Session 2007/2008
Third Report
The Committee for Health, Social Services and Public Safety
Report on the Inquiry into
the Prevention of Suicide
and Self Harm
Volume One
TOGETHER WITH THE MINUTES OF PROCEEDINGS AND MINUTES OF EVIDENCE
RELATING TO THE REPORT
Ordered by The Committee for Health, Social Services and Public Safety
to be printed 1 May 2008
Report: 27/07/08R Committee for Health, Social Services and Public Safety
PUBLISHED BY AUTHORITY OF THE NORTHERN IRELAND ASSEMBLY
BELFAST: THE STATIONERY OFFICE
£20.00
This document is available in a range of alternative formats.
For more information please contact the
Northern Ireland Assembly, Printed Paper Office,
Parliament Buildings, Stormont, Belfast, BT4 3XX
Tel: 028 9052 1078
Committee for Health, Social Services
and Public Safety
Membership and Powers
The Committee for Health, Social Services and Public Safety is a Statutory Departmental Committee established in accordance with paragraphs 8 and 9 of the Belfast Agreement, section 29 of the Northern Ireland Act 1998 and under Standing Order 46.
The Committee has power to:
- Consider and advise on Departmental budgets and annual plans in the context of the overall budget allocation;
- Consider relevant secondary legislation and take the Committee stage of primary legislation;
- Call for persons and papers;
- Initiate inquires and make reports; and
- Consider and advise on any matters brought to the Committee by the Minister for Health, Social Services and Public Safety
The Committee has 11 members including a Chairperson and Deputy Chairperson and a quorum of 5.
The membership of the Committee since 9 May 2007 has been as follows:
Mrs Iris Robinson MP (Chairperson)
Ms Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Mrs Carmel Hanna
Rev Dr Robert Coulter
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Table of Contents
Volume One
- Introduction
- Background
Suicide
Self Harm - Trends
Northern Ireland
International Comparison
Self Harm - Strategic Approach to Suicide Prevention
Implementation Structure
Evaluation and Review
Funding
Targets - Stakeholder Involvement
Development of the Strategy
Ongoing involvement through SSIB
Families and Community Groups
Cross-Departmental Role
Role of Schools and Colleges
Role of Churches
Role of Sport and Exercise
Role of Local Authorities - Services and Support
Training
ASIST Training
Training for clergy and church workers
Training for PSNI
Telephone Helpline
Self Harm Service
Talking Therapies - Experience Elsewhere
- Other Issues
Role of Media
Public Information Campaign
Chill Out Room
Card Before you Leave
Communication
Support for Frontline Staff - Conclusion
Appendix 1:
Minutes of ProceedingsAppendix 2:
Minutes of EvidenceVolume Two
Appendix 3
Written Submissions
Appendix 4
Other Evidence Considered by the Committee
Appendix 5
List of Witnesses who Gave Oral Evidence to the Committee
Executive Summary
The number of suicides in Northern Ireland has been increasing in recent years. Currently, about 195 people take their own life each year while a further 4,500 people are admitted to hospital having attempted suicide or inflicted serious injury from engaging in deliberate self-harm. Launched in October 2006, a national suicide prevention strategy entitled Protect Life: a shared vision has been developed within the context of a rise in the number of people dying by suicide and engaging in self-harm. Protect Life represents a major step forward in the efforts to reduce this needless waste of life. However, suicide is not a matter of figures or statistics but each person who takes their own life is a life prematurely cut short and a tragedy and a trauma beyond words for the family, for their friends and relatives, and for society as a whole.
The Committee has examined the scope and appropriateness of the strategy and its implementation to date. The level of engagement, particularly with community groups and families bereaved by suicide, in drawing up the strategy has been extensive and lessons have been learned from international best practice. Throughout its Inquiry, the Committee discovered a substantial level of commitment and endeavour in delivering the full implementation of the strategy and ensuring improvements in levels of support for those affected by suicide.
The Committee identified a number of areas where it believes the strategy can be strengthened and enhanced. These include the following:
- There is a recognition that one size does not fit all and the focus of the strategy needs to be refined to take account of the significant suicide risk among older people and those living in rural areas.
- Central co-ordination and delivery of the strategy could be improved by the establishment of a designated suicide prevention director. This would help to build a higher degree of expertise and experience in planning and delivering the strategy, working closely with the Suicide Strategy Implementation Body and taking account of the views of key stakeholders, and providing a direct central contact point for all stakeholders.
- The funding provided to implement the strategy must remain ring-fenced for a number of years and community groups need a greater degree of financial certainty and sustainability to concentrate on providing their services.
- Preventing suicide and providing help and support for those affected is not solely a matter for the Department of Health, Social Services and Public Safety. Greater commitment and involvement is required from all other Departments. For example, the Department of Education can play an influential role in supporting primary and post-primary schools in the development of coping skills and character building which can better equip young people in confronting the challenges of modern life.
- The level of stakeholder involvement could be further enhanced by incorporating a greater role for churches and developing strong partnerships with local authorities and sporting bodies.
- A suicide prevention telephone helpline provides a vital lifeline for those in crisis but it must be backed up with sufficient referral and support services. The decision to set up a regional helpline, without an evaluation of the pilot in north and west Belfast and in the absence of an assessment of existing referral and support services to cope with a significant increase in calls, was considered premature.
- Extensive training has already taken place particularly through the ASIST (Applied Suicide Intervention Skills Training) programme. However, there is still a significant need for additional and improved training for those who may come into contact with people at risk of suicide.
The Committee learned of many excellent services throughout Northern Ireland, provided by local community groups and others, that aim to prevent suicide and self-harm, to deal with those who may attempt suicide, and to cope with the aftermath of suicide and provide support to bereaved families. The Committee also saw exemplary models of counselling and other services in operation in Dublin and in Scotland and would urge the Minister to explore how these could be replicated in Northern Ireland by building on existing experience and capacity.
It is well recognised that the media can play a positive role in raising awareness of issues relating to good mental health and can have an impact in combating any associated stigma. At the same time irresponsible reporting of suicides can increase the risk of copycat suicides. Increasingly concerns have also been raised about the influence of the internet and the prevalence of social networking sites that are used to promote suicide among young people. The Committee commends the efforts being made by the Minister to engage with the local media and with internet service providers.
The awaited response by the Department of Health, Social Services and Public Safety to the recommendations in the Bamford Review of Mental Health and Learning Disability provides a unique opportunity to develop and strengthen links between the suicide strategy and the provision of mental health services. This is particularly important in relation to the development of child and adolescent mental health services.
Summary of Recommendations
1. The development of the Protect Life suicide prevention strategy has been a major step forward in the battle to reduce the incidence of suicide in Northern Ireland. We recognise the benefits of the dual population and targeted approach but we believe that the focus of the targeted approach needs to be re-examined and redefined to include other priority groups, such as older people and those living in rural areas. (Paragraph 35)
2. We have major concerns that the current structure lacks a dedicated directorate to manage and act as a central focus for the implementation of the suicide prevention strategy. We call on the Minister to establish a designated suicide prevention directorate as part of the proposed new Regional Public Health Agency. (Paragraph 41)
3. It is of the utmost importance that robust review and evaluation arrangements are in place to examine the key elements of the strategy and learn lessons as the strategy develops. While provision for such review and evaluation was built into the strategy we have major concerns that this has not yet taken place. We call on the Minister to commission an urgent independent, time-bounded evaluation of the key elements without further delay and to take account of the findings of this Committee Report in the review of the strategy. (Paragraph 44)
4. We note the overall level of funding for implementation of the strategy and recognise that it compares favourably on a per capita basis with Scotland and the Republic of Ireland. We strongly urge the Minister to ensure that this funding remains ring-fenced for a number of years to sustain and implement the Protect Life strategy and that there is full transparency, accountability and scrutiny of how this funding is used.. (Paragraph 50)
5. We commend the sterling work carried out by community groups and we fully recognise the vital importance of their involvement in the strategy to reduce suicide and support bereaved families. The assurance by the Department that over £2 million in 2008-09 is being allocated to support community initiatives is welcome. However, we are greatly concerned at the ongoing uncertainty and insecurity caused for those groups by single year funding. This must be addressed urgently. We call on the Minister to provide funding support for community groups on a minimum of a three yearly basis. (Paragraph 51)
6. We fully recognise the difficulties involved in measuring suicide rates, the dangers of putting too much emphasis on a single year’s figures, and the arguments for and against setting specific targets. We note the target of a 10% reduction by 2008 and we urge the Minister to review the targets when figures for 2008 become available and to consider setting targets for the reduction of self-harm. (Paragraph 56)
7. We fully appreciate the first hand knowledge and understanding that bereaved families bring to bear in the efforts to deal with suicide and the positive contribution that they have made to the development of the strategy. We commend the many families who have come together to set up Family Voices and we urge the Minister to ensure that their views are taken into account. (Paragraph 66)
8. We welcome the establishment of the Ministerial Co-ordination Group on Suicide Prevention chaired by the Health Minister and involving a number of other Ministers. We urge the Executive to acknowledge that suicide prevention is not solely a health issue and to examine how the role of the Ministerial Group can be further developed to secure a greater commitment and involvement by all Departments. (Paragraph 69)
9. We welcome the introduction of the independent counselling support service in post primary schools and call on the Minister for Education to extend this service to the primary sector as soon as possible. We also welcome the work that is underway to develop a Pupils’ Emotional Health and Wellbeing Programme for the post primary sector. However, we believe that developing coping skills and building young peoples self esteem should begin at an early age and we call on this programme to be extended to all schools. (Paragraph 76)
10. We welcome a number of useful initiatives linked to the prevention of suicide and self harm currently being undertaken by the Department for Employment and Learning. These include the services provided by Opportunity Youth and Include Youth to young people on the Jobskills and Training for Success Programmes. We also recognise the value of the Bytes Project, jointly supported by the Department of Education, which targets ‘hard to reach’ young people who are not in education, employment or training. We call on the Department for Employment and Learning to review its contribution to implementing the Protect Life strategy and, in particular, to ensure that initiatives taking place in some FE colleges are available to all in that sector. (Paragraph 78)
11. We welcome the commitment by the leaders of the four main churches in Northern Ireland to play their part in tackling the issue of suicide and self harm. We urge greater collaboration with the Suicide Strategy Implementation Body in the development and delivery of training for all clergy in dealing with people who may be at risk of suicide and in supporting families and communities in the aftermath of a suicide. (Paragraph 84)
12. The positive role of sport and exercise in combating stress, anxiety and depression is well established and widely recognised. We urge the Minister to explore how the prescribing of an exercise regime can be developed and promoted for use as an option by GPs in appropriate circumstances. (Paragraph 91)
13. We are disappointed that Sport NI and the main sports bodies in Northern Ireland have not been directly involved in developing and delivering the strategy to prevent suicide. We call on the Minister for Health, Social Services and Public Safety to explore with the Minister for Culture Arts and Leisure how Sport NI and other sports organisations can fully participate in delivering the suicide strategy. We strongly commend the Scottish model of involving sporting icons and using major sporting occasions to raise awareness of the issue and to encourage young people, particularly young men, to seek help. (Paragraph 92)
14. There is clear potential for local authorities to play a significant role in the ongoing development and delivery of the Protect Life strategy. We urge the Minister to explore with local authorities how solid partnerships can be developed. We believe that this should include full participation in the Suicide Strategy Implementation Body and other structures. (Paragraph 96)
15. The importance of training and development in suicide awareness, in identifying early warning signs and in knowing how to respond to those signs has been incorporated into the strategy. The merits of the ASIST (Applied Suicide Intervention Skills Training) programme are widely recognised. We believe that the time is right to examine the progress of the training programme to date and identify any gaps. (Paragraph 107)
16. We have major concerns that the decision to extend the pilot telephone helpline in north and west Belfast into a regional helpline at this time was rash. We believe that a number of key issues should have been fully addressed before any decision was taken to go live. These include
- a thorough evaluation of the pilot in north and west Belfast to learn lessons from that experience;
- a detailed assessment of whether adequate referral and support services are in place to cope with a significant increase in calls;
- detailed discussion with the Samaritans to avoid duplication and to develop a strong working partnership; and
- consideration of additional sources of support and funding, for example, from mobile phone providers as has happened in Scotland.
We believe that the regional helpline should have an easily identifiable title, such as ‘lifeline’ and that the launch should have been accompanied by a high profile media awareness campaign. However, we would now urge caution about a high profile publicity campaign until an assessment of the adequacy of existing referral and support services has been carried out. (Paragraph 117)
17. We are greatly concerned about the lack of focus on providing psychosocial assessment and follow-up care for those who self-harm. We welcome the pilot self-harm service in north and west Belfast and call for it to be evaluated urgently and extended to all A&E departments. (Paragraph 122)
18. There is an urgent need for greater access to talking therapies to treat people with depression and anxiety disorders. We welcome the assurance of a significant investment in psychotherapies and the development of a psychotherapy strategy and we call for this to be implemented without delay. (Paragraph 128)
19. We welcome and recognise the value of co-operation between countries at a strategic level on issues relating to the prevention of suicide. The Committee fact finding visits to Scotland and the Republic of Ireland also highlighted that there are often many lessons to be learned from ground-breaking and innovative services that are pioneered and developed at a local level. We call on the Minister to consider, perhaps through the Five Nations Forum, how information on innovative activities at a local level can be shared between countries. (Paragraph 132)
20. We strongly recommend that the Minister set up a separate dedicated Protect Life website, similar to the Choose Life website in Scotland and the Reach Out website in the Republic of Ireland. We believe that this would provide a key resource to augment implementation of the strategy. (Paragraph 133)
21. We strongly support calls for more responsible reporting of suicide and related issues in the media and we welcome the action taken by the Minister to engage with the local media. We particularly welcome and support the initiative by the Minister to tackle the issue of internet sites that promote suicide. We call for a Northern Ireland version of Headline, a media monitoring programme, to be established and implemented as soon as possible. (Paragraph 139)
22. We recommend that the current general mental health media campaigns be subjected to a robust evaluation and that urgent consideration be given to how the specific issue of suicide and self harm can best be addressed through a public media campaign. (Paragraph 142)
23. We recognise the critical opportunity that is provided to influence the lives of people who present in crisis at A&E departments of hospitals. We call on the Department to require Boards and Trusts to carry out an urgent examination of ways in which a chill-out room can be provided in or adjacent to all A&E departments in hospitals. (Paragraph 145)
24. We recommend the urgent introduction of a ‘card before you leave’ system to provide people at risk of suicide or self-harm who attend A&E departments or who are discharged from hospital with a definite follow-up appointment. (Paragraph 147)
25. We are greatly concerned that lessons about the need for better communication highlighted in a number of reports have not been implemented. We fully support the recommendations in the O’Neill Report in relation to communication. (Paragraph 149)
26. We recognise that healthcare and other frontline staff are themselves at increased risk of suicide and we recommend that urgent consideration be given to the establishment of a structured system of care and support similar to that in place in Ayrshire and Arran NHS. (Paragraph 151)
Introduction
1. The number of suicides in Northern Ireland soared from an average of 150 between 1999 and 2004 to 291 by 2006.The Committee, conscious of the serious and growing concerns about this increasing incidence of suicide, set aside other scheduled work to examine the current strategic approach to the prevention of suicide and self harm in Northern Ireland.
2. This report sets out the results of the Committee examination of:
- the scope and appropriateness of the strategy ‘Protect Life: A Shared Vision’;
- the level of stakeholder involvement;
- the level of services and support available to promote good mental health, to prevent suicide and self harm; and to support those affected by suicide; and
- any further action required, taking account, as appropriate, of experience elsewhere.
3. In undertaking the Inquiry the Committee wrote to a wide range of organisations and groups within Northern Ireland and further afield inviting written submissions. Notices were also placed in the main newspapers. The Committee recognises that tackling suicide and self harm is not an issue for one Department and is conscious of the recently established Ministerial Co-ordination Group on Suicide Prevention. The Committee, therefore, invited views from all Departments and Assembly Committees. Visits to Edinburgh, Ayr and to Dublin were undertaken to learn from the experience in Scotland and the Republic of Ireland where comprehensive strategies have been in place for some time. The Committee also visited a Self Harm Service based in north and west Belfast organised by the Belfast Health and Social Care Trust. The Committee took formal evidence from many organisations both in Parliament Buildings and at various locations throughout Northern Ireland. We are grateful to all those who helped us with this Inquiry, including those who provided oral or written evidence. We are particularly grateful to the families of those bereaved by suicide for sharing their views and concerns with the Committee.
Background
Suicide
4. “Suicide itself is not an illness or a condition, … it is an act that can occur as an outworking of various factors. … Suicide is a final act which always arises as a consequence of a great complexity of issues.”[1]The evidence produced during the course of the Inquiry demonstrated beyond doubt that there is no single reason why someone takes their own life and the risk factors associated with suicide are exceedingly complex and multi-faceted. As well as mental health issues the factors highlighted to the Committee that may be linked to suicide ranged from social pressures, low self esteem, lack of opportunity, limited education and employment opportunities, limited access to mental health support, lack of communication and interpersonal skills, to sectarianism, intimidation or involvement with paramilitaries. Other factors highlighted were the impact of bullying or of being subjected to physical or sexual abuse, the impact of alcohol or drug misuse, long term medical conditions and post natal depression.
5. Particular groups or sections of society may be subject to specific influences. Age Concern stated “Depression is the leading cause of suicide in older people. Other risk factors include sleep problems such as insomnia, and alcohol consumption, particularly in men.”[2] The Rural Community Network reminded the Committee that farmers and farm workers have been identified as a high risk group for stress, depression and suicide and suggested that “Restructuring of farming, crises such as BSE and Foot and Mouth have placed immense strain on farmers and farm families struggling to make ends meet.”[3]
6. The National Union of Students identified the pressures facing students while Youth Action NI highlighted that “Young men aged 15-18 years are extremely vulnerable and it is in this period that they may begin to experience the stress, bullying, confusion, pressure etc which impacts on their later decision to attempt suicide or self harm.”[4] NIACRO pointed out that “Asylum seekers and other ethnic minority prisoners may be at heightened risk of self harm or suicidal behaviour.”[5] Raymond Craig, Oakleaf Rural Support Network highlighted that “There is a seriously high suicide rate in the gay and lesbian community — it is in crisis.”[6] The views of a group of young people were reported to the Committee by VOYPIC (Voice of Young People in Care). The young people ranked the following in order of importance as the issues of greatest concern in relation to suicide: “i. bullying- this could occur in the work place, school or where person is living; ii. alcohol and drugs, this could be use by parents or self; iii. stigma– included mental health and being seen as different because of clothes, music, sexuality; iv. no family contact; v. low self esteem; and vi. loneliness”[7].
7. Professor Hugh McKenna, University of Ulster, told the Committee that “Suicide and self harm are much commoner in younger people (15 – 24) than in other age groups. … Issues such as bullying, sexual orientation and difficulty in relationships frequently are often at the root of suicide and other related behaviour. The empirical literature suggests that young people have difficulty with problem solving or coming to terms with complex issues in life.”[8]
8. At the outset of the Inquiry, the Chairman of the Royal College of Psychiatrists described the factors that influence suicide prevalence as falling into three broad categories, namely mental illness; emotional or psychological factors; and socio-cultural factors. The Law Centre NI pointed out that “There is an established link between mental ill health and suicide. According to the World Health Organisation mental disorders (particularly depression and substance abuse) are associated with more than ninety percent of all cases of suicide.”[9] This assertion was further strengthened by Professor Kevin Malone, University College Dublin, who told the Committee that “All the international studies clearly demonstrate that a significant component of suicide deaths is associated with varying degrees of mental illness.”[10] The Eastern Health and Social Services Board concluded that “Whilst there are a range of factors which give rise to an increased risk to suicide … the single greatest predictor of future suicide is previous suicide attempts.”[11]
9. Concerns were also expressed that sensationalist media reporting of suicide and irresponsible internet sites can have a detrimental influence. Rt Rev Dr John Finlay told the Committee that “we are concerned that the prevalence of suicide in an area — especially among teenagers — can, sadly, create a copycat culture. We fear that the situation is exacerbated by the media and by the influence of soaps.”[12] Dr Tom Black, BMA, said that “one of the main problems with suicide is that it is contagious. People talk about ‘imitation’ and ‘copycat’ behaviour. … I prefer the word ‘contagious’. Suicides then happen in clusters, as we have seen in Northern Ireland”[13]. Mr Colm Donaghy, Chairman of the Suicide Strategy Implementation Body, also argued that “the media and the internet have big impact on our young people. Some 6% to 7% of suicides are copycat suicides, and that is primarily due to the impact of the media on young people. In Northern Ireland terms that equates to 20 young people. Those would be eminently preventable suicides if we could ensure that our media reported responsibly on suicide”[14].
Self-Harm
10. The Royal College of Psychiatrists defines self harm as “a deliberate non-fatal act, including overdosing, cutting and attempted hanging, done in the knowledge that it is potentially harmful”[15]. The British Psychological Society states that cutting and burning are the most common forms of self-harm, but it also includes scratching, head banging, poisoning, skin picking, hair pulling, interfering with wound healing, asphyxiation and biting. Self-harm is often seen as a means of coping with particular problems or situations. However, the Western Health and Social Services Board told the Committee that “Numerous studies have found that engagement in deliberate self-harm (DSH) is the strongest predictor of future suicidal behaviour, both fatal and non-fatal. It is estimated that at least one third of all suicides have a history of deliberate self harm.”[16] Dr Tom Black, BMA, told the Committee that “the key relationship between the two is that 51% of suicide victims have self-harmed before their death”[17].
11. The Royal College of Nursing urged the Committee to note that “the DHSSPS strategy seeks to address the issue of self-harm as well as suicide. The two issues are broadly linked but not necessarily mutually inter-dependent.”[18] Dr Rory O’Connor in his evidence to the Committee noted that “self-harm is the key predictor of completed suicide” but he also pointed out, in relation to the Scottish Suicide Prevention Strategy ‘Choose Life’ that it “is not a self-harm prevention strategy”[19].
12. The Royal College of Psychiatrists pointed to recent research which “suggests that full assessment of self-harm case is possibly the most important suicide prevention measure that can be taken. Of those who self harm, 1% are likely to complete suicide within the next year, an increase in risk of 100 times. This is clearly an easily identifiable group of people who are at risk and who can and should be offered thorough assessment and, if necessary, follow up”[20]. The Royal College also pointed out that the NICE (National Institute for Health and Clinical Excellence) Guidelines require every patient to be given a full psychosocial assessment after self–harm.
13. Dr Philip McGarry, Royal College of Psychiatrists, expressed concern “that 10% of those who self-harm and attend hospital departments are adolescents, and we do not have the appropriate follow-up or back-up services there”[21]. He also pointed out that “most psychiatrists who see self-harming patients in general hospitals would reckon that, in over 50% of cases, alcohol has been taken. In many of those cases, had those individuals not taken alcohol, they may well not have harmed themselves”[22].
Trends
Northern Ireland
14. While there has been a prevalence of suicide among the young adult population for many years, the number of registered suicides in Northern Ireland has effectively doubled since 2004. During the period 1987 to 2004, there were 2,732 registered deaths from suicide in Northern Ireland. This number peaked in 2000 at 185 deaths, while the lowest number of suicides during this period was in 1987 when there were 122 registered deaths.
15. The average number of suicides per annum between 2000 and 2004 was 163. However, the 2005 figure registered a 46% increase rising to 213 deaths (167 males and 46 females)[23] while 291 suicides were recorded (227 males and 64 females) in 2006, representing a 37% rise in the number of registrations on the 2005 figure.[24] The figures for 2007 just published highlight a reduction in the number of registered suicides to 242. While the reduced figure for 2007 is important, the overall average between 2000 and 2007 has increased to approximately 195.
Table 1: Suicide and Undetermined Deaths for Northern Ireland 2000-2007[25]
| ... | 2000 |
2001 |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Registered |
185 |
158 |
183 |
144 |
146 |
213 |
291 |
2421 |
||||||||
Year Occurred |
(186) |
(181) |
(196) |
(157) |
(220) |
(206) |
||||||||||
Male/Female |
140 |
45 |
132 |
26 |
142 |
41 |
112 |
32 |
105 |
41 |
167 |
46 |
227 |
64 |
175 |
67 |
16. The Committee noted that when a suicide death is referred to the coroner, as is the protocol in all instances of suspected suicides, there is quite often a delay between the actual death and date of registration. For example, a significant number of suicides registered in 2006 occurred in the preceding years. Of the 291 deaths by suicide registered in 2006, 52 occurred in 2004, with 37 occurring in 2003 or earlier.[26] In Table 1, the figures in brackets highlight the number of suicides and undetermined deaths in the year that they actually occurred.
17. While the overall suicide rate is 11.4 per 100,000 persons, there are considerable variations in the prevalence of suicide across Northern Ireland. One of the ways in which Protect Life highlighted the large differences in suicide rates was through comparison of local Parliamentary Constituencies. In their submission to the Inquiry, the Department reaffirmed the fact that the North and West Belfast constituencies continue to experience the highest rates of suicides where currently the rate is 20 and 15.3 per 100,000 persons respectively.
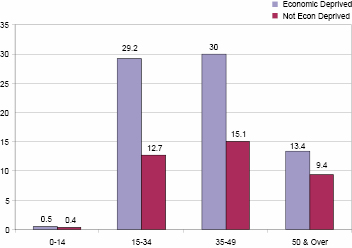
18. Table 1 above clearly demonstrates that suicide is much more prevalent among males than females. Figures 1 and 2 below also illustrate the fact that suicide is more prevalent in young adults and supports the view that suicide is more prevalent in urban and economically deprived areas. It is also worth noting the findings of a recent piece of longitudinal research conducted by O’Reilly et al from Queens’ University Belfast which concluded that ‘differences in rates of suicide between areas are predominantly due to population characteristics rather than to area-level factors…suggesting that policies targeted at area-level factors are unlikely to significantly influence suicide rates.’[27]
Figure 1: Average suicide rate per 100,000 persons by rurality and age band[28]
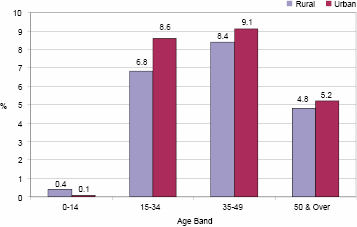
Figure 2: Average suicide rate per 100,000 persons by economic deprivation and age band[29]
International Comparison
19. The situation in Northern Ireland is congruent with the wider global trend of a growing number of people dying by suicide in almost every region of the world. The scale and pervasiveness of the problem is reflected in the fact that for some time suicide has been the third biggest cause of “years of lives lost” after cardiovascular disease and cancer. An estimated 877,000 lives were lost prematurely worldwide due to suicide in 2002.[30] According to the World Health Organisation (WHO), around one million people worldwide currently die from suicide each year and 10 to 20 times more attempt suicide. This represents an average of one death every 40 seconds and one attempt every 3 seconds.[31] In 2005, 6,045 suicides and undetermined deaths were registered in the United Kingdom and the Republic of Ireland[32] with approximately 5,000 deaths registered in England alone.[33] Alongside these deaths, there are a very large number of people, estimated to be as many as 142,000 who are admitted annually to Accident and Emergency (A&E) departments because they have harmed themselves non-fatally. Among admission to A&E departments for non-fatal self-harm, the majority involve self-poisoning. Between 10% and 15% tend to be cases of self-injury, with most of these involving cutting.[34]
Figure 3: European Union total population suicide rates per 100,000 persons[35]
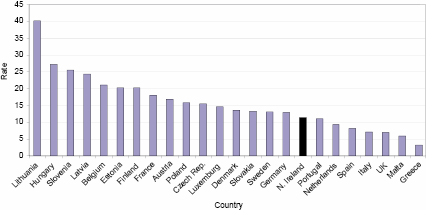
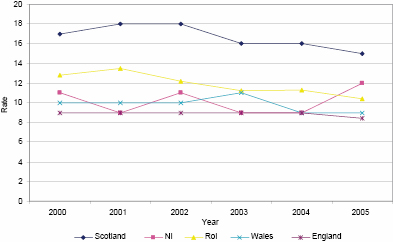
20. The overall suicide rate in Northern Ireland, currently 11.4 per 100,000 persons (as of April 2008), is higher than the rates in England, Wales and the Republic of Ireland but less than the rate in Scotland. It is important to note that this figure is based on a rolling average between 2002 and 2006. It represents a rise in the original figure of 9.7 per 100,000 persons outlined within the Protect Life strategy which itself was based on a rolling average between 2000 and 2004.[36]
Figure 4: National suicide rates per 100,000 persons in England, Scotland, Wales, Northern Ireland and the Republic of Ireland[37]
Self-Harm
21. As set out in Protect Life, the average rate of admissions to hospital each year in Northern Ireland as a result of self-harm is 280 per 100,000 persons[38] or almost 4,500 admissions each year. However, the seriousness of the problem and the need to tackle it alongside the increasing prevalence of suicide is only partially reflected in the recorded statistics. This is because deliberate self-harm continues in many respects to be a ‘hidden problem’ involving young people who often only present themselves to Accident and Emergency departments when such behaviour has resulted in serious injury. Moreover, the figures are furthered distorted by the fact that only a proportion of those individuals who have self-harmed and present themselves for medical attention at Accident and Emergency departments are admitted to hospital.
22. The Department’s submission indicates that, ‘the term self-harm covers a wide range of behaviours including ‘parasuicide’[39] and habitual self-cutting and poisoning which involves differing degrees of risk to life and differing degrees of suicidal intent.’ Incidents of self-harm which result in admissions to hospital are recorded in the DHSSPS Hospitals Inpatients System (HIS) which uses the same International Statistical Classification of Diseases and Related Health Problems (ICD) used in the classification of deaths.[40] The latest hospital admission figures relating to self-harm are illustrated in Table 2.
Table 2: Number of hospital admissions as a result of self-harm (2002/03-2006/07)[41]
Year |
2002-03 |
2003-04 |
2004-05 |
2005-06 |
2006-07 |
Total |
|---|---|---|---|---|---|---|
Admissions as a result of self-harm |
4,591 |
4,517 |
4,704 |
4,494 |
4,112 |
22,418 |
All admissions |
487,518 |
508,824 |
521,123 |
532,670 |
537,193 |
2,587,328 |
% of all admissions |
0.94% |
0.89% |
0.90% |
0.84% |
0.77% |
0.87% |
Strategic Approach to Suicide Prevention
23. Professor Hugh McKenna, University of Ulster, pointed out that “many eminent researchers will agree that preventing suicide in its totality is near impossible. Nonetheless, many will also agree that the reduction of suicide and other related behaviour such as self harm can be achieved. This type of thinking requires a mind shift by Government. Much of the current research focuses too much on causative factors and how people commit or attempt suicide. There is a need to focus on factors that have helped people to regain their will to live.”[42]
24. The development of a regional strategic approach to the prevention of suicide and self-harm is a relatively recent method of tackling the issue. Dr Rory O’Connor, a leading chartered health psychologist and member of the International Association for Suicide Prevention, explained that “the first national suicide prevention strategy was developed in Finland and launched in 1986 and has influenced national strategies throughout the world. It was a ten year strategy and it has been evaluated internally and externally. It has been seen largely as a success. … A number of other countries, Norway, Sweden, New Zealand, Australia, United Kingdom, Netherlands, Estonia, France and the South of Ireland have all got suicide prevention strategies.”[43]
25. Dr O’Connor also told the Committee that suicide prevention strategies across the world tend to be made up of six components. These are: undertaking education and awareness; screening those at risk; providing treatment for psychiatric disorders; restricting access to lethal means of carrying out suicide; developing guidelines for dealing with media reporting; and undertaking research.
26. In 2005 an increase in the number of suicides, particularly among young people, led to the establishment by the Department of a multi-sectoral taskforce charged with the development of a suicide prevention strategy for Northern Ireland. In drawing up the strategy the taskforce undertook a very extensive engagement process which included meetings and consultation workshops with a wide range of sectors and stakeholder organisations throughout Northern Ireland. Bernie McNally from the Belfast Health and Social Care Trust commended the process saying “It is the Trust’s view that the development process of the Protect Life Strategy was an example of effective stakeholder involvement across the statutory, community, and voluntary sectors.”[44]
27. The resulting ‘Protect Life: a shared vision’ suicide prevention strategy, published in October 2006, includes all six components identified by Dr O’Connor and it also incorporates a number of important guiding principles including, the development of links to others relevant strategies such as Investing for Health, the mental health strategy, the alcohol and drug strategy, and the children’s strategy, the recognition of the need for joined-up working at Government level, and the need for ongoing engagement with primary stakeholders particularly bereaved families.
28. The strategy has adopted a dual population and targeted approach. As explained in the strategy document “The population approach seeks to tackle the issue of suicide in a wider generic context, with actions aimed at protecting the general population of Northern Ireland. The targeted approach seeks to tackle the issue by focusing action on those who are most at risk.”[45] The document stresses that the dual approach is complementary.
29. Mr Francis Rice, Southern Health and Social Care Trust explained that the action plan is also divided into two different approaches. “The first is a population-based approach under which we have specific objectives and targets that deal with communities; families, children and young people; health and personal social services; workplaces; emergency services; Churches; and the media. We then move on to more specific, targeted approaches that have objectives with specific outcomes and deal with areas such as self-harm and mental illness; drug and alcohol misuse; young males; those bereaved by suicide; survivors of sexual, physical and emotional abuse; marginalised and disadvantaged groups; high-risk occupations; and prisoners.[46]
30. Professor Hugh McKenna, University of Ulster, described the Strategy as “probably the most important document that has been produced in recent times in Northern Ireland … This document has a number of well made points with regard to suicide. Its proposed strategy of targeting vulnerable populations is to be commended. It identifies young males and those bereaved by suicide as being particularly vulnerable”[47].
31. However, a number of respondents expressed some unease that the emphasis on tackling the suicide risks among young people could detract from the needs of other groups or sectors. The Northern Health and Social Care Trust stated “A concern would be that in focussing so strongly on the very real needs of younger people the strategy may play down the needs of older people who also sadly suffer high rates of suicide.”[48] Age Concern argued that “suicide and self-harm is also an issue in later life, with suicide rates across the UK remaining high for both older men and women, especially those aged 75 and over. …Older people should be identified and included as a priority group within the scope of the strategy.”[49] Professor Hugh McKenna, Queens University Belfast, also drew attention to suicide among older people and concluded that “ a pre-emptive approach to older suicide is needed”[50].
32. Mr Iain McGowan, on behalf of a multi-disciplinary group of clinicians, stated “we hold that the focus [of the strategy] on young males and those bereaved by suicide limits its scope. It would be damaging to set to one side other demographic categories in which suicide is a notable issue, for example, suicide in pregnant women and new mothers, in those who struggle with sexual identity and in those over the age of sixty-five”[51].
33. The Niamh Louise Foundation argued that one size does not fit all and stressed the need for a different approach in urban and rural areas. The Foundation stated that “this does not seem to have been included in the development of the strategy and the principle that one method works well in all areas should be readdressed and special attention given to how to create awareness and response mechanisms in the aftermath of a suicide in our rural areas”[52].
34. Research by Dr Dermot O’Reilly, Queens University Belfast, presented to the Committee found that ‘differences in suicide rates are predominantly due to population characteristics rather than area-level factors’. It suggests that once ‘individual characteristics and household factors (i.e. marital status, household composition, socio-economic and employment status and baseline health status) are adjusted for, the association between suicide risk and area deprivation and levels of social fragmentation disappeared.’ Dr O’Reilly told the Committee that the lesson for the suicide strategy was that “While the current efforts focus on the need for support for individuals and especially for younger people …, it ignores the wider social background to suicide risk. Our research clearly shows that suicide risk is greatly increased amongst those not in employment and those individuals living in disadvantaged circumstances. … factors which improve the levels of employment and increase the social wellbeing of the population are likely to have a significant impact on suicide risk for the Northern Ireland population. As is often the case, the factors that most impact on our health lie outside the caring and curative services.”
35. The development of the Protect Life suicide prevention strategy has been a major step forward in the battle to reduce the incidence of suicide in Northern Ireland. We recognise the benefits of the dual population and targeted approach but we believe that the focus of the targeted approach needs to be re-examined and redefined to include other priority groups, such as older people and those living in rural areas.
Implementation Structure
36. Following publication of the Suicide Strategy the Department set up a Suicide Strategy Implementation Body (SSIB) “to oversee and drive forward the implementation of the Strategy”[53]. The SSIB, with a membership of more than 40, comprises very wide ranging representation from, inter alia, health related organisations, bereaved families, PSNI and various Government Departments. The SSIB meets bi-monthly and the secretariat is provided by the Department.
37. STEER Mental Health argued that “If suicide prevention is to be recognised as a priority by all relevant Government Departments, the Suicide Strategy Implementation Body should be located within the Department of the First and the Deputy First Minister.”[54] This was a view supported by the Health and Social Services Councils. North Down & Ards Community of Interest group queried “how progress can be made on so many actions, given that ‘lead’ partners are not clearly identified and much of the responsibility for driving action lies with the DHSSPS.” The group also pointed to the “danger of services being driven via DHSSPS and the potential therefore to ‘medicalise’ the solutions to the issue”[55].
38. The co-ordinator in the South Eastern Trust expressed concerns that “a robust system of communicating the progress of SSIB to the local community level is lacking” and also that “there is a feeling that while SSIB members are given due respect and a hearing that major decisions taken at the inception of the strategy cannot be easily influenced”[56]. The Health and Social Services Councils were concerned that the Suicide Strategy Implementation Body was a misnomer and that it had “remained as an advisory body to the Department rather than an implementation body”.[57]
39. Mr Seamus McCabe, PIPS, said “The strategy is a bottom-up strategy, and it was put in place as a result of lobbying that bereaved families carried out. … when work reaches a certain level, the Department takes ownership of it, and we are cut off. The community groups take the work as far as they can, and the Department then takes over.”[58]
40. In the Republic of Ireland a National Office for Suicide Prevention [NOSP] has been established within the Health Service Executive to oversee the implementation of ‘Reach Out’ the National Strategy for Action on Suicide Prevention. NOSP in a submission to the Committee suggested “It would be helpful if there was a similar organisation to the NOSP in NI as this would allow for one contact point for this office. Also in our experience the establishment of the office has provided a national focus for all our initiatives as well as a central coordination role. For government it provides a single channel through which Department of Health and Children funding and policy monitoring can take place. We would urge you to establish a team within the health/ social care statutory set up to undertake this work.”[59] Health and Social Services Councils agreed that there were merits in establishing a similar body in Northern Ireland. Speaking about another issue Pat McGreevy, Coordinator South Eastern Health and Social Care Trust said “Unlike Scotland and the Republic, we do not have a designated suicide prevention office to get the message out.”[60]
41. We have major concerns that the current structure lacks a dedicated directorate to manage and act as a central focus for the implementation of the suicide prevention strategy. The SSIB, which is charged with overseeing and driving forward the strategy, provides a vital structure to bring together the many stakeholders and to help develop policies. However, with more than 40 members we believe it is too large and unwieldy to undertake the role of driving forward the strategy. We call on the Minister to establish a designated suicide prevention directorate as part of the proposed new Regional Public Health Agency.
Evaluation and Review
42. The Department advised that the Strategy will be reviewed on an annual basis and that the first review is due to be completed “by end of March 2007”[61]. The review will consider the actions, timescales, structures etc and make recommendations. In its submission to the Committee the Department stated that it had commissioned the Institute of Public Health in Ireland (IPH) “to develop a monitoring and evaluation framework that will assist with the future assessment of key elements of the Strategy’s implementation. … IPH is currently consulting with key stakeholders on the development of this framework, and it is anticipated that this work will be completed by the end of November 2007”[62].
43. When the Committee met representatives of families and community groups one of their main concerns was the absence of any evaluation to date. Michael Doherty, West Belfast Suicide Awareness and Support Group, said “the strategy was 12 months old in September 2007. It is now January 2008, and no adequate evaluation of the strategy has been carried out. A lot of money has been spent on it, and perhaps another £3 million will be spent this year, but we want an adequate evaluation that considers whether the actions that were planned for the first year have taken place and, if so, what the outcomes have been. We must learn from those outcomes in advance of moving into the second year of the strategy.”[63]
44. It is of the utmost importance that robust review and evaluation arrangements are in place to examine the key elements of the strategy and learn lessons as the strategy develops. While provision for such review and evaluation was built into the strategy we have major concerns that this has not yet taken place. We call on the Minister to commission an urgent independent, time-bounded evaluation of the key elements without further delay and to take account of the findings of this Committee report in the review of the strategy.
Funding
45. The Department provided funding of £1.9 million in 06/07 and £3.06 million in 07/08 to implement the Strategy. Approximately £0.95 million in 06/07 and £1.8million in 07/08 of this was allocated as part of a community support package. In addition in January 2008 the Minister announced the establishment of a Regional Suicide Prevention Helpline and stated that it will cost approximately £3.5million each year to run the helpline. The Minister stated “this development means that a total of over £6million has now been allocated each year to implement the suicide prevention strategy.”[64]
46. The level of funding provided was acknowledged by the Samaritans as “generous in relation to the other administrations and the size of population”[65]. In Scotland “£12 million was made available … in 2003-2006 and a further £8.4 million was made available for 2006-2008”[66]. During the visit to the Republic of Ireland the Committee was told that the total funding available there to support suicide prevention initiatives in 2007 was €8 million (£6.78m approx[67]) and this level of funding continues into 2008. An additional €1.2 million (£1.02m) was allocated in 2006 and a further €1.85 million (£1.58m) in 2007 to develop and implement national training programmes and to provide self-harm services through A&E departments.[68]
47. Dr Rory O’Connor pointed to the experience in Scotland where funding was earmarked “for local projects, for local development and local skills, so in each of these areas, there was someone who was designated as a lead person to develop the strategy.”[69] He stressed that “having ring-fenced money is particularly important.”[70] However, during the visit to Scotland the Committee learned that ring-fenced funding for the Choose Life Strategy was likely to cease in 2008 and that future funding for the suicide strategy would be included in the overall allocation to Boards. The importance of ring-fencing funding for suicide prevention was also stressed by colleagues in the Joint Committee on Health and Children in the Republic of Ireland.[71]
48. Community groups expressed grave concerns about the level of funding and the uncertainty for their groups after April 2008. Michael Doherty, West Belfast Suicide and Awareness Support Group told the Committee “When the strategy was first launched, people lauded it and the additional money that came with it. However, funding has been totally inadequate, as well as the manner in which it has been handled. … funding must be for a three-year period. …the funding that we have been allocated is inadequate, and we do not know what funding we have beyond March 2008”[72]. Phillip McTaggart, PIPS, said “I constantly hear about £3 million that is being invested in suicide prevention. However, the real figure for the money that goes to work on the ground is only £1·3 million”[73]. When questioned about the funding issue in April 2008 Martin Bell, DHSSPS, assured the Committee that “in 2008-09, over £2 million, of the £3 million budget, will be allocated as part of a community-support package for local health boards, to help local communities to develop initiatives”[74].
49. On the issue of providing sustainable funding over a longer period Andrew Elliott, DHSSPS, said “The Department looks to the Boards to let organisations know as soon as possible about their funding. There is a reasonable degree of certainty now as a result of the completion of the CSR. ... There are mechanisms evolving through which we can consider the possibility of two-year funding. Boards will be given a little more flexibility in that regard”[75].
50. We note the overall level of funding for implementation of the strategy and recognise that it compares favourably on a per capita basis with Scotland and the Republic of Ireland. We strongly urge the Minister to ensure that this funding remains ring-fenced for a number of years to sustain and implement the Protect Life strategy and that there is full transparency, accountability and scrutiny of how this funding is used.
51. We commend the sterling work carried out by community groups and we fully recognise the vital importance of their involvement in the strategy to reduce suicide and support bereaved families. The assurance by the Department that over £2 million in 2008-09 is being allocated to support community initiatives is welcome. However, we are greatly concerned at the ongoing uncertainty and insecurity caused for those groups by single year funding. This must be addressed urgently. We call on the Minister to provide funding support for community groups on a minimum of a three yearly basis.
Targets
52. The Department in its submission states that “the Strategy sets a target of reducing the overall Northern Ireland suicide rate by 15% by 2011, from a baseline of 12.6 in the three year rolling average period of 2004-2006”[76]. Others highlighted that the target is 10% by 2008 with a further 5% by 2011. Dr Rory O’Connor felt that these were “really ambitious targets”[77] and he pointed out that some countries have set targets while others have not. He raised concerns about the implications for the strategy if targets are not met and particularly how it might affect morale or be viewed in the media.
53. The Department argued that progress in reducing the stigma surrounding suicide might mean that more deaths are officially recorded as suicide and thereby artificially increase the recorded suicide rate. It concluded that “if this occurs it should not be interpreted as a failure of the Strategy to achieve its goals”[78]. Dr O’Connor welcomed the fact that “the Northern Ireland Strategy has looked at this and identified secondary targets”[79].
54. In the Republic of Ireland the Reach Out strategy sets clear targets for reducing suicide levels. The Director of the National Office for Suicide Prevention pointed out “While we originally did not set targets due to concerns over the reliability of data we have now done so ... We have taken the view that a target does allow us all to focus our efforts and be accountable for actions taken. … we have also set a target for the reduction in the rate of repetition of self harm”[80].
55. STEER Mental Health believes that “Suicide rates are an unknown quantity and an accurate system for recording suicide statistics must be developed as a priority”[81] so that progress can be measured. The Northern Ireland Commissioner for Children and Young People, while accepting that reducing the suicide rate will be very difficult, argued that “a 10% reduction is too low, and would suggest a target rate of 33%”[82].
56. We fully recognise the difficulties involved in measuring suicide rates, the dangers of putting too much emphasis on a single year’s figures, and the arguments for and against setting specific targets. We note the target of a 10% reduction by 2008 and we urge the Minister to review the targets when figures for 2008 become available and to consider setting targets for the reduction of self-harm.
Stakeholder Involvement
Development of the Strategy
57. A number of respondents agreed that there had been widespread consultation with the community and voluntary sector and with bereaved families during the initial development of the draft strategy. The Rays Crisis Centre, for example, told the Committee that “bereaved families generally felt that they had been listened to, and that their opinions, experiences and concerns had been taken on board.”[83] However, this does not appear to have been maintained. ZEST stated “From a community perspective there are concerns in relation to equal partnership and, in particular, equality in the decision-making process.”[84] This sentiment was supported by Youth Action Northern Ireland which stated “There was no follow up after this point to engage with us as an agency and how the strategy was being implemented on the ground.”[85]
58. The Rays Crisis Centre reported that “the families felt that a significant number of issues had been omitted from the draft version of the strategy ... The Families had been informed but feel they have had no real consultation: as their ideas and inputs were not included in forming the final outcomes of the strategy.”[86] Another community group STEER stated its belief that “stakeholder involvement is merely a ‘box ticking’ exercise by some agencies”[87]. Youth Action Northern Ireland concluded that “Involvement of all stakeholders is key to the success of the strategy and more needs to be done to share the learning and experiences from other projects”[88].
59. Mr Iain McGowan, University of Ulster, argued that “There has been a lack of local academic input into the suicide prevention strategy. As far as I am aware, no one from any of the three higher education institutes was a member of the strategy group. We accept that there were eminent academics and suicidoligists providing quality assurance, but it would have been useful to have had someone with local knowledge as a member of the group”[89].
Ongoing involvement through SSIB
60. The level of stakeholder involvement was commended by some “given that there are 35-40 groups and organisations represented at the Suicide Strategy Implementation Body”.[90] The Southern Health and Social Care Trust stated “Given the multi-sectoral nature of the strategy at regional, area and local levels, coordination is vital. ... Representation on these groups by service providers, commissioners, individuals and communities is critical in ensuring firstly that responses are targeted at addressing the needs of those who have experienced first hand the effects of suicide and self harm and secondly that these responses are multifaceted in nature thus ensuring a holistic response to need.”[91]
Families and Community Groups
61. The Department pointed out that “bereaved families played a key role in the development of the Strategy and are represented on the SSIB. A Families Forum (now Family Voices) was established in August 2006 to ensure that they continue to have a powerful voice in the implementation process.”[92] There were mixed views on how successful the engagement with bereaved families has been. North Down & Ards Community of Interest Group, for example, told the Committee that “there is limited engagement at present locally from families bereaved by suicide and this may take time to develop”[93].
62. The Committee met with a number of representatives of bereaved families and community groups from across Northern Ireland and were greatly impressed by their courage, passion and energy. As Bobby Cosgrove, Family Voices, told the Committee “We do not come at the issue from a professional background; the only hidden agendas that we have are lying in graves. That is where we are coming from. With our hearts and souls, we want to help people through what we went through and to try to make life easier for them. We see the horrors that are happening, and we believe that we can make an impact.”[94] Mr Cosgrove also said “Nineteen years ago, my son took his own life. I had absolutely no one to turn to. I went everywhere. I just wanted answers to simple questions to make sure that I was not going insane. No support was available to me. Twelve years ago, Ann’s son did the same thing. Again, there was no support. Over the past five years, the families have made massive changes. It is the families who have made those changes.”[95]
63. Mr Seamus McCabe, PIPS, explained that the organisation “Family Voices is the result of a lot of families getting together from across the Province, and it allows us the opportunity to share information. It meets on a regular basis.”[96] Anne McGarrigle, Family Voices, told the Committee “We are trying to include all suicide-prevention groups, and we have appealed to all of those groups to be part of Family Voices. It is difficult and tiring for bereaved people to talk about their story, but we need to know the issues and act on those as a collective bunch.”[97]
64. The Minister in evidence to the Committee acknowledged the important role of families. He said “Families who have been bereaved by suicide play a key part in the suicide strategy implementation body, … There are a number of key stakeholders, but the representatives of bereaved families and communities play a very important role, because they have intimate first-hand knowledge of the consequences of suicide — not just of the event but of living with it afterwards.”[98]
65. Colleagues in the Republic of Ireland saw Family Voices as perhaps a model to be emulated. The National Office for Suicide Prevention told the Committee “We have been impressed by the work of the Families Forum in NI and whilst we have similar families groups in the South they do not yet meet together as a national grouping. There is an opportunity in the future to establish an all island network of bereaved families.”[99]
66. We fully appreciate the first hand knowledge and understanding that bereaved families bring to bear in the efforts to deal with suicide and the positive contribution that they have made to the development of the strategy. We commend the many families who have come together to set up Family Voices and we urge the Minister to ensure that their views are taken into account.
Cross-Departmental Role
67. There is a recognition that implementation of the Strategy is not solely a matter for the Department of Health, Social Services and Public Safety. Four other Departments, Education, Agriculture and Rural Development, Employment and Learning, and Social Development, are represented on the SSIB. In addition, the Executive has established a Ministerial Co-ordination Group on Suicide Prevention chaired by the Health Minister and including the Education Minister and the two junior OFMDFM Ministers. The Minister accepted a suggestion from this Committee that the Minister for Employment and Learning should also be part of the Group. He said “I shall discuss that matter with the ministerial group and with the Minister for Employment and Learning. That is a good suggestion, bearing in mind the link between suicide and young males, and DEL’s role in further and higher education — as well as the link between employment and self-esteem.”[100]
68. The Royal College of Nursing was critical of the level of involvement by other Government Departments, saying “the leadership and personal commitment being shown on this issue by the Minister for Health, Social Services and Public Safety is exemplary. … However, and despite the fact that the broader issue of suicide arguably touches upon the responsibilities of every single Stormont department, there is no discernible evidence of the inter-departmental commitment that the strategy envisages. It is difficult to avoid the conclusion that the Northern Ireland Executive appears to regard suicide and suicide prevention solely as a health issue, when it is in fact far broader.”[101] The Committee for Social Development also called for greater cross-departmental involvement saying “The Committee recognises that other departments and agencies should be involved in education campaigns, particularly the Department of Education and the Department for Employment and Learning, and would encourage strong cross-departmental working.”[102]
69. We welcome the establishment of the Ministerial Co-ordination Group on Suicide Prevention chaired by the Minister for Health, Social Services and Public Safety and involving a number of other Ministers. We urge the Executive to acknowledge that suicide prevention is not solely a health issue and to examine how the role of the Ministerial Group can be further developed to secure a greater commitment and involvement by all Departments.
Role of Schools and Colleges
70. A number of respondents, including the NI Commissioner for Children and Young People (NICCY) and BMA NI, pointed to the important role that schools have in helping young people to build self esteem, resilience and develop coping skills. NICCY stated that this was particularly important “in relation to young males who may find it difficult to articulate and deal with their feelings.”[103] BMA NI stated that “the educational sector is in an important position in the delivery of these much needed skills”[104].
71. Sharon Sinclair, Aware Defeat Depression, also highlighted the need for “action to equip people with the skills in problem-solving, conflict resolution and building self-esteem. Those skills can effect a significant change in help-seeking behaviour by those in psychological distress and can help to avoid the kind of progression into hopelessness that will often prompt suicidal behaviour. Again, we feel that such work must begin at school age and on a widespread basis.”[105] Aware Defeat Depression and Action Mental Health gave details of their work in schools which includes a depression-awareness programme for young people between the ages of 14 and 16. Colin Loughran, Action Mental Health, told the Committee “It used to be difficult to get into schools because teachers were afraid of the consequences of recognising the issue. However, there has been a significant increase in the number of schools that are prepared to allow organisations with expertise to conduct sessions and support their pupils.”[106]
72. The Committee noted a recent call by the Ulster Teachers’ Union for suicide awareness training for teachers ‘as they face a growing epidemic of mental health issues among pupils[107]. However, a representative of Family Voices cautioned that “child-protection issues put teachers in a delicate position. Often, when a child indicates that something is wrong, we cannot ask questions — the matter must immediately be passed on to designated personnel in the school. In many ways, teachers’ hands are therefore tied. As professionals, we often feel that we would like a little more scope to deal with situations. The pastoral system that is up and running in many schools is patchy and varies between schools. The action that is taken by a school depends on its principal and policies.”[108]
73. The Department of Education in its submission emphasised the priority it places on developing the emotional health and wellbeing of pupils and stated that work is underway to develop a ‘Pupils’ Emotional Health and Wellbeing Programme’ with the focus on the post primary sector. An independent counselling support service has been made available to all post primary schools from September 2007 with funding of £1.8m from the Children and Young People’s Funding package. Contact Youth was appointed in October 2006 to provide this counselling support to schools and the Department indicated that 95% of post primary schools have taken up the service. Other schools continue to use existing counselling services. The Department also stated that “A strategy for the provision of counselling is being provided and it is hoped that the service may in time be extended to primary schools to address issues with younger children, where appropriate”[109].
74. NICCY called for counselling services to be made available in all schools and emphasised that “it is essential … that any service is developed in consultation with children and young people to ensure that the service is designed to meet their needs”[110].
75. Rt Rev John Finlay said that the experience of pastoral care would indicate that “people are not coping in the same way as past generations may have done.”[111] This was borne out in other responses. NIAMH referred to a conclusion reached by number of international suicidologists that “by teaching young children how to cope with difficulties they should be able to handle problems and crises in adolescent and adult life. ….. Such an approach is essentially different to the pathogenic approach which seeks to identify children who have mental health problems or who are perceived as being especially vulnerable”[112].
76. We welcome the introduction of the independent counselling support service in post primary schools and call on the Minister for Education to extend this service to the primary sector as soon as possible. We also welcome the work that is underway to develop a Pupils’ Emotional Health and Wellbeing Programme for the post primary sector. However, we believe that developing coping skills and building young peoples self esteem should begin at an early age and we call on this programme to be extended to all schools.
77. The Department for Employment and Learning affirmed its full commitment to the Protect Life strategy and to continue to engage with the SSIB. The Department provided examples of initiatives that contribute to the mental wellbeing of students in further education and indicated that universities and teacher training colleges provide a counselling service for students.
78. We welcome a number of useful initiatives linked to the prevention of suicide and self harm currently being undertaken by the Department for Employment and Learning. These include the services provided by Opportunity Youth and Include Youth to young people on the Jobskills and Training for Success Programmes. We also recognise the value of the Bytes Project, jointly supported by the Department of Education, which targets ‘hard to reach’ young people who are not in education, employment or training. We call on the Department for Employment and Learning to review its contribution to implementing the Protect Life strategy and, in particular, to ensure that initiatives taking place in some FE colleges are available to all in that sector.
Role of Churches
79. The Committee for Social Development highlighted the fact that “Faith leaders are in a key position to provide guidance to those who present with suicide and self-harm tendencies and influence societal attitudes.[113]” This view was echoed by Mr Iain McGowan, on behalf of a multi-disciplinary group of clinicians, who stated “We strongly advocate the involvement of ministers and religious leaders and representatives of voluntary sector organisations in discussions about mental healthcare provision and suicide prevention work”.[114] Health and Social Services Councils also supported “the need for suicide and depression awareness training for all church and religious leaders”.[115]
80. When churches in general failed to respond to a request for written views on suicide prevention the Committee invited the leaders of the four main churches in Northern Ireland to give evidence. Bishop Patrick Walsh told the Committee that clergy are involved in three areas relating to suicide, “they are among the first to be called out to a suicide incident, which is a very harrowing experience. Secondly, they are then involved with the care of the families, and that is a most important part of pastoral ministry for all our churches. Thirdly, they are, very often, the first port of call for someone who is contemplating suicide, or who has indulged in some sort of self-harm. …. we are all very conscious of the need for them to be trained.”[116]
81. Rev Roy Cooper said “The Church’s role in suicide prevention may include as many efforts as possible to develop experiences of community. Indeed, for many in town and country, the Church is their basic community. There may be other initiatives, including co-operative working and being prepared to talk openly about suicide, thereby giving opportunity to challenge its perceived role as a solution to problems.”[117] Rev Cooper indicated that depression “headed the list of the most important issues the Church had to deal with”[118] and he highlighted the problem of isolation for young and old alike in rural areas.
82. Rt Rev Dr John Finlay told the Committee that “We are always willing and desirous to be a comfort and counsel to those who have suffered, especially the families. Perhaps our concern and our frustration is that, more often than not, people who take their own lives are very peripheral to our membership and association with the Church”[119].
83. Archbishop Harper spoke of his concern that “Societal change also includes problematic substance and alcohol abuse. There is significant evidence that that may be directly correlated with mental-health issues. When I speak of mental health, I do not want to suggest that suicide is merely a matter of mental ill health. It is not. To deal with it simply as a mental-health matter will address some, but by no means all, of the issues.”[120]
84. We welcome the commitment by the leaders of the four main churches in Northern Ireland to play their part in tackling the issue of suicide and self harm. We urge greater collaboration with the Suicide Strategy Implementation Body in the development and delivery of training for all clergy in dealing with people who may be at risk of suicide and in supporting families and communities in the aftermath of a suicide.
Role of Sport and Exercise
85. The beneficial effect of regular exercise, whether through organised sport or otherwise, on both physical and mental well-being is well established. Dr Kremer, Queens University Belfast, pointed out that “there is a positive correlation between exercise, self-esteem, self-efficacy, well-being in general and cognitive functioning; and a negative correlation with anxiety, stress and depression”[121]. He said “Critically, in relation to self-harm and suicide, there is an emerging literature that suggests that those who exercise are less prone to suicide attempts”.[122]
86. Dr Kremer explained that “Mood state, for example, responds well to certain types of exercise. ….. it is now well established that an effective treatment for depression — and most especially for clinical depression — is regular exercise. ... Anxiety has also been shown to respond well to exercise, especially programmes that last longer than 20 minutes”[123]. But he cautioned “it would be over-egging the case to say that exercise provides an answer to all the problems. It is more likely that exercise can act in combination with other interventions to help to stop people who are already heading down a suicide route.”[124]
87. Professor McCartan, Sport NI, advised the Committee that “there is clear empirical evidence … that GPs are prescribing exercise and physical activity as a remedy to deal with depression, anxiety and the continuum that leads to self-harm and suicide, rather than simply prescribing pills.”[125] But Dr Kremer pointed out that “A major culture shift is needed to recognise that GPs using exercise as a form of treatment is not a second-class option or a poor cousin. In a well-maintained and well-managed environment, that can be a long-term solution to many of those problems”[126].
88. Another issue identified by Dr Kremer is that those who are most likely to benefit from exercise are also likely to be those who are least inclined to take exercise. He argued that “Fresh thinking is needed to consider how to engage with those hard-to-reach, marginalised people. They need to be encouraged to engage in activities that they may well have been put off at an early age.”[127]
89. During the visit to Scotland the Committee learned that well-known sports personalities are being used there to encourage people, particularly young men, to talk about their feelings and to overcome the stigma relating to depression. Major sports occasions are also used to distribute literature encouraging people to talk about the issue. Professor McCartan, Sport NI, told the Committee that “The Scottish Parliament allocated sportscotland around £13 million from the health budget to help in the development and promotion of such programmes. We would seriously consider developing such a programme and promoting it at major international football matches in Windsor Park, at major rugby and Gaelic matches and at the North West 200. They are probably our four biggest crowd-pullers.”[128]
90. The Committee was concerned to learn that sports organisations were not involved in drawing up the suicide strategy and are not involved in the SSIB. Professor McCartan, Sport NI, told the Committee “To the best of my knowledge, we were not consulted on the strategy, but we are aware of it”[129].
91. The positive role of sport and exercise in combating stress, anxiety and depression is well established and widely recognised. We urge the Minister to explore how the prescribing of an exercise regime can be developed and promoted for use as an option by GPs in appropriate circumstances.
92. We are disappointed that Sport NI and the main sports bodies in Northern Ireland have not been directly involved in developing and delivering the strategy to prevent suicide. We call on the Minister for Health, Social Services and Public Safety to explore with the Minister for Culture Arts and Leisure how Sport NI and other sports organisations can fully participate in delivering the suicide strategy. We strongly commend the Scottish model of involving sports icons and using major sporting occasions to raise awareness of the issue and to encourage young people, particularly young men, to seek help.
Role of Local Authorities
93. Anne Donaghy, Antrim Borough Council, acknowledged that “Local government takes a keen interest in the Protect Life strategy” but when asked about the extent of local government involvement in developing the strategy she said “we could have added more. We submitted a paper, but we would have welcomed more open discussion”. Heather Moorhead, NILGA, told the Committee that “There is a massive role for local authorities, but their work is piecemeal”. Heather Moorhead summed up the involvement of District Councils in suicide prevention initiatives by saying that “some local authorities are doing a lot; others are doing something, while some are not doing anything”.
94. Anne Donaghy, Antrim Borough Council, spelt out what she saw as the important role for local Government saying “We can help to target resources and to ensure that those that are set aside for suicide prevention can be used more effectively. … local government has the ability to co-ordinate a streamlined partnership approach, in which we can connect organisations and individuals, such as the Churches and health professionals, who have an important role to play”[130]. She also identified specific ways in which existing local Government services could be used to help reduce suicide saying “We have rural connections; rural suicide is as big an issue as it is anywhere else, and it affects young and old. … We can channel our sports and leisure and community development resources”[131].
95. Anne Donaghy stressed that “local government wants to be involved in the implementation and evaluation of the Protect Life suicide strategy. We want to channel the capacity that exists — and the resource that is paid for — to the community and address the issue.”[132] NILGA called for a more proactive approach and proposed the setting up of a “working group with some of the other key providers … We want to define the type of role that we believe that local authorities could be playing and the things that we could be doing.”[133] She stressed that suicide “is not just a health issue: it is a societal public-health issue, and a solution cannot be arrived at with only a health mindset; a broader mindset is required”[134].
96. There is clear potential for local authorities to play a significant role in the ongoing development and delivery of the Protect Life strategy. We note the position in Scotland where local authorities are major partners in delivering the strategy and have appointed suicide co-ordinators in each area. While current participation is described as piecemeal many District Councils are keen to play their full part. We urge the Minister to explore with local authorities how solid partnerships can be developed. We believe that this should include full participation in the Suicide Strategy Implementation Body and other structures.
Services and Support
Training
97. The taskforce set up by the Department to draw up the suicide strategy identified the need for training and development, firstly for frontline health and social care staff, secondly additional training for others including health professionals, clergy, and those whose occupations may bring them into contact with people at risk of suicide, and thirdly the introduction of coping skills in schools. Subsequently the need “to provide appropriate training for people dealing with suicide and mental health issues” was identified as one of the key objectives of the strategy. The need for additional or improved training for all those who may come into contact with people at risk of suicide was a recurring theme of many of the submissions to the Committee.
ASIST Training
98. Dr Philip McGarry, Royal College of Psychiatrists, explained that “In the workplace, a great deal of work has been done using ASIST, which is Applied Suicide Intervention Skills Training, and that started in Canada, 20 years ago. … The two-day course is geared towards people such as youth leaders, community workers, police officers, fire services, and so forth. It educates people on how to identify any early warning signs shown by an individual and how to deal with that person. That training continues, and the voluntary and statutory sectors are doing good work rolling it out.”[135] Pat McGreevy, South Eastern Health and Social Care Trust, compared ASIST to CPR and said “Youth club leaders, teachers, bus drivers and the police have all been trained, and that training is continuing to spread. Those people are not therapists; they are first-aiders in suicide. The ASIST programme has been running for five years, and we must keep rolling it out.”[136] However, while much progress has been made it is clear that more is needed. Marie Osbourne, West Belfast Parent and Youth Support Group, told the Committee “My group has taken part in training with front-line medical staff in the Royal Group of Hospitals. Training must be provided, not only to doctors, but to receptionists, nurses and so on. The way that people are treated in the Mater Hospital is abominable.”[137]
99. Many respondents expressed concern about the uptake of training by GPs. For example, Rays Crisis Centre said “the GP education and training programme to increase detection of depression seems to be inadequate … Many GPs have been resistant to the ASIST training”[138]. The Niamh Louise Foundation put it bluntly saying “It is distressing that GPs are unwilling to avail of the training made available to them at present especially when they are the gatekeepers from the community to the mental health care system”[139]. At the outset of the Inquiry in September the Minister told the Committee “To date, 161 GPs have received training, and approximately another 200 will have received training before December 2007. In addition, 71 practice managers and nurses have received related training”[140].
100. Noel Graham, Northern Health and Social Services Council, highlighted the crucial importance of suicide and depression awareness training for all front-line staff dealing with people in distress, particularly GPs. He said “We have some concerns about the varying levels of uptake by GPs of this training: uptake in some areas has been slow”[141]. His colleague, Maggie Reilly, Western Health and Social Services Council, pointed to the 99% uptake among GPs in the Western Health and Social Services Board area and explained that “The Western Board addressed the issue of training by closing practices and introducing out-of-hours emergency care to provide services, so that GPs got protected time to train. Consequently, the uptake was extremely high, and we encourage other Boards to consider following that lead”[142].
101. Dr Maria O’Kane, Royal College of Psychiatrists stated that “ASIST is an excellent programme for the voluntary sector. Health professionals have told us that it is extremely good, but that they would like the next stage. One of the reasons that GPs find ASIST difficult to take up is that, like everything else, there are competing needs”[143]. Dr Tom Black, on behalf of the BMA admitted that “There were some initial problems, but the good news is that one third of all GPs have already been trained. … A GP will come across a patient who takes his or her own life only every six years, so it is a rare occurrence for a GP. It will happen about once every one or two years in a practice. We have bought into the training, because self-harm is common.”[144] The BMA in its written submission also expressed disappointment that medical professionals had not been involved in designing the awareness training programme.
102. Mr Colm Donaghy, Southern Health and Social Care Trust, explained that “The outcome of the General Practitioner Training programme provided through the Health Promotion Agency is as yet unclear. There is a need to assess the relevance, appropriateness and therefore uptake of the current training provision and to explore more fully if it is indeed addressing the real needs of General Practitioners. It is vital that General Practitioners are made more aware of what services are currently available in their respective communities and as a result encouraged to make referrals to these services for more sustained and longer term support.”[145]
103. Ms Sharon Sinclair, Aware Defeat Depression, stressed the need for on-going training in the longer term. She said “To appropriately support people at risk, targeted efforts are needed to enhance depression and suicide awareness among professional groups in health, education, human resources, the criminal justice system and so on. In the voluntary and community sectors, those initiatives need to be continued. A commitment to skills development of the kind that we have seen over recent years is equally important so that people can access appropriate training, including depression awareness, mental-health first aid, and ASIST (Applied Suicide Intervention Skills Training) programmes. In our view, they must remain as part of the long-term strategy.”[146]
104. Mr Colin Loughran, Action Mental Health, said “An evaluation has been completed for the Southern Health and Social Services Board area. ASIST was evaluated as a part of that. The indications are that ASIST is appropriate and helpful to front-line practitioners, but, for the general population, it may not be the most effective source of training. Something pitched at a lower level, aimed at a general understanding of mental and emotional health, would be more effective for the wider public.”[147]
Training for clergy and church workers
105. The Church Leaders agreed that training of clergy and church workers was a very significant issue for all of them. The Most Rev Alan Harper, Church of Ireland, pointed out that a survey of clergy a couple of years ago indicated that suicide was a major issue and many clergy felt “they were seriously under-resourced in dealing with it. … they needed to know how to recognise the signs of self-harming or suicidal behaviour, and to help subsequently in dealing with the outcomes, whether that involved dealing with survivors or bereaved families”[148]. Rev Harper also said that the clergy training programme was receiving a radical overhaul at the moment and that “Suicide awareness will be a significant component in that. However, that is only a forward projection. We have some structures in place, but they are insufficient for upskilling the clergy to deal with an issue that many of them will not have encountered face to face”[149]. Rev John McClure reported that funding for the Churches to train new and existing clergy was available through the SSIB.
Training for PSNI
106. Mr Pat McGreevy, South Eastern Health and Social Care Trust, highlighted that “Working with the police is crucial because, being the first on the scene, their attitude can affect a bereaved family and how they feel about help, and hope, in general. If a family experience an insensitive reaction from those first responders, it can put them off seeking help at all, so it is crucial that the police are aware of, and sensitive to, the needs of families”[150]. Mr McGreevy indicated that “A couple of initiatives are already in place in the Eastern Board area. We have developed a training programme for police officers that raises awareness about suicide, considers what can be done to intervene with people at risk and also deals with the issue of responding to bereaved families in a sensitive manner.”[151] Brendan Bonner, Western Health and Social Services Board, pointed to work taking place there with PSNI “to ensure that all officers likely to attend the scene of a suicide undertake ASIST training”[152]. Melanie McClements, Southern Health and Social Care Trust, said that engagement with PSNI in the Trust area had resulted in “the idea that we will influence the foundation training for new officers on the necessary skills. … The PSNI is working with us on inter-agency protocols, from the first response, to the media, funeral directors, the PSNI and our own service”[153].
107. The importance of training and development in suicide awareness, in identifying early warning signs and in knowing how to respond to those signs has been incorporated into the strategy. The merits of the ASIST (Applied Suicide Intervention Skills Training) programme are widely recognised. The range of people who will benefit from such training is extensive and includes not only frontline health and social care staff but also other health professionals, clergy, police and other emergency services, and those whose occupations could bring them into contact with people at risk of suicide. Many issues about training were raised during the Inquiry including concerns about the uptake of GP awareness training and calls for training to be extended to other groups, for example, clergy, teachers and all staff who work in A&E departments. We believe that the time is right to examine and evaluate the progress of the training programme to date and identify any gaps.
Telephone Helpline
108. The Department launched a pilot 24/7 suicide prevention telephone helpline in October 2006 in North and West Belfast and explained that it “specifically targets young people and is supported by additional peer mentoring and counselling services”[154]. There was a general recognition from respondents that the helpline was “an important and accessible contact in providing an initial crisis response”[155]. The Southern Health and Social Care Trust argued that it needed to be “more widely targeted at addressing the needs of all communities across the province and not just those within one specific geographical area. In addition, it is essential that these services establish more effective links with local service providers thus improving their ability to signpost those in need to appropriate, locally based services”[156]. Some including the Committee for Social Development called for it to be “extended throughout Northern Ireland as a matter of urgency”[157].
109. However, others including Pat McGreevy, Suicide Coordinator in the South Eastern HSC Trust, urged caution. He argued that “A 24/7 suicide helpline should become a regional resource for people of all ages but only when a proper review of the pilot has been undertaken and if no other alternative models are considered to be more effective”[158]. The Niamh Louise Foundation also urged care saying “it is important to rethink how it can be rolled out in the rural areas and how the advertising and follow up procedures are addressed”[159].
110. On 31 January 2008 the Minister announced the launch of a regional suicide prevention helpline across Northern Ireland and described it as “a key element in meeting the objectives of the Suicide Prevention Strategy’ and stated “I will ensure that the helpline is evaluated during its first year to ensure that it is meeting its objectives”[160].
111. Representatives of community groups and bereaved families expressed very serious concerns that the helpline had been expanded without an evaluation of the north and west Belfast pilot and that proper back-up services are not yet in place. Michael Doherty, West Belfast Suicide Awareness and Support said “We are asking for the back-up services that are needed in the community. … the Minister went ahead and tendered for a new regional helpline in the absence of a proper evaluation. I know that the helpline does good work, but concerns about it have been raised constantly. However, those services do not exist. A strategy must be adopted to ensure that adequate services will be set up. Let us not build up people’s expectations”[161].
112. Philip McTaggart, PIPS, supported this position pointing out that 15 months after the pilot was set up no evaluation has been carried out. He said “I am not suggesting that that helpline does a bad job. It has good elements, but it also has weaknesses. …. Had an evaluation of the pilot scheme been carried out, weaknesses might have been discovered and corrected. … We are finding that, after taking a call, the helpline will ring us and refer a client to us for help. We already have waiting lists; we are snowed under.”[162] Vincent Donaldson, West Belfast Suicide Awareness and Support, said “The helpline is not ready to go regional yet …We are in favour of a 24-hour helpline, but it has to be properly managed. If it is not, death will be the result. ... The problem that we had with it was that there were a lot of faults during the pilot period, and, all of a sudden, before it has been evaluated, it is being expanded.”[163]
113. The Samaritans stated that the pilot itself was announced “against the advice of Samaritans in the early days of the action plan. It duplicates much of our own long established and respected service and for Samaritans this is a disappointment. Having come forward early in the development of the strategy to offer our support and with the benefit of our 50 plus years of experience we feel that there is little benefit to the NI population by creating another helpline”[164]. Suzanne Costello, Samaritans, told the Committee “The phone line … has aspects that our service does not provide, but there are significant areas of overlap and there could be better synergy if we were able to work more closely with the Department”[165].
114. The Minister in a written response to the Committee explained that he “decided to establish a regional 24/7 crisis response helpline because of the high volume of calls to the pilot, which was receiving in the region of 100 calls per day. Approximately half of these were from outside the N&W Belfast area, which clearly indicated the growing demand from elsewhere in Northern Ireland. … My judgement was that action was needed at a regional level”[166].
115. The launch of the regional helpline has been relatively low key and witnesses attending the Committee after the launch, including local suicide coordinators, were themselves unsure of the helpline telephone number. Mr Brendan Bonner, coordinator with the Western Health and Social Services Board, acknowledged that “there is much debate about it being rolled out before it has been evaluated, but at least it will be a service that people can contact.”[167] Mr Pat McGreevy, South Eastern Health and Social Care Trust coordinator, suggested “Perhaps the Health Promotion Agency for Northern Ireland (HPA) could be tasked with promoting and publicising the helpline as part of its strategy.”[168] The church leaders were aware of the helpline but not the number and Archbishop Harper suggested that it needed a title similar to ChildLine with which everyone was familiar. He said “the new helpline must have a strap line that communicates its services to young people — a trigger that enables people to act according to their needs at a particular time. If it is to be described as something along the lines of ‘a suicide and self-harm helpline’, we may forget the whole thing.”[169] Martin Bell, DHSSPS, admitted that “we are aware of the present lack of publicity. As we speak, a substantial advertising campaign is being developed, which will soon go live”[170].
116. During the visit to Scotland the Committee was briefed on the ‘Breathing Space’ helpline in use there. The issue of such a helpline being accessible to young people through mobile phones and other modern media was highlighted and the Committee learned that the Breathing Space helpline is supported by four of the major mobile phone providers in Scotland.
117. We have major concerns that the decision to extend the pilot telephone helpline in north and west Belfast into a regional helpline at this time was rash. We believe that a number of key issues should have been fully addressed before any decision was taken to go live. These include
-
a thorough evaluation of the pilot in north and west Belfast to learn lessons from that experience;
-
a detailed assessment of whether adequate referral and support services are in place to cope with a significant increase in calls;
-
detailed discussion with the Samaritans to avoid duplication and to develop a strong working partnership; and
-
consideration of additional sources of support and funding, for example, from mobile phone providers as has happened in Scotland.
We believe that the regional helpline should have an easily identifiable title, such as ‘lifeline’ and that the launch should have been accompanied by a high profile media awareness campaign. However, we would now urge caution about a high profile publicity campaign until an assessment of the adequacy of existing referral and support services has been carried out.
Self-Harm service
118. The BMA stated that “the average age of onset of self-harm is 12 years. A two-year national inquiry carried out by the Camelot Foundation and Mental Health Foundation found that self-harm is an issue that is poorly understood, even among professionals and school staff, and that treatment is often inappropriate, for example focusing on the self-harm rather than the underlying causes.”[171] Dr Tom Black, BMA, told the Committee that “In the year after a self-harm incident, there is a 1% possibility of a person’s attempting suicide, but that percentage rises to 3% to 4% within five years. Therefore, we should focus on the self-harm group and ensure that they receive follow-up care”[172]. This approach was supported by the Royal College of Psychiatrists which argued that “if we specifically target those who have harmed themselves, which is a high-risk group, we could do a lot of good.”[173]
119. Dr Philip McGarry, Royal College of Psychiatrists, pointed to the National Institute for Health and Clinical Excellence (NICE) guidelines on self harm produced in 2004 which recommends the care and treatment services for people who self harm and includes the need for psychosocial assessment. Dr McGarry also referred to a major audit being carried out by the Royal College of Psychiatrists, the Royal College of Nursing, the Faculty of Accident and Emergency Medicine, and the Ambulance Service. He concluded that “We are improving on what we can do, but we are not doing enough, because there are insufficient resources to provide a full assessment and follow-up for those who have harmed themselves”[174].
120. The Committee visited a temporary project on self harm provided by a team at the Mater Hospital, Belfast and led by Dr Maria O’Kane, Chairperson of the NI Faculty of Psychotherapy. The team provides evidence based and structured treatment for people who self harm, particularly those who repeat self harm or traditionally have not engaged with any service. It also provides expertise, support, supervision and education for mental health care professionals, the voluntary sector, users and carers to better understand and help those who self-harm. The team reported that a comprehensive psychiatric assessment is therapeutic and reduces the likelihood of repetition by 50%.
121. The Committee learned about an initiative launched recently in the Western Health and Social Services Board area to collect data on self harm. The aim is to develop and pilot a self harm register in local A&E departments in keeping with the Protect Life Suicide Strategy. This register is being developed jointly with the National Suicide Research Foundation in the Republic of Ireland.
122. We are greatly concerned about the lack of focus on providing psychosocial assessment and follow-up care for those who self-harm. We welcome the pilot self-harm service in north and west Belfast and call for it to be evaluated urgently and extended to all A&E departments.
Talking Therapies
123. The Royal College of Psychiatrists called for more talking therapies or psychotherapy. Dr Philip McGarry explained that “Psychotherapy relieves emotional distress through the use of a talking technique. … Psychotherapy moves beyond counselling in that it is very much about the therapist trying to understand the individual and get to the root of the problem, and enabling a person to use that analysis to help themselves. Historically, the provision of psychotherapeutic services in Northern Ireland has not been as good as it should have been.”[175] A number of respondents, including Professor Hugh McKenna, University of Ulster, the Law Centre (NI), and the East Belfast Mission also called for increased availability of psychological therapies. The Law Centre (NI) argued that there was a need for “an increase in provision and education on the benefits of ‘talking therapies’ including but not limited to cognitive behaviour therapy”[176]. The Committee for Social Development expressed concern about the “lack of access to psychiatric services including psychotherapeutic treatments”[177].
124. Dr McGarry, Royal College of Psychiatrists, explained the potential benefits of talking therapies saying “it is relatively rare for patients to have straightforward depression. … other factors will also be involved — their family or home situation, work issues, educational and employment issues, debt, alcohol, and so on. ... it takes a great deal of time to work on those. However, the evidence shows that, if the effort is put in, good results can be achieved”[178].
125. The Department in its submission pointed out that “The Bamford Review acknowledged that psychological therapies are an important tool and should be routinely considered as an option when treating mental health problems. As an initial step to developing a strategy to improve access to psychological therapies, the Department has commissioned a mapping of existing training in and provision of psychological therapies.”[179]
126. The Committee noted that in October 2007 the health secretary, Alan Johnson, announced a major investment of £170m for psychological therapy services to treat 900,000 patients with depression and anxiety in England over the next three years. This was seen as a Government commitment to implement the National Institute for Health and Clinical Excellence (NICE) guidelines for depression and anxiety disorders by ensuring that everyone who needs it will have access to psychological therapy.
127. Dr Bernie Stuart, DHSSPS, told the Committee “In response to the recommendations of the Bamford Review, and as a result of the money that we received from the comprehensive spending review, we have a significant amount to invest in the development of psychotherapies. The process of developing a psychotherapy strategy is ongoing, and we hope to have it ready later this year. In advance of that, targets have been set — by March 2009, no patients should have to wait for more than 13 weeks from when they are referred to when they get access to psychotherapy treatment.”[180]
128. There is an urgent need for greater access to talking therapies to treat people with depression and anxiety disorders. We welcome the assurance of a significant investment in psychotherapies and the development of a psychotherapy strategy and we call for this to be implemented without delay.
Experience Elsewhere
129. Professor Kevin Malone, Professor of Psychiatry in University College Dublin, pointed out that “much can be learned from the response to suicide statistics in other countries. For example, Finland has experienced a significant reduction in suicide deaths over the past fifteen years. Their approach was extremely methodical and focused particularly on early recognition of treatment of depression and alcohol problems, as the major planks of their strategy.”[181] Professor Hugh McKenna, Queens University Belfast, referred to similarities between the suicide rate among older people in Northern Ireland and Poland. The Department clearly recognises the benefits of learning from experience elsewhere and advised that a Five Nations Joint Working Forum involving Northern Ireland, Republic of Ireland, Wales, Scotland and England, has been established “to facilitate the sharing of best practice between the nations and enhance co-operation on mutually beneficial areas of work.”[182]
130. The Department and the National Office for Suicide Prevention in Dublin both pointed to the detailed cross border co-operation that is taking place and highlighted the all-island action plan on suicide prevention. The National Office stated “there are substantial advantages to joint working not least the cost effectiveness of combining resources and not reinventing actions already taken. We can learn from each others experience of implementation. Indeed, we can and are learning from our UK and worldwide colleagues”[183].
131. Dr Paul Corcoran, National Suicide Research Foundation in the Republic of Ireland, provided the Committee with details of a proposed all-Ireland research inquiry into suicide which is being developed with the Department in Northern Ireland. As part of this a cross-border pilot self-harm register in A&E departments is being established.
132. We welcome and recognise the value of co-operation between countries at a strategic level on issues relating to the prevention of suicide. We note the positive links with Scotland in the development of the Northern Ireland Strategy, the ongoing work of the Five Nations Joint Working Forum, and the all-island action plan on suicide prevention. The Committee fact finding visits to Scotland and the Republic of Ireland also highlighted that there are often many lessons to be learned from ground-breaking and innovative services that are pioneered and developed at a local level. For example, in Scotland we were greatly impressed by the energy and enthusiasm of a number of local projects in Ayrshire such as ‘bibliotherapy – read yourself well’, a walking project, and school based drama activities. In Dublin we visited Pieta House a model community-based centre for those who have attempted to take their own lives or who have engaged in self-harm. Pieta House is an exceptionally good example of best practice and we urge the Department to consider how it could be replicated in Northern Ireland. We call on the Minister to consider, perhaps through the Five Nations Forum, how information on innovative activities at a local level can be shared between countries.
133. We strongly recommend that the Minister set up a separate dedicated Protect Life website similar to the Choose Life website in Scotland. We believe that this would provide a key resource to augment implementation of the strategy. It would be a useful point of contact on sources of help, support and guidance and could include links to publications, such as annual reports, media guidelines, research, and statistics, as well as acting as a bulletin board to facilitate links between all those working in the area of suicide prevention and bereavement support.
Other Issues
Role of Media
134. The role of the media was highlighted by the Royal College of Psychiatrists which stated “There is an abundance of international evidence that shows the role the media has in combating the stigma of mental health problems, but also the risk of triggering suicide through irresponsible reporting or portrayal”[184]. The Department acknowledged that “the media also has a role to play in preventing suicide. Research shows that how suicide and related issues is portrayed in the media can have a huge impact on the issue”[185]. The Minister told the Committee that he met with editors of newspapers and television “not to point out deficiencies but to see how we can help them and how they can work with us. They have a duty to report, and we must look at how we give them the information to allow them to do that”[186].
135. The Samaritans and the Irish Association of Suicidology have developed media guidelines aimed at those reporting suicide in any media from factual description to dramatic portrayal. The guidelines briefly outline suicide facts, media myths, signs of suicide risk and offer recommended phrases to use when talking about suicide. Anthony Langan, Samaritans, told the Committee “We will be examining new media guidelines some time this year, and we will also consider the issue of new media and the Internet to explore how we can build in some guidance for people making use of those services”[187]. Pat McGreevy, Suicide Coordinator, South Eastern Health and Social Care Trust welcomed the media guidelines but cautioned that “a structure needs to be put in place to ensure regular ‘reminders’ and a permanent method of ‘policing’ media reports on suicide deaths”[188].
136. Colm Donaghy, Chair of the SSIB, reported that the “implementation body and the Department are examining a facility called Media Watch, which we will pay to monitor how the print, television and radio media deal with incidents of suicide. If they deal with it improperly we will raise the matter and make complaints. … Unfortunately, we have found that the media respond but fall into old ways when getting a story; the difficulty for us is to ensure that we sustain media interest in suicide prevention and how they report suicide. Research shows that if the media report responsibly, we will prevent some suicides”[189].
137. Headline, a national media monitoring programme, working to promote responsible and accurate coverage of mental health and suicide related issues within the media, was launched in the Republic of Ireland in April 2007. Suzanne Costello, Samaritans, pointed to the benefits of such monitoring saying “There were some horrendous breaches of the guidelines after the suicides of two young men in Omagh last year. The difficulty for charities taking up those breaches individually is that they are subsequently penalised by the papers, and it becomes very difficult for an individual charity to take that on. Headline comprises a group of charities and people working in the mental-health and suicide-prevention field who feel that when problems are tackled as a group, its voice is much stronger.”[190]
138. The Minister reported that he also met with internet providers last year to discuss the need to clamp-down on social networking sites which are being used to promote suicide among young people. He has now joined forces with the Department of Health in England which is taking forward a UK Government review of internet sites which encourage suicide.[191]
139. We strongly support calls for more responsible reporting of suicide and related issues in the media and we welcome the action taken by the Minister to engage with the local media. We particularly welcome and support the initiative by the Minister to tackle the issue of internet sites that promote suicide. We call for a Northern Ireland version of Headline, a media monitoring programme, to be established and implemented as soon as possible.
Public Information Campaign
140. The Health Promotion Agency (HPA) set out details of a major public information campaign, commissioned by the Department and launched in March 2007, which is aimed at de-stigmatising mental health, promoting awareness and understanding of issues relating to mental health and suicide. The HPA explained “The campaign approach was two fold, a broad population based approach targeted at all age groups entitled Its Me and a targeted campaign for young men aged 16-24 yrs entitled Share It. There were a number of aspects to the campaign including mass media TV ads, Radio ads, posters, leaflets and a newsletter outlining the key campaign messages. … The HPA has also been working closely with colleagues in HSE and the National Office for Suicide Prevention in RoI in the development of the Public Information Campaign and both ads have been shown in the Republic of Ireland”[192].
141. However, community groups expressed concerns about the approach adopted. For example, the Rays Crisis Centre argued that the campaigns “have been oriented towards mental health instead of suicide and self harm – money has been taken from the Suicide and Self Harm budget and used for advertising mental health only. This has lead to an ineffective advertising campaign. The advertising campaign needs to have ‘impact’ to begin to address the area of suicide and self harm.”[193] The Southern Health and Social Care Trust acknowledged that it “has focused on a Mental Health Promotion message rather than directly addressing the issue of suicide. Whilst it is acknowledged that there is a need to avoid a sensationalist and “scare mongering” approach there is a need to balance this with an ability to begin a direct debate and dialogue about suicide within our wider community.”[194] The Law Centre NI also cautioned about the need to ensure that “such campaigns are closely monitored in order to determine effectiveness” and argued that “if there are insufficient support services on the ground to assist people who respond to public campaigns the success will always be limited”[195].
142. We recommend that the current general mental health media campaigns be subjected to a robust evaluation and that urgent consideration be given to how the specific issue of suicide and self harm can best be addressed through a public media campaign.
Chill out Room
143. In July 2007, before the commencement of the Inquiry, the Committee met with representatives of families bereaved by suicide. At the meeting Mary Creaney as argued that “lost opportunities at accident and emergency departments can be fatal, especially for those with alcohol or drug problems, as they are six times more likely to die as a result of suicide. She called for a place of safety or a ‘chill out room’ to be provided in A&E departments “until a proper assessment can be conducted on those who present themselves because of self-harm or suicidal tendencies”[196]. She suggested that “volunteers could sit with them until they were well enough to have a psychiatric assessment” and pointed to examples of best practice on this issue in other parts of the UK and in the USA. The Committee subsequently explored this issue during the Inquiry.
144. The Minister indicated that he was sympathetic to the idea of providing “space in A&E departments where a patient who is presenting in crisis can be taken”[197]. Dr Tom Black, BMA NI, supported the proposal saying “We must have that open-arms attitude and take those young people down a different path, because they often present in crisis, often with what we might consider to be behavioral problems and often with alcohol consumed. Dedicated areas in A&E units would be a good idea.”[198] Dr Maria O’Kane, Royal College of Psychiatrists, said that this has been considered at both the Mater Hospital and the Royal Victoria Hospital but that “they are confined by space. We started by trying to identify a space within the A&E department where a person could be assessed quietly without fear of interruption, and with solid walls instead of curtains. Finding such a space is a challenge in itself. Those two A&E departments have worked very hard with us to try to achieve that. Things are far from perfect, but they are better than they were.”[199]
145. We recognise the critical opportunity that is provided to influence the lives of people who present in crisis at A&E departments of hospitals. We call on the Department to require Boards and Trusts to carry out an urgent examination of ways in which a chill-out room can be provided in or adjacent to all A&E departments in hospitals.
Card Before You Leave
146. Mr Gerard McCartan, PIPS, highlighted a problem relating to follow up appointments for those who self harm or who are at risk of suicide and suggested a simple solution. He said “When someone is discharged after admission to a psychiatric ward, he or she must wait for a letter detailing an appointment to be posted to them. Sometimes, the letter does not arrive, and people cannot understand why the hospital does not simply give them an appointment card, because a confirmed appointment is a lifeline to people who are being treated and to their carers”[200]. When asked about the ‘card before you leave’ proposal the Department explained that it is “aware of major issues concerning the use of hospitals in a crisis situation and has work under way to examine crisis intervention in accident and emergency departments. … we will consider the Committee’s suggestion when developing guidance on those services”[201].
147. We recommend the urgent introduction of a ‘card before you leave’ system to provide people at risk of suicide or self-harm who attend A&E departments or who are discharged from hospital with a definite follow-up appointment.
Communication
148. Mr McCartan referred to an independent review into the tragic death of his son Danny by suicide in 2005. That report published in June 2007 found that there had been “a distinct lack of communication across the interfaces culminating in the poor transition arrangements when Danny was moved between services”[202]. Mr McCartan claimed that this has not changed. He said “When Danny was in Knockbracken, his records did not go to the Mater Hospital as they should have. When the Belfast Health and Social Care Trust was established, it stated that such an occurrence would not happen again. However … the same thing is still happening.” The Committee also noted that poor communication was the major factor in the circumstances surrounding the deaths of Madeleine and Lauren O’Neill[203]. In response Dr Bernie Stuart, DHSSPS, said “The issue of poor communication has been raised in many independent inquiries. We are considering the issue in a more general way. Apart from reinforcing the existing guidance, we are considering how to train people to communicate better.”[204]
149. We are greatly concerned that lessons about the need for better communication highlighted in a number of reports have not been implemented. We fully support the recommendations in the O’Neill Report in relation to communication.
Support for frontline staff
150. The Committee recognises that frontline staff who have to deal directly with incidents of suicide may themselves need support and counselling. In Scotland the Committee met with Rev Roddy McNidder, who leads a Critical Incident Stress Management Team in Ayrshire and Arran NHS. The team has been set up to provide a structured system of care to reduce the adverse reactions that can often occur following a critical incident. In the Northern Ireland context Dr Philip McGarry, Royal College of Psychiatrists, acknowledged that “Doctors are at a higher risk of suicide than average members of the population. That is a well-recognised fact. ...Psychiatrists and anesthetists are also prone to that higher risk. In the past, that was ignored. We are dealing with that better than we did in the past. There is some support out there, and that is something that we must examine. As part of the work of the task force, we looked at particular risk groups. We mentioned farmers as a particularly high-risk group, although we did not mention healthcare staff. We are not always great at looking after ourselves.”[205]
151. We recognise that healthcare and other frontline staff are themselves at increased risk of suicide and we recommend that urgent consideration be given to the establishment of a structured system of care and support similar to that in place in Ayrshire and Arran NHS.
Conclusion
152. The publication of the Protect Life: a shared vision suicide prevention strategy in October 2006 was the culmination of an extensive consultation exercise and represented a major advance in the efforts to reduce the needless loss of life through suicide in Northern Ireland. The strategy incorporated lessons learned from international best practice and involved a close working relationship with Scotland and the Republic of Ireland. However, the development of the strategy is just the first step and it requires ongoing concerted action to achieve results.
153. We identified a number of areas where we believe the strategy can be enhanced and improved. We believe structures could be strengthened by the establishment of a designated suicide prevention directorate as part of the proposed new Regional Public Health Agency, similar to the National Office for Suicide Prevention in the Republic of Ireland. We are calling for the central focus of the strategy on ‘at risk’ groups to be expanded to include older people and those living in rural areas.
154. One of our major concerns is that eighteen months after its introduction a proper evaluation of the key elements of the strategy has not taken place. In particular, we have grave concerns about the decision to introduce a regional telephone helpline at this time without learning the lessons from the pilot exercise.
155. The level of stakeholder involvement is considerable and there are currently over 40 members of the Suicide Strategy Implementation Body. We believe that two other major sectors have a significant contribution to make to the delivery of the strategy and should be included, namely, local authorities and sporting bodies.
156. The important role that bereaved families and community groups currently play and the empathy and understanding that they bring to the issue cannot be overstated. We commend the courage and dedication of all those involved.
157. One of the guiding principles of the Protect Life strategy is a development of links to other relevant strategies. We believe that an opportunity now exists to strengthen the links with mental health services through the forthcoming implementation of the recommendations in the Bamford Review of Mental Health and Learning Disability, particularly so in relation to the development of Child and Adolescent Mental Health Services.
[1] Volume 1, Appendix 2, Paragraph 138
[2] Volume 2, Appendix 3, Page 215
[3] Volume 2, Appendix 3, Page 382
[4] Volume 2, Appendix 3, Page 391
[5] Volume 2, Appendix 3, Page 466
[6] Volume 1, Appendix 2, Paragraph 480
[7] Volume 2, Appendix 3, Page 355
[8] Volume 2, Appendix 3, Page 369
[9] Volume 2, Appendix 3, Page 424
[10] Volume 2, Appendix 3, Page 227
[11] Volume 2, Appendix 3, Page 401
[12] Volume 1, Appendix 2, Paragraph 1041
[13] Volume 1, Appendix 2, Paragraph 353
[14] Volume 1, Appendix 2, Paragraph 522
[15] Volume 2, Appendix 3, Page 221
[16] Western Health and Social Services Board publication Mentoring Pilot to Improve Life for those who Self-Harm (July 2006)
[17] Volume 1, Appendix 2, Paragraph 315
[18] Volume 2, Appendix 3, Page 281
[19] Volume 2, Appendix 3, Page 617
[20] Volume 2, Appendix 3, Page 218
[21] Volume 1, Appendix 2, Paragraph 142
[22] Volume 1, Appendix 2, Paragraph 149
[23] Registrar General Northern Ireland (2007) Registrar General Northern Ireland Annual Report 2006, Northern Ireland Statistics and Research Agency: 21.
[24] Registrar General Northern Ireland (2007) Registrar General Northern Ireland Annual Report 2006, Northern Ireland Statistics and Research Agency: 21.
[25] Figures obtained from the Northern Ireland Statistics and Research Agency (NISRA).
[26] Registrar General Northern Ireland (2007) Registrar General Northern Ireland Annual Report 2006, Northern Ireland Statistics and Research Agency: 21.
[27] O’Reilly, D., Rosato, M., Connolly, S. and Cardwell, C. (2008) ‘Area factors and suicide: 5-year follow-up of the Northern Ireland population,’ The British Journal of Psychiatry, 192: 106-111.
[28] DHSSPS (2007) Submission to the Inquiry, DHSSPS: 58.
[29] DHSSPS (2007) Submission to the Inquiry, DHSSPS: 66.
[30] DHSSPS (2006) Protect life: a shared vision - Northern Ireland suicide prevention strategy and action plan 2006–2011, DHSSPS: 7.
[31] World Health Organisation (1999) Figures and Facts About Suicide, Geneva: WHO.
[32] Figures obtained from the Sa maritans website at: http://www.samaritans.org/about_samaritans/facts_and_figures/uk_and_roi_suicide_information.aspx
[33] Department of Health (2002) National Suicide Prevention Strategy for England, Department of Health.
[34] Hawton, K. and Fagg, J. (1987) Attempted Suicide: A Practical Guide to its Nature and Management, Second edition, Oxford: Oxford University Press cited in D.Duffy and T. Ryan (eds.) (2004) New Approaches to Preventing Suicide – A Manual for Practitioners, London: Jessica Kingsley Publishers.
[35] Figures illustrated here were obtained from the World Health Organisation website.
[36] When considered on an annual basis the national suicide rate (combining the suicide and undetermined death rates) in Northern Ireland was 12.4 per 100,000 people in 2005 and 16.7 per 100,000 in 2006. These figures were provided by NISRA.
[37] Figures illustrated in this graph were obtained from the Samaritans website accessed at: http://www.samaritans.org/about_samaritans/facts_and_figures/facts_about_suicide.aspx - The figures were collected from a number of statutory agencies in each jurisdiction including the Office for National Statistics (England and Wales), General Register Office Scotland, The Northern Ireland Statistics and Research Agency and the Central Statistics Office (Republic of Ireland).
[38] DHSSPS (2006) Protect Life: A Shared Vision – The Northern Ireland Suicide Prevention Strategy 2006-2011, DHSSPS: 13.
[39] According to the World Health Organisation (WHO) parasuicide is defined as ‘an act with non-fatal outcome, in which an individual deliberately initiates a non-habitual behaviour, without intervention from others, will cause self-harm and which is aimed at realising changes which the subject desired via the actual or expected physical consequences’.
[40] DHSSPS (2007) Submission to the Inquiry, DHSSPS: 74.
[41] Figures obtained from the Hospital Information Branch, DHSSPS.
[42] Volume 2, Appendix 3, Page 368
[43] Volume 2, Appendix 3, Page 614
[44] Volume 2, Appendix 3, Page 458
[45] DHSSPS (2006) Protect life: a shared vision - Northern Ireland suicide prevention strategy and action plan 2006–2011, DHSSPS
[46] Volume 1, Appendix 2, Paragraphs 527 & 528
[47] Volume 2, Appendix 3, Page 368
[48] Volume 2, Appendix 3, Page 478
[49] Volume 2, Appendix 3, Page 215
[50] Volume 2, Appendix 3, Page 370
[51] Volume 2, Appendix 3, Page 267
[52] Volume 2, Appendix 3, Page 271
[53] Volume 2, Appendix 3, Page 496
[54] Volume 2, Appendix 3, Page 248
[55] Volume 2, Appendix 3, Page 253
[56] Volume 2, Appendix 3, Page 419
[57] Volume 1, Appendix 2, Paragraph 1339
[58] Volume 1, Appendix 2, Paragraph 827
[59] Volume 2, Appendix 3, Page 233
[60] Volume 1, Appendix 2, Paragraph 1222
[61] Volume 2, Appendix 3, Page 499
[62] Volume 2, Appendix 3, Page 499
[63] Volume 1, Appendix 2, Paragraph 615
[64] DHSSPS Press Release ‘31 January 2008 – Regional suicide prevention helpline launched’
[65] Volume 2, Appendix 3, Page 634
[66] Volume 2, Appendix 3, Page 615
[67] Based on exchange rate of €1.18 at 18 April 2008
[68] Briefing to the Committee by the Minister of State, Dr Jimmy Devins TD, in Dublin on 21 February 2008.
[69] Volume 2, Appendix 3, Page 616
[70] Volume 2, Appendix 3, Page 616
[71] Deputy Jan O’Sullivan, Vice Chairperson, Joint Committee on Health and Children, 21 February 2008
[72] Volume 1, Appendix 2, Paragraph 616 & 617
[73] Volume 1, Appendix 2, Paragraph 623
[74] Volume 1, Appendix 2, Paragraph 1550
[75] Volume 1, Appendix 2, Paragraph 1555
[76] Volume 2, Appendix 3, Page 495
[77] Volume 2, Appendix 3, Page 617
[78] Volume 2, Appendix 3, Page 495
[79] Volume 2, Appendix 3, Page 617
[80] Volume 2, Appendix 3, Page 233
[81] Volume 2, Appendix 3, Page 248
[82] Volume 2, Appendix 3, Page 247
[83] Volume 2, Appendix 3, Page 397
[84] Volume 2, Appendix 3, Page 255
[85] Volume 2, Appendix 3, Page 390
[86] Volume 2, Appendix 3, Page 397
[87] Volume 2, Appendix 3, Page 248
[88] Volume 2, Appendix 3, Page 390
[89] Volume 1, Appendix 2, Paragraph 967
[90] Volume 2, Appendix 3, Page 419
[91] Volume 2, Appendix 3, Pages 385 & 386
[92] Volume 2, Appendix 3, Page 496
[93] Volume 2, Appendix 3, Page 253
[94] Volume 1, Appendix 2, Paragraph 851
[95] Volume 1, Appendix 2, Paragraph 850
[96] Volume 1, Appendix 2, Paragraph 778
[97] Volume 1, Appendix 2, Paragraph 779
[98] Volume 1, Appendix 2, Paragraph 33
[99] Volume 2, Appendix 3, Page 233
[100] Volume 1, Appendix 2, Paragraph 55
[101] Volume 2, Appendix 3, Page 282
[102] Volume 2, Appendix 3, Page 400
[103] Volume 2, Appendix 3, Page 246
[104] Volume 2, Appendix 3, Page 366
[105] Volume 1, Appendix 2, Paragraph 862
[106] Volume 1, Appendix 2, Paragraph 943
[107] ‘Union calls for training as suicide levels soar’, Belfast Telegraph, 14 March 2008
[108] Volume 1, Appendix 2, Paragraph 771
[109] Volume 2, Appendix 3, Page 544
[110] Volume 2, Appendix 3, Page 246
[111] Volume 1, Appendix 2, Paragraph 1040
[112] Volume 2, Appendix 3, Page 644
[113] Volume 2, Appendix 3, Page 400
[114] Volume 2, Appendix 3, Page 268
[115] Volume 1, Appendix 2, Paragraph 1325
[116] Volume 1, Appendix 2, Paragraphs 1027, 1028, 1029 & 1030
[117] Volume 1, Appendix 2, Paragraph 1034
[118] Volume 1, Appendix 2, Paragraph 1035
[119] Volume 1, Appendix 2, Paragraph 1038
[120] Volume 1, Appendix 2, Paragraph 1052 & 1053
[121] Volume 1, Appendix 2, Paragraph 1387
[122] Volume 1, Appendix 2, Paragraph 1386
[123] Volume 1, Appendix 2, Paragraph 1388
[124] Volume 1, Appendix 2, Paragraph 1392
[125] Volume 1, Appendix 2, Paragraph 1410
[126] Volume 1, Appendix 2, Paragraph 1407
[127] Volume 1, Appendix 2, Paragraph 1445
[128] Volume 1, Appendix 2, Paragraph 1398
[129] Volume 1, Appendix 2, Paragraph 1400
[130] Volume 1, Appendix 2, Paragraphs 1454 & 1458
[131] Volume 1, Appendix 2, Paragraph 1460
[132] Volume 1, Appendix 2, Paragraph 1462
[133] Volume 1, Appendix 2, Paragraph 1494
[134] Volume 1, Appendix 2, Paragraph 1496
[135] Volume 1, Appendix 2, Paragraph 230
[136] Volume 1, Appendix 2, Paragraph 1262
[137] Volume 1, Appendix 2, Paragraph 638
[138] Volume 2, Appendix 3, Page 398
[139] Volume 2, Appendix 3, Page 272
[140] Volume 1, Appendix 2, Paragraph 12
[141] Volume 1, Appendix 2, Paragraph 1324
[142] Volume 1, Appendix 2, Paragraph 1343
[143] Volume 1, Appendix 2, Paragraph 253
[144] Volume 1, Appendix 2, Paragraphs 331 & 334
[145] Volume 2, Appendix 3, Page 386
[146] Volume 1, Appendix 2, Paragraph 863
[147] Volume 1, Appendix 2, Paragraph 937
[148] Volume 1, Appendix 2, Paragraph 1055
[149] Volume 1, Appendix 2, Paragraph 1056
[150] Volume 1, Appendix 2, Paragraph 1243
[151] Volume 1, Appendix 2, Paragraph 1244
[152] Volume 1, Appendix 2, Paragraph 1239
[153] Volume 1, Appendix 2, Paragraphs 1245 & 1246
[154] Volume 2, Appendix 3, Pages 496 & 497
[155] Volume 2, Appendix 3, Page 459
[156] Volume 2, Appendix 3, Page 386
[157] Volume 2, Appendix 3, Page 400
[158] Volume 2, Appendix 3, Page 420
[159] Volume 2, Appendix 3, Page 271
[160] DHSSPS Press Release ‘31 January 2008 – Regional suicide prevention helpline launched’
[161] Volume 1, Appendix 2, Paragraphs 634 & 635
[162] Volume 1, Appendix 2, Paragraphs 696, 697 & 698
[163] Volume 1, Appendix 2, Paragraphs 637, 719 & 720
[164] Volume 2, Appendix 3, Page 635
[165] Volume 1, Appendix 2, Paragraph 882
[166] Volume 2, Appendix 3, Page 540
[167] Volume 1, Appendix 2, Paragraph 1257
[168] Volume 1, Appendix 2, Paragraph 1277
[169] Volume 1, Appendix 2, Paragraph 1163
[170] Volume 1, Appendix 2, Paragraph 1552
[171] Volume 2, Appendix 3, Page 363
[172] Volume 1, Appendix 2, Paragraph 316
[173] Volume 1, Appendix 2, Paragraph 139
[174] Volume 1, Appendix 2, Paragraph 140
[175] Volume 1, Appendix 2, Paragraph 144 & 146
[176] Volume 2, Appendix 3, Page 423
[177] Volume 2, Appendix 3, Page 399
[178] Volume 1, Appendix 2, Paragraphs 147 & 148
[179] Volume 2, Appendix 3, Page 501
[180] Volume 1, Appendix 2, Paragraph 1538
[181] Volume 2, Appendix 3, Page 227
[182] Volume 2, Appendix 3, Page 498
[183] Volume 2, Appendix 3, Page 232
[184] Volume 2, Appendix 3, Page 220
[185] Volume 2, Appendix 3, Page 499
[186] Volume 1, Appendix 2, Paragraph 124
[187] Volume 1, Appendix 2, Paragraph 918
[188] Volume 2, Appendix 3, Page 419
[189] Volume 1, Appendix 2, Paragraph 585
[190] Volume 1, Appendix 2, Paragraph 922
[191] DHSSPS Press Release ‘20 March 2008 – Positive discussions on internet providers and suicide risks – McGimpsey’
[192] Volume 2, Appendix 3, Page 470
[193] Volume 2, Appendix 3, Page 398
[194] Volume 2, Appendix 3, Page 386
[195] Volume 2, Appendix 3, Page 425
[196] Families Bereaved by Suicide, 5 July 2007 (Hansard) http://archive.niassembly.gov.uk/health/2007mandate/moe/070705b.htm
[197] Volume 1, Appendix 2, Paragraph 58
[198] Volume 1, Appendix 2, Paragraph 326
[199] Volume 1, Appendix 2, Paragraph 171
[200] Volume 1, Appendix 2, Paragraph 738
[201] Volume 1, Appendix 2, Paragraph 1522
[202] Final Report of an Independent Review Panel of the Eastern Health and Social Services Board: Complaint made by Mr and Mrs McCartan, June 2007 (Anonymised version)
[203] Report of the Independent Inquiry Panel to the Western and Eastern Health and Social Services Boards – May 2007: Madeleine and Lauren O’Neill
[204] Volume 1, Appendix 2, Paragraph 1537
[205] Volume 1, Appendix 2, Paragraphs 289 & 291
Appendix 1
Minutes of Proceedings
Thursday, 13 September 2007
Room 135, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mrs Elaine Farrell (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Mark McQuade (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Miss Michelle O’Neill MLA
The meeting commenced at 2.39 pm in closed session.
2. Suicide and Self Harm
The Committee agreed to put the Healthcare Associated Infections Inquiry on hold while it conducted an urgent inquiry into the current strategic approach to the prevention of suicide and self harm.
The meeting moved into public session at 2.57 pm
[EXTRACT]
Thursday, 20 September 2007
The Board Room, Craigavon Area Hospital
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Ms Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mrs Elaine Farrell (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Mark McQuade (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Mr John McCallister MLA
12. Inquiry on Suicide – Draft Terms of Reference
Agreed: the Draft Terms of Reference for the Inquiry on Suicide as amended.
Agreed: a Draft Press Release for the Inquiry on Suicide as amended.
Members noted that the Minister will attend the Committee meeting on 4 October 2007 to provide an update on the work of the Ministerial Co-ordination Group on Suicide and deal with other issues.
Agreed: to undertake a visit to Scotland in November in connection with the Inquiry on Suicide.
[EXTRACT]
Thursday, 4 October 2007
The Senate Chamber, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Rev Robert Coulter MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallaher MLA
Mr John McAllister MLA
Ms Carál Ní Chuilín MLA
Ms Michelle O’Neill MLA
Ms Sue Ramsey MLA
In Attendance:
Mrs Debbie Pritchard (Principal Clerk)
Mr Hugh Farren (Clerk)
Mrs Elaine Farrell (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Mark McQuade (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Mrs Carmel Hanna MLA
5. Evidence Session with the Minister for Health, Social Services and Public Safety
The Minister was accompanied by:
Dr Andrew McCormick Permanent Secretary
Dr Miriam McCarthy Director of Secondary Care
Mrs Patricia Osborne Health Development Directorate
Members were briefed on the Department’s Suicide Strategy and work on the Ministerial Co-ordination Group on Suicide.
A question and answer session ensued. The Minister and officials agreed to report back on a number of issues raised in relation to the Suicide Strategy.
[EXTRACT]
Thursday, 18 October 2007
Room 135, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallaher MLA
Mrs Carmel Hanna MLA
Mr John McAllister MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mrs Elaine Farrell (Assistant Clerk)
Mrs Judith Murdoch (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Mark McQuade (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Ms Michelle O’Neill MLA
1. Evidence session with the Royal College of Psychiatrists
Members took evidence from the following:
Dr Philip McGarry Consultant Psychiatrist
Dr Maria O’Kane Chair of NI Faculty of Psychotherapy
Dr Peter Gallagher Chair of NI Child and Adolescent Faculty
Anne XXXXX Mater Hospital Service User
A questions and answer session ensued. The Chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 15 November 2007
The Board Room,
Northern Ireland Hospice Care
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallaher MLA
Ms Michelle O’Neill MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Ms Ruth Barry (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Mrs Carmel Hanna MLA
The meeting commenced at 2.12 p.m. in private session
The meeting Moved to public session at 3.04 p.m.
2. Suicide Inquiry - Evidence session with the British Medical Association
Members took evidence from the following:
Dr Tom Black Deputy Chairman BMA NIGPC
Mr Danny Lambe Deputy Secretary BMA (NI)
Mr Ivor Whitten Assembly & Research Officer
A questions and answer session ensued. The Chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 29 November 2007
Room 135, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Ms Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallaher MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
Rev Robert Coulter MLA
Mrs Carmel Hanna MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mrs Elaine Farrell (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Miss Ruth Barry (Clerical Officer)
5. Committee Inquiry into the Prevention of Suicide and Self Harm
Evidence session with the Rural Community Network and the Niamh Louise Foundation.
Members took evidence from:
Raymond Craig Oakleaf Rural Support Network
Michele Baird South Antrim Rural Support Network
Catherine McBennett Niamh Louise Foundation
James McBennett Niamh Louise Foundation
2.50 p.m. Mr John McCallister arrived.
3.05 p.m. Mr Tommy Gallagher left the meeting.
3.25 p.m. Mr Tommy Gallagher returned to the meeting
A question and answer session ensued. The Chairperson thanked the witnesses for attending.
3.36 p.m. Mr Thomas Buchanan left the meeting.
3.38 p.m. Ms Sue Ramsey left the meeting.
3.38 p.m. Ms Carál Ní Chuilín left the meeting.
Evidence session with the Southern Health and Social Care Trust
Members took evidence from:
Mr Colm Donaghy Chief Executive, SHSCT
Mr Francis Rice Director of Mental Health and Disability Services
3.48 p.m. Mr Carál Ní Chuilín returned to the meeting.
3.55 p.m. Ms Sue Ramsey returned to the meeting.
4.00 p.m. Mrs Carmel Hanna left the meeting.
A question and answer session ensued. The Chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 10 January 2008
Everton Complex, Ardoyne Road, Belfast
Present:
Ms Michelle O’Neill MLA (Deputy Chairperson)
Ms Carál Ní Chuilín MLA
Mr Alex Easton MLA
Ms Sue Ramsey MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Apologies:
Mrs Iris Robinson MP MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Thomas Buchanan MLA
Rev Robert Coulter MLA
Mr Tommy Gallagher MLA
The meeting commenced at 2.28 p.m. in public session with the Deputy Chairperson in the Chair.
6. Committee Inquiry into the prevention of Suicide and Self Harm
Members took evidence from the following witnesses:
Jo Murphy PIPS Project.
Philip McTaggart PIPS Project.
Marie Osborne West Belfast Suicide Awareness.
Vincent Donaldson Suicide Awareness Support Group.
Roberta Coates Rays Crisis Centre.
Phyllis McDoal Rays Crisis Centre.
Michael Doherty Lenadoon Community Counselling.
Seamus McCabe PIPS Project, Newry & Mourne.
Gerard McCartan PIPS Project.
Maureen Young Northern Health Board Area.
Robert Doyle The Association of Mental Health new Northern Ireland Children’s enterprise,
West Belfast Suicide Awareness Support Group.
Bobby Cosgrove South & East Belfast Families Bereaved through Suicide.
Ann McGarrigle North West Bereaved by Suicide group.
A questions and answer session ensued. Members agreed to write to the Department for Social Development regarding the renewal of funding for community based groups. The Chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 31 January 2008
Room 135, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Ms Carál Ní Chuilín MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
In Attendance:
Mr Kevin Shiels (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Mr John McCallister MLA
Ms Sue Ramsey MLA
The meeting commenced at 2.35 p.m. in public session.
6. Committee Inquiry into the Prevention of Suicide and Self Harm
Evidence session with representatives of Action Mental Health, the Samaritans and Aware Defeat Depression
Members took evidence from the following witnesses:
Anthony Langan Public Affairs Manager, Samaritans
Suzanne Costello Director for Ireland, Samaritans
Colin Loughran Action Mental Health
Sharon Sinclair Chief Executive, Aware Defeat Depression
A questions and answer session ensued. The Chairperson thanked the witnesses for attending.
4.05. p.m. Mr Tommy Gallagher rejoined the meeting
4.12. p.m. Ms Michelle O’Neill left the meeting
4.22. p.m. Ms Carál Ní Chuilín left the meeting
4.27. p.m. Ms Michelle O’Neill rejoined the meeting
4.28. p.m. Mrs Carmel Hanna left the meeting
Evidence session on research into Suicide.
Members took evidence from the following witnesses:
Mr Mike Tomlinson Queens University, Belfast
Mr Iain McGowan University of Ulster
A questions and answer session ensued. The Chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 7 February 2008
Senate Chamber, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
The meeting commenced at2.36 p.m. in public session.
5. Committee Inquiry into the Prevention of Suicide and Self Harm
Evidence session with Church Leaders
Members took evidence from the following witnesses:
Rev Roy Cooper President Methodist Church in Ireland
Rev Dr John Finlay Moderator, Presbyterian Church
Archbishop Alan Harper OBE Church of Ireland Archbishop of Armagh
Bishop Patrick Walsh Roman Catholic Bishop of Down and Connor
Mr Lindsay Conway Director for Social Services, Presbyterian Church
Rev John McClure Church of Ireland
Dr Oliver Woods Advisor to Bishop Walsh
A questions and answer session ensued. The Chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 28 February 2008
Senate Chamber, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Dr Robert Coulter MLA
The meeting commenced at 2.39 p.m. in public session.
5. Committee Inquiry into the Prevention of Suicide and Self Harm
Evidence session with Local Suicide Coordinators
Members took evidence from the following witnesses:
Brendan Bonner Western Health & Social Services Board
Melanie McClements Southern Health & Social Care Trust
Pat McGreevy South Eastern Health & Social Care Trust
Gabrielle Nellis Northern Health & Social Services Board
A questions and answer session ensued. The Chairperson thanked the witnesses for attending.
3.20 p.m. Mr John McCallister joined the meeting.
3.33 p.m. Ms Sue Ramsey left the meeting.
3.53 p.m. Mrs Carmel Hanna left the meeting.
3.57 p.m. Ms Sue Ramsey rejoined the meeting.
4.15 p.m. Mrs Iris Robinson left the meeting.
4.15 p.m. Ms Michelle O’Neill took the Chair
4.15 p.m. Mr Tommy Gallagher left the meeting.
4.22 p.m. Mr Tommy Gallagher rejoined the meeting
4.26 p.m. Ms Carál Ní Chuilín left the meeting.
4.29 p.m. Ms Carál Ní Chuilín rejoined the meeting
6. Committee Inquiry into the Prevention of Suicide and Self Harm
Evidence session with Dr Dermot O’Reilly, Queens University
Members took evidence from Dr Dermot O’Reilly, Queens University.
A questions and answer session ensued. The Deputy Chairperson thanked Dr O’Reilly for attending.
[EXTRACT]
Thursday, 13 March 2008
Senate Chamber, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr John McCallister MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Mrs Carmel Hanna MLA
Ms Carál Ní Chuilín MLA
The meeting commenced at 2.35 p.m. in public session.
5. Committee Inquiry into the Prevention of Suicide and Self Harm Evidence session with Sport NI
Members took evidence from the following witnesses:
Professor Eamonn McCartan CEO, Sport NI
Dr John Kremer Queens University, Belfast
A question and answer session ensued. Professor McCartan agreed to send the Committee a copy of research carried out by Dr Murphy. The Chairperson thanked the witnesses for attending.
3.08 p.m. Mr Tommy Gallagher joined the meeting.
6. Committee Inquiry into the Prevention of Suicide and Self Harm Evidence session with the Health and Social Services Councils
Members took evidence from the following witnesses:
Noel Graham Chief Officer, Northern Health & Social Services Council
Maggie Reilly Chief Officer, Western Health & Social Services Council
The Chairperson apologised for the evidence session previously being postponed at short notice. A question and answer session ensued. The Chairperson thanked the witnesses for attending.
3.34 p.m. Ms Sue Ramsey left the meeting.
3.56 p.m. Ms Sue Ramsey rejoined the meeting.
3.56 p.m. Mr John McCallister rejoined the meeting.
4.02 p.m. Mr Tommy Gallagher left the meeting.
4.12 p.m. Mr Thomas Buchanan joined the meeting.
[Extract]
Thursday, 3 April 2008
Senate Chamber, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
The meeting commenced at 2.34 p.m. in public session.
5. Committee Inquiry into the Prevention of Suicide and Self Harm Evidence session with NILGA
Members took evidence from the following witnesses:
Heather Moorhead Chief Executive, NILGA
Sean McPeake Vice President, NILGA
Anne Donaghy Director Environmental Services, Antrim Borough Council
The Chairperson apologised for the evidence session previously being postponed at short notice. A question and answer session ensued. The Chairperson thanked the witnesses for attending.
3.14 p.m. Ms Carál Ní Chuilín left the meeting.
3.14 p.m. Ms Carál Ní Chuilín rejoined the meeting.
3.23 p.m. Mr John McCallister joined the meeting.
6. Committee Inquiry into the Prevention of Suicide and Self Harm Evidence session with Departmental officials
Members took evidence from the following witnesses:
Andrew Elliot Director of Population Health Directorate
Dr Bernie Stuart Director of Mental Health & Disability Services Directorate
Gerard Collins Health Improvement Policy Branch
Martin Bell Health Improvement Policy Branch
Officials agreed to send the Committee information on the Training of Accident and Emergency staff. The Chairperson thanked the witnesses for attending
3.38 p.m. Mr Tommy Gallagher left the meeting.
3.52 p.m. Mrs Carmel Hanna joined the meeting.
3.53 p.m. Mr Tommy Gallagher rejoined the meeting.
3.54 p.m. Dr Kieran Deeny left the meeting.
3.57 p.m. Dr Kieran Deeny rejoined the meeting.
4.07 p.m. Mr Tommy Gallagher left the meeting.
4.15 p.m. Mr Tommy Gallagher rejoined the meeting.
[EXTRACT]
Thursday, 17 April 2008
Room 135, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Michelle O’Neill MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Ms Hilary Bogle (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
The meeting commenced at 2.34 pm. in public session.
7. Consideration of draft Report on the Committee Inquiry into the Prevention of Suicide and Self Harm
4.27pm Mr Tommy Gallagher left the meeting.
4.3 pm Ms Sue Ramsey left the meeting.
4.42pm Mr Tommy Gallagher returned to the meeting.
4.46pm Ms Sue Ramsey returned to the meeting.
The Committee considered paragraphs 1 – 56 of the Draft Report.
[EXTRACT]
Thursday, 24 April 2008
Room 135, Parliament Buildings
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Dr Kieran Deeny MLA
Mr Tommy Gallagher MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Sue Ramsey MLA
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Mrs Carmel Hanna MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
The meeting commenced at 2.32 p.m. in public session.
3.52 p.m. the Committee adjourned.
4.06 p.m. the Committee resumed in closed session.
7. Consideration of draft Report on the Committee Inquiry into the Prevention of Suicide and Self Harm.
The Committee noted a report on the Committee visit to Dublin and agreed that this be included in an appendix to the Committee report.
The Committee considered the draft report from paragraph 57 to the end of the report.
4.44 p.m. Mr John McCallister rejoined the meeting.
4.52 p.m. Ms Sue Ramsey left the meeting
4.52 p.m. Mr Tommy Gallagher left the meeting
4.57 p.m. Ms Sue Ramsey left the meeting
4.57 p.m. Ms Carál Ní Chuilín left the meeting
Members agreed a Committee motion to have the report debated and approved by the Assembly.
[EXTRACT]
Thursday, 1 May 2008
Knockbracken Hall,
Knockbracken Healthcare Park
Present:
Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Dr Kieran Deeny MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Carál Ní Chuilín MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
In Attendance:
Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies:
Rev Robert Coulter MLA
Ms Sue Ramsey MLA
The meeting commenced at 2.34 p.m. in public session.
4.44 p.m. the Committee adjourned.
4.50 p.m. the Committee resumed in closed session.
8. Consideration of draft Report on the Committee Inquiry into the Prevention of Suicide and Self Harm.
The Committee considered the Draft report on the Inquiry into the Prevention of Suicide and Self Harm paragraph by paragraph. The Committee agreed the main body of the report:
Paragraphs 1 – 3, read and agreed
Paragraphs 4 – 13, read and agreed
Paragraphs 14 - 22, read and agreed
Paragraphs 23 – 56, read and agreed
Paragraphs 57 - 96, read and agreed
Paragraphs 97 – 128, read and agreed
Paragraphs 129 – 133, read and agreed
Paragraphs 134 – 151, read and agreed
Paragraphs 152 – 157, read and agreed
The Committee agreed the Executive Summary
The Committee agreed the Summary of recommendations
The Committee agreed that Appendix 1 to 5 be included in the report.
The Committee agreed that an extract of today’s Minutes of Proceedings should be included in Appendix 1 of the report and were content that the Chairperson agrees the minutes relating to this to allow them to be included in the printed report.
The Committee agreed that a printed copy of the report be sent to each of the witnesses who gave oral evidence and those organisations who made written submissions to the inquiry
The Committee ordered the Report on the Inquiry into the Prevention of Suicide and Self Harm to be printed.
[EXTRACT]
Appendix 2
Minutes of Evidence
4 October 2007
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Rev Dr Robert Coulter
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Mr Michael McGimpsey |
The Minister of Health, Social Services and Public Safety |
|
Dr Miriam McCarthy |
Department of Health, Social Services and Public Safety |
1. The Chairperson (Mrs I Robinson): The Committee welcomes the Minister of Health, Social Services and Public Safety and his officials: Dr Andrew McCormick, who is the Department’s permanent secretary; Dr Miriam McCarthy, who is the director of secondary care; and Ms Patricia Osborne, who is from the health development directorate.
2. The evidence session will consist of two elements: we shall first discuss the inquiry into the prevention of suicide and self-harm in Northern Ireland, and that will be followed by a discussion on other issues. The Minister is not yet in a position to propose an urgent amendment to The Children (Northern Ireland) Order 1995, so that item of business has been left off the agenda.
3. Further to the Committee’s decision to conduct an urgent inquiry into the prevention of suicide and self-harm, the Minister has been requested to brief the Committee on the Department’s strategy, particularly on the work of the ministerial co-ordination group on suicide prevention. Members should note that the Assembly’s Research Service has prepared a paper on that strategy.
4. I invite the Minister to brief the Committee on the suicide-prevention strategy and the work of the ministerial co-ordination group.
5. The Minister of Health, Social Services and Public Safety (Mr McGimpsey): Thank you. Before I start, and in response to remarks about carers and the Caring for Carers strategy, I must state that I am happy to discuss mutual interests with colleagues on the mainland. However, this is a devolved matter, so we are not bound by what is decided in England. We are taking our own strategic approach, which is based on a comprehensive consultation exercise; raising awareness of carers’ issues and addressing the deficit in information; introducing legislation, structures and procedures; developing monitoring arrangements to offer assurances that carers are being identified; and the necessity to expand and improve the range of services that are available to carers. That is a rough synopsis of the current situation.
6. The Assembly debated the Caring for Carers strategy on 25 June 2007. That matter is of interest to the Assembly and the wider public, and correspondence relating to it continually appears in my mailbag.
7. I am delighted to be here. This is the second time that I have attended a meeting of the Committee for Health, Social Services and Public Safety Committee in my capacity as Minister, and I look forward to a fruitful discussion.
8. I welcome the Committee’s inquiry. The background to this serious and tragic problem, which affects everyone in our society, is that the previous Administration developed a suicide-prevention strategy, and a suicide strategy implementation body (SSIB) was set up in September 2006 to deal with that. That approach must be constantly reassessed, and it is important to state that there is no quick fix. This is a challenging matter, which requires concerted cross-sector work. In 2006, there were 291 recorded instances of suicides. That stark figure that does not begin to reflect the individual tragedy that lies behind each death.
9. From the outset, I accept that mental-health services are not good enough. That is a big issue in Northern Ireland, where needs are 25% greater than in England, even though our spend is approximately 25% less pro rata.
10. The recently completed Bamford Review of Mental Health and Learning Disability (Northern Ireland) was a major exercise that was conducted over several years. It investigated Northern Ireland’s mental-health and learning-disability requirements, and contains more than 60 recommendations.
11. In 2007-08, £3 million was allocated to the suicide-prevention strategy, of which £1·8 million was invested to support communities. The suicide strategy implementation body includes key stakeholders, bereaved families and local communities. That body began with a series of actions: a self-harm mentoring scheme was established in the Western Health and Social Service Board area; a pilot suicide-prevention 24/7 telephone helpline was established in north and west Belfast; and research began into the effects of the Troubles on mental health and suicide rates. We are all aware of having come from a period of more than 25 years of conflict, which played a part in our figures and in suicide rates.
12. A GP depression-awareness training programme has been launched. To date, 161 GPs have received training, and approximately another 200 will have received training before December 2007. In addition, 71 practice managers and nurses have received related training. All GPs have received the related CD-ROM training package. There has been a joint North/South public information campaign, and we are working with the media to encourage responsible and sensitive reporting. Ireland-wide media guidelines are in place. We have been working with key website providers, with whom I have met. That meeting was facilitated by the Home Office, because it is primarily its responsibility. I anticipate that further meetings will take place because of Internet involvement in adolescent suicides.
13. In June 2007, I established the Mental Health and Learning Disability Board, which is chaired by Professor Roy McClelland. The board’s prime roles are to champion the Bamford Review’s recommendations and to challenge my Department and me on the implementation of those recommendations. Its first piece of work is to consider the underlying causes of suicide, and it is doing that in conjunction with the Queen’s University research and development department.
14. I have also instructed that the pilot telephone helpline should go throughout Northern Ireland. The helpline has proved to be seriously oversubscribed, so it must be expanded throughout Northern Ireland, as must the self-harm mentoring scheme.
15. Alcohol and drugs misuse is a factor. In the United States, for example, one third of all adolescent suicide attempts involve intoxication. There is a clear relationship between suicide and alcohol and drugs, but we are not sure exactly what that is. We know that alcohol plays a role by removing inhibitions, and I am considering a way forward. Drugs are illegal, so their misuse is a law and order issue, but alcohol is licensed. We are looking at ways in which to make progress in that area through our drugs and alcohol task force. The impact that such substances have on young people in crisis is a significant factor in suicide attempts.
16. There is also cross-jurisdictional work. A five nations group that deals with suicide has been established that comprises England, Wales, Scotland, the Republic of Ireland and Northern Ireland. That group will continue to meet — its next meeting is on 12 November. An all-island action plan has been developed. I am meeting representatives from the Department of Health and Children in Dublin, including my counterpart Mary Harney, Dr Jimmy Devins and Pat the Cope Gallagher, to discuss ways in which to advance the all-island action plan.
17. The Executive have established a ministerial co-ordination group on suicide prevention, which I chair. It includes the Minister of Education and both junior Ministers. That was established in June 2007 to enhance cross-departmental co-ordination. It has met twice and is due to meet again on 16 October 2007.
18. The group has discussed a range of issues, including irresponsible reporting, bullying, evaluation, support in schools, drop-in centres, additional support for parents and the effect of the Internet. It is considering ways in which to take make progress on those matters, as well as on mental-health promotion and services, the implementation of the Bamford Review, and so on.
19. That is a quick résumé of work that the Department has done on suicide prevention. As I have said, I welcome the Committee’s inquiry into the prevention of suicide and self-harm, because suicide and self-harm can affect society right across Northern Ireland. Every single life that is lost to suicide is a precious one. The situation is made more poignant by the fact that the suicide rate has almost doubled during the past four years. The increase in the number of suicides has been among young people and adolescents. Therefore, suicide prevention is currently the burning mental-health issue.
20. The Chairperson: Thank you, Minister, for that brief outline of the Department’s work. Before we kick-start discussions, I want to flag up a few issues. This morning, I took a tour of the psychiatric nursing unit (PNU) at Ards Hospital and saw the abysmal provision of services there. Conditions there are so bad that a patient who came to the unit with minor depression would be more depressed when he or she left.
21. Clinicians at the unit take short-term relief from the fact that they hope, in 18 months’ time, to move to the Ulster Hospital site. However, that will be only an interim move. They tell me that they need a purpose-built facility for the treatment of people with a variety of mental-health problems, particularly self-harmers and those who contemplate suicide.
22. The Committee has seen two excellent facilities. One is already up and running near to Altnagelvin Area Hospital, and the other is in the late stages of completion in the grounds of Craigavon Area Hospital. They are both excellent models. Therefore, I wonder why money is being wasted. I do not suggest that money should not be spent on the care of individuals who present with mental-health problems. However, various professionals, who were glad that the Minister would be in Committee to hear the point that I am about to make, told me this morning that it would be more cost-effective to provide a purpose-built facility and to bypass temporary solutions. I am aware that a business case is being made at present. Mental health comes under the third phase of that business case.
23. Does the group that is considering the roll-out of the Bamford Review include people who have suffered as a result of suicide tragedies? Has there been any professional input other than from those who were tied to the review?
24. Mr McGimpsey: Both the Chairperson and I visited the McKelvey building this morning.
25. The Chairperson: You did not have to do that, Minister. The meeting was supposed to be private.
26. Mr McGimpsey: I am from Newtownards. I had my tonsils taken out in the McKelvey building 40 years ago.
27. The Chairperson: As did I.
28. Mr McGimpsey: The building has not changed since then. I was shocked to see its condition. I agree with you on that, Chairperson. The necessary investment has not been made, and that is a matter of regret to me. It is, however, part of the plans to implement the Bamford Review’s recommendations.
29. The model at Craigavon Area Hospital, which I have visited, is an example of good practice in design and build.
30. However, consultant Jim Anderson said this morning that offering care in the community and supported living to individuals means that they do not become institutionalised. We must give people the support that they need in sheltered accommodation outside of institutions. That is Jim Anderson’s number-one priority. I have seen examples of the type of supported-living development that is required.
31. There will, of course, always be a need for acute beds, and there is a plan to move from the McKelvey building to a refurbished part of the Ulster Hospital. The consultant was at pains to say that he saw that as a temporary move, and we both agreed with him, Chairperson. A business case is due, and I will examine that. I am bound by the three-year comprehensive spending review (CSR), not simply on resources and revenue but on capital spend. Now that I have seen the need for care in the community, I will have no compunction in moving forward immediately if I have the resources, although investment is anticipated from the CSR bid, as well as capital spend.
32. The mental health and learning disability board comprises four mental-health professionals and two people from learning-disability services. The board is a strategic oversight group that knows Bamford intimately, and it exists to challenge the Department on the implementation of the Bamford Review’s recommendations. As I have said, the board will act as champions for the sector and is led by Professor Roy McClelland.
33. Families who have been bereaved by suicide play a key part in the suicide strategy implementation body, which is chaired by Colm Donaghy. There are a number of key stakeholders, but the representatives of bereaved families and communities play a very important role, because they have intimate first-hand knowledge of the consequences of suicide — not just of the event but of living with it afterwards.
34. The Chairperson: Thank you for that detailed response.
35. Mr Easton: I am pleased with what you have outlined today, Minister, but there are a few issues on which I would like reassurance.
36. I am pleased that you will be working with the education sector. Can you assure me that there will be someone in each school who can identify possible mental-health problems early, and step in straight away? It is obvious that prevention is better than cure.
37. Can you advise me of what plans you have for prisoners in Northern Ireland? There seems to be very little that can be done if a prisoner with a mental-health issue does not consent to help, and, going on meetings that I have had recently, there seems to be a high level of mental-health problems in the prison population.
38. Can you assure me that you will consider educational programmes that will help GPs and doctors to identify mental-health problems, perhaps through a yearly one-day course? Although doctors receive training on mental-health issues when they go through medical school, a refresher course would draw their attention to the use of early prevention measures. People sometimes return time and again to accident and emergency (A&E) departments with the same problem, and that can be an indication that there is an underlying mental-health problem. If an A&E doctor could identify that problem, he could fill in the form that goes back to a GP after a hospital visit, and the GP could follow that up by ascertaining whether help is required.
39. Mr McGimpsey: The Minister of Education has taken steps to ensure that someone, who may not be a teacher, can take responsibility in each school. That is what is anticipated, as I understand it.
40. The mental health of prisoners is currently the Northern Ireland Office’s responsibility. That responsibility is due to pass to the Department of Health, Social Services and Public Safety in the near future. Paul Goggins and I have discussed that handover and the resources that are allocated to prisoners. Those resources will not begin to meet their physical- or mental-health needs, so that must be addressed.
41. Ms Patricia Osborne (Department of Health, Social Services and Public Safety): My understanding is that a counsellor is present in all post-primary schools for half a day every week. The Department is working closely with the Department of Education to devise a mental-health first-aid training programme to enable teachers to deal with mental-health issues. That is my understanding. I cannot clarify that now, but I will find out more for the Committee.
42. The Prison Service was represented in the development of the suicide prevention strategy, and it is also represented on the implementation group. The Prison Service examined its suicide and self-harm policy, which was revised on foot of recommendations from a number of reports, including that of Professor McClelland in 2006. The suicide strategy implementation body is aware of that, and it is working with the Prison Service on that issue.
43. Mr Easton: Do GPs receive any suicide-awareness training or yearly refresher courses?
44. Mr McGimpsey: There is ongoing GP awareness training, and some GPs, practice managers and practice nurses have participated in that. Such training is also being rolled out to A&E staff, because people who are troubled are likely to attend A&E departments. We are not entirely content that those who present at A&E receive the necessary sympathy. A CD-ROM has been produced that addresses that issue, and has been widely circulated throughout the profession. A refresher course is a useful suggestion, and I will take advice on that. We must keep this issue to the fore and on the agenda so that the professionals who work on the front line can facilitate a proper and fast response, ensuring early intervention.
45. The Chairperson: The House of Commons Northern Ireland Affairs Committee is coming to speak to the Health Committee on 16 October about mental-health issues in the Prison Service.
46. Ms S Ramsey: I welcome the Minister and his team, and I welcome his personal commitment to the prevention of suicide and self-harm. Alex mentioned GP awareness training, but families who have been bereaved through suicide are concerned about the take-up of such training. Minister, you said that 161 GPs have participated in that training, and 200 GPs are to receive it before Christmas. What is the shortfall? When the families who had been bereaved through suicide appeared before the Committee, they stated that that was one of their concerns.
47. I wish to raise some other issues, such as the whether a chill-out room — for want of a better term — should be provided in health centres and hospitals for those presenting with problems who may have drink or drugs in their systems.
48. Such people are sometimes not examined. A room should be made available in hospitals and health centres so that those people are not refused treatment or told to go away.
49. I turn to the subject of the availability of beds for children and adolescents. Answers to written questions that I have sent you indicate that there will be additional beds. However, we must deal with the current situation. We are investing for the future, but temporary solutions must be put in place to deal with the present.
50. There is also concern about the issue of under-18s using antidepressants. That matter arose during the investigation into the death of Danny McCartan. Many under-18s were continuously being prescribed antidepressants.
51. Minister, despite the commitment to additional funding that you made during your presentation — £1·8 million in 2007-08 to go directly to communities — my colleagues and I have met a number of community groups that are concerned about the future of long-term funding. Some of that funding is piecemeal; some comes from DSD and some from your Department. However, community groups cannot plan ahead or become involved in proactive strategies because they are wasting much of their time trying to secure additional funding or to safeguard their own funding.
52. I welcome the ministerial co-ordination group on suicide prevention, which you said also involves the Minister of Education and the OFMDFM junior Ministers. As you stated — and as we are all aware — statistics show that the majority of people who take their own lives are young men. Therefore, I am concerned that there was no mention of the Department for Employment and Learning during your presentation. Should DEL not have a role in the ministerial group, given the connection between higher and further education, and the social demographic most likely to commit suicide?
53. It was mentioned that less money is spent on mental-health issues here than in England. Can you guarantee that that situation will change after the Budget and comprehensive spending review?
54. Mr McGimpsey: I have placed a three-year bid for funding as part of the CSR and I am arguing my case. It is for my Executive colleagues to accept or reject the case that I make for prioritising health. Health is an important issue for the general public: in a recent poll conducted for the ‘Belfast Telegraph’, 79% of respondents said that health should be one of the top three priorities for the Executive, which was a long way ahead of the next issue, which polled approximately 50%. I would be grateful for any help that you and your colleagues can give me in furthering that bid.
55. The suggestion that DEL become involved in the ministerial co-ordination group on suicide prevention is very useful. I shall discuss that matter with the ministerial group and with the Minister for Employment and Learning. That is a good suggestion, bearing in mind the link between suicide and young males, and DEL’s role in further and higher education — as well as the link between employment and self-esteem.
56. My Department is releasing funding at the rate of £3 million per annum, £1·8 million of which goes to local communities. Those resources are secure, because that is year-on-year funding. I welcome bids from local community groups, and I agree that continuity in funding is crucial to ensure that such groups do not spend half their time running around, making business cases and proposals for funding.
57. On the issue of available beds, Foster Green Hospital currently has 15 beds in its child-and-family centre, and eight beds in its adolescent unit — with an additional four beds being made available this month, with a further four to follow. The plan — the proposal is currently held up in planning — is for two new hospitals by 2009: an 18-bed adolescent unit and a 15-bed child-and-family unit.
58. I empathise with the remarks that you made about GPs and particularly with your remarks about the provision of space in A&E departments where a patient who is presenting in crisis can be taken. Perhaps one of my colleagues will deal with the issue of antidepressants and the under-18s.
59. Dr Miriam McCarthy (Department of Health, Social Services and Public Safety): A formal course exists for updating GPs’ skills. GPs, in common with all doctors, have a professional responsibility to maintain their skills, expertise and knowledge. They will participate in a variety of courses as part of continuous professional development, a proportion of which is likely to be on the subject of mental health — even if it is not a particular, formal course. The course, which can be done online, can be quite challenging because it is largely interactive, and asks questions. That is a recognised form of continuous professional development. Therefore, there are a number of means whereby GPs and other professionals can gain further skills and experience.
60. Ms Ramsey: Although you probably do not have the figures at present, I would appreciate it if you could provide us with them. Families who have been bereaved through suicide have told us that they have a concern about the uptake of courses. You told me that 361 people will have completed the course by December. Therefore, I would like to know what the shortfall is.
61. Was there not a recommendation, stemming from the Danny McCartan case, that there should be a review of the prescribing of antidepressants to under-18s?
62. Mr McGimpsey: The figure was 161 trained GPs. It is anticipated that, by Christmas 2007, 200 GPs will have undergone the training. I will return to you on that matter and, specifically, about the issue of prescribing antidepressants to under-18s.
63. The Chairperson: It was the Committee’s view — after listening to the families and to Dr Paul Miller, who gave evidence to the Committee about suicide issues — that it would be helpful if there were a dedicated chill-out room where volunteers, such as the Samaritans, could calm the person down while waiting for the statutory agencies to take over responsibility.
64. I became aware of a constituency problem whereby a gentleman, who was in his 30s, was about to hang himself. His mother pulled him off the garage posts and managed to save him, just in time. He was about 30 years of age and was suffering from post-traumatic stress disorder, as a result of his service in Iraq. His mother went to Newtownards Hospital, and to many other places, but she could not get help anywhere. When he presented at an A&E department again, he was given a few tablets which would take four weeks to have an effect. Therefore, that mother will be watching over her son for the next four weeks until, hopefully, the drugs begin to calm him, and until he can get an appointment with a consultant. Therefore, the chill-out room is an important factor in controlling and dealing with those people who come in off the street, looking desperately for help.
65. Rev Dr Robert Coulter: I am pleased that so much activity is taking place in this field. Most of my concerns have been addressed already. However, there is one area that is of particular concern to me; namely the co-ordination of training with stakeholders in the community. I am thinking, in particular, of the various Churches. Churches are at the front line when it comes to dealing with the trauma associated with suicide. Has any thought been given to the co-ordination of training? We have talked about GPs and teachers. However, there has not been any talk about pastors, ministers and the Churches.
66. Mr McGimpsey: I entirely agree with you. Clergy played an important role in Craigavon, as they have in other areas. I shall ask Patricia to answer your question.
67. Ms Osborne: The suicide strategy highlights the need for training of GPs, teachers, youth workers, Churches and A&E staff, as front-line people. The suicide strategy implementation body is aware of that issue. At the moment, a variety of training is available. There is mental-health first-aid training, and the applied suicide skills intervention training programme. At present, the Health Promotion Agency is undertaking an audit of training; of the results of any evaluations of that training; and of what would be the most appropriate training for particular groups, be they GPs or A&E staff.
68. We have discussed training with the Churches, and we intend to meet them again.
69. Rev Dr Robert Coulter: Have you been to the theological colleges to discuss such training with people on the ground?
70. Ms Osborne: I do not think so. My understanding is that the meetings were with the leaders of the five main Churches.
71. Mr McGimpsey: Were meetings held with individual members of clergy, on the ground?
72. Ms Osborne: Yes.
73. Mr McGimpsey: That is another interesting suggestion — and I am open to all suggestions — that the Department will consider taking up. I will talk to you about that again, Ms Osborne.
74. Mr Gallagher: It is encouraging to hear about some of the steps that are being taken. However, I am sure that everyone will agree that, given the scale of the problem, those are small steps, at this stage.
75. I want to examine how the misuse of alcohol and drugs is being addressed. It is good that that issue is being addressed in school, which is an obvious place to start. However, I noted that Patricia said that her understanding is that a counsellor works for half a day a week in all post-primary schools.
76. I accept that she described it thus, because I too have an understanding, but it does not match hers. My understanding is that there are not counsellors in all schools. In any case, I would question how there could be counsellors in all schools, given that they are so scarce on the ground?
77. I hear that teachers are being offered a couple of days’ training so that someone is available to offer counselling in schools. That has potential. However, the quality of the available counselling is important. I want the Department to examine that matter and to come back to the Committee with more information. Although some counsellors visit schools, I hear from the non-statutory organisations in the large towns of my constituency that their funding is being scaled down. Those organisations provide help and support for those who misuse drugs and alcohol. When they ask why their funding is being scaled back, they are told that support is already available in schools.
78. If it is decided to go down the road of diverting money for counselling to schools, we must have a clear understanding of why funding to groups that are available to offer help and support at the weekends — when vulnerable people often need it — is being scaled down. Is that the best road to take, and would that be money well spent?
79. We need answers to those questions, although I am sure that they cannot all be answered today.
80. Mr McGimpsey: Tommy, there is no single answer. The Department has no basic plan that I can assert will work. We are taking action in a number of areas, which everyone acknowledges is required. At a ministerial group meeting, counselling in schools was identified by the Minister of Education Caitríona Ruane, among others, as an important issue.
81. I must consult with her to get the detail that the Committee may need about the roll-out of that programme. That is important because the Department of Education works with schools and young people.
82. Drugs and alcohol were mentioned. Research over the past 20 years has shown that one-in-three adolescents who die by suicide are intoxicated at the time of death. Alcohol and substance abuse are important predictors of eventual suicide among young people. Young suicides have a high rate of alcohol and substance misuse and dependency. I do not say that that is universal, but it is a factor. The Department of Health in England states that:
“The implications for prevention and intervention are clear: focusing on drug and alcohol abuse would have a greater impact on adolescent suicide rates than any other primary prevention programme.”
Moreover, the percentage change in alcohol consumption has the single highest correlation with changes in the suicide rate among young people. There is a clear link. I do not say that if we deal with alcohol and substance abuse, everything will be fixed. However, it is an important factor.
83. Ms Osborne: I spoke of the situation of counselling in schools as “my understanding”, because I do not want to give misinformation. However, I think a relatively new counselling service has been put into post-primary schools and that a counsellor is available for one half day each week. I believe that to be separate from provision for drugs and alcohol counselling. I shall, however, seek clarification on that matter with officials from the Department of Education.
84. The Chairperson: The Committee has advertised in the press its intention to take evidence, and it will call spokespersons from the Department of Education. The Royal College of Psychiatry will also give evidence.
85. Dr Deeny: I am delighted that the Chairperson is wearing a badge promoting the zero-tolerance campaign against attacks on healthcare staff. I am not wearing mine because I have nowhere to pin it on my jacket.
86. I have been involved in medicine for more than 20 years. Many matters have been covered, but the bigger picture should concern us all. It seems that the more affluent we become, the more prevalent suicide becomes. That seems to be the case in Japan and similar countries. As a GP, I agree with what has been said so far. A multi-disciplinary approach must be adopted, because many factors combine to cause suicide. It is not simply alcohol, although that is a major factor.
87. In my professional life, I have, unfortunately, been called to three suicides. The last one was over a year ago, when a young man hanged himself. Suicide is devastating for everyone. Many of those who take their own lives suffer from mental illness. Many have serious mental conditions, such as depression, psychotic diseases or schizophrenia. Cases in which no mental illness has been diagnosed are particularly frustrating for health professionals. The cases that shock health professionals are those in which there have been no signs whatsoever, when, out of the blue, a person takes their own life. That was the situation in two of the cases to which I was called. No one was aware that the subjects were mentally ill. They had not visited a GP, or any health professional.
It seems to me, and I have been in my job for 27 years, that suicide is a societal problem. Young people are becoming more affluent and are better provided for, and they have no hardships and difficulties in their lives. As a result, their coping strategies are not the same as those of previous generations.
88. Health professionals must step up to the mark. We must be there to pick up the signs of depression, and treat it. Do you agree, Minister, and do you know what is happening in Scotland?
89. Bob mentioned our Churches and clergy. We must tell our young people that life is precious and wonderful. I have seen young mothers left to bring up young children. I dealt with a family that lost an only son. All those people say that, if their loved ones had only known what devastation they would cause by taking their own lives, perhaps they would not have done it.
90. We need to get that message across to young people. Are the clergy and educators going to be involved in not only mopping up the aftermath of suicide and dealing with the resultant devastation through counselling, but in trying to get the message across that life is precious and the greatest gift that we have all been given? Young people need to know that, if things are not going well for them — for example, if a relationship breaks down — they cannot simply choose to take their own lives, because they will destroy the people that they leave behind.
91. Lastly — perhaps the Committee will find out more when it visits Scotland — from a medical point of view, Minister, there is an absolute dearth of mental-health facilities for children and adolescents. That must be addressed.
92. Mr McGimpsey: You made the link between affluence and suicide, which is one possible link among the many that I have mentioned. However, suicide can strike youngsters from the most deprived and disadvantaged backgrounds, as well as those from affluent homes. Some of the families that I have talked to showed no signs of affluence.
93. However, resilience and coping strategies are important, and we must imbue our young people with the ability to cope with life’s knocks. We must help them to understand that that is all part of life, and that life is precious, and that things will always change, no matter how black they might seem.
94. As for signs that might raise concern, I have often met families and communities who told me that there was no sign of what was to happen. Perhaps there were signs, and that is where GP and A&E awareness training is important. I do not have the exact figures, but, in several cases, a person had visited his or her GP in the previous 12 or six months, and showed no detectable signs of depression. The other part of the problem is the way that suicide strikes without warning.
95. Perhaps Patricia would like to add some comments. Scotland and New Zealand have strategies that appear to be models that we might follow. As part of the Department’s work through the five nations group, we are sharing experiences with the Irish Republic, Scotland, Wales and England. Although the incidence of suicide is not as great in England and Wales, there appear to be peaks in Scotland. Scotland appears — touch wood — to be getting over that peak, so we are looking at practice there. The same is true for the Irish Republic.
96. Ms Osborne: The task force on suicide visited Scotland, and the approach that was taken there was fully considered in the development of the Northern Ireland suicide strategy. The Department feels that the suicide strategy should not be looked at in isolation, because there are several factors that must be taken into consideration, as the Committee knows.
97. The Department sees all the strategies — on physical activity; sexual-health promotion; the promotion of good diet; drugs and alcohol awareness; teenage pregnancy; and the promotion of mental health — feeding into the work on suicide, so that it is not seen in isolation. Most of those strategies — for example, the teenage pregnancy, mental-health promotion and sexual-health strategies — promote coping skills, personal-development programmes and parenting skills. All those measures will help to ensure that young people are fit to cope with the world and with today’s society. Therefore, we do not view the suicide strategy in isolation; we see all those other strategies feeding into it.
98. Ms Ní Chuilín: You are all very welcome today.
99. We met with a group of nurses and midwives, and they raised their growing concerns about treating pregnant women with mental-health difficulties. Some of those women may have self-harmed or given staff sufficient cause for alarm that additional nursing staff have been allocated to them while they are in hospital. Members of that group told us that that has been their experience across all the trusts, not just those in Belfast. They suggested that there should be better provision in hospitals for pregnant women with mental-health problems, and that there should be particular supervision for them, more space, specialised support and better staff-to-patient ratios.
100. I ask the Minister to elaborate on another issue. Not so long ago, we visited the home-treatment base at the Mater Hospital site in Belfast, and it is very impressive. Issues such as funding and the community link are important there. Sue Ramsey mentioned those issues, and you acknowledged them, too. However, funding and resources for the future cropped up time and again. Is it a pilot scheme or a one-off scheme, or will it be part of an integrated strategy that deals with suicide prevention and mental-health provision? It is widely accepted that A&E departments are not for people with mental-health problems, yet, even so, when someone in crisis goes to A&E, nobody is on call to help them. That is not the case in all hospitals, with Craigavon Area Hospital being an exception. However, at the Mater Hospital, for example, no one is on 24-hour call. The home-treatment teams that provide care and support at home, and the after-hours and on-call services, are invaluable.
101. Sue and Iris mentioned chill-out rooms. Without linking both matters and without sounding as if I am contradicting myself, I suggest that there is a definite need for a dedicated space for someone under the influence of drugs or alcohol who has asked for help. At the same time, staff, particularly A&E staff, who provide a very valuable service, definitely must be protected.
102. Can consideration be given to midwives’ queries about maternity care for women with mental-health difficulties? Can you also elaborate on the home-treatment side of mental-health provision? If you cannot do that now, will you do so at a later stage?
103. Ms Osborne: I will take back to the Department the queries from nurses and midwives about self-harm. The Department can speak to the nursing profession and examine the suicide-prevention strategy to see what it can do.
104. When I talked about the other strategies earlier, I should have mentioned healthy workplaces and health-promoting hospitals. We see that as very much in line with work in the whole area of health improvement, and mental health would obviously fall within that. I will take back to the Department the points that you have raised. The Department will consider them and discuss them with the implementation body.
105. Ms Ní Chuilín: If it has not already happened, will you consider talking to the Royal College of Midwives and the Royal College of Nursing? They represent the staff who deal with those matters almost daily, so they will provide some valuable insight into what is needed.
106. Ms Osborne: The Department is looking at the idea of chill-out rooms in A&E departments. The matter has been raised before.
107. Dr M McCarthy: In addition to what Pat has said, the Department is aware of the likelihood of mental-health issues coming to the fore during pregnancy. It is a stressful time. It can be particularly stressful for a single parent or a teenage parent. There is, of course, well-documented evidence that post-natal depression affects a significant proportion of new mothers. The community midwives who visit women at home after they have given birth are very conscious of all the emotional and mental-health issues.
108. Following an audit, a group is considering some aspects of maternity services. It is chaired by the Chief Nursing Officer, and I am happy to bring to his attention what you have asked. His group is considering correct staffing and the right balance among midwives, assistants and nursing staff. If we have any further information, I will be happy to provide you with it.
109. Dr Andrew McCormick (Department of Health, Social Services and Public Safety): As the Minister has said, now is a critical time in the funding cycle. A debate is taking place about the allocation of resources, and about mental health in general. Suicide issues, in particular, are at the forefront of what we are seeking in improvement of services and provision. We must ensure that that fact is highlighted. Although a great deal of responsibility lies with the Department of Health, Social Services and Public Safety, other Departments can contribute, and that may benefit the economy. The effects of the difficulties that we face on mental health are significant for sick absence and employment, not to mention for Dr Deeny’s point about the value of life and the contribution that people can make. We must make a serious difference, and the challenge to do so is immense. Earlier, the Minister gave figures that our pro rata need for spending on mental health is 25% greater than that of England, yet we have 25% less pro rata funding. The Appleby Review recognised that a large reason for those funding differentials is the fact that we are so far behind in our approach to mental health and learning difficulties. That is at the heart of the issue. It is important that our Department, as well as other Departments, keep suicide issues at the forefront.
110. Mr Buchanan: I thank the Minister for his attendance. It is encouraging to hear about some of the strategies that are being rolled out. Robert Coulter talked about rolling out the suicide awareness strategy to Churches and Church leaders. In sparse rural areas, community groups should be involved in the strategy.
111. The Minister also said that funding had been secured for the next few years and that he would stress to his Executive colleagues the need for extra finances. Does the Minister accept that, in order to meet the demand and the increasing costs of providing services, the Department must consider modernising its methods, with more innovations and incentives to improve performance? I ask that because I have been informed that five people in Omagh were trained recently to work in the mental-health sector, at a cost of £178,000. I am told that, when that training had been completed, the Western Health and Social Care Trust decided that those posts were no longer required. That is an example of financial wastage in the Health Service. Issues such as those must be addressed. Although the Minister can appeal to his Executive colleagues for more funding, wastage in his own Department must also be identified. If that wastage is cleared up, more funding will be available for front-line services, such as those that are being discussed today. Can the Minister elaborate on that issue?
112. Mr McGimpsey: There is a clear need for efficiencies. Thus far, under the Gershon efficiencies, £140 million has been contributed, and we are signed up to the 3% CSR efficiencies, which is a further £340 million. That amounts to almost £500 million in efficiencies, and that is big money. I will pass over to Andrew for him to talk further on that.
113. Dr McCormick: The Department is developing a whole range of different responses to the challenge of improving efficiency. Much depends on how the people are used. Most of the budget is spent on people; therefore, investing in training and in the workforce is exactly what is required, and we need to ensure that that is aligned with the Health Service’s needs. That is a complicated task, but it is one that we must improve on and ensure that we deliver.
114. The efficiency programme that the Minister mentioned includes many elements that are aimed at securing continued and sustained improvements in efficiency and productivity. Those improvements will depend on the professionals taking responsibility and showing leadership. We want to secure their involvement and commitment.
115. One reason for some of the changes that are currently taking place is to ensure that all the professions are fully involved and engaged in sharing the responsibility. That will ensure that the training is well used, and that we can get a stable and strong plan to allocate resources, staffing time and staffing attention to those critical needs, rather that continually chopping and changing.
116. As has been said, it is vital that we do that in partnership with other sectors. I am not sure whether Pat can add anything on the involvement of the voluntary and community sectors, but there are definitely areas that they can reach that we cannot.
117. Mr McGimpsey: Professor John Appleby has pointed out in his report that the Health Service here is more inefficient than that in England — a clear price tag can be put to that. The gap between here and England is growing all the time. We are working hard to get more money. The proposition that there is enough in the budget to close that gap — if only we were more efficient — is incorrect.
118. An important factor that must be considered when making comparisons between Northern Ireland and England is that professionals and staff in the Health Service benefit from national pay deals. I am a supporter of that. However, we do not have any control over those pay deals — we are unable to negotiate them, yet we are obliged to implement the outcomes. Therefore, Health Service employees here get paid the same as those in England, but we do not receive as much funding. That must be considered, and although there are areas in which we can be more efficient, a huge gap still exists between here and England. Patricia will talk about the voluntary and community groups.
119. Ms Osborne: The Department is aware of the difficulties in rural areas, particularly their isolation. We have been working with the Department of Agriculture and Rural Development since the last outbreak of foot-and-mouth disease, and both Departments provide support to the rural support network. That support has continued since that last outbreak.
120. The rural support network was involved in the development of the suicide-prevention strategy, and it is also represented on the implementation body. Both Departments meet with that organisation at least twice a year. Therefore, we are aware of all the difficulties, particularly those that the farming community are experiencing.
121. The Chairperson: I have given everyone an opportunity to pose questions to the Minister. This discussion highlights the fact that the Committee is concerned about mental-health provision.
122. Have you had any contact with the media and Internet providers, Minister? We know only too well that, sadly, people have been able to use the Internet to encourage others to take their lives. An example of that was that dreadful incident some time ago when two strangers met up and took their own lives — it later turned out that they had been influenced by a website.
123. The media have been accused of sensationalising suicide. However, it is hard to make a distinction when three young people from the same school, in quick succession, take their own lives in copycat fashion. Have you had any dealings with the media? Are you taking any findings?
124. Mr McGimpsey: Both the print and broadcast media have been very responsible. I recently met with editors of newspapers and television — not to point out deficiencies but to see how we can help them and how they can work with us. They have a duty to report, and we must look at how we give them the information to allow them to do that.
125. My dealings with individuals and organisations in Northern Ireland have, by and large, been good. I met with Internet providers, and I will have more meetings with them. The Internet is facilitated by the Home Office — it is responsible for regulating the Internet. The response from the Internet providers was positive, but more can be done. We are teasing out what they can do and encouraging them to do it.
126. The incident to which you referred was disturbing, but it is by no means the only example. Some of the messages and chatroom conversations that I have seen, and that were reported to me, are equally disturbing.
127. The Chairperson: In closing, I wish to highlight an issue that greatly annoys me morally. The Westminster Government have extended drinking hours in pubs. They permit the morning-after pill, which I believe is encouraging sexual activity from an early age and putting pressure on young people to conform, to be prescribed without telling those young people that it is right to say no to sexual activity. The Government are not encouraging young people to say no.
128. The Government have also introduced online gambling. Are you looking at any of those issues, because drugs, alcohol, and so on, fall under your responsibility?
129. Mr McGimpsey: There is a clear correlation between drugs and alcohol. The gambling issue is a reserved matter, although I have my own views on online gambling. The prescription of the morning-after pill is the responsibility of GPs and doctors. It is not for me to try to tell them what they should or should not be allowed to do.
130. The Chairperson: My reason for raising the issue of the morning-after pill is that if young girls do get caught and become pregnant, that can lead to the breakdown in the social fabric of their family unit and can cause them to contemplate the easy way out, as they see it, which is to end their lives. That is not the answer.
131. Dr Paul Miller made the point in Committee on 5 July 2007 that suicide is a permanent solution to a temporary problem. All that we can do is to encourage you, Minister, to ensure that mental-health services receive the appropriate level of attention, and that any moneys directed to those services are ring-fenced and cannot be used or abused because of shortfalls in other areas of delivery.
18 October 2007
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Dr Philip McGarry |
Royal College of Psychiatrists |
|
Anne |
Mater Hospital service user |
132. The Chairperson (Mrs I Robinson): I welcome the representatives of the Royal College of Psychiatrists to this formal evidence session, which forms part of the Committee’s inquiry into the prevention of suicide and self-harm. I refer members to the college’s written submission to the Committee. The Royal College of Psychiatrists representatives are: Dr Philip McGarry, consultant psychiatrist; Dr Maria O’Kane, chairperson of the Northern Ireland faculty of psychotherapy; Dr Peter Gallagher, chairperson of the Northern Ireland child and adolescent faculty; and Anne, a Mater Hospital service user.
133. Witnesses, you are all very welcome. We have about an hour; and we look forward to hearing what you have to say.
134. Dr Philip McGarry (Royal College of Psychiatrists): We thank the Committee for inviting us to speak. We are grateful for the opportunity. We have sent a written submission to the Committee; I will talk about that briefly, and then I will ask Anne to talk about some of her experiences, as someone who has been involved with our service.
135. The Royal College of Psychiatrists of Great Britain and Ireland was founded in 1859, and it is an all-island and all-archipelago body. It long predates partition. It represents psychiatrists in Britain and in Ireland.
136. The Royal College of Psychiatrists is responsible for the supervision, training and accreditation of psychiatrists, and for providing guidelines and advice regarding treatment, care and prevention of mental disorders. Approximately 230 members of our college lead multi-disciplinary teams throughout Northern Ireland. Psychiatric care is delivered through a multi-disciplinary team, which is led by a consultant psychiatrist. Nurses, social workers, occupational therapists and psychologists, among others, work together in that team. We work on a team basis.
137. Throughout Northern Ireland, each locality has a consultant-led team that provides a service. Psychiatrists work day in, day out, with large numbers of patients. Every time we see a patient, part of the assessment involves consideration of the potential risk of suicide. Our junior psychiatrists learn about that in their first week of psychiatry. We must address the issue of suicidal risk every time we see a patient.
138. Suicide itself is not an illness or a condition, such as depression or schizophrenia — it is an act that can occur as an outworking of various factors. Suicide may be closely related to major mental illness, such as schizophrenia, manic depressive illness or severe depression. Often, it is associated with factors such as the use of alcohol or drugs, severe social difficulties, personality factors and elements that are less immediately remediable by pure medical intervention. There is also a broader societal background. For example, America has a high suicide rate, which could be dramatically reduced overnight by gun-control laws. If America wants to reduce its suicide rate, more psychiatrists should be employed, and gun control laws introduced. That would have a dramatic effect on suicide and homicide. It is a complex subject.
139. We have identified three key areas in our document that we would like to raise today, on which I shall welcome members’ questions. The first area deals with those who have engaged in self-harm. Our report states that, each year, approximately one person in 10,000 will take their own life. That is a standard figure. People who have been admitted to hospital, having harmed themselves, are at a one-in-100 risk over the following year. In other words, the risk of suicide is upped by a factor of 100 among those who have self-harmed. Therefore, if we specifically target those who have harmed themselves, which is a high-risk group, we could do a lot of good. The National Institute for Health and Clinical Excellence (NICE) guidelines of 2004 recommended that we improve the services that we offer to people in that situation.
140. For the past two or three years, the Royal College of Psychiatrists has been working on a major audit project with our colleagues in the Royal College of Nursing, the Faculty of Accident and Emergency Medicine, and the Ambulance Service. We are improving on what we can do, but we are not doing enough, because there are insufficient resources to provide a full assessment and follow-up for those who have harmed themselves.
141. Last year, I spoke to one of the top UK gurus in the field, Dr Navneet Kapur from the Manchester suicide centre. I asked him what one thing he would do to tackle suicide, and he said that he would consider what he could do for patients who have harmed themselves. We could do better than we are presently. In Northern Ireland, we are trying hard, and members will hear about the project at the Mater Hospital shortly.
142. We are also concerned about the fact that 10% of those who self-harm and attend hospital departments are adolescents, and we do not have the appropriate follow-up or back-up services there. That is an ongoing problem. Members will be aware of the difficulties with recruitment in child and adolescent psychiatry, but we could do a lot better. Therefore, there should be a major focus on those who have harmed themselves.
143. At the Mater Hospital, there has been departmental funding for a team until the end of March 2008. That team is led by Dr O’Kane, and it does a lot of work with people who have harmed themselves and provides follow up for a short period afterwards. Those who have harmed themselves repeatedly have been given active, intensive support, which is producing encouraging results. The team is only a temporary project — it is not permanent yet — but it is producing work that is of a very high standard.
144. The second area that I would like to mention is the need for more talking therapies or psychotherapy. Psychotherapy relieves emotional distress through the use of a talking technique.
145. The Chairperson: It is a mentoring therapy.
146. Dr McGarry: That is part of it. Psychotherapy moves beyond counselling in that it is very much about the therapist’s trying to understand the individual and get to the root of the problem, and enabling a person to use that analysis to help themselves. Historically, the provision of psychotherapeutic services in Northern Ireland has not been as good as it should have been. Doctors now see many patients with very complex problems, and Dr Deeny will be well aware of that from his own experience.
147. It is relatively rare for patients to have straightforward depression. Most patients whom I see will have a depressive illness, but other factors will also be involved — their family or home situation, work issues, educational and employment issues, debt, alcohol, and so on. Many factors may contribute to the problem, and it takes a great deal of time to work on those.
148. However, the evidence shows that, if the effort is put in, good results can be achieved. We are aware of the Minister’s announcement last week about funding for psychotherapy, and we would welcome the Committee’s support in sending a loud and clear message to the Minister that more psychotherapy services are needed in Northern Ireland. That would have an impact on the problems faced by some of our self-harm patients.
149. The third matter that I wish to highlight is alcohol. Most psychiatrists who see self-harming patients in general hospitals would reckon that, in over 50% of cases, alcohol has been taken. In many of those cases, had those individuals not taken alcohol, they may well have not harmed themselves. Obviously, that raises the issue of alcohol addiction services, which we believe are pretty good in Northern Ireland. They could be better resourced, but the community addiction teams do an excellent job. Major public health issues arise in that area, which we, as a society, must examine.
150. There are also political considerations, including issues such as the price of alcohol, the availability of alcohol, sponsorship of sports by drinks companies — some of us find it difficult to understand why such sponsorship is accepted by sporting organisations — and advertising. Those issues must be addressed on a political level. We have a binge-drinking culture here; it is considered quite acceptable. Those issues are not simple; they are complex, but they must be addressed.
151. The problem is underpinned by certain factors. Our society has had its difficulties, and suicide rates are higher in societies in which there are high levels of unemployment and social deprivation. There is no doubt that our history of violence has left a legacy, and that is understandable. However, we are now moving on from that legacy, and that is very encouraging.
152. We must create a society that advocates respect for other people and for ourselves. If we do not respect other people, we will not respect ourselves. Suicide and homicide are two sides of the same coin. We must create a culture that promotes the understanding of others and respect for others and ourselves. That effort must involve everyone, not just psychiatrists, although we have a role to play. Community and voluntary groups, politicians, families and individuals all have a part to play too. Work must be carried out in schools and in the youth sector, and, as has been pointed out earlier, the Department of Health, Social Services and Public Safety and the Department of Education must work together to address this issue. The Department of the Environment must also be aware of the need to create a decent environment when building new housing.
153. In recent years, the media have been very helpful to us in their coverage of our anti-stigma campaign, Changing Minds. Much good work has been done to promote awareness of the importance of positive mental health — it is as important as physical health — and to promote awareness of the signs of mental ill-health that should prompt people to seek help.
154. However, media reports have also been unhelpful at times. We sound a note of caution about the potential, on some occasions, for the reporting of suicides to be counter-productive. I know that the Health Minister is considering the matter of working with the media, and we are also doing some work on that. In general, the media have been incredibly helpful in their coverage of work in the mental-health field, but it is important that they be careful to report suicide in a sensitive manner.
155. I would like to introduce Anne, who has used Dr O’Kane’s service in north Belfast. She would like to make a few comments.
156. The Chairperson: Anne, you are very welcome.
157. Anne: Two years ago, I was sent to see a self-harm team because I was suffering from depression. At that stage, I was very low. I did not want to go to meet the team, and I did not want to be around my two children. As a mum, it is very difficult for me to admit that. With the help of the self-harm team and my GP, I have come out the other side. I have come a long way.
158. I am one of the lucky ones. I had cut my arms, and I do not do that any more. I received intense help through psychotherapy and through talking with the doctors and with my community psychiatric nurse (CPN). That has been really great. I would not have had that opportunity anywhere else.
159. Such help should be readily available for anyone who needs it. People benefit, and not just the person who self-harms, but the whole family. My family unit has changed: my kids are more relaxed, and I am more relaxed. I am getting married. I would not have been able to sit here and talk to you two years ago, and that in itself shows that I have come a long way. The service is beneficial to the whole of society; it should be there and it should stay there.
160. Dr McGarry: Thank you for inviting us. Psychiatrists work every day at a clinical level, seeing patients and trying to help. However, we also want to help with policies, and if we can be of any assistance to the Committee today or at any other time, we will be pleased to help.
161. The Chairperson: Peter and Maria, do you wish to add anything before members ask questions?
162. Dr Peter Gallagher (Royal College of Psychiatrists): It might be of more use if we responded to members’ questions.
163. Dr Maria O’Kane (Royal College of Psychiatrists): Yes, we are happy to respond to members’ questions.
164. The Chairperson: Thank you for that very interesting synopsis of the problems, and for telling us about your work. Dr Paul Miller, one of your colleagues from the Mater Hospital, came before the Committee in July. He made a very telling point when he said that suicide is a permanent solution to a temporary problem. That comment has resonated with me ever since. We must reach out to people before they get to that stage. Prevention is the key.
165. Your submission states:
“Of those who self harm, 1% are likely to complete suicide within the next year, an increase in risk of 100 times. This is clearly an easily identifiable group of people who are at risk and who can and should be offered thorough assessment and, if necessary, follow up.”
166. I take it that the reason that they are identifiable is because they present themselves.
167. Dr McGarry: Yes. Anyone who comes to an A&E department will be, and should be, well documented, and will be offered psychiatric follow-up. The problem is that, across Northern Ireland, the services in general hospitals have been poor, particularly at weekends. Some hospitals may have one liaison nurse who is excellent, but when she is on leave, off sick or off at weekends, there is very little help available. There may be an emergency junior doctor on call who is doing a lot of other things and does not have the time to do things as thoroughly as would be liked. That is an area for which extra resources should be found. That would not need to be massive extra resources, but it would be very worthwhile.
168. The Chairperson: The Committee has been discussing this matter in great detail and has identified that a room should be set aside in every A&E department where a voluntary group — the Samaritans or some other group — could be there to settle someone until the appropriate clinician arrives and assesses the person to ascertain whether they need to be admitted or not. However, we are teasing out that issue, and I would be glad to hear your opinions on that.
169. I know from personal experience that there seems to be a rash of young girls who are self-harming. I am not just referring the Ulster Hospital, but it is in my constituency. When such girls went to that hospital, no one was available to assess them at weekends, and they were placed in a general ward, or perhaps a geriatric ward. That is not conducive to helping young people.
170. Dr McGarry: Dr O’Kane is running a pilot scheme at the Mater Hospital examining that type of work.
171. Dr O’Kane: We have had to think about that matter. That issue has been raised through the college audit, which is being carried out at the minute through the Royal Victoria Hospital’s and the Mater Hospital’s A&E departments. Obviously, they are confined by space. We started by trying to identify a space within the A&E department where a person could be assessed quietly without fear of interruption, and with solid walls instead of curtains. Finding such a space is a challenge in itself. Those two A&E departments have worked very hard with us to try to achieve that. Things are far from perfect, but they are better than they were.
172. Our statistics show that 80% to 90% of people who require psychiatric care who present at A&E have taken an overdose. They may also have cut or burned themselves, or engaged in some other form of self-harm. Those people need some form of medical treatment. Having a room set aside would be helpful for some people, but the majority of the rest would probably need medical intervention, so we require access to the A&E area.
173. In the course of the audit, we visited various facilities throughout England. We found that those facilities attempted to provide a room for a family member to be present, but it was not as well organised as we would like. We were unable to find a perfect situation. Sometimes, those rooms were very isolated. If there was a bereaved family to be accommodated, or victims of a road-traffic accident, services had to be offered to them and the room was automatically taken over. That is a difficult target to achieve.
174. The idea of having someone to accompany and support a person who has self-harmed is a good one. We have been exploring that with the voluntary agencies, with which we work closely. As you know, there are three agencies in particular which operate in north and west Belfast: the West Belfast Self-Harm and Suicide Prevention Initiative; RAYS, which is based in the greater Shankill area; and the PIPS project, which is in north Belfast. When those groups are made aware of adults who present with problems, they will try to accompany them to an A&E department. That has worked extremely well.
175. We considered reintroducing the “pink ladies”, who were — famously — the ladies who brought tea to people who were waiting in A&E departments. Together with the voluntary agencies, we have begun to think about how we could use people who are trained to competent-helper level. That is being considered. However, inevitably, when one starts off with 100 people who are willing to train as competent helpers, one ends up with only a few who finish that training.
176. To support people who have a high level of distress when they present is difficult. People find such situations very distressing. One needs to be sure that the person who is offering support is sufficiently robust to do that adequately, rather than reinforce the sense of hopelessness and neglect that people who self-harm have.
177. The Chairperson: That is a difficult balance to achieve. I believe that greater use of volunteers would be very helpful. There is a wealth of intelligent people with common sense, which could be tapped into. That is more important than a list of letters after one’s name. Many would jump at the opportunity to help young people. The Committee believes that that is a good way in which to proceed.
178. I meant to say Anne that I am delighted that you have come through to the other side. It is good to see and identify people who have come through the gamut of depression. There is hope at the other end. I am delighted to see you doing so well, and I wish you well on getting married.
179. Members may now ask questions.
180. Ms Ní Chuilín: Well done, Anne. I wish you all the best — you have been on a journey. Good luck.
181. I live in north Belfast, and it disturbs me greatly that I am continually hearing stories of people going to A&E, having to wait for six and a half hours, and then having to leave, unattended. We all hear those stories, no matter what the hospital. That is very frustrating for staff. Everyone who has to deal with such situations is totally frustrated.
182. I have read your recommendation that there should be a rota of adolescent-mental-health professionals. It seems unlikely that that can be organised in the near future, given recruitment problems.
183. I had thought that things may have improved. We visited the home-treatment centre at the Mater Hospital, and I was really impressed. That is the way forward.
184. Groups such as PIPS and RAYS and others work at weekends. If their services are continued, if recruitment targets can be met, and if projects such as the home-treatment centre — or your own, Maria — are continued, they may be little rays of light for us.
185. Dr McGarry: The recruitment issue is particularly acute in child and adolescent psychiatry. Some argue that the home-treatment team and some of the new advanced teams are recruiting excellent staff and creating a deficiency of staff elsewhere in the system. As you know, there is a big shortage of nurses in Northern Ireland, which is a continuing problem. The point about recruitment and staffing in child and adolescent psychiatry is very important.
186. Dr P Gallagher: The key issue, assuming that we regard mental health as a Cinderella service, and taking on board the Minister’s comments, is that we have 25% more mental-health difficulties in Northern Ireland, but 25% less funding allocated to child and adolescent-mental-health services. I use the term “mental health” in the broadest sense, not in the narrow specialist sense that implies mentation, which is just the way in which we think about something, and which influences the way in which we do things.
187. Notwithstanding that, Northern Ireland has a very high percentage of young people who have mental-health difficulties — between 20% and 40%. Northern Ireland has a higher percentage of people under 18 years of age — between 27% and 33% — in contrast to the UK, where that figure is about 21%. Between 2% and 5% of mental-health funding goes to the child and adolescent sector, so there is a huge gap between those figures and what is actually required. We know that our society is toxic to children’s development, and if we look at the way in which the media acknowledges the difficulties that surround the issue of self-harm, to injure oneself is now almost a cultural norm with which to define one’s distress.
188. There are many interventions that must be tried, but the key issue is resources, both human and financial, which must be yearly and sequential. There is no point in being handed a large amount of money tomorrow morning, because there will not be enough staff available to make use of it, particularly not in an accident and emergency department. Although it is helpful to have a mentoring process in an A&E department, children and young people have a tendency to only get one bite at the cherry. The person with whom they form a relationship, and the nature and quality of that relationship at the beginning, will determine whether they will come back to a specialist service to address some of the issues that have led them to take an overdose or self-injure.
189. That requires someone to be available in an A&E department because, if that is not the case, the young people will vote with their feet and not return. They will, however, keep coming back because, in a sense, self-injurious behaviour is the end stage of a distressing event. Despite the way in which it is portrayed by the media, no one who attempts to end his or her life as a solution to their difficulties does so lightly.
190. We must treat this problem with the gravity that it deserves and provide the interventions at the coal face. It would be most helpful to have on hand a trained mental-health worker who would assess those youngsters and begin to transfer them to specialist mental-health services. That service should be available in every A&E department, Monday to Sunday, 24 hours a day. That is a key intervention, and it can make a difference. Unless that happens, we will only be mopping up, because we are on the cusp of the way in which human beings define their distress.
191. It is important to have an aggressive advertising campaign about self-respect and, as Dr McGarry said earlier, about how society values the individual. Services should be available, and we should be our brother’s keeper, and, more importantly, we should become our brother’s saviour. Mentoring is valuable, but unless we have therapeutic endeavours that help people to give order and meaning to the difficulties that they are experiencing, and address their distress, they will just repeat the process.
192. Ms Ní Chuilín: That is what is happening now.
193. Dr P Gallagher: Yes, indeed.
194. Mr T Gallagher: I would like to thank the witnesses for their attendance and contributions. The scarcity of resources and trained personnel was mentioned. There is no doubt: it is clear that mental-health problems in society have increased markedly, and some of the relevant figures have been mentioned.
195. No one is going to wave a wand and deliver all the resources that are required to deal with this problem. Philip, you mentioned high-risk, vulnerable people who self-harm. Let us suppose that £12 million was made available; how would you like to see that amount distributed? Should that be spent on people who self-harm, or should only some of it be spent in that way, with the rest spent on therapies for other types of poor mental health?
196. A witness at one of the Committee’s previous meetings commented on problems of that nature, and took a strong view that the education system should be providing children with information about good mental health. What do you think of that?
197. Dr McGarry: I am not overly pessimistic; the services will not necessarily need a huge amount of money. The new trust system might help. I know from working in the Mater Hospital that, in Belfast, I was working with patients from six different trusts. Now there is one mental-health director, the situation is much better. Things are changing, which is good, and we can work more efficiently.
198. I have talked to suicide experts in England who believe that examination of the self-harm population is very important, as is meeting the NICE guidelines. If NICE says that a drug is recommended for treating a certain condition, we assume that people will get it. However, NICE recommends assessments for people who self-harm, but many people do not get them. That is unacceptable.
199. The solution need not be massively expensive. A few extra staff in Belfast could cover the Mater, Royal and City Hospitals. There could be one person in the hospital and one on call, if necessary. That would not require massive expenditure.
200. The trusts will need to refocus the way in which they work. Historically, general hospital staff felt that self-harm came under the remit of psychiatry, rather than surgery or medicine, and that it had nothing to do with them. The community trusts felt that it came under the acute hospitals’ remit, so it fell between stools. The Royal Victoria Hospital has no liaison psychiatrist, for example. The new system offers an opportunity for joined-up thinking.
201. We do not need a massive amount of money, and it is important to make that clear. However, we need someone to say that providing the service is worth doing, and to work out how to do that efficiently. That does not require many personnel; just a sufficient number of people who are linked with the rest of the services. That is not to say that an adolescent might be seen by Dr Gallagher the next day, but he or she could be put in touch with a person who could decide whether the case was urgent and ensure that the patient is seen that day, or whether an appointment could wait for two weeks. Joined-up thinking is more important than massive amounts of money.
202. Mr T Gallagher: What about the education programme?
203. Dr McGarry: Peter will speak about schools, and what can be done there.
204. Dr P Gallagher: There are several requirements. The first is a media campaign that promotes mental health. Secondly, there should be a link person, in case anything happens. That will not cost an enormous amount of money, because he or she would be required only for critical periods. For example, someone could work from 9.00 am to 5.00 pm during the week and at certain hours at the weekends.
205. Thirdly, support in the school system is important. For example, a young person might know of someone who is vulnerable, but he or she might have the idea that it is wrong to intrude. We need to emphasise that people are connected; we are social beings, and, consequently, we cannot avoid relating to one another. We must connect with, and care about, one another. The availability of some type of counselling service in the school system would be very helpful. Funding could be made available for more specialist services, as they are needed.
206. Your question is apposite. We must think about what each bit of the service could do if it had a certain amount of money that might alleviate the problems, instead of seeing the issue as just one person’s problem.
If each community, hospital, school, education, adult college and mental-health system were to join together, do one bit and ask what the next person could do, there would be less likelihood of reading in the papers about another suicide.
207. Dr Deeny: Thank you very much for your presentation. Anne, your story really made me feel good, and you reminded me of a patient of my own. It just shows that you can get out of hell, and it is wonderful that not only do you feel good having done that, but you make others feel good.
208. One of my questions has perhaps been touched on. The child and adolescent recruitment problem was mentioned. We have a very good professional in Omagh, but she is on her own and there is a long waiting list, although we can ring her directly. Is there a lack of interest in child and adolescent health? I hope not.
209. Dr P Gallagher: It is partly a lack of resources, not a lack of interest. To put that in context: in Northern Ireland, between 2% and 3% of the total mental-health budget is spent on child and adolescent mental-health services; across the water it is between 10% and 15% for the rest of the UK. If you assume that the prevalence rates for adult mental-health difficulties are exactly the same as for child and adolescent mental health — which they are — and that between 27% and 31% of Northern Ireland’s population is under 18 years old, then the budget should be higher — more like 25% to 27%. Assuming that that will not happen tomorrow morning, planned development is needed. Not only psychiatrists are needed, but social workers, mental-health nurses, clinical-nurse specialists and psychologists, because we are an integrated system.
210. This Committee could perhaps persuade the Department to begin to plan sequentially, to allow for the feast or famine that tends to happen in systems, when money cannot be used because the people are not there. If every organisation were to increase its staff by a factor of 20%, year-on-year over a two-, three-, four- or five-year period, it would be possible to absorb and train people, and therefore expand part of the capacity of that service. That needs to happen; moreover, it is part of what the Bamford Review recommended. It should operate sooner rather than later.
211. Dr Deeny: Thank you, Philip, for pointing out something that the public needs to be told. I will never forget the young fellow that I found hanging from the rafters. None of us knew anything about him, and no one knew that he was mentally ill. The whole suicide issue is multi-factorial, and you mentioned personality difficulties, inter-personal and social.
212. Post-natal depression concerns me. A young mother came in to see me last week with post-natal depression, and no woman should focus on that when she has just had a baby. I came across a woman who had suffered with depression for nine years and, after GP and consultant help, it was discovered that she had prolonged post-natal depression.
213. One area where the media has helped is in demystifying suicide, although I know it can make a mess of things and some of the copy-cat suicides can be put down to it. In America people have perhaps gone to the other extreme with openness; however, people talk about mental health, which is a really good thing.
214. We need to get to our young people, perhaps in school, and particularly to young men who, because of the whole macho image thing, will not talk about their problems. With regard to psychotherapy, your handout mentioned that psychiatrists and GPs are frustrated, and that could not be more correct. A third of our consultations are on mental health and, although the medication we prescribe may help, we know that it is not the answer. Psychotherapy is the answer.
In the past week I had a patient with problems which — in my opinion — did not require a drug solution. I latched on to the fact that she might have some marital problems and that she might need psychotherapy. I gave her telephone numbers for Relate and Accord because they could provide her with some sort of therapy. Had it not been for the link with a marital problem — and perhaps I was jumping at that — there was no other facility to which I could have referred the woman. We have cognitive behavioural therapy at an excellent facility in Omagh, and, I am sure, there are others in Northern Ireland.
215. What do we need? Do we need more funding? It is great to hear from the professionals in the psychiatric mental-health area. I am sure that you will get the backing of the Committee, which has talked about the issue of mental-health and is committed to it. Do we need to put funding into psychotherapy so that I, or any other GP, can say that that option is available? We see so many people with mental-health illnesses who do not even get as far as seeing a psychiatrist.
216. Dr McGarry: It came through that you have a special expertise on the matter.
217. Dr O’Kane: I will address two issues before answering your question on psychotherapy. Fifty per cent of the people that we see are parents with very small children. I accept Peter’s point about the need for child-and-adolescent-service development. However, I am more mindful of the fact that a lot of our patients are parents, as Anne pointed out. That is terribly important as regards improving the environment in the home. That is why we feel that our work is important.
218. One of the difficulties with psychotherapies is that there is a huge level of interest across psychiatric services in the development of talking therapies. As you know, there has been an expansion in CBT; however, there has been less of an expansion in the other psychotherapies. The difficulty is that one must be able to think in order to do CBT, because it is a cognitive therapy. A lot of the people with whom we are in contact are not able to think, because they are so overwhelmed by what is presented to them that, sometimes, we need to start at a lower baseline and then work our way up. We are conscious that, in mental-health services, accessing CBT is a little easier than accessing some of the other psychotherapies. Nevertheless, we see many people respond well, for example, to family therapy and individual interpersonal therapy. It is not a case of one therapy fitting all; there is a whole gamut of therapies, and access must be expanded.
219. There are quite a lot of people who are trained in the mental-health workforce. However, the difficulty for them is that they are not in jobs where they can deliver that, day-on-day, in the way that would be preferred. For example, although a significant proportion of our nursing staff have training in family therapy and in some of the other therapies, and use those skills to enhance the job that they do, they cannot fully concentrate those skills in that area because that is not the way in which they are employed. Recognition of a variety of therapies that will allow people to progress into posts for which they have been trained must be encouraged — and not only in the Health Service. Overall, there must be support for the importance of psychotherapy in the NHS.
220. Mr Easton: Thank you for your presentation; it was helpful to the Committee. I was particularly interested in hearing about funding 24-hour cover in A&E; that is critical in improving that service. I was also interested in the profile of service-users on the last page of your submission to the Committee, particularly in drug and alcohol abuse, which seems to be a big factor. Does Northern Ireland need a stand-alone centre to deal with drug and alcohol abuse? We do not have that type of facility, and patients have to go to England or Scotland for treatment. Would it be helpful to have such a unit?
221. Dr O’Kane: The services for alcohol and drug misuse are reasonably well-developed in Northern Ireland. There tends to be a good working partnership between the voluntary and statutory agencies. We see many people who use alcohol and drugs, not because it is their primary addiction but as a means of alleviating distress. A joined-up approach would be very helpful in providing a good outcome for a person who presents because of self-harming and the use of alcohol and drugs. People see trained mental-health practitioners and others in a position to help, but it must be recognised that those services need to work together, rather than having people attend one place for drug and alcohol problems and another for mental-health problems. There must be better working practices across the agencies.
222. The difficulty has been that the drug and alcohol services are reasonably well developed, but other services less so. Inevitably, therefore, people who avail of services to deal with drug and alcohol problems probably receive some help to manage those. Alcohol and drug practitioners do good work, but it is not possible for them to deal with people’s underlying distress and their situation as a whole, because they do not have that expertise.
223. Mr Easton: The agencies need to come together to a greater extent.
224. Dr O’Kane: Yes.
225. Mr McCallister: That was an interesting presentation. Anne, it was courageous of you to come here and share your story, and I am glad that you were fit to do so. It is important to send out the message that people who have gone through particularly low periods in their lives can come through. You have my every good wish for your forthcoming wedding.
226. Peter, you made a point about funding. Throughout so much of Government, the way that some of the budgets are allocated can mean a feast or a famine. We must consider a better system of securing streams of funding, because the training of people to deliver mental-health services cannot be turned on and off like lights. It takes a long time before they are fully trained and in place. Will you perhaps comment further on that?
227. Some colleagues mentioned the mental-health agenda for schools and education. Have you any thoughts on, for example, first aid for mental health in the workplace too? When considering the overall health-promotion strategy, what areas of the mental-health agenda should we include?
228. Philip, you and Alex mentioned alcohol and drug issues. Have you any further thoughts on any recommendations that we should make? What are the key areas when considering alcohol restriction? What did you think of the statement of the Chief Constable of North Wales, when he advocated the legalisation of drugs? I understand that you may not wish to go down that road, but it is part of the overall debate on an alcohol and drugs strategy.
229. The Chair mentioned that the community and voluntary sector plays a vital role in so many ways, and, as Maria said, it is important that it takes an important role in tackling drug and alcohol addiction. What more can we do to stop it getting to the stage that it is a problem? How do we address the binge-drinking culture? Is it all down to the price of alcohol?
230. Dr McGarry: In the workplace, a great deal of work has been done using ASIST, which is applied suicide intervention skills training, and that started in Canada, 20 years ago. I was involved in taking a course with two nurses and someone from PIPS. It has been rolled out to over half a million people worldwide. The two-day course is geared towards people such as youth leaders, community workers, police officers, fire services, and so forth. It educates people on how to identify any early warning signs shown by an individual and how to deal with that person. That training continues, and the voluntary and statutory sectors are doing good work rolling it out.
231. Ms Ní Chuilín: Is that ASIST?
232. Dr McGarry: Yes.
233. Mr McCallister: How many people in Northern Ireland have been trained?
234. Dr McGarry: There has been fairly extensive training in Northern Ireland in which PIPS, some of the nurses from the Mater Hospital and various others have been active. ASIST is good and continues to develop. It is an example of a great joint initiative that informs people in positions of leadership, the local communities and the clergy how to deal with that single issue. It is a case of the more joint initiatives, the better.
235. Alcohol is a bigger factor in suicide than drugs. I will not take the line of the Chief Constable of North Wales in this forum. Binge drinking is a cultural matter, which would remain even if opening hours and advertising were restricted. In France, where there are long opening hours, the culture of going out and getting boozed-up does not exist. There is a weekend-binge culture in Northern Ireland. Kevin Malone, who is a professor of psychiatry in Dublin, has carried out examinations of young people’s brains. Evidence from post-mortem studies shows that alcohol affects cerebral biochemistry: the levels of serotonin and noradrenalin. Professor Malone suggests that young people are more vulnerable to the biochemical effects of alcohol than older people. At present, there is a big disparity between the number of young men and women who commit suicide. The potential danger of the binge-drinking culture is that increased drinking among young women may result in more of them taking their own lives. A wide spectrum of measures must be taken, involving advertising, sponsorship, and so on. There should be a public debate on the matter. It is everyone’s responsibility.
236. Mr McCallister: As Dr McGarry has mentioned, the drinking culture in continental Europe tends to be much more family oriented.
237. Dr McGarry: People will have a glass of wine followed by a coffee. Then they will go home.
238. Mr McCallister: That is interesting. We can forget about views on drugs.
239. The Chairperson: For your information, Dr McGarry, Professor Malone has sent the Committee a submission.
240. Ms S Ramsey: Like other members, I thank Dr McGarry for his presentation. Anne, I too wish you well. You have made a wedding present of this matter. It is nice to see something positive come out of those horrible statistics.
241. The Committee is conducting an inquiry into suicide and self-harm. I want to try to tease out some information from Dr McGarry’s paper. The Committee would have no difficulty in being critical of the Department. I hope that at the outcome of the inquiry, the Committee will be able to make recommendations.
242. The paper identifies key areas that the Royal College of Psychiatrists believes are essential to tackle the problem of suicide, three of which are highlighted. Has the Department agreed with those recommendations? If so, what has it done? If not, why not?
243. I have several questions. Should I ask them all at once, Chairperson, or one after another?
244. The Chairperson: Perhaps wait and ask them one by one.
245. Dr McGarry: Those issues have been raised with the Department in different contexts over the years. There is a yearly speciality advisory committee, where the profession meets with senior officials from the Department of Health. The Department is aware of such issues as liaison psychiatry in general hospitals, and psychotherapy over the years. The college has been engaged in consultation processes as far back as it has been able to do so. At present, I cannot say what the Health Department’s priorities are or what its thinking is. I hope that the Committee will help to put further pressure on the Department. The college will support it in doing so.
246. Ms S Ramsey: Page 2 of the submission states that:
“The NICE Guidelines (2004) demand that every patient is given a full psychosocial assessment after self-harm.”
247. I am concerned about whether that happens because I am aware of several incidents in which A&E doctors have not necessarily said whether patients have self-harmed and have told them to go home and give their heads a shake.
248. Dr McGarry: The answer is no. However, the situation is improving. Dr O’Kane can explain her project.
249. Dr O’Kane: One issue that was identified in the audit that we carried out was that as low a percentage as 30% of such patients who attended A&E at any given time were given a psychosocial assessment. That was one of the statistics that compelled us to request funding to set up a team that could tackle that. At present, the audit is mid-cycle. Our informal audit has picked up that statistics in the Mater Hospital and the Royal Hospitals have probably gone up to 60% or 70%. However, the limiting factor is access to staff.
250. One of the things pointed out earlier was that if a person has a particularly long time to wait, he or she will leave. We have been trying to improve that by contacting the person after he or she has left, if we are aware of that, with regard to social assessment or engagement. I am involved with that function of the self-harm team. However, we are concerned about the fact that things are not done as comprehensively as they could be, and that people slip through the net.
251. Ms S Ramsey: Families are concerned about the lack of GP uptake and training, so there might be an issue with the ASIST programme.
252. Dr O’Kane: GPs on the ASIST programme have said that the training is helpful to them when dealing with a suicidal person. However, they are also interested in the next level of training — the STORM project — which, although there are various other training schemes, is recommended by the Department in its high-risk-management guidelines. We have started discussions with the Health Promotion Agency and the Beeches, which is the nurse-training centre for the Belfast and south-east trusts, in an effort to try to spread the training out and make it available to GPs and other health professionals. Several staff are trained to deliver STORM, and we are trying to train more, so that there will be more hope of rolling it out and sustaining it.
253. ASIST is an excellent programme for the voluntary sector. Health professionals have told us that it is extremely good, but that they would like the next stage. One of the reasons that GPs find ASIST difficult to take up is that, like everything else, there are competing needs, including diabetes, epilepsy care, and so on.
254. Ms S Ramsey: You said in your paper that you welcome the £3 million funding that has been made available, etc. However, groups in the community and voluntary sector have problems with planning ahead, because of the issue of long-term funding. I do not ask you to get involved in a political issue but, in relation to children and young people and the lack of services in adolescent mental health, there is speculation that the Children’s Fund and children’s services will be hit big time in the Budget. Will that set us back further?
255. On a positive note, you referred to working in schools. At a previous Committee meeting we made a suggestion to the Minister about the ministerial task force. The Department of Education is involved, but there was no involvement by the Department for Employment and Learning. The Minister agreed with that and said that he would take it on board.
256. You mentioned the lack of communication. How can that be dealt with? My final point relates to the figures showing the profile of the service users, and Alex and John have already referred to those. It is useful to have a profile of the service users. Are there any plans to be proactive on the figures? They show that 23% of those who self-harm had been in care as children. Are there any future plans to target people in a care setting? Are we tying in with Sure Start, or organisations that deal with teenage pregnancies, so that we do not always react to issues? We want to be proactive.
257. Dr McGarry: We welcome the funding made available and the task force. I was on the task force and it has a multi-agency, multi-factorial approach, and it is important that that is kept up. There are 19 trusts, and I was not clear what the channels were for me to know what was going on in the community and vice versa. We need more funding for the community and probably more for ourselves, working together. As Maria said, it works well with PIPS and the other organisations in north and west Belfast. There is work that we are best-placed to do, and work that the voluntary sector is best-placed to do, and it is good to know what each is doing. I hope that the situation will improve when we are down to five new trusts. It is important, and I believe that the new trust system will benefit that.
258. Dr O’Kane: We do not think that service users have been profiled before in Northern Ireland; we were certainly not aware of it. We have been able to look retrospectively at the profiles of patients who come to us.
259. I have spoken about the issue to Bernie McNally, who is our director of children’s services for the Belfast Health and Social Care Trust. She is proactive in such services. She is the chairperson of the audit, and she was our original director of mental-health services. She has given some thought to developing children’s services and to the issue of patients as parents and the impact that that has on families. There is no formal process in place to try to use that information to help development in other areas.
260. Dr P Gallagher: We need to target money to the appropriate services. Between 65% and 95% of children who have been in care will have a severe mental-health difficulty, but they are limited in the services that are provided for them. That causes long-term problems in their education, their socialisation and their future development. Again, the difficulty is that child and adolescent mental-health services compete for little, and they are at the bottom; therefore, it is similar to trying to rearrange the deckchairs on the Titanic. That is all that is going on, unless a sequential fund is provided for those services, but it is a huge area. Lack of funding can lead to further problems in the future, because those children and adolescents will continue to be users of such services, and we know that early intervention has an effect.
261. Mrs Hanna: You are all very welcome. The Committee is trying to be as well informed it can, so that it can be as helpful as possible, particularly with the Bamford Review. It is seen as an opportunity. How much input did the Royal College of Psychiatrists have? Maria talked about training, but the Bamford Review refers to working smarter, and better team-working, and it sets out a vision. How involved has the college been in setting out that vision, putting it in place and making it work? You talked about training and anticipating future needs, about prevention and about all the societal reasons, such as lack of respect. Peter talked about the continuum. When you do something good, how is that mainstreamed so that it simply forms part of what everyone is doing? You mentioned the talking therapy, which makes sense, as it is always helpful to talk things through with someone. How much of the funding, if any, will be skewed towards adolescent services, since that is where there is a great need?
262. You talked about young parents. Many adolescents are also young parents, which is a huge responsibility for a young person to cope with. Then there is alcohol, which is a huge issue, and is probably the biggest public-health challenge that we face, particularly now that we have tackled smoking to some extent. It is probably the next-biggest issue.
263. How much influence and input did the Royal College of Psychiatry have in the Bamford Review? I believe in prevention rather than in picking up the pieces. How much of the budget will go on underlying causes and prevention? They are huge societal issues, but we will always be picking up the pieces unless there is more focus on particular services. How much of a mental health budget goes towards the prevention and the underlying causes, particularly of self-harm?
264. Dr McGarry: Many of our members were involved in the Bamford Review. It is a massive review, so many folks were involved. The college supports the product of Bamford, but it is a massive document with many recommendations, and, from what we hear, the funding is not that marvellous. Although we are here on behalf of the college to talk about suicide, we cannot suggest that severe schizophrenia, for example, should be ignored in the large mental hospitals.
265. We do not feel that what we are stressing would necessarily cost a massive amount of money — I want to make that clear. It is absolutely crucial that we work a bit smarter with the voluntary sector, and them with us.
266. Mrs Hanna: It seems that what you are describing is part of a snapshot of what needs to be done, and where that fits in with the overall strategy.
267. Dr P Gallagher: Proper allocation of funding is required in order to set clear projects for children and young people. The problem that all of us face is that most of the funding tends to occur on a non-recurrent basis, and it is possible for our achievements get lost because of competing demands. Therefore, a model is required in the Department to audit what funding has been used for, and then, if the evidence base is valid, to ensure that recovery can follow on from that.
268. Mrs Hanna: You are talking about Maria’s example — establishing good models, then mainstreaming them.
269. Dr P Gallagher: The Bamford Review made a lot of recommendations. To tackle death by suicide, we need to begin to target particular areas, consider funding for those areas and monitor the outcomes. It would then become a little easier to bring those plans together. That is the key for the future.
270. Mr Buchanan: Today’s discussions have covered a lot of ground. There is no doubt that prevention is the key to the whole issue. However, no matter how many preventative steps are in place, this difficulty is still going to exist because of the current culture in society.
271. After someone has had problems and has received treatment, it is the follow-up programmes that become important when that person is back in the community. What types of follow-up programmes exist, for instance, for visiting a person at home on a regular basis after they are released? If that does not happen, more problems will be created due to the stigma that is attached to this issue.
272. Dr McGarry: The home-treatment team manage people at home rather than having them go into hospital — that is the best model of psychiatry. That is not always possible, but it is more so now than it was five or 10 years ago. Preventing admission to hospital through intensive support at home with up to four visits a day is particularly effective in some cases. That model has been rolled out across Northern Ireland, and it is very good.
273. When someone is admitted to a psychiatric hospital, we have a duty to ensure that the planning for what happens after the patient is discharged is of the highest quality. That requires us to work with the multi-disciplinary team in the community, including the psychiatrist, the CPN, or the lead person in the follow-up, the social worker and the occupational therapist. That is an area of which we, as a college, are acutely aware.
274. There has been discussion of the 2004 guidelines on that matter. We are conscious of the need to ensure that everything is in place before someone is discharged, and of the need to ensure that we have the resources to support that person, and a contingency plan if something goes wrong. We are increasingly getting better at doing that than we have been in the past.
275. Some of our mental-health teams have their own recruitment problems, and that creates difficulties. We all know about the number of nurse vacancies. However, good mental-health care requires a proper treatment package for a patient — whether they are at home, in hospital or in the community.
276. Dr O’Kane’s team provides a treatment plan for when a person is discharged. That may involve the patient seeing a therapist for six weeks, it may require organising medication, or it may involve the person attending some type of day facility. That person should have a treatment plan with which they and their carers are involved.
277. We are increasingly working more closely with users and carers, and that is a crucial part of our efforts. Currently, we are not bad at that, and we will continue trying to improve what we do in respect of follow-up action.
278. Someone who has been discharged should always be aware that, in a crisis, he or she can contact the hospital or the CPN. That is happening more than it did in the past; but we could keep on improving the service.
279. Mr T Gallagher: There is a short paragraph in your submission about the issue of advertising by alcohol companies and sports sponsorship. You state that that situation is particularly alarming and that we need to examine that. I presume that you are using the royal “we”.
[Laughter.]
280. Dr McGarry: If the members do not mind that term being used, that is fine. I refer to all of us.
281. Mr T Gallagher: Do you wish to say anything more about a possible link between that matter and suicide?
282. Dr McGarry: We have little doubt that the cult of binge drinking contributes to self-harm and suicide. As a society, we must look at that very seriously. One cannot consider that without addressing some of the prevention issues. There is treatment for addiction, but, in this respect, prevention would be even better.
283. We must examine the issue of advertising and sponsorship. I am not saying that that should all be banned tomorrow, but there should be a robust debate. We must be direct with the powers that be, and the vested interests. We would be supportive of such an approach, and so would the BMA and the Royal College of Physicians, who have worked with us on addressing liver disease and the risks associated with alcoholism. If the Committee wants our support for being assertive or aggressive in that respect, you are pushing at an open door.
284. Ms S Ramsey: Professional sportspersons might not like their big wages being cut.
285. Dr McGarry: When we see young people and children with football shirts advertising beer, there is something wrong.
286. The Chairperson: I agree. The two certainly do not marry.
287. Have all the members had a fair opportunity to question the panel? I am delighted to have had an opportunity to meet you all — particularly Anne, who is a shining example of how one can come through the process successfully.
288. There are a number of small points that I wish to raise. I am not being flippant, but, given the pressures on psychiatrists, psychologists and the front-line services, who looks after your mental health? I ask because the Committee will be travelling to Scotland to see Roddy McNidder, who oversees the services provided for front-line NHS workers there.
289. Dr McGarry: Doctors are at a higher risk of suicide than average members of the population. That is a well-recognised fact.
290. Ms Ní Chuilín: That is true of vets, too.
291. Dr McGarry: Yes. Psychiatrists and anaesthetists are also prone to that higher risk. In the past, that was ignored. We are dealing with that better than we did in the past. There is some support out there, and that is something that we must examine. As part of the work of the task force, we looked at particular risk groups. We mentioned farmers as a particularly high-risk group, although we did not mention healthcare staff. We are not always great at looking after ourselves. Thank you for making that valid point.
292. The Chairperson: I think that that is an important point, having talked to so many psychiatrists who see the level of despair, anxiety and stress to the point of contemplating suicide. One cannot keep listening without being affected.
293. So many people visit my constituency office who have borne so many different problems and pressures. The problems that they have to face are remarkable. One family man has had successive tragedies in three successive years. His son was involved in a road accident; and his son is now paraplegic. The following year, his wife had a car accident. She was the main carer for the son, but she cannot now cope because her back is so badly injured. The husband has just had a car accident. The lives of all three members of that family have been wrecked by car accidents. Some of the stories that I have heard are very distressing; and I am not a professional counsellor. Because psychiatrists hear the worst — the darkest aspects of mental health — it is important that they too are looked after.
294. Dr McGarry: In my profession, we run sessions called Balint groups, where professionals discuss how they feel about the patients with whom they are dealing and the emotions that are engendered. Dr O’Kane is involved in that. Perhaps we should offer that service to our politicians. That issue is a bit like carer fatigue, and we are aware of that problem.
295. The Chairperson: It is a matter of finding a way to switch off. You folk deal with the worst cases and the lower end of the mental-health spectrum, so I am anxious that you should be looked after. I look forward to travelling to Scotland to hear about the provisions that are in place there for healthcare professionals.
296. I am delighted that there is now wider public interest in mental-health issues. That has happened for many reasons, not least because the Assembly is now up and running. We are determined to highlight the lack of mental-health facilities and tackle that problem.
297. Cross-sectoral departmental work is also important. So many young people have told me about how their mental-health and self-harm problems have arisen as a result of bullying. That is a major problem that sets a pattern in young people’s lives and leads to low self-esteem. The Internet also adds to those difficulties. There is evidence of Internet footage that shows people how to commit suicide. Do you write to the relevant authorities and the various Internet agencies to ask them to do as much as possible to remove such material from websites?
298. I am also aware that, because of text messages, a person can be exposed to bullying in their own home, even their own bedroom. I have heard about all those problems. Have you made any presentations or offered any input on the storylines of television programmes? I know that some of the television soaps have covered that subject.
299. Dr McGarry: The Royal College of Psychiatrists centre in London has a very active media unit, and it does a fair amount of work in that area. The Northern Ireland division of the college is trying to be more proactive in those areas. I know that, centrally, the college was involved in discussions on Internet sites, and it worked quite closely with the media on that issue. A part-time media officer has been appointed to the Northern Ireland division, so we are now able to be more proactive in our approach. We have a voice in those matters, just like anyone else. We must contribute on the broader issues that are involved, not just deal with mental illness on its own — and members have mentioned the importance of prevention. We have contributed and will continue to do so, and hopefully we can do more in that area.
300. The Chairperson: How accurate and reliable are the current statistics on deaths by suicide? At one stage, the figure was 150, but it has now risen to 300. How is a figure identified?
301. Dr McGarry: The current figure is probably fairly accurate. I carried out some research 20 years ago, and the figures were not that accurate then. Open verdicts were often declared at inquests because it was not considered right to say that a person had committed suicide. However, the figures from the Central Statistical Office are now quite accurate. The figures for the last couple of years have been quite bad, but I hope that, in 10 years’ time, we might look back and say that they were just two very bad years.
302. In the Republic, it was reported earlier this year that there was a significant reduction in the number of suicides. We should be very wary of year-on-year suicide statistics — it is important to stand back from that because so many factors are involved, and we do not know what they are. I believe that the suicide figures are probably fairly accurate at the moment.
303. The Chairperson: I would have liked to see at first hand the work that is being done in the Mater Hospital. The model that is being used there seems to be the one that everyone is talking about. I know that Sue has already visited the hospital. It would be nice for members to have an opportunity to visit.
304. Given that the Committee is investigating mental-health issues, we would like to take a more hands-on approach. I appreciate that, in one sense, it might seem invasive, and we do not want to involve ourselves in confidential matters. However, it would be good to see how the services operate. That might give you a headache, but it is important to see how services are delivered. I am very keen to pay the hospital a visit, so I am inviting myself and my Committee members along. A wee bit of power goes a long way. [Laughter.] I hope that the Committee will be able to liaise with you on that.
305. Thank you for your attendance. This subject is close to all our hearts and, as a Committee, we take it very seriously. All of our constituents are presented with these issues and we must work with one another collaboratively to help to resolve them. Mental-health problems do not respect creed, religion or social status. I hope that we can work together in the future and that we can secure a good outcome for mental-health provision. Thank you for your time.
15 November 2007
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Mr Tom Black |
British Medical Association in Northern Ireland |
306. The Chairperson (Mrs I Robinson): I welcome Dr Tom Black, the deputy chairperson of the Northern Ireland general practitioners’ committee (NIGPC) of the British Medical Association in Northern Ireland; Dr Danny Lambe, the deputy secretary of BMA(NI); and Mr Ivor Whitten, who is the Assembly and research officer for BMA(NI). I invite the witnesses to make a five- to 10-minute presentation. We will then have questions from Committee members.
307. Mr Danny Lambe (British Medical Association in Northern Ireland): I will say a few words, but first I would like to correct you, Chairperson — it is “Mr”, not “Dr”, Lambe.
308. I am the deputy secretary of the BMA in Belfast. The BMA is the professional association and trade union for doctors in the UK. Across the UK, more than three out of four practising doctors and the majority of medical students are members of the association. In Northern Ireland, the BMA represents approximately 4,000 members from every branch of the medical profession.
309. As I have said, we are the recognised trade union for doctors, and we negotiate on behalf of the Government on contracts and on terms and conditions. We produce a range of publications on health matters and medical ethics, and we also produce the ‘British Medical Journal’, which is an internationally renowned medical publication.
310. Dr Tom Black (British Medical Association in Northern Ireland): Thank you very much for this opportunity to appear before the Committee, Chairperson. The Committee has already received our submission, so I will not read through it.
311. Given that the Committee has seen a great deal of information on the subject of suicide and self-harm, I am sure that it will appreciate that it is one of the most intractable and difficult problems that we face. Earlier, Sue Ramsey discussed the case in Omagh, and as she was saying, every case is a dreadful tragedy. No two cases are the same — each has its own story and background. Each suicide appears to be a single event that is similar to others, in that it is an end point. However, the stories that lead up to each suicide are different. It is a bit like asking whether we can find a cure for cancer. That cannot be done unless we must look at the different types and causes of cancer. Dealing with suicide is as complex a problem as that. Therefore, it is a multilayered and multifactorial problem, and we need complex and holistic solutions — all the buzzwords are there.
312. I would like to hit a few of the targets that I see as a GP who works at the coalface. The first is, obviously, prevention. We are looking at ways in which to raise awareness; training issues; ways in which to help bereaved families; and risk factors, such as alcohol and drugs. A huge amount of work is being done on the matter, so, needless to say, I have spent the past three weeks reading everything that has ever been written in Northern Ireland on the subject. The amount of work and training that already goes on would knock members down. For example, in the Foyle Health and Social Services Trust, which covers the Derry area, 600 people trained on suicide awareness alone. That is an amazing number, and that pattern is replicated throughout Northern Ireland.
313. Secondly, we must also recognise depression early, and provide treatment. We must consider the number of psychiatrists that we have, as well as the number of available beds in psychiatric units, and strike a balance between treating patients through drugs and through talking therapies. Cognitive behavioural therapy (CBT) is the one most commonly used.
314. A third area, which is close to my heart, is emergency assessment. The speed of response for somebody who is in crisis is crucial. They must be assessed on the day, and, if necessary, brought to a safe place.
315. Self-harm is the fourth area that I wish to highlight. Although suicide is a huge problem, self-harm is 30 to 40 times greater. The key relationship between the two is that 51% of suicide victims have self-harmed before their death. That means that, were self-harming dealt with, 51% could be caught.
316. Admittedly, not every person who self-harms will go on to commit suicide. In the year after a self-harm incident, there is a 1% possibility of a person’s attempting suicide, but that percentage rises to 3% to 4% within five years. Therefore, we should focus on the self-harm group and ensure that they receive follow-up care. Everyone who self-harms is offered follow-up care, but 60% do not receive it. It is important to ensure that those individuals undergo psychosocial assessments and that a care plan be devised for them. We must work really hard and focus on those who are most vulnerable, and then consider the number of psychiatric beds and psychiatrists available.
317. I have also spoken to a number of child psychiatrists and adult psychiatrists to try to tease out the issues involved. Where I work, there are many problems with suicide. The public come to see us to express their concerns, one of which concerns the issue of detention. For example, some people may tell us about a relative in crisis who was admitted to hospital, only to sign himself or herself out after a few days.
318. That issue must be examined, particularly for those people with a personality disorder. Under current legislation, a personality disorder is not classed as a mental illness. Therefore, people with a personality disorder can undergo an assessment, yet they are allowed to discharge themselves because they are not considered mentally ill. Only people who are deemed mentally ill in law can be detained. Issues will arise in future as a result of the Bamford Review of Mental Health and Learning Disability. We will be able to consider mental capacity instead of mental ill health in an effort to detain people who are a risk to themselves but who may be assessed as having a personality disorder rather than a mental illness. However, I acknowledge that that will raise human-rights issues.
319. Finally, I want to emphasise the huge amount of work that is being carried out in the voluntary sector. I could rhyme off a list of acronyms of organisations from now until tomorrow, all of which are doing very good work. We have already heard about how schools are involved in that work. Again, I do not want to talk about specific cases, so I will try to talk in general terms. If a schoolchild has had a particular experience, one could perhaps go to the school to ensure that it offers the counselling required and that the child can access the necessary services and expertise through the local health board and the health trust.
320. If it suits the Committee, I will end my presentation there and take questions.
321. The Chairperson: You may be aware that the Committee has just returned from a visit to the Scottish Parliament, where we looked at its model of care for suicide prevention. The Executive’s strategy and action plan, ‘Choose Life’, which was introduced in 2002, seems to be at a fairly advanced stage. Has BMA(NI) looked at that model or at any of the materials that it has made available to target self-harmers in particular? Have you done anything to replicate Scotland’s efforts? Have you made any proposals that would reflect how well the Scottish Parliament has succeeded in preventing suicide? There has been a significant turnaround in Scotland — 117 suicides were prevented between 2000, when records were first kept, and 2006. There was a drop in the number of suicides in Scotland in that period.
322. Dr Black: Scotland has a big problem with suicide. It has an incidence of 17 suicides per 100,000 people. I have no intimate knowledge of the Scottish model. I recommend the huge amount of work that is being carried out on the suicide prevention strategy by boards and trusts. Much good work is being done here.
323. My reading of international information is that, if we do all the right things and work very hard on awareness and intervention, the initial result will probably be an increase in suicide rates in the first two years. That appears counter-intuitive, but it is the international experience. In five to 10 years, however, information suggests a decrease in instances of suicide of somewhere between 15% and 20%. That is a quite disheartening statistic. We must appreciate that, even if we do all the right things, a problem with suicide in Northern Ireland will remain. We still need to do all the right things and try to achieve that 15% to 20% reduction, if only to stem the tide. Northern Ireland’s target is a 15% reduction in suicides by 2011. It will be difficult to achieve that target.
324. The Chairperson: The Committee has discussed young people who present in distress at A&E units. More often than not, their behaviour is erratic, so security guards tend to remove them. Such behaviour is obviously a cry for help, but those young people go off into the night and, unfortunately, proceed with suicide.
325. What is your view on having dedicated areas in A&E units in which voluntary groups, such as the Samaritans, could be in attendance on a rota basis? They could help to settle that young person. The necessary clinical expertise that is required to help them could then be provided, on another rota basis, that might prevent that young person from going off into the night distressed and possibly taking his or her life.
326. Dr Black: I have worked in A&E units, out-of-hours services and general practice, so I deal with such issues daily. I work in a deprived area of Derry, the Bogside, which has faced problems similar to those being faced in parts of Belfast. We must be more receptive and display an open-arms attitude to those young people, particularly to young men, because they are the most vulnerable group. The male to female ratio of suicides in people of that age is 10 to one. We must have that open-arms attitude and take those young people down a different path, because they often present in crisis, often with what we might consider to be behavioural problems and often with alcohol consumed. Dedicated areas in A&E units would be a good idea.
327. The Chairperson: As you have said, there are higher suicide rates among young men. In Scotland, cards are distributed at football stadia that state that it is OK to talk. That is a worthwhile strategy. There is a macho image of men being incapable of opening up in the same way in which women will in the hairdressers’, over coffee or in shopping centres. Women are good at talking. Men are also good at talking but not about personal health issues or depression.
328. The Scottish strategy of targeting masses of young men at football matches was innovative. The cards that were handed out were fantastic. They made it clear that it is right to talk and that it is right to contact someone. The cards also provided emergency contact numbers. That idea could equally effective if rolled out here.
329. Dr Black: The first poster that people see as they enter my surgery is titled “If your head’s away, just say”. They then come across is an image of John Duddy, the famous boxer from Derry, who supports the Samaritans. We also have cards bearing his image. Those posters represent attempts to identify that group of people to which you refer. However, that is difficult to do, as young men often do not self-harm or suffer from depression — they just present without any warning and leave their families devastated.
330. Mrs O’Neill: What are your views on the GP uptake of training in suicide and self-harm prevention? Does more need to be done to attract more GPs to it? How successful has the Department been in getting GP buy-in to the Protect Life strategy?
331. Dr Black: There were some initial problems, but the good news is that one third of all GPs have already been trained. Next week, Dr Deeny and I will go to our training in the Western Health and Social Services Board where we will be training every GP.
332. Ms S Ramsey: Did Dr Deeny not take up the training?
333. Dr Black: He is going for the second time. We will cover every GP in the Western Board, so more than half of the GPs will have then been covered. I would rather give you that piece of good news than say that there was some bother at the beginning.
334. A GP will come across a patient who takes his or her own life only every six years, so it is a rare occurrence for a GP. It will happen about once every one or two years in a practice. We have bought into the training, because self-harm is common. We carry out assessments, and, at times, we need to then take a psychiatric assessment of a patient. However, we still go home at night with that worry in the back of our minds.
335. Mrs O’Neill: There is a tendency to refer to the next level those children who have emotional difficulties. Is putting more resources into primary care the way in which to deal with the problem? For example, should children be referred in order that they might be treated with talking therapies, and so forth?
336. Dr Black: Sure Start is great; health visitors are brilliant. a great deal of work is being done in that area, and we hope that it is targeted at the areas in which it is needed.
337. Child and adolescent psychiatry is a difficult area. Doctors might wait a couple of years, or write numerous letters and make many telephone calls, to get a referral, while knowing fine well that children who are in a worse condition than their own patients are blocking the system. During the week, I spoke to a psychiatrist who deals with children, and I asked her whether she had any suggestions. She said that more funding and more jobs were necessary. However, she also said that even though a funded job is currently available, it cannot be filled. Therefore, whoever gets that job will have to be trained.
338. Interestingly, that psychiatrist also said that children have to be reached before they are five years old. However, psychiatrists who work with adults tell me that patients need to be reached before adolescence. That is what Sure Start does, and it is well funded for that purpose. I congratulate the Assembly for pushing lots of money on to that project. We hope that it works, as it is certainly getting a great response.
339. Ms Ní Chuilín: You said earlier that 51% of suicide victims self-harmed before their death. That is very concerning. Although I am not saying that everyone who self-harms goes on to end his or her life, that figure is an indicator, and, somewhere along the line, it is being ignored. Even certain professionals, such as those in the veterinary, dental and medical professions, are at a high risk of suicide.
340. You mentioned out-of-hours surgeries. Were you referring to a service that is similar to the Association of Belfast Doctors-on-Call (BELDOC), or to an out-of-hours surgery for people who are suicidal? We have all raised that issue. A&E is great for treating a broken finger, but it is not great for people who have mental-health problems. It is too busy and chaotic, and it deals with acute complaints. As Iris pointed out, people need to go somewhere that is separate from A&E if they are under the influence of drugs and alcohol. Out-of-hours surgeries need resources in order to make them safe. People do not use a Monday to Friday, 9.00 am to 5.00 pm surgery to ask for help but often go to after-hours surgeries. New Lodge and Ardoyne are in my constituency, which is a stone’s throw away from here. There are terrible incidences of suicide and self-harm in those areas. I feel sorry for A&E staff, because some youngsters go to the hospital who, if they are not seen right away, walk out. Could more be done to provide for a better out-of-hours service? Could such a surgery be provided beside an A&E unit, even if it were separate?
341. Dr Black: I am talking about GP surgeries and the out-of-hours surgeries in the Western Health and Social Care Trust, which before that were known as Foyle Doctors-on-Call (FOYLEDOC). We tend to have patients who ring to say that they have suicidal ideation or intent and that they have a history of depression. We bring them to the surgery, do an initial assessment with the community psychiatric nurse (CPN) to whom we have access to ascertain whether the person needs to be formally admitted to hospital. That works well. Many people use the out-of-hours surgery; probably about two or three times more than use A&E make use of the out-of-hours surgery. That represents an interesting shift, because the perception is that A&E catches all types of patients. As we know, suicide involves no single issue; therefore, A&E catches a different patient profile, such as those who present with overdoses, because that is the appropriate place for them. A&E also takes in people who have been knocked unconscious through inebriation or through the inappropriate use of illegal drugs. Therefore, those patients get a different profile. That means that both types of profile need to be covered.
342. Given that GPs know their patients and their history, they should be the first port of call. Histories for patients such as those about whom we are talking are repeated. Without going into individual cases, patients who self-harm do not disappear but come back repeatedly. Their GP may refer them to many places, but they do not follow up on one appointment, do not attend others or discharge themselves from hospital. A GP can see a crescendo building as the patient’s life deteriorates. Of course, they do not all commit suicide — perhaps only one in 20 does so.
343. Dr Deeny: I welcome Danny, Tom and Ivor. I, too, have a great professional interest in those aspects of health provision.
344. Chairperson, I read your newspaper article on talking therapies. Those certainly seem to be the way forward. We certainly do not have enough provision. Tom referred to the fact that it is so frustrating for a GP who is confronted with such illnesses, particularly in a young person. I tell people that I wish I could have them seen next week, but I cannot do that. Sometimes, therefore, a GP is forced into prescribing medication that may or may not be appropriate. That is a terrible tragedy.
345. I must mention something that is important for Tom, the whole medical profession and, indeed, for society. I worry that everything is being medicalised — every behaviour seems to be considered a medical condition these days. Personality disorder has been mentioned. It is a most frustrating problem. Some people will be referred to in the community as having psychopathic or sociopathic personalities; however, they do not have a mental illness, according to the criteria. There are no powers available to force them into hospital or to keep them there, yet they are liable to do anything. That is a major problem for society. However, one cannot medicalise everything or make every behaviour a medical condition.
346. My question, addressed to all the witnesses, but to Tom in particular, is as follows. A macho culture is a serious problem here, as I am sure is true of Scotland as well. All health professionals must play their part; however, the education authorities and the Churches have a major role to play in placing the value of human life back of on the agenda. People seem to think nowadays that taking their own life is an option.
347. We have seen an awful event this week in Omagh. I do not intend to highlight that case alone, but if that case is as it appears to be, not only has a person decided to take his own life, but he has decided to take his whole family with him. That is an awful situation. We must liaise with the Churches and the education authorities in stressing the value of human life to children from an early age.
348. Perhaps I am asking this question of the wrong people, and I should be asking the Department, but has this situation arisen due to a lack of funding? Is it about under-resourcing, or bad resourcing? Witnesses have mentioned that there should be wider access to talking therapies. As doctors and members of the Committee, everyone here agrees on that. Every one of us supports better funding for mental-health services. Is the money all going in the wrong direction? We need more people to do the talking and the counselling.
349. That is the frustrating thing that Tom described well. In my time as a practitioner, I have come across two young fellows who gave no indication of sinking into depression, yet, without warning, they killed themselves. We had no means of predicting that that might happen. If they had had somewhere to go to talk through their problems, or to get rid of their macho image, that might have made a difference.
350. I am also concerned about the state of paediatric medicine. The way that society is going means that everyone is worried about being sued. My brother is a solicitor, and I often tell him that his profession is destroying our world. Everyone talks about suing. It seems to me that that has resulted in fewer doctors wanting to study paediatrics and to become child and adolescent consultants. They have concerns about working with children, because of the possibility that something unfortunate might happen. That is a sad situation. Tom mentioned an example of an available child-psychiatrist post, and it worries me that there has been difficulty in filling it. In Northern Ireland, GPs wait for a year or more for appointments and homes for their young patients.
351. Does Tom want to see money redirected from wastage in the Health Service into those services? In particular, does he want to see a concentration on talking therapies and on child and adolescent mental health?
352. Dr Black: I will take those points in order.
353. One of the main problems with suicide is that it is contagious. People talk about “imitation” and “copycat” behaviour. I do not like those terms — I prefer the word “contagious”. Suicides then happen in clusters, as we have seen in Northern Ireland. A problem that then develops is that communities lose faith in us, the public servants — in health, in the community and in politics — to whom they look for resolution of the situation. Kieran is correct. It is not a medical model that is required but an integrated one.
354. One hears about multidisciplinary teams, but the community, the Churches, the police, the schools, the voluntary sector and everyone must be involved. The more that I consider this problem and the more BMA presentations that I give, the more I sound like my granny. Young people must drink less and be home at an earlier hour. They must do as their parents tell them. They should be going to a church of some sort so that they develop a moral spine and core values. That all sounds very Victorian, but it would be good for them and good for us. We are all part of the community, so this is not a medical model; it is an integrated model.
355. I give two types of interview every year. One interviewer starts from the premise that GPs prescribe too many antidepressants; and the second interviewer starts from the premise that GPs are not prescribing enough antidepressants — that we are under-diagnosing. There is always a gap between these interviews, but sometimes the gap is as little as two weeks. The situation lies somewhere between those two extremes. My practice has a 50% above average rate for antidepressants, because of the location in which I work and also because my patients have to wait three to six months for access to CBT. The access that I have is group therapy, and that does not suit young men. It would be great to have better access to CBT.
356. The tension between medical and legal aspects is well founded. It does not affect GPs too much at the moment, because the relationship between the GP and the patient is based on continuing care. Most people are still with the same medical practice that they started with — I am. A bond of trust builds up between a patient and the GPs who have been in that practice for 20 or 30 years.
357. However, the medical/legal issue is an increasing problem in hospitals. The recent Queen’s Speech contained an announcement that the standard of proof required to take a complaint against a doctor to the GMC will be changed from the standard of proof in criminal cases — “beyond reasonable doubt” — to the civil standard of proof — “balance of probabilities”. That means that doctors will now lose cases on a 51% probability. When that provision becomes law, people should expect defensive medical practice.
358. I will make a brief point here, although I should not really do so on this occasion. That issue will come to the Assembly, which has legislation rights on medical regulations, so Members can make up their own minds. The situation will get much worse. We do everything like the Americans do, although we are 10 years behind them. In many parts of America, people are unable to obtain the services of an obstetrician, because it costs obstetricians $300,000 to pay for legal defence, so they are unable to work.
359. I am sorry: I digress.
[Laughter.]
360. The Chairperson: You may as well make the most of your opportunities.
361. Ms S Ramsey: I thank the witness for his presentation: there is a lot of common sense in it, so I do not mind his digression.
362. Committee members visited Scotland recently. The Committee is conducting an inquiry into the issue of suicide and self-harm, and I hope that, when it is finished, members will be able to make recommendations. I assume that the Committee will have the co-operation of two other Departments besides the Department of Health, Social Services and Public Safety, because a joined-up approach is necessary.
363. I was interested to hear your comments that suicide is contagious, presents in clusters and affects the community in that it loses faith in its leaders. For a long time in the medical profession — in hospitals, social services and among GPs — the right hand did not know what the left hand was doing. I do not mean to be negative, because the Health Service is making progress. Will the amalgamation of Health Service trusts, and hospital trusts, make a difference in that various sectors will communicate better? Young people present themselves at hospitals with a multitude of issues, but the relevant community services did not know what was happening to them. I hope that the services will use a joined-up approach to provide individual packages of healthcare to people who present.
364. Dr Black: Communication among primary care, secondary care, community care and the voluntary sector is the key. The last time that I spoke to Ms Ramsey, we talked about the Hayes Report, which dealt with the integration of social care, healthcare and community care. The logic is that it should work better. One cannot fail, when considering the report, to realise that it is the sensible model to adopt. I hope that that is the case and that it does improve matters. Generally, GPs are of a mind that a community psychiatric nurse (CPN) should be attached to their practice, so that he or she can deal with the patient’s family. At my surgery, the health visitors are brilliant. They know what happened to a child with whom they dealt five years ago, and what has happened to his or her cousin, and so forth. The BMA thinks that a CPN should probably be attached to a GP’s surgery. Most of those services are attached to areas or patches. However, that is a different argument.
365. Ms S Ramsey: As the Committee is now coming to the end of its inquiry, I am trying to tease out matters so that they may be addressed in our proposals. You mentioned suicide clusters — or that suicide is contagious — and said that the community is losing faith. In my opinion, the reason that communities are losing faith is because they were not inundated with help or support, whether that be from GPs, CPNs or people in the community. That is the point which Kieran and the Chairperson made earlier. There must be a proactive approach to whatever is happening in the community, and the recent fire tragedy in Omagh relates to that. Rather than waiting for things to happen, society should be proactive. Do you think that society has been proactive, up to the point where the professionals — in a community and a medical sense — are on the ground and targeting whatever issues are there in an effort to try to stop the contagion of suicide?
366. Dr Black: That is a good point. The reason that I raised that issue is because I am a member of my community. I will try not to mention specific cases — because there have been quite a few in Derry recently — but I will say that I talk to people, and they will ask me why a particular patient was not detained? Why was that patient unable to access that service? What has been done about that matter? I have tracked those complaints.
367. Last Friday, I had a meeting with the deputy chief executive of the Western Health and Social Care Trust, Joe Lusby, who is the director of planning and performance. I discovered that a lot is going on in the background. I also talked to the co-ordinator of the suicide intervention group, who is working with schools, and to the psychiatrist who is dealing with the issue of detention for people with personality disorders. A lot of work is being done behind the scenes that is not being publicised and explained to the community. I wonder if that is a good or a bad thing because, as we all know, there are consequences if we raise too high an awareness of the issue. Obviously, a balance must be found. Therefore, GPs and local politicians have a role to play by going to the media and saying that the matter is being dealt with, that counselling is available in such and such a school, that we will consider the issue of detention for people with personality disorders, and so forth. We need to build up the community’s confidence. However, a huge amount of work is being undertaken by many people.
368. Mr Easton: Drugs and alcohol play a role in some suicides or affect some of the people who have presented to you with mental-health issues. Do you feel that Northern Ireland is falling behind in the provision of services for people with alcohol or drug addictions, and that — even when we do have those services — we fail to follow up on mental-health issues that are derived from those addictions? I am also keen to explore whether the media has a role to play in a suicide prevention strategy and in the comments that they make — at times — in their reports?
369. Dr Black: Alcohol has a huge part to play in the matter. It exerts, perhaps, four times the influence of that of drugs. The BMA has a policy that states that an increase in the price of alcohol will lead to a decrease in access to it. If access to alcohol is decreased, the consequences are similarly decreased. Personally, I would like to double the price of alcohol tomorrow. I would like to do that because it is 40% cheaper than it was 15 years ago. If the price were doubled tomorrow, that would constitute a 20% increase in the price of alcohol when compared with that of 15 years ago. That is all that would happen. Therefore, if the price of alcohol were doubled, that would improve matters. I realise that that is another issue, and that my solution is rather simplistic.
370. In the Western Board area, there are 90 registered agencies that deal with alcohol and drug treatment. Our problem is that young men who have alcohol problems have tried at least six of those agencies. I sometimes wonder whether there is too much choice. They go into the Northlands Treatment Centre, and they either like it or do not like it. They may go into an addiction treatment unit, which, again, they might or might not like. Then they might go down to Sister Consilio at Cuan Mhuire. There is a lot of choice about access to treatments.
371. Alcoholism is an intractable problem and the success rate is low. Much work has been done on alcohol treatment; however, in considering suicide prevention, it is a key area. At the time of committing suicide, 37% of people have taken alcohol. I sound like my granny again in suggesting that the price of alcohol should be increased. That message is not popular, and one sounds like an old fuddy-duddy who is ruining everybody’s fun. There would be a huge improvement in healthcare if ordinary people who drink a bit too much were persuaded to drink less. That would not address the problem group, but consumption could be reduced by such a general proclamation.
372. The media have a huge role to play, and people in the media have undertaken suicide awareness training and are careful in how they treat the subject. Nowadays, the news of many suicides is passed by word of mouth, and, because the media is so careful, one does not hear about them on the media.
373. The Chairperson: An exception to that was the news of the three young boys who took their lives. I thought that that coverage was insensitive and sensationalist.
374. Mr Buchanan: You mentioned the huge amount of behind-the-scenes work. How is that work being integrated? What could the Department do to assist those people at the coal face who are attempting to improve services for people with mental-health problems?
375. Dr Black: If you ask a GP a question, you will get a GP answer. People attend various hospitals, A&E departments, community psychiatric nurses and psychiatric services. Therefore, because records of any such visits come back to a patient’s GP, GP records are the only integrated healthcare record that is available. It worries me a little that some voluntary-sector services do not provide GPs with records. If a person with alcohol or drug-abuse problems enters a voluntary-sector institution for six weeks, perhaps his or her GP should know about that. However, that raises issues of confidentiality, and so forth. The general practitioner should be the single integrated point of record. GPs have the primary-care responsibility and are often the person that the patient comes to see. People who commit suicide have, on average, seen their GP in the previous two months.
376. My answer on how the Department could help is probably the wrong one. There is no single thing that the Department can do. Assistance is multilayered and multifactorial, and the Department’s focus should be on the voluntary sector, communities, schools — on everything — and not just on cognitive behavioural therapy. The worst thing is that there might be some improvement only if everything is done correctly.
377. The Chairperson: Although you felt that you were beginning to sound like your granny, I am a granny, and I believe that you are absolutely right. Society has lost many core values, and the solutions to its problems will not simply come from the statutory and voluntary sectors; they must also come from the community — particularly from the Churches, the police, schools and educational institutions.
378. If nothing else, we must get across to people that they must seek out others in order to talk and explore what is going on in their heads. Perhaps, that will cut the number of tragedies that families across Northern Ireland are experiencing. As Kieran mentioned, rural communities must also deal with a lack of infrastructure, and people there are isolated.
379. Age Concern’s submission to the Committee highlighted suicide statistics for older people and stated that the leading cause of suicides in that age group is depression. The document also states that nearly half of the older people who take their lives visit their GP in the month before they commit suicide. What more can GPs can do to detect and treat older people who may be at risk?
380. Dr Black: Much has been done about making connections. When a house in Galliagh burnt down, I discovered that the local community group phoned 300 old people in the area every morning. I never knew that, even though many of my patients live in the area.
381. Ms S Ramsey: That project is called Good Morning Galliagh; I know about it, even though I live in Belfast.
382. Dr Black: So much good work is being done. GPs see each elderly patient about 12 times a year, so they probably would see them in the last month of their lives. The keys are recognising social isolation and the early diagnosis of depression. So many symptoms of depression can be construed as symptoms of old age, and we must keep an open mind about that. I hate to say it, but we have been seeing an increase in the diagnosis of depression among elderly people recently. I have no doubt that I will be interviewed about that soon. GPs have a definite role to play in preventing suicide among elderly people.
383. The Chairperson: Thank you for giving the Committee your time, for your very interesting presentation and for answering our questions. It is fair to say that the Committee is very much with you in trying to deal with the dreadful issue of suicide and finding a means for its prevention. The Committee has a lot more work to do, and it cannot be complacent. Thank you, Tom, Danny and Ivor, for coming today.
29 November 2007
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Rev Dr Robert Coulter
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Mr James McBennett |
Niamh Louise Foundation |
|
Ms Michele Baird |
South Antrim Rural Support Network |
|
Mr Raymond Craig |
Oakleaf Rural Support Network |
|
Mr Colm Donaghy |
Southern Health and Social Care Trust |
384. The Chairperson (Mrs I Robinson): This is a joint evidence session with representatives of the Rural Community Network and the Niamh Louise Foundation. Members have been provided with the witnesses’ written submissions.
385. I welcome Raymond Craig from Oakleaf Rural Support Network, Michele Baird from the South Antrim Rural Support Network, and Catherine McBennett and James McBennett from the Niamh Louise Foundation.
386. I do not know whether you are aware of the procedure for a Committee meeting, but you are most welcome, and we look forward to hearing your presentations. You have 10 minutes to make your presentation, and then we shall open the meeting for discussion.
387. Mr Raymond Craig (Oakleaf Rural Support Network): Thank you for the opportunity to contribute to the discussion on suicide prevention.
388. We, of course, have a particular interest in the issues of rural communities — although that does not mean we are in any way at odds with urban communities. Some 40% of the population of the Province live in rural areas, so we are concerned with a significant number of people.
389. As members know, there is a distinction between rural and urban settlement patterns; their way of life; the way in which people do things; and the concerns that they have. One of our main concerns is how we can ensure that the rural population has access to services that are comparable with those for people who live in cities. I am sure that members will take up that point later, and develop it through questions.
390. What makes living in a rural area different? There is a problem with the perception of confidential material in rural areas, because there are generations of people who know one another in those neighbourhoods, and people are inclined to keep their business to themselves. There is also a crisis in the farming and agriculture industry in respect of debt management. The rural way of life can result in particular pressures, and there may be a stigma attached to accessing help and support, particularly when one does not know how to go about doing that, because access to such support is not as well signposted as it could be.
391. I do not intend to hog the floor — my colleagues have plenty to say as well.
392. I shall finish on a statistical point: the rural population has experienced suicide rates of up to 12 per 100,000 people. The urban rate is around 8·6 per 100,000 people and, unfortunately, Banbridge has the highest rate of suicide, at 14·5 per 100,000 people. I say that to illustrate the point that suicide affects the entire Province.
393. I know for a fact that many of our incidents may be confused with, or concealed as, accidents. Often, when we hear stories about young people alone in their cars hitting trees on a straight piece of road at 3.00 am in the morning, we question what really happened. The statistics may not reflect the true depth of the problem.
394. Ms Catherine McBennett (Niamh Louise Foundation): I am wearing two hats today: I am representing the Niamh Louise Foundation, but I am also speaking from personal experience as a bereaved mother. I lost my 15-year-old daughter to suicide, and the idea of setting up the foundation was a reaction to the lack of services that I encountered after the death of my child. There were plenty of such services in urban areas, but nothing to meet our needs at that time.
395. Since then, with old traditional standards still being very prevalent in rural areas, and even though we are campaigning locally every day, the stigma is still very strong. The foundation and local groups need more help to destigmatise the issues of suicide and self-harm. The foundation is not only concerned with prevention — it is also trying to help families in the aftermath of suicide and to encourage them to come forward.
396. There is a suicide and self-harm strategy in place, and I welcome that, but, in rural areas, a more softly-softly approach is required, owing to the stigma and the old traditional values.
397. The key is the allocation of resources and the use of prevention, rather than intervention, which reduces stigma through education.
398. Ms Michele Baird (South Antrim Rural Support Network): Towards the end of last year, the Northern Health and Social Services Board commissioned us to carry out a mapping and scoping exercise into the provision of services for mental health and suicide prevention in the Northern Health and Social Services Board area. From that exercise, we found that there was no evidence of postvention work or of self-help groups operating in the northern board area. That was particularly evident in Ballymena, which had just witnessed a spate of suicides by young people when we visited.
399. We also found that there were over 102 community and voluntary-sector organisations in the northern board area that had registered that mental-health care was either their primary or secondary objective.
400. The board provides a wide range of services in respect of mental ill health and suicide prevention. However, we contend that the problem is not a lack of available support services — except in postvention work — but a lack of co-ordination among those services. In partnership with the board, the Investing in Health strategy, and other networks in the area, we are examining specific ways to overcome that. One is a co-ordinated approach at local level — through voluntary and community-sector provision — and through the board, which is examining how it can co-ordinate with Departments and sectors.
401. The need to access services was identified as a key priority and, with that in mind, we examined the idea of establishing a physical hub in two or three locations within the northern board area that people could identify as a point of access to the available services. We recognise that access to a physical hub may not always be appropriate in rural areas because — as Catherine has highlighted — there is a stigma attached to mental-health problems, and a feeling of isolation. We want to start a series of training exercises and identify key community leaders — from Churches or the community — who can be trained to support people with mental-health problems or those who are suicidal.
402. The provision of a range of co-ordinated services at various levels will provide a more effective response than the one that is currently in existence.
403. The increased numbers of foreign nationals who live in rural areas, particularly in the northern board area, bring specific and separate issues. In the first instance, many are not registered with GPs, so the first point of contact is not available. Furthermore, when foreign nationals are placed under emotional or financial stress, the pressure is greater for them than for indigenous people because there is no family structure available as a support mechanism.
404. Ms C McBennett: Michele has talked in depth about the rural issues in the northern board area. I want to highlight those issues that overlap the northern and southern board areas. Everyone seems to have their own remit. That is why we are representing both the southern and northern board areas. The issues overlap from one area into another, and we feel strongly that that must be addressed. We have taken the initiative to come to this meeting together, even though we are from different board areas. Rural issues cannot simply be put into boxes.
405. Mr R Craig: To extend that point, there are 12 rural support networks that cover all of Northern Ireland, two of which are represented here today. They offer a clear delivery mechanism for support for local people. We cover a range of topics that affect rural communities, including issues facing new citizens and migrant workers. Within our delivery mechanism, there is an opportunity to provide co-ordinated support to rural communities.
406. However, each network receives a different level of funding from its respective health board. An audit of the 12 networks showed that they all work actively with the health boards, but that does not mean that their actions are co-ordinated. Community groups may be able to access money to deliver programmes aimed at the prevention of suicide, but their product is not being harmonised, and, to extend the analogy, there are 12 different shops. Although each health board is proactive in using the mechanism of the rural support networks, those networks do not deliver a harmonised product, and it may be useful to consider that.
407. The Chairperson: I am delighted to welcome you to our meeting. On behalf of the Committee, I extend our sympathy to you, Catherine and James, on the loss of Niamh Louise in 2005. It is said that time is a great healer, but it is hard to accept that any amount of time is enough for a parent to get over the loss of a child. Our condolences are with you.
408. The broad theme of your presentation is that there should be a holistic, seamless approach to the services that are available throughout Northern Ireland, and that the back-up support should be the same wherever one goes, rather than being provided in isolated boxes. I take the point that Churches and others, such as educational groups, must be involved, and the Committee has taken steps to engage with such groups.
409. The Committee has targeted this particularly traumatic area of provision because of the rise in completed suicides throughout the population. There is no pattern, nor does suicide affect any particular age group. It affects people right across the board and of every social status. That is why we embarked on tackling what we consider an extremely important issue and why we invited you here today. We will hear from further witnesses before preparing a report for the Minister.
410. I invite members of the Committee to ask questions or comment on what they have heard.
411. Mrs O’Neill: You are all very welcome; thanks for coming along today. Catherine, in your written submission, you highlighted the poor communication between public bodies and organisations such as yours. Has the Protect Life strategy improved the level of communication? Is the Southern Health and Social Care Trust of great support to your foundation?
412. Ms C McBennett: The strategy is only a starting point. There is always a need for more communication, but groups such as ours are not sufficiently referred to in research and information. The many leaflets that are handed out rarely refer to bereaved families or to how organisations such as ours manage to intervene and enable people to access the appropriate resources.
413. The Protect Life strategy is a start, but it is not enough, and, without meaning to sound derogatory, there must be improvement and a more direct link with community organisations such as ours.
414. Mrs O’Neill: Your submission also mentioned how you would like to open a centre where people can call in and get information. Is that being progressed with the help of the trust?
415. Ms C McBennett: I put my views strongly to the trust, which is aware of our plan. However, since the introduction of the Protect Life strategy, the trust has also started work on suicide prevention, and I respect it for doing so.
416. We take a ground-level view: meeting people who are self-harming and who are suicidal, and the bereaved families, and what we have learned is that they do not want to walk into a centre that is labelled “suicide awareness” or “mental health”. They would rather go to a place where there is access to information or help, within a resource centre where there is perhaps a coffee shop, a library, and a drop-in centre, but, bearing in mind the rural stigma, where no one will notice them walking in — which might prevent them from seeking help. The idea of such a resource centre is to take away the whole problem of stigma, so that people can access help through correct information and available counsellors, and to give it a friendlier, open-door atmosphere.
417. Mrs O’Neill: I represent Mid Ulster, and I entirely understand where you are coming from. I am very aware of the situation in rural areas, where everyone knows everyone else’s business. Your idea is fantastic, and I will support you as much as I can in moving it forward.
418. Ms C McBennett: Thank you.
419. Mr Easton: You mentioned the stigma that is attached to suicide in rural communities. In what way will you try to address that?
420. Mr R Craig: The stigma stems from the culture, and the approach needs to be based on education and information. Suicide will not be understood as a journey, and not just a final act, until there is greater awareness of the suffering that anxiety causes — mild and serious anxiety can lead to depression. There is an entire journey before the final act of suicide.
421. Through education, information and raising the topic in a public setting, we can increase awareness, because a stigma goes on existing when an issue is kept in the closet.
422. Ms C McBennett: I agree with Raymond. We have actually been told not to speak in public about our daughter’s suicide in case it would ideas into someone else’s mind. However, as research has shown, when someone is thinking of suicide, it is already on their mind. Talking about it can only destigmatise it and open the door for therapeutic intervention. Therefore, the more we talk about it in a natural way, the better.
423. There is no stigma attached to going to hospital for a physical complaint, such as a heart attack, and yet there is when it comes to mental health. We in the foundation want to see people getting help without feeling guilty about being on antidepressants, which carries a stigma of its own. We must try to get rid of that and encourage people to seek help, because there is nothing to be ashamed of. Depression is an illness like any other, and, as Raymond said, getting help can prevent that final act of suicide, which is the final straw when someone has not had the appropriate intervention.
424. Ms Baird: We have all seen television reports of how whole communities feel they have been affected when suicide happens in an urban area — everyone feels the impact, and so the family feels the support of everyone around them. In a rural area, however, the family is more isolated, because the wider impact does not seem to be felt by the wider community.
425. We need to take a step back and examine the issues that affect the entire rural community, such as the changes in agriculture, the impact of recent diseases in animals, and other external pressures, and use them to create a sense that suicide affects the wider community, and not just an individual.
426. Mr R Craig: There is also an opportunity to address the issue in a positive way, because people find it very difficult to talk about suicide. Positive mental-health attitudes need to be encouraged, such as involvement in sport, daily activities, and awareness of the impact of alcohol and drug abuse on the body. We need to educate young people, and everyone else, to understand the risks that they engage in due to the lifestyle that they adopt. Talking up the positive will help to prevent suicide.
427. Dr Deeny: Thank you. You are more than welcome, and I am sorry that I missed the first few minutes of your presentation.
428. I have worked as a GP for 21 years in a rural area, and I take on board what you have said. The aim should be to prevent all illnesses, and particularly to prevent suicide. Catherine and James, all members of the Committee feel for you.
429. I have encountered cases of suicide as a GP, and I could not agree more that a stigma is attached, even after the event, because people do not want to talk about it. I remember one family who did not even want suicide to appear on the death certificate. That stigma must be challenged.
430. The Committee is determined to address mental-health issues, and suicide is the first area that we are examining to try to evolve a strategy. I spent some time in America, and I know that people in the US may go overboard a bit, and talk too much, but at least they talk about mental-health issues. You are quite right to say that there is a culture in Northern Ireland of not talking about mental health. That culture is perhaps even stronger in rural areas, where sometimes what the neighbours think is considered to be more important than how people feel. We must overcome that culture. In rural communities, everyone knows what everyone else is doing, and people dare not let others find out certain things about them. I could not agree more with everything that you said.
431. At a recent Committee meeting, I mentioned — and I think that I am correct — that my large rural practice, with more than 8,000 patients, is the only one in Northern Ireland to have patients from three different health board areas. Down the years, I have seen the problems that that can cause, owing to the lack of harmonisation. We must encourage young people to talk and to focus on positive mental health and self-esteem.
432. Many GPs are being encouraged to avail of GP awareness training, although I have not yet done so. A couple of times, the first I heard of a young person’s mental-health problem was after the individual had taken his or her life, and it was too late. I felt so helpless; if only I had known those young men, or they had spoken to someone.
433. The Committee’s examination of this matter is at an early stage. However, we have made it an extremely high priority, and rightly so. The Committee must develop a strategy that considers the needs of urban areas, represented my some members here, where suicide is a major problem. However, a strategy must also recognise the unique needs and differences of rural communities. The development of a strategy must be complemented by the harmonisation of services, and everyone on the Committee is on board, if you will excuse the pun. In my years of experience of the four health boards, one did not know what the other was doing, probably due to lack of collaboration or joined-up thinking.
434. Approaches to health issues must be consistent throughout Northern Ireland. There is an opportunity to try to improve all areas of health, particularly mental health. Is there anything else that you can suggest that rural GPs could, or should, be doing? I have found it particularly frustrating to be made aware of a mental-health problem only when I have been called out to attend to someone who has already taken his or her own life.
435. Ms Baird: One of the main points to emerge from our focus-group consultation was that an individual sees the GP as the first port of call. However, the difficulty is that the GP can respond only if the individual visits the surgery and tells the GP about the problem. We came across several families who had not gone to their GP or sought help after the suicide of a child. Their attitude was that there was nothing wrong with them, and that the GP could not bring their child back.
436. However, all evidence shows that there is a tendency for one suicide to be followed by another, and that is probably partly due to the lack of support after the first suicide in the family. You mentioned depression-awareness training, but GPs are under great stress.
437. Perhaps there is another form of resource that could be made available through the surgery to support people in that situation.
438. Mr R Craig: There was an interesting pilot scheme in Eglinton, outside Limavady, where, in co-operation with an organisation known as Northwest Counselling, patients who were on repeat antidepressants were targeted and offered the opportunity to have counselling to examine what was going on in their lives that might have caused depression in the first place. There is a lot of merit in counselling and support, rather than solely depending on prescription drugs — perhaps the two should run in parallel.
439. It is very distressing that only one-in-10 suicides engage with the Health Service. Most suicides are not known to the Health Service before that point. That is why Oakleaf Rural Support Network plays a major role in engaging with communities and the public as a point of contact, rather than the Health Service being the first point of contact, although, obviously, that is where people will end up. Suicides will generally not see the Health Service as being the place where they would first go.
440. Ms C McBennett: Speaking from the point of view of a bereaved family, the PSNI and the GP are the first to arrive on the scene, and afterwards you look to your GP for help. Our GP was very good in the knowledge that she had, and it would be good if all GPs had such knowledge. We were given a book that we did not look at, instead of having a community organisation, such as the Niamh Louise Foundation, to go to.
441. I would like GPs to be aware of a bereaved person’s need to talk, although I know that their time is in great demand, but listening for five or 10 minutes may be all that is needed, if they are aware of what help is available, for them to refer someone on. In rural communities, people tend to go with who they know, and will not invite strangers into their homes. We were the same — we would not have sought help from someone we did not know, and we did get help by being referred by someone we knew. It would be very helpful if GPs could refer people to where they can get help.
442. The Chairperson: We all agree that talking therapies are an essential part of either preventing suicide, or helping the family come through the other side. There is a very staunch view in Northern Ireland that men and boys, in particular, should not cry, or talk about their problems.
443. The Committee went to Scotland to gather evidence, and found that they have a very innovative way of reaching men there, by targeting football stadiums, and issuing cards with the message that it is all right to talk. Women talk in hairdressers, shopping centres and over coffee about not feeling up to the mark, which is a natural ability that we have — I am sometimes told that we talk too much — but we have that resource. In the rural community, talking is more difficult because of the isolation of homes, and neighbours being a long way away.
444. It would be good to see a programme of information cards rolled out in all our sporting facilities. It would be excellent if we could get the proper structures in place for a one-stop centre for therapy, a coffee shop, aromatherapy, etc, under one roof, so that no one would know why people were entering the building.
445. Mr Buchanan: Over the past few years, three families in Drumquin have suffered bereavement as a result of suicide. The families said that there were no telltale signs of any problems. The young people had no financial problems, they were happy and content, and there was no breakdown in family communications. The fact that the families were unaware of any problems adds to their sense of loss and makes it more difficult to overcome. It is difficult to know what to do to tackle the problem. A one-stop shop has been suggested where people can go if they have something on their mind. That could be a step forward in addressing the issue.
446. Is there any follow-up action to help families that have been bereaved as a result of suicide? There needs to be work to ensure that any follow-up action is adequate.
447. Ms C McBennett: I agree. We were in that position; Niamh’s suicide came as a bolt out of the blue; it seemed that there were no warning signs. However, in hindsight, as a mother I could see that there were warning signs.
448. Michael McGimpsey should provide people with more education. When Niamh was two or three years old I took her to get her injections; she got all the vaccinations that I was aware of for illnesses such as tonsillitis and chicken pox. However, I never once thought of suicide; not once did I think that my child would ever have a mental-health problem. There was no family history of mental-health problems; I knew nothing about it, and it was not brought to my attention. Therefore why would I look out for it?
449. In the run-up to Niamh’s death, I did start to question myself and felt that something was not right. However, I come from a rural background with traditional values, and I chastised myself for thinking that about my own child. I now wish that I had acted on my instincts.
450. Parents are made aware when their children are very young of problems to look out for such as chickenpox, cancer and so on. They should also be made aware that their children could have mental-health issues in their teenage years. It is not scaremongering; it would simply be to advise them what to look out for, what to do about it, where to go for help and not to neglect the issue.
451. The issue could be addressed by early education; schools need to be more open about possible problems. We are able and willing to go to schools to give presentations; however, people in rural schools are reluctant to talk to us. There is a fear that when one suicide takes place it could happen to others. That fear needs to be eliminated.
452. As Raymond said, the information needs to be given out in a positive way to let people know that if the problem is acknowledged their child can be saved and be happy. People need to be made aware that it is no different from going to a doctor about a physical illness; there is no shame in it. They need to be told to get their child sorted out to enable them to lead a normal, healthy life.
453. That will not always be the case. Education as early as possible is required to make it worthwhile. It is a mother’s job to watch out for all those illnesses, and we watch out for everything from when the child is born until they die.
454. Mr J McBennett: I would like to say something about postvention services. From the perspective of a bereaved family, there was no one to help us when Niamh died. Our GP did her best, but our families simply did not know what to say, which further isolated us. Even now, some 18 months later, that sense of isolation continues.
455. We try to be active in postvention services in the greater Tyrone and Armagh areas that we represent. We set up a support-group mechanism called ALO, which is Latin for support; it meets every second Thursday in a specific area. At the first meeting, 10 families who had been bereaved by suicide joined the group; some had never spoken about the suicide before, even those who had suffered bereavement some 10 or 15 years previously.
456. The group is beginning to go out into rural areas, but the stigma —even of coming to the group — is so great that it prevents some people from attending. We have tried to create a comfortable environment in an area, and at a time of night, that means that people who attend will not be as visible. We try to accommodate the wishes of the families.
457. We have been proactive in addressing the needs of young people by establishing a presence on the Bebo website, which is extremely popular with young people. The charity incorporates a youth group that regulates a Bebo-linked site with almost 100 members, and it is run for the youth by the youth. We moderate the site, which is totally dedicated to suicide awareness and prevention. Mr Buchanan mentioned that people do not realise that such things happen, but young people usually talk to one another.
458. Niamh had spoken to someone about how she was feeling, but this person, perhaps out of loyalty to her friend or peer pressure, did not act. It is vital that we have created a forum for young people through the Bebo site, and anyone who links into it will see that the discussions between kids are unreal.
459. Although we have been proactive on postvention through setting up the support group and providing a link from the Bebo site, much more must be done in rural areas. More support mechanisms must be made available, because it not good enough that we have to travel to cities to access services. The journey from a rural area to a city can last longer than the counselling session. Support must be hands-on, and it must be available when we need it.
460. The Chairperson: May I ask a very personal question? If you prefer not to answer, that is fine. You said that your instincts told you that something was wrong but that you felt guilty about thinking that. What did you think was going on? I suppose that you did not want to be having such thoughts and told yourself to move on.
461. Ms C McBennett: I am happy to answer the question. Niamh had mood swings. As a teenager, she was facing —
462. The Chairperson: I imagine that you put it down to hormones.
463. Ms C McBennett: When she reacted to me, sometimes it was Niamh; at other times it was as though she were a completely different person. She had an air of royalty about her, and we would laugh about that because she was a bit of joker. It was hard to distinguish between reality and her messing about.
464. Parents sitting at the dinner table, watching the children banter with another notice any slight change in their personalities. All I noticed was a slight change in Niamh’s personality. She could be extremely high one minute, and the next minute change completely. Her mood was extremely high or extremely low.
465. When she was on an extreme high, she could do no wrong, but that was followed by an extreme low, which I did not recognise and which is very hard to diagnose. A mother’s instinct told me that something was wrong. I asked her what was wrong and told her that I knew that something was not right with her, but she refused to speak.
466. When we ask young people why Niamh did not talk to me, they say that children to not want to worry their parents, and that goes back to culture and traditional values. The youth do not want to speak out primarily because they do not want to worry their parents and because they are anxious about how their parents will react.
467. Knowing what I know now, I would have reacted wrongly, because I did not know how to react. The issue is how parents react when their child approaches them and says that he or she has been self-harming. Would parents be so horrified that the children would keep anything else to themselves? There must be an educational process in which parents teach each other how to react. That does not apply only to parents: everyone in the community needs to know how to sit, listen and react accordingly when a young person tells them that he or she has been self-harming or is thinking of suicide, rather than becoming defensive and making the young person retreat.
468. I do not want to focus totally on parenting because my reaction would have been the same as that of any parent. Niamh spoke to her friends, but misguided loyalty prevented them from telling anyone; had there been an educational programme in schools, they might have spoken out. They knew about drugs, alcohol and sex, but no one knew how to respond if one of their friends started talking about suicide websites, as Niamh did. We are only scratching the surface here today; a much broader education package is required.
469. Unfortunately, parents lump problems together as symptoms of children going through their teenage years, but that is not the case. There are so many pressures on young people, such as bullying, peer pressure, and whatever messages are being sent to their mobile phones, that it is almost incomprehensible.
470. Ms Baird: There is a need for greater peer support. My daughter self-harmed and made a suicide attempt that, fortunately, was unsuccessful. However, even when the signs are recognised and help is sought, the problem is that the stigma is transferred to the parents: they feel that they must be failing and that it is their fault. When everything around the child appears to be normal, the implication is that the parent must be doing something wrong. The child reacts against the parent and those who want to provide support; it would be better to have support from peers, GPs and psychiatric services.
471. Ms S Ramsey: Thank you for your presentation. I commend you, because it is very hard to deal with bereavement and to cope with what you are going through as well as trying to help others. You will probably be glad to know that the next person to give a presentation is the chairperson of the suicide strategy implementation body.
472. As the Chairperson said, we are taking this inquiry seriously. Although she and I represent city constituencies, all members have probably been directly or indirectly affected by suicide, and, therefore, it is problem of which we are aware. We do not have all the answers, and therefore it is useful to talk to people who have been directly affected or who deliver support services.
473. It is a pity that most groups that support others are set up by grieving families, and society must examine that. I am conscious that sometimes we indirectly create a rural versus urban divide, but suicide and self-harm know no boundaries. Have you established links with other groups? I know that most of them are probably based in cities, but it is important to learn the positives and negatives from one another, because you suffer as much as those families.
474. The Bamford Review was seen as the be all and end all of dealing with mental health, and it highlighted many issues. However, none of us is an expert in identifying mental-health problems. Nevertheless, Bamford was seen as a start, and with the fanfare that introduced it there seemed to be a possibility that it would make changes when it was implemented. However, going by the information that we have received, there is a strong possibility that that will not happen.
475. Ms C McBennett: The Niamh Louise Foundation works very closely with the West Belfast Support Group, the Public Initiative for the Prevention of Suicide and Self-Harm (PIPS) in Belfast and Newry, and with all the Derry groups, but it takes all an organisation’s energy to cover its own area. We meet them regularly, and if I need anything I can lift the phone to any one of those groups; but they are consumed, as we are, with the needs of their own communities. I cannot say whether they have considered rural issues — I can only go by what we are doing — but there is a network and we are all part of Family Voices, which was set up to bring us all together.
476. We communicate and talk together, but the differences between rural and urban areas are so immense that it is very hard to explain them to a group that may think that one shoe should fit all. Unless you have lived in a rural area, it is very hard to understand; I have not lived in Belfast or Newry so I cannot speak for people who live there. Working as I do at ground level, I have not seen any evidence of effective co-operation. We are not against the idea of working with urban groups — far from it: we encourage joined-up working and have learned from the organisations that went before us; we hope that there will be more co-operation in future. However, because of boards’ restrictions, the suicide prevention strategy, money and the fact that everyone is fighting for their own area, groups often feel isolated, and that is not how it should be. The aim is to reduce suicide. We should forget about what each area needs and remember the overall objective — bringing rural and urban together.
477. Ms S Ramsey: I do not deny that there are issues specific to rural areas, but there should be joined-up thinking; we should not create a gap between urban and rural, because lessons can be learned from both.
478. Mr R Craig: I come from a further education background; I was the project manager of Limavady Learning Partnership, the aim of which was to raise attainment rates. Each of the schools involved was preoccupied with its own agenda, but after three years we managed to raise the attainment rates in Key Stages 1, 2 and 3 in all schools. Culturally, we are not comfortable with collaborating — and the Committee’s experience with the health boards will tell it that. Professionals tend to regard the community and voluntary sector as poor cousins, and that has to be addressed. If we are to co-operate in partnership, we need to be trained in that culture. We come to the table wondering what we will get out of it, when the challenge is what solutions we can bring to it.
479. The Committee has a great opportunity to advance joined-up thinking, although I do not like the term, because much more is involved — we must have a passion for what we do. We must consider our resources in a different, corporate way beyond the geography of our own townland and council area because, as Sue said, there is no curtain dividing rural and urban. This is about saving lives and improving the quality of life, which should be lived to the full, whatever your disposition or religion.
480. There are already hotspots. There is a seriously high suicide rate in the gay and lesbian community — it is in crisis. People end up in hospital through self-harm and are given the Samaritans’ number. That is wholly inadequate. They need on-site counsellors who can be available within 24 hours. All the groups attended a conference in Kilkenny, where we were presented with research that showed that certain actions have very good outcomes, such as a councillor being available within 24 hours of an attempted suicide. At that point the person is much more receptive to help and support, but leave it 48 hours and they go into denial. They will say that they are OK and that they will not do it again; they will simply want to get away. However, that is e when they are at risk.
481. We know that there are actions that have positive outcomes. We also know that the problem will not necessarily be solved through more money: collaboration between all the different tiers is the key. Some people are involved at the point of contact, and we have considered the issue on a sub-regional basis. Those areas need to be brought together so that the issue can be addressed comprehensively.
482. Ms Baird: I work in the Northern Health and Social Services Board, covering the whole of Newtownabbey Borough Council area, Carrickfergus Borough Council area and Antrim Borough Council area; I work with groups including PIPS, Cruse and the Samaritans. There are lessons to be learned and we are taking on board their experiences, knowledge and training that we can transpose.
483. It is important to emphasise that although there are elements of their work that are good and that we can apply, work is also required that is specific to rural areas so that local people can identify with it.
484. Ms S Ramsey: Do you have any views on the Bamford Review into mental health and the possibility of not getting funding to address the issues that were highlighted?
485. Mr R Craig: I am not familiar with it.
486. Mrs Hanna: You are all very welcome. The Committee does not have the answers either; however, it can bring the statutory agencies and the Department of Health together with groups such as yours and the wider community. I know that it is difficult for the families. It is through your sad loss that you can help to inform future services. It is important for you to have the courage be involved.
487. Raymond made some important points about co-operation. Colm and his colleagues will give evidence next and perhaps they will give us a more holistic view. This issue has to be dealt with comprehensively; it has to be inclusive, and it has to be so many different things to different people.
488. Your work will not bring Niamh back, but it might save other young lives. A young lad called Francis who lived next door to me took his own life; his family felt hurt because people did not want to talk about it. The stigma attached to suicide has to be dealt with. As Catherine said, people do not mind saying that they have had a heart attack or have cancer, but they do not like to admit that they cannot cope.
489. Some of us were at the presentation given by the Northern Ireland Association for Mental Health, which outlined the economic case. It is terrible to have to talk about making an economic case; but that is what we have to do.
490. Early intervention, prevention, good health promotion and raising awareness with parents are all important. As Catherine said, parents take their children to the doctors for vaccinations, but they are not trained to look out for their children’s mental health. There should be awareness training for parents, teachers and in the schools. The association spoke about encouraging positive thinking and self-esteem and the importance of simply talking; and we have heard about the talking therapies. All those areas must be brought together in a comprehensive service. There is now a great opportunity to do that because of increased awareness.
491. We are trying to do something similar to address the needs of victims and bereaved people. We need the best service available and we need to ensure that it reaches rural areas. People in rural areas feel isolated, as perhaps they do not have a next door neighbour that they can talk to.
492. This Committee does not have the answers, but we are determined to play our part in getting them and creating a far more comprehensive service.
493. The Chairperson: Part of the Committee’s deliberations will cover the fact that accident and emergency units should contain dedicated rooms with volunteers who can talk to people and calm them down until the professionals can do their work. I take the point that as time moves on people with problems get annoyed and embarrassed and that they will want to get out as quickly as possible, but, as Raymond said, the first 24 hours are vital.
494. Dr Deeny: How do we overcome the stigma attached to suicide? I mentioned two individuals for whose families it came as a bolt out of the blue because the individuals concerned had not seen a health professional. I also felt helpless. Although, looking back, it did seem that one fellow had had problems.
495. I am also thinking about the stigma that attaches to mental ill health. I have looked at the results achieved by Alcoholics Anonymous and Narcotics Anonymous whereby people can go to meetings and help one another. By talking to one another their lives can be saved and transformed.
496. I do not know whether you are aware of a group in Northern Ireland called Emotions Anonymous. It deals with people who have problems with emotions and feelings. Should we provide such facilities for young people? Indeed, for all people, because suicide affects people of all ages. There should be places where people can meet to talk through their problems without fear of being identified. Such a facility would allow young people’s peers to say in confidence that they have concerns about their friends. I am trying to think of ways in which the current situation could be prevented.
497. Ms C McBennett: That is a great idea. It is something that we have tried with our youth group, all of whom have had some experience of suicide and self-harm through knowing Niamh or someone like her. We gave them a platform on which to speak. It is not a counselling session: we are not counsellors. They talk among themselves, and they are very passionate about creating awareness about self-harm and suicide. It was they who created the website on Bebo. That healing method works; I have seen it work with the youth group. I have seen individuals being healed through taking ownership and saying that either they or their friends are battling with problems and that they are going to help one another. However, such a scheme needs to be operated anonymously. We tell newcomers that they are helpers and that no one need know why they have come. If they need to see a counsellor, we can direct them.
498. I agree that if such a scheme were rolled out it would be of benefit.
499. Ms Baird: We have been rolling out a small grants scheme in partnership with the Northern Health and Social Services Board targeting specific mental-health and suicide-prevention initiatives. One scheme that we recently funded is in a primary school in Antrim and it is similar to the one that has just been described. It targets children in P1 to P4 and is about allowing them to talk about their emotions and deal with emotional situations such as bullying and how they feel about other people and themselves. Although it is a pilot scheme at the moment, it will be interesting to see how it turns out.
500. The Chairperson: There is great value in having a counselling facility in schools in addition to the other kinds of support that we talked about. To call a spade a spade, there is a problem with attitudes and it comes from our Churches.
501. Throughout history, Churches have not always adopted a positive, caring role. They sometimes have had closed minds about completed suicides, and Churches have a big part to play in transforming mindsets so that everyone can rally round and support families that are left blaming themselves or wondering what they did wrong. Churches have a key role in helping our society to move on from strict interpretations in respect of such traumatic experiences, which are on the increase in Northern Ireland.
502. We have come to the end of the question-and-answer session. I thank all of you sincerely for coming along, particularly Catherine, James and Michele, for allowing us insight into a sensitive and personal part of your lives.
503. Mr R Craig: Thank you very much, Chairperson. I hope that our contribution was useful.
504. The Chairperson: It was very helpful, believe me.
505. We shall now move to the second evidence session, with the Southern Health and Social Care Trust. I welcome Mr Colm Donaghy, chief executive of the Southern Health and Social Care Trust, and Mr Francis Rice, the trust’s director of mental health and disability services. Ten minutes have been allocated for your presentation, and then we will open the session for questions and answers.
506. Mr Colm Donaghy (Southern Health and Social Care Trust): Thank you, Chairperson. I am wearing two hats today.
507. The Chairperson: I should have said that you are also the chairperson of the Suicide Strategy Implementation Body. I apologise.
508. Mr Donaghy: The trust has provided a written submission to the Committee. As director of mental health and disability services, Francis will take the Committee through the key action points of that written response. I will begin by giving the Committee an insight into the work of the Suicide Strategy Implementation Body, before Francis makes his presentation.
509. The Chairperson: That would be very helpful.
510. Mr Donaghy: My formal involvement in suicide prevention goes back to 2005, when the then Minister with responsibility for health, social services and public safety, Shaun Woodward, asked me to chair a suicide task force to develop a suicide prevention strategy.
511. The engagement process that was used to develop the suicide prevention strategy was unique. We engaged with statutory bodies, families who had been bereaved through suicide, the Churches, the PSNI and all the relevant professionals. The task force was composed of those groups, as well as representatives of the relevant Departments.
512. Following the development of the strategy, at its launch, the then Minister with responsibility for health, social services and public safety, Shaun Woodward, announced that I would chair a suicide prevention strategy implementation body — hence the establishment of that body.
513. The title of the body is a misnomer, because the Suicide Strategy Implementation Body does not have any executive powers or the authority to implement recommendations, nor, I believe, should it. The authority and the executive powers should remain with those statutory and community organisations that are tasked with implementing the strategy. Instead, the Suicide Strategy Implementation Body’s role should be that of a scrutineer or, when required, an adviser to the Department.
514. An indication of that oversight and collaborative role is that six of the seats on the Suicide Strategy Implementation Body are reserved for members of families that have been bereaved through suicide. For example, Catherine McBennett, who gave evidence to the Committee earlier, sits on the body, as do several other people who have been bereaved through suicide.
515. I had the heroic intention of establishing a membership comprising 12 to 14 people. In fact, there are 38 members, and counting. That is not to say that the body is any less effective. In fact, I believe that it is more effective and that that level of membership indicates people’s interest and commitment to be involved in suicide prevention. Therefore, the body is composed of representatives of the relevant statutory Departments, the boards and community and voluntary organisations that play a part, including, for example, the rural support networks. The body’s composition is therefore unique, and no similar body exists in other jurisdictions. Thus, it has a high level of expertise on which to draw, and advice can be sought on specific areas, some of which has been acted on by the Department.
516. Bearing in mind that the suicide prevention strategy is a long-term one, it will take time to ascertain whether it has directly impacted on suicide statistics. On a positive note, although the figures may not be linked to the strategy, and one should not assume a direct correlation, compared to the first six months of last year, the Registrar General’s statistics for this year show a 25% reduction in suicides. At this stage, those figures are encouraging and offer a positive message for Northern Ireland, and we hope that that trend continues.
517. The Suicide Strategy Implementation Body believes that, in order to implement the strategy, several areas require strengthening, one of which is in the co-ordination of performance management of the implementation of the strategy. I am aware that the Committee has visited Scotland, and I have also been there to visit Choose Life, Breathing Space and See Me. I was struck by infrastructure — which does not exist in Northern Ireland — that is in place to implement the Scottish suicide prevention strategy. My role, as chair of the Suicide Strategy Implementation Body, is not just to criticise the statutory organisations involved in the implementation of the strategy — including my own — but also to criticise the Department and other organisations that are not playing the part that they should.
518. A firm of management consultants gave us the opportunity to review the community-support model, and to consider the co-ordination of performance management of the implementation of the strategy. I discussed that matter with departmental officials and the Minister, who were supportive. As chair of the Suicide Strategy Implementation Body, I asked the consultancy firm to review the co-ordination and implementation of the strategy and to consider a community model and principles that might be adopted in order to deliver such a model in the future.
519. The Bamford Review was mentioned earlier, and it is a key element in the prevention of suicides. We have drawn a distinction between prevention and treatment in the strategy. However, we have called on Government to implement the recommendations of the Bamford Review, which deals with the service and treatment of mental-health services.
520. Several other areas have been mentioned, including cross-departmental working. I am delighted that we now have an inter-ministerial group examining suicide prevention, and I have attended those meetings on several occasions. Government are very open to ideas and suggestions on how we can improve the strategy’s implementation.
521. I want to mention two specific areas. We commissioned work on the evidence of what would help to prevent suicide, and it became apparent that, globally, there is not a lot of evidence of what works in suicide prevention, although there is some — hence the GP training awareness programme. One of the stark statistics in the strategy, which is not a criticism of GPs but gives us a potential, is that 80% of people who have taken their own lives had been to see their GP in the previous six months. That gives us an indication of some of the potential. That is not to say that they went to see their GP with a mental-health or emotional problem, but it gives us an incentive for the GP training. More research must be done — and that is another serious recommendation.
522. My final point — and I am conscious of time — concerns the media. A lot of work is ongoing with the media. The media and the Internet have a big impact on our young people. Some 6% to 7% of suicides are copycat suicides, and that is primarily due to the impact of the media on young people. In Northern Ireland terms, that equates to 20 young people. Those would be imminently preventable suicides if we could ensure that our media reported responsibly on suicide.
523. I have several other points that I would like to make, but I will raise them during the course of the discussion.
524. Mr Francis Rice (Southern Health and Social Care Trust): I will take the Committee through the action plan that the Southern Health and Social Care Trust has established to take forward the Protect Life strategy. I will also address some of the issues that face the trust. I have copies of the action plan and the trust’s engagement paper, which deals with the issue of how communities and agencies can be engaged. I shall circulate those papers to the Committee.
525. The Chairperson: Thank you. That would be helpful.
526. Mr Rice: I will refer first to the inter-agency action plan, and then the engagement paper.
527. The trust’s approach follows the approach of the suicide prevention strategy. There is a correlation between the two, but we have built and customised our approach to suit the needs of the southern trust. The action plan is divided into two different approaches. The first is a population-based approach under which we have specific objectives and targets that deal with communities; families, children and young people; health and personal social services; workplaces; emergency services; Churches; and the media.
528. We then move on to more specific, targeted approaches that have objectives with specific outcomes and deal with areas such as self-harm and mental illness; drug and alcohol misuse; young males; those bereaved by suicide; survivors of sexual, physical and emotional abuse; marginalised and disadvantaged groups; high-risk occupations; and prisoners.
529. It is important to point out that the process is evolutionary. It has been agreed in the terms of reference that, as we work through the process, we will modify it to suit the needs that have been identified in our communities.
530. Approaches are targeted from the point of view of prevention, intervention and postvention. The trust has initiated a collaborative approach that is populated by people from statutory services, communities and voluntary groups. The action plan reflects the shape of the regional strategy and, under the population approaches, I will explain the specifics. The action plan focuses on the key population groups that are identified in the suicide prevention strategy and includes action such as awareness raising, education and training. That refers not only to training inside statutory services, but across all communities, and involves voluntary groups.
531. The specific objectives of the population approach are: to develop peer education and mentoring support; the development of action to support families; to try to identify and address the broader needs of communities; to build capacity within communities; to develop the resource and support that is available within communities; to work with schools to promote positive mental health; and to ensure that there is easy access to support for children and young people.
532. Our targeted action is focused on developing mechanisms to improve joined-up working across sectors, and improving communication and information. As part of the action plan, we will develop an information and communication strategy. Other targeted action includes improving our research base and sharing best practice, and I will explain more about the regional research that the trust is currently involved with.
533. The trust aims to improve co-ordination and links among services to reduce duplication and improve client and patient flow, and to address the gap areas. Further objectives are: to reduce the stigma of suicide; to improve access and signposting to specialist intervention services, such as child and adolescent mental-health services, and the transition between services; to improve support for families and people who care for someone with a mental illness, where suicide has been experienced; to ensure that responsive self-harm services are in place; to develop agreed protocols for those who may be at risk as a result of drug and alcohol influences; and to target the particular needs of looked-after children, black and ethnic groups, and high-risk occupational groups. Under each of those areas, we have specific objectives, actions and outcomes.
534. I currently chair the trust’s Protect Life implementation group, and we have built in monitoring and review mechanisms. That will be reflected in how we choose to develop new objectives with new outcomes and police the progress made against those objectives.
535. Since we last addressed the Committee, the southern trust has become involved with the Belfast Health and Social Care Trust, the University of Ulster and Queens University Belfast in a suicide-research project, which has national and international links. We are pleased to be involved in that significant project. It has just received ethical approval, and it will start at the beginning of December.
536. I am happy to apprise the Committee of the developments since we last spoke. Some of the areas that we have progressed are mentioned in our submission. The trust has now developed a number of community-development workers that are provided by community and voluntary groups. We have contracts with those groups, with specific service-level agreements so that we can ensure that they provide a range of services to meet the wide and varied needs of our population. The service-level agreement ensures that we can measure outcomes, but also that we monitor the identified needs to ensure that they are being met.
537. There are also now six pilot resource centres across the southern trust area. Those have been developed primarily with community and voluntary groups, with input from statutory services. Those services are mainly drawn from mental-health services, child and adolescent mental-health services, and children’s services where specific intervention is required. Those resource centres focus on specific needs of their localities. The trust did a lot of consultation as to where those centres should be sited because of the size of the southern trust and the locality-versus-urban argument.
538. We are monitoring the progress of those initiatives, and regard the resource centres as a one-stop shop, in which people can access a range of services, even if it is just talking therapy — someone to have a cup of tea with — or specific counselling. Access to statutory virtual team services is also available, where appropriate. We have also developed locality-based counselling services, because, as the Committee is aware, that was a particular issue of concern across the region. People felt that they were not always able to access local counselling services. We have worked hard to put that in place.
539. We now have a portfolio of training, and a training co-ordinator, who is employed by the trust. It is important to note that that training is provided to statutory services, voluntary agencies, community organisations, the education sector and the police. We analyse what training and education is available. Our aim is to determine whether or not that is effective, and, if it is not, to stop it and develop new needs-based programmes through the resource centres, which are becoming more sophisticated in relation to the needs of the localities and their populations.
540. The trust has attached such significance to the action plan that it has appointed a trust co-ordinator to implement it. The co-ordinator comes from a community-development background; has significant links with the southern trust area and is well known in the area; and has the ability to work across the trust area with community and voluntary organisations. The co-ordinator’s credibility in the area is very important, because of the work that we need to do.
541. Having listened to the earlier evidence, it is clear that there is an issue about people working collaboratively. To be frank, some people tend to deliberate on their own organisation’s needs. We want to create a mechanism that allows people to get together in a consortia arrangement. We want to cultivate a culture whereby specific communities or voluntary groups specialise in certain aspects of service provision, rather than all of them doing the same thing, leaving us unable to offer the full range of services.
542. We are examining mentoring programmes and new models of service delivery. The southern trust is reviewing all of its mental-health services, which is opportune, because we can build all of this work into that review and involve all the appropriate people, such as crisis-response and home-treatment services. We will examine primary-care and secondary-care services, and acute-care services, because they are significant, particularly in relation to accident and emergency services.
543. As members can see from the engagement paper, the action plan implementation group comprises 42 people. It is quite a task to manage that, so, with their agreement, we have developed a strategy to better engage people. We have proposed the development of a management group and a stakeholder network that will take forward the issues raised in the action plan and others which arise in the southern trust area. People feel that they can sign up to that arrangement.
544. The implementation group will meet next Monday to discuss the engagement paper. As members can see, the main purpose of the paper is to engage and represent everyone’s views, not just in relation to the implementation of the action plan, but in respect of the suicide strategy and all of the issues that arise in the southern trust area, and all of the needs that we are charged with meeting. A situation will be created in which we can adopt a collaborative approach to the representation of views and the provision of services to meet identified needs.
545. I am happy to take questions.
546. The Chairperson: Those are useful documents. I congratulate you both on the way in which you are moving forward in trying to address a difficult issue.
547. Mrs O’Neill: Colm, you talked earlier about ideas for strengthening the strategy and about co-ordination. Will you outline more of your views on that? Obviously, that is something that the Committee will want to include in our report to the Minister when our inquiry is complete.
548. The clinical-excellence guidelines state that suicide rates can be reduced by targeting specific groups. One of those groups is people who self-harm. How effective has that strategy been? Does everyone who is treated for self-harm in the southern trust area quickly receive a follow-up appointment?
549. Mr Donaghy: In respect of co-ordination, I am not necessarily referring to how the strategy is implemented locally by people such as Catherine McBennett, local community groups, and others from whom the Committee has heard today. Better co-ordination of the implementation of the strategy is about holding people to account. Therefore, it is important to ensure that the performance-management element is strengthened.
550. Scotland has a programme named Choose Life, which is a national strategy and action plan to tackle suicide, and which consists of up to 11 staff. I am not proposing anything such as that for Northern Ireland. However, as I have said, that programme has up to 11 staff helping to co-ordinate the implementation of that strategy and holding people to account.
551. There is a National Office for Suicide Prevention in the Republic of Ireland. Five or six members of staff are involved in ensuring that that strategy is being implemented across the country. Nothing of that nature exists in Northern Ireland.
552. This year in Northern Ireland, £3 million has been specifically earmarked for suicide prevention. Although £3 million is not a great deal of money, £1·8 million of that is earmarked for the development of local community plans. It is important to have in place an accountability arrangement that ensures that those plans are developed in a way that is consistent with the strategy, and that will actually make a difference.
553. Therefore, the co-ordination that I am referring to is about holding people to account in respect of the implementation of the strategy.
554. A good point was made earlier on the self-harm issue. During the development of the strategy, we heard many stories about people who had seriously self-harmed — either self-cutting or self-poisoning — being discharged from hospital after one night and not getting an appointment with mainstream services for two or three months. Invariably, the person does not keep the appointment, and there was no follow-up action.
555. In the north-west region, the Department has put in place a pilot scheme as a result of the strategy that utilises Zest — a community and voluntary organisation — and Altnagelvin Area Hospital, which refers people to that organisation. Zest has properly trained mentors who are prepared, when someone self-harms and is being discharged into the community, to provide six sessions with that individual.
556. That tends to begin to build a symbiotic relationship between the statutory and voluntary sectors. When people who have self-harmed are discharged, the statutory sector refers them to Zest, which then provides that mentoring service, providing the individual agrees. That is designed to bridge the gap between the discharging of people who have self-harmed and the time when they can access mainstream services.
557. There is other work that we are taking forward locally in respect of people who self-harm. I shall hand over to Francis to talk about those.
558. Mr Rice: Since many people turn up in accident and emergency units, we are trying to develop psychiatric liaison services so that they have access to appropriate medical and nursing services. That was not available previously. We have just appointed a second psychiatric liaison nurse so that we can look at the matter from a statutory perspective.
559. I referred to the mentoring systems that we are examining. We have looked at Zest, which operates in the Western Health and Social Services Board area, and with the additional moneys we propose to augment the statutory services with access to an appropriate service, such as that provided by Zest.
560. In addition, we are working on an information leaflet, part of which deals with suicide prevention, self-harm and self-help. It lists all the organisations that people can be referred to while they wait for or are receiving psychiatric or statutory services. To be honest, we are still developing it because we realise that there is an issue. I was asked recently to join a departmental group to examine the interface between psychiatric liaison and accident and emergency services with specific reference to that issue.
561. Mr Easton: Should there be a suicide prevention strategy for the whole of Northern Ireland or should it be the responsibility of specific trusts?
562. Mr Donaghy: It is better to have one prevention strategy for a population of 1·7 million; however, different areas might have different implementation structures and plans. There was discussion earlier about the different needs of urban and rural areas, and sometimes a different response is required in a rural area. Suicide is no respecter of urban or rural demarcations, although the response to a suicide prevention strategy might differ from one area to another, as might its implementation. Nevertheless, the strategy must straddle the entire population.
563. Dr Deeny: My first question has just been answered. I commend Mr Donaghy and Mr Rice for taking on such a serious issue. It is very important that they do and it is good to hear about it. First, Colm mentioned a 25% reduction in six months. What do you attribute that to, primarily?
564. Secondly, suicide cannot be treated; it can only be prevented. Treatment is reserved for the families. I would like to think that the work that you are doing with conviction and determination will be rolled out and will be taken up by other trusts, for example the Western Heath and Social Care Trust, according to a strategy for the whole of Northern Ireland. Francis, you talked about a one-stop shop and pilot resource services, and that is a wonderful idea. I have often thought that there should be a half-way house that people could go to. Did you mention six or eight centres?
565. Mr Rice: Six.
566. Dr Deeny: Can you tell us about the one-stop shop? Colm and I mentioned that some people see their GPs before committing suicide, but it can be impossible to detect suicidal tendencies in some people. At times of trouble, adolescents and young people need places where they can seek help. How long would the one-stop shops be open and how would they be staffed?
567. Mr Donaghy: I wish I knew how the 25% reduction was achieved, but I do not. However, I hope that it has something to do with our work over the past two years and the work of our local communities before that, because our communities are the reason that we have a suicide prevention strategy. The commitment and resilience of our communities have meant that we have begun, I hope, to turn the tide. That said, I might be proved wrong; it depends on the statistics that appear in six months’ time.
568. I can give a positive example of prevention that will have long-term effects. As a part of the strategy development, we lobbied the Department of Education hard to introduce into the school curriculum a compulsory element of coping and life skills for children. I am encouraged to find that, from 1 September 2007, that has been an essential part of pastoral care responsibilities. It may not prevent every suicide, but it will give young people something else in their armoury when they encounter problems in later life and it may stop them taking their own life. That is part of the preventative strategy. It is a long-term measure, but it is important that we do not lose sight of the preventative element.
569. Dr Deeny: That is wonderful news; I am glad to hear it.
570. Mr Rice: Resource centres are primarily operated by community and voluntary groups; however, we have service-level agreements on how we want them to operate. It is important that the resource centres have access to statutory services where appropriate so that when someone is in crisis they can access those services.
571. The resource centres fulfil a useful purpose, as people told us that not everyone who was in difficulty wanted to go to a GP or felt that they could go. Therefore this is an interim arrangement: if they are getting into difficulties, they can go to a resource centre anonymously — if that is what they want — to access services. In that way, they can begin to tease out their issues, address some of the coping mechanisms, and staff can work with them to enable them to deal with their problems.
572. There is also a recognition that staff should also have access to specialist statutory services where appropriate: childcare services, child/adolescent services or mental-health services. That is because it is not just young people who access the centres. Over the summer, we had an issue with some young children in the Southern Health and Social Care Trust area; however, we also have a problem with men aged 40 upwards. We are trying to address those issues and make the resource centres attractive so that people feel they can pop in to discuss their problems.
573. Dr Deeny: What are the centres’ opening hours?
574. Mr Rice: The resource centres do not open 9.00 am to 5.00 pm; much depends on volunteering, week in, week out. We cannot afford to keep them open 24 hours day, but they open out of hours. Furthermore, if they are open out of hours, they can contact statutory services. An on-call arrangement operates there. We will continue to review the service to see what we can add to it.
575. Mr McCallister: That was an interesting presentation. I was encouraged to hear the witnesses’ answer to Michelle’s question.
576. What is the best way of ensuring that people do not fall through the cracks between different board areas?
577. I am pleased that groups follow up after instances of self-harm or attempted suicide; that is vital. Earlier evidence told us how important it is that it is done as quickly as possible.
578. In the ‘Protect Life: Northern Ireland Suicide Prevention Strategy’ document, I was encouraged to find that people are expected to take a lead, that there are expected outcomes and that individuals are held to account.
579. Where are we with that? It is easy, with something on this scale, to produce only warm chat with no real substance without any follow-up.
580. It is about co-ordinating all the various groups. The Chairperson spoke earlier about getting the message out to football clubs. Some of the groups that I have been involved with look at every area of life. In rural areas that means communicating with farmers and their families at livestock marts and in youth clubs, schools and churches.
581. I would also value your comments on the media. Colm said that 6% to 7% of suicides were copycat incidents and that they claimed some 20 lives. It is important to educate the media. I know that the Minister has visited his Home Office colleagues to discuss the role of the Internet. What has been the general response of media outlets to your submission to the Department — which, hopefully, has been sent to the Home Office — on control of the Internet?
582. Mr Donaghy: I will answer your question about the media first and then talk about mentoring and people who fall between stools. The media are important and will become more important as the Internet becomes more widely available and becomes young people’s chosen source of information and news, as some of our regional newspapers will testify.
583. The Irish Association of Suicidology and the Samaritans have produced very good guidelines. We were involved in their preparation and have recommended them to our local media. We have on occasions sent them to the local media about their reporting of specific incidents of suicide.
584. Mr McCallister: Have you monitored its use?
585. Mr Donaghy: The suicide strategy implementation body and the Department are examining a facility called Media Watch, which we will pay to monitor how the print, television and radio media deal with incidents of suicide. If they deal with it improperly we will raise the matter and make complaints. We have identified volunteers and others in Northern Ireland who will take part in the Media Watch campaign to ensure that the media report suicide responsibly. Unfortunately, we have found that the media respond but fall into old ways when getting a story; the difficulty for us is to ensure that we sustain media interest in suicide prevention and how they report suicide. Research shows that if the media report responsibly, we will prevent some suicides. It is worth concentrating on that 6% to 7% of young people.
586. The Internet is not controllable. The Minister has met Internet providers, and one concession has been given that has proved effective to some extent. When the word “suicide” is typed into Google, the first sites that appear will be suicide prevention sites such as those provided by PIPS, which encourage people to prevent suicide. It ensures that the first site to appear is not one that tells people how to take their own lives. That was not the case before, but it is happening now. The number of hits on suicide prevention sites in Northern Ireland has gone up as a result. The traffic is going first to sites that advise on suicide prevention.
587. The issue of people falling between stools is difficult. The mentoring scheme that I mentioned is a pilot scheme. It is running only in the north-west but not in other parts of Northern Ireland. However, a similar, although not identical, pilot is running in the Mater Infirmorum Hospital. The hospital provides a discussion forum for young people in north Belfast who have presented at accident and emergency having self-harmed. The suicide strategy implementation body advises the Department to take seriously the evaluation and outcomes of those pilots; if they show benefits, the body will urge the Department to roll them out at some stage.
588. Mr McCallister: How long has the pilot been running?
589. Mr Donaghy: It has been running since September 2007. Given the nature of the scheme, it has taken a long time to train mentors, to get ethical approval and to get over hurdles of data confidentiality.
590. Mr McCallister: When the Committee visited Scotland, it discovered that a key aim was to get good evaluations of such schemes.
591. Mr Donaghy: Indeed. The Health Promotion Agency has been tasked with ensuring proper and robust evaluation of the pilots so that any lessons that can be learnt will be learnt. If the pilot proves beneficial, I hope that further schemes will be rolled out.
592. Mr Rice: In the north-west, 40 people have been trained in mentoring, so the evaluation should yield good information.
593. The Chairperson: Mentoring makes sense. Often, all that someone needs is a listening ear and some sound advice. Although that is not always the answer, in most cases when someone is going through an extremely anxious period in his or her life, it is certainly helpful to be able to turn to someone who has been in the same situation or someone who has taken a course in how to generate discussion and offer sound advice. A price cannot be put on that.
594. Mr Gallagher: I thank the Southern Health and Social Care Trust for its enlightening submission. I want to ask a question that is particularly relevant to my own constituency and probably to others in the Committee. How does the strategy relate to health authorities across the border? It was mentioned that when someone is taken into casualty, there is a mechanism by which a trained person will follow up the case. However, a young person from a border area might be in Bundoran and could be admitted to Sligo General Hospital; if someone was in Monaghan, he or she could be admitted to Cavan General Hospital, Louth County Hospital or Dundalk. Is work being done with counterparts across the border?
595. Recently, the Committee received a submission that promoted the benefits of workforce training. What is the trust’s experience of that?
596. Mr Donaghy: I will deal with cross-border co-operation first. There is an all-island action plan for suicide prevention, so we work closely with our counterparts in the Republic of Ireland. It makes sense that programmes on research, training, and development are not carried out in isolation.
597. However, there is not only a cross-border aspect to that work but a five-nations aspect as well. We meet our counterparts from Scotland, England, Wales and the Republic of Ireland in a five-nations working group that examines how our resources can be brought together to ensure that, for example, future research is not duplicated. There is a great deal of co-operation on suicide prevention.
598. The Committee may already be aware of two recent television awareness campaigns, one of which was known as ‘It’s me’ and featured Lynda Bryans. The other was known as ‘Share it’ and featured a young man who carries a large box around with him. The box gets smaller and smaller the more he talks to people until eventually he can put the box in his pocket and walk alongside his friends without the box being an obtrusion.
599. Both those campaigns were funded through the suicide prevention funding. It was to promote awareness that people should talk and that the stigma should be removed from mental ill health.
600. The ‘It’s me’ campaign was taken by our colleagues in the Republic of Ireland. They ran the same advertisement but without Lynda Bryans, as they did not think that she would be recognisable in the Republic. We did the work and they lifted it. Subsequently, they developed another phase of the awareness campaign, which some of you may have seen. People’s faces show the effect that isolation and marital breakdown can have on mental health; it promotes the idea of talking and getting help for problems. It was developed by our colleagues in the Republic of Ireland and we ran it on television in the North.
601. I wear another hat as director general of an organisation called Cooperation and Working Together, which looks at where it makes sense to co-operate across the border on community, social, secondary or primary care services. A substantial amount of work is being done to examine how we ensure that services are delivered as seamlessly as possible as well as aspects of cross-border mobility. Recently, you may have seen in the media the announcement that people in south Armagh can now access the out-of-hours GP service in Castleblaney. That is to encourage people to access the out-of-hours service closest to them, irrespective of the jurisdiction.
602. Much is being done on self-harm; we are learning from our colleagues in the Republic of Ireland about the self-harm registry, which is to improve the recording of and the follow-up care for people who self-harm. We are repeating a self-harm registry in the north-west that we hope will roll out across Northern Ireland. It deals with how we register people who have self-harmed in hospital and accident and emergency departments.
603. Ms S Ramsey: The information from the Department says that from 2002 to date, more than 22,000 people have been admitted to hospital as a result of self-harm. That is a sizeable number.
604. Mr Donaghy: It is merely the tip of the iceberg because not all people who self-harm present to accident and emergency.
605. Ms S Ramsey: You are carrying out positive work, even at the trust level. The ‘Protect Life’ paper from the implementation group says that its aims are to ensure the implementation of the recommendations in the Southern Health and Social Care Trust area between 2006 and 2011. You say that you will ensure that the recommendations are implemented; however, we are in the midst of a debate on the Budget and the Programme for Government.
606. Mr Donaghy: We plan to ensure it with the resources that we have to the greatest extent that we can. We will ensure that the roll-out of the Protect Life strategy is funded as best we can. In the Southern Health and Social Services Care Trust our share is just over £400,000 of the £1·8 million community total. A sizeable percentage of that is non-recurring; however, if what we put in place proves beneficial, the funding should be made recurring. We plan to use the funding to deliver on those outcomes and objectives.
607. Mrs O’Neill: In the Protect Life strategy the funding is run out over three years. Is that more beneficial?
608. Mr Donaghy: That is where we have a big opportunity in Northern Ireland compared to Scotland.
609. When I was in Scotland, about a year and a half ago, a debate was triggered because the funding for the Choose Life strategy was running out and some of the co-ordinators were thinking about applying for other posts.
610. The positive aspect of funding here, which the suicide strategy implementation body has welcomed, is that the Department said that the £3 million earmarked for suicide prevention in Northern Ireland is recurring: it is not three-year funding, nor is it time-limited.
611. The Chairperson: Colm and Francis, thank you for coming today. It was most informative, and I congratulate you on your project. I hope that somewhere down the line it can be rolled out as a model of excellence that everyone in Northern Ireland can tap into.
10 January 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Alex Easton
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Mr Bobby Cosgrove |
Families Forum |
|
Mrs Jean Carson |
West Belfast Suicide Awareness and Support |
|
Mr Séamus McCabe |
PIPS |
|
Ms Roberta Coates |
RAYS |
|
Ms Marie Osbourne |
West Belfast Parent and Youth Support Group |
612. The Deputy Chairperson: We turn to an evidence session with two sets of representatives of local community and family groups. Those will be formal evidence sessions as part of the Committee’s inquiry into the prevention of suicide and self-harm. I refer members to a number of submissions from the local groups, which are contained in members’ packs. I invite the first group of witnesses to the table.
613. From the outset of the inquiry, the Committee was keen to engage directly with stakeholders such as you, who are carrying out the work on the ground. We wanted to ensure that you had an opportunity to talk to the Committee, and I welcome you. I understand that you have broken into two groups, and that each group will deal with different issues. Mary Creaney, who helped the Committee to organise today’s event, cannot attend, but we are grateful to her for the work that she has done to bring people together. We are pleased that she has been able to arrange for Robert Doyle to be here. You are very welcome Robert, thank you for coming.
614. I have a list of the names of witnesses, but it might be better for witnesses to introduce themselves and give their presentation. Members may then ask questions.
615. Mr Michael Doherty (West Belfast Suicide Awareness and Support Group): We want to raise a number of issues today. The first concerns the evaluation of the current suicide strategy. As members will be aware, the strategy was 12 months old in September 2007. It is now January 2008, and no adequate evaluation of the strategy has been carried out. A lot of money has been spent on it, and perhaps another £3 million will be spent this year, but we want an adequate evaluation that considers whether the actions that were planned for the first year have taken place and, if so, what the outcomes have been. We must learn from those outcomes in advance of moving into the second year of the strategy.
616. Secondly, we want to discuss funding. I will talk about funding from a community perspective, and Roberta Coates will talk specifically about the funding of the RAYS project. When the strategy was first launched, people lauded it and the additional money that came with it. However, funding has been totally inadequate, as well as the manner in which it has been handled. The next funds will be made available in April 2008, but nothing seems to have been learned from previous funding scenarios. Attempting to deal with issues of suicide prevention and intervention in a short-term manner is totally inadequate. Particularly in the community sector, funding must be for a three-year period. Last year, for example, we heard in July that funding had been granted for services that had been up and running in our areas since the previous April.
617. Groups had to lucky enough to be able to borrow money to continue providing services such as counselling. Last year, our funding was due to end at the end of the financial year in March. We were told in March that it was not known whether any funding would be available, but we still were receiving people who had attempted to take their own lives — or family members of people who had taken their own lives — who were referred to us for counselling. Decisions had to be made about whether to tell our clients in the middle of counselling sessions that we did not know whether we had the money to sustain our services. Groups on the ground took the decision to continue with those services. However, we are in the same position this year — the funding that we have been allocated is inadequate, and we do not know what funding we have beyond March 2008.
618. We will be in exactly same position at the end of March as we were last year, and we will have to decide whether to tell people — who are living in tragic circumstances — that we do not know whether we can continue to provide our services.
619. Ms Roberta Coates (RAYS): I am the co-ordinator of RAYS crisis centre on the Woodvale Road. Under the suicide strategy, our priority has been to ensure that prevention, intervention and postvention support and signposting services exist in our area. We have been funded by the Renewing Communities fund over the past 16 months. That funding was for an 18-month project and concludes in March.
620. We are in a precarious position because we do not have our own management committee — we are non-constituted — and the project was set up under a service-level agreement. As our funding will finish in March, and there is no sign of any further funding from the Renewing Communities fund, can the Department confirm — as soon as possible — whether the Renewing Communities fund will receive money after March 2008 so that organisations such as RAYS can look to the future with some degree of hope?
621. An absence of funding would mean an end to our services as we have no means of sustainability. We are totally dependent on the Forum for Action on Substance Abuse (FASA), which houses us at the moment, and it is not feasible for it to support us after March 2008 with its current level of funding. If money is not going to be available through the Renewing Communities fund, I ask for a commitment that money will be available to RAYS through the SSIB. We have not received SSIB funding in the past and realise that doing so will have an impact on similar services because the same money will have to be divided among more recipients. We are weeks away from closure and realise that we are in a particularly difficult situation.
622. Ms Phyllis McDoal (RAYS): I am a member of RAYS and a member of a bereaved family. If the services of RAYS are taken away in March, who will give me the help and support that I get from RAYS, which I would be lost without? I need to know who will help me — and others like me — if that money is not going to be available.
623. Mr Phillip McTaggart (PIPS): I work with the PIPS project. I constantly hear about £3 million that is being invested in suicide prevention. However, the real figure for the money that goes to work on the ground is only £1·3 million.
624. Michael Doherty is right about the services that we provided when there was no funding for them. We took the decision to pay for those services with money that the community and others raised for us. However, when we tried to recoup that, we were told that no money was available, and so it was lost.
625. We had a heavy fight amongst ourselves to decide who got what money, and a lot of us had to cut our counselling hours and our art therapies to ensure that we all benefited. That is the reason that I say that when the funding reaches us it amounts to just over £1 million.
626. There is another funding issue that I do not understand — I might be a bit thick about it — and I hope that someone will explain it to me. We have three co-ordinators in Belfast: one in the north, one in the west, and one in the Shankill. We do not know whether funding will be available to carry those co-ordinator posts through to next year. It would make sense if we knew, before devising programmes of work, that we will have co-ordinators who will implement the programmes.
627. There are a total of eight co-ordinators, a number of whom were already employed as suicide co-ordinators in the Department of Health. Perhaps I am not picking up correctly on what has happened, but I would like to know the reason that those co-ordinators are now being paid with money from the Protect Life policy. Where did their salary go, given that they were already working on suicide prevention in the first place? It seems to me that they have jumped from one job to another and are now taking money from the Protect Life policy funding.
628. Where is the money that those co-ordinators were being paid in their previous jobs? Why did they have to move jobs? How did they get the co-ordinator jobs in the first place, when they would have had to have been advertised? If the funding that we received was additional money, where has the money gone that was previously being used to pay those co-ordinators? I cannot work out that out, and I cannot work out how those co-ordinators were slipped into those positions.
629. We have three people from the community occupying co-ordinators’ positions, yet other people are also doing Department-based co-ordinator jobs. I cannot give an accurate account of who they all are. Is the Department just looking after itself — is that the way it is? I think that it is a case that it is jobs for the boys. Is that true? I am not criticising them because they do good work, but that needs to be examined seriously.
630. The Deputy Chairperson: Does anybody else want to speak before we take more questions?
631. Mr Vincent Donaldson (West Belfast Suicide Awareness and Support Group): I support what my colleagues have said. We would like the Committee to recommend that funding is examined seriously and that it is provided as a three-to-five-year package, rather than annually. Also, beyond what is happening in the communities, the relevant structures in the Health Service do not know whether they will retain funding after March. That is ludicrous. People are in suicidal crisis. The people who are trying to hold their finger in a dyke are those who are under the most pressure.
632. We want to see real recommendations from the Committee saying that funding should be granted on a three-to-five-year basis. That would allow us to plan for what needs to happen, and it would also benefit the structures in the Health Service. That is what we are looking for.
633. Mr M Doherty: I know that the Committee has heard a lot about funding, but I want to point out that the majority of work being done by community groups is on a voluntary basis — it is not funded. I am talking about people who work 24/7 and who will respond when they get a call on their mobile phone at 2.00 am or 3.00 am. Those people are not looking for any funding for that work.
634. We are asking for the back-up services that are needed in the community. For example, in north and west Belfast we ran a pilot helpline under the strategy, and the Minister went ahead and tendered for a new regional helpline in the absence of a proper evaluation. I know that the helpline does good work, but concerns about it have been raised constantly.
635. Through the SSIB and other avenues, we have raised the point that once the regional helpline is up and running and being used, as was the case in north and west Belfast, the expectation will be that after a call is made, a back-up service will be available. It will not. There are not enough resources to cope with what is already happening in north and west Belfast. I do not believe that such resources are available in the rest of the Six Counties, in areas such as Fermanagh. If I were someone from a rural area talking to a person on the regional helpline, my expectation would be that, as a result of my phone call, the person at the other end of the line would get help for me or my family the next day. However, those services do not exist. A strategy must be adopted to ensure that adequate services will be set up. Let us not build up people’s expectations.
636. Mr V Donaldson: In support of what Mr Doherty is saying, we must consider the work that is not being funded. The existence of a strategy gives the community the impression that services are in place. Services are not in place. When people’s expectations are raised in that way, and they go looking for a service that does not exist, you are dealing in death.
637. Crisis-intervention teams provide voluntary services — they are not paid, yet they work all hours of the night. The helpline is ready to go regional, yet, as Mr Doherty says, if people who are in a dark place when they lift the phone are told that the help and resources that they need are not available, again, you are dealing in death. The services must be stepped and properly evaluated in order to determine what is available and what back-ups are in place.
638. Ms Marie Osbourne (West Belfast Parent and Youth Support Group): I want to reiterate what Mr Donaldson is saying about the crisis-intervention teams. In some cases, they are needed to bring people to the Mater Hospital. The people who those teams bring to that hospital are badly treated by front-line medical staff. Something must be done about that. I am from the suicide awareness and support group, Zest. My group has taken part in training with front-line medical staff in the Royal Group of Hospitals. Training must be provided, not only to doctors, but to receptionists, nurses and so on. The way that people are treated in the Mater Hospital is abominable.
639. Mr McTaggart: We try to work in partnership with the different Departments. We believe that we can learn from them. However, they need to know that they can learn from us. We are on the ground, working with families. It is right that we bring people to hospital. We have come up against medical staff who have not been friendly towards individuals. However, in my experience, all the doctors and nurses have been good.
640. The problem has always been that when a person is in dire need of help and support, the facility is not available — a bed or the doctor who must treat that person is not available. It is left to the person’s family to take him or her home. That is unfair on the family. We are constantly being told and encouraged to get in touch with the Department of Health because it will help us out in any way that it can. However, in September 2007, we asked the Department to consider a proposal for a newbuild development of two houses. Since that proposal was sent, we have not heard a word about it.
641. I have absolutely no doubt that each of our groups saves the Health Service a lot of money. We are saving lives. If the Department, the Health Committee and other agencies work in partnership with us, we will save many more lives and a lot more money. It is about working in partnership, yet it sometimes feels as though that does not happen.
642. The Deputy Chairperson: The Committee is conducting the inquiry because it agrees with all your points. It is hoped that at the end of the process, the Committee will be able to tell the Department how the situation stands and how the strategy is being rolled out. It wants there to be a better system. Consistency is needed. All your groups provide brilliant services. Even from the Department’s perspective, your contribution is immeasurable. However, constantly having to go through a raft of funding applications is taking away from the resources that you provide.
643. What Phyllis does is an example of the good work that can be done for people, and through such efforts, we can see what can be achieved and where we would be if such activities were not carried out.
644. We will now open the meeting for members to ask questions.
645. Mr V Donaldson: I would like to make a couple of small points before we go on. I recommend to members that they try to access all the relevant services that are listed in the Yellow Pages. Have any members ever tried to do that? They should try it and see what they find.
646. Over a year ago, we asked that a simple A-Z be compiled of the available services that deal with suicide — be that people in suicidal crisis, or people needing counselling — and the answer was no. That was because no one knew whether those services would still be there after March, and therefore money could not be put into devising that list. That is one example of why a three to five-year package is needed.
647. Ms S Ramsey: Thank you for your presentation. I commend you all, because I am aware of the good work that you and others do. I agree wholeheartedly with Phillip that a holistic approach is required. The work that you and your colleagues do every day probably saves the Health Service millions of pounds. You should not lose sight of the fact that you are doing very positive, good work.
648. With regard to the inquiry, the Committee wants to reach the point at which it can make recommendations to the Minister and the Department. We also want any strategy that is proposed to get the agreement of the Assembly. If that happens, a contract will exist between the Committee and the Department, and we can hold it to the agreement and tell it that it needs to do A, B, C, D and E.
649. I will try and tease out some information from you, and if you cannot provide it today, you can forward it to the Committee at a later date.
650. In human terms, what resources are currently lost due to your organisations’ having to use someone to access funding? If you get money for A, B and C, you must have to use someone’s time, energy and effort to access funding. As Phillip said, even though £1·3 million is available on the ground, the actual amount is probably less than that given that half of an employee’s time is spent trying to access funding. We must try to humanise the process and see what happens.
651. How many projects involved with Renewing Communities will be affected come April 2008? The Committee should write to the Department for Social Development and ask where it stands with Renewing Communities. It is now January, and some groups do not know whether they will still exist in March. Is there any indication that where projects have been funded through Renewing Communities the SSIB will pick them up?
652. Mr V Donaldson: It is a waiting game. The people who organise strategy money say that they do not know what happens under Renewing Communities. If the money that is available under that scheme is recurring we will not have to worry about it. If it does not recur, we will have to go back to the drawing board, and everyone will have to tighten their belts again to try and make sure that funding is available for another co-ordinator.
653. Mr McTaggart: We could not do that again. We already had to tighten our belts last year as regards counselling, therapies and the programmes of work that we were already doing. We had to do that only with regard to our work in north and west Belfast. Let us throw west Belfast into the mix. All the co-ordinators’ posts are essential for the work that is involved in suicide prevention. On top of those posts, we would not be able to operate without administrative support. That applies to all the groups. Therefore, we need to take account of three co-ordinators’ posts and three administrative posts before we look at programmes of work. We will have people in post but no programmes of work.
654. Ms S Ramsey: Does that mean that, when you get the resources, less money is available?
655. Mr McTaggart: Yes. We depend on people in the community raising funds for us.
656. Ms S Ramsey: I just want to tease out that issue, so that we get all the information.
657. Ms Osbourne: Can I just say that the groups first received money in October 2006? It came from the strategy money, and it was for north and west Belfast — the Shankill was not included. The only certainty about that funding was that the three co-ordinators’ posts would be safe until March 2008. Therefore, everybody here is in the same boat; we only know that we have money until March 2008.
658. Ms S Ramsey: Therefore, it is now January, and from what you have said, nobody in the Department’s senior management knows at this stage whether Renewing Communities or SSIB will continue the projects?
659. Ms Coates: No. We do not know.
660. Mr McTaggart: Nobody is telling us. They say that they do not know.
661. Mr McCallister: Does that mean that all the co-ordinators are on notice?
662. Ms Coates: Yes. We must put them on notice.
663. Mr M Doherty: I am conscious that another delegation of witnesses is due to speak, but bad as the situation that we are describing sounds, we are hearing mainly from people in urban areas. The situation in rural areas is worse. We hear that there are three co-ordinators: one each for the Shankill, west Belfast and north Belfast. In the rural areas, as Phillip McTaggart mentioned earlier, the co-ordinators, by and large, are people who are already employed by trusts or boards. In rural areas, the majority of the money that has been given to suicide prevention projects is not reaching the communities.
664. Mr McTaggart: I am not hammering anyone or suggesting that anyone should lose a job, but I am concerned about that situation. I have talked to people in rural areas who did not even know that positions were available. For instance, I would be delighted if people who are working on the ground here took up those posts, because that is what I imagined would happen. The backup support could then come from those individuals who are employed by the trusts. It should not be the other way around; trust employees should not jump ship into the Protect Life strategy and access that money.
665. Ms S Ramsey: It is a question of accountability, and that is what the Committee is here to ensure. I take on board your point; nobody is saying that the co-ordinators are not the right people for the job. Is the money, therefore, not additional funding?
666. Mr V Donaldson: No.
667. Ms S Ramsey: That is something that we could examine.
668. Mr M Doherty: Accountability cuts both ways; it applies to us also. Every penny of the Protect Life money must be accounted for. Every ha’penny that we as community groups get should be monitored and evaluated. The schemes must be run according to best practice. Ultimately, if we do not deliver, we should not get money. All that we are asking for is an opportunity, and not just to get money.
669. I do not want to hear, on 30 March 2008, that Lenadoon counselling project has a particular amount of money for the next 12 months. We deliver counselling for whatever money our project gets. Not one ha’penny goes into administration. We deliver counselling for half the price that people pay anywhere else. I signed a service-level agreement, which says that over the next 12 months we will deliver 2,000 counselling sessions — or whatever number — to people who are referred to us because they are suicidal or are at risk of suicide. That includes their families. Every single ha’penny goes directly to that service.
670. I do not know whether I can offer the service beyond April this year, despite the fact that we fill in monitoring and evaluation sheets every month that list what we delivered for the money that we got. If we are delivering the services that we are being asked to — cost effectively and in accordance with best practice — we cannot keep going back every six or nine months to ask for money again.
671. Ms S Ramsey: I have just one more quick question, and I am conscious that other Members want to ask questions. I take on board Michael’s point. We have all been members of groups that have been asked to jump through hoops to receive money — that is fair enough. In a presentation that we received this morning, the evaluation was brought to our attention, so, to be fair, the professionals are also raising the issue. We have agreed to write to the Minister to find out where that matter stands.
672. I was interested to hear about the healthcare professionals. On reading one of the documents that the Committee received, it struck me that although GPs are being asked to sign up to the applied suicide intervention skills training (ASIST), organisations have concerns about surgery managers, receptionists and triage nurses. We should take that on board.
673. Finally, I would like to hear more information about the project that you are still waiting to hear word about.
674. Ms Ní Chuilín: We walked through the A&E department of the Mater Hospital this morning to see what it is like. We asked about ASIST being made available for everybody who might be involved, and we will pursue that matter. Anyone who is experiencing mental-health problems is in a distressed state. Their family may not be with them, but by the time that they hear about it and look for them, the person’s distress might have increased. When a person reaches the A&E department, the last thing that they need is to be met by a cheeky receptionist. Therefore, we will highlight that issue.
675. We all wanted to carry out this inquiry because we all live in areas that are affected by suicide and because we know what the problems are. The budgets will be for three years, because, up until last year, there was no locally devolved Assembly. The Budget is set from 2008-11, and, if organisations do not get money for three years, that raises an equality issue.
676. Sue is right; she has already mentioned that you need to let us know about any outstanding queries and correspondence that you have with the Departments before you appear in front of the Health Committee. We all live in the communities, and we all have offices around the corner from you. That is what we are here for, and it is a problem if you cannot get access to us. If you have any outstanding matters, concerning either your building or anybody else’s money, you should bring them to us and we will raise them formally through this Committee.
677. There is a huge urban/rural divide. We have heard evidence from the Niamh Louise Foundation. That divide is apparent in healthcare across the board — people in country areas cannot even find dentists. The stigma that is attached to mental-health issues, particularly suicide, is 10-fold in those areas.
678. However, we will be asking about the process that was used to employ people in those areas, because it has been mentioned in the public arena that the employment and recruitment procedures elsewhere were not applied as robustly as they were for the three posts in Belfast. If it is the case that those people are employed through the Protect Life strategy, we will also be asking whether that is value for money and a fair use of resources.
679. We will most definitely be asking about evaluation. If every aspect of this strategy is to be evaluated, for example, phone-line services and so on, the common-sense approach would be to evaluate any programmes before putting them out to tender or releasing more money. If your funding was held up due to evaluation issues, you could have looked at an interim arrangement. However, that is not the case. No evaluation has even been instructed. If it were any other service that had been contracted out, evaluation would have been part of it.
680. Mr V Donaldson: They get monitoring forms on a monthly basis, so it can be evaluated as it goes along.
681. Ms Ní Chuilín: If there is a framework for evaluation, such as your monitoring returns, you need to know that. However, at the minute, there is no framework. Therefore, if funding were withdrawn rather than secured or extended at the end of the cycle, you would need to know the reason. If you did not have the chance to address that through a monitoring and evaluation process, equality concerns then become an issue. To be frank, this whole issue should have been subject to an equality impact assessment from the start. Healthcare should be based on need, rather than matters that are politically opportunistic. Anyway, that is our beef. It is important to bring any issues to the attention of the Committee, because this is the first statutory inquiry in which it has been involved.
682. Funding is a major issue, and we have heard about others. If there are other issues that relate to the inquiry, such as problems with the building or being unable to find out about funding, bring them to the Committee’s attention. I know that Roberta Coates is here, but I will be honest: it was me who asked whether Renewing Communities initiative money would be directed towards the services that we are talking about. We are dealing with a health issue. Suicide and mental health is a social, cultural and economic issue: social development work should come from the Department for Social Development, and health-related work should originate in the Department of Health. I understand the reason that the money was with DSD in the first place, and if work on aspects that Department’s remit is to continue, so be it. The draft Budget should be amended to provide an increase to cover the needs that you have raised with the Committee, rather than people having to tighten their belts and effectively squeeze each other, which you do not wish to do.
683. Finally, we are concerned about the impact that the draft Budget will have on mental-health issues; for example, it has not been made a sufficient priority, and many Members have said as much in the Chamber. I realise that the consultation process ended on 4 January, but I would like to have seen some results. I hope that you provided an input to the process, because it is important that it is not only politicians who are involved, because it will look as though we are being politically astute or manipulative, rather than responding to the needs of the people.
684. Mr M Doherty: Three or four groups responded to the consultation.
685. Ms Ní Chuilín: I am delighted to hear that.
686. Mr McTaggart: We set out to raise funding for the building, but we then heard that the Minister had said on radio that if we had sent him a proposal, he would have looked on it favourably. We sent a proposal that very day. In fact, three proposals were sent to various Departments — that is neither here nor there.
687. Ms S Ramsey: That is the reason that he has not looked at the proposal.
688. Mr McTaggart: We had an idea for a respite centre. I am not concerned about whether it would be a PIPS project or a west Belfast project; we just wanted something in Belfast that would provide a halfway house for people. The majority of people who have issues simply need to talk to someone. In some cases, they need to be kept safe and to feel safe, and that burden needs to be removed from the family for 24 or 48 hours.
689. There are respite centres in England, and many of them are run without any medical staff. Such centres make sense. If money were put into the provision of a respite centre, it would save the Health Service an absolute fortune in the long term. It does not make sense to totally ignore such things. We have said it many times, and we have put it in proposals, but they have been totally ignored. A bit of money may need to be spent, but, in the long term, money will be saved because we are doing the work. We are willing to do that work. We are asking only for services and facilities.
690. Ms Ní Chuilín: We are all based locally, so you should tell us about those things, because we will raise the issue as part of the inquiry. We should agree to send the proposal to Michael McGimpsey, or the Department, or both. If the proposal was sent in September and you have had to wait for the outcome of the inquiry, that is a problem.
691. Mr McTaggart: We never received a reply
692. Ms Ní Chuilín: That means that there is an issue that must be addressed.
693. Mrs Hanna: Good afternoon. I have met you all before on previous occasions. I acknowledge what you have said about evaluation and accountability, and we are aware that we must be accountable for the money. However, we also want to be appreciated when we do good work, and we want to know that the outcomes can be measured. Therefore, if something works, we can repeat it, and, if not, we can try something else.
694. I want to ask a few practical questions about the helpline and the people who man — or woman — it. I presume that, quite often, callers may be in a distressed state. Is a team available late in the evening and at weekends that can react immediately, by getting someone to hospital or by giving some advice? You said that there is no backup. What do you consider the most essential backup?
695. Mr McTaggart: One of the pilot schemes that was set up under the Protect Life strategy was a helpline for north and west Belfast. That was established, and the Minister launched it. Contact Youth Counselling Services and Opportunity Youth won the contract to deliver that service. However, some 15 months later, no evaluation of that helpline scheme has been carried out.
696. The West Belfast Suicide Awareness and Support Group has two mobile telephones, which members — mainly members of bereaved families — carry at all times. The number is publicly advertised. That helpline is not publicly funded. The two phones that they carry are manned by bereaved family members and volunteers. I am sure that PIPS and RAYS are in the same position. However, the pilot scheme — the helpline that is publicly funded — has been up and running, but has not been evaluated. I am not suggesting that that helpline does a bad job. It has good elements, but it also has weaknesses.
697. The Minister has now tendered for a new regional helpline. Had an evaluation of the pilot scheme been carried out, weaknesses might have been discovered and corrected. A helpline is needed most after 9.00 pm and at weekends. When I asked the question at SSIB four months ago, I was shocked to discover that that helpline operates only one line after 9.00 pm. I could be on the end of that helpline for two hours and no one else would be able to get through during that time.
698. Mrs Hanna asked about backup services. I am a local service provider with our counselling project; so are members of most of these groups. We are finding that, after taking a call, the helpline will ring us and refer a client to us for help. We already have waiting lists; we are snowed under.
699. Mrs Hanna: Are they being referred for counselling?
700. Mr McTaggart: It is for counselling and other services.
701. Mrs Hanna: I am trying to build up a picture of your circumstances. I wonder whether a record is kept of calls to the helpline. The Committee needs to find out about measurement of outcomes: if there is none, it is difficult to know how the helpline is performing.
702. How well do you liaise with professional staff? We were given presentations by Mary Black from the Northern and West Belfast Health Action Zone, and from Dr Maria O’Kane. They reported that a joint approach is working for the community. I believe professionals and volunteers are working together.
703. All of you, as volunteers, have been trained in counselling. The professionals also have roles to play, depending on the severity of the patient’s state and whether he or she has to be admitted to hospital. How well does the relationship between professionals and volunteers work?
704. Ms J Murphy: Good partnership working is the key to our area of work. In our organisation, PIPS, good partnerships make it work. That should be reinforced at departmental level.
705. Ms Hanna: That must be formalised.
706. Ms J Murphy: We, on the ground, know that. We have boundaries, and we bring the key players with us.
707. Mr McTaggart: There are barriers to be broken down, not only in suicide prevention, but between volunteers and professionals too.
708. The only reason I am involved in this work is because I lost a son. Like other family members, I do not want that to happen to anyone else. We should not tell doctors and others what to do. However, believe it or not, because we come from the community, we can sometimes see better ways of doing things. We might say: why not try this?
709. Mrs Hanna: The professionals have acknowledged that.
710. Mr McTaggart: Sometimes, they have letters after their names, and so on. However, a lot of negative attitudes have been broken down. We are now working much better with professional services.
711. The Deputy Chairperson: Volunteers and professionals complement one another.
712. Mr McTaggart: Exactly. I do not mean to knock the professionals. We are getting better at working together. There was, and there may still be, some barriers to be broken down in that respect.
713. Mrs Hanna: The pilot scheme is working and is being evaluated, but there is no funding. However, the Committee wants to see you all working together to get people better. That is the bottom line for us all. We want to see, perhaps a year down the road, young people and others ceasing to self-harm and fit in well with their families. We must be able to measure that and to continue with what is working well.
714. Ms S Ramsey: The point that needs to be made is that the helpline is funded by the Department. If it were funded through community infrastructure, and was not evaluated, it would be crucified. There cannot be double standards.
715. Mrs Hanna: I was just trying to find out how it works. I appreciate what has been said. I was referring to a different issue.
716. Ms Osbourne: I do not know how the helpline monitors and evaluates its calls. By chance, I recently met someone who works on the helpline. She told me that she was unaware that we operated a 24/7 helpline, although that is stated on all of our documentation. She said that a young person called from Belfast City Cemetery, and they did not know what to do with him. She went on to say that had they known that we operate a 24/7 helpline, they would have transferred him to us.
717. Mrs Hanna: That is a problem.
718. Ms Osbourne: They simply wanted to hand him over to us.
719. Mr V Donaldson: We are in favour of a 24-hour helpline, but it has to be properly managed. If it is not, death will be the result. I am part of the crisis intervention team. At weekends, I am sometimes out at 3.00 am and 4.00 am, trying to keep young people safe and get them to where they need to be. I do not want to have to do that, but I am aware that nothing else is available.
720. If the 24/7 helpline is properly managed, I will not have to do what I have been doing. There could then be a crisis team that goes out to talk to those people. Sometimes, all they need is someone to talk to, and sometimes someone has to stay with them until a doctor or counsellor becomes available the next morning. As I have said, if the helpline is properly managed, there should be no problem. The problem that we had with it was that there were a lot of faults during the pilot period, and, all of a sudden, before it has been evaluated, it is being expanded.
721. Mrs Hanna: That is helpful. It gives us a fuller picture of what goes on.
722. The Deputy Chairperson: It is a point well made. Schemes should not be tendered for if they have not been properly evaluated in the first place.
723. I am conscious of time, and we have yet to hear from the second set of witnesses. A number of points have been raised, including the evaluation of the pilot helpline; funding; the appointments process; the application for the respite centre; the ASIST training; and the role of DSD and the Renewing Communities fund. The Committee will raise those points with the Department and with the Minister.
724. Ms S Ramsey: There is also a point to be addressed regarding the A-Z directory.
725. Ms Ní Chuilín: Let us know if there are any other issues that you think of when you leave.
726. The Chairperson: I thank the first set of witnesses, and I welcome the next group. Thank you for waiting. Would you like to introduce yourselves?
727. Mr Séamus McCabe (PIPS): I am chairperson of the PIPS project in Newry and Mourne. I am here to represent the rural community.
728. Mr Gerard McCartan (PIPS): I represent the PIPS project in Belfast.
729. Ms Maureen Young (Families Forum): I represent the areas covered by the Northern Health and Social Services Board.
730. Mr Robert Doyle (West Belfast Suicide Awareness Group): I represent the Northern Ireland Association for Mental Health, Northern Ireland Children’s Enterprise and the West Belfast Suicide Awareness and Support Group.
731. Mr Bobby Cosgrove (Families Forum): I represent the south-east Belfast Families Bereaved by Suicide group.
732. Ms Ann McGarrigle (Families Forum): I represent the north-west region, from Omagh to Limavady, of Families Bereaved by Suicide. Our meetings are held in the headquarters of Foyle Search and Rescue.
733. Mr McCartan: I will talk mainly about the availability of beds for children and adolescents. After I lost my son to suicide, the major independent review of his death made many recommendations. Therefore, I speak as someone who has experienced the healthcare system with a child who was mentally ill, self-harming, and was unable to get any help. We had to fight to try to get help. I could not believe that, at that time, there were only 12 beds for children and adolescents in the whole of the North of Ireland. We could not get my son any of those beds, and he was admitted to an adult ward, where he continued to harm himself.
734. When the suicide strategy was announced, Shaun Woodward said that a new unit would be up and running within 12 weeks. I challenged him to tell me where he would get the necessary staff. That unit never materialised. Unfortunately, the unit at Knockbracken Healthcare Park was destroyed by fire. We have heard that another unit will be built at Forster Green Hospital in 2009, but I remain sceptical.
735. Carál, you said that you visited the Mater Hospital today. I do not know whether you visited the psychiatric unit but, unfortunately, it is a very scary place for a child. Children from north and west Belfast are being admitted to what for them is a terrible place.
736. Jo Murphy, my wife, Carol, and I are involved in a project to oversee the implementation of the recommendations that were made after the death of my son. A few moments ago, I was talking to someone outside who told me that four beds will be partitioned off in the Dorothy Gardner and Donard adult wards at Knockbracken — two for boys and two for girls. We have been told that the funding has been approved, and that the go-ahead is forthcoming. Next week, I will visit Knockbracken to see exactly how that has been done.
737. The criteria state that there should be 28 beds for children and adolescents in 2008. There is some confusion but, as far as I am aware, there are only six. Under the Freedom of Information Act 2000, ‘The Irish News’ discovered that, over a period of five years, some 500 kids were admitted to adult wards. However, given that £5 million was spent sending kids to England, Wales and the Republic of Ireland, the money is available for extra beds. The situation simply does not make sense.
738. Daily, we hear about a simple problem that would cost nothing to rectify. When someone is discharged after admission to a psychiatric ward, he or she must wait for a letter detailing an appointment to be posted to them. Sometimes, the letter does not arrive, and people cannot understand why the hospital does not simply give them an appointment card, because a confirmed appointment is a lifeline to people who are being treated, and to their carers. I see a definite increase in that problem.
739. Mr Cosgrove: When the suicide strategy was first introduced in March 2006, the lack of adolescent beds was raised at the first meeting in the Culloden Hotel. At that time, there were four beds for kids. The pressure from families that was applied through the Suicide Strategy Implementation Body led to the number being increased to, at one time, 14. The number has now decreased again, and the total lack of facilities for 16- to 18-year-olds in the Health Service is scandalous.
740. When we first received the SSIB strategy, it informed us that when an individual takes his or her own life, it costs the Government £1·2 million. When we asked how that was possible, we were told that the figure was arrived at by calculating lost income based on age and various other factors. My group deals solely with families, and trying to help them. We do not take phone calls, etc. However, considering the work that Phillip McTaggart and others in this room have done, and the number of lives that they have saved, they have saved the Government, according to their own figures, one hell of a lot of money.
741. When we first started, we received £1·9 million for the first six months, which has still not been accounted for. We have accounted for the funding that we received. However, people in the statutory bodies have not accounted for what they did with their share of quite substantial sums of money. Dr Brian Gaffney, chief executive of the Health Promotion Agency, received quite a substantial sum of that money to run mental-health GP training, and so forth. As families, we repeatedly ask questions. In fact, Dr Gaffney walked out of a meeting in Derry one night because of the questions that he was asked. Nevertheless, they were realistic questions. I asked him to account for what happens. For example, if he takes £350,000 for GP training, and he only spends £100,000 on that training — which is probably closer to the sum that has been spent on training the number of GPs that we have been told about — no one has told us what happens to the other £250,000.
742. There is an ongoing television campaign that focuses on the issue of mental health. The Dublin Government’s mental-health logo appears at the bottom of the advertisement. That has nothing to do with suicide awareness, yet Suicide Awareness is paying for the advertisement. That is coming out of our budget. Those are the types of issues that we, as families, feel strongly about. We believe that those matters need to be examined to see whether we are getting value for money. In this game, £3·1 million is not a lot of money. If we save three lives — PIPS and Suicide Awareness have probably saved between three to five times that number of lives — we have saved the Government £12 million pounds. Therefore, we are entitled to answers.
743. Mr Doyle: My contribution is more of a personal perspective on dealing with people — I am not a great man for facts and figures. Yesterday, I looked at the strategy document, ‘Protect Life: A Shared Vision’, and read about the action to be taken and the three targeted approaches. I also looked at the section on children and young people. I echo the first group of witnesses when I cite the importance of an evaluation of whether the targets have been met — and how and why they have or have not been met — and what can be done, using the resources of community, voluntary and statutory organisations, if they have not been met.
744. I want to mention schools, and I would like the Committee to consider the development of an emotional literacy programme, or healthy living programme, or whatever you would like to call it. That programme should be something that does not carry a stigma and that children will be comfortable to learn about, regardless of their age. It should be practical and capable of being evaluated. It should also be standardised and have protocols for teachers and staff on the ground.
745. I have spoken to many teachers who have asked about the signs that they should look out for and what do they do if they see those signs. They want to know whom they should contact. They do not know the answers to those questions. As a result, they are not engaging with individuals with whom they have a close enough relationship to talk about suicide, self-harm or mental distress. Action must be taken to address that situation. Committee members, if they examine the issue, can decide for themselves the action that should be taken.
746. In respect of front-line Health Service staff, many of the young people with whom I come into contact through my work in mental health have been taken to hospital, and end up discouraged from going back because of negative reactions that they have received there. On the other hand, there are some individuals who have had positive experiences and would be willing to go back for further help. The people who have been involved in many of the negative cases that I have seen are fearful of the rigmarole around initial assessment, questioning and waiting around. We need, as has already been said, a centre of which everyone in the community, and other organisations, is aware. That should be a centre that specialises in dealing with children, can think outside the box, and can think beyond the medical approach, assessment, detainment if need be, or medication.
747. The young people with whom I come into contact who have been through that system will continue to go through it. They are grand for a while, but things deteriorate; they go back into the system and, before long, their situation resembles that which adults must deal with — they are in the same situation as before, or worse. We must take that into consideration, try to catch them early, and attempt to introduce positive coping strategies. That point may emerge after evaluation, but I am not sure whether it has been implemented in all schools.
748. I am aware that all schools have pastoral-care systems and contracts with organisations such as Opportunity Youth and Contact Youth, but are those services effective for everyone who engages with them? We must find out.
749. Creative therapies such as art or music therapy have been mentioned. Is it possible to conduct research to find out whether such therapies are effective or beneficial? The work that is done on the ground involves such therapies, and the feedback that I have received from children and young adults is that, having felt crap when they came in, those therapies really worked and helped them to bring out their problems and work through them. Obviously, more is required and no one solution can offer a magic cure for everything. However, society, Government and the relevant agencies must work in conjunction with one another and start to think outside the box. They must ensure that they have a joint aim, they know how that aim will be achieved, and, if it is not achieved, that they know how, why, and what must be done at the next stage.
750. Mr McCabe: As I said earlier, I represent PIPS in Newry and Mourne, which covers a population of more than 90,000 people from Crossmaglen to Banbridge, and from Armagh to Kilkeel.
751. PIPS stands for the Public Initiative for the Prevention of Suicide and Self-Harm, and we have experienced several issues relating to self-harm because the resources to deal with that problem are non-existent. Although members of the Committee may not have heard of us because we are from a rural area, PIPS in Newry and Mourne was established in 2003 and constituted and registered in 2004 — shortly after PIPS in Belfast.
752. In our attempts to access self-harm resources, it has been difficult even to get information, and we have had to go through various voluntary groups such as Zest, which has outreach counsellors. In rural areas, getting information and accessing the available resources are major concerns. It is almost impossible to get our hands on anything.
753. I will touch on several points that have already been covered by Michael Doherty and Phillip McTaggart, and I will speak about rural areas and the problems we have with — here we go again — funding. I am sure that Committee members love to hear that word. However, it is a big issue, and it cannot be overlooked.
754. The first group of witnesses represent inner-city areas. PIPS in Newry and Mourne, as I said, was constituted in 2004, and we have a major problem. This time last year, we made a request for a co-ordinator. We cover a population of 90,000 — PIPS Belfast covers a similar population, but has three co-ordinators in place. To date, we have only just received confirmation that we will receive funding for a one-year non-recurrent post that must be shared between ourselves and the Niamh Louise Foundation.
755. According to the southern area action plan, which members may check on the Internet, and as Phillip McTaggart said earlier, everything is trust led. PIPS in Newry and Mourne has been established for more than four years, and has done much of the groundwork. Our experience is that many jobs are being restructured — people are taking on different jobs — and the funding is coming out of the same pot.
756. This time last year, we applied for the post that I mentioned, and we were told that not enough money was available. We are now told that, because the end of the financial year is approaching, last year’s money is now available for non-recurrent posts. Therefore, we will be funded for one shared, non-recurrent post for one year.
757. The action plan also stated that a co-ordinator post would be created. That position has been claimed by the trust — the Southern Health and Social Services Board now has a member from the trust who has filled that post. The two non-recurrent community-development posts for PIPS in Newry and Mourne and the Niamh Louise Foundation must correspond with the trust at every opportunity. That is totally inadequate. We have been doing all the groundwork, and the wheel is now being reinvented.
758. There was a cluster of suicides in the Kilkeel area last year. Eleven suicides occurred within a three-mile radius among a group of young people aged between 18 and their early 20s. At the request of the community, we did not attract any attention to those suicides. The Committee will be aware of the media frenzy in the aftermath of the suicides of three young people in the Tandragee area. Eleven young people took their own lives in Kilkeel. We put a number of projects in place and did all the groundwork. We contacted all the people in the Department who needed to be contacted, and they arrived at a later stage. They came back at the postvention stage, but we were there for the prevention and intervention stages, and we are still there for the postvention stage. We did all the groundwork, but feel that we are just being pushed aside to let the trusts and all the other statutory groups take control of everything yet again.
759. It is very unfair, and, as Michelle O’Neill said earlier, the voluntary groups need consistency. We cannot achieve consistency with a one-year, non-recurrent post. That post must be offered on a three-to-five-year basis, otherwise people will not come on board.
760. Like Phillip, I became involved in this work because of a personal tragedy — I too lost a son. However, I am here, and I work with a passion. That passion can last for only so long, because people tire themselves out, and run out of breath. The people from the trusts are bringing a different agenda. At the end of a nine-to-five day, they can go home, watch Coronation Street and go to bed, or whatever. On the other hand, we in the families sector do not have those options. If a bereaved family member makes a phone call or other form of contact, we have to be there for them. We feel that none of those considerations are being taken on board, and that the view is that the community and voluntary groups can be left to do the work, because they do not have to be paid and they will do the work anyway.
761. Ms Ann McGarrigle (Families Forum): I am from the north west, and, as part of the suicide strategy, Zest was one of the teams that received some money for a pilot self-harm and suicide young people’s mentoring project. If I had been talking to you a few months ago, I would have told you that I was seriously concerned, because the group could not get up and running owing to all of the protocol and data that had to be attended to. Every time the group was ready to go, something else would crop up. I am very pleased to say, however, that the group is up and running, and will eventually be able to provide some evaluation figures.
762. We are different: we are part city, part country; we work in places such as Limavady and Dungiven. Like Bobby Cosgrove’s group, our wee support group does not do any intervention; we offer support. I am a member of the Western Health and Social Care Trust’s suicide strategy implementation group, comprising seven people from statutory bodies, five from the community and voluntary sectors, and two bereaved parents — I represent the city and Limavady, and Brian Rogers represents Omagh and Fermanagh. We cover a massive area, but we seem to be able to bring town and country together.
763. Most bereaved people want help and support. They want to talk to others, to meet and help one another to fix things. Rural areas are different: there are more elderly people, who might come along to one conference and never be seen again. It is enough for them to know that there is a number that they can call to get support. Counselling is on offer in the west, and it is working. In the Omagh area, counselling is provided by the Tara Centre, which is an excellent venue, providing various therapies. In Derry, Cruse Bereavement Care is paid for its counselling service. The funding for those counselling services came from money provided by the Western Health and Social Care Trust.
764. The last time I came before the Committee, I told members about a spate of suicides among young people in one specific area. Through money that was made available by the Western Health and Social Care Trust, a plan involving youth clubs and a mental-health team will provide a clinic where young people can mix. That funding will also provide for a music programme in conjunction with the Nerve Centre and the Verbal Arts Centre, which will help to build self-esteem.
765. I also work in the further education sector, and we provide a lot of pastoral care. Although each college does that differently, they work alongside one another. Education has a role to play in pastoral care. Ms Young will back me up when I say that nothing is definite. At the same time, though, wherever something happens, we have applied for small amounts of money to deal with people who have displayed poor mental health, or some other incident, in that area, and we have been given it.
766. It is hard to keep bereaved families together. Young people will not mix with older people. Two or three families visit us from over the border in Donegal. We are fortunate in that we have the services of Foyle Search and Rescue Service. It provides intervention through the great work that it does on the River Foyle, and it also allows us to use its premises. ASIST is also delivered to all the taxi drivers in the area. Those measures work. However, suicide figures have not been quashed; there is still much work to be done. Between Halloween and Christmas, there was a spate of suicides, although, as I was told at a support group meeting on Monday night, there were not so many during Christmas. In fact, there were not that many attempted suicides. Therefore, we wait in anticipation to hear how effective Zest’s work is.
767. With regard to the music sessions, the co-ordinator that Mr McTaggart and others mentioned also works with us. Tomorrow, I will meet with Barry McGale, who was our suicide awareness co-ordinator. He has now been appointed as an intervention officer for families, and he carries out similar work to that which is being done on the ground by the groups in Belfast. Dermot Lynch is doing that work in the Omagh and Fermanagh area. Such matters have, therefore, been covered.
768. We are also involved in training with the Churches, and that strategy has been a big initiative in rural areas. Events have also been held in the City Hotel in Derry. All that work adds up to our being involved in events. For example, on 16 February we are holding a hope and healing conference in Fermanagh. That has been funded with money from the suicide strategy. In 2007, the same conference was held in Derry. I can, therefore, report that events are being held, and a lot of work is ongoing. I asked the support group whether there was anything that it wanted to be introduced. It asked whether it would be able to hold a residential. That is not for the Committee to decide; it is for us to decide tomorrow. However, those are measures that seem to help and support people in getting them over the second and third stages of recovery, and we deal with people of all ages.
769. It must be remembered that if the regional helpline is introduced, people of all ages will have to be dealt with and work on it. Someone from a remote farmyard could need immediate help, so he or she must be able to speak to someone else of an appropriate age group. Indeed, yesterday I heard that someone in Magherafelt had phoned the north and west Belfast helpline.
770. Ms Young: As Ms McGarrigle has said, the Northern Health and Social Services Board area stretches from Newtownabbey to Coleraine. Therefore, it has a wide geographical spread. The suicide co-ordinator who has been appointed there is doing a great job — she has hit the ground running and has introduced many initiatives. Her work has meant that a directory is available of the various organisations that are involved in suicide prevention. Again, the same issues apply — money must be guaranteed for the continuation of jobs and appointments.
771. Mr Doyle and Ms McGarrigle also referred to education. The Committee needs to be aware that child-protection issues put teachers in a delicate position. Often, when a child indicates that something is wrong, we cannot ask questions — the matter must immediately be passed on to designated personnel in the school. In many ways, teachers’ hands are therefore tied. As professionals, we often feel that we would like a little more scope to deal with situations. The pastoral system that is up and running in many schools is patchy and varies between schools. The action that is taken by a school depends on its principal and policies.
772. Given that I am involved with the Families Forum and in teaching, I sometimes wonder whether teachers realise fully what they are being asked to do. Much emphasis has been put on education. If one were to talk to teachers, 99·9% of them would say that they already have enough to do. They say that they are willing to help, but that they are unable to take full responsibility for it.
773. Ethnic issues also arise for the Northern Board. Last year in Cookstown, a spate of tragic incidents occurred that involved people from eastern Europe. Language difficulties meant that unfortunately, it became too late to intervene. More resources and availability of help must be concentrated on that area, and that is perhaps even more important as we approach a slight economic recession. I heard a story about St Vincent de Paul having to provide heating oil for a Cookstown family at Christmas. Many issues and problems can arise from that type of situation.
774. Bobby Cosgrove mentioned GP training. That has been offered by the Northern Board and the Western Board, and we understand that it has been taken up fairly well. However, we would like to know the numbers of GPs that have availed themselves of the training that has been carried out so far.
775. I realise that time is an issue, so that is all that I want to say.
776. The Deputy Chairperson: Thank you all for your contributions. A lot of your points were also made by the previous group, and we certainly take those points on board. Maureen, you are right to point out that there is disparity in the uptake of ASIST across the area. Some areas might be stronger than others in that respect, and in some hospitals the front-line staff might have taken up the training more than others.
777. Issuing a patient with an appointment card when they leave hospital is a simple suggestion, and we can recommend that in our conclusions. The emotional literacy programme in schools is an excellent idea, and it is also something that we must consider. So far as people who live in rural areas are concerned, the representative from the Niamh Louise Foundation told us that that organisation was formed because her family felt that it had nowhere to turn. From speaking to the witnesses, I know that you are a great help to each other. Has the fact that you have reconstituted yourselves as Family Voices made a difference to how you are heard in the SSIB?
778. Mr McCabe: Family Voices is the result of a lot of families getting together from across the Province, and it allows us the opportunity to share information. It meets on a regular basis.
779. Ms McGarrigle: We met just before Christmas, and we will meet again on Saturday 19 January. We are trying to include all suicide-prevention groups, and we have appealed to all of those groups to be part of Family Voices. It is difficult and tiring for bereaved people to talk about their story, but we need to know the issues and act on those as a collective bunch. The group will meet prior to the hope and healing conference, and we are hopeful that that will allow people who might come to our meeting only once to raise issues that they have with the coroner or A&E units.
780. The Deputy Chairperson: When Mary Creaney attended a previous Committee meeting, she said that she felt that families’ voices were not being heard. I wonder whether the organisation has helped to strengthen those voices.
781. Ms McGarrigle: We are still trying hard. We have not given up, which is the main thing.
782. Mr McCabe: One of the major concerns for the southern area is the fact that, because it is a rural area, it does not have the same voice. I do not think that there are any representatives here from a rural area.
783. The Deputy Chairperson: I am from the mid-Ulster area.
784. Ms S Ramsey: I used to live in a rural area, then 70,000 houses were built.
785. Mr Cosgrove: In early October 2007, the Committee sent an email asking people to respond to its inquiry into suicide. Did you get many responses to that, and have those responses been collated?
786. The Deputy Chairperson: Yes. We received roughly 65 responses, and we are meeting people and trying to put all the evidence together. All the evidence will be published in the report: we make sure that all contributions are recognised in the Committee’s recommendations.
787. Mr McCabe: The main issue is the reason that the trusts take ownership of everything. We are doing a lot of groundwork, and when the action plan was released, there was no word at all about voluntary groups taking ownership of anything — the trusts were taking the lead and giving wee bits and pieces to the voluntary groups to keep them happy. We have received £2,000 from the strategy to date, but having said that, there has now been an offer of a post. We have not received much from the Department.
788. The Deputy Chairperson: It is concerning that someone was working in a post that was paid for by the trust at one stage but is now being funded from elsewhere.
789. Mr McCabe: We have a co-ordinator who was employed in November, but obviously, funding for that could end in March. The probability is that the post will be recurrent. That post was made available for them, despite the fact that we submitted an application form for it this time last year. Our application was not looked at until later in the year, and even then we were given another recurrent post for a year and told that that was all that was available.
790. The Deputy Chairperson: That point was well made.
791. Ms Ní Chuilín: Presentations were made to the Committee this morning by Mary Black and Maria O’Kane, who are consultant psychiatrists. Mary Black told the Committee that there will be a conference on 6 February to examine good practice across Belfast and to set future priorities for the action plan. Are you aware of that conference?
792. The Deputy Chairperson: The groups that are here now deal with areas beyond Belfast.
793. Ms Ní Chuilín: Ann, if your group is meeting next Saturday, that conference should be discussed then. It is important that we hear from families and groups who have not only been bereaved through suicide, but who have to live with the consequences of self-harm. It would be worthwhile to find out what the main issues are. That conference will examine good practice, which should include the recruitment and retention of staff, evaluations of phone lines, the disparity in funding between urban and rural areas, and the issues that Robert spoke of, such as self-esteem, confidence building and —
794. Mr Doyle: Personal skills development.
795. Ms Ní Chuilín: — personal skills development in schools. I know that money was invested in such services after three young people took their lives, but was that a one-off, short-term solution? We will ask what each Department is doing to ensure that the strategy is implemented.
796. Mr McCabe: That is one of our points. In the case that you mentioned, the Department intervened only in the aftermath of that tragedy when a media frenzy was going on. That tragedy happened in Kilkeel, and when we needed the Department to intervene, it still did not get involved until a later date. Therefore, it perhaps takes such a media frenzy to catch the Department’s attention.
797. Ms Ní Chuilín: That is a problem. Michael McGimpsey met Internet providers and media representatives, and our parties have also met with media representatives. The Samaritans published guidelines on how to report instances of suicide. However, there are big lessons for us to learn. The difficulty is that, although we have a responsibility and do not want to sensationalise incidents, we want to use any means possible to raise awareness. Therefore, a balance must be found.
798. We are happy to include in our report instances of people behaving sensitively but not feeling that they are getting the Department’s support. There are big disparities, in some instances due to bigger populations, and the resources do not meet needs. It is important for you, Gerard, to talk about your views on the recommendations in the report, which were a result of the treatment that Danny received, and the subsequent treatment of your family.
799. Mr McCartan: People are still going through what we did two and a half years ago.
800. Ms Ní Chuilín: Absolutely.
801. Mr McCartan: When Danny was in Knockbracken, his records did not go to the Mater Hospital as they should have. When the Belfast Health and Social Care Trust was established, it stated that such an occurrence would not happen again. However, someone rang us today who is in Windsor House and is waiting for an appointment in the Mater Hospital because their records have not arrived. That person is in limbo — they have no psychiatrist and no community psychiatric nurse (CPN) because their records are in Windsor House instead of the Mater Hospital. Therefore, the same thing is still happening.
802. The Secretary of State gave £400,000 to the Children and Young Peoples’ Funding Package for Sure Start. Half of that has been spent, meaning that £200,000 is still available. However, organisations are having trouble finding staff. Why is that?
803. An excellent woman called Dawn Rees is involved in the project, and she has worked with the Department, helping to pull all the co-ordinators together in England. She seems to know what she is talking about, and I think it would benefit the Committee to meet with her.
804. Ms Ní Chuilín: Please bring to us any information or lessons that can be learnt, because some of the recommendations are that no other family should have to go through what yours did. We do not want to single out any families. I imagine that there will be resolution when you feel that no other family will have to go through what you went through.
805. However, there is a statutory obligation and a duty of care to look after children, and it is a problem if they are still consistently being put into adult wards. Given that child protection issues are involved, it would be worth the Committee’s asking how many children are put on adult wards. I have spoken to hospital staff who literally watch children 24/7 by sitting beside their beds. That is not good for the child or young person, the staff, or the family. It is also not good for the service, because it means that people will lose confidence in it.
806. Mr McCartan: That is the reason that a respite centre is an excellent idea. That would get the young person out of the damaging environment, the family would get a break, and the young person would be safe and looked after.
807. An organisation charity called Winston’s Wish has been established in England. That is a community-based charity for bereaved children that has excellent programmes for young people until they see representatives of the statutory agencies.
808. Ms Ní Chuilín: Obviously, respite for the entire family, and certainly for the children and young people, is needed.
809. The Deputy Chairperson: It is disappointing for you to have to say today that lessons have not been learnt, because people are still ringing you with the same problems in 2008. Carál is right when she says that many lessons are still to be learnt.
810. Ms S Ramsey: Thank you for the presentation. I have a couple of comments to make, and I will then ask one or two questions.
811. First, you should not be downbeat, because the Committee has raised with the Minister some of the issues that you highlighted in your previous presentation. I will give you a couple of examples.
812. You raised the issue of young people in further and higher education, and we pushed the Minister on that, and, in fairness, he was going to talk to the Minister for Employment and Learning to get his Department involved in the ministerial task force. Therefore, suggestions and recommendations that come from organisations such as yours allow us to do that.
813. I remind you all that this Committee is independent, and that no one will be pulling our strings when we write our report. We are not answerable to anyone except the Assembly and the people who vote for us, so we can make as many radical recommendations as we choose. We could ask the Department now for an update on the recommendations from the inquiry, and even a time frame for when they will be implemented in full. When the findings of previous investigations were produced, everyone and their granny said that they would learn lessons from them and implement certain recommendations. However, I feel that some lessons have not been learnt. Therefore, using our scrutiny role, we can probably get an update without having to wait until we write our report.
814. To give you some information about what will happen and to reiterate my point about not being downbeat, any issues that you raise with the Committee will be taken on board by the parties and others in civic society who are working on a bill of rights. As you are aware, that will mean that certain provisions will be set out in legislation. For my sins, I am working on the children and young people’s section of that, and the provision of child and adolescent psychiatric beds is one of the main areas of health and education that we are considering. Indeed, Sinn Féin has been fighting for the availability of more beds for a long time.
815. The Departments have a moral and legal duty to ensure that services are provided where they are needed. Through the bill of rights, we are pushing to have that provision included in legislation to which the Departments cannot legally or morally fail to adhere. We are able to do that in large part because of the evidence of groups such as yours. Although the Committee may be able to make a difference, the bill of rights will also have a role to play.
816. Lessons must be learnt. Bobby, it struck me that you said that when a family is bereaved through suicide, there is no joined-up approach by the PSNI, the coroner and social services. I raised that point this morning when I met people representing the health action zones. That issue will be taken on board, because the last thing that a parent wants to do when struggling to come to terms with the death of a loved one is deal with all those separate agencies. If simple issues such as that are addressed, a big difference will be made to individuals and families.
817. It is unfortunate that you have become the experts and are in the position of being able to bring the solutions to us. It is up to the Committee to include those in the inquiry’s report and to push the Executive to encourage all the Departments to take a holistic, joined-up approach. The Department of Health, Social Services and Public Safety, the Department of Education, the Department for Social Development, the Department of Culture, Arts and Leisure and the Department of Finance and Personnel should all adopt such an approach.
818. Thank you again for coming back today and giving us a great deal of information and knowledge.
819. Mr McCallister: I have a couple of comments to make. I am aware of PIPS in Newry and Mourne, because I come from Rathfriland and am a member for the South Down constituency. I am aware of the good work that you do, and I am more than happy to meet with you there sometime.
820. Several years ago, before I became involved in politics, I worked on strategies in Banbridge and Craigavon. I agree with your comments about funding a post for a year. To employ anyone for a year ends up being almost pointless, because everyone has bills to pay, so once in post, the individual starts to look for another job. If the individual leaves before the year is over, the appointment has been a waste of time, and employers end up running around chasing their tails.
821. The previous presentation also made it clear that funding mechanisms must be established to secure streams of funding for probably at least three years, and perhaps for as long as five years.
822. Hearing about your experiences has made this an interesting afternoon. I am grateful to you for sharing them with us, as, I am sure, are all the Committee members. It is important that all the work in which we are involved is evaluated properly. It would be great if we could consider our final Committee report as a true representation of our vision of what should happen.
823. As Sue rightly mentioned, no one pulls the strings here: the Committee will stand over its decisions. It would be nice to see a report that challenges the Health Department and, as was mentioned earlier, other Departments that have an interest in the issue. If they disagree with any aspects of the Committee’s report, they should state the reasons and be asked to suggest better alternatives. The Departments must be held to account, and we must check their progress on the implementation of any part of the report for which they are responsible.
824. Too often, a nice report is compiled that simply collects dust on a shelf somewhere; it does not become a living, working, breathing report with measures that are being implemented on the ground. All Assembly Members, not only Committee members, should be encouraged to listen to groups from their constituency to hear what is happening on their patch. That is more of a comment than a question. I wish you well in your work.
825. Mr Easton: Most of my points have been raised already. However, one point that I picked up in our session with the other groups — and perhaps more so from listening to your contribution — is that there seems to be a lack of a joined-up approach from Departments, boards and so on. They seem to give you a small amount of funding and talk to you a little, but when matters reach a certain level, they do not want to take them any further — they do not seem to want to listen.
826. Do you agree that any inquiry that this Committee conducts, or any measure that the Minister puts in place, will be pointless unless Departments and boards get to the bottom of this matter with the local community groups and the families who face the issues daily or weekly? Do you agree that it is vital not only that we put that point across in our work, but that the Minister takes it on board, too? No approach can work unless we have your and the families’ input.
827. Mr McCabe: I agree. The strategy is a bottom-up strategy, and it was put in place as a result of lobbying that bereaved families carried out. As you said, when work reaches a certain level, the Department takes ownership of it, and we are cut off. The community groups take the work as far as they can, and the Department then takes over. That is the way it is. I do not know how the system works in the inner city, but I know that that is how it works in rural areas.
828. Mrs Hanna: Hello again. I know that it is hard for you to come back because you feel that you have been there; it has happened to you. You can see some of the solutions, and it is frustrating when there does not seem to be any change.
829. As each of you spoke, I made a few notes. Séamus, from listening to you, the main point that emerged was the poor relationship with the trust, which Alex mentioned. You are like the poor relation. It is somewhat like the situation with carers; similar to them, you are the people who have the practical experience, and no approach can work unless a real and meaningful partnership exists. Both sets of people must be involved: you, the people with the experience who know what happens in the community and who can see the solutions; and the professionals, who also have their role to play. However, a genuine partnership must be established.
830. Gerard, you talked before about the lack of beds, and a respite centre has been discussed. Some people perhaps need an acute bed to get them through the first 24 hours. The whole focus now — and this was apparent even from talking to Dr Maria O’Kane this morning — is on keeping people out of hospital if possible. However, people still need hospital treatment if they are in the acute phase. Medical professionals are now talking much more about counselling and talking therapies, in which, again, so many of our first group of witnesses are very much involved. It seems crazy that your idea about an appointment card cannot be introduced. That seems like one of the simple things that certainly should be happening.
831. Professor McClelland from the Bamford Review group has made it clear that there are no easy answers to mental-health problems and self-harm and suicide issues: there is no magic solution. He talks a great deal about the need for new ways of working together and for a better and different kind of training. Raising awareness among everyone is important, especially among staff, teachers and parents.
832. Robert, a very good presentation was held in the Long Gallery on the Bamford Review. Again, the economic argument for prevention and early intervention was made, and some good schools’ programmes were mentioned. Introducing coping strategies and raising self-esteem were discussed at that presentation. People who are trained in the matter must come into the schools to deliver those programmes. Many of those training programmes already exist, but we must make sure that they are actually delivered.
833. Mr Doyle: Those are the sorts of programmes that I deliver daily, because it is the adults who I work with who need them. We are developing the courses carefully and taking our time. We are developing similar programmes with the Northern Ireland Children’s Enterprise (NICE) so that they are appropriate for our target audience.
834. Mrs Hanna: NICE had very good programmes. Its members gave a presentation with Dr Graham McDonald, who was here today, and they have written a book on the issue. Their work is excellent, and they were interesting to listen to.
835. Not all the answers can be found, and perhaps they never will. However, we must try different things that will help some people. Some of the issues relate to self-esteem and people feeling as though they have a meaningful role in life. Some people will search for ever for reasons, but they get no answers. We do not have the answers.
836. However, we will listen to you and to the professionals, and, as John said, we will try to develop a vision of a better way in which to deal with the problem and get the resources to deal with it. It was good to hear from Ann about some of the good things that are happening.
837. Ms McGarrigle: I am glad to have been able to do that.
838. Mrs Hanna: There are some good things amidst it all. Everybody gets frustrated —
839. Ms McGarrigle: We say that west is best.
840. Mrs Hanna: Your work is good, and it gives us all a lift sometimes to hear that some good things are happening. I hope that Bobby, and others like him, hang in there and keep going. Thank you.
841. The Deputy Chairperson: Thank you all for coming along. Your contributions are vital in order that the Committee can create a robust document, which it will present to the Department at the end of its inquiry.
842. You made several points, and, if I have missed anything, you can tell me before you leave. You mentioned a specialist respite centre for children and adolescents and the lack of adolescent beds in general. There is a need to recognise the rural aspect of access of funding and services, and that one must realise that size does not fit all. There must be a collective approach; this is a cross-departmental issue, not one for the Department of Health, Social Services and Public Safety or the Department of Education. Given that this is a social issue, Departments must work together. You also mentioned the uptake of GP training and taking note of the change in our population, with the increase in migrant worker population. That is something of which we must be mindful when taking a strategy forward.
843. The television campaign was discussed, including the fact that suicide was not mentioned in the advertisements. Sue mentioned that we must be proactive in promoting the positive aspects of the work that the families and groups do to help people. The appointment card is another issue. Have I missed anything?
844. Mr McCabe: Self-harm.
845. Ms McGarrigle: Please mention the directory again. I talk about this all the time, but I want to know whether there is any possible way that a directory could be created that people in every area could use.
846. Ms S Ramsey: That should come with a health warning, depending on funding.
847. Ms Ní Chuilín: Michelle, could you also mention the lessons that were learnt from Gerard McCartan’s story.
848. The Deputy Chairperson: Yes. I have that.
849. Mr Cosgrove: On behalf of the families, I thank the Committee for inviting us, for listening to us and for taking on board what we have been saying.
850. Briefly, I will tell you how far we have moved on. Nineteen years ago, my son took his own life. I had absolutely no one to turn to. I went everywhere. I just wanted answers to simple questions to make sure that I was not going insane. No support was available to me. Twelve years ago, Ann’s son did the same thing. Again, there was no support. Over the past five years, the families have made massive changes. It is the families who have made those changes.
851. We do not come at the issue from a professional background; the only hidden agendas that we have are lying in graves. That is where we are coming from. With our hearts and souls, we want to help people through what we went through and to try to make life easier for them. We see the horrors that are happening, and we believe that we can make an impact.
852. As far as I know, our offer to speak at GP training courses in the future has been accepted. We have been fighting for that with different trusts for 18 months or two years. That is at least a small development.
853. Thank you very much for listening to us.
854. The Deputy Chairperson: Thank you.
31 January 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Ms Carál Ní Chuilín
Witnesses:
Mr Colin Loughran |
Action Mental Health |
|
Ms Sharon Sinclair |
Aware Defeat Depression |
|
Ms Suzanne Costello |
Samaritans |
855. The Chairperson (Mrs I Robinson): I welcome Mr Anthony Langan, the public affairs manager of Samaritans; Ms Suzanne Costello, director of Samaritans Ireland; Mr Colin Loughran of Action Mental Health; and Ms Sharon Sinclair of Aware Defeat Depression.
856. Ms Sharon Sinclair (Aware Defeat Depression): I thank the Committee for giving Aware Defeat Depression this opportunity. I know that other Aware representatives have met several members individually, but we provide a range of support and information services for adults across Northern Ireland who are affected by depressive illness and bipolar disorder, and we run a number of mental-health promotion programmes in schools and in the wider community. Our work is very much grounded in self-help principles, and the bulk of it is carried out by volunteers, the majority of whom have had personal experience of depression.
857. Suicide is a recurring theme in our support-group meetings and in a proportion of the calls to our helpline. One of our local facilitators described suicide as “the unseen guest at the table”. Volunteer staff and service users across the organisation have welcomed the Protect Life strategy, not least because it acknowledges and highlights the very strong link between depression and suicide. Those are both complex issues and are, therefore, unlikely to have simple solutions. For us, the vital element in the strategy will be a commitment to long-term, wide-ranging and sustained action on the issues, building on emerging evidence and promoting cross-departmental and cross-sectoral work.
858. The level of stakeholder engagement to date has been very impressive, and my experience has been largely positive, but there is clearly room for improvement in communication and networking and so on, but some of my colleagues will address that matter.
859. I am mindful of the Committee’s wide knowledge of the subject matter and the amount of evidence that it has already taken, as well as the time constraints today. We have already provided the Committee with a written submission, so I will restrict myself to a few key remarks on where we believe the potential for development lies.
860. It has been estimated that only about half of people with depression seek help for their condition. The other half do not even attempt to access services or support. Our service users tell us that the main barrier to seeking help is the stigma attached to mental-health issues, and the consequent fear that they will lose the esteem of family members, friends, colleagues, employers and so on.
861. As a starting point, Aware Defeat Depression believes that a successful suicide-prevention programme will not be possible without significant change in public and professional attitudes to suicide and mental-health problems in general. As we know from the Health Promotion Agency’s public attitude survey, there is still a way to go in that regard. The attitudinal shift that we believe society must undergo needs to begin to be addressed in, or before, the teenage years. Therefore, continued public-information campaigns of the type that have been launched over the last year must be evaluated regularly and remain a core element of the strategy.
862. The potential for the development of public attitudes also needs to be coupled with action to equip people with the skills in problem-solving, conflict resolution and building self-esteem. Those skills can effect a significant change in help-seeking behaviour by those in psychological distress and can help to avoid the kind of progression into hopelessness that will often prompt suicidal behaviour. Again, we feel that such work must begin at school age and on a widespread basis.
863. To appropriately support people at risk, targeted efforts are needed to enhance depression and suicide awareness among professional groups in health, education, human resources, the criminal justice system and so on. In the voluntary and community sectors, those initiatives need to be continued. A commitment to skills development of the kind that we have seen over recent years is equally important so that people can access appropriate training, including depression awareness, mental-health first aid, and ASIST (applied suicide intervention skills training) programmes. In our view, they must remain as part of the long-term strategy.
864. I know that colleagues will touch on service provision, so I will not do so now other than to point out that we see the implementation of the Bamford Review as a fundamental aspiration in this regard.
865. On a broader level, we need to continue to address the wider determinants of mental and physical ill health, which include poverty, low educational attainment and social isolation. We also need to reduce the negative impact on individuals of life crises, such as loss in childhood, family breakdown, abuse and chronic physical ill health, which are factors in suicide. There is a need to increase public awareness and recognition of drug and alcohol problems and their link to depression and suicide. Action is required to seek to reduce alcohol consumption. It is important that everyone’s behaviour — in public life and in the media — emphasises the individual value of all citizens and the importance of strong family and community bonds, which are key protective factors against suicide.
866. The high level of interest in and commitment to mental-health and suicide-prevention issues that has been shown by this Committee and other public representatives is regarded as very positive by our members and service users. After so many years of neglect, people find that affirmative and they feel that it is making a positive contribution to keeping hope alive for people in their struggle against depression.
867. Mr Colin Loughran (Action Mental Health): I concur with a lot of that. On behalf of Action Mental Health, I thank the Committee for the invitation to attend here today and for its involvement in the Protect Life efforts at regional, board, trust, community, and voluntary levels.
868. My organisation has over 40 years of experience in providing services for people with severe and enduring mental-health problems and people with learning disabilities. The neglect of investment in this sector, particularly at community level, has been a big problem in properly addressing the needs of those with severe and enduring mental-health problems. The ‘Protect Life’ document describes such people as being one of the groups at the highest risk of suicide. As an organisation, we applaud Government on their recent investment in mental-health services and we advocate the continuation of that. The Bamford Review should be committed to on a long-term basis and its recommendations should come to fruition.
869. Continuing support for mental health and learning disabilities, particularly at community level, is important. Furthermore, cross-departmental support is necessary to tackle suicide rates and promote suicide prevention. It is not simply a health issue; it spans the spectrum of Government, and it is important that it is not only the Health Committee that shows an interest in that work. Issues such as poverty, housing problems and so on need to be addressed; they are key factors in the full recovery of the people that we serve.
870. Better communication and clarity is necessary in relation to Protect Life, particularly if it is to reach the cutting edge at grass-roots level where people are self-harming or contemplating suicide. It is vitally important that structures are clear and that there is a clear awareness about where the sources of support are. I am aware of models of good practice, which may get mentioned during the discussion. However, even where those models exist, it is still difficult for them to reach everyone. Therefore, a continuous effort is vitally important in order to reach people who feel alone, isolated and unsupported.
871. My organisation supports a focus on preventative approaches. We have seen, and are glad of, crisis response and response to particular events. However, I would like to see a longer-term vision of a healthier community. We must start to build resilience in children — and those who are vulnerable — at an earlier age and end the stigma of taking the pathway to support, which often prevents people from accessing the support that they require at times of distress.
872. Ms Suzanne Costello (Samaritans): I echo my colleagues in thanking the Committee for giving us the opportunity to give evidence. Samaritans is an international charity which has been at the forefront of suicide reduction since 1953. I slightly differ from my colleagues because my position, as director of Samaritans Ireland, is a new one, which was created to help volunteers across Ireland fully implement our projects and initiatives on a local basis. I have been in that role since March 2007 and can offer my impressions as someone relatively new to the area.
873. Samaritans Ireland has 21 branches, eight of which are in the North of Ireland. We have approximately 600 volunteers in Northern Ireland and we deal with 73,500 dialogue contacts, which are occasions of emotional support offered by a volunteer and accepted by a caller.
874. I have paid a lot of attention to suicide in Northern Ireland — when I started last summer, the deaths in Laurelvale and Craigavon focused everyone’s minds intensely. It is heartening that suicide prevention is so high on the agenda of politicians and wider society in Northern Ireland. I have received a very warm welcome for the work that Samaritans does from everyone working in the sector, but in particular from the community groups — there has been a historical difficulty in connecting and establishing where the synergies could exist between community groups and a large voluntary organisation like Samaritans. I particularly acknowledge the help of Mary Creaney and Philip McEntaggart in that.
875. Based on my experiences so far, I am concerned about the duplication and replication of services, the lack of evaluation of initiatives that are started in the community, and the complexity of accessing funding. My point is not about the funding itself, but rather the accessibility of that funding to volunteer-led organisations. They are often faced with 50- or 60-page applications for relatively small sums. That can be daunting for people who volunteers who have signed up to help people experiencing despair and isolation, not to carry out administration.
876. The biggest challenge that Samaritans faces in the community is anonymity, which is a big part of being a Samaritans volunteer — especially in Ireland, as I am sure you will appreciate. In small and rural communities it is vital that Samaritans do not speak about being volunteers in case it prevents someone from seeking help. That presents us with a challenge, because our work is not always acknowledged. Although we are best known for our telephone service, we are accessible by email, and live emotional support will soon be available by text. We work in prisons and have extensive school and workplace programmes. Volunteers are sometimes frustrated that their work is not widely acknowledged. However, we appreciate that it is the nature of our organisation that we do not seek that type of recognition, and we try to balance that.
877. Samaritans can bring two benefits to Northern Ireland. The first is partnership; we use an extensive range of technology and are at the cutting edge of innovation — for example, the text-messaging live support pilot scheme has been very successful. We want to deliver that service as widely as possible in partnership with other organisations.
878. My colleague Anthony Langan has done some work on the other thing that we can bring to the table. As an international charity, we are able to access key groups that are not necessarily available to people working only in Ireland. For instance, on the issue of suicide and the Internet we have been able to facilitate Department of Health officials to directly meet key people in the large Internet service providers to tackle the specific difficulties that have been so prominent recently, and we would very much like to continue that.
879. The Chairperson: I am delighted to meet you, Ms Costello. I have been using your good services for one of my constituents. I cannot praise enough the efforts that your organisation has put in to that constituent, who has a problem with alcohol abuse.
880. The key to this issue is stigma, and, having had depression at one time in my life, I take it all very seriously. Two psychiatrists are working with me on a part-time basis to see the workings of the Bamford Review roll out.
881. Mrs O’Neill: Thank you for coming to talk to us; it helps us as we go through the inquiry. Ms Costello, you spoke of duplication, and we have also heard that from other groups. We have heard concerns about the establishment of the Department’s phone line, and in your submission you said that the Samaritans is progressive and have had a phone line for a number of years. Do you feel that the Protect Life strategy creates unnecessary duplication, especially with the phone line?
882. Ms Costello: There is duplication in certain areas. The phone line that is to be rolled out in the next couple of months has aspects that our service does not provide, but there are significant areas of overlap and there could be better synergy if we were able to work more closely with the Department. There would also be a cost saving. Although cost is not the principal factor — that is the delivery of a valuable service at the right time — the costs must be borne in mind if we are to achieve long-term sustainability, which is absolutely vital. It is important that the services are still in operation in 10-15 years’ time. As we are working all the time on public awareness and removing the stigma from depression and suicide, it is important that people know where to seek help.
883. Mrs O’Neill: As an all-island charity, do you feel that you are more involved with the strategy in the South than you are here? Can lessons be learned from your involvement there?
884. Ms Costello: I am loath to make comparisons. The South has a different structure in that it has a National Office for Suicide Prevention. Therefore, there are three or four individuals who form the point of contact for every aspect of suicide prevention, making the process swift, flexible and clear. Everyone has access to those key individuals, whether a small charity in a rural part of the country or the larger charities. From that point of view, it is a fair and transparent process.
885. Dr Deeny: You are all very welcome, and I applaud the work that you do. I like being on this Committee, because it impacts on the work I do — I have been a GP for over 20 years. I am sure that you know that, of our consultations, around 30% are [Inaudible].
886. I divide health into three areas. I notice that your document refers to emotional health, and that is very important. To me, the concept of emotional health means happiness, contentment and peace of mind. If a person’s emotional health is good, their mental health and physical health tend to follow. As a GP, I find that people who are emotionally unwell sometimes end up with full-blown clinical depression.
887. Some years ago, I used to have leaflets from Aware Defeat Depression — which was then called Aware — in my surgery, and I directed people to that organisation. I work close to Omagh in County Tyrone, and it would be a good to idea to keep GPs such as me in tune with your organisation. Does Aware Defeat Depression still hold local meetings?
888. All the charities that are represented here are involved in the talking therapies, which is important. Conventional medicine is deficient and is failing the public in that respect. I have seen many people who I know, if they could talk about it, would — particularly young men. I have seen suicide before in my patients and their families. It is devastating; I know of one family that has gone to pieces. That might have been avoided if he had been able to speak to someone. In my opinion, the National Health Service is failing with regard to the talking therapies.
889. Openness about mental health is important and must be encouraged. In Northern Ireland, more people are talking openly about mental-health problems on television and radio programmes, and it is good for people to understand that talking is better than worrying. I have told many people who are depressed about their lives that they can recover.
890. Ms Costello, you mentioned bureaucracy, which sends a shiver up my spine because GPs are inundated with forms for this, that and the other, and it drives us round the bend. Surely to God, there must be some way that the Committee can help to ease the bureaucracy that holds back people who are trying to help those with mental- and emotional-health problems. It is ridiculous that time that would be better spent attending to people’s lives is taken up by filling in 60-page forms. Do you feel that there are any bureaucratic areas that we can help you with?
891. Ms Costello: We raised that issue at the last suicide strategy implementation body meeting and got a positive response. Structures are in place for us to apply for funds regionally. My role is to take the pressure off volunteers, allowing them to concentrate on providing the helpline service. If we can access that regional funding mechanism, the volunteers can be relieved from administrative fund-raising duties, which they find daunting and which, in many cases, is not very fruitful.
892. Dr Deeny: And the leaflets?
893. Ms Sinclair: Aware Defeat Depression was involved with the Health Promotion Agency in the design and delivery of the depression-awareness training programme for primary-care providers. As a consequence of that programme, each GP practice in Northern Ireland should have received a stock of our ‘Depression: The Facts’ publication and a general leaflet about our services. If they have not arrived at your practice, I will follow up on that. Hopefully, those leaflets will be supplied annually.
894. The evaluation from the GP training programme showed that GPs want access to good, straightforward, user-friendly information about depression that they can give to their patients and information about services for their own benefit, and we are committed to providing such information. In our organisation, we often say that people with mild or moderate depression are either at their GP surgery or at home, and those are the places in which we must connect with them. I will check up on those leaflets.
895. Dr Deeny: Are Aware Defeat Depression’s clinics convenient to most areas?
896. Ms Sinclair: At any time, we have about 20 support groups in Northern Ireland. Currently, there are 23, and there are active groups in the Omagh, Cookstown and Magherafelt areas. I will supply you with specific information about that.
897. Concerning talking therapies, it is one of our policy aspirations for people with mild to moderate depression to have better access to cognitive behavioural therapy, because evidence-based research shows that that helps in the recovery process.
898. In addition, we have developed, and are in the process of piloting, a six-week, structured-workshop, group-education programme with the Northern Ireland Centre for Trauma and Transformation — based in your hometown of Omagh. That programme imports the best cognitive behavioural therapy principles into group support sessions. [Inaudible.]
899. The Chairperson: On the heels of that, Sharon, it is worth remembering that there are 108 MLAs, and each party has two or three offices in each constituency. Our offices have a high footfall of people with big problems. It might be helpful if packages of leaflets were to be sent to all our advice centres, which are listed in the telephone directory. In my office, there is a display of all types of information, but, sadly, I have nothing that gives direction to people who need that sort of help. That is one area that you could consider.
900. Ms Sinclair: I am aware of the funding difficulties, because I have had some experience of having to submit many funding applications for fairly modest amounts of money. One of my staff refers to that as “dear money”, because the effort required to access it costs more to the organisation than the sum received. Therefore, we are very pleased that the implementation body has agreed to examine regional organisations that deliver a comprehensive service throughout their region and that the key people will facilitate the progression of a regional strategy that will allow people to put more of the scarce resources into front-line services.
901. Mr Easton: My first questions are directed at Sharon. Correct me if I am wrong, but I think that you said that a suicide strategy will not be successful unless we change public attitudes. You went on to talk about society letting its children down. Why do you feel that there were fewer suicides 10 years ago, and what is causing the current trend? Why does it seem that people coped better years ago? You also mentioned alcohol and drugs, both of which can contribute to depression and suicide. We hear about stand-alone units, and the Committee visited the small one at Antrim Area Hospital, which seems to be successful. What more would you like to see being done in that area? Perhaps we have not explored that as much as other areas.
902. My final questions are directed at Suzanne, because the Samaritans runs a depression helpline. Do you think that the proposed 24-hour helpline should deal with issues other than suicide? For example, should it extend to depression and other mental-health issues, or should there be two separate helplines?
903. Ms Costello: I can respond to that question straight away. It is a massive undertaking for the group that will run the new Province-wide helpline. What it is trying to achieve should not be underestimated. Running a 24-hour helpline of any sort is extremely difficult. The majority of calls to the Samaritans come between 10.00 pm and 2.00 am. As you know, the Samaritans is staffed by volunteers — people who feel very passionately that they want to help and that they are making a difference. That is what spurs them on to sit there at 2.00 am, 4.00 am and 5.00 am, which is not easy. They genuinely believe that they are having an impact, and that is why they do it.
904. I am not desperately familiar with the new helpline, but, as I understand it, it will have many facets. I understand that counselling will be suggested to people, calls will be followed up — perhaps the staff will ring a person back, having made a call or a counselling appointment — and callers will be taken right through the process and put into counselling, if that is appropriate and if that is what they want. In that sense, it will be directional. That is somewhat different to the service that the Samaritans offers.
905. The Samaritans is best known for suicide reduction. If you were to ask people in the street about us, they would say that people who are suicidal phone the Samaritans. In fact, people call us for a range of reasons across the emotional-health spectrum. About 20% of the callers to our helpline are actively suicidal. We would place the remainder of people somewhere between good mental health and serious despair, but we actively encourage those calls, because we consider that as early intervention.
906. Ms Sinclair: The attitude of the public is crucial in creating the context that enables people to seek help, because one can develop gold-standard services and support, but if people feel that they will lose esteem by being seen to use them then you are putting the cart before the horse. Statistics from the Health Promotion Agency’s public-attitude survey showed that 54% of people in Northern Ireland said that if they were experiencing a mental-health problem, they would not tell anyone about it, which is the reverse of what we are trying to achieve [Inaudible].
907. I am loath to proffer an explanation on suicide trends, because there are differing views on the causes, ranging from geography, age, gender, and so forth. One theory is that the pace of change in human development is so rapid that psychologically, and often physically, we have to run much faster to keep up, and when people have difficulty adjusting to that speed, it can have a negative impact on their emotional well-being. However, with any depression or suicidal tendencies, there is a complex series of factors at play, including low self-esteem, early-life events in childhood and social determinants such as poverty, ill health and educational attainment, which have impacts on communities and individuals.
908. Mr Anthony Langan (Samaritans): There is a key role for coroners and the Coroners Service for Northern Ireland in the strategy, both in the recording of deaths in a standard way and also in identifying trends by passing information on.
909. The Chairperson: Representatives from the Churches will be giving evidence to the Committee next week. They have a major role to play, and I am looking forward to hearing from them.
910. Mr Loughran: Those involved in investing in health in the Southern Health and Social Services Board area commission small grants to local organisations. Work was done with the Churches in Dungannon to raise the profile and need for support, because when suicide occurred and people turned to a Church for support, it was not there. Church representatives are involved in some of the work that I undertake in the voluntary and community sector, and they need help to understand what support they can give when presented with mental-health needs and also what support is available to them. A wide range of organisations and religious bodies can offer support, which is encouraging, but it is at an embryonic stage.
911. The Chairperson: Some Churches have their own Christian counselling services, which is tremendous. We must welcome everyone working together.
912. Ms Ní Chuilín: Anthony, you mentioned the Coroners Service and the reporting of statistics, and NISRA has been mentioned in connection with deaths through MRSA and C difficile. Years ago, people ended their lives, but suicide was not recorded on their death certificates if the family did not want it to be. I know that there have been different ways of reporting deaths over the years, but there is still anecdotal evidence that suicide is not reported as much as it is happening. What are your thoughts on that?
913. The Samaritans produced good guidelines on reporting suicide through the media, which I meant to bring to the Committee. Can the Committee have a copy of those guidelines? In north Belfast, where I live, a couple of people ended their lives a few years ago, and some of the media coverage bordered on being grotesque. Those families lived just round the corner from me, and, as an elected representative, I felt that it was almost as though the media were trying to sensationalise the grief that those families were experiencing.
914. When I saw the guidelines, I quite happily went to almost all the editors involved, although that had already been done by the Samaritans. Since then, there has been a difference, even in the way that questions are asked. However, that may all depend on whether the papers are local, because they would report local issues more sensitively. A national paper with a wider circulation may have some sensitivity but not to the same extent. We all have a job of work to do in that area.
915. I would like your thoughts on coroners and how the Committee should approach that issue. Are there any updates or ongoing work with media outlets, because the media affect the way in which families are allowed to grieve?
916. Mr Langan: The Samaritans had hoped that there would have been a coroners Bill in the Queen’s Speech. Unfortunately, that did not happen, but we are pushing for such a Bill in the next parliamentary term, if possible. We are working with the Ministry of Justice and the Department of Health in England to change the rules for coroners so that they have a remit to identify trends in deaths, and we want to carry that work over into Northern Ireland.
917. We want standardisation of reporting. There must be training for coroners and the Coroners Service, so that they understand the implications and how to work with families in the recording of deaths. There should be some balance and sensitivity about how families feel. However, we will never learn from those situations unless we begin to record those deaths properly.
918. I sent copies of the media guidelines to the Committee Clerk, and I hope that members may have seen them. We will continue to work on improving those guidelines. We have been successful in working with the Press Complaints Commission in England to improve the code for editors on reporting of suicides, and we hope to extend the voluntary uptake of that code. We will be examining new media guidelines some time this year, and we will also consider the issue of new media and the Internet to explore how we can build in some guidance for people making use of those services.
919. Ms Ní Chuilín: We have received the guidelines.
920. Mr Langan: We can make the guidelines available to MLAs through our branches.
921. The Chairperson: That would be very helpful, because we all face that dreadful situation.
922. Ms Costello: I do not know whether the Committee is aware of Headline, which was formed recently. It monitors the media for irresponsible reporting of suicides and mental-health issues. There are moves to have Headline operational in Northern Ireland. There were some horrendous breaches of the guidelines after the suicides of two young men in Omagh last year. The difficulty for charities taking up those breaches individually is that they are subsequently penalised by the papers, and it becomes very difficult for an individual charity to take that on. Headline comprises a group of charities and people working in the mental-health and suicide-prevention field who feel that when problems are tackled as a group, its voice is much stronger.
923. Ms Ní Chuilín: I had occasion to complain about an editor when the media were saying that it was not good enough that the person ended his or her life. The media were asking the entire community a list of horrendous questions, particularly when a cluster of young people had ended their lives — copycat suicides. Committee members are subject to reporters asking really bad questions that they do not expect. It is hard enough for us to field off those questions, but it must be much harder for people without such experience.
924. The establishment of Headline is a good move, because it means that no one person or group will be left vulnerable, and there will be confidence in being part of a collective.
925. Ms Costello: We have run some awareness-raising workshops. The media and people who are involved in the charity are aware of copycat suicides, but the wider public are not. If they were aware of that factor, they would possibly shun the type of coverage that they see. Therefore, it is important to get that message across.
926. Mr Loughran: We developed working relationships with eight editors in the Southern Health and Social Services Board area, because the mental-health promotional material that we sent out under our youth programme — AMH MensSana — was not being reported at all. The articles were well written, and they provided good information and sources of support that we thought would be useful. However, they were not effective, so we decided that the only way to get the message across was to go out and nurture relationships with editors. That has been a long, sustained piece of work, which must continue, or it will fall. Unfortunately, however, when those editors move to new posts, we must start the whole process again
927. Ms Ní Chuilín: The situation is different in cities.
928. Mr Loughran: There must be a strategically sustained focus on the media. Last week, the ‘Belfast Telegraph’ inaccurately reported a recent suicide, according to guidelines.
929. The Chairperson: We need to keep on top of that issue.
930. Mrs Hanna: The Mind your Head television advertisement was good in addressing the stigma attached to mental health, which is a huge issue. The advertisement showed a high-profile woman admitting that she had a mental-health problem. People will admit to many things, but they will not admit to being unable to cope.
931. I agree with you on the bigger societal issues — talking about the wider determinants and the risk factors. Sharon and Colin mentioned the importance of models of good practice. In our anti-poverty strategy, we must get into the details and consider narrowing the gap that is widening all the time. We must also start to measure where we are making a difference in our strategies, such as the drug and alcohol abuse strategy, rather than simply producing glossy brochures.
932. It is important to address the issue of duplication, because we want the best service and the best cover, with models of good practice to ensure that things are being done correctly. When people contact the helpline, volunteers must be trained to address issues such as talking them through the problem or signposting them on. If someone needs help there and then, volunteers need to know whether they could be referred until the following day or whether they should be kept on the line. There are many issues to be addressed so that the best care can be provided for those people. People must work together. There is no point in phoning one helpline and getting one piece of advice, and phoning another helpline and listening to an answering machine message telling them that someone will talk to them tomorrow. The issue must be addressed by professionals.
933. Sharon mentioned the level of training. We have heard about the ASIST programme, but psychiatrists need to have an input to ensure that the training is appropriate. It is great that much work is going on in the voluntary and community sector, but that must be measured to ensure that there are models of good practice and that services are not being duplicated. If someone is really desperate and phones a helpline, best practice is essential. I agree with the societal issues involving families, Churches, better parenting programmes and early-years programmes, and I understand the economic argument. There should be upfront measures to prevent those problems rather than picking up the pieces when the problems arise.
934. Mr Loughran: There is great determination in the voluntary sector for much of that work to be done. Action Mental Health certainly advocates the need for resources. We are in a position where we can signpost people on. However, I would urge caution that organisations are not overstretched before additional resources are available. Organisations such as Action Mental Health work to capacity, whether through direct contact with our client group or through AMH MensSana service in mental-health promotion. It is important that resources are available.
935. Ms Costello: Everyone is in a similar situation. All Samaritans volunteers undergo a rigorous training programme. The charity has psychiatrists and psychologists involved at every level: in trusteeship, policy, training, research and best practice. There is a rigorous system of training and checking. For example, in individual branches, when a caller needs help, a psychiatrist is involved in taking the decision about how best to react.
936. Mrs Hanna: It is important to evaluate that training and to ensure that everyone is trained to the same standards.
937. Mr Loughran: An evaluation has been completed for the Southern Health and Social Services Board area. ASIST was evaluated as a part of that. The indications are that ASIST is appropriate and helpful to front-line practitioners, but, for the general population, it may not be the most effective source of training. Something pitched at a lower level, aimed at a general understanding of mental and emotional health, would be more effective for the wider public.
938. Mr Buchanan: Sharon spoke earlier about her work with schools. How are you received by the pupils? Are they prepared to admit that suicide is a problem? Will they talk about it? Do you work with social workers? Social workers deal with families at early stages, perhaps in cases of child abuse. When a child becomes a teenager, that earlier abuse can lead to depression and suicidal tendencies. Do social workers who work with children who may have been abused follow up their work to check whether the abuse has led to suicidal problems?
939. Ms Sinclair: In schools, Aware Defeat Depression runs a depression-awareness programme for young people between the ages of 14 and 16. It aims to alert them to the signs and symptoms of depressive illness, to highlight the importance of help-seeking behaviour and to indicate the ways in which they can improve their emotional health. The programme is generally well received by young people. It is delivered by young facilitators; 14- to 16-year-olds think that anyone aged over 25 is ancient. We use facilitators who are in their mid-20s so that there is a higher degree of empathy.
940. The programme has been externally evaluated a number of times, and we now have longitudinal evidence about how well the pupils take the learning on board. That yields interesting information on the need to build skills, and so on. We find that, after 12 to 18 months, a high percentage of young people — more than 50% — remember the key signs and symptoms of depression. They remember what should be done to try to improve mental health and the importance of seeking help. However, a substantial number say that they would not necessarily take the step of asking for help. Therefore, pupils take the information in, intellectually, but they do not necessarily translate that into behavioural change. Much work needs to be done in developing skills; but the programme is generally well received by young people and schools.
941. It is not marketed as a suicide-prevention programme; it focuses on the development of positive mental health and recognises that depression is the main source of mental ill health. We advise young people that depression is the most likely form of mental ill health that they are likely to experience in adulthood, whether it affects a family member or someone in the wider community, and so on.
942. Mr Loughran: It is more important that schools address the issue rather than simply children recognising it. I am involved with AMH MensSana, which, like Aware Defeat Depression, has a programme for post-primary young people up to the age of 25.
943. It used to be difficult to get into schools because teachers were afraid of the consequences of recognising the issue. However, there has been a significant increase in the number of schools that are prepared to allow organisations with expertise to conduct sessions and support their pupils. That is what I was referring to earlier when I mentioned cross-departmental support. Such issues need to be embodied in the Department of Education, and schemes need to be progressed and embraced.
944. My son is in the process of choosing his secondary school, and we have been visiting the various schools. I have been encouraged by posters, and so on, around the schools that identify sources of stress for young people, which may lead on to more prolonged and enduring mental-health problems. That was not the case when I was at school; those types of issues were not discussed. The existence of pupil support workers is an excellent development.
945. The Chairperson: Our time is almost up. I will refer briefly to the judicial system, which is an issue that we have not yet discussed. A number of my constituents have looked to the judicial system for help after suffering as a result of incest. Often, as people get older, such issues come to light, and they discover that their siblings have also been interfered with. If the judicial system lets them down, they feel that there is no hope and that they are not going to get justice.
946. In a recent court case, an offender received a sentence of two years and nine months for interfering with two young girls aged five and six. The judge made a comment that he did not think that the children would be adversely affected. I went on ‘The Stephen Nolan Show’ — although I sometimes question whether I should — and absolutely berated that judge for his attitude. I pointed out that the lives of those five- and six-year-olds could be destroyed: they may be unable to have relationships later on; they could become suicidal, alcoholics or drug addicts; and they may flit from relationship to relationship because they cannot settle down.
947. I threatened to go to the Lord Chief Justice to raise the issue of sentencing; he later phoned me and invited me to visit him at the Crown Court. He said that the judge’s comments were regrettable. He explained that judges have to tick boxes and that if offenders meet certain criteria, they receive a shorter sentence. He also pointed out that 50% remission is still granted. Therefore, the legislation that governs the judicial system restricts the sentences that judges can give.
948. However, victims often find it difficult to face the fact that the offender will be released in a short time. Victims simply have to get on with their lives, even though they are left scarred — mentally, physically, and so on. They often feel that they have been let down and that their only recourse is suicide, which is a dreadful situation.
949. Therefore, the judicial system and the issue of 50% remission in Northern Ireland also have to be considered in order to address the issues of suicide and mental-health problems.
950. The Committee Clerk: Recently, I was the Committee Clerk for the Ad Hoc Committee on the Draft Criminal Justice (Northern Ireland) Order 2007. As soon as that Order is introduced, there will no longer be automatic 50% remission. It will no longer be unconditional, but it does not apply retrospectively.
951. The Chairperson: That is right. That is the problem. I just wanted to highlight that issue, because I am very concerned about it.
952. Thank you all for making the time to come along; it has been really worthwhile and very interesting to hear your views. I wish you all well in the difficult work that you have to do. No doubt we will see you all again.
31 January 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Ms Carál Ní Chuilín
Witnesses:
Mr Mike Tomlinson |
University of Ulster |
953. The Chairperson (Mrs I Robinson): I now welcome Mr Mike Tomlinson of Queen’s University Belfast and Mr Iain McGowan of the University of Ulster. You will have five minutes each to make an introductory presentation, which will be followed by questions.
954. Mr Mike Tomlinson: I thank the Committee for allowing us to give evidence and for taking an interest in this subject. I am not here on behalf of Queen’s University; I am here because of research that I conducted personally, and which was commissioned as part of the suicide prevention strategy. The Department asked me to take an overview of established research evidence about the relationship between our conflict — and war in general — and suicide. What evidence do we have to show that what we are dealing with in relation to suicides is past trouble? Are there legacies that, in some senses, explain what appears to be an increase in trends? I am pleased to table that report and to be able to come here to present it.
955. The report is wide-ranging and deals with global trends, international and domestic conflict situations, and a variety of consequences of conflict situations. Some of those have already been touched on today, such as child abuse and the impact of sexual violence on women, and how that, in turn, translates into poor mental well-being and can result in suicide. My memorandum simply highlights some of the key points from the research that I think may be of interest to the Committee, particularly in its examination of the suicide prevention strategy, Protect Life.
956. I was particularly interested to hear discussion focusing on the data on suicide and the processes that produce the figures that we all depend on to shape our basic understanding of what is going on in society. Much of the report deals with those issues. I do not intend to talk very much about the data and the processes of recording and registration. However, when it appears that the suicide rate is getting out of control, it is worth reminding ourselves that the last set of figures produced by the Northern Ireland Statistics and Research Agency (NISRA) registered 291 suicides for 2006. Only 72 of those suicides actually occurred in 2006. I am quite prepared to believe that there were more than 291 suicides in 2006, but we will not know whether that is the case for at least another two years.
957. It is important for the Committee to focus on what is happening with processes of registration and recording. Everything that has been said so far about the role of coroners, the reporting structures, the early warnings, how that information gets registered and the delays in the system is very important. We must move towards the Scottish system, whereby an approximate figure is published much more quickly, which gives a much better sense of the real trends.
958. At the moment, our understanding of changes in trends comes from the experience of communities, which is why I remarked on the importance of funding the groups that support parents and communities. Very often, the politicians and community representatives are the first to hear about suicide. NISRA is the last to hear, in a sense. That involvement provides an important detection service. Nonetheless, we could improve the data to develop an early warning system about what is going on, not just in terms of prevalence, but also the age groups that are affected, broken down by sex and so on.
959. Much of the work in my report is not useful as regards front-line prevention activity. It is not about psychiatric interventions or explaining people’s psychological states of being. Rather, it focuses on the evidence on social circumstances, social structures and social change, all of which can lead to poor mental health and contribute to suicide rates. The report is pitched very much at a level that involves the kinds of factors that the other groups have mentioned today — for example, prevention, and an understanding of the issues that contribute to depression. There is very good population-based evidence to show that people who were closest to the conflict — who either were in the front line or lived in communities where they witnessed murders, shooting and mayhem, or who were personally affected by bereavement, injury or disability — have much poorer mental health than others. That is a very important starting point in any effort to move forward and deal with some of the legacy of the past.
960. Finally, it is not easy, or, in fact, possible, to distinguish completely between Troubles- and non-Troubles-related effects. That is simply impossible. We must accept that those are the circumstances in which we have lived and which have shaped our society: we must deal with that in whatever way we can.
961. Mr Iain McGowan (University of Ulster): Thank you for the invitation to address the Committee. I am present on behalf of the dean of the faculty of life and health science, Professor Hugh McKenna.
962. I will briefly explain my background and why the professor has asked me to be here. Ten years ago, I qualified as a mental-health nurse. I started work in the Mater Hospital in Belfast and was fortunate enough to set up and run its Assert (action on suicide, support, education, research and training) project. It was a fairly well-evaluated and successful project which operated primarily in north and west Belfast. I joined the university in 2002. During the 10 years that I have worked on suicide, the vast majority of my research has been on suicide in Northern Ireland.
963. I am currently working with Professor Marlene Sinclair, who is professor of midwifery research at the University of Ulster, on a book for midwives that examines suicide during pregnancy and the first post-partum year. That is currently being developed. Recently, I have also been invited to join a Europe-wide group of academics who seek to understand suicide in areas that are experiencing, or have recently come through, conflict. The group includes colleagues from Serbia, Bosnia, Kosovo, and Israel. We aim to develop that international group on suicide in conflict areas.
964. I will not go through my written submission. However, I will refer to three points, if I may. The first salient point to come through is the idea, which was referred to earlier, of the complexity, multifaceted nature and multidimensionality of suicide. My colleagues and friends Dr Paul Miller, who gave evidence to the Committee in July, Dr Philip McGarry, who gave evidence in October, and, I believe, Dr Deeny, have all pointed out that suicide is not simply a mental-health issue. To a certain extent, even though there is recognition that there are multifaceted underlying causes of suicide, the discussion always seems to return to mental-health services. We want that discussion to be widened.
965. I was heartened to hear Mrs Hanna talk about the anti-poverty strategy and the effect that poverty can have on an individual’s choice to take his or her own life. It is very much my belief that the causes of suicide are wider than mental health. The ongoing research that the university has presented has been along the lines of how analytical chemistry — examining hair fibres, and so on — could be used. One of my supervisors is a theoretical physicist. Through my PhD, I seek to determine whether some of the models that are used by theoretical physicists can be transferred across to the study of complex human behaviour. There is wider scope for study than just the consideration of the mental-health aspect of suicide.
966. Talking therapies have been discussed previously. It is to be welcomed, although, again, not necessarily for the sake of therapy and for being seen to provide something: it must be relevant to the individual’s needs and appropriately resourced. We have suggested other therapies in our submission. Several of my colleagues and I — Dr Derek Loughlin, Dr Paul Miller and Dr Michael Patterson — are currently putting the finishing pieces to a case study on psychological therapy for trauma and eye movement desensitisation and reprocessing. A side effect for one individual who was working through her trauma is that she stopped cutting herself. We are writing that up as a case study, because it was an unexpected bonus. There must be an innovative approach when we seek to develop the type of services that we can provide.
967. There has been a lack of local academic input into the suicide prevention strategy. As far as I am aware, no one from any of the three higher education institutes was a member of the strategy group. We accept that there were eminent academics and suicidoligists providing quality assurance, but it would have been useful to have had someone with local knowledge as a member of the group.
968. Dr Deeny: I am interested in this subject. It has, quite rightly, taken up much of the Committee’s time. Mr Tomlinson, Committee members and the Chairperson have all referred to the responsibility on doctors to record accurate information on death certificates. Due to the stigma, even after death, relatives have asked me not to register suicide as the cause of death. As Carál mentioned earlier, they do not want depression or alcoholism put down as causes. It is almost as if the family still, even after death — it is shocking. It is something that we are going to have to face up to as a society.
969. I agree with Mr McGowan; I have also come across situations where I could not honestly say. I am delighted that you said that. We have mentioned before how important it is for education facilities to be involved. I am shocked to hear that there was no higher education involvement in the strategy. Schools and churches must also be involved, because suicide affects our entire society.
970. I have been working in the Health Service for a long time, and it seems to me that the older generation were able to cope much better. Perhaps they had it harder, and were more used to dealing with hardship. People now seem to find it extremely difficult to cope. I will not mention any names, but there was some young fella from in and around these parts whose brother committed suicide in the past week. He could not get over breaking up with his girlfriend, but relationship break-ups have been going on since time began.
971. Are we all at fault, providing too much for young people, so that they cannot cope when anything goes wrong? I wonder whether I am as guilty as everyone else in that as society becomes more affluent, we provide more and more for young people, and they get everything that they want. Do we spoil our kids, so that when they grow up they have not been used to hardship and cannot cope when they encounter it? I am interested in your views on that.
972. There are Church representatives due to appear before the Committee. Is the message not getting through to young people that life is precious? As I said earlier, I have seen the effects of suicide on the families who are left behind.
973. Mr Tomlinson: The traditional age profile of suicide in most countries has been that the highest rates of suicide are among elderly people: the further up the age range, the higher the prevalence of suicide. Therefore, I do not know whether it is a question of people becoming less resilient. The global trend suggests that suicide rates are increasing in some parts of the world. That is partly explained, as in Northern Ireland, by greater prevalence of suicide in the younger age groups.
974. However, it does not go down that far. There is a tendency to focus on teenagers and the horrendous tragedy of 10- to 14-year-olds committing suicide — and I made the point in my submission that there is evidence of a trend. However, the basic pattern is that elderly people are most likely to commit suicide.
975. I want to make a broader point about concealment and revelation. Some people, particularly the closest relatives, have a propensity to want to conceal suicide, and they want it to be turned into an accidental death, through poisoning or whatever. The data shows a direct association between suicides through poisoning and accidents through poisoning. Therefore, there is a relationship that is to do with exactly the phenomenon that you are talking about.
976. There are certain social circumstances in which a lot of publicity has been given to the tragedy of individual cases. The very idea of suicide was unknown to me until I was 18 years of age, but now there are kids of 11 who understand what suicide is. We must ask: where does that idea come from? Where are they getting this concept? Who is reproducing it, and who is giving them ideas about how to put the idea into operation? Those are very relevant questions.
977. We have talked about the media. We must make use of all the new forms of communication that are available to young people these days, such as texting and Internet chat rooms. We do not know the half of it when it comes to the ways in which young people transmit ideas within their youth clubs, schools and peer groups, and internationally, in chat rooms and so forth.
978. Much of this is to do with the ideas that people have and the stigma that may or may not be attached. The trends reveal some interesting information. As communities become more emboldened in explaining suicide among their closest relatives in terms not of family dynamics but of the legacy of conflict, they are more prepared to come out and say, “That was suicide, it was not my fault”, recognise it, register it, and even campaign for more mental-health services. I am trying to make a point here: the social and political circumstances shape the willingness of individuals to come out about suicide — there are processes of concealment and revelation, which change according to social circumstances.
979. Chairperson, you made a point about the Churches’ role in this subject. If suicide is illegal, if it is a sin, if you are not going to get a burial, and if you are going to have your goods and chattels taken away from you, then that is not conducive to admitting that a suicide has taken place in your family.
980. The Chairperson: Absolutely. I could not agree more.
981. Mr McGowan: I concur with Mr Tomlinson. However, there is another issue around stigma. It may be that an individual who feels like taking his or her own life, or makes an attempt to do so, does not seek help because of the stigma. That is the other side of the coin; the family of that individual says that it does not want the stigma. If that individual feels suicidal and is looking for a way out, but cannot do so because of the associated stigma, perhaps it is time to examine some of the more innovative interventions. If you turn up at an accident and emergency centre and say that you are suicidal, you will be assessed by a healthcare professional who will determine whether or not that is the case. If you say that you do not want to go into hospital, you are likely to be detained. To go back to my original point, it may not be just a mental health issue, and that intervention may not be the most appropriate one. The stigma has something to do with it, but it must be addressed in the overall context of how we provide help and support for people who feel vulnerable.
982. Mr Tomlinson: People who are determined to kill themselves will do so. However, there is a group of people who are determined to kill themselves, but it turns into a cry for help. They do not succeed, and they are very glad of that. There are some people who self-harm quite seriously — to the point of being hospitalised — who never really intended to carry it through; that is also a cry for help. There is a whole spectrum of behaviours, but, for the most determined, it is too late. They should have been helped years and years ago in order to interrupt that process and that determination. If one is really determined to end one’s life, one does not talk to anybody — one just does it. That is what is so distressing about —
983. Mr McGowan: Mike made some good points. Perhaps this is an appropriate point at which to make the Committee aware that Professor Hugh McKenna, Dr Joanne Jordan and I are currently working on the research and development of a funded project at Queen’s University Belfast. The project examines the service needs of young men in the four groups that Mike has outlined. They include: groups that are engaged in services; those who have engaged in services and have dropped out; those who engage with voluntary services; and those who have not talked to anyone but who are suicidal. I hope that some of Mike’s points will be addressed through our research findings.
984. I disagree with Mike that people who are intent on taking their own life do not necessarily communicate with other people. I accept that they may not outwardly say to someone that they are thinking of taking their life. I would argue that — from my experience of working with people who are suicidal and who access psychiatry, from reading and from my own work — that, in some way, shape or form, they will communicate their intent. It may be communicated by their returning gifts or returning items that they borrowed two or three years ago, after the original owner has given up on their return. Then suddenly the object is returned. Why has the object been returned, and why has it been returned now?
985. A case study has been published — and I am happy to provide the Committee with a reference to it — of a girl who borrowed a kettle from a friend. The original owner had considered it as lost. However, the kettle was returned 30 months later. The girl said that all she really wanted, at that time, was for someone to ask her why she was returning the kettle. Unfortunately, the friend was busy and simply thanked her for its return. Fortunately, the girl survived that particular suicide attempt. Subtle changes such as that can communicate that, perhaps, something out of the ordinary is happening.
986. The Chairperson: There are also cases where people start to explain their endearments — such as “I really do care about you” — and telling the children that, whatever happens, they care passionately about them.
987. Ms Ní Chuilín: There is a saying that suicide is everyone’s business. It is not simply a matter for health professionals. That view is supported by the Bamford Review — which was cross-departmental — which examined issues that affect people with mental-health needs or learning difficulties, because those groups are particularly vulnerable. Older people were included in those groups.
988. During the Committee’s visit to the Scottish Parliament, an MSP who represented the Lowlands said that there is a high incidence of suicide among doctors, vets, farmers and older people. Perhaps we do not know enough about those older people, because the media can more easily sensationalise the deaths of younger people. Most deaths of older people by suicide are not reported. During the past 30 years, people stuck together and worked together. They had to live, work and survive, despite what was happening around them. When those times ended, the survival instinct started to erode.
989. People become older, and families are displaced because they cannot afford to buy a house. All those issues matter. People move away and communities are broken up, which is quite different to how it used to be. Most of us no longer live cheek by jowl. When one speaks to older people about anything — perhaps they are complaining about something — they often recount their entire life experiences. Although one knows that they are vulnerable once one leaves their home, those people will never say that they are vulnerable. Therefore, it is not simply about stigma but pride.
990. The Bamford Review refers to living fuller lives. However, C difficile has affected many older people. The attitude seems to be that older people are affected, but they are sick, anyway. An attitude and a culture exist in which only services for younger people, such as youth clubs, teachers and parenting, are considered. In my community, young people do not go to Mass unless they are dragged there. Older people do go to Mass, but they do not get the comfort that they expected. They realise the stigma, which relates to a time when people died in questionable circumstances, no candle was lit at the altar and they were buried in unconsecrated ground. Older people know all that, but it is still hard for them to access services. Therefore, how will a person who is depressed and has come through a lot go about accessing services that they feel are appropriate to them, most of which are not available? How will they be able to talk about how they are feeling when they are proud and do not know how to describe their feelings? Many more services and initiatives are directed at younger people.
991. It is easier to cover up the deaths of older people by saying that they did not end their own lives or that they died through a mistake because they were doting. If an older person took an overdose, it might be described as being unintentional. From talking to colleagues in Dublin, I know that until the National Office for Suicide Prevention was set up and specifically considered the issue of the deaths of older people not being reported, such deaths were always viewed as mistakes, and suicide was never viewed as being intentional. A job of work must be done on that issue, and as you are involved in research, that is your bread and butter. The social aspect must be examined.
992. I was reared to look after my neighbours, and they would look after me. I have great neighbours of all ages, and if I had not seen one of them for a couple of days, I would knock on their door, because that is the way in which I was reared. My neighbour is grand; she has a big family and is very lucky. However, the break-up of communities definitely has an impact on older people, as does the lack of available services.
993. The removal of centres offering advice on welfare rights has had an impact, because there is no longer much money available for community groups. Those advice centres, especially when people needed some help with pensions or housing benefits, were a great gateway that allowed the opportunity to suss out what people were going through. The removal of that gateway prevents an opportunity to tune into what else that person might need, other than getting their cracked window fixed or having their pension aligned. That is a big gap, which you should also consider in your research. The removal of advice centres for welfare rights has definitely had an impact.
994. Mr McGowan: You are right, although I do not know whether I would use the term “survival instinct”. It is more to do with social cohesion, and I agree that that has started to fragment over the past five, six to seven years. When you raise the issue of older people taking their own life, you highlight one of the problems of having a specific population-based suicide-prevention strategy. Older people are not one of the populations that were included in the strategy. The reason for that is, perhaps, historical. I published a paper with Stephen Hamilton and Paul Miller in 2005 — ‘Contrasting Terrorist-Related Deaths with Suicide Trends over 34 Years’; it showed that the suicide rate dropped after the age of 54 and that Northern Ireland is only one of two countries in the world where that has happened. Anecdotal evidence suggests that the suicide rate among the older population is starting to rise. Mike mentioned that, and that is starting to reflect global trends. That suggests to me that something has changed over the past seven or eight years. I take Ms Ní Chuilín’s point that perhaps we need to take some risks in the funding that we need for research. That is not a direct plea for money, but it is a massive area and work needs to be done locally on that issue. We also have a role to play internationally in saying that we have come through the Troubles, and we are a changing society that is moving on. We can share our experience and how we dealt with the Troubles, and people can learn from us.
995. The Chairperson: Do you want to say anything about that, Mike?
996. Mr Tomlinson: Psychiatrists will tell you that more psychiatrists are needed, and, of course, social researchers will say that more social research is needed. A study was conducted in areas of Scotland, and many places in Scotland are among the top 20 areas throughout England, Scotland and Wales for suicide rates. The Shetland Islands tops the bill, which says something about rurality and rural isolation.
997. One of the best pieces of social research, rather than psychological research, on suicide was done by social geographers. They were able to predict the suicide rate precisely in every parliamentary constituency in Britain on the basis of three variables, which they said were the most important markers of social isolation.
998. As we were talking about elderly people, I was reminded of that study, because one of the major factors in relation to suicide is single-person households, and many elderly people live on their own. The second factor is population mobility, where there is much inward and outward migration and communities are mixed up and unstable. Immigrant populations create change, which means that areas are dynamic. The final factor is detachment from the labour market, which is a huge problem, because many of us derive our social networks and supports from our place of work.
999. Those are three important background variables. Social isolation affects elderly people along with all the changes that are taking place. They are also detached from the labour market, and they may go to a local advice centre or post office only to collect their pension and meet people. If the post office closes down and those older people have no family, there is no other framework or basis on which to meet other people, and they become socially isolated.
1000. The Northern Ireland suicide prevention strategy refers to the relationship between suicide, deprivation and poverty, and so forth, but they are not the main causes. The main problem is social isolation, which is connected to the other factors. Detachment from the labour market also plays an important part, because a lack of income shapes poverty.
1001. Mr Easton: That was fascinating. The statistics are very interesting.
1002. Mike, is there a possibility that antidepressants have contributed to some suicides, perhaps because of misdiagnosis or the wrong type of drug being prescribed?
1003. Mr Tomlinson: I urge the Committee to consider that issue in more detail. We are going through a period of major change, socially and politically, and people have to come to terms with massive changes in the way that they think about others. There is evidence of mass medication, whether that is with alcohol or antidepressants, and the Committee must seek an explanation. Are pharmaceutical companies using doctors to push their products because of the new generation of drugs? Are people presenting with more mental distress, anxiety and depression because of changes in social circumstances? What is the cause? That is a big question, because I am alarmed by the increase in prescriptions.
1004. I have examined studies relating to Northern Ireland, and the results are contradictory. On the one hand, it could be argued that the more medications that are in people’s cupboards, the more likely it is that they will get into the wrong hands for the wrong purpose, and we end up with attempted, or actual, suicide. On the other hand, some studies defend the medications and conclude that they prevent suicide. There is no clear-cut answer, but it is an important question.
1005. Mr Buchanan: Some of the issues have already been touched on, but, on glancing through your two submissions, I notice that Iain referred to low-skilled workers, people in temporary or unstable employment and people with low educational attainment and material status — all of whom can have suicidal tendencies. That crosses many Departments: Education; Employment and Learning; Enterprise, Trade and Investment; Finance and Personnel; and Health, Social Services and Public Safety. Mike’s submission refers to areas that have an above-average rate of suicide. It mentions Omagh and Strabane among other places. Recent and not-so-recent reports identify those places as areas of high deprivation, and so forth. You also spoke about social isolation. Are you saying that a lack of skills and areas of high deprivation affect people with suicidal tendencies?
1006. Mr McGowan: That is my belief.
1007. Mr Tomlinson: We have spoken about the factors that build up people’s esteem. If people have a sense of direction and a future, if they are well educated and can escape the confines of a traditional community and have a future in that sense, those factors will contribute to a sense of ambition, esteem and progression. If a person feels trapped, he or she is isolated in a different way. He or she will feel isolated from all the things that other young people seem to be getting, from progressing or from the idealised lives that surround us in every way. One can be isolated in that sense. One might be living with one’s family in a rural community but might feel isolated in that other sense.
1008. Mr Buchanan: No doubt there is a huge job of work to be done in those areas.
1009. Mrs O’Neill: I suppose it is a matter of getting the right balance of prevention, intervention and postvention. Should there be less focus on the general population and more focus on specific groups, such as people who self-harm? One of the NICE (National Institute for Health and Clinical Excellence) guidelines recommends targeting people who self-harm. That is one element of the strategy, and trusts are seeking to ensure that there is proper follow-up for people who present with self-harm. However, many people slip through the net. A person might attend an accident and emergency unit with self-inflicted injuries, but he or she might not be seen again until the same thing happens again. Should there be more focus on specific target groups, as opposed to a general approach, or should there be a balance between both?
1010. Mr McGowan: There must be a balance. I can see the value in highlighting particular “high-risk” groups. However, there would always be a risk of alienating other people or missing a group, such as older people, pregnant women or new mothers. My colleagues Wendy Cousins and Sharon Milner and I are publishing a paper next week that will show an increase in the rate of suicide attempts and self-harm in children living in state care in Northern Ireland. That is another target group. Although I can see the value of interventions with specific groups, there must be a balance in order to take account of those people who do not fall into groups.
1011. Mr Tomlinson: Self-harm covers such a spectrum of behaviour. The self-harm that presents as a suicide attempt in a hospital is very different to 15-year-olds scratching themselves with a pen in school, which is no more or less distressing for teachers. We need an understanding of where the pressure points are.
1012. The Chairperson: Everyone has now had an opportunity to speak. I thank Mike and Iain for attending the Committee. As Alex said, this has been a very interesting session. There are so many complications in the entire process that one wonders where to start in helping to solve the issues. Thank you for the work that you are doing. We appreciate that you have given of your time to come to the Committee.
7 February 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
The Most Rev |
The Roman Catholic Church |
|
Rev Roy Cooper |
The Methodist Church in Ireland |
|
The Right Rev |
The Presbyterian Church in Ireland |
|
The Most Rev |
The Church of Ireland |
1013. The Chairperson (Mrs I Robinson): I extend a warm welcome to Rev Roy Cooper, President of the Methodist Church in Ireland; Rev Dr John Finlay, Moderator of the General Assembly of the Presbyterian Church in Ireland, accompanied by Mr Lindsay Conway, the Presbyterian Church’s director of social services; and the Most Rev Alan Harper OBE, Church of Ireland Archbishop of Armagh and Primate of all Ireland, accompanied by Rev John McClure. We have received an apology from his Eminence Cardinal Sean Brady, the Roman Catholic Archbishop of Armagh and Primate of All Ireland. However, he is ably represented by the Most Rev Patrick Walsh, Roman Catholic Bishop of Down and Connor, who is accompanied by Dr Oliver Woods. You are all very welcome.
1014. I invite each of the Church leaders to make a short presentation of about five minutes, then we will open up the Floor for questions. I cannot reiterate enough that you are all very welcome.
1015. The Most Rev Patrick Walsh (Roman Catholic Bishop of Down and Connor): It is good to come off the substitutes’ bench and score the first goal. We are grateful for the opportunity to address the Committee today. The fact that the four Churches are represented at this high level shows that we regard this topic as an important one in our pastoral ministry. We support the fact that the issue of suicide and self harm received prominence in the draft Programme for Government. It is clear from that, and from the minutes of your last meeting, that the Minister and the Committee are very much involved in the issue.
1016. All of the Church leaders will say pretty much the same thing today. We have met regularly to discuss various social issues, and each Church has given a great deal of thought to the problem, but we have not met to prepare for this meeting; therefore, we will probably repeat each other. However, from a Christian point of view, we speak with one voice on this important issue, as we do on many social issues.
1017. In the Catholic Church there is a group of people called the Northern Ireland Catholic Commission on Social Affairs, and Dr Oliver Woods is a member of that group. When it was preparing its submission to the draft Programme for Government, the commission received a full briefing paper from the Royal College of Psychiatrists. I understand that the Committee has met members from the Royal College, so we do not need to repeat what was in that paper. I found that a most interesting and enlightening document.
1018. I would like to talk about the emphasis put on the group that is attached to the Mater Hospital: the Self Harm Service for North and West Belfast. Currently, there seems to be a preponderance of suicide incidents in those parts of Belfast. Self harm is obviously an important issue, and the report says that is the one issue that really must be tackled in the prevention of suicide.
1019. As a trustee of the Mater Hospital, I take a certain pride in the group, and the Mater Hospital is the first general hospital to have a dedicated psychiatric service. I understand that the group is funded by Department of Social Development, not by the Department of Health, Social Services and Public Safety, and the funding will be there until April 2008.
1020. Psychiatrists have stressed the importance of having such groups based in general hospitals. Is there any indication that they will be replicated throughout the Province? Can the Committee give some guidance?
1021. The Chairperson: The Committee is concerned that there is only one pilot scheme in north and west Belfast, and it is incumbent upon us to see that rolled out right across the Province. A gentleman who gave evidence to the Committee last week told us that suicide is not determined by location or areas of social deprivation, and I am gravely concerned about people in rural constituencies who are isolated, who have many problems and who do not have direct access to doctors, psychiatrists and accident and emergency units.
1022. I hope that we, as a Committee, to a man and a woman, will ask the Minister to look at rolling that programme out in all areas, with the trusts providing a back-up service for those who self- harm or contemplate suicide.
1023. Bishop Walsh: I am very glad to hear that, and thank you. It is being funded by DSD rather than by Health?
1024. The Chairperson: Yes, but it should be funded by the Health Department.
1025. Bishop Walsh: I will not enter into that. [Laughter.]
1026. The Chairperson: We will chase the Minister about that.
1027. Bishop Walsh: Everyone will want to talk about involvement of the clergy, therefore I will not take up time. They are involved in three areas of suicide. The first is that, from time-to-time, they are among the first to be called out to a suicide incident, which is a very harrowing experience.
1028. Secondly, they are then involved with the care of the families, and that is a most important part of pastoral ministry for all our churches.
1029. Thirdly, they are, very often, the first port of call for someone who is contemplating suicide, or who has indulged in some sort of self-harm.
1030. Those are the three main areas that the clergy are involved in, and we are all very conscious of the need for them to be trained. I am sure that those points will be taken up by my colleagues.
1031. Rev Roy Cooper (President of the Methodist Church in Ireland): The Methodist Church is, along with other churches, concerned about suicide and that is evident from the following statement found in our publication ‘Methodist Beliefs’: “We recognise that suicide is a complex issue, which presents many challenges in developing appropriate responses. We believe that the Church’s role is to show, in speech and action, the compassion of God for those who are suffering. We seek to promote deeper understanding of the many causal factors that lead to suicide. We work for the development of sensitive, pastoral responses for all affected by suicide.”
1032. As a Church we recognise that suicide affects all age groups. Economic difficulties, health concerns and that difficulties in relationships can become exacerbated when people are isolated or involved in occupations, such as farming, where they are on their own for considerable periods of time. Psychologists like Rory O’Connor of the University of Stirling have underlined the link between rumination, that is the continued dwelling on a problem, and the ideation of suicide, which allows for the possibility of suicide as a way out of a problem, where one otherwise feels trapped.
1033. I served in the Irish Republic for 18 years. My last parish was in County Wexford and shortly before I left in 1996 there were six suicides, four of which were among the farming community. Part of the problem was that lending agencies and banks had thrown lots of money at those people and, when things did not work out, the lending agencies and banks put the squeeze on them. Many young men resorted to suicide to solve their problems.
1034. The Church’s role in suicide prevention may include as many efforts as possible to develop experiences of community. Indeed, for many in town and country, the Church is their basic community. There may be other initiatives, including co-operative working and being prepared to talk openly about suicide, thereby giving opportunity to challenge its perceived role as a solution to problems.
1035. We have an annual conference — “Autumn Soul” — for young people aged between 12 and 18, which is the largest gathering of young people in our Church. One of my colleagues, John Alderdice, carried out a major survey among those attending the 2004 conference, and found that depression headed the list of most important issues that the Church had to deal with. About 9% acknowledged that they did not enjoy life and that they felt inadequate and of less worth. As a result, a programme was set up through our youth department, which organises groups in churches and among young people, such as youth fellowships, etc.
1036. There is isolation for the young and old alike in rural areas. We have produced a book through our council on social responsibility, and many topics are germane: for example, understanding suicide; personal stories; responding as individuals; and responding as churches. The book was produced and printed by Veritas, and has been used by many churches. Veritas has said that it has finished its final publication and that the book is sold out. I am cheeky enough to wonder whether there is any finance available in the Department and whether it might be able to effect the publication of that book. Lindsay Conway tells me that he uses the book regularly. That is my pitch for some finance.
1037. In relation to clergy training, courses are provided for those studying at our theological colleges, while further study days on the topic have been organised by our director of ministry for those in parish work who await ordination. Moreover, our laity has been offered seminars on the topic at our theological colleges. We want to try to do that as Churches. Hopefully, today will show not just the Committee, but those watching or listening, that the Churches do speak with one voice on the matter; we are not simply trying to pick up on each other, we move together. Our presence here today shows just that.
1038. The Right Rev Dr John Finlay (Moderator of the General Assembly of the Presbyterian Church in Ireland): I reiterate the appreciation that we all have as Churches for the opportunity of sharing with you this afternoon. We are always willing and desirous to be a comfort and counsel to those who have suffered, especially the families. Perhaps our concern and our frustration is that, more often than not, people who take their own lives are very peripheral to our membership and association with the Church. We are frequently unaware of the need, and sometimes the families involved are unaware of the particular problems or circumstances that may create a suicide situation.
1039. As you might expect, we have absolute confidence in the hope and the purpose of the message that we bring, and in the support and the helpfulness that the Church can be, given the opportunity. However, we accept that the challenge — especially for us — is the provision of some sort of preventative measures.
1040. Our Church, like most denominations, has first-hand experience in dealing with a wide range of mental-health issues. Our ministers deal with members who are depressed and who are suffering from alcohol or drug addiction. Sadly, ministers increasingly have to deal with members who have taken their own lives. I have had to deal with a couple of such incidents in the recent past, and I know one minister, in a rural setting, who has had to deal with four instances in one year. Therefore, pastoral-care situations clearly indicate that people are not coping in the same way as past generations may have done.
1041. Furthermore, we are concerned that the prevalence of suicide in an area — especially among teenagers — can, sadly, create a copycat culture. We fear that the situation is exacerbated by the media and by the influence of soaps.
1042. Our board of social witness has produced a suicide awareness leaflet, which has been reprinted three times. We also offer a Christian-based counselling service to the whole community, and this year, our chaplains’ conference is considering the subject of suicide and church. Therefore, we accept that we have a clear role in what is a major social problem.
1043. We are committed to reducing the risk of suicide by offering a listening ear and a safe place to address problems. During lunchtime, I spent an hour at a cross-community and inter-denominational project in Ballynahinch. Its main focus is mainly, though not entirely, on youth work, and it has made a significant difference on the streets of that town. It has created a sense of a safe place to which those who are potentially suicidal can come. That project has been effective and encouraging, and it is something that we would like to see repeated in other areas of the Province, especially through our own Church.
1044. One request that we might make is for encouragement and possibly help with the provision of training, not only for clergy but for others who are involved in this field.
1045. The Most Rev Alan Harper (The Church of Ireland Lord Archbishop of Armagh and Primate of All Ireland): Thank you for giving me the opportunity to address the Committee. This is the fourth time that you will have been thanked.
1046. The Chairperson: It is lovely.
1047. Archbishop Harper: It is a privilege to be here. The Committee will be aware that essentially similar issues and similar levels of suicide exist in both political jurisdictions of this island. I say that because I am responsible for a cross-border diocese, and suicide is not merely confined to the part of that diocese that is in Northern Ireland. That, perhaps, provides a small corrective to the too simplistic analysis that suicide is some sort of direct outcome of 30 years of community discord.
1048. I included that information in a paper to the Irish Association of Suicidology a couple of years ago. In that paper I suggested that high levels of suicide could be associated with rapid societal change — the kind of rapidity with which people find it difficult to grapple — and community change.
1049. The parallel example that I used referred to studies of the Inuit, which is a highly traditional society in the north of Canada. Everything in their lives is changing — not just climatic change but everything relating to family and social structures. Their levels of suicide are higher than ours.
1050. Obviously, among other things, societal change includes the role of religion in society. I do not think that any of us would be foolish enough to suppose that that is not a major concern for all of the Churches. We see a significant decline both in religious affiliation and in religious practice. However, there is a significant amount of research to demonstrate that having some definite philosophical and religious commitment provides people with satisfaction, happiness and well-being. Therefore, that is a serious challenge to all of the Churches, and I suspect that it is an issue that we need to correlate in some way with the increasing tide of secularisation.
1051. Societal change includes issues such as family stability and the collapse of family structures, which deeply concern the Churches. Other concerns include small issues such as deference, which is an indicator of how people relate to one another and the way in which they acquire some sort of validation from other people in their social network.
1052. The last matter that I want to draw attention to is one of concern for all of us. Societal change also includes problematic substance and alcohol abuse. There is significant evidence that that may be directly correlated with mental-health issues.
1053. When I speak of mental health, I do not want to suggest that suicide is merely a matter of mental ill health. It is not. To deal with it simply as a mental-health matter will address some, but by no means all, of the issues.
1054. What are the Churches responses and opportunities? First of all, information and communication are key. The Churches that we all represent are social networks with significant social capital, but significantly dependent upon volunteers, and volunteerism is not necessarily on the increase at present. Before we came in, we reflected that there is a helpline, but no one knew the number. There is an issue about disseminating information. There is no reason at all why Churches at parochial level — let alone, at diocesan level — could not be significant players in disseminating the kind of information that might enable people to access the help they want when they want it. That would not necessarily require people to disclose that they have a problem to a group that they might not want to expose that problem to.
1055. That is one issue; a second is the training of clergy and church workers, which has been mentioned by several of my colleagues. In the Church of Ireland, we conducted a survey amongst clergy on the issue a couple of years ago. The overwhelming number of clergy said that it was a major issue for them; however, they felt that they were seriously under-resourced in dealing with it. They said that that they needed to know how to recognise the signs of self-harming or suicidal behaviour, and to help subsequently in dealing with the outcomes, whether that involved dealing with survivors or bereaved families. Clergy need to be able to address questions such as: “Why?”, “How?” and “What was my responsibility?”
1056. Training is a very significant issue for us. We are reconstructing our clergy training programme: a radical overhaul is being conducted at the moment. Suicide awareness will be a significant component in that. However, that is only a forward projection. We have some structures in place, but they are insufficient for upskilling the clergy to deal with an issue that many of them will not have encountered face to face.
1057. In my diocese last summer, in one small area bridging two parishes, four young people, three of them in the same class at school and belonging to the Church of Ireland community, took their own lives — two of the four in an identical fashion. The impact of that on the whole community was incalculable on that class and school, and the response that the Church had to make was demanding on the clergy in the area. We are deeply aware of the problems.
1058. If there is even a scintilla of truth in the notion that there is a societal rather than a mental-health issue involved, then we certainly need joined-up thinking and acting. I welcome very much the suicide strategy implementation task force. I have stressed that all suicide is not connected with mental-health issues, although there may be a connection between those and problematic substance abuse. I would love to see the Bamford Review revisited, to see the proposals brought forward and implemented and to have it extended to include consideration of personality disorders as a category. That is not dealt with at all in the Bamford Review, and there is no strategy provision of any sort to deal with that, admittedly, very difficult area. However, it needs to be addressed.
1059. Finally, I publicly welcome the support that many bereaved families and survivors of suicide attempts get from community groups such as the Public Initiative for the Prevention of Suicide & Self-Harm (PIPS) and Rural Support. I echo earlier comments about the issue not being confined merely to deprived inner city areas: it is also a rural issue. Although suicide is portrayed largely as an issue for young males, which statistically it may be, I am concerned that the number of suicides among elderly people has been under-recorded due to their deaths, for one reason or another, being put down to different causes.
1060. Thank you for giving me the opportunity to address the Committee today.
1061. The Chairperson: Thank you very much for your input, gentlemen. The Committee takes the issue of suicide and self-harm very seriously, which is why we immediately launched an inquiry into it. We have received more than 65 submissions, and we hope to examine those at Easter. We will collate all that information and produce a report that we can look at after Easter, DV. We can tweak that report and, hopefully, have something to present to the Minister.
1062. It would be helpful if we could have copies of the papers and pamphlets that you all mentioned, as they would be useful to have as evidence. Rev Cooper, you mentioned a book that was available.
1063. Rev Roy Cooper: I have brought a copy of the book for the Committee.
1064. The Chairperson: Thank you. We can collate that information and study the advice that you give to your parishioners. We could lose sight of the fact that it is not just young men who commit suicide, although it is predominantly young men. Some women suffer from post-natal depression; some suffer depression as a result of sexual abuse, and so on. The law may never have protected them, as their problem may have been brushed under the carpet. There are many types of depression and many types of mental illness, and, as you said, they should not simply be lumped together.
1065. I welcome this opportunity to hear your views, and I will now open up the meeting for questions from members.
1066. Mr Easton: I better behave myself, because my brother is a Church of Ireland minister. Would it be helpful if the Department of Health, Social Services and Public Safety provided training for clergy of all denominations? How do you envisage building up a good working relationship with the Department of Health to work on those issues? The Church does not represent the whole community, but it represents a huge and very important part of it. It is essential for us to tap into it and to assist it.
1067. During the Troubles, there did not seem to be as many cases of suicide as there are now. I am not trying to connect the two issues, but attendances have dropped off across all the Churches. I was wondering whether some people cannot cope with the pressures of life, because they are no longer getting that pastoral care and that input from the Church in their lives. How do you feel about that?
1068. Rev Roy Cooper: Our Church, through our council on social responsibility, would be happy to engage with Government and to get involved.
1069. The decline in church attendances is not only among young people. Even grandparents now are non-churchgoers. When I was growing up, I remember that if someone’s mum and dad did not go to church, their auntie would have. There was always some connection, but now it is so tenuous.
1070. Churches need to say that they were perhaps too judgemental in the past. Maybe they were not prepared to accept certain situations that people were going through. I knew someone who took his own life. He took the courageous step of coming out and saying that he was living as a homosexual. He thought that that was the way in which his life was going. However, he felt that he could not say that to his minister or to the youth club leader, because, at that stage, people would have been judgemental. Maybe the Churches pushed people away by adopting that attitude. However, as we have said in the book, we are now taking a different attitude; we are not condoning or condemning things, but we are making ourselves more user-friendly, from that point of view. That is my answer to your question.
1071. Rev Dr John Finlay: As I implied earlier, statistically, it is less likely that someone will commit suicide if he or she has a close church connection. I am not sure whether that was the case in the past; it would be presumptuous of us to say, “Oh, yes”, just because that situation has arisen.
1072. The challenge that faces us, and which we take very seriously, is to find a relevant and helpful way in which to connect with a community that is distanced from us, and which may be, largely, disinterested in what we are trying to do and in the message that we are trying to bring. We are all challenged to do that effectively. We take that challenge seriously, and we are seeking to address it. It is a question of building a bridge. As I implied earlier, the problem is finding the people who are in that sort of need. Often, they may not be the people whom we would target.
1073. The Chairperson: Will someone deal with the issues of training the clergy?
1074. Rev John McClure (The Church of Ireland): I have been speaking to an official in the suicide strategy implementation body, and there is funding for the Churches to train new and existing clergy. The four Churches must put together a finance plan to show what it will cost, but I have been informed that the money is available.
1075. To go back to the points made by Bishop Walsh, I have been involved with the Mater Hospital’s programme for people who self-harm. At the last meeting, I was told that another six hospitals are to get involved in it. The Mater Hospital has been running a pilot programme, and it has been so successful that another six hospitals will take it up.
1076. The Chairperson: That information has not yet reached the Committee, but the Minister will be coming to brief us.
1077. Rev John McClure: The programme has been successful. About 7,000 people self-harm each year in Northern Ireland.
1078. The Chairperson: The statistics are horrendous.
1079. Rev John McClure: For some people, the programme is a way of staying alive.
1080. Mr Lindsay Conway (The Presbyterian Church in Ireland): Finally, from the point of view of theological training, we are more and more conscious that candidates for the ministry, licentiates and those already in ministry must be trained. They must be aware of what to look out for at a pastoral level. Although church attendance may be falling, there is clear evidence that some of the counselling services and some of the other supports — whether through playgroups or some recreational element of church life — provide the safe place that the moderator mentioned. People need somebody who will listen, and listening posts and counselling services will do that. The number-one issue is that people, from a younger age, suffer from what we used to call “feeling down”. In their language it is depression, and they say that they can take no more, that life is not worth living. It comes back to the lack of a coping mechanism. Yet the Churches of all denominations still provide, at a conservative estimate, 60% of the youth and children’s work in Northern Ireland.
1081. Archbishop Harper: Seventy-eight per cent of the registered youth work in Northern Ireland is carried out by the Churches.
1082. To follow on from what Lindsay said, one of the things that we are in the process of providing for — and in which we would be very pleased to receive assistance — is the training of those people who are not necessarily clergy but are youth workers in the Church. Currently, in the Church of Ireland, we employ approximately 80 paid youth leaders. Last March, we had a joint conference — with the Methodist Church — of 50 youth leaders that dealt to some degree with that matter. They are probably in a more accessible position than the clergy to deal with, or at least to begin to recognise, issues that might lead to suicide among young people. It is a bigger issue among them than it is among the clergy.
1083. There is a phrase, in another document that I am almost too familiar with, that clergy are the “gatekeepers of change” in the Churches, which is true. Therefore, it is important to have the clergy better informed and more open about those issues.
1084. Mr Conway: Given that we are an all-male team, which is just a fluke —
1085. The Chairperson: I was not going to comment on that. [Laughter.]
1086. Mr Conway: There is an argument that, because, statistically, males are more at risk than females, we avoid and neglect women’s issues. We cannot do that, because when you consider the matter of self-injury, the opposite prevails. We must take that on board, and with that mass of youth work and children’s work, we are well-placed to do so. It is the self-esteem factor and the self-image that we have to impact on.
1087. Bishop Walsh: Reading about the subject during the past few days, in our personal preparation for today’s meeting, has helped us — it has certainly trained me, somewhat. We would be happy to agree to a joint programme of training for clergy and youth workers such as that mentioned by Archbishop Harper. The issue of suicide is taken seriously in our seminaries. In the year before ordination at Maynooth College, there is quite an emphasis on training in the various aspects of pastoral ministry, including the issue of suicide. However, it is the ongoing information that tends simply to drift away, and much of it is provided on an ad hoc basis.
1088. We should all fully support, and get together on, a more formal programme of training for clergy and youth workers. This morning, I spoke to the director of our youth commission. He told me that a lot of people in the youth clubs are undertaking training. I think that he said that it is funded by the Department and that training was available for youth workers.
1089. Mr Easton asked about the link between suicide and the Troubles. Again, I spoke to one of my priests who served for many years in a parish that was at the centre of conflict. He told me that there was a dramatic rise in the number of suicides after the ceasefire. He was able to provide me with figures. I was surprised by what he said, but it is a definite fact.
1090. Mr Easton’s other question was about communication with the Health Committee. I know that, from my own experience, we have good links with the Department of Education, for obvious reasons. However, this is the first time that I have attended a meeting of the Health Committee. We were not really aware of the channels of communication that could be built up in the Department. I have met the Minister of Education and the permanent secretary about various issues. However, it has been useful to have the opportunity to come to Committee and meet a wider cross-section of MLAs. Is this channel open to us at any time?
1091. The Chairperson: Yes, at any time.
1092. Bishop Walsh: I know that, as you mentioned, our family ministry commission attended an earlier meeting of the Committee. It was the commission’s idea to ask for that meeting. It would be helpful if it were known that people could ask for meetings of that kind.
1093. The Chairperson: This Committee is one of the busiest, with regard to lobbying and hearing presentations. We could, literally, spend all week hearing presentations on all aspects of health provision and delivery. We brought in 20 different groups, on one day, because we had such a backlog.
1094. Indeed, we are contemplating bringing in another large group of people who want to lobby us on specific issues, although they are not the top priority. They are important matters, but issues such as cancer are seen as being more important. However, we want to hear from everyone, and our door is always open. That is why we decided to keep the good wine to the last, and invite you folk to give your views on this very difficult matter.
1095. Ms S Ramsey: I welcome the fact that the Churches are here as a collective voice, and I think that that is useful. It strikes me that Bishop Walsh has said that there is a lack of sharing of information and resources. No matter what is said about attendances, the four main Churches are seen as the heart of the community in the majority of areas, and they do have an input. A sharing of resources and information between the Churches would be useful.
1096. This is not a criticism, but it strikes me that none of the Church leaders know the number of the 24-hour helpline. I do not know the number either, so there is a lack of information across the board. If the helpline is to be extended, we must consider how to get that information out to the communities.
1097. Mention was made of GPs and medical professionals taking up the assist training. Although the Department has provided funding for new clergy to be trained, I am concerned that the old timers should also get that training. Furthermore, laypeople who are involved in youth work must be considered. A number of people are involved, not only the clergy.
1098. When considering school involvement, we must talk about prevention as well as dealing with people who self-harm or take their own lives. Schools and youth clubs have a solid foundation to get involved in prevention.
1099. I agree with Rev Roy Cooper that, for a long time the Churches have been too judgemental. Families have told the Committee about the impact that language can have when people take their own lives. I have attended a number of funerals of people who have taken their own lives, and the language that some of the clergy used during the funeral services was, although not deliberate, quite hurtful to the families. They told us that they wanted to get away from people saying that someone “committed” suicide. To the families, that makes it seem as if the person has committed a crime.
1100. Today has been helpful, and I would like to know if information could be shared formally, or if a formal gathering could take place so that the Churches could discuss about how they might strategically impact on the communities that they represent. Can the Churches come together with a collective strategy, rather than working piecemeal all over the place? I think that today’s meeting has been positive.
1101. Bishop Walsh: Sue’s point about funerals is interesting, because my priests say how difficult they find those. It is often a question of language, and you said the word “committing” suicide is language that should not be used. The priests say that they are hesitant about preaching about the subject in their ordinary Sunday Masses, when the opportunity might arise. They feel that someone in the congregation might have been through that and that they might be hurt by what is being said. You raise a very important issue, and how to cope in those situations could be an important aspect of training for our priests. Some priests are instinctively extremely good at doing that, others, particularly those who have to deal with it for the first time, find it difficult.
1102. Rev Roy Cooper: I suspect that, at times, some families have a sense of guilt. In some respects, therefore, they are not hurt by what is said about their son or daughter, but rather by thoughts that they did something, failed to hear them, despised what they were like or undermined them. Obviously, the Church has its ritual for dealing with grief in the form of services; however, although I have never had to deal with families suffering as a consequence of suicide and I am speaking hypothetically, I feel that such people require pastoral care in their homes — not in order to dissect the situation, but to build a relationship that will allow them to talk about what they are really feeling.
1103. The parents often carry a feeling of guilt, and their reaction is a way of hitting out. They think that we are attacking them because they were inadequate mothers or fathers. There must be a period of pastoral care for such people in order that they can feel safe enough to open up.
1104. Mr Conway: The situation can be likened to GPs diagnosing meningitis — they may only encounter it once in their career, but they must get it right. Ms Ramsey is right — I agree with her — that the final words about a family’s loved one at a church service are the words that the family will go away with and carry into the next day, month or year.
1105. Roy referred to the book, ‘From Despair to Hope’, which deals with suicide in a systematic and pastoral manner. I am not defending anybody, but there are two or three days to prepare for a service — there is no rehearsal. The responsibility is there and the consciousness is at a level that it has never been before. I hope that you find that encouraging.
1106. Archbishop Harper: I wish to pick up on something. The sharing of information and resources was mentioned, and, perhaps, the Churches should take a more systematic approach. That is a good idea, and for an additional reason. By working together in a training programme, people build up personal networks and become better at relating to the clergy of other denominations. The ability to be able to network across the community is very important. You can not only gain insights and share information but you have the opportunity to get to know people whom you might want to call on for assistance when dealing with a difficult situation. The benefits of that apply not only to clergy but to all church workers, including youth workers.
1107. In addition, I am concerned about the aftercare provision for clergy who have dealt with significantly traumatic incidents, some of which may not be traumatic in how they present themselves, but which are traumatic in the enormous maelstrom of emotions that must be navigated.
1108. The Chairperson: That is an important point. The Committee visited Scotland, and Dr Paul Miller, a consultant psychiatrist who presented evidence, spoke about his weekly attendance at the “Who Cares for the Professionals?” initiative, which should be rolled out not only for the professional healthcare sector but across the spectrum of clergy and laypeople in order to demonstrate that someone is also there for them. They have to deal with people who open up to them about the most traumatic and dreadful stories and situations. It is important that someone should be there for them.
1109. Archbishop Harper: May I add to that? There are fewer clergy than there used to be in most parochial situations. It is almost analogous to the old model of medical care in which there was a single practitioner. Most medical practitioners are now in groups so that they have a support system of colleagues and a wider support system around them. Many clergy are not in that situation now, so they have to look for those support systems elsewhere. That support does not necessarily come directly from the next-door neighbour; it might come from a whole range of other opportunities.
1110. Rev Dr John Finlay: May I ask Lindsay to say something about our pastoral care committee?
1111. Mr Conway: We have acknowledged that that situation exists, and we have talked about it on different levels with the Archbishop. The Presbyterian Church in Ireland has taken that forward and has considered the pastoral care of ministers and manse families, and those in full-time work. It has looked not only at church models, which are well-rehearsed in relation to the pastor pastorum groups that Archbishop Harper mentioned, but at an external body that could examine those issues totally independently from the Church. We look at how we relate to a professional service, so that an anonymous service will be there to link in to for ministers and manse families. That is progress, at least.
1112. Rev Roy Cooper: We have some of those structures in various dioceses too.
1113. Rev Dr John Finlay: May I respond to a point that Sue Ramsey made? Please understand that I am not being defensive. There are exceptions; none of us is perfect, and we all need to learn — we accept that. Normally, however, Churches generally deal sympathetically and sensitively, through their services and their ministry, when an issue like this arises and they are involved in it. I am sure that Sue will agree with that.
1114. Ms S Ramsey: I do agree, but we must also take on board the sensitivities of families. The use of the phrase “committed suicide” has a negative impact on families. That point was made in the evidence session as well.
1115. Rev John McClure: I have known too many people who have lost their lives, and there was not a bad one among them — they were beautiful people. The phrase “committed suicide” came up only in the past three or four years, and that was in west Belfast. I know the people there, and they are great. It is a word that we all use. Society was totally ignorant of suicide. It is only in the past couple of years that we have gained knowledge. In the Church of Ireland, when someone takes his or her own life, we are there to help the minister to know what to say and what not to say, and to help him afterwards, because it is a totally draining experience. The Church of Ireland offers that support. You are right, Sue. We have to be careful, because the families are very sensitive.
1116. There is a big problem about a lack of information for groups outside the churches, such as those in west Belfast or the Public Initiative for the Prevention of Suicide and Self-harm (PIPS) project, about sharing information with each other. I know that there is a lot of disagreement among them about that. Martin Bell and I and a few others want to bring all those groups under one umbrella. I do not know whether we will be successful, but we must be brought in, because we are the first port of call, and we help the people who sit on those groups. However, the Churches have been excluded. That cannot go on.
1117. The Chairperson: That situation must be resolved. We said earlier that the churches were the first port of call for the families of the victims, and were tasked with bringing families through the trauma caused by the taking of a life.
1118. I do not wish to be rude, but we must adhere to the time allotted. There are several speakers, but it is not necessary for everyone to address the issues related to the Churches. We are running out of time.
1119. Dr Deeny: You are very welcome, gentlemen. I will try to be brief. I am delighted that you are here. I speak as a member of this Committee and as someone who has been a GP for many years. I agree with the comments made by all four of you and by your colleagues. This not just a mental-health issue, as Archbishop Harper said. It is the duty of health professionals, the representatives of the Health Department, educators, Churches and community and voluntary groups to work together on this terrible issue.
1120. As Bishop Walsh said, we too are like the Church. An interesting point was made about people being called to scenes of suicide — I have been called twice to suicides in the past few years, the memory of which will stay with me forever. In those two cases, there was no evidence of mental-health problems; unhappiness due to the break-up of relationships and an inability to cope with that seemed to be the reason. That is why it is great that suicide will be treated as a societal issue, and that we will deal with it as a society.
1121. Doctors also have to deal with the aftermath of suicide and grief suffered by families, and, as Bishop Walsh said, people often visit us to talk. I totally agree about the problem of suicide in rural areas: down the years, a major problem has been caused by farmers becoming depressed. As with all problems resulting in death — for the most part, illnesses — the main issue about suicide is prevention and the part that we can play in that. Dr Finlay, it would be interesting to hear more about the youth project that you mentioned, because I am originally from Downpatrick, which is close to Ballynahinch.
1122. Mental health problems play a major part in suicide, and it is our job — as health professionals — to detect and treat those problems if we get the opportunity. I agree that depression has been used to describe all types of symptoms such as unhappiness and the inability to cope with life. It is the job of health professionals to treat people with those problems. As I mentioned, talking therapies and the provision of facilities for young people to talk to professionals are very important. We must get rid of the macho male culture in this country — north and south. It is interesting that, although females talk a lot more, they self-harm more, yet there are more suicides among males. The macho image, of which I was guilty for most of my life, of men dealing with their problems on their own and not discussing them, must be dealt with.
1123. We must get the message through in schools, without making judgements on those who have taken their own lives. Suicide is an illness, with an aftermath that devastates families. Relatives have told me that, if the person who committed suicide knew the devastation that it had caused to the family, he or she would not have done it. In schools, the affect that suicide has on families could be highlighted. That would not judge those who have taken their own life. I wonder if, at an early stage in schooling, we could send the message that the greatest gift that anyone receives is human life and that it is precious. Do young people not understand that? Is that a message that we should be sending in schools?
1124. How can we provide more facilities like those in Ballynahinch? I work near Omagh, and it would be nice to have something similar for our young people to use. I know well the families of the two young men that I mentioned. If those young men had had someone to talk to, they might not have committed suicide. Education in schools that life is precious and that one suicide devastates many lives is also needed. It is important to send that message without judging those who have taken their own lives.
1125. Rev Roy Cooper: At the heart of the Church’s message is that people are of value, and that is shared with people Sunday by Sunday. Part of the problem is that when people feel that they are of no worth to their family or society, they question the point of continuing with life. We must find a new vocabulary to help people see that they are valued. That is not the whole answer, but we must begin by sending the message that we value those people because God does. I would start there.
1126. Bishop Walsh: The point that Dr Deeny made about the talking therapies is important. The Royal College of Psychiatrists’ report refers to the lack of facilities for talking therapies and that although psychiatrists can do a certain amount, there is a requirement to talk to patients after that treatment. That is a valid point and one that the Health Committee should take on board.
1127. The Chairperson: Yes, very much so.
1128. Bishop Walsh: There is huge devastation for the family. Again, that is where the pastoral ministry of the priest and the clergy comes in. They spend time with the families. Priests have told me that the statutory agencies move in very quickly — community nurses, and so on, visit — but they are thin on the ground and are overstretched. After a few days, they have done their bit and move on — I do not want that to be misinterpreted. It is the clergy and the local parishioners who must be constantly with the families. That is where the real efficacy of the priests and the clergy comes in; they can spend time — and should be able to spend time — in the home with those families.
1129. Archbishop Harper: It is only when that time is spent that people, who may be in deep despair, feel that they have either the courage or the opportunity to share the problem. People are unlikely to share a problem with someone whom they do not know, or if they are fearful that that person will be judgemental or — worse — dismissive. The human relationship is important. Talking therapies is another issue that needs to be addressed seriously.
1130. Rev Dr John Finlay: I want to say a little more about the project in Ballynahinch. I said earlier that our problem was that there are people with whom we do not have contact in the first place because they are outside the immediate parameters of the Church. The Ballynahinch project addresses that problem at teenage level. It involves youth clubs and full-time youth workers, and it is interdenominational and cross-community. The project has involved the renovation of an old building, which is not connected to the Church. The Churches all have their own responsibility, but this building is separate from that. It is a neutral space, as far as religion is concerned, and a deliberate effort has been made to reach out to young people who do not go to Church youth clubs — those young people who are basically on the streets. It gives them a safe place to establish relationships. I was impressed by the wee room that has been set up, into which only one or two are allowed access — a counselling room, but I don’t know if they call it that. The project allows those young people to connect with people with whom they would not otherwise connect, and those running the project can be the eyes and ears, or can simply be available. To that extent, and in that localised situation, the project seems to have worked, because it arose out of a multiple-suicide situation.
1131. However, on a different dimension, the cases of suicide of which I have experience involved young men in their twenties and thirties who are disconnected from the Church, and that presents a different challenge.
1132. The Chairperson: It is also worth nothing that we should be going to the where the masses are. In a recent visit to Scotland, the Committee learned of a very good model that targets men, in particular. Women are more likely to be self-harmers, but women can meet to talk. Men think that it not macho to cry or to express their feelings in the way that women do. The campaign targeted football grounds. Cards were distributed that encouraged men to talk and included telephone numbers for counselling groups, helplines and so on. That is an important element of reaching out before something dreadful happens, rather than simply picking up the pieces afterwards. The Committee felt that that is a good model to adapt for Northern Ireland.
1133. Ms Ní Chuilín: I welcome you all here today. I know Rev John McClure, who along with Rev Bill Shaw and Fr Aidan Troy, has done great work in North Belfast on suicide prevention.
1134. To pick up on Sue’s earlier comment, I am old enough to remember a time when, if someone took their own life, no one ever mentioned the word “suicide”. I remember the experience of one family in particular, and how no one knew how to tell them that they were sorry for their loss. That is awful.
1135. It is not promoting it, or condoning or condemning it. However, clergy being there, and being seen to be there, has made a difference to people. That might be a way of the Church or community making a connection and sustaining it.
1136. I, and others, have completed the Assist training in conjunction with the Church and the youth of the area. When someone ends his or her life in north Belfast, as soon as the PSNI come on the scene they ask that a priest or a politician go to the family. They have taken on board people’s sensitivities. Roy Cooper mentioned value, and the Church’s presence in the community and voluntary sector, helping those who are volunteering, has been most beneficial. It is expected of next-door neighbours, parishioners and youth leaders to be involved in that sort of work. That is what they have always done. For the Church to become involved is not to for it to condone suicide, but rather to show that it understands. That involvement saves people from forever feeling pain because someone in their family has taken his or her own life. I do not use the phrase “commit suicide” because it implies committing sin.
1137. I support the idea of making that training available for Churches. I have seen it work well, on a cross-community level, as well as inter- and intra-denominational levels. I am familiar with the work of both PIPS and of the west Belfast group. For that work to continue, the more people who avail of the Assist training, or any other training that brings awareness and a level of understanding, the better. More often than enough, we hear of suicide attempts after the event. We are looking at ways of preventing someone from making that awful decision and leaving family, friends and community to grieve for evermore.
1138. The Committee is keen to promote the involvement of the Churches or the community in preventative work. The Churches have done well. None of us is perfect; we all want to do our bit and more. Keep up the good work.
1139. The Chairperson: Not so much a question as a compliment.
1140. Ms Ní Chuilín: Absolutely.
1141. Mr McCallister: I will be brief. It is excellent to have you all present.
1142. I agree with much of what has been said. I certainly agree with Mr Cooper that, on a range of social issues, the Churches need to be as user-friendly as possible. In the past, they were not all as user-friendly as they might have been.
1143. I represent a rural constituency and am part of a farming family. The evidence that the Committee heard in Scotland backs up what we have heard about isolation. It is a problem in all age groups and especially in rural areas.
1144. I was interested to hear Dr Finlay’s comments on the Ballynahinch project. It is vital that the clergy are trained: what are your thoughts on how to expand training provision to youth leaders in the Boys’ Brigade, Girls’ Brigade and similar organisations? How do we make it available? The church is a centre of activity in rural areas; however, reaching those who do not live in such areas may be difficult. I am interested in reaching beyond the youth groups to older generations. We must cut across the responsibilities of Government Departments, voluntary organisations and Churches. It will take a team effort to address this difficult issue. How does one make it available to hard-to-reach sectors? It needs to permeate Churches, youth clubs, bowling clubs and whatever else is organised. How do we make the training available?
1145. Rev Dr John Finlay: Obviously it is a lot easier to prepare established programmes of training inside rather than outside, and that would not be difficult, because the structures are already in place to process information.
1146. I do not have an answer to the other question, because we are all splashing our heads on how to connect with the people most likely to be in need.
1147. Lindsay, do you want to say anything about training?
1148. Mr Conway: There is a challenge for the Boy’s Brigade, Girl’s Brigade, Scout and Guide Associations, who have a traditional approach of promoting healthy living through fitness and diet, etc, and they need to get out of those safety zones and deal with the various issues that affect children. They may just be having a bad day or feeling down and unhappy, and they use extreme language to describe that, but if we cannot reach them at the youth club, during badge work and all the other works that go on in youth organisations, we are missing an opportunity to make an impact.
1149. Churches of all denominations have a major challenge in equipping those who go out and visit the lonely and isolated in their homes, because we know from the study that was released last week by Queen’s University that they are the most vulnerable.
1150. The Presbyterian Church in Ireland counselling service came up with the idea of a mentor for those who are not engaging in bowls, or other activities, so that they will have someone to ring them every morning just to say “How are you?”, and last thing at night to ask “Are you ready for bed?”. I do not mean that we do not need thousands of pounds, but those schemes cost nothing in church life, whether at the level of elders, select vestry or at diocesan level. That is what it is about. It lets people know that someone cares. That is what churches are good at.
1151. The Good Samaritan story ends with the Samaritan telling the innkeeper that he will pay him anything else he owes him on the way back, which refers to sustainability. It was not a one-off act, but one that could be expected to be repeated. That is what the church does.
1152. Mrs Hanna: You are very welcome, and it is good to see you here.
1153. You all made clear the need for training, and, of course, that must be achieved. Bishop Walsh said that the clergy were often the first at the scene to give pastoral support, and I wonder if the suicide rate has anything to do with fewer young people going to church. Church provides a support system around the family, and that is why its involvement as a natural part of community groups is so important.
1154. Dr O’Kane, with others in the Mater Hospital, is very involved in the talking therapies, and it will be good to hear how that pilot scheme will be rolled out, because it has been assessed as very successful.
1155. Societal issues were mentioned. There is a feeling among young people that they should be happy and successful. Much of it is materialistic, so is it any wonder that young people feel that they are failures, who are not valued, when they do not have what others have?
1156. The Committee had a presentation on the coping strategies, self esteem and values that are taught in schools, values in society, and how value is placed on young people. All of us have responsibilities in that regard; there are big societal issues, as well as alcohol and drug abuse, and their impact.
1157. You said that the Churches also need help and that you need the wider Church to work with you, because you cannot do it all on your own. It is vital that you are part of the support that is available in the community.
1158. The passing of information between groups has been mentioned, and there must be joined-up working. There is no point in duplicating services, or leaving a gap, or having a bit here and there. The work of the Churches must be linked with that of the healthcare professionals to ensure that it is along the right lines and that no gaps are left.
1159. That applies to the new helpline. What is happening with that? Does it provide a signpost to appropriate services or offer direct support? Sometimes, when there is a feeling that something must be done quickly, people rush to act, rather than thinking through what would be the best course of action.
1160. Carál mentioned the importance of language. Suicide used to be such a taboo subject that at one time it did not even appear on death certificates. When I was nursing, “committing suicide” was the phrase used, by which no harm or offence was intended. However, many issues centre on the use of language. Everyone knows that meeting a person who has been recently bereaved, whether through suicide or some other cause, is ritualistic because it is difficult to know what to say. I understand that it is impossible for the clergy to try to be all things to all people and send out a message of hope at the same time.
1161. Thank you very much for coming today, and keep up the good work.
1162. Archbishop Harper: Your comments are most helpful. You pointed out that fewer young people attend church than was formerly the case. I do not know whether it is significant, but it is true that fewer men attend church now, and I refer to Dr Deeny. If as many men as women attended church, we would probably have to install additional seats. There is a male issue as far as church attendance is concerned. You were also right about the culture of celebrity. That aspiration manifests itself not only in suicidal or self-harming behaviour, but in dietary behaviour, and so forth.
1163. However, as you were speaking, it struck me that everyone in this room has heard of ChildLine, although we may not know the telephone number. However, if young people want to get in touch with a group that will listen to their issues, they know to look up ChildLine in the telephone directory. Therefore, the new helpline must have a strapline that communicates its services to young people — a trigger that enables people to act according to their needs at a particular time. If it is to be described as something along the lines of “a suicide and self-harm helpline”, we may forget the whole thing. Some thought must be given to the way in which the service is badged to ensure that people know how to access it.
1164. Bishop Walsh: It is true that there has been a fall in the number of people who attend church across all age groups. However, when it comes to death, there is a residual bond with the Church, and the first person in the community to whom a bereaved family turns is the clergyman or the priest. They are in the front line from the moment that death occurs — no matter what its cause.
1165. To follow on from what Carmel said, I wonder if there is a problem with the link between the statutory agencies and the many different voluntary agencies that beaver away, often acting alone. There seems to be a gap between the two, and a better partnership may be required.
1166. The Chairperson: The Committee received some correspondence that flags up the issue of partnership. If some voluntary agencies that provide much relief and help through their outreach work in the community do not get money after March, they will collapse and close down. Their funding is running out, and they would prefer to be part of mainstream funding rather than having to wait each year to see whether they can survive.
1167. Mrs Hanna: Those pilot group schemes that have been evaluated as doing a good job should be eligible for mainstream funding.
1168. The Chairperson: I agree, and we will consider that carefully when we are completing our report.
1169. Mr Gallagher: I reiterate what the witnesses and others have said: we are all in this together, and it is a huge issue. No one has the answer to it, but we must all keep working at it. Therefore, I was stunned when I heard that some groups that provide support to people who are close to suicide exclude the Church. I cannot understand that; it does not make sense. Rev John Finlay said earlier, and I believe more strongly than ever, that there is a link between good mental health and a religious or spiritual dimension to a human being’s life.
1170. Most of you have mentioned how important youth work, youth services and education are. You are probably more familiar than we are with the close link between youth services and education. Issues are being kicked around and being developed to do with where youth services are going in the future. Those services may not stay with education; they may be moved elsewhere. Do you feel that it is important in relation to the issue of suicide, and other issues, to keep a link between youth services and the education service?
1171. Archbishop Harper: I will respond in general, rather than specific terms. This is a cross-cutting issue. It is an issue for the medical profession and the hospitals; the educational service; voluntary organisations that work with young people; and voluntary organisations and statutory bodies that deal with elderly people. It is difficult to imagine how all of those concerns could be addressed by a single Department, but since the issue is a cross-cutting one, it requires a co-ordinated response, rather than an incoherent response. A start has been made on that, and, although perfection has not yet been achieved, it is better to deal with the issue in a joined-up fashion, not least to share information, but to use resources more efficiently. It is better than everyone doing their own thing and having to rely entirely on their own individual resources. It is a no-brainer.
1172. The Chairperson: Gentlemen, it has been really enlightening, constructive and helpful to have had you here this afternoon. I am more heartened than ever that, collectively and individually, you are doing so much to try to deal with the issue of suicide and self-harm. The Royal College of Psychiatrists said that there is no health without mental health. We must also recognise that healthy spiritual lives are also important. I was especially impressed by the efforts that are being made to engage with professionals, including mental-health professionals, in respect of the training events that are being facilitated by the Churches. Through one of my senior advisers, Dr Paul Miller, I am aware of the good work of the Church of Ireland Youth Department (CIYD). Dr Miller’s twin brother, Rev Robert Miller from Maghera, chairs the executive committee of the central board of the CIYD. I applaud that. Equally, I know that much work is being done by all of the Churches.
1173. We must bear in mind, however, that it is not one issue; it is many issues. It requires many groups of people to become involved and connected, and to work in a seamless way. Often we use buzzwords, but life is precious — we all agree about that. The most important outcome for the Committee would be the prevention of people going down the road to completed suicide. Your points of view will be very helpful to us when we collate all of the submissions that we have received.
1174. Even though the Rev Roy Cooper brought his little book that he had prepared earlier, I would ask the Churches to let the Committee have some of their advice literature. It will help us to formulate our end product, which is a report for the Minister.
1175. Thank you very much for attending the Committee. I wish you all a safe and pleasant journey home.
28 February 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Mr Brendan Bonner |
Western Health and Social Services Board |
|
Ms Melanie McClements |
Southern Health and Social Care Trust |
|
Mr Pat McGreevy |
South Eastern Health and Social Care Trust |
|
Ms Gabrielle Nelli |
Northern Health and Social Services Board |
1176. The Chairperson (Mrs I Robinson): The Committee will now have two formal evidence sessions for its inquiry into the prevention of suicide and self-harm. The Committee Clerk has prepared a briefing paper for members’ information. The first session will examine the implementation of the Department’s Protect Life strategy in the four health and social services board areas. Members have been given a copy of the boards’ submissions.
1177. On behalf of the Committee, I welcome the first set of witnesses. I apologise for the late start and for having to go through the Committee’s general business first. I welcome Mr Brendan Bonner from the Western Health and Social Services Board, Ms Melanie McClements from the Southern Health and Social Care Trust, Mr Pat McGreevy from the South Eastern Health and Social Care Trust, and Ms Gabrielle Nellis from the Northern Health and Social Services Board. I invite you each to make a five-minute presentation, and then we will have a question-and-answer session, lasting about an hour.
1178. Ms Gabrielle Nellis (Northern Health and Social Services Board): I am employed as a suicide-prevention co-ordinator in the Northern Health and Social Services Board. On behalf of all four of us, I thank the Committee for inviting us to give evidence. To save confusion, I should explain that we each represent a board area, but some of us are from boards and some are from trusts. In our presentations, we will cover areas such as background and funding processes, and to illustrate our points, we have each selected a couple of examples of achievements or developments that have been made up to this point.
1179. The Northern Health and Social Services Board and the Northern Health and Social Care Trust both cover the council areas of Coleraine, Ballymoney, Ballymena, Moyle, Cookstown, Magherafelt, Antrim, Carrickfergus, Larne and Newtownabbey. The board deals with a population of over 400,000.
1180. A multi-sector steering group was set up in February 2007 to implement the local suicide-prevention action plan of the Northern Health and Social Services Board and the Northern Investing for Health Partnership. That action plan implements the objectives of the Protect Life strategy, and the joint steering group deals with both the suicide-prevention strategy and the ‘Promoting Mental Health Strategy and Action Plan for 2003-2008’ to ensure that there are no overlaps and that both strategies complement each other.
1181. So far, at least 42 representatives from statutory, voluntary and community organisations — including Family Voices — community networks and local forums, churches, the education sector, youth services, mental-health services and local councils are involved in the steering group. I am sure that I have missed out some sectors, but that gives you an idea of who is involved. They have been developing joined-up working, local needs assessments and local action plans. The partnership agreed that there was a need for a co-ordinator to help implement the action plan. I was employed as the Northern Board’s suicide prevention co-ordinator in March 2007, and the review of public administration (RPA) means that I am working on a temporary contract until September 2008. I am the only co-ordinator in the Northern Board area.
1182. I have played a leading role in the development of the local action plan through local partnerships, developed effective communication with the partners and researched models of evidence-based effective practice for guidance on suicide-prevention initiatives in the local communities. I have also co-ordinated relevant training on, for example, ASIST — the applied suicide intervention skills training — and recently, with the Northern Board’s drugs and alcohol co-ordination team, I co-developed training to meet gaps in drugs and alcohol-related abuse-prevention training. That programme is called DASH — drugs, alcohol, suicide and self-harm prevention practitioner training. I am also involved in other strategies.
1183. The suicide-prevention and promoting mental-health action plans 2007-08 were finalised in May 2007 through consultation with local communities. In July 2007, open advertisements were placed in the local and regional press to attract funding applications to implement those action plans. A funding-assessment panel that comprised cross-sector representatives met for five days to assess the bids that were received.
1184. I have selected five examples to demonstrate how much of the work that has contributed to the Northern Board’s achievements, particularly that which concerned community involvement, is continuing into 2008-09. Through the Northern Board’s community small grants scheme, the board allocated funding for each council area via 10 community networks that cover all the Northern Board areas. That amounted to £220,000. Those networks have links to many and diverse local youth and community groups in every community in the Northern Board, and they involve a lot of rural outreach work. The small grants scheme promotes suicide-prevention and mental-health initiatives in the local community.
1185. The Northern Board’s ongoing public-awareness campaign has been effective in engaging communities, of which seven have been involved so far. It is led by the community networks on our subgroup and by me. It is open to people of all ages from all communities in the Northern Board, and it aims to provide communities with information on local and regional support. Furthermore, it aims to reduce the stigma that is attached to seeking help, encourage local community actions, promote small grant schemes, provide support for the bereaved, and highlight the local and regional developments that have been made in suicide-prevention schemes.
1186. Community networks such as Coleraine rural and urban network (CRUN), south Antrim rural network (SARN) and Newtownabbey community voice have come together to co-ordinate two suicide-prevention conferences, which will be held in March and April. They will target people from the Northern Board areas. The south Antrim rural network, in tandem with the Northern Investing for Health partnership and the Northern Board, has been taking the lead on a successful funding application to the Big Lottery Fund’s Safe and Well funding. Money received from that will be used to consider the feasibility of developing community-support hubs in areas across the Northern Board. That will provide community ownership and capacity building in order to reduce the extent of mental-health issues in local communities.
1187. I am also proud of an inter-church day that we organised on suicide and self-harm. More than 100 inter-church and inter-faith people turned up for what proved to be an informative day. Through evaluation, we have agreed to make that an annual event and develop work that arises from that.
1188. Ms Melanie McClements (Southern Health and Social Care Trust): I am assistant director of promoting well-being in the Southern Health and Social Care Trust. I have responsibility for community development, health improvement and the work of the health action zone.
1189. The Southern Health and Social Services Board is tasked with leading the implementation of the Protect Life strategy in the southern area. To date, the work of its strategy steering group has included the commissioning of two pieces of research to identify needs and develop primary-care staff training. It has also been involved in campaigns that encourage the disposal of unused medicines, and it has established a community engagement forum, and commissioned services from the trust and its partnerships.
1190. To complement that approach, the Southern Health and Social Care Trust, led by its director of mental-health services, has identified suicide and self-harm as priorities on which action must be taken. Several consultation meetings have been held, which has led to the establishment of a Protect Life implementation group. That group is chaired by the trust and comprises 40 partners from the community, voluntary and statutory sectors.
1191. A joint action plan has been developed, reflecting the priorities of the regional strategy and the requirements of our local communities. To inform the work, all partners have implemented a common needs-assessment framework that considers prevention, intervention and postvention of suicide and self-harm.
1192. The Southern Health and Social Services Board was allocated £406,000 in 2007-08 from the Protect Life strategy, £232,000 of which was allocated non-recurrently to the Southern Health and Social Care Trust to support the work of the inter-agency group. Of that, 15% was allocated to trust-based work and 85% to the community and voluntary sector.
1193. Implementation of the action plan has resulted in: the appointment of two community-development workers to work in local communities — one with the Niamh Louise Foundation, and one with PIPS Newry and Mourne; seven local community resource centres to provide drop-in facilities, assessment and signposting to a range of supportive services and health programmes; increased counselling provision and post-bereavement support; a multi-agency awareness-raising and training programme; local databases to facilitate self-help and access to services; and a cross-border suicide conference to showcase best practice and the support that is available in local communities.
1194. Mentoring programmes are being developed to target the requirements of at-risk young people, and initial groundwork has been done to develop effective inter-agency protocols. We have also been given the opportunity to participate in an international research project on self-harm and suicide prevention. That project aims to influence future service shape and design.
1195. The focus in the Southern Health and Social Care Trust area has been to establish a strong needs-led approach with an emphasis on inter-sectoral and partnership approaches.
1196. Mr Pat McGreevy (South Eastern Health and Social Care Trust): I am one of the suicide-awareness co-ordinators in the South Eastern Health and Social Care Trust, but I am here to represent the Eastern Health and Social Services Board. The Eastern Board has two trusts — the South Eastern Health and Social Care Trust and the Belfast Health and Social Care Trust, which have a combined population of 660,000.
1197. Before those trusts were established, community of interest groups were set up in south and east Belfast and Castlereagh, north Down and Ards, north and west Belfast, and Down and Lisburn. Those groups bring together community, voluntary and statutory partners to plan, agree priorities and decide how strategy moneys should be invested. To date, 120 groups and organisations are represented in the community of interest groups. The model is bottom-up and ensures that there are local decision-making processes to direct and shape investment and service delivery.
1198. The Eastern Board has also established a suicide-strategy implementation group to enhance co-ordination in the board area, exploit the benefits of joined-up service delivery and report to the suicide-strategy implementation body. Several themes have emerged from the work of the Eastern Board, including: support for bereaved families; raising awareness; education and training; counselling services; mentoring services; support for those who are at risk; complementary therapies; and greater co-ordination throughout the board area.
1199. Funding for the four communities of interest groups comes from the Investing for Health strategy. Those groups decide collectively what the priorities are for that money, and they then commission services and implement a service-level agreement approach to fund the schemes that are chosen. Partners and groups in a community of interest group can bid against project-development moneys to explore and meet previously unmet requirements.
1200. I will highlight four of the main achievements in the Eastern Board area. First, the applied suicide-intervention skills training began in the Eastern Board area through the work of the former Down Lisburn Health and Social Services Trust, and there are now 170 trainers across the region. The next training for them begins in two weeks. Two candidates from south Wales will be joining us, given the situation in that area.
1201. We are pleased to be building on the training that is available for families who have been bereaved by suicide and for people who facilitate support groups on their behalf. Therefore, we are pleased that Dr Frank Campbell from Baton Rouge in the United States will attend the next stage of that training next month.
1202. We have noticed that some young people who are at risk do not engage well with mental-health services. There is therefore a need to expand floating support for those young people. That support has proved successful in helping the young men, in particular, and young women who are at risk. Indeed, it has saved lives potentially. We now have a better and quicker response to families who are bereaved and affected by suicide so that we can provide them with a timely and more accessible service.
1203. Mr Brendan Bonner (Western Health and Social Services Board): I am the Investing for Health manager in the Western Board area, and I have responsibility for community development and all aspects of health improvement.
1204. When the draft strategy was launched, we immediately started a public consultation process, to which over 108 organisations and individuals responded. The key developments that they wanted to see were: greater integration in the community and statutory organisations; more intensive support for people who have been bereaved by suicide; support for the most vulnerable, particularly young people and people with mental-health problems; better links with other strategies and initiatives beyond suicide prevention; more accurate information about what is happening; quicker response times to any issues that have been raised; improved access to services; and greater user and service involvement. In response, we immediately set up the Western Suicide Strategy Implementation Group (WSSIG). The group has 14 members, seven of whom are from the statutory sector and five of whom are from the community and voluntary sector and two from families. It has two co-chairs, one from the statutory sector and one from the non-statutory sector. The group nominates representatives to the families’ forum and the suicide strategy implementation group, and it makes recommendations on funding.
1205. Initially, we agreed to focus on non-recurrent funding to address the immediate priorities of pilot projects, information, data issues and community grants. It was later agreed that it was time to adopt a long-term strategy that was about a redesign of the whole service, not only in the statutory sector, but in the community and voluntary sector. That redesign includes several initiatives. A new pilot initiative with the PSNI on the reporting of suspected suicides is in place. We have redesigned the roles of the suicide awareness co-ordinators to provide intense, immediate support for families and communities.
1206. We have developed a community response plan, which is being implemented in all the councils, to deal with potential cluster suicides. We have created the new post of strategy-link officer, whose job is to link not only strategies in health and social care, but initiatives such as neighbourhood renewal and extended schools. We have given recurrent funding to Foyle Search and Rescue Service, which is a voluntary organisation that works in the north-west along the River Foyle. We have a training and development programme, the particular priorities of which are the applied suicide-intervention skills training, mental-health first aid and safeTALK training programmes.
1207. Two new posts have been created to deal specifically with self-harm in accordance with National Institute for Health and Clinical Excellence (NICE) guidelines. We are about to sign a contract for a new integrated community delivery project in the community sector to support the networking and delivery of services for community and voluntary organisations. Some of the young people who are involved developed a youth-support programme that identifies a number of priorities that they wish to have addressed. We have introduced intensive support for quicker access to counselling for families who have been bereaved by suicide. One project in particular considers the relationship between mental health and debt. We are also committed to the ongoing monitoring and evaluation of all initiatives.
1208. We are involved in four other initiatives. A pilot mentoring project is being delivered by Zest, which is a community and voluntary organisation. We are involved in a cross-border initiative on the recording of self-harm. We support the review of child and adolescent mental-health services (CAMHS) and the implementation of the recommendations of the Bamford Review. We are involved in ensuring that the mental-health promotion strategy is closely aligned with the suicide-prevention strategy.
1209. On behalf of the boards, I thank the Committee, and we are happy to take questions.
1210. The Chairperson: Thank you for those interesting presentations; the list of members who wish to ask questions is growing.
1211. Do the boards and trusts have any facilities to deal with a young person who presents at an accident and emergency department and is anxious, stressed and talking about suicide? Would they be sent away with a card to say that they will get an appointment for a consultation, or would something be done at the accident and emergency unit?
1212. Mr McGreevy: In the first instance, they would be triaged by staff in the casualty department. If it is clear that they are at risk, or are having suicidal thoughts, they are offered a mental-health or a psychosocial assessment from mental-health services. There is a daytime service, and most places have an out-of-hours service to ensure that people are seen. Depending on their assessment, they may be admitted, offered an urgent psychiatric appointment, or some type of follow-up. That is the system in most areas.
1213. Mr Bonner: The situation would depend on the condition of the young person when they arrive. If he or she has consumed alcohol or taken drugs, we would have to wait until they are in a condition that allows us to be able to talk to them.
1214. One of our concerns — particularly in the Western Health and Social Services Board area — is that around 950 admissions to acute services present with self-harm. That is a huge demand on staff resources, and that is one of the reasons that we have created those two new posts to deal with self-harm. We can ensure that, once a person is discharged, follow-up is available. That follow-up is available not just from the statutory sector; we can also ensure that the community and voluntary sector is tied into the process.
1215. Mr Easton: It seems as though a great deal of good work is going on. One of the witnesses mentioned the seven drop-in centres. When the Committee was in Dublin, it visited a centre that is similar to a drop-in centre. That centre is doing a lot of good work. Are centres such as that specifically for people who are threatening suicide? Do the board areas have similar facilities? The Committee was excited about the instrumental work going on in Dublin, and we would like to see something similar introduced in Northern Ireland.
1216. Speaking as a member of the public, I do not see any evidence on the ground of the work that you are doing. How is the stigma being broken down, and how is your message being put across to the general public? I am referring not just to community groups, but to groups right across the board. Everyone is affected.
1217. When the Committee visited the Everton Complex in north Belfast, some of the community groups that we met complained about the lack of a joined-up approach, sharing views and accessing information. They also spoke about longer-term funding and about the problems of being funded on a year-to-year basis only. How are those issues being addressed?
1218. Ms McClements: I will answer the first part of the question about resource centres. Predominantly, we want resource centres to be available for self-referral; if someone wants help, they should feel that they can open the door and, hopefully, be empowered and proactive enough to access that service themselves. However, we also want the range of partners with which we work — not just those in the statutory sector —to recognise those centres as a resource into which they can signpost people. We also hope to build a range of statutory services into the resource centre so that it operates as an outreach model. We have the potential to further introduce a range of other services, such as a parenting-support programme or a counselling service.
1219. The board commissioners asked us to pilot one such centre in the southern area. However, when we engaged with the community and voluntary sector partners, they were not happy about piloting just one centre. They pointed out that if a centre were to be piloted in Kilkeel, someone from as far away as Armagh might need help. We felt that we needed to go for an equitable approach across the area, which is why we have gone down that route. The process is in its first year, and we are aware that the seven centres are at different stages of going live. However, there is a commonality in services; for example, the meet-and greet-facilities, drop-in services, someone skilled to assess a person’s needs and to see whether onward referral is needed, and the facility to make the range of support programmes fully available to the person in question. It is an exciting development that has potential.
1220. We have a range of public relations campaigns that involve more than just sending messages to groups. They can involve live work with the media and working in harmony with our partners. If some of our partners have information relating to mental health or suicide prevention, we will work in a joined-up way to get that across. Partnership and non-recurring funding are important issues for us; in order to build credibility and commitment, especially from community and voluntary sector partners, the money needs to be released to trusts recurrently so that we can build sustainable resources.
1221. Mr McGreevy: In the Eastern Health and Social Services Board area, families bereaved by suicide saw a need to open drop-in centres. People at risk of suicide and people who were worried about someone at risk of suicide focused on those centres. The Eastern Board has supported and funded Reaching Across to Reduce your Risk of Suicide and Self-Harm (RAYS) on the Shankill Road, PIPS in north Belfast, and the suicide awareness and support group. Although the centres were set up primarily to consider families bereaved by suicide, they are also examining prevention, awareness raising, intervening with people at risk and looking after families that have been bereaved and affected by suicide; all those measures are supported by the board.
1222. Unlike Scotland and the Republic, we do not have a designated suicide prevention office to get the message out. However, perhaps the suicide strategy implementation body (SSIB) will consider that matter. There is no central focal point that can be visited or accessed by people who want to find out about suicide prevention.
1223. Mr Bonner: Drop-in centres may work very well in an urban setting. In the Western Board area, however, we have a huge problem with rural issues and suicides. One cannot, therefore, have drop-in centres, which makes things difficult. However, the board is working with organisations that provide that type of support — for example, an organisation in Derry called Zest: Healing the Hurt and other organisations such as Foyle Search and Rescue, which is not a drop-in centre, but its personnel walk the banks of the Foyle.
1224. The Chairperson: We met representatives from Foyle Search and Rescue and were very impressed with what they do.
1225. Mr Bonner: It is more to do with outreach, which is an alternative to a drop-in centre. Regarding publicity, we had a series of bus campaigns — Don’t Drown Your Sorrows — and the current campaign, Listen. We also had a television advertisement campaign — If Your Head’s Away, Just Say. There has been a series of articles in the press advising people where they should go for support when they need it, and we are working with councils to make local representatives aware of what services are available. We agree with the joined-up process, which is why we are about to sign the contract on the integrated community development project.
1226. Recurrent funding is a big issue. When this new money became available, the first message that we were given was that it was not to be used to fund services that already existed; it was for new initiatives. Immediately, there was a challenge: existing organisations were delivering excellent services, but we could not fund them from this new money. Therefore, we have tried to be innovative and get them to collaborate through the integrated community development project.
1227. Ms Nellis: To be honest, the Northern Board is a bit behind in bereavement support. However, in relation to support centres and self-help issues, there is a massive gap in bereavement services in the Northern Board area, which is extremely rural. A community development worker will soon be employed for three years through the Northern Health and Social Care Trust to work with communities across the region to establish bereavement support facilities.
1228. In addition, the community networks have made a grant application to the Big Lottery Fund’s Safe and Well programme. Across the Northern Board, the networks target a range of small rural areas that cannot always be reached by services. Even I, for example, cannot get out to every area on every occasion. The networks are a perfect way to get the word out. They can work not only with constituted groups but with the general public. The networks decided to make the grant application in partnership, because, in order to be successful, it needed to be a statutory, community and voluntary sector partnership. The support hubs are not only for people who are affected by suicide or self-harm but they will try to redress the issues that might lead people to such a situation — for example, financial or relationship crises. People will know who to approach locally.
1229. Lack of transport is another problem; people cannot travel to the bigger towns such as Ballymena and Antrim where the services are based.
1230. The community networks have been fantastic in getting the word out. If it had not been for their taking a lead on many issues, much work in the past year would not have been done so quickly. The community networks and I led on the public-awareness campaign, which has been open to all. We advertised in all the local chronicles, church bulletins and newsletters, and flyers were put through letter boxes.
1231. On average, 50 to70 people turn up at meetings. In areas such as mid-Ulster, where the suicide rate is higher, we had large attendances. The good thing about opening it up to all is that we can emphasise that it is not a “them and us” situation: even people who work in statutory services can be affected by suicide at any time. We have been trying to get the message across that, if people live or work in the Northern Board area, they are a part of the community.
1232. The general structure of the meetings is as follows. I talk about the overall picture of the Protect Life strategy and about everything that is happening locally in order to keep people up to date with that. People from the Samaritans talk about general suicide awareness in the local community. PIPS has participated in every awareness night that we have held. Its representatives emphasise that the community can come together to develop something in its own area: it does not have to wait for ages to get money to organise. PIPS started from a couple of concerned people.
1233. After the meeting, people can mingle and get information on support services. I bring along a lot of information about statutory and voluntary organisations that can help the local community. We have had present: bereaved people; people who have been through the psychiatric services; and local district council representatives, who can help to get something up and running in the local community. Statutory services sometimes turn up, as do voluntary sector organisations such as Contact Youth and Aware Defeat Depression, which can provide some support. It is a large area, but so far, so good.
1234. Ms Ní Chuilín: I am keen to find out whether there is a standardised approach to training with the PSNI when suicides occur. More often than not, the PSNI are the first on the scene. Recently, there has been an improvement, but that has not been the experience across the board. Is that within your remit? If so, can you explain that standardised approach?
1235. Can you tell us about the after-hours services in your areas. When Committee members visited the Mater Hospital, we talked about the establishment of an after-hours service on site.
1236. You are correct about rural areas: the rural experience is completely different to the urban one. Rural people should have equal access to services. People should not be excluded because they live in the countryside.
1237. Mr Bonner: I will answer your question about the PSNI. In the past, the problem was that, when a suicide occurred, most health officials were unaware of it, until the community or — more likely — the press contacted them for a comment.
1238. Therefore, we worked with the PSNI and the Chief Forensic Medical Officer to devise a mechanism whereby, when suicide is suspected, a report is sent to the Western Trust. That report gives details of the location and the methodology. An important element records whether police officers have spoken to the family and whether our services can approach the family to offer support. That report is sent to the trust and is referred to the suicide co-ordinators, who then contact the family.
1239. We can now monitor what happens so that we can pick up quickly on whether clusters are forming. We look for connections: are they known to mental-health services? We are working with the PSNI to ensure that all officers likely to attend the scene of a suicide undertake ASIST training; all forensic medical officers should also undertake ASIST training. The PSNI is also considering whether they can embed safeTALK training and make it available to all officers. At the moment, that is available only in G division in the north-west; we are now rolling it out to F division in the south-west. It has been in operation only since October, so it is too early to try to ascertain how effective it has been. We have noticed, in talking to bereaved families, that early intervention of the available services and a connection with them has been important.
1240. Access to out-of-hours services is still being developed. However, community and voluntary sector organisations have told us that, because of the awareness that has been created, they are getting better access to out-of-hours services and are receiving the support that they need, which had not happened previously. The system is not perfect and much work remains to be done. However, we are committed to pushing that through.
1241. Ms Nellis: During the most recent ASIST training for trainers course, a PSNI community policewoman joined our team as a trainer. She has since started to do more awareness work in the Police Service and is trying to get the work joined up regionally. Little things like that are happening, which has been very beneficial for links with the police,
1242. I am a youth and community worker and am still learning a lot about the services offered by the Northern Health and Social Services Board. However, I am aware that there is an out-of-hours crisis response service in Antrim that deals with self-harm and suicide. We will soon link up closely with the mental-health management team to try to bridge the gap between its work and development work in the Northern Board area, because that team connects with many bereaved people. It is possible to see trends in certain areas and age groups, so a subgroup will shortly be set up; meetings have already been held to arrange that.
1243. Mr McGreevy: Working with the police is crucial because, being the first on the scene, their attitude can affect a bereaved family and how they feel about help, and hope, in general. If a family experience an insensitive reaction from those first responders, it can put them off seeking help at all, so it is crucial that the police are aware of, and sensitive to, the needs of families.
1244. A couple of initiatives are already in place in the Eastern Board area. We have developed a training programme for police officers that raises awareness about suicide, considers what can be done to intervene with people at risk and also deals with the issue of responding to bereaved families in a sensitive manner. Many reports state that police officers are sensitive in most cases. However, there can still be thoughtless comments that can have a long-lasting effect — hence the training for police in the Eastern Board area.
1245. Ms McClements: After the spate of suicides among young people last summer in the Southern Trust areas of Mullavilly and Tandragee — of which I am sure you are aware — PSNI engagement with the Southern Health and Social Care Trust was terrific. Something positive that came out of that engagement was not only the need for local training but the idea that we will influence the foundation training for new officers on the necessary skills.
1246. The internal communication processes in the PSNI came to light, because different officers and different divisions did not necessarily communicate with one another, so they have started to work on that. The PSNI is working with us on inter-agency protocols, from the first response, to the media, funeral directors, the PSNI and our own service. It can be difficult to ring a trust and try to talk to the appropriate person. Therefore, we must examine our internal arrangements and consider how people access our service and get to the right person, so that has been beneficial. The PSNI has also been involved in community schemes — for example, schemes such as midnight football, which provide a diversion for young people, have been terrific. The PSNI involvement has been positive.
1247. Our crisis response teams work out of hours, and we have also been working on a self-harm pathway to consider people receiving immediate responses within the first 24 hours or the first three days, depending on their level of need. The value of the partnership and the resource centres is important, because we have a mixed economy, and can examine the skills in different sectors. Therefore, we are able to tell people who are living in a rural community that, although they might not be able to access their local A&E department, there is a service in their local community — through the voluntary and community sector or the statutory services — that we hope they can connect with.
1248. Mr McGreevy: The South Eastern Health and Social Care Trust is working on a document that we hope to leave with families that have been bereaved by suicide. It will outline the role of all the people who will respond to them, from the ambulance paramedics to the police, their GP and the clergy. The family will therefore know what those people do and what they can expect from those services.
1249. Dr Deeny: I welcome Gabrielle, Melanie and the two gentlemen whom I already know, Pat and Brendan. One of you mentioned suicide clusters; I have been reading that another two young boys who attended a school in County Mayo have committed suicide, eight days apart. My thoughts are: here we go again.
1250. In the coming days, another family will bury a daughter in County Tyrone following a terrible car accident. I have been working as a doctor for 27 years, and every death is tragic and devastating. However, if I had to select a worst cause of death, it would be suicide, because of the devastation it brings and the work that it requires of doctors. I mean no disrespect in saying that, and you all mentioned how everyone must work with the devastated bereaved families.
1251. My main interest is prevention. As I have said to other members of the Committee, young people are taking their lives before doctors, relatives and friends even know that there is a problem. The first we hear is that they are dead. Those young people experience a vulnerable period of a week, or perhaps even a couple of days. If, during that time, they can be persuaded to contact someone who can talk them through that difficult period and follow-up therapy can be provided, if required, that must be the way forward.
1252. Melanie, you talked about drop-in centres. How qualified are the staff? Brendan rightly said that there is a difficulty with locating drop-in centres in rural areas. However, that should not exclude access to support, and I know that he was not suggesting that it should. The Committee has talked about how every child knows about ChildLine. We need a catchy phrase so that people know who to phone for help. There must also be the facility for immediate, direct referral, not only by medical staff, police and accident and emergency departments but by friends, spouses and girlfriends, who can phone and get immediate help for the individual concerned.
1253. Brendan, you told the media that you have informed people of where they need to go for help. To what places did you advise them to go? To repeat my colleague’s words, last week the Committee was highly impressed when it visited the Pieta House facility in Lucan. It provides exactly the service that I outlined, although it is not yet available 24 hours a day. It provides direct, immediate access to services and the facility of self-referral to help people through that extremely vulnerable period. Staff there told us that 1,100 people have used the facility in the past two years, and, as far as I know, not one of them went on to take his or her life or to self-harm. That is staggering. If our Health Service were to match that achievement, we would be extremely proud.
1254. I used to work as an out-of-hours doctor, but I can no longer do so because I have to run about all over the place. However, during that time, out-of-hours doctors were accompanied by a community psychiatric nurse — not throughout the night but at least a specialist health professional was available. Perhaps we should consider that option, because there must be immediate, direct referral to prevent the suicide of people who never become clinically depressed but simply experience an event in life that to them was a crisis. To the rest of us, it may be nothing more than a life event, and someone could talk them through it.
1255. Mr Bonner: As over 70% of people who take their lives are not known to mental-health services, your point is correct. Last year, in response to a suicide by a relative of mine, we took a particular course of action. He had been involved in a sports club, so we went there, through the community and voluntary sector, and we worked with the coaches and parents to persuade them to talk to the young people. They identified five serious cases, and one parent went on to prevent a suicide.
1256. It is a matter of local intervention and encouraging those who work with, and are trusted by, young people to talk to and listen to them. We want that strategy to be rolled out more widely, particularly the safeTALK programme, which is a good example that can be adapted and to which people respond well.
1257. I agree that there must be immediate support available when people need it, particularly for those with mental-health problems and their families, because the carers are also at risk and require support. A regional helpline is due to be launched, although there is much debate about it being rolled out before it has been evaluated, but at least it will be a service that people can contact.
1258. Dr Deeny: Is that helpline for Northern Ireland?
1259. Mr Bonner: People seem to forget that the Samaritans is open 24/7. I attended a public meeting in Strabane recently, and a woman there said that there was nowhere for people to telephone in a crisis. When I mentioned the Samaritans, she said that she had forgotten about it. Yet, its reputation and the service that it provides are excellent.
1260. There was a question about the information that we provide in the media. A list of all available services in the community and voluntary sector appears in all the media in the Western Health and Social Services Board area. If someone has a relationship problem, they can contact Relate, or, if they have a drugs or alcohol problem, they can contact the drugs and alcohol intervention education and referral team (DIVERT) or SOLACE.
1261. One of the greatest problems is that the list of organisations can take up a full page in the newspaper; therefore, we are trying to create an integrated approach to reduce the amount of telephone numbers. There are so many organisations out there, and our concern is that every time there is an unfortunate loss of life through suicide, the families affected respond by setting up another project. We must work with those families not to create new projects but to get various initiatives working together. That is vital.
1262. Mr McGreevy: I will take up the points about suicide prevention and the media. The ASIST programme is a vital prevention programme. If someone has a heart attack, there are people trained in cardiopulmonary resuscitation (CPR) to help them; the ASIST programme provides a similar service for those who are contemplating suicide. People are trained in the statutory, voluntary and community sectors to recognise signs of distress that may be a warning signal that a person is having suicidal thoughts. Youth club leaders, teachers, bus drivers and the police have all been trained, and that training is continuing to spread. Those people are not therapists; they are first-aiders in suicide. The ASIST programme has been running for five years, and we must keep rolling it out.
1263. The Health Promotion Agency runs a public information campaign, which is a slow-release campaign. We hope that we will soon be able to tackle the issue of suicide and the myths surrounding it. For instance, some people think that talking about suicide puts the idea into people’s heads. Therefore, it is vital that we explode some of those myths through a media campaign.
1264. Ms McClements: Dr Deeny enquired about resource centres. They are staffed by a range of paid and volunteer staff in the voluntary and community sector, and they manage the seven resource centres. When we were standardising those centres, we were careful to ensure that the person who meets and greets people has, for example, suicide-awareness/first-aid ASIST skills. Therefore, that is built into the training programme so that the first point of contact can offer some sort of service. We have worked hard to create a locality database for a wide range of issues, including financial, mental-health and relationship issues. Therefore, we can maximise the opportunities that are out there rather than always feeling that we have to recreate new services, which is a big link into signposting. I hope that a regional helpline with a catchy telephone number will also highlight immediate points of contact for people.
1265. The assessment by the psychiatric nurses in our out-of-hours crisis response team is essential. We need to provide services for people outside the 9-to-5 window for that initial assessment and onward referral. Furthermore, there is a healthy living centre in Banbridge, which, according to the 2005 figures, was the area with the highest suicide rate in Northern Ireland. However, that may not be the case any more. A co-funded project among the business community, the GPs, the trust and some of the Protect Life funding examined a service for people at risk in that local healthy living centre. There have now been 150 referrals from GPs to that project. Therefore, there is some value in that pilot project. We know that 80% of people who die by suicide have visited their GP in the past six months, and 36% of them have visited their GP in the past month, not always with a mental-health-related issue. However, we must maximise that critical link between the GP and the community and primary-care fields.
1266. Ms Nellis: You mentioned the model in the South, but I would like to find out more about the Maytree Respite Centre in Finsbury Park, London. It is a community house that offers four nights’ respite for people in a crisis. It is a self-referral centre. I heard about that model at the International Conference on Suicide Prevention in Killarney, and it involves an inter-agency committee. The centre is in a terraced house with gardens, and it offers people a place to stay and basically escape from life for four days. The training that the volunteers receive is similar to that received by those who work in the Samaritans and with the helping skills model, but staff can also give people information on where to access help after they leave. A mother or father can refer their son or daughter to the centre, or people can refer themselves. The centre provides the proper assessment under psychiatric care. If people have been involved with mental-health services, they would need to go back to those services. The centre knows that it cannot take anybody and everybody, and it is a small model, but one that the Committee might be interested in considering. I have not got round to examining it properly yet, but I would like to do so.
1267. On a personal note, the frustrating aspect of working on suicide prevention is that many funding decisions are made on the basis of statistics, and, as everybody knows, those statistics are not definite. There can be a delay in getting definite statistics on suicide — as definite as statistics can be. By the time those statistics are available, the decisions have been made on how much money goes to each area. The money is put in only when the problem gets so big that it can no longer be ignored. However, that approach is more reactionary than preventative. We should be given the money to introduce preventative measures so that the problems can be dealt with before they escalate. For example, I heard yesterday that suicide rates in the south Antrim and mid-Ulster areas are now above the Northern Ireland average, whereas two months ago I was told that the rates were below the average and that there would be no additional in-year funding. Now, however, we might get that funding. Thus, we are given the money because the problem has escalated. In my opinion, that is a problem with any issue in Northern Ireland.
1268. Mr Gallagher: Thank you for outlining the good work that the trusts and boards are carrying out. You all mentioned the resources that are drawn down, particularly for community initiatives — healthy living centres and such like. I often hear how those kinds of agencies have difficulty because of short-term funding arrangements. Does that create difficulties for the trusts and boards? It must be frustrating, because it is important to build trust and develop relationships with those at risk. Those funding arrangements lead to a high staff turnover, and everybody, including the person at risk, is set back as a consequence.
1269. Ms McClements: We now have a strategy with recurrent resource, but we are still being issued non-recurrent resource to trust level. That is an issue in our work to build relationships with the community and voluntary sector. Short-term posts are less of a risk for statutory agencies, because, as a bigger organisation, they can carry that risk. However, a small community group in the voluntary sector cannot take those risks. They must have some form of sustainability.
1270. There is a grey area in that we do not have a solution to suicide and self-harm. We must grow our own local evidence, but to do so involves investing and taking risks. If we opt for permanency and it does not work out, that creates many issues. We need small windows of opportunity to enable us to develop innovative practice, but we really must have recurrent funding. Commitment and vulnerability are big factors, especially for the community and voluntary sectors so we must be able to give some sort of longer-term sustainability.
1271. Mr Bonner: That is a problem for all aspects of health issues, not just suicide. One of our initiatives has three-year funding, and that allows us to commit for three years but also to tie in a robust monitoring and evaluation. That arrangement will help us to decide how that project evolves, so the relationship can be worked on. It is a three-year funding programme with options to develop either an exit strategy or a focus on sustainability. Therefore, we can be open-minded about that programme.
1272. The Chairperson: At the end of January, the Minister announced the introduction of a regional 24/7 helpline. Are co-ordinators aware that that helpline has been introduced? If so, do you think that they can quote the number?
1273. Ms McClements: It is 0800 0808 0880
1274. Mr McGreevy: Is it 0800 800 8000?
1275. The Chairperson:
1276. That seems to prove our point. Given that the pilot exercise is ongoing, the Committee felt that the helpline was introduced prematurely. None of the Committee members could have quoted the correct number either, so you are not alone.
1277. Mr McGreevy: Perhaps the Health Promotion Agency for Northern Ireland (HPA) could be tasked with promoting and publicising the helpline as part of its strategy.
1278. Ms Nellis: There is also talk that the number may be changed to comprise three digits, making it like 999.
1279. The Chairperson: The pilot will prove useful when it is finalised and implemented. The creation of a booklet that can be distributed to every home seems logical. None of us know what is behind a face, even in our own households. Sometimes we do not know what our children are thinking. They cover up bullying and peer pressure, or they are picked on because there is a stigma attached to not wearing designer clothes, for example. Therefore, a booklet containing all the appropriate numbers should be sent to every household, thus allowing easier access to the proper services — when they are established — across Northern Ireland.
1280. I thank all of you sincerely for attending. You have been a great help to the Committee, and I wish you a safe journey home.
28 February 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr John McCallister
Ms Carál Ní Chuilín
Ms Sue Ramsey
Witnesses:
Dr Dermot O’Reilly |
Queen’s University Belfast |
1281. The Deputy Chairperson (Mrs O’Neill): I welcome Dr Dermot O’Reilly from Queen’s University Belfast, who has recently co-authored an article on suicide risk. Members will have a copy of Dr O’Reilly’s article.
1282. Dr O’Reilly, I invite you to make a short presentation, after which members will ask questions.
1283. Dr Dermot O’Reilly (Queen’s University Belfast): Thank you; I shall make a short presentation.
1284. We set out to answer one simple question: are suicide rates affected by where someone lives? Throughout Northern Ireland, and, indeed, in most European countries, there are variations in suicide rates. The question that has been asked is whether those variations have something to do with the areas in which people live, or whether they simply reflect the types of people who live in those areas.
1285. It could be said that people in rural areas are isolated. However, there is a good case for saying that people in certain parts of the cities are also isolated. Cities can be considered to be hostile and antisocial places, which are factors that may increase the risk of suicide. Furthermore, it could be suggested that living in deprived areas is itself depressing, and that may also increase the risk of suicide. Therefore, a case could be made that the character of an area in which people live adds to their risk of suicide.
1286. The question of whether the areas or the type of people who live in those areas increase the risk of suicide could not have been answered previously for Northern Ireland. However, we now have a new data set, called the Northern Ireland Longitudinal Study, which allows us to answer that question and which provides a wonderful tool that enables us to learn more about the health of the population, and, in this instance, about suicide rates. Committee members may want to ask me about that study.
1287. The characteristics of individuals and of the areas in which they live need to be considered. Those two aspects then need to be separated. The longitudinal study starts with the census, which is a rich data source. The mortality statistics for the five years after the census was taken are then examined. Therefore, five years after the census is conducted, we can find out who has died and who is still alive. The factors that are associated with an increased risk of suicide can then be gleaned from that information.
1288. We considered individual factors — the sort of information that the census provides, such as age, gender, martial status, and indicators of the extent of deprivation or disadvantage of the household in which they live. We also considered economic activity, as it is known that unemployment and economic inactivity increase the risk of suicide.
1289. We then added three indicators about the character of the area in which people live. The first concerned deprivation, which, rather than concentrating on the family, asks whether the area itself is disadvantaged. The second was about urban and rural residence; therefore, we used population density, which is a good proxy for that indicator. The third was about social fragmentation, which could be considered as the opposite of social capital, about which the Committee is probably aware. Social fragmentation is evident in a community that is not close-knit and in which people feel isolated and have no sense of cohesion or trust.
1290. More recent research that was published in the British Medical Journal (BMJ) suggested that social fragmentation was even more of a risk factor for suicide than deprivation. That research found that areas with high levels of social fragmentation were more likely to have higher suicide rates. Furthermore, it showed that the more fragmented that areas became, the more likely it was that suicide rates would increase.
1291. By examining individual and household characteristics, we confirmed that the factors that have been shown to increase the risk of suicide in other countries were also relevant to Northern Ireland. Our research found that young people are more at risk of committing suicide than older people; males are three times more likely to commit suicide than females; and single people, including those who are divorced or separated, are at higher risk than those who are in a relationship. I have provided the Committee with more detailed data on that.
1292. Our research also showed that people who live in deprived households are five to six times more likely to commit suicide than those who live in more affluent households. Unemployment also increases the risk significantly. Finally, there is a suggestion that people who live alone are at greater risk of suicide than those who do not, and that could be linked to a sense of social isolation.
1293. We then considered area characteristics. We replicated the analysis that was conducted some years ago in Northern Ireland that showed that people in deprived areas and socially fragmented areas are at a higher risk of committing suicide. We could not, though, identify an urban-rural gradient. However, there was a suggestion — but only a suggestion — that suicides rates tended to be a little higher in both the most urban and the most rural areas, but they did not reach the levels of statistical significance that may have been expected.
1294. When the individual and area factors were added in to the analysis, the area factors lost their significance. Therefore, the conclusion was that individual and household characteristics are important, not where an individual lives, or whether that area is deprived or affluent, urban or rural, or socially fragmented. Let me put the conclusions another way: if a person is young, male, and unemployed, irrespective of where they live — whether their area is deprived or affluent, socially fragmented, urban or rural — the risk of suicide for that individual is high. If a person is older, female, and in a relationship — regardless of where they live — their risk is lower.
1295. The Deputy Chairperson: OK, thank you very much. May I ask whether your findings are at variance with other research, or does it support your conclusions?
1296. Dr O’Reilly: There is no equivalent research in the UK. We could have conducted the research in England, Wales, or Scotland, but because of the Northern Ireland Longitudinal Study, we decided to attempt to find a Northern Ireland solution to a Northern Ireland problem. Our research is in keeping with the wonderful record-linkage studies of some Scandinavian countries. Researchers in Denmark and Finland, where the populations are larger, have examined the issue for several years. Their findings are similar to ours: it is who you are rather than where you live that affects your suicide risk.
1297. Ms Ní Chuilín: Thank you very much for your presentation. I am surprised at your findings because I would have thought that where an individual lived had a bigger influence on suicide risk than you have claimed. I suppose that your conclusions were reached after an assessment was carried out of the various factors that contribute to people ending their lives. However, I am not entirely clear: are you saying that the social, rather than the physical, factors have the real influence? Do you believe that a person who lives in a high-rise block of flats is at no more risk of committing suicide than someone who lives in a house in the same area?
1298. Dr O’Reilly: Areas can be characterised in different ways. We have looked at three such characteristics: deprivation, urban-rural, and fragmentation. I am sure that you could come up with other traits that we have not measured that influence suicide risk. However, we cannot be sure about those traits.
1299. Ms Ní Chuilín: In my constituency of North Belfast, which is a very deprived area that has a massive housing problem and lots of other social problems, there is a lot of self-harming and mental ill-health. The suicide rate is high, particularly among young people.
1300. When we were in Scotland, examining evidence and sharing experiences, we found that older people living in rural communities, particularly the Highlands, were at the greatest risk of suicide. Therefore, we automatically thought that where a person lived was a massive contributory factor. I am not contradicting what you are saying; I am not in a position to do that. However, having read your paper and heard your testimony, I am surprised that you do not consider that where a person lives has a greater impact on their risk of suicide.
1301. Dr O’Reilly: I concur with your feeling. Understandably, deprived areas have the highest rates of suicide in Northern Ireland. People who are deprived and live in materially disadvantaged households are, by and large, based in impoverished areas. Therefore, the rates of suicide in deprived areas are higher, not because the area itself is destitute, but because there is a high concentration of deprived people in that locality. We are merely suggesting that if those people who are deprived happened to live somewhere more affluent, they would be at the same risk of suicide.
1302. Ms Ní Chuilín: Do you believe that it is the individual rather than the environment that affects the risk of suicide?
1303. Dr O’Reilly: If you walk or drive around deprived areas, they are depressing to look at. However, that does not seem to add anything to an individual’s risk. I should also point out that the risk factors for self-harm and suicide are not quite the same. The epidemiology and risk factors overlap to a certain extent, but there is a distinct epidemiology behind both self-harm and suicide. Therefore, we cannot make a direct comparison.
1304. The findings for Northern Ireland might not apply in other parts of the world. Our findings equate to those from some Scandinavian countries. However, in certain parts of the United States, suicide rates tend to be higher in rural than in urban areas, but in other parts of the world that is reversed. To some extent, the results depend on the country.
1305. Dr Deeny: Thank you, Dermot. I am interested in this topic, as a GP and as a member of the Committee. I am a little surprised, but not completely shocked, at what you say about social fragmentation. We tend to think that rural communities are strong and that people help each other, but some suicides still shock us completely, so what you say does not entirely surprise me.
1306. Given that you attribute the risk factors to individual circumstances, does that suggest that we should examine families that have a history of suicide? Your research looked specifically at areas, but it does not explain why so many more men than women — especially young men —commit suicide and why many more young women self-harm.
1307. Dr O’Reilly: No; that was not the question that the research set out to answer. There is a tendency to examine individual suicides from which to extrapolate theories. That cannot be done. The circumstances surrounding each suicide are unique. We have tried to draw out the general patterns from the 566 suicides in Northern Ireland that we examined. One or two cases may not fall into the pattern that we have established, given that those people were influenced by what happened locally. Our results show what happens in general. We cannot say what the risk factors are for individuals or why men, especially young men, are more at risk of suicide.
1308. Another study has been commissioned by the Northern Ireland research and development office, of which the Committee will know. That is a psychological autopsy study that will try to understand, as far as possible, the reasons behind suicide in individual cases.
1309. Dr Deeny: Is it possible that family history plays a part?
1310. Dr O’Reilly: I really cannot answer that from the data, and I do not want to speculate. I must be careful, because some people might think that there is a genetic propensity towards suicide. I suggest that, if suicides happen to occur in certain families, the reasons are much more likely to be environmental. Families share much more than genes; they share an environment as well as levels of material disadvantage, isolation and so on.
1311. Ms S Ramsey: On that point, I know that Dr Deeny was not implying anything, but we must be careful not to scaremonger. We are dealing with several families who are suffering because of suicide or self-harm, and we do not want to add to the pressure that they are under by assuming that other family members could take their own lives. We must conscious of that.
1312. The Deputy Chairperson: How do your research findings correlate with the suicide-prevention strategy? Do you feel that, based on those findings, the strategy must go in a different direction?
1313. Dr O’Reilly: No. About five or six years ago, there was a suggestion from the research field that we needed to take the policy initiative in a different direction and that we needed to examine specifically certain factors at an area level. This is where it gets tricky. When I say area-level factors, I do not mean that we should not concentrate on areas. It is evident that we should do that, because, for example, there are likely to be many people at risk in deprived areas. However, we should not aim to change the characteristics of areas and expect that to have an impact on suicide risk. The evidence from my study, and from the Scandinavian studies, suggests that that will not have a significant impact on suicide risk.
1314. The Deputy Chairperson: As members have no more questions, I thank you for coming today to help us with our inquiry.
Correspondence from Dr Dermot O’Reilly
Hugh,
Yesterday, the chair asked if our study findings would indicate a need to change anything the orientation of the mental health strategy. My response now would be ‘yes’.
While the current efforts focus on the need for support for individuals and especially for younger people (all very worthwhile and probably useful approaches), it ignores the wider social background to suicide risk. Our research clearly shows that suicide risk is greatly increased amongst those not in employment and those individuals living in disadvantaged circumstances. The corollary to this and the point to be made is that factors which improve the levels of employment and increase the social wellbeing of the population are likely to have a significant impact on suicide risk for the Northern Ireland population. As is often the case, the factors that most impact on our health lie outside the caring and curative services.
It might be informative if these sentiments could be included in the report.
With best wishes
Dermot
13 March 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr John McCallister
Ms Sue Ramsey
Witnesses:
Mr Noel Graham |
Northern Health and Social Services Council |
|
Ms Maggie Reilly |
Western Health and Social Services Council |
1315. The Chairperson (Mrs I Robinson): I would like to apologise to Noel and Maggie from the health and social services councils for having to cancel an evidence session that they had previously been due to attend, and for cancelling it very late in the day. We had to postpone it because of the Committee’s consideration of the clostridium difficile issue. However, you are here now, and I would like to welcome you on behalf of the Committee. I invite you to make a five- to 10-minute presentation, and then we will allow up to an hour for discussion between members and yourselves on any issues that they may wish to raise.
1316. Mr Noel Graham (Northern Health and Social Services Council): Thank you for inviting us to give evidence on behalf of the health and social services councils to Committee’s inquiry into the prevention of suicide and self-harm. Our response is on behalf of the four health and social services councils. My name is Noel Graham, from the northern council, and my colleague Maggie Reilly is from the western council.
1317. I will first provide some background on the health councils. They were set up in 1991 as statutory bodies charged with representing the views and opinions of the public. The councils are based in four local offices — in Belfast, Broughshane, Lurgan and Omagh — and are independent from those who plan, manage and provide health and social care.
1318. The subject under discussion today is something in which individual councils have taken a keen interest. We submitted a written response some time ago, following a joint council forum that was held on 25 October 2007, which discussed the Protect Life strategy. Before discussing that issue, members of the four health councils heard presentations from Colm Donaghy, who chairs the regional strategy implementation body, a GP, a suicide awareness co-ordinator from the western area, and Ann McGarrigle of the Families Forum.
1319. Councils have raised concerns in the past about the lack of a co-ordinated approach to suicide prevention, and the most recent phenomenon of suicide clusters among young people in Northern Ireland.
1320. We note that there are four main points in your terms of reference, and we hope to address those in turn. The first is about assessing the scope and appropriateness of ‘Protect Life: A Shared Vision’. Prevention of suicide and self-harm is not just a health or social care issue. The strategy is led by the Department of Health and Social Services and Public Safety, but implementation of most of the actions will depend largely on working in partnership with other agencies. We strongly believe that the strategy should have had a wider cross-departmental authorship and, perhaps, could have been championed through the Office of the First Minister and deputy First Minister (OFMDFM), as was the child poverty strategy.
1321. We welcomed the population and the targeted approach that was used in the strategy. The first section deals with population approach. We feel that, in that section, there needed to be a specific action for children and education: after all, children spend anything between 12 and 17 years in education. Regarding the action-area dealing with communities, we endorse the public information campaign that has begun, but we want ongoing action, not just a short-term approach. We agree that public policy has the potential to have an adverse effect on the mental health and well-being of local communities. The strategy encourages all statutory public bodies to carry out health impact assessments on their policies, but we ask how that will be monitored and who is responsible for carrying it out.
1322. In principle, we agree with the actions identified in the strategy in relation to the family. However, we question whether, in practice, such support-mechanisms are in place, and we are concerned that the success of the support and interventions proposed will depend on the capacity of , and the funding available to, the voluntary and community sectors.
1323. The next action-area dealt with children and young people. We are concerned that the level of investment required for children and adolescent mental-health services, as envisaged by the Bamford Review, has yet to be realised. The current target for outpatient waiting is 13 weeks, which is not being met, and is far too long for children in crisis to have to wait for appropriate intervention. We want to see a greater priority in developing and implementing practices, protocols and referral pathways, to smooth the transition from youth to adult health and social services.
1324. Regarding the action-area concerning health and social services, we fully support the suicide and depression awareness training, as a priority for all front-line staff dealing with people in distress — particularly for GPs, primary care and accident and emergency (A&E) staff in the health and social services. We have some concerns about the varying levels of uptake by GPs of this training: uptake in some areas has been slow. We want to see evidence that, where one GP from a practice has been trained, knowledge has been cascaded to other staff in the practice, or that it has impacted upon working practices. We are concerned that the development of clinical guidelines for health and social services staff who deal with people who are at risk of self-harm has a medium-term timescale. Greater priority should be placed on that work.
1325. In the action-area concerning churches and religious bodies, we support the need for suicide and depression awareness training for all church and religious leaders. In addition, we endorse the actions proposed in relation to the media.
1326. Sections B and C relate to targeted approach and overarching actions, and we fully endorse all the actions in both sections. We repeat that, without the full and active involvement of all the delivery partners, the strategy is unlikely to be fully implemented.
1327. The second area in the terms of reference was about examining the level of stakeholder involvement. Chapter 3 of the strategy recognises and indeed highlights the need for the stakeholders to work together to achieve the aims of the strategy. However, we noticed that, within the taskforce membership, two thirds, or 20 of the 32 members, come from a health and social care background. Only three of the members are from the education sector; six from the community and voluntary sector background; one from the Department of Social Development; and one each from Prison Service and the juvenile justice service.
1328. We were disappointed to an extent that neither the family nor the survivor voice was represented on the task force. One of the guiding principles of the strategy on engagement is continuing consultation with bereaved families, survivors, carers and their representatives. Through speaking to family representatives, we are aware that they were consulted, but that does not always equate to real engagement, which must recognise and support bereaved families who are faced with their own difficulties at such a vulnerable time. They may be endeavouring to support their own family or other bereaved families. Perhaps they are involved in fundraising for, and the running of, local services, as well as contributing to strategic discussions about the future planning and delivery of services. Further work must be done on the best way of supporting families in shaping the delivery of services and contributing to the strategic direction of the strategy. The health councils feel that the opportunity should have been taken to have greater involvement and input from people who have attempted suicide and survived.
1329. Ms Reilly: The third point on the terms of reference was on the level of services and support that are available. Provision of timely services is a long way from being in place. Urgent attention must be paid to the provision of a broad range of services, to which GPs can refer individuals.
1330. Young adults, in particular, are not as quick to engage with traditional mental-health services. Therefore, the design of future services must include new and innovative ways of engaging with young people. The previous speakers explained some of those ways, and we fully endorse what they said. Priority must be given to the early identification of people who are at risk. There are recognised suicide-risk factors, such as the increase of alcohol and drug use, depression, separation and bereavement. GPs and educators are often the first points of contact for people who are at risk. More resources must be directed at primary care and the education sector. Parents need information and support to enable them to recognise and deal with risk-taking behaviour in their children.
1331. In summary, the strategy can succeed only if it becomes genuinely cross-departmental and is driven by the Assembly as a political priority. It is worth examining the possibility of having OFMDFM drive the strategy, similar to the way in which it has driven the strategy for children and young people and the child poverty strategy. It should ensure that housing, social security, education and local government are integral to delivering on the strategy.
1332. There must be regional co-ordination of local plans and cross-departmental activity. Further research is needed to assist communities in answering the big question of why suicides happen. That would support the development of preventative services and help to counter the ripple effect of suicide and attempted suicide.
1333. There must be an increasing understanding that suicide and self-harm are not solely a threat to young people. The needs of people of all ages must be built into the strategy. We note that figures in the consultation document, ‘Protect Life: A Shared Vision — The Northern Ireland Suicide Prevention Strategy and Action Plan 2006-2011’, show that around 20% of deaths by suicide involve people who are under 25, but that 67% are in the 25-to-54 age bracket.
1334. The central role of GPs must be strengthened by further training and increased engagement with the strategy. More resources must be made available to primary care, including training in early detection for at-risk patients and for patients who are accessing counselling and support that is delivered by trained professionals who work with GP practices. Health and social care trusts should be required to put a family-support service in place that is capable of providing intervention to a bereaved family within 48 hours.
1335. We strongly believe that the proposals of the Bamford Review should be fully implemented. The Protect Life strategy’s overall aim is to reduce death by suicide by 15% by 2011. However, it does not clearly define how the implementation of the 62 separate action areas will be measured in order to achieve that. In order to understand what was successful and unsuccessful about the strategy, those measurements would have to be clearly defined.
1336. The health councils have welcomed the opportunity to reflect on the strategy and, as part of our continuing role to represent the public interest in health and social care, we will continue to scrutinise and comment on the implementation of the strategy. I thank the Committee for the opportunity to give our views today.
1337. The Chairperson: Thank you, Maggie and Noel. Before members put their questions to you, in case you are not aware, representatives of the four main Churches have given evidence to the Committee, which was a useful exercise.
1338. Mrs O’Neill: I thank the witnesses for coming to give evidence today. Your submission refers to the need for the establishment of a co-ordinating office, the main function of which would be to establish and co-ordinate local plans and regional activity. When Committee members visited the Dáil, we met staff from the National Office of Suicide Prevention. Are there merits in establishing such a structure here?
1339. Ms Reilly: We heard talk of examining the issues of suicide throughout the 32 counties. There are some merits to establishing such a body here. We are concerned that the implementation body seemed to be a misnomer — the body remained as an advisory body to the Department rather than an implementation body. There was, therefore, a potential gap in ensuring that the actions were implemented in a co-ordinated fashion. As a subject, suicide has tended to be quite bitty, so it would be worth investigating the possibility of a similar structure here.
1340. Mrs O’Neill: Your submission refers to the lack of uptake by GPs of training on suicide. In the absence of making training compulsory, have you any ideas about how to increase the uptake?
1341. Mr Graham: The figures that we saw were lower in some board areas than in others. However, in some cases, when a GP or individual from a practice had attended the training, the practice was included in the number of practices who had taken part. Some calculations were based on the number of practices that had taken part, rather than on the number of GPs out of the total number who could have been involved. I do not know the detail of the level of training that is provided, but I read in the media that there has been some criticism, and perhaps some GPs felt that it was targeted at too low a level. Therefore, some discussion with GPs is required on the content of the training.
1342. Mrs O’Neill: The level of training was highlighted in several submissions to the Committee. Perhaps the training should be ongoing or pitched at a different level.
1343. Ms O’Reilly: In the Western Board area, there was a 99% uptake of training. We checked to ensure that the figure of 99% applied solely to GPs. The Western Board addressed the issue of training by closing practices and introducing out-of-hours emergency care to provide services, so that GPs got protected time to train. Consequently, the uptake was extremely high, and we encourage other boards to consider following that lead.
1344. Dr Deeny: Welcome, Noel and Maggie. I am glad that you are here today.
1345. Thank you for mentioning those figures, Maggie, because that is exactly what happened in the Western Board area. The reason that so many GPs in the west trained in suicide awareness is because we pressed the local medical committee for protected time to train. For half a day every two or three months, the out-of-hours cover ensures that GPs are free to train.
1346. As you said, you represent the public and patients, which is an honourable role. I wonder how the new plans for healthcare in Northern Ireland will affect how we try to put in place health services from the bottom up, based on what we know the patients need. How will you work with the local commissioning groups? After all, you are the patients and the public’s representatives. The five local commissioning groups will be part of a regional commissioning body — there have been so many changes that I forget its title.
1347. I have heard you on the radio, Maggie, and you have probably heard me, but we have seldom met. However, I often wonder how the people whom you represent approach you.
1348. I could not agree with you more that whether the condition is epilepsy, diabetes or whatever, no one can speak better and teach others about the subject than the patients who have suffered from it. Therefore, families who have experience of suicide must be involved, as must patients who have come through periods of feeling suicidal. That point was made earlier by people who suffer from chronic ill health, and they had been asked to represent their fellow sufferers to the public, who may not have any knowledge of the condition.
1349. Finally, you are quite right — GPs do not have enough access to alternative therapies. I admit that, often, we have no option but to prescribe antidepressants when we know that talking therapy would be much more effective. The benefit of exercise was mentioned earlier; it, too, should be prescribed more often.
1350. The Committee has discussed the lack of facilities in Northern Ireland — not just for adolescents and young people who are under 18 years of age, but for young mothers who have post-natal depression. There is absolutely nothing. I could not agree with you more on that issue. I have had to deal with it for years. Young people would feel threatened by, and may run away from, treatment in an old-fashioned mental institution. They would respond better to talking therapy, which could be rolled out through the provision of counsellors in the new general practices and health centres of the future. People who are trained in talking therapies could be available to offer those services. What do you think of that idea?
1351. Ms Reilly: I will deal with those points in sequence. People approach us in a variety of ways. For example, if we speak on the radio, a plethora of people flood to us for help. Obviously, we would be better known if we were better resourced. We support people in making complaints, raising issues and act in an advocacy role on their behalf. The more work that we do, the more people promote the council as being able to help. People become aware of us through word of mouth. We also use various PR methods.
1352. The council has 24 members. Those 24 members represent the council in the communities that they represent. The public know those representatives and through them, approach the council. Therefore, knowledge of our activities is spread through word of mouth. Awareness is not as good as it ought to be. We hope that in the new world, when there is a new patient/client council, it will be better resourced in order to allow us to deal with a greater number of the public. Frankly, however, if more people were to come to us at present, we would not have the resources to cope with them. That is a major concern.
1353. Mr Graham: One of the difficulties that we have been burdened with from the start is our name — the Northern Health and Social Services Council — partly because people think that we are a health and social services board and, in some cases, they confuse the social services bit with social security. Quite a number of people have contacted us about benefit issues. We have tried to get the message across in the telephone directory, in which we run a half-page advertisement. That has had a downside, because we get loads of enquiries from people who cannot find their trust or local services and ring the council to find out the information that they need. However, because we are in contact with them we can redirect them or signpost those other services.
1354. As you are probably aware, there are two options for the new structure of the patient-and-client council body. Recently, after the consultation started, we were involved in a joint workshop with council members. We plan to hold another one on 1 May. However, in the meantime, we are engaged with community groups, and we hope to engage with local politicians as well within the timescale — taking account of Easter — that is available. When that concludes, we hope to produce a joint response from the four councils on how the new body might operate most effectively.
1355. Ms Reilly: I want to return the issue of mental health that was discussed earlier. I am glad that post-natal depression was mentioned. This morning, I listened to the Chairperson’s comments, which were a powerful testimony on how women relate to the issue. It is absolutely scandalous that there is no service for women. We are talking about the baby blues that occur for a few days after the birth, right through to the much more serious scale of post-natal depression that has been discussed on ‘The Stephen Nolan Show’. It is a scandal that a service has not been provided.
1356. In a previous life, I used to talk to women’s groups about good mental health. I spoke to young women and was shocked to discover that some of them were already single parents, were isolated, and had all the problems that go with being in that situation. They were quite intelligent women, and declared quite openly to me that they had found ways to get round the system so as not to let health visitors know that they might be depressed, because their greatest fear was that social workers would come and take their babies from them.
1357. Something needs to be done about that; those were vulnerable young women. Afterwards, I put them in contact with the appropriate people, and assured them that that was not how such business should be conducted; rather that it should provide help and support. However, that is how those young women viewed the system generally, and they would tell their friends the same. There is a tool that asks a series of questions in order to determine the level of post-natal depression; those women would answer those questions in such a way as to keep their depression hidden. They knew how to tailor their answers so that it would not look like they were depressed, and yet they were significantly depressed. Something needs to be done about that. I am glad that you are inviting Breda Hughes to come along to address that issue because it falls under the mental-health continuant.
1358. The Chairperson: I could not agree more with what you have said.
1359. Mrs O’Neill: I have gone to tribunals where people seeking incapacity benefit have been turned down because of their reluctance to admit that they have mental-health problems; they do not want to admit to it for fear of losing their children. That is a massive problem that we must challenge.
1360. The Chairperson: There should not be a stigma attached to mental-health problems.
1361. Dr Deeny: Do you see yourselves as the future patient and client council — whether that is one or five —working along with the local commissioning groups and planning healthcare? Do you think the best way forward is to have councillors in less-threatening environments, such as modern health centres, rather than patients having to attend old mental institutions?
1362. Ms Reilly: We will not have a future at all unless we can engage with local commissioning groups; that is where the decision-making process is at. It is our job to present knowledge of, and background to, what local people say that they need, and where they feel there are gaps in the system.
1363. However, we are not the proxy patient, nor are we going to be put into that position. It is important that the voices of the real patients are heard. We can assist the capacity-building for individuals and communities to have their voice heard. However, it is imperative that we work closely with local commissioning groups on this matter.
1364. Dr Deeny: What are your thoughts on patients being able to visit councillors in health centres rather than having to go to mental-hospitals?
1365. Ms Reilly: I absolutely agree with that idea. There is a stigma associated with the traditional mental-health services; young people simply will not engage with mental-health teams. There should be a system whereby the GP can see Johnny, for example, in the health centre — a non-threatening environment — and then send him two doors down to speak to the councillor for 20 minutes, an hour, or whatever. That scenario would not have the same stigma attached to it as the current process of attending a particular building that everybody knows is a mental-health institution. If a real difference is to be made, that system must be changed.
1366. Mr Gallagher: You have both referred to serious gaps in the mental-health service. Is there a lack of proper referral services everywhere, or do those vary depending on the postcode?
1367. Ms Reilly: No, the board does not particularly see the problem as varying according to postcode.
1368. Mr Graham: We would not be aware of the postcodes – it is a more general problem.
1369. Ms Reilly: I was aware of a lack of psychology services in the western area, but my colleagues in the other councils informed me that that was also an issue for them. There was a difference between the terms and conditions for psychologists in the various board areas but that has, to some extent, been ironed out by the Agenda for Change. There is a lack of investment in talking therapies per se, and there has not been enough recognition of the importance of that role.
1370. The Chairperson: It is coming to the fore that talking therapies are preferable to arming people with so much medication that they literally become zombies.
1371. There are a number of concerns relating to funding, and inadequate service provision, among community-based and families groups involved in suicide prevention, such as PIPS, RAYS, Families Voices, West Belfast Suicide Awareness and Support. What role do the councils perform in voicing those grievances with the national and local implementation bodies involved in the Protect Life strategy; do you speak up as an advocates grouping on the subject?
1372. Mr Graham: It is only because we concentrated on the strategy when it came out and heard from organisations such as Family Voices that we became aware of the services and support mechanisms that are out there. We visited the local branch of the Samaritans in our area to find out what they did. They would like to have some involvement with accident and emergency departments at local hospitals, because they felt that people who presented there with attempted suicides or other issues could be referred to them and could be helped. They do not have that role at the moment. I am not sure, however, that the Samaritans would have the capacity and the funding to carry out that role.
1373. Ms Reilly: We genuinely believe that what has happened in the community traditionally is that the community and voluntary sector has been put upon to provide services. Sometimes, when there is a lot of media attention, particularly around the clusters of suicides of young people, there have been knee-jerk reactions and the demand that somehow, the community had the answer. However, the resources did not follow, and tremendous pressure was put on local groups who had people coming to them.
1374. At every opportunity, whether it is with the Children’s Commissioner or with the Department, we are raising that issue and saying that these are core services that the Minister and the Department should be funding. They should not rely on the community and voluntary sectors to do that work. Those sectors have an important role to play, and perhaps can provide a quicker service that is more flexible towards the needs of the population than that provided by the statutory sector, but they must be funded to do that.
1375. The Chairperson: I am delighted that you are conveying that opinion at every opportunity. It is a serious area of concern, and we must ensure that we have an outcome that will deliver to the people who are affected. Thank you all for coming along. It has been a very interesting session.
13 March 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr John McCallister
Ms Sue Ramsey
Witnesses:
Professor Eamon McCartan |
Sport NI |
|
Dr John Kremer |
Queen’s University Belfast |
1376. The Chairperson (Mrs I Robinson): The next two evidence sessions are part of the Committee’s inquiry into the prevention of suicide and self-harm. A paper related to these sessions has been provided to members. The first evidence session is with Sport NI, formerly known as the Sports Council. A copy of its presentation has also been provided to members. I am pleased to welcome Professor Eamon McCartan, chief executive of Sport NI, and Dr John Kremer from Queen’s University, Belfast. I invite you to speak for five or ten minutes, and there will be an opportunity after your presentation for members to ask questions. I will allow about an hour for the ensuing debate.
1377. Professor Eamon McCartan (Sport NI): As chief executive of Sport NI, I would like to introduce my colleague Dr John Kremer from Queen’s University, Belfast, who has written extensively on sport, physical activity and health. I would like to thank the Chairperson for the opportunity to present evidence relating to the Committee’s inquiry into the prevention of suicide and self-harm. Members have been provided with a copy of our presentation. We do not propose to talk through it in detail; instead, we will focus on the key messages. We are very happy to take questions.
1378. Sport NI is aware of the Northern Ireland suicide prevention strategy, the aim of which is to reduce the Northern Ireland suicide rate, particularly among young people and others in high-risk groups, and to highlight the issues facing Northern Ireland in relation to suicide and self-harm. We know, personally and professionally, that suicide and self-harm are more prevalent among young males than young females, and young adults aged 15 to 34 years of age. It is more prevalent in urban areas than in rural areas, and it occurs more frequently in deprived areas than in non-deprived areas.
1379. I will try to give the Committee a brief introduction to the role of Sport NI. In doing so, I will explain our definition of sport. We hope that through our presentation, members will have a greater awareness and appreciation of the evidence that highlights the contribution that physical recreation, physical exercise and sport can play in preventing suicide and self-harm. Article 21A of the European Sports Charter’s definition of sport will help the Committee to understand sport. It defines sport as:
“all forms of physical activity which, through casual or organised participation, aim at expressing or improving physical fitness and mental well-being, forming social relationships or obtaining results in competition at all levels.”
1380. It is in that context that we define sport — not in the traditional context of the playing fields, but in the context of expressing or improving physical fitness and mental well-being.
1381. Sport NI has a vision, which is, through sport, to contribute to an inclusive, creative, competent, informed and physically active community. In practice, that means that Sport NI creates and develops programmes and partnerships that will contribute to our strategic objectives. The most important of those is increased participation in sport and physical activity. We believe in the value that sport can add to the promotion of social inclusion, creating active citizens and enhancing the image of Northern Ireland at home and abroad.
1382. Equally, we must not lose sight of the contribution that physical recreation, physical exercise and sport can make to broader Government policies such as better health, better education, a better economy and better communities. A significant part of the work that Sport NI undertakes is to create policies, programmes and partnerships to increase levels of physical activity and to increase capacity and social well-being, particularly among young people and under-represented groups.
1383. That is done through a series of programmes, one of which is the community sport programme, the aim of which is to improve health and well-being, to build capacity in individuals and to increase sustained participation in physical activity and exercise.
1384. Dr John Kremer (Queen’s University, Belfast): There has been a long-standing recognition that the physical and the psychological go hand in hand. Mens sana in corpore sano: healthy mind, healthy body. Therefore, it is very welcome to have an opportunity to talk about how the psychological may have an impact on such a significant social issue as self-harm and suicide. Exercise psychology in particular is well positioned to talk about such matters. I would like to take you through some of the key findings about the relationship between the psychological and the physical.
1385. Concerning the healthy body part of that equation, the evidence is unequivocal, namely that there are so many somatic health benefits attached to doing physical exercise. Turning to the psychological, one finds a far more complex picture. However, the general statement that can be made with a degree of certainty is that physical exercise correlates positively with psychological health except where the motives for exercise might be more questionable. There are examples in which excessive use of exercise in relation to body image might cause problems. Generally speaking, however, the picture is positive.
1386. Critically, in relation to self-harm and suicide, there is an emerging research literature that suggests that those who exercise are less prone to suicide attempts. Of the three studies mentioned on the presentation slide before the Committee, the most important is probably that by Simon et al (2004) which states that:
“suicide attempters were far less likely than controls to report involvement in physical activity in the past month.”
Almost half as likely. When demographic factors including age, race, education and morality are removed, that affect is still found. There is a strong correlation between maintaining an exercise regime and a host of psychological variables.
1387. There is a positive correlation between exercise, self-esteem, self-efficacy, well-being in general and cognitive functioning; and a negative correlation with anxiety, stress and depression. At the same time, there is recognition that gender-effects play their part. In competitive sports, for example, there is a phenomenon known as FAT — the female athlete triad, which is a combination of amenorrhoea, osteoporosis and disordered eating which can accompany excessive exercise. However, such conditions tend to be exceptions rather than rules. In the United States it has long been recognised by physicians that exercise is a routine form of treatment that would be prescribed. In the UK, there is increasing evidence that GPs are turning to exercise as a treatment for forms of psychological malaise. However, where and at what point still tends to be patchy. There is no consistent theme, especially in a culture best described as a “pill culture” in which people expect to be prescribed a pill for whatever illness they present.
1388. Particular effects are associated with exercise. Mood state, for example, responds well to certain types of exercise. For some strange reason, it seems to be repetitive, boring, aerobic exercise that has the most positive effect on mood state. Most literature on the subject concerns depression and it is now well established that an effective treatment for depression — and most especially for clinical depression — is regular exercise. Aerobic exercise seems to be the most effective. Such exercise is, typically, carried out several times a week, and the longer the regime, the more likely there are to be positive effects. Maintaining a regime can sometimes be difficult for those who are not inclined to exercise because they are depressed, so there is a degree of circularity. Anxiety has also been shown to respond well to exercise, especially programmes that last longer than 20 minutes, after which time aerobic exercise then kicks in. In relation to anxiety, however, the type of exercise seems to be unimportant.
1389. Those who maintain a reasonable level of physical fitness and engage in physical activity also seem to be well buffered against ordinary life stresses, including illness. There is a positive relationship between exercise and self-esteem, but it tends to operate only in relation to specified domains and, as one might expect, in particular in relation to domains related to physical competence.
1390. A gender effect cannot be ignored in relation to exercise, however, and there is increasing evidence that young men are not exercising to lose weight but, to use a modern phrase, to “bulk up”. They have concerns about the initial states of their bodies and a desire to increase muscle bulk, whereas women traditionally exercise to lose weight.
1391. Nobody is absolutely sure yet why beneficial effects occur, but there are at least four hypotheses to which people work. The first is that, by engaging in exercise, one is breaking some sort of cycle. There is a psychosocial hypothesis which says that by exercising or engaging in activity one breaks free from everyday anxieties and worries. Another hypothesis is based simply on body temperature, in that by exercising one increases one’s body temperature, which has a positive effect on mood and, more generally, on psychological well-being. Pleasure peptides, the runner’s “high” and similar explanations are abroad, but they are probably not as popular as they once were. As to which hypothesis works, it is almost certainly a combination of all of the above effects that explains why engagement in exercise can help to address psychological morbidity.
1392. In conclusion, there is no question that physical exercise helps people to deal with a range of psychological conditions, and, in relation to self-harm and suicide, there is increasing evidence to suggest that it can play a preventive role. However, it would be over-egging the case to say that exercise provides an answer to all the problems. It is more likely that exercise can act in combination with other interventions to help to stop people who are already heading down a suicide route.
1393. If one reviews the various intervention packages that exist, it is interesting to note how few of them mention exercise; yet many of them have time-out interventions of various sorts. Perhaps now is the time to examine more structured interventions to see where exercise can play a positive role alongside other forms of support in helping people to move further away from that route.
1394. Unquestionably, there is a paradox in all of this. The people who are most likely to benefit from exercise are also likely to be those who are least inclined to take exercise, and that remains a significant challenge for people who work in that area. Thank you.
1395. Professor McCartan: In conclusion, we would say that the sporting sector and Sport Northern Ireland seek to provide structured interventions that provide the opportunity for exercise or physical activity to men, to young adults, to people who live in urban areas and, most importantly, to people who live in deprived areas. Thank you.
1396. The Chairperson: Thank you very much, Eamon and John. During a visit to Scotland, the Committee heard how major sporting occasions, such as premier-league football matches, and major sports personalities are being used to encourage people — particularly young men — to talk about their feelings and to overcome the stigma attached to admitting to suffering from depression. As part of the programme of reaching out, they distributed little cards at all the major stadia, which gave a helpline number and said that it is good to talk. Has your group looked at that approach? Would you contemplate doing that, and if not, why not?
1397. Professor McCartan: I am happy to answer that question.
1398. A programme is being run in stadia across Scotland, and another programme uses icons of sport to encourage people to talk about the issue. In fact, Neil Lennon, formerly of Glasgow Celtic, came out and outlined the problems that he had experienced in his personal life. That was a mechanism for increasing awareness and for encouraging people to talk about the issue. We have not been directly involved in a programme for rugby, soccer or gaelic in Northern Ireland. The Scottish Parliament allocated sportscotland around £13 million from the health budget to help in the development and promotion of such programmes. We would seriously consider developing such a programme and promoting it at major international football matches in Windsor Park, at major rugby and gaelic matches and at the North West 200. They are probably our four biggest crowd-pullers.
1399. Mrs O’Neill: Thank you for coming along and giving us an insight into the issues. Your contribution will help us with our inquiry. You said that those who would benefit most would be least likely to participate in the programmes. You also talked about people from disadvantaged communities. Are there any programmes that could target those groups specifically? Has the Department sought your views? Were you consulted on the suicide strategy? Finally, are you involved in the implementation body?
1400. Professor McCartan: No. To the best of my knowledge, we were not consulted on the strategy, but we are aware of it. John outlined empirically that sport in the European definition has an important role to play with regard to physical exercise and activity. When we received your invitation to give evidence, we thought that it would be worthwhile to present evidence and to illustrate how sport can help people.
1401. Dr Kremer: Someone once famously remarked, “no action without research; no research without action”. Many of the intervention programmes do not focus too much on the research. A range of activities may have been mentioned, but no one has actually decided which programmes are likely to be the most effective. If you read the literature, you would be disappointed by the small number of programmes that consider exercise as a form of therapy, even though it gives a sense of purpose and identity to those who suffer from hopelessness. The programme in Scotland targets people attending events. That is useful, but only in so far as it identifies people who may be at risk. However, we must target those people and encourage them to engage in lifestyles involving physical exercise which is sustainable in the longer term. It would be good if that sort of work could be mainstreamed into the many and varied interventions.
1402. Mrs O’Neill: I would like to begin with health promotion, Investing for Health and encouraging people to participate in sport at an early age.
1403. Professor McCartan: Sport Northern Ireland runs a successful community sport programme, which aims to promote individuals’ health and well-being. The programme is targeted at areas of social need, and it is designed to build capacity, self-worth and self-esteem. It is aimed at increasing the participation and the regulatory of participation in sport. Participation in sport, particularly in aerobic activity, a couple of times a week for 30 or 40 weeks a year was found to be the most beneficial for treating certain types of depression and anxiety.
1404. Mrs O’Neill: You talked about an over-reliance on pills, and you are right in saying that there is a pill culture here. However, we are finding that other interventions can play a vital role. I hope that that is something that will come out of our inquiry.
1405. Mr Easton: What we have often been told that exercise is good for people mentally and physically, so it is good to have that confirmed. Exercise is part of the prevention and part of the cure for people with mental-health issues.
1406. Do you think that GPs should automatically refer patients with mental-health problems to undertake some form of exercise programme, rather than simply prescribe pills or make a further referral? For example, establishing a connection between GPs and sports clubs or leisure centres to form part of the treatment might be useful. Similarly, would an exercise regime for patients admitted to hospital with mental-health problems be beneficial?
1407. Dr Kremer: The most effective regimes operate in total-treatment institutions, where people are required to exercise. That can have quite a dramatic effect on clinical depression, and over several months a radical decline in those symptoms is visible. A major culture shift is needed to recognise that GPs using exercise as a form of treatment is not a second-class option or a poor cousin. In a well-maintained and well-managed environment, that can be a long-term solution to many of those problems. However, there is still resistance to such concepts. The recent debate questioning the effectiveness of drugs like Prozac is an interesting one; those antidepressants may simply be placebos. Exercise provides a cheaper and potentially more effective remedy.
1408. The Chairperson: Castlereagh Borough Council operates a referral scheme, helps promote a healthy lifestyle and outlook and permits its premises to be used to promote well-being.
1409. Professor McCartan: I congratulate Castlereagh Borough Council and Belfast City Council on their efforts to combine health and leisure services. Sport NI seeks to increase rates of participation in sport and physical activity in Northern Ireland. Clear empirical evidence shows that people who participate in sport and physical activity are less likely to self-harm or commit suicide. Therefore, if more people engage in physical activity, the pool of individuals who are vulnerable to self-harm and suicide should, theoretically, reduce. Those are the preventative measures.
1410. Moreover, there is clear empirical evidence — and thank God that it is the case — that GPs are prescribing exercise and physical activity as a remedy to deal with depression, anxiety and the continuum that leads to self-harm and suicide, rather than simply prescribing pills.
1411. Dr Deeny: As a GP of over 20 years, I have no doubt that a person who is emotionally and mentally well will improve physically, and vice-versa. Sporting activity fills a vital role. The Committee is gradually recognising that all the different parts of the jigsaw must combine to tackle the awful scourge of suicide. Drugs have a part to play. All GPs prescribe them, and, as I have stated previously, sometimes there is no alternative. Talking therapy is also important.
1412. However, people who are good at sports at school are more likely to continue participating when they leave school, whereas those who are not so good tend to feel a sense of failure and are more likely to give up. To a certain extent Alex has touched upon this question, but how do we encourage those non-sporting people to continue to engage in physical activity after leaving school? John mentioned pleasure peptides — is that what used to be known as endorphins? I have not exercised for about nine months, and I do not feel as good. I am going to start soon because physical exercise undoubtedly makes people feel better.
1413. A pilot study was carried out — although I do not know the results — but we, as rural doctors in Tyrone, felt a little bit cheated. We were not allowed to prescribe exercise in the local leisure centre in Omagh for our patients, but the GPs in the town were. I thought that that was wrong. As Alex said, I have no doubt that most GPs would be very keen to prescribe exercise, rather than write prescriptions for Flouxetine — or Prozac, as it is better known. It costs £4 for a session in the training zone in the leisure centre, and that is cheaper than most drugs. GPs should be prescribing exercise. What are your views on that?
1414. The big challenge for GPs and anyone else dealing with people who are depressed, feel worthless and have low self-esteem, is to get them motivated and interested. They lose interest and motivation and they even lack energy. We must get those people into the gyms, on to the equipment and exercising.
1415. Part of the solution is getting the first line of contact — people working with our youth — involved in exercise. I go along with what Alex said about preventative measures, and what Eamon said about remedial measures and getting people involved in exercise. If we can get more people involved, there is no doubt that it will lessen the pool of the people who are liable to develop feelings of hopelessness and, ultimately, suicide.
1416. Dr Kremer: One of my more interesting PhD students was a life prisoner in Maghaberry, and he did his thesis on exercise and psychological well-being among life prisoners. There was a whole array of factors about taking people to the gym, but one of the most significant factors was peers. If you are involved with a group of people who are also exercising, they were chivvying you up to go along and it was difficult to escape — [Laughter.] They tended to be the ones who kept exercising. The others were more sporadic.
1417. However, there is a whole host of other factors at work as well. The critical one that was mentioned was the transition from organised sport at school through to voluntary sport when young people leave school. That has been a thorny issue. How do we bridge that gap? The people who are already good and talented are naturally carried forward on a tide past school into sports clubs. The rest of the young people have to find their own way. There is a void that is very difficult to cross over, unless there is a strong family connection with sport. Much work still needs to be done on that transition. It can be seen in Queen’s, where there are a lot of interesting programmes to try to encourage people back into sport.
1418. Major cultural issues still have to be overcome, going back to the pill culture —
1419. Dr Deeny: Can you explain what those issues are? Are they cultural issues with GPs, or is it a community attitude?
1420. Dr Kremer: As Eamon pointed out, the definition of sport is very broad. We still carry a layperson’s definition in our heads, which is around competitive sport and the group of people that becomes the chosen ones whom we then go and watch. That is quite different from encouraging a much broader body of people to engage in exercise more for its own sake. Sometime the emphasis on competition in school sports, in terms of the body of a school, can get in the way of long-term commitment to a sport.
1421. Some people have to rediscover running, after having taken part in cross-country at school, which hurt and which they did because they were made to. One has to rediscover the enjoyment of just going out and jogging.
1422. Professor McCartan: May I just add to that? As I look round the room, we are all of an age that has a traditional view of sport, which is associated with school teams, performance and competition. What we, and what many in education are trying to do, is to look at sport in terms of the European definition, which should include physical exercise and physical activity, and put that in the context of healthy living, and life-long healthy living. We are trying to take exercise away from the traditional view of sport and to look at it as physical exercise and physical activity.
1423. The traditional view has a place, and I am not saying that that should be done away with. However, we must broaden sports participation to people who may not be particularly well adapted for sports but who — like the rest of us — require physical activity not only when they are young but for the rest of their lives, and, in order to maximise physical and mental well-being from such activity — whether it is walking, jogging, cycling, disco dancing, or whatever — it must become, as Dr John Kremer said, an integral part of their healthy-living programme.
1424. We all remember the plump kid in school who, from a class of 30 pupils, was never picked to play football because he or she was not particularly good at it. Guess what? People do not do that which they are not good at, and if they are told that they are not good at something, they tend to shy away from it. Therefore, given that some people are not particularly good at team games, alternative activities must be added to the physical-education curriculum in order to provide an opportunity for such people to access the benefits of physical exercise, which might then become embedded in their lifestyles.
1425. Dr Deeny: If clinical grounds exist — whether for mental-health, self-esteem or even physical benefits — should GPs be allowed to prescribe physical exercise on the NHS?
1426. Dr Kremer: Without question; the evidence has been so well established over decades that there is now no question about the benefits of physical exercise. One caveat to that is motivation. Some people use exercise dysfunctionally. Nevertheless, if screening mechanisms are in place, the general answer to your question is yes.
1427. The Chairperson: Down through the years, I have learned about another difficulty. If a person is suffering with depression or anxiety, he or she can hardly get out of bed in the morning, never mind getting involved in walking or running — the motivation simply is not there. The dilemma is that if such a person has cut themselves off, is isolated and does not want to see people, that message is difficult to put across.
1428. Dr Kremer: It is, and the management of such experiences is so difficult. The challenge in this area is that, subsequent to prescription, implementation can be so difficult.
1429. Professor McCartan: The buddy system is one technique that can be used in such circumstances. As you rightly said, people cut themselves off, they are isolated and they find it difficult to move or get out of bed. Consequently, the early initiation of a buddy system gives such people the encouragement and support they need.
1430. Last week, I attended a conference at which Dr Maureen Murphy, on behalf of one of the health boards, presented a report — the title of which my colleagues are likely to know — about her study of the prescription of exercise. Her findings were quite exciting and, with the Committee’s permission, I will forward those findings for it to consider.
1431. The Chairperson: That will be helpful to us in finalising our proposals for the Minister.
1432. Ms S Ramsey: Like other members, I thank you for your presentation. I have a couple of comments to make, followed by a few questions.
1433. I am interested in what you said about the Scottish Executive giving additional money to sports in order to address suicide and self harm. When discussing participation in sport, which tackles social inclusion — an issue that affects my constituency and others — it strikes me that we are losing a lot of money because of the Olympics. That might be a good thing; however, when communities attempt to gel and encourage people to become involved in all sports, they reach the last hurdle only to discover that the money has been whipped away. You must be well aware of that. On the one hand, we appear to take a step forward on the issue of suicide and self harm, but, on the other, we take two steps back on the issue of social inclusion between communities.
1434. Michelle O’Neill said that sport has a role to play not only in relation to this issue but in Investing for Health, and we have witnessed the benefits of that.
1435. I cannot avoid coming back to Dr Deeny’s point. Some people in the medical profession have the mindset that there is a pill for every ill. That is another component part that needs consideration.
1436. The Chairperson made a valid point — that Scotland has taken the lead in relation to sporting icons or heroes. That is something that should be utilised here, as there are good, prominent role models in the sporting sphere. If another Government is utilising that, it could be implemented here without our having to reinvent the wheel.
1437. Looking at some of the sporting organisations that cover the island of Ireland — particularly the GAA and rugby — do you plan to address the issues with your counterparts on an all-island basis? Strategies could be developed to tackle the issues of obesity and depression, for example, rather than only addressing the issues of suicide and self harm. As many people as possible — irrespective of gender and age — should be encouraged to get involved in sport.
1438. I am very concerned about the issues of suicide and self harm, and an inquiry has been established to address those issues. It is encouraging to hear what is happening in relation to that. On the other hand, we are losing millions of pounds in funding due to the 2012 Olympics. Where does that leave communities that have been severely affected by suicides? People in those communities are trying to get off their knees, but every hurdle they face is higher than the last.
1439. Professor McCartan: To put the record straight; the £13 million in funding given to the Scottish Sports Council by the Scottish Parliament was not for dealing with the issue of suicide alone; it was for health generally. A series of programmes was set up to address issues like obesity and poor cardiac health.
1440. It is true to say that we have had a reduced budget because of the 2012 Olympics. That has impacted on all of our programmes, including community sport. In defence of the Culture, Arts and Leisure Minister, Mr Poots, he is fighting hard for additional funding for that particular deficit, and we will be discussing that issue with the CAL Committee next week.
1441. Ms S Ramsey: I am not being critical. What I am saying is that we are talking about having a joined-up approach to this. We are in an Executive, and need to have a joined-up approach from all Departments. If the Health Department or the Education Department tries to tackle the issues of suicide and self harm, sport has a role to play in that. That is how the jigsaw fits together.
1442. Professor McCartan: I agree entirely with that view.
1443. We are aware that various studies have taken place into suicide and self harm. A 2004 study identifies suicide as a major issue in the Republic of Ireland, just as it is in Wales — as we have seen recently in south Wales. It has also been a major issue in Scotland, as it is in the constituency of West Belfast; where there is a prolific cluster — that is statistically incorrect, but it is evident that there is a rise in the rate of suicide there. We liaise very closely with the Irish Sports Council. We are meeting them on 3 April, and suicide will be an item on the agenda.
1444. Dr Kremer: There is a conundrum here, because the traditional channels that one would work through, in relation to accessing people involved in sport, do not work when it comes to social issues such as suicide, because the people who are most at risk are the least likely to be involved in organised sport.
1445. Fresh thinking is needed to consider how to engage with those hard-to-reach, marginalised people. They need to be encouraged to engage in activities that they may well have been put off at an early age. They may have developed a lifestyle that is quite removed, and that which most people who are involved in sport would not be used to. A fresh approach is needed in order to establish who those people are, and there is a need for a culture shift.
1446. If any of you walk in the Mournes, it is quite interesting — and has been confirmed in a recent participation report produced by Sport NI — that you will meet more people walking there who are not from Northern Ireland than people who are. You will hear more southern, eastern European, or English accents than Northern Irish accents. That is a real wake-up call, because it is a stark reminder of the cultural obstacles that still need to be overcome.
1447. The Chairperson: I think that, to a degree, the legacy of the Troubles and of coming out of conflict has added to those cultural obstacles. Both communities in this society have been marginalised, and in the past people did not walk or go past their own boundaries. In my own part of Strangford we now have the Comber Greenway, which consists of many miles of straight paths for cyclists and walkers. When one does go out it is quite amazing to see that it is mostly local people using it, who can not believe that they have this facility on their doorstep, stretching from Comber right through into east Belfast. It is many miles long, and the number of people who are now using it is quite amazing; the only problem is that the “hoodies” are out on their motorbikes, and that dissuades a lot of people from using it. However, I totally concur that healthy lifestyles produce healthy minds.
1448. Everyone who had wanted to speak has now been given that chance, so I would like to thank John and Eamon for coming along. Thank you very much indeed for your attendance.
3 April 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Witnesses:
Mr Sean McPeake |
Northern Ireland Local Government Association |
|
Ms Anne Donaghy |
Antrim Borough Council |
1449. The Chairperson: Today, there will be two evidence sessions as part of the Committee’s inquiry into suicide and self-harm, which will conclude the oral evidence for that inquiry. Representatives from the Northern Ireland Local Government Association (NILGA) will give evidence first. Their presentation is at tab 3 of the Members’ pack.
1450. On behalf of the Committee, I welcome the witnesses from NILGA and apologise that a previous evidence session, which was arranged for 14 February, had to be cancelled because the Committee had to consider the important matter of clostridium difficile. I welcome the chief executive of NILGA, Heather Moorhead, my dear friend and colleague whom I have known for many years; Sean McPeake, who is the vice president of NILGA, and Anne Donaghy, who is director of environmental services at Antrim Borough Council. I invite all of you to make comments for five or 10 minutes, after which members will ask questions.
1451. Mr Sean Mc Peake (Northern Ireland Local Government Association): Thank you very much, Madam Chairperson and members of the Committee, for allowing us the opportunity to speak to you this afternoon on how local government envisages a better joined-up approach being taken on the important issue of suicide prevention. There are many good examples of that in the local government sector. However, in view of Minister Foster’s RPA statement to the Assembly on 31 March, it is an opportune time to get some clarity on the matter. Perhaps the community-planning remit will be the vehicle with which to take that forward. That is primarily what I will discuss today; the greater roles that we envisage in health provision in light of the Minister’s recent announcement. In fact, we are lucky to have the Minister attend our full NILGA meeting tomorrow to explain the matter further.
1452. I will hand over to Anne Donaghy who is an officer at Antrim Borough Council. Anne wears two hats — she does much work in suicide prevention for the council and similar work throughout the region for the community and voluntary sector, which she shall explain.
1453. Ms Anne Donaghy (Antrim Borough Council): Thank you, Madam Chairperson and members. After I have made my comments, I will ask Heather to expand on other activities in different local authorities across Northern Ireland. I will concentrate on the contribution of local government from a political and leadership perspective.
1454. Local government takes a keen interest in the Protect Life strategy. We believe that we have an important role to play in that. We can help to target resources and to ensure that those that are set aside for suicide prevention can be used more effectively. We have local knowledge and can use it to help to target resources on the ground.
1455. From a community point of view, when a suicide happens, the bereaved are very often left to pick up the pieces. Those are the people who will establish community groups to try to co-ordinate services. The councils can help them to do that. My involvement is through a local community group, which asked me, because of my local government skills, to help it to find funding, to influence the right people and to get a joined-up approach in order to streamline the partnership.
1456. We have come a long way, but when local communities come up with those types of initiatives, they put in a lot of their own time and resources. Local government can help those groups by providing its available skills and capacity to achieve funding and to form projects that address real issues. Young people — young men in particular — the elderly and farmers have been driven to the extreme of committing suicide. There is a key role for local government. I have seen instances in which local government has helped to save lives by talking to community groups. The networks already exist, and I urge local government to take a stronger role.
1457. Local government is involved in several strategies, such as Investing for Health, the health action zones and Healthy Cities. However, there could be a stronger role for the Protect Life strategy, to make it more effective where it is needed. Strategies come and go, but Protect Life must be introduced to local communities. Our elected members and officers know the local communities. When someone commits suicide, the bereaved relatives will often turn to the officer or elected member whom they know. Sometimes, they cannot go back to work. We can be used as a signposting service, for example, to help those people to get some money to sustain them until they can go back to work.
1458. I know that local government has the ability to co-ordinate a streamlined partnership approach, in which we can connect organisations and individuals, such as the Churches and health professionals, who have an important role to play. Some of the “softer” roles can be taken on by local government officials and elected members, who can take a synergistic approach. Those of us who are involved in local government really want to see this strategy put in practice. We would like to put into practice some of the projects that have been suggested by local communities.
1459. Rather than allowing piecemeal projects to use up funding, we want to be involved in making a co-ordinated strategy work. There is so much emphasis on road traffic accidents, but there are far more deaths by suicide in Northern Ireland than there are on the roads. We must make people aware of those facts. Local government has a strong voice in the community, and with MLAs. We can use that strong connection to promote the issue. As members will be aware, suicide has a stigma, and local government can help to remove it.
1460. We have a central role to play. We have rural connections; rural suicide is as big an issue as it is anywhere else, and it affects young and old. We can use some of the existing local government services to help to eradicate suicide. We can channel our sports and leisure and community development resources. There is a real need for an evidence-based evaluation of suicide. I know that some work has been undertaken, but we must be more involved in that. There must be clear communication between all the players.
1461. It is not only an issue for the health profession; it is an issue for the Churches and local government. Clarity is needed between those areas, and it must be ensured that the precious resources that have been set aside are used to make a change on the ground. As I said earlier, local government has the capacity to address suicide. We have an opportunity to work in a co-ordinated fashion with all the other professionals, the Churches, and the community, which is crying out for help to make that happen on the ground and to share best practice.
1462. I propose the creation of a task and finish working group to consider the issues and to decide how the recommendations can be taken forward practically. The key is that local government wants to be involved in the implementation and evaluation of the Protect Life suicide strategy. We want to channel the capacity that exists — and the resource that is paid for — to the community and address the issue. We want to connect and co-ordinate the key players to have a streamlined approach. We want to help the communities to achieve funding, set up systems, make connections and have influence so that they can focus on the real issues in their communities — young people and the people who are under threat from suicide.
1463. Ms Heather Moorhead (Northern Ireland Local Government Association): I want to highlight what councils are doing. There is a massive role for local authorities, but their work is piecemeal. Many things are happening on the ground and we want to pick a few of those that highlight and explore, with our other partners, how we can step up to the plate and have a much more strategic role so that we are adding value. Clarity is needed because everyone who works at local government level is stepping over each other and no one knows what is happening.
1464. We have listed seven or eight excellent examples that are making a real difference at local level in different areas. The Lord Mayor of Belfast has set out suicide prevention as a priority, and Belfast City Council has been working for a long time in north and west Belfast through the health action zone. In the southern region, local government has worked through the Investing for Health partnerships. Five councils have worked together, employing three officers. They are carrying out training and raising awareness on the ground, which is another initiative. Strabane District Council and Omagh District Council have decided to work together; Strabane District Council’s chief executive is leading a convening partnership to consider delivery of the strategy. Derry City Council has been working on the issue for a long time, and it convenes a local partnership through its Healthy Cities work. Newry and Mourne District Council has community safety officers, who are supporting a community initiative. The community started those initiatives and the council is supporting them.
1465. Some other councils are not doing anything at all because suicide is not seen as a problem in their areas; either no one person has been interested in an initiative or the council has seen suicide prevention as a health issue. NILGA should be able to provide a lot of support to the Health Service to make a real difference in communities. As 26 disparate councils, we need to find a more strategic approach to working with the Health Service, in particular, and the other organisations in that area. Therefore, we have made a practical proposal to set up a task and finish working group to define the role of considering strategic issues so that NILGA and, particularly, the environmental health and community development professions provide a way to promote that in the councils.
1466. The Chairperson: I will open up the discussion for questions. From what I gather, the work of the councils is piecemeal and not all the 26 councils are engaged. That answers a question that I was going to ask about the level of engagement between district councils and trusts in local implementation. If all the councils are not involved, that falls short in every sense.
1467. Ms Ní Chuilín: The review of public administration puts an emphasis on coterminosity. That means working together better in a more joined-up way. What opportunities are there for that under RPA? What community planning will take place?
1468. As you say, people in rural and urban areas will have different experiences of this. It is important to respond to the needs of people, instead of presenting services and hoping that people will respond to them. How will you go about using the reorganisation of local authorities, community planning and RPA as an opportunity to get a better response to suicides?
1469. Ms Moorhead: We see great opportunities here. We have an issue with coterminosity, and we welcome the opportunity of exploring that with the Minister and the commissioning groups. It is very important for us.
1470. Community planning in other regions yields much fruit on what are known as “wicked” issues, those on which it is nearly impossible to make a difference. Here is an example: in Nottingham, 36 budgets were operating for youth and antisocial behaviour, but they were making no difference. In the community-planning process, all the agencies clubbed together their budgets and set new stretch targets. Those agencies were able, within a two-year period, to transform the situation, as everyone worked to the agreed strategy.
1471. We hope that community planning will not wait until 2011: we are starting to form transition committees. We welcome the opportunity to have a community-planning pilot scheme at an early stage. Some of the issues are more pressing than others, and it depends on the area concerned, as everything is not appropriate in every area. However, it is important to take a lead and pilot measures that make a difference locally. That is our main priority, and it is something that we will explore with the Minister. It is important for this issue.
1472. Mr Easton: It is vital that all the community groups that deal with suicides get together and adopt a joint approach with councils and the Health Service. Otherwise, everyone will go his or her own way, and that will not help to tackle the problem.
1473. Does NILGA feel that that is the way forward? In every council area, or Westminster constituency, should there not be a body at which all the community groups, together with the council and the Health Service, get together once a month to co-ordinate an approach on suicide, decide on programmes and work together?
1474. Ms Moorhead: That is the current concept. The Department for Social Development (DSD) has a community development budget, which will be devolved entirely to councils, so that, at local level, there will be a community forum and a community support plan. Each forum will decide upon priorities. During the community-planning process, that forum will be able to contribute to environment, health and other aspects. However, there will also be thematic groups in the community-planning process: one for health, another for environment, another for the economy, and so on, meaning that there will be a proper interface.
1475. To be honest, in our experience, the lack of co-ordination at local level is a major block to getting collective action on the ground. So much time is spent negotiating, arguing, checking, and passing things from one group to another, that those transactions are all very wasteful. A local authority, however, can work magic in a local area to join up efforts. We hope that community planning will make a big difference, but we should not underestimate the difficulty of that.
1476. That is our vision; that is how it should work. There is everything to play for, if we get support at local level.
1477. Dr Deeny: Thank you, Heather, Sean and Anne for attending. The Committee has been looking into this for some time now.
1478. Anne mentioned the need for a synergistic approach, the united approach that society must take. She talked of strategies and practical solutions. I have worked as a doctor for 27 years, and I have heard repeatedly about strategies. What is needed is progress on the ground.
1479. I am thinking of structures, and Heather mentioned that local commissioning groups will have council input. That decision was made — correctly — by the Minister. The Committee visited Pieta House in Dublin, which provides a facility, which seemed to me — as a doctor who has dealt with suicides and the family devastation left in the aftermath — to be the answer. The building provides support for the whole Dublin area and has a lot to do, but, still, it achieves fantastic results. It is non-threatening, which is important because, as a doctor, I see that when young people leave the old-style psychiatric hospitals, they feel almost more suicidal than they did when they went were admitted.
1480. We must find a practical solution: for example, a building in each of the five trusts where councils have an input, and where young people can gain immediate access through accident and emergency departments, the police, GPs, themselves, families and girlfriends or boyfriends. That is what happens in Pieta House — the staff get to patients in their vulnerable first few days when they are most likely to commit suicide and before they have been near a health professional. Do the witnesses agree that a facility such as that is required?
1481. I am on the local commissioning group, although I am not sure if I will be on the next one. There may be three different councils. Local government will have an influence on the commissioning of healthcare. We should not just look at the strategies, which can overwhelm people and — as Alex said — leave people not knowing what they are doing. We should also look at building a non-threatening structure, which may not even be medical, that young people can access immediately. As I have mentioned in other Committee meetings, I know two young men who took their lives before anyone knew that they were depressed. Does NILGA see a practical way forward rather than just strategies?
1482. Ms Donaghy: The only way to advance suicide prevention is on a practical basis. I have worked in the community on the front line with young people who have been suicidal, and the bereaved families of those who have committed suicide. Those people do not want to know what the strategy is — they just want the problem to be resolved.
1483. On average, one person commits suicide each day in Northern Ireland, which demonstrates the enormity of the problem. When someone commits suicide, it is often the local MLA or the council officer to whom those people turn. I am an example of that. The group that I have worked with spans the Armagh and Tyrone areas, and its members did not know what to do. The people who try to address the problem of suicide are often bereaved themselves — either through a loss in the local community or their own sons or daughters — and are trying to help those who are about to be bereaved or who have a child or adult whom they do not know what to do with. Sometimes, the health profession or the Churches fail those people. Often, the problem is that no one in the local community knows where to get help. Even when they do find out where to get help, the professional often acts on a piece of medical information or assesses the situation from a religious or local government viewpoint. The process is not joined up enough for people to know that they have covered all angles. As a result, people sometimes slip through the net.
1484. Therefore, there must be a joined-up approach, which can only be achieved on a practical project-approach basis, with everyone around the table. Otherwise, we will continue to lose people, young and old, and particularly men, to this terrible disease.
1485. The Chairperson: I agree with Kieran — everyone who was at Pieta House left wishing that we had community houses dotted around each trust area. The level and depth of creating the right ambiance and the work that went into creating the beautiful facility, down to the colours, the paintwork and the candles, resulted in a beautiful setting. All the various groups were at hand, including psychiatry and the Churches. Everyone was involved, but the community was driving it. Nobody was turned away. If someone presented at accident and emergency, he or she did not fall out at the bottom; people were taken by taxi to Pieta House, where they immediately received a cup of tea and were able to relax. Everything was well thought out, even down to the seating, where the psychiatrists were sitting lower than those who were traumatised or distressed, and they were followed through the system. Around 1,100 people were catered for in two years, and not one was lost because of the community-based house approach. It was a tremendous inspiration to us all, and we were very envious.
1486. Mr Buchannan: Much of the ground has been covered. I agree with Kieran, in that practical solutions are needed. Obviously, there should be non-threatening areas, with no stigma attached, where those people can go.
1487. The work that bereaved people are doing to help others in a similar situations was mentioned. In some instances, a person who has been bereaved and has gone through that experience can offer help that no one else can provide. Only someone in that position knows exactly what has happened and can remember the signs. It is important that someone who has been bereaved is part of the group, so that he or she can give assistance and guidance on the way forward.
1488. The work of some of the councils was mentioned. Has NILGA made contact with all the 26 councils on the issue and, if so, have any of those councils refused to take up and work on those issues?
1489. Ms Moorhead: NILGA has not done a lot of work on that, because of the capacity issue more than anything else, and so much is happening in RPA. It could do some work to encourage councils to get involved. However, support is needed to have a strategic approach and to define a role and a partnership for local authorities. That would all help to step up the matter.
1490. Ms Donaghy: The 26 councils and NILGA made practical solutions and a joint response through Heather’s offices. We tried to say that local government needs an input at the early stage. Bereaved people have an understanding of the situation, which is essential, and the skills to listen and guide others. However, they should not be spending their time setting up meetings and applying for funding, which they seem to be doing. That diverts them from the help that they are prepared to give, and into a more bureaucratic role. Local government has the skills to help them with that.
1491. The Chairperson: Do you feel that you did not get enough involvement and input into the strategy?
1492. Ms Donaghy: Certainly, we could have added more. We submitted a paper, but we would have welcomed more open discussion. However, we still want to do that, and to add further to our comments and give practical examples and solutions to the issues in the communities.
1493. Mr Buchanan: Is NILGA proposing to contact local councils again about that issue, because it seems that many of the councils are doing absolutely nothing? As you say, they have the skills and the expertise. Is NILGA thinking about making contact again with councils to try to get the necessary input?
1494. Ms Moorhead: We were thinking that a more proactive approach would be a task and finish working group with some of the other key providers so that we could go back and add something productive instead of just saying please get involved. The question is: get involved in what, or do what? We want to define the type of role that we believe that local authorities could be playing and the things that we could be doing.
1495. The important aspect about community planning is that many issues are dealt with at only the coalface instead of there being a long-term public health prevention role. Suicides happen in a society in which things are going wrong. If councils are to have a power of well-being, the question is what role do they need to provide in order to create a sense of well-being, safety and community support in a more fragmented society over the long term rather than dealing with this issue at the sharp end only? Community planning provides for that approach. However, as Anne would say, local government covers a range of services and does not look at the issue in silos.
1496. This is not just a health issue: it is a societal public-health issue, and a solution cannot be arrived at with only a health mindset; a broader mindset is required. As a result, when we become involved in dialogue, we can add value and provide more creative and powerful solutions with a broader approach. Those are some of the solutions that we would like to see coming out of this meeting. Perhaps there are a few of your colleagues in the Health Service at ministerial level with whom we could explore some of those issues and then return with recommendations that councils could be invited to consider. This is just a snapshot: I did not carry out a full survey of all local authorities. However, my point is that some local authorities are doing a lot; others are doing something, while some are not doing anything.
1497. Mr Gallagher: Thank you for that. It is important that there are good links with other agencies, particularly with the Health Service. In the new structures, the Minister of Health, Social Services and Public Safety announced greater opportunity for representation from elected representatives on those structures. Perhaps NILGA is not entirely happy with that arrangement and would like a greater proportion of elected representatives. In addition, has the Department consulted NILGA on the new health structures, and is NILGA one of the consultation team?
1498. Ms Moorhead: We are really pleased that the Minister has singled out NILGA for a proper dialogue with our elected members, and that issue is coming before a full NILGA meeting tomorrow. We are also pleased that the Minister has responded to our request for greater public representation in the new health structures. We want to discuss with the Minister how to get best use from those structures, because we want elected members on the new structures but we also want them to have an institutional relationship with the councils and through community planning. Therefore, we welcome the opportunity; we think that it is a positive move; and we will be looking to see how we can best do that. We find that policy is better when we are engaged at the front end instead of policy being produced and then us being consulted because, by that stage, policy is almost set.
1499. The Chairperson: I thank Anne, Sean and Heather for coming today. That concludes almost everything in our consultation process. We take on board all your views, and we thank you for your paper, which is very helpful. We believe that this is too important an issue to let go; and the Minister, in all fairness, recognises that the way to proceed is to involve as many community groups and elected representatives as possible in drawing up plans to try to alleviate this dreadful curse on the communities that we represent. Thank you for your attendance.
3 April 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Carál Ní Chuilín
Witnesses:
Mr Martin Bell |
Department of Health, Social Services and Public Safety |
1500. The next evidence session is with officials from the Department of Health, Social Services and Public Safety. I remind members that this is the final oral evidence session in which to clarify issues with the Department.
1501. Welcome to Andrew Elliott, director of the population health directorate, Dr Bernie Stuart, director of the mental health and disability services directorate, and Gerard Collins and Martin Bell from health improvement policy branch. You are aware of the format of the session; although we will not be watching the clock, you will have approximately 10 minutes to make a presentation, followed by questioning. I look forward to hearing what you have to say.
1502. Mr Andrew Elliott (Department of Health, Social Services and Public Safety): Thank you. We are most grateful for the opportunity to participate in the inquiry into suicide and self harm. On the two previous occasions that I was in front of the Committee, I was able to begin by saying “This is a highly technical matter”, and then there were no questions, which was wonderful. This occasion is clearly the reverse of that situation.
1503. Suicide and self harm are highly sensitive issues that are most challenging for officials to work on, not only because of the anguish and despair of the affected families, about which the Committee has heard, but because it is difficult to devise interventions that we know will be effective in reducing suicide rates, which are a worldwide problem. Across the globe, people are attempting to find successful means of tackling the problem.
1504. I say that in order to set the context; however, we have developed a strategy. There will always be scope for improvement — for example, we will want to improve the strategy in light of the inquiry’s report — but the strategy provides a good balance of the crucial elements that must be in any strategy if it is to successfully combat suicide. In a nutshell, there are four elements: better joined-up working, particularly in working with communities, which was not always the case in the past; a bigger focus on training and development, which must be implemented across communities, particularly in relation to talking therapies; general improvements in mental-health development; and changes to the way in which services are delivered and resourced.
1505. As I said, there is scope to continue to work on and improve the strategy. Importantly, it was designed to incorporate regular review opportunities. We anticipate that the inquiry will be an important contribution to the next strategy review, providing an opportunity to evaluate and amend it. Therefore, we have followed the inquiry with considerable interest.
1506. Although I do not wish to cover ground that has already been covered, members are aware that the average number of suicides rose from 150 a year between 2000 and 2004 to almost 300 a year by 2006. The 2007 figures indicate a reduction in the suicide rate; however, up to September 2007, 166 suicides were recorded, which means that a great deal of work must still be done to reduce the rate even to 2000 levels. It is well documented that suicide rates tend to fluctuate. Therefore, I am hesitant to claim that the strategy has had any real effect on the figures to date. It is only over the long term that, hopefully, one might begin to detect real changes.
1507. It is also worth reminding ourselves that much of the impetus for the work that we are doing came from families and communities that had been affected by suicide. They had the courage and energy to make the matter a much higher priority than it had been in the past. That has affected the focus of the strategy on issues such as reducing the stigma surrounding mental health in general and suicide in particular.
1508. It is important to say that suicide is often a manifestation of poor mental health and, just as importantly, poor mental well-being. It would be a mistake to try to tackle suicide in isolation from the wider work that is being done in mental health. The Department must always try to keep those two areas of work in tandem.
1509. One in five people here experiences a mental-health problem at some point in their lives. I have read some statistics that suggest that the figure is one in four. There are particular points in people’s lives when they are more vulnerable than at other times, and can be prone to depression, for example. It is important that we be ready and able to help people in those circumstances.
1510. When we assess the various risk factors, we are increasingly seeing the scope for benefits that result from tackling the levels of hopelessness that are to be found in certain parts of society, and in addressing mild depression as well as more severe forms of mental illness. Some pioneering work is going on in Scotland in that regard, particularly in Dumfries and Galloway. We will examine that work closely to determine whether we can use some of the funding that is available as a result of the Bamford Review in that way.
1511. The Department has allocated just over £6 million per annum to suicide-related issues, and some recent developments since the Committee last met have included the establishment of the regional telephone helpline. I am sure that we will talk more about that. Research has begun into the specific effects of the Troubles, how they came to an end and what impact they had on the number of suicides that has occurred.
1512. The new GP depression awareness training programme is also under way. It took a long time to progress, and there is more to do, but a great deal of work has been done in that programme, which is a positive start. We have developed a new North/South public information campaign, which will be beneficial in reaching the wider population. We have also begun to develop a crisis intervention service.
1513. Suicide does not respect boundaries. It is important that we work beyond our borders where necessary, particularly in learning, and we are working with our nearest neighbours in that regard. We must also work more effectively across sectoral boundaries. The various sectors of Government in Northern Ireland can work together more effectively, as indicated in the Investing for Health strategy, in order to achieve better results.
1514. The Department is going through a massive learning process on those issues, and we will know more as a result of this inquiry. We look forward to your questions.
1515. Ms Ní Chuilín: This has been a very important piece of work for us all. There is a massive amount of interest in the outcome of our inquiry. However, there is even more interest in what the Department is going to deliver.
1516. I want to draw the attention of the policy-makers to the lack of an equality impact assessment of the Protect Life strategy. That is a missed opportunity; there are impacts and variations between rural and urban groups in their experiences of the conflict/Troubles, even in relation to age. Our inquiry is time-bound and age-limited, but the Department must return to those issues.
1517. I also want to highlight the “card before you leave” practice, which has been raised time and time again. It is an important issue on which we have received some correspondence. When someone goes to hospital feeling suicidal, they walk out again with no card, no appointment and no hope. They are put on an endless list. That is a basic measure that could be implemented easily, and would give people something to physically and emotionally hold on to. Families, practitioners, stakeholders in the community and those who have used the accident and emergency departments have suggested such a scheme and, therefore, it cannot be ignored. This is the last opportunity to introduce the measure, which would have a big impact on the ground, unless there are massive financial implications. However, even if that is the case, how can financial implications be compared with potential loss of human life?
1518. Ongoing stakeholder involvement is crucial. I know that Mr Bell has worked with groups such as the Public Initiative for the Prevention of Suicide and Self-Harm (PIPS) and Reaching Across to Reduce your Risk of Suicide and Self-Harm (RAYS) in the Shankill area. Unfortunately, while the number of people taking their own lives fluctuates, there is a massive increase in the number of people who are self-harming. The demands are stringent, the services are scarce, and — as Anne Donaghy said earlier — the bereaved receive little support.
1519. The Protect Life strategy and the budget need to recognise, value and support the contribution of those who deliver that vital service while dealing with their own bereavement and grief; they feel the need to help other people by attracting resources and money.
1520. Finally, I want to discuss the monitoring and evaluation of the helpline. The Committee welcomes the introduction of a 24/7 helpline but, as has been raised previously, few members know the number, and when we spoke to families in the Everton Complex, very few of them knew the number either. Although I do not dispute the number of calls that the helpline may receive, it would receive more if awareness were increased. Equally, the groups who work on the ground with bereaved families were not asked their opinion on the delivery of the helpline, and that is crucial, because its success will be underpinned by awareness and knowledge. We must increase access to information, help and support.
1521. Mr A Elliott: I am pleased that Bernie Stuart is in attendance; she is the director responsible for mental-health services policy in the Department, and many of the issues before the Committee straddle service provision, mental-health promotion and suicide prevention. Between us, hopefully, we can answer most questions that may arise.
1522. Dr Bernie Stuart (Department of Health, Social Services and Public Safety): Ms Ní Chuilín talked about the introduction of a card system in hospitals; I am keen to consider that. The Department is aware of major issues concerning the use of hospitals in a crisis situation and has work under way to examine crisis intervention in accident and emergency departments. There are crisis intervention teams in the various board areas, which consider crises from one perspective. The Department is also examining the type of people who attend hospital and are discharged, so we will consider the Committee’s suggestion when developing guidance on those services. We want to develop a protocol that everyone can follow, irrespective of whether the person has, or is on the fringe of, a personality disorder or a mental-health problem.
1523. In our response to the Bamford Review, which is nearing completion, carers’ support is an issue that the Department has raised. The statutory sector must develop its partnership with the voluntary and community sector. That is at the fore of the Department’s strategy, because it is important that the new money gained from the comprehensive spending review is spent not only on the statutory sector but on developing meaningful partnerships with all stakeholders, including the carers’ organisations. The Department has already started to work on that.
1524. Mr A Elliott: The first issue that Ms Ní Chuilín raised was the lack of an equality impact assessment (EQIA) on the Protect Life strategy, which was slightly before my time. However, the strategy will have been screened and a judgement made that an EQIA was not necessary. Given that the Committee has raised the issue, the Department will reconsider the evaluation of the strategy and examine whether more work needs to be done. As Ms Ní Chuilín rightly pointed out, suicide has a differential impact on various groups.
1525. Ms Ní Chuilín: I asked the question because suicide has different impacts. Not to consider those differences would create more inequality for those people in the community who are more socially excluded, and that is the last thing that we want to do. I am not asking for an EQIA for the sake of it but to serve a definite purpose.
1526. With respect, it is not enough for a civil servant to screen the strategy and decide that an EQIA is not appropriate. An EQIA is appropriate, because screening it out means that an extremely marginalised group may be excluded. After all the time that Committee members have spent on this subject, we do not want that to happen. My purpose in asking for an EQIA is not to give you more work, or to make you do it because it is politically correct or trendy; it is because of the differentials in the strategy’s impact. I accept, however, that the decision not to carry out such an assessment was made before your time.
1527. Mr A Elliott: I do not for a moment mean to suggest that EQIAs are done purely for the sake of it.
1528. Ms Ní Chuilín: There has been a culture of that kind of thinking, although I accept that it is not of your making. However, it is important, particularly for people who are extremely vulnerable, that an EQIA be carried out.
1529. Mr A Elliott: The strategy details some stark figures on the differential impacts on, for example, deprived and non-deprived communities.
1530. The question of stakeholder involvement was also raised. The Department considers that the establishment of the implementation body and the opportunity that that provides for a wide range of stakeholders to become involved in influencing and affecting the direction of the strategy will have the greatest impact. We want that to be an effective mechanism and, if there is anything that we can do to strengthen or improve the body, we will consider it.
1531. The Chairperson: I want to flag up a topical and sad issue. The basic finding of the report of the independent inquiry into the case of Madeleine and Lauren O’Neill was that there was poor communication between the professionals involved in Madeline’s care. Reading the report, I was appalled to discover that two thirds of counselling work takes place outside the National Health Service. There is little recognition of professional counsellors who work outside the Health Service and the communication between the private and statutory services is poor — and not just in Madeleine’s case.
1532. What is being done in light of the report’s recommendation that feedback should be available on communication between the private and statutory sectors? In Madeleine’s case, for example, her counsellor had no input into the involvement of the statutory sector in her case. The report suggests that her counsellor was, at best, treated with indifference. Can I be given an assurance that there will be a learning curve from that case, and that we can ensure that the public know and are given some cause to believe that a working engagement exists?
1533. Mr A Elliott: I will speak about the issue in general; not specifically about the O’Neill case. I will then ask Bernie to make a few comments.
1534. The Chairperson: I am referring to the wider issue. Two thirds of counselling work is conducted outside the remit of the NHS. Why is there that lack of communication, which seems to be one of the pitfalls that led to that untimely incident?
1535. Mr A Elliott: An ongoing area of work for the Health Service generally — not simply in Northern Ireland — is to ensure that the statutory services appreciate and value work that is often conducted effectively in the community and voluntary sectors. Such work is not always valued. It is an ongoing cultural issue that we must address.
1536. Dr Stuart: The O’Neill case raised many terrible issues. All the recommendations that have been mentioned are being progressed.
1537. The issue of poor communication has been raised in many independent inquiries. We are considering the issue in a more general way. Apart from reinforcing the existing guidance, we are considering how to train people to communicate better.
1538. Communication between the counselling services of the different sectors was mentioned. In response to the recommendations of the Bamford Review, and as a result of the money that we received from the comprehensive spending review, we have a significant amount to invest in the development of psychotherapies. The process of developing a psychotherapy strategy is ongoing, and we hope to have it ready later this year. In advance of that, targets have been set — by March 2009, no patients within a certain range should have to wait for more than 13 weeks from when they are referred to when they get access to psychotherapy treatment.
1539. The relationship between the private sector and the statutory sector will have to be developed further as part of the wider work on that issue. Workforce issues are part of the response to the recommendations of the Bamford Review. We have realised that it will be a major shift to move towards more delivery of health services in the community, and less in the hospitals, which will require a different workforce. Therefore, a project to consider that issue is under way.
1540. Committee members will be aware that last autumn, the Minister announced a campaign to try to recruit extra mental-health nurses and learning-disability nurses. However, those are not the only areas in which there is a shortfall. We are considering new ways of training more counsellors in order to be able to meet the increasing demand. That will mean that people with mild or moderate depression will have access to that type of service.
1541. We are also considering other innovative ways of addressing that kind of need so that people who do not need access to the most highly qualified psychiatric nurses, can get access to those with lower-level qualifications.
1542. There are probably issues about the standard training of counsellors in general. Some work is under way in England to consider the level of NVQ that should be required in order to allow people to practice. We are awaiting the outcome of that.
1543. In certain cases, people will need to be highly qualified in order to deliver certain services. However, other services — for example, those that require early intervention — may be able to be delivered by someone with a relatively low qualification.
1544. I do recognise the point that much better co-operation is required between both sectors. We do not want all the psychotherapy services to be delivered by the statutory sector, and that will never be the case.
1545. Mr Easton: The document focuses on the statutory medical bodies, as opposed to those based in the community, although you did touch on those, which I was glad to hear.
1546. As regards the community approach, it is important that community groups, the Churches, councils and the various bodies are taken extremely seriously and that they are involved fully in partnership with Department. Without that, the strategy will not work or, at least, its impact will be lessened. I urge the Department to put that approach at the forefront of its thinking. That is vital.
1547. As Carál said, when patients are discharged from hospital, they should be given an appointment card to give them hope. She said also that discharged patients should not merely be given a card and the number of a 24-hour helpline: other services must put in place. We should have a drop-in house, as they have in Dublin, where people affected can contact, for example, local churches. There must be a joined-up approach; people affected should be able to consult ministers or external councillors. All those services must be available to support patients when they come out of hospital and when they are away from their doctors. Things to do should also be organised. When the Committee visited Scotland, we saw how walking groups and reading clubs had been formed. Such activities take people’s minds off problems, and provide a focus. That type of approach is crucial: I urge the Department to consider seriously such activities, in addition to its general approach.
1548. The Chairperson: The house in Dublin, which Alex mentioned, is called Pieta House. It is a model with which all Committee members are very impressed. If you have not visited it, you should make a date to see it. It is community-led, but all the relevant professionals are on hand. It is hoped that it can be turned into a 24/7 service. People presenting at accident and emergency units can be taxied to the house and treated immediately. They are followed and supported throughout their recovery until they are able to cope. Of the 1,100 people who have crossed the threshold, not one has been lost to a completed suicide, which is amazing. It is an excellent model that should be rolled out in every trust area.
1549. Mr Martin Bell (Department of Health, Social Services and Public Safety): I may be able to provide some more information on the community aspects. With respect to Ms Ní Chuilín’s question, working with communities and bereaved families has been one of the most the most rewarding aspects of the strategy.
1550. In ensuring that representation is as it should be, we have not always got it right. That is something that we are learning, and getting better at. For example, local communities and bereaved families have substantial representation on the regional suicide strategy implementation body, and they play an important part in oversight of the whole strategy. A reflection of the importance that we attach to that issue is that in 2008-09, over £2 million, of the £3 million budget, will be allocated as part of a community-support package for local health boards, to help local communities to develop initiatives that will help to tackle suicide and self harm.
1551. We are still learning, but we are keen, and the Minister has given a commitment that communities and bereaved families will be at the heart of everything that we do. Where we have got that wrong, we will change it; we have done so in the past. We are open to making those changes.
1552. With respect to the helpline number, we are aware of the present lack of publicity. As we speak, a substantial advertising campaign is being developed, which will soon go live. Interestingly, prior to the formal announcement of the helpline, Contact Youth, which conducted the pilot scheme, received up to 100 calls per day. Caller activity has increased to between 200 and 250 calls per day, and that is before the advertising campaign has begun. It is clear that knowledge of that helpline has spread by word of mouth. However, we are aware of the need to have a formal campaign, and that will go live shortly.
1553. Mr Easton: We were told that groups such as the PIPS project had to apply for funding a year at a time, and had to spend most of their time trying to obtain funding from different sources. Is it possible to introduce three-year funding cycles to make it easier for such projects to spend more time on their strategies and work, and spend less time chasing after funding?
1554. The Chairperson: We are now in April. What is the situation regarding the funding of the voluntary sector? Are there moneys in place to allow voluntary organisations to continue?
1555. Mr A Elliott: The Department looks to the boards to let organisations know as soon as possible about their funding. There is a reasonable degree of certainty now as a result of the completion of the CSR. There are opportunities, if we move quickly, to get things working. The finance division of the Department has examined the issue of one-year funding, which causes uncertainty until the following year. There are mechanisms evolving through which we can consider the possibility of two-year funding. Boards will be given a little more flexibility in that regard. I understand completely the frustrations created by one-year funding. It not only affects suicide prevention projects, it has an impact across a range of areas, and it provides a real challenge.
1556. The Chairperson: We must always recognise the sterling work carried out by voluntary groups, and how they contribute to the well-being of the communities that they serve.
1557. Dr Deeny: I wish to thank all four of you for meeting the Committee. I have had an interest in these matters not just politically but also as a health professional for some years. Sadly, I have had to deal with suicides and the family devastation that follows. Mr Elliott mentioned the number of people who have mental-health problems. I believe that the number is even higher. Any GP will tell you that 25% to 30% of their consultations are about mental health. Even though that is the case, sadly, some of our patients can, in the space of six months or a year, become actively suicidal and take their own lives. In other countries, as well as our own, there are people who put the rope around their necks, so to speak, even before they have seen a health professional, which is very worrying.
1558. Having been a doctor for some years now, I believe that there is a vulnerable period when a person can become actively suicidal. That is the challenge that we face. How do we get to those people, or get them to the appropriate person during that vulnerable period, before they commit suicide?
1559. The Chairperson made reference, as we did in the previous presentation, to the facility that we saw outside Dublin. As a doctor, that is the best facility that I have ever seen. It is a community-based, friendly centre. It was not an old psychiatric institution with a threatening atmosphere that carried a stigma, which sometimes makes a situation worse; nor did it have a waiting list. We have a waiting list that goes way beyond the vulnerable period. The facility gave immediate access to relatives and friends, accident and emergency departments, GPs and the police. I was glad to hear Dr Stuart mention that, because GPs have been admitting for some time that they have had to prescribe anti-depressants because they do not have access to talking therapies. That is a major problem, so it is good to hear that some of the money that is to be made available as a result of the Bamford Review’s recommendations will be used for the talking therapies. We need well-trained counsellors, and I am glad to hear Dr Stuart say that those therapies will be of an acceptable standard. That is what we saw in Dublin. The Chairperson mentioned that 1,100 people had passed through that facility, which was so friendly, and did not look like a hospital or a health centre at all. As far as I know, not one of those people has committed suicide, which, as a doctor, is a staggering fact for me to hear.
1560. Can the Department see a situation where, given the financial help for talking therapies and by working along with the Northern Ireland Local Government Association, councils, and, indeed, the new commissioning groups, a building could be provided in each of the five trusts that would be immediately accessible to people who are feeling suicidal?
1561. I believe genuinely that, as we saw in Dublin, the telephone helpline provides virtually immediate access, and that service must be provided. A person may not be able to wait over a weekend for support, and may have hung themselves by the Sunday. That is the big challenge. I must admit that I do not know the details of the telephone helpline service, although I should know. Does it have a name? For example, everyone — certainly children — knows about Childline, so perhaps it should be called something such as “Lifeline”, something catchy that people will know about. It should also have a short number, and people should be able to get through to an operator quickly, and, perhaps, be directed to one of the centres. If a person is genuinely feeling suicidal, he or she should be able to lift the phone and speak to someone who will advise where in the trust area he or she can go immediately to receive support. If we can meet that challenge, we will save lives.
1562. Mr A Elliott: In relation to the final point, we see the launch of the telephone helpline as being an opportunity to raise its profile, and to create something that, at least as far as telephony is concerned, is available 24/7. The helpline service should be something that people know about, with a recognisable name, and those aspects are being planned. It is interesting that Dr Deeny mentioned the name “Lifeline” because that is one of the names that is being considered for the telephone helpline. We must make the service something that everyone everywhere knows is available, in case they find themselves in a position where they need it. Bernie will discuss the buildings.
1563. Dr Stuart: As I said earlier, we are looking at developing a psychotherapy strategy. We have the money for that. We have not got as far as spelling out exactly what the community infrastructure will be, but our response to the Bamford Review states that it is not enough to say that we do not need as many hospital places — we need a community infrastructure, and we are working on how that will be implemented. I am interested in exploring how Pieta House in Dublin operates, to see whether something similar to that could be one of the options.
1564. However, we recognise the importance of immediate access to care. As members know, the crisis intervention teams that are in place are all operational to a certain extent but they are not fully staffed yet. Those teams are only working from nine to five but, where possible, we are planning to extend that, in conjunction with the work that we are doing on emergency access with accident and emergency departments. I agree that it is vital that community infrastructure is available to match the need for it, and that matter will be considered more closely.
1565. Mr A Elliott: The thinking about some of the therapies, particularly the talking therapies, is potentially very positive. Some of the work from Scotland that I have seen shows that the benefits of those therapies may extend beyond mental health. If we can successfully find the interventions that build resilience in people, there are potentially significant benefits to be had in reducing cancer, cardio-vascular disease, and a whole range of issues that we deal with. Those interventions are likely to be high quality talking therapies; however, getting from talking therapies to high quality talking therapies is itself quite a big step. Much work must be done to ensure a meaningful delivery of that service in Northern Ireland.
1566. The Chairperson: Unfortunately, we seem to live in a society where people lack coping skills, particularly younger people. Of course, the breakdown of the family unit is an additional problem. However, I hope that you will visit Pieta House and take cognisance of that model, as I suspect that, when you see what it is achieving, you will come back as enthused about it as we were.
1567. Mr Buchanan: Obviously, a lot of work remains to be done between the statutory and community sectors in order to put the jigsaw together and provide the required services for these vulnerable people. That may well leave a vacuum in the short term. Have we fully trained staff in every accident and emergency department in Northern Ireland who can recognise and deal with a suicidal individual who comes through the hospital doors?
1568. Dr Stuart: I will have to come back to members on that. All accident and emergency departments should recognise a serious case. However, we must examine interventions in borderline cases — when it is not clear that somebody is suicidal.
1569. Mental-health disorders do not always show themselves in the same ways. For example, mental-health disorders in young people do not necessarily show themselves in the same ways that they do in adults.
1570. In theory, the answer is yes — we have staff in every accident and emergency department who can recognise and deal with suicidal people — but there are sad cases when people leave accident and emergency departments and commit suicide. There is more work to be done on that.
1571. The qualifications of the staff are not in question; they have the ability to cope with people with serious mental-health problems in a hospital. We want to consider borderline cases, and early intervention, to prevent situations becoming worse.
1572. The Chairperson: We all welcome the ongoing project in north and west Belfast. The sooner that we get those programmes rolled out in east and south Belfast, and within rural constituencies, the better. Indeed, the need can be greater in rural settings due to the isolation that people can suffer.
1573. We all aim to achieve the same objective — a first-class service for those who require it, from the mildly depressed to those who present with very serious psychotic problems.
1574. I thank you all for coming along and for your help. It has been a pleasure working alongside you and seeing you on the number of occasions that we have. No doubt we will see you again soon.
