable and some of the myths that surround suicide e.g. talking about suicide will put the idea in the person’s head are barriers to prevention. The current public information campaign based on a ‘slow release’ approach needs to talk about suicide sooner rather than later and tackle these myths.
To ensure early recognition of mental ill health and to provide appropriate follow-up action by support services
If the goal is to prevent suicide, then the early recognition of people at risk of suicide needs to be the objective. Training programmes such as ASIST (Applied Suicide Intervention Skills Training) and SafeTALK (Suicide Alertness for Everyone) help people from all backgrounds to identify people at risk of suicide and people with thoughts of suicide at an early stage
To develop co-ordinated, effective, accessible and timely response mechanisms for those seeking help
There are noticeable gaps that need to be addressed if this objective is to be met. People not deemed to have a psychiatric diagnosis but still at risk of suicide are sometimes left with no service. Sometimes there is a diagnosis of ‘personality disorder’ for which psychiatric services can offer little in terms of treatment. More needs to be done for this group who often are at high risk of suicide. People who care for someone who has made several attempts to end their lives are often left to carry this burden of caring without adequate information, support, respite and guidance on taking care of their own needs.
To provide appropriate training for people dealing with suicide and mental health issues
Appropriate training does exist, but will need adequate resourcing and standardisation across the region. The review of Mental Health Promotion and Suicide Prevention training being conducted by the Health Promotion Agency on behalf of the Suicide Strategy Implementation Body is welcome and the findings eagerly awaited.
To enhance the support role currently carried out by the voluntary / community sectors, bereaved families and individuals who have made previous suicide attempts
Suicide prevention is everyone’s business. The community and voluntary sectors should be seen as full partners in the suicide prevention enterprise.
In each locality a network of voluntary, statutory and community responses can be created based on the principles of evidence based practice, appropriate training, supervision and evaluation for all partners
To support the media in the development and implementation guidelines for a suitable response to suicide related matters
Media guidelines have been produced and are welcome. A structure needs to be put in place to ensure regular ‘reminders’ and a permanent method of ‘policing’ media reports on suicide deaths.
To provide support for research and evaluation of relevant suicide and self-harm issues;
There is a growing research interest in the phenomena of suicide and self harm. Consideration should be given to linking the two local universities in a virtual suicide prevention research institute. Such an institute could attract some of their own funding and cater for the increasing numbers of students wishing to research areas of self harm and suicide.
There is little evidence to date that the recommendations / findings of the National Inquiry into Self Harm Among Young People: Truth Hurts, Mental Health Foundation (2006) is being considered or implemented.
To restrict access, where possible, to the means of carrying out suicide
One year on from the launch of the strategy it is not known how much has been done to meet this objective.
In some local areas disposal of unwanted medicinal products have been piloted and these could have value in regional campaigns.
Analysis of current methods used to effect suicide should highlight other prevention initiatives.
Level of Stakeholder Involvement
The level of stakeholder involvement is commendable given that there are 35 -40 groups and organisations represented at the Suicide Strategy Implementation Body.
There are two concerns however
i a robust system of communicating the progress of SSIB to the local community level is lacking. Perhaps short communiqués under the headings of Strategy Objectives would be very helpful;
ii there is a feeling that while SSIB members are given due respect and a hearing that major decisions taken at the inception of the strategy cannot be easily influenced e.g. Depression Awareness Campaign for GPs and Public Information Campaign even though the feeling at community level that both these initiatives require a major rethink. The decision to roll-out the 24/7 helpline without a formal evaluation is questionable and again some stakeholders feel powerless in their attempts to secure a formal review.
Level of Services and Support Available
to: promote good mental health
prevent suicide and self harm
support those affected by suicide
Systems and initiatives to promote good mental health seem robust. The promotion of mental health using settings approaches e.g. home, schools, workplaces seem to have had a good impact and need to be supported. Standardised mental health promotion programmes across the region would be very helpful as would wide publicity to alert the general community that these programmes are being implemented.
The growing collaboration between the Education and Health sectors in promoting mental health at local levels and increasingly at Departmental levels is very welcome. The initiatives such as teachers being trained in the ‘Mind Out’ mental health promotion and that across the Education Spectrum i.e. teachers, psychologists, youth workers and education welfare officers being trained in ASIST is also very welcome.
The recent changes in the school curriculum will help focus on emotional and mental health and enhance this health / education collaboration.
Looking at services to prevent suicide and self harm there is a clear need to look at new and enhanced models of service. The locality partnership model referenced earlier would help to link the support needed for people at risk. Ideally a community should have youth counselling services, floating support, adult counselling, ASIST trained caregivers, rapid psychiatric assessment, psychiatric beds, crisis beds for short term non psychiatric crisis and a comprehensive response to people affected / bereaved by suicide and services for those caring for someone who is suicidal.
Current guidance on what services are available now with signposting information for each locality would be very valuable.
A 24/7 suicide helpline should become a regional resource for people for all ages but only when a proper review of the pilot has been undertaken and if no other alternative models are considered to be more effective.
For people bereaved by suicide there are a number of key needs that have yet to be met. Bereaved families and their support groups need someone in a paid position to coordinate their efforts, make the links between the groups, outreach to individual families, facilitate the setting up of support in areas where none exists and support the Families Voices network administratively.
Further Action Required (including experience elsewhere)
- Review the 24/7 helpline pilot before any regional roll out
- Scope the role and appoint a regional families worker for those bereaved by suicide and their support group
- Review the progress and direction of the Public Information Campaign and in particular the ‘slow release’ approach and apparent reticence about talking about suicide and the myths that surround it
- Review the Depression Awareness Campaign for doctors. A programme that trains some primary care staff in suicide Interventions (ASIST) and the remainder in suicide alertness (SafeTALK) would seem to be more effective if suicide prevention is the aim
- Explore the provision of ‘crisis beds’ for people at risk of suicide who do not require full psychiatric admission but who require short term supervised care
- Support the work of local district and city concils and others in taking specific suitable prevention initiatives e.g. Lisburn City Council: funding for 4 ASIST workshops in council premises enabling caregivers from all backgrounds to intervene with people at risk of suicide
- Review the progress in implementing the National Inquiry into Self Harm Among Young People ‘Truth Hurts’, Mental Health Foundation (2006)
Board for Mental Health &
Learning Disability
Thank you for inviting a response from the Board for Mental Health & Learning Disability to your Committee’s enquiry into suicide. I note the Terms of Reference for this enquiry. I am also acquainted with the present Strategy “Protect Life: A Shared Vision”. While as Chairman of the Board for Mental Health & Learning Disability I have an overarching interest in the entirety of proposed reforms detailed in the Bamford Review, I have had a long standing interest in suicide prevention.
As a general comment I would add a strong endorsement for the present Strategy and the central drive and direction given to this by the Minister and the Department. This has been long overdue. I would caution against an over-rigorous analysis of the effectiveness of the Strategy at this early stage of implementation. Nevertheless I am encouraged to see the plans being unfolded for a rolling evaluation and have recently met with Lesley Boydell who has been commissioned to develop this evaluative work. Her proposed work which includes a heavy emphasis on qualitative evaluation is I believe essential for an understanding of the impact of interventions on the complexity of processes impacting on suicidal behaviour.
I have also been impressed with the robustness of the arrangements underpinning the piloting of the helpline and 24-7 crisis service provision. In particular I would like to endorse the emphasis being placed on standards of counselling, training and support. The early take up of this facility is encouraging.
While central initiatives and strategic support will be essential for the success of our suicide prevention Strategy, local initiatives overseen by each Board area must be facilitated and developed, sensitive to local issues and need. There are examples of good practice in Board areas including the level of stakeholder involvement.
Statistics. The statistics from the General Registrar’s Office is an important resource for the challenge of suicide. It draws attention to significant demographic variability itself the subject of recent research analysis (Dermot O’Reilly, personal communication). This research suggests that individual level variables such as disadvantage and health are significant influencers of suicide rather than geographical variation per se. The present statistics also indicate that the majority of people taking their own lives are in the adult age range (20-50 years).
There are also issues regarding the reliability and the interpretation of statistics on suicide particularly year on year. This includes the difference between the time of occurrence of individual suicides and reporting, which can be months and years later. The sheer variability in this interval between occurrence and reporting can itself lead to spurious peaks and troughs on the reported suicides and suicide rate. Since, and including 2006, there has been a significant effort by the Coroner’s Office to reduce the variability of reporting.
The suicide Strategy is inevitably a long haul process. Particular interventions within the Strategy and directed at both prevention and post-vention must be linked to upstream elements within mental health promotion and service provision identified within the Bamford Review. A major concern is the chronic lack of resourcing for both mental health promotion and service modernisation. The mental health and resilience of our young people and all citizens must be at the heart of a prevention strategy. Suicide prevention must also recognise those most at risk suffer from mental health problems and are often in contact with mental health or primary care services. These services must be more responsive to the needs of vulnerable individuals. The resourcing of mental health promotion and service reform must go hand in hand with specific interventions identified within the suicide Strategy.
I expect many of the foregoing comments and observations may already be familiar to the Committee and nevertheless trust that the comments may be of assistance in the context of the wider responses to the Committee enquiry.
Thank you for the opportunity to respond.
Roy McClelland
Chair
Roy J McClelland (Professor)
Enc
Law Centre (NI)
Summary of Main Concerns
In this submission, we draw the Committee’s attention to our key concerns and recommendations relating to the prevention of suicide in Northern Ireland. We recommend the Committee give consideration to the following:
- the full implementation of the recommendations of the Bamford Review;
- cohesive planning and implementation of the Bamford Review, the Suicide Prevention Strategy and The Promoting Mental Health Strategy and Action Plan;
- the development and inclusion of specific performance measurement indicators that could monitor the progress of actions in delivering on quantifiable targets;
- commissioning of research on the specific needs of communities within Northern Ireland;
- the use of the European Convention on Human Rights through the Human Rights Act 1998 in the promotion and protection of suicide prevention in Northern Ireland;
- an increase in provision and education on the benefits of ‘talking therapies’ including but not limited to cognitive behavior therapy;
- the introduction of mandatory training for nominated GP’s and other health/social care professionals on depression awareness;
- the inclusion of effective monitoring and follow-up for public campaigns on mental health;
- increased access to effective crisis services, including community services as well as in-patient wards;
- better targeting of high risk groups in the provision of services and support;
- school and/or community programmes to equip young people with effective problem-solving skills.
1. Introduction
1.1 Law Centre (NI) is a public interest law non-governmental organisation. We work to promote social justice and provide specialist legal services to advice organisations and disadvantaged individuals through our advice line and our casework services from our two regional offices in Northern Ireland. It provides a specialist legal service (advice, representation, training, information and policy comment) in five areas of law: mental health, immigration, social security, community care, and employment.
1.2 Our services are provided to almost 500 member agencies. Members include local Citizen Advice Bureaux, independent advice agencies, local solicitors, trade unions, social services, probation offices, constituency associations of local political parties, libraries and other civic organisations.
1.3 Law Centre (NI)’s mental health legal service provides advice and legal representation in relation to issues around admission to hospital for assessment, capacity, treatment, discharge delay, community services and other mental health related legal issues. We welcome the opportunity to respond to this inquiry and commend the Committee on its interest and commitment to this important issue.
2. Suicide and Mental Health
2.1 Between 2000 and 2004 there were approximately 150 suicides recorded annually in Northern Ireland, with over forty percent being young men aged under 35 years. In recent years there has been a significant increase in the number of suicides, with 291 suicides recorded in 2006.[1]
2.2 According to the World Health Organisation in the last 45 years suicide rates have increased by sixty percent worldwide. Suicide is now among the three leading causes of death among those aged 15-44 years (both sexes); these figures do not include suicide attempts up to twenty times more frequent than completed suicide. Suicide worldwide is estimated to represent 1.8 percent of the total global burden of disease in 1998, and 2.4 percent in countries with market and former socialist economies in 2020.[2] Although traditionally suicide rates have been highest among the male elderly, rates among young people have been increasing to such an extent that they are now the group at highest risk in a third of countries, in both developed and developing countries. Indeed within Northern Ireland’s Suicide Prevention Strategy, ‘Protect Life: A Shared Vision’, males aged between 18 and 34 have been identified as a specific priority target area.
2.3 There is an established link between mental ill health and suicide. According to the World Health Organisation mental disorders (particularly depression and substance abuse) are associated with more than ninety percent of all cases of suicide.[3] Research shows that poor mental health is often a contributory factor in many suicides in Northern Ireland. With one in six people in Northern Ireland suffering from a medically identified mental illness at any one time[4] it is clear that urgent work is required to address the lack of services and support for those with mental ill health to stem the increase of suicides within Northern Ireland.
2.4 The Bamford Review of Mental Health and Learning Disability provides a comprehensive analysis of mental health and learning disability services, policy and legislation in Northern Ireland.[5] Suicide and suicide prevention is a major feature across many of the Review’s reports. The Review makes many detailed recommendations regarding suicide prevention which Law Centre (NI) support and commend. We would recommend that the Committee as part of this inquiry call for the full implementation of the recommendations of the Bamford Review.
3. Reviews and Research
3.1 The inquiry is timely with the release of the final report of the Bamford Review and the current review of the Suicide Prevention Strategy and The Promoting Mental Health Strategy and Action Plan. It is critical that all of these reviews and reports are taken forward in a cohesive and effective way. As part of the inquiry we would advocate for the development and inclusion of specific performance measurement indicators that could monitor the progress of actions in delivering on quantifiable targets.
3.2 Research helps determine which factors can be modified to help prevent suicide and which interventions are appropriate for specific groups of people. Further specific research needs to occur within Northern Ireland to ensure that appropriate and effective services and support systems are put in place to deal with the specific needs of communities. Before being put into practice, prevention programs should be tested through research to determine their safety and effectiveness. For example, because research has shown that mental and substance-abuse disorders are major risk factors for suicide, many programs also focus on treating these disorders. Consideration therefore needs to be given to the collation of Northern Ireland specific data and the creation of programmes aimed at the particular needs of Northern Ireland communities.
3.3 Consideration should also be given to the use of the European Convention on Human Rights through the Human Rights Act 1998 in the promotion and protection of suicide prevention in Northern Ireland. Article 2 is particularly relevant as it places a positive duty on governments to protect life.[6] There is a growing body of case law on the use of Article 2 in suicide related cases, many of which relate to investigations into suicide or attempted suicide in prison.[7]
4. Training and Public Awareness
4.1 We are aware that the Protect Life strategy includes a commitment to the provision of training in depression awareness for General Practitioners and other primary care professionals and staff. We understand that the take up of this training across Northern Ireland has been limited and would welcome further information as part of the inquiry regarding the reasons for this and action plans to encourage the take up of this vital training. We recommend that consideration be given to the introduction of mandatory training of this nature with the requirement that each GP practice nominate at least one staff member to undertake the training to ensure that each practice has at least one ‘specialist’ in this field.
4.2 We welcome the development and roll out of the “Minding Your Head” campaign by the Department of Health, Social Services and Public Safety, though the Health Promotion Agency for Northern Ireland, as part of the ongoing implementation of the Protect Life strategy. We note that the campaign highlights how mental illness can affect anyone and the need for individuals to take control of their own mental health. Mental health promotion and prevention is closely linked with suicide prevention and campaigns need to integrate both issues.
4.3 Stigma and discrimination against people with mental health problems is rife through all areas of society and its impact is far reaching and goes beyond just the impact on an individual to society as a whole. Sixty-three percent of people surveyed in Northern Ireland underestimated the proportion of people who might have a mental health problem at some point in their lives while over half said that if they were experiencing mental health problems they wouldn’t want people knowing about it.[8]
4.4 Northern Ireland has seen two other campaigns this year by BBC Northern Ireland and Rethink, to address the stigma and discrimination associated with mental health. The success of these campaigns is yet to be determined but we are encouraged by the positive work undertaken by agencies in Northern Ireland to address this issue. Further work, however, needs to be done to ensure organisations working in the field of mental health and learning disability are sufficiently resourced to enable them to work on campaigns to create long-term positive impact.
4.5 The inquiry should consider ensure that any such campaigns are closely monitored in order to determine effectiveness. High profile media campaigns can be expensive and there is often a lack of follow through at the conclusion of such campaigns. While the issues may be highlighted if there are insufficient support services on the ground to assist people who respond to public campaigns the success will always be limited.
5. Services and Support
5.1 Studies in the United States showed that cognitive behaviour therapy (CBT) reduced the rate of repeated suicide attempts by 50 percent during a year of follow-up. A previous suicide attempt is among the strongest predictors of subsequent suicide, and cognitive therapy helps suicide attempters consider alternative actions when thoughts of self-harm arise.[9] As highlighted in the Bamford Review further resources are required to provide adequate psychological therapies for the treatment of mental ill health. We are encouraged by the increase in availability of CBT in Northern Ireland through the Northern Ireland Centre for Trauma and Transformation but more needs to be done. Further consideration needs to be given to other ‘talking therapies’ including dialectical behavioural therapy which can have extremely positive results in the management and prevention of mental ill health.
5.2 There is a clear need for increased access to effective crisis services, including community services as well as in-patient wards to meet the needs of those at risk of suicide or self-harm. As part of the provision of effective services consideration must be given to better targeting of high risk groups as highlighted within the Protect Life strategy but which in reality has seen little action on the ground.
5.3 While we welcome the increased awareness of the needs of children and young people within the Bamford Review and the recent increase in provision of facilities for Child and Adolescent Mental Health Services. Consideration must also be given to prevention and the provision of school or community programmes to equip children and young people with effective problem-solving skills to develop coping skills and awareness of mental health which will aid the prevention of suicide.
4. Conclusion
4.1 Law Centre (NI) welcomes the opportunity to provide a submission to the Committee. We trust you will find our comments helpful. If there is any further way in which we could contribute to this process we would welcome the opportunity to do so.
[1] See http://www.northernireland.gov.uk/news/news-dhssps/news-dhssps-july-2007/news-dhssps-100707-mcgimpsy-announces-relaunch.htm
[2] See http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
[3] Supra
[4] Northern Ireland Department of Health, Social Services and Public Safety, “Effectiveness Evaluation: Health and Social Care”, 2003, chapter 7
[5] For further information on the Bamford Review of Mental Health and Learning Disability (N. Ireland) see http://www.rmhldni.gov.uk/
[6] For more information on the European Convention on Human Rights and the Human Rights Act see Allamby, L, Rights in Progress, 3rd edition, Law Centre (NI), 2007
[7] Cases include Keenan v UK (2001), R(D) v Secretary of State for the Home Department (2006) and re Mongan’s application (2006)
[8] Health Promotion Agency, Research into Public Attitudes to Mental Health 2006, at www.healthpromotionagency.org.uk
[9] Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association . 2005 Aug 3;294(5):563-70.
The Health & Social Services Councils
1. The Health & Social Services Councils (HSSCs) were set up by Government in 1991 to represent the views and opinions of the public. There are four Councils in Northern Ireland with local offices currently based in Belfast, Broughshane, Lurgan and Omagh. We are independent from those who plan, manage and provide health and social care.
2. The HSSCs welcome the opportunity to provide evidence to the Health Committee Inquiry into the prevention of suicide and self harm. This is a topic that individual Councils take a keen interest in because we feel that this issue goes to the core of the health and social care needs of our communities. This response has come out of a joint Council Forum on the Protect Life strategy held on 25 October 2007.
3. This response will comment on each of the Committee’s terms of reference.
4. Assessing the scope and appropriateness of ‘Protect Life’:
a. The strategy has been extremely useful in focusing attention on the issue.
b. There is concern that the strategy has ‘hit the target and missed the point’ in that while of the strategic aims of bringing people together has been achieved, this has not necessarily been reflected in more timely service delivery.
c. Some of the activity is in danger of becoming a box ticking exercise eg the depression awareness training for GPs. Take up in some areas has been slow. Where one GP in a practice has been trained, there is little evidence that this has been cascaded to other staff in the practice or has impacted on working practices.
d. When a GP identifies mental health problems, there is often a difficulty with the lack of readily available services for onward referral. Long waiting lists may mean that the patient is left with little support. Referral to on-line resources may work well for some people but we feel that this requires personal contact to ensure the ongoing well-being of the patient. Where interim mentoring services are put into place to support families, there needs to be a clear treatment and ongoing support pathway identified.
5. Examine the level of stakeholder involvement:
a. Stakeholder involvement appears to have been proactive and at the heart of the strategy and the Task Force’s work.
b. However, it appears that some stakeholders still require to take greater ownership of their role. For example, the evidence suggests that mental health issues may occur in one-third of GP consultations. This indicates the importance of the mental health component of core general practice training as well as the need for GPs to up-take on additional training opportunities such as the depression awareness initiative.
c. Involvement of bereaved families is a positive element in the work of the Task Force and the implementation of the strategy. The personal commitment of bereaved family members involved in the Task Force and local support groups is to be commended. However, the experience of the Family Forum/Families’ Voice and the local support groups shows the difficulties faced by bereaved families. At such a vulnerable time, they are endeavouring to support their own families and other bereaved families. They are perhaps involved in fund raising for, and running, local services as well as contributing to strategic discussions about the future planning and delivery of services. Further work needs to be done on the best way of supporting families in shaping the delivery of services and contributing to the strategic direction of the strategy.
6. Level of services and support available:
a. The provision of timely services is a long way from being in place.
b. A range of services is required for GP referral and self referral.
c. The early identification of those people at risk appears to be a gap in service provision. This needs to be supported by adequate research to underpin service development.
d. Parental support in regard to recognising risk taking behaviour in their offspring appears to remain a gap in service provision.
e. Additional support to schools to tackle this area is required.
7. Further action required:
a. The Bamford Review proposals should be adopted.
b. The strategy can only succeed if it becomes genuinely cross-Departmental and is driven by the Assembly as a political priority.
c. A Northern Ireland co-ordinating office should be established to co-ordinate local plans and regional activity.
d. Further research is needed to assist us as a community in answering the question ‘why’? This would assist in the development of preventative services and help to counter the ‘ripple’ effect of suicide and attempted suicide.
e. Clear regional targets should be set. These should include a range of targets for referral/service delivery eg 13 week target of cognitive behavioural therapy.
f. There needs to be an increased understanding that suicide and self harm is not solely a threat to young people. The needs of people of all ages require to be built into the strategy.
g. The central role of GPs requires to be strengthened by further training and increased engagement by GPs with the strategy.
h. HSC Trusts should be required to put in place a family support service capable of providing intervention within 48 hours to a bereaved family.
i. Responsibility for implementing the Protect Life strategy lies with those bodies funded to deliver against its objectives. These may be statutory or voluntary organisations. There needs to be an across the board evaluation of the outputs and outcomes delivered to date to ensure that the strategy develops as an evidence based process.
8. The HSSCs have welcomed the opportunity to reflect upon the Protect Life strategy. As part of our role to represent the public interest in health and social care, we will continue to scrutinise and comment on the implementation of strategy.
S Cunningham
26 October 2007
The College of Occupational Therapists
1. The College of Occupational Therapists (COT) represents over 29,000 occupational therapists, students and support workers across the United Kingdom, of which over 900 are either working or studying in Northern Ireland. Occupational therapists (OTs) work in the NHS, Local Authority Social Services and Housing Departments, schools, primary care settings, and a wide range of vocational and employment rehabilitation services.
2. Occupational Therapists are regulated by the Health Professions Council, and work with individuals of all ages with a wide range of occupational problems resulting from physical, mental, social or developmental difficulties. The philosophy of occupational therapy is founded on the concept of occupation as a crucial element of health and wellbeing. Practice is based on holistic, person centred care.
3. In response to the inquiry being carried out by the Assembly Health Committee to examine the current strategy to prevent suicide and self-harm, The College of Occupational Therapists (COT) would like to make the following points.
4. In ‘Protect Life A Shared Vision, The Northern Ireland Suicide Prevention Strategy and Action Plan 2006-2011’ (October 2006), the profession would like to see more emphasis being given to the importance of occupation and activity to wellbeing and health throughout the strategy. Much of ‘who we are’ is ‘what we do.’ Occupational therapists in Northern Ireland would like to see recognition of the relationship between occupation, mental health and wellbeing
5. During the Northern Ireland Assembly debate on 17 September 2007, Ad Hoc Committee on Suicide, Iris Robinson said, ‘Society will never effectively deal with suicide by expecting mental-health professionals alone to solve the challenge. However, by accepting that suicide is a social, biological, spiritual and mental-health problem, all those areas can be examined to find a solution.’ Practice of occupational therapy is based on holistic, person centred care, so with this in mind, we agree that the issue should be looked at holistically.
6. Cases of suicide where the person has never been known to services indicates the necessity to look at the needs of the whole population. Identifying factors, which affect individuals and communities in Northern Ireland, should be considered. In Northern Ireland life has changed dramatically over the past number of years. How have people been affected and how have they coped with the transitions they have had to face as well as the consequences they have not been prepared for? As one example, in rural areas many have had to leave the farming industry or have had to diversify. As well as erosion of occupational roles, ways of life associated with rural farming has changed. Community and individual, social and leisure activities have changed and are continuing to do so, for example many young people socialise through computers and mobile phones. The way that work is carried out has changed. There is a sense of ‘personal contact’ being lost in how people carry out their roles, which only adds to the sense of isolation that some people may feel and dissatisfaction for those both doing the job and those at the receiving end of it. The social aspect of work is eroded as performance, targets and results are scrutinised. In the past people in the workforce may have conversed over shared lunch or even taken part in an activity or game. Such social engagement and activity is becoming rare. Changes in the pace of change of working practices along with new working initiatives may result in people feeling they have no control over their lives when expected to adapt rapidly. Lifestyles, occupation and activity have changed dramatically along with expectations of others and ourselves. It does seem some practices from the past may have been better for our overall wellbeing and health. However, we are not so much commenting here on whether these changes are good or bad, but we do feel the issue of coping with change and transition in life should be examined. Strategies for coping and looking at measures to ensure balanced lives should be promoted for positive mental health.
7. Iris Robinson at the same debate also said that, ‘The young and the old may be at risk from suicide because they feel useless and worthless. They have no purpose in their lives and, worst of all, they have no hope that that will change. Research has consistently shown that hopelessness puts a person who is contemp¬lating suicide at high risk.’ The College feels that aims, objectives and actions should be targeted for people in all life stages and all age ranges and once again would like to reassert the profession’s belief that ‘occupation’ is essential to health and wellbeing.
8. The centrality of occupation in human life is fundamental to the practice of occupational therapy. Having the opportunity to engage in occupation in its widest sense, including paid and voluntary work, recreation and leisure activities is a fundamental human right and a route to participation and social inclusion. The College has sought to promote that ‘Occupation Matters’ and that services intended to meet individual needs must help people to engage in those occupations that add purpose and richness to their lives.
9. We enclose a copy of ‘Recovering Ordinary Lives. The strategy for occupational therapy in mental health services 2007-2017. A vision for the next ten years’, which we hope, you find useful. It presents a user-led vision of how such services should be delivered. http://www.cot.org.uk/newpublic/about/new-pubs.php (College of Occupational Therapists)
Belfast Health & Social Care Trust
National Suicide Research Foundation
Proposal to Establish an All-Ireland Inquiry into Suicide
In Ireland, North and South, significant progress has been made in suicide research and prevention. Despite this, there are major gaps in our knowledge and understanding of the causes of suicide. We also struggle to respond to the occurrence of suicide clusters and the bereaved are often unaware of the relevant support services that are available.
A target of reducing the incidence of suicide by 10% by 2010 was set for Reach Out, the National Strategy for Action on Suicide Prevention while a 10% reduction in suicide by 2008 was set for Protect Life, the Northern Ireland Suicide Prevention Strategy and Action Plan. However, the reliability of suicide statistics, North and South, may undermine the reaching of these targets.
The National Suicide Research Foundation has proposed that a National Inquiry into Suicide be established in Ireland in order to address the above issues. We propose that such an inquiry could be established on an all-island basis. The Inquiry would directly address a range of actions in both Reach Out and Protect Life.
The Foundation has established the National Registry of Deliberate Self Harm in Ireland, collecting data from every general hospital accident and emergency department in the country. The Registry has reliably established the incidence and pattern of deliberate self harm in Ireland. It is informing service providers in hospitals and policy makers in the Health Service Executive. A target of reducing repeated deliberate self harm has also been set for Reach Out, the evaluation of which will rely on the Registry data.
To develop and pilot a self harm register in local A&E departments was a specified action of Protect Life. The National Suicide Research Foundation is working with colleagues in Northern Ireland’s Department of Health, Social Services and Public Safety, Co-operation and Working Together and the Western Trust to establish the pilot self harm register. Such co-operation and partnership shows the feasibility of adopting a common inquiry system for investigating, understanding and responding to suicide.
The main objectives of an All-Ireland Inquiry into Suicide would be to:
- identify and better understand the causes of suicide
- improve the provision of support to the bereaved
- identify and respond to clusters of suicide and filicide-suicide
- improve the accuracy of suicide statistics
The Inquiry would operate in close collaboration with coroners, North and South. The Inquiry would obtain data on possible suicide deaths shortly after they occur through notification by the coroners. It would support the provision of information on suitable support services to the bereaved. It would obtain relevant data on factors associated with the death and the deceased in an appropriately sensitive and confidential manner from sources including coroners, the family, general practitioners and mental health professionals.
Adopting a common approach to the Inquiry North and South would mean achieving the above objectives with the added benefits of greater economies of scale, comparability of data and evidence for the development of preventive measures. Developing a suicide inquiry and a self harm register on an all-Ireland basis would address all nine of the overarching actions specified in Protect Life.
Contributors: Dr Ella Arensman, Dr Paul Corcoran and Eileen Williamson, National Suicide Research Foundation.
Western Health & Social Services Board
The Western Health and Social Services Board have established a WHSSB Suicide Strategy Implementation Group, to take forward the recommendations and actions emanating from the Northern Ireland Suicide Prevention Strategy – Protect Life.
Remit of the Group
A. Aim
Develop and implement an action plan, using the recommendations of the NI Suicide Prevention Strategy – Protect Life in the WHSSB area, and oversee and monitor the actions identified;
B. Objectives
- Drive forward (the NI Suicide Prevention Strategy) in line with the IFH Strategy and other regional strategies
- Prioritise the action plan and establish appropriate sub-groups to take the work forward
- Establish a process to identify representation on the Suicide Strategy Implementation Body (SSIB) from the community and voluntary sector in the West
- a mechanism to influence the work of the SSIB and also to communicate back to the wider community of the work and development driven by the SSIB
- partnership working between statutory service providers and those in the community and voluntary sector
- the implementation of the Suicide Strategy and make recommendations, amendments and changes as necessary
- Influence current and future investment within the Strategy.
C. Membership
The forum will be made up of 7 statutory and 7 non-statutory representatives and will be co-chaired by both Mrs Dorothy Hutchinson (WHSSB) and a non-statutory member.
Membership of the Western Suicide Strategy Implementation Group is currently being finalised;
- Statutory
- Dorothy Hutchinson (Co-Chair)
- Brendan Bonner (IFH)
- Jim Simpson (WHSSB)
- Barry McGale (Health Promotion)
- Dermot Lynch (Health Promotion)
- Gabriel Carey / Bernard McAnaney (New WHSST)
- Philomena McDermott (WELB)
- Non-statutory
- Ciaran Fagan (STEER)
- Pat Lynch (Aware Defeat Depression)
- Noella McConnallogue (Zest – Co-Chair)
- Alicea McDaid (Cruse)
- Anne McGarrigle (Foyle Bereaved Family Rep)
- Brian Rodgers (SPLK Forum – Bereaved Family Rep)
- Caroline Ferguson (New Horizons)
The membership will be restricted to the number deemed suitable to carry out tasks required, given that a smaller group potentially could be more able to progress the work forward.
D. Meetings and Structure
The Strategy Implementation Group should meet initially on a monthly basis. Sub-groups will have been established, as has deemed appropriate to take forward the work of the group.
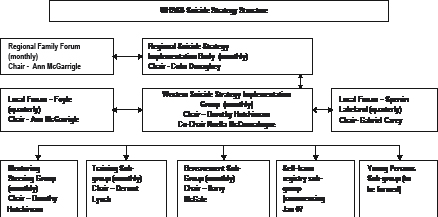
E. Decisions on funding
The accountability and responsibility for all funding remains with the WHSSB or any structure in place after the implementation of RPA. This is non-negotiable and the forum will be required to ensure that any funding allocation process is taken in accordance with all financial control procedures exercised by WHSSB. All funding proposals should be presented for approval at the Boards SMT and Social Care Committee.
It is envisaged that the WSSIG will have a key role to play in the decision-making process on the allocation of funding and subsequent selection process. The WSSIG will also be responsible for the monitoring of funding allocated to its geographical
jurisdiction and ensuring effective and efficient use of public moneys in the terms of the NI Suicide Prevention Strategy.
1. Recurrent Investment Plan – 2007 / 2008
A number of recurrent investment proposals have been agreed.
1.1 Re-configuration of Current Suicide Service Provision
Considerable learning has emanated from the recent suicide clusters both in the west and other areas of NI. This coupled with additional funding has provoked rethinking of the total service provision. Demand has increased to support postvention to families and communities bereaved by suicide. It has led to a mobilisation of the elected representatives particularly in the Derry City Council Area where agreement has been reached to develop a Community Response Plan incorporating a wide range of stakeholders across agencies and society as a whole.
The commissioner, the WHSSB, requires a change in service provision based on the assessment of need and the lessons learned. Other models of provision have been researched internationally and consideration has been given to the Baton Rouge model from Louisiana, USA.
Within the statutory sector there are currently two officers employed as Suicide Awareness Coordinators based in the Health Promotion Department in WHSCT. Their role has developed over the past few years and a greater emphasis has been placed on supporting families and communities who have suffered as a result of a suicide(s). The commissioner now proposes the WHSCT refocuses this provision to place the emphasis on postvention support.
At the Board’s request the Trust has established a working group chaired by Dr. Maura O’Neill to give consideration to this service redesign. The group has been working on a service redesign based on remodelling of the 2 Suicide Awareness Officers into Bereaved Family Support Officers. Those bereaved by suicide are extremely vulnerable and a high-risk group and therefore a priority for support within the strategy. The HR Department and the line manager are involved in the change and the officers have been consulted and are in agreement with the proposed amendment.
This service redesign will ensure that the Western area is well placed to meet the following objectives as outlined within the Protect Life Strategy, which identifies both a population and targeted approach
- Population Approach– seeks to tackle suicide in a wider context whereas
- Targeted approach – seeks to tackle the issue by focussing action on those who are most at risk.
The objective of this reconfiguration is to ensure that accessible information and timely support, both at community, voluntary and statutory level is available to all those bereaved by suicide at to encourage the development of support groups/networks.
Cost = nil
Timescale =Short to medium term
1.2 Re-launch the Integrated Community Delivery Programme
The previous Tender for these services received no applications from the voluntary and community sector despite active interest. Further consideration has been given to the proposal with both the WSSIG and a joint group of Board and Trust officers. It has been agreed to redesign this proposal to incorporate a Community Development Officer for the western area whose role it will be to develop programmes to target young people in the first instance, on the outcomes identified within the Target Youth Subgroup and the youth planning day scheduled for September 07. This post will be integral in supporting the Community and Voluntary Sectors to work closer together and to develop the crucial interface with the Statutory Sector. The post will incorporate such projects as Teen Scene, The Edge Project and Getting it Together into the overall programme.
It is proposed to re-advertise the programme again based on the agreed changes. There will be a requirement to hold an information meeting with C&V sector organisations that deliver services in the field of mental health promotion and suicide prevention to increase an understanding of the process and encourage collaboration.
Total costs = £98,000 pa
This approach will address the following objectives under the population approach.
Action Area - Communities- to support and encourage the development of community based suicide prevention initiative and support mechanism within the short term.
Action Area - Health & Social Services – to develop enhanced linkages between Health & Social Services and the Community and Voluntary counselling and support network particularly in relation to transition services and to bridge any gaps in service provision within the medium term.
Timescale = short to medium term
1.3 Commission a specialist counselling service provision for those bereaved by suicide
It is proposed to commission an additional service specifically targeting those in need of counselling who have been bereaved by suicide. Funding will be provided to the Western Trust to commission this service.
This initiative comes under the targeted approach objective bereaved by suicide. The objective is to ensure that accessible information and timely support, both at community, voluntary and statutory level is available to all those bereaved by suicide at to encourage the development of support groups/networks.
Timescale – short to medium
Cost - £20,000
1.4 Mental Health & Debt
Under non-recurrent funding in 2006/07 a pilot project working with those who have a mental health problem and in debt was piloted with New Horizons. An evaluation of the project was completed and there was evidence of significant improvements in client’s ability to articulate their emotions, money management and address issue of debt. The recommendation of the report was that the training and support programme should be rolled out to other service providers and those who support individuals who have mental health problems. It is proposed to do this for a further year and evaluate outcomes and the end with the intention of mainstreaming the service if considered appropriate.
This funding will be used to address the targeted approach area of marginalised and disadvantaged groups where the objective states, “to ensure that appropriate support services reach out to all marginalised and disadvantage groups …… those people who are economically deprived”.
Cost = £10,000
Timescale = Short to medium
1.5 Development of a Strategy Liaison Officer
An integral part of the redesign will be to provide a whole system approach to such a complex issue. It is proposed to develop the above post to compliment the work of the Bereaved Family Support Officers.
One of the key challenges within the Suicide Prevention Strategy is the need to ensure that we link the various strategies together to address the issue of suicide and this will be the fundamental role of this post.
It is suggested that this new post should be based in Health Promotion Department of the Trust. The post holder will have the responsibility of linking the Mental Health Promotion & Suicide Strategies with other key internal strategies such as drugs and alcohol, sexual health etc and external strategies such as poverty and neighbourhood renewal.
A key role of the post will be development and training so that capacity will be released from the existing roles of the Suicide Awareness Co-ordinators to facilitate the redesign. (Outline of proposed job role and function on appendix 2).
This initiative meets with the Guiding Principles of the strategy 1.1 developing links to other strategies.
Cost = £37,000 (FYE)
Timescale = Short to medium term
1.6 Additional Support to Reduce the Risk for those who Self-Harm
Another highly vulnerable group at risk of suicide are those known to the service and who have been treated in an acute setting for the results of self-harm and are then discharged or have been treated in A&E before returning home. A psychosocial assessment takes place prior to discharge but often the patient is still under the influence of alcohol or drugs. It is recognised this may not be in the most ideal environment for assessment and or to give help. It has been proposed to have a follow up assessment for those patients who have not received a referral to statutory services or who indeed have left hospital without any initial assessment having been completed. This additional service would be established in the Erne and in Altnagelvin Hospitals. It is proposed to build the capacity within the Primary Care Response Teams to enable them to take this work forward.
This service will address the objective under the targeted approach within the area of self-harm to ensure that responsive self-harm support services are in place in all Health and Social Services Trusts.
It will also support the implementation of programmes that enhance the coping and problem-solving skills of those who self-harm and which reduce the risk of repeat self harm.
Cost = £45,000 pa
Timescale = Short to medium term
2. Non-recurrent Investment Plan
No. |
Organisation |
Project |
Cost |
2.1 |
WHSSB |
Database on suicides among people known to services - 4 month research project to identify trends |
£12,500 |
2.2 |
WHSSB |
Community Grants Scheme |
£35,000 |
2.3 |
CRUSE |
Training programme for volunteers on suicide awareness, anger management, stress management for self and clients Volunteer training to increase number of volunteers and reduce waiting times |
£6,000 £8,000 |
2.4 |
Fermanagh New Horizons |
Training Motivational Interviewing Training Arts Project |
£600 £1,400 £4,000 |
2.5 |
ZEST |
Additional counselling hours to reduce waiting lists Distribution of leaflets and fliers to advertise the service |
£8,000 £5,000 |
2.6 |
ZEST |
Complementary Therapies |
£3,500 |
2.7 |
IFH/HAZ |
Debt and Suicide Research |
£15,000 |
2.8 |
Health Promotion Department |
Hope and Healing Conference – February 2008, Fermanagh Winston’s Wish Training |
£10,000 £5,000 |
2.9 |
PATHS Bereavement Group |
Fast Track Counselling |
£2,000 |
2.10 |
Taxi Watch Project |
Equip and train taxis / drivers in life saving equipment |
£2,000 |
2.11 |
Foyle, Search & Rescue |
Life Boat Advertise for volunteers Equipment |
£15,000 £4,500 £6,500 |
2.12 |
IFH/HAZ |
Mental Health and Debt Research |
£15,000 |
2.13 |
Oak Healthy Living Centre |
Targeting Youth Suicide Awareness – music event |
£17,000 |
Total |
£190,000 |
||
3. Community Plan on Prevention/Containment of Possible Suicide Clusters
Based on a model of best practice from the Centre for Disease Control (CDC) in the USA a community led initiative is to be developed for the WHSSB area. The structure is similar to that of Emergency Planning and will be amended to take account of local structures and linkages. There is no identifiable cost in relation to this; the aim is about networking and collaboration.
This meets the population approach action area of Communities where the objective states, “to support and encourage the development of community based suicide prevention initiatives and support mechanisms.”
Cost = £5K
Timescale = short term
4. Performance Management
It is vital to be able to measure the extent to which the strategic aim of the Strategy has been met. To this end specific performance measurement targets have been suggested for the action areas. Overarching objectives have also been developed for both the Population and Targeted sections of the Regional Action Plan. The achievement of these targets/objectives will play a central role in the annual review of progress being made towards implementation of the Strategy.
The Western Suicide Implementation Group will undertake to develop a performance management framework in line with the Regional performance management framework, which reflects the proposals being taken forward in the West.
5. Conclusion
The outlined plan in this document has been discussed and approved by the WSSIG and a joint Board and Trust officer group for implementation. The plan addresses a strategic approach in terms of addressing service redesign and improvement on;
- Prevention/Mental Health Promotion
- Early Intervention
- Engagement in Primary Care and Statutory Services Provision
- Admission to Intensive Support/Acute admission
- Loss of Life.
The model also allows for ensuring that there is connectedness between each level in terms of the experience of the individual, service users and service providers. The process of monitoring the model will be through the WSSIG under the leadership of WHSSB or subsequent commissioning organisation.
The plan also provides for a process of spending in year slippage that can be targeted toward localities/geographies of high risk and individuals who are vulnerable. The Action Plan will address the core issues that contribute to a poor mental health and possible causal factors, which lead to in suicide.
Director,
Mental Health and Disability Services,
Northern Ireland Health and Social Care Trust
Promoting Mental Health Action Plan 07/08 -
Update on progress
Funding allocations still under assessment.
A number of gaps were identified in terms of the Promoting Mental Health Strategy, and actions were added into the action plan around these. The assessments of all the applications have not yet been completed but it is envisaged that they will be very soon.
Some of the projects/gaps in the action plan that it is hoped will be filled and taken forward are
- Work with black and ethnic minorities (Communication and creative arts workshops for black and ethnic minorities)
- Training for community members around mental health promotion / stress management etc.
Progress on actions to date -
Action 5.1 – Small Grants Scheme
- Continued support from NHSSB & Northern HSC Trust
- Feedback from Community Network Representatives.
Action 5.3 – Relaxation and time out for carers
- 27th September 2007 at Drummalis Retreat – Event for Carers from Ballymena/Antrim area, where there will be alternative therapies etc provided for the carers.
Action 5.4 – Homelessness Action Plan
- Eric Woods to feedback.
Action 5.6 – Condition Management Programme
- This is being delivered in the pilot areas of Newtownabbey, Ballymoney and Magherafelt. This service is to be rolled out to 9 jobs and benefits offices in Jan 08 with staff being recruited to deliver this.
Action 5.11 – Mid Glens Pilot
- Started up by SHPO, Causeway and is now being taking forward by Cushendall Development Group and the local pharmacist in Cushendall. A steering group is being formed with representation also from Investing for Health, Community Involvement Project Worker. A luncheon club is to commence for older people in the autumn.
Action 5.14 – Online CBT programme.
- Living life to the full online programme has been launched.
Action 5.15 (B) Information for older/vulnerable patients on discharge from hospital
- Leaflets / posters have been distributed around 5 hospital sites. Also staff and ward managers have been spoken to regarding the “Good Morning” Service
- 75 questionnaires have been sent out to various ward Departments and other organisations
Action 6.2 - Dementia Conference
- This conference is for statutory, voluntary and community representatives – 11th October, Ross Park Hotel, Kells.
- Aims of the conferences – To raise awareness of dementia / to provide info about aspects of dementia care / To showcase good practice initiatives
Action 7.2 – Physical Activity
- All Active Ageing Co-ordinators have been appointed except for Cookstown
Action 10.2 – Staff Health and Well-being strategy within the Causeway Locality
- Discussions are underway within the Trust at Senior Management level in terms of this action and the organisation of a seminar/workshop.
Action 10.3 – Northern Trust Health and Well-being initiative
- New group is being established at present / in planning stages
Action 10.4 – Stress Seminar
- Exploring practical workplace solutions – The Glenavon Hotel, Cookstown – 21st June
- 68 attendees including speakers and support.
- Presentations are available from the Investing for Health website
- Future steps around this are to be discussed by the planning group in the near future. Recommendations to be addressed
Action 14.2 – Health Promoting Activities for Mental Health staff and service users within the Causeway locality
- An interactive health and well-being day took place in July for Mental Health staff and service users, which was held in The Ross Thomson Unit. Evaluations have been positive to date.
Action 14.3 - Increasing mental health literacy with a focus on young people/educating general public
- Resilience through the lifespan presentation by Dorothy Rowe – 8th October 7pm, Recreation Hall, Holywell. Open to Statutory, voluntary and community individuals.
- Awareness of World Mental Health Day – article has been written around the promotion of positive mental health and will be circulated to all Trust staff.
- Article written to go into all local newspapers within the NHSSB area for World Mental Health day – to raise public awareness of mental health and provide simple steps/ educate the general public on how to protect their mental health.
- School Journal, which was developed in the South Of Ireland, is to be piloted in 2 schools within the NHSSB area, and it is hoped the pilot will involve evaluation involving the school children and links with VOYPIC. The journal Includes simple messages around protection and promotion of mental health – includes info on relationships, stress of exams, sexual health, drugs and alcohol, family, anger management, bullying etc. Links between CAMHS and Contact Youth.
- Discussions around the use of drama / creative arts to produce material around positive mental health for young people. It is hoped that young people will be consulted in the production of this material with links to CAMHS.
Action 14.5 – Joined up working between sexual health, smoking, drugs and alcohol action plans relating to mental health and risk taking behaviours
- Antrim Borough Council held a workshop on 19th June to present the findings of a research project that was carried out – “A health profile of young people in Antrim”. Presentations were given by SHPO (Sexual Health), Senior Drugs and Alcohol Co-ordinator, Tobacco Control Co-ordinator and the Commissioner for Health Promotion.
- From the event both mental health and suicide were identified as issues that need to be addressed. As a result a group has been formed comprising of Councillors, community workers, Health Promotion, PSNI, NEELB and Youth Justice, with the first meeting in October.
Action 14.6 – Positive Mental Health within University of Ulster
- 1 full program has been delivered to Careers staff within the University
- A Mental Health Training Programme has been agreed/developed and is commencing in October, both in the University of Ulster in Coleraine and Jordanstown. The programme is to be offered to all Student support staff, Mental Health Mentors and other interested academics.
Action 16.1 – Youth Justice needs assessment of staff and parents training requirements
- has been carried out and is currently awaiting approval from the steering committee.
Action 18.1 Parent/Teenagers Programme - Talking Teenagers training
- Training is being delivered in September and November – linked into Youth Justice. A section has been added around self-harm and one has yet to be added around sexual orientation.
- It is hoped there will be more courses delivered next year.
Action 20.1 Emotional Resilience work with young people - Bounce Training
- This new training promotes and supports the development of resilience in young people and covers issues such as developing self-esteem, drugs and alcohol misuse, avoiding negative outcomes, relationships and sexual health.
- 2 SHPO’s from Health Promotion will be undertaking the training for trainer’s course on1&2 October –It is envisaged that this course will be rolled out across the NHSSB area with 2 courses being delivered before the end of March.
Action 20.2 – Mindset Training
- Training that has been developed by Action Mental Health and addresses the issue of the stigma of mental illness among young people. It also raises awareness of the different mental health conditions, their signs and symptoms as well as looking at support services that are available.
- New links made with the University of Ulster as well as Greenmount and Loughry College in terms of offering the training.
- 2 sessions have been completed to date within University of Ulster, Jordanstown for students.
- 1 road show being held on World Mental Health Day in Greenmount College for students.
- Workshops for staff within FE Colleges in process of being arranged.
Action 22.1 Education and prevention programmes, Youth Justice
- ongoing in each of the 6 projects(Antrim, Ballymena, Coleraine, Magherafelt, Newtwonabbey, Larne) across the board area. Training is being provided to staff, young people and parents around drugs and alcohol. Training around mental health has been developed and dates for training are currently being organised.
Jayne McConaghie, SHPO, Mental Health
Northern HSC Trust, 17.09.07
Introduction
The Regional Promoting Mental Health Strategy and Action Plan was launched in 2003. The Strategy outlines an integrated approach, which addresses the wider determinants of mental health and focuses particularly on inequalities.
The Regional Promoting Mental Health Strategy and Action Plan is set within the Investing for Health Strategy framework and contributes to the achievement of the identified target of
‘To reduce the proportion of people with a potential psychiatric disorder (as measured by the GHQ 12 score) by a tenth by 2010.’
Below is an Action Plan setting out the identified priorities and actions to be taken forward 2007/08 by NIFHP partner organisations.
These have been identified in meetings with partners and key stakeholders and take account of local needs and issues.
It is intended to review this action plan on an annual basis and any comments or suggestions on the actions identified within it would be welcome.
Jayne McConaghie
Senior Health Promotion Officer, Mental Health
Homefirst Community Trust
Health Promotion Service
Spruce House
Cushendall Road
Ballymena
BT43 6HL
028 2563 5575
jayne.mcconaghie@homefirst.n-i.nhs.uk
Promoting Mental Health Strategy & Action Plan
Implementation Plan 2007/2008
Action Point |
Activity |
Lead |
Others Involved |
Timescale |
Intended |
Methods For Monitoring /Evaluating Activities |
Action 4 + 7 |
To develop the Active Ageing Project within the NHSSB area |
Physical Activity Co-ordinator SHPO (Older people) |
Physical Activity Project Workers |
2007/2008 |
Increased number of walking groups within the Northern Trust area |
Evaluation report |
Action 4 + 7 |
To provide a wide range of physical activity initiatives with a wide range of people within different settings |
Physical Activity Co-ordinator |
Statutory, community and voluntary organisations |
2007/2008 |
Improved physical activity levels Improved mental and emotional well-being Reduction in stress levels |
Evaluation reports |
Action 5 |
Develop policies promoting mental health (revisit after suicide prevention strategy and RPA roll out) |
H&SS Boards and Trusts |
Community and voluntary groups Trauma Counsellors Primary Care |
2008/2009 |
Specific policies and programmes |
Benchmark against Best Practice review of policy |
Action 5 |
To provide a wide range of activities to patients within Holywell Hospital as well as training for staff |
Joy Hammond (OT Services Manager, Homefirst) |
Artscare Local Councils FE Colleges Conservation Volunteers |
2007/2008 |
Smoking cessation brief Intervention delivered to patients Green Gym project delivered Breakfast Club delivered over 5 days and will be implemented in Ward 8, Whiteabbey Hospital Patients within Holywell provided with tai chi, aromatherapy and yoga Range of activities carried out with Artist in Residence as well as leisure groups Technical Instructor staff trained in Health for Life |
Evaluation |
Action 5 |
To provide a range of activities for individuals with mental health problems being supported in the community |
Joy Hammond (OT Services Manager) |
Conservation Volunteers Artscare Local Councils Occupational Therapy |
2007/2008 |
A fathers group will be set up in Magherafelt addressing parenting skills and health issues Green gym will be delivered Leisure groups will be delivered |
Evaluation reports |
Actions 5, 7 & 14 |
To continue to facilitate co-operative working where possible between this group and other partnerships such as NDACT, Trauma Advisory Panel, Neighbourhood Renewal, Northern Physical Activity Partnership, etc. |
NIFHP NHSSB |
All partners |
Ongoing |
Improved Communication sharing of resources and expertise Increased capacity among all partners to contribute to implementing Strategy |
|
Actions 5,7,14 |
To facilitate co-operative working between the various strategies e.g. Teenage Pregnancy and Sexual Health, Drugs and Alcohol and Smoking Cessation |
SHPO (Mental Health) |
SHPO (Sexual Health) Senior Drugs and Alcohol Co-ordinator Smoking Cessation Co-ordinator |
Ongoing |
Improved communication on sharing of expertise, information and resources |
|
Action 5 & 9 |
Continuation and further development of the Intergenerational “Mentoring Mothers Project” |
SHPO (Sexual Health) |
Homefirst Larne Community Care Centre Age Concern NI Youth Justice Agency Larne Parental Support Project |
2007/2008 |
Improved mental and emotional well being Creation of a support network for younger and older people Linkages created with young women attending “Just” Larne Project (joined up services and training) |
Age Concern NI developing evaluation tool |
Action 5 + 11 |
Facilitate a health and well-being event for the farming population |
SHPO (Older People) Homefirst |
Homefirst Causeway United Hospitals Ulster Farmer’s Union Statutory, voluntary and community sector IFHP NHSSB |
2007/2008 |
Increased health and wellbeing among the farming population addressing issues around mental health, smoking etc |
Evaluation and recommendation report |
Action 5+11 |
Distribution of newsletter “Farmers Friend” among rural population |
SHPO (Older People) Homefirst |
Homefirst Causeway United Hospitals Ulster Farmer’s Union Statutory, voluntary and community sector IFHP NHSSB |
2007/2008 |
Increased health and wellbeing among the farming population addressing issues around mental health, smoking etc |
Evaluation report |
Action 5 + 14 |
Raising awareness of “Good Morning Projects” |
Health Promoting Hospitals Co-ordinator (UHT) |
Statutory, voluntary and community organisations |
2007/2008 |
Increased awareness of the Good morning projects particularly by nursing staff in hospitals Increased uptake of referrals |
Ongoing evaluation |
Action 5 +14 |
Wide range of initiatives for older people both in community and hospital setting |
Health Promoting Hospitals Co-ordinator (UHT) |
Antrim Borough Council Age Concern CAB Nursing Over fifties forum |
2007/2008 |
Increased mental health, support and reduced isolation for this group |
Evaluations |
Action 6 |
Continued support for joint Causeway Trust/ Alzheimer’s Society Project to support carers (Recurrent funding from Causeway Trust and Commissioning team for older people NHSSB) |
Causeway Alzheimer’s Society |
NHSSB NIFHP |
2007/2008 |
Carers affected by dementia in Causeway area have access to information, support and practical assistance Carers skills developed to help them cope with needs of dementia patients and demands of family life |
Evaluation report |
Action 6 |
Delivery of PREP – Education programme for carers of individuals with severe mental illness |
CAUSE |
Mental Health professionals – Homefirst Trust |
2007/2008 |
Increased awareness about severe mental illness Awareness of coping strategies, problem solving, communication as well as symptom and medication management Ongoing carer support |
Evaluation report |
Action 6 |
Explore the possibility of facilitating a event around the issue of dementia for Trust staff |
SHPO (Older people) Homefirst |
Homefirst Alzheimer’s Society Carer’s NI |
2007/2008 |
Increased awareness of the issue Improved communication and sharing of expertise |
Full evaluation and recommendation report |
Action 6 |
Facilitate events for carers |
SHPO (Older People, Homefirst) |
Homefirst Statutory Community and Voluntary organisations |
2007/2008 |
Improved social support for carers Increased linkages and forms of support Increased awareness of importance of mental and emotional well-being |
Evaluation report |
Action 6 |
Explore the need for addressing the issues of Carers who look after individuals with Alzheimer’s within Homefirst area |
SHPO’s (Older People, Homefirst) |
Alzheimer’s Society Homefirst |
2007/2008 |
Appropriate support services identified Improved social support and reduced isolation for carers |
|
Action 6 |
Explore the possibility of establishing a multi-agency group to address the issue and raise awareness of post-natal depression as well as looking at resources |
SHPO(0-5) |
SHPO (Mental Health) Homefirst Health Visitors GP’s CPN’s Social Workers |
2007/2008 |
Increase awareness of post-natal depression Potentially improves support services and resources available |
|
Action 7 |
To provide social support and skills to rural and isolated older residents in the Mid-Glens Area –providing a 1year pilot of mental and physical health improvement activities acceptable to residents |
Geraldine McDonnell (SHPO, Causeway) |
Cushendall Development Group North Antrim Community Network SVDP Local Pharmacist BCPP |
2007/2008 |
Older people’s group established in the area Isolated older people will have access to social support and activities that will link them into the community |
|
Action 7 |
To improve the mental health of older people living in residential and nursing care through the pilot Health Promoting Care Home initiative |
Geraldine McDonnell (SHPO, Causeway) |
Trust Nursing Homes Private Sector nursing and residential care homes Voluntary sector |
2007/2008 |
Increased knowledge of, and access to existing HSC services among vulnerable remote residents Local activities funded and sustainability potential identified Local Health Promoting Care Home Implemented Mental Health Promotion Principles and activities highlighted within pilot Mental Health Promotion Standards |
|
Action 7 |
Service Providers to have Mental Health Promotion Policy (revisit after suicide prevention strategy and RPA roll out) |
H&SS Boards and Trusts |
Service Providers |
2008/2009 |
Specific policies |
Benchmark against Best Practice review of policy |
Action Point 7 |
Range of activities within Homefirst Trust for the older population – Reminiscence, Falls Training & Home Safety |
SHPOs (Older people) Homefirst |
Voluntary organisation Older people’s groups Day Care Staff |
2007/2008 |
Improved mental and emotional well being |
Evaluation report |
Action Point 10 |
Development of a staff health and well-being group to include - Exploring the development of a wellbeing at work policy - Delivery of stress management training to both managers and staff on the ground - working towards the HSE Stress Management standards |
SHPO (Mental Health) SHPO (Primary Care) |
Homefirst Trust Health &Safety MDTU , Holywell Human Resources Occupational Health |
2007/2008 |
Development of a Wellbeing at work policy Health needs identified within Trust Increased awareness of stress and the management of the same |
Training evaluations |
Action 10 |
To provide stress management workshops for managers and staff (linked to above action) |
SHPO (Mental Health and 0-5) Homefirst |
Homefirst Community Trust HR Occupational Health |
2007/2008 |
Improved knowledge and skills of staff |
Staff evaluation forms |
Action 10 |
Delivery of balanced lifestyle training |
Health Promotion Manager (UHT) |
United Hospitals staff |
2007/2008 |
Improved knowledge and skills of staff |
Training evaluation forms |
Action 10 |
To continue to seek ways to reduce stress within the workplace across Causeway Trust area |
Geraldine McDonnell (SHPO, Causeway) |
Carecall |
2007/2008 |
Measures to reduce staff stress implemented |
Evaluation |
Action Point 10 |
Facilitation of a seminar around workplace stress |
Northern Group Systems |
NIFHP WIFHP SHPO (Mental Health) Voluntary, Statutory, Community and private organisations |
June 07 |
Increased awareness of stress as a workplace health issue Increased awareness of models of good practice |
Evaluation and recommendation report written |
Action 13, 14 + 20 |
Raising awareness and education of general public around positive mental health and surrounding issues with particular focus on young people |
SHPO (Mental Health) CAMHS |
Homefirst Trust Statutory, Voluntary and Community organisations Youth Service |
2007/2008 |
Increased awareness of positive mental health and mental health issues with the general public Production of material relevant to age group around the issue of positive mental health |
|
Action 14 |
Review of current directories of mental health services – consider feasibility of combining existing directories |
Promoting Mental Health Strategy Implementation group |
Homefirst Causeway |
2007/2008 |
Updated information on support services amalgamated in one document ???? |
|
Action 14 |
Map existing referral pathways for young offenders to support staff in their referral to agencies which can provide support around mental health |
SHPO (Drug and Alcohol Programme) |
SHPO (Mental Health) YJANI Statutory, community and voluntary organisations |
2007/2008 |
Concise information on support services Development of new referral pathways to specialist services |
|
Action 15 |
Continue to work in partnership with Education and Library Board to compliment aspects of the revised curriculum which focuses on promoting emotional health and well-being by addressing the issue within the context of a healthy school. |
NIFHP NEELB |
SHPO (Schools) |
2007/2008 |
Education and Library Board more actively involved in implementing Strategy |
ELBs |
Action 15 |
Implementation group to meet quarterly with regular information sharing |
Implementation group NHSSB IFH SHPO (Mental Health) Suicide Prevention Co-ordinator |
. | 2007/2008 |
Improved communication and information sharing Minutes of regional meetings to be distributed among group Relevant info regarding training opportunities to be distributed Representation of group reviewed and extended |
|
Action 15+21 |
Facilitate “Open your mind” public speaking initiative within schools |
SHPO (Schools) |
SHPO (Mental Health) NEELB |
2007/2008 |
Increased awareness of mental health issues among school children Increased awareness also amongst teaching staff Stigma of mental illness etc addressed and removed |
Evaluation report |
Action 16 + 18 |
Needs assessment around training requirements for young people aged 10-17 who are offenders or are at risk of offending as well as staff and parents |
SHPO (Alcohol and Drugs Programme) |
YJANI Statutory, voluntary and community organisations SHPO (Sexual Health and Mental Health) |
2007/2008 |
Needs identified |
|
Action 18 Education/Training (Youth) |
Improving parenting skills Parent / Teenagers programme |
SHPO (Sexual Health) |
ACET Statutory, community and voluntary organisations |
2007/2008 |
Delivery of 2 training sessions Increased awareness of parenting skills Self-harm and sexual orientation information/sections added to resource pack |
Training evaluation report |
Action 20 |
Emotional Resilience work with young people – Bounce Training programme |
SHPO (Sexual Health) |
SHPO (Mental Health) HAZ Statutory, community and voluntary organisations |
2007/2008 |
2 Trainers trained Delivery of 2 training sessions Increased awareness of issues among staff who work with young people |
Evaluation report |
Actions 20 & 21 |
Delivery of programmes within FE setting around mental health – e.g.Mindset / Balanced Lifestyle Training |
SHPO (Mental Health) Action Mental Health |
Homefirst Trust Causeway Trust FE, HE, SELB & NEELB |
2007/2008 |
Promotion of improved mental and emotional well being of young people and staff through training. Increase awareness and equip staff groups with the ability to support young people presenting with issues more effectively |
Evaluation report |
Action 22 |
Delivery of health promotion and management programmes for young people in Youth Justice Agency Community Projects as well as the staff that work with them and parenting skills etc for their parents |
SHPO (Alcohol and Drugs) |
SHPO (Sexual Health, Mental Health) |
2007/2008 |
Increased awareness among these particular groups of issues such as drugs/alcohol, mental health and sexual health Reduced levels of substance misuse of young people in Community projects Increased parenting support skills |
Ongoing evaluation |
Actions 21-30 Suicide Prevention & awareness (See separate Suicide Strategy action plan) |
Suicide Prevention Co-ordinator |
Department of Agriculture and Rural Development
Director of Social Services, Family
and Child Care Belfast Health and
Social Care Trust
I refer to your recent correspondence in relation to the above and understand that a response has been submitted from the Belfast Trust.
I wish to provide you now with comments in relation to the current strategic approach to the prevention of suicide and self-harm from a Child and Adolescent Mental Health Services perspective.
Assess the scope and appropriateness of the DHSSPS Strategy “Protect Life A Shared Vision
The Trust is supportive of the recommendations within this strategy, particularly the emphasis on prevention and early intervention. The focus of this strategy on building resilience and developing protective factors for children, young people their families and of local communities is critical in improving mental health and emotional well-being.
It is clear the protect life strategy provided a platform for action and has helped to facilitated the development of a more joined up approach in tackling issues of self-harm and suicide.
It is the Trust’s view that the Bamford recommendations, in particular those outlined in “Building a Comprehensive Child and Adolescent Mental Health Services”, “Promoting Mental Health and well-being a Personal, Public and Political Issue”, and “Alcohol and Substance Misuse” frameworks complement all of the recommendations captured within the Protect life Strategy. These strategies should therefore act as the catalyst for change across Education, Health and Social Services, Juvenile Justice and within the Community and Voluntary sectors. It is critically important that actions associated with the implementation of the Protect life Strategy and the Bamford review are joined across all these sectors. This will require cross-departmental planning and leadership
It is also the Trusts view that the scope of these reports, if fully resourced and implemented will contribute significantly to improving mental health and emotional well being within families and local communities.
Stakeholder Involvement
It is the Trust’s view that the development process of the Protect Life Strategy was an example of effective stakeholder involvement across the statutory, community, and voluntary sectors. In taking forward future action in relation to promoting good mental health and emotional wellbeing it is essential that young people should be proactively involved at all levels of implementation.
The Trust also recognises the value of the Investing for Health Partnerships and their Mental Health and Emotional wellbeing Communities of Interest as a vehicle for developing local action.
Whilst at an early stage of development most of these Communities of Interest have established a number of sub-groups specifically focused on prevention of self-harm/suicide and on the needs young people. Currently within Belfast this forum has commissioned a mapping exercise of all statutory, community and voluntary sector activity associated with promoting mental health and emotional wellbeing. These forums if properly resourced have the potential of delivering partnership-based approaches in addressing mental health and emotional well being at local community level.
Level of services, support available to promote good mental health to prevent suicide and self-harm; and to support those affected by suicide and Consider what further action is required, taking account as appropriate of experience elsewhere
The Trust recognises that whilst some progress has been made in developing a range of services designed to promote good mental health and prevent suicide and self-harm that further co-ordination and resourcing is required to make the objectives outlined in the strategy a comprehensive reality.
The Trust welcomes the development of counselling in school initiative currently provided by Contact Youth. This development is important in the context of providing early detection and intervention. The Trust also supports the development of the new personal development curriculum in schools designed to develop emotional intelligence in our young people.
The Trust strongly supports the Assist training programme, (First Aid Training in the Prevention of Self harm/Suicide), however we believe this needs to be rolled out for all front line care staff that work with vulnerable young people. This is particularly important for General Practice, Accident and Emergency and in social services.
The provision and potential extension of the 24-hour help line provides an important and accessible contact in providing an initial crisis response. The Trust recognises the value that such a helpline can play in containing and preventing self-harm.
The Trust is planning to develop closer links between the providers of the help line and our Child and Adolescent Mental Health Crisis Assessment service.
The Trust under the Secretary of State’s Children and Young Person funding package has developed a Crisis Assessment and Intervention Service known as CAIT. This service is focused on children and young people who are at risk due to a significant mental health presentation in and out of hours. Eight experienced practitioners will be appointed supported by CAMHS Consultants. They will be available to assess, provide consultation, and formulate treatment plans for the management of young people who present to primary care and A&E departments. It is anticipated that the service will be provided incrementally from November 2007. The service will enable emergency response in-hours and will also provide next day assessment for young people with mental health needs including Weekends and Bank holidays between the hours of 8am and 2pm.
The Trust believes that children and young people in crisis need a range of well co-ordinated responses at both community and health and social care levels.
Based on the work of the Thomas Coram Research Institute (University of London) into CAMHS Crisis Out of hours arrangements, the Trust supports the view that one of the most effective models for crisis intervention in respect of young people, is to ensure that front line services such as GP’s Accident and Emergency staff, and emergency social work services are well trained in assessing, managing and containing initial presentation of self harm, backed up by a robust specialist CAMHS next day assessment service. The Trust is working with the EHSSB in establishing the most effective model to achieve this.
In June 2007 the EHSSB has commissioned the Belfast Trust to provide all of specialist CAMHS across the Eastern Board area. This decision was made to overcome organisational and services boundaries, and brings together all of the five CAMHS providers across the EHSSB area under a single management structure. This will also:
- Improve the overall planning and delivery of CAMHS
- Enable the streamlining and integration of CAMHS care services
- Facilitate the targeting of specialist CAMHS resources to those young people must in need.
The Trust also considers that it is essential to create the capacity for specialist CAMHS clinicians to outreach into Primary care, Education, Social Services. This outreach support should be targeted at young people in need, particularly those children and young people in the looked after care system and Juvenile Justice systems. It is well recognised now that our Looked After Children/Youth Justice population perform much less well than their peers in terms of their emotional, social and cognitive development, educational achievement, their career opportunities and the security of the intimate relationships they develop. Unfortunately this is one of the highest risk populations for self-harming and suicidal behaviour.
Whilst, this outreach objective is worth pursuing, it should be noted this is made difficult by the current lack of capacity within specialist CAMHS. This is due to primarily to the under resourcing of specialist CAMHS services. To illustrate this point, The Royal College Psychiatrists (England) in their paper “Building and Sustaining Specialist CAMHS” recommend that specialist CAMHS services, as a minimum requires 15 (non-teaching) to 20 clinicians per 100,000 total populations up to 16th birthday. The English National Service Framework for Children and Young People and the Bamford review “A Comprehensive CAMHS ”has also adopted these recommendations.
This review estimates that in Northern Ireland specialist CAMHS requires between 20 and 25 whole time equivalents staff per 100,0000 population. This they argue is particularly important in creating the capacity within CAMHS to undertake outreach work. This is critical in addressing the needs of children and young people who self harm.
In EHSSB Board terms this would require between 100 to 134 full time staff working in specialist CAMHS. Currently there are approximately 37 whole time equivalent staff are working in core community CAMHS, although this will rise to 52 upon the appointment of the additional specialist posts. However, even by counting the limited range of designated mental health tier 2 services such as those provided in Family Centres, Adolescent Teams, Primary Mental Health Workers there remains a significant shortfall when set against this benchmark.
It is important to note that this is an average and when applied to Northern Ireland would need to take the following factors into account:-
- That the age standardised population of children and young people in Northern Ireland is approximately 4%.
- Northern Ireland has higher levels of socio-economic deprivation and the correlation between deprivation and poor mental health is well established.
- Mental Health needs in Northern Ireland are estimated to be higher than that of the England. The Chief Medical Officer’s report “Health of the Public in Northern Ireland” estimates that more than 20% of young people have suffered significant mental health problems by their 18th birthday. In Eastern Board terms this would mean an estimated 31,336 young people experiencing a significant mental problem at some time. Most of these will not be treated by CAMHS, but managed within primary care.
- CAMHS in Northern Ireland are provided up to 18 years old as opposed to 16 years. Bamford also recognise that young people between 16-18 require double the resources of young people 0-15.
- A recent snap shot analysis of CAMHS case loads shows that between 10-13 % of CAMHS work involve the provision of care to young people with self-harming presentations. This is significantly higher than some English levels of 1-3%. In addition the CAMHS clinician group argues that many of the referrals presenting within CAMHS have co-morbidities (21%) in that the young people present with more than one mental health need. As a consequence their needs are more complex and require more intensive treatment.
The Irish College of Psychiatrists also make a number of recommendations in relation CAMHS provision for a total population. Their recommendations on staff levels tend to be higher than the levels recommended in the UK. This they argue is more reflective of the mental health needs of children and young people in Ireland.
There is also a clear need to develop primary mental health work focused on early detection, assessment and treatment for young people with mental health needs
The Trust recognises that the constituents of good mental health are developed within the context of the family and therefore as recommended in Bamford, there is a need to develop infant mental health approaches as a integral part of any prevention strategy. In respect of infant mental health the literature and research base on the link between psychological resilience and the quality of attachment relationships formed in the first years of life is now so well established that it cannot be ignored in any discussion of psychological vulnerability in later life, i.e. in adolescence and adulthood. The understanding of attachment theory, combined with the research discoveries in developmental psychology, has led to the development of Infant Mental Health services in the USA, in Scandinavia, in other parts of Western Europe and in Great Britain. The Scottish Executive, for example, has appointed a full-time worker to develop Infant Mental Health Services. Here in Ireland whilst we are now recognising the importance of the infant mental health we have not yet organised services in any adequate way to respond to this.
It is also clear that further investment is needed in tackling drug and alcohol problems among young people. Currently in Northern Ireland there are a limited range of specialist services for young people with both alcohol and mental health needs
It is important to reflect the valuable contribution the community and voluntary sector make in addressing the mental health and emotional wellbeing needs of children. However such organisations struggle year-to-year due to the non-recurring allocation of resources. This needs to be addressed as part of a whole systems approach in order to produce stability and continuity of services.
Currently the Trust and the EHSSB within the context of the Project Board charged with making improvement in Child and Adolescent Mental Health (CAMHS) is investigating the need for a specific crisis service for Adolescents and young people at risk of suicide, (such an (recommendation 7.4 of the independent review panel). The review will include:
- Seeking to establish the current levels of self-harm by young people. This will involve collecting available data from hospitals, G.P out of hours and other sources such as the self-harm audit carried out at the Mater Hospital.
- Considering the impact of the Telephone helpline funded by the Protect Life Strategy and is to be rolled out across Northern Ireland could play in providing initial crisis response
- Considering the mentoring service in the WHSSB area again funded from the Protect Life Strategy and how it could contribute to supporting young people at risk
- Looking at models of service elsewhere, for example the recent study undertaken by the Thomas Coram Research Unit. This study describes a number of models in relation to out of hours crisis CAMHS services.
- Considering how existing out of hours services could contribute to the provision of a crisis service for example the Adult Mental Health Crisis Response/Home Treatment Services and Emergency Duty Social Services, G.P Out of Hours provision and the role of the current CAMHS Inpatient Services out of hour’s rota.
It is anticipated the Trust in partnership with the EHSSB will conclude this work and have produce a plan for a crisis service early in December 2007.
The Trust would also point the committee to a number of reports that may be helpful in their deliberations:-
1. National Suicide Research Foundation who compiled the Republic of Ireland Register of deliberate self harm “National Register of Deliberate Self Harm Annual Report 2005”. This report details both attendance at A&E departments and Hospital admissions and captures data relating to all ages ranges. Currently there is no Northern Ireland equivalent. However the EHSSB have recently undertaken an analysis of hospitals systems and have identified the number of young people who have attempt self harm. This has been submitted to the Committee by the EHSSB.
2. The Trust would recommend that in the longer term such a register be commissioned, alongside the development of a Child and Adolescent Mental Health Mapping exercise, similar to the UK CAMHS Mapping process conducted by Durham University on behalf of the Department of Health England.
3. UK National Statistics Agency 2001 report “Children and Adolescents who try to harm, hurt or kill themselves”. This report is further analysis from the national survey of the mental health of children and adolescent in Great Britain in 1999. The report presents prevalence rates of self-harm among children and adolescents aged 5-15 in England, Scotland and Wales during the first half of 1999.
4. The Royal Australian and New Zealand College of Psychiatrist 2000 Guidelines for the Management of Deliberate self harm in young people. This guidance recommends a range of approaches to the management of self-harm in Accident and Emergency Departments.
5. NHS National Institute for Clinical Excellence Quick reference guide on Self Harm “The short-term physical and psychological management of self harm in primary and secondary care.
In Conclusion
In addressing self-harm and suicide, research indicates that mental health and emotional wellbeing needs to be promoted across 3 core components;
1. Primary Prevention – this involves the development of strategies, which strengthen families through effective parenting and working in partnership with education in developing emotional health in young people. Importantly there is also a need to reduce stigma by raising awareness of mental health.
2. Early Intervention – This involves targeting support and resources at those young people at risk through developing strategies, which deliver earlier intervention.
3. Rehabilitation – this involves effective crisis intervention and the development of psychological/family therapies to enable young people and their families to resolve and develop protective factors in addressing their psychological and emotional needs.
The Trust would urge the committee to advocate for additional resources to be made available to address the recommendations of the Bamford review and any subsequent service frameworks. There is also a need to ensure action is thoroughly joined up and embedded with action of the “Protect Life Strategy”.
I trust you will find these comments helpful.
NIACRO
1. Introduction
1.1 NIACRO welcomes the opportunity to respond to the new policy on Self Harm and Suicide Prevention management. As a voluntary organisation working closely with partners in the Criminal Justice System and particularly with the Northern Ireland Prison Service (NIPS), we place a high value on consultation and discussion.
1.2 NIACRO has experience of working with prisoners in all of the establishments in Northern Ireland and provides services to prisoners, ex-prisoners and their families.
2. The Policy
2.1 NIACRO welcomes the NIPS policy on Self Harm and Suicide Prevention Management policy document. It is a thorough and useful document which will hopefully be of great benefit to staff, prisoners and their families.
2.2 We would like to make a number of observations and highlight areas where clarification would be helpful to ensure that the policy and procedure are effective.
2.3 NIACRO believes that persons suffering from Mental Ill Health should be screened at the point of arrest in order to ensure the earliest detection of concerns. While several such schemes have operated in the past, we are not sure what the current practice is or whether it is consistent across police stations. It will be important in order to support the provision of an effective and consistent service that Forensic Medical Officers who attend police stations and the PSNI are aware of this policy and how the information they hold on at-risk prisoners is fed into the system.
3. Section One - Intervention
3.1 A prisoner who needs outside clinical intervention. It may be useful for NIPS or the individual establishments to have made arrangements for how that service will be provided to the prisoner. For example, it would be helpful to have a specifically named psychiatrist or a community psychiatric nurse who would work with Healthcare staff in providing a specialist clinical service to prisoners identified. The local Health and Social Services Trusts or Boards could be involved in discussion at this early stage about their willingness to allocate named staff to work with the prisons on this issue.
3.2 The prison regime will need to be flexible and modify their management of an individual while they are undergoing treatment or the treatment may not be effective. The specific effects of treatment should be clearly stated on the care plan for the prisoner and all staff made aware of the need for special support and intervention.
3.3 We would recommend that the section on support from persons outside the prison is strengthened to include families, friends and significant others, for example, previous support worker or counsellor may have a real role to play in helping the prisoner through a crisis. Confidentiality for the prisoner is important but it is also an essential element of recovery from mental ill health that those people who are important in the prisoner’s life can play a role in reassuring, supporting and showing love and concern for them. It is extremely important therefore, at the initial reception interview that the prisoner is asked who the people are that they rely on for support and who they would want contacted if they were to have a crisis while in prison. That information should be easily accessible on the PAR1 and the Residential Manager would then inform those named outside the prison in the event of a crisis.
3.4 The section on regime opportunities could be strengthened as it is important that a care plan agreed for a prisoner to address a crisis is implemented and an integral part of that plan for example, may be purposeful activities, telephone contact with family, friends, increased visits and a reduction in isolation in their cell as far as possible. The quality and consistency of the regime operating in the prison will have a major supportive effect on prisoners in crisis as well as raising the morale of prisoners and staff generally.
3.5 The training offered to the Suicide Prevention Team and key staff should include specific training on mental health issues, clinical interventions and managing risk of suicide and self harm and be provided by psychiatric staff with an expertise in this area.
4. Section Two – Roles and Responsibilities.
4.1 Managers will support staff involved in incidents of self harm or suicide. It may be beneficial to specify what that support will entail. NIACRO believes that following traumatic incidents, staff should be offered at least two sessions with a qualified independent counsellor to talk through what has happened and the impact it has had on them, this could be provided through Occupational Health Services. By stipulating a minimum level of support, rather than leaving staff to opt or not for support has the longer term potential to impact positively on staff sickness levels.
4.2 Individual managers will also offer at least one debriefing session to prison staff where issues such as their responsibilities for reports, attendance at case conferences, police interviews etc., can be discussed. This is a different focus than 4.1 above but should also be offered in a supportive, understanding manner.
4.3 Prison officers will be expected to offer maximum contact and support to a prisoner thought to be at risk. See 3.3 above, the regime in the prison will need to ensure that the prison officer is able to fulfil this important function for prisoners at risk.
4.4 Training and support should be available to all who will be asked to support a prisoner at risk. This should include specialist mental health training and support. As part of induction they should be advised who to speak to within the internal Healthcare staff, external psychiatric support available and those other prison staff who have received enhanced training in the area of mental health, followed then by formal training.
4.5 Support for prisoners who are living alongside the prisoner at risk or following an incident is important. The support should include individual sessions with a trained independent counsellor and group work can also be an effective method of helping prisoners voice their concerns and support for each other.
4.6 Probation Officers role could also include the passing of information to families where that is agreed with the prisoner. Probation Officers can also inform other agencies working with the family in the community if agreed, so that the partner and family receive support during a crisis period. It is an extremely difficult experience for a family who are aware that someone may be at risk of suicide and self harm given their lack of face to face contact with their loved one and they may feel very powerless. The case conference should consider how families can be an integral part of the support package for the prisoner while in prison as well as part of their resettlement plan.
4.7 Involvement in resettlement planning can be a very positive experience for a prisoner who may be suffering from mental ill health giving them hope for the future and something to plan for. Therefore, the implementation of Resettlement planning across the prison estate will be very beneficial in supporting this policy.
4.8 There is no reference to other staff in the prison such as NIACRO project workers, visitor centre staff, gym and leisure staff, drug and alcohol project staff etc., from the voluntary and independent sector. It is essential that these staff are also aware of the Policy and are involved in training regarding its use and implementation. They may be an important source of referrals and information alongside Education and Vocational Training staff. They may also be an important source of support in the care plan for prisoners at risk or in crisis.
4.9 It may be useful to consider having a member of the voluntary sector project staff on the Self Harm and Suicide Prevention Group both to ensure good communication on prisoners at risk or in crisis within the prison and to add value to the formulation of support for the prisoner on release within their resettlement plan.
4.10 NIACRO welcome the fact that the Self Harm and Suicide Prevention Co-Ordinator will have the role of compiling monthly statistical reports and would request that information on Self Harm and Suicide issues be included in the regular report received from NIPS in the weekly situation report.
5. Section Three – Risk Assessment
5.1 The reception officers must ensure that details of family members and significant others are available on the prisoners file and that they are specifically asked who they would want contacted if a crisis or emergency situation arose.
5.2 The Healthcare staff that are completing the health screening form or the Medical Officer need to ascertain the details of important persons in the previous support and treatment of the prisoner and ensure they are written onto the file.
5.3 It is important that reception and healthcare staff have appropriate training in the area of mental health and management of risk and access to specialist psychiatric professionals as necessary.
5.4 Where a PAR1 is raised the details of who the prisoner has agreed should be contacted as support to him/her must be written onto the form and the Residential Manager will inform them appropriately.
6. Section Four – Caring for an at-Risk Prisoner
6.1 The care plan should also include a specific section on family or significant others support for the prisoner and their role in the care plan. The Probation service should act as a link with the family and those supporting them in the community.
6.2 The case conference should include family members if possible, both to ensure that outside issues of relevance to the prisoner’s mental health and well being can be addressed and also to clarify what support they can offer on visits and telephone contact in terms of supporting the overall care plan. For example, the family may well know that an upcoming event in family life, a christening, wedding etc., will effect the prisoner deeply and it is important in managing risk for the prisoner to have that information.
6.3 NIACRO welcome the policy that no prisoner will be transferred without the receiving Governor and healthcare staff being made aware of the facts regarding the risk of Self Harm and Suicide of a prisoner being transferred.
6.4 NIACRO welcome the policy that no prisoner receiving ongoing psychiatric intervention will be transferred to an establishment where the facilities are not considered to be adequate to his/her individual needs.
6.5 Non-Custodial Disposals. The release of a prisoner at risk or in crisis from court underlines again the importance of family members and significant others in their support network being aware of the current situation while the police at court could be asked to ensure that family members at court are made aware of the Exceptional Risk status of the prisoner.
6.6 The policy needs be specific as to who in the prison is expected to follow up on the disposal at court ie., who the police are expected to ring in the prison to inform of the disposal of an at risk prisoner and what the identified prison staff are expected to do in these circumstances.
6.7 Healthcare staff must always know who the prisoners GP is and if they do not have one this should be addressed urgently with the family or by Probation. Healthcare staff must inform family members and Probation accordingly.
6.8 Requests for Temporary Release. Again family support in the community will be an essential part of decision making as regards the granting of home leave or compassionate temporary release. It is important that their view is sought and that they are aware of any medical needs of the prisoner and who they can contact for advice/ support while the prisoner is on release. They will probably undertake the most important role of monitoring and support for the prisoner in that period.
6.9 The GP should be informed where a prisoner is to be granted temporary release and they will inform community psychiatric services.
6.10 Release on completion of sentence or on license. As above.
7. Annex A – Preventative Measures
7.1 A section could be included here on the role of family support in helping a prisoner through a crisis permitting for example, extra telephone contact to reassure them, extra visits etc.
8. Final Observations
8.1 Asylum seekers and other ethnic minority prisoners may be at heightened risk of self harm or suicidal behaviour. The regime can help to overcome some of this risk by ensuring that; translators are available regularly; staff are trained in cultural awareness and sensitivity; food choices are available; association with other people from a similar cultural background is permitted; that there is support with family contact and access to refugee support project workers.
8.2 Young people who have been subject of punishment beatings and shootings are also at a heightened risk of self harm and suicidal behaviour. They will be severely traumatised though are unlikely to admit that to themselves or staff. Therefore, special attention must be paid by reception and health care staff to the counselling and support needs of these young people.
8.3 A leaflet should be made available for families of prisoners explaining what the policy is and the process by which self harm and suicide risks will be managed in the prison. A leaflet should also be available for prisoners alongside the anti- bullying policy leaflet.
8.4 The resettlement process currently being advanced in all the prisons needs to take account of the specific needs of prisoners who have received mental health services while in prison. The plan will need to consider what extra support, types of accommodation, employment or training opportunities will be most appropriate for and supportive of the prisoner’s resettlement plan.
9. Conclusions
9.1 NIACRO welcomes the commitment shown in this document to the appropriate management of and support for prisoners at risk of self harm and suicide. We also believe it will offer much needed support to prison staff who are dealing with this difficult issue on a regular basis.
Health Promotion Agency for Northern Ireland
Introduction
The Health Promotion Agency for Northern Ireland (HPA) is the major regional provider of health promotion services and plays a leading role in policy development and the provision of advice on health promotion issues. The HPA is committed to working with many statutory, voluntary and private bodies and with national and international health promotion organisations.
By working with others we aim to shift the emphasis of modern health services towards prevention, protection and education, to reduce the need for treatment or rehabilitation and improve overall quality of life. Priority areas of work include nutrition, physical activity, drug and alcohol misuse, smoking, mental health and sexual health.
The Health Promotion Agency recognises Suicide as a major public health issue and is committed to working with all key partners and organisations involved in the implementation of Protect Life: a Shared Vision – the Northern Ireland Suicide Prevention Strategy and Action Plan 2006-2011.
The impact of suicide is devastating on the families directly involved and indeed on the wider community, in fact it is difficult to estimate just how many people are affected by the death of someone to suicide.
It is also recognised that the causes of suicide are extremely complex and as such are very difficult to tackle by any one agency or organisation therefore efforts to address the issue of suicide requires joint action across all government departments and locally in communities at large.
The HPA has been involved in the development and implementation of both the Protect Life and Promoting Mental Health Strategy and Action Plan 2003-2008 and it is recognised that efforts which address the broader mental health agenda also contribute to prevention of suicide.
The following submission is split into 2 sections. The first section provides a summary of the work that has been directly commissioned from the HPA by the Department of Health, Social Services and Public Safety relating to recommendations included within Protect Life – a Shared Vision. The second section details the broader background and a more comprehensive description of the work undertaken by the HPA which relates to the overall goal of helping to improve mental health wellbeing within Northern Ireland.
Section 1: Protect Life: A Shared Vision – summary of HPA actions
1. Public Information Campaigns
The HPA was commissioned by the Department of Health, Social Services and Public Safety, to develop a major public information campaign aimed at de-stigmatising mental health, and promoting awareness and understanding of issues relating to mental health and suicide.
Many organisations and individuals are very aware of the impact which self harm and suicide has on families and communities. However, research by the HPA into public attitudes to mental health indicates that the general public is still uncomfortable, and even negative, towards issues relating to mental health. Members of the public need information and opportunities to raise and discuss their own and others’ mental health and to be aware that mental health can be promoted and protected.
The evidence for a broad based approach to public information has been accepted by every country which has implemented a suicide prevention strategy. This approach has underpinned the Northern Ireland mental health promotion campaign. As well as a whole population approach we were able to develop a specific campaign targeting young men – we know young men are reluctant to discuss these issues or share their concerns to help improve their mental health.
The broad based approach has since been adopted by our colleagues in the Republic of Ireland. They have developed a similar campaign (in which we have been an active partner) based on their own research and review of the evidence of effective approaches to suicide prevention. We are currently involved in the second phase of the public information campaign. This will form part of an all-island campaign, with the third phase due to commence early next year.
2. Depression awareness training for primary care
The HPA was asked to develop and deliver depression awareness training for primary care health professionals including GPs, practice nurses and practice managers. This work has been carried out in consultation with all key stakeholders, including families bereaved by suicide as represented on the Families Forum. The programmes were developed over a six month period and delivered over the final three months of the last financial year. We depended very much on the Health Boards and Trusts for the organisation of the actual delivery locations and dates. More than a third of practices had a representative at the training and we hope this will be extended further this autumn.
In addition, the HPA developed an information pack over the same period which was delivered to every GP. An evaluation report on the training is currently being collated. I will send you a copy of the report when it is available.
3. Other developments
The HPA has also worked on other strands of the suicide prevention strategy including:
- helping to develop the peer mentoring scheme in Derry;
- helping to develop the North-South monitoring of self harm attendance in A&E departments;
- working with the Coroner’s Office and the Registrar General to improve the collection of information and the processes around the occurrence of suicide;
- the development of the helpline;
- the collation of information on all training in the field of suicide.
To inform future training developments the HPA has been appointed to carry out a comprehensive audit and evaluation of training programmes related to mental health promotion and suicide awareness.
We have carried out a review of research and other literature relevant to suicide prevention and used the results to inform policy and programmes being developed as part of the implementation of the suicide prevention strategy. We have also advised on specific research initiatives proposed as part of the implementation strategy. We are currently overseeing an audit of the suicide helpline which was piloted in North and West Belfast. This will help the development of a larger regional helpline to be developed and evaluated later this year.
Conclusion
The HPA has played a key role to date in responding positively across a range of pressing targets as identified within the Protect Life strategy. This must be viewed against a background of difficult operational conditions brought about by constraints imposed by the Reforms in Public administration, in particular relating to the appointment of staff.
Notwithstanding, the HPA has continued to demonstrate its ability to lead the delivery of Health Promotion services and play a major role in safeguarding Public Health as a priority within Northern Ireland. The Agency would welcome the opportunity to discuss with the Minister and members of Committee for Health, Social Services and Public Safety the best means of safeguarding its role and position as an independent body within future administrative structures.
Section 2: Promoting Mental Health and Suicide Prevention – An Overview
Policy and strategic context
In 2002 the World Health Assembly (WHA)3 adopted a resolution urging the WHO as the lead international agency with responsibility for health, to facilitate the effective development of policies and programmes to strengthen and protect mental health. The Mental Health Declaration for Europe 20054 advocates making mental health an inseparable part of public health and thus recognise the need for action across a range of areas and consideration of the impact of all policies on mental health.
It is recognised that the promotion and maintenance of mental health at a population level requires a collaborative approach including effective policies and strategies at international, national, regional and community levels. The wider determinants of health which include for example, poverty, housing, employment, and education all influence mental health and therefore need to be addressed by working across all sectors within Northern Ireland society. Partnerships at Governmental level which influence policy decisions at a regional level have recognised the importance of addressing mental health as a public health issue, however more emphases needs to be placed on making mental health a priority for funding and ensuring that it is incorporated at all levels of decision making.
Mental Health as a Public Health Issue for Northern Ireland
The Investing for Health Strategy (IFH)5 has as one of its objectives “To promote mental health and emotional wellbeing at individual and community level” and further sets a target “To reduce the proportion of people with a potential psychiatric disorder (as measured by the GHQ12 score) by a tenth by 2010”.
IfH also recognises that mental and emotional health is fundamental to our sense of wellbeing and quality of life and needs to be addressed as part of improving our health status. The strategy outlines actions relating to a number of key issues affecting the mental health and wellbeing of the population of Northern Ireland including: suicide and attempted suicide, working environment, the affect of the Troubles, education and domestic violence. It is also recognised that there are links with mental health and other health risk behaviours including alcohol and drug misuse and sexual health.
In January 2003 the DHSSPS launched Promoting Mental Health Strategy and Action Plan 2003-2008 (PMH)1 which outlined the strategic direction for mental health promotion for Northern Ireland. The strategy outlines 30 actions under four key areas: policy development, raising awareness and reducing discrimination, improving knowledge and skills and preventing suicide. It is acknowledged that mental health promotion depends on expertise, resources and partnerships across all sectors and disciplines and is relevant to a wide range of policy initiatives including New Targeting Social Need, the equality agenda, neighbourhood regeneration and community development.
A multi-agency Implementation group was established in 2003 to oversee the implementation of the strategy and action plan. This group which is chaired by Dr. Brian Gaffney Chief Executive of the HPA reports to the Ministerial Group on Public Health annually on progress made on the implementation of actions within the strategy.
In June 2005, following growing concern about the increase in the numbers of suicides in Northern Ireland a sub-group was established to review the ten actions relating to Suicide Prevention within the PMH Strategy. This review resulted in the establishment of a Task Force in July 2005 to oversee the development of a new suicide prevention strategy for Northern Ireland. Following extensive public consultation Protect Life: a Shared Vision – The Northern Ireland suicide prevention strategy and action plan 2006-20112 was launched in October 2006. Protect Life acknowledges “the need for suicide and wider mental health matters to be recognised as a major public health issue and to be recognised accordingly” and identifies specific actions, timescales and delivery partners for each of the areas within the population and targeted approach. The population approach seeks to tackle the issue of suicide in a wider context, with actions aimed at protecting the general population of Northern Ireland while the targeted approach focuses on actions relating to those most at risk.
The Health Promotion Agency has four priority business areas: policy development, public and professional information, training and research and evaluation, below is an outline of work which specifically relates to actions outlined within PMH and the Suicide Prevention Strategies.
Policy Development
The HPA has worked with the DHSSPS on the development of both PMH and Suicide Prevention Strategies. This has involved policy advice, organising public events including a major international Suicide Awareness conference in August 2005, public consultation events, responding to draft strategies and providing ongoing policy advice to the DHSSPS on issues relating to both the PMH and the Protect Life strategies.
Public and Professional Information
The HPA was commissioned by the DHSSPS to develop a major public information campaign aimed at de-stigmatising mental health, promoting awareness and understanding of issues relating to mental health and suicide.
In March 2007 the HPA launched phase one of a major public information campaign aimed at increasing public awareness of mental health, reducing stigma and improving help seeking behaviours.
The campaign approach was two fold, a broad population based approach targeted at all age groups entitled Its Me and a targeted campaign for young men aged 16-24 yrs entitled Share It.
There were a number of aspects to the campaign including mass media TV ads, Radio ads, posters, leaflets and a newsletter outlining the key campaign messages. A website entitled www.mindingyourhead.info has also been established to provide information and advice to both the public and professionals on a wide range of issues relating to mental health and includes a directory of services containing a wide range of information on services across Northern Ireland which can be accessed by individuals concerned about their mental health and wellbeing.
The need for such a campaign has been outlined in actions within both PMH and Suicide Prevention Strategies. Evaluation of phase one has been completed and a full copy of the evaluation report can be accessed from the HPA.
The HPA has also been working closely with colleagues in HSE and the National Office for Suicide Prevention in RoI in the development of the Public Information Campaign and both ads have been shown in the RoI.
In October 2007 the RoI launched phase one of its Public Information Campaign entitled Your Mental Health, which the HPA has also been involved in helping to inform its development and this is currently being aired on TV in Northern Ireland.
Training
As part of the HPA ongoing training and development programme which focuses on building capacity for Mental Health Promotion and suicide prevention, a number of training events have been offered which directly relate to actions outlined within PMH and Suicide Prevention strategies.
Some examples are as follows:
- Motivational Interviewing,
- Building Capacity for Mental Health Promotion Train the Trainer,
- Depression Awareness for General Practice,
- Assessing Depression Effectively,
- Mainstreaming Mental Health Promotion in Primary Care Train the Trainer, Young People relationships and self-esteem,
- Mental Health First Aid
- Young Men and Mental Health
- Child and Adolescent Mental Health and
- Promoting Young Peoples Mental Health through physical activity.
The Work Well programme which has been developed by the HPA in Partnership with HSENI also includes mental health promotion in the workplace setting as part of its ongoing training programme.
Mental Health First Aid
In 2005/06 the HPA worked in partnership with CAWT and Aware Defeat Depression to pilot Mental Health First Aid Programme within the CAWT area.
This 12 hour evidence-based training was originally developed in Australia and adapted for the Scottish Executive’s national programme for improving mental health.
The training is designed to improve the mental health literacy of the community and is based on the better-known concept of first aid training. It teaches the participant to recognise the signs and symptoms of someone with mental health problems, such as depression, anxiety and psychosis, and to help deal with a crisis situation through guiding someone towards professional and other help. It is suitable for delivery to a range of audiences, including the general public.
An extensive evaluation of the pilot programme was carried out by the HPA which showed very promising results. A summary of the key findings are outlined below:
Mental Health First Aid – Evaluation findings:
Over 230 participants from a range of backgrounds attended the training as part of the pilot. The findings from the evaluation of the training were positive, showing participants who received MHFA training were satisfied the training provided information that would allow them to recognise and provide initial help to someone with the symptoms of mental illness. In the three month period after receiving training, almost 8 in 10 participants said they had encountered someone experiencing a mental health problem and offered MHFA.
Participants reported that MHFA had a positive effect on their knowledge, skill, motivation and confidence to offer someone with a mental health problem help. Results of the evaluation showed participants helped clients or colleagues at work, family and friends, callers to a helpline, those attending support groups and members of the general public
The HPA plan to adapt Mental Health First Aid programme for Northern Ireland and are currently working in collaboration with colleagues from RoI on plans for an All Island version of the training programme. Mental Health First Aid continues to be delivered by instructors who have been trained as part of the pilot and the HPA will be offering a further two training courses in December 2007 and January 2008.
There is a continued demand for Mental Health First Aid and it has been recognised as one of the key training programmes funded under the Choose Life Suicide Prevention Programme in Scotland.
Depression Awareness Training for General Practice
In response to actions outlined in PMH and the Suicide Prevention Strategy the HPA was commissioned to develop and deliver depression awareness training for primary health care professionals including GP’s. This work has been ongoing since July 2006 and has been carried out in consultation with all key stakeholders including Health and Social Care Trust personnel, BMA, Aware Defeat Depression and Families Bereaved by Suicide. The training programme include the development of supporting materials including two CD Roms, and a fact sheet which was developed by the HPA in partnership with Aware Defeat Depression. This training has been evaluated and phase two of the training is ongoing across all 5 Health and Social Care Trust areas since September 2007. The Steering Group continues to meet and it is envisaged that the more long term sustainability of this training will be agreed following the completion of phase two of the current training programme. A copy of the evaluation report is available from the HPA however the following is a summary of the key findings:
Depression Awareness Training course – evaluation findings
General views on course
- 88% of GPs said that the training course and met some or all of their expectations;
- 68% of GPs felt that their colleagues would benefit from the course, with most (59%) saying they would recommend it to their colleagues;
- 41% of GPs who had attended the course said that they had used course materials and resources with colleagues;
Learning Outcomes: changes in diagnosis and treatment of depression by GPs
- 20% of GPs said that following training they had adopted new approaches to the diagnosis of depression; 9 out of 10 GPs were already using standardized questionnaires to aid diagnosis prior to training.
- 67% of GPs following training said that they would consider a range of treatment options therapies for the treatment of depression;
- 40% of GPs reported trying new techniques for the treatment of depression;
- following the training course, there was a fall of 6 percentage points (34% to 28%) in the proportion of GPs prescribing antidepressants for more than half of their patients(with depression);
- compared with a control group of GPs, those GPs who had participated in the training course were less likely to prescribe antidepressants for their patients (100% vs. 88%);
- following the training course, GPs were less likely to use antidepressants as the first course of action in the treatment of mild or moderate depression (38% vs. 27%);
- following the training course, GPs were more likely to use treatments such as:
- sleep and anxiety management techniques (up from 84% to 95%),
- encourage social support and befriending (up from 64% to 74%),
- Computer Cognitive Behavioural Therapy (up from 2% to 23%),
- ‘watchful waiting’ (up from 30% to 54%).
- 70% of GPs had shared aspects of the training with others in their practice;
Attitudinal change among GPs
A standardized questionnaire, Depression Attitude Questionnaire, used to measure attitudinal dimensions to depression, found no significant differences in GP attitudes pre and 3 months post training, although there were some positive shifts in attitudes when individual items were analysed;
- following training more GPs reported to be comfortable in dealing with depressed patients (up from 68% to 79%);
- following training fewer GPs agreed wit the statement that Antidepressants usually produce a satisfactory result in the treatment of depressed patients in general practice, (down from 76% to 63%);
- more GPs agreed with the statement that “Depressed patients are more likely to have experienced deprivation in early life than other people”- up from 36% to 54%.
GP views on local services
- the majority of GPs were satisfied with the quality of available services (e.g. psychiatry, community psychiatric services etc) available to support people suffering from depression;
- compared with service quality, GPs were less satisfied with service accessibility,
- with 4% satisfied with access to psychology services,
- 22% with access to counseling services and
- 48% with access to community psychiatric nursing services;
- 40% of GPs were unaware of voluntary and community services available to support people with mental health problems;
- Compared with a control group of GPs, those GPs who had attended the training course were more likely to have used a range of support services such as Action Mental Health, the Samaritans and Aware Defeat Depression.
Key learning outcomes and suggestions for future work
- According to GPs the key learning outcomes from the course were consideration given to a broader range of treatment options, the awareness of networks and computerised CBT;
- The most popular suggestions for improving the course were to make greater use of e-learning and to have shorter more focused courses;
- GPs felt that the most relevant aspects of the course were the review of treatment options, updates on new medications / antidepressants, the information on contributory factors leading to depression and the course content relating to communication skills;
- In terms of practice needs, GPs called for a list of self-help groups within their local area, regular updates on new therapies / medications;
- GPs identified the main patient needs as access to CBT, information leaflets on depression and lists of self-help groups;
Training Strategy Development
In April 2007 the HPA appointed a Mental Health Promotion Coordinator: Training and Development to coordinate the development of a strategy for training across both the MHP and Suicide Prevention Strategies. This work includes a detailed consultation with all key stakeholders including service users, carers and those bereaved by suicide. A mapping exercise is ongoing to establish training which is currently being delivered and accessed by organisations across NI relating to both strategies. This exercise is also taking account of RoI, UK and International perspectives and will make recommendations which will help inform future developments relating to training under both the PMH and Suicide Prevention Strategies.
Research and Evaluation
A number of research projects which the HPA has been involved in have been directly lined to both PMH and Suicide Prevention Strategies. The most recent of these has been a major study into the Public Attitudes and Perceptions of mental health in Northern Ireland which helped to inform the development of the public information campaign outlined above. The first of its kind to be carried out in NI, this research established that mental health is a complex issue and any attempt to address publics perceptions need to take account of these findings. A full report of the findings is available on the HPA website www.healthpromotionagency.org.uk A number of the key findings are as follows:
The survey revealed that people do not immediately think of mental health when asked to consider health problems facing Northern Ireland. Knowledge about specific problems is very limited, with the youngest and oldest age groups being the least knowledgeable. People greatly underestimate the level of mental health problems experienced. In addition, when asked if they themselves had experienced a mental health problem, 15% admitted they had. However, studies estimate that the actual figure is around one in five (20%).
This under-reporting may be due to stigma about the issue, or lack of awareness. The issue of stigma is complex and this was explored through attitudinal questions relating to mental health and mental illness.
There was no variation in responses between the genders or age groups; however, findings suggested a variation between social class groupings. Interestingly, the DE social class group displayed least stigma, with respondents more likely to admit that they themselves had experienced a mental health problem. It is generally accepted that help-seeking is prevented by stigma, and findings from this survey suggest this is the case.
However, the knowledge and literacy findings also suggest that for some, especially younger people and males, help-seeking is just as likely to be prevented by lack of recognition of a problem or symptoms. In turn, low knowledge of mental health is related to lack of willingness to acknowledge the issue in society, which is perhaps due to stigma. The survey also revealed that fewer people know or understand they can protect and improve their own mental health in the same way that physical health can be protected and improved.
Primary School Survey
A survey of the health of primary school children in NI has been carried out by the HPA which includes findings relating to mental health and emotional wellbeing. Results of this study have not yet been published however the HPA are planning to use the results to help inform a number of developments relating to programmes which address the mental health and emotional wellbeing of children and young people.
The HPA continues to provide ongoing support for the development of an evaluation framework relating to the Suicide Prevention Strategy and is also involved in ongoing developments relating to plans for the establishment of a regional 24 hour crisis helpline.
Other work relating to the Suicide Prevention Strategy which is not directly linked with our core business areas are as follows:
- Advice and support for the development of the peer mentoring scheme on Self Harm in Derry
- Work with the Coroners Office and the Registrar General to improve the collection of information and the processes around the occurrence of suicide
- Support for the establishment of the North-South monitoring of self-harm attendance in A&E Departments.
- Involvement in a 5 Nations Suicide Prevention group to share information and best practice across all areas of MHP and Suicide Prevention work.
Design for Living Partnership
A partnership between the HPA, Action Mental Health and the Youth Council for Northern Ireland was established in 1999 to respond to the growing concerns about the mental health needs of young people in Northern Ireland.
In 2000 this partnership commissioned research to establish the mental health needs of young people aged 16-25 and in response to the findings published two resources entitled Sound Mind which aim to support the mental health and emotional wellbeing of young people aged 13-18 in the post primary school setting. These resources – one for teachers and the other for young people have been distributed to all post primary schools since 2000 and demands continue to grow each year. Copies of both resources are available to download from the HPA website www.healthpromotionagency.org.uk
Mind Your Head.
In partnership with the National Union of Students/Union Students of Ireland NUS/USI, the HPA published a resource for students in the Further and Higher Education settings. These resources which outline information aimed at encouraging young people to make health choices regarding their mental are made available to all first year students each year. A support guide is also made available which is aimed at student support workers, tutors and counselling/support staff within the FE and HE settings. The HPA are currently working on the rewriting of these resources based on feedback from students and colleagues in NUS/USI. The new resources will be available to students in the 2008/09 academic year.
Ru Right in the head?
In 2004/05 the HPA commissioned resources focusing on mental health of young men and for those who work with young men in a range of settings. Developed by Dr Ken Harland from the University of Ulster and a regional advisory group including representatives from the Curriculum Development Unit, Youth Action, Parents Advice, Opportunity Youth, the Rainbow Project, Southern Area Health Promotion and the then Westcare Business Services the resources were disseminated at a 4 training events attended by 79 practitioners. The resources and training addressed key issues relating to the mental health and emotional wellbeing of young men including masculinity, sexual identity, help seeking and health risk behaviours.
Healthy Schools Programme
The HPA recognizes the schools as a key ecological setting for health promotion. Through the adopting of a whole school approach, mental and emotional health can be addressed across all sectors and disciplines. It is a place where health programmes and education can have their greatest impact as they reach pupils at influential stages in their lives; childhood and adolescence. Central to this is the importance of investing in a healthy school. The HPA continues to be involved in the promotion of healthy schools in Northern Ireland and have developed a toolkit to assist school development planning for health and wellbeing taking a whole school approach. Copies of the toolkit are available on the HPA website www.healthpromotionagency.org.uk The Extended schools initiative also adopts a whole school approach through engagement in collaboration and partnership working with schools and community groups.
UK Enquiry into the Mental Health in Later Life
The HPA has been involved with Age Concern and the Mental Health Foundation who launched the three year UK Inquiry into Mental Health and Well-Being in Later Life in late because of a shared concern that mental health in later life is a much neglected area. It focused on the gaps between policies and services for mental health, and those for older people.
The Inquiry into Mental Health and Well-Being in Later Life is a three-year, UK-wide project that aims to:
- Raise awareness of mental health and well-being in later life
- Involve and empower older people
- Create better understanding and build an evidence base
- Influence policy and planning, and
- Improve services.
The Inquiry worked in two stages:
The Stage One report focused on the promotion of good mental health and well-being in later life. A report of findings and recommendations from this stage was published in June 2006. (copies of the report are available on Mental Health Foundation (MHF) website www.mhilli.org
The Stage Two report was published in August 2007 and focused on services and support for older people with mental health problems and their carers. A report on stage two is available on the MHF website as above. (copies of the report are available on MHF website www.mhilli.org
The reports highlight that promoting mental health and well-being in later life will benefit the whole of society by maintaining older people’s social and economic contributions, minimizing the costs of care and improving quality of life. Evidence about the factors that affect mental health and well-being has increased. Activity to promote good mental health and well-being in later life could be integrated into current developments in policy and practice, nationally and locally, and add to the existing momentum for change. The reports have been circulated in Northern Ireland to all political parties, as well as to key stakeholders in order for the findings o influence policy.
References
1. Department of Health, Social Services and Public Safety. Promoting mental health strategy and action plan 2003-2008. Belfast: DHSSPS, 2003
2. Department of Health, Social Services and Public Safety. Protect Life – a shared vision, the Northern Ireland suicide prevention strategy and action plan 2006-2011. Belfast: DHSSPS, 2006
3. World Health Assembly (WHA) 55th World Health Assembly May 2002
4. World Health Organisation. Mental health action plan for Europe: facing the challenges, building solutions. WHO Geneva. http://www.euro.who.int/document/mnh/edoc07.pdf October 2005
5. Department of Health, Social Services and Public Safety. Investing for Health strategy 2002. Belfast: DHSSPS, 2002.
Northern Health and Social Care Trust
I refer to the letter from the Committee for Health, Social Services and Public Safety regarding the Committee Inquiry into the prevention of suicide and self harm and would respond as follows.
Scope and appropriateness of the Protect Life strategy:
There is a lot of overlap within the actions in the Strategy. Certainly much work could be done on the ground with communities in the area of promoting mental health and building resilience and social capital, as we know that to effectively address the issues of individuals we need also to address environmental and community factors. A concern would be that in focussing so strongly on the very real needs of younger people the strategy may play down the needs of older people who also sadly suffer high rates of suicide.
Suicide in young people:
Measures need to be put in place from a very young age. Over the last 50 years there has been a shift in how children are brought up. So much emphasis has been placed on shielding young people from adversity that when they face issues in teenage years, such as changes of school, break up of relationships, family problems etc they often do not have the necessary life skills to cope. This also links into the risk taking behaviours that teenagers carry out, if they are shielded from challenges and not allowed to take risks when they are growing up. Then when they grow up they have no understanding of boundaries and get involved in risk taking behaviours, yet not really understanding the consequences. A statistic recently quoted in a seminar in England was that 39% of 15 years olds have not climbed a tree. This is a very simple statistic but it illustrates this point.
Stakeholder involvement:
I do believe that there does need to be more joined up working, although I do think it is improving.
Support and services available to promote positive mental health:
There are different initiatives taken forward by the Trust and Northern Board that seek to do this alongside other organisations. Suicide prevention work is essentially the promotion of good mental health in dealing with coping abilities, support service etc and in this area is led on by the NHSSB (Suicide Prevention Co-ordinator).
Support for those bereaved by suicide:
A bid has been submitted by this Trust to the Northern Board to address this issue with the employment of development workers.
I would also highlight the work undertaken by our Crisis Response Service in the Homefirst legacy area which provides a self harm assessment service to A&E departments on a 24/7 365 day basis. One issue we do need to be mindful of is the requirement for targets to join up across service areas. An example of where there could be problems is in the 4 hours A&E target as often people who present with Self Harm at A&E can not safely participate in a mental state assessment due to being under the influence of drugs or alcohol. Statistics indicate that these are high risk people and it’s important that they are not discharged from A&E without having received a mental state assessment. This may require them to wait in A&E as a place of safety until they have sufficiently sobered up, which may take in excess of 4 hours.
Regarding the future:
There is a balance between needing to raise public and professional awareness of this topic whilst at the same time ensuring we are not publicising it in unhelpful ways.
There needs to be more joined up working on a regional basis to learn from what has worked in other areas and also more joined up working at a local level between education, youth sector etc. We need to continue to invest in the Protect Life Strategy on a year on year basis. We also need to continue to ensure that both regionally and locally that there is buy in from other key statutory and voluntary sector partners. Finally we should also be aware of the very significant investment recently announced in England to improve access to psychological therapies. This will build on a base line which is already much better resourced than the position in N Ireland. Speedy access to these types of services working into primary care has been demonstrated to be effective in dealing with a range of mental health problems including depression.
I hope these comments are helpful and I look forward to the outcome of the Inquiry
Norma Evans
Chief Executive
UNISON
Introduction
UNISON is the leading trade union in Northern Ireland and the largest trade union in the UK with over 1.3 million members.
In addition to representing workers delivering essential public services in health; social services; education; local government and private companies providing public services; UNISON organises nearly 2000 members in the local Community and Voluntary sector.
Many of our members work in areas of high deprivation and with disadvantaged groups linked to higher levels of suicide. A Co-convenor of the Equality Coalition and member of the Human Rights Consortium, UNISON’s membership also reflects all categories of affected groups specified in Section 75 of the Northern Ireland Act.
Key issues
1. Research v action: the Department has been for some time trapped in a mindset of ‘more research needed’. The need for research is unquestionable, particularly on the linkage to Troubles issues. The fundamentals of support and response are, however, the pressing issues on the ground.
Preventing the taking of life, and supporting those dealing with the consequences, require responses; resources; best practice; targeted outcomes; and a robust approach to challenge and change. These should be the focus for recommendations and outcomes from the work of the Committee.
2. Planning: the 2006 consultation and strategy process caused significant confusion by analysing suicide rates both at the level of pre-RPA Trusts and by the existing District Council boundaries. The latter have never been the basis for any other form of Health analysis and planning. Future planning should use data at the level of the five post-RPA Trusts – who will be the main service providers – and within these boundaries, focusing on Targeting Social Need clusters based on Noble Indices. The evidence on deprivation links is clear; the issue is to reflect it in the planning of services.
3. Formal resources: much of the community concern in recent years has rightly focused on the absence of service provision or its variable delivery (e.g. failure or delays in answering telephones). Central to this has been perceived failures in resource allocation. We can all recall discovering that most Belfast-based therapists were working in the former South and East Trust when an acute need for service provision and support was in North and West. Historically, the location of many services, their availability, and their delivery has been in areas of comfort rather than discomfort.
UNISON has therefore been calling for the creation of a baseline model for suicide intervention and support that specifies process and result targets; resources, budgets and staff; and the configuration of social work and clinical skills (e.g. cognitive behaviour, psychotherapy) across a pathway of community and acute support. This should express the basic level of support for all our citizens. It can then be used to allocate additional resources in an accountable and variable way to locations where need is greatest, and allow for visible review, reallocation, and growth to meet need.
The Committee should therefore consider whether current resources are sufficient; what level of additional resource, including best practice configuration, is needed to create a baseline model as set out above; and the resource required to meet needs over and above the baseline. The extent to which this approach is represented in current budgets or those in the Programme for Government and Draft Budget 2008-2011 (out for consultation) is crucial. Budgets need to move from historic categories set out for administrative convenience to ‘outcome’ budgets linked to Mental Health and within this category specific allocations for Suicide intervention and support.
4. Programme for Government/Draft Budget 2008-2011: the text in the Health Departmental Budget commits to a 15% reduction in suicide rates over 2008-2011. There is no specific reference to this in the Programme for Government, and the Mental Health commitment on unnecessary hospitation in the Programme, while excellent, will not achieve it. As part of wider engagement with the current consultation, the Committee may wish to determine the extent to which the 15% commitment and the measures required to achieve it are funded within the 2008-2011 Draft Budget.
5. Local and Community groups: the growth and excellent outcomes achieved on the ground by these initiatives have been the key development in our society’s approach to Suicide since the original work that lead to ‘Protect Life’ – in which local initiatives were not seen as an emerging and crucial resource.
UNISON engagement with groups at regional and branch level has lead us to the clear conclusion that they deliver their specific outcomes on the ground in a far more effective way than the public resources – or lack of them – that have been there to date. Therefore the way forward is to move to genuine partnership working in which the resources and delivery of the services of the state complement the value added by local community initiatives.
This means ongoing funding for groups over and above the welcome £1.8 m the Minister has announced for 2007-2008. It is essential that this funding addresses core costs issues, since most groups lack the basic infrastructure to sustain delivery. It should also not be hamstrung by the additionality principle of only funding new rather than existing work. It must sustain groups in ‘looking out’ and taking risks rather than ‘looking up’ to funders and their bureaucratic requirements.
Sometimes the simple initiatives are the ones that are overlooked. We attach for the information of the Committee the poster created by our UNISON Youth group, which lists resources and support with the permission of all the providers, and is being distributed and placed on notice boards by all our branches.
6. Training: we are currently in a process of engagement with members working in Mental Health, and delivering Mental Health Awareness programmes open to all members in partnership with Rethink, plus ASIST Suicide Training. One early informal conclusion from this process is that many members not specifically designated Mental Health workers frequently work with clients and patients with key indicators of suicide and self-harm, and yet have received no formal Mental Health training. We would trust the Committee will consider the adequacy and content of suicide-related training for all those delivering Health and Social Care, and future needs.
A welcome feature of the consultation that lead to Protect Life was the proposal for Mental Health Awareness Training to be delivered in all public and private sector workplaces by the rapidly approaching date of 2009. UNISON endorsed this approach, and instigated its endorsement by NIC-ICTU.
The Department now needs to take this forward. It is essentially a matter of will, not of funding at this stage. UNISON’s proposal is for the creation of a learning network to be established by a mix of private and public employers working in partnership with trade unions on pilot programmes, and then feeding back and spreading good practice and learning with the endorsement of the Department. This is an opportunity for the Committee to call upon the wider resources of civic society to take a key element of the Protect Life strategy forward.
7. Mainstreaming Equality: we indicated in the run-up to Protect Life that a wider and more inclusive equality consultation process was needed, despite some good work done, and the visible inclusion of representatives from the Lesbian and Gay community.
Our evidence base, including our own literature search, is that there is significant read across between suicide impacts and the nine categories in Section 75. We would therefore urge the Committee to ensure recommendations include a requirement for full equality screening and assessment by the Department, including full public consultation.
Conclusion
We thank the Committee for the opportunity to submit written evidence and welcome your initiative in raising the profile on this issue through your work. We will be available to give oral evidence if requested.
Department of Health, Social Services and Public Safety
Department of Health, Social Services and Public Safety
Tab B
November 2007
1. Introduction
2. Development of Suicide Prevention Strategy
3. Suicide Prevention Strategy
4. Strategy Review and Evaluation
5. Bamford Review and Mental Health Services
6. Annex 1 – Terms of Reference and Membership of Taskforce
7. Annex 2 – Updated Analysis of Suicdie and Self Harm in Northern Ireland
8. Annex 3 – Membership of Quality Assurance Group
9. Annex 4 – Suicide Prevention Action Plan
10. Annex 5 – Terms of Reference & Membership of Suicide Strategy Implementation Group
11. Annex 7 – Membership of Mental Health & Learning Disability Board
1. Introduction
Suicide
1.1 In the last few decades, large increases in rates of suicides have been reported across most regions of the world, particularly in New Zealand, the United States, Ireland, France, Norway and Brazil. It is widely accepted that suicide is the third biggest cause of ‘years of lives lost’ after cardiovascular disease and cancer.
1.2 There have been significant increases in the Northern Ireland suicide rate in recent years, and since 2004 local suicide rates have almost doubled. In addition, provisional figures for the first quarter of 2007 show that there were 65 suicides recorded, an increase of 20% from the 54 recorded in the same period in 2006. From January – June 2007 112 suicides have been recorded which represents a 24% fall from this period last year.
1.3 Suicide is an emotive and sensitive subject. It represents a tragic loss of life and leaves a difficult legacy for families and those close to the situation.
1.4 Currently there is little evidence as to why people take their own lives, or what interventions have a real impact. Risk factors include depression, alcohol and drug misuse, personality disorder, hopelessness, low self-esteem, bereavement, break-up of a relationship and social isolation. While no specific intervention has been found to be universally effective it is important that the risk factors are addressed as part of a broader approach to promoting mental health and wellbeing.
1.5 As it is a complex and multi-faceted issue there are no simple short term solutions. For example, while some vulnerable individuals show signs of risk and can be targeted for additional support and services, in other cases the warning signs may be absent or less evident.
Self-Harm
1.6 The term self-harm covers a wide range of behaviours including parasuicide (an apparent attempt at suicide in which the aim may not have been death), habitual self-cutting, and poisoning. Self-harm involves differing degrees of risk to life and suicidal intent, and it is often considered to be a coping mechanism, or a means of helping someone deal with their life. There are many reasons why a person self-harms. These can include a need to release tension, a perceived punishment for being “bad”, a desire to see blood as a means of cleansing.
1.7 There are many myths surrounding self-harm, one being that all of those who self-harm are seeking attention, but in reality many go to great lengths to hide their injuries. Another myth is that in all cases someone who self-harms is trying to take their own life, and while it is true that those who self-harm are more at risk of attempting suicide it is not true that the majority will go on to die by suicide.
Mental Health
1.8 It is estimated that mental health needs in Northern Ireland are at least 25% greater than England. Suicide can be seen as one manifestation of the poor mental health and wellbeing here, although this is not to say that all suicides are the result of poor mental health. Many factors impact on mental health and wellbeing including alcohol and drugs misuse, sexual health and abuse or violence. The Department has a range of policies aimed at tackling these issues, which should contribute to promoting positive mental health and also to a reduction in the levels of suicide. It is difficult to tackle suicide effectively if it is done in isolation from a wider strategy to improve mental health and well being in the population.
Promoting Mental Strategy and Action Plan
1.9 The Investing for Health Strategy, published in March 2002, provides the framework for the Government’s approach to improving health and wellbeing and reducing health inequalities. It identifies the need to promote mental health and emotional wellbeing at individual and community level, and in particular the importance of tackling the difficult issue of suicide.
1.10 The Promoting Mental Health Strategy and Action Plan, published by the Department of Health, Social Services and Public Safety (the Department) in January 2003, contains 30 actions which are designed to support mental and emotional wellbeing. Ten of these actions focus specifically on suicide prevention, including the promotion of coping skills, the development of suicide awareness programmes, and the need for enhanced outreach work with young people in areas of need.
1.11 Actions flowing from the strategy include local programmes to promote mental health, programmes aimed at improving coping capabilities, support for the farming community, provision of information about local sources of help, training of staff, suicide awareness programmes and outreach work with young people. Initially, the Strategy implementation was allocated £300,000 per year. In 2005 this was increased to £600,000 per year.
1.12 An Inter-sectoral Implementation Group was established in September 2003 to direct and oversee implementation of the Strategy. The Group, which includes representation from relevant statutory and voluntary organisations, is chaired by the Chief Executive of the Health Promotion Agency. Given the work to develop and implement the new Suicide Prevention Strategy, the steering group found itself in hiatus for a significant period of time, re-convening in November 2006.
2 Development of Strategy
2.1 As a result of concern about an increase in the number of suicides, particularly among young people, a multi-sectoral Taskforce was established in July 2005 to develop a Suicide Prevention Strategy for Northern Ireland. The Terms of Reference and its membership are attached at Annex 1
Engagement
2.2 At the outset, the Taskforce (which was chaired by Colm Donaghy, Chief Executive of the Southern Health and Social Services Trust, and now the Chair of the Suicide Strategy Implementation Body) acknowledged the importance of taking views from interested stakeholders and affording them the opportunity to influence the content of the new strategy before it was fully developed. It undertook an extensive engagement process which included:
- publicly advertised open consultation workshops in each health and Social Services Board area;
- meetings with bereaved families and relevant support groups;
- meetings with political parties, local churches, coroners, the Prison Service, the Police Service, and the Northern Ireland Commissioner for Children and Young People;
- consultations with health service professionals and the statutory sector;
- meetings with young people;
- a workshop for regional community and voluntary sector organisations;
- a major international suicide prevention conference; and
- a two-day workshop bringing together community groups, bereaved families and relevant health service professionals.
2.3 The issues raised included:
Improved Joined Up Working
- the new strategy should contain strong linkages to other Government strategies;
- inter-Departmental commitment is required, as the new strategy will cut across several Government Departments;
- closer co-operation between local communities, voluntary/community organisations and the statutory sector; and
- better co-ordinated services must also be sensitive to the needs of those in crisis and those bereaved by suicide.
Training and Development
- need to ensure improved training and development for frontline staff in health and social services particularly in A&E, and primary care, including GP’s;
- provision of additional training, such as ASIST, for health professionals, clergy, people in local communities, and for occupations which regularly come into contact with those at risk of suicide; and
- introduction of social/coping skills for young people still in school.
Key Service Issues
- need to develop more accessible services outside normal working hours and potential alternatives to hospital admission/attendance, particularly in response to crisis in the community e.g. 24/7 community based crisis response service;
- lack of follow up for vulnerable groups, particularly those who self-harm;
- need to ensure service delivery is patient centered and services are sensitive and responsive to patient needs, especially in the transition from adolescence to adulthood; and
- need to monitor and regulate the prescribing of anti-depressants to the under 18 age group.
Promoting Good Mental Health
- the need for suicide and wider mental health matters to be recognised as a major public health issue and to be resourced accordingly;
- providing a trusting environment for young people to be able to express their feelings;
- raising suicide awareness, and reducing stigma for those seeking help should be a high priority in a range of areas including schools, prisons, youth work, local communities, universities, the armed forces and health and social services;
- need to reduce the level of stigma around mental health issues, and in particular those seeking help; and
- work with the media to ensure more sensitive reporting and portrayal of suicide.
General Issues
- the strategy should be a “living document” that will be reviewed regularly, effectively implemented, and properly resourced;
- need to reduce the waiting period and enhance the sensitivity of the coroner’s office systems;
- support for Professor Bamford’s recommendation that the implementation of the local suicide strategy should be separately resourced from, but run in parallel to, the Promoting Mental health Strategy and Action Plan;
- need to ensure that strategy implementation funding is ring fenced, and made recurrent; and
- acknowledgement of the need for churches to engage further with local communities in relation to how best to tackle the suicide problem.
Scotland
2.4 Over recent years Scotland has seen a decline in its suicide rate, which now stands at 14.7 per 100,000 in 2006, a fall of 13% from 2002. During the development of the Northern Ireland Strategy, Colm Donaghy, Taskforce Chair, and Departmental officials met with representatives of ‘Choose Life’ the organisation who are taking forward the implementation of the Scottish Suicide Prevention Strategy, “Choose Life” to learn from their experience in developing a regional Suicide Prevention Strategy.
Guiding Principles
2.5 The following guiding principles were adopted during the development of the Strategy:
- Links to Other Strategies – to develop strong links to other relevant strategies including Investing for Health, Promoting Mental Health Strategy and Action Plan, New Strategic Direction for Alcohol and Drugs (2006-2011), Neighbourhood Renewal, the Children’s Strategy and the Bamford Review of Mental Health and Learning Disability (NI).
- Joined-Up Working – the need for joined-up working at Government level, and between the statutory and Voluntary/Community sectors.
- De-stigmatisation – of mental health issues and to encourage help seeking behaviour.
- Best Practice – continuous commitment to achieving and sharing best practice.
- Engagement – support for, and commitment to, continued consultation with bereaved families, survivors, carers and their representatives.
- Dual Approach – to adopt a dual population and targeted approach when implementing the Strategy.
- Working Together – support for shared working with counterparts in the Republic of Ireland, Great Britain and beyond, where mutually beneficial.
Other research and analysis used in the Strategy Development Process
2.6 To help in the development of the new strategy the Taskforce also commissioned the following work:
- an analysis of the levels of suicide and self-harm in Northern Ireland;
- a review of the evidence base and identification of best practice in Northern Ireland and elsewhere.
- a review of the implementation of the ten suicide prevention action points in the Promoting Mental Health Strategy and Action Plan; and
Analysis of the levels of suicide and self-harm in Northern Ireland
2.7 To help inform the Taskforce the Department undertook an analysis of suicides and self-harm in Northern Ireland over the last five years for which data was available (1999 – 2003). Some of the key findings were outlined in the draft Suicide Prevention Strategy and also in the final Strategy. The Department has recently updated the analysis (2002 – 2006) - a copy is attached at Annex 2
Review of Evidence Base
2.8 In order to inform the development of the Suicide Prevention Strategy the Taskforce also commissioned a review of the evidence base relating to suicide and self-harm. The literature review was carried out to provide a pragmatic evidence base on which to develop the Strategy. A brief summary is outlined in the following paragraphs and the full report is available online at: www.investingforhealthni.gov.uk/documents/reviewofbase.pdf
2.9 There is limited evidence available in relation to interventions that are effective in reducing the risk of suicide and self-harm. In many instances studies show conflicting results and in general more evidence is required before strong recommendations can be made.
2.10 It is important to note that most interventions that are assumed to prevent suicide, including some that have been widely implemented, have yet to be evaluated to determine their effectiveness. Nevertheless the following interventions have shown promising results:
- GP education programmes aiming to increase detection of depression;
- restriction of access to means of suicide; and
- education of community gatekeepers e.g. school and prison staff.
2.11 There is also some evidence that the following may be effective:
- treatment of mental illness, especially depression;
- some specific psychotherapies to prevent repetition of self harm;
- follow-up after self harm; and
- responsible media reporting.
2.12 Outcomes from this review were incorporated throughout the Strategy. Some other key issues arising from the review include:
- almost 80% of those who die by suicide in Northern Ireland had seen their GP in the 6 months prior to their death (although not necessarily in relation to mental health), with 36% having seen their GP in the month prior to their death;
- of the people who died by suicide 98% over the age of 30 years old and 74% under the age of 30 are likely to have had a psychiatric illness;
- 7% of those who died by suicide had been discharged from psychiatric hospitals in the 3 months before their death; and
- initial research has suggested a linkage between the per capita alcohol consumption of Northern European countries and the suicide rate, particularly amongst young people
Review of Suicide Prevention Actions
2.13 As part of the review of the ten suicide prevention action points in the Promoting Mental Health Strategy and Action Plan the Taskforce undertook an extensive series of meetings with relevant Government Departments, Health and Social Services Boards and Trusts, as well as interested voluntary/community organisations. In summary the main findings are:
- three of the ten action points had been met in full and six had been partially met;
- one action point, the development and delivery of a depression awareness training programme for GPs, had not yet been actioned;
- the most successful regions in delivering the action points tended to mirror those Health and Social Services Boards that have previously suffered from a spate of suicides, and that have therefore had dedicated suicide prevention resources in place for sometime; and
- the main barriers highlighted as preventing achievement of the ten action points included, lack of recurrent funding and dedicated resources, lack of co-ordination and health service priority, and inability to successfully engage GPs and other health professionals on this issue.
Economic Cost of Suicide and Self-Harm in Northern Ireland
2.14 The Department also undertook an exercise looking that the economic cost of suicide and self-harm in Northern Ireland. This review clearly highlighted that suicide and self-harm have a substantial impact on Northern Ireland, both in terms of lives lost and the resulting trauma for bereaved families and the local community. The evidence also suggested that the cost of suicide and self-harm has a significant economic impact on Northern Ireland as a whole.
2.15 During 2004, there were 146 suicides recorded in Northern Ireland, equating to 4,350 potential years of life lost for that year. Associated with each suicide are the direct costs such as the post mortem and funeral costs; the indirect costs such as the value of the potential earnings lost; and the intangible costs which estimate the human costs such as suffering, grief and loss of non-market outputs such as voluntary work or housework. For 2004, the total estimated cost of suicide to Northern Ireland was in the region of £202 million, which equates to £1.4 million per suicide.
2.16 The benefits of prevention of suicide and self-harm are therefore clear and quantifiable in terms of health benefits and economic costs, and these include:
- the potential to save lives;
- improved quality of life;
- interruption of the cycle of self harm and suicide experienced in some communities and families;
- reduction in the cost of hospital care associated with episodes of self-harm and poor mental health; and
- improved productivity through people’s contribution to the economy.
Impact Assessment
2.17 As part of the development of this Strategy, the Department used the Integrated Impact Assessment Screening Tool to determine if the Strategy had any negative economic, health, rural, environmental, social, human rights, homelessness, victims, or community safety impacts. Additional consideration was given the to the Strategy’s equality impacts.
2.18 It was considered that the policy should impact positively on the health and emotional wellbeing of the general population, and that the Strategy and Action Plan did adversely impact on any of the Section 75 groups and therefore a full Equality Impact Assessment was not required. The conclusions from this screening exercise are available online at http://www.investingforhealthni.gov.uk/documents/IntegratedImpactAssessmenScreening.pdf
Draft Suicide Prevention Consultation Process
2.19 The Draft Northern Ireland Strategy and Action Plan was launched for a formal 12 week public consultation on 30 March 2006. In addition to issuing the consultation document and questionnaire to all those on the formal consultation list, and key stakeholders, the Taskforce also arranged a number of pro-active consultation events in each Health and Social Services Board area. The NI Children’s Commissionaires “Message to the Minister” campaign also fed into this consultation process.
2.20 The Department received over 170 responses to the formal consultation process. Following the close of the consultation period, all the consultation responses were analysed, and the Strategy revised in light of these comments.
Quality Assurance
2.21 The Department established a virtual “Quality Assurance Group” of international experts to consider the final draft of the Strategy before its launch, membership of this group is included in Annex 3 The Group’s comments were incorporated into the final version of the Strategy.
3. Suicide Prevention Strategy
3.1 The Suicide Prevention Strategy ‘Protect Life a shared vision’ was published in October 2006.
Aim
3.2 The overall aim of the Strategy is:
to reduce the suicide rate in Northern Ireland.
Objectives
3.3 The key objectives of the Strategy are:
- to raise awareness of mental health and wellbeing issues;
- to ensure early recognition of mental ill-health, and to provide appropriate follow-up action by support services;
- to develop co-ordinated, effective, accessible and timely response mechanisms for those seeking help;
- to provide appropriate training for people dealing with suicide and mental health issues;
- to enhance the support role currently carried out by the Voluntary/Community sectors, bereaved families and individuals who have made previous suicide attempts;
- to support the media in the development and implementation guidelines for a suitable response to suicide related matters;
- to provide support for research and evaluation of relevant suicide and self-harm issues; and
- to restrict access, where possible, to the means of carrying out suicide.
Target
3.4 The Strategy sets a target of reducing the reduce the overall suicide Northern Ireland Suicide rate by 15% by 2011, from a baseline of 12.6 in the three year rolling average period of 2004-2006.
3.5 However, the Strategy recognises that paradoxically, its success in reducing the stigma that surrounds suicide may adversely affect the ability to meet the targets set out above i.e. increased willingness on the part of families and coroners to have deaths acknowledged and officially recorded as suicide, or improved recording arrangements, may actually create an artificial rise in the recorded suicide rate. Therefore, if this occurs it should not be interpreted as a failure of the Strategy to achieve its goals.
Action Plan
3.6 The Strategy contains 62 actions aimed at tackling suicide – Annex 4. The analysis of suicide in Northern Ireland carried out in the development of the Strategy highlighted that there is a direct association between suicide rates and gender, age groups, and socio-economic status. Therefore, in order to reduce the suicide rate in Northern Ireland the Strategy adopted a dual population and targeted approach.
Progress to Date
Implementation Body
3.7 Following publication of the Strategy an inter-sectoral Suicide Strategy Implementation Body (SSIB) was established to oversee and drive forward the implementation of the Strategy. Membership includes representation from bereaved families, as well as members of those communities most affected by suicide. The Terms of Reference and membership of the Implementation Group are attached at Annex 5. The SSIB meets bi-monthly. It will report progress on an annual basis to the Ministerial Group on Public Health
Families Voices
3.8 Bereaved families played a key role in the development of the Strategy and are represented on the SSIB. A Families Forum (now Families Voices) was established in August 2006 to ensure that they continue to have a powerful voice in the implementation process.
Local Implementation
3.9 Local Implementation groups have also been established in each Health and Social Services Boards area to develop and oversee local suicide prevention action plans. The Department has asked Boards to ensure these local groups also engage with all the key stakeholders, including professional, statutory organisations, community/voluntary representatives and bereaved families representatives.
Funding
3.10 The Department provided funding of £1.9 million in 06/07 and £3.06 million in 07/08 to implement the Strategy. The allocation of the 07/08 funding was agreed between the Department and the SSIB.
Community Support Package
3.11 In 06/07, approximately half of Strategy’s £1.9 Million funding was allocated as part of a community support package. In 07/08 this funding was doubled to £1.8m. The funding was distributed via the four local Health and Social Services (HSS) Boards, to be used to:
“support local communities with the development of initiatives, inline with the actions set out in Protect Life, which will help achieve a reduction in the levels of suicide and self-harm in Northern Ireland. Specific provision should be allocated for:
- the development of programmes which reach out to young males;
- the development of initiatives that encourage partnership working between the community, voluntary and statutory sectors; and
- the development of initiatives that include both local and regional actions”.
Pilot Projects
3.12 Mentoring – a pilot mentoring scheme for persons who self-harm, which involves the A & E department in Altnagelvin hospital working in partnership with local voluntary organisations to provide additional support for those who self-harm, was launched on 9 January 2007.
3.13 An appointed mentor supports the client throughout the programme, and identifies and fast tracks them into the most appropriate specialist support service. If the client turns down the initial invitation to enter the scheme they are given the opportunity to self-refer at a later stage.
3.14 Helpline – a 24/7 suicide prevention telephone helpline, which is being piloted in North and West Belfast, was launched on 30th October 2006. The helpline specifically targets young people and it is supported by additional peer mentoring and counselling services. The pilot helpline, which is currently receiving over 100 calls per day (approximately 50% of which are received from outside the North and West Belfast area).
3.15 Self-Harm Registry - a piloting of the National Suicide Research Foundation’s Irish National Registry of Deliberate Self Harm in the Western Health and Social Services Board Area has commenced. The aim of the pilot is to define the true extent of the problem of suicidal behaviour by collecting data from hospital accident and emergency departments on specific trends in deliberate self harm, and allow comparison with the Republic of Ireland. The analysis of this information will inform the development of policies and shape the implementation of measures aimed at preventing suicide and self-harm.
Suicide Prevention Helpline.
3.16 In response to the rising levels of local suicides, and taking account of feedback from local communities the Minister announced his intention to establish a 24/7 NI Crisis Response and Suicide Prevention Telephone Helpline, with associated support services. It is anticipated that the new Helpline will be established in this financial year.
GP Depression Awareness Training
3.17 Current research suggests that GP training in depression recognition and treatment can show positive impacts on the level of suicide. A new depression awareness training programme has been developed. A Steering Group was established to drive this process forward, and its membership includes representatives from each Health Board, primary care & public health professionals, the British Medical Association (BMA), families bereaved by suicide, and key voluntary organisations such as Aware Defeat Depression.
3.18 At the end of October 2007 218 GPs have participated in this training programme, and a further 71 practice managers / practice nurses have received related training. The roll-out of this programme will continue and it is anticipated that a further 277 GPs will have participated in the training before the end of December 2007. In addition, all GPs have now received related CD-Rom training packages that contain up to date information on the depression and suicide related issues.
3.19 The Chair of the SSIB has also recently written to the Dean of the Faculity of Medicine and Health Science in the Queens University Belfast in relation to the inclusion of related training in relevant medical undergraduate courses.
Audit of Training Programmes
3.20 There is currently a range of suicide prevention and mental health promotion training programmes and seminars available across Northern Ireland, many of which haven’t been evaluated. The SSIB has asked the Health Promotion Agency to carry out an audit of all the relevant suicide prevention and mental health promotion training programmes available.
Public Information Campaign
3.21 In line with the Strategy the Health Promotion Agency (HPA) developed a public information campaign aimed at de-stigmatising mental health, and promoting awareness and understanding of issues relating to suicide.
3.22 The two new adverts, “It’s Me” and “Share It”, were launched on 12 March 2007 and are supported by the “Minding your Head” website. The “Its Me” advert was also broadcast on media in the Republic of Ireland as part of ongoing North/South collaboration on suicide prevention. The “Share It” advert, which specifically targets young people, was re-run in appropriate media in July 2007.
3.23 Phase two of this campaign was developed in liaison the National Office of Suicide Prevention in the Republic of Ireland, and was launched earlier this month.
Research
3.24 Underlying causes - the Strategy highlighted the need to understand the underlying causes of why people here take their own lives. The new Mental Health and Learning Disability Board have been asked to look into this issue as its first priority. The Chair of the Board, Professor Roy McClelland, has already met with officials from the Department and the Research & Development Office to discuss this work in more detail. Work will begin shortly to commission this research.
3.25 Effects of the Conflict - The Department also commissioned a review of literature into the effects of the troubles on the mental health and well-being of the people of Northern Ireland, especially in relation to suicide. The Review, which was published on 28 June 2007 and is available at http://www.investingforhealthni.gov.uk/documents/trouble-with-suicide.pdf, concludes that the conflict shaped the recording of local suicides in significant ways, and that its legacy continues to influence the challenge of reducing suicide in the future. In particular, it suggests that changes in the relationship between state bodies and communities and individuals most affected by the conflict have impacted on the registration of suicide, the recognition of the issue, and the speed and nature of the response to it. It also sets out a number of potential areas for further research.
3.26 The Department is also in discussions with the Research and Development Office about the potential to commission a general call for suicide prevention related research.
Suicide Recording Arrangements
3.27 The Strategy highlights concerns about the accuracy and timeliness of the current arrangements for officially recording deaths by suicide. The Department has established a working group, involving the Coroners Office, the General Registrar’s Office, the Northern Ireland Statistics and Research Agency, the HPA, and The Courts Service, to look at the current recording arrangements and make relevant recommendations.
Cross-Jurisdiction Work
3.28 Five Nations Group - many of the issues in Northern Ireland are also challenges for colleagues in England, Wales, Scotland, and the Republic of Ireland. A Five Nations joint working forum has been established to facilitate the sharing of best practice between the nations and enhance co-operation on mutually beneficial areas of work. The next meeting will take place in Belfast during November 2007.
3.29 All-Island Action Plan - the Strategy highlights the benefits of parallel implementation of the Republic of Ireland’s Suicide Prevention Strategy “Reach Out”. Therefore, an All-Island Action Plan has been developed in conjunction with counterparts in the National Office of Suicide Prevention in the Republic of Ireland. A copy of the action plan is attached at Annex 6
Ministerial Co-ordination Group
3.30 To ensure and enhance co-ordination on suicide prevention and mental health promotion across Government the Executive has established a Ministerial Co-ordination Group. It is chaired by the Health Minister and includes the education Minister and the two junior OFMDFM Ministers. The Group has met on three occasions.
The Internet
3.31 There have been growing concerns about the impact the internet can have on vulnerable people, especially at times of crisis. Minister McGimpsey recently met with key internet industry stakeholders, including Bebo, Google and Vodafone, in London to highlight and discuss the concerns. All those involved in the meeting have now responded positively.
3.32 In particular, they have highlighted their intention to continue to promote positive mental health, and to encourage people to seek help and support at times of crisis. For example, in future, users of Myspace, Bebo and other services will be directed to suicide prevention and positive mental health and well-being sites should they search for suicide related terms. Officials have had further discussions with the stakeholders and Minister McGimpsey will be meeting them in the near future.
The Media
3.33 The media also has a role to play in preventing suicide. Research shows that how suicide and related issues is portrayed in the media can have a huge impact on the issue, for example, a campaign to decrease media coverage of subway suicides in Vienna in the late 1980s cut subway suicides by 80%. Evidence such as this has led to the development of media guidelines in the UK and Republic of Ireland. Minister McGimpsey met with local editors in September 2007.
4. Strategy Review and Evaluation
Review
4.1 The implementation of the Strategy will be reviewed on an annual basis, with the first review due to start 12 months from the date of publication of this Strategy. Responsibility for initiating the review will rest with the SSIB, although final ratification of any proposed changes to the Strategy will remain the responsibility of the Department. The first annual review of the strategy will commence in November 2007, and be completed by end of March 2007.
4.2 The review will consider the appropriateness of the actions, delivery partners and timescales set out in the Strategy, and make recommendations to revise these as required. The review will also need to consider if the structures that have been put in place to implementation the strategy are appropriate, and are ensuring that the Strategy is being taken forward in the most effective manner.
Evaluation
4.3 The Strategy stated that where following evaluation an intervention, programme or initiative is not having the desired effect funding should be re-invested to other areas were it can be used more effectively.
4.4 The Department has commissioned the Institute of Public Health in Ireland (IPH) to develop a monitoring and evaluation framework that will assist with the future assessment of key elements of the Strategy’s implementation, including:
- the current implementation process, and in particular the appropriateness of both the existing local and regional implementation structures;
- the mentoring pilot scheme for people who self-harm
- the pilot suicide prevention helpline;
- the local community support funding package;
- delivery of the All-Island action plan;
- the GP Depression Awareness Training programme; and
- the public awareness information campaign.
4.5 IPH is currently consulting with key stakeholders on the development of this framework, and it is anticipated that this work will be completed by the end of November 2007.
5. Bamford Review,
Mental Health and Suicide Prevention Services
5.1 The Strategy acknowledges that its successful implementation, and the achievement of its aim, will be influenced by the progress on the delivery of the Promoting Mental Health Strategy and the Bamford Review of Mental Health and Learning Disability (NI).
Bamford Review of Mental Health and Learning Disability (NI)
5.2 The findings of the Bamford Review, an independent review of mental health and learning disability services have provided compelling evidence of the need for comprehensive reform, modernisation and investment. The review has been wide-ranging and will provide the vision for service delivery across the spectrum of mental health and learning disability services. It has highlighted the need for appropriate cross-sectoral working by raising issues relating to areas including education, training, employment, housing and social security benefits as they impact on people with a mental health problem or a learning disability. The review therefore requires not just a Health and Social Care sector response but a Government wide response as it cuts across all sectors. An inter-departmental task force has been established to take this forward. For the Health and Social Care Sector the thrust of the Bamford review is to provide patient-centred, seamless community-based services, informed by the views of services users and their carers and making prevention and early intervention key priorities. This must be achieved through a joined-up approach to maximise people’s ability to live full lives within their own community.
Mental Health and Learning Disability Board
5.3 A new Mental Health and Learning Disability Board was recently established to act as champions for people with mental health and learning disabilities and to be one of the driving forces in delivering the Bamford reforms.
5.4 The Board, which is chaired by Professor Roy McClelland, held its inaugural meeting on 9 August 2007 and the Health Minister intends to meet with the entire Board bi-annually. Membership of the Board is set out at Annex 7.
Range of Mental Health Services
5.5 Mental health is influenced by many factors including genetics, childhood experiences, life events, individual ability to cope, access to social networks and wider social and economic circumstances. The majority of people with a mental health problem will be treated by a GP and the aim is to treat people with mental health problems as early as possible to aid recovery.
5.6 A programme of GP depression awareness training programme has recently been developed and is currently being rolled out across Northern Ireland as current research indicates that training in depression recognition and treatment can show a significant positive impact on the level of suicide.
5.7 There will always be a need however for some people to be referred to more specialist mental health services for assessment and treatment. The key challenge is resourcing the development of community mental health services so that this care is provided as far as possible in the community and that acute admissions to hospital are kept to a minimum.
Community Mental Health Services
5.8 The main elements of community services are:
- Community mental health teams
- Home treatment
- Assertive outreach
- Crisis Response
5.9 The Community Mental Health Team provides emotional, social and practical support to service users who are living in the community with severe mental health needs. The aim of the Community Mental Health Team is to enable them to live as independently as possible.
5.10 The aim of the intensive Home Treatment service is to provide an acceptable non-restrictive alternative to acute inpatient care. While the crisis assessment portion of the service intends to avoid inappropriate admissions, the home treatment service offers choices that might replace admission entirely or significantly shorten the duration of that admission.
5.11 The Assertive Outreach service aims to proactively meet the needs of the most severely mentally ill clients in the community. Normally, it deals with service users who have been on a caseload of the Community Mental Health Team for at least six months. Access is restricted to those diagnosed with severe and enduring mental illness.
5.12 The team’s prime aim is to empower and enable people to manage their problems more effectively. Staff seek to enhance the quality of life and mental stability of service users and to encourage their participation in short and long term recovery by focusing on their strengths. They also work to reduce crisis admissions to hospital and to improve the efficacy of all admissions by providing consistent, planned and intensive support.
5.13 The Crisis Response Team is a flexible 24 hour service, delivered seven days per week to meet the needs of those experiencing acute mental health crisis. The service aims to enable individuals in crisis to remain in their own homes, where appropriate, by enabling qualified staff experienced in mental health matters to contact and provide assistance as soon as possible. The team works alongside existing mental health services and works in collaboration and partnership with primary care providers such as GPs in order to enhance service provision for those with mental illness in crisis.
5.14 Community mental health teams are in operation across Northern Ireland, but require more staff to provide an effective service. Home treatment, crisis response and assertive outreach services are operating in some areas, but these require considerable development. There are also specialist community based-services dealing with, for example, children and young people, those with addictions and eating disorders and those in contact with criminal justice services. An under 18s crisis intervention specific service is now operational in the Eastern and Southern Board Areas and is in the process of being put in place in the Northern and Western Areas.
Counselling & Psychotherapy Services
5.15 The term “Counselling” covers a wide range of services, which are provided in a range of settings by the voluntary and statutory sectors. Depending on the severity, treatment can be anything from informal befriending to more formal and intensive psychotherapy.
5.16 The Bamford Review acknowledged that psychological therapies are an important tool and should be routinely considered as an option when treating mental health problems. As an initial step to developing a strategy to improve access to psychological therapies, the Department has commissioned a mapping of existing training in and provision of psychological therapies.
5.17 The Department’s report ‘Counselling in Northern Ireland: Report of the Counselling Review’ (2002) made recommendations to improve the quality of counselling services. One of the key recommendations was that all counsellors and psychotherapists should be subject to statutory regulation and registration by the introduction of arrangements under development on a UK-wide basis. There are complex issues involved and it will be some time before statutory regulation will be introduced.
5.18 The Department has consulted on a draft set of standards of good practice for counselling services as an interim measure until statutory regulation is introduced. However, a decision has not been taken yet on how best to promote these standards.
In-Patient Beds
5.19 There are 6 psychiatric hospitals based on an old county asylum model throughout Northern Ireland with approximately 1200 available beds fro adults. There are also approximately 200 adult mental health beds available in other Psychiatric Units.
5.20 The Bamford review advocates moving away from large psychiatric institutions to smaller psychiatric units as part of general acute hospitals and with a smaller number of beds overall. This will be taken forward in the context of our capital investment strategies.
5.21 There are particular difficulties with inpatient beds for young people. Donard Ward at Knockbracken Health Care Park caters for adolescents from 14 – 17 years and currently provides 9 beds, which are all fully occupied. The Unit also provides up to 6-day care places. Work has recently been completed which will bring the capacity of the adolescent unit to 12 beds incrementally The Trust has also recruited additional nursing staff to support the delivery of care for these additional beds.
5.22 In the longer term, it is anticipated that around late 2009 / early 2010 a replacement 18-bedded unit will be open to provide care to adolescents with mental health needs. It is also planned to build a replacement 15 place children’s unit (under 14 years) on the same site as the adolescent unit and sharing some common facilities. The new units will provide an overall total of 33 places.
Risk Management
5.23 Mental Health Services continually face the challenge of determining and managing the risk that some people may pose either to themselves or others. In the vast majority of cases Mental Health Services provide safe and effective care, minimising such risks through good professional practice. Inevitably however some adverse incidents will occur.
5.24 A regional group on risk assessment and management in mental health services to ensure appropriate risk assessment and management procedures are in place has been established. This Regional Steering Group will oversee the development of standards, processes, policies and training strategies to enhance the assessment and management of risk in our local adult mental health services.
Alcohol and Substance Misuse
5.25 The Bamford has reported that the rates of co-occurrence of mental health problems and substance misuse problems are high. Approximately 1⁄3 of individuals with a mental disorder have experienced a substance misuse disorder, 1⁄3 of individuals with an alcohol problem have experienced a mental health disorder and 1⁄2 of individuals with an illicit drug problem have experienced a mental health problem.
5.26 Bamford has also reported that substance misuse is an important risk factor of suicide and homicide. In Northern Ireland the estimated risk of suicide in the presence of current alcohol misuse or dependence was found to be 8 times greater than in the absence of current alcohol misuse or dependence.
5.27 The Department is already implementing a New Strategic Direction in relation alcohol and drug misuse and a number of the recommendations in the Bamford review report are already being addressed within this.
Annex 1
Membership And Terms of Reference of the Suicide Prevention Taskforce
Terms of Reference
1 |
Develop a regional strategy for Northern Ireland for prevention of suicides, with particular reference to prevention of young male suicide. |
2 |
To produce an analysis of suicides and severe self harming in Northern Ireland in the last 5 years. |
3 |
Review the current provision in health, education and the voluntary sectors in prevention of suicide strategies including a review of the 10 action points in the Promoting Mental Health Strategy and Action Plan2. |
4 |
Review factors and relevant research on suicide and self harm in Northern Ireland; elsewhere in the United Kingdom and the Republic of Ireland; and evaluation of best practice in Northern Ireland and elsewhere. |
5 |
Consider and evaluate options and make recommendations for preventing suicide and self harm. |
6 |
Examine provision and scope for a dedicated helpline for Northern Ireland and examination of existing telephone counselling service provision within statutory and voluntary agencies. |
7 |
Examine option of developing greater links with existing voluntary agencies which provide counselling services in this sector. |
8 |
Design and implement a survey for Northern Ireland of families of suicide victims, those who have self harmed and those experiencing counselling and working professionally with potential suicide victims and individuals who severely self harm. |
9 |
Organise a conference in Belfast on Thursday 25 August 2005 to encourage debate and share best practice in Northern Ireland, elsewhere in the United Kingdom and the Republic of Ireland in prevention of suicide strategies. |
10 |
Provide an interim report by 31 October 2005. |
11 |
Provide final report by the end of the year, with a costed regional action plan. |
Membership
- Mr. Colm Donaghy, Southern Health and Social Services Trust (Chair)
- Dr. Brian Gaffney, Health Promotion Agency
- Mr. John McGeown, North and West Belfast Trust
- Mrs. Jo Murphy, North Belfast Partnership
- Mrs. Patricia McQuillan, Lenadoon Counselling Project
- Mr. Malcolm Emery, Rural Support
- Mr. Shay McGovern, Department of Health & Children
- Dr Stephen Bergin, Southern Health and Social Services Board
- Ms. Madeline Heaney, Northern Health and Social Services Board
- Mr. Barry McGale, Westcare Business Services
- Mrs. Maureen Ferris, Eastern Health and Social Services Board
- Mr. Pat McGreevy, Down Lisburn Trust
- Dr. Philip McGarry, The Royal College of Psychiatrists
- Dr. Ian Wales, Royal College of General Practitioners
- Mr. Joe Ferns, Samaritans
- Mr. Hugh McCann, Principal of St Colman’s High School
- Ms. Irene Ooi, Juvenile Justice Centre for NI
- Ms. Helen McNamee, The Rainbow Project
- Ms. Sally Newton, N Ireland Prison Service
- Ms. Dorothy Angus, Department of Education
- Mr. Mark O’Donnell, Department of Social Development
- Mr. Anthony Langan, Samaritans
- Mr. John McCavana, Department of Education
- Dr. Denise O’Hagan, Southern Health and Social Services Board
- Dr. Glenda Mock, Department of Health Social Services and Public Safety (DHSSPS)
- Dr. Tracy Power, DHSSPS
- Mr. Charlie Bamford, DHSSPS
- Mrs. Pat Osborne, DHSSPS
- Mr. Aidan McCann, DHSSPS
- Mr. John Breen, DHSSPS
- Mr. Martin Bell, DHSSPS
- Mr. Gary Maxwell, DHSSPS
Annex 2
Update of the Section 75 Analysis of Suicide and Self-harm in Northern Ireland (2002-2006(P))
Information Analysis Directorate
Annex 2, Castle Buildings
Stormont Estate
Introduction
Of the various causes of death in Northern Ireland, suicide is regarded as being one of the most tragic and difficult to understand. It is now one of the major causes of death in young adults, particularly young males and various studies have indicated that it is on the rise. Incidents of self-harm are also seen to be on the increase. While this is not the same as attempted suicide those who self-harm are more likely to go on to die from suicide and level of self-harm may thus be a helpful indicator in identifying those persons more at risk[1]. This paper presents an analysis of data held by the General Register Office (GRO) and the Hospital Inpatients System (HIS) regarding deaths due to suicide and incidents of self-harm over the last five years in Northern Ireland, examining its impact on the various Section 75 equality groups.
Recording suicide in Northern Ireland
When a death is suspected to be a suicide, the death is referred to a coroner and goes through a formal inquest. Upon completion the coroner will provide a summary of findings to the Registrar and the death is coded by the General Register Office (GRO) of Northern Ireland. It is usually evident from the coroner’s finding whether or not the death is a suicide. In cases where it is unclear, GRO staff will contact the coroner for further clarification before coding the death using the International Statistical Classification of Diseases and Related Health Problems (ICD)[2], as a ‘suicide’ or death by ‘self-inflicted injury’. In some cases a death by ‘events of undetermined intent’ is recorded where the intent is unclear or the coroner is reluctant to say that the death was a suicide.
This process, particularly the inquest, results in a time delay between the actual death occurring and the date the death is registered, which can be up to several years. Based upon GRO data from 1999 to 2003 and including deaths due to undetermined events, only 24.3% of suicides are registered within six months of the actual death occurring, 69.4% are registered within a year and 2.9% take two years or more. This means a long period of time can pass before a complete picture of the total number of suicides occurring in a given year is available.
With the exception of 2005 and 2006(P) in which deaths have probably occurred but have not yet been registered, the figures from 1990 onwards are quite close when comparing occurrences and registrations, with the increasing trend in suicides being present in both sets of figures. These differences however are variable with no direct relationship between the two existing.
Comparing deaths data with registrations data shows only a small disparity between the figures. Given the closeness of the figures and the time delay in obtaining a full years set of suicide figures the approach of reporting suicides by year of registration will be used (this is consistent with the way death statistics are reported by NISRA[3] and ONS[4]). This is particularly important when looking at the most recent data available as the registrations will give a more accurate impression of the trends in recent years, whereas the death figures give a false impression of falling rates.
Deaths from undetermined intent
In reporting statistics on suicide, it is conventional to combine cases where the cause of death is classified as ‘suicide and self-inflicted injury’ with cases where the cause of death is classified as an ‘event of undetermined intent’[5]. Both NISRA and ONS quote the combined figures whenever producing statistics on suicide but are clear that they include deaths due to events of undetermined intent. Traditionally however, DHSSPS has quoted figures solely using the ‘suicide and self-inflicted injury’ category. This report adopts the more general approach of combining the two sets of figures and the term ‘suicide’ will cover both sets of deaths.
2006 Death figures
At the time of issuing this report, finalised death figures had not yet been published by the General Register Office. Death figures for 2006 should be treated as provisional.
Suicide rates in Northern Ireland
During the period 1991 to 2006(P) there were 2,629 registered deaths from suicide in Northern Ireland. The number of suicides registered peaked in 2006(P)[6] with 291 suicides while the lowest number of suicides in this time period occurred in 1992 when there were 128 cases. Table 1 illustrates the increasing trend in suicide registrations but also highlight the considerable variation each year in the number of cases. Consistent trends are not immediately apparent. For instance, the 21.3% decrease from 183 incidents of registered suicides in 2002 to 144 incidents in 2003 is not necessarily an indication of a change in the trend.
Table 1: Number of suicides (1991-2006(P))
Year |
1991 |
1992 |
1993 |
1994 |
1995 |
1996 |
1997 |
1998 |
1999 |
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006(P) |
All |
148 |
128 |
151 |
151 |
146 |
143 |
138 |
150 |
154 |
185 |
158 |
183 |
144 |
146 |
213 |
291 |
Male |
105 |
103 |
120 |
117 |
105 |
114 |
108 |
113 |
127 |
140 |
132 |
142 |
112 |
105 |
167 |
227 |
Female |
43 |
25 |
31 |
34 |
41 |
29 |
30 |
37 |
27 |
45 |
26 |
41 |
32 |
41 |
46 |
64 |
Suicide levels in Northern Ireland
There are approximately 15,000 deaths in Northern Ireland each year with 72,158 recorded in total in the five year period from 2002 to 2006(P). Over this period, suicide represented 1.4% of these deaths. For the purpose of this analysis we will refer to such a percentage (i.e. the percentage of deaths which have suicide attributed as the cause) as the suicide level.
Equality Groups
Suicide information is taken from information on deaths recorded by the General Register Office, which does not record data on all nine equality groups outlined in the Northern Ireland Act (1998). Information is only readily available for sex, age and marital status. However the full postcode is recorded which allows various geographical comparisons to be made.
This analysis will mostly examine the impacts of suicide on equality groups in two ways. Firstly, the suicide level across each group will be compared and contrasted (i.e. the proportion of deaths attributable to suicide that occurred during 2002 and 2006(P)). A limitation of this approach is that all deaths are understandably dominated by older persons whose characteristics can differ from younger persons (e.g. marital status). The second method compares the average number of suicides each year for each equality group expressed as a proportion of the total population within each group (2004 Mid Year Estimate of Population (MYE)). As the numbers tend to be quite small, the average suicide rate will be expressed as a ratio of each 100,000 persons in the population. Both methods will be used in conjunction to attempt to ascertain differential impact.
Sex
Overall males accounted for almost four-fifths of the 977 suicides (77.1%) that occurred in Northern Ireland between 2002 and 2006(P).
Figure 1: Proportion of all deaths due to suicide by sex
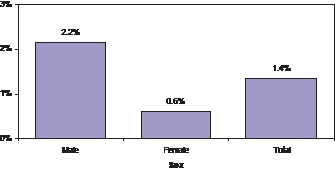
Overall the suicide level for males (2.2%) was considerably higher than that of females (0.6%). This shows that there is differential impact acting against males.
Figure 2: Average suicide rate per 100,000 persons by sex
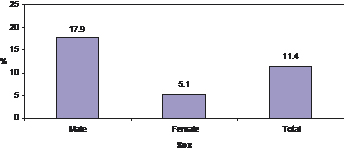
On average there were 17.9 male suicides per 100,000 persons, which compares with 5.1 female suicides. This provides further strong evidence of differential impact acting against males.
Age
Almost two fifths of all suicides in NI that occurred during 2002 and 2006(P) were carried out by persons in the 15 to 34 age group. A further third of suicides were carried out by those in the 35 to 49 age group. The mean age for all those committing suicide was 40 years of age, while the median[7] age is 39 years old.
Figure 3 below shows the proportion of all deaths due to suicide by age band. It is clear that there is a distinctive pattern across the age bands.
Figure 3: Proportion of all deaths due to suicide by age band
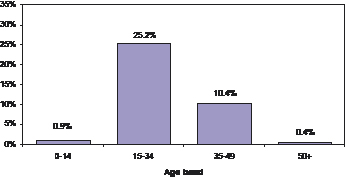
One quarter of all deaths (25.2%) of persons aged between 15 and 34 years of age between 2002 and 2006(P) were attributable to suicide. This compares with 10.4% of those aged 35 to 49 years of age. Suicides accounted for proportionately few of the deaths of those aged 14 years and under and those aged 50 years and above. Therefore it would appear that there may be potential differential impact against the 15 to 34 age group.
Figure 4: Average suicide rate per 100,000 persons by age band
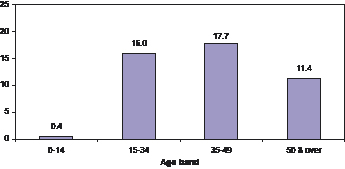
Comparing the numbers of suicides with the 2004 MYE shows that the 35 to 49 age group has the highest numbers of suicides per 100,000 persons (17.7).
Religion
The information recorded by GRO for deaths does not include the religion of the deceased person. However by using the full postcode, which is recorded, it is possible to assign a proxy for religion. Using information from the 2001 Census of Population, the religious composition of each Census Output Area (COA) can be determined. The postcode allows each death (and therefore incidence of suicide) to be assigned to a COA. For the purposes of this analysis, an area that has 80% or more of its resident population being Protestant is deemed to be a predominantly Protestant Area. Similarly an area with a population that is 80% or more Roman Catholic has been deemed a predominantly Catholic Area. All other areas are assumed to be of mixed composition, or not determined. The Census population figure for each COA was updated with age and gender specific population growth rates derived from 2004 population mid-year estimates in order to update the population weights.
Overall, 35.3% of the population were living in predominantly Protestant Areas, 26.2% in predominantly Catholic Areas and 38.5% in fairly mixed Areas. Within all the areas deemed Protestant and according to the 2001 census, 89.3% of the population were Protestant. Within all the areas deemed mostly Catholic, 93.8% of the population were Roman Catholic. Within the “Fairly Mixed Areas” 52.4% of the population were Protestant and 43.8% were Catholic.
Figure 5: Proportion of all deaths by proxy religion
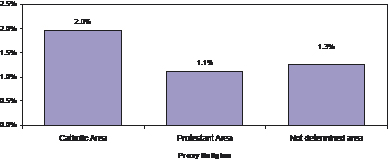
As can be seen from figure 5, suicides account for a higher proportion of deaths in predominantly Catholic areas (2.0%) than in Protestant areas (1.1%) or mixed areas (1.3%). This might suggest that there is differential impact acting against Roman Catholics. However a firm conclusion on whether differential impact exists cannot be reached due to the fact that there will be a substantial proportion of Catholics living in mixed areas. The observed effect could in fact be an area effect, in that it is due to the relative affluence/deprivation or rurality present in each area.
Figure 6: Average suicide rate per 100,000 persons by proxy religion
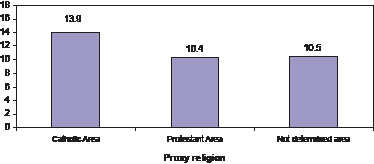
Comparing the average suicide rate between 2002 and 2006(P) with the composition of wider population, shows that a higher suicide rate per 100,000 persons occurred in predominantly Catholic areas (13.9) than in Protestant (10.4) and mixed areas (10.5).
Marital status
Figure 7: Proportion of all deaths due to suicide by marital status
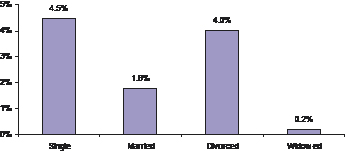
From figure 7 it can be seen that the single marital status group witnesses the highest proportion of suicides when looking at all deaths. There is also a high level within the divorced marital sector, however this figure is high due to the fact that it is a proportion of total deaths and there are also low numbers of deaths in this group. When the divorced and widowed groups are combined the results are very different, contributing only 0.6 % of total deaths for these groups.
Figure 8: Proportion of all deaths due to suicide by marital status and sex
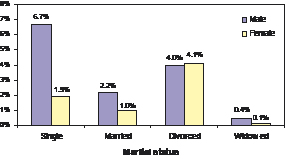
The suicide level amongst the male single marital status group (6.7%) was considerably higher than in the other groups. This would suggest that there is differential impact against the single male group. Although the lower suicide levels among the married and widowed groups may be due to some extent to the age distribution of deaths (a large proportion of deaths occur in the older population). It is notable that there are also high proportions of suicides in the female divorced marital status group (4.1%). This is unusual as suicide levels tend to be dominated by males.
Further disaggregations
Further analysis is required to establish whether the observed effects constitute actual differential impact and that they do not occur due to interactions with other variables.
Gender and age
Figure 9: Proportion of all deaths due to suicide by sex and age band
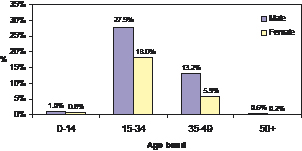
The suicide level for males was higher than for females across each age band. In the 15-34 age band the male suicide level was almost 50% higher than that for females. Also in the 35-49 age bands, the male suicide level was more than twice that for females. Therefore age does not provide an explanation of the overall gender difference. As with males, suicide within the 15-34 age band accounts for the largest proportion of females deaths. This would suggest that there is also an age effect present.
Gender and religion
Figure 10: Proportion of all deaths due to suicide by proxy religion and sex
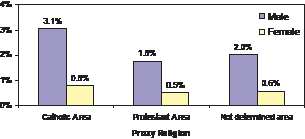
Suicides account for around four times the proportion of all male deaths than female deaths across each category. The male and female figures show a similar trend to the overall figures (see fig 5) with suicides in predominantly Catholic areas accounting for one and a half times the proportion of deaths within the other areas. Therefore it can be concluded that the slight religion or area effect cannot be explained by differences in gender composition.
Age and religion
Figure 11: Proportion of all deaths due to suicide by proxy religion and age band
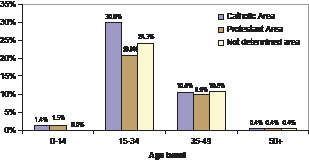
Suicide levels by age band are broadly similar across the majority of categories although the 15-34 proportion is higher in predominantly Catholic areas than in Protestant and mixed areas.
Marital status and gender
Figure 12: Proportion of all deaths due to suicide by marital status and sex
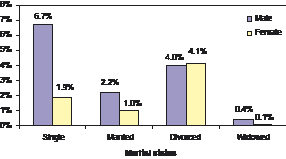
Although the proportion of deaths that can be attributed to suicide was higher for males than females across the majority of marital status groups, the obvious disparity with the proportion of single males with all other groups would indicate differential impact acting against single males.
Marital status and age
Figure 13: Proportion of all deaths due to suicide by age band and marital status
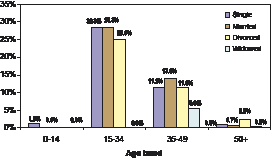
Figure 13 shows a clear age effect with the highest proportions of all deaths due to suicides occurring within the 15-34 age band. Apart from the widowed group, the proportions of suicides within each marital status group in the 15 to 34 age group are broadly similar.
Conclusion – Equality groups
From the analysis, there is evidence of a strong differential impact against males and also the 15-34 age group. There also seems to be a lesser differential impact against ‘predominantly Catholic areas’ which cannot be explained by differences in sex and age. However due to the fact that a large proportion of all Roman Catholics actually live in mixed areas, no firm conclusion can be reached on whether there was real differential impact. The apparent differential impact in predominantly Catholic areas may actually be due to the deprivation/rurality of these areas. Any apparent differential impact on the single marital status group can be explained by differences in the sex and age composition of the group.Rurality
Overall, approximately one third of the population in Northern Ireland (35%) live in rural areas. A higher proportion of the population in rural areas (50.7%) were male than in urban areas (47.9%). Very similar proportions of the population in rural (48.83%) and urban (48.85%) areas were aged 34 years or less.
Figure 14: Proportion of all deaths due to suicide by rurality
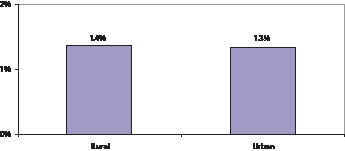
Figure 15: Average suicide rate per 100,000 persons by rurality
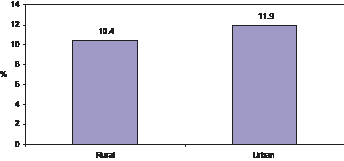
Overall suicides accounted for the same proportion of all deaths in both rural and urban areas (see figure 14). However, there was a higher average number of suicides per 100,000 persons in urban areas (11.9) than in rural areas (10.4).
Rurality by sex
Figure 16: Proportion of All deaths due to suicide by rurality and sex
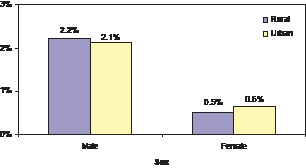
Figure 17: Average suicide rates per 100,000 persons by rurality and sex
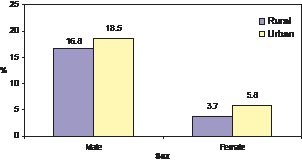
The proportion of all deaths accounted for by suicides was broadly similar for both males and females in rural and urban areas (fig 16). The average suicide rate per 100,000 persons was higher in urban areas for both males and females.
Rurality by age band
Figure 18: Proportion of all deaths due to suicide by rurality and age band
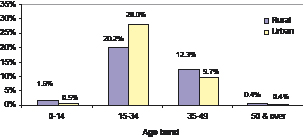
Figure 19: Average suicide rate per 100,000 persons by rurality and age band
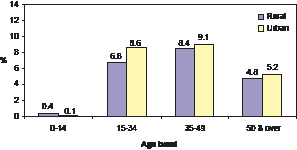
Apart from the 15-34 age group, the proportions of all deaths due to suicide were broadly similar across age bands in urban and rural areas. Within the 15-34 age group, the proportion of suicides for urban areas (28.0%) was almost one and a half times the proportion in rural areas (20.2%). The average suicide rate per 100,000 persons for both the 15-34, 35-49 and 50 & over age bands was higher in urban areas (see figure 19).
Conclusion - Rurality
From this analysis, it would seem even when controlling for age and gender that suicide is more prevalent in urban areas. This is confirmed by comparing the proportion of deaths due to suicide of males in the 15-34 age group. The average suicide rate per 100,000 persons was notably higher in urban areas.
Economic Deprivation
Economic Deprivation is based on the Northern Ireland Multiple Deprivation Measure (2005), looking specifically at the Income, Employment and Proximity to Services Deprivation domains. The measure is calculated at Census Output Area (of which there are 5,022 in Northern Ireland). “Economically deprived” areas for the purpose of this analysis are defined as the top 20% most deprived Census Output Areas (1,004). Looking at the 2004 population figures (Census figs with 2004 MYE age and gender specific LGD growth rates), 18.9% of the overall population live in “economically deprived” areas. Broadly similar proportions of males and females live in economically deprived areas (18.5% and 19.3% respectively). However the population living in economically deprived areas tended to be younger with 52.5% of the population aged 34 or younger compared with 48.0% in non-deprived areas.
Figure 20: Proportion of all deaths due to suicide by economic deprivation
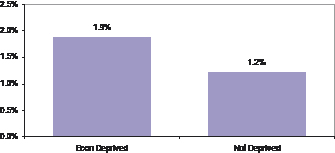
Figure 21: Average suicide rates per 100,000 persons by economic deprivation
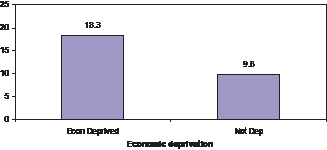
A higher proportion of all deaths were due to suicide in economically deprived areas (1.9%) than in non-deprived areas (1.2%). The average suicide rate per 100,000 persons in economically deprived areas (18.3) was twice that in non-deprived areas (9.8).
Economic Deprivation by sex
Figure 22: Proportions of all deaths due to suicides by economic deprivation and sex
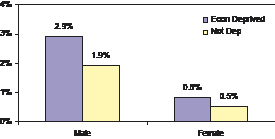
Figure 23: Average suicide rate per 100,000 persons by economic deprivation and sex
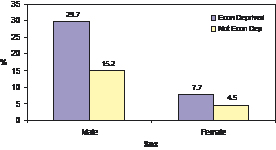
Both the suicide level and the average suicide rate per 100,000 persons were higher in economically deprived areas for males and females.
Economic deprivation by age band
Figure 24: Proportion of all deaths due to suicide by economic deprivation & age band
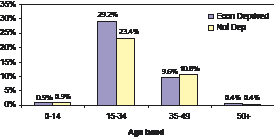
Figure 25: Average suicide rate per 100,000 persons by economic deprivation and age band
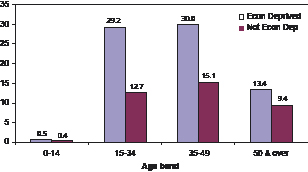
The proportion of deaths due to suicide was slightly higher in economically deprived areas for the 15-34 age group. The average suicide rate per 100,000 persons was higher in each age category in economically deprived areas, with the largest disparity occurring in the 15-34 and 35-49 age bands.
Conclusion- Economic Deprivation
Suicide is more prevalent in economically deprived areas than in non-deprived areas. The difference between deprived and non-deprived areas is more evident when looking at the suicide rate within the population than as a proportion of deaths. Economic deprivation offers one possible explanation of the higher prevalence of suicide in predominantly Catholic areas as 59.3% of these were economically deprived. This compares with 18.5% of predominantly Protestant areas and 15.0% of mixed areas.
Socio-economic Group
This analysis is based on the National Statistics Socio-economic Classification (NS-SeC) which has been used by GRO to classify deaths occurring since 2002.
Figure 26: Proportion of all deaths due to suicide by socio-economic group
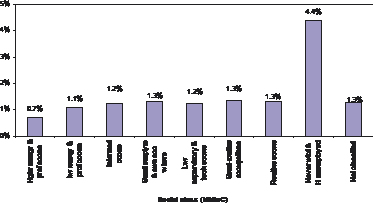
The highest suicide level was within the never worked and unemployed social class. Higher managerial and those in a professional occupation experienced the lowest suicide levels (0.7%). The suicide level amongst the other socioeconomic groups were broadly similar.
Geographical area
Local Government District (LGD)
Figure 27: Proportion of all deaths due to suicide by LGD
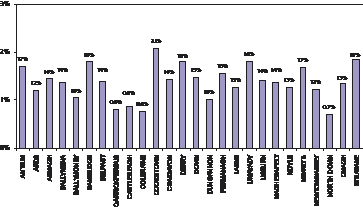
Figure 28: Average suicide rates per 100,000 persons by LGD
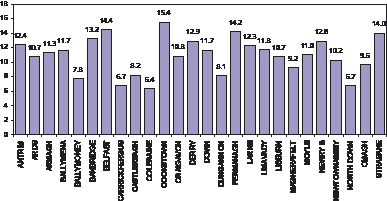
The highest suicide level occurred in Cookstown LGD (2.1%) whilst the lowest proportion was in North Down LGD (0.7%). Cookstown LGD (15.4) also had the highest average suicide rate per 100,000 persons and Coleraine LGD (6.4), the lowest. There were also relatively high average suicide rates in Belfast LGD (14.4), Fermanagh LGD (14.2) and Strabane (14.0).
Parliamentary Constituency Area (PCA)
Figure 29: Proportion of all deaths due to suicide by PCA
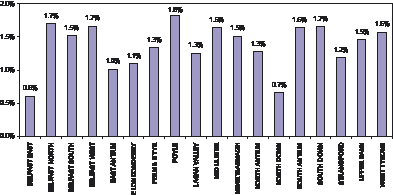
Figure 30: Average suicide rate per 100,000 persons by PCA
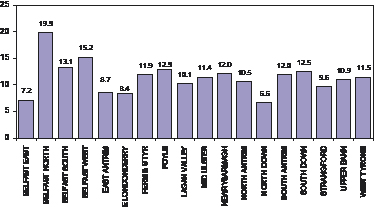
The highest proportion of all deaths due to suicide was in Foyle (1.8%) whilst the lowest was in Belfast East (0.6%). Belfast North and Belfast West had the highest average suicide rate per 100,000 persons (19.9 and 15.2 respectively). The lowest suicide rates were in North Down (6.6) and Belfast East (7.2).
Overall Conclusion - Suicide
Suicide is clearly most prevalent in males and young adults. However there is also evidence to suggest that it is more prevalent in urban and economically deprived areas. Cookstown LGD and Belfast North Parliamentary Constituency Area are relatively badly affected by suicide whereas Coleraine LGD and North Down PCA are least affected by the problem. Seemingly differential impact on the single marital status group can be explained by differences in the sex and age composition of each group whereas any impact on Roman Catholics may be explained by economic deprivation. Due to the limited equality data for deaths recorded by GRO, it is quite possible that there may be differential impact on other equality groups that have not been analysed such as sexual orientation, disability status, ethnicity and those with/without dependants.
Table 2: Summary table
Differential impact (Y/N) |
Against |
Possible causal factors |
|
Sex |
Y |
Males |
|
Age |
Y |
15-34 and to a lesser extent the 35-49 age groups |
|
Religion |
Y |
Catholics |
Economic Deprivation |
Marital status |
Y |
Single group, also potentially against widowed/divorced group (but could not confirm due to the relatively small numbers in the group) |
Sex and age |
Rurality |
Y |
Urban areas |
|
Economic Deprivation |
Y |
Economically Deprived areas |
Self Harm in Northern Ireland
The term self-harm covers a wide range of behaviours including parasuicide[8] and habitual self-cutting and poisoning which involves differing degrees of risk to life and differing degrees of suicidal intent. Incidents of self-harm which result in admissions to hospital are recorded in the DHSSPS Hospital Inpatients System (HIS) which uses the same International Statistical Classification of Diseases and Related Health Problems (ICD) used in the classification of deaths[9].
Over the five year period, 2002/03 to 2006(P)/07, the number of admissions to hospital[10] as a result of self-harm was 22,337 (Table 3)[11]. Admissions due to self-harm peaked in 2004/05 (4,704) and were lowest in 2006(P)/07 (4,027). Total admissions over this five year period due to self-harm represent 0.9% of all hospital admissions.
Table 3: Number of hospital admissions as a result of self-harm (2002/03-2006(P)/07[12])
Year |
2002/03 |
2003/04 |
2004/05 |
2005/06 |
2006(P)/07 |
Total |
Admissions as a result of self-harm |
4,591 |
4,517 |
4,704 |
4,498 |
4,027 |
22,337 |
All admissions |
487,518 |
508,824 |
521,123 |
532,670 |
537,198 |
2,587,333 |
% of all admissions |
0.94% |
0.89% |
0.90% |
0.84% |
0.75% |
0.86% |
While the numbers of admissions to hospital as a result of self-harm are high, the percentage of persons who die as a result of their injuries while in hospital is small. Such patients are likely to be registered as a death by suicide or event of undetermined intent by the General Register Office once any inquest is completed.
Equality groups
Currently the DHSSPS HIS only contains information on the sex and age equality groups. In order to compare the level of self-harm that is prevalent within each equality group, the average number of admissions each year between 2002/03 and 2006(P)/07 is expressed as a ratio to each 100,000 persons within the total population (2004 Mid Year Estimate (MYE)).
Sex
Females accounted for 12,267 of the total admissions to hospital (54.9%) for self-harm between 2002/03 and 2006(P)/07.
Figure 31: Average admissions as a result of self-harm per 100,000 persons by sex
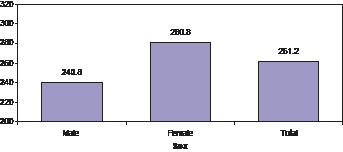
Overall, there was an average of 261.2 admissions per 100,000 persons as a result of self-harm in each year. Self-harm is more prevalent for females (with an average of 280.8 admissions per 100,000 persons) than males (240.8 admissions).
Age
Almost three-quarters of all self-harm admissions (73.7%) between 2002/03 and 2006(P)/07 were for persons aged 44 or younger.
Figure 32: Average admissions as a result of self-harm per 100,000 persons by age band
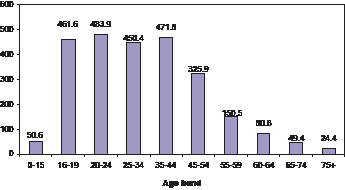
Noticeably, the highest average admission rates for self-harm were for persons aged between 16 and 44 years old. The admission rate was lowest for the very young (0-15 age group) and the very old (65-74 and 75+ age groups).
Figure 33: Average admissions as a result of self-harm per 100,000 persons by sex and age band
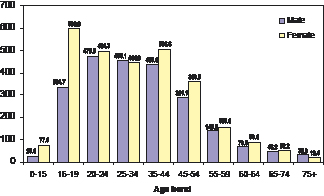
Females had a higher average admission rate than males for self-harm across every age band (except 25-34 and 75 & over). The highest average admission rate was for the female 16-19 age group (596.0) admissions per 100,000 persons. This compares with 334.7 admissions for the male 16-19 age group.
Conclusion – Equality groups
Due to a lack of equality information currently available, any equality impact assessment of self-harm will be extremely limited. It is clear that admissions for self-harm are more prevalent for females and also the population aged between 16 and 44 years old. Whilst it is unlikely that the apparent differential impact on females and certain age groups would totally disappear, some of the differences may be explained by other equality information, e.g. religion, marital status, sexual orientation etc.
Geographical area
Hospital
Figure 34: Average admissions for self-harm per 100,000 hospital admissions
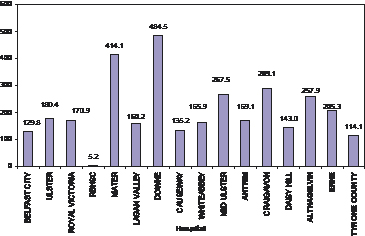
It should be noted that figure 34 does not include hospitals where none or only a very small number of admissions were made for self-harm. Down hospital (484.5) had the highest admissions for self-harm per 100,000 admissions. The Mater also has a high number of self-harm admissions per 100,000 admissions.
Figure 35: Average admissions for self-harm per 100,000 persons by Local Government District (LGD)
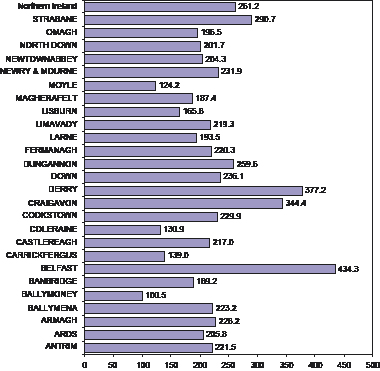
The highest average number of admissions for self-harm per 100,000 persons were in Belfast (434.3) and Derry (377.2) Local Government Districts. In contrast, Ballymoney LGD had the lowest admission rate for self-harm with an average of 100.5 admissions per 100,000 persons.
Figure 36: Average admissions for self-harm per 100,000 persons by Parliamentary Constituency Area (PCA)
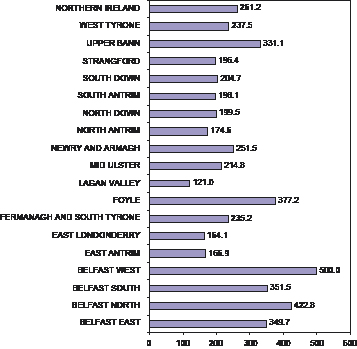
Belfast West PCA had the highest average number of admissions for self-harm per 100,000 persons (500.0). There were also relatively high average admission rates in Belfast North (422.8) and Foyle (377.2) PCAs. Lagan Valley PCA had the lowest admission rate for self-harm with an average of 121.0 admissions per 100,000 persons.
Annex A
ICD codes for intentional self-harm and event of undetermined intent
X60-X84 Intentional self-harm |
|
X60 |
Intentional self-poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics |
X61 |
Intentional self-poisoning by and exposure to antiepileptic, sedative-hypnotic, antiparkinsonism and psychotropic drugs nec |
X62 |
Intentional self-poisoning by and exposure to narcotics and psychodysleptics [hallucinogens], not elsewhere classified |
X63 |
Intentional self-poisoning by and exposure to other drugs acting on the autonomic nervous system |
X64 |
Intentional self-poisoning by and exposure to other and unspecified drugs, medicaments and biological substances |
X65 |
Intentional self-poisoning by and exposure to alcohol |
X66 |
Intentional self-poisoning by and exposure to organic solvents and halogenated hydrocarbons and their vapours |
X67 |
Intentional self-poisoning by and exposure to other gases and vapours |
X68 |
Intentional self-poisoning by and exposure to pesticides |
X69 |
Intentional self-poisoning by and exposure to other and unspecified chemicals and noxious substances |
X70 |
Intentional self-harm by hanging, strangulation and suffocation |
X71 |
Intentional self-harm by drowning and submersion |
X72 |
Intentional self-harm by handgun discharge |
X73 |
Intentional self-harm by rifle, shotgun and larger firearm discharge |
X74 |
Intentional self-harm by other and unspecified firearm discharge |
X75 |
Intentional self-harm by explosive material |
X76 |
Intentional self-harm by smoke, fire and flames |
X77 |
Intentional self-harm by steam, hot vapours and hot objects |
X78 |
Intentional self-harm by sharp object |
X79 |
Intentional self-harm by blunt object |
X80 |
Intentional self-harm by jumping from a high place |
X81 |
Intentional self-harm by jumping or lying before moving object |
X82 |
Intentional self-harm by crashing of motor vehicle |
X83 |
Intentional self-harm by other specified means |
X84 |
Intentional self-harm by unspecified means |
Y10-Y34 Event of undetermined intent |
|
Y10 |
Poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics, undetermined intent |
Y11 |
Poisoning by and exposure to antiepileptic, sedative-hypnotic, antiparkinsonism and psychotropic drugs, not elsewhere classified, undetermined intent |
Y12 |
Poisoning by and exposure to narcotics and psychodysleptics [hallucinogens], not elsewhere classified, undetermined intent |
Y13 |
Poisoning by and exposure to other drugs acting on the autonomic nervous system, undetermined intent |
Y14 |
Poisoning by and exposure to other and unspecified drugs, medicaments and biological substances, undetermined intent |
Y15 |
Poisoning by and exposure to alcohol, undetermined intent |
Y16 |
Poisoning by and exposure to organic solvents and halogenated hydrocarbons and their vapours, undetermined intent |
Y17 |
Poisoning by and exposure to other gases and vapours, undetermined intent |
Y18 |
Poisoning by and exposure to pesticides, undetermined intent |
Y19 |
Poisoning by and exposure to other and unspecified chemicals and noxious substances, undetermined intent |
Y20 |
Hanging, strangulation and suffocation, undetermined intent |
Y21 |
Drowning and submersion, undetermined intent |
Y22 |
Handgun discharge, undetermined intent |
Y23 |
Rifle, shotgun and larger firearm discharge, undetermined intent |
Y24 |
Other and unspecified firearm discharge, undetermined intent |
Y25 |
Contact with explosive material, undetermined intent |
Y26 |
Exposure to smoke, fire and flames, undetermined intent |
Y27 |
Contact with steam, hot vapours and hot objects, undetermined intent |
Y28 |
Contact with sharp object, undetermined intent |
Y29 |
Contact with blunt object, undetermined intent |
Y30 |
Falling, jumping or pushed from a high place, undetermined intent |
Y31 |
Falling, lying or running before or into moving object, undetermined intent |
Y32 |
Crashing of motor vehicle, undetermined intent |
Y33 |
Other specified means, undetermined intent |
Y34 |
Unspecified means, undetermined intent |
Y87.0, Y87.2 Sequelae |
|
Y87.0 |
Sequelae13 of intentional self-harm |
Y87.2 |
Sequelae of events of undetermined intent |
Annex 3
The “Protect Life – A Shared Vision” Quality Assurance Group
- Dr. Maila Upanne, National Research and Development Centre for Welfare and Health, Finland
- Professor Keith Hawton, Centre for Suicide Research, Oxford University, England
- Dr. Annette Beautrais, Canterbury Suicide Prevention Project, Christchurch, New Zealand
- McClelland, Chairman, Bamford Review of Mental Health & Learning Disability, Northern Ireland
- Denise O’Hagan, Western Health and Social Services Board, Northern Ireland
- Rory O’Conner, Suicidal Behaviour Research group, University of Stirling, Scotland
Annex 4
Suicide Prevention Action Plan
Section A – Population Approach
Action Area: Communities
Action To Be Taken |
Timescales |
Delivery Partners |
To initiate a major public information campaign that aims to de-stigmatise mental health, and promote awareness and understanding of issues relating suicide and self-harm. |
Short Term |
DHSSPS, HPA, HSS, local authorities, local community and voluntary partners. |
To support and encourage the development of community based suicide prevention initiatives and support mechanisms. |
Short Term |
DHSSPS, DSD, HSS, local authorities, local community and voluntary partners. |
To encourage all statutory public bodies to carry out health impact assessments on their policies, in terms of possible adverse effect on the mental health and wellbeing of local communities. |
Ongoing |
DHSSPS, all NICS Departments and Public Bodies, HSS, local authorities, HPA, PSNI and Prison Service. |
To restrict access to means and methods of suicide in our communities, including the identification of “hotspots”, the promotion of safer prescribing, a reduction in the accessibility of certain over the counter drugs, and restriction of access to firearms. |
Ongoing |
DHSSPS, Planning Authorities, local authorities, Health & Safety Executive, HSS, Police, Prisons, DSD, DARD, DOE. |
Action Area: Family
Action To Be Taken |
Timescales |
Delivery Partners |
To provide families with the opportunity to avail of non-stigmatising practical interventions to help consolidate parenting, coping, and life skills. |
Medium/Long Term |
DHSSPS, HSS, HPA, DE, DEL, DSD, local authorities, local community and voluntary partners. |
To ensure that in times of distress families have the opportunity to access a local emotional health and wellbeing support network, including community/voluntary sector provision. |
Medium Term |
DHSSPS, SSA, DSD,HSS, DE, DEL, local authorities, local community and voluntary partners. |
Action Area: Children and Young People
Action To Be Taken |
Timescales |
Delivery Partners |
To promote the inclusion of promoting positive mental health as a key element of the “Healthy Schools” programme and ensure that children and young people are protected from all forms of bullying |
Medium/Long Term |
DHSSPS, DE, DEL, HSS, local authorities, HPA, local community and voluntary partners. |
To raise awareness of, and ensure availability and timely access to, appropriate intervention services (e.g. Child and Adolescent Mental Health Services, mentoring schemes and other appropriate statutory and voluntary services) |
Short/Medium Term |
DHSSPS, DE, DEL, HSS, HPA, local authorities, local community and voluntary partners. |
To make suicide awareness and positive mental health & wellbeing training, including how to deal sensitively with disclosure of self-harm or suicidal behaviour, a priority for teachers, youth workers, etc. |
Short/Medium Term |
DHSSPS, DE, DEL, HPA, HSS, local authorities, local community and voluntary partners. |
To promote a culture of help seeking behaviour, particularly among young people |
Medium Term |
DHSSPS, DE, DEL, HPA, HSS, local authorities, local community and voluntary partners. |
Encourage the inclusion of coping and life skills, emotional literacy, and programmes that promote positive mental health in the school curriculum. |
Medium term |
DHSSPS, DE, DEL, HPA, HSS, local authorities, local community and voluntary partners. |
To develop and implement practices, protocols and referral pathways to smooth the transition from youth to adult Health and Social Services.. |
Medium Term |
DHSSPS, DE, DEL, HSS, HPA, local community and voluntary partners. |
Action Area: Health and Social Services
Action To Be Taken |
Timescales |
Delivery Partners |
To develop enhanced linkages between the Health and Social Services and the community/voluntary counselling and support network, particularly in relation to transition services and to bridge any gaps in service provision. |
Medium Term |
DHSSPS, HSS, HPA, local community and voluntary partners. |
To make depression and suicide awareness/prevention training a priority for all front line staff dealing with people in distress, particularly for GP’s, Primary Care and A&E staff in the HSS |
Short/Medium Term |
DHSSPS, HSS, HPA, SSA |
To develop clinical guidelines for all HSS staff to use when dealing with people who are at risk of suicide/self harm. |
Medium Term |
DHSSPS, HSS |
Action Area: Workplaces
Action To Be Taken |
Timescales |
Delivery Partners |
To implement a targeted information campaign aimed at enhancing the mental health and wellbeing of all members of the workforce. |
Short/Medium Term |
DHSSPS HPA, Health & Safety Executive, DEL, DETI, Trade Unions |
To ensure that positive mental health training is available to relevant members of the workforce including small/medium enterprise employers. |
Medium Term |
HPA, Health & Safety Executive, DHSSPS, DETI, DEL, Trade Unions |
Action Area: Police and Emergency Services
Action To Be Taken |
Timescales |
Delivery Partners |
To ensure that suicide prevention is included in all Emergency Services Public Service Agreements, and reflected in individual services annual priorities. |
Short/Medium Term |
DHSSPS, Police, Prison, Ambulance, Fire and Lifeboat Services. |
To make suicide awareness/intervention training a priority for all frontline emergency services staff. |
Short/Medium Term |
DHSSPS, Police, Prison, Ambulance, Fire and Lifeboat Services, NICS Departments. |
Action Area: Churches and Religious Bodies
Action To Be Taken |
Timescales |
Delivery Partners |
To support the development of enhanced links between churches/religious bodies and the local community support networks. |
Short/Medium Term |
DHSSPS, HSS, DSD, Churches/ Religious Bodies, local community and voluntary partners. |
To make suicide/depression awareness type training available for all church/religious leaders. |
Short/Medium Term |
DHSSPS, HSS, Churches/ Religious Bodies, local community and voluntary partners. |
Action Area: Media
Action To Be Taken |
Timescales |
Delivery Partners |
To work with the National Union of Journalists, and the Association of Editors, in relation to implementation of effective media guidelines in relation to the reporting of suicide and self-harm issues. |
Short Term |
DHSSPS, HPA, NUJ, Association of Editors, Voluntary and Community Partners |
To pro-actively work with the media to promote positive mental health and raise awareness of sources of support for individuals or families experiencing mental health problems. |
Short/Medium Term |
DHSSPS, HPA, NUJ, Association of Editors, Voluntary and Community Partners |
To develop and implement appropriate media monitoring mechanisms. |
Short/Medium Term |
DHSSPS, HPA, NUJ, Association of Editors, Voluntary and Community Partners. |
To provide media volunteer training for nominated Bereaved Families Representatives. |
Short Term |
DHSSPS, HPA, Voluntary and Community Partners, Bereaved Family Members |
Section B – Targeted Approach
Action Area: Self-Harm
Action to be Taken |
Timescale |
Delivery Partners |
To ensure that responsive self-harm support services, including mentoring support, are in place in all Health & Social Service Trusts. |
Short/Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
To implement programmes that enhance the coping and problem solving skills of those who self-harm, and which reduce the risk of repeat self-harm |
Short/Medium Term |
DHSSPS, HSS, DE, DEL, HPA, Local Community and Voluntary Partners |
To improve detection of, and access to, support services for people who engage in less serious forms of self harm |
Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
Action Area: Mental Illness
Action to be Taken |
Timescale |
Delivery Partners |
To ensure that those in contact with Mental Health Services are followed up at appropriate intervals, with assertive outreach where necessary, to assess suicide and self-harm risk. |
Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
To ensure that all Health & Social Service Trusts, and other relevant bodies, have pro-active suicide awareness/intervention programmes in place for staff who work with people who have mental health difficulties. |
Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
To provide appropriate support and information to promote awareness of suicide risk among people caring for someone with a mental illness. |
Ongoing |
DHSSPS, HSS, Local Community and Voluntary Partners |
To provide timely and appropriate support and follow up for patients discharged from psychiatric units |
Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
Action Area: Drug and Alcohol Misuse
Action to be Taken |
Timescale |
Delivery Partners |
To ensure that appropriate suicide awareness/intervention training is available for all frontline health services staff, police officers, and other relevant professionals who come into contact with people with alcohol and drug problems. |
Short/Medium Term |
DHSSPS, HSS, SSA, Local Community and Voluntary Partners, PSNI, DE |
To develop agreed protocols concerning the assessment and management of patients at risk while under the influence of drugs and/or alcohol. |
Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners, PSNI |
Action Area: Young Males
Action to be Taken |
Timescale |
Delivery Partners |
To ensure that targeted outreach programmes for young males, who may be at risk of suicide and self-harm, are available in local communities and in all Health & Social Service Trusts. |
Short/Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners, Youth Justice, PSNI, DSD, DEL, DE |
To implement a targeted information and awareness campaign for young males, aimed at breaking down the current male culture of not discussing their problems openly. |
Short/Medium Term |
DHSSPS, HPA, Local Community and Voluntary Partners, DE, DEL |
To enhance the role of the community/voluntary sector concerning the provision of mentoring support for young people at risk of suicide and self-harm. |
Short/Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
Action Area: Bereaved By Suicide
Action to be Taken |
Timescale |
Delivery Partners |
To ensure that accessible information and timely support, both at community/voluntary and statutory level, is available to all those bereaved by suicide, and to encourage the development of support groups/networks. |
Short/Medium Term |
DHSSPS, HSS, HPA, Local Community and Voluntary Partners, HPA |
To work with the Corners Office to facilitate the provision of sensitive and timely information to those bereaved by suicide. |
Short Term |
DHSSPS, Coroners Office, HPA, Local Community and Voluntary Partners, HPA |
To raise awareness among local health and education service providers, especially within Primary Care and education settings, of the increased risk of self-harm and suicide among those bereaved or affected by suicide. |
Ongoing |
DHSSPS, HPA, HSS, DE, DEL, Local Community and Voluntary Partners |
Action Area: Survivors of Sexual, Physical and Emotional Abuse
Action to be Taken |
Timescale |
Delivery Partners |
To provide an accessible support network in local communities for all survivors of abuse. |
Short/Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners, PSNI |
To initiate an information campaign that seeks to sensitively raise awareness of the increased risk of suicide among all survivors of abuse, and encourage survivors of abuse to seek help in times of crisis. |
Short/Medium Term |
DHSSPS, HSS, HPA, Local Community and Voluntary Partners, PSNI |
To make training available to support workers for survivors of abuse. |
Short/Medium Term |
DHSSPS, HSS, HPA, Local Community and Voluntary Partners |
Action Area: Marginalised and Disadvantaged Groups
Action to be Taken |
Timescale |
Delivery Partners |
To ensure that appropriate support services reach out to all marginalised and disadvantaged groups, in particular lesbian, gay, bi-sexual, and transgender groups, rural communities, ethnic minorities, and to those people who are economically deprived. |
Short/Medium Term |
DHSSPS, HSS, Local Community and Voluntary Partners |
To initiate a targeted information campaign that seeks to sensitively raise awareness of the increased risk of suicide among those groups identified as marginalised and disadvantaged, and encourages them to seek help at times of crisis. |
Short/Medium Term |
DHSSPS, HSS, HPA, Local Community and Voluntary Partners |
Action Area: High Risk Occupations
Action to be Taken |
Timescale |
Delivery Partners |
To raise awareness of high risk occupations and develop a culture of help seeking among people in occupations that have a high risk of suicide and self-harm. |
Medium Term |
DHSSPS, HSS, Local Community/Voluntary Partners, DEL, DETI, DARD, Health & Safety Executive, Trade Unions |
To develop a crisis plan for targeting people in high risk occupations, as and when emergency situations arise. |
Short Term |
DHSSPS, HSS, Local Community and Voluntary Partners, DEL, DETI, Health & Safety Executive, Trade Unions |
Action Area: Prisoners
Action to be Taken |
Timescale |
Delivery Partners |
To make appropriate mental health and suicide awareness, prevention and intervention training a priority for all frontline prison and police custody staff, and where possible identified “listener” inmates. |
Medium/Long Term |
DHSSPS, Prison Service, PSNI, Local Community and Voluntary Partners, “Listener” Inmates |
To ensure that the environment for those held in custody, in both prison and police stations, has been suitably adapted to reduce the possibility of suicide. |
Medium Term |
DHSSPS, Prison Service, PSNI |
To work with the Prison Service to provide access to appropriate services for all prisoners with mental health difficulties illness, including the development of appropriate “listener” groups. |
Medium Term |
DHSSPS, Prison Service, PSNI, HSS, Local Community and Voluntary Partners |
To ensure that all remand and sentenced prisoners continue to receive initial and ongoing monitoring of their mental health, and assessment of their risk of suicide. |
Ongoing |
DHSSPS, Prison Service, PSNI, HSS |
To liaise with the prison and probation service about the provision of follow-up support for those who have been recently released from custody. |
Short Term |
DHSSPS, Prison Service, Probation Service, Local Community and Voluntary Partners |
To provide appropriate support in relation to the removal of stigma from those who have been released from custody without charge. |
Short Term |
DHSSPS, Prison Service, PSNI, Local Community and Voluntary Partners |
Section C – Overarching Recommendations
Recommendations |
Timescale |
Delivery Partners |
To liaise with the Coroners Office to minimise delays in the reporting of suicide, and to ensure increased sensitivity to the needs of bereaved families |
Short Term |
DHSSPS, HPA, Coroners Office, PSNI, GRO |
To liaise with the Coroner’s Office and the General Registrar’s Office to further enhance the classification and recording arrangements for deaths by suicide |
Short/Medium Term |
DHSSPS, HPA, Coroners Office, PSNI, GRO. |
To develop and pilot a self-harm register in local A&E departments, in conjunction with our counterparts in the Republic of Ireland. |
Short/Medium Term |
DHSSPS, HSS. |
To develop a mechanism to allow timely access to statistics and geographical/demographic information at local level so that potential clusters of suicides/self-harm can be identified early and appropriate preventative action taken |
Medium/Long Term |
DHSSPS, HSS, HPA, Coroners Office, PSNI, GRO. |
To initiate further in-depth research into the underlying causes of suicide and self-harm in Northern Ireland |
Medium Term |
DHSSPS, HSS, Local Community/Voluntary Partners |
To review the suicide reduction targets highlighted in the strategy, and in particular the baseline figures used for the establishment of these targets |
Short Term |
DHSSPS, HSS, DFP |
To undertake a long-term study on the effectiveness of interventions on the general population |
Long Term |
DHSSPS, HPA. |
To initiate research into the additional risk factors faced by the “new populations”, in conjunction with our counterparts on the Republic of Ireland |
Short / Medium Term |
DHSSPS, HSS, local authorities, local community and voluntary partners. |
To identify areas of co-operation on a North/South basis, including research, reporting mechanisms, and public information. |
Short/Medium Term |
DHSSPS, HPA, Department of Health and Children, Health Service Executive (ROI) |
Annex 5
The Suicide Strategy Implementation Body
Terms of Reference
Chair: Colm Donaghy
Role: The SSIB will oversee and co-ordinate the implementation of the Northern Ireland Suicide Strategy. The SSIB will not directly be responsible for the allocation of funding.
Secretariat: DHSSPS Investing for Health Team
Term of Office: Initially 1 year, pending consideration of the implementation of the Bamford review.
Primary Functions
- To facilitate and oversee the implementation of the recommendations and various actions within the strategy.
- To drive forward the implementation of the strategy by providing strong and visible leadership.
- To oversee and monitor the progress of the various suicide prevention pilot projects established by the Minister.
- To provide advice and strategic direction on all relevant issues relating to suicide and self-harm.
- To facilitate the establishment of a bereaved families forum.
- To develop intermediate milestones for achievement of the targets in the Strategy.
- To consider the need for additional resources to assist effective implementation and monitoring of the Strategy and Action Plan.
- To monitor progress against targets and produce a report on progress on implementation for the Ministerial Group on Public Health at the end of year one.
- To agree a process for the investment of available resources, and to monitor as appropriate.
- To undertake an annual review of the implementation of the suicide strategy
Performance Management Arrangements
- To develop appropriate data collection arrangements in order to allow for monitoring of progress.
- To develop a mechanism for regular reporting to the SSIB by relevant organisations.
- To identify barriers to progress and report feedback to MGPH and relevant organisations.
- To publicise progress.
Membership
- Colm Donaghy, Chief Executive of the Southern Health and Social Care Trust (Chair)
- Dr Brian Gaffney, Health Promotion Agency
- Barry McGale, Western Health and Social Services Board
- Madeline Heaney, Northern Health and Social Services Board
- Hugh O’Connor, Eastern Health and Social Services Board
- Stephen Bergin, Southern Health and Social Services Board
- Dorothy Angus, Department of Education
- Harry Gracey, Department of Agriculture and Rural Development
- Mervyn Langtry, Department of Employment and Learning
- Angela Clarke, Department for Social Development
- Kevin Toner, Health and Safety Executive
- Pat Osborne, Department of Health, Social Services and Public Safety
- Maureen McCartney, Department of Health, Social Services and Public Safety
- Geoff Day, National Office of Suicide Prevention (ROI)
- Anthony Lagan / Suzanne Costello, Samaritans
- Colin Smallwood, NEXUS
- Colin Loughran, Action Mental Health
- Pat McGreevy, South East Health and Social Care Trust
- Dr Judith Lee, Northern Ireland Association for Mental Health
- Denis McKay, North Antrim Community Network
- Ivor Mitchel, Bangor YMCA
- Michael Goodman, South Belfast Highway to Health
- Alan Craig, Northern Ireland Prison Service
- Mirjam Bader, Rainbow Project
- Miss Blanaid McKinney – Rural Support
- Ms Judy Colhouln, Aware
- Michael Doherty, Lenadoon
- Jo Murphy, PIPS
- Anne Bill, FASA
- Yvonne Davidson, Police Service of Northern Ireland
- Six Bereaved Families Representatives from across NI
Annex 6
All–Island Action Plan on Suicide Prevention
An All-Island Action Plan on suicide prevention has been developed in conjunction with the National Office of Suicide Prevention in the RoI.
The plan consists of a rolling list of items which are considered to have the potential to enhance the lives of those people in crisis across the Island, and the potential for this co-operation is also reflected in the respective strategies (Protect Life – A Shared Vision (2006) NI and Reach Out (2005) RoI). Items currently listed for action are as follows:
All-Island Plan: Overview
1. Training
2. Resource Officer/Co-ordinators meetings
3. Media Watch/Volunteers/Guidelines
4. Men’s Health Forum
5. Registry of Self Harm
6. Suicide Data Collection Arrangements
7. Awareness campaign
8. Co-operation and Working Together (CAWT)
9. Implementation Groups Membership
10. XXIV Biennial Congress of the International Association of Suicide Prevention
To date significant progress has been made on the following action areas
1 Training
Training in Safe Talk, a new intervention programme, took place in June 2007 with trainers from north and south participating. Safe Talk is a shortened version of ASIST Training (Applied Suicide Intervention Skills Training).
The Health Promotion Agency (NI) have appointed a training officer for mental health and suicide prevention, and the National Office for Suicide Prevention (RoI) have appointed a national training and development officer – offering an opportunity for joint strategic planning and evaluation of all relevant training. Both officers have already met on a number of occasions.
3. Media Watch/Volunteers/Guidelines
Headline, which was officially launched in the Republic of Ireland in April 2007, is a national media monitoring programme, working to promote responsible and accurate coverage of mental health and suicide related issues within the media. Headline has been operational now for over a year and is seeking to change/improve the media’s coverage and portrayal of suicide/mental health.
Preliminary discussions have already taken place with colleagues in Northern Ireland and the NI Suicide Strategy Implementation Body supports the establishment of an NI version of headline.
4. Registry of Self-Harm
A National Registry of Deliberate Self-Harm has been operating in hospitals in the Rep of Ireland since 2001. Following consultation with the Suicide Strategy Implementation Body in Northern Ireland, a sub-committee was established to to oversee the piloting of the registry in the Western Health & Social Services Board area. The pilot data collection scheme will use the same methodology as that used by the National Suicide Research Foundation in the South.
5. Awareness Campaign
Phase One of an all-island mental health awareness campaign was launched in March 2007. TV and cinema adverts have been produced and other promotional materials have been widely disseminated. Development of Phase Two of the campaign was led by the National Office for Suicide Prevention and was launched on 9th October. The aim of the campaign is to positively influence public attitudes on mental health, and follows on from that originally developed in NI.
10. XXIV Biennial Congress of the International Association of Suicide Prevention
As co-sponsors of the world congress, both the HSE’s National Office for Suicide Prevention and the Department of Health, Social Services and Public Safety in NI were represented on the Organising Committee for this event. The World Congress offered an important and unique opportunity to highlight progress in implementing the respective suicide prevention strategies, and to highlight the ongoing all-island cooperation.
The congress was attended by over 800 delegates from over 40 countries, and it is anticipated that feedback from this international event will help better inform future areas for co-operation on the Island of Ireland. It is also intended that this learning will also be shared at the next meeting of the 5 nations working group on 12th November 2007.
In Addition
The Concerned About Suicide information leaflet has been reproduced as part of all-island cooperation on suicide prevention. This is a unique and practical resource, intended as an initial source of information for parents, friends and family members who may be concerned about a loved one. The leaflet was originally produced by the Resource Officers for Suicide Prevention (HSE) and the NI Suicide Awareness Coordinators with support from CAWT (Cooperation And Working Together).
Annex 7
Mental Health & Learning Disability Board
Roy McClelland Chairman of the Board a Consultant Psychiatrist at Belfast City Hospital and Emeritus Professor of Mental Health at Queen’s University.
Marie Crossin Chief Officer of CAUSE (Carers and Users Support Enterprise), a voluntary organisation providing support for carers and families of people with mental illness.
Joanne McDonald User of Learning Disability Services. Is a member of Buzz which is a self advocacy Group on health education work and social issues. Employed as an equality officer with Mencap.
Roy McConkey Professor of Learning Disability at the University of Ulster. Has worked in the field of learning disability for over 30 years previously holding posts at the University of Manchester, in Dublin and in Scotland.
Dawn Rees National Implementation lead for the Department of Health/DfES sponsored National CAMHS Support Service in England. A member of the interim management team which leads a wider service improvement programme supporting the National Service Framework for children, young people and families.
Antony Sheehan Recently appointed as Chief Executive of Leicestershire Partnership NHS Trust but has previously worked for Department of Health for 7 years as head of mental health and set up the National Institute for Mental Health.
[1] Source: Hospital Inpatients System and Samaritans Information Sheet on Self-Harm and Suicide (www.samaritans.org/know/informationsheets/selfharm/selfharm_sheet.shtm).
[2] This classification is revised periodically to reflect changing mortality patterns and since 1979 deaths have been classified using version 9 up to 2000 and version 10 since 2001. Slight discontinuities in the data may be introduced by revisions to the ICD but these are generally small in their effect.
[3] Northern Ireland Statistics and Research Agency (which includes GRO).
[4] Office of National Statistics – the NISRA equivalent in England and Wales.
[5] ICD codes used in classifying ‘suicide and self inflicted injury’ using ICD10 are X60 to X84 and Y87.0. The equivalent codes using ICD9 are E950 to E959. In coding ‘events of undetermined intent’ the ICD10 codes are Y10 to Y34 and Y87.2 and using ICD9 they are E980 to E989. See Annex 2 for a complete list of ICD10 codes used in this analysis.
[6] Data for this year is provisional and therefore subject to change.
[7] A quantity, term, or value that is the midpoint of a set of values, such that the variable has an equal probability of falling above or below it, i.e. the middle term of a series of values arranged in order of magnitude (or, if there is no middle term, the mean of the middle two terms).
[8] Parasuicide according to the World Health Organisation (WHO) is defined as ‘an act with non-fatal outcome, in which an individual deliberately initiates a non-habitual behaviour that, without intervention from others, will cause self-harm and which is aimed at realising changes which the subject desired via the actual or expected physical consequences’.
[9] ICD codes used in classifying self-harm using ICD10 are X60 to X84 and Y87.0. A full description of these codes is given in Annex B.
[10] Deaths & Discharges are used as an approximation for admissions.
[11] These figures represent instances of self-harm, they do not represent individuals as a person may have more than one instance of self-harm.
[12] These figures are provisional and are therefore subject to change.
[13] Late effects
Department of Health, Social Services and Public Safety
Department of Education

Department of the OFMDFM
Families Bereaved Through Suicide for South/East Belfast
My name is Bobby Cosgrove and I am the Chairperson of the families bereaved through suicide for South/East Belfast, we call ourselves the S O S Group “Survivors of Suicide” and I have been asked to contact you on their behalf.
The aim of our group (which meets monthly) is to help the families and friends of those who have taken their own lives, we through the group make ourselves available to talk to, listen to and signpost them to the services that are there for them.
We invite speakers from different agencies involved in the suicide field to come and address the group and answer the questions that most times go unanswered.
Some of the issues that we would like you to look at in your committee are as follows:-
We would like to see an appraisal of the decision to move forward and invest a large sum of funding in the telephone network to cover the whole of Northern Ireland.
It is felt that there has not be enough investigating, nor has there been an in-depth study done on the Pilot Scheme that took place in North and West Belfast, I sit on the S S I B and we in the family groups feel that a serious report on this study has not been produced and to do a nationwide link based on the information available is not going to be value for money.
We are aware that there has been an increase in funding for the incoming year but overall it is a drop in the ocean when we look at the increase in suicides and we feel as all families that this money. The funding was only given after lobbing by families and it needs to be spent wisely and on projects that will yield results.
There is a need for a phone network but it has got to be right. It is no use having a NI wide telephone helpline unless there are strategies in place to signpost callers to places where they can receive help such as counselling.
We also feel that there is a shortfall in the G P and front line training on Suicides there is a programme in place but the uptake by all the frontline staff is minimal.
One of the often forgotten groups in this bracket is the manager of surgeries of G Ps and the reception and Triage Nurse in the local A & E Departments, these are normally the first point of contact by those people seeking help to cope.
We also think that some of those organizing events in the first round have not yet given reports on how they spent there share of the funding and also what impact if any it returned.
The other point that I have been asked to raise is the lack of statistics which leads to deaths by suicide being under reported. We feel that it is time to make it compulsory to put the real cause of death even if it hurts, we must stop hiding from the truth.
It does no one in the Suicide field any use if we cannot get the proper figures to produce a programme to fight suicide, we believe that we have to take the stigma out of Suicide and if people are honest from the start then we can overcome the stigma and in doing so start the healing process earlier.
We would also like the committee to consider the lack of co-operation between agencies when a suicide occurs. Members of the group have found that there was no liaison between the PSNI, Coroner’s Office or Health & Social Services to provide information or support to relatives. There should be more joined up working so that relatives can access information from one point rather than have to contact different people which is the last thing they feel like doing after a suicide occurs.
There are other subjects that we hope to see addressed and maybe when we can get this programme of advice put together then these will also be looked at.
On finishing I would like to inform you that if any member of your committee would like to visit our group to hear first hand from families we would gladly welcome you.
Bobby Cosgrove
Department for Employment & Learning
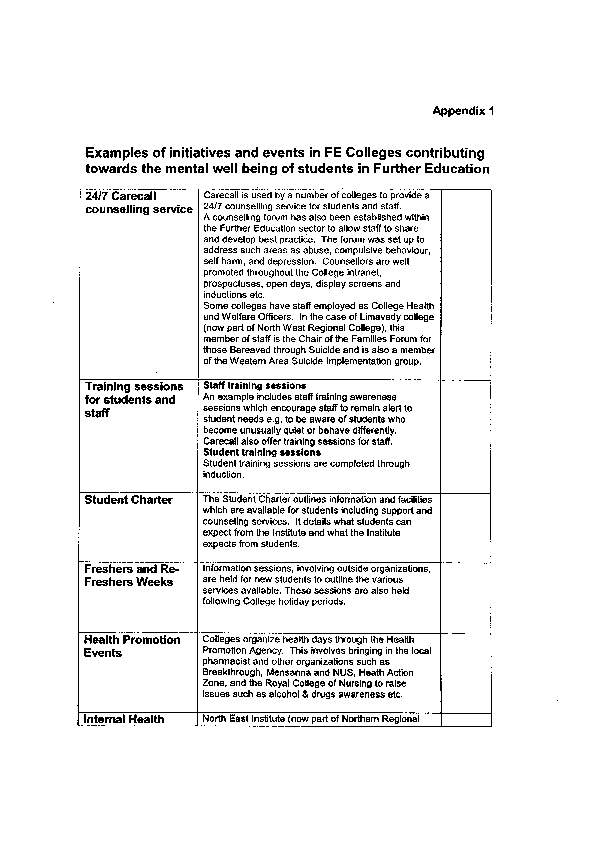
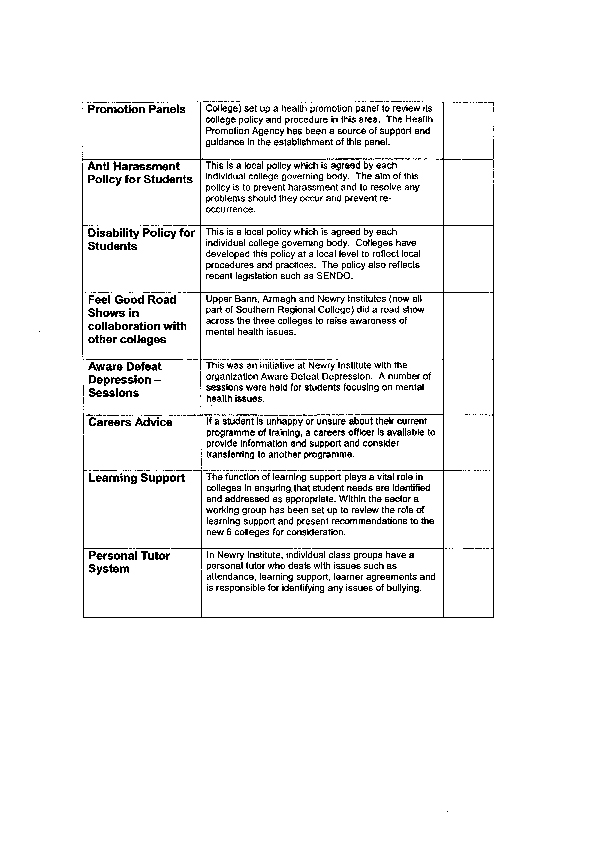
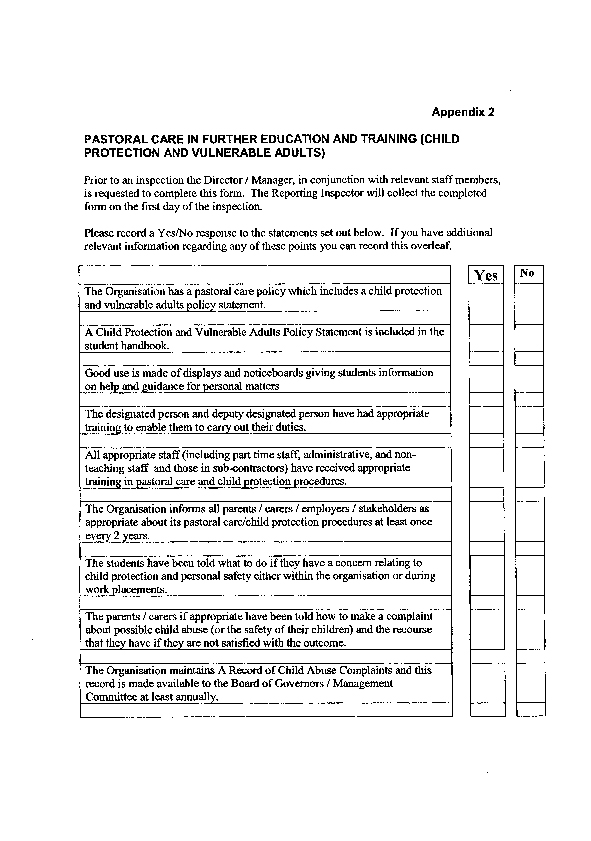
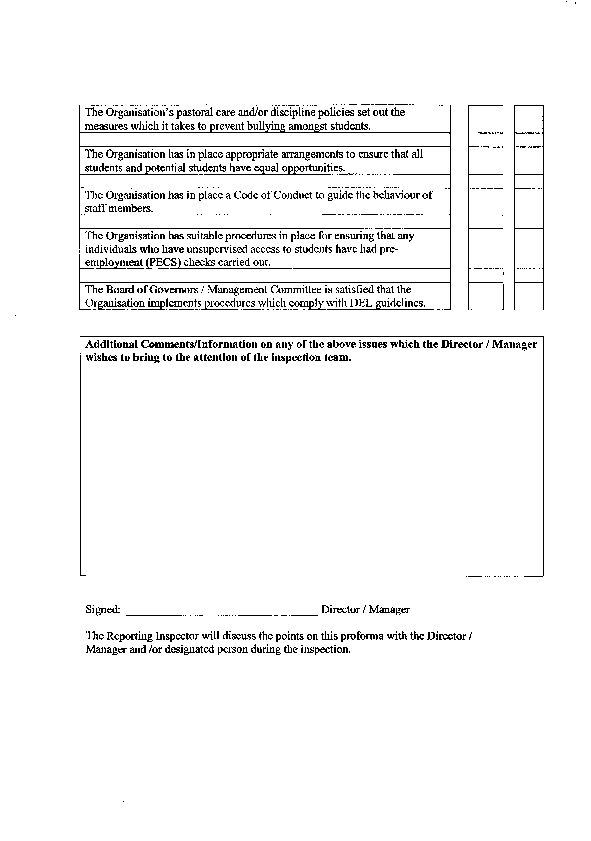
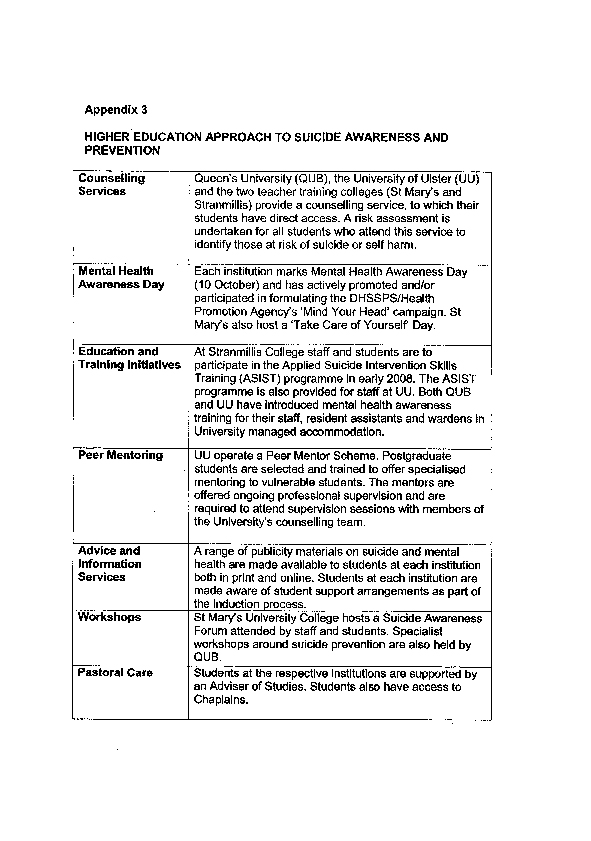
PIPS/RAYS Rights Group
In response to the current inquiry into suicide, please find below a submission made on behalf of the PIPS/RAYS Rights Group and the PPR Project.
Background: The work of the PIPS/RAYS Rights Group
Since October 2006 the PIPS/RAYS Rights group has been carrying out a development programme with the Participation and Practice of Rights (PPR) Project. The group is made up of individuals from two suicide/self harm support groups in North Belfast – PIPS (Public Initiative on the Prevention of Suicide) and RAYS (Reaching Across to prevent your risk of Suicide). The PIPS/RAYS rights group is mainly family members bereaved by suicide as well as crisis workers who are the first point of contact for people in the community at risk of suicide.
The PIPS/RAYS Rights Group has worked with other mental health service users, to select a small number of issues which they, as individuals with experience of using mental health services, feel could be addressed with ease and make a marked difference to families and individuals in distress who access local mental health services.
The information below is structured in direct reference to the Inquiry’s terms of reference.
Scope of Health Committee Inquiry
To consider the level of services and support available to promote good mental health, to prevent suicide and self harm; and to support those affected by suicide/ Further action required, taking account, as appropriate, of experience elsewhere.
On the 28th November 2007 the PIPS/RAYS Rights Group and the PPR Project held an event ‘Rights in Action: Changing Mental Health Services’. (See conference report enclosed.) At this event the PIPS/RAYS Rights Group presented their work and their timetable for change to an international panel of experts on mental health and human rights and to the wider community. The next step for the group is to monitor whether the many programmes and policies in place to improve mental health services translate into progress on the ground on these issues over the course of a year.
Recent years and months have seen a flurry of activity as government programmes and committees have directed their attention and some mental health resources towards addressing suicide. The primary concern of the PIPS/RAYS Rights Group is to improve the impact these policies and programmes are having in their communities, among the people who need the services the most.
The group will use indicator measurements to monitor their selected issues over the course of the next year. The focus of their monitoring will be to gauge whether any improvements are being felt by the mental health service users in their own communities. This unique approach is based on the work of the UN Special Rapporteur on the Right to Health Paul Hunt, who has added his support to the groundbreaking work the PIPS/RAYS Rights Group are undertaking, (see Appendix 1, Message of Support from UN Special Rapporteur Paul Hunt). The group has gained the support of a broad range of organisations, including NICCY, the Committee on the Administration of Justice, and Psychiatrist Mike J Crawford, Reader in Mental Health Services Research, Imperial College London (see Appendix 2, List of Organisations in Support).
In the course of their work, the PIPS/RAYS Rights Group found that National Guidance recommends discharged patients with severe mental illness or recent history of deliberate self harm are followed up within one week. (See Appendix 3, Discharge Protocol for the Mater Hospital). However, when they surveyed 57 mental health service users on the issue, they found that only 13% had received a follow up appointment within a week. Many of those surveyed felt that receiving a follow-up appointment after discharge was a ‘lifeline’. It provided the proof that they were still plugged into services, and its absence and the subsequent effort required on the part of the patient or his/her family to secure an appointment was often a source of great distress. The PIPS/RAYS Rights Group believe this is an issue which could be addressed at minimal cost, and would be of concrete and immediate benefit to those using mental health services.
The findings from ‘Rights in Action: Changing Mental Health Services’ were launched on the 26th February 2008 in Clifton House. (See enclosed Findings of the International Panel). The findings contained a number of recommendations, both general and specific, on how mental health services could be improved. On the same day, the PIPS/RAYS Rights Group launched their campaign for ‘A Card Before you Leave’ – in order that those suffering from severe mental illness or at risk of self harm, receive the date of their next appointment before they are discharged from hospital. As best practice NHS guidelines state that such patients should have been seen face to face within a week, the group has identified this as the first step towards the guidelines being fulfilled. The international panel’s findings emphasised the modest and reasonable nature of this change, particularly with regard to the health service’s current financial constraints. The PIPS/RAYS Rights Group has been gratified to note that the Deputy Chairperson of the Health Committee has also remarked on the simplicity of this change during evidence given on the 10th January and stated that it could be recommended in the Committee’s conclusions.
Scope of Health Committee Inquiry
To consider the scope and appropriateness of the Department’s strategy
‘Protect Life: A Shared Vision’
Under s75 of the Northern Ireland Act 1998, public authorities including the Department of Health are under an obligation to pay due regard to promoting equality of opportunity in all their functions among those of different age, religious belief, political opinion, racial group, marital status or sexual orientation, and also between men and women, persons with a disability and persons without, and persons with dependents and persons without.
Among the requirements under s75 is the obligation for public authorities to carry out equality impact assessments (EQIA) to gauge the effect of their policies on the affected groups.
Neither Protect Life nor its predecessor Promoting Mental Health, underwent a full EQIA.
Preliminary research done before the suicide strategy identified a number of factors that increased the likelihood of requiring mental health services e.g., the high level of young males dying by suicide. Despite these findings, the Protect Life Strategy was deemed incapable of having a significant impact on equality of opportunity and ‘screened out’ stating:
“The Department considers that the policy should impact positively on the health and emotional wellbeing of the general population. The Department considers that the Strategy and Action Plan does not adversely impact on any of the s75 groups and therefore a full Equality Impact Assessment is not required.”
This is a misreading of the purpose of an EQIA – which is about assessing how best to get at need affecting different groups. It is not enough that the policy is deemed to be of benefit to all, or that it won’t have adverse impact. There is a positive legal duty contained in Section 75 to proactively target inequalities identified between groups and the EQIA is the tool to identify the groups most in need and to find ways of making improvements. The policy’s impact must also be consistently monitored so that one can assess how well that policy addresses the various needs of different groups. Currently the arrangements for monitoring the impact of the Suicide Strategy on the equality categories and those most in need are unclear. Indeed concerns about the monitoring of the policies and programmes put in place to address suicide prevention have already been made to the Health Committee during it’s hearing of Evidence on the 10th January 2008. The innovative and important work carried out by the PIPS/RAYS Group is done with the express purpose of measuring impact of policies on the ground – the only place where it can meaningfully be measured.
Scope of Health Committee Inquiry
Examine the level of stakeholder involvement
In May 2007, Professor Roy McConkey of the University of Ulster, spoke before the Assembly Health Committee. He stated:
“In Northern Ireland, there has been a deficit in the involvement of users and carers, and of our accountability to them”
Indeed, ‘partnership with users and carers in the planning, development, evaluation and monitoring of services’ was one of the main principles of the Bamford Review.
Recognition of the importance of including health service users in all stages of policy making processes is emphasized by its inclusion in the Health and Social Services (Reform) (Northern Ireland) Order 2007, which places a statutory duty on public bodies to consult users of health services in planning services and to show how much of their input is taken on board.
Protect Life itself was a hard won victory for families who had been bereaved by suicide. Alongside Protect Life, a Suicide Strategy Implementation Body was set up with the purpose of facilitating the participation of those affected by suicide in the implementation of the strategy which they had been instrumental in achieving through the Families Forum. Yet the extent to which the family members were able to fully participate has been questioned. One of the family members involved in the Families Forum stated in front of the Assembly Health Committee in July:
“ …[former direct rule Minister Paul Goggins] said that a forum would give us a powerful voice, but that did not materialise. We knew that we would never have a veto, but our voice was never as powerful as we had envisaged…There was a very well publicised mental health programme rolled out in February. We are not against it, nor would we say anything about it. However, approximately £380,000 was spent on that campaign yet not one member of our forum was involved in the programme. The forum was set up in September 2006, and it was well known that we were representing people across the Province as best we could. Therefore, it was embarrassing not to have had more involvement it the campaign”
Through their survey, the PIPS/RAYS rights group found that 79% of the mental health service users they questioned rated their level of involvement in decisions made about health services as between 1-3 on a scale of 1 (not involved) -10 (very involved).
The full involvement of mental health service users in planning, implementing and evaluating strategies to achieve better mental health care should not take place solely because it is a government commitment, but also because in the context of the Programme for Government and reduced health budget for an already ‘Cinderella’ service, it makes good sense.
We hope you find the above information of assistance in your Inquiry into the Prevention of Suicide and Self Harm. If you require any further information please do not hesitate to contact us care of Nicola Browne, PPR Project at nicola@pprproject.org or 028 90326980.
Yours sincerely,
Gerard McCartan Rhonda Hill
PIPS/RAYS Rights Group PIPS/RAYS Rights Group
Organisations Supporting the PIPS/RAYS Rights Group Campaign
- Aware Defeat Depression
- Shankill Womens Centre
- Committee on the Administration of Justice (CAJ)
- Disability Action
- Centre for Human Rights and Disabled People
- Shankill/Ardoyne Healthy Living Centre
- UNISON
- Psychiatrist Mike J Crawford, Reader in Mental Health Services Research, Imperial College London (author of ‘Suicide following discharge from in-patient psychiatric care’ in Advances in Psychiatric Treatment 2004)
- Law Centre (NI)
- Eastern Health and Social Services Council
- Northern Ireland Commissioner for Children and Young People (NICCY)
- Mental Disability Rights International (USA)





Dr Rory O’Connor
My name is Rory O’Connor and I am a Chartered Health Psychologist and a Reader in Psychology in Stirling University, where I lead the Suicidal Behaviour Research Group. I am also the UK Representative of the International Association of Suicide Prevention, and I am a member of various suicide prevention organisations, such as the American Association of Suicidology, the American Foundation of Suicide Prevention and the International Academy for Suicide Research. I have been conducting research into suicide and suicidal behaviour and self harm over the past 14 years originally in Northern Ireland, but more recently in Scotland.
I am not involved with the Choose Life Strategy directly. I am an academic although I have provided input on the evidence and research element of the strategy. I was a member of the Quality Assurance Group for the Northern Ireland Protect Life Strategy and provided comment on the draft of the Strategy.
Suicide prevention strategies across the world tend to be made up of six components and the Northern Ireland Strategy incorporates these six components. They are:
- Education and awareness: dealing with stigma and the reduction of stigma
- Screening of those at risk
- Treatment of psychiatric disorders, includes not just the treatment, but also looks at barriers to access to services. In the Northern Ireland Strategy I think there are statistics which indicate that about 80-90% of over 30’s had access to services in the months prior to suicide. We know that in people under 30 the statistics are not that high and indeed they are often not presenting to services with mental health problems or maybe seeing their GP with general health concerns or sleep problems. So a key element with respect to psychiatric problems is to look at getting access to services.
- Restriction of access to lethal means. In England in 1998, in consultation with Keith Hawton, the UK/Westimister Government introduced blister packs and reduced the number of paracetamol to 16 per pack and that seems to have had an effect. Going back further we had the substitution of coal gas for North Sea gas, which is non-toxic and an associated reduction in suicide.
- Media & media reporting. There is the whole issue of contagion or potential contagion or suspect clustering going on in some communities in Northern Ireland, and that is a phenomenon which is witnessed throughout the world. The Irish Association of Suicidology and others, National Union of Journalists, have developed guidelines, as have the Samaritans, for dealing with media reporting.
- Lastly is research. If you look at suicide prevention across the world, the one element which is core and common to them all is research. However the money made available for research is miniscule compared with other aspects of the strategy.
The first national suicide prevention strategy was developed in Finland and launched in 1986 and has influenced national strategies throughout the world. It was a ten year strategy and it has been evaluated internally and externally. It has been seen largely as a success, albeit the suicide reduction target was not quite met, but in terms of the process, increased services and promoting positive mental health, it seems to have been quite successful. A number of other countries, Norway, Sweden, New Zealand, Australia, United Kingdom, Netherlands, Estonia, France and the South of Ireland have all got suicide prevention strategies.
The key thing which distinguishes all the strategies, as well as the six components, is the extent to which communities are involved. I think that without question a strategy will not be successful if it does not involve grass roots. All levels of community, from the grass roots right up to government need to be involved to give those in the front line dealing with suicide crises the best hope of success. Again Finland led the way here. They were very strong at involving communities in all aspects of the development of the strategy. The strategies in Scotland and Northern Ireland have taken that approach as well.
If you look at any suicide strategy, such as Scotland, Northern Ireland or the Republic of Ireland, they are not based upon a huge amount of empirical evidence, because if you look across the literature on suicide prevention, the evidence base is small. There are a number of reasons why this is the case. Firstly, suicide as a phenomenon is obviously a low-rate behaviour, so when it occurs it is, relatively speaking, statistically rare. So it is very difficult to develop interventions which we will be able to be evaluate systematically. Some of the strategies have been evaluated such as Finland but it is very difficult to determine which components of each strategy have been effective.
What is more shocking is that I don’t think any country has carried out an economic evaluation. However, in Scotland the first stage of the Suicide Prevention Strategy has incorporated an economic evaluation and has estimated that for every 1% reduction in the number of suicides will save up to £10 million over the lifetime of these individuals. So there is not only a substantial personal and societal tragedy to suicide, but it is economically really important as well.
The whole premise of the Choose Life Strategy in Scotland is based upon the notion that suicide is everybody’s business. So in terms of responsibility, in terms of bringing in support, in terms of increasing goodwill, that is what has driven the suicide strategy. I believe Northern Ireland has a similar approach.
Recognising that it is everybody’s business means that you have to look at prevention, crisis intervention and postvention together. I am sure you are all aware of the Choose Life strategy’s 10 year plan to reduce the rate of suicide by 20% by 2013. If you look at suicide prevention strategies all over the world, some have reduction targets, while others do not.
Substantial funding, £12 million, was made available in Scotland in 2003-2006 and a further £8.4 million was made available for 2006-2008. I think an advantage of this phased approach is that the first three years have been evaluated in an informed way, so that the evaluation of the first phase will impact on what has been implemented in the second phase.
The main aim of the strategy and action plans associated with the strategy was to develop and build on national and local skills, because in terms of looking at sustainability and mainstreaming, the development of suicide prevention skills ought to become part of everyday practice.
One of the longer term aims of the Choose Life strategy is that it becomes a self sustaining strategy. A key dimension is to increase awareness and knowledge of what works. The overall aim is to reduce and prevent premature loss of life, and also to improve hope. One of the key elements of the Scottish strategy is that it is part of the national programme to improve mental health and wellbeing for all the people of Scotland. So it can be seen within that broad programme, and if we look at the most recent consultation going on in Scotland, where we are talking about not just the avoidance of mental ill health but promoting positive mental health. Again, similar to the Northern Ireland strategy, there are a number of objectives which cover all aspects of prevention right through to postvention and there are a number of priority groups.
In terms of the positive aspects of the strategy, I think that the strategy is going well, but obviously there is a long way to go as it is a ten year strategy. One of the key strengths is that it has been framed within the broader mental health policy, and the national programme for the improvement of mental health and wellbeing has three key areas.
- First of all there is mental health improvement, which is about promotion and prevention and I think that it is crucial and has worked very well in Scotland.
- Secondly, this strategy tries to address the stigma associated with mental health. I think if we can address stigma it would go a long way to bringing down barriers to young people, in particular young men, accessing health services.
- The third strength is that it is chaired by a government minister, so it has weight, it has government backing and support, and indeed one of the main drives of the programme is in terms of looking at reducing health inequality and the promotion of social justice.
So one of the advantages of the strategy is that it is not just dealing with suicide, it is looking at suicide in the broader mental and social well-being context, and there is a similar model in Northern Ireland.
Another key strength, and something to think about for the Northern Ireland strategy perhaps, is that there is a National Implementation Support Team for the Choose Life Strategy. Certainly as an outsider looking in, what seems to be helpful here is that things have been divided up, so there is someone in charge of different areas of potential development. In other words, in respect of trying to make the strategy work at a local level, developing partnerships, providing support and so on, there is a group of people who look at what works to ensure that new developments are based upon the evidence base. Also someone is looking at training and indeed in Scotland there has been the development of a national training programme in terms of skill development for those in the front line, and there is a marketing communications aspect to Choose Life and this is key to looking at the media and developing a pro-active strategy for dealing with the media.
In terms of how the strategy has been implemented on the ground, there are 32 local authorities in Scotland and all of them have had to develop local action plans. I have experience of those in Glasgow and Stirling, they are genuinely cross-body and cross-interest groups, where social work, health, police, justice, all come together as well as voluntary groups and others, and this has been really beneficial.
Another aspect that has been particularly beneficial is the funding. Out of the £12 million that was originally allocated to the Suicide Prevention Strategy, £9 million of that was earmarked for local projects, for local development and local skills, so in each of these areas, there was someone who was designated as a lead person to develop the strategy. Having ring-fenced money is particularly important and also that there is a monitoring support structure in place and an implementation team working more broadly.
Another key thing, which links with the Northern Ireland Strategy, is that we also have a dual track approach in terms of suicide prevention. Looking at the general population and also looking at high risk groups.
We all endeavour to develop and deliver evidence based practice and intervention. The aspiration to implement good practice, especially at local level is important, but it is difficult to try to balance the support for innovative ideas and evidence-based practice. Often these innovative ideas are not based upon evidence and so that can raise some tension. Another key thing is evaluation which has already happened in phase 1 of the strategy. The result of the evaluation was published in 2006, and it has raised some interesting points for the implementation of phase 2 of the strategy.
Another distinct feature of the Scottish Strategy was the development of SIREN (Suicide Information Research and Network) and I am on the steering group of that. This has brought together practitioners and academics, so the academics are talking to the people who actually deliver and who will implement some of their findings and I think that this has worked really well. We are hoping that this will lead to a Scottish Association of Suicide Prevention in the long term.
The work with the Scottish Prison Service has also been particularly innovative and has led to additional funding. Choose Life was able to make money available for initial innovations in the Scottish Prison Service, particularly for those who are leaving prison, and this has been quite effective in securing independent funding thereafter.
The last point in terms of positive components is that SIREN runs an annual conference and seminars around Scotland. Also Choose Life Co-Coordinators have an annual summit which is great for empowering and great for learning lessons from one another but also learning about the difficulties that people experience.
While the strategy is going in the right direction, there are lessons to be learned. These include the need for more support earlier in terms of implementation and support before the launch of the strategy. Obviously that has passed now but perhaps there is a need for more international evidence sharing. At the outset the National Implementation Support team didn’t have the links they have now and were starting out cold so to speak. The team consists of excellent strategists and policy makers, but they had to learn the evidence base and know who to contact and I think that is particularly important.
There is also an issue around how local action plans or localised support are evaluated. You have the fantastic innovations, this fantastic support, but at local level, with a small local authority, how do you know it is any good and then conversely if we think it will be good, how do we evaluate that, and that can be a problem. Funding is tight and it is difficult to justify spending a lot on evaluation. This is one of the general points I would argue, especially in Scotland, we need to find the balance between innovation and evidence base and the need for evaluation. Again one of the things in Scotland I think you will find was that local authorities often did not draw upon the international evidence base as much as they might have.
Another key issue linked with the Northern Ireland Strategy is the notion of self-harm. One of the targets for suicide prevention is looking at what is self-harm. Self-harm is the key predictor of completed suicide. One of the things we grappled with in Scotland is the distinction between serious and non-serious self-harm, and that is a really difficult area, and indeed it is something that Scotland is dealing with because the Suicide Prevention Strategy is not a self-harm prevention strategy therefore additional resources are required for self-harm and maybe that is something you would look at as well.
Because the Scottish strategy, one would argue is a Public Health Strategy, perhaps there should have been more intervention or clinical services involved. Services, such as drug misuse services and mental health services, should have been integrated with the public health strategy earlier. Psychiatry has a key role and it is an important role because of Scotland and Northern Ireland’s broader social justice/equality agenda. It is important that we look at this more closely and perhaps you can look at that more closely in Northern Ireland.
The last point I will make on lessons learned is in relation to the debate about local innovations versus research evidence base. The argument is that some people think that there is too much autonomy at local level and that there has to be more control over how funding is allocated in the future.
Turning to general issues I think that a key one is the setting of targets for suicide prevention and it goes back to this issue of self-harm and what are your indicators of improvement or success. In Northern Ireland there is a goal to reduce suicide levels by 10% by 2008 and by a further 5% by 2011. These are really ambitious targets. Some countries have targets and some do not and I can see the political need for targets and how they can be quite useful. My concern is about what happens if you do not meet the targets. How is that going to play in the media and affect morale. The Northern Ireland Strategy has looked at this and identified secondary targets and I think it is important that you do that. The other thing about targets is how do you report them? Do you use a three year or five year rolling averages? Whatever you do, avoid using one year rates.
One issue in Scotland we looked at was public attitudes as a secondary indicator of effectiveness. We undertake a public attitude survey every two years and I know there is a public attitude survey in Northern Ireland, and that is something which is also identified in the Northern Ireland strategy.
Looking at self-harm as a proxy for suicidal behaviour is an important thing in terms of hospitalised self-harm. I think that you record this in Northern Ireland, but I don’t think that you record hidden self-harm or self-harm among young people in the community. That is something we are doing over here now in our research group in Stirling.
The objectives in the strategy are another thing, but what are the benchmarks, how are the objectives going to be measured? That again is something you need to consider.
Another general issue in Scotland is that the recent evaluation in Scotland suggested that deprivation in the east end of Glasgow is a huge risk factor for suicide. We already know that deprivation is a key risk factor but some might argue that it wasn’t recognised early enough. The point I am making is don’t forget that health and inequality are issues within themselves and within a broader strategy.
A further point is how do we address issues of developing infrastructure in terms of building capacity and skills? In Scotland ASIST is rolled out nationally. I know in some areas in Northern Ireland ASIST has been delivered too, but it has not been evaluated yet. There is an evaluation taking place in Scotland and the results will be published in January/February of next year, I think. That is an example of capacity building as those who are trained can become trainers and in some cases this may become mainstreamed.
The last point is primary research. Northern Ireland is in a good position as it is relatively small and can look at issues which larger countries could not look at due to population size. Fund more research. My final piece of advice is not to think of evaluation as an add-on and it does not come cheap.
Issues raised during questions:
Relationship between the ‘troubles’ in Northern Ireland and recent increase in suicide numbers
Impact on mood of alcohol and drugs and the relationship between alcohol and drugs and suicide
NICE guidelines on self harm
Impact of ASIST training for GPs
Discussion of resources – Scotland well funded. If no money for local intervention strategy won’t be effective but with adequate funding it can bring huge benefits.
Northern Ireland Office
Introduction
Woodlands is a purpose built 48 bed secure unit which provides accommodation for young people in the 11-18 age group, who come before the justice system in Northern Ireland. Although some of our clients may be with us for one night only, many spend lengthy periods of their adolescence with us as a result of repeat offending behaviours, and some of the more serious offenders may spend up to 2-3 years in custody.
The most common offence categories would be property related crime such as theft, burglary and vandalism, with car crime a close second. In recent years there has been an increase in the numbers charged with drug-related offences and also with violent crimes such as assault, sexual offences, arson and murder.
While the agency’s overall aim is the reduction of juvenile crime levels, we are also in a prime position to comment on the high levels of emotional distress and mental ill-health evident in the children we serve, and we welcome any and all initiatives which may lead to improvement in the mental health services available to them.
At the outset however, I feel it is important to emphasise, that although we cater for a client group who present with a very high level of mental health needs, we are not a mental health facility nor are we staffed as such. On any given day we have one nurse with a part time mental health remit and one psychologist on duty Monday-Friday, to meet the needs of approximately 32 young people, who are among the most distressed disturbed and disturbing young people in the province.
Children are placed with us by the courts in relation to offending behaviours usually for an indeterminate length of time, and we have little or no control over decisions made re who come here, whether this is an appropriate placement, or indeed when they leave, and where they go on discharge. This poses a number of dilemmas for us in relation to what is possible within these uncertain time frames, what is essential to their well being here and how to make the best use of the scarce mental health time available to them while in custody, as well as supporting the unit staff in relation to managing the risks they present with. We are aware that this input often falls far short of what they need.
Most of the young people sent here would benefit from, comprehensive mental health assessments and intensive therapeutic interventions, but we can only offer these services to a very limited number at any one time. We rely a lot on our Community Services, outside agencies and CAMHS teams to carry on the work identified in our in-house assessments.
Over the years we have revised and refined our contact with the young people who pass through the Centre in an attempt to promote their mental health and wellbeing and develop their resilience, while at the same time carefully collecting and sifting the information we have on them to ensure that as far as humanly possible, given our limited resources, those with mental health issues are identified, prioritised and offered the best supports that our service can provide.
If one considers the target groups that have been identified as most at risk of suicidal & self harm behaviours most of the young people in our centre would fit into one or more of these groups. ie: They are by large, young males/females with lifestyles involving heavy use of alcohol and drugs. Many of them have been referred to mental health services at an early age. Most of come from disadvantaged communities and many have histories of adverse life experiences such as sexual, physical and / or emotional abuse and neglect. It is not uncommon for them to have parents / carers who suffer from mental health problems themselves, and indeed a disproportionate number of them have a relative or close friend who died by suicide.
A snapshot taken of the residents of the centre here today serves to illustrate this point.
32 young people in custody – 8 on a custodial sentence – 24 remandees
8/32 have at least one suicide attempt on record
5/8 attempted hanging
2/8 overdosed requiring hospital admission
1/8 attempted to jump to his death
7/8 have been in care
2/8 have been in secure care
7/8 were also self-harmers
NB all 8 young people would admit to mis-using drugs and alcohol regularly
When one considers self harm behaviour separately:-
17/32 have a history of self harm
15/17 involved self cutting
2/17 involved violent head banging
Of the 17 self harmers
11/17 have been in care
6/11 have been in secure care
17/17 have admitted mis-using drugs and alcohol on a regular basis.
On a more general note:-
20/32 children listed today have a diagnosed mental health disorder
4/32 have a history of confirmed sexual abuse ) These figures are
5/32 have a history of confirmed physical abuse ) conservative, as the real
9/32 have a history of emotional abuse. ) figures for all three categories are
probably much higher
If we consider the figures above as a typical breakdown of the characteristics of our client group, I would hope this serves to illustrate the high risk population we work with and the extent of the problems therein.
In my response to your request for “written evidence” from ourselves in relation to our current strategy for the prevention of suicide and self-harm, I have tried to give an account of our work which highlights how our system intervenes at various points during the young person’s time in custody, to assess and address their mental health needs.
This paper is broken up into a number of sections for ease of reading.
1. |
Design and Specification Physical Environment of JJC |
Prevention |
2. |
Emotional Environment of JJC |
Promotion of Good Mental Health. Continuous assessment and recording of a young person’s state of mind and behaviours. Encouragement of appropriate support seeking behaviour |
3. |
Staffing |
Co-working |
4. |
Staff Induction and Training |
De-stigmatising mental ill health |
5. |
Initial Assessment by Psychiatric Nurses |
Mental health screen. |
6. |
Referral to Psychologist/ Psychiatrist |
Co-working with nursing social workers psychology and psychiatry |
7. |
Ongoing Assessment |
Close liaison with significant others ie family, schools, family GP, social worker, CAMHS Referral/consultation with nurses and psychology re management intervention |
8. |
Education/Daily routines |
All clients attend school daily Normal school day and routines Curriculum adapted as necessary to meet individual needs. All work accredited. |
8. |
Programmes and Groupwork |
Prevention, awareness raising |
9. |
Family Work |
Prevention, intervention, Promotion of family support Repair or support for family relationships |
10. |
Spiritual Oversight |
Prevention, intervention, Promotion of support systems both with in and out of the centre. |
11. |
Discharge |
Planning |
12. |
GAPS |
Lack of secure beds |
13. |
Conclusion |
Physical Environment
Building and Living Environment
Woodlands was designed taking into account all the learning points gleaned from enquiries that were set up to look into tragedies that took place in other care and custody establishments worldwide.
Design
The design of the building is such that the risk of an actual successful suicide attempt is minimised. All rooms are equipped with furniture, fittings, and viewing panels designed with the disturbed/distressed/suicidal child in mind and are as far as possible “ ligature free”. The power and water supplies in the bedrooms can be controlled externally, and access to en-suite bedrooms can be closed off if the risk assessment deems this necessary.
Room Searches
Room searches are also carried out both routinely and randomly, for drugs, ligatures, cutting implements and weapons, with extra vigilance if a young person’s mood or life circumstances indicate increased risk.
Counting and Checking Routines
We also have a number of counting and checking routines in operation throughout our living units and school premises eg: all sharps, cutlery and tools are checked after every meal/class/ activity and pens, cooking implements and tools used in classrooms, workshops or common rooms are counted in and out.
However, in spite of our vigilance, staff regularly come across new possibilities for everyday objects; eg stone chippings from the grounds or staples from magazines etc. Again, we do all in our power to minimize the risks, realising that none of our strategies are foolproof, as young people who are determined to self–harm can be very resourceful.
In exceptional circumstances plastic eating utensils and cutlery are available, as are safety bedding and pyjamas (made from rip-proof material) although use of either of these extremely rare and used as a last resort . Because of this policy, signatures from senior management are required before these items would be used.
Risk Assessment Prior to Acquisition of Electrical Appliances
Our residents also acquire rewards in the form of electrical appliances such as radios, personal stereos, TV’s and DVD players .Obviously all this equipment has self-injury potential and each young person is assessed from shift to shift, to ensure that the likelihood of them misusing such items, eg electrical leads, pieces of plastic, glass, metal from broken articles etc. is updated, thus informing decisions made about a young person`s access to them.
Medication Controls
All controlled medication used in the centre is administered by the medical department. If there is any concern re a young person secreting and/or hoarding prescribed medication rather than swallowing it, extra precautions are put in place to make this as difficult as possible ie giving meds in liquid form or close supervision and oral checking for consumption etc. Household remedies are dispensed at the discretion of Unit Managers. We have also had difficulties in the past with parents or visitors passing drugs, lighters or cutting implements during visits, but this has largely been eradicated with the restrictions on what can be brought into the visiting area and closer supervision of visits where this is deemed a risk.
Emotional Environment
The living spaces in the centre are open, comfortable and pleasant to live and work in and staff work very hard to create a safe, supportive and stimulating group living environment which promotes emotional wellbeing, social skills, self esteem, respect for each young person as an individual and consideration for others. Every effort is made to modify dysfunctional social behaviours and promote the development of pro-social attitudes and values.
Staff are sensitive to a young person`s changing moods and life circumstances and are ready with 1-1 time as and when it is required. Each child is assigned a key worker, a co-worker and a case manager each of whom take a personal interest in each child as an individual and who consult with the mental health and family workers in the centre for advice and support for mental health issues that arise in the course of their work.
Bullying Policy
We also have a zero tolerance of bullying in the centre and staff, are constantly vigilant for those who have the potential to bully and indeed those who have been victimised in the past or are vulnerable in any way. (see induction section)
Progressive Regime
As mentioned earlier Woodlands operates a positive –reinforcement system known as the progressive regime which is used to encourage and promote positive behaviours and modify negative ones. The regime works well and for the most part young people respond well to it. It often brings stability and predictability and a sense of personal control into the lives of children who have been out of control for years and highlights the role that positive parenting, consistent boundaries and predictable consequences play in supporting children with difficult and challenging behaviours. It also enhances self esteem and teaches new self respect and a model for group living.
The personal hygiene, healthy nutrition, self care and family atmosphere in the units promote alternative ways of relating to others sharing the same living space. Also the suspension of drug and alcohol abuse, normal school routines and structured use of leisure time also offers the possibility of a substance free lifestyle and the return to mainstream education with all the opportunities that flow from this.
Staffing/Staff Care
Woodlands employs staff from a wide range of backgrounds and disciplines with most qualified staff in the house units having a professional background in social work or youth work. A smaller set of specialist staff are also on duty from 9-5 ie: 1 mental health nurse (3½ nurses in total over 3 shifts), 1 Forensic Psychologist (with adolescent specialism), 1 Family Therapist, 1 Part time family link worker, 1 Part time Niacro Link Worker and a Psychiatrist who visits the centre approximately once per fortnight to prescribe and monitor Psychotropic medication.
We are in the process of recruiting another nurse at present which hopefully will free the mental health nurse up to do more direct intervention work with the more high risk children, as at present the mental health service is really consultation ,risk assessment and crisis response only, as the medical department is working a “skeleton” service due to long term staff illness and we are becoming increasingly concerned about the extremely high numbers of clients with serious mental health difficulties that are being sent into custody . Even more worrying at times is how many of the young people are returned to the community who should really be provided with Secure Care or mental health beds for their own safety. Despite our best efforts to obtain safe accommodation for these children, they often end up back in circumstances which are far from ideal and which take little or no account of the risks we identify. We rely heavily on our links with Community Service teams and outside agencies to do the necessary follow up work in relation to these risks.
Staff Training
Obviously in order for us to meet the needs of the client group our staff require a high level of up to date training. Over recent years there is a recognition of the need to inform and encourage all staff to be mental health aware, thus ensuring that we begin to address the stigma of mental ill health and at the same time, we would hope that it will also promote peer support among our staff in relation to personal and work related stress in themselves or in others.
It is no secret that our staff work with a high risk client group, where verbal and physical threats and assaults on staff unfortunately do happen, and highly stressful situations can erupt at any time. To address this, Mental Health First Aid, which is a personal care initiative, has been recently approved for all our workers. In conjunction with this, we also employ staff care services who provide a counselling and support service which can be assessed confidentiality and staff are encouraged to make use of this service as often as they need to. Having thus provided this model to the staff themselves, they are then offered a series of training events designed to enable them to identify, assist and respond appropriately to mental health issues our young people.
The key training events organised to address suicide/self harm in the young people in custody in the centre are -:
- YOUNG PEOPLE AND MENTAL HEALTH AWARENESS
- TCI
- ASSIST
- SAFE TALK
- SEXUAL ABUSE AWARENESS
- BULLYING
- DRUG AND ALCOHOL AWARENESS
- PCC training is also mandatory to ensure safe methods of physical control
However, our training manager is currently struggling with the constraints of a limited budget, and while we recognise that all these extra courses are crucial to ensure that our young people receive the highest quality of care possible, it will be some time before all staff will be enabled to avail of the training outlined above. At present, only a few staff from each house unit can be offered this training at any one time.
For now regular consultation, co-working and feedback from sessions with the mental health nurses and the psychologist in the centre go some way towards meeting the need and ensuring good practice and sensitivity to the key issues involved.
Initial Assessment
The most important aspect of our work in relation to the mental health of the young people who pass though our centre hinges on the initial and ongoing assessments carried out by our mental health team, and our social work staff.
Mental Health Screening
Immediately on admission to the centre, each young person is interviewed by one of our mental health nurses, and a self report mental health screen is administered. This screen (SQUIFA) assesses the young person’s willingness to admit to being troubled by a range of mental health difficulties. I.e.: drugs and alcohol abuse, depression, anxiety, PTSD, self harm, suicidal ideation, or psychotic type symptoms.
Follow up phone calls are then made to parents, carers, children’s homes, schools, GP’s, Community Services, probation, juvenile liaison, and/or CAMHS Teams, to check the validity of the responses, as young people are not particularly reliable sources of information, and indeed they are often under the influence of drugs or alcohol when admitted, and/or are unwilling to admit to difficulties of this nature. The most risky children are sometimes those who are unknown to any other system, and whose parents/carers cannot be contacted at that time.
Follow-up In-depth Assessment
When, and if, any mental health concerns are suspected or confirmed, our nurses then arrange to carry out a more comprehensive assessment of the areas involved, in the form of a series of one to one interviews (SIFA). If we have information that a young person has made an attempt on their own life at any time, or if they appear to have evidence of serious self injurious behaviours, a risk assessment form is completed, and sent to all relevant departments. The nursing staff then either do the follow-ups themselves or liaise with the centre psychologist for co-working, consultation or follow-up (see next section) This risk assessment is regularly updated, and kept as a record in the young persons central file. Handover meetings are held at the end of each shift in each house unit to ensure verbal communication to all staff of relevant risk emotional well being related information.
If CAMHS have been involved before, links are made to seek advice re: previous interventions, and to ensure continuity of care we also try to facilitate out-patients appointments which were set up prior to admission to custody (risk assessment permitting)
Observations and Monitoring to Cover Risk
For the first 24 hours in custody, all young people are observed closely, as per initial risk assessment, as research indicates that admission to custody can be a trigger for impulsive self harm/suicidal behaviour. Following this, observations are reviewed regularly by the mental health staff, in consultation with unit managers, key workers, and parents, to ensure that any changes in presentation, life circumstances or risk are noted, recorded and acted upon. Our observation schedules range from every 15 minutes (Standard Care), to constant contact obs, with the majority of our high risk children on intermittent observations, with between 2 and 5 minutes in between checks. The design of the observation panels in the young peoples bedrooms are such, that the opening and closing of viewing panels, are electronically recorded and monitored, on a central computer in the control room, thus ruling out human negligence or error. A strategy meeting is called as soon as possible following admission, to pull information, and resources, from outside agencies, who maybe, or need to be involved.
Ongoing Assessment
Recording and Monitoring
Written recordings of all significant daily events, in relation to each child, both within and out with the centre, are recorded in the daily log. Special care is taken with the recording and monitoring of young people who either choose to separate themselves from the group, or who are removed to their rooms for time out, as this often has a bearing on their emotional state, and their coping strategies for dealing with stress or conflict. Also when serious untoward incidents occur in the group setting, and young people are required to be removed to their room by staff for their own, or other people’s safety, a life space interview is conducted as soon as possible, to address the issues that led to the removal. We would hope that this provides Young People with a model for problem-solving and conflict resolution that does not involve impulsive, violent or harmful behaviour.
Onward Referral to Outside Agencies
Also, if during his or her stay in JJC, the Staff here, or visiting family or professionals, believe that the young person may be developing mental health problems, that were not previously identified prior to admission, these concerns are shared with all relevant parties, and a referral to appropriate sources of support is made prior to their release by the mental health staff who were involved with them in the centre. E.g., CAMHS, Contact Youth, New Life, Chill, Opportunity Youth, etc. Unfortunately, many of our young clients who appear to be motivated to get help while in custody, often fail to attend appointments, set up for them in the community upon their release. This is a significant problem in planning and delivering services for this client group, as it is often necessary to track these young people down in order to develop relationships which will then motivate them to attend of their own accord. This is costly in terms of time and resources, but is often the only way to engage disenchanted young people in work which addresses their emotional well being and their high risk behaviours. The MST team at Linden are an example of this approach and practice.
YJA Community Services
Our community services teams also link with the centre and often step in to breach the gap between young people leaving custody and getting mental health appointments with a local CAMHS team to increase the chances of their attendance by maintaining the link with them in the interim.
Psychology
Most cases referred to psychology come through the medical staff or the case management process. This ensures that only cases where there are serious concerns are seen. Children with serious self harm issues or suicidal ideation or behaviours are prioritized. These sessions are usually co-worked with key workers or the psychiatric nurses. `The young person is engaged in a discussion as to their life circumstances and difficulties and the thinking behind their behaviours. An assessment of their levels of hopelessness, depression, suicidal ideation and self-esteem is carried out, with further sessions involving exploration of key themes highlighted therein.
The circumstances surrounding each self-injurious or suicidal behaviour incident are explored in detail to help identify triggers ,antecedents , methods and means considered and the accessibility of these .These are balanced with current emotional presentation, personal resilience, reasons for living , protective factors and potential supports that would be acceptable to the young person.
These assessments quite often reveal high levels of stress in their lives, high levels of unresolved trauma and serious problems with the misuse of alcohol and drugs, which quite often started as a way of coping with difficult feeling s and life events.
Intervention flowing from these assessments, involves exploration of alternate coping strategies for dealing with emotional distress, self esteem enhancement and focused therapy sessions in relation to past trauma where time frames allow. When this is not possible, referrals are sent to the most appropriate external agency and motivational work is done to encourage them to attend appointments we set up for them following discharge.
Many of our clients report that they self-harm or take risks with their lives, while under the influence of drugs and / or alcohol and later have virtually no memory of what they did. However, there are others for whom the option of suicide or self-harm presents itself again and again as a way of solving or resolving problems in their lives that they can see no way through.
Liaising with Other Interested Professionals
Our awareness of such coping mechanisms means that a large part of the work of the mental health workers involves liaising closely with social workers, GP’s, children’s homes, hostels and family members if appropriate, to alert them to the risks identified and advise them accordingly.
However our mental health resources are overstretched at present in relation to the throughput of high risk children in our system in recent months. So much so, that we have recently approached senior management with recent data which highlighted our concerns that our mental health resources are totally inadequate to ensure best practice in every case to deal with the risks we carry. Ethical practice demands that if assessment highlights/identifies a need, then every effort should be made to address that need as promptly as possible and while we make every effort to do this, given our limited resources and competing demands on our time, there is always the possibility that we will miss something and a tragedy will ensue.
We are now in the process of negotiating a fast track through to CAHMS in all 4 boards for young people that we are particularly concerned about, and a new psychologist post’s with a link to CAHMS teams throughout the province but it will be some time before these arrangements are finalised.
In the meantime, we will continue to prioritize these children and do everything in our power to ensure their safety and wellbeing both while they are in the centre and also when they re-enter the community.
Education/Daily Routines
As a contrast to the often chaotic lives these young people have lived, when in their own community, where behavioural programmes, truancy, and exclusion from school feed into criminal activities, and misuse of alcohol and drugs, Woodlands runs a normal school day, for all those in custody, with education packages tailored to meet individual needs We offer a balance of basic skills, (English, maths and reading recovery) and vocational studies such as woodwork, car mechanics, catering, music and art, providing opportunities to experience success, enhanced self esteem, and enjoyment in learning, thus supporting each child to explore and exploit their natural potential.
All school work is accredited at a level appropriate to each child’s ability and attainment level and they leave with certificates to this effect ranging from basic AQA awards to GCSE’s.
Educational Assessment
This is made possible by a comprehensive educational assessment being done, within their first few days in the centre, which includes intelligence, literacy, and numeracy assessment. More recently we have introduced an assessment of resilience, influenced by research, indicating that this can and should inform all interventions designed to help young people find their way through what are often very difficult life circumstances.
The education assessment has great value, as it provides data on children who sometimes have evaded the assessment process for years, and thus provides all workers and agencies involved in planning interventions for him/her with vital information on their intellectual strengths and limitations. Largely as a result of this, school refusal is a rare phenomena at Woodlands.
On occasion, educational assessment also leads to questions being asked as to whether some young people have an undiagnosed disability, such as Autistic Spectrum Disorders, or to questions being asked as to whether some young people are even fit to plead, and therefore at times, recommendations for consideration of specialised assessments leading to alternative disposals other than custody, e.g. mental disability services, and provision.
Education/Training/Employment Links with Outside Agencies
We also have an educational link worker who sets up work, education, training, and employment opportunities for those leaving the centre. It is hoped that these placements provide them with new opportunities to integrate into mainstream society, give a meaningful structure to their day when they leave, and the hope of a better future.
Daily Routines
Woodlands has a no-smoking policy which encourages yp to experience and consider a healthier lifestyle free from cigarettes, drugs and other substances which they often believe on first entering the centre, that they cannot live without.
They are encouraged to shower daily, organise their own laundry and take pride in their personal space and belongings. Healthy eating and regular use of the gym, the pool and the fitness suite and access to creative activities such as music and art play their part in promoting good physical and mental health. Each day is structured to ensure that the children have a balance of intellectual and physical stimulation and relaxation. Requests for private time alone are respected within reason, but all residents are expected to conform to group living rules and expectations. Pro-social modelling is used at all times and non-violent conflict resolution and negotiation skills are taught, both directly, through key work sessions, and indirectly through incident management.
Programmes
Following initial assessment by our nursing staff each young person is introduced to life in Woodlands through a standard induction procedure. The daily routines, visiting and telephone arrangements, support systems and complaints procedures are explained both verbally and in booklet form and the bullying policy is gone through very carefully on a 1-1 basis assessing for comprehension levels and potential for victimisation and/or perpetrator behaviour.
Induction
The first programme input takes place at the induction stage in the form of a problem-solving programme delivered individually to each child, as it is recognised that this is a core life skill that is often deficient in young offenders. It is also noted to be lacking in many young people who resort to self harm or suicidal behaviours, and we reinforce the use of problem solving skills at every opportunity throughout their time in the centre.
Groupwork Programmes
Each young person in the centre participates for one session every day in a range of group work programmes, especially selected to encourage personal and social development, and to address issues directly relevant to the needs of young people in our society today. Examples of the programme on offer are emotional intelligence, drugs and alcohol awareness, self esteem enhancement, coping with stress, suicide awareness, safe talk, bullying, sexual health, problem solving, parenting, moral reasoning, conflict resolution, and anger management. We also provide games on teaching thinking skills, anger management and social skills, and activities and workshops addressing bereavement and loss, domestic violence, sexual exploitation and homelessness.
Helpline Personnel
For some of these programmes, we invite outside agencies such as Pips, Niacro, Contact Youth, Samaritans, Out of the Shadows, Simon Community etc, to take the groups, and thus introduce them to the people at the other end of the telephone numbers on the contact cards we encourage them to use as a lifeline when they are back in their own communities, and feel they have nowhere else to turn.
It is perhaps worth mentioning, that on the last occasion that the suicide awareness programme was delivered in almost every group of six to eight young people, there were at least two to three present who had personally known someone who had succeeded in taking their own life. As a result of discussion in relation to this, many young people expressed an interest in partaking of the SAFETALK training. This training should give those young people trained in it full justification and validation for passing on information about other young people`s feelings or intentions to staff, family members or appropriate adults in the community without fearing retribution or loss of face for sharing confidences.
It is hoped that this training will also give these trainees a certain kudos within their peer group and build another block in their skills repertoire.
Family Services
We have a family service team in the centre consisting of one fulltime family therapist and 1 part –time family link worker and one Niacro link worker. They have close links with our community service teams most of whom are trained in systemic practice. This ensures that links with families of our young people can be promoted, both in the centre, and back the community.
This is a very important service as it not only gives our workers an insight into the dynamics of the a young person’s family of origin but also it provides a support service which makes constructive problem-solving and dialogue possible between the young person and parents /carers who are often under considerable stress due to conflict in the home and strained relationships within the community as a result of the young person’s offending behaviour and lifestyle.
Parent’s Group
The family service in liaison with Niacro, also run a support group for parents one night per week, at which a range of topics relevant to parenting adolescents are discussed. Eg: Drugs, self –harm, suicidal behaviour, sexual abuse, suicide awareness, parenting skills etc. More recently, following the recent spate of adolescent suicides, they intend to offer Assist training to any and all parents who wish to attend. They expect a good response to the offer of this course to parents, as hopefully it may empower them to respond appropriately to the distress signals that are sent out by their children, and to know where to go for help and support in times of crises in their own lives as well.
One of the issues raised as a result of this support group was the high levels of mental ill health evident in the extended families of young people in custody, and the very real challenges these parents face in their attempts to offer consistent care and control to young people, who often present experienced professionals with real dilemmas in how best to handle them.
In a recent meeting of the family support group, 50% of the participants shared that they had had a family member who had either attempted or completed suicide. (In some cases, more than one family member had done so). This demonstrates the high levels of distress and need present in the families we serve, and obviously also presents the workers with an opportunity to assist parents to link up with counselling and support services available to them in the community.
Spiritual Guidance and Support
All young people have weekly contact with Ministers of religion in the living units. Again all significant information related to personal .family and community circumstances is passed on during these visits, and all residents are encouraged to avail of this service. Obviously they play a special role in relation to those who have no family contact or visitors and those who receive news of the deaths of family or friends while in custody, particularly those that occurred as a result of a violent incident, and/or those who may have taken their own life
In the Past 2 months alone we have had two children who have had to cope with this type of loss with all the risks that flow from that.
Discharge Planning
In high risk cases staff from the centre will contact GP’s, parents, children’s homes, YOC and CAMHS teams when the young person is being discharged from custody, highlighting areas of concern or risk and urging for urgent intervention when necessary. We strive to ensure a seamless delivery of care centred on the young person. We inform them of any serious self –harm incidents and or suicidal ideation and behaviour and antecedents to this.
If there is a link between substance misuse and high risk behaviours we make a referral to services who specialise in this. We are currently in the process of revising and refining our communication systems with outside agencies in relation to discharges requiring follow-up services, as we feel that this is an area with room for improvement.
We also provide each young person leaving the centre with an emergency contact card, on which numbers of the main telephone help-lines targeted at our age group are listed.
It is our hope that these cards might mean the difference between life and death and that if this helps even one child they have served their purpose.
GAPS
From our experience in dealing with this very risky client group the following gaps in service provision come up again and again.
- A shortfall in the number of secure beds available to young people, are putting themselves or the community at risk by their high risk behaviours. Many young people are bailed back in to the community to family or children’s homes placements, when we have highlighted a very real risk of suicidal behaviour or have expressed concerns about a young person’s mental health.
- A shortfall in the number of secure psychiatric beds for adolescents suffering from depression, psychotic illness and/or bizarre complex presentations which render them unsuitable for placements at home or in the community, where they will continue to abuse drink and drugs as a way of coping with their emotional distress.
- A need for an adolescent forensic mental health facility for those young people who require in-depth mental health interventions and who also come into contact with the juvenile justice system for more serious crimes, but who are unsuitable for placement in Woodlands.
- Shortage of residential accommodation/hostels/staffed hostels for the vulnerable 16+ age group who are too difficult to manage in a children’s homes and yet too immature to function in semi-independent living placements. Many of theses children abscond from the placements they are sent out to and eventually end up homeless which obviously puts them at even greater risk.
- A need for more resources targeted to meeting the needs of young men and women who have experienced sexual or physical abuse in childhood and who, have not yet received treatment for this. Many of our clients require long term therapy in relation to past abuse.
- A need for more specialist foster placements for vulnerable/troubled 11-18 year olds where being, part of a family will actually go some way to addressing issues of rejection, abuse or neglect in families of origin, and for whom children’s homes, hostels etc are regarded as inappropriate/or inadequate to meet their needs.
Ongoing Action Points
As is evident, I’m sure, in my response, there are a number of action points in Protect Life – A Shared Vision, which we are already taking forward in relation to ourselves. These are, namely:
- to continue to press for more resources in our mental health department including administrative support
- to promote the recognition of the priorities identified within the suicide strategy to be recognised by NIO and reflected in individual departmental annual priorities
- to improve our links and information sharing protocols with tier 2, 3 and 4 services to ensure that those who are identified in our system as having mental health difficulties receive the interventions they require
- to continue to promote the information and awareness campaign for young males, aimed at breaking down the current male culture of not discussing problems openly through key-work and group-work programmes
- to raise awareness of the links between sexual and physical abuse and self harm/suicidal behaviours, and to encourage our young people to break the silence of undisclosed abuse and access the supports available to them
- to raise awareness and provide information education re the support systems and social networks available to young people who are in crisis re their sexual orientation, and to challenge all forms of bullying and prejudicial attitudes and behaviour toward minority groups in general and those of homosexual, bisexual and transsexual orientations in particular
- to continue to avail of and support Niacro in its mentoring schemes for vulnerable young people
- to continue to implement a targeted information campaign aimed at enhancing the mental health and well-being of all members of our workforce and our client group as a whole
- to continue to encourage the development of personal coping skills and problem-solving skills in the children we work with and to continue to draw attention to the need for more in-depth work and follow-up with those who present with serious self-harm and suicidal ideation and behaviour
- to liaise with DAST in relation to young people who have problems of this nature to ensure that every effort is made to support them to reduce their intake of drugs and alcohol and find meaningful ways to fill their lives
- to continue to provide up to date training events to inform and enable our care staff to work more effectively towards the reduction of self harm and suicidal behaviours
- to continue to provide families with support to improve parenting skills, family relationships and coping strategies for dealing appropriately with their children’s communications of distress and help seeking behaviour
- to develop a better understanding of the role the internet may play in changing the culture of suicidal behaviour among young people
- to continue to support any and all initiatives which improve the mental health provision for those who are no long classified as children by virtue of the fact that they have turned 18, and yet whose needs cannot be fully met in adult psychiatric facilities.
Conclusion
As is evident , I am sure ,in my response, we in Juvenile Justice Centre perceive our role in relation to this problem as mainly prevention through education and skills training , risk assessment, risk management and onward referral to intervention services in the community. We are restricted by the conflicting demands of the justice system, limited resources in the mental health department and the responsibilities of catering for such a large throughput of high risk children every year.
Hopefully, our submission will serve to illustrate that we take our responsibilities to these children very seriously, and we are well aware of the part we play in recognising and identifying their needs, and facilitating their access to the mental health services they require.
We consider ourselves to be pro-active participants in the “shared vision” of the Suicide Task Force and look forward to a reduction in the tragic loss of life that led to this initiative in the first place.
Samaritans
A. Introduction: Samaritans.
Samaritans is a non-religious, non-partisan organisation representing 202 organisations across the UK and Ireland working under a constitution that seeks to provide confidential support to people in distress and despair, including those considering suicide.
Samaritans was founded by the late Reverend Chad Varah in 1953 and is regarded as the UK/I’s first “helpline”, providing support to people in distress and despair, including those considering suicide. Samaritans is a volunteer led organisation, headed by a small board of trustees and an association made up of the lead volunteer from each of the 202 autonomous federated branches. Samaritans network of branches developed slowly as a community led initiative wherever suicide was recognised as an issue.
What Samaritans offer
Samaritans mission is to be available 24 hours a day to provide confidential emotional support for people who are experiencing feelings of distress or despair, including those which may lead to suicide.
Our vision is for a society in which
- fewer people die by suicide
- people are able to explore their feelings
- people are able to acknowledge and respect the feelings of others
Our mission and vision are based on the following values that underpin our policies and in our responses to external environments including public policy.
The importance of having the opportunity to explore difficult feelings
That being listened to, in confidence, and accepted without prejudice can alleviate despair and suicidal feelings
That everyone has the right to make fundamental decisions about their own life, including the decision to die by suicide.
Samaritans services in Northern Ireland are delivered through 8 branches.
Samaritans Branches in Northern Ireland
Ballymena |
Craigavon |
Bangor & North Down |
Derry |
Belfast |
Newry |
Coleraine |
Omagh |
In 2004 Samaritans received over 4,500,000 contacts across the UK with over 73,000 of the contacts received in Northern Ireland. Samaritans service is provided via telephone, text-phone, email, face to face contact and letter. Samaritans in Northern Ireland volunteered over 95,000 hours of active listening
Running in parallel with our support service we provide a number of targeted interventions under the banner of Emotional Health Promotion. Emotional Health is the part of our overall health concerned with the way we think and feel. It refers to our sense of well-being and our ability to cope with life events. Emotional health is about our ability to acknowledge and respect our own emotions as well as those of others.
B. General comments on the consultation
1. Background to our involvement in Protect Life
Samaritans was happy to be invited to sit on the Suicide Prevention Task Force (initiated by Minister Shaun Woodward) taking this as evidence of our expertise in this area and reflecting our input into the sister strategies of the neighbouring administrations of the UK and Ireland. Samaritans remains happy to continue working with the Department in the delivery of the Protect Life strategy and hope this examination will deliver new insights that will lead the strategy to even further success.
However we cannot claim that we pursued a strategy for Northern Ireland. We must applaud the community, particularly the commitment of the families bereaved by suicide, for their sustained work in keeping this issue on the agenda and driving the delivery of the strategy. We hope that we can also work more closely with these groups in the future
The development of a national strategy is a positive step but is only one step in actually trying to reduce suicide. Samaritans was supportive of the previously published, and more expansive, Mental Health Promotion Strategy and was disappointed that due to a number of reasons, including lack of monitoring and proper resource allocation that this strategy failed to deliver on its 10 objectives. It is critical that those empowered to deliver the strategy ensure that this initiative is non-stigmatising in its approach.
2. Protect Life
Samaritans welcomes the Protect Life initiative despite these limitations, as this strategy draws attention and resources to an important issue. From our work in other administrations it is clear that Protect Life draws from the best practice in this area and that it also seeks to work in parallel with similar work that is taking place in the Republic of Ireland. We applaud the Government’s resolve to reduce suicides, and wish to play a key role in this work based on our long experience of delivering a valued, experience based, service
However, Samaritans is concerned that the desire to deliver innovative interventions means that established interventions have been sidelined, or have been neglected as the early promising results of pilot work are taken as a guarantee of efficacy. We have particularly seen this in the perception of, and attitude towards our own work (of which we would be happy to say more about in person to the committee), where too often we hear that “all Samaritans do is listen”. This is disappointing and represents a failure to understand the nature, not only of our service, but of the needs of people in distress and those who are suicidal.
We have seen models of our work, in delivering a helpline known for its work on reducing suicide and in delivering longer term support to outpatients from A&E picked up by the strategy. Though this is gratifying we are again concerned that the desire to act quickly on this issue means that these projects are moving forward without sufficient evaluation. This is disappointing and has left Samaritans with no choice but to step away from the operational delivery of this work.
A concern with the value system underpinning Protect Life is that it could be seen to focus on stopping the event of suicide but not on addressing what it is that leads to a desire to kill oneself. We do not feel that the democratic freedoms of an individual can be ignored or summarily disregarded except in the exceptional circumstances where they are judged to be incapable of making a decision. Where they are, as can happen if an individual approaches statutory services or a helpline that focuses on getting a declared individual into counselling or hospital is that these forced and directed interventions tend only postpone the event. We also hear anecdotally that once these services are experienced the individuals avoid them after that first experience because they have lost control of their life decisions.
C. Specific comments on questions raised in the consultation paper
1. What is the scope and appropriateness of the Department’s strategy ‘Protect Life: A Shared Vision’;
From Samaritans perspective, having input to the other existing suicide prevention strategies in the UK and Ireland it appears that the strategy has learnt from the best of the strategies. It is also clear to Samaritans that the strategy has been developed with a clear view to how closer working can be developed with agencies working in the Republic of Ireland to make this an All Island Strategy.
Central to Samaritans vision is a society in which there are few suicides. It is our firm belief that this vision is achievable through the provision of confidential emotional support, information provision, changing attitudes and promoting healthy coping skills.
2. What is the level of stakeholder involvement;
We have already applauded the Government and the Families Forum for their work to reduce suicides, our concern is that the role of the specialist charities working to reduce suicides has not to date been allowed to play the role they could. There is no conspiracy to stop them but the set up of the delivery mechanisms has failed to recognise their needs. There are key areas in particular where we feel action is needed.
a. Representation
Samaritans was fortunate enough to secure its place on the Taskforce and Implementation body citing our experience in other administrations suicide prevention policies. However the implementation body has focussed predominantly on the action of the Boards and Trusts to develop their own sub-strategies and spent little time examining the plans of the formal voluntary sector. In the time of the strategy Samaritans has launched interventions for the school and workplace, developed support service for jurors, a new method of access to our service via SMS text message and a major campaign on improving access to support service for vulnerable people using the internet
b. Funding
We are concerned that funding for this initiative; though generous in relations to the other administrations and the size of population is again locked into the formal sub-regional health structure and for the purposes of national organisation dictates that in order to gain funding for region-wide work requires multiple applications to be submitted. Each of which is independent of the rest. There is therefore the potential for service delivery to be fragmented because of this. We have also had feedback from our branches (of which there are 8 in Northern Ireland) that the bureaucracy in applying for funds in overly onerous. This is also a criticism we have of the fund management we currently have to navigate for the annual grant we are fortunate to receive from the department which this year totals £15,000 to cover the work of 8 branches, each of which requires approximately £20,000 to keep open. Though Samaritans is the most well known agency involved in suicide reduction work it is regrettable that to date we have not benefited from any of the specific funding for suicide prevention available for our work in Northern Ireland.
c. Cross Government Engagement
It is a much abused term that suicide should be “Everybody’s Business” and in attempting to make suicide prevention in Northern Ireland a cross-government strategy the DHSPSS is to be applauded. Samaritans strongly believe in the role of educational interventions from a young age to help individuals in society build up their emotional health, resiliency and abilities to seek help at the earliest opportunity. We have seen the educational initiatives developed to date and in use by the Department of Education and commend their work to address this area. We too have developed a number of resources for sc schools and would look to the Education department for support in promulgating our resources, particularly the Developing Emotional Awareness and Learning (DEAL) resource which will be covered in more detail later in this submission.
3. To examine the level of services and support available to promote good mental health, to prevent suicide and self harm; and to support those affected by suicide
a. Emotional Support Services
Samaritans Emotional Support Services can be accessed by a variety of methods, we are best known for our telephone service but we also offer support by face to face contact, email, letter, text-phone and SMS text message and are know examining the use of instant messaging services. The telephone service has been in existence for over fifty years and in the course of these years Samaritans has expended significant resources in ensuring that the support line provides the most relevant and up to date approach for potential users by modifying our service, clarifying and codifying our systems and making use of innovative technology solutions to ensure that those in distress have the best chance of making contact with the service. An example of this is the development of a telephone call answering system that when accessed by use of our 08457 90 90 90 phone number routes the call the nearest branch and should that be busy onwards to the next ten geographically closest branches. This gives Samaritans a less than 1% engaged rate.
One of the concerns of our engagement with the strategy has been the commitment of time and resource into the development of “all embracing” telephone helpline to stop suicides, currently being piloted in North and West Belfast and now out for regional tender. This service was announced by Minister Woodward against the advice of Samaritans in the early days of the action plan. It duplicates much of our own long established and respected service and for Samaritans this is a disappointment. Having come forward early in the development of the strategy to offer our support and with the benefit of our 50 plus years of experience we feel that there is little benefit to the NI population by creating another helpline. However, we remain keen to work with the operators of the service and hope that they will engage with us so we can share our expertise in talking with emotionally distressed individuals.
If we do have to step away from this project it will be because we would not feel it right to attempt to stretch our existing and respected service to replicate and integrate the distinct service offerings of the NSPCC, Papyrus or statutory services. Our service exists to give people time and space to explore the implications of a situation, including suicidal ideation. We do not promote suicide, but we do promote options and implications of those options.
Samaritans will continue to provide emotional support services and will also extend our service to new technologies wherever these are identified as practical and useful for our callers. We are currently developing guidance for our branches on the use of online access methods including the use of social networking sites such as Bebo, Facebook and MySpace and working with the UK/I governments on best practice in these environments to reduce suicides.
b. Emotional Health Promotion Services
Samaritans work is about providing emotional support to those in crisis and promoting emotional health by changing attitudes, providing information and promoting healthy coping skills. These approaches go hand in hand since we need to promote a better understanding of emotional health and encourage people to seek help (emotional health promotion) if we are to effectively run emotional support services. Emotional health promotion has been recognised by the strategy, alongside risk reduction, as an equally significant factor in reducing suicides.
To date we have developed interventions for Schools and Workplaces, both of which we feel provide a good fit with the Protect Life strategy. A copy for each committee members is enclosed.
i. DEAL – Developing Emotional Awareness and Learning.
DEAL is a programme of resources designed by Samaritans for use as part of a whole school approach to emotional health and wellbeing, focusing on resiliency building and the development of coping skills. Aimed at secondary schools, it comprises a range of resources developed by Samaritans, which includes a six part DVD, cross-curricular lesson plans, an information booklet and training exercises for teachers. It also includes fact-sheets and links to further resources.
The materials have been developed, in partnership with Royal and Sun Alliance, for use in secondary schools with young people aged between 14 and 16 years old. DEAL contains footage of young people and teachers who have used the DEAL resources talking about their experiences. It explains how emotional health is an integral part of school life and addresses some of the fears teachers have about delivering this topic.
In developing DEAL we commissioned qualitative and quantitative research amongst young people to learn more about their current understanding of emotional health and areas where DEAL could be useful. DEAL was developed by teachers and Samaritans volunteers and in partnership with other specialists in the field. A two phase pilot process was undertaken to thoroughly test the materials involving 1000 students across 11 different schools to test the materials and this feedback was incorporated into a second draft of the materials.
The materials were sent to every secondary school in UK and Ireland in October 2006. Though we have had some engagement with the Department for Education regionally, and with the Education and Library Boards due to a lack of resources with Northern Ireland we have found it difficult to maximise these relationships.
ii. Work Life
To complement our interventions in schools, and in line with best practice in the area of Mental Health promotion Samaritans has also developed an intervention for workplaces know as WorkLife which aims to help managers and employees find a sustainable work-life balance and to operate in effective, harmonious teams.
Based on our own research and drawing from the work of the Health and Safety Executives’ Stress Management Standards we believe that Work-Life makes a substantial contribution to the aims of the strategy.
The benefits of this work will be to reduced absence and improve morale. It will allow staff to feel valued improving retention in work, which has been shown to be a key structure to maintaining good mental health. We believe this will also help businesses increase their productivity
4. Consider what further action is required, taking account, as appropriate, of experience elsewhere.
Samaritans has welcomed the opportunity to work with government, industry and third sector colleagues on initiatives to reduce the number of suicides, and has through its ability to work across administrations been able to examine this work from a unique perspective. It is our wish therefore that this experience and work is drawn on and used rather than duplicated or discounted.
The example that we would draw to the committee’s attention to is that of suicide and the internet. Samaritans has sat on a number of bodies looking at cyber-bullying, social networking and with the recent Byron Review of young people and access to technology. This work in other administrations especially where it relates to global issues or where the matter is not entirely reserved, because it has implication for devolved matters such as health and education, needs to be seen as part of wider picture and cannot solely be seen as regional matter.
As suicide prevention strategies mature we would also suggest that the committee look towards the learning from other countries in how they further this work. We fully believe that a difference can be made to the number of lives lost to suicide and are keen to bring our experience to any forum of the government to play a full part in this. We are happy to explore any issue presenting with the committee and would welcome the opportunity to do so.
Anthony Langan.
Public Affairs Manger, Samaritans.
NI Music Therapy Trust
Green Gym, Conservation Volunteers Northern Ireland
Green Gym: Promoting health, fitness and the environment
Green Gym is a health initiative delivered by Conservation Volunteers Northern Ireland which offers individuals an outdoor alternative to conventional gyms. Creating the opportunity to increase physical activity levels through participation in locally based practical conservation work that has a proven impact on physical and mental health and social well-being whilst also benefiting the environment.
Through a flexible needs-based approach, focusing on increased outdoor physical activity enhancing local environments, the Green Gym tackles, the sometimes overlapping, issues of: obesity, sedentary lifestyle, poor mental health, the balance of good health, unhealthy environments and poor quality of life, social exclusion and lack of social cohesion.
Conservation Volunteers Northern Ireland has been a registered charity involving all sections of the community for 24 years. We’re aiming for a better environment where people feel valued, included and involved. Every year Conservation Volunteers Northern Ireland, which is part of BTCV, connects with 29,800 people who make positive differences to their local communities and their environments. The Green Gym project contributes 14.97% of Conservation Volunteers annual volunteer work days. Our mission is to create a more sustainable future by inspiring people and improving places.
Background
The Green Gym concept was developed in the mid-1990’s as a partnership between an Oxford GP, Dr William Bird and BTCV. The Green Gym provides physical activity alternative for people who may not be attracted to a leisure centre setting, creating healthy people and healthy places. This innovative approach recognises that being healthy is not just about being fit, but also stressed the importance of the triadic relationship between the health of the local community, the local environment and the individuals within that community / environment. The first Green Gym project opened in 1997 in Sonning Common, Oxfordshire, with more than 95 groups running across the UK.
The Green Gym has been monitored and evaluated by Oxford Brookes University, Centre for Health Care Research & Development using a range of broadly accepted tools to measure indicators of health, including the SF-36 (Jenkinson et al 1996) and Medical Outcomes Trust Short Form (SF-12) questionnaires and the EQ-5D among others. The Green Gym has major social, physical and psychological impacts in addition to the environmental ones demonstrated by research evaluations in Oxfordshire and East Sussex, England (Reynolds 2001).
Green Gym in Northern Ireland
Since 1999, Conservation Volunteers Northern Ireland, have developed and delivered the Green Gym project across Northern Ireland in close partnership with local Health Trusts. This has included the former Health Trusts of Armagh & Dungannon, Causeway, Foyle, Homefirst, South & East Belfast, Sperrin-Lakeland and Ulster Community Hospital.
The Green Gym project works in close partnership with Health Trusts directly targeting individuals who traditionally do not get the opportunity to be involved in this type of work.
Initially involving individuals based within Day Care Services the Green Gym has progressed to incorporating a wider audience of groups and individuals, for example; disadvantaged communities, women’s groups, schools, BME and elderly.
NI Strategies
The Green Gym project meets the needs which have been clearly outlined in a number of Northern Ireland Regional Strategies. The impact on mental health is highlighted below.
Mental Health
Mental health problems are a leading cause of illness, distress and disability in Northern Ireland with over 100,000 people seen by general practitioners each year. Around 11,000 people are referred to be seen by a psychiatrist each year.
Mental ill-health affects every fourth citizen in Northern Ireland and cost an estimated 3-4% of GDP through loss of productivity - over 3 million working days are lost every year. Mental ill health is as common as heart disease, 3 times as common as cancer and 3,000 time more common than HIV / Aids.
The Bamford Review of Mental Health & Learning Disability (N.Ireland) 2006 provides compelling evidence of the need for comprehensive reform and modernisation of services. Further concerns are based on how our society treats people with mental health needs or a learning disability, people who still experience social exclusion, stigmatisation, discrimination and erosion of their fundamental rights and dignity.
The cost of failing to address these issues are far-reaching, impacting on the quality of life of individuals and families, their physical health and capacity to make effective use of health services, their employment and productivity and the general economic capital of the entire community. An inter-departmental and cross sectoral approach is central to the successful implementation of the Bamford review, emphasis on promoting the mental health of the whole community and supporting mental health through preventative action.
Conservation Volunteers Northern Ireland strongly promote and successfully deliver the Green Gym to people who experience mental ill health as well as other socially excluded groups. The Green Gym conveys a range of social and mental health benefits, for example, working with others encourages participation in the local community, learning new skills and successfully completing a task builds confidence and self-esteem, ‘working out’ in the fresh air, in contact with nature relieves stress and anxiety.
Due to the proven benefits of the Green Gym on improving fitness, relieving stress and increasing feelings of well-being, Conservation Volunteers have been able to establish strong working partnerships with Occupational Therapy Departments to promote the Green Gym to their patients. Initially developed within The Mater Hospital Psychiatric Ward, Finneston House Downpatrick, Holywell Antrim and more recently Shannon Clinic Knockbracken, the Green Gym has positively engaged adults suffering from a severe and enduring mental illness.
The Green Gym is highly valued by the Multi Disciplinary Team within the Mater Day Hospital setting as it fills a need and gap in services especially from male referrals. In the In-patient psychiatry wards the Green Gym is particularly useful in aiding discharge due to the flexibility in project delivery. Through regular monitoring 85% of participants strongly agreed to a perceived increase in their mood and self-confidence, 90% stating they felt more positive about themselves through their involvement in activities (NI Green Gym 2007).
The OT Staff at the Shannon Clinic, Knockbracken stated ‘The Green Gym has been an amazing programme which allows us to observe our patients in many different environments. Many patients who have not engaged well in groups within Shannon have responded incredibly well to the Green Gym group and have consistently attended sessions. Despite some of their mental states being still in acute stages they have shown ability to work through and complete tasks, working well with others which at times is not observed in the ward environments. We feel much of this success is due to the expertise of Conservation Volunteers staff, the suitability of the tasks and pace of learning, and the sheer sense of fun the patients experience when out on the Green Gym. All of our patients have been observed to be more spontaneous, relaxed and generally in better mood when out with the Green Gym which continues on their return to the ward.’
Conservation Volunteers strongly believe that through strong partnership working the Green Gym can play an active role in tackling these issues with young people. In Northern Ireland where we have directly targeted children, the projects have not had a mental health specific focus, reports from the state teachers that the outdoor gardening activities have positively engaged pupils whom are normally disruptive and difficult to work with. The teachers also reported better behaviour and concentration in class following their pupils participation in physical activities associated with the Green Gym. Sustainable delivery, close monitoring and analysis are needed in this area to provide a more conclusive evidence base.
BTCV Green Gym projects have been subject to three research studies by Oxford Brookes University. The second of these, an evaluation of the Portslade Green Gym, aimed at determining its impact on psychological health, found that 44% of participants reported moderate to severe impairments in anxiety and depression at the beginning of the study (EQ-5D health related quality of life instrument). It reported, in the first three months of taking part in the Green Gym, there were significant improvements in mental health component scores of participants, 90% are showing an improvement, the mean average score of participants with an initial score below 50 (mean) has increased by 2.7, and a strong trend in the decrease in depression (Reynold 2001).
As outlined by Health Minister Michael McGimpsey ‘It is vitally important if we are to improve health and meet the challenges ahead, that we continue to work in partnership, combining our efforts on those issues and settings where we can make a real contribution’ (IFH Conference 2007) .
The Green Gym can play a key role in achieving these objectives and those outlined in the Regional strategy and action plan 2003 –2008 Promoting Mental Health. This identifies that mental health and emotional well-being are influenced by many factors which lie outside the control of the Health and Social Services and indeed the government. Good mental health promotion depends on expertise, resources and partnership across all sectors including statutory, voluntary, community and business sectors.
In 2006, 291 people in Northern Ireland took their own lives, an increase of 102 per cent from 2003. Suicide may be an extreme result of poor mental and emotional health with many contributory risk factors. One study from Northern Ireland is cited in which a psychological autopsy was carried out on all suicides for a twelve month period in 1992/3. A strong gender effect was observed with ‘major unipolar depression’ as the principal diagnosis for 52 per cent of the women but only 26 per cent of the men. Age was also significant with depression as the principal factor in three quarters of the suicides of those over 65yrs and 27 per cent for those under 65, Foster et al 1997.
While no specific intervention has been found to be universally effective, these risk factors must be addresses as part of a broader approach to mental and emotional health. Preventive measures include; reducing access to the means of suicide; promoting coping skills in the general population; targeted work with vulnerable groups; well managed and responsive health and social services which can recognise mental problems early and make timely interventions. These actions can and should be tackled through a wide range of settings and sectors.
In the past 18 months through partnerships with OT Departments within psychiatric services, Conservation Volunteers have gained experience of this complex area of mental health. A number of individuals involved in the Green Gym to date were disclosed as having suicidal thoughts and / or recognised self-harmers, but only limited detailed evaluation has been completed into their behavioural changes through participation on the Green Gym.
There is growing interest in the mental health impact of violent conflicts and disasters. In societies characterised by military conflict of whatever scale, the sources of everyday stress and uncertainty are considerably magnified, for example, through unexpected disruptions of daily routine, forced displacement, loss of jobs and shocks of death and injury. Unemployment and poverty typically increase and fewer resources are devoted to health services, trends which sometimes continue long after the cessation of hostilities.
Poor mental health is costly for employers and state services, a personal hurt which impacts on immediate relationships and wider society. It also acts as a barrier to post-conflict reconstruction, especially when, as some argue, the whole society has been traumatised by violence. In this view the, ‘troubled mind’ of Northern Ireland is dominated by an emotional intensity that resonates from the interpersonal to the political (Kaper & Campbell 2004). Northern Irish society, so the argument runs, is pathological; it has become ‘dehumanised’ and ‘day-to-day societal relations are infected by destructive processes.’
Conservation Volunteers have extensive experience of involving communities who have suffered long-term deprivation in successful community led practical conservation projects. Following community development models the Green Gym is delivered in a non-threatening, non-competitive environment, where participants of all ages and backgrounds work towards a common goal. This is a slow process which takes many years of building trust to break down barriers to inclusion when the true success can be measured.
Extensive research has shown that physical activity can be an effective method of improving psychological well-being, reducing clinical depression, risk of depression, anxiety and stress, and improving aspects of mental functioning such as planning, short-term memory and decision making. It has also been mooted that people have a biologically-based attraction to nature (‘biophilia’) and that being in and connecting to nature can itself provide mental health benefits (Mental Health Foundation 2007).
Qualitative research also confirms the mental health benefits of involvement in the Green Gym. One participant on the Mater Green Gym diagnosed with a paranoid psychosis, was forced into early retirement due rapid deterioration of his mental ill health. ‘I was experiencing severe anxiety and not coping well in open spaces, since attending the Green Gym I have built confidence in a supported environment.’
The Green Gym is an interactive and inclusive project which has proven successful in refreshing community connections, raising local motivation in bringing people together to work towards a shared goal and help raise and tackles communal health and environmental issues, irrespective of age, background or ability of those directly involved.
Conservation Volunteers Green Gym, through six years of dedicated project development and delivery, are uniquely places to be a key community based player in designing and delivering the future strategies for health improvements for Northern Ireland, especially mental health and obesity. We have strong experience and an adaptable delivery style which can incorporate regional strategy aims and objectives into local preventative action. The Green Gym is a holistic approach to tackling health and community issues which we view should be embedded into the strategic thinking in the changing climate for Northern Ireland.
Dianne Keys
Health & Community Development Manager
January 2008
The Northern Ireland Association for Mental Health
The Northern Ireland Association for Mental Health (NIAMH) welcomes all Government Initiatives that attempt to deal with the endemic problem of suicide in our society. Bongar (1992)[1] expressed the view that the common consistency in suicide is with life long coping patterns. This has led a number of international Suicidologists to consider the question of teaching coping skills as a Primary Prevention Programme. A simple concept was formulated – by teaching young children how to cope with difficulties they should be able to handle problems and crises in adolescence and adult life. Thus, the Zippy’s Friends Project was set up in Canada, Denmark and Lithuania and is suitable for five, six and seven year old children of all abilities. Evaluation of pilot studies have shown excellent results and the programme is now being made available internationally in eleven countries with endorsement by the World health Organisation.[2]
Such an approach is essentially different to the pathogenic approach which seeks to identify children who have mental health problems or who are perceived as being especially vunerable. The pathogenic model is a necessary one. There is however the need to consider the ‘up stream’ approach and international experts are increasingly seeing the wisdom of mental health improvement and well-being in the early years. Prof Aaron Antonovsky, Author of the Salutogenic Model, referred to what he called ‘the bias of the down stream focus i.e. the devotion of the disease care system to saving swimmers drowning down stream by heroic measures, rather than asking who or what is pushing them into the river in the first place’.[3]
Helping young children developing positive coping strategies, as opposed to maladaptive ones, has a number of benefits. Investing in the early years yield not only better mental well-being in children and young people but also help prevent mental illness, as well as substantial economic benefits. Improved mental health and well-being is a worthwhile goal in itself and leads to better outcomes in physical health, educational performance, employability and productivity at work, crime reduction and pro-social behaviour. Positive mental health benefits physical health by improving protection from heart disease, stroke incidence and survival, harmful health behaviours (smoking, drinking, and drugs) and increasing overall lifetime mortality rates and life expectancy.[4]
A recent Public Health Draft Guidance Report by NICE on promoting the well-being of children in primary education recommends that Commissioners and providers of services to children in primary schools need to ensure that primary schools promote the emotional and social well-being of children. All primary schools should have a comprehensive programme that is based on a whole school approach. There needs to be a curriculum on emotional and social development, covering such development skills as problem solving, coping, conflict management and emotional literacy. The report emphasises the need for Teachers to be trained and for a cross-sectoral approach between Education and Child and Adolescent Mental Health Services.[5]
[1] Bongar, B. (1992) Suicide, Guidelines for assessment, Management and Treatment.
[2] Bale, C., Early start suicide prevention.
[3] Health Promotion Journal, 1996. Vol. 11 No 1. The Salutogenic Model as a theory to guide health promotion.
[4] Friedli and Parsonage. (2007) Mental Health Promotion: Building the Economic Case. NIAMH. Belfast
[5] National Institute for Clinical Excellence (March 2008). Public Health Draft Guide. Promoting the mental well-being of children in primary schools.
Northern Ireland Local Government Association Briefing Paper 3 April 2008
General Overview of Strategy.
“Protect Life’ sets out its aim as
To reduce the Northern Ireland suicide rate, particularly
among young people and those most at risk.”
and sets targets of reducing suicide overall rates by 10% in the first two years and a further 5% by 2011.
It takes a two pronged approach in that it seeks to look at the whole population and then to target specific groups of people who have been found to be most at risk.
In the whole population it will work with families, communities, Children and Young People, Health and Social Services, Workplaces, Police and Emergency Services, Churches and Religious Bodies, and the Media.
It will target people in at risk groups which are, people who self harm, people with a mental illness, people who misuse drugs and/or alcohol, young males, people who have been bereaved by suicide, victims of abuse, marginalised and disadvantaged groups, high risk occupational groups and prisoners.
It sets out a number of high level objectives, targets and timescales for all of these.
Analysis of Strategy
Generally the strategy is to be welcomed, especially in its emphasis on prevention and protection and the promotion of a more balanced well-being model rather than a purely medical one. However, there are a few issues that need to be better thought through before it is finalised. Notably in the areas of
- Evidence Based Practice
- Analysis Of Existing Provision
- Review Effect of Previous Strategy
- Local Planning and Accountability
- Prioritisation
- Resource Issues
- Targets and Timescales
- Communication Techniques
- Use of Language
- Training Issues
This document will go on to outline the various issues that are raised in these areas.
Evidence Based Practice
As a strategy it sets out one of its principles as using an ethos of evidence based practice. Yet the only use of monitoring and targets recommended is for the voluntary sector. In section 3.14 it sets up a self imposed test of ‘Action, Implementation and Review’. Review is dealt with in one paragraph and is not among individual actions for each of the themes. Good practice dictates evaluation techniques should be planned as part of the strategy and reviews made an explicit part of the action planning process. As it is presently written they are either non-existent or at best implicit. Neither of which is good enough.
Analysis Of Existing Provision.
It provides good quality information on the extent of suicide in Northern Ireland and the different factors that increase the risk of someone taking their own life or self harming. It does not set out what organisations, networks and services are currently working to prevent, or help to prevent, suicide, nor does it analyse their effectiveness, efficiency or economy.
Review Effect of Previous Strategy
In 2003 the government published a strategy on mental health and included in it were 10 recommendations regarding suicide.
Three of the ten action points have been achieved in full (two of these were the sole responsibility of the Northern Ireland Prison Service), six have been partially achieved, and no action has as yet been taken on the remaining point. There was no analysis of what partially achieved means – i.e. was it 10% or 90% achieved. The main barriers cited as preventing full achievement of the action points included lack of recurrent funding and dedicated resources; lack of co- ordination; the need to address competing health service priorities; and insufficient engagement of GPs and other health professionals on the issue of suicide and self harm..
The strategy is very strong on better co-ordination but it does not specifically address any of the other reasons for non performance, specifically, dedicated recurring resources and professional engagement. Therefore it is at risk of making the same mistakes again. Also in seeking to co-ordinate local and regional actions it does not seek to integrate with other strategies such as community plans or the community planning process.
Local Planning and Accountability
The strategy suggests the use of Investing for Health Partnerships as a means of better local planning. It should also be thinking of post RPA community plans and more fundamentally not only using local bodies for planning but also for better accountability.
There should be a specific section on local accountability mechanisms.
The potential for North/South and East/West co-operation can bring benefits but there are also potential pitfalls of unnecessary complexity and bureaucracy that will take away from the delivery of services that meet the needs of patients, families and communities that are affected by suicide and self-harm.
Prioritisation
The strategy divides its work between looking at the population as a whole and at targeting specific groups within it. However, it does not say how these interrelate or which has priority. A strategy should allow for positive and negative contingencies otherwise it is merely a plan or a wish-list.
The strategy sets out a framework in Annexe 5 for the necessary components in a suicide prevention strategy yet in section 4.6 it sets out largely the same actions in different areas with differing priorities without explaining why they have decided to change it.
More importantly the best practice model (in Annexe 4) commends the promotion of protective factors that does not seem to be adequately mirrored in the strategy as a whole and specifically in the Over-Arching Objective for the Targeted Approach. Should it not be to reduce risk and promote protective factors?
Resource Issues
It has little reference to resources or the implications of implementation on the organisations that will deliver the strategy. It does not state whether it expects the resources to come from existing budgets or from a new bid to DHSSPS/DFP. It does not say how they will be allocated between boards, trusts or other providers such as the community and voluntary sector. Nor is there even a statement of principles that the funders can be expected to follow. We welcome the use of the Investing for Health Partnerships as a mechanism for local action planning. There is no analysis of the likely cost of implementation or what will have to change or stop in current delivery mechanisms.
In not specifying what is a priority it is making nothing a priority. In not helping managers and workers to agree on priorities it has the potential of sacrificing its long-term effectiveness to short-term political, financial or organisational expediency.
Only in the section on mental illness is there an explicit request for regular and on-going support.
Targets and Timescales
The setting out of targets and timescales is to be welcomed. However, they are often couched in terms so vague that it is possible to comply with them yet make no discernable difference in preventing suicide. This places the emphasis on what the strategy does (inputs and processes) rather than what it achieves (outputs and outcomes) and again takes away from the centrality of effectiveness, review evaluation and evidence based medicine as stated in the principles commitment to best practice. For instance Action E in the section on health and social services (p45) commits them to “assess with a view to implementing best practice’ rather than assess and implement or even better just implementing it.
Notable exceptions are is the sections that are not under DHSSPS control viz. the media, the emergency services and prisons where the targets and actions are well formed, clear, focussed and accountable.[1]
Evidence based evaluation should be put at the centre of every piece of work commissioned under this strategy.
In Section 2.4 it notes that changes in the way that suicides are recorded by the Coroner’s office may increase the number of suicides recorded and so undermine the perceived effectiveness of the strategy. This has the potential to undermine any attempts at evidence based medicine or action and so this potential should be allowed for and planned around.
Why is the strategy targeting young males when according to the data in the strategy over 50% of male suicides are aged 35 years or more?
Why is the strategy concentrating on the rural community when this is not supported by the evidence set out in chapter 2? If there are rural hot-spots then let that be said.
Communication Techniques
The strategy in various sections refers to ‘information’ campaigns, this is an interesting use of language that blurs the distinction between information and understanding and again goes to the heart of the strategy’s unwillingness to be measured in terms of clear evidence of success. If an organisation puts out information that is not widely understood or does not achieve its aims it will have succeeded in terms of the target but failed in terms of the strategy. The targets and the strategy should be aligned. Information alone is not usually enough to engage the emotions and to achieve changes in perception, attitude and behaviour. A concerted campaign that involves the emotions and the intellect, that challenges assumptions and deals with negative stereotyping is needed. There must be elements of two way information exchange and sharing and challenging of views for it to be effective.
Use of Language
The strategy uses much language that is vague, jargonistic and unmeasurable, for example non p39 it states it will
‘provide families with the opportunity to avail of practical intervention skills’
Do you know many families that would know what that means never mind how it helps them to prevent a suicide? Similarly in setting targets for workplaces (p46) it stipulates that positive mental health training courses are ‘made available’ to employers. While it is only common sense to accept that you cannot force individual families or employers to take part, you can set global targets for their participation. This is similar to the way that you cannot force any individual to buy a Mars Bar but you can set a target for the Mars sales force.
The strategy regularly uses ‘enhance’ instead of ‘improve’. It is a subtle distinction but one that emphasises actions over results again. One can enhance a service by making changes that make no measurable improvement in achieving target numbers.
In all but the section on vulnerable groups it uses accessibility and availability interchangeably when they are in fact two different things. For instance a counselling service might be available to young people but if there is a two-year waiting list, it is not accessible.
Training Issues
The strategy has set down training priorities that do not take account of organisations’ other training needs, priorities or likely resources. It uses significantly different language when setting out training requirements for non HSSPS bodies (the training is mandatory) than for primary care staff (it is a priority). Yet again this shows the lack of proper consultation and third party engagement in the development of the strategy.
[1] Note there were no journalists or police officers on the steering committee
Appendix 4
Other Evidence Considered by the Committee
Research Paper
Protect Life – A Shared Vision
Northern Ireland’s Suicide Prevention Strategy and Action Plan 2006-2011
Aim of the paper
This briefing paper seeks to provide information to support consideration of Protect Life – A Shared Vision (The Northern Ireland Suicide Prevention Strategy and Action Plan 2006-2011). In doing so the paper will provide a brief overview of the key components which form the basis of other suicide and self-harm prevention strategies as well as an examination of the key structures and action plan underpinning the Protect Life strategy.
Introduction
Over recent decades, suicide has become a major cause of death affecting every region around the world. The scale and pervasiveness of the problem is reflected in the fact that for some time suicide has been the third biggest cause of “years of lives lost” after cardiovascular disease and cancer. An estimated 877,000 lives were lost prematurely worldwide due to suicide in 2002.[1] Suicidal behaviour continues to represent a significant global public health problem and the development of prevention and postvention strategies provide an on-going major challenge to health and social services at every level. Figure 1 illustrates the scale of the problem of suicide internationally with comparable suicide rates from a selection of European states. It highlights the fact that, in the period 1999-2003, Northern Ireland had more suicides per 100,000 persons than England or Wales, though less than Scotland or the Republic of Ireland.[2]
Figure 1: Suicide rate per 100,000 persons (1999-2003)
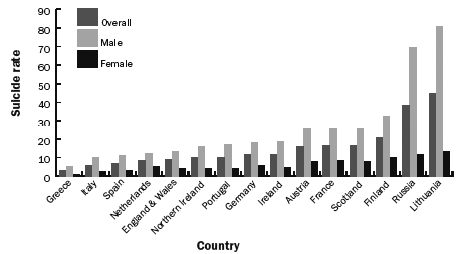
The causes of suicide are complex and are likely to involve an inter-play of psychological, biological, social and environmental factors in the context of a person’s negative experiences over a lifetime, sometimes aggravated by a recent personal difficulty. Premature death from suicide has many adverse consequences, not only for the family and friends of those who die but for all of those in the wider community who have to cope with the impact of the tragedy.[3]
An editorial published in a leading academic mental health journal noted that in response to the significant rise in rates of suicide and self-harm in many Western countries (from the mid-1980s onwards), particularly among young males between fifteen and twenty-four years of age, a number of national suicide prevention strategies were developed. Finland, Norway and Sri Lanka were among the first countries to develop national suicide prevention plans in the 1990s. In terms of evidence of what makes an effective strategy, the editorial states that:
While there is comparatively little evidence-based information at either a program or intervention level, or at a national strategy level, about programs that are successful in reducing or preventing suicidal behaviour, there is now a large volume of information from mental health epidemiological, genetic, biological and psychosocial research which gives a generally coherent and consistent picture about the risk factors for suicidal behaviour. This body of evidence provides a framework within which we can identify likely points for preventative interventions from knowledge about risk and protective factors for suicidal behaviour. In addition, we can review current knowledge about suicide prevention plans at national, local and community levels. It should be noted however, that despite our vastly increased knowledge about the causes of suicidal behaviour we know relatively little about what is the most effective in preventing suicide.[4]
Evidence about the risk and protective factors associated with suicidal behaviour and the casual pathways that lead to this behaviour may be summarised and synthesised as follows:
The background causes of suicide span a number of domains of variables which range from individual level factors (e.g. genes, personality, sexual orientation) to macrosocial factors (e.g. unemployment rates), and which include exposure to trauma, family factors, life stresses, social supports, socio-economic factors, cultural factors and macrosocial factors. A major route by which these background factors contribute to suicidal behaviours is by influencing individual susceptibility to mental health problems and, notably, such conditions as mood disorders, substance abuse, anxiety disorders and antisocial and offending behaviours.[5]
Figure 2 provides an illustration of the interplay between the various factors involved in suicidal behaviour and strategic engagement of prevention interventions that can be employed to reduce rates of suicide and self-harm.
Figure 2: Targets of Suicide Prevention Interventions[6]
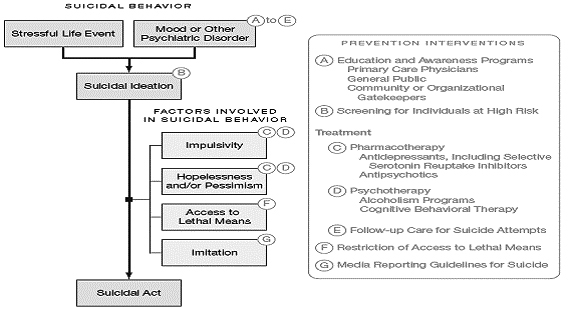
A brief outline, supported with examples, of these seven key interventions is provided below.[7]
(a) Informational and education programs for professional groups - A series of educational, collaborative care, and nurse case management programs which focus on enhancing the ability of primary care groups to better identify, treat and manage depressions and suicidal behaviour have been shown to reduce suicide rates.
(b) Screening programs - Programs which either screen directly for suicide risk, or for depression or substance abuse with which suicidal behaviour is associated, have been developed and applied in a range of institutional settings including schools, prisons and juvenile detention centres and have been applied both to youth in general, and to at-risk youth such as those who receive child welfare services. These programs have been shown to be reliable and valid in identifying at-risk individuals, and some programs have doubled the number of identified at-risk individuals. There is no evidence that screening for suicide risks increases the risk of suicidal thinking or behaviour. Screening. However, it has been suggested that, amongst other things, further consideration needs to be given to determining the costeffectiveness of screening general populations vs identified at-risk populations for reducing suicide rates
(c) Treatment and support for mental illness and suicide - The majority of those who die by suicide in Australia and New Zealand, as in most Western countries, have at least one mental disorder when they die, and most of these disorders are untreated. In particular, most depression is untreated or under-treated, even after suicide attempts. The presence of a mental disorder increases the risk of suicide ten-fold. There is also a great deal of evidence that suggests that having made a suicide attempt increases the risk for further suicidal behaviour, and for suicide. For these reasons, treating mental illness and providing long-term management and support for those who have made suicide attempts, are important approaches to suicide prevention.
(d) Restricting access to alcohol – National Strategies which seek to improve control of alcohol may have the added benefit of reducing suicidal behaviour by decreasing the risk of acute alcohol intoxication (which is associated with impulsive suicide attempts), and by reducing the fraction of the population with alcohol use disorders, which are precursors of suicide attempts. In both Iceland and the former USSR, suicide rates decreased following the introduction of strong national anti-alcohol policies.
(e) Follow up care after suicide attempts - A history of suicide is a strong risk factor for further suicidal behaviour including suicide. Further, there is increasing evidence that many mental illnesses, including depression, as well as suicidal behaviour, may be recurrent and chronic. Compliance with medication and treatment regimes for chronic conditions is often poor. For these reasons, strategies which try to improve acute and long-term for people who make suicide attempts have the potential to decrease rates of suicidal behaviour. A Norwegian program which focuses on integrating support and care to individuals after discharge following a suicide attempt also found decreased rates of further suicide attempts.
(f) Restricting access to lethal methods of suicide - Restricting access to lethal methods of suicide is an often under-valued approach to suicide prevention. However, research from a number of countries suggests that reducing access to particular means of suicide reduces suicide by that method, and sometimes, decreases total suicide rates. These findings span a range of means including: the detoxification of domestic gas and of carbon monoxide emissions from vehicle exhausts; various levels of legislative restriction on ownership of, and access to, firearms; restrictions on the pack size of analgesics; installation of barriers at sites of jumping and at subways to prevent people leaping in front of trains; the use of clinically safer drugs and restriction of access to highly toxic drugs and pesticides which are lethal in overdose.
(g) Media coverage of suicide – A substantial body of evidence suggests that certain ways of presenting and portraying suicide in the media appear to precipitate suicidal behaviour in vulnerable individuals, particularly if the media coverage is repetitive, details methods or highlights the suicide death of a celebrity or well known person. This evidence has led to most national suicide prevention plans developing media guidelines, which advocate that suicide be reported in a muted and cautious manner.
Development of strategic response to suicide prevention in Northern Ireland
As highlighted in an earlier research paper, in recent years, Northern Ireland, like other jurisdictions has witnessed an increase in the number of suicide deaths and acts of self-harm. As illustrated in Table 1, the average number of suicides per annum between 1999 and 2004 has been 150. However, the 2005 figure registered a 46 per cent increase amounting to 213[8] deaths while there were 291 suicides recorded in 2006[9].
Table 1: Suicide Figures for Northern Ireland 2000-2006[10]
2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
185 |
158 |
183 |
144 |
146 |
213 |
291 |
Following the examples of other jurisdictions, a number of government departments in Northern Ireland, coordinated through the DHSSPS, have responded to the increasing public health concern around suicide and self-harm by developing a suicide prevention strategy. Within Northern Ireland, a key step in this process was publication by the DHSSPS in January 2003 of the Promoting Mental Health Strategy and Action Plan 2003-2008, as part of the wider Investing for Health Strategy. A central aim was to ‘prevent, or reduce the incidence and impact of, mental and emotional distress, anxiety, mental illness and suicide’. The overarching target set within the Promoting Mental Health Strategy was to:
reduce the proportion of people with potential psychiatric disorder (as measured by the GHQ 12 score[11]) to 19.5% by 2008 against a baseline of 21% in 2001.[12]
Protect Life: A Shared Vision
Central Targets and Funding
The overall aim of the strategy is “to reduce the suicide rate in Northern Ireland” and specifically to:
I. Obtain a 10 per cent reduction in the overall suicide rate by 2008; and
II. Reduce the overall suicide rate by a further 5 per cent by 2011[13]
In terms of central targets it is worth noting that in:
England – the National Suicide Prevention Strategy for England[14] launched in September 2002 aims to achieve the central target of a reduction in the death rate from suicide and undetermined injury by at least 20 per cent by the year 2010.
Scotland – the Choose Life strategy launched in December 2002 which like other strategies has a number of short, medium and long-term targets is seeking to achieve the key strategic target of a 20 per cent reduction in suicides in Scotland by 2013.[15]
Wales - Currently, the Welsh National Assembly has not devised or implemented a National Suicide Prevention Strategy for Wales, however suicide prevention is a priority for services in Wales.[16]
Republic of Ireland – the Reach Out strategy launched in 2006, while not identifying a specific figure for reducing the suicide rate does nevertheless explicitly commit itself to the ‘fundamental aim of preventing suicide and deliberate self-harm, and reducing levels of suicidal ideation in the general population by tackling contributing factors.’[17]
Implementation
At the strategic level, there are 3 key elements to implementation of the Protect Life strategy:
Suicide Strategy Implementation Body (SSIB)
The Suicide Strategy Implementation Body (SSIB) was established by the DHSSPS as a cross-sectoral delivery vehicle charged with the responsibility of overseeing and driving forward the implementation of the Protect Life strategy which in turn will report annually to the Ministerial Group on Public Health (itself a cross-departmental body responsible for driving forward the Investing for Health strategy). The SSIB will continue to review the overall implementation of Protect Life including the central targets outlined above.
Ministerial Co-ordination on Suicide
The Minister for Health, Social Services and Public Safety made reference to the Ministerial Co-ordination Group during and Assembly debate on Suicide on the 17th September 2007. This Ministerial Group has been established by the Executive to ensure co-ordination across relevant departments and to continue to prioritise the issue.
Alongside the Minister for HSSPS, the Group also includes the Minister of Education, Caitríona Ruane, and the two junior Ministers, Gerry Kelly and Ian Paisley Jnr. According to the Minister for HSSP, ‘The co-ordination group has the potential to provide Ministers with the wider context and support that will allow us to work in an integrated and joined-up manner in order to deal with the devastating effect that suicide and self-harm has on all our communities.’[18] The Group is due to meet again in October 2007.
Families Forum
Working in conjunction with the SSIB, the Families Forum was established by former Health Minister, Paul Goggins in July 2006 to provide a voice to families bereaved by suicide. According to Goggins, ‘The Families Forum will be able to nominate representatives to sit on the Suicide Strategy Implementation Body. Bereaved families will have a major say in the way the Strategy is introduced. I look forward to working with them and share their commitment to reduce suicide and self harm in Northern Ireland’.[19] Similar sentiments were voiced recently by Health Minister Michael McGimpsey who maintained that ‘families must continue to have a strong voice in suicide prevention’.[20]
Members may wish to consider the potential effectiveness of the overarching arrangements to ensure implementation of the strategy. In particular Members may wish to consider the extent and nature of the involvement of the Families Forum as part of these arrangements.
In terms of implementation, the strategy highlights the potential for North/South Co-Operation stating that:
The parallel implementation of the Republic of Ireland Suicide Prevention Strategy, “Reach Out”, is of particular relevance, given the potential for mutually beneficial North/South working. Obvious examples of this potential include liaison on the development of future public information campaigns and closer alignment of suicide and self-harm recording in Northern Ireland and Republic of Ireland.[21]
As highlighted in the guiding principles of Protect Life, the development of strong links with other relevant strategies is an important prerequisite to ensure successful implementation and positive outcomes from the suicide strategy. The Protect Life strategy itself states that:
The successful implementation of the Strategy, and the achievement of its aim, will be influenced by two other factors. Firstly, the recognition of suicide prevention as a priority by all relevant Government Departments. Secondly, implementation of the Suicide Prevention Strategy in parallel with progress being made on the delivery of the Promoting Mental Health Strategy and the Bamford Review of Mental Health and Learning Disability.[22]
This is particularly pertinent in relation to developing synergy between Protect Life and the key recommendations of the Bamford Review of Mental Health and Learning Disability (NI).
Central to the implementation of Protect Life is the employment of a complementary dual strategy which combines a focus on dual population and a targeted approach in which ‘Actions Plans’ target the general population and those individuals and communities most at risk from suicide and self-harm. Consequently, these Action Plans contain short (up to one year), medium (one to three years) and long-term (up to five years) targets with a focus on specific issues, groups, areas and agencies within Northern Ireland aimed at both protecting the wider population and those individuals and families directly affected by suicide and self-harm.[23] The Protect Life Action Plan is included as an Appendix 1 to this research paper.
In terms of specific actions, a systematic review of suicide prevention strategies concluded that, whilst other interventions needed more evidence of efficacy, ‘physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates’.[24]
Research carried out in New Zealand,[25] where male youth suicide rates had doubled over two decades, concluded that the increase was accounted for, almost entirely, by increased use of hanging (71% of total increase) and vehicle exhaust gas (26% of total increase). The research concluded, therefore, that limiting access to means of suicide is a strategy which is unlikely to play a major role in reducing suicidal behaviour among young people in New Zealand. The same may be true of limiting access to means of suicide in Northern Ireland. GP training, however, has the potential to impact positively to reduce the number of suicide deaths in Northern Ireland. The Promoting Mental Health Strategy contained a target[26] relating to GP training, as does the Protect Life Strategy.
Appendix 1
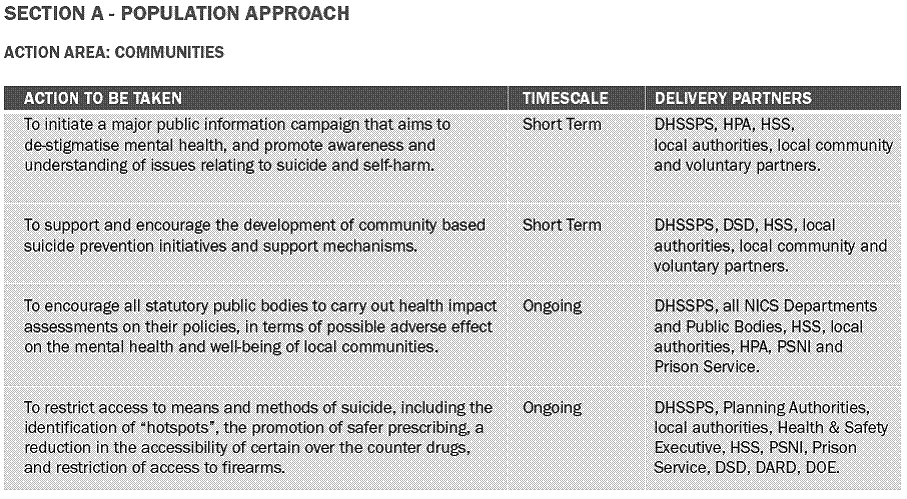
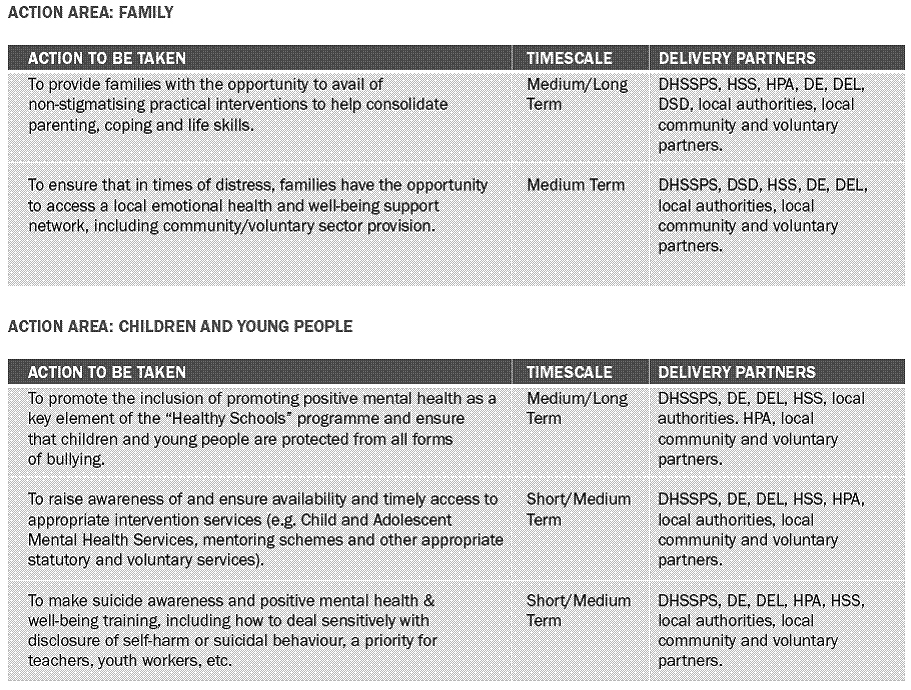
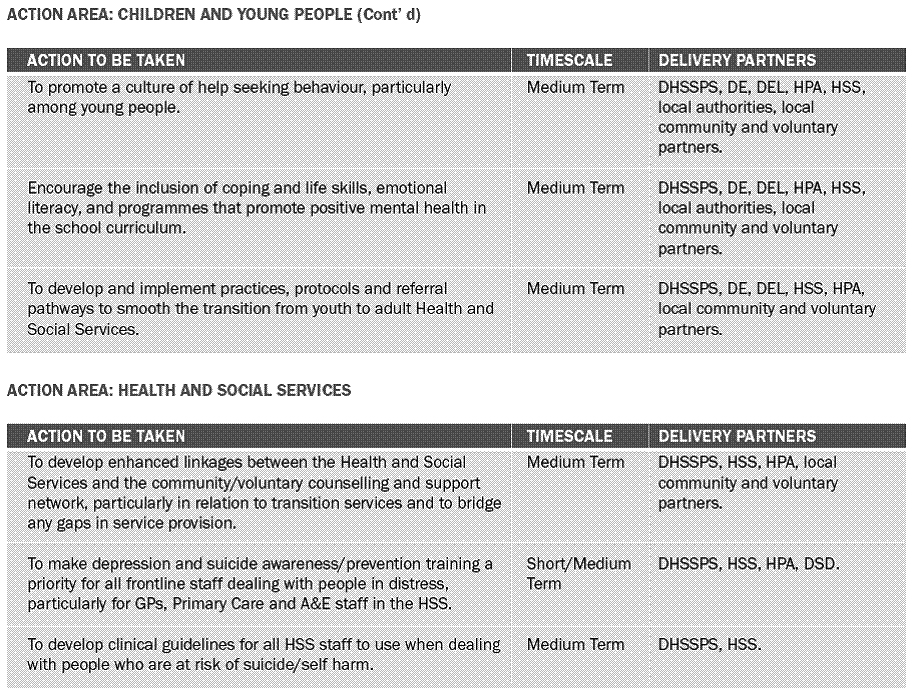
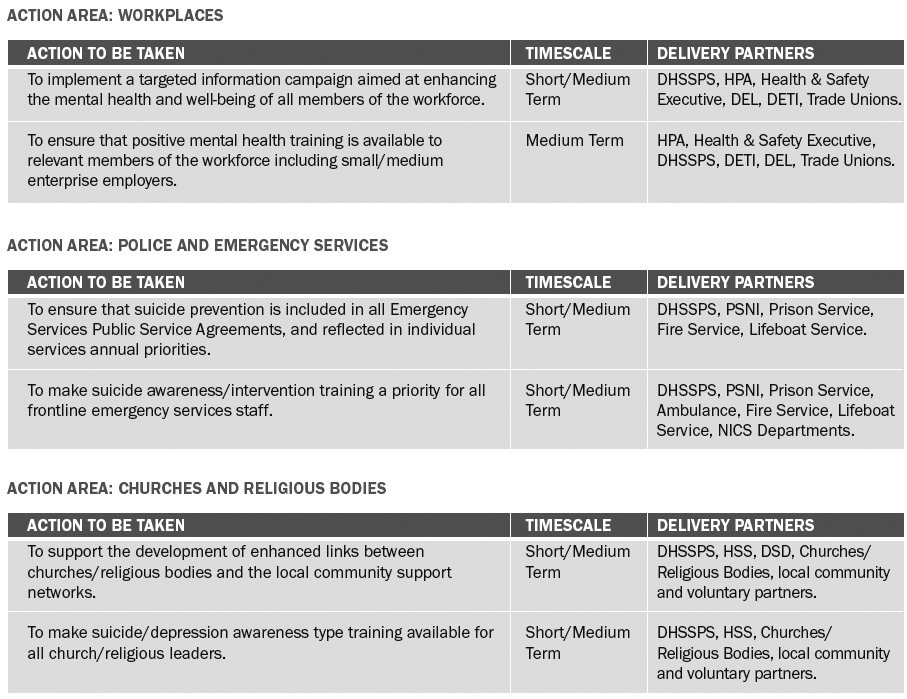
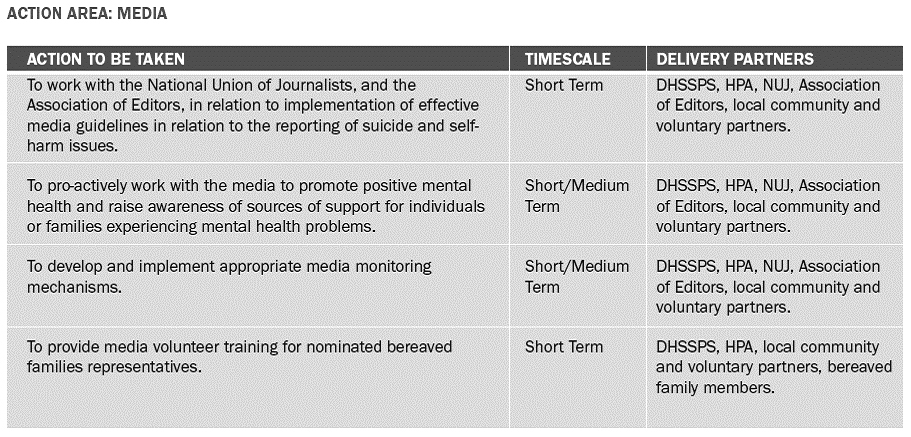
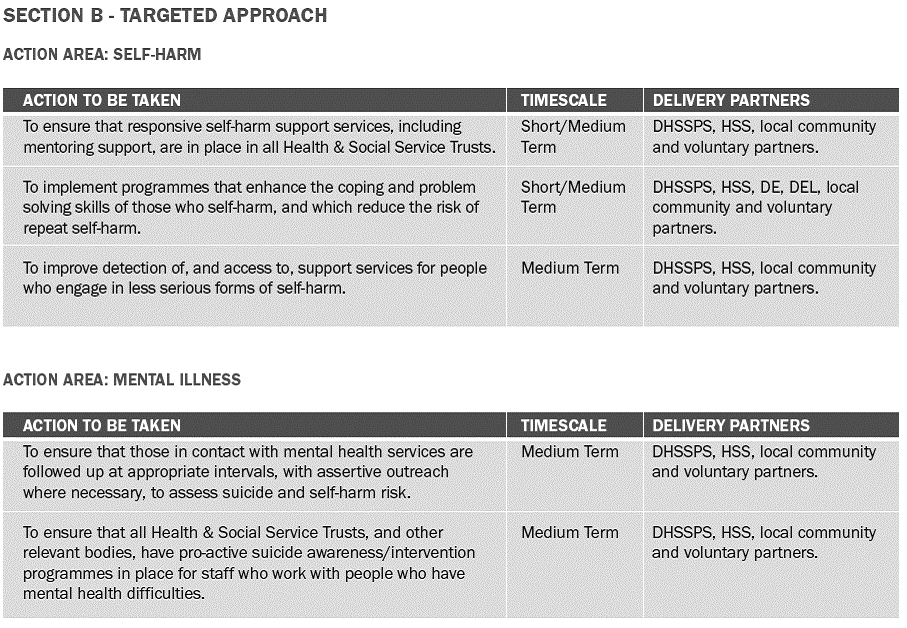
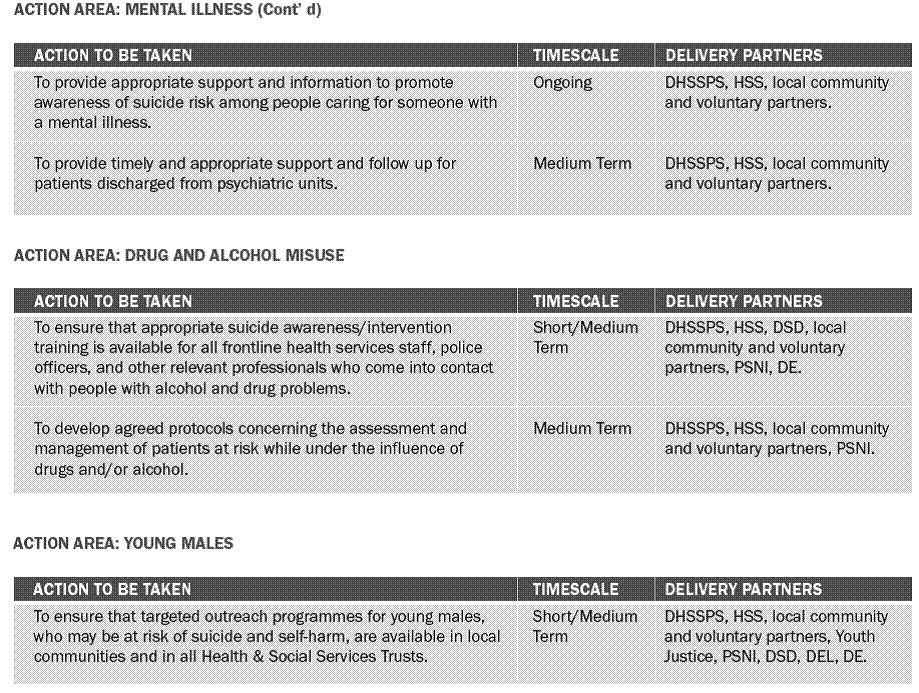
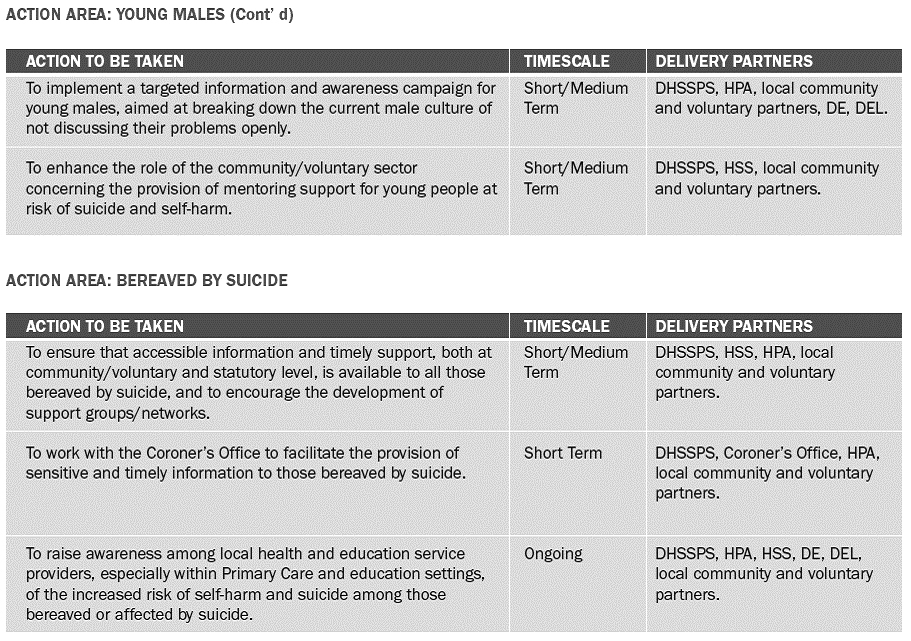
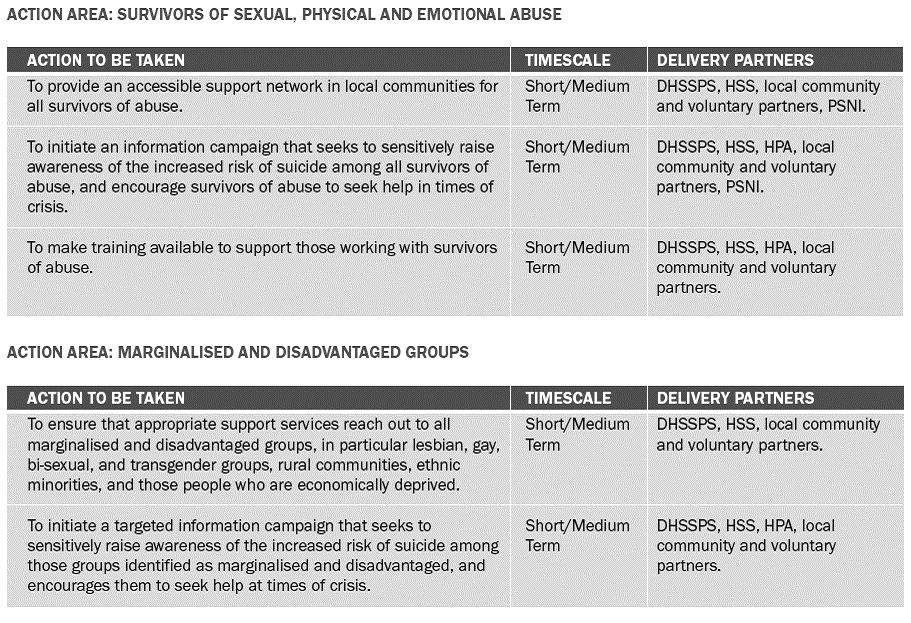
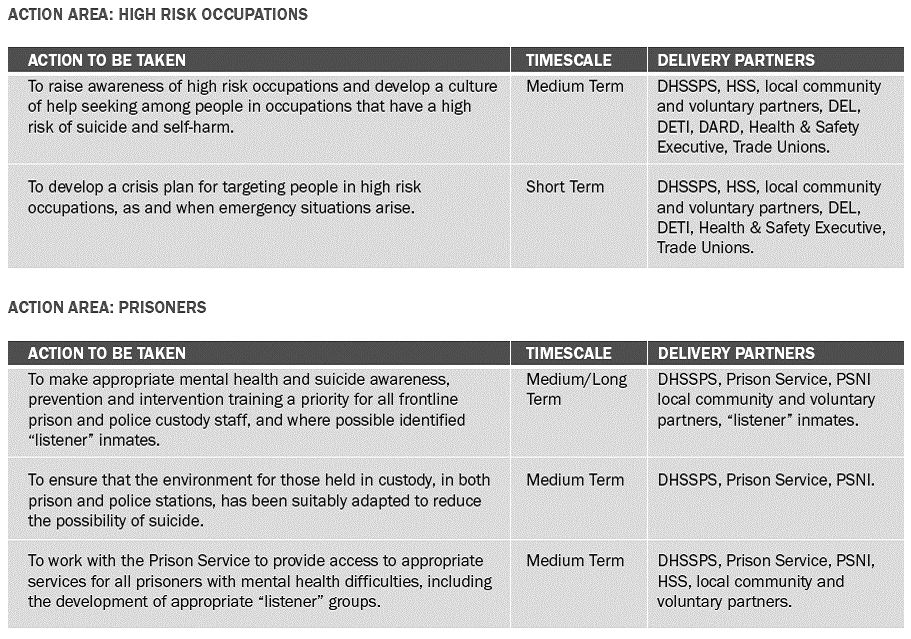
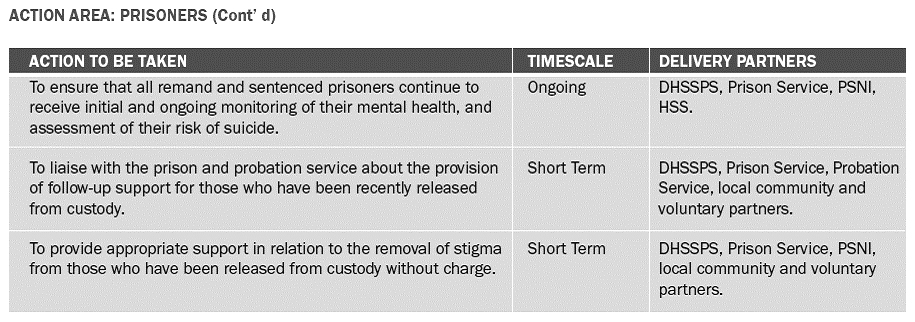
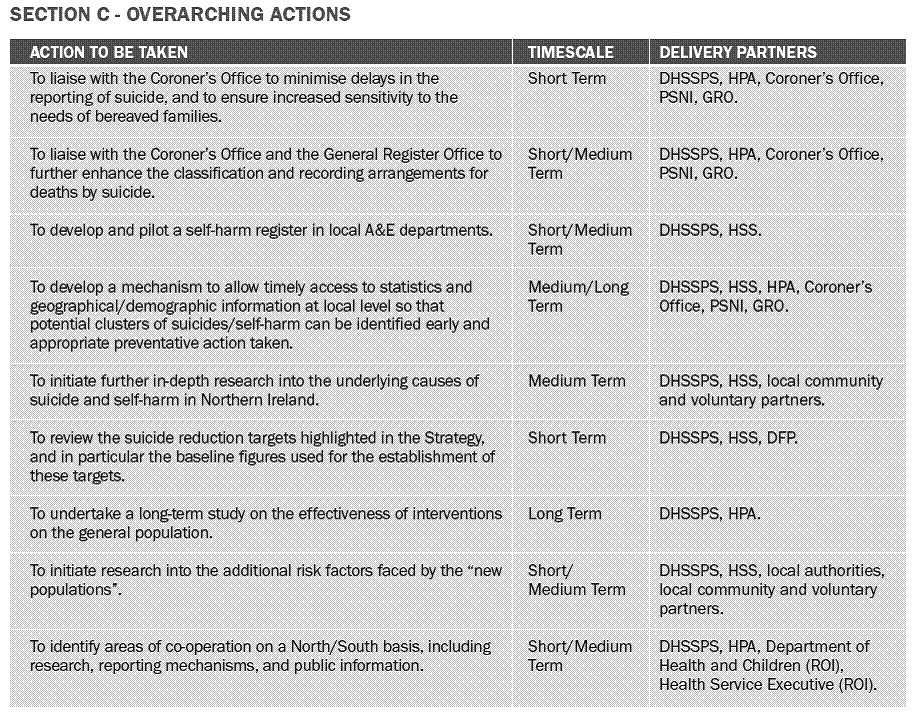
[1] DHSSPS (2006) Protect life: a shared vision - Northern Ireland suicide prevention strategy and action plan 2006–2011, DHSSPS: 7 – document accessed online at: www.dhsspsni.gov.uk/phnisuicidepreventionstrategy_action_plan-3.pdf
[2] DHSSPS (2006) Protect life: a shared vision – Northern Ireland suicide prevention strategy and action plan 2006-2011, DHSSPS: 7.
[3] Department of Health and Children (2006) Reach Out: Irish National Strategy for Action on Suicide Prevention 2005-2014, Department of Health and Children: 4.
[4] Beautrais, A. (2006) ‘Suicide Prevention Strategies 2006’, Australian e-Journal for the Advancement of Mental Health (AeJAMH), Volume 5, Issue 1: 2.
[5] Beautrais, A. (2006) ‘Suicide Prevention Strategies 2006’, Australian e-Journal for the Advancement of Mental Health (AeJAMH), Volume 5, Issue 1: 2.
[6] Mann et al (2005) ‘Suicide Prevention Strategies – A Systematic Review’, Journal American Medical Association (JAMA), Vol. 294, No.16
[7] Information in (a) to (g) below taken from Beautrais, A. (2006) ‘Suicide Prevention Strategies 2006’, Australian e-Journal for the Advancement of Mental Health (Ae JAMH), Volume 5, Issue 1: 3-6.
[8] DHSSPS (2006) Investing for Health – Update 2006: 33
[9] DHSSPS (2007) Press Release, 4th June.
[10] Figures obtained from the DHSSPS.
[11] This is a set of twelve questions form the General Health Questionnaire which indicates the possible presence of psychiatric disorder.
[12] Health and Wellbeing Survey
[13] DHSSPS (2006) Protect life: a shared vision. Northern Ireland suicide prevention strategy and action plan 2006–2011, DHSSPS: 21.
[14] Department of Health (2002) National Suicide Prevention Strategy for England http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009474 (June 2007)
[15] Scottish Executive (2006) Evaluation of the First Phase of Choose Life: the national strategy and action plan to prevent suicide in Scotland, Scottish Executive: 27.
[16] Information obtained from the MIND website at: http://www.mind.org.uk/Information/Factsheets/Suicide/
[17] Department of Health and Children (2006) Reach Out: Irish National Strategy for Action on Suicide Prevention 2005-2014, Department of Health and Children: 8.
[18] Abstract from an Assembly Debate on ‘Ad Hoc Committee on Suicide’, 17th September 2007.
[19] DHSSPS (2006) Press Release, 10 July.
[20] DHSSPS (2007) Press Release, 4th June.
[21] Protect Life: A Shared Vision paragraph 22
[22] See DHSSPS (2006) Protect life: a shared vision. Northern Ireland suicide prevention strategy and action plan 2006–2011, DHSSPS: 39.
[23] See DHSSPS (2006) Protect life: a shared vision. Northern Ireland suicide prevention strategy and action plan 2006–2011, DHSSPS: 23-37.
[24] Beautrais, A. (2006) ‘Suicide Prevention Strategies 2006’, Australian e-Journal for the Advancement of Mental Health (AeJAMH), Volume 5, Issue 1: 2.
[25] Beautrais, Annette L. ‘Methods of youth suicide in New Zealand: trends and implications for prevention Australian and New Zealand’ Journal of Psychiatry, Volume 34, Number 3, JUNE 2000 , pp. 413-419(7)
[26] Action 26: HSS Boards and HSS Trusts in co-operation with Primary Care will develop and deliver a Depression Awareness Training Programme for GPs.
Families Bereaved by Suicide
5 July 2007
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Rev Dr Robert Coulter
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Mrs Jean Carson
Ms Mary Creaney
Ms Rhonda Hill
Mr Séamus McCabe
Mr Gerard McCartan
Ms Ann McGarrigle
Ms Maureen Young
1. The Chairperson of the Committee for Health, Social Services and Public Safety (Mrs I Robinson): I welcome representatives from families bereaved by suicide to the Assembly. This is a difficult subject with which to deal, and I can appreciate how much it has cost you all to come here and open up on the delicate and sensitive matter of bereavement.
2. I welcome Mary Creaney from north-west Belfast; Maureen Young from mid-Ulster, Séamus McCabe from Newry; Rhonda Hill from south Belfast; Gerard McCartan from north Belfast; Ann McGarrigle from the north-west; and Jean Carson from west Belfast. You are all very welcome. You will have 10 minutes to make a presentation, although I am sure that that could be extended a little due to the number of witnesses. Members of the Committee will then ask questions. Who will start?
3. Ms Mary Creaney: We are a group of parents and families who have been bereaved through the tragedy of suicide, and I have been nominated as spokesperson for today’s session. I welcome the opportunity to speak to the Committee for Health, Social Services and Public Safety.
4. Our group’s first concern relates to depression-awareness training for general practitioners (GPs). The GP is likely to be the first person in the primary care setting to whom individuals go to report depressive symptoms. That first contact can be particularly difficult for the individual who presents with depression, and the initial support and treatment from the GP are critical for the person involved. As families, we continually hear horror stories about how families are treated with condescension or perhaps even ignorance by some GPs. Some GPs treat individuals with the greatest respect and provide adequate care, but there are those who do not.
5. One action point from the Northern Ireland suicide prevention strategy ‘Protect Life — A Shared Vision’ was the development and delivery of a depression-awareness training programme for GPs. To date, 161 GPs from the four health board areas have attended a total of 10 courses. There is obviously an inability to engage successfully with GPs to avail of training. GPs were offered locum support for their surgeries while they undertook the training, which is delivered in a three-hour period. Plans are being developed for the second phase of training for GPs, but that is questionable, given the Health Promotion Agency’s inability to attract more GPs and surgeries to undertake such vital training for depression awareness.
6. We believe that the depression-awareness training programme should be made compulsory for all GPs, particularly at the contract stage between them and the Department of Health, Social Services and Public safety. The Committee should investigate the nature of GP training in the South of Ireland — where depression-awareness training is compulsory — and examine policies there in the hope of adopting best practice and bringing it to the North of Ireland.
7. The Belfast Health and Social Care Trust is commissioned by the four health boards to provide adolescent psychiatric inpatient services at a regional inpatient unit. At present, sadly, there are five adolescent beds to cover four health board areas, with a pending increase to eight beds by the end of July and a purpose-built bed unit by 2009. Meanwhile, adolescent and young people are exported to various parts of England to receive the treatment that they require.
8. The Bamford Review of Mental Health and Learning Disability (Northern Ireland) ‘A Vision of a Comprehensive Child and Adolescent Mental Health Service’ states in its introduction:
“At present the workforce profile of Child and Adolescent Mental Health services clearly shows them to be wholly inadequate. Despite many examples of good practice the overall quality, consistency and accessibility of services is so inadequate that urgent strategic action is needed to tackle these shortages.”
9. One year into the implementation of the Protect Life strategy, the dearth of adequate services for children and adolescents still prevails. This week, the office of the Northern Ireland Commissioner for Children and Young People published a report that stated that Northern Ireland’s Department of Health, Social Services and Public Safety’s spending on healthcare provision for children and adolescents is half that of Scotland and one third of the spending budget for such services in England.
10. The fact that resources are inadequate and that services are underfunded was reinforced by the Bamford Review of Mental Health and Learning Disability (Northern Ireland), which, in 2005, put in place a strategic framework for mental health services. Families are concerned and need more information on the 24/7 regional response teams, as well as information relating to child and adolescent mental-health services (CAMHS), particularly when working with those in crisis. Families need access to pathways to those services; information is often fragmented and referral pathways to services are sometimes confusing. Clarity is, therefore, required, and we would like the Committee for Health, Social Services and Public Safety to help us to obtain it.
11. Individuals present themselves at accident and emergency departments because of self-harm or following a suicide attempt. If individuals present having consumed drugs or alcohol, they will not receive any kind of psychiatric assessment and could be sent home to injure themselves further or to attempt suicide.
12. Lost opportunities at accident and emergency departments can be fatal, especially for those with alcohol or drug problems, as they are six times more likely to die as a result of suicide. Lost opportunities cost lives, and accident and emergency service provision at primary care level needs policy development and delivery of adequate services in order to provide a place of safety until a proper assessment can be conducted on those who present themselves because of self-harm or suicidal tendencies. There are best practice models in parts of England, Scotland and Wales.
13. One concern raised by families is unique to Northern Ireland: in the past, families have highlighted the problem of bullying by paramilitaries in loyalist communities. Such bullying has a detrimental impact, particularly on young men, who may go on to self-harm or to develop suicidal tendencies. Families feel that that issue needs to be raised because it is detrimental to the well-being of those young people.
14. The urban/rural divide is represented today, and that brings a particular set of problems.
15. We ask the Committee for a follow-up meeting to discuss our concerns in more detail and to form a working relationship with Committee members. The overarching aim of the suicide strategy is to reduce the suicide rate in Northern Ireland, and we hope that the members of the Committee for Health, Social Services and Public Safety will feel that they have a vested interest in that.
16. Each of today’s witnesses has the same aims, which we hope Committee members share. Our aims are not only, eventually, to save lives, but to help bereaved families. Until recently, there was no service provision for those who had been bereaved, and there were gaps and deficiencies in the services. Often, people do not realise that when a loved one dies due to suicide, close relatives automatically go into a high-risk suicide category. It is, therefore, imperative that adequate services be put in place for bereaved families.
17. I thank the Committee for listening to us today. We have a host of other concerns, such as education, training, and interdepartmental relationships. However, we have brought to the table the concerns that we felt needed to be highlighted today.
18. The Chairperson: Does anyone want to comment before the discussion is opened up?
19. Ms Rhonda Hill: Mary made the point that we represent the rural/urban divide, which is important. I come from mid-Ulster, and the needs of the people in the Sperrins and the outlying farming communities are different from those of people in intercity areas.
20. The Chairperson: That brings us to a new area, which includes the suicides following the BSE outbreak.
21. Ms Hill: Age is not a limiting factor: my husband was 50 when he died, so suicide does not happen just among young people.
22. The Chairperson: We realise that although the media concentrate on suicide among young adults, a wide age spectrum is involved.
23. Ms Creaney: Last week, in a programme on suicide among the elderly, Dot Kirby, the health correspondent for BBC Northern Ireland, reported that one in eight suicides in Northern Ireland is in the over-60 age group.
24. The Chairperson: We were not aware of that.
25. Mr Séamus McCabe: I represent the Newry and Mourne branch of the Public Initiative for the Prevention of Suicide and Self Harm (PIPS). In rural, areas resources are scarce. There has been a spate of suicides in Kilkeel and Tandragee. The media coverage of those incidents amounted to frenzy, and there was no evidence for, or truth in, much of what was published. We are greatly concerned about the news media’s coverage of suicides, especially when two or three suicides occur in a short time, as happened in Tandragee.
26. The Chairperson: Did the media sensationalise those events or was its coverage over the top?
27. Mr McCabe: The entire community in the surrounding area of Tandragee was affected — and is still greatly affected — by the way in which the media reported those suicides.
28. The Chairperson: Do you have difficulty with the media highlighting the issue? Good can come out of that.
29. Mr McCabe: Suicide is contagious: a person who has been exposed to suicide becomes at risk of suicide. That community was exposed to suicide and consequently became at risk. When the news media sensationalise a suicide, it heightens the risk and extends it to a wider population.
30. The Chairperson: I concur with you.
31. Ms Ann McGarrigle: That is similar to experience in the north-west. I represent families in Limavady and Derry/ Londonderry. As Rhonda said, suicide does not just affect young people. Four people, two of whom were over 30 years of age, took their lives last weekend, yet their ages were not mentioned in the news media. Suicide among younger people is highlighted rather than cases involving older people.
32. I also work in education, and I am keen to ensure that efforts in that sector are co-ordinated. The health of young people must be examined from primary school onwards. As regards the problem of suicide, Northern Ireland is different from the rest of the United Kingdom.
33. The Chairperson: Another tragedy occurred in Armagh today: a 16-year-old boy took his life. We all feel for the families affected by that dreadful event.
34. Ms Ní Chuilín: I welcome the delegation. Most Committee members are also the health spokespersons for their respective parties, and we are all very keen that the issues of suicide and suicide prevention are kept to the fore. I am anxious that that be put on record.
35. As my colleagues from the UUP can testify, the Minister of Health, Social Services and Public Safety, Michael McGimpsey, has appeared in the Chamber almost every week since devolution. The issue of mental health is raised almost weekly during Oral Answers to Questions and in various debates. The issue is very much to the fore.
36. However, debating the issue and raising awareness is only one part of the solution; finding the necessary resources is a separate task. I see the members of the delegation nodding their heads in agreement. The suicide prevention strategy and the initiatives associated with it must be accompanied by adequate resources.
37. I have no wish to put members of the delegation under further pressure; however, at some stage, voluntary groups must quantify the hours spent working on this cause in their communities. The Committee has stressed that point to other delegations. Those hours need to be totted up and costed. Protect Life is a three-year strategy. When voluntary groups seek funding from the Department or other bodies, the financial cost of volunteering should be identified. The financial cost of suicide must also be calculated, and that issue has also come to the fore. The caring work of voluntary groups must also be costed.
38. I ask voluntary groups to do that, even though they are already under pressure and helping people. Sometimes, however, talking about financial costs or money that has been saved as a result of saving lives receives attention. That is what people will listen to. Committee members are all sympathetic to your cause, and I urge the delegation to consider quantifying its work in that way.
39. The Committee has considered the use of the terms “suicide”, “taking one’s life” and “ending one’s life”, and Sue may wish to comment on that. Families’ groups have lobbied against the use of the term “commit suicide” in the news media, and Sinn Féin has instructed its party spokespersons to avoid using such terms. Other Committee members may have done the same with their parties; I cannot speak for them.
40. The Committee is very keen to help bereaved families, so if there is anything else that the Committee can do, please let us know. I am aware that I have asked the volunteer groups to do much more work, but the Committee is here to support bereaved families in any way that it can. However, as regards resources, groups need to start totting up the exact cost of volunteering and the cost of caring.
41. Mrs Jean Carson: It is very difficult to put a cost on that work. Like Mary, I have been a member of the suicide awareness and support group based in west Belfast for the past seven years. People think that support for families bereaved through suicide is new — seven years is not what I would call new. We have provided support for the past seven years, but we secured funding only last October. We are grateful for the funding that we have received.
42. I hit John McGeown with figures from the documentation. A life lost to suicide costs the Government £1·9 million. In the past two weeks, the suicide awareness support group based in west Belfast completed 11 interventions — 11 lives have been saved that would have been lost to suicide. The most recent case was this morning, when we handed a man over to accident and emergency at 2.15 am. Three members of our support and awareness group were volunteering in the middle of the night. We had to work with the person at risk and get his permission to involve the emergency services.
43. A price cannot be put on the work that we do. People are getting paid to man phone lines, but our support group owns only two mobile phones, which we pay for and run ourselves. Our support group has one worker, Mary, and the rest are volunteers. If our funding were snatched back tomorrow, west Belfast would still have a suicide awareness and support programme. Money is not our main issue — although it makes it much easier for us to deal with matters.
44. The Chairperson: You say that you have prevented the deaths of 11 people. As those young people are alive and can talk about their experience, have you established a pattern as to why they felt that their lives were not worth living?
45. Mrs Carson: The man from last night was 45 years old. Suicide knows no age barriers.
46. The Chairperson: Were most of those 11 people young or were they from different age groups?
47. Mrs Carson: Many of them were young.
48. The Chairperson: Have you established a pattern or contributing factors, such as bullying?
49. Mrs Carson: Nothing that we could identify, only that they were desperate, sad, isolated and, at the time, felt that suicide was their only option. As a result of the interventions, we have opened up other ways for them. They all now receive counselling, and they have opened up to their families — initially, no one but themselves knew how desperate they were. Thank God that 11 people are still alive because of those interventions.
50. The Chairperson: Why do you think that they do not talk to their families?
51. Mrs Carson: I have learnt that they do not want to burden their families. It is easier for people to shut down and keep their feelings to themselves rather than feel that they are a burden to their family. However, the devastation to families in the event of a suicide is much worse than a family member being burdensome in life. We could all cope with burdens in life, but it is very hard to cope with the loss of a loved one to death by suicide.
52. Mr Gerard McCartan: At the start of the year, we were involved in an intervention with a young man. No drugs or drink were involved, but he had attempted suicide a couple of times before. We kept a close watch on him and did what we could. His GP gave me his private mobile number in case anything should happen, which is rare for a GP to do. We got to the root of the situation. The process is exactly as Jean described it: we talked to him, and he told us that he just did not want to live life. He thought that he was a burden and a waster — those are his words. He did not want to tell his mother because he did not want her to be worried, but deep down he did want to tell her.
53. We took a chance and got him into a house. We brought him into the kitchen and made him a cup of tea to settle him down, and we sent for his mother. We brought them both into the front room and the two of them burst out crying. That was a relief for him. He is now working in the town and has just come back from a holiday in Turkey. He opened up. He really wanted his mother to know, but he did not want to be a burden to her. That is what working on the ground is about — taking that chance. It took a few weeks to get to that point, but we took a chance, and it worked out for the best.
54. Mr McCabe: We held workshops in Kilkeel following the suicides there. A couple of workshops involved youths from youth clubs, gyms and the Kingdom GAA club. We asked them to write down, anonymously, their thoughts, concerns and suggestions and post them into a pillar box. Most of the comments expressed concerns about who they were going to hear had died the following weekend. They were also very concerned for their own safety, because they did not know themselves how much at risk they were, and they were afraid that it might impact heavily on them. The young people involved in those workshops were aged between 13 and 18.
55. Despite their ages, it was very mature of those young people to do and say what they did. Their major concerns were: about whose death would they hear next; how that would affect them, and whether it would have such an impact on them that they would consider doing the same.
56. Ms McGarrigle: I have visited five different homes in the north-west in the past fortnight. Three were the homes of young people, and alcohol had been the underlying issue. The other two were: a nurse in her fifties and a man in his forties both of whom had been afraid of losing their jobs. Change at that stage of life, and the sense of hopelessness that it brought, made them depressed. However, they were reluctant to go to their GPs because they thought that they would lose face.
57. Therefore, there is a need to heighten awareness. As Carál said, everybody needs to be aware of suicide. We have reached the stage where it is everybody’s business — everybody in this room, every member of the press, everyone. If we ask a person how they are feeling, we must take the time to listen. It could be you, or me, or any of us: it is happening now.
58. I do not know how to answer Carál’s question in the time available. When people ring us, it is because they have obtained our numbers, and they know that we have experience of death by suicide. We cannot turn them away. At the same time, we cannot say to counsellors that they owe us travel expenses. I do not know how to answer the question.
59. Ms Ní Chuilín: I would like to clarify my point, because I have been misunderstood. I am not saying that you should not do what you do; I want to make that clear. When the Department of Health, Social Services and Public Safety and other Departments set budgets — which they will not do for a while — someone needs to demonstrate, even on your behalf, that your voluntary work is valued by costing the number of voluntary hours that you do regardless of the time, day, or season.
60. Mrs Carson: Our work is 24/7, Carál.
61. Ms Ní Chuilín: Absolutely. However, your work needs to be factored in.
62. Mr McCabe: Given that we were told that an application for funds for a full time co-ordinator, an administrator and premises had to be submitted for April, we applied to the Suicide Strategy Implementation Body (SSIB) in March. The premises are in Newry and Omagh and they are still awaiting the funding. It is now the middle of July, and still no money is available. Last year we were told that £1·1 million was available. The southern area that covers Armagh to Kilkeel and Crossmaglen to Banbridge received 18% of that. Despite submitting our proposal, we are now being told that there might not be enough money to appoint a co-ordinator.
63. The Chairperson: I understood what you were trying to get at, Carál.
64. Ms S Ramsey: I want to put on record that I thank you for the work that you are doing, because I know that, directly or indirectly, you are suffering yourselves. You need to be commended for the fact that you are doing positive work in the communities. You have given the Committee an idea of how many people’s lives you have had an impact on and possibly saved. On behalf of my party, and my colleagues, I commend you for all that work.
65. The Committee received a briefing paper from the Assembly’s Research and Library Service. I commend the team for putting a great deal of work into that paper. What strikes me about it reflects a point that Carál also made. The papers states:
“for 2004, the total estimated cost of suicide…was in the region of £202 million, which equates to £1·4 million per suicide.”
66. Therefore information is available and can be used, and the knock-on effect that suicide has on individuals, families and young people must be taken into account. I am not unique — suicide has touched my family also. The research paper also states:
“Suicide is a permanent solution to a temporary problem.”
67. That point struck me, and it is something to consider, especially where young people are concerned. I represent West Belfast, which has been dealing with suicide for a long time.
68. I do not want to come across as someone who just talks about the issue. Some of you know me and know that I like to get things done. You are not just here to make a presentation and listen to us telling you how good we are. Ms Creaney said that, to date, 161 doctors have taken depression awareness training. I want to hear more about that, because if there are obstacles preventing other doctors taking that training, I want to do something about it. Whether as individuals, family members or community or political representatives, we are trying to focus on suicide prevention. If there is a blockage in the system, we must unblock it.
69. Ms Creaney: I can provide an evaluation of the training that has taken place to date. There are more than 1,000 GP surgeries in the north of Ireland and it is deplorable that only 161 doctors have taken up the training. In the north of Ireland, 25% of GPs run surgeries on their own and do not avail of any type of training. However, the majority have not signed up for depression awareness training. A GP is normally the first port of call for a person facing a crisis, so it is imperative that they take up the; lives could be saved. It is only three hours long; surely they could spare that amount of time.
70. Further to the depression awareness training, GPs can avail of Applied Suicide Skills Intervention Training (ASIST), which is a two-day workshop providing skills in suicide first-aid and intervention. If 10 GPs and their staff in west Belfast gave up one weekend, that programme could be delivered to them at very little cost. Surgery managers do not always have hands-on relationships with patients therefore all the receptionists and GPs could have the ASIST training in their own surgeries over one weekend.
71. Ms S Ramsey: Please leave the details with the Chairperson, and members will receive a copy. As individuals or Committee members, we can do something about that.
72. I have a couple of other points. Ms Creaney mentioned a 24-hour response team; we need to know more about that. The Committee can do several things; it can write to the Minister to get the clarification needed. However, all of the information must be put together.
73. According to the Bamford Review, bereaved families should have a major influence on the introduction of a suicide prevention strategy. What I am hearing is that this is not happening. Would Ms Creaney make some brief comments about that?
74. Ms Creaney: Ms McGarrigle was the chairperson of the recently established Families Forum, and I was its secretary. The NIO Minister Paul Goggins had the idea of bringing families on board, because it was they who were pushing to establish the campaign and without them, the strategy would never have been implemented.
75. Mr Goggins valued our contribution and wanted to do something about the problem. He said that a forum would give us a powerful voice, but that did not materialise. We knew that we would never have a veto, but our voice was never as powerful as we had envisaged. Sadly, the Families Forum was dissolved two weeks ago. However, the network of connections established via the forum will be kept going, and we will meet at least four times a year, so that the issues that we have talked about today can be raised with local and regional health and personal social services boards.
76. We were really enthusiastic about the concept of a families’ forum, its establishment and its ethos, because it was new and was evolving. Indeed, a group of families in New York had developed something similar. However, while we were enthusiastic, we had to be aware of the issue of accountability, and we had to be accountable to ourselves, especially when we realised that the forum was not doing what had been intended.
77. Ms McGarrigle: There was a very well publicised mental-health programme rolled out in February. We are not against it, nor would we say anything about it. However, approximately £380,000 was spent on that campaign yet not one member of our forum was involved in the programme. The forum was set up in September 2006, and it was well known that we were representing people across the Province as best we could. Therefore, it was embarrassing not to have had more involvement in the campaign.
78. Ms S Ramsey: I am trying to tease out how the issues can be tackled. I hope that you picked up my point earlier about your not just coming to give a presentation and then leaving. Earlier, Carál Ní Chuilín mentioned the terminology that is used when discussing suicide. What is the proper terminology so that we can educate people? Education is crucial, and attitudes must change. Without going into detail, I am dealing with a case in which a professional who works for an out-of-hours-service told someone flippantly: “Go on to a railway track and take your own life.” It is important that we change attitudes.
79. Ms Creaney: As bereaved families, we hear stories like that all the time. The word “committed” has legal, ethical and moral connotations — suicide was once a crime. It was decriminalised here in the 1960s and in the South of Ireland in the 1990s. Therefore, it is hurtful for families to hear it being said or reported that someone has “committed suicide” because that phrase slices through those who have recently been bereaved. If the words used were changed to “died by suicide” or “died through suicide” it would help reduce the unbelievable stigma that is attached to the word “committed”.
80. Rev Dr Robert Coulter: I admire immensely the work of the bereaved families. As someone with experience of counselling people who have gone through such trauma, I have found that Churches get involved only after an event. Could more be achieved through Churches becoming involved at an earlier stage?
81. Ms Creaney: Last year, we gave a presentation to the Knights of Colombanus, a lay organisation in the Catholic Church that is similar to the Freemasons. After the presentation, the Knights of Colombanus started to take the ASIST workshop as they visit the homes of people in their parishes who are in suicidal crises.
82. My experience from attending funeral masses in Catholic churches is that the comments made by older priests with an old-fashioned mentality can often be hurtful. All the Churches must be educated about suicide, because, although it is no longer considered a sin, many older priests and ministers believe it to be sinful. That attitude must change, and it must start in the seminaries where priests are being taught. The theology around suicide must be reconsidered.
83. Rev Dr Robert Coulter: In my experience, Churches might be able to do more in the period after funerals. Could they do more to help those with guilt complexes and who wonder whether they could have done more to prevent the suicide?
84. Mr McCabe: We have had the same experience. The public initiative for the prevention of suicide and self-harm (PIPS) project has support groups that facilitate both sides of the community. The concern is that Churches perform no follow-up action in the aftermath of suicides. That has created a great deal of resentment, because it is felt that Churches should act as a support mechanism for the community. Although Churches on both sides of the community provide support in other circumstances, they seem to withdraw when it comes to suicide. They especially withdraw in its aftermath. I am talking about both sides of the community because, although I am a Catholic, our support group facilitates both sides of the community.
85. Ms McGarrigle: I am a Presbyterian, and I have noticed some change in the Presbyterian Church’s attitude. When my son took his life 12 years ago, we were fortunate to have a good minister. I told him that he had to come to me. My 20-year-old son, in common with the behaviour displayed by most young people, had not gone to him.
86. I lobbied the Presbyterian clergy in my area, and, subsequently, Church House has produced a good leaflet about suicide. However, there is still much to do. Barry McGale, the suicide co-ordinator for the north-west, ran workshops that have been attended by clergy from all sides. They learned a lot, particularly about good practice, and we hope that there are more such initiatives.
87. Rev Dr Robert Coulter: When I attended college, the subject was never mentioned.
88. Mr McCabe: Eighteen months ago in Dublin, the Catholic bishop’s conference addressed the issue of suicide by sending a letter to each church to be read during the homily at morning Masses. The letter spoke of openness and suggested that congregations should be more sympathetic towards families that have been bereaved through suicide. However, that was all that was heard, and there has been no follow up.
89. Ms Maureen Young: It is the luck of the draw. I was lucky to have had good support. However, I appreciate that the experiences of many people have been as negative as mine was positive. We must also appreciate that church attendance among young people has fallen. Other areas that could be used to reach young people are through organisations such as the GAA in which a lot of interaction is structured around playing sport and training.
90. Ms Creaney: Sometimes, in the aftermath of a suicide, families are stigmatised by their community, including the clergy, which reaffirms the general lack of understanding. People cross the street before stopping to talk to a bereaved person.
91. Ms McGarrigle: They do not know what to say.
92. Ms Creaney: Therefore, the bereaved person must also contend with the stigma that arises after a death.
93. Ms Young: It is a matter of education. Public-awareness must be increased, and there must be a drive to address that perceived stigma. Suicide echoes mental health in that, as Ann McGarrigle said, people are afraid to go to their GPs. There is a huge problem with how people perceive mental illness.
94. The Chairperson: Many people just do not know what to say.
95. Ms McGarrigle: There was a cluster of suicides in Ballymagroarty or Ballymac. On Sunday week ago, despite its being a miserably grey and wet summer evening, a fabulous and most moving homily was held to attract young people. Initially, I was sad that more people such as us attended rather than young people. Later, I thought more positively. About 200 young people were changing the 16 Stations of the Cross and there was music. In that church setting, with Fr Chris, it was a positive, forward-looking event for people in the north-west. I am sure that similar events take place in north and west Belfast. There are changes afoot among the clergy, and we must encourage more of that.
96. The Chairperson: They are supposed to look after us from the cradle to the grave, and in between.
97. Mr Gallagher: Thank you all for coming along. Most of you have been through difficult and challenging experiences and are taking a positive approach to suicide.
98. Policies and resources have been mentioned. It was suggested that not everything is being done as regards primary care and accident and emergency (A&E) provision that could be done. What is best practice elsewhere?
99. Resources are scarce. However, if resources could be made available, for what purpose should they be used? Should they be used to make counselling more accessible and readily available, or should they be used for 24/7 response teams?
100. Ms Creaney: As regards best practice in A&E — in America, if people present themselves at a hospital’s A&E department and are suicidal and have taken alcohol or drugs, they are kept in a secure place until a psychiatric assessment has been done.
101. The abuse of staff and the damage that is done to A&E departments due to people’s consumption of alcohol is well known. We have always said that if a room were made available for individuals who present at an A&E department as being suicidal through self-harm, nursing staff would not necessarily have to baby-sit them. Volunteers could sit with them until they were well enough to have a psychiatric assessment. That is one solution to the problem at A&E departments.
102. Sometimes, it is at the discretion of a psychiatrist as to whether or not a person who has taken alcohol or drugs would be given a psychiatric assessment. Sometimes, psychiatric assessments are given, but those are usually the exceptions to the rule. We want individuals to be kept in a secure place until a psychiatric assessment can be done.
103. If the recommendations of the Bamford Review were implemented adequately, it would make such a difference to mental-health services. In 2005, in north and west Belfast alone, there was an estimated underspend of £2·5 million on mental-health provision. I do not know what the current figure is as I have been unable to obtain that information. More resources would be welcome.
104. I agree with Ann’s comments about the Health Promotion Agency’s Minding Your Head public information campaign and the amount of money that was spent on it. Sometimes people think that by throwing money at a problem, it will be solved. However, it is how and where the money is spent that is important. Creating safe environments in A&E departments would be a good place in which to put resources.
105. Ms Young: I have talked to people on the Northern Health and Social Services Board, and its primary care team would like more training equivalent to that, which was given to GPs. Also, the board feels that its rapid response team is far too small for the geographical area that has to be covered.
106. Mr McCabe: It might be worthwhile incorporating some mental-health training into the medical curriculum. As things stand, the curriculum does not include that.
107. Mr McCartan: The Minister of Health, Social Services and Public Safety has said that 33 beds will be available in 2009. On three separate occasions a consultant told my son that he should be in hospital — but hospital was not the place for him. So, where did he go? He went back home. I would like to see a halfway house where patients could be away from their daily environment and getting a wee bit of respite. As parents, we would know that our sons or daughters were in a safe environment for a couple of days.
108. Mr McCabe: I had a different experience. My son had no mental-health problems of which I was aware. He did not exhibit any signs. He was a bright lad at university and he was outgoing. Caroline Farquhar is head of implementation for the Choose Life anti-suicide strategy in Scotland and her research has shown that 7% of those who take their lives are not in the mental-health system.
109. Of the 30% who are in the mental system, 1% receives the largest amount of funding — that is for those who are in-patients. The problem is community based, and we who are working at community level need to get the resources to do our work. At present, the SSIB funding is going out to everybody and their granny while many people who are doing the heavy groundwork with the communities are not accessing those funds.
110. Mr Gallagher: Are you talking about a kind of counselling services?
111. Mr McCabe: We buy in counselling services. Contact Youth provides the biggest counselling service. They got a lot of funding for north and west Belfast.
112. Mr McGarrigle: That was part of the Minister’s strategy.
113. Mr McCabe: It was launched on 30 October 2006.
114. Mrs Carson: We want emotional literacy to be included in children’s early education — not starting in post-sixth- and seventh-year education.
115. Let us start to educate young people early that it is OK for them to say that they feel sad. They should be comfortable with such language, be able to say that they do not feel right, and be able to ask whom to talk to about it. With the stiff upper lip attitude, no one dares mention sadness in case people will think that they are not right in the head. It must be OK for people to say that they do not feel well.
116. In the Linda Bryans’ campaign — and people in this room know how much money was put into that campaign — the word “suicide” was not mentioned once. Another campaign slogan was, “If your head’s away just say”, and rightly so, but who can you say it to? The resources are not there for people to say that their “heads are away”.
117. The 24/7 youthline is going to be extended. It will be inundated with calls, as are we in the West Belfast Suicide Awareness and Support Group, but the resources are not available to deal adequately with the calls. The Government is throwing good money after bad. They need to listen to the people who are working from the bottom up — we definitely do not work from the top down. We deal with the issue 24/7; we cannot walk away from it, but we are not paid to do it.
118. The 24/7 help line does not answer the calls on a 24/7 basis. I tried it; I targeted that help line over the Christmas period. I called it six times during the three-day period, Christmas Eve, Christmas Day and Boxing Day, and I got the “engaged” tone. I have taken up the issue with Opportunity Youth and Contact Youth because it is not providing the service it claims to provide. Opportunity Youth is having massive amounts of money thrown at it to provide that service.
119. Mr McCabe: I would like to pass a card around that will show the Committee what PIPS has done. We distributed 40,000 such cards in the Kilkeel area to address the issue of suicide. It is a help card that offers advice to young people who feel suicidal. It simply refers to us as PIPS Newry and Mourne. It gives a number for the 24/7 free-phone Youth Line, as well as the numbers for the Samaritans, the out-of-hours GP service and Childline. It also has spaces in which to add the numbers of three friends, which they are advised to enter into their mobile phones. It also mentions the T.A.L.K. model, which breaks down advice to the following:
“Tell someone
Ask for help
Listen to advice
Keep safe”.
120. I will pass the card around so Committee members can look at it.
121. The cards have been well accepted in the community, and the Probation Board in Belfast contacted us to get some of them. That is the sort of work that is happening on the ground.
122. Ms McGarrigle: I work in education, and information sources such as that card are very useful. I use materials from the north and west Belfast groups, and the PIPS Newry and Mourne card, which I leave in foyers for people to pick up. It is wonderful to see how many are lifted. Young people want advice and help.
123. The Chairperson: That is an excellent card. It is lovely that it says:
“MY PROMISE FOR TOMORROW: If I feel helpless, hopeless or confused. I promise to talk to someone.”
124. It is all about talking, and young kids should be encouraged to start talking when they recognise that they do not feel the same as their friends and siblings.
125. Mrs Hanna: You are all very welcome. As you said, suicide is difficult to talk about, and it is difficult for the Committee too, because nobody has the answers. It is a complex issue, which, as you know, is different for everybody. I have four children, three of whom are open and outgoing and one who is quite introverted. He would not talk about his feelings at all. Some people find it easier to talk than others.
126. You talked a lot about training. People such as yourselves, who have the experience, must be listened to. Training programmes should be rolled out for peers and relatives first and then for the professionals, such as GPs, teachers and nursery schools, so that they will be more aware of the issues.
127. There are some good schemes. I have worked with PIPS in north Belfast and with some of the schools. There is a very good programme in the Holy Family Primary School in north Belfast. All the teachers there have been trained to be aware of the problems. If they feel that children need to open up, they try to encourage them to talk about their feelings, and they try to work with the parents. The message must be spread. There are no easy answers.
128. Suicide is no respecter of age or class. I represent South Belfast. In the space of two weeks, three young people, one of whom was my next-door neighbour, took their own lives. Another good friend of mine, a man of my age, who was very outgoing, was a teacher and was involved in many charities, took his own life. He was the last person that anybody, including his family, would have thought might do such a thing. His suicide appeared to be out of the blue. Mental health is not always about obvious problems, but sometimes it is.
129. As has been mentioned, some stigma is still attached to admitting that we need help with mental-health issues. If people suffer a broken bone or even if they have cancer, it is easy for them to go to hospital to ask a doctor for help. However, admitting that one cannot cope is the hardest thing in the world. I suppose that all of us — starting with very young children — need to be encouraged to speak about our feelings and to recognise when we have a problem.
130. As a midwife for many years, I never heard the term “early intervention”, but I knew very quickly that some babies and parents needed help —better parenting skills, for example — to cope better. The sooner that we all give that help, the better.
131. The problem is a societal one. We no longer have the values and support systems of family and the Churches; we are too materialistic and do not appreciate the simple things any more because we live in a society in which we throw everything away. We will never get back to quite where we were, but we need to get back to stronger family values and support systems; we need to start with the family and then consider the wider community.
132. We can do that through the Bamford Review, which talked about the need to look at the big picture while making small incremental steps. Those small building blocks need to start with the likes of our witnesses today and other health professionals and educators who can provide training and raise awareness to get things started. Sometimes the issues are so complex that it is difficult to know where to start. We should look at the big picture, listen to the people who have experience and then take the first small steps. However, that is not easy for any of us. There are no easy answers, but everyone wants to help. It is not just a question of resources — although they are part of it — but of knowing exactly what is required and having a plan. It is about how we start to put things together.
133. The Chairperson: Thank you, Carmel. That was not so much a question as an observation —
134. Mrs Hanna: The issue is really about values.
135. The Chairperson: Yes; if only we could get back to the tradition of family.
136. Mrs O’Neill: I thank all the witnesses for sharing with us today. Who better to hear from than people who have been bereaved by suicide and are aware of what is happening?
137. A nurse told me that there are great concerns about local accident and emergency services: if someone presents with self-harm at, say, 12 o’clock at night, there is no one to whom the person can be referred until the next morning. Is that the case? If the patient chose to leave before then, that would create a massive problem.
138. Mr McCabe: It is very hard to keep people over the age of 18 on board because so much red tape is involved. We have that problem with our services in Kilkeel. The referral system for people up to the age of 16 is easily accessible because services are available 24/7 and there are many resources that people can access. After the age of 18, people need to go through the adult system, which can take three or even four days.
139. Mrs O’Neill: The rural/urban divide has been mentioned. Has the Department taken a blanket, one-size-fits-all approach? Should more be done on a rural-specific and urban-specific basis?
140. Ms Young: It is for people like us to — for want of a better term — fight our corner. It is important that the powers that be are aware of the different needs; we must emphasise those needs as well as addressing the issue of stigma.
141. Mr McCabe: Cities get more attention than rural communities. For example, there are three co-ordinators in the Belfast area — and rightly so, as they are needed — but there is nothing for the Southern Health and Social Services Board area, which I represent. We have put in a proposal, but we have no co-ordinators for suicide prevention and intervention in the whole southern board area.
142. Ms Young: We deal with a different type of people. In the rural farming communities that I mentioned earlier, people have more resilience so, as Carmel said, the last thing that they want is to tell someone that they cannot cope and to admit that they are helpless. That is not part of their mentality.
143. We must break that down and get across the message that it is OK to feel that way, and that everybody is the same.
144. Mrs Carson: Everyone has a role to play in addressing suicide, whether in rural or in urban areas. Rhonda lost a 13-year-old daughter; my son was 21; Maureen has told you that her husband was 50; Gerard and Séamus lost young sons; Ann’s son was 20; and I think that Mary’s brother was 47. Gender and age are not relevant.
145. Everyone hears about young people who have committed suicide because such stories make for good media, but we have not heard in the media about Carmel Hanna’s neighbour. During our car journey here, Séamus said that a 70-year-old in his area had committed suicide. Local people hear about such incidents, but they will not be covered in the papers because they do not make for sensational journalism. We need to have journalists on our side. I speak to journalists regularly, and they have a role to play.
146. Our loved ones died through suicide — I am not ashamed of that. I have to get on with life, do the best I can, and walk this walk. Sadly, the people alongside me are walking the same walk. We have all had the same experiences of suicide. Media hype must be addressed. Where suicides occur, whether in rural or in urban areas, does not matter.
147. Members of the Committee will be aware that I am from west Belfast, which has been socially and economically deprived for many years. Suicide is expected there. My child died as a direct result of sexual abuse, as has been well documented. Knowing the reason for my son’s suicide does not change the fact that we lost our child. The person who abused my child might as well have murdered him because my son was left with his own life sentence — he could not live in darkness any longer.
148. Which professions does the Committee think have the highest rates of suicide? It is not the working class of west Belfast; it is our dentists, anaesthetists and farmers. Because they have means, the other needs of those people are not met. We will lobby wherever is necessary because we have a voice and we will be heard; in contrast, the higher echelons of society often hide the stigma of suicide. They fear that because their relative was an anaesthetist or ran their own business, they dare not reveal that they committed suicide; instead, they say that their loved ones died of massive heart attacks or strokes. We deal with the reality, and I am not ashamed to say that my child died through suicide.
149. The Chairperson: I take your point. A psychiatrist will give evidence to the Committee later, and I hope that you can stay to hear what he has to say. The Committee would be delighted to meet you again if there are any updates or other problems that you wish to highlight. The Committee holds working lunches every Thursday before it meets, and it also visits outside venues and can address specific issues, the Bamford Review and its consequences for example. The Committee is happy to meet you again either here or in your areas so that we can observe a session with those who have come to you for help — if they do not mind our being there.
150. There will be a Hansard report of today’s meeting, which we will send to the Minister immediately so that he can read of your concerns and outline how he will implement appropriate back-up services.
151. The suggestion to set aside a room in the accident and emergency departments of hospitals to deal with those who present with suicidal tendencies was extremely good and should be highlighted. It is sad that so few GPs attended the three-hour training programme, given what is happening in our society — that should be highlighted.
152. I thank all the witnesses. It was very brave — I mean that in no patronising way — to express what you feel should be done to help those in the same situation as yourselves and others who will, sadly, experience such dreadful trauma in the future.
Committee Fact-finding trip to Scotland
Committee for Health, Social Services & Public Safety
Room 412, Parliament Buildings,
Stormont,
Belfast
BT4 3XX
Tel: 90521360
Mob:07900278992
hugh.farren@niassembly.gov.uk
To: Chairperson & Members
From: Hugh Farren, Clerk
Date: 29 April 2008
Subject: Committee Fact-finding trip to Scotland
On the 7th November 2007, eight members of the Northern Ireland Assembly’s Committee for Health, Social Services and Public Safety went to Scotland on a fact finding visit to see first hand how the Scottish Government is tackling the problem of Suicide. The following report summarises the meetings which took place over the duration of the two day visit.
The Committee Members were:
Mrs Iris Robinson MP MLA (Chairperson)
Ms Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
Mr Tommy Gallagher MLA
Mr John McCallister MLA
The Committee Staff who accompanied the Members were:
Mr Hugh Farren – Clerk to the Committee
Mr Joseph Westland – Clerical Supervisor
Mr Neil Foster – Assembly Research
Thursday 8th November
On the Thursday morning, the Committee members met with Dr Rory O’Connor, the UK representative for the International Association for Suicide Prevention. Dr O’Connor briefed the Committee on the history of international suicide prevention strategies, from the initial Finnish strategy, right through to the Choose Life strategy being carried out in Scotland.
Dr O’Connor identified various positive aspects of the Scottish strategy and pointed to the benefit of using evaluations from the first phase to impact on what happens in the second phase.
Various lessons which were learned during the roll out of the Scottish strategy were discussed. These included the need for more support before the launch of the strategy and in the implementation, also the role of evaluation at the local level. Another important lesson was the need for international evidence sharing. Dr O’Connor then focused on the role of targets and his concerns if these targets are not met.
A transcript of the presentation by Dr O’Connor has been attached
After the question session with Dr O’Connor, the Committee met with members of the Scottish Health and Sports Committee. The members were:
Mr Ross Finnie MSP (Deputy Covener)
Dr Ian McKee MSP
Ms Mary Scanlon MSP
One of the main topics raised during this meeting was the role of social deprivation in suicides. Ms Scanlon MSP raised the point that while this was an important issue, her own constituency (The Highlands and Islands) has had the highest suicide rate in Europe for a number of years. Ms Scanlon MSP pointed out that the majority of completed suicides in this area had been carried out by males who were financially well off. She went on to say that one of the reasons why these events took place was the environment, the bleak and lonely nature of the Highlands and Islands. Ms Scanlon MSP stated that any future National Suicide Strategy needed to look at support services for those at risk in rural areas.
After Lunch and a tour of the Parliament buildings, the Committee met the Minister for Public Health, Shona Robinson MSP. Ms Robinson MSP stressed the financial support given to the Choose Life Campaign and the need for any project that has been granted funding, to have the ability to become self-sustaining. The short meeting with the Minister was followed by a more detailed briefing on the Choose Life Strategy with Officials in Leith.
The budget outcome in Scotland was due to be announced shortly. Ring fenced funding for Choose Life ceases in 2008 and it seemed likely that any future funding for the suicide strategy would be included in the overall allocation to Boards. Another point raised was that of private sector involvement. This was highlighted by the presentation given by representatives from Breathing Space, which is a phone line service set up as a support for anyone feeling depressed or suicidal. The telephone helpline was supported by four of the major mobile phone vendors. Another innovative link-up was with various sporting associations, such as the SFA and SRFU, who have given permission for card with helpline numbers to be given out at matches and events all over Scotland, thus raising the profile of the services at a national level.
Friday 9th November
The focus of the second day of the visit was looking at how the Choose Life Strategy is delivered within a local context.
The day started with a visit to A&E and other facilities in Ayr Hospital followed by a meeting with senior representatives of the NHS Ayrshire & Arran. Issues raised in this meeting included the role of the Community Planning Partnerships in implementing and evaluating Local Action Plans and activities, making sure that funding was efficiently managed, that the issue of stigma was addressed locally as well as early intervention and prevention, response to immediate crisis and setting up coping strategies not only for families dealing with completed suicide, but staff as well.
A copy of the presentation has been attached
These final points were addressed in more detail as the Committee went to the Strathlea Resource Centre in Kilmarnock to meet with Local Choose Life Co-Ordinators.
The Committee met with co-ordinators from the three Ayrshire regions (North, East and South). The Co-ordinators stressed the need to co-ordinate resources on an Ayrshire level for issues such as Commitment-Seven training (training in suicide awareness for front line medical staff). The Co-ordinators briefed the Committee on the variety of projects which were talking place in each region, such as the award-winning bibliotheraphy utilised in East Ayrshire to the Green Gym initiative used in South Ayrshire.
A copy of this presentation has been attached
The Committee then visited the North West Kilmarnock Area Centre, a multidisciplinary centre, which contains a wide range of facilities including a health centre, fitness facilities, housing offices and dental school. During meetings with the staff it was noted that this type of centre is to be set up all over Scotland.
The Committee then met with Rev Roddy McNidder, head of the Critical Incident Stress Management Team (CISM), which has been set up to provide a structured system of care in order to reduce the adverse reactions that would often occur following a critical incident. Rev McNidder discussed the need for counselling services for frontline staff.
After the brief presentation, the Committee visited Crosshouse Hospital, where the CISM team have set up accommodation for staff to go and talked to trained professionals. The Committee members talked briefly to members of the CISM team before leaving for the airport
Committee visit to Scotland -
Choose Life presentation
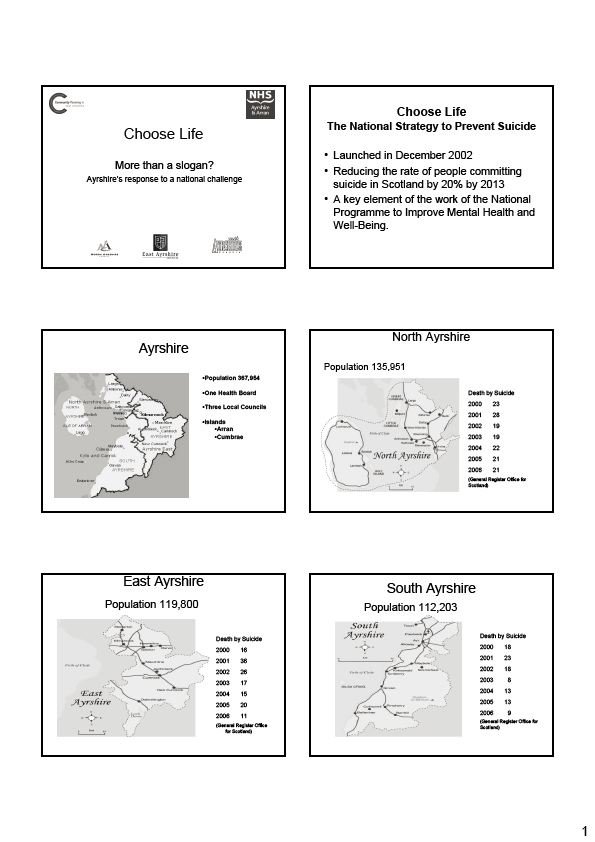
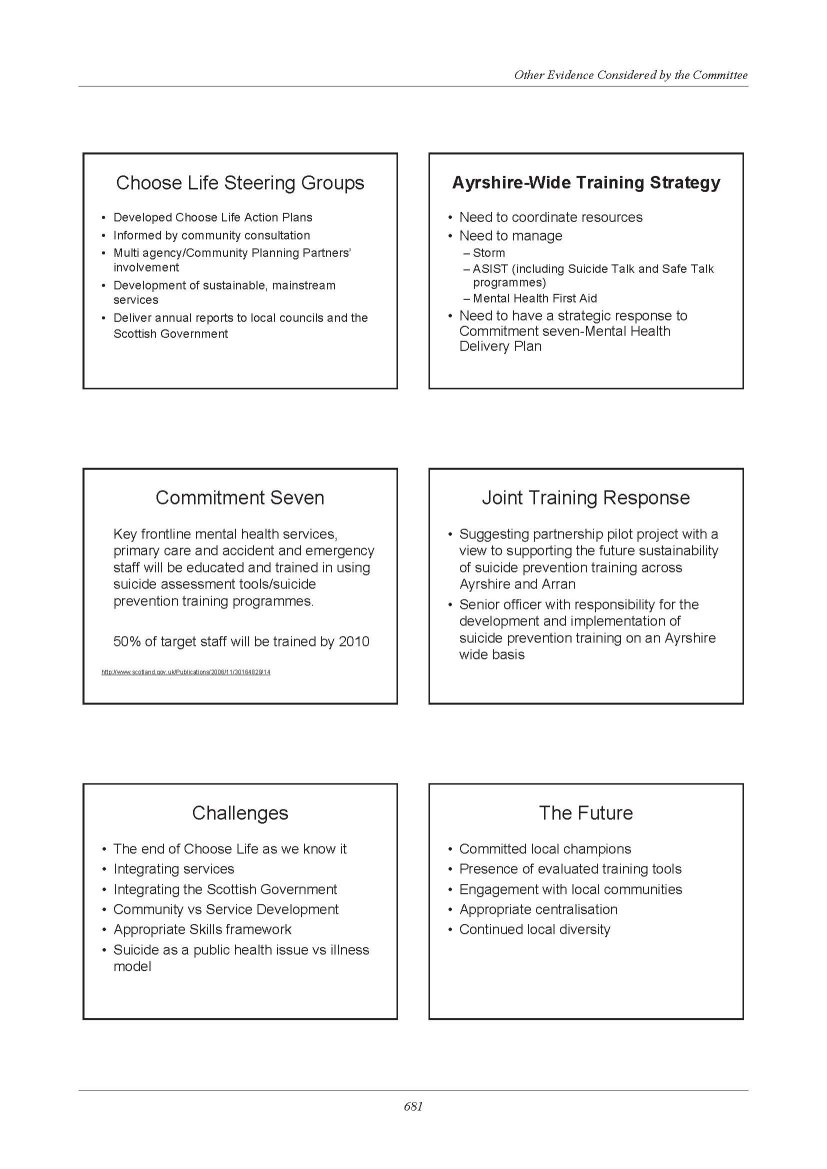
Committee Fact-finding trip to Dublin
Committee for Health, Social Services & Public Safety
Room 412, Parliament Buildings,
Stormont,
Belfast BT4 3XX
Tel: 90521360
Mob:07900278992
hugh.farren@niassembly.gov.uk
To: Chairperson & Members
From: Hugh Farren, Clerk
Date: 29 April 2008
Subject: Committee Fact-finding trip to Dublin
On the 21st February 2008, eight members of the Northern Ireland Assembly’s Committee for Health, Social Services and Public Safety travelled to Dublin on a fact finding visit to see first hand how the problem of Suicide was being tackled in the Republic of Ireland. The following report summarises the meetings which took place.
The Committee Members were:
Mrs Iris Robinson MP MLA (Chairperson)
Ms Michelle O’Neill MLA (Deputy Chairperson)
Rev Dr Robert Coulter MLA
Mr Alex Easton MLA
Dr Kieran Deeny MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Ms Carál Ní Chuilín MLA
The Committee Staff who accompanied the Members were:
Mr Hugh Farren – Clerk to the Committee
Mr Mark McQuade – Assistant Clerk
Mr Neil Foster – Assembly Research
Committee Members first visited Pieta House in Lucan. Following an introduction by Joan Freeman, Chief executive of Pieta House and a tour of the facilities, Members were briefed on the Prevention, Intervention & Postvention (PIP) approach for treating Suicide & Self Harm.
Freda Manweiler briefed the Committee on the Prevention work carried out by the drama group Smashing Times who teach coping skills to teenage children through role-play.
Joan Freeman briefed the committee on the intervention work carried out by Pieta House. Pieta House offers a treatment programme for people who have attempted to take their lives and people who have engaged in self-harm. Pieta House, in a regular suburban setting, is community based and offers treatment in a non threatening environment. It receives some Government support but relies mainly on community support. It believes this is important to maintain its autonomy. It is staffed by paid qualified counsellors and managed by volunteers. Pieta House has treated 1,200 patients since it was set up two years ago and so far none have gone on to take their own lives.
George Brogan briefed Members on the work of Turas Le Cheile with families bereaved by suicide.
The Committee then travelled to Leinster House were they met with members of the Joint Committee on Health and Children. A transcript of the meeting is attached.
After Lunch the Members met the Minister of State, Dr Jimmy Devins TD, who briefed the Committee on the background to ‘Reach Out- A National Strategy for Action on Suicide Prevention’, and Geoff Day, Director of the National Office for Suicide Prevention, who briefed Members on the work of the National Office. Copies of both presentations are attached.
The meeting ended with a presentation by Professor Kevin Malone from University College Dublin on his work on the INSURE Project.
Comhchoiste Um Shláinte Agus Leanaí
Joint Committee On Health And Children
The Joint Committee met at 12 noon.
Members Present:
Deputy Bobby Aylward,
Senator Frances Fitzgerald
Deputy Catherine Byrne*
Senator Phil Prendergast
Deputy Margaret Conlon
Senator Mary M. White.
Deputy Kathleen Lynch
Deputy Dan Neville
Deputy Rory O’Hanlon
Deputy Jan O’Sullivan
*In the absence of Deputy James Reilly.
In attendance:
Deputies Caoimhghín Ó Caoláin and Dinny McGinley.
Deputy John Moloney In The Chair.
Incidence of Suicide: Discussion with Delegation from Northern Ireland Assembly.
Chairman: I welcome everyone to the meeting. I have received apologies from Deputies Bernard Allen and James Reilly. The joint committee expresses its condolences to Deputy Reilly on the death of his brother, Dr. William Reilly.
The purpose of today’s meeting is to meet members of the Committee for Health, Social Services and Public Safety from the Northern Ireland Assembly. It gives us great pleasure to welcome the Chairperson, Vice Chairperson and members of the committee to Dublin. We have with us Ms Iris Robinson, MLA, Chairperson; Ms Michelle O’Neill, MLA, Deputy Chairperson; Mr. Alex Easton, MLA; Dr. Kieran Deeny, MLA; Ms Carál Ní Chuilín, MLA; Mr. Tommy Gallagher, MLA; Ms Carmel Hanna, MLA; and the Rev. Dr. Robert Coulter, MLA. I ask members of the joint committee to introduce themselves.
Senator Frances Fitzgerald: I am a representative of Fine Gael and the party’s leader and spokesperson on health in the Seanad.
Deputy Jan O’Sullivan: I am Vice Chairperson of the joint committee and Labour Party spokesperson on health.
Deputy Catherine Byrne: I am not a member of the joint committee and I am deputising for Deputy James Reilly who cannot attend due to the death of his brother.
Deputy Dan Neville: I am a member of the joint committee and Fine Gael spokesperson on mental health.
Senator Phil Prendergast: I am a member of the Labour Party.
Deputy Kathleen Lynch: I am the Labour Party spokesperson on equality and disability.
Deputy Caoimhghín Ó Caoláin: I am the Sinn Féin spokesperson on health. While I am not a full member of the joint committee, I regularly attend its meetings.
Deputy Margaret Conlon: I am a member of the committee and represent the Cavan-Monaghan constituency.
Deputy Rory O’Hanlon: I am a Fianna Fáil member of the joint committee.
Deputy Bobby Aylward: I am an ordinary Fianna Fáil member with no additional titles.
Senator Mary M. White: I am the Fianna Fáil spokesperson on children, older people and mental health in the Seanad. I have taken up the issue of a positive action programme against suicide.
Chairman: We will have a short meeting as the delegation has a long agenda. I compliment officials from the Assembly on the tight schedule and work programme they have drawn up for the delegation. We intend to conclude the meeting by 1 p.m. for lunch and I understand the delegation will meet the Minister of State at the Department of Health and Children, Deputy Jimmy Devins, at 2 p.m. The joint committee looks forward to many further such meetings.
This is the first time the health committee from the South has met its counterpart from the North. This is a small island and we have many issues in common. From speaking to members of the delegation last night, I noted we share similar difficulties. I hope we can pool our resources and expertise to promote good health on the island.
The Committee for Health, Social Services and Public Safety has prioritised suicide prevention. The joint committee made suicide prevention a priority in 2005. I recognise the major contribution of Deputy Dan Neville who has been to the fore on this issue for many years. In more recent times, Senator Mary White has taken a major interest in this area. In prioritising suicide prevention in 2005, the joint committee produced 33 recommendations. I understand the delegation has had a brief period to read the report in question.
While I do not intend to discuss all aspects of the report, several points were highlighted by members. They include the close connection between suicide and mental illness; the need to ring-fence in the health budget funding for treatment and the upgrading of mental health services; the issue of adolescent difficulties and the need to target specific funding at this area; and the role of alcohol in the high incidence of suicide.
I invite the party spokespersons from the joint committee to contribute, after which I will ask Ms Iris Robinson, MLA, and her colleagues to respond.
Senator Frances Fitzgerald: I congratulate the Chairman on organising this meeting. It gives me great pleasure to extend a warm welcome to the Committee for Health, Social Services and Public Safety of the Northern Ireland Assembly. I hope today marks the beginning of what should be a productive and mutually beneficial relationship in which we can exchange ideas and learn from our experiences. As the Chair noted, this is the first official meeting between committees of the Northern Ireland Assembly and Oireachtas and, as such, it is of historic importance.
It is appropriate that we should at the outset discuss the area of suicide and mental illness because mental illness recognises no boundaries, borders, emblems or creeds. It is a difficulty and challenge which all societies are facing and a particular difficulty for us in Ireland. I have no doubt we can exchange much useful information and learn from each other.
The Chairman has pointed out that funding remains a huge concern for us. All member of the committee are concerned to ensure that the issue of mental health, mental illnesses and facilities are accorded the priority they deserve. This is especially the case given that one in four people will experience a mental health difficulty in the course of their lifetime. Every family is affected by mental health issues and it is therefore appropriate this is the topic we have chosen as the key topic to discuss at our first meeting.
The committee has issued a comprehensive report on this area. Much of the work to be done is concerned with implementing its recommendations. To highlight a few key points, the study shows that alcohol plays a major part in the majority of suicides and attempted suicides amount young adults. In this regard I am sure there is scope for cross-Border co-operation to reduce the prevalence of drug and alcohol abuse. This would reduce suicide in both societies. Aspects for consideration include common policies towards alcohol sponsorship of sports. Banning the association of alcohol brands with sporting activities would help reduce the use of alcohol among young people. Studies have shown a correlation between suicide and the extent of young people’s exposure to alcohol advertising. That is a key area for us to examine.
The breakdown of community is a factor we also need to consider, as less support is available to people. In many ways economic progress has put more pressure on individuals and families. This is another area of mutual concern. Perhaps we can examine the community organisations that operate all over the island and investigate how their resources can be brought together to help young people.
I understand that in Northern Ireland there are approximately 150 suicides every year and that many of them are of young men. The average number of suicide deaths each year is approximately 500. That is the official figure. The real figure is probably higher. This is a significant issue for us. We also have a high number of people who deliberately self-harm.
As the Chair stated, my colleague, Deputy Dan Neville, has played a key role in increasing awareness and helped to alert individuals, families and communities to the cries for help that exist. It is very important that we are all alerted to the signs in a timely way.
I thank the group for its attendance. I wish its members a very productive and enjoyable visit and l hope for a long and productive relationship of co-operation between us. I look forward very much to hear the points of view and experiences of the group and what it is doing to tackle the problem of suicide.
Deputy Jan O’Sullivan: I welcome the delegation also. This is an historic occasion. I hope we will be able to learn from each other and work together for the benefit of people on this island. I acknowledge the work of the previous committee, of which I was not a member, on suicide and suicide prevention. The report it produced is a fine one. I believe the Chairman will distribute copies to everyone.
It is most important to ensure funding is ring-fenced for suicide prevention and mental health generally. The Chairman referred to this area. We have already seen examples where money was set aside for mental health purposes by the Health Service Executive but which has not been spent on mental health. That is a cause of concern for all of us. Some members attended a meeting this morning on eating disorders, which is a separate issue to suicide but there are connections, where we were told that money which was specifically allocated for that purpose was not spent on it. A nice phrase was used to indicate that, effectively, the money was spent on something else. The provision of the service was “put on hold”. We must ensure that money allocated for purposes about which we feel strongly is not diverted elsewhere.
I believe a rationalisation of health services in Northern Ireland is ongoing. Similar to what happened here, the intention is reduce a large number of bodies to a smaller number. We now have one body, namely, the Health Service Executive. Members of all political parties have difficulties in ensuring that plans are delivered on and that the money allocated is spent. We have a mental health programme called A Vision for Change, where there is already slippage in terms of providing funding for services for people with mental health issues.
We can achieve a great deal in co-operation with each other. As the Chairman indicated, we share a lot of common ground and the reasons why people are suicidal are similar, irrespective of the Border. We can learn a lot from each other, especially in terms of research, which is emphasised in the recommendations of the report. There is no reason to separately research the same issue when we can co-operate in this area.
A number of support groups work in this area. People who deal with the issue all say that we need accessible services where young people feel they can go to talk to someone who will listen and understand if they have a problem. The last thing people need is to be told they must go on a waiting list when it is clear they have an acute issue that needs to be addressed. This is an area where we have something in common.
I do not wish to speak at length, as there are many others who wish to contribute, and it is important to exchange views and hear from each other. We must ensure that this area of our health budget is not treated as a Cinderella, which has been the case very often in the past. On this side of the Border there are indications, unless we are very determined, that this will happen under the large bureaucracy of the Health Service Executive, which much of the time seems to focus more on meeting budgetary requirements than providing care. There is a danger, especially in this area, that it will be swamped by other demands and pressing needs.
Chairman: Deputy Rory O’Hanlon is our spokesperson but he has deferred to Senator Mary White who has expressed a special interest in this area.
Senator Mary M. White: I thank Deputy O’Hanlon. The delegation is very welcome. I know many of its members from my past involvement in the peace process in the North.
I compliment this committee on the ground-breaking work it did in 2006 in producing its report on suicide. It was an innovative project. I also compliment Deputy Dan Neville of Fine Gael who has singularly spearheaded this issue, which is a very difficult and dark one.
I am a spokesperson on children and older people. When I was involved in my Seanad campaign this year a number of county councillors asked me to take up the issue of suicide which they felt, from their experience on the ground, had reached epidemic proportions.
In 2006 we had 409 registered deaths from suicide. They are the declared ones; we cannot say how many people actually died as a result of suicide as families do not want to admit to it. We had 366 deaths as a result of road traffic accidents yet all the focus and money to date has been on the prevention of road traffic accidents. The budget for the National Office of Suicide Prevention is very small. It is only €4.5 million. We need to get more funding for this office.
From my research to date, I concluded it is not just a question of funding for this organisation, but it is about what local communities can do. I came to this issue cold last September. There are so many opportunities for community groups, residents’ associations, clergymen and clergywomen, voluntary groups and active retirement groups to do something to reach out to people in their communities.
The rate of suicide in Ireland is the fifth highest in the EU. It reached a plateau in the past year but there is anecdotal evidence of an increase in suicide among older men, especially as a result of the decline of the traditional way of life in the agricultural community. Creameries, and in many cases cattle marts, are gone, as is the rural pub. From studying this matter in depth in recent months I concluded that there is a need to change the way older people live. Older people cannot just say they will go out a couple of times a week or that their social recreation is to go to the pub. We have stringent drink-driving laws now which we all support. However, the local groups I mentioned must put pressure on older people to engage in a different manner socially. I meet many active retirement groups nationally and tell them to keep going to meetings, on the grounds that they will live longer if they do so. It is all about social intercourse.
I could keep elaborating on this. In 1993 we decriminalised suicide in Ireland and it is only since then that the issue has been on the radar. My bottom line is that there should be a 24-hour emergency helpline service with psychiatrists, nurses and social workers at the other end who will listen and offer advice. They will determine whether the caller is experiencing a short-term social crisis or needs to be hospitalised. In the Republic, the only 24-7 helpline we have is provided by the Samaritans. They listen but do not refer to the medical or other relevant services. It has been proven in the United Kingdom that where the emergency service exists, there has been a decline in suicide. I would like the delegates’ opinions on this because I know they have a service in the North similar to that for which I am calling.
Sadly I have learned that many suicides are preventable. The word “suicide” is treated like the word “sex” was 20 years ago in that people are afraid to say it. Depression and mental illness are stigmatised and we must address this. Perceptions are out of date and we must talk about suicide. The bottom line is that many people would not have died had they had somebody to listen to them and offer help. It is not just a question of money but of people in one’s community reaching out in new ways to get people out of their homes to meet people.
Chairman: It gives me great pleasure to invite Ms Iris Robinson to speak to the committee.
Ms Iris Robinson, MLA: On behalf of the members of the Heath, Social Services and Public Safety Committee of the Northern Ireland Assembly, I thank the committee for inviting us today. The meeting has been interesting thus far and I am sure it will remain so.
Our committee has been in existence since last May, at which time devolved government returned to Stormont. This was a very positive step and I supported it wholeheartedly despite some of the negative remarks from some of the media. I am conscious that the Oireachtas Joint Committee on Health and Children has been in existence for an even shorter period, that is, from November. Although both committees are in existence for a relatively short period, ours is already starting to have an impact. Ours, like this one, has identified a number of priorities.
The first priority concerns mental health and learning disability. This area has been described as the Cinderella of the health service and has been neglected badly over many years. The spotlight has been focused on the issue by the publication of the Bamford Review of Mental Health and Learning Disability in Northern Ireland. It is a comprehensive and wide-ranging review that produced ten separate reports on different aspects. The committee is taking a keen interest in how its recommendations will be implemented. I refer not only to securing the necessary resources but also to how the numerous recommendations will be prioritised and put into operation.
The committee considers it can make the greatest impact through committee inquiries. By undertaking an inquiry, the committee can set its own agenda and select an area or issue for detailed examination, and then make strong recommendations to our Minister for Health, Social Services and Public Safety.
The first inquiry focused on health care-associated infections, mainly MRSA. This has caused grave concern among many, particularly those who have gone into hospital, even for minor operations. In September, the committee decided it should put that inquiry on hold for a time while carrying out an urgent inquiry into the growing scourge of suicide, particularly among younger people.
The issue of hospital infections has returned to the glare of publicity in Northern Ireland following an outbreak of clostridium dificile in Antrim Area Hospital. Just last week the committee called in the chief executives of the health trusts to question them on the extent of the outbreak and the actions being taken to tackle it.
On the 24-hour helpline referred to by Senator Mary White, this morning we visited Pieta House, a charitable organisation. This State already has something on its doorstep that should be funded as a mainstream project because it is doing excellent work. In the two years since its establishment, 1,100 people have passed through the doors and not one of those who wanted to engage in self-harm or was contemplating suicide followed through in this regard. This figure alone demonstrates how well the project is doing. The chief executive, Joan Freeman, stated suicide is not just a health issue or political problem but that it is also a community problem. The project needs to be considered with a view to being supported by the Government. I pay tribute to those involved in the Pieta House project.
The committee inquiry into the prevention of suicide and self-harm is the main reason for our visit to Dublin today but I am sure there are many other issues of concern to our two communities. I hope we will have an opportunity to explore some of them today. On our suicide inquiry, we are nearing the end of our evidence-gathering phase and hope to produce a report shortly after Easter. We have received approximately 65 written submissions and have taken oral evidence from a range of organisations, not just those in the field of health. For example, the leaders of the four main churches were before our committee to discuss the role the churches can play in preventing suicide and dealing with bereaved families. Interesting issues arising from that meeting revolved around the training of the clergy and clerical students and how the stigma associated with suicide and mental illness must be tackled. Churches can also play an important role through their work with youth groups, scouts and guides.
Last November we visited Scotland to see what suicide strategy was in place. It was called “Choose Life” and has been in place for a few years, and it is therefore well ahead of that in Northern Ireland. We learned a number of valuable lessons from the Scottish experience. Our visit to Dublin presents an opportunity to hear from the Minister and departmental officials about the Reach Out strategy and its impact to date with a view to comparing it with the action being taken in Northern Ireland. We are aware of the considerable co-operation that exists through the joint cross-Border action plan, which exists at both ministerial and strategic levels to tackle the issues of suicide and self-harm.
One of the main issues for our committee has been examining the level of stakeholder involvement in drawing up and implementing the strategy. There are many family and community groups throughout Northern Ireland working to support vulnerable people and provide support to bereaved families. Our visit to Pieta House in Lucan was very interesting and informative and demonstrated how stakeholders are involved in the Reach Out strategy. Our committee is called the Committee for Health, Social Services and Public Safety, which covers a wide range of issues. I look forward to a fruitful discussion on some of our common issues and hope we can draw on each other’s experiences to act in areas of mutual interest, to help those who suffer and need compassion and tender loving care.
Chairman: I also welcome a fellow Ulster representative, Deputy Dinny McGinley. I will ask one member from each party to speak and will then invite members from Ms Robinson’s committee to speak.
Deputy Dan Neville: I welcome the delegation. Our previous committee visited Scotland and was impressed by the work there, where suicide rates are dropping significantly as they are in other countries. We must quash the notion that there is nothing to be done about it. That is not so. We have seen very effective suicide prevention programmes in Australia, Canada, Scotland and Finland, although the rate remains high there. From 1997 to 2002 suicide in Australia dropped by 27%.
Community involvement is significant in this area but it requires leadership because those who wish to do something do not know how to act. They fear it but could get involved if there was investment and commitment. I am sure if we asked them, the GAA, the FAI and the IRFU would embrace an invitation to help us identify issues surrounding suicide among young people and train some of their leaders, as would other groups and organisations. It is not easy to identify someone who is suicidal. While 500 suicides is too many, a GP might encounter only one every five years on average. There are 30,000 deaths a year in Ireland, of which 500 are caused by suicide. To have the fifth highest rate of youth suicide after countries from the eastern bloc, and Finland, is highly significant and serious. Will the rate drop or will it continue at that level? As the 20 and 30 year olds age, will the rate remain the same? The rate is lower in older groups.
This is not a political issue. I said at a Sinn Féin conference in September that the State has a duty to, and does, respond to the express needs of our people at election time but political parties do not respond to the unexpressed need because they see no return on that. Mental health problems and suicide are an unexpressed need but will hopefully be expressed some day. We see the outcome now of burying unexpressed needs in the 1940s and 1950s. We have a duty to respond to unexpressed needs. The Northern Ireland suicide prevention office has a budget of £3 million. Our service receives €4.5 million, whereas an equivalent fund in terms of population and the exchange rate would be €20 million.
We need to do more to respond to psychiatric illness by ensuring services are available because it is contradictory to alert people to use services that do not exist but we must alert people in order to de-stigmatise the problem. Only then will people feel free to ask me to help their son or daughter who has been waiting four years for psychiatric intervention. We do not hear that at election time or any other time because of the stigma surrounding the problem.
We must also, however, be careful about how the media handle the issue. There are common media guidelines here and in Northern Ireland. I am involved with the Irish Association of Suicidology which is a 32-county organisation. We and the Samaritans have strict media guidelines but the press often does not adhere to these and sensationalises suicide. In Wexford, for example, there was a serious problem and the media showed coffins, families, grief, etc. Several suicides followed and we are always concerned about the copycat issue. The media must discuss suicide. Without its intervention we will not be able to communicate the difficulties or the need, or to tell young people that it is alright not to be alright and to seek help. Many young people suffer minor depression without recognising it. They go on a drinking binge and the problem becomes chronic for a time. That is a serious situation. Education and investment are needed.
The current service in this area is inadequate. Most of the recommendations made in July 2006 were ignored. A total of 96 minor recommendations of Reach Out have been introduced. The first report was published in 1999 containing 82 recommendations, of which only 10% were introduced before there was another Reach Out, which contained most of the recommendations of the 1999 report. Failure to get a political response or of the will to do something is frustrating.
Even today, on the Order of Business in the Dáil, the Tánaiste referred to massive advancements in mental health care in the past 20 years. They did not happen. Patients are still being treated in a hospital built in the 1840s. According to the 1984 report, they should have been gone by 1990. Perhaps these meetings and reports help, but one must invest in resources to change things and put in community-based multidisciplinary teams, as recommended in the 1984 report, that do not exist anywhere in Ireland. Child and adolescent psychiatry is in its infancy here, with only 20 beds. I know a woman who has a 13 year old child who has been in a hospital ward for nine months with patients aged between 50 and 80. We have a great deal of work to do.
My association has significant co-operation with people in Northern Ireland. Roy McClelland, professor of mental health at Queen’s University, Belfast, was chairman of the Irish Association of Suicidology. We look forward to working with the delegation over the years.
Ms Michelle O’Neill, MLA: As many members said, we are a small island and we have much to learn from each other. Health inequality knows no boundaries. It is an issue that needs to be tackled on an all-Ireland basis. This morning, we visited Pieta House, a shining example of good community and voluntary work on the ground. If any strategy is going to be successful, it is vital it has community grassroots involvement. Do members believe there is enough tie-in with voluntary community groups on this issue? Do families fit into the whole analysis of the strategy?
Deputy Caoimhghín Ó Caoláin: On behalf of the Sinn Féin Members, both in the Dáil and the Seanad, I warmly welcome Ms Robinson and the full team from the Assembly. This meeting of the two committees is an important and historic opportunity. It is appropriate to address an issue that knows no political boundaries which we all recognise as an urgent and pressing matter for collective address. Only collectively can we hope to impact on it in any appreciable way.
The report of the former committee entitled, The High Level of Suicide in Irish Society, was referred to by other speakers. It contained one damning statement on the reality of how suicide is addressed in this State. It stated, “The provision of mental health services for adolescents is high on aspiration but low on action”.
Deputy Caoimhghín Ó Caoláin: I was the Deputy referred to by Deputy Neville who raised this matter with the Tánaiste and Minister for Finance on today’s the Order of Business. It was against the backdrop of this week’s announcement by child and adolescent psychiatric services in counties Cavan and Monaghan advising GPs that, because of the under-resourcing of the service, they will only be able to take emergency referrals for at least the next four months, when it will be reviewed.
Given the population base of the area we need a multidisciplinary team of 22, with three secretaries. Instead, we have 6.5 whole time equivalent posts in place. They cannot cope.
The delegation will later meet with the Minister of State at the Department of Health and Children, Deputy Devins. As an Opposition voice on health and children, I recognise that the Government’s stated policy, and one which we have all signed up for, A Vision for Change, is a worthy document. However, the important issue is the manner in which it is worked out in the delivery and resourcing of services. Implementation of the policy is where the real failures are occurring.
This morning we attended a briefing by Bodywhys on the area of child and adolescent eating disorders. If young people are going to have important interventions, then it is hugely important they begin at the earliest opportunity. Self help starts with the GP and the psychiatric services. We have a situation in Cavan-Monaghan where the GPs cannot refer cases except in the most serious situations. Early intervention is suspended.
We need to be honest with each other about the realities with which we are contending. The last health committee spelt it out in clear terms. Deputy Neville referred to attending the conference hosted by my colleague, Gerry Adams, in Stormont last year which he addressed. People of all opinions attended it. I commend Deputy Neville for his role as president of the Irish Association of Suicidology. Michael McGimpsey, the Minister for Health, Social Services and Public Safety, addressed it too and his contribution was equally welcome and important. Out of the meeting came a shared hope and intent to move forward. We need to find the mechanism by which we can do this in a practical way. I hope today’s engagement will offer such a vehicle.
I was a member of the now defunct North Eastern Health Board for several years. It was one of those health authorities involved in North-South co-operation on a mental health project - CAWT - for 12 years. One of the areas addressed in common with North-South co-operation was information on suicide prevention. It did not present itself in any great in-depth way but it was the publication of an information brochure for distribution North and South that had a common message clearly understood and appropriate. We need to build on that in real and practical areas of co-operation in order to get the statistics down.
Regarding Deputy Neville’s point about the numbers of people who have died from suicide - or as Senator Mary White said, from known suicides - it raises the question as to what is the real figure. On the point about the number in proportion to the overall death rate, I do not believe that is the ratio we need. All suicides must be viewed at least as potentially avoidable deaths. That is the big distinction.
We need to act urgently. This problem is not confined to our island. We need to know it is contagious and epidemic. We do not want to see a scenario occur similar to the recent tragic situation that has arisen in Bridgend on the neighbouring island.
Chairman: I do not wish to curtail debate but I remind members we have only ten minutes remaining.
Reverend Dr. Robert Coulter, MLA: I thank the committee for hosting us. I believe this is the beginning of something which will be of benefit to all of us. So far as I am concerned, suicide prevention is above all politics of whatever shade. This is something that is vital for our communities. If we have any love for our communities at all, we must make every effort to join together in producing a system that will be of benefit and reduce the number of suicides in our land.
While I endorse and support all that has been said this morning, there is one aspect which has not been touched on. Going back to my earlier life in the church, it is the aspect of families in which there has been a suicide. I have found there is a lingering sense of guilt. While we are putting all our effort into preventing suicide, I feel we must take on board that siblings, the wider family and in particular mothers, suffer. I urge the committee to examine that aspect of the situation and in the round we can achieve something that is worthwhile for our communities.
Deputy Rory O’Hanlon: Like everyone else, I welcome our parliamentary colleagues from Northern Ireland. It is a subject important to all of us on the island.
When Reverend Coulter referred to the church, I was reminded of when I was young that people were afraid of what happened after life which was enough to ensure many people never contemplated suicide. It was rare when I was young. Of those who commit suicide 55% die at the first attempt. I believe that if those who survive that first attempt received help the majority of them would not make another attempt. I have spoken to people who have attempted suicide. One medical colleague in the west of Ireland actually bought a rope. He heard one of his children cry, went into the room to attend to the child and thereafter never attempted it.
I do not want to go over everything that was said because I can identify with the views expressed by all the speakers. However, I want to touch on something Deputy Dan Neville said concerning the question of community and what can be done in that regard. One of the difficulties is that regardless of how good the statutory services are, it is very hard to make contact with them 24 hours a day - and that applies to any statutory service. The fact that defibrillators are being dispersed throughout the country and that community groups are learning to use them is a recognition that no matter how good the State services are, they cannot be everywhere when they are needed. The question of communication within families is very important, where young people with problems can speak to a parent. Teachers, the primary care services, the medical profession, nurses, anyone in the community, can have a role to play in this regard, including the Garda and prison officers because, unfortunately some of these people find themselves in trouble with the law. It is a question of ensuring all have sufficient training in identifying those at risk.
Health promotion should be part of every activity in the community because 50% of illness is self-induced, one way or another. I always recommend to youth groups that they should spend five minutes a month at their meetings discussing some aspect of health promotion. I believe positive mental health is something that is very important and should be part of the school curriculum. It should be pursued by all voluntary sporting and community groups, including the GAA, FAI and IRFU. They should all involve themselves so that communities are better aware of the people who are likely to commit suicide. Again, the people likely to commit suicide will not seek the help of services. They need to talk to somebody who will advise and encourage them to go. I believe this is an area to be explored, apart from the psychiatric and support services at statutory level.
With regard to my colleagues in the north east to whom Deputy Ó Caoláin referred, I have no doubt that if somebody needs a service, irrespective of what level, he or she will find a way of circumventing whatever new rules are brought in by the psychiatric service, and that people will not be left to suffer.
Ms Carmel Hanna, MLA: I take this opportunity to say how pleased I am to be here today. It is very important that we share knowledge and learn from each other, particularly in the area of mental health and suicide. I want to say a few words about the Bamford Review of Mental Health and Learning Disability in Northern Ireland, RMHLDNI. Some of the committee will know Professor Roy McClelland who took over the chairmanship of the review. Our committee has spent much time considering the review. We now have the resources, at least to get us up and running and hopefully implement the review’s recommendations. Even with so much fair wind behind us it is an enormous challenge because we are coming from so far behind, in terms of getting things up and running, figuring out the building blocks and working from small pieces.
It should be borne in mind that the whole mental health area is like looking at a map and it is difficult to know where to start. It is important to start on the ground, however, and listen to people. We know this from going out and about in the community and meeting people who have been bereaved. We must first listen to them and realise how important it is for them to talk.
Many of the professionals refer to the importance of the talking therapies. That area is not very developed with us. Deputy Dan Neville mentioned Australia and the need to learn from other places. Sweden is another country where the suicide rate is very low, and one must wonder why.
The changing community values and family structures must also be considered. These questions are part of the wider issue for all of us. Even when Professor McClelland talks about Bamford, he emphasises the importance of the reskilling in team working, a totally different approach in terms of working with the community. The big issue for us is co-ordinating and integrating the statutory, voluntary and community resources, so that they all work together. That seems to be the key.
We are working on some aspects of this problem but it is very difficult to link up all the effort involved, particularly community support. There are so many areas at the community level where people so want to get involved, but leadership is needed to ensure that the resources are complementary, achieving positive outcomes and that there is good value for money as well. Much of this will depend on training and there is much talk about assistance training at different levels. A great deal of work needs to be done towards ensuring that where communities are involved, their efforts are linked into the voluntary and statutory agencies, if positive outcomes are to be achieved and to make a difference. It will make a difference when we see the suicide and self-harm numbers going down.
The statistics for suicide are very high among older people. I am talking about people my own age, say, the over 60s, and those living in rural areas.
Deputy Margaret Conlon: I, too, welcome the delegation from the Northern Ireland Assembly. As somebody who was involved in education, I believe this has a significant role to play, particularly in the whole area of health promotion. I would be interested in getting details from the delegation, not necessarily today, about the programmes that are being used in Northern schools from which we might be able to learn. In the north east many of the second level schools are involved in the “Mind yourself” programme, which is very worthwhile for transition year students. It is a ten-week programme, where students look at health promotion and developing strategies towards positive mental health, which is enormously important. It is an unfortunate but sad fact of life that because of altered family structures and the major changes in society, young people often find themselves stressed out and under pressure and believe they have nobody to turn to.
Another initiative in which we were involved was a mentoring system, where senior students counselled their junior colleagues, particularly in first year, where many children who formerly attended, say, a two teacher primary school, would now find themselves at second level and in a year group of 100 or 120. From an educational viewpoint, it is very important that this good work continues, but we need to expand it. In our situation here the social, personal and health education, SPHE, programme is only in place up to junior certificate. We need to look at something for senior students, because they equally face pressures, if not added ones, and they need to be able to deal with them and cope with entry into the world of work and a changing world, where life is not as structured as it is at school and where the difficulties and challenges are increasing with every passing day.
As all members have said, the challenge facing us knows no boundaries. All of us have much to learn and I should be interested in any documentation members of the delegation might have or can forward to me with regard to the educational programmes they are using.
Dr. Kieran Deeny, MLA: Thank you, Chairman. I am delighted to be here. I am in politics because I am a doctor and it is like coming back to where it all started, because I qualified up the road in UCD in 1980. I am still a practising GP and am learning about this issue in my professional job, and not just as a member of a health committee that is very committed to mental health. I was delighted to hear Deputy Neville speak about community and about how we need leadership. In our own committee, we discussed how this is a societal problem. In recent years there were two very tragic suicides in our own practice, involving young people who were not clinically depressed. We were often asked why the depression was not picked up, but both events came from a relationship breakdown.
For a long time suicide has been seen primarily as a mental health issue, to be picked up and dealt with by medical professionals. However, we have seen that is not the case. There is a very dangerous period following a relationship breakdown or a bout of alcoholic excess, when the health services will not get to these people in time. Deputy O’Sullivan correctly pointed out that the old-fashioned method of seeing a GP and being referred to a waiting list is just not acceptable.
I was very impressed with this morning’s visit to Pieta House. The witnesses talked about how they deal with each of the patients on the physical, emotional and spiritual levels. The setting was not in the old style psychiatric hospital outpatient department, which is a very threatening and unwelcome situation. Patients have told me in the past that they were often worse coming out of such a setting than they were going in. In this case, we had a very welcoming setting.
References were also made to problems being solution centred, which is important. Rather than just listening to people, we need to be able to find solutions to their problems. Some of these problems have been mentioned already, such as the life events that occurred to people who were not clinically depressed but who could not cope. The question is about how to get to them during this very dangerous period. Talking therapy is very important and we need to have a system in both our countries where we can pick these vulnerable people up at that particular time.
I worked in an out-of-hours centre in my own area for a while, and we involved a community psychiatric nurse with us, so we could have psychiatric backup 24 hours a day. The issue is about getting to those people. If they need further psychotherapy or any other help with their health, then that can be arranged. However, it is about carrying them through a dangerous period after a certain life event with which they cannot cope. The first thing we often hear is that they have ended their life. I have certainly learned a lot from today and I hope to learn more.
Deputy Catherine Byrne: I think the Reverend put his finger on the button when he said it was about family, community and church. It is not about the colour of our party or the colour of our skin, but about human beings. Prior to being elected to the Dáil last year, I was involved in youth work for a long time. We could actually pinpoint some young children as being those who were never going to reach their 20th birthday. Unfortunately, many of them passed on, often through suicide and drug addiction.
Ms Robinson correctly pointed out that it is about small projects in communities that are accessible on the ground. This is particularly the case with voluntary youth work in situations where a young person might be on the edge on any given evening, but there is nothing out there. That was certainly the case 30 years ago, but it has improved a little since. There is a project in England called YAP, or Young Action Project. There is one similar project in Ireland, but there are quite a few of them in England. These projects bring in the most vulnerable people in the community. They have a beginning, middle and end and when they leave after a couple of weeks they are different people. I have met some of them who participated in the project we have in Ireland. It is a very positive way to change young people’s lives and it gives them a new identification with who they are and where they are going.
I welcome this morning’s meeting. As someone who is still involved in the local community, I feel that suicide must be tackled at grassroots level. Much suicide is due to people living in very deprived areas with very poor social housing and a lack of early intervention in education. I am here in place of Deputy James Reilly, whose answers may have been more eloquent than mine.
Chairman: Not at all. We all welcome Deputy Byrne’s contribution. Before we finish, I would also like to say a word of thanks. The last committee published its report only two or three years ago. The 33 recommendations within that report should be borne in mind, because it is clearly nonsense for people to talk about an old report when it is far from that. I was delighted to chair that committee and was ably assisted by my colleagues from this committee.
One very important aspect was touched upon by Ms O’Neill, namely, the involvement of the community. Every group that comes before our committee wants to do something about the problem, but they always feel that it is not targeted properly and that is where our problems begin. Of all the issues that came out of the report, one simple target is that we should be able to reduce the incidence of suicide in this State by 20%. That is the most important target. It might be unrealistic but I am delighted to see that Deputy Neville is saying that is not the case. However, the report stated that we could achieve that figure if we adopted a targeted approach, as has been done in Scotland and has been the root cause of success there.
I noted from Ms Robinson’s contribution that her committee’s report will be ready by Easter. I am delighted to hear that her committee has had 65 submissions. We had a similar number of submissions from professionals and families involved. I do not know the protocol for my suggestion, but I would like to see a situation arise where three members of this committee could sit with three members of Ms Robinson’s committee after her report is published. We could see whether our recommendations are similar to the recommendations in her report. If they are similar, then what we are about on this island would be all the one. It is important to see if that is the case.
I thank the committee members from Northern Ireland for attending. We have all made our contributions and we recognise that there are other issues as well, such as waiting lists, accident and emergency departments, MRSA and so on. These issues have clearly affected both sides of the island. We would like to meet with Ms Robinson’s committee on a more regular basis. I will not even say that we are postponing our next meeting, but rather that we are adjourning until the next meeting.
Senator Frances Fitzgerald thanked me for organising this meeting, but as we know Ms Áine Breathnach and her staff are the people who do all of the work. We feel that we can learn a lot from our counterparts on the Northern Ireland committee and I am sure they can learn from us as well. We hope that we can get together informally to work out how we get together more often, how we organise specific agendas and hopefully each year report back to this committee on what we have achieved and the targets we are setting.
It is important to believe that we can reduce the incidence of suicide. It is up to us to put the methods in place. If we are seen to work together on this specific issue, I am certain it will give hope to many on the island that people are getting together to recognise the great difficulties that exist. I will allow Senator Mary White to speak before we finish. I will then call on the chairperson to wind up the meeting.
Senator Mary M. White: The National Office for Suicide Prevention has set a of target of a 10% reduction by 2010, so it will be interesting to see what happens. It is a short time away but it is important it has agreed to set that target.
I have organised a conference on suicide prevention for Friday and Saturday of this week. Among the speakers will be Deputy Dan Neville. As noted by Reverend Coulter, this issue is beyond party affiliation. The National Office for Suicide Prevention and the North Clondalkin Action Group Against Suicide, a local community group in west Dublin which came together because of the suicides in its area, will speak tomorrow night. I will provide the witnesses with a programme.
Chairman: It is my pleasure to invite the chairperson, Ms Robinson, to wrap up the meeting.
Ms Iris Robinson, MLA: I thank everyone who has contributed. As the Chairman says, this is only the beginning and we will learn much from one another. We must always bear in mind that life is precious and we must value it. The targets are aimed at turning people away from death. We must remember that targets are human beings. It is about turning them around from thinking that life is not worth living to valuing life. The three areas pinpointed by the Pieta organisation, the physical, the emotional and the spiritual, are what we need to examine, along with community involvement.
I thank the committee for the opportunity to meet with it and look forward to a more informal gathering at lunch. I would be very disappointed if, having produced this document, little of it is run with. I hope that when we get to the point of preparing our report to give to our health Minister, we will not be sitting back - I do not mean this committee is doing so - or accepting a small percentage of rollout of any suggestions we will make. We will certainly sit on our Minister’s case and watch vigilantly to ensure whatever recommendations we make will be enacted for the good of all the people of Northern Ireland. That is the approach we would all take.
There is goodwill out there to make progress on mental health and all the related issues around it, such as anorexia and bullying, which can trigger so many people into thinking the only way out is to take their lives. I hope we can all make a difference in the end in terms of the proposals we will bring forward after Easter.
I thank the Chairman. Before I finish, I wish to make a small presentation on behalf of the Northern Ireland Assembly. It is a beautiful print of our Assembly. It gives me great pleasure on behalf of the committee to present it to the Chairman.
Chairman: I thank Ms Robinson. It is much appreciated.
The joint committee adjourned at 1.15 p.m. until 3 p.m. on Tuesday, 26 February 2008.
Briefing for Northern Ireland Assembly Health Committee - meeting with Minister Devins on Thursday 21 February 2008
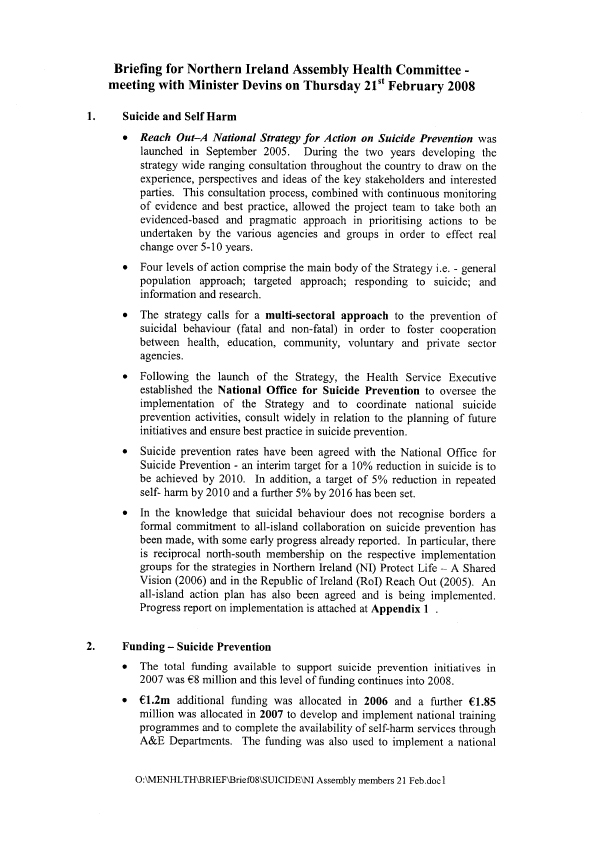
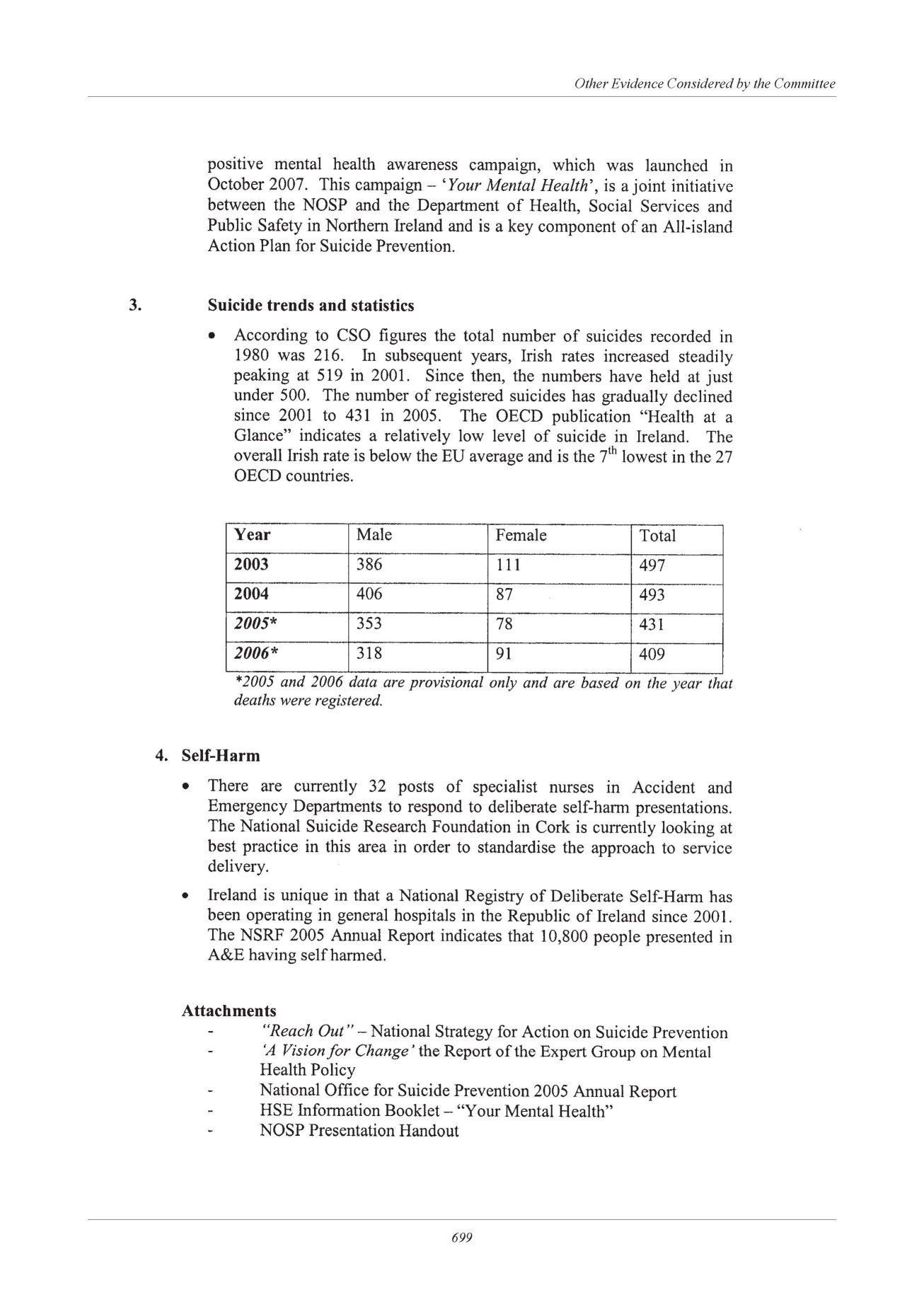
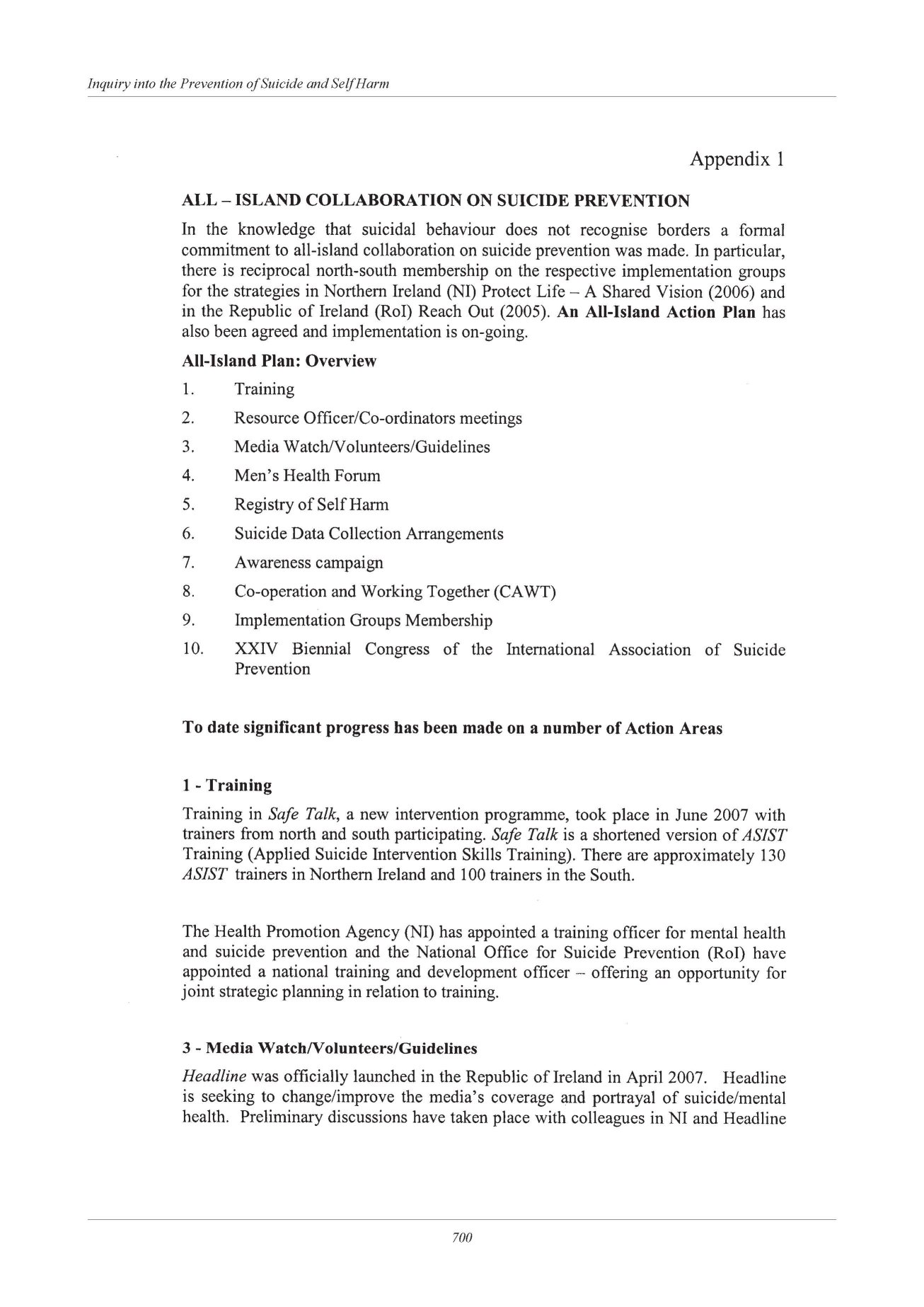
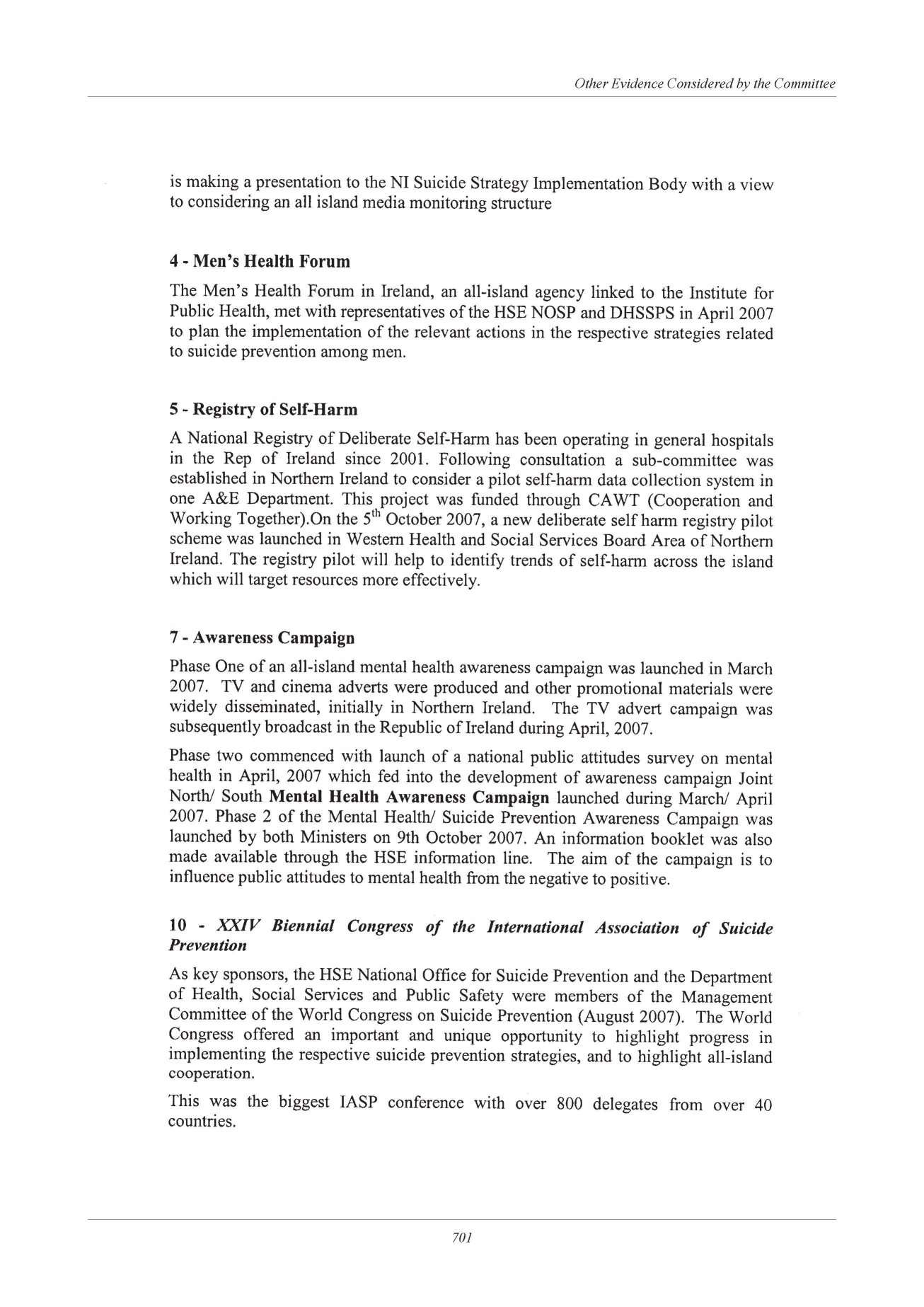

HSE National Office for Suicide Prevention
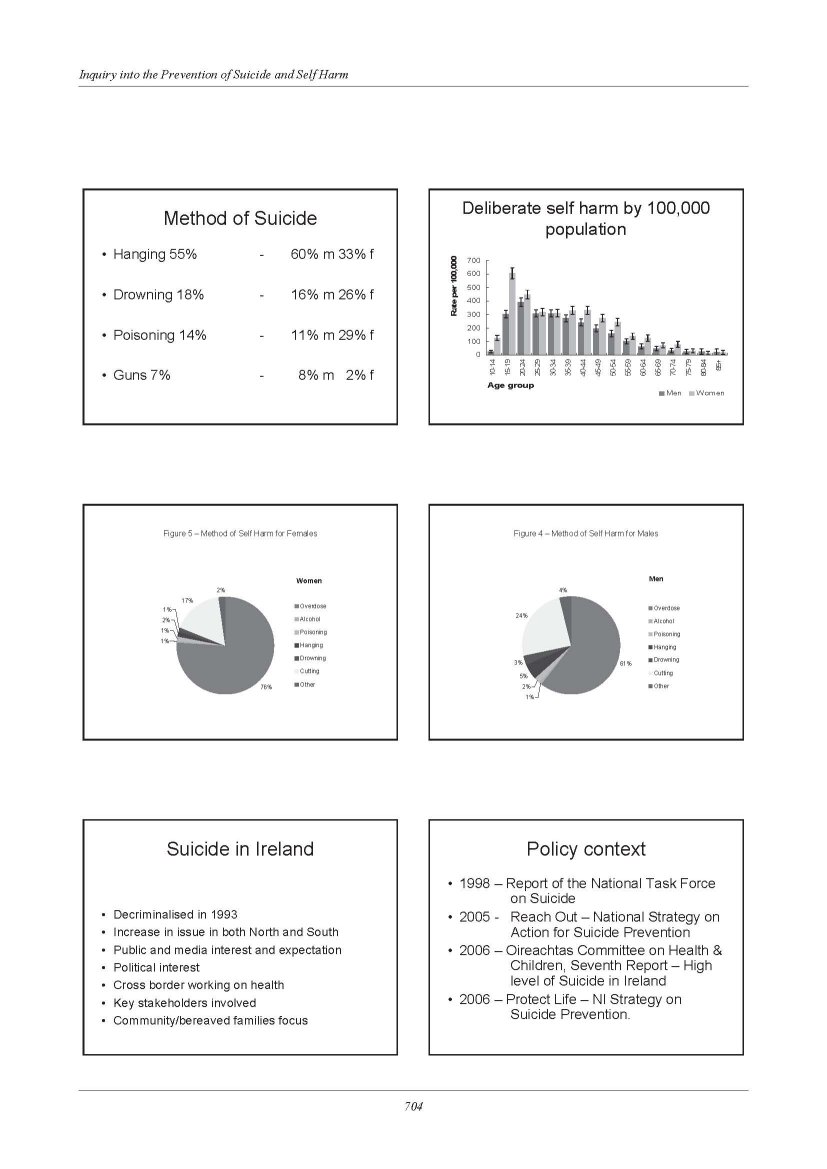
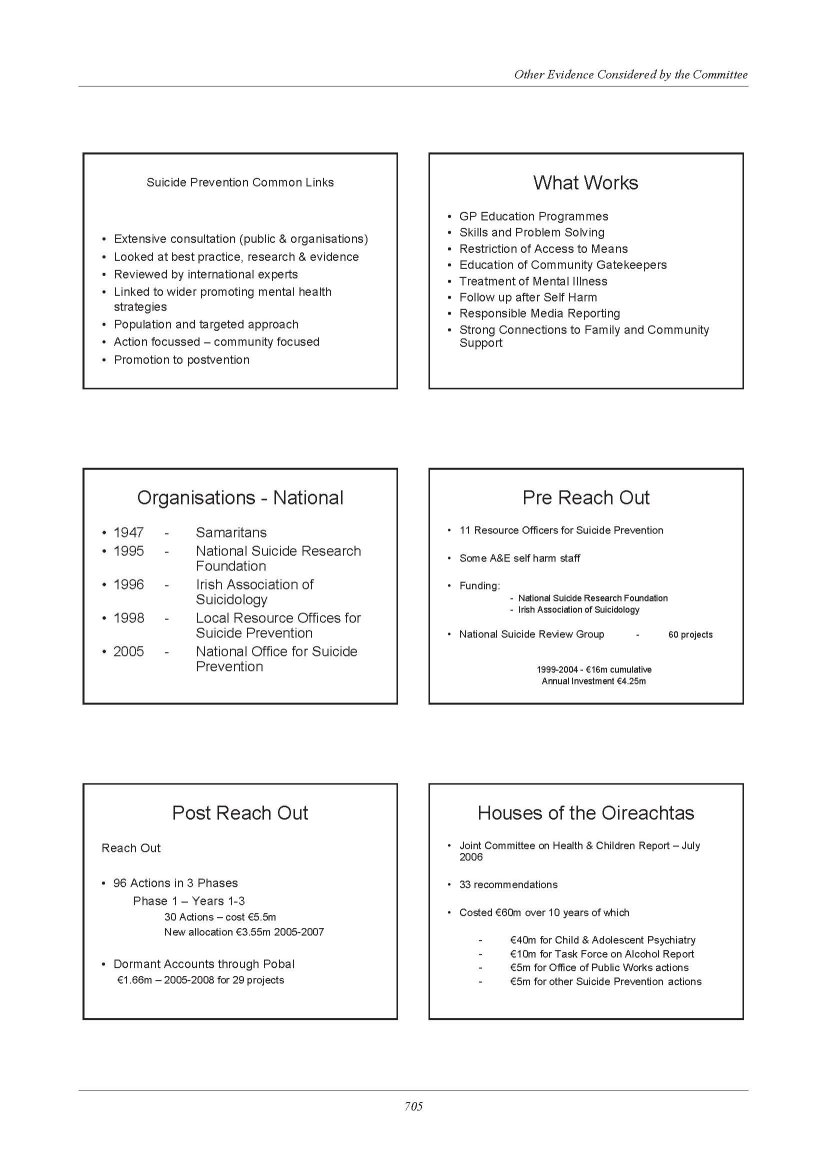
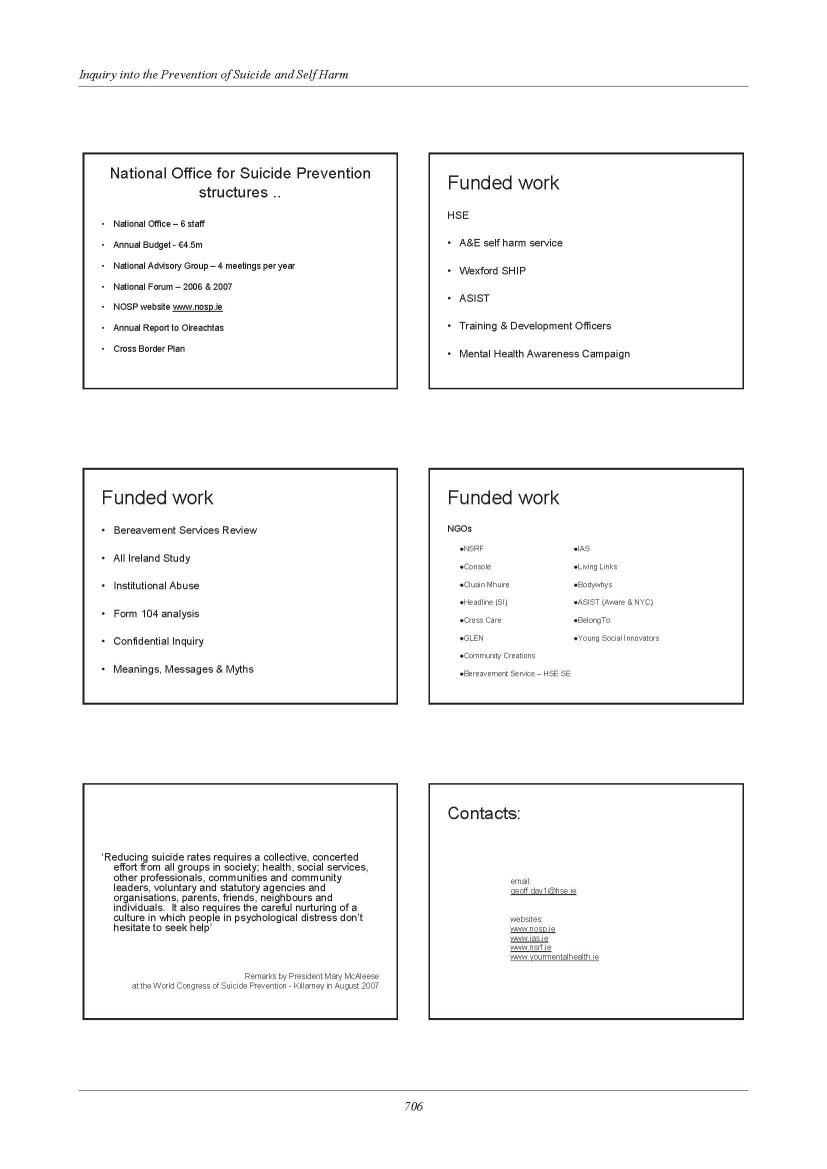
Belfast Health & Social Care Trust
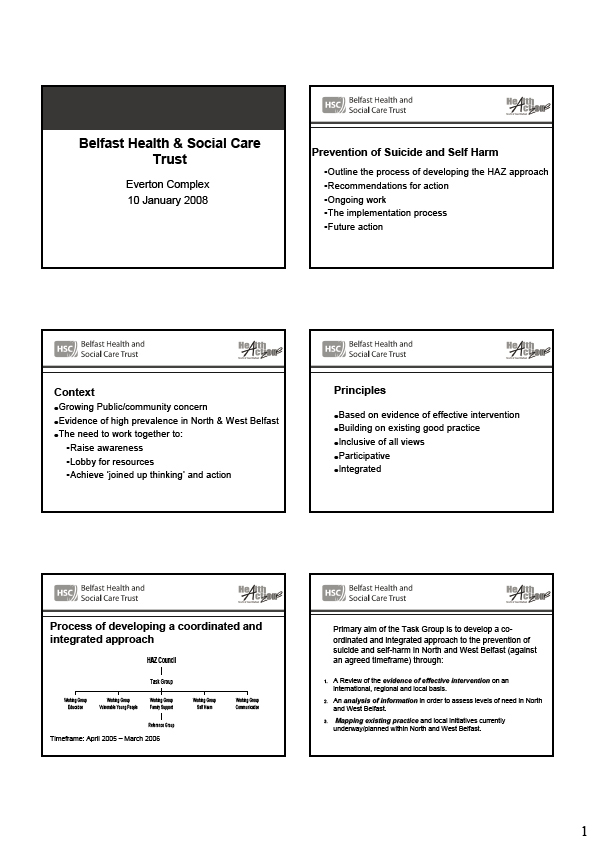
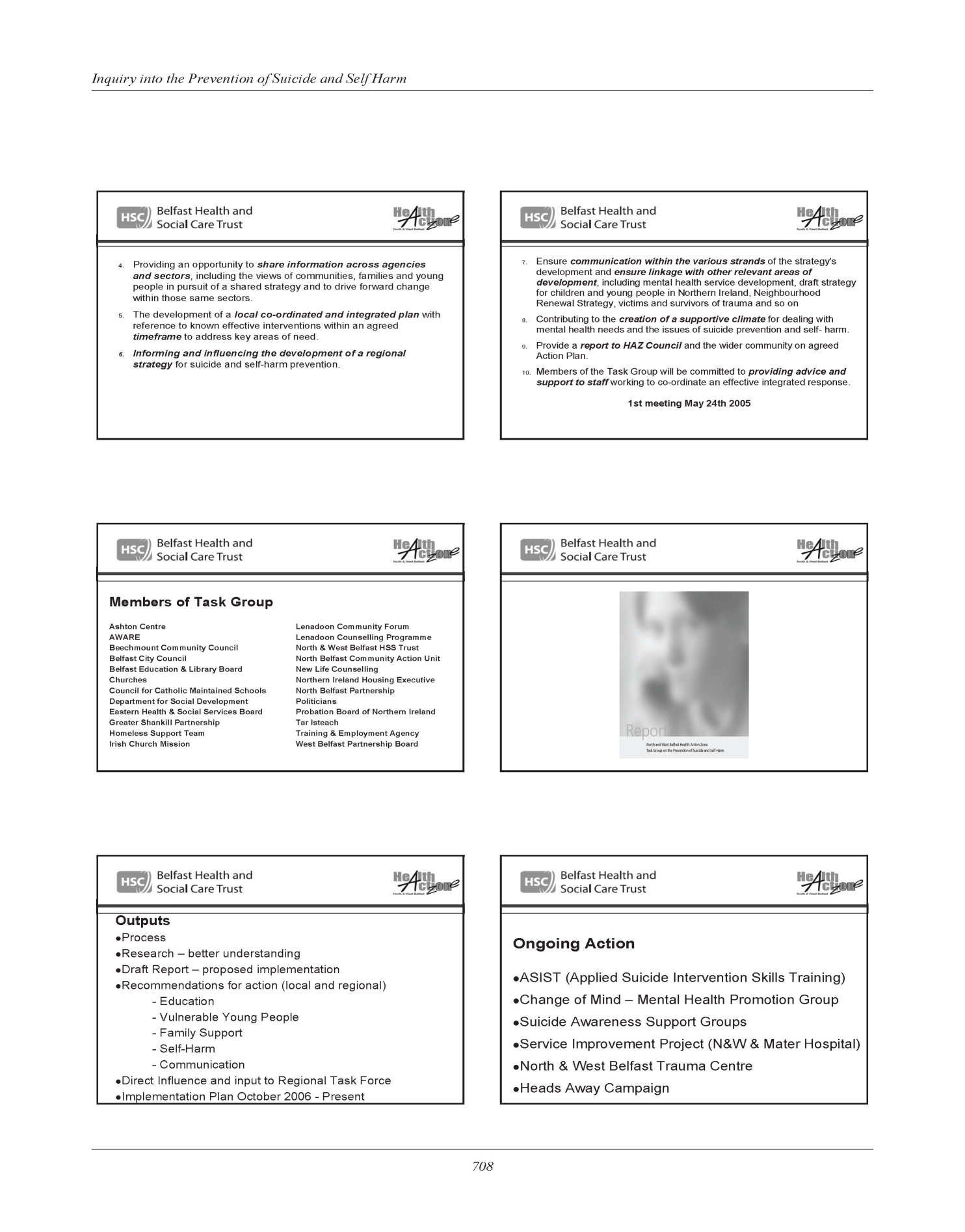
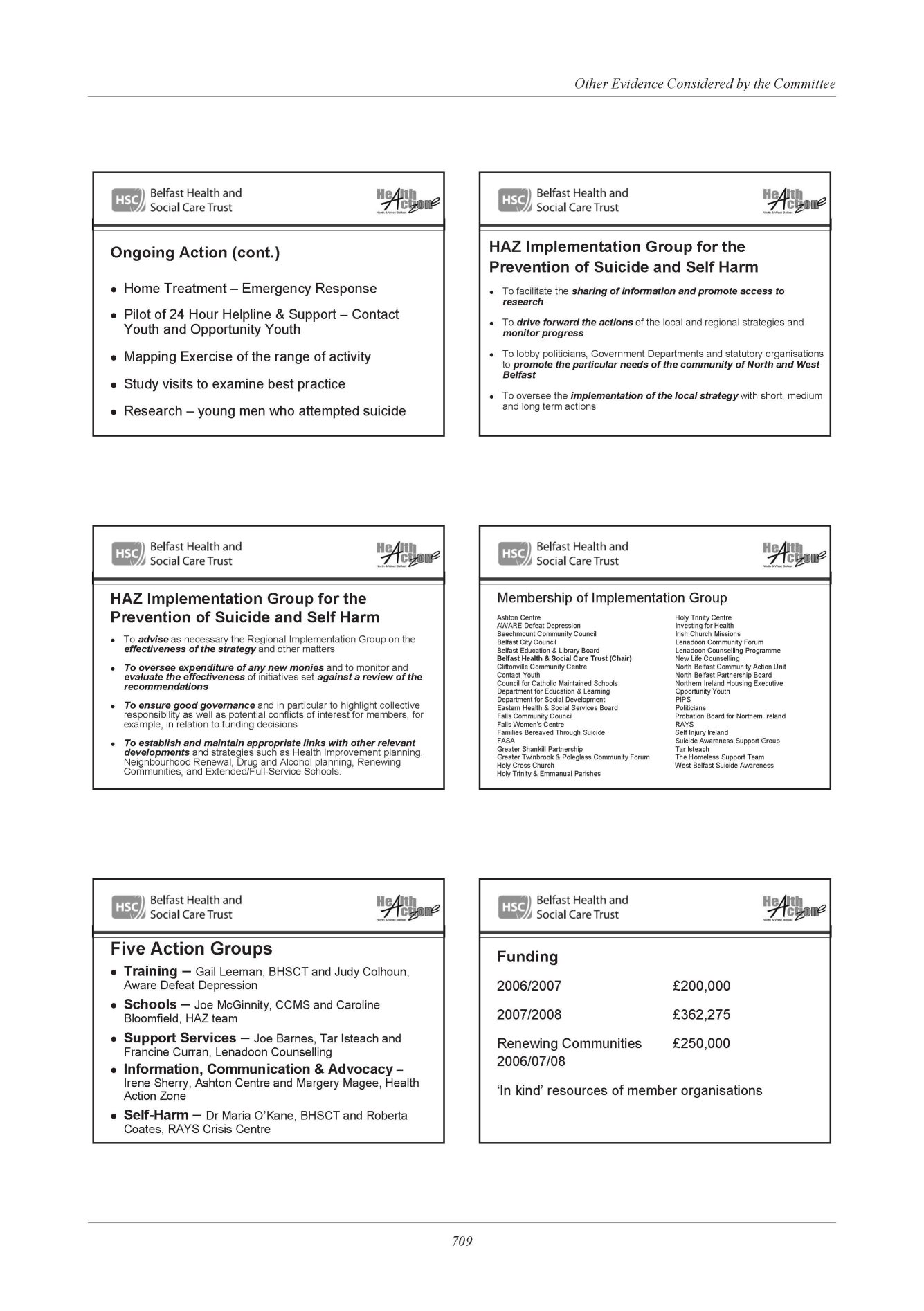
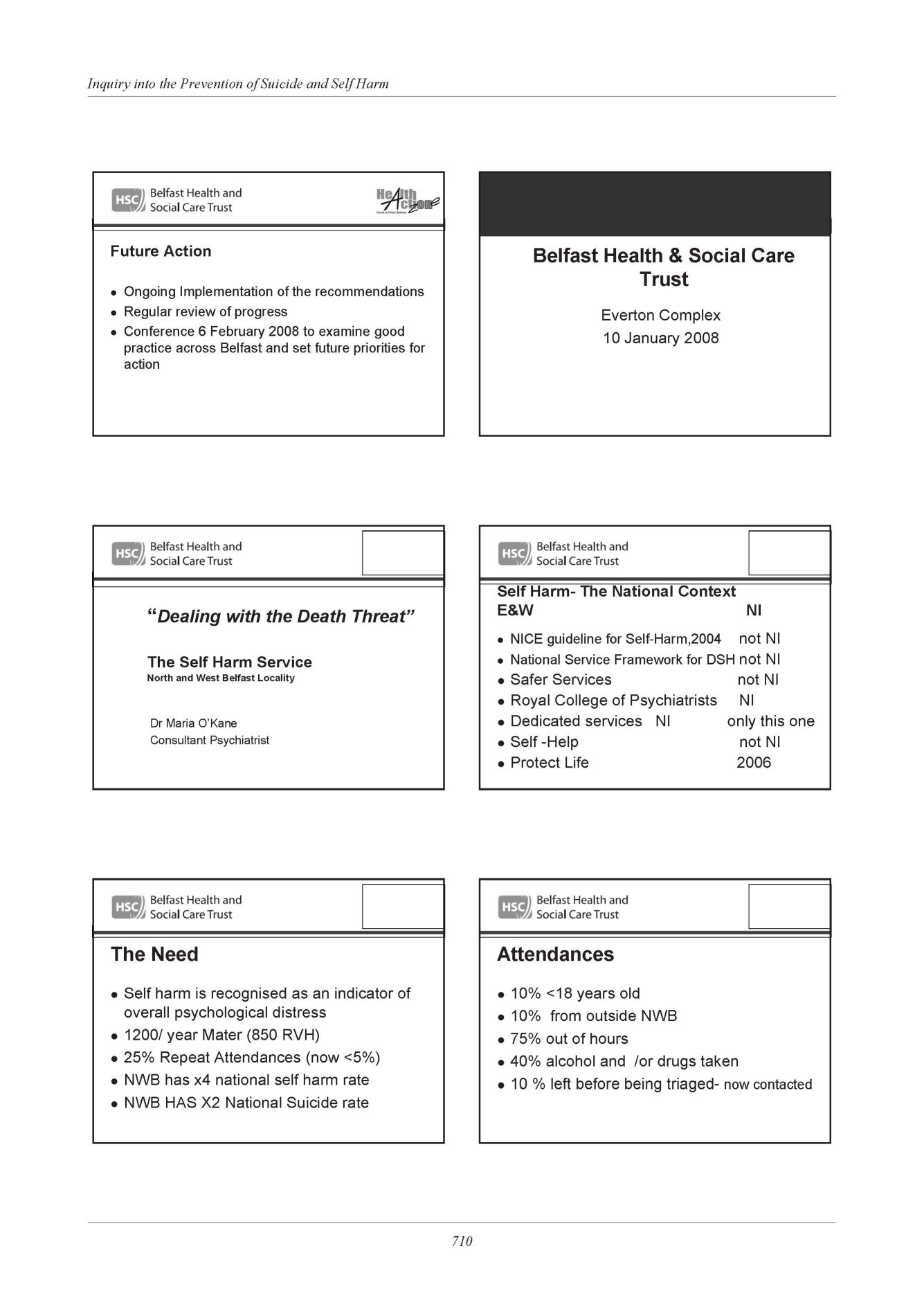
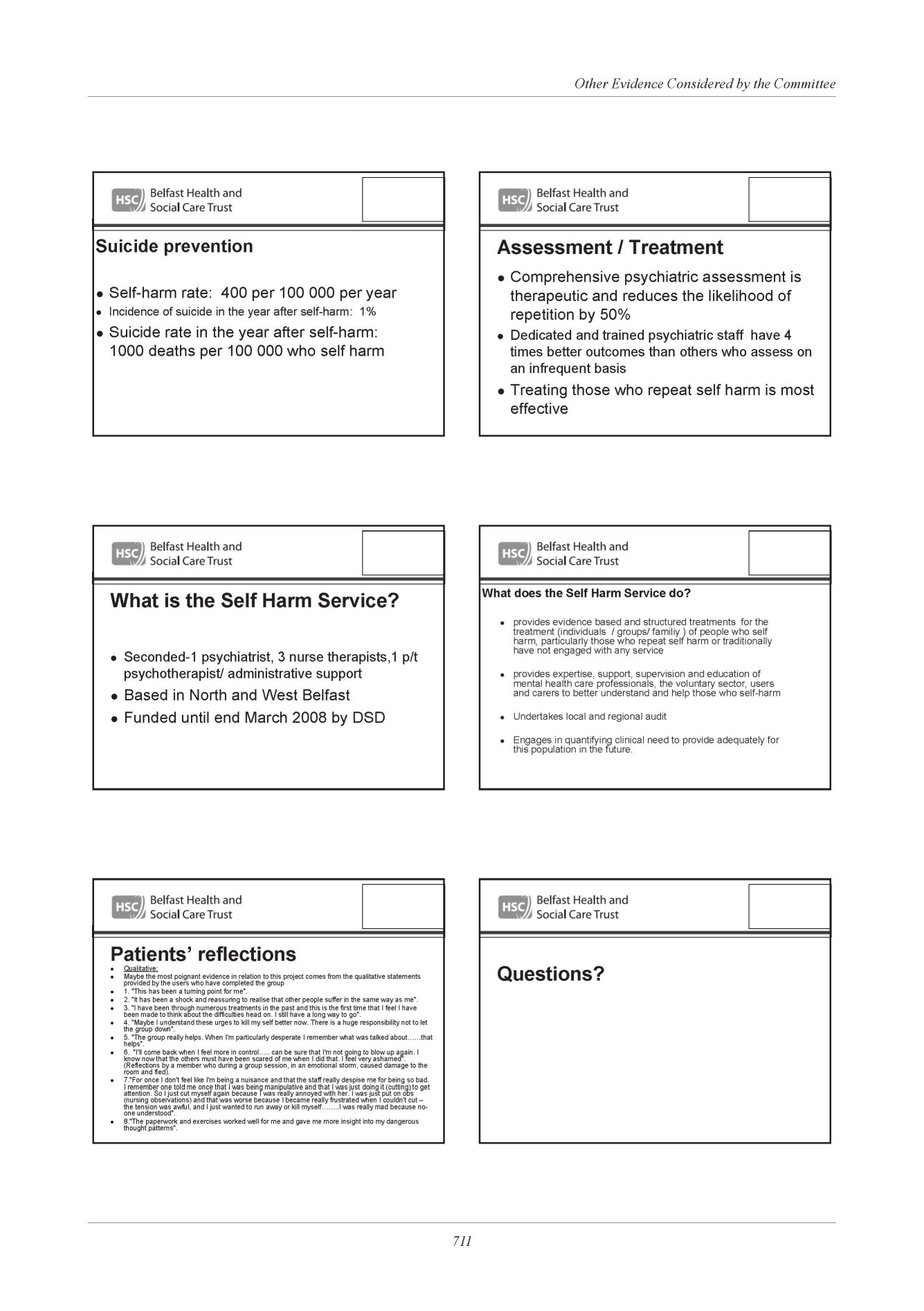
Sport NI
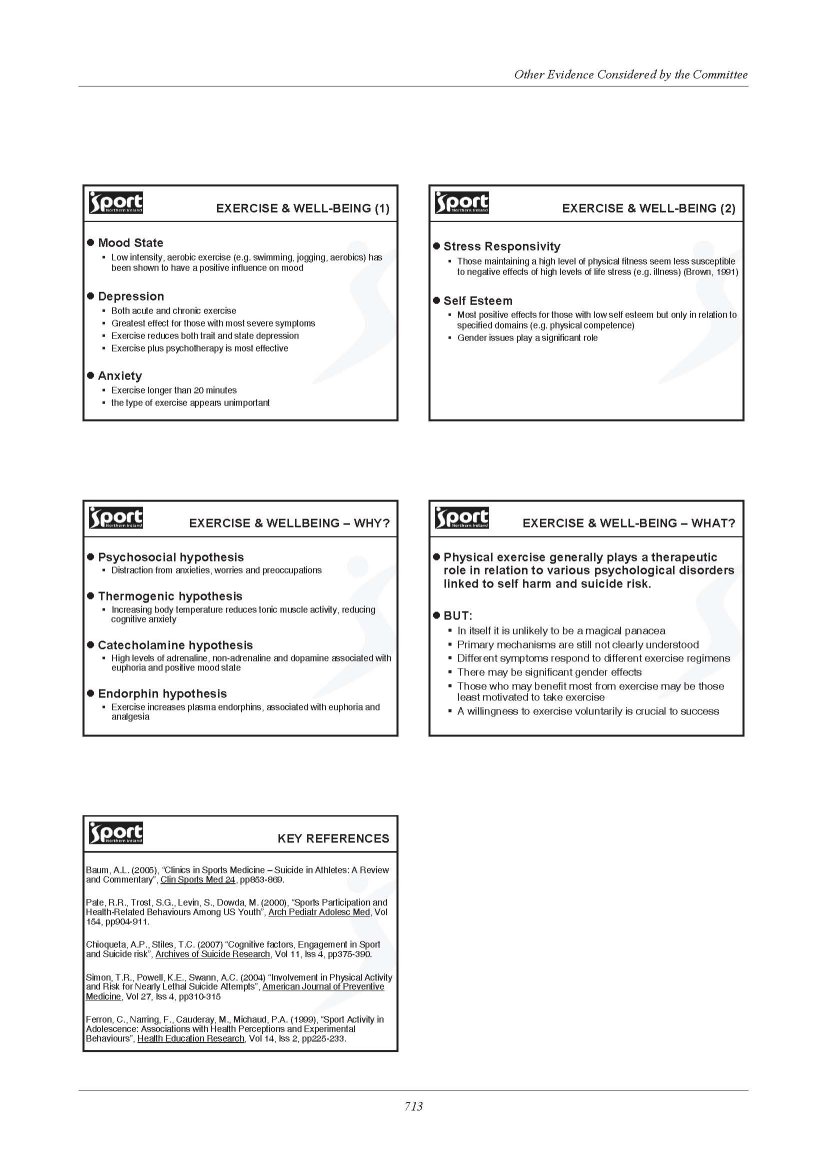
Southern Health and Social Care Trust
Protect Life Suicide Implementation Group
1. Purpose of Paper
The purpose of this paper is to consider the way forward for the Southern Trust Protect Life Implementation Group (PLIG) in relation to its ability to engage and represent the views of local stakeholder interests across the Southern area. The paper will consider membership and representation and the development of mechanisms to ensure effective communication and networking across a wide base of interested groups and organisations.
2. Context
The Southern Trust PLIG has recently been established in response to the Northern Ireland Suicide Prevention and Action Plan 2006 – 2011 - “Protect Life A Shared Vision.” Its purpose is to develop a common framework for action across community, statutory, voluntary and private sector partners that will result in a more co-ordinated and integrated approach to long term, sustainable action targeted at reducing the incidence of suicide across the Southern area.
The Aims of the PLIG are therefore to:
- Ensure the implementation of the recommendations of the Protect Life Suicide Prevention Strategy and Action Plan 2006 – 2011 within the Southern Trust area;
- Develop a comprehensive Action Plan that will address the Aims, Objectives and Actions of the “Protect Life” Strategy and that reflect the core values and corporate objectives of the Trust and its partners and the needs and priorities of communities across the Southern Trust area;
- Develop a monitoring and evaluation framework;
- Ensure the involvement of all stakeholders in the planning, implementation and monitoring process with a particular emphasis on the community/voluntary sectors.
The outworking of these Aims will be realised through a number of Key Tasks which further define the work of the PLIG. These are detailed in Appendix 1.
In establishing the PLIG it was not the intention of the Trust to substitute or duplicate the existing structures or work of community and agency partners but rather to facilitate and support specific actions that can best be addressed by organisations, groups and communities working together at local level.
In light of the significant and potentially growing interest in this issue the PLIG is therefore seeking to maximize its ability to engage, communicate and coordinate action across all stakeholders within the Southern Trust area.
3. Membership and Engagement
The current membership of the PLIG is in excess of some 40 individuals representing a range of statutory, voluntary and community agencies. Whilst this potentially is a large group it is important that the PLIG retains the ability to engage in a meaningful way with all stakeholder interests across the Southern Trust area.
The culture of the Trust as expressed though its Core Values (Corporate Plan -2007) seeks to ensure inclusivity, openness, effective and meaningful partnership working, the full engagement of local communities and the effective and efficient use of resources that will achieve the best possible outcomes for its community.
In keeping with these values the PLIG will therefore seek to ensure it is both inclusive and representative of stakeholder interests whilst developing effective and efficient mechanisms to engage and communicate with partners and communities across the Southern Trust area. The following proposals have been made with this in mind:
(i) A core Management Group should be established that will have responsibility for ensuring the ongoing development, coordination and implementation of priorities, actions and investments across the area. It is envisaged that within this group there should be a balance between statutory and community/voluntary interests with members having a responsibility to ensure they effectively represent not just their own organisational views but also the views of others within their sphere of interest.
Membership should be representative of Community/Voluntary Partners, and Statutory Partners including PSNI, Councils, SELB and Trust. The Trust will provide Chair and Secretariat functions for the group. The group should retain the ability to co-opt and engage specific individuals from time to time to provide specialist advice, help and support to its work. It is proposed that the membership of the group should be reviewed and updated where necessary every two years.
It is recognised that there is a need to ensure close working relationships between the PLIG and the Southern Board Implementation Group. A number of those currently involved with PLIG are also involved in the Southern Board Group and it is therefore proposed that these individuals provide an appropriate mechanism for the sharing of ideas, information and direction. The Trust will also retain a management link with the Board for the development of priorities and the allocation and reporting on resource utilisation.
(ii) PLIG should establish a Stakeholder Network which will have a broad and inclusive membership representative of all those who express an interest in working collaboratively on this issue across the Southern Trust area. A key role for this network will be to assist in the identification of needs and priorities and to ensure the provision of a high level of information on service provision is maintained within communities.
It is recognised that within this group individuals may wish to engage at various levels and not necessarily on a continual basis. To this end membership should be open and accessible to all with flexibility to participate as and when individuals feel appropriate. It is also envisaged that engagement mechanisms should be developed at local level as a means of encouraging local involvement and participation.
Where possible current structures within communities and localities whether initiated by the Trust or its key partners should be utilised to engage local interests. Examples of these include the Southern Area Community and Voluntary Forum (established under SHSSB Protect Life action Plan). Where these structures do not currently exist, it will be the responsibility of the Protect Life Coordinator in conjunction with the Protect Life Community Development Workers and other local partner interests to initiate opportunities to engage with local people.
The Protect Life Community Development workers will have a particular responsibility for developing, initiating and supporting the engagement with local communities across the Southern area with direction and support from the Protect Life Coordinator. They will engage with families and local groups to provide a vehicle for them to express their interest s and concerns and to agree how best these can be addressed.
Use should also be made of the wide variety of communication mechanisms currently in existence both within the Trust and across community, statutory and voluntary partners. The Protect Life Coordinator will work to ensure that there is a high level of information and profile on the issue of suicide and self harm and the respective services that are in place to address this issue across the area. This will include the development of a regular progress bulletin which can be widely circulated and the provision of information for Trust and other partner websites.
It is anticipated that there will be a need to establish specific task groups to address emerging needs and priorities particularly at local level. Membership for these groups should be drawn from local partners and stakeholder interests. These groups will be facilitated where appropriate by the Protect Life Community Development Workers or the Coordinator and relevant partners.
Reports on the engagement of stakeholders across the Southern Trust area will be provided to the PLIG on an ongoing basis. The Protect Life Coordinator will have responsibility for the coordination of these reports in conjunction with the Community Development Workers and local partner organisations.
4. Conclusions
The Proposals as outlined above should ensure that the working of the PLIG is both effective and efficient whilst retaining an ability to be inclusive and embracing of all those interested in preventing suicide and self arm across the southern Trust area. It will be important to keep the mechanism under review and to ensure they contribute to the purpose and aims of the group.
Appendix 1
Key Tasks for the Southern Trust PLIG
In seeking to realise its purpose and aims a number of Key Tasks have been identified for the PLIG:
- Establish a strategic planning framework that will realise the outworking of the “Protect Life Strategy” within the Southern Trust area;
- Develop a shared vision and a common set of priorities that will guide investment and action across the area;
- Develop an Interagency Action Plan that will ensure actions are targeted at addressing local need and circumstances over the short, medium and long term;
- Ensure the effective co-ordination and implementation of the Action Plan across the Southern Trust area;
- Work collaboratively to maximise the current resource within partner organisations in addressing agreed targets, issues and priorities and utilise the additional resource available within the Regional Strategy to address agreed priorities and needs;
- Endorse and support the work of partners in delivering policies, strategies and programmes that will assist in realising the aims, objectives and targets of the Regional Strategy;
- Ensure a shared and co-ordinated programme of community needs assessment and data collection and analysis that will inform and shape the design, development and delivery of priorities, programmes and actions;
- Develop approaches and initiatives that will facilitate and support the engagement of communities and organisations to work together to address local agendas;
- Oversee the development and implementation of an Information and Communication Strategy to ensure a high profile is maintained of local action;
- Provide a co-ordinated approach to the monitoring, evaluation and reporting of activity across organisations and partners within the area.
Appendix 5
List of Witnesses who
Gave Oral Evidence
to the Committee
Witnesses who gave Evidence to the Committee
Mr Michael McGimpsey Minister of Health, Social Services and Public Safety
Dr Miriam McCarthy Department of Health, Social Services and Public Safety
Dr Andrew McCormick Department of Health, Social Services and Public Safety
Ms Patricia Osborne Department of Health, Social Services and Public Safety
Mr Andrew Elliot Department of Health, Social Services and Public Safety
Mr Martin Bell Department of Health, Social Services and Public Safety
Mr Gerard Collins Department of Health, Social Services and Public Safety
Dr Berne Stuart Department of Health, Social Services and Public Safety
Dr Philip McGarry Royal College of Psychiatrists
Dr Maria O’Kane Royal College of Psychiatrists
Dr Peter Gallagher Royal College of Psychiatrists
Anne Mater Hospital service user
Mr Tom Black British Medical Association in Northern Ireland
Mr Danny Lambe British Medical Association in Northern Ireland
Mr Ivor Whitten British Medical Association in Northern Ireland
Mr James McBennett Niamh Louise Foundation
Ms Catherine McBennett Niamh Louise Foundation
Ms Michelle Baird South Antrim Rural Support Network
Mr Raymond Craig Oakleaf Rural Support Network
Mr Colm Donaghy Southern Health and Social Care Trust
Mr Francis Rice Southern Health and Social Care Trust
Mr Bobby Cosgrove Families Forum
Ms Ann McGarrigle Families Forum
Ms Maureen Young Families Forum
Mrs Jean Carson West Belfast Suicide Awareness and Support
Mr Michael Doherty West Belfast Suicide Awareness and Support
Mr Vincent Donaldson West Belfast Suicide Awareness and Support
Mr Robert Doyle West Belfast Suicide Awareness and Support
Mr Séamus McCabe PIPS
Mr Gerard McCartan PIPS
Mr Phillip McTaggart PIPS
Ms Jo Murphy PIPS
Ms Roberta Coates RAYS
Ms Phyllis McDoal RAYS
Ms Marie Osbourne West Belfast Parent and Youth Support Group
Mr Colin Loughran Action Mental Health
Ms Sharon Sinclair Aware Defeat Depression
Ms Suzanne Costello Samaritans
Mr Anthony Langan Samaritans
Mr Mike Tomlinson Queen’s University
Mr Iain McGowan University of Ulster
The Most Rev Patrick Walsh The Roman Catholic Church
Dr Oliver Woods The Roman Catholic Church
Rev Roy Cooper The Methodist Church in Ireland
The Right Rev Dr John Finlay The Presbyterian Church in Ireland
Mr Lindsay Conway The Presbyterian Church in Ireland
The Most Rev Alan Harper, OBE The Church of Ireland
Rev John McClure The Church of Ireland
Mr Brendan Bonner Western Health and Social Services Board
Ms Melanie McClements Southern Health and Social Care Trust
Mr Pat McGreevy South Eastern Health and Social Care Trust
Ms Gabrielle Nellis Northern Health and Social Services Board
Dr Dermot O’Reilly Queen’s University Belfast
Mr Noel Graham Northern Health and Social Services Council
Ms Maggie Reilly, Western Health and Social Services Council
Professor Eamon McCartan Sport NI
Dr John Kremer Queen’s University Belfast
Ms Heather Moorhead NILGA
Mr Sean McPeake NILGA
Ms Anne Donaghy NILGA