Session 2009/2010
First Report
COMMITTEE FOR HEALTH, SOCIAL SERVICES AND PUBLIC SAFETY
Inquiry into Obesity
Together with the Minutes of Proceedings of the committee,
minutes of evidence and written Evidence relating to the report
Ordered by the Committee for Health, Social Services and Public Safety
to be printed 1 October 2009
Report: 10/09/10R (Committee for Health, Social Services and Public Safety)
This document is available in a range of alternative formats.
For more information please contact the
Northern Ireland Assembly, Printed Paper Office,
Parliament Buildings, Stormont, Belfast, BT4 3XX
Tel: 028 9052 1078
Committee Powers and Membership
The Committee for Health, Social Services and Public Safety is a Statutory Departmental Committee established in accordance with paragraphs 8 and 9 of the Belfast Agreement, section 29 of the Northern Ireland Act 1998 and under Standing Order 46.
The Committee has power to:
- Consider and advise on Departmental budgets and annual plans in the context of the overall budget allocation;
- Consider relevant secondary legislation and take the Committee stage of primary legislation;
- Call for persons and papers;
- Initiate inquiries and make reports; and
- Consider and advise on any matters brought to the Committee by the Minister for Health, Social Services and Public Safety
The Committee has 11 members including a Chairperson and Deputy Chairperson and a quorum of 5.
The membership of the Committee is as follows:
Mr Jim Wells4 (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mrs Carmel Hanna Dr Kieran Deeny
Mr Alex Easton Mrs Claire McGill1
Mrs Dolores Kelly3 Ms Sue Ramsey
Mr Sam Gardiner2 Mrs Iris Robinson MP5
Mr John McCallister
1 with effect from 20 May 2008 Mrs Claire McGill replaced Ms Carál Ní Chuilín.
2 with effect from 15 September 2008 Mr Sam Gardiner replaced Rev Dr Robert Coulter.
3 with effect from 29 June 2009 Mrs Dolores Kelly replaced Mr Tommy Gallagher
4 with effect from 4 July 2009 Mr Jim Wells replaced Mrs Iris Robinson
5 with effect from 23 September 2009 Mrs Iris Robinson replaced Mr Thomas Buchanan
Table of Contents
Volume 1
1. Introduction
2. Background
Health Implications
Cost of Obesity
Measuring Obesity (BMI)
Causes of Obesity
3. Trends
A Major Global Health Problem
Obesity Prevalence in the UK and ROI
Obesity Prevalence in Northern Ireland
4. Current Approach
Targets
Funding
Life Course Approach
Leadership
Co-ordinated Approach
Existing Initiatives
5. Weight Management
Primary Care
Secondary Care
Bariatric Services
6. Diet and Exercise
Healthy Eating
Food Labelling
Food Portion Sizes
Mixed Messages
Exercise
7. Role of Other Departments, Bodies and Sectors
Role of Local Authorities
Role of the Media
8. Obesogenic Environment
9. Other Issues
Health Inequalities
Community Approach
Workplace Health
Research
Data Collection
10. Conclusion
Appendix 1:Minutes of Proceedings 49
Appendix 2:Minutes of Evidence 73
Volume 2
Appendix 3:Written Evidence
Appendix 4:Other Evidence considered by the Committee
Appendix 5:Minutes of Evidence Session held on 19th May 2009 699
Appendix 6:List of Witnesses who gave Evidence to the Commitee 797
Executive Summary
Obesity is a major global public health problem. Recent decades have seen a significant rise in levels of overweight and obesity in many countries around the world. In a number of the major developed countries, including the UK and the USA, the rates of obesity have doubled in the last 25 years and this relentless increase is predicted to continue in the decade ahead. The most recent Health and Social Wellbeing Survey in Northern Ireland in 2005 found that 59% of all adults here were either overweight or obese, with 24% of adults obese. Worryingly, data from the Northern Ireland Child Health System in 2004/05 found that 22% of children are either overweight or obese, with more than 5% already obese.
The 2007 Foresight Report, a report complied by a panel of leading experts and commissioned by the UK Government, warned that if trends in overweight and obesity continue to rise, there is a real prospect that by 2050, ‘Britain could be a mainly obese society’. It predicted that by that date, 60% of men and 50% of women in the UK could be obese. The Department’s Investing for Health Strategy in 2002 had estimated that by 2010 the cost of obesity to the NI Economy could exceed £500m per annum.
Obesity has been variously described to us as a ‘well established epidemic’, a ‘tsunami’, a ‘crisis’ and a ‘population time bomb’. It is a problem that will have an enormous impact, not just on the health of the population, but something that threatens to engulf the entire health service and it will have a very serious impact on society and the economy. For many people obesity is seen primarily as a vanity or aesthetic issue. However, it has very serious and life-threatening health implications through a wide range of conditions, such as heart disease, type 2 diabetes, some forms of cancer, and high blood pressure. We were told that obesity could cause the present generation growing up to have a shorter life span than their parents.
In this report the Committee looked at both the current strategic approach to the prevention of obesity and the availability of weight management or other services to deal with obesity related ill health.
Prevention
To date, no country in the world has been able to develop an overall strategic approach that has significantly reduced obesity prevalence. However, the recent development of the Healthy Weight, Health Lives strategy in England, represents the first national population-wide strategy but it is too early yet to judge its effectiveness. It is clear that obesity levels have increased steadily over many years and it will take a long-term response to reverse this trend.
In Northern Ireland the Department of Health has moved away from the Fit Futures initiative, which focussed on tackling obesity in children and young people, and has begun to develop a whole life course approach, similar to the Healthy Weight, Health Lives strategy in England. While we support the development of the life course approach we have concerns that the Fit Futures initiative has not been formally signed off and implemented.
All Departments and sectors have a crucial role to play in tackling obesity and all need to be involved and committed to the development of the new life course strategy. We recommend that the strategy should be jointly led by the health and education Departments, as has happened in England. There must be single strong effective leadership to drive the strategy forward and, given the potential for significant cost benefits and the consequences of failure to invest, it needs to be provided with significant resources.
Most Departments outlined the action they currently undertake relating to obesity. As identified in the Fit Futures initiative the importance of working with children and young people on nutrition and exercise cannot be over emphasised. The Department of Education has a particularly crucial role in this and, while we welcome the action being taken on nutrition in schools, we call on that Department to make PE in schools compulsory and subject to regular monitoring.
We recognise the potential for the draft 10 year Strategy for Sport and Physical Recreation in Northern Ireland, developed by the Department for Culture, Arts and Leisure in 2007/08, to contribute to a reduction in obesity and we call for it to be resourced and implemented without further delay.
While the cause of obesity can be described in simple terms as an imbalance between the amount we eat and the level of exercise we undertake it cannot be solved by individuals alone. There are many and varied environmental factors, from the accessibility and marketing of food, to transport, planning and other issues that dissuade a healthy diet and physical exercise and these must be tackled. Referred to as the ‘obesogenic environment’, its influence and impact is not widely understood or adequately addressed.
Other issues dealt with in the report include, the role of the new Public Health Agency, the role of local authorities, the potentially positive and negative roles of the media, as well as the need for a community approach and the need to tackle health inequalities. We also identify the need for better co-ordinated research and more representative and reliable data collection.
Weight Management Services
We are very concerned to learn about the current levels of obesity related ill health throughout Northern Ireland and particularly by the number of severely obese patients for whom lifestyle and drugs have failed. These patients now face the prospect of bariatric surgery and the subsequent need for lifelong medical follow-up treatment. We are gravely concerned at the dearth of services at primary and secondary level to deal with those who have serious medical conditions related to severe obesity and the absence of any services to prevent further weight gain in patients with lower degrees of overweight.
We witnessed the frustration of frontline clinicians who told us that services designed to address specific clinical conditions, such as diabetes, cannot adequately address the needs of obese patients. The absence of effective interventions for children with obesity was also highlighted to the Committee.
It is estimated that as many as 50,000 people in Northern Ireland may be eligible for bariatric surgery and this service is currently not provided within Northern Ireland. Last year around 80 people were referred for bariatric surgery to Great Britain. It has been estimated that the cost of treating just 1,000 patients and providing the necessary medical follow-up could be around £10 -£15 million.
On the positive side we recognise that small weight losses do produce health gains and research shows that even a modest reduction in weight of 10% can have a significant impact on a patient’s health. Further delay in providing a comprehensive range of appropriate weight management services will result in greater long term costs. An urgent review to develop such a range of services must be undertaken now.
Summary of Recommendations
1. Obesity is the most serious and most challenging public health issue that we face at this time and it is also one of the most complex. There is therefore an urgent need to develop and implement a comprehensive and robust strategy to address the issue. (Paragraph 49)
2. We share the deep concern of those who expressed regret that the Fit Futures Implementation Plan has not been formally signed off and implemented. The failure to do so has, we believe, created uncertainty and a potential hiatus until a full strategy is in place. (Paragraph 50)
3. We welcome and support the plans by the Department to develop a life course strategy however we fully recognise that tackling obesity effectively is not solely a matter for the health service. We note that the Fit Futures Report contained a joint target with the Departments of Education and Culture, Arts and Leisure. We strongly recommend that the new life course strategy be developed jointly in partnership with other departments, particularly the Department of Education, as has happened in England. (Paragraph 51)
4. Growing levels of obesity will continue to generate enormous costs to society, particularly the health and social care sector in the years ahead. Given this and the potential for significant cost benefits, we belief it is imperative that substantial and sustained resources are provided to implement the new life course strategy. We would urge that this funding be ring-fenced for at least the first phase of implementation (3-5 yrs) to ensure that it is not impacted by other acute and emerging priorities.(Paragraph 52)
5. It is very clear that single strong effective leadership is crucial in tackling obesity but the exact locus of that leadership has been the subject of debate. We recommend that the question of who provides overall leadership be considered in depth during the development of the Life Course Strategy and widely consulted upon before reaching a decision. (Paragraphs 57-58)
6. We recognise that the establishment of the new Public Health Agency provides a unique opportunity to develop a joined-up approach across all Government Departments, public sector agencies including local authorities, the private sector, and the voluntary and community sectors to tackle obesity. We advocate that the Agency make this issue a top priority and we urge all departments to play their part in delivering a concerted long-term response. (Paragraph 62)
7. We recommend that the Department commission an urgent audit of existing obesity-related initiatives so that the need for evaluation or further research can be identified and examples of good practice can be rolled out more widely. We recommend that the Public Health Agency, perhaps in conjunction with the planned All-island Obesity Observatory, develops and maintains a central data base of projects and develops standardised evaluation tool kits. (Paragraph 70)
8. We recommend that the Department, in conjunction with the Health and Social Care Board, develops a range of evidence-based referral options for use by primary care practitioners. (Paragraph 82)
9. We urge the Minister to exert influence at a national level to introduce the allocation of Quality and Outcomes Framework (QOF) points for positive obesity management rather than simply for maintaining a register of obese patients. (Paragraph 83)
10. We call on the Minister, as a matter of urgency, to undertake a comprehensive review of weight management services at all levels for adults and children. The review must address the need for dedicated obesity clinics and a separate bariatric service for Northern Ireland, including the provision of bariatric surgery and the lifelong medical follow-up for individuals required following such surgery. The review should also consider the merits of adopting examples of good practice from elsewhere, such as the Counterweight programme in Scotland and the Carnegie Weight Management programme in England. (Paragraph 100)
11. We urge the Department and the Food Standards Agency to continue to work with manufacturers and to exert pressure at a national and European level to introduce regulatory controls on the levels of salt and saturated fat in manufactured foods. (Paragraph 108)
12. We fully support the calls for a single, consistent food labelling scheme using the traffic light system and urge the Minister and the Food Standard Agency Northern Ireland to consider whether such a system could be made mandatory on all food retail products. We also call for more action to enforce a similar clear and simple nutrition labelling system at non-retail outlets, such as restaurants and catering establishments. (Paragraph 114)
13. While recognising the difficulty in regulating food portion sizes in catering and similar settings, we urge the Department and the Food Standards Agency Northern Ireland to examine how issues like food promotion and pricing impact on portion sizes and how they might be influenced. (Paragraph 118)
14. We believe there is confusion over what exactly constitutes ‘five portions of fruit and vegetables a day’ and particularly around the size and content of a portion. We urge the Public Health Agency to examine how greater clarity and understanding about this health message, and how it might impact on levels of obesity, can be achieved. (Paragraph 120)
15. We call on the Executive to ensure that the Strategy for Sport and Physical Recreation in Northern Ireland is properly resourced and implemented without further delay and that this work dovetails with the development of the life course obesity strategy. (Paragraph 128)
16. We urge each and every Department to recognise that they have a crucial role to play in responding to the obesity epidemic either through direct action or through policies and practices that impact on the obesogenic environment. (Paragraph 135)
17. We call on the Department of Education to make at least 2 hours of PE in schools compulsory and subject to regular monitoring by the Educational and Training Inspectorate. (Paragraph 142)
18. We urge the full involvement of local councils in developing the new life course strategy. (Paragraph 147)
19. We urge the Minister to work with colleagues throughout the UK to explore the feasibility of banning the advertising of food and drink products that are high in fat, salt or sugar before the 9 pm watershed. (Paragraph 152)
20. We call on the Minister to develop a comprehensive media approach as part of the life course strategy and to consider, for example, how new and emerging media such as text and Twitter could be used to engage with young people. (Paragraph 153)
21. We call on the Executive to fully recognise the potential impact of the obesogenic environment on the health and wellbeing of the population and to consider the merits of introducing a system whereby the impact of all major policy decisions are subject to an obesity proofing exercise. (Paragraph 162)
22. In developing the Life Course Approach we urge the Department to take account of health inequalities and particularly the need to address the higher levels of obesity in areas of social deprivation. (Paragraph 171)
23. We recognise the benefits for both employers and employees of promoting healthy lifestyles in the workplace and we urge all employers to consider initiatives that promote healthy eating and greater levels of exercise in the workplace. (Paragraph 176)
24. We urge the Department to examine how data collection can be improved through reform and better funding of the Child Health System. This should facilitate extending BMI measurements beyond Primary One children. Enhanced funding should also facilitate better collection of adult data based on actual BMI measurements rather than self-reporting. (Paragraph 187)
Introduction
1. Obesity is a complex condition which poses a serious threat to health and well-being on a global scale and, to date, no country in the world has been able to develop an effective overall approach to successfully address the issue. The Committee is conscious that within Northern Ireland around 60% of the adult population and 25% of children are either overweight or obese and this is predicted to grow significantly over coming years. The Committee recognises that action must be taken now to prevent the cost to the health service and to society generally from escalating out of control.
2. This report sets out the results of the Committee examination of the current strategic approach to tackling obesity and its impact on health and well-being. In particular the Committee has looked at:
- the scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change;
- the availability of weight management or other intervention services to tackle obesity related ill health; and
- what further action is required, taking account, of the potential to learn from experience elsewhere.
3. The Committee invited written submissions from a wide range of organisations and groups both within Northern Ireland and further afield and placed notices in the main newspapers. As with many public health issues the Committee recognised that tackling obesity is not just a matter for the health Department and, accordingly invited views from all Departments and Assembly Statutory Committees. The Committee took formal evidence from seventeen separate organisations over a four month period from February to June 2009. Recognising the importance of research into methods of tackling obesity and the need to incorporate that research into policy and practice, the Committee organised a Research Round-Table Event in Parliament Buildings involving a number of eminent academic experts in the field from throughout the United Kingdom and the Republic of Ireland and a small number of key stakeholders.
4. We are grateful to all those who helped us with this Inquiry, including those who provided oral or written evidence and those who participated in the Research Event. We are particularly grateful to those from outside Northern Ireland who came and shared their expertise and experience with us.
Background
Health Implications
5. The Department defined obesity as “a condition where weight gain has got to the point that it poses a serious threat to health".[1] The severity of that risk to health from being overweight or obese does not appear to be widely recognised or understood. The Executive Director of the Northern Ireland Food and Drink Association reminded the Committee that only 6% of people understand the risks of being overweight. He said “Obesity is seen as a vanity rather than a health issue, and we must change that mindset".[2] The British Medical Association put it very starkly saying that obesity “is a population time bomb that will, perhaps, cause the generation growing up to have a shorter lifespan than their parents".[3] The Public Health Agency pointed to recent studies which “suggest that the risk of premature death in people with obesity is similar to that seen in people who smoke more than 10 cigarettes a day. Obesity is therefore not an aesthetic issue – it shortens life and increase the risk of a range of conditions".[4]
6. The Department in its evidence listed ten serious conditions associated with obesity and added that, “evidence also indicates that obesity can reduce life expectancy by approximately 9 years; and can impact on emotional/psychological well-being and self-esteem, especially among young people."[5] The British Medical Association listed the four most common health problems associated with obesity as heart disease, type 2 diabetes, hypertension and osteoarthritis.[6]
7. The British Heart Foundation Northern Ireland pointed out that, “heart and circulatory disease is Northern Ireland’s biggest killer – responsible for more than one in three deaths each year"[7]. The Foundation stated that, “obesity is, in itself, an independent risk factor for heart disease, but it can also be seen as an accumulator, in that it has an effect on other risk factors including diabetes and hypertension, which is also linked to stroke".[8] The British Heart Foundation Northern Ireland referred to the INTERHEART study which estimated that 63% of heart attacks in Western Europe are caused by abdominal obesity[9].
8. Mr Iain Foster, Diabetes UK, explained the impact of obesity as a significant factor in the number of those suffering from type 2 diabetes in Northern Ireland. He stressed the importance of getting beyond the misconception that diabetes is a mild condition. He said, “It is not mild; it is a chronic condition that has no cure. Type 1 diabetes will take up to 20 years off a person’s life expectancy. Type 2 diabetes will take up to 10 years off a person’s life expectancy." Mr Foster stressed that while obesity has no connection to type 1 diabetes “weight contributes to around 80% of cases of type 2 diabetes".[10] Dr Michael Ryan, a frontline clinician, estimated that “about 90% of the patients that attend my diabetes clinics have weight-related issues". Dr Naresh Chada, DHSSPS, pointed out that 65,000 to 70,000 people suffer from type 2 diabetes and said that, “if we do not halt the year-on-year increase in obesity, we could have another 10,000 to 15,000 people with diabetes in Northern Ireland by the early to middle part of the next decade."[11]
9. A Report by the Northern Ireland Audit Office into Obesity and Type 2 Diabetes in Northern Ireland[12] confirms that weight gain is a major influence on the prevalence of type 2 diabetes which is the most common form of diabetes. The Report also highlighted the increasing prevalence of type 2 diabetes in younger people, partly due to lifestyle factors such as diet, lack of physical activity and obesity. This supports the statement by Dr Ryan who said that, “When I was training, type 2 diabetes was called ‘maturity-onset diabetes’. Nowadays, I see 18 and 19-year-old people with that condition, and paediatricians are seeing it in the under 16s. That was unheard of."[13] The Health Minister, in a debate in the Assembly on diabetes, acknowledged that, “the Health Service as we know it will be overwhelmed in twenty years time if we do not tackle diabetes, obesity, and lifestyle. Hospitals are filled with people, who, had they made different lifestyle choices 20 or 30 years ago, would not be there."[14]
10. The link between obesity and cancer is perhaps not so widely recognised. However, Dr Chada, DHSSPS, warned that, “Cancer — particularly gynaecological cancers — are also associated with obesity. I refer to cancer of the uterus, cervix and ovary. Men may be affected by bowel and prostate cancer. A certain proportion of cancers can be attributed to obesity."[15] Action Cancer highlighted that, “two thirds of cancer can be prevented through lifestyle changes, such as more exercise and a change in eating habits"[16] while the British Medical Association pointed out that “obesity increases the likelihood of developing cancers such as breast, colon, endometrial, oesophageal, kidney and prostate cancer by up to 33%"[17].
11. The Royal College of Psychiatrists argued that, “people with mental illness and those with learning disabilities are more likely than the general population to be obese, to have physical health problems arising from this, and to have difficulty managing weight." The Royal College suggested that the reasons for this are complex and could include living in an area of social deprivation, inactivity, medication factors, emotional eating, as well as a reluctance of medical practitioners “to raise the issue of weight with a person who is already vulnerable"[18]. The Belfast Health and Social Care Trust Physiotherapy Service agreed that, “people with mental illness are predisposed to the development of obesity by the nature of their illness; the situation is however made worse by the fact that the medication prescribed for the treatment of their condition does in fact further increase their likelihood of developing obesity".[19]
12. The Chartered Society of Physiotherapy suggested that, “The incidence of falls is another factor that has an impact… an obese person’s muscles become weaker — their muscle tone lessens and their balance reduces; therefore, the risk of falls or of osteoporosis from not doing weight-bearing exercises is increased."[20]
13. Nevertheless, the British Medical Association and others stressed to the Committee “there is nothing about this problem that is inevitable"[21]. Dr Ryan agreed, saying that, “The impact of obesity and overweight is worse than all the cancers put together, on an epidemiological basis, and yet we can intervene, and it can be prevented if caught early enough."[22] In his written evidence Dr Ryan stated that, “there is incontrovertible evidence that weight reduction, however achieved, is effective in reducing morbidity and prolonging life".[23] The Belfast Health and Social Care Trust Physiotherapy Service referred to the Crest Guidelines which “highlight the fact that even a 10% reduction in weight can induce up to a 50% reduction in obesity related cancer deaths, up to a 50% reduction in the development of diabetes as well as having a significant positive impact on lowering blood pressure and cholesterol levels."[24]
Cost of Obesity
14. In addition to the serious health implications for individuals, policymakers are increasingly concerned that the growing obesity problem will place a substantial financial burden on their respective health finances. This is particularl y pertinent within the four universal, tax-funded health systems of the NHS. According to the 2007 Foresight Report in the United Kingdom “by 2050, 60 per cent of males and 50 per cent of females could be obese, adding £5.5 billion to the annual cost of the NHS, with wider costs to society and business estimated at £49.9 billion."[25]
15. Many of the submissions to the Inquiry pointed to the enormous social and economic costs of obesity, not only for the health and social care service, but for the overall economy and wider society. Belfast City Council pointed out that, “the social and economic costs of obesity are enormous and have the potential to increase significantly over the coming years."[26] The Institute of Public Health told us that, “The loss of productivity and the costs of care and treatment of obesity and related conditions have serious effects on the economy and threaten to engulf the health service. Obesity is estimated to cause 450 deaths per year, £14.2 million in lost productivity and £90 million cost to health and social care."[27]
16. The Northern Ireland Audit Office Report[28] concluded that in Northern Ireland the cost attributable to the lack of physical activity includes over 2,100 deaths each year but it found that no robust estimate of the overall health care costs of treating diabetes was available from the Department. Sustrans reminded us that the Department’s Investing for Heath Strategy back in 2002 had estimated that obesity caused over 450 deaths per annum; equivalent to over 4,000 expected years of life lost; 260,000 working days lost each year; and the approximate cost to the economy of £500 million.[29] The British Medical Association suggested that, “tackling obesity could save the health service in Northern Ireland £8.4 million, reduce sickness absence by 170,000 days and add an extra ten years of life onto an individual’s life span."[30]
17. There were also warnings that things could get worse. Professor McCartan, Sport NI, said that, “One of our concerns is that, if we do not act quickly, the problem will simply get bigger. That is why we are saying that Government must act now. The longer we delay, the more it will cost in future and the bigger the problem will be when we finally decide to act."[31]
Measuring Obesity (BMI)
18. One of the key methods used to measure obesity prevalence around the world is Body Mass Index (BMI). BMI is a simple index of weight-for-height and is recognised by the World Health Organisation (WHO) as the most useful mechanism in providing a population-level measurement of overweight and obesity. Adults with a BMI of 25-30 are classified as being overweight and those with a BMI of 30 or more are classified as obese. However, it is also recognised that there are certain limitations associated with BMI while recent research has advocated the measurement of waist circumference as being more closely associated with mortality and morbidity than BMI.[32]
19. The Obesity Management Association, for example, argued that, “BMI as a benchmark is outdated and restrictive – it does not allow all health factors to be taken into account."[33] Dr Ryan said, “I accept that the BMI is an imperfect measure. I have been waiting for 20 years for the perfect measure. The difficulty is that meanwhile, patients are dying. We cannot wait for the perfect measure".[34]
Causes of Obesity
20. Historically, obesity had been thought of as a simple matter of an imbalance between energy intake and energy expenditure or, in other words, an imbalance between the amount we eat and the level of physical activity we undertake. However, many of the submissions to the Inquiry were keen to point out that the cause of obesity is often a complex mix of genetic, physiological, behavioural and environmental factors. Although the specific causes of obesity at an individual level are varied it is accepted that, “at the heart of obesity lies a homeostatic biological system that struggles to maintain energy balance to keep the body at a constant weight. This system is not well-adapted to a fast-changing world, where the pace of technological progress has outstripped human evolution."[35]
21. The South Eastern Health and Social Care Trust suggested that, “obesity should be understood in a wider context than simply a lifestyle choice concerning nutrition or physical activity. Obesity is often combined with issues of mental health, self esteem, isolation, family support and emotional wellbeing."[36] Ballymena Borough Council argued that, “One school of thought would suggest that obesity is due entirely to personal lifestyle and diet choices. Another however is that people today generally do not have less willpower nor do they eat more than previous generations and that it is important to look beyond the obvious and to accept that society has radically altered over the last 5 decades, with major changes in work patterns, transport, food production and sales. It is thought that these changes have exposed a common underlying biological tendency to both put on weight and retain it.[37]
22. Action Cancer pointed out that, “it is important to remember that nobody chooses to be overweight. People choose certain behaviours that have poor health consequences."[38] Conservation Volunteers argued that, “It is recognised that the fundamental causes of obesity are lack of physical exercise and poor diet. A number of other factors are also being taken into consideration, such as increased consumption of high calorie energy dense foods, increased levels of TV watching, use of games consoles, advertising and promotion of unbalanced diet, availability of convenience food, cost of healthy food options, inadequate cooking skills, and transport and planning decisions."[39] It is also clear that there are definitive links between poverty, poor diet and obesity – see paragraphs 163 et seq.
23. It is also accepted that the pattern of growth during early life is one determinant of the future risk of obesity. “A baby’s growth rate in the womb and beyond is in part determined by parental factors, especially with regard to the mother’s diet and what and how she feeds her baby".[40] The period soon after birth is believed to be a time of ‘metabolic plasticity’ and while there is less evidence of a link between actual birth weight and obesity, it is weight gain in early life that appears to be the critical issue. Breast-fed babies show slower growth rates than formula-fed babies and this may contribute to the reduced risk of obesity later in life. It appears that low birth weight babies may be susceptible to a catch-up rapid weight gain while other babies may experience this as a direct result of their diet.[41]
24. Research published recently also suggested that there is a strong link in obesity between mothers and daughters and fathers and sons, but not across the gender divide. The study concluded that, “Childhood obesity today seems to be largely confined to those whose same-sex parents are obese, and the link does not seem to be genetic. Parental obesity, like smoking, might be targeted in the interests of the child."[42]
25. Dr Jane Wilde, Institute of Public Health in Ireland, summed it up saying, “At the heart of the problem is the imbalance between what we take in and what we put out — in other words, the energy we expend. All the studies that have examined the issue from a scientific angle say that the problem will not simply be solved by individuals … we really must take a wider view and see the problem in a social, environmental and economic context."[43] The recognition that obesity is a complex issue therefore means that it requires, as the Public Health Alliance pointed out, “integrated cross-cutting solutions and involve much more than interventions and services aimed at addressing lifestyle and behaviours".[44]
Trends
A Major Global Public Health Problem
26. In recent decades, there has been a significant rise in levels of overweight and obesity in many countries around the world. According to the World Health Organisation (WHO), excess body weight poses one of the most serious public health challenges of the 21st century.’[45] According to the WHO’s latest projections, globally, in 2005 there were approximately 1.6 billion adults (15 years and over) overweight and at least 400 million obese. Twenty million children under the age of 5 years were overweight globally in 2005. Furthermore, the WHO projected that by 2015, there will be approximately 2.3 billion overweight adults and more than 700 million will be obese.[46] In Europe alone, it is projected that the rapidly increasing prevalence of obesity will include 150 million adults and 15 million children by 2010.[47]
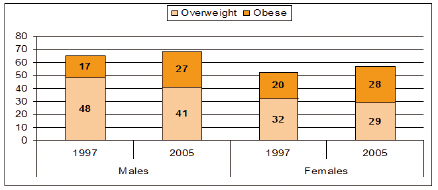
Figure 1: Percentage of the adult population assessed as obese in a selection of countries from around the world (Obese defined as BMI = 30kg/m2)[48][49]
27. A substantial body of research and empirical evidence in recent years highlights the continuing rise in overweight and obesity within both industrialized and developing/low income countries around the world. In a number of the major developed countries including the UK and the USA, the rates of obesity have doubled in the last 25 years. An OECD report published in 2009 analyzing past and projected future trends in a number of selected member countries concluded that prevalence rates of obesity and pre-obesity have been continuing to increase relentlessly in recent decades and will continue to do so in the decade ahead. The report states that, “projected trends in adult overweight and obesity (15-74 years) over the next 10 years…predict a progressive stabilization or slight shrinkage of pre-obesity rates in many countries with a continued rise in obesity rates."[50] This statement correlates with the percentage of obese adults within many of the industrialized countries around the world, including within the United Kingdom and the Republic of Ireland as illustrated in Figure 1. While specific figures for Northern Ireland are not included in Figure 1, levels of overweight and obesity continue to rise with around a quarter of the adult population in Northern Ireland classified as obese (see below). This follows a similar trend in other parts of the United Kingdom and the Republic of Ireland.
Obesity Prevalence in UK and ROI
28. Overweight and obesity prevalence rates among children and adults throughout the United Kingdom and the Republic of Ireland have continued to rise in recent decades to the extent that the scale of the problem is increasingly recognized as having become an ‘epidemic’. Available data for the four jurisdictions of the United Kingdom and the Republic of Ireland show significant prevalence rates for obesity and overweight. According to the Foresight report[51], in 2003/2004, the mean body mass index (BMI) of men and women in the UK general population was 27kg/m2, which is outside the healthy range of between 18.5-25 kg/m2. Significantly, the Foresight report warned that if trends in overweight and obesity continue to rise, there is a real prospect that by 2050, ‘Britain could be a mainly obese society’. According to the report, the rates of obesity are estimated to rise by 2035, to 47% of men and 36% of women in the UK. The headline figure that emerged from the report is that by 2050, 60% of men and 50% of women in the UK could be obese.[52]
29. Meanwhile, in the Republic of Ireland, the 2007 Survey of Lifestyle, Attitudes and Nutrition in Ireland (SLAN) reported that 39 per cent of the adult population were overweight and 25 per cent were obese. Following a similar trend in the UK, overweight and obesity levels in the Republic of Ireland have continued to rise or remained the same over the period of the previous two surveys in 1998 and 2002. Obesity levels based on self-reported data have increased over the period of the three surveys, from 11% in 1998 to 15% in 2002 and levelled off at 14% in 2007. Overweight levels have increased between 1998 (31%) and 2002 (33%) and increased again in 2007 (36%).[53] While these figures do not include measured BMI of individuals and are reliant on self-reported data through completion of questionnaires, the data indicates there has been a significant rise in the prevalence of overweight and obesity in the Republic of Ireland in the last decade.
Obesity Prevalence in Northern Ireland
30. Like other parts of the United Kingdom, levels of overweight and obesity have risen significantly throughout the population of Northern Ireland in recent years. On 13 November 2008 at the opening of the All-Island Conference on Obesity (‘Obesity: weighing up the evidence’), Health Minister, Michael McGimpsey, acknowledged that “There is no doubt that the obesity time bomb in Northern Ireland is ticking louder than ever. Our level of obesity, especially amongst our children is incredibly worrying."[54]
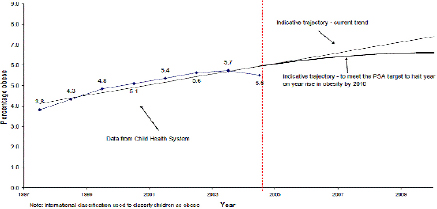
31. At the same conference, Dr Brian Gaffney, chief executive of the former Health Promotion Agency, citing figures from Northern Ireland’s 2002 public health strategy Investing for Health stated that an estimated 450 deaths a year are attributable to obesity and that obesity costs the local economy approximately £500 million per year. Investing for Health predicted that if the upward trend in the rising obesity levels continued ‘by 2010, 23% of women and 22% of men will be obese’. The extent and seriousness of the obesity problem in Northern Ireland is reflected in the fact that figures predicted in Investing for Health were already surpassed by the figures to emerge from the 2005/06 Health and Social Well-Being Survey. According to the survey, 25% of men and 23% of women in Northern Ireland were identified as having a BMI of 30 or over and therefore classified as obese.
Table 1: Proportion of Adults in each Health and Social Services Board areas who were overweight or obese by gender (2005-2006)[55]
| Overweight | Obese | |||||
| HSSB | All | Male | Female | All | Male | Female |
| Eastern | 32% | 36% | 29% | 21% | 21% | 21% |
| Northern | 37% | 38% | 35% | 26% | 27% | 24% |
| Southern | 35% | 41% | 29% | 28% | 27% | 28% |
| Western | 36% | 44% | 28% | 23% | 26% | 21% |
| NI | 35% | 39% | 30% | 24% | 25% | 23% |
32. According to the Child Health System (managed by the former four Health and Social Services Boards) in 2003-04, one in four girls and one in five boys in Northern Ireland were found to be overweight or obese in Primary One. The percentage of children classified as obese in Primary One has increased year on year since 1997. More recent data from DHSSPS shows that the level of obesity in Primary One has declined slightly since 2003-04 from 5.7% of the age group to 5.1%. Moreover, the Young Hearts study of 12 to 15 year olds living in Northern Ireland reported that levels of overweight and obesity increased in the decade 1990-2000.[56]
33. In September 2007, the DHSSPS provided additional funding across the former four Health and Social Services Board areas to collect and record BMI measurements of all Year 8 and Year 9 pupils. In their submission to the Inquiry, the Southern Health and Social Services Board noted that, ‘To date, 89% of Year 8 pupils [have had] their weight recorded and this indicates that 11% of children weighed fell into the obese category and 1% in the underweight category’.[57]
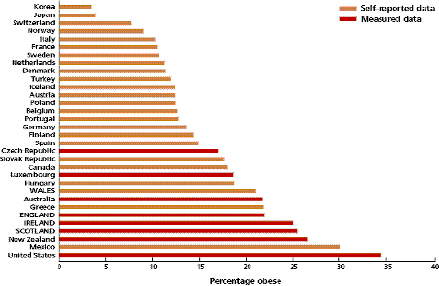
Figure 2: Obesity prevalence trends in Northern Ireland from 1997/98 to 2004/05 for P1 pupils, with possible trajectories for 2005/06 to 2010/11[58]
34. In her review of the comparative analysis of anti-obesity policies in operation throughout the devolved regions, Musingarimi[59] highlights a number of points which currently undermine the comparative analysis of the prevalence rates across the UK. Firstly, she points to the fact that in the UK data on health (including overweight and obesity) are collected separately in the devolved regions and currently there is no single UK-level obesity surveillance survey undertaken. Musingarimi argues that the employment of different methods of data collection within the UK undermines the quality of data available ‘which inhibits any truly reliable comparison of obesity prevalence rates in the four countries’. For example, data for measuring levels of obesity and overweight in England and Scotland is collected using actual measurements of height and weight, whereas in Wales and Northern Ireland less reliable self-administered questionnaires are used. Secondly, Musingarimi concludes that there are ‘critical issues’ particularly in Wales and Northern Ireland relating to the availability of reliable and accurate data on the prevalence rates of obesity
Current Approach
35. The Department in its written submission explained the development of policy over recent years in relation to tackling obesity.[60] The Department referred to the publication of the Investing for Health Strategy in March 2002 which set out how the commitment of ‘working for a healthier people’ in the Programme for Government would be achieved.
36. The development of policy subsequently included the establishment by the Ministerial Group on Public Health of the Fit Futures Taskforce to examine options for preventing overweight and obesity in children and young people. Considerable consultation and engagement took place leading to the publication of the Fit Futures Report in 2006. Following completion of the report a Fit Futures Implementation Plan was developed and published for consultation in February 2007. However, shortly after publication of the draft Implementation Plan, which focused on children and young people, the Department altered its approach stating that it recognised the need to develop a whole population approach to tackling obesity.
37. The Northern Ireland Commissioner for Children and Young People pointed to the fact that, “to date no information is available on the Department of Health, Social Services and Public Safety (DHSSPS) website as to the status of the implementation plan… If these actions are fully implemented it will have a positive effect on the health and wellbeing of children, in particular the levels of child hood obesity."[61] The Department acknowledged that the Fit Futures Implementation Plan was not finalised and it sought to reassure the Committee that, “while this implementation report was not formally published by the Department, progress has been, and continues to be, made to deliver on its recommendations and actions at both the regional and local level."[62]
Targets
38. The Department pointed out that the Fit Futures Report “contained a joint target, between DHSSPS, the Department of Education (DE), and the Department of Culture, Arts and Leisure (DCAL), ‘to halt the rise in obesity in children by 2010’"[63]. The Committee also noted that the 2002 Investing for Health Strategy contained a target ‘to stop the increase in the levels of obesity in men and women so that by 2010 the proportion of men who are obese is less than 17%, and of women, less than 20%’.[64] This target will clearly not be achieved and it may be appropriate to question the determination to do so given that the emphasis until recently has been on efforts to reduce overweight and obesity in children. The Committee notes that a review of Investing for Health Strategy is currently underway.
Funding
39. The Department in its submission to the Inquiry stated that it had “allocated £832,000 to the implementation of Fit Futures in 08/09. In addition, a further £550,000 and £300,000 has been allocated for work around promoting physical activity and improving food and nutrition respectively." By comparison the Department noted that in Scotland an additional £40 million has been allocated over a three year period under the Comprehensive Spending Review 2007.[65]
40. The provision of specific funding to address obesity was not identified by respondents as a major issue at this juncture. The Committee recognises that, while it is clear that adequate resources to tackle the problem must be provided, it is difficult to identify the extent of existing resources devoted to the issue. The Committee noted, for example, that the Department was unable to provide the Northern Ireland Audit Office with any robust estimate of the overall health care costs of treating diabetes.[66]
Life Course Approach
41. The Department advised the Committee that as a result of the findings of the Foresight report it decided to develop a life course approach to preventing obesity. As part of this the Department established a cross-sectoral Obesity Prevention Steering Group in February 2008 “to oversee the progress against the Fit Futures recommendations, and lead the development of an overarching policy to prevent obesity across the life course". To support the work of the Obesity Prevention Steering Group four policy advisory sub-groups have been set up to deal with food and nutrition; physical activity; education, prevention and public information; and data and research.[67]
42. In its final evidence to the Committee on 18 June 2009 the Department gave further details of the plans and timescale for addressing obesity across the life course. Officials stressed that the 10-year strategic framework “will be outcome-focused and outcome-based. It will take a thematic approach to the life course." The planned timescale involves the development of the framework between October 2009 and January 2010 and, following public consultation, “we hope to launch the strategy by June 2010".[68]
43. The proposed strategy in Northern Ireland is based on the approach adopted in the English obesity strategy Healthy Weight, Healthy Lives launched in January 2008. The English strategy, which is the only population-wide strategy being implemented in the United Kingdom currently, was developed in response to the findings of the Foresight Report.[69] The strategy in England is being taken forward by a Cross-Government Obesity Unit led jointly by the Department of Health and the Department for Children, Schools and Families and reports to a new Cabinet Committee on Health and Well-being. Clara Swinson, Deputy Director of the Cross-Government Obesity Unit in the Department of Health, told the Committee that, “in England, about 60% of adults and 30% of children are overweight or obese. The Foresight expert review, launched in 2007, said that that figure would rise if nothing was done. The experts predicted various stages up until 2050, by which time the majority of adults would be obese and only 10% would be a healthy weight... our strategy is based on the areas that are identified in the Foresight report, which looks at both individual action and the wider environment because of the obesogenic and passive-obesity issues."[70]
44. A number of respondents expressed mixed views on the Department’s current approach. Sustrans stated that, “We believe that policy in Northern Ireland is moving the right way. Fit Futures is offering a vision of joined-up policy on physical activity... However, until recently, there has been little done to actually implement Fit Futures and despite good initiatives by the Health Promotion Agency and the Physical Activity Coordinators the most recent NI Physical Activity Strategy was back in 1998-2002. It is therefore welcome and of the utmost importance, that the DHSSPS is producing an Obesity Strategy for Northern Ireland".[71]
45. However, Belfast City Council argued “that despite the increased focus afforded by government, obesity is becoming more prevalent and the current strategy and target to ‘by March 2010, halt the rise in obesity’ does not yet appear to be delivering significant outcomes."[72] Iain Foster, Diabetes UK said, “Andrew Dougal [NI Chest Heart and Stroke Association] and I sit on the Department’s obesity prevention steering group, and although it is still early days for it, neither of us is overly excited or optimistic about it making one dot of a difference to most people’s lives."[73]
46. Ballymena Borough Council expressed concern that “there appears to be no cohesive strategy available at present for guidance for those with an interest in this issue… This strategy [Fit Futures] remains in draft format although many of the key priorities contained within it are being addressed by various organisations through their own agendas ... This lack of strategic direction has led to a very ‘piecemeal’ approach to the issue of obesity".[74] Banbridge District Council called for a Northern Ireland strategy to tackle adult obesity to be “drafted and implemented as soon as possible."[75]
47. Pauline Mulholland, British Dietetic Association, expressed concern that allied health professionals are not directly involved in the obesity prevention steering group arguing that they have an important role to play on the group. She also pointed out that, “the British Dietetic Association was not invited to sit on the food and nutrition subgroup, even though such matters are our core business" but she acknowledged that this has been rectified and there is now a dietician on the subgroup.[76]
48. In developing its strategy the Department of Health in England has as its ambition “to be the first major nation to reverse the rising tide of obesity and overweight in the population by ensuring that everybody is able to maintain a healthy weight".[77] DHSSPS has also adopted an optimistic approach telling the Committee that, “there are opportunities for Northern Ireland to take a leading role in this worldwide problem by developing and implementing a cross-cutting, comprehensive, long-term strategy that brings together multiple stakeholders. The Department through its development of an Obesity Prevention Strategic Framework is determined to take on this challenge."[78]
49. Obesity is the most serious and most challenging public health issue that we face at this time and it is also one of the most complex. There is therefore an urgent need to develop and implement a comprehensive and robust strategy to address the issue.
50. We share the deep concern of those who expressed regret that the Fit Futures Implementation Plan has not been formally signed off and implemented. The failure to do so has, we believe, created uncertainty and a potential hiatus until a full strategy is in place.
51. We welcome and support the plans by the Department to develop a life course strategy however we fully recognise that tackling obesity effectively is not solely a matter for the health service. We note that the Fit Futures Report contained a joint target with the Departments of Education and Culture, Arts and Leisure. We strongly recommend that the new life course strategy be developed jointly in partnership with other departments, particularly the Department of Education, as has happened in England.[79][100]
66. Dr Wilde, Institute of Public Health in Ireland, took a similar view saying “there are hundreds of small interventions in schools, communities, workplaces, and so forth. That must be set in a regional strategy so that there is some coherence between what happens across Northern Ireland and what happens locally."[101] Pauline Mulholland, British Dietetic Association, concurred saying, “The point is to combine the best examples of what has worked across the region and to roll them out in the mainstream. At the same time, we must consider what has been tried and tested and what fits with a particular local community, because all communities are different."[102]
67. The British Medical Association felt that it was a role for the Public Health Agency to “research what works and what does not work … many people have been working hard in health action zones, and so forth, in communities. … the best practices have not been spread throughout the Province."[103] The British Dietetic Association shared the view that, “the new Regional Agency for Public Health and Social Well-being provides the opportunity to evaluate such schemes across Northern Ireland and to decide which of them to commission to create the best outcomes for the public."[104]
68. This issue was also recognised by the Public Health Agency, as Dr Carolyn Harper told the Committee, “We cannot tackle obesity through single, small-scale interventions. Given the limitations of available funding, that approach has had to be taken. However, we want to take a dual approach. First, we want to draw in additional funding, and, secondly, we want to connect the existing services and programmes not only in the health and social care service but in transport and education to get the most of that resource. We want to take a fresh look at how we connect people to all available services."[105]
69. We found that there are numerous initiatives throughout Northern Ireland aimed at addressing or preventing obesity, which have been developed and implemented by a very wide range of bodies and agencies. However, lots of these initiatives have been developed in isolation and many have not been evaluated to assess their effectiveness. In addition there is no central data collection or inventory of projects and this undoubtedly leads to duplication of effort.
70. We recommend that the Department commission an urgent audit of existing obesity-related initiatives so that the need for evaluation or further research can be identified and examples of good practice can be rolled out more widely. We recommend that the Public Health Agency, perhaps in conjunction with the planned All-island Obesity Observatory, develops and maintains a central data base of projects and develops standardised evaluation tool kits.
Weight Management
71. A major element of our terms of reference is to look at the availability of weight management and other intervention services to treat people suffering from obesity related ill health. We have already seen that around 24% of the adult population are clinically obese and many of them have significant health problems directly related to their obesity. The Department stated that, “Obesity management is integral to the management of other conditions such as coronary heart disease, stroke, atrial fibrillation and diabetes."[106] Dr Michael Ryan, a consultant chemical pathologist who described himself as a ‘clinician in the front line’, told us that, “90% of the patients [he sees] for diabetes; about 80% who attend cardiac clinics; 70% who attend our gastrointestinal clinics, and about 60% who attend respiratory clinics have significant co-morbidity that is linked to weight and obesity."[107] The Obesity Management Association reminded the Committee that, “Overweight people will become obese, by which time the challenge to provide effective treatment has multiplied… Early medical intervention is essential rather than a last option".[108]
72. Dr Ryan went on to say that, “the difficulty is that there is no service for those patients. A large proportion of the population needs professional help."[109] He argued passionately in written and oral evidence to the Committee that, “the lack of a comprehensive, strategically planned service for the overweight and obese adult is a major shortcoming of the current healthcare system." He suggested that, “The current ‘system’ consists of a wide range of ‘interventions’ championed by enthusiastic and well meaning individuals but the lack of overall co-ordination renders many of the programs difficult to evaluate."[110]
Primary Care
73. The Department in its submission pointed to two elements of the 2004 General Medical Services Contract that provide incentives for GP practices to help improve the quality of care provided to patients with conditions related to obesity.[111] Under the Quality and Outcomes Framework (QOF) GPs receive additional funding based on achievement against a number of indicators. The Department advised that since April 2006 the establishment of a register of patients who have a Body Mass Index (BMI) of 30 or more has been included as a QOF indicator. The Department explained that the purpose of this was to encourage GPs to “provide interventions, that would, based upon the best available evidence and recommendations by the National Institute for Health and Clinical Excellence (NICE), reduce the prevalence and severity of conditions linked to obesity".[112] In addition the Department stated that it had provided an additional £800k from 2006 by way of a Directed Enhanced Service (DES) to enable GPs to develop a written protocol for patients with a BMI of 30 or more. Directed Enhanced Services are a series of more specialised services that GPs may choose to provide.
74. The Department reported that all GP practices in Northern Ireland have fully participated in these schemes. However, Abbott, a private global healthcare company, pointed out that points under the QOF scheme are only available for maintaining a register of patients with a BMI of 30 or over and not for providing advice to patients on weight management. Abbott argued that, “allocating QOF points to obesity management, as has happened with smoking cessation, would be an effective way of incentivising better weight management in primary care and improving patient outcomes".[113]
75. Dr Theo Nugent, British Medical Association NI, suggested that GPs are well placed to identify patients with weight management problems and to manage some of the associated health related illnesses but that they “are not terribly well placed to give people good advice on how to control their obesity". He explained that, “there is little problem when someone turns up with a fallout from his or her obesity, such as diabetes. There are services available to help them to deal with that. However, a colossal workload is required when an individual is referred with what the dietetic service term ‘simple obesity’… There is a limit to where we can send people before they develop problems, and it is difficult for GPs to see how they can motivate individuals or encourage self-motivation in families."[114]
76. The British Medical Association and a number of district councils referred to the Healthwise Scheme which is run by councils in conjunction with HSC Trusts and allows participating GPs, nutritionists, physiotherapists and specialist nurses to prescribe exercise to patients they think will benefit from supervised physical activity. However, it is not available in all areas. Katrina Morgan, NILGA, explained that Healthwise, which runs in a number of council areas, “is funded by the Eastern Health and Social Services Board and offers a free 12-week programme. Patients are referred to a leisure centre to participate in the programme, and that referral can be based on anything from weight or obesity problems to general health problems. The participants are evaluated at the end of the 12-week programme."[115] Teresa Ross, Chartered Society of Physiotherapy, gave further details saying, “the fitness instructor and the physiotherapist in a leisure centre work in partnership to assess the patient and set up an individual programme for them. The fitness instructor then takes control of the exercise programme."
77. Ms Ross suggested that this was “a positive way to progress and would allow the health system to target people who are at risk of ill health, as opposed to those who are actually ill. Therefore, it is important to develop the idea of prescribing exercise, and it should be rolled out."[116] Gerry Bleakney, Public Health Agency, confirmed that, “there is a scheme in the eastern area and part-schemes in the southern and northern areas." However, she suggested that “the evidence base to support it is questionable ... Clients from general practice, primary care and secondary care give good reports about the scheme in the east, and we think that it is working. We will continue to assess the scheme because it is an expensive intervention. It is also a potentially very cost-effective intervention given the health outcomes that it creates."[117] The Western Health and Social Care Trust advised that there are three successful GP exercise referral schemes running in the western area.[118]
78. Professor Eamonn McCartan, Sport NI, argued strongly that, “GP referrals can address some of the barriers that prevent people who are not particularly active, who are overweight and who have an issue with their body image from exercising… People need a pathway, encouragement, direction and mentoring. That can be done, particularly for those social groups that cannot see the benefits of physical activity and exercise."[119]
79. The Committee noted that an evidence-based Care Pathway for the management of overweight and obesity in primary care was published by the NHS in England in 2006. For adults, the priority of intervention in primary care is reducing risk factors for the patient “rather than to return them to an ‘ideal’ or healthy weight range".[120] This acknowledges the fact that small weight losses do produce health benefits, while more significant changes result after a loss of 5-10 per cent of body weight. The aim is also to prevent further weight gain in patients with lower degrees of overweight.
80. A good practice example of a Primary Care Specialist Obesity Service, established to treat people with morbid obesity within a primary care setting, is that established by Birmingham East and North PCT. The aim of the service is to provide more intensive specialist support, than would generally be possible in a primary care setting, from a multi-professional team.[121]
81. Dr Ryan suggested that we adopt the approach of the Counterweight programme used in Scotland. He explained that it “is primary-care based and provides specifically trained staff to deal with obesity. It is rigorously evaluated by the University of York and the University of Aberdeen. Counterweight has produced credible evidence of the cost-effectiveness of that type of programme."[122] Professor Iain Broom, Robert Gordon University in Aberdeen and Chairman of Counterweight, and a colleague Hazel Ross, took part in the Committee Research Event and elaborated on the Counterweight programme and confirmed that it “is the first large scale primary care weight management programme in the UK to show clinically effective weight reduction using a structured approach to care".[123]
82. We are concerned about the lack of clear direction for dealing with obesity in primary care settings in Northern Ireland. We are also concerned that initiatives such as the Healthwise Scheme, whereby supervised physical activity can be prescribed, are not available in all areas. We recommend that the Department, in conjunction with the Health and Social Care Board, develops a range of evidence-based referral options for use by primary care practitioners.
83. We urge the Minister to exert influence at a national level to introduce the allocation of Quality and Outcomes Framework (QOF) points for positive obesity management rather than simply for maintaining a register of obese patients.
Secondary Care
84. The Department told us that, “Patients with significant weight management/obesity issues which may be directly or indirectly linked to their condition are seen and treated in almost every service within secondary care… Historically it has been the presenting condition that is treated and managed, although obesity issues may be one of a number of contributing factors in the development of the disease/condition."[124]
85. Dr Ryan argued that this was still the case saying that, “Current clinical services, designed to address specific clinical conditions, such as diabetes, cannot adequately address the special needs of the obese patient. Clinical services are becoming effectively ‘silted up’ with patients whose primary cause for attendance is ‘overshadowed’ by the co-morbidity of excess weight. Addressing the obesity can be more beneficial, in terms of health gain for the patient, than dealing with the ‘primary’ cause of attendance."[125] The Department did acknowledge that, “specialist supporting dietetic services need to be further developed to meet current and anticipated future demands. There will need to be additional staff, primarily dieticians and nurses, and training/specialist knowledge enhanced in secondary care."[126]
86. Pauline Mulholland, British Dietetic Association, stressed the key role undertaken by dieticians in the management of clinical obesity and said that, “People aspire to lose a significant amount of weight over a short period, and sometimes that puts them off accessing our services. We need to manage such expectations and promote the message that if individuals can be encouraged to lose 10% of their weight and to maintain that weight loss, they can achieve significant health benefits. The evidence shows that a 10% weight loss will reduce blood pressure and cholesterol, improve the control of blood sugar for people with diabetes, and reduce the death rates for a number of conditions."[127]
87. Dr Ryan argued for the use of a managed clinical network model of services delivery saying that, “it is now well established and has been shown to be an effective means of delivering targeted services for specific reasons. The approach to weight management at all levels of intervention should be supported by the managed clinical network. Much of the cost of such a programme is already embedded in the system".[128]
88. The need for effective interventions for children was also highlighted to the Committee. Currently one in four children in Northern Ireland is either overweight or obese and Dr Wilde, Institute of Public Health in Ireland, pointed out that, “The evidence shows that most children who are overweight or obese carry that through the rest of their lives."[129] Dr Mark Rollins, consultant paediatrician, argued that, “there are 400,000 children in Northern Ireland, 100,000 of whom are currently overweigh and obese. Some 60% to 70% of children are going to be obese as adults. That is a fact… In Northern Ireland, we have no intervention programmes at all. We are starting from a complete base."[130]
89. At the Committee Research Event Professor Paul Gately, Professor of Exercise and Obesity at Leeds Metropolitan University, spoke about an academic unit called Carnegie Weight Management that he leads. He highlighted a major concern that while “there are 4.5 million children in the UK who are overweight or obese… 70% of parents identify their overweight child as having normal weight".[131] Carnegie Weight Management provides family based multi-disciplinary intervention programmes at a range of levels from after-school activities to a residential camp for severely obese children. The Committee noted ongoing discussion between Carnegie and clinicians in the Northern Health and Social Care Trust and welcomed plans by Helping Hand Ltd to develop five pilot intervention programmes based on Carnegie for post primary children throughout Northern Ireland.[132]
90. The former Southern Health and Social Services Board stated that, “People who are obese are initially provided with advice through primary care services. They can access specialist drug treatments and dietetics advice through this route. NI has high rates of prescriptions of drug treatments for obesity. There is little evidence that attendance at specialist secondary care obesity clinics is more effective in achieving weight loss than interventions in primary care. However, such clinics may have a role in assessing patients who may be eligible for surgical intervention. As NI does not have a surgical treatment programme, there is no specialist obesity clinic in NI at present."[133]
91. The former Western Health and Social Services Board took a different approach arguing that, “while many patients can be managed in a community obesity clinic setting, there is a need for investment in specialist services in secondary care. We acknowledge that physicians in diabetes and endocrinology are appropriate specialists to manage such a service. However, they are already overwhelmed by the demand, as the diabetes epidemic has put additional pressure on the services that they are facing."[134]
Bariatric Services
92. The needs of very severely obese patients often require special services. Tracey Gibbs, College of Occupational Therapists, explained that, “On a day-to-day basis, that has major implications for transporting patients in hospital beds, the use of hoists and porters’ chairs, and for the use of seating in hospitals and in the patient’s home." However, she cautioned that “Although there is a lot of emphasis on the global epidemic of obesity, it is also important to consider the needs of the obese person. It must be ensured that they are treated with respect and dignity and that stigma and discrimination are avoided. A person who is overweight may feel socially isolated or excluded."[135]
93. In the course of the Inquiry the Committee learned, for example, that the NI Fire and Rescue Service had been called out on 40 occasions over the past five years to deal with bariatric incidents at a total cost to the Fire and Rescue Service of £85,000. These were mainly calls to assist ambulance personnel or other health services staff to deal with severely obese patients.[136]
94. Bariatric surgery has increasingly been used as a method of treating severely obese patients when other approaches fail and research suggests that this type of surgery has increased “more than five-fold within 5 years in most developed countries".[137] Bariatric procedures can be divided into those that reduce food intake (gastric restrictions) and those that reduce food uptake from the digestive tract (malabsorption).
95. Guidance from the National Institute for Health and Clinical Excellence (NICE) in 2008 recommended that bariatric surgery to aid weight loss should be available to patients meeting certain body mass index (BMI) criteria. The former Southern Health and Social Services Board told us that, “It is estimated that there are more than 50,000 people in NI who could be eligible for bariatric surgery using NICE criteria. This number is expected to rise at a further 5% each year. Although NICE estimate that only 2-4% of these people would come forward for surgery, this is by no means certain. The cost of treating only 2% of the eligible NI population (i.e. 1,000 patients) and providing the necessary long-term follow-up could be in the order of £10 - £15 million."[138] The Board also explained that “a multidisciplinary team assessment is necessary to ensure patient suitability for surgery and the long-term lifestyle changes it requires. In addition, surgeons need to be able to offer a full range of techniques, including laparoscopic surgery, and undertake a minimum volume of procedures to achieve and maintain skills. Appropriate follow up services, including the input of dieticians and specialist physicians, need to be in place. At present not all of these skills are available within NI… In light of the potential numbers of patients in NI who would meet NICE criteria, the current funding position, and the financial consequences of providing treatment for all those who might present, it has been agreed by Boards that, within the current CSR period, bariatric surgery cannot be commissioned routinely for patients meeting the NICE-recommended BMI criteria."[139]
96. The former Western Health and Social Service Board agreed saying that, “There is a lack of funding around bariatric services for patients in Northern Ireland who have persistent obesity when lifestyle and other drugs fail. Bariatric surgery has been shown to reverse diabetes and reduce mortality and there is an issue about equity to services which are available in other parts of the UK."[140]
97. David Galloway, DHSSPS, told us that, while bariatric surgery is not currently commissioned by the health boards in Northern Ireland, “last year, £1·5 million was made available to ensure that some 120 people had access to bariatric surgery from providers in Great Britain. The boards are currently discussing how they might progress that issue in 2009-2010 to ensure that that service is provided to the people who are most likely to benefit from it."[141] The Department subsequently advised that approximately 80 patients had bariatric surgery outside Northern Ireland in 2008/09 and that “for 2009/10 the legacy Health Boards agreed to fund short term bariatric services pilot with a budget of £1.5m and a target of providing treatment in England during the year for between 100 and 150 patients. The Department has no plans at this time to provide this surgery in Northern Ireland."[142]
98. Elsewhere in this report we deal with the need for a strategic approach to the prevention of obesity. However, we are gravely concerned about the extent of existing obesity-related ill health and the distinct absence of appropriate services at all levels. We are shocked to learn of the number of severely obese patients that attend diabetic and other clinics and particularly by the realisation that more than 50,000 people in Northern Ireland may be eligible for bariatric surgery.
99. We highlight the fact that even a modest reduction in weight can have a significant impact on a patient’s health and that addressing obesity may be more beneficial than dealing with the resulting illness.
100. We call on the Minister, as a matter of urgency, to undertake a thorough review of weight management services at all levels for both adults and children. The review must address the need for dedicated obesity clinics and the critical and urgent need for a separate bariatric service for Northern Ireland, including the provision of bariatric surgery and the lifelong medical follow-up for individuals required following such surgery. The review should also consider the merits of adopting examples of good practice from elsewhere, such as the Counterweight programme in Scotland and the Carnegie Weight Management programme in England.
Diet And Exercise
101. While the rapid increase in obesity over recent decades has not simply been down to an imbalance between diet and exercise it is clear that these two issues need to be addressed from a range of perspectives. As Newry and Mourne District Council pointed out “poor dietary habits and decreasing physical activity have become ingrained in the population and it will take a long-term approach involving many organisations to make any substantial changes in this culture".[143] In this chapter we look at what is being done to address these issues and to encourage the adoption of healthier lifestyles.
Healthy Eating
102. A major contributory factor behind the rising levels of overweight and obesity in Northern Ireland is that people are consuming food and drink products that contain high levels of saturated fat, sugar and salt. Dr Jane Wilde, Institute of Public Health in Ireland, said it was important to examine what the food sector might reasonably be expected to do about addressing obesity and suggested “if we let the situation continue as it is, without some greater checks on what is happening to the food sector, we will do a grave disservice to people in Northern Ireland. There is a requirement on the food sector to act responsibly within a certain timescale. It is important to go beyond a voluntary approach by the food sector… we are talking about issues such as food labelling, pricing, availability, subsidies, local production, and so forth. That is a crucial issue."[144]
103. The Food Standards Agency Northern Ireland is the body charged with responsibility to ensure that all food is safe to eat and has as its vision ‘healthy eating for all’. The Agency is closely involved in the Obesity Prevention Steering Group and leads the Food and Nutrition subgroup. The Agency was keen to point out that “healthy eating is all about balance". Its three key work strands are, “Firstly, influencing food products to ensure that healthier options are made available to people so that they can make their own choices; secondly, influencing people so that they are aware that the healthy choice is the easier choice; and thirdly, influencing the environment, particularly the food environment, so that some of the barriers to making healthy choices are removed."[145]
104. One of the Agency’s dietary heath targets is to reduce the population’s intake of salt and saturated fat. Andrea Marnoch, Food Standards Agency Northern Ireland, explained that, “We know that on average, people eat far more saturated fat than is recommended, and rising levels of obesity suggest that energy intakes exceed energy requirements. Following the success of the FSA’s work on salt reduction, the agency developed a programme of initiatives to try to reduce the level of saturated fat from its current level of 13·3% of energy intake to the recommended level of 11%."[146] Michael Bell, Northern Ireland Food and Drink Association, agreed that there is a need for balance and claimed that “Correcting the ingredients of the members of the association’s products is like squeezing a balloon. If the balloon is constricted so that, in the retail channel, one can buy only products that are low in sugar, fat, salt and, therefore, somewhat bland, people will eat more carry-outs or make alternative meals at home, adding more salt."[147]
105. The Food Standards Agency Northern Ireland advised that it “has identified the key food groups that contribute to levels of saturated fat and added sugar intakes, and it is working with the food industry on reductions in those food groups. The focus for that work is dairy products, meat and meat products, biscuits, cakes and pastry, snacks, confectionery, soft drinks and retail sectors."[148] Maria Jennings, Food Standards Agency Northern Ireland, explained that, “the issue is to drive down the overall amount of saturated fat that people are eating and to increase the levels of polyunsatured fats that they consume."[149]
106. The Committee recognises that much of the work with food manufacturers and major food retailers takes place at a UK level but the importance of action at a local level cannot be ignored. Clara Swinson, Department of Health in England, explained that, “We are looking to increase the information that is available to consumers through, for instance, nutritional labelling on products in supermarkets and stores, and labelling in non-retail settings such as fast-food restaurants."[150]
107. At an individual level, Dr Michelle McKinley, Queens University Belfast, suggested that, “More work must be done to find out what exactly are the best dietary approaches to offer to people who are trying to lose weight and to find dietary approaches that will not have any detrimental effects on the health of that person in the longer term. More research must be done, but the low-fat, high-fibre approach is still the standard weight-loss diet that is recommended and supported by health professionals."[151]
108. We welcome and encourage the ongoing work of the Food Standards Agency Northern Ireland to reduce the levels of saturated fat, salt and sugar in food. This has made significant progress to date but we believe that much more needs to be done. We urge the Department and the Food Standards Agency to continue to work with manufacturers and to exert pressure at a national and European level to introduce regulatory controls on the levels of salt and saturated fat in manufactured foods.
Food Labelling
109. Many respondents referred to the need for improved food labelling. Victoria Taylor, British Heart Foundation, argued that there needed to be “a single system of front-of-pack food labelling that is clear and that people will understand."[152] Andrew Dougal, NI Chest Heart and Stroke Association, supported this call saying, “Government should act now to empower people to make sensible choices. They will not be able to do so unless there is effective, simplified and comprehensible nutritional labelling on the front of the pack — it should not be written in tiny figures on the side panel, making it difficult for some people to read."[153]
110. Maria Jennings, Food Standards Agency Northern Ireland, explained that, “The agency has been working for a long time to provide a simple signpost on the front of food packaging that will let consumers know exactly what is in a pack… After extensive consumer research, the agency produced a simple scheme that is based on traffic lights — red, amber and green — for the four main nutrients, that is, fat, saturated fat, salt and sugar. A number of retailers and manufacturers, including several in Northern Ireland, have adopted the agency’s scheme. During the same period, a number of similar schemes appeared. Consumer and health groups started to ask for one simple and easily understood scheme that could be applied to all foods."[154] The Agency advised that an alternative front of pack labelling approach based on Guideline Daily Amount information, known as GDA Scheme but without use of traffic light colours, has been adopted by some retailers and manufacturers.[155]
111. Commenting on the Guideline Daily Amount scheme Andrew Dougal, NI Chest Heart and Stroke Association said that, “I am not innumerate, but I find it difficult to understand them. I find the traffic light system to be very positive, as is using the terms “low", “medium" and “high" to describe the various contents of food. Sixteen major companies have deviated from the traffic-light system recommended by the Food Standards Agency before it had the opportunity to launch that campaign. That has caused huge public confusion… We would like to see all companies sticking to one simple system that people understand."[156] Michael Bell, NI Food and Drink Association said that, “Our members are increasingly engaged in providing nutritional labelling on packaging. Virtually all our members’ products at the retail channel display either the Food Standards Agency (FSA) traffic-light system or the guideline daily amount (GDA) system. To date, that is less developed at the food service channel."[157]
112. Ms Jennings also referred to an independent survey of food labelling commissioned by the Department and the Agency which published its report in May 2009. She said that, “Not surprisingly to us, the study found that a single, consistent front-of-pack labelling scheme would be most helpful to consumers. Overall, the evidence shows that the strongest label is that which combines the words “high", “medium" and “low" with the traffic light colours red, amber and green, and with the percentage guideline daily amounts (GDA), with levels of nutrients expressed as a portion of the product."[158] Ms Jennings advised that the findings of the survey will be considered and there would be consultation on the next steps.
113. Dr McKinley, Queens University Belfast, explained that measures like food labelling “have been designed to help the consumer to make healthier choices, and research now focuses on whether those strategies are helping the consumer effectively or whether other approaches should be considered."[159] The Food Standards Agency Northern Ireland pointed out that, “evidence from adopters indicates high levels of consumer approval for this approach, shifts in sales towards healthier products and that the traffic light approach provides a powerful incentive to companies to reformulate their products to reduce levels of the nutrients highlighted on FoP [Front of Pack]".[160]
114. We believe that clear and simple food labelling is essential to enable consumers to make healthy choices. We fully support the calls for a single, consistent Food Labelling scheme using the traffic light system and urge the Minister and the Food Standard Agency Northern Ireland to consider whether such a system could be made mandatory on all food retail products. We also call for more action to enforce a similar clear and simple nutrition labelling system at non-retail outlets, such as restaurants and catering establishments.
Food Portion Sizes
115. The Department in its submission acknowledged that increased food portion sizes is one of a number of factors put forward in hypotheses to explain the general increasing intake of energy. This hypothesis is supported by research undertaken by the Centre for Food and Health at the University of Ulster and presented to the Committee at the Research Event. The research found that ‘increased food portion sizes resulted in significant and sustained increases in food intake in both men and women’ and that ‘the ready availability and consumption of large food portions (particularly of energy dense foods) may be a major factor in contributing to the obesity epidemic’.[161]
116. It is also an issue recognised by others including the Public Health Agency. Dr Carolyn Harper told the Committee that, “families are a priority. Parents influence what their children eat, and children influence their parents. Our approach is to give practical skills and knowledge of what a normal diet is and to address the shift towards fast food and larger portion sizes, which, subtly and latently, have become normal behaviours and patterns. It is about reframing and helping people to understand what a healthy, normal diet is."[162]
117. The Food Standards Agency Northern Ireland told us that it “is working with the food industry to identify opportunities to reduce the size of single serve portions, for example of soft drinks and sweet and savoury snacks. It is also considering how best to provide consumer advice on appropriate portion size. An academic workshop has concluded that the evidence base on portion size and weight gain justifies these actions. Re-alignment of in-store promotions which could encourage increased consumption of energy dense, salty foods to promotion of healthier foods also has a part to play."[163]
118. Larger food portion sizes are undoubtedly contributing to increasing obesity prevalence and this issue must be addressed seriously. While recognising the difficulty in regulating food portion sizes in catering and similar settings, we urge the Department and the Food Standards Agency Northern Ireland to examine how issues like food promotion and pricing impact on portion sizes and how they might be influenced.
Mixed Messages
119. Some respondents to the Inquiry referred to the campaign which promotes eating five portions of fruit and vegetables a day to stay healthy. The Committee recognised that while this campaign has been ongoing for a number of years there is still confusion over what it means in practice and how people can fulfil their five a day target. Mrs Marnoch, Food Standards Agency Northern Ireland, explained that, “according to the World Health Organisation, one should eat at least five portions of fruit or vegetables a day. Therefore it is recommended that you eat more than five."[164] Dr Eddie Rooney, Public Health Agency, acknowledged the confusion and said that, “The five-a-day message has been around for quite some time, but we need to do some more work on public awareness."[165]
120. We believe there is confusion over what exactly constitutes ‘five portions of fruit and vegetables a day’ and particularly around the size and content of a portion. We urge the Public Health Agency to examine how greater clarity and understanding about this health message, and how it might impact on levels of obesity, can be achieved.
Exercise
121. A number of respondents referred to fundamental changes in our lifestyles over recent decades and suggested that through undertaking less manual work, the introduction of machines, changes in methods of transport, and by our children undertaking less active play and spending long hours on computer games, that we have moved from being an active society to a sedentary society. The Northern Ireland Commissioner for Children and Young People claimed that children “cannot find safe, affordable, accessible and age appropriate play and leisure activities. This is having a profound impact on the ability of children and young people to stay active and healthy."[166] John News, Sport NI, pointed out that, “It is a startling figure that 70% of us are not physically active enough… more than 2,000 people in Northern Ireland will die this year as a result of physical inactivity."[167]
122. The World Health Organisation defines physical activity as ‘all movements in everyday life, including work, recreation, exercise and sporting activities’.[168] Sport NI pointed to the value of sport and physical activity as a means of ensuring that people have a better physical and emotional quality of life. Sustrans highlighted the focus on promoting walking and cycling as a beneficial physical activity in the NICE Guidance[169] but expressed concerns about the regular policy references to sport. Sustrans argued that, “it is most important that policy makers recognise sport as only a minority slice in the pie of physical activity, and not the most likely to appeal to currently inactive and/or overweight individuals."[170] Sport NI was keen to point out that, “there is a traditional framework for sport as it is seen on television, but sport is a much more expansive and expanded sector than simply competitive sport … there are various forms of physical activity".[171]
123. Sustrans pointed out that, “historic approaches to the promotion of physical activity have often sought to promote ‘exercise’, ‘fitness’ and ‘sport’ … these are not likely to be appealing to most inactive or overweight individuals. As the Chief Medical Officer for England has put it, ‘for most people, the easiest and most acceptable forms of physical activity are those that can be incorporated into everyday life. Examples include walking or cycling instead of travelling by car’."[172]
124. The Department of Culture, Arts and Leisure advised that, “Over the past 2-3 years DCAL, in partnership with SNI [Sport NI], has been developing a new 10 year Strategy for Sport and Physical Recreation in Northern Ireland. The aim is to provide a high level template for the development of sport and physical recreation in Northern Ireland which reflects the aspirations and priorities of all sports stakeholders. The new Strategy is also expected to inform the direction of future investment."[173] DCAL also provided details of a three month consultation in 2007/08 and pointed out that “the draft estimated at the time that the funding the shortfall facing stakeholders to fully deliver all targets at c.£20m per annum over 10 years". DCAL went on to explain “Following completion of the consultation exercise in January 2008, a final version of the Strategy for Sport and Physical Recreation was submitted to the Northern Ireland Executive in December 2008 for consideration at a future meeting."[174]
125. The Northern Ireland Commissioner for Children and Young People acknowledged that the strategy “is comprehensive and if implemented in full would provide increased opportunities for children and young people to participate in quality sport and physical recreation across a range of settings but mainly through schools and community based activities." However, the Commissioner expressed serious concern that, “the draft strategy was subject to consultation in late 2007 and to date it has not been finalised nor has it been implemented. DCAL must allocate appropriate funding to the all actions to ensure the full strategy can be implemented in full."[175]
126. Sport NI praised the strategy saying that it “will have a significant effect in increasing participation in sport and in increasing the physical activity of our young people, although not only of our young people. Properly resourced and implemented, it will go some way to addressing obesity levels." However, Sport NI would not be drawn on the reasons for the delay in finalising the strategy saying, “Responsibility for publishing the strategy lies with others, not with us."[176]
127. Other Departments sought to assure the Committee of their commitment to promote exercise. The Department for Employment and Learning pointed out that it “is an active member of the NI Physical Activity Implementation Group. This Group is taking forward the recommendations in the NI Physical Activity Strategy which aims to increase levels of health related physical activity particularly among those who exercise least."[177] The Department for Regional Development pointed out that it “has developed strategies over recent years and put operational initiatives in place to encourage a change in travel behaviour, away from the use of the private car towards more sustainable and healthier means of travel, such as walking and cycling".[178] [See also paragraph 132 below]
128. We welcome the development of the draft 10 year Strategy for Sport and Physical Recreation in Northern Ireland by the Department for Culture, Arts and Leisure. However, we have major concerns about the ongoing delay in finalising and implementing this strategy. We believe the strategy has the potential to contribute significantly to increasing levels of physical activity and counteract growing obesity prevalence. We therefore call on the Executive to ensure that the Strategy for Sport and Physical Recreation in Northern Ireland is properly resourced and implemented without further delay and that this work dovetails with the development of the life course obesity strategy.
Role of other Departments,
Bodies and Sectors
129. There was a clear recognition among respondents that tackling obesity is beyond the capacity of the health service alone. The Northern Ireland Commissioner for Children and Young people summed it up saying “While the Department for HSSPS must take a lead in implementing measures to tackle childhood obesity, other departments have an important role in implementing other strategies and policies that have an impact on the ability of children and young people to lead healthy and active lifestyles."[179] All Government departments were invited to make a submission to the Inquiry. Most departments responded highlighting the work they are undertaking in the battle against obesity particularly through actions related to the Fit Futures Strategy for children. Three Departments, the Office of the First and Deputy First Minister, the Department of the Environment, and the Department of Enterprise, Trade and Investment, indicated that they had no comments on the Inquiry.
130. The Department for Employment and Learning (DEL) assured the Committee that it “is committed fully to the aims and objectives of Fit Futures, the Investing for Health Strategy, and the NI Physical Activity Strategy, all of which focus on the importance of tackling obesity". DEL also highlighted its role in working with further and higher education bodies and in sector skills development.[180] The Department for Culture, Arts and Leisure explained the work it has been doing over the past 2-3 years, in partnership with Sport NI and other stakeholders, to develop a new 10 year Strategy for Sport and Physical Recreation in Northern Ireland (see paragraphs 124-126 above).[181] The Minister for Finance and Personnel stated that he was “supportive of the strategy of prevention not only because it can reduce treatment costs but also because of the wider economic and societal benefits." He added, “Nevertheless, I would stress that any funding required to implement future recommendations from the Inquiry will need to be secured from the existing departmental budgets."[182]
131. The Minister for Agriculture and Rural Development pointed to a strategy in preparation by the Forest Service to develop the recreational and social use of its forests and suggested that, “the draft strategy … recognises a number of opportunities relating to health and well-being that are relevant to the obesity inquiry". The Minister also suggested that “promoting the consumption of natural farm products, including milk, could form part of a wider drive to encourage healthier diets".[183]
132. The Department for Regional Development explained that it “has developed strategies over recent years and put operational initiatives in place to encourage a change in travel behaviour, away from the use of the private car towards more sustainable and healthier means of travel, such as walking and cycling." DRD pointed out that the Regional Development Strategy in 2001 “recognised the importance of the need to change the local travel culture and at the same time contribute to more active and healthier lifestyles. In particular, the Strategy recognised the need to revive the healthy habits of walking and cycling, for short journeys, by people of all ages". DRD also highlighted the potential positive impact of the Regional Transportation Strategy, the Cycling Strategy, the Walking Strategy, and the Travelwise Safer Routes to Schools Initiative.[184]
133. The Department for Social Development pointed to “an overall programme focus on healthy lifestyles, healthy eating and weight management" supported under the Department’s Neighbourhood Renewal Strategy. DSD also advised about the introduction of a specific new medical code for obesity in October 2008 which has enabled the department to record that “from that date there are 52 Disability Living Allowance (DLA) claims and 64 Incapacity Benefit (IB) claims where obesity is recorded as their main disabling condition".[185]
134. Northern Ireland Environment Link (NIEL) pointed to the links between poverty, poor diet and obesity and argued that, “the department with responsibility for targeting social need and the anti-poverty strategy therefore needs to be fully involved in the development and implementation of plans and programmes designed to tackle obesity issues."[186] We note and welcome the recent Inquiry into Child Poverty by the Committee for the Office of the First and deputy First Minister.[187]
135. We urge each and every Department to recognise that they have a crucial role to play in responding to the obesity epidemic either through direct action or through policies and practices that impact on the obesogenic enviroment.
136. The Department of Education (DE) in its submission recognised the vital role that education has in equipping children and young people for life and that, “the education system in general has always been to the forefront in encouraging healthy lifestyles and providing children and young people with the foundations on which to build for active and healthy lives in the future".[188] In evidence to the Committee officials from the Department of Education explained the development of a rolling programme to implement new nutritional standards in schools between 2005 and 2007 and referred to the provision of “an additional £3 million to support the increase in quality of schools meals". Officials also explained that the Educational and Training Inspectorate now looks at how schools are performing in this area and said that “the results have largely been very positive in the first tranche of schools to have been inspected".
137. DE also recognised that, “competing sources of food in schools were reducing the impact of the new nutritional standards" referring to “other food that is provided in schools through vending machines, tuck shops, break-time snacks and drinks, breakfast clubs and food brought into schools in packed lunches and snacks". As a result the Department has developed a ‘whole school approach to nutrition’ and officials advised that consultation on that policy is due to start in September 2009. [189] Alan McMullan, DE, told the Committee that, “the food in schools policy will bring forward proposals for legislation that will affect other food in schools and give us the power to totally ban things".[190]
138. The Committee noted the CATCH program (Coordinated Approach to Child Health), which operates in over 7,000 schools in the USA and has been evaluated in over 80 peer reviewed publications. It brings together schools, families and communities to teach children how to be healthy for their lifetime. Healthy behaviours are reinforced through a coordinated approach in the classroom, in the cafeteria, in physical education and at home.[191]
139. In relation to physical activity in schools Louise Warde Hunter, DE, pointed out that, “PE is a separate area of learning in the curriculum, which is compulsory across all key stages. At least two hours of PE per week is recommended, but how schools take that recommendation onboard may vary". When asked about how this target is monitored and whether there is any way to enforce the minimum of two hours of PE each week, Ms Hunter acknowledged that data on this is not gathered by the Department and said “Our position is that these are guidelines, and an inspection could ask how those guidelines are being followed and whether it is appearing in the school development plan." Jill Fitzgerald, DE, explained that “The scenario here is different to that in England where two hours of PE a week has been made compulsory. We are in a scenario where no subject is compulsory for any given time. Therefore, although a subject is compulsory in the curriculum — as PE is — the Department is not in a position to say how much time it should be allotted. To do it for PE would make it different from all other subjects and constrain schools in their teaching of the curriculum."[192]
140. Apart from the Health Department, we believe that the Department of Education has probably the most pivotal role to play in tackling obesity. This view is reflected in our recommendation (see paragraph 51) that the development and implementation of the Life Course Approach should be undertaken jointly by these two Departments.
141. We welcome and support the work that is taking place to develop and implement high nutritional standards in all schools and we encourage the Department of Education to explore whether any lessons can be learned from the CATCH (Coordinated Approach to Child Health) programme in the United States.
142. We are greatly concerned that the two hours PE per week in schools is not compulsory, as is the case in England. We are also concerned that data indicating whether schools are adhering to this recommendation is currently not being collected. We call on the Department of Education to make at least 2 hours of PE in schools compulsory and subject to regular monitoring by the Educational and Training Inspectorate.
Role of Local Authorities
143. Karen Smyth, NILGA, told the Committee that, “Local government is particularly well placed to tackle regional issues such as obesity at local level and to initiate projects that make a real difference to local communities".[193] Many District Councils highlighted specific initiatives they currently undertake to tackle obesity in their areas. NILGA, at the request of the Committee, undertook a survey of all district councils and 14 responded. Details are at Appendix 3, Page 482.
144. In addition a number of respondents pointed to the potential for district councils to increase and enhance their efforts to tackle issues like obesity under the new structures arising from the current Review of Public Administration. Specifically, a number saw the introduction of community planning in 2011 as providing “opportunities for Councils to come together with other organisations to undertake the sort of work, which can make a difference on this issue"[194]. Belfast City Council referred to opportunities arising from the reorganisation of health and social care structures arguing that they will mean “a greater role for local government through participation in the new Regional Agency for Public Health and Social Wellbeing and in local commissioning".[195] Sport NI agreed that, “a central tenet of the review [of public administration] is community planning" and suggested that, “Sport Northern Ireland can take the lead role in the development of a physical activity strategy in partnership with the district councils and their agents. In that way, we can establish the major objectives, key performance indicators and a level of accountability as has been experienced in Scotland."[196]
145. Ballymena Borough Council argued that, “Interventions based on improved nutrition and increased physical activity can be effective for some individuals, but tackling the obesity problem for the total population will require interventions that target the environment as well, for example food policy and marketing and the transport infrastructure… the ideal forum for addressing such wide-ranging topics would be through the process of community planning and the associated power of well-being, roles to be assigned to the new Councils through the current RPA."[197]
146. Teresa Ross, Chartered Society of Physiotherapy, was positive about the opportunities saying, “the new agencies provide a positive forum for us to build upon. Their involvement in local communities will be a good influence, and the involvement of local council representatives will help to build a better future."[198] Rob Phipps, DHSSPS, also supported the importance of community planning saying that it “will give a role to the agencies and the local councils. Local councils will be important, and leisure centres, in particular, will have a crucial role to play."[199]
147. We fully recognise and endorse the crucial role local councils currently play in tackling obesity. We welcome the commitment by councils to expand and enhance their role further when the new community planning proposals come into effect. We urge the full involvement of councils in developing the new life course strategy.
Role of the Media
148. There is a general recognition that “the power of advertising is massive, particularly on young people"[200] and that “the media has a role to play in encouraging improvements in children’s diet and exercise".[201] The British Heart Foundation argued that, “children need to be protected from aggressive marketing of foods high in fat, saturated fat, salt and sugar" and it called “for a ban on such advertisements on television before 9 pm."[202] The British Medical Association also called for “the banning of advertising and marketing to children of unhealthy foods."[203] Diabetes UK called for “Increased pressure/partnership with the food industry in relation to food production, labelling and advertising".[204]
149. Ofcom, the media watchdog, explained that research had found that, “advertising (amongst other factors) had a modest, direct effect on children’s food choices and a larger but unquantifiable indirect effect on children’s food preferences, consumption and behaviour." Ofcom also explained that it had introduced a range of measures between February 2007 and January 2009 which restricted the scheduling of television advertising of food and drink products that are high in fat, salt or sugar in or around programmes aimed at children on the main commercial channels and on children’s channels. In a subsequent review in December 2008 Ofcom found that as a result “overall children saw 29% less HFSS (food high in fat or salt or sugar) advertising between 18.00 and 21.00." and it “estimated that the advertising restrictions, once fully implemented, would reduce child HFSS impacts (the number of times an HFSS advert is seen by a child aged 4-15) by some 41% of the 2005 level".[205]
150. The British Heart Foundation expressed concern that despite the Ofcom restrictions “millions of children are still exposed to such adverts during pre-watershed family programmes such as the X Factor or Coronation Street" and it called on the Assembly to “adopt a position of favouring a mandatory ban on pre watershed advertising of HFSS foods to children on television, and strict regulation of non-broadcast marketing methods".[206]
151. There were concerns expressed by some respondents that a negative message in advertising simply turns people off. Michael Bell, Northern Ireland Food and Drink Association, argued that, “some of the approaches that have been taken involve trying to win over the public by negative rather than positive messaging. The FSA used images of sick bags and slugs to try to change consumer behaviour at various points in the food industry. That imagery turns people off instead of encouraging them to carry the message forward."[207] The Obesity Management Association also argued that, “advertising by the Government puts the accent on obesity and becoming ill, however advertising that if you become slim, you become fit and happy tends to work better – especially with children."[208]
152. The power of advertising and the media as both a positive and a negative influence in relation to obesity cannot be over emphasised. It is clear that the advertising of food and drink products that are high in fat, salt or sugar have a significant impact particularly on young people. We urge the Minister to work with colleagues throughout the UK to explore the feasibility of banning the advertising of food and drink products that are high in fat, salt or sugar before the 9 pm watershed.
153. We support the approach of promoting healthy eating and exercise through positive advertising rather than negative messages. We call on the Minister to develop a comprehensive media approach as part of the life course strategy and to consider, for example, how new and emerging media such as text and Twitter could be used to engage with young people.
Obesogenic Environment
154. Several respondents, including the former Northern Health and Social Services Board and the Northern Ireland Cycling Forum, were keen to remind the Committee that the causes of the obesity epidemic are complex and that leading authorities, such as the World Health Organisation and the authors of the Foresight Report, had highlighted “the need to tackle the obesogenic environment in which a range of factors in our physical, socio-economic and cultural environment act to promote calorie intake and discourage physical activity."[209] The Department also pointed out that, “Increasingly it has been acknowledged that the causes of obesity are associated with a wide range of inter-related factors, from the physical, socio-economic and cultural environment, which act to promote calorie intake and discourage physical activity. These factors are referred to collectively as the ‘obesogenic’ environment."[210]
155. In relation to physical activity, Sustrans argued that, “the key factor, but one which is unfortunately sometimes overlooked in discussion of policy and interventions on active living, is that the environment is the central determinant in people’s individual choices. Over recent decades we have allowed the environment within which we live to become dissuasive of physical activity … In order to raise physical activity levels, we need to make the environment more conducive to active living, and this includes transforming the streets to be more walking and cycling friendly."[211] Sustrans also referred to a paper it had co-authored in 2003 which had proposed that, “modification of social, economic, and environmental factors may yield greater health dividends than individual lifestyle approaches. Indeed such interventions may be necessary before individual lifestyle approaches can be effective."[212]
156. Food environments include availability and accessibility to food and food advertising and marketing. It is recognised that the food environment and the built environment are closely related and the Foresight Report concluded that further work is required “to examine how aspects of the built environment or building design influences people’s food habits e.g. the proximity of shops to schools or the location of vending machines".[213]
157. DHSSPS acknowledged that, “There are many and varied contributors to the obesity problem and these are societal as well as individual responsibilities. This idea suggests that understanding and tackling the obesogenic environment is necessary to complement school and family-based interventions."[214]
158. Sport NI suggested a number of practical measures relating to planning, play facilities and public transport and argued that, “in the long term, those decisions will create a situation whereby society, by default, encourages a culture of physical activity. Physical activity should not be considered a bolt-on; we must plan for such a society now, because it will be cheaper in the long run."[215] The British Heart Foundation urged the Assembly to “oversee urban planning policies which promote physical activity" and called on the Assembly to “dedicate at least as much energy on encouraging participation in physical activity as for competitive sports."[216]
159. Tackling the obesogenic environment was also an issue raised at the Research Event and it concluded that, “it is only when the Government take obesity seriously, and when there are proper policies that relate to obesity at Government, economic, financial and pricing level, that we are going to see really good change."[217]
160. The Committee learned that organisations, academics and communities in the North East of England, recognising that obesity cannot be successfully addressed with isolated interventions, have come together to form an obesogenic environment network (North East Obesogenic Environment Network). It regards tackling the obesogenic environment as looking at the environment, planning, design, transport, physical activity, food, policy and culture. The aim of the network is to have an impact on obesity “through integrated cross-sectoral initiatives and projects".[218]
161. The obesogenic environment can have a major impact on both our eating habits and the amount of physical exercise that we undertake. However, we believe that the link between ‘passive obesity’ and the environment is not yet widely understood. Initiatives tend to be isolated and piecemeal. The full impact of the obesogenic environment needs to be addressed in a comprehensive and empirical manner.
162. We call on the Executive to fully recognise the potential impact of the obesogenic environment on the health and wellbeing of the population and to consider the merits of introducing a system whereby the impact of all major policy decisions are subject to an obesity proofing exercise.
Others Issues
Health Inequalities
163. Many respondents highlighted the links between poverty and obesity. Action Cancer pointed to research which found that, “people on lower income have higher propensity for fast food diets and food with little nutritional value. Additionally, people with little disposable income are less motivated to engage in regular exercise due to the high costs associated with gyms or sports clubs."[219] Dr Colin Hamilton, British Medical Association, suggested that, “looking back 50 or 60 years, one discovers that obesity was not a working-class problem, but, rather, one of the middle and other classes — the people who had money to spend on food. Nowadays, the situation has totally reversed."[220] John News, Sport NI, agreed saying that, “the settings are important; not everyone wants to go to a council-owned leisure centre, but neither can everyone afford to go to a private health club or leisure centre. The health inequalities across Northern Ireland show a definite correlation between socio-economic status and participation in sport and physical activity."[221]
164. The Public Health Alliance pointed to research it had undertaken in 2007 to examine the scope and extent of food poverty in Northern Ireland. That research concluded that, “there is strong evidence to indicate that people living in food poverty almost always have a diet which predisposes them to the risk of obesity".[222] Andrew Dougal, NI Chest Heart and Stroke Association, pointed out that success in preventing heart disease and stroke had been achieved in the higher socio-economic groups and while he agreed with the total-population approach he argued that, “there may be a need to focus on the more deprived groups in society to ensure that those people are empowered to change their lifestyles".[223]
165. Andrea Marnoch, Food Standards Agency Northern Ireland, reported on the findings of the low income diet and nutrition survey (LIDNS), carried out between 2003 and 2005, and published in 2007. Its aim was to study material deprivation in the diets of the bottom 15% of the population. It concluded that, “compared with the general population, the low-income population was less likely to consume wholemeal bread and tended to consume more non-diet soft drinks, more processed meats, more whole milk and more table sugar. Consumption of fruit and vegetables fell well below the recommended level of five portions a day, and consumption of oily fish was very low."[224]
166. While the rates of obesity have increased most among adults and children from poorer backgrounds, research has also found that the widening of obesity inequalities is more evident among women than men.[225] The Fit Futures Report also suggested that, “Higher rates of obesity have been found in adults, especially women, with mild to moderate learning disabilities that live in the community than in the general population"[226] while, as noted earlier, the Royal College of Psychiatrists reported that, “people with mental illness and those with learning disabilities are more likely than the general population to be obese". [227]
Community Approach
167. Many respondents, including Health and Social Care Trusts and former Health and Social Services Boards, highlighted the need to take a community-based approach to tackling obesity. A number pointed to a project developed in France entitled Ensemble, Prévenons l’Obésité des Enfants (EPODE), which means ‘together, we can prevent obesity in children’ as an example worth emulating. Dr Eddie Rooney, Public Health Agency, explained that, “EPODE is a holistic project that is taken forward by the mayor of the local town or city. It develops community spirit and engagement around social action for change. EPODE is about physical activity and healthy eating rather than obesity, although its outcomes influence obesity."[228] The former Northern Health and Social Services Board argued that the most promising approach is through “community based interventions focussing on diet and physical activity in children and have been used as the basis for a programme involving over 130 towns in France, Belgium and Spain. The early data available is encouraging but full report won’t be available for several years (EPODE)."[229]
168. Clara Swinson, Department of Health, London, explained that England had set up a specific community project based on the EPODE idea. She said, “The healthy community challenge fund, which we abbreviate to Healthy Towns, is a fund of £30 million over three years. We looked at some successes achieved in towns in France through the EPODE project and developed the idea for England. Evidence shows that, although no society as a whole has tackled obesity, there has been some success on a community level when people really got together and worked across agencies."[230]
169. In evidence to the Committee, the new Public Health Agency was keen to stress that it will be addressing issues like obesity from a community perspective. Dr Rooney said that, “We have to break down the message and understand it from the perspective of people living in the community, as opposed to the message descending from on high… It must be done in communities and working with them…There is a need for animation in communities and a real desire to do something. However, people struggle with how it can be achieved, and extra support is needed to make it happen. We must fill that challenging gap."[231]
170. Professor Frank Kee, Queen’s University Belfast, referred to a new social marketing campaign document, issued recently by the Department of Health in London, which focuses on how people make decisions and introduces the idea of rewarding healthy choices. He explained that, “An innovative research scheme, Points4Life, has been launched in Manchester. It is based on loyalty cards for supermarkets, and people will be rewarded with more points if they buy healthy options or if they take more exercise…Before the scheme was launched, consumer market research was carried out in Manchester to find out what the voters wanted, so Points4Life is exactly what the community wants." Professor Kee also advised that he has included the concept in a research proposal that, “will study the impact of the Connswater Community Greenway in east Belfast … on physical activity behaviours in the local area. We will build the idea of a loyalty card into that project, whereby people who use the Greenway can be rewarded with redeemable points in local retail outlets." [232]
171. In developing the Life Course Approach we urge the Department to take account of health inequalities and particularly the need to address the higher levels of obesity in areas of social deprivation.
172. We applaud and support the recognition by the Public Health Agency that it needs to address issues like obesity from a community perspective.
Workplace Health
173. The British Heart Foundation and others pointed out that, “The workplace offers significant potential as a setting to promote healthy lifestyles to the adult working population. This is well recognised in the UK but to date under-utilised."[233] Dr Colin Hamilton pointed to variations in workplace schemes saying that, “the BMA has a good programme of yearly checks for its staff, including blood pressure, weight, and so forth… the NHS is a poor employer in that respect… There are some good employers in the Province and others that are not so good. During a credit crunch, the temptation is probably to run down, rather than improve, such services."[234]
174. Other examples of workplace health schemes included Newry and Mourne Council which advised that it has developed a number of programmes such as encouraging the use of the Council’s leisure facilities by staff and Councillors through reduced rates and free access. The Council said that, “a weight management support group has also been set up for staff to encourage each other to reach and maintain a healthy weight."[235] The Assembly, in a written submission, highlighted the positive action it is taking as an employer to promote healthy eating in the workplace and to encourage greater levels of exercise.[236]
175. The British Heart Foundation also highlighted the Well@Work workplace health initiative which it jointly funded across nine regional projects and 32 workplaces in England. Evaluation of this two year initiative found that, “several projects achieved modest increases in employees’ healthy behaviours. However…one-off projects did not sustain behaviour change in the absence of strong management involvement and supportive environments within the workplace." The Foundation called for the Northern Ireland Assembly to “Review and update the Workplace Health Strategy to ensure that workplaces are helping to support health and wellbeing."[237]
176. We recognise the benefits for both employers and employees of promoting healthy lifestyles in the workplace and we urge all employers to consider initiatives that promote healthy eating and greater levels of exercise in the workplace.
Research
177. A number of organisations highlighted the need for greater co-ordination of research. The former Western Health and Social Services Board called for “a better evidence-base of what interventions actually do work which reflect the setting and target audience for which they are being designed".[238] Belfast City Council agreed highlighting “a real need for rigorous and robust research in the field of prevention during an individual’s life course and in particular preventing childhood obesity and promoting early years intervention…There are few local studies on prevention; much of the research which has been carried out is inadequate to allow for specific recommendations to be made."[239] Action Cancer told the Committee that, “We have found that the outcomes of academic research are not always passed to community organisations quickly enough. Funding may be going into academic streams to inform research, but there can be a delay in getting the findings to community groups and those who are offering provision. Therefore, the impact can either be delayed or missed."[240]
178. At the outset of the Inquiry Dr Jane Wilde, Institute of Public Health in Ireland, drew attention to this need “to bring research, policy and practice together to try to work out what we know and also to identify any gaps". She said that, “there is every danger in Northern Ireland that there will be more and more interventions, and we will not know what is working or not working."[241] At Dr Wilde’s suggestion the Committee convened a round-table meeting of leading academic researchers on obesity from throughout the United Kingdom and the Republic of Ireland, a small number of key stakeholders from within Northern Ireland and members of the Committee. (Details of the Research Round-Table Event are at annex 5) The aim of the Research Event was to make practical recommendations to include in this report.
179. A number of important issues were identified at the Research Event. The conclusions included:
- The importance of a strong partnership between the research community, stakeholders, communities, politicians and policy makers;
- The need to develop a database of existing interventions and ensure that they are based on firm evidence of effectiveness;
- The need to identify examples of good practice and roll them out across Northern Ireland;
- The need to learn from experience elsewhere and adopt not just short-term interventions but longer-term research based systems interventions;
- The need for cross-government working to ensure that obesity is seen as a top priority for Northern Ireland and the Executive and not just a matter for the health service;
- The need to address the dearth of existing weight management interventions urgently;
- The need to challenge sectors in the obesogenic environment that may not be obesity friendly; and
- The need for government to take obesity seriously and address pricing at different levels.
180. A number of respondents pointed to the development of an all-island Obesity Observatory similar to one funded by the Department of Health in England. The Department indicated that this was one of a number of outcomes of cross-border co-operation.[242] In evidence to the Committee Dr Wilde suggested that the obesity observatory “will be a one-stop shop for evidence and data, particularly local data."[243] Professor Frank Kee, QUB, agreed saying that the observatory “will help us to communicate more effectively to various bodies, including health bodies and local councils, our knowledge of what works and what does not work". He went on to argue that it “must be multi-sectoral and multidisciplinary. It is important for the new [Public Health] agency, and for academics, to build capacity that will help us to model the consequences of different policies."[244] The former Western Health and Social Services Board claimed that “there is a need for further development of the All-Ireland Obesity Observatory, in terms of ensuring that we can get a better understanding of what initiatives are being taken forward and have greater collaboration between those identifying core issues and those delivering appropriate services."[245]
Data Collection
181. The primary method employed by the DHSSPS to collect and analyse overweight and obesity prevalence rates among children in Northern Ireland is the Child Health System. Currently, as part of this, the School Nursing Service undertakes the measurement and recording of the weight and height of Primary One children on an annual basis.
182. In addition to the data generated by the Child Health System, the other key source of data informing the development of Fit Futures and the wider Investing for Health Strategy is the Health and Social Wellbeing Survey which was last carried out in 2005-2006. The Health and Social Wellbeing Survey which was previously conducted in 1997 and 2001 focuses on a range of different health issues including mental health, cardiovascular disease, physical activity, smoking and drinking and obesity. The Survey takes the form of self-reporting questionnaires. Therefore a certain degree of caution needs to be employed when considering the overweight and obesity figures, given the potential for underestimation of weight and overestimation of height.
183. During the Committee’s Research Round-Table Event, Professor Frank Kee and Professor Barbara Livingstone highlighted the need to improve the data collection systems currently supporting the Department’s obesity prevention strategy. Professor Kee stated that, ‘We need surveys that are fit for purpose, and for the last two iterations of the health and well-being survey we have not had measures of BMI. We must ensure that we have physical measurements in future health and well-being surveys in Northern Ireland.’[246] Professor Livingstone argued that, ‘one of the major gaps in this part of the world is that that we do not have really good surveillance on monitoring data, and you cannot really evaluate anything until you have that in place.’[247] We note that, for example, in New Zealand the Healthy Eating, Healthy Action strategy launched in 2008 is supported by an integrated research, evaluation and monitoring framework which measures the effectiveness of on-going initiatives while building a strong evidence base.[248]
184. It is widely accepted that the availability of reliable and accurate data is critically important in the continued development and implementation of a regional or national obesity strategy. The data provides not only an indication of the effectiveness of existing strategies in place but also feeds critical information into the on-going evaluation process to ensure specific initiatives are tailored to different population groups. The need for effective surveillance data becomes even more important within the current context of the development of a life course strategy in Northern Ireland.
185. We stress the importance of a strong partnership between researchers, stakeholders, communities, politicians and policy makers. We welcome the fact that one of the four policy advisory sub-groups, set up as part of the Obesity Prevention Steering Group, will deal with research and data and that it is led by an academic researcher.
186. We strongly support the development of the All-island Obesity Observatory which will have an important role in providing effective obesity surveillance and intelligence to practitioners, policy-makers and the wider community.
187. We share the concerns expressed about the current limitations in the collection and measurement of obesity among children and adults in Northern Ireland. We urge the Department to examine how data collection can be improved through reform and better funding of the Child Health System. This should facilitate extending BMI measurements beyond Primary One children. Enhanced funding should also facilitate better collection of adult data based on actual BMI measurements rather than self-reporting.
Conclusion
188. The levels of obesity in Northern Ireland, as elsewhere, have increased dramatically in recent years and it is without doubt the most serious and complex public health challenge facing society today. Despite this the enormity of the situation is not widely recognised. Obesity threatens to overturn the considerable health gains of recent times and, if not checked, will have grave implications for the economy and for society and could totally overwhelm the health service. As one witness told us, “Smoking and drinking may be damaging to public health, but they are nothing compared with what obesity will do to our population over the next 10 or 20 years."
189. There is an urgent need to develop and implement a broad and vigorous strategy to begin to turn the tide of obesity across the different population groups in Northern Ireland. We note that the Department has moved away from a strategic response focusing on tackling obesity in children and young people to the development of a life course approach to obesity prevention. We welcome and support the life course approach but it must have clear, effective leadership that fully engages all departments and sectors with a focus on continuous evaluation and improvement.
190. In tackling obesity the potential impact of a wide range of factors in the physical, socio-economic and cultural environment, known as the obesogenic environment, on both our eating habits and our levels of exercise needs to be better understood and addressed.
191. As well as taking action to reduce and prevent obesity, an effective range of services to manage and treat the rapidly increasing number of people who currently suffer from serious and life threatening obesity-related illnesses must be put in place. Obesity is already ‘silting up’ a range of clinical and other services and it is not sufficient to treat the medical symptoms without addressing the underlying weight problems. Even a modest reduction in weigh of 10% can have a dramatic impact on a patient’s health.
192. Throughout this report we have referred to valuable examples of good practice in other jurisdictions that we could learn from. Perhaps the most important of these is the recent development of the Healthy Weight, Health Lives strategy in England, the first national population-wide strategy aimed at tackling obesity. In relation to weight management services we have highlighted established and effective initiatives in England and Scotland that may be of benefit in Northern Ireland.
[1] Volume 2, Appendix 3, Page 288
[2] Appendix 2, Paragraph 1245
[3] Appendix 2, Paragraph 316
[4] Volume 2, Appendix 3, Page 578
[5] Volume 2, Appendix 3, Pages 288-289
[6] Volume 2, Appendix 3, Page 431
[7] Volume 2, Appendix 3, Page 365
[8] Appendix 2, Paragraph 1043
[9] Yusuf S et al on behalf of the INTERHEART Study Investigators (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study), The Lancet; 364: 937-952
[10] Appendix 2, Paragraph 1058
[11] Appendix 2, Paragraph 119
[12] Obesity and Type 2 Diabetes in Northern Ireland, Report by the Comptroller and Auditor General, NIA 73/08-09 14 January 2009
[13] Appendix 2, Paragraph 463
[14] Official Report Volume 41 No 6, Monday 8 June 2009, p 243
[15] Appendix 2, Paragraph 120
[16] Appendix 2, Paragraph 240
[17] Volume 2, Appendix 3, Page 431
[18] Volume 2, Appendix 3, Page 237
[19] Volume 2, Appendix 3, Page 353
[20]Appendix 2, Paragraph 524
[21]Appendix 2, Paragraph 316
[22]Appendix 2, Paragraph 442
[23] Volume 2, Appendix 3, Page 275
[24] Crest ‘Guidelines for the Management of Obesity in Secondary Care’ June 2005; OB32
[25] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 5
[26] Volume 2, Appendix 3, Page 315
[27] Volume 2, Appendix 3, Pages 356-357
[28] Obesity and Type 2 Diabetes in Northern Ireland, Report by the Comptroller and Auditor General, NIA 73/08-09 14 January 2009
[29] Sustrans OB37; Investing for Health, DHSSPS March 2002
[30] Volume 2, Appendix 3, Page 432
[31] Appendix 2, Paragraph 758
[32] Price et al (2006) ‘Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index is associated with a greater risk of death’, Am J Clin Nutr, 84 (2): 449-460 cited in P. Musingarimi (2008) Obesity in the UK: A Review and Comparative Analysis of Policies within the Devolved Regions, International Longevity Centre: 8.
[33] Volume 2, Appendix 3, Page 247
[34]Appendix 2, Paragraph 247
[35]Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3, page 48
[36] Volume 2, Appendix 3, Page 332
[37] Volume 2, Appendix 3, Page 381
[38] Appendix 2, Paragraph 241
[39] Volume 2, Appendix 3, Page 234
[40] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.2, page 47
[41] Volume 2, Appendix 4
[42] E M Perez-Pastor et al. Assortative weight gain in mother–daughter and father–son pairs: an emerging source of childhood obesity. International Journal of Obesity 33: 727-735
[43] Appendix 2, Paragraph 10
[44] Volume 2, Appendix 3, Page 364
[45] World Health Organisation (2007) The challenge of obesity in the WHO European Region and the strategies for response, WHO: 1.
[46] World Health Organisation (2006) ‘Obesity and Overweight’, Fact sheet No.311.
[47] World Health Organisation (2007) The challenge of obesity in the WHO European Region and the strategies for response, WHO: 1
[48] National Obesity Observatory (2009) ‘NOO News – Newsletter from the National Obesity Observatory’, Issue 2, May, NOO: 6.
[49] Reference to ‘Ireland’ within Figure 1 reflects the percentage of obesity among the adult population in the Republic of Ireland and illustrates figures from the Survey of Lifestyle, Attitudes and Nutrition (SLAN) commissioned for the Department of Health and Children.
[50] Sassi, F. et al (2009) The Obesity Epidemic: Analysis of Past and Projected Future Trends in Selected OECD Countries, Organisation for Economic Cooperation and Development: 42.
[51] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 24.
[52] See Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 24-41.
[53] Department of Health and Children (2007) Survey of Lifestyle, Attitudes and Nutrition in Ireland – Main Report, Department of Health and Children: 100-101.
[54] DHSSPS (2008) ‘Obesity time bomb is ticking louder than ever – north and south’, Press release.
[55] Data in this table provided by Public Health Information and Research Branch, DHSSPS.
[56] International Journal of Obesity (2005) Ten year trends for fatness in Northern Irish adolescents: the Young Hearts Projects, repeat cross-sectional study, 29: 579-585 – cited in NIAO (2007) The Performance of the Health Service in Northern Ireland, NIAO: 14.
[57] Southern Health and Social Services Board and Southern Investing for Health Partnership (2009) Submission to the Inquiry: 2.
[58] DHSSPS (2009) Evidence to DHSSPS Health Committee inquiry on Obesity, DHSSPS: 4.
[59] Musingarimi, P. (2008) Obesity in the UK: A Review and Comparative Analysis of Policies within the Devolved Regions, International Longevity Centre: 11.
[60] Volume 2, Appendix 3, Pages 291-296
[61] Volume 2, Appendix 3, Page 257
[62] Volume 2, Appendix 3, Page 291
[63] Volume 2, Appendix 3, Page 292
[64] Investing for Health, DHSSPS March 2002, Chapter 13
[65] Volume 2, Appendix 3, Page 293
[66] See paragraph 16 above
[67] Volume 2, Appendix 3, Page 294
[68] Appendix 2, Paragraph 1408
[69] Butland, B. et al (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science.
[70]Appendix 2, Paragraphs 1374- 1375
[71] Volume 2, Appendix 3, Page 373
[72] Volume 2, Appendix 3, Page 316
[73] Appendix 2, Paragraph 1106
[74] Volume 2, Appendix 3, Pages 381-382
[75] Volume 2, Appendix 3, Page 267
[76] Appendix 2, Paragraph 542
[77] Healthy Weight, Healthy Lives: One Year On, Department of Health, April 2009, Executive Summary
[78] Volume 2, Appendix 3, Page 299
[79] The Cross-Government Obesity Unit in England is led jointly by the Department of Health and the Department for Children, Schools and Families.
[80] Appendix 2, Paragraph 14
[81] Appendix 2, Paragraphs 1069-1070
[82] Volume 2, Appendix 5, Paragraph 327
[83] Volume 2, Appendix 5, Paragraph 358
[84] Volume 2, Appendix 5, Paragraphs 374-375
[85] Appendix 2, Paragraph 862
[86] Volume 2, Appendix 3, Page 270
[87]Appendix 2, Paragraph 1383
[88] Volume 2, Appendix 3, Page 580
[89] Volume 2, Appendix 3, Page 236
[90]Appendix 2, Paragraph 1051
[91]Appendix 2, Paragraph 9
[92]Appendix 2, Paragraph 883
[93] Appendix 2, Paragraph 12
[94] Volume 2, Appendix 3, Page 280
[95] Volume 2, Appendix 3, Page 261
[96] Volume 2, Appendix 3, Page 381
[97] Appendix 2, Paragraph 251
[98] Appendix 2, Paragraph 686
[99] Volume 2, Appendix 3, Page 367
[100]Appendix 2, Paragraph 785
[101]Appendix 2, Paragraph 13
[102] Appendix 2, Paragraph 532
[103]Appendix 2, Paragraph 330
[104] Appendix 2, Paragraph 499
[105] Appendix 2, Paragraph 898
[106] Volume 2, Appendix 3, Page 295
[107]Appendix 2, Paragraph 424
[108] Volume 2, Appendix 3, Page 247
[109]Appendix 2, Paragraph 424
[110] Volume 2, Appendix 3, Page 278
[111] Volume 2, Appendix 3, Pages 295-296
[112] Volume 2, Appendix 3, Page 296
[113] Volume 2, Appendix 3, Page 325
[114]Appendix 2, Paragraphs 335-337
[115]Appendix 2, Paragraph 681
[116]Appendix 2, Paragraph 551
[117]Appendix 2, Paragraphs 918-919
[118] Volume 2, Appendix 3, Page 477
[119]Appendix 2, Paragraphs 778-779
[120] NHS, Care pathway for the management of overweight and obesity, May 2006, www.library.nhs.uk/SpecialistLibrarySearch/Download.aspx?resID=270413 page 6
[121] http://domuk.org/wp-content/uploads/2008/05/ben-pct-primary-care-specialist-obesity-service-march-08.ppt
[122] Appendix 2, Paragraph 490
[123] Volume 2, Appendix 5, Page 737
[124] Volume 2, Appendix 3, Page 297
[125] Volume 2, Appendix 3, Page 275
[126]Appendix 2, Paragraph 490
[127]Appendix 2, Paragraph 501
[128]Appendix 2, Paragraph 432
[129]Appendix 2, Paragraph 70
[130] Volume 2, Appendix 5, Paragraph 90
[131] Volume 2, Appendix 5, Paragraph 44
[132] Volume 2, Appendix 3, Paragraph 561
[133] Volume 2, Appendix 3, Paragraph 328
[134] Volume 2, Appendix 3, Paragraph 269
[135]Appendix 2, Paragraphs 506-507
[136] Volume 2, See Appendix 4
[137] Korenkov, M. and Sauerland S. (2007), Clinical Update: bariatric surgery, The Lancet, 370, 1988-1990
[138] Volume 2, Appendix 3, Paragraph 328
[139] Volume 2, Appendix 3, Paragraph 329
[140] Volume 2, Appendix 3, Paragraph 269
[141]Appendix 2, Paragraph 130
[142] Volume 2, Appendix 3, Page 309
[143] Volume 2, Appendix 3, Paragraph 345
[144]Appendix 2, Paragraph 21
[145]Appendix 2, Paragraph 940
[146]Appendix 2, Paragraphs 942-943
[147]Appendix 2, Paragraph 1273
[148]Appendix 2, Paragraph 946
[149]Appendix 2, Paragraph 979
[150]Appendix 2, Paragraph 1377
[151]Appendix 2, Paragraph 642
[152]Appendix 2, Paragraph 1053
[153]Appendix 2, Paragraph 1073
[154]Appendix 2, Paragraphs 948-951
[155] Volume 2, Appendix 3, Page 540
[156]Appendix 2, Paragraph 1041
[157] Appendix 2, Paragraph 1238
[158]Appendix 2, Paragraph 952
[159] Appendix 2, Paragraph 640
[160] Volume 2, Appendix 3, Page 540
[161] Volume 2, Appendix 5, Paragraph 110
[162] Appendix 2, Paragraph 896
[163] Volume 2, Appendix 3, Page 539
[164]Appendix 2, Paragraph 1004
[165]Appendix 2, Paragraph 921
[166] Volume 2, Appendix 3, Page 259
[167] Appendix 2, Paragraph 788
[168] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 25
[169] National Institute for Health and Clinical Excellence Guidance on physical activity and the environment, 2007
[170] Volume 2, Appendix 3, Page 373
[171]Appendix 2, Paragraph 753
[172] Volume 2, Appendix 3, Page 372
[173] Volume 2, Appendix 3, Page 334
[174] Volume 2, Appendix 3, Page 335
[175] Volume 2, Appendix 3, Page 260
[176] Appendix 2, Paragraph 792
[177] Volume 2, Appendix 3, Page 231
[178] Volume 2, Appendix 3, Page 361
[179] Volume 2, Appendix 3, Page 261
[180] Volume 2, Appendix 3, Pages 231-235
[181] Volume 2, Appendix 3, Page 334
[182] Volume 2, Appendix 3, Page 436
[183] Volume 2, Appendix 3, Page 394
[184] Volume 2, Appendix 3, Pages 361-362
[185] Volume 2, Appendix 3, Page 442
[186] Volume 2, Appendix 3, Page 348
[187] Volume 2, Appendix 3, Page 227
[188] Volume 2, Appendix 3, Page 453
[189]Appendix 2, Paragraph 1309
[190]Appendix 2, Paragraph 1343
[191] www.catchinfo.org/whatis.asp
[192]Appendix 2, Paragraph 1328
[193]Appendix 2, Paragraph 670
[194] Volume 2, Appendix 3, Page 345
[195] Volume 2, Appendix 3, Page 316
[196]Appendix 2, Paragraph 811
[197] Volume 2, Appendix 3, Page 383
[198]Appendix 2, Paragraph 530
[199]Appendix 2, Paragraph 1417
[200]Appendix 2, Paragraph 824
[201] Volume 2, Appendix 3, Page 434
[202] Volume 2, Appendix 3, Page 367
[203] Volume 2, Appendix 3, Page 434
[204] Volume 2, Appendix 3, Page 547
[205] Volume 2, Appendix 3, Page 221
[206] Volume 2, Appendix 3, Page 367
[207]Appendix 2, Paragraph 1279
[208] Volume 2, Appendix 3, Page 248
[209] Volume 2, Appendix 3, Page 403
[210] Volume 2, Appendix 3, Page 296
[211] Volume 2, Appendix 3, Page 372
[212] Lawlor et al, Journal of Epidemiology and Community Health 2003;57:96–101
[213] Butland B. et. al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.4.3, page 54
[214] Volume 2, Appendix 3, Page 290
[215]Appendix 2, Paragraphs 822-823
[216] Volume 2, Appendix 3, Page 366
[217] Volume 2, Appendix 5, Paragraph 362
[218] Research paper appendix 4 p 13 of 33. www.neoen.org.uk
[219] Volume 2, Appendix 3, Page 312
[220]Appendix 2, Paragraph 396
[221]Appendix 2, Paragraph 810
[222] Volume 2, Appendix 3, Page 364
[223]Appendix 2, Paragraph 1108
[224]Appendix 2, Paragraph 963
[225] Law, C. et. al. (2007), Obesity and health inequalities, Obesity Reviews, 8 (Suppl. 1), 19-22
[226] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 35
[227] Volume 2, Appendix 3, Page 238
[228]Appendix 2, Paragraph 920
[229]Appendix 3, Page 403
[230]Appendix 2, Paragraph 1391
[231]Appendix 2, Paragraph 932
[232]Appendix 2, Paragraph 609
[233] Volume 2, Appendix 3, Page 369
[234]Appendix 2, Paragraph 329
[235] Volume 2, Appendix 3, Page 345
[236] Volume 2, Appendix 3, Pages 552-560
[237] Volume 2, Appendix 3, Page 369
[238] Volume 2, Appendix 3, Page 270
[239] Volume 2, Appendix 3, Pages 318-319
[240]Appendix 2, Paragraph 253
[241]Appendix 2, Paragraph 23
[242] Volume 2, Appendix 3, Page 295
[243]Appendix 2, Paragraph 24
[244]Appendix 2, Paragraph 635
[245] Volume 2, Appendix 3, Pages 269-270
[246] Volume 2, Appendix 5, Paragraph 279
[247] Volume 2, Appendix 5, Paragraph 267
[248] See Ministry of Health (New Zealand) (2008) Healthy Eating – Healthy Action Oranga Kai- Oranga Pumau: Progress on Implementing the HEHA Strategy: Ministry of Health: 23.
Appendix 1
Minutes of Proceedings
Thursday, 15 January 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
The meeting commenced at 2.01 pm in public session with the Deputy Chairperson in the chair.
9. Consideration of the Terms of Reference for the Committee Inquiry
The Committee agreed the Draft Terms of Reference for the Inquiry on Obesity.
The Committee agreed a list of relevant organisations for a consultation on the Inquiry on Obesity with one addition.
The Committee agreed a Draft Press Release for the Inquiry on Obesity.
The Committee agreed to liaise with the Public Accounts Committee regarding the Northern Ireland Audit Office Report on Obesity and Type 2 Diabetes in Northern Ireland.
[Extract]
Thursday, 26 February 2009
Senate Chamber, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Ms Sue Ramsey MLA
The meeting commenced at 2.09 pm in public session.
6. Committee Inquiry into Obesity
Evidence session with the Institute for Public Health in Ireland
Members took evidence from:
Dr Jane Wilde Chief Executive, Institute for Public Health
A question and answer session ensued. The Chairperson thanked the witness for attending.
4.40 p.m. Mr Tommy Gallagher left the meeting.[Extract]
Thursday, 5 March 2009
Room 135, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
The meeting commenced at 2.01 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity
Evidence session with Departmental officials
Members took evidence from:
Andrew Elliott Director of Population Health
Naresh Chada Senior Medical Officer
Rob Phipps Health Development Branch
David Galloway Acting Director of Secondary Care
A question and answer session ensued. The Chairperson thanked the witnesses for attending.
2.08 p.m. Mrs Carmel Hanna joined the meeting.
2.12 p.m. Mr Thomas Buchanan joined the meeting.
2.30 p.m. Mr Tommy Gallagher left the meeting.
2.40 p.m. Mr Tommy Gallagher rejoined the meeting.
2.57 p.m. Ms Sue Ramsey left the meeting.
3.05 p.m. Mrs Carmel Hanna left the meeting.
Evidence session with Action Cancer
Members took evidence from:
Geraldine Kerr Acting Chief Executive, Action Cancer
Caroline Hughes Research & Evaluation Officer, Action Cancer
Treasa Rice Health Promotion Manager, Action Cancer
A question and answer session ensued. The Chairperson thanked the witnesses for attending.
3.06 p.m. Mrs Carmel Hanna rejoined the meeting.
3.14 p.m. Mr John McCallister joined the meeting.
3.20 p.m. Ms Sue Ramsey rejoined the meeting.
3.43 p.m. Mrs Carmel Hanna left the meeting.
3.53 p.m. Mrs Carmel Hanna rejoined the meeting.
[Extract]
Thursday, 12 March 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mrs Carmel Hanna MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mr Tommy Gallagher MLA
The meeting commenced at 2.03 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity
Evidence session with the British Medical Association (Northern Ireland)
Members took evidence from:
Theo Nugent BMA (NI) General Practitioners Committee
Colin Hamilton BMA (NI) Committee for Public Health Medicine and Community Health
Chairman
Nigel Gould BMA (NI) Deputy Secretary
Ivor Whitten BMA (NI) Assembly and Research Officer
A question and answer session ensued. The Chairperson thanked the witnesses for attending. The Committee agreed to write to the Health & Social Care Trusts to request a sample of hospital menus.
2.14 p.m. Mr John McCallister joined the meeting.
2.17 p.m. Mr Thomas Buchanan joined the meeting.
2.55 p.m. Ms Sue Ramsey left the meeting.
2.58 p.m. Mr John McCallister left the meeting.
2.58 p.m. Dr Kieran Deeny left the meeting.
3.02 p.m. Dr Kieran Deeny rejoined the meeting.
3.06 p.m. Ms Sue Ramsey rejoined the meeting.
[Extract]
Thursday, 26 March 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mrs Carmel Hanna MLA
Mrs Claire McGill MLA
The meeting commenced at 2.10 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity
Evidence session with Dr Ryan, Northern Health & Social Care Trust
Members took evidence from:
Michael Ryan Consultant Chemical Pathologist, Northern Health & Social Care Trust
A question and answer session ensued. The Chairperson thanked the witness for attending.
2.20 p.m. Dr Kieran Deeny joined the meeting.
2.48 p.m. Mr John McCallister joined the meeting.
[Extract]
Thursday, 2 April 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mrs Carmel Hanna MLA
Ms Sue Ramsey MLA
The meeting commenced at 2.04 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity
Evidence session with the Allied Health Professions
Members took evidence from:
Pauline Mulholland Board Member, British Dietetic Association (NI)
Tracey Gibbs Chairperson, College of Occupational Therapy
Teresa Ross Chartered Society of Physiotherapy
A question and answer session ensued. The witnesses agreed to provide the Committee with additional information. The Chairperson thanked the witnesses for attending.
2.54 p.m. Mr Tommy Gallagher left the meeting.
[Extract]
Thursday, 23 April 2009
Queens University Belfast
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Ms Sue Ramsey MLA
Dr Kieran Deeny MLA
The meeting commenced at 2.11 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity
Evidence session with Queens University Belfast
Members took evidence from:
Professor Frank Kee Deputy Director, Centre for Public Health, QUB
Dr Michelle McKinley Principal Investigator, Centre for Public Health, QUB
Ms Mairead Boohan Deputy Director, Centre for Medical Education, QUB
A question and answer session ensued. The Deputy Chairperson thanked the witnesses for attending.
2.20 p.m. Mr Thomas Buchanan joined the meeting.
The Committee noted a number of research topics for consideration at a round table event being organised for Tuesday 19 May 2009. Members were asked to provide any views to the Committee office.
Evidence session with NILGA
Members took evidence from:
Karen Smyth Head of Policy, NILGA
Katrina Morgan Leisure Operations Manager, Belfast City Council
A question and answer session ensued. The witnesses agreed to provide the Committee with additional information. The Deputy Chairperson thanked the witnesses for attending.
3.04 p.m. Mr Tommy Gallagher left the meeting.
3.21 p.m. Mr Tommy Gallagher rejoined the meeting.
[Extract]
Thursday, 30 April 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr John Render (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
The meeting commenced at 2.03pm in public session with the Deputy Chairperson in the chair.
3. Committee Inquiry into Obesity, Evidence session with Sport NI
Members took evidence from:
Eamonn McCartan Chief Executive, Sport NI
John News Participation Manager, Sport NI
A question and answer session ensued. The witnesses agreed to provide the Committee with additional information. The Deputy Chairperson thanked the witnesses for attending.
3.00 p.m. Ms Sue Ramsey left the meeting.
3.07 p.m. Ms Sue Ramsey rejoined the meeting.
[Extract]
Thursday, 14 May 2009
Room 135, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr John McCallister MLA
The meeting commenced at 2.02 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity
Evidence session with the Public Health Agency
Members took evidence from:
Dr Eddie Rooney Chief Executive, Public Health Agency
Dr Carolyn Harper Director of Public Health, Public Health Agency
Ms Gerry Bleakney Health Promotion Commissioner, Public Health Agency
Before the evidence on obesity Dr Rooney and Dr Harper updated the Committee on Swine Flu. Following the presentation on obesity a question and answer session ensued. The witnesses also advised on the implementation of a recommendation by the Committee on suicide & self harm. The Deputy Chairperson thanked the witnesses for attending.
2.26 p.m. Dr Kieran Deeny joined the meeting.
3.10 p.m. Mr Alex Easton left the meeting.
3.11 p.m. Dr Kieran Deeny left the meeting.
10. Any other business
The Deputy Chairperson reminded Members of a round table research event taking place on Tuesday 19 May as part of the Committee’s inquiry into obesity.
[Extract]
Thursday, 21 May 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr Sam Gardiner MLA
Ms Sue Ramsey MLA
The meeting commenced at 2.05 pm in public session with the Deputy Chairperson in the chair.
6. Committee Inquiry into Obesity
Evidence session with the Food Standards Agency
Members took evidence from:
Maria Jennings Deputy Director, Food Standards Agency
Andrea Marnoch, Head of Dietary Health Unit, Food Standards Agency
A question and answer session ensued. The witnesses invited the Committee to visit the office of the Food Standards Agency. The Deputy Chairperson thanked the witnesses for attending.
2.37 p.m. Mr Tommy Gallagher left the meeting
2.51 p.m. Mr Tommy Gallagher rejoined the meeting
2.54 p.m. Dr Kieran Deeny left the meeting
2.56 p.m. Mrs Carmel Hanna left the meeting
2.57 p.m. Dr Kieran Deeny rejoined the meeting
2.57 p.m. Mrs Carmel Hanna rejoined the meeting
Evidence session with the British Heart Foundation, Northern Ireland Chest Heart and Stroke Association and Diabetes UK.
Members took evidence from:
Andrew Dougal Northern Ireland Chest Heart and Stroke Association
Iain Foster Diabetes UK Northern Ireland
Victoria Taylor British Heart Foundation
A question and answer session ensued. The Deputy Chairperson thanked the witnesses for attending.
3.01 p.m. Mr John McCallister joined the meeting
3.28 p.m. Mr Tommy Gallagher left the meeting
3.58 p.m. Mr Tommy Gallagher rejoined the meeting
[Extract]
Thursday, 28 May 2009
Room 135, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
The meeting commenced at 2.03 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity.
Evidence session with Dr Una Lynch, Queens University Belfast.
Members took evidence from:
Dr Una Lynch Queens University Belfast
A question and answer session ensued. The Deputy Chairperson thanked the witness for attending.
[Extract]
Thursday, 11 June 2009
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr John McCallister MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
The meeting commenced at 2.03 pm in public session with the Deputy Chairperson in the chair.
5. Committee Inquiry into Obesity.
Evidence session with Northern Ireland Food & Drink Association.
Members took evidence from:
Michael Bell Executive Director, Northern Ireland Food & Drink Association
Mr John McCallister made a declaration of interest that he was a shareholder in a food processing company which may be a member of the Northern Ireland Food & Drink Association
A question and answer session ensued. The Deputy Chairperson thanked the witness for attending.
9 Committee Inquiry into Obesity.
Evidence session with officials from the Department of Education
Members took evidence from:
Louise Warde Hunter Department of Education
Alan McMullan Department of Education
Jill Fitzgerald Department of Education
A question and answer session ensued. The witnesses agreed to provide the Committee with additional information. The Deputy Chairperson thanked the witnesses for attending.
[Extract]
Thursday, 18 June 2009
Room 135, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Sam Gardiner MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
The meeting commenced at 2.02 pm in public session.
2.43 p.m. Ms Sue Ramsey left the meeting.
2.59 p.m. Mr Alex Easton left the meeting.
2.59 p.m. Dr Kieran Deeny joined the meeting
5. Committee Inquiry into Obesity.
Evidence session with the Department of Health, London
Members took evidence from:
Clara Swinson Deputy Director, Cross Government Obesity Unit
A question and answer session ensued. The Chairperson thanked the witness for attending.
3.02 p.m. Mr Alex Easton rejoined the meeting.
3.15 p.m. Ms Sue Ramsey rejoined the meeting.
Evidence session with officials from the Department of Health, Social Services and Public Safety
Members took evidence from:
Rob Phipps DHSSPS
Christine Jendoubi DHSSPS
Dr Naresh Chada. DHSSPS
Dr Kieran Deeny made a declaration of interest that he was a member of a local Commissioning Group.
A question and answer session ensued. The Chairperson thanked the witnesses for attending.
[Extract]
Thursday, 10 September 2009
Senate Chamber, Parliament Buildings
Present: Mr Jim Wells MLA (Chairperson)
Mr Alex Easton MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mrs Dolores Kelly MLA
Mr John McCallister MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance: Mrs Stella McArdle (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Mr Thomas Buchanan MLA
Mrs Claire McGill MLA
The meeting commenced at 2.00 pm in public session.
4.38 p.m. the meeting moved to closed session.
11. Consideration of draft Committee report on obesity
The Committee considered and agreed paragraphs 1 –70 of the draft report.
[Extract]
Thursday, 17 September 2009
Senate Chamber, Parliament Buildings
Present: Mr Jim Wells MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mrs Dolores Kelly MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
Mrs Iris Robinson MP MLA
In Attendance: Mrs Stella McArdle (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies:
The meeting commenced at 2.03 pm in public session.
4.19 p.m. the meeting moved to closed session.
4.35 p.m. Ms Sue Ramsey left the meeting.
10. Consideration of draft Committee report on obesity
The Committee considered and agreed paragraphs 71 – 91 of the draft report.
The Committee considered and agreed paragraphs 92 – 99 and deferred consideration of paragraph 100 of the draft report.
The Committee considered and agreed paragraph 101 of the draft report.
The Committee considered and agreed paragraphs 102 – 107 and deferred consideration of paragraph 108 of the draft report.
The Committee considered and agreed paragraphs 109 – 128 of the draft report.
The Committee considered and agreed paragraphs 129 – 133 and deferred consideration of paragraphs 134 - 135 of the draft report.
The Committee considered and agreed paragraphs 136 – 192 of the draft report.
The Committee considered and agreed the executive summary of the draft report.
[Extract]
Thursday, 1 October 2009
Senate Chamber, Parliament Buildings
Present: Mr Jim Wells MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mrs Dolores Kelly MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mrs Iris Robinson MP MLA
In Attendance: Mrs Stella McArdle (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Neil Sedgewick (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr David Irvine (Clerical Officer)
Apologies: Ms Sue Ramsey MLA
The meeting commenced at 2.01 pm in public session.
5.22 p.m. the meeting moved to closed session.
10. Consideration of Committee report on obesity
The Committee considered the draft report on its Inquiry into obesity.
The Committee considered and agreed amendments to paragraph 22, 62, 83, 95, 96, 97, 100, 108, 114, 120, 129,134, 135 and 152 of the draft report.
The Committee agreed the summary of recommendations
The Committee agreed that Appendix 1 to 6 be included in the report.
The Committee ordered the Report on the Inquiry into obesity to be printed.
The Committee agreed that an extract of today’s Minutes of Proceedings should be included in Appendix 1 of the report and were content that the Chairperson agrees the minutes relating to this to allow them to be included in the printed report.
The Committee agreed that a printed copy of the report be sent to each of the witnesses who gave oral evidence and those organisations who made written submissions to the inquiry.
The Committee agreed that the Department should be provided with a copy of the report in advance of the debate in the Assembly.
The Committee noted that a motion for the debate of the report in Plenary would be discussed at the next Committee meeting.
[Extract]
Appendix 2
Minutes of Evidence
26 February 2009
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Witness:
Dr Jane Wilde |
Institute of Public Health in Ireland |
1. The Chairperson (Mrs I Robinson): This evidence session will form part of the Committee’s inquiry into obesity. Members will find a briefing paper from the Clerk, and other relevant information, in their packs. We have already received a large number of submissions, copies of which are also provided for members’ attention.
2. Dr Wilde, you are very welcome. The usual format will apply — you will have up to 10 minutes for your presentation, after which members may ask questions.
3. Dr Jane Wilde (Institute of Public Health in Ireland): Thank you very much indeed. First, I want to say how pleased we are that the Committee has chosen to hold an inquiry into obesity. In particular, we believe that a focus on prevention is a very important part of tackling the problem, and it is on that aspect that I will concentrate today.
4. I very much welcome the opportunity to appear before the Committee. I think that the best way to approach such a complicated subject is to select five or six points to talk about. First, I want to comment on the extent and impact of obesity. Secondly, I will talk about why I think there has been such a huge rise in obesity, and why we need a strategic response that is long term and sustainable. Of course, in the short term, we also need a response to the problems that currently exist.
5. Thirdly, I want to emphasise the importance of a cross-Government approach to this very important public health issue — and I am sure that the Committee has heard that point many times. However, I will also highlight the need to reach well outside Government to the community and private sectors, because if we do not do that, there is no way in which we can tackle this huge issue.
6. My fourth points relate to evidence: what we know, and how we need to build a better evidence base about what actually works and what will help to stop the big increase in obesity levels. Finally, I want to say something about what we need to learn from elsewhere, because, of course, very many countries are facing the same crisis.
7. I will start with the first point about the extent and the impact of obesity. There is no one here who does not know that obesity is on the rise. However, it is really alarming when one starts to examine the problem in more detail. Obviously, like yourselves, I was aware of the rise in obesity levels, but when I think of how obesity is a risk factor for so many conditions — whether it be heart disease, cancer, joint problems or hypertension — I begin to see that it really matters and has a profound effect on the health of people in Northern Ireland.
8. Recent data suggests that well over half of the adult population, nearly 60%, is either overweight or obese, with about a quarter of adults being obese. Of course, there is also a huge rise in obesity levels among children. Nearly one quarter of primary 1 children will be overweight or obese in the next few years.
9. We carried out a study to find out about the rates of diabetes, and we forecast that, between 2005 and 2015, the number of people in Northern Ireland with diabetes will rise by about 17,000. As a result of that increase, by the year 2015, about 84,000 people in Northern Ireland will have type 2 diabetes. We considered the issue across the island and reckon that that number will be 280,000. Therefore, the scope of the problem is large, and its impact huge. Not only is there a cost to individuals, but there is the cost to society through loss of productivity and the cost to the health and social care system.
10. Thus, we are facing a very big issue. Why is that happening? At the heart of the problem is the imbalance between what we take in and what we put out — in other words, the energy we expend. All the studies that have examined the issue from a scientific angle say that the problem will not simply be solved by individuals. Quite honestly, it is not as though half a million adults in Northern Ireland decided that they wanted to get fatter. It is not about that. Yes, that is an issue, but we really must take a wider view and see the problem in a social, environmental and economic context.
11. I very much hope that, during the course of the inquiry, the Committee will see the obesity problem as a wider societal issue. Although there is obviously a need to inform and educate individuals, any action must reach out to include the food sector, the planning sector, practically every Government Department, and people right across Northern Ireland. That is really all I want to say about the extent and impact of the problem.
12. To follow on from that, we have watched obesity levels rise over perhaps 20 or 30 years, so we must plan a long-term response. It will not be a case of being able to say in the next two years, “OK, we have sorted this problem out". Yes, there could be short-term gains, but we really must be in this for the long haul, and we must have a strategic response. I know that the Department of Health, Social Services and Public Safety is putting together a briefing paper for the Committee to outline how the issue is being tackled, and hopefully departmental officials will appear before the Committee to explain it. I will not say any more about that because that is the Department’s work.
13. However, the purpose of the strategy is to ensure some coherence between what is happening locally and what is happening across Northern Ireland. Someone asked me whether much was being done, and I said that there are hundreds of small interventions in schools, communities, workplaces, and so forth. That must be set in a regional strategy so that there is some coherence between what happens across Northern Ireland and what happens locally.
14. We also have to be clear about who is responsible for what, because, with so much going on and so many people and organisations being involved, it is really important that there is some leadership, accountability, responsibility and a mechanism for reporting on what is happening. As well as the long-term strategy, we need things right now. Many adults are overweight, and we need to decide how we will help them and how we will stop them from becoming more overweight. I am not concentrating on the treatment care side, because that is not my prime business, but we need to be very careful, particularly with the recession, that what is happening with regard to eating and physical activity is not causing people more harm.
15. Cost is a big issue, and we have to think about the people who will be disproportionately affected by the recession and about what we can do to try to make it easier for people to eat healthy, nutritious food on a low income. That is an urgent issue, and some ideas about what we could do include, for example, having good studies and good co-ordinated action, particularly with young people.
16. What about cross-Government action? If one considers the reasons for obesity, it is clear that all Departments need to be involved. A major issue is how the Committee for Health, Social Services and Public Safety can help by advocating cross-departmental, cross-party support for such an important issue. I am not sure whether it is standard practice to write to all the other Committees.
17. The Chairperson: We have done that.
18. Dr Wilde: It is important to get a call from the other Committees about how they view the issue in relation to their policies, because the last thing that we need in Northern Ireland is one Department going in one direction and the other Departments going in a different direction. It is so easy for action in one area to undermine action in another area. For example, we could say that we want the built environment to concentrate on encouraging physical activity and by providing green space and play space, but, at the same time, other Departments could be developing plans for building on similar sites. If we were not to take that into account, it would totally undermine the health benefits.
19. Many of the issues concerning obesity are upstream, in that they are trying to create a wider social policy. During the recession, when finances are really under pressure, it is important that those sorts of issues do not get lost, and they can get lost. Therefore, I urge that some emphasis be given to those issues if possible.
20. The Committee could play a significant role by insisting on the health impact assessment of Government policy. All planning applications should be examined in relation to their impact on health and on the obesogenic environment — for example, questions must be asked about whether they are helpful or harmful with regard to obesity. I am sorry about the terminology.
21. Although the impact of obesity falls on the health sector, and there is much that the health sector can do, it is up to many other sectors outside Government to do something. For example, I am particularly interested in what the food sector might reasonably be expected to do about addressing obesity. Obviously, it is a complicated area. However, if we let the situation continue as it is, without some greater checks on what is happening to the food sector, we will do a grave disservice to people in Northern Ireland. There is a requirement on the food sector to act responsibly within a certain timescale. It is important to go beyond a voluntary approach by the food sector. It is such a big area that I hardly know where to start, but we are talking about issues such as food labelling, pricing, availability, subsidies, local production, and so forth. That is a crucial issue.
22. The issue of how to integrate research into policy is huge. Perhaps the Committee might consider convening a round-table meeting of some of Northern Ireland’s leading researchers on obesity, diabetes prevention, and so forth, to try to gather the scientific evidence that might help in order to have a conversation about what you need to know and what they have to offer.
23. It is important to bring research, policy and practice together to try to work out what we know and also to identify any gaps. There is every danger in Northern Ireland that there will be more and more interventions, and we will not know what is working or not working. The idea of a continuous improvement in evidence is very important.
24. At the institute, we are trying to develop an initiative, currently called an “obesity observatory", to which we hope people will be able to turn for evidence when it is gathered. It will be a one-stop shop for evidence and data, particularly local data. People will be able to find out about the obesity situation, and obesity determinants, in their own council areas. I hope that that will be a helpful addition.
25. I have not mentioned the role of different sectors of the Health Service, whether in primary care or public health; I hope that there may be some questions or debate about that.
26. Northern Ireland is not the only place that is facing this problem. It is a major issue for all middle- to high-income countries, and is, sadly, becoming an issue in low-income countries. Not only are there one billion people across the world who do not have enough to eat but one billion people who have had too much to eat and are overweight or obese. We are facing an amazing global situation in relation to food.
27. Closer to home, what can be learned from Europe, the UK and the island of Ireland? We can probably learn quite a lot, but we are all struggling. The big issue might be for us to decide what we want to co-operate on rather than simply saying that we should have good relations with other parts of the UK and other parts of Ireland. Let us actually decide what it is that we want to learn from other places, and what we can test to help other places.
28. I will finish by acknowledging that the issue of obesity is very important and to wish the Committee good luck with the inquiry. I am happy to answer any specific queries. Thank you.
29. The Chairperson: Thank you very much for your presentation. It is an all-encompassing issue. We have written to Departments, but I think that, so far, there has been very little uptake.
30. The Committee Clerk: There have been a couple of responses.
31. The Chairperson: The deadline has just passed, so those Departments have not stepped up to the chalk line.
32. Mr Gardiner: It is lovely to see you, Jane, and you are very welcome. I will give you a little bit of encouragement; I was pleased to hear yesterday evening, at a meeting of the board of governors of Dickson Primary School in Lurgan, that an additional 10 children now attend the breakfast club. That is where we have to start — the primary school. Parents are dropping their children off — I will not saying “dumping" — on their way to work, and whereas those children would normally have had a packet of crisps and a bar of chocolate or something like that, they are now eating healthy food and fresh fruit. I welcome that.
33. Those children all have their own bottles — plastic, admittedly — with their names and the name of the school on them, and there is a water fountain so that they can get water as often as they need to during the day. I think that we are making a start. We must start at an early age.
34. Perhaps it is slow learners or people with a disability who are not active or fit who fall into the category of obesity. How do we get over that difficulty?
35. Dr Wilde: Breakfast clubs play an important role not only in nutrition but in wider health and well-being, social cohesion, and so forth. They are to be welcomed and should be protected during any public finance pressures.
36. Your second point was about the connection between obesity and people who have difficulty learning. There is ongoing research in your local health board area into that issue. I do not know whether there are any results yet, but I know that special programmes have been developed.
37. Mr Gardiner: Is that happening in areas other than Craigavon?
38. Dr Wilde: I do not know, but that is well worth exploring.
39. Mr Gardiner: It is worth checking out.
40. Dr Wilde: I am happy to follow that up.
41. Mr Gardiner: More publicity is needed on the subject to bring it home to people.
42. The Chairperson: Quite a number of schools across Northern Ireland have embarked on breakfast clubs with an emphasis on healthy eating. As Sam said, many parents have to hold down two jobs and are, therefore, rushing off to work and are leaving — not dumping — their children off as soon as the school gates open, so it is good to know that they are getting a sensible breakfast. That is important to the education of young people.
43. Mrs O’Neill: Thank you, Jane, for your presentation. A key point that you made was that the impact falls on the Department of Health, Social Services and Public Safety. Although a consistent approach must be taken across all Departments, the brunt of the financial cost of tackling obesity and the associated health problems falls on that Department. That is important for the Committee’s inquiry.
44. Many good things are happening, but, according to the University of Ulster, no country has led the way or been able to bring a marked turnaround or a significant change in how obesity affects their country. Are you aware of examples of good practice to which we could look? The Department’s submission states that there is an opportunity for it to take a leading role in that worldwide problem. That is an ambitious target. There is much work to do, including pushing Departments to work together and to co-ordinate their approach as to how they tackle it. What are your thoughts on that?
45. Dr Wilde: You raised the issue of whether any country has really cracked the problem of obesity. Many countries have good strategies and plans, but the issue is to find out what is actually working. Norway, for example, has been able to shift its national diet in a positive way. It has done so by a combination of pricing, subsidies, information, education and labelling. A strong Government–society approach was taken seriously, and a major effort was made.
46. Mauritius and Brazil have also had strong initiatives. Brazil promoted physical activity, and Mauritius focused on food. I hear that the levels of obesity are levelling off in France, but I do not think that we can turn to any one country, particularly one that is close to us, and copy it. All countries are struggling with the problem a little bit.
47. If we decided that we wanted to become the best country in that regard, we could do so. However, that would take some going. I would love to be able to be part of Northern Ireland’s becoming the best at obesity prevention. We would be doing such a wonderful thing for the health of people in Northern Ireland, and we would save a fortune in lost productivity and health and social care costs. Who knows what the opportunities might be for local food co-operatives and for achieving better educational results in schools from children who were well fed? The benefits could be gigantic. That would happen only if the issue of obesity were made a serious cross-Government priority, and that is a big ask.
48. Mrs O’Neill: A Programme for Government commitment is to halt the rise in obesity by 2011, so at least that is down on paper.
49. Dr Wilde: It is down on paper, and that must also mean something serious in practice.
50. Dr Deeny: You are very welcome, Jane. I agree with you; those of us who provide primary care must do our bit as well.
51. I want to focus on education; which is a cross-departmental issue. Nowadays, some schools place a great deal of importance on academic qualifications and do not give enough time to sport, exercise and physical education. That is a concern in my local area. Should schools be required to devote a certain amount of hours in the week to physical exercise and sport? I am worried that children are very wrapped up in GCSEs and A levels.
52. I am not one to talk; I need to lose a bit of weight myself. However, there is a huge difference between Omagh 15 years ago and the town today. I see young girls who are much heavier than girls of the same age 15 years ago. I do not think that they are getting the amount of exercise and physical education in school that they should. Academic achievement is so important now, that exercise is not a priority. Should the Department of Education say to schools that they should devote two or three hours a week to physical exercise for their pupils?
53. Dr Wilde: Absolutely; I totally agree with you. To go back to the previous question: can we be the best? Yes we can, but only if we have that kind of serious commitment. What you are saying is spot on. I echo the point that you made. One only has to walk around to see what is happening. Children do not engage in enough physical activity, but that could be changed.
54. Mr McCallister: You have probably gathered that the Chairperson’s suggestion to hold this inquiry received unanimous support. It is such an important issue for the Committee. Most of my colleagues are in agreement; one of the biggest difficulties for the Committee and for the Department of Health, Social Services and Public Safety is getting other Departments to buy in and invest in what is needed. There is no financial reward; as Michelle pointed out, the burden falls entirely on the Department for Health, Social Services and Public Safety.
55. Committee members spent the morning with representatives of the British Heart Foundation and discussed the problems of obesity and diet. You mentioned diabetes; in your opening remarks, you also mentioned writing to other Committees. I sit on the Committee for Regional Development, which takes a significant interest in initiatives such as the Safe Routes to Schools programme. That programme is running in 18 schools across Northern Ireland, and it gets parents and kids to walk to school in order to build an exercise regime into their day and take away their excuse that they do not have time to take exercise. We must replicate that across all Departments.
56. As Kieran said, the Department of Education must have a role, and so should the Department for Regional Development. We must make exercise safe, accessible and easy for people. The Department of Education can play a role in teaching people about diet and about preparing a healthy meal on a budget. There are many issues to discuss.
57. I come from an agricultural background, so food labelling has always been a concern. I was speaking to my colleague Jim Nicholson MEP a few nights ago, and he told me that the European Parliament has been discussing food labelling for more than 20 years, and whether food labels should include health information and other details such as the country of origin and the ingredients. There is also an issue about making such information easy to read. Those are important matters for us all; European rules limit what we can do in Northern Ireland about food labelling.
58. Dr Wilde: You identified excellent local interventions and asked whether they can be mainstreamed across Northern Ireland. It would be great to have the determination not to leave such interventions to be replicated at a gradual pace. Rather, on recognising a good intervention that is seen to work, whether it is regulatory or involves physical activity, it should extend to all schools.
59. Europe presents a difficulty in that measures that were introduced to protect people now act against them. However, there are ways in which Northern Ireland can get round some of the difficulties. It is amazing how many people are interested in obesity. Even as I waited before today’s meeting, I talked to various people about the subject. Everyone has a part to play, and everyone has an idea about what could be done better to tackle obesity. Of course we should be able to introduce good labelling systems here, and we should not tolerate systems that are bad for our health. Why should we? It is ridiculous.
60. I want to pick up on the cost to the Health Service. It occurred to me that, although much of the cost falls on the Health Service, if we consider the issue in a wider sense and take into account the loss of productivity, and so forth, a significant amount of the cost falls on other Departments; but it is not necessarily calculated in the same way. Perhaps more evidence to demonstrate that might stimulate other Departments to make further efforts.
61. Mr McCallister: To follow on from employment issues, time lost as a result of obesity and, as Kieran mentioned, its effects on education, perhaps the cost to business could also be measured. In the Department of Health, Social Services and Public Safety, the cost is measured in pounds, shillings and pence.
62. Dr Wilde: Given the huge impact of obesity on the people of Northern Ireland, it seems strange that it is not a high priority across Government. It is not as though the people who make policies and devise programmes are immune to the harm that we are discussing.
63. Mrs Hanna: Good afternoon, Jane; you are most welcome. We all have a personal interest in trying to control our weight.
64. The Programme for Government identifies obesity as an issue, which is a start. The Committee has talked about having a cross-departmental meeting on children’s mental health with the Committee for Education. Obesity, with its effect on self-esteem, creates huge mental-health issues for children, particularly if they continue to carry excess weight that they find more and more difficult to lose. The Committee has discussed and analysed obesity, and there is a huge interest in the subject. You mentioned evidence, and that is important; many pilot schemes are not picked up on because of a lack of evidence that they work.
65. I am trying to think of small, practical measures that could make a difference. Schools, for example, can take practical initiatives, such as having breakfast clubs and making sport fun rather than purely competitive, which applies to girls in particular. Girls tend not to play sport and seem to walk around eating crisps. When driving through any town or through the countryside at the end of a school day or at lunchtime, boys are at least kicking a ball around.
66. More legislation is also required, particularly in the food sector, because nothing changes behaviour more than that. Any legislation must be based on ensuring that people understand obesity, and it must take into account the issues of poverty and affordability. Some people do not have the choice, even when they know that they should be eating more fruit, to go to Marks and Spencer to buy lovely berries, mangoes, and so forth, and they need much more support.
67. I hope that tackling obesity will be a priority of the new public health agency, and that you and others who have been working on the issue will have a huge influence on that. At an informal meeting, the Committee heard an extremely interesting presentation on obesity. I cannot remember the doctor’s name, but much of his presentation focused on mind over matter and the psychology of obesity.
68. The Chairperson: The doctor is called Michael Ryan.
69. Mrs Hanna: Michael Ryan; I found him fascinating. People need to be motivated and to want to change. It is not that we do not all want to lose that half-stone, stone, or whatever; it is about being so motivated that it will happen. Much more interesting work could be done. I know people — not too far from me and from my heart — who have an issue with their weight. It is difficult, because people get very defensive and upset when they talk about losing weight, even though they want to. It is a hugely difficult area, and the psychology around it is important. That, along with the small, practical things that we can do at the start, make a difference.
70. Dr Wilde: The evidence shows that most children who are overweight or obese carry that through the rest of their lives. There is a high risk that, if a child is overweight or obese, he or she will be overweight or obese as an adolescent and as an adult, which has a harmful effect on people’s psychological well-being.
71. What role could the new public health agency and the new structures play? I would like the issue to be co-ordinated and, as they say, “rolled out". One often asks what small, practical things could happen. Part of my difficulty is that I find it hard to grasp what is happening across Northern Ireland. I would like the agency to play some role in putting together an inventory of what is happening, but I do not mean that it has to spend five years doing that. It could highlight what is working, what may be working and what is not working. We should be replicating situations that are working. It is not that I have a whole range of other small ideas; in fact, lots and lots of small ideas may not be the way forward. However, that is not to take away from the urgency of the situation. We must develop a system whereby we learn from what we are doing, rather than doing this, that and the other, and seeing how it goes.
72. A point was made about making things attractive. At the heart of the matter, there is the issue of how we make it attractive to eat more fruit, vegetables and salads, and how we make it attractive to exercise. That is what the creation of a better social environment is all about. We should learn a little from what has happened in other public-health issues, such as smoking. Everybody tried to turn the tide from smoking being seen as attractive thing to do, to smoking being seen as not attractive. There are definite possibilities in relation to physical activity and nutrition.
73. Mrs Hanna: What is your view on mind over matter? Michael Ryan had a theory that people needed to be put into a particular frame of mind to be ready to lose weight.
74. Dr Wilde: That makes sense to me. However, I do not know enough about the science of it. Nevertheless, one could imagine that that is true. If one is feeling low, one does not believe that anything can be done. It reminds me of the question about Northern Ireland being the best. It will not be the best if everyone believes that they are hopeless.
75. Mrs Hanna: Dr Ryan said that there are techniques to motivate people.
76. The Chairperson: One of the saddest things that I heard some time ago was about children who were afraid to get dirty because of the nature and quality of their clothes. I thought that it was very sad that children were afraid to get their clothes dirty and that their mothers did not allow them to go out to play. They then become couch potatoes and obese because there is no physical activity in their lives. If we are to consider children specifically, we also want to get them away from sitting for hours on end at computers. That is another area that needs to be addressed.
77. There is great concern in respect of those people in areas of deprivation. However, another tier of people is falling into that trap because of high mortgage payments going out, while their properties are worth less than half the value of what they used to be. They too are struggling, and something has to give; sadly, that is usually the quality of food. As houses are taken over by building societies and banks, I think that we will see more people fall into the trap of need.
78. Mr Easton: I have just eaten a packet of Minstrels so I am feeling a bit guilty. I consider myself to be a typical ordinary person who goes out shopping and, I have to be honest, does not read labels — my wife should be doing that but she is not. I believe that the majority of people do not read labels, and therefore, it will be a really tough task not only to educate people, but to try to make them do it. I do not know what the answer is; it is going to be very difficult. I am guilty of it and I will admit to that.
79. I do not understand why the cost of food is so high among all the big retailers, given that oil prices have gone down. In shops such as Tesco, there will be two packets of biscuits for the price of one, or something like that, and, I have to admit, I will buy them. Reductions do not tend to be on the good food, they are always on junk food. We need to look at what can be done to try to make retailers reduce the price of good food. I am guilty of all those things; however, I acknowledge that there could be huge savings for the Health Service, and an improvement in people’s general health, if something could be done.
80. The Chairperson: To save your marriage — and you are only just married — I will presume that you meant that you and your wife should do the shopping together. [Laughter.]
81. He is only a few months married, so one has to give him a little bit of leeway.
82. Dr Wilde: I totally understand your position regarding labels; apart from anything else, the labelling is usually so small that you need to have very good eyesight to read it. Other things, such as the traffic light system — which I am sure you have heard of — are more straightforward, and organisations such as the Food Standards Agency will be able to give you information about that system.
83. There is the further issue of how to make sure that what is sold in supermarkets is not always biased toward the unhealthy option, and it would be good to have some conversations on that with the food industry in Northern Ireland. You are similar to many in the population, in that for at least half the population, health is not a driving force when they go shopping. Therefore, we have to acknowledge that people are not necessarily going into shops to look for the healthy option; they are going in for high quantity and low cost. It is quite unrealistic for us to be pushing the healthy option if that is not aligned with the cost option. We have to take that on.
84. The Chairperson: The manufacturers and the food industry have to revisit the whole concept of how they promote foods, given that, worldwide, there is an economic spiral which does not seem to be petering out.
85. Mr Gallagher: Do you view alcohol and its associated lifestyle as a problem? Are there measures that should be taken to tackle problems such as alcohol advertising?
86. Dr Wilde: Public health problems such as alcohol, obesity, diabetes and heart disease — and the approaches to them that would make a difference — are all related. Education, for example, should be provided on all aspects of health, including alcohol, mental health, food and exercise. There should be an integrated approach to health and to cross-Government interest in it.
87. If I were asked whether obesity should be the top priority, I would say that it must be a key priority. The top priority should be to have a strong public-health approach that recognises the need to integrate our education, school, food and private-sector policies. Otherwise, it will be a case of having a discussion about obesity, then a discussion about alcohol, and then a discussion about something else. That is not the way forward.
88. Legislation on alcohol is a completely different issue, about which I did not come prepared to talk. I may have missed the point of your question. Perhaps I would be in a better position to respond if you clarified your thinking on the matter.
89. Mr Gallagher: There is a rise in alcohol consumption here, and I think that there is health damage associated with that. I want to know what you think about that issue.
90. Dr Wilde: There are major public-health issues associated with alcohol and young people’s use of alcohol. There are also issues in relation to pricing and availability. The general points that I have made about obesity also apply to alcohol.
91. Mr Gallagher: Is there a link between alcohol and obesity?
92. Dr Wilde: Alcohol is full of calories and could, therefore, be related to weight. I am not sure about the exact nature of the relationship between alcohol and obesity. Perhaps Kieran could help me out on that point; I need some assistance. [Laughter.]
93. Dr Deeny: The relationship is basically as you have described — it concerns the amount of calories that alcohol contains.
94. Dr Wilde: Alcohol is a risk factor for most of the illnesses for which obesity is a risk factor, such as cancer, heart disease, high blood pressure and stroke. Part of the purpose of trying to do something about obesity is to reduce levels of heart disease, cancer, and so on. Therefore, we should be doing something about alcohol as well.
95. The Chairperson: All of the members who indicated that they wanted to ask questions have done so. I will read a piece of information and then ask a couple of related questions.
96. Research Services’ ‘Obesity Inquiry Research Paper’ quotes ‘Tackling Obesities: Future Choices — Project Report’ and states:
“Research commissioned by the UK Government’s Foresight programme examining ways of tackling obesity, revealed that, ‘the causes of obesity are embedded in an extremely complex biological system, set within an equally complex societal framework [and] will take several decades to reverse those factors driving current obesity trends.’ "
97. It goes on to state that a key difference between the devolved regions in addressing obesity is the setting of obesity-related targets. England and Northern Ireland — where the current targets set by the Department of Health, Social Services and Public Safety are to halt the rise in obesity by 2011 — have set direct obesity-related targets, but Wales and Scotland have not.
98. Is setting such a general and short-term target realistic? Is it achievable or measurable? Can I canvass your views in relation to the effectiveness of setting targets as part of an overarching strategic framework?
99. Dr Wilde: I will answer the second question first, on whether I think that setting targets is a good idea. I personally think that it is a good idea, because it gives us something to aim for. It forces us to measure things which will help us to work out what the gap is: it is only when you set the target that you can see what needs to be done, and where we are in relation to that.
100. There are issues around whether the targets should be as general as halting the rise in obesity, or whether it should also be about setting specific targets for men, women, young people, and different ethnic and geographical groups, as the Northern Ireland Audit Office report recommended, which would make this a bit more sophisticated. I think that we should be doing that. In some cases, we do not have the information or data to be able to do that, but a debate around targets would encourage us to get that information, which I believe is important.
101. The important thing is not to have endless discussions about what the targets are — that would become a complete waste of time — but to set some general targets, like halting the rise in obesity, and then set some specific targets. The halt in the rise of obesity target is aimed at children. We should have a target for adults, and we should have a target for men and women, but we really need to think, not just about end-point targets, but about what the intermediate indicators are, that would be a bit more practical.
102. For example, to return to Kieran’s point about physical activity, we could gather information on how many hours of physical activity that children get in schools, and set a target for that. We could find out how many people are eating five portions of fresh fruit and vegetables a day, and so on, and that would help us to work out where we are in relation to what might be called intermediate indicators, that we assume would lead to a reduction in obesity.
103. Yes, there should be a good monitoring system with good targets, and good data to support that, which would be fed back. One of the things that I did not say is that in all of the work that is going on, and as the Department develops its strategy, it is really important that things are put back into the public domain so that we know what is happening; so that people like you, the politicians, get a sense of what is going on. That would help to better inform the public about what action is happening, and I think that targets can help that.
104. The Chairperson: Thank you, Jane for your time and for answering questions. It is a huge subject matter, which is far-reaching, and affects all Government Departments and every walk of life. It will be interesting to see what comes out of the inquiry.
5 March 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
Dr Naresh Chada |
Department of Health, Social Services and Public Safety |
105. The Deputy Chairperson (Mrs O’Neill): I welcome Andrew Elliott, the director of population health, Dr Naresh Chada, a senior medical officer, Rob Phipps from the health development branch, and David Galloway, the acting director of secondary care. I invite the witnesses to make a short presentation, which will be followed by questions.
106. Mr Andrew Elliott (Department of Health, Social Services and Public Safety): Thank you for inviting us here today and for helping me to skip introducing my colleagues. My responsibilities include improving and protecting the health of the population — in other words, the public health policy remit, reporting to the Chief Medical Officer — and I am accompanied by David Galloway, who will pick up on matters of concern to the Committee, concerning the treatment of obese people.
107. The Department of Health, Social Services and Public Safety welcomes the Committee’s interest in this important health issue for our times and for the future. As members are probably aware, this matter has been described as a time bomb, which will have a significant impact on the health and, indeed, wealth of all our futures. We live — at least in this part of the world — in a time of abundant food, but our ancient physiology is based on famine. Consequently, our bodies are designed to seek out, and consume at every possible opportunity, salt and — more pertinently for the purposes of this discussion — sugar. Therefore, it is no surprise that the food industry has recognised that fact. In a time of plenty, it is well placed to offer us whatever our genes have told us to desire. Furthermore, in recent decades, there has been a significant change towards more sedentary lifestyles, and there is a real issue with changes to our built environment not only in Northern Ireland but elsewhere.
108. No doubt Committee members have had an opportunity to read the Department’s written submission, and I do not propose to repeat it. Instead, I shall mention some of the key issues.
109. It is important to articulate that tackling obesity is one of the most important public health issues with which the Department is dealing. The ‘Northern Ireland Health and Social Wellbeing Survey 2005/06’ indicates that 59% of adults surveyed were either overweight or obese. The figures for children were lower, but they are still extremely worrying and are on the rise: 5% of five-year-olds are already obese, and 22% are overweight. The fact that the trend is rising gives enormous cause for concern, although the most recent figures indicate a little easement. We can return to that point.
110. It is important to note that the figures that I have quoted are similar to those found in Europe and North America, so we are all facing a similar problem. Therefore, a component part of the Department’s work will be to monitor interventions elsewhere closely, particularly if they are found to be effective.
111. The twin problems of too much energy in and not enough energy out — in other words, the lack of a healthy diet and an inadequate amount of physical activity — have long been recognised as risk factors for coronary heart disease. That fact was recognised here in the late 1980s, and those factors became the two essential targets in the Change of Heart programme, which some members may remember.
112. Throughout the 1990s and the early part of this decade, resources were directed towards promoting healthy eating and increasing physical activity, and those measures continue to form part of the Department’s work. In 2002, the Department launched its acclaimed Investing for Health public health strategy, which was important because it picked up on many factors relating to health determinants and wider issues.
113. At that time, there was a key change in strategic thinking, resulting in the Department identifying the need to focus on childhood obesity. It is not just an issue for the Department of Health, Social Services and Public Safety but one for cross-Government action, which is why the Fit Futures task force emerged in order to put in place an action plan aimed at preventing children and young people being overweight or obese. It contained recommendations for integrated cross-departmental action. That was made manifest by the development of a joint target among the Department of Health, Social Services and Public Safety, the Department of Education and the Department of Culture, Arts and Leisure to halt the rise in obesity in children by 2010. The final report of the Fit Futures task force was published in 2006, which identified a number of priority approaches: over 70 recommendations for action were made.
114. The Department’s current position on prevention is to build on Fit Futures, but to move to a position founded on recognition of the importance of addressing obesity across the entire life course. The vast bulk of our present work on obesity is founded on that principle of aiming at the whole life cycle. We remain committed to a cross-departmental and cross-sectoral approach. We recognise that, as well as the Department of Education and the Department of Culture, Arts and Leisure, other Departments also have a vital role to play. We will continue to press for a greater use of health impact assessments by Departments with responsibility for the built environment and for regulation of the food industry.
115. Our written evidence shows that we committed to developing an obesity prevention strategic framework by spring 2010. In the meantime, actions and initiatives that address childhood obesity in support of Fit Futures will continue. The new framework will not be a panacea. Challenges remain, particularly those related to what is known as the obesogenic environment, an environment in which it is more difficult for people not to become overweight. We are trying to tackle a long-term lifestyle issue in a world where the emphasis is often placed on short-termism. Our obesity prevention strategic framework must address those kinds of challenges and turn that trend around. That will not be easy, and it will not be possible for my Department to achieve that on its own.
116. I hope that we will have a chance to pick up on those issues in more detail during questions. I ask Dr Chada to make a few introductory remarks about the health and wealth impacts of obesity.
117. Dr Naresh Chada (Department of Health, Social Services and Public Safety): Thank you very much for outlining the key issues, Andrew. I speak as a doctor and a public health specialist; I am extremely concerned about obesity, as are other colleagues in the Department of Health, Social Services and Public Safety, particularly the Chief Medical Officer.
118. I will give the Committee a quick overview of some of the health impacts associated with obesity. We are all aware that heart disease and strokes continue to be among the biggest killers in Northern Ireland, and smoking causes much of that. However, obesity is an important risk factor for those conditions. If someone is under the age of 50 and happens to be obese, he or she is twice as likely to suffer a heart attack or have a stroke.
119. We are all aware of the many people in Northern Ireland who have diabetes: 65,000 to 70,000 people suffer type 2 diabetes. If one happens to be obese, one is 20 times more likely to suffer from that condition. The Institute of Public Health in Ireland has done much detailed modelling, particularly with respect to the way in which type 2 diabetes is likely to increase over the next five to 10 years. If we do not halt the year-on-year increase in obesity, we could have another 10,000 to 15,000 people with diabetes in Northern Ireland by the early to middle part of the next decade. That is also a matter of particular concern.
120. Other health issues are not as intuitively obvious. Cancer — particularly gynaecological cancers — are also associated with obesity. I refer to cancer of the uterus, cervix and ovary. Men may be affected by bowel and prostate cancer. A certain proportion of cancers can be attributed to obesity. Conditions of the respiratory system are also associated with obesity, including sleep apnoea and associated breathing problems.
121. We are all aware of the problems that orthopaedic conditions cause, both with regard to pressures on the Health Service and the wider workforce. Lower back pain, hip and knee issues are also associated with being overweight and obese.
122. That is a range of the issues that are associated with obesity and the public health impact that are important to everyone. I am sure that the Committee will consider those as serious issues.
123. I want to talk about health economics issues. Health economics is an inexact science, but I will quote some facts and figures associated with the costs of obesity. The 2003-04 House of Commons Select Committee on Health Third Report estimated that the cost of obesity was £3·7 billion per annum, which is a considerable resource.
124. The ‘Foresight: Tackling Obesities: Future Choices’ project report — to which we will refer throughout the evidence session and which forms a large part of the evidence base and policy behind current thinking on obesity — suggests that, by 2050, at current prices, we will be spending £10 billion a year across the country on direct Health Service costs associated with obesity. There will also be costs of around £50 billion a year associated with the loss of productivity and workforce issues. Huge resources are involved if we do not tackle the issue of obesity.
125. There are other estimates relating to Northern Ireland. It has been estimated that 260,000 working days are lost each year because of obesity-related conditions, costing the economy approximately £500 million. A recent Northern Ireland Audit Office report, ‘Obesity and Type 2 Diabetes in Northern Ireland’, states that, throughout the UK, diabetes is thought to cost the Health Service around £1 million an hour. In Northern Ireland, that translates into around £1 million a day. Type 2 diabetes is closely related to obesity and has a huge economic impact.
126. Mr David Galloway (Department of Health, Social Services and Public Safety): Generally, people present in the health system through morbidities other than their weight. That is recognised in the general medical services contract through the use of quality and outcomes framework (QOF) points and directed enhanced services (DES) for long-term conditions management. Some £800,000 has gone into supporting those DES directions, and 90% of GP practices have signed up to them. We have very high rates of achievement in the DES points, and high scores against QOF points.
127. Currently, we do not have any clear data to show the difference that primary care activity has made for those people. When they come into the secondary care system — Naresh has already outlined the impact of obesity on the health of those individuals — there is a significant knock-on effect for the secondary care sector.
128. There are services that are more specifically directed toward treating obesity and overweight people. We can refer people to a dietetic service, which can examine their diets. People who present for surgery will undertake preoperative assessments that offer them advice about managing their body weight, lifestyle, nutrition, exercise, and so on.
129. At the far end of that spectrum of activity is the possibility of surgery for those who are extremely obese. In the past, the National Institute for Health and Clinical Excellence (NICE) has issued guidance on access to bariatric surgery, and the Department has endorsed a clinical guideline for Northern Ireland. As such, it remains an aspirational programme.
130. Bariatric surgery is not currently commissioned by the health boards in Northern Ireland, although, last year, £1·5 million was made available to ensure that some 120 people had access to bariatric surgery from providers in Great Britain. The boards are currently discussing how they might progress that issue in 2009-2010 to ensure that that service is provided to the people who are most likely to benefit from it.
131. The Deputy Chairperson: Obesity is a cross-departmental issue, although the Department of Health, Social Services and Public Safety will carry the brunt of the cost of providing treatment and helping people. The steering group has been going for almost a year. Is there a good level of engagement by the other Departments that are represented on the steering group?
132. Mr Rob Phipps (Department of Health, Social Services and Public Safety): The short answer is yes. We mentioned the public service agreement (PSA) target for childhood obesity in our written submission. It is shared among the Department of Health, Social Services and Public Safety, the Department of Education and the Department of Culture, Arts and Leisure. There has been a strong partnership since 2004, but the steering group has invited other Departments to become involved. When we start to develop the framework, we will go back to those Departments to ask for outcomes; it is not enough simply to attend the meetings. I assume and expect that further discussions will take place.
133. The Deputy Chairperson: As you develop your framework, this inquiry will feed into it.
134. Mr Phipps: The timing is brilliant.
135. The Deputy Chairperson: It has worked out well.
136. Dr Deeny: I also have an interest in this subject. I see that three Departments are involved.
137. We all know about diet and exercise. There is a strong focus on diet, which is as it should be. However, there is a lot of talk about exercise but, perhaps, not enough action. Families and schools are important. I said last week that I believe that some schools have placed too much importance on academic achievement as opposed to exercise. Those of us who are privileged and lucky enough to have children have a responsibility to see that they get good exercise. I have two sons who are heavily involved in sport, but I have a daughter who is not getting enough exercise. In this electronic age in which there are so many interesting things to do on a computer, for example, I wonder what we should do as a Committee.
138. Should it not be mandatory for schools to provide at least two to three hours of exercise a week for our young people? I have seen what is happening in general practice. I have been a GP for many years, and I am now seeing young girls who tell me that they are smoking. When I ask them why — because we have to record information about their smoking — they tell me that it curbs their appetite. That is a worrying development, not to mention the fact that they are not getting enough exercise. We are too focused on what young people should not eat, but they are doing something that is harmful to their health in order to curb their appetite. We should focus on getting young people to take more exercise. Is the Department of Education thinking along those lines? I think that it should be. Should we be saying that the Department of Education should play a role and act quickly? It is just not good enough that schools concentrate on getting top marks at the expense of ensuring that young people get enough exercise.
139. Mr A Elliott: The support of the Committee on issues such as this is important. Each Department has its own challenges to face and has a lot to deal with. It is also important to say that, when it comes to the capability to learn, the mental health and well-being of children are paramount, and sport and activity can contribute to that. There is a double benefit in tackling obesity in that it helps to improve mental health and well-being.
140. Mr Phipps: Will you invite the Department of Education to this Committee?
141. The Deputy Chairperson: We have not decided that yet.
142. Mr Phipps: Physical education is a compulsory part of the curriculum for children in years 1 to 12.
143. It is up to each school, but Department of Education guidance states that they should do at least two hours’ exercise a week. In 2007, the Minister of Education launched the Curriculum Sports programme for primary schools, which aims to develop physical literacy skills. Therefore, schools are putting an emphasis on physical activity.
144. There is also the Health Promoting Schools programme, which addresses all areas. Therefore, although there is an emphasis on food and healthy eating, there is also an emphasis on physical activity. There are local activities and initiatives that involve young people of school age in physical activities, which are possible because of the Fit Futures funding that we provide to the health boards.
145. You may wish to ask the Department of Education about its guidance, but our view is that it recognises the importance of physical activity.
146. Dr Deeny: Is guidance good enough? Certain schools do not seem to be following the guidance. Is there no way to pull those schools up on that?
147. Mr Gallagher: The Department of Education will say one thing on guidance but then say that there must be 27 curriculum choices delivered at post-primary level. The Department is defeating its own guidance on exercise, because PE, games and sport are squeezed because of pressure from the other curriculum choices. Therefore, there is a bit of a problem.
148. Mr A Elliott: Schools will only ever be one component in tackling obesity — it will never be enough to rely on schools to solve the problem on their own. I can remember a piece of correspondence that our Minister received in which a doctor wrote that there was a school on the outskirts of a Fermanagh village that had no pavement for, perhaps, 100 yards from the school gate. If the authorities had designed the pavement in a different way, many more children could have been walking to school instead of being driven, because their parents were worried about them being knocked down.
149. There are many issues about how the Government and their agencies think about health and creating opportunities for movement and activity, even short of the formal sports curriculum. It is important for politicians, Ministers and Departments to begin to tackle and wrestle with those issues if we are to succeed in reducing the obesity problem.
150. The Deputy Chairperson: We must work together rather than in silos.
151. Mr Gardiner: Prevention is better than cure. Rather than nine of us on the Committee for Health, Social Services and Public Safety sitting around and listening, we must put our hand to the plough and see the work through. Along with the Departments, I hope that we can launch a publicity campaign by engaging with the ‘Belfast Telegraph’ and booking a page in all the local papers and the better-selling papers to get the message across.
152. Mr Buchanan: That will cost.
153. Mr Gardiner: It will cost more to treat a patient than to advertise to the public what they can do to prevent some of the illnesses associated with obesity. That can even be done at school level. We must work on getting that message to the public — we will not be able to get the message out as things stand, and people will continue to die. We must get the message across, come hell or high water.
154. The Deputy Chairperson: Are you talking about a Committee initiative?
155. Mr Gardiner: The Committee can push the initiative and push the Department to act. There could be a joint effort. I do not care who is involved, as long as we get the message to the public.
156. The Deputy Chairperson: We can explore that further.
157. Mr Phipps: Some of the funding that we have given to the Health Promotion Agency has been to promote physical activity through campaigns.
158. Mr Buchanan: It is not working.
159. Mr Phipps: As Andrew said, one of the key issues and difficulties is sustainability. The same applies to climate change — you have to keep going.
160. One of the difficulties that we have had in the past, because of the nature of the funding, is that one cannot get that degree of sustainability. I totally agree that we need to engage the population. It is a kind of social marketing. A number of countries are developing a social-marketing approach, which includes campaign work and getting the support of environmentalists. If there is to be a physical activity campaign, it is essential that the infrastructure is in place.
161. Schools were mentioned. Everyone should be on board, otherwise the campaign will sit by itself. The Foresight report states that there cannot be a series of one-offs; it must all be brought together. A campaign is absolutely right, but it must form part of the whole picture, and it must bring other Departments on board and get them involved. We must get the other bits together.
162. Mr Gardiner: We must start to get it right. There is not much point in sitting here talking about it. We want action.
163. Mr Phipps: I agree totally; we need action, and we also need other people on board.
164. Mr A Elliott: There is also a health inequality dimension, which is important to articulate. If a child happens to be lucky enough to be in a wealthier household, that child’s parents may drive him or her around from one interesting activity to the next on many evenings each week. If a child comes from a home without that luxury, he or she may be considerably disadvantaged as regards the risk of obesity. Therefore, we must see what we can do. For example, there is a beautiful natural environment around Belfast, but how accessible is it, how much is it used, and how safe do people feel when they use it? There is a whole host of issues that must be played into this discussion to get people moving and to get them out into the natural environment. I am thinking of Black Mountain, for example.
165. Mr Buchanan: No doubt, this is a huge concern right across Northern Ireland, when one considers the amount of working days that are lost and what that costs the economy and the Health Service. It is a big issue that must be tackled.
166. I was going to ask a question about education programmes, but that has already been answered. Schools used to buy into them. Programmes are in place in schools, and perhaps they could be widened in order to make sport or some such activity more creative for the children. Some children do not like sport as much as others. We must open it up and make it more creative to get them involved in some other type of physical activity. However, it goes wider than that.
167. What initiatives are available at GP surgeries or in local health centres, so that patients who attend those centres are made aware that there is an obesity problem that must be dealt with? Those patients need to take on the responsibility to deal with their situation. District councils provide parks and leisure facilities. However, we must get the message across to people to use those facilities, which will help them to tackle their obesity problems.
168. There is another element. Some people are on the edge of obesity, and they do not realise it. They may be slightly overweight and think that their condition is not too bad. It does not register with them that they are in that situation — perhaps I am there myself. However, we need to consider that issue.
169. I listened to Sam’s suggestion, but the Committee do not have the finances available to do that campaign. However, the new public health agency has been set up specifically to deal with such issues. Perhaps the Committee should write to the agency and ask it what strategies it has in place and how it proposes to tackle the issue of obesity.
170. Members are well aware of the DUP stance on the public health agency. There is no point in setting up such a body only to find out that the Committee has to pick up on something that the agency was established to deal with. As a Committee, we have to hold that body to account and examine exactly what it is doing.
171. Another challenge is the modern world of technology. Everybody is sitting pressing buttons rather than being active. We must tackle that issue in order to overcome obesity.
172. Is obesity more prevalent in socially deprived areas?
173. The Deputy Chairperson: We received a submission from the current public health body, the Health Promotion Agency. When the new public health agency is formed on 1 April 2009, we intend to invite its representatives to a meeting to put that question to them. That will probably be after the Easter recess.
174. Mr Galloway: I will start by explaining the primary care end of things. Primary care has a vital role to play in communicating the right messages about obesity and how people could try to manage their own weight, diet and level of physical exercise. Material is available to assist general practices to do that. In my introductory remarks, I said that that has been recognised in the formal structures for the general medical services contract.
175. Other options are available. In some parts of Northern Ireland, GPs are able to refer people to physical activity programmes that are run in conjunction with local authorities. That is not universally available across the Province, but that is the sort of activity-driven solution that GPs can offer when they believe that the issue is about encouraging someone to take part in physical activity. Those are the major elements with which GPs will deal without going into other forms of treatments, such as drug therapies, to curb diet or deal with weight gain.
176. Mr Phipps: There is a gradient of social class. A smaller proportion of social class A or 1 is overweight or obese than social classes D, E or 5. There is a whole range of issues around inequalities and access, which is very difficult to untie. The facts are there, but people give various reasons to explain them. There are certainly issues around access to fresh food and the kind of pressures that people may or may not be under. It is a very complex issue.
177. Dr Chada: I reinforce Rob’s comments. For most diseases and illnesses, there is usually some sort of social class gradient, which is prevalent and ubiquitous in public health. As Rob said, it appears that that is the case for obesity. There is probably a great deal of regional variation, both at a micro level and nationally. Again, one could try to unpick what the reasons for that may be, but it is likely to be a number of factors.
178. Mr Phipps: One of our responses to the board is to ensure that any initiatives are targeted at health inequalities so that localised targeting also occurs. There is a range of initiatives.
179. Ms S Ramsey: I think that I will be a fly in the ointment today. Before I do that, I declare an interest as somebody who is overweight.
180. You said that your Department, the Department of Culture, Arts and Leisure and the Department of Education have a shared commitment to tackling obesity, and thank you for providing the Committee with a good paper on the various steering groups and working groups. However, it strikes me is that, having seen some good advertising campaigns on television, there needs to be an overarching publicity angle. That follows on from earlier points: Samuel was right about the need for publicity and, as Thomas said, district councils also have a responsibility to publicise their leisure facilities. My district council, of which I was a member for several years, provides 26 play parks, but only one of them is in a nationalist area. We must consider the cost of entry to leisure facilities. You made a point about what is happening in Belfast, but there are other issues.
181. My concern is about overall responsibility: can the Department of Health, Social Services and Public Safety simply take the lead on tackling obesity? Departments are arguing about which of them should fund schemes such as Sure Start or after-school projects. Who intervenes to say that enough is enough and tell an individual Department that it must fund a particular project or scheme? Representatives from areas of social disadvantage are fighting with the Department for Social Development about neighbourhood renewal. Who intervenes to demand that it be funded? An overarching strategy exists to deal with obesity and associated illnesses. However, if one Department says, for example, that it will not fund Sure Start or an after-school project, or if a council refuses to set up particular play facilities, who intervenes to insist that the funding goes ahead? Each Department is fighting for its budget.
182. It takes me back to the Investing for Health strategy. It was a key document at the time and all Ministers signed up to it. We now need to put Ministers and the Executive behind the eight ball and tell them that it is one thing to agree to the strategy, but they must be aware of what is happening on the ground.
183. The other day, the Assembly debated the advertising of cigarettes. Where do the supermarkets and manufacturers sit on the issue of obesity? Sometimes it is cheaper to buy frozen and convenience foods than fresh food. Who is responsible for improving that situation? I mean no disrespect to you or the Department, and I am not saying that a commissioner is needed, but whatever you do will be a drop in the ocean until someone says that enough is enough. If the Department for Social Development, the Department of Education, the Department of Culture, Arts and Leisure or the councils cut funding or do not go down the line that we want them to, can the Minister of Health, Social Services and Public Safety go to them and say that enough is enough and outline what they need to do?
184. Mr A Elliott: I will respond briefly on a couple of those points. There is no doubt that, in identifying the early-years issue, you highlighted an important component of a range of public health issues that we are trying to tackle. The parts of the developed world that will be quickest and most successful in addressing obesity and noticing a real change will be those that are best at joined-up government. Their Ministers will be able to sit down and work closely together to determine what each of them needs to do to contribute to the overall package. The challenge for all of us is to try to ensure that, by working cross-departmentally, we achieve the most bang for the buck.
185. There are some positive elements to what is happening in healthcare. In setting up the public health agency, the Minister made it clear that he wants close linkages with local government. He wants the public health agency to be central to community planning and to all the activities that we expect to see local government doing more of in the future, particularly after the review of public administration is complete. That is encouraging and has the potential to tackle not only obesity but a range of other determinants of health.
186. Mr Phipps: One of the ironies of obesity is that most of the work upstream is, arguably, conducted outside the Health Service. You put your finger on an extremely challenging issue: for the strategy to work, we must negotiate with all the other Departments, because they each have a role to play. The next year will be interesting as those discussions develop, because we are adopting the approach of asking Departments where they want to be in 10 years’ time. The questions we will ask are: how do we get there and what are the barriers?
187. Ms S Ramsey: How do we enforce that? Kieran mentioned guidelines. For whatever reason, Belfast City Council or Omagh District Council may decide not to invest more money into play and leisure facilities. However, a key factor in tackling obesity is ensuring that people exercise. Who makes the councils accountable for making that happen? The steering group includes a representative from the Northern Ireland Local Government Association (NILGA). However, no representatives on the steering group have the authority to say to Lisburn City Council that of the 26 play parks under its control only one is in a nationalist area and that issues of ill health must be tackled, especially in socially deprived areas. However, it seems that no one on the steering group can do that.
188. Mr A Elliott: Are you suggesting that we introduce a mechanism to reach all the councils?
189. Ms S Ramsey: Yes I am, and I also want the Department’s strategy to be enforced. It is positive that some Ministers have adopted a joined-up approach, but other Ministers need to come into play. Local government is the key to all this, because it provides the leisure centres, the parks, and so forth.
190. Dr Chada: That is a very important point. You mentioned the Northern Ireland Local Government Association and its representation on the steering group. Certainly, involving local government is one element. Eventually, we will have to move towards mechanisms through which local people can influence what is happening. Such mechanisms will ensure that local players who are interested in public health can influence decisions locally, which is what you want to see ideally.
191. We are trying to put some of the building blocks for that in place by encouraging local government, as well as the regional and local elements of the new public health agency once it comes into play, to take a greater interest in public health.
192. Mr Phipps: Perhaps one of the ways forward is through PSA targets. One approach could be to have more shared targets. What you spoke about is what we will be grappling with over the next 12 months. Ms Ramsey’s point about securing buy-in is, to a certain extent, one of the challenges that we will have to address.
193. Mr A Elliott: We need to think about your point. Essentially, the issue is about how to engage effectively with the local councils and capture their attention. We will take that thought away with us.
194. Mr Phipps: The world is changing slightly, and we have to work our way through those changes at the same time.
195. The Deputy Chairperson: Community planning will be the key to taking this forward. Therefore, you will need to get that right before anything can get up and running. It is hard to change something that has become embedded. Therefore, we need to tack health inequalities onto community planning from the start. A pilot might be run in one of the areas, so it would be good to monitor that and see how it plays out.
196. Mrs Hanna: I certainly agree with Sue; we are all looking forward to the new public health agency and to seeing how well it works across the sectors. In the Assembly, we have a responsibility to work together and to work cross-departmentally, but we do not do that. We do, however, pay lip service to that responsibility, and we know it.
197. The Committee agreed that it should set up a group on young people and mental health with the Committee for Education to examine school projects and ways of supporting young people, such as coping strategies. We need to do far more on that, and we need to do it formally. For example, what is the Department of Agriculture and Rural Development doing about food labelling? Food labelling might not be DARD’s responsibility entirely, but it is its responsibility to some extent.
198. What is the Department of the Environment doing about open spaces? In rural areas, there are lovely parks and some great facilities; however, those do not exist in built-up areas. When I was a child, I was chased out of the house to play; now, even my granddaughter and grandson, who are 18 months old, have their own DVDs. In fact, I have been given a DVD for them to watch when they are at my house so that there is no problem. We did not have DVDs when I was young so we had to go out to play. That is part of the problem; however, it is far more than that.
199. I was a midwife for many years, and I believe that the way to tackle obesity is to focus on prevention and early intervention. Much of that should start at the antenatal clinic, if not before. A mother should be supported and educated about diet and exercise, because, as Kieran said, obesity is certainly connected to lack of exercise.
200. There has been a cultural shift from simply going outside to play to watching DVDs and sitting around waiting to be entertained. Given that shift, as Sue said, we must involve local government, and I think that it wants to become involved. Councils have some good facilities, but they must engage with people.
201. I worked on the reception desk of a leisure centre for about a year, and I knew all the people who visited. However, although it was free to attend the leisure centre, the people whom we wanted to visit did not do so. How will we engage with those people and make them visit leisure centres? How do we prevent them becoming obese in the first place? Obesity is an addiction, and, at that stage, it is difficult for people to lose weight. It is not as easy as visiting the GP, asking for help, receiving diet sheets and going on a diet.
202. I wonder about psychological therapies, because losing weight is very much about people’s frame of mind. I keep mentioning the informal meeting that members had with Dr Michael Ryan, which I thought was fascinating. Those ideas should be incorporated into our strategy on obesity, because they are not currently. It is up to the Assembly and the Department to address that matter.
203. We all work in silos, and although we talk about the Executive’s poverty strategy, the issue of obesity is linked to poverty and to the widening gap between the haves and the have-nots. We still have the same poverty strategy. In fact, it is a read-across from Westminster, and there have been no changes to it. The Committee for Health, Social Services and Public Safety has a lead role but not a full role, and members cannot address the matter unless we work with other Departments and find the key and the secret to engaging the public and getting the message to the relevant people. That must be done through the community, because many people become engaged in that through peer pressure and peer support.
204. We have analysed all the issues and have reached certain conclusions. However, we must establish how those conclusions will make a difference. We have not unlocked that matter yet. The only way to engage everyone is through the new public health agency’s working with all Departments and all Assembly Committees. What is the Department of Health, Social Services and Public Safety doing with other Departments? Is it asking questions about green spaces, food labelling and exercise in schools? We must ensure that all Departments play their part.
205. Mr A Elliott: The Department has recently been involved with Sir Michael Marmot’s work with the World Health Organization. He also did some work in England to tackle health inequalities. At one of those events, someone told me that, in order to tackle health inequalities successfully, the most important factor is to examine the first four years of life up to the age of three. It is interesting to note that money invested in early years, and before birth, could bring a much greater return on health outcomes on a range of issues.
206. Mr Easton: In various ways, obesity costs £500 million a year. That amount of money would represent a good efficiency saving for the Minister, instead of the number of nurses being cut back. However, as Sue and, to a lesser extent, Carmel said, the Health Promotion Agency and sporting initiatives will not make a huge difference. Legislation needs to be changed.
207. No matter how much exercise schools offer, as soon as it is break time, children go to the tuck shop to buy crisps or Mars bars, which undoes all the good work. School meals are mainly junk food, and, unless we change the law, force schools to offer healthy meals, remove tuck shops, tackle retailers and monitor what ingredients the food producers are using, we will not be effective. In order to make any difference, we need extremely radical proposals.
208. Mr A Elliott: We cannot speak for the Department of Education, but that Department would probably say that it has put a lot of energy into the Health Promoting Schools approach and tackling the issue of tuck shops. There have been some real changes. No doubt there are still some examples of poor practice, and the Department has started to focus on that issue.
209. Mr Phipps: Schools have new nutritional standards, and changes have been made to make them more rigorous. Schools have also been able to increase the amount of money that they can spend. Work has been done.
210. Mr Gardiner: There are also breakfast clubs, which promote healthy eating.
211. Mr Easton: No one denies that, but I am suggesting that it does not go far enough. We need something totally radical in order to make a difference.
212. The Deputy Chairperson: We intend to invite officials from the Department of Education to discuss that further with the Committee.
213. Ms S Ramsey: I agree with Alex, and I know what Sam is talking about; it is about changing a mindset. Not so long ago, there was a row in the Assembly about whether the Department of Health, Social Services and Public Safety or the Department of Education was funding the breakfast clubs and after-school clubs. It is about changing Departments’ mindsets. The will is there, but we need to change the mindset of civil servants. Instead of cooking the books, we must ensure that we are cooking the right stuff.
214. Mrs McGill: I have a question about children and young people in relation to the graph and some of the figures that you have presented on pages 3 and 4 of your written submission. The figures date back to 1997 and 1998, and there are also some figures for 2004 and 2005. However, the rest of the graph relates to possible trajectories. There is a gap from 2005 until now.
215. Mr Phipps: Those figures need to be updated.
216. Mrs McGill: That is a bit out of date. The graph is an illustration of possible trajectories, but it would have been better to have a more up-to-date analysis of the situation in relation to children and young people.
217. As a personal observation, I do not see obesity in young children when I meet them. I read your figures, but I do not actually see evidence of obesity, although, obviously, what I see is limited.
218. Mr Phipps: That is interesting, because research has been carried out into parents’ views of their own children, and many parents cannot see that their children are overweight, although the figures suggest that they are; there is a perception that parents do not always recognise their children being overweight.
219. Adults and parents do not always see the link between being overweight and ill health, as Dr Chada pointed out. They think that a child may be overweight but that he or she is still healthy. People’s perceptions are an issue. Awareness must be raised of the health risks associated with obesity. Your point is absolutely valid.
220. Mrs McGill: That is not really my point. When I see groups of young people — and many visit this Building every day — I do not look out to see who is obese and who is not, but I do not see such levels of obesity.
221. Mr A Elliott: Only 5% of children are obese, but a higher percentage of children’s BMI is not at a healthy level. Perhaps that is not as obvious in a group of people wearing blazers.
222. Dr Chada: There are two issues here. First, as Rob and Andrew pointed out, the prevalence of children who are overweight or obese is much lower than it is in the adult population. Secondly, as Rob also said, it is a matter of perception and norms. Over time, people have been getting heavier, and there is a higher prevalence of people who are overweight or obese. Therefore, what we now consider to be normal might not have been considered to be normal 20 or 30 years ago. Therefore, there are many subtle issues that point to how we perceive matters.
223. The Deputy Chairperson: You said that the statistics here are not dissimilar to other areas. Have you examined how successful other countries have been in tackling the problem? Perhaps you could share with us success stories and good practice elsewhere?
224. Mr Phipps: I attended an EU meeting recently, and it was fascinating to hear about all the countries that we assumed would not have had an obesity problem. For example, Italy is very concerned about obesity, as are Spain, Portugal and the Czech Republic. Interestingly, the Czech Republic has great difficulty in getting young people to eat traditional Czech food. Therefore, it is the same issue — it is about the globalisation of food patterns.
225. Sweden has had some success, and it has seen a reduction in obesity among young people, but it has been honest in saying that it does not know the reason for that. Nevertheless, it has seen a slight decline.
226. A programme called Ensemble, Prévenons l’Obésité des Enfants (EPODE), which means “together, we can prevent obesity in children", has been implemented in France and Belgium, and it focuses on the local community. England is considering adopting a similar programme called Healthy Towns, which takes a community-driven approach to tackling the problem.
227. Therefore, there are some examples of good practice, but, interestingly, much of Europe is saying that there is a problem, and we are not too sure how to address it. People want to find the best way forward, and the approach that we propose to take is one that Holland and other countries are keen to follow. Therefore, other people are thinking of taking the approach that we are taking, so we are almost leading in the overarching obesity framework.
228. The Deputy Chairperson: Finally, the Health Promotion Agency’s submission to the Committee stated that its weight management clinics are not consistent across the North and that access varies depending on where people live. Do you have any comments on that?
229. Mr Galloway: That is the situation. In response to Mr Buchanan’s question, GPs can refer people to activity programmes, which are delivered in leisure centres. However, that is not universal. Therefore, there some work to be done to ensure that the services are available so that people can be referred and can receive advice and information about how they could better manage their weight.
230. The Deputy Chairperson: Obviously, consistency is important.
231. Mr Galloway: Consistency is the issue. Over time, the four boards have taken different approaches to issues in their own areas, so the situation has developed in slightly different ways in the four board areas.
232. Dr Deeny: What does PSA stand for?
233. Mr A Elliott: It stands for public service agreement.
234. The Deputy Chairperson: Thank you very much for coming along.
5 March 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
Dr Caroline Hughes |
Action Cancer |
235. The Deputy Chairperson: The next evidence session is with representatives of Action Cancer. I welcome Geraldine Kerr, acting chief executive of Action Cancer; Caroline Hughes, research and evaluation officer; and Treasa Rice, health promotion manager. Members have a copy of the written submission.
236. You are welcome to this afternoon’s Committee meeting. Geraldine Kerr will make a short presentation, and that will be followed by members’ questions.
237. Ms Geraldine Kerr (Action Cancer): Thank you for inviting us — we have not presented to a body such as this before. I will provide a brief overview of the document that we have presented to you. Details on statistics, for instance, will emerge in the discussions afterwards.
238. Obesity is a complex issue, and there are various facets involved. We examine the issue in two strands: society and the individual. Previous concentration was on societal issues such as food labelling, cycle lanes, etc, and the need to work cross-departmentally, from the top down.
239. I want to focus on the individual and what our work can do to inform the inquiry. I will explain the reasons for our work, our aims, the programmes that we use, how they can help and contribute to the approaches — particularly in respect of obesity — and how they could be applied within a strategy.
240. It is important to remember that the health consequences associated with obesity are a primary concern. Obesity cannot be viewed in isolation. A number of factors contribute to weight gain. It is not solely about the food that we eat, the amount of alcohol that we consume or our lack of energy output. A lot of it relates to one’s lifestyle. Our lifestyle programmes are focused on cancer. Two thirds of cancer can be prevented through lifestyle changes, such as more exercise and a change in eating habits. We concentrate on lifestyle changes. There is some relevant learning as a result of some of our programmes.
241. It is important to remember that nobody chooses to be overweight. People choose certain behaviours that have poor health consequences. We have to provide more knowledge about those behaviours and why people make those choices.
242. Treasa Rice is our health promotion manager, and she can provide more detail. We are a regional service; we go to primary and secondary schools, community groups and workplaces to provide different levels of programmes. Our programmes include education on cancer awareness, cooking and eating, and physical activity — with “boxercise" and “dancercise". That exercise input is aimed at active measuring and addressing some of the issues.
243. I do not know whether members are aware of our Big Bus initiative; I know that Carmel knows about it. It is a regional mobile unit that provides a breast-screening service. Other important services that it provides are the health checks for men and women. Those checks provide an overview of body mass index (BMI), cholesterol and blood pressure. An evaluation has been completed on that service, and we can provide more detail on that. It is interesting to know that 45% of the people who came to the Big Bus would not have had their health check if it had not been for the bus. The health checks have also provided cancer awareness and an awareness about self-checking, diet and lifestyles.
244. Caroline will provide more detail on the evaluations, but there have been increased awareness and lifestyle changes as a result of that.
245. Certain schemes that work well are the school programmes and the health checks. We feel that it is important, as has been identified in other people’s input, that an overall strategy be adopted, which is connected from the ground to the top in a completely co-ordinated way. Everything that we do in our programmes aligns with various strategies — for example, the Investing for Health strategy.
246. It is good to be able to go into schools, because young people provide a nice, set audience. Informing people from a young age is easier because we are able to target our work to that audience and there is less need to change behaviour. If we get the message across to people early enough, we can inform behaviour that will carry into adult life.
247. Our regionally based service is provided on a consistent basis, and that work will be important in informing some of our insights and recommendations about how things need to be taken forward. Our evaluations show that people’s knowledge about the need for a healthy diet — eating fruit and vegetables, for example — is very high, but they also show that we need to develop our programmes to examine attitudes and motivational issues, and move from having that knowledge base to actually applying that knowledge. We are doing that, and we can give you more details on that as we go through this session.
248. As I said, 45% of the people who we are reaching through the Big Bus mobile service would not have had their checks were it not for that service. That is very significant and highlights the importance of the statutory and voluntary sectors adopting a community approach, because the Big Bus brings services into socially deprived areas where such services may not normally be available. That service involves working with local trusts and other agencies in a connected way to allow that provision to go into communities, and it is that partnership that gets the Big Bus into communities and increases the uptake of services.
249. A very interesting finding from our men’s health checks is that there are discrepancies between individuals’ actual diet and their perceived diet. People feel that their diet is healthy when, in fact, it is not. We can provide the Committee with some information on that, if that would be helpful.
250. We believe that there is a need for improvement in the strategies aimed at changing lifestyles, because we think that that is key when dealing with obesity. Obesity cannot be looked at in isolation; it is a lifestyle issue, and changing those lifestyles will be very important. Some of our programmes have elements that could, perhaps, be included in such a strategy.
251. There is no central source of information on what programmes are available across Northern Ireland and what other groups are working on health promotion and other related areas. It is important to have some sort of audit to understand what services exist. We have a regional base and operate in schools; therefore, we have a good basis from which to develop those areas, just as other agencies have. We should be trying to secure a more consistent approach and join up services, rather than having a situation in which everyone is working individually.
252. Not all programmes use a robust evaluation system. I note from previous input into this inquiry that groups have talked about the need for co-ordinated research, and that is something that we endorse. However, it is the level of evaluation that takes place, and the fact that that is done in a consistent way, that is important. That will give people a wider information base and will inform what needs to go into a strategy and how that needs to develop.
253. We have found that the outcomes of academic research are not always passed to community organisations quickly enough. Funding may be going into academic streams to inform research, but there can be a delay in getting the findings to community groups and those who are offering provision. Therefore, the impact can either be delayed or missed. It is important that, right from the start, there is a connection with the workers on the ground, so that problems can be addressed.
254. As previously identified with regard to schools, education strategies and interdepartmental working are vital. Obesity cannot be considered in isolation. Some of our ideas for addressing obesity through lifestyle change must be supported by education strategies: they need time and funding to be effective. The connection or interfacing with education is important to the success of the strategy. I can offer an example: to effect a real change in lifestyle, we may need to find classroom time. However, short of that, support from the education strategy and willingness among everyone to work in a connected way must suffice.
255. Funding must be made available, but it should be targeted and co-ordinated to improve knowledge as to what strategies on obesity and other health issues are effective. There must be a link from research, through evaluation, to effective practice. Funding may be on offer, but people may not be made aware of what is available. That starts with the audit. Practices that are already in place and known to be effective must be used. Evaluation and research will provide knowledge about what is effective. We must find ways of measuring the effectiveness of each funding stream, so that research can be widened to find a more coherent way of approaching the problem. In that way, there will be more than just pockets of funding available. I can offer an example: we have applied for funding from the Big Lottery Fund for work with complementary therapies. We drew upon the work of all the charities and hospices, and anyone working in that area, to do that evaluation in the same way, in order to gather more information within the same timescale. In that way, we must carry out an audit in order to find out what should be our key measurements and targets.
256. It is important that we have a steering group to co-ordinate that work, and it should have clear timelines and targets. Although strategic targets will be set, it is also important that smaller, measurable targets should be set alongside those. Some of the aspects we have thought about are leisure centre use, food purchase, activity levels and knowledge base. We can provide some information on how that knowledge base can be measured and how behaviours have changed as a result. Another way of measuring progress is through the uptake rates of programmes.
257. That is all that I have to say at present, but I can offer more information in answering your questions.
258. The Deputy Chairperson: Thank you very much for that, Geraldine. It was most informative. I must ask about the surveys you compiled on the Big Bus project, which show the difference between what people perceive to be healthy and what is really healthy. Have you any ideas as to how that can be tackled?
259. Dr Caroline Hughes (Action Cancer): One part of the health check is a form that participants fill in. They are asked: do you think that your diet is healthy? About 75% of respondents think that it is. However, the next question is: do you eat five portions of fruit and vegetables each day? To that, only 50% of respondents give a positive answer. That range of yes/no questions highlights that, although people might think that they are being healthy, their behaviour belies that.
260. A masters student is to carry out a small piece of research for us to find out what is going on — why people come for health checks, why people think that they are healthy when their behaviours are not, and so on. That research is the first step of the process.
261. The Deputy Chairperson: That is very important. People are often on fad diets that they chop and change all the time. It is obviously unhealthy to be on a WeightWatchers diet one week, a Unislim diet the following week, and something else the next week.
262. Dr Hughes: Yes, and people receive a lot of mixed messages. Many people pick up their knowledge from adverts and hear phrases such as “no added sugar" and “fat free". Those people think that they are being quite healthy, but that is often shown not to be the case when their diets are broken down.
263. The Deputy Chairperson: It all comes back to informing people through an education programme. You said that research shows that a lot of people do not realise that obesity is the second biggest risk factor for some cancers. That is a very strong message that people would take on board, one that you are always trying to get across, and it comes down to education and promotion.
264. Dr Hughes: Yes, and that is one of the messages in our health action programme.
265. Ms Treasa Rice (Action Cancer): The health action programme covers a range of lifestyle-choice topics such as smoking, alcohol, cancer awareness, healthy eating and exercise. We are sending out a number of messages about healthy eating and exercise, for example, so that young people and children in schools become aware that obesity is a big cause of cancer.
266. Mr Gallagher: Thank you for coming along today and making your very useful presentation. The paper that you provided for the Committee outlines what is working well. It states that the health action programme is reaching large numbers of young people right across Northern Ireland and that the key messages are, therefore, being highlighted on a Province-wide basis. Will you elaborate on that and tell us why you think those programmes are working well? I do not doubt that the programme is reaching people right across Northern Ireland, but I would like to hear more about it.
267. The Deputy Chairperson talked about the differences between what is perceived to be a healthy diet and what is actually a healthy diet. You mentioned that a lot of people say that they do not eat a certain amount of fruit each day. Has your research and study given any indication that there are some fruits that people should not eat? Are there foods on sale that are not good for one’s health, particularly in their impact on weight increase? That is an important point that may inform the Committee’s report on obesity.
268. Dr Hughes: The health action programme is about changing knowledge levels. For that reason, we have before-and-after evaluations of the programme. We measure people’s knowledge levels before they start the programme and after they finish, and then we make comparisons between the figures. The evaluation indicates that the programme increases knowledge levels on issues such as smoking, body awareness and cancer awareness.
269. We have been doing that for about 18 months, and data collection will continue until the end of the current school year. By then, we should have about 350 before-and-after questionnaires that have been completed by young people from across Northern Ireland. Our health promotion officers use the evaluation figures, which definitely show that the programme improves knowledge levels.
270. One finding that emerged from the evaluation is that knowledge levels are reasonably high, so there is an awareness that smoking is bad for them and that they should be eating five portions of fruit and vegetables a day. Therefore, young people already know something about healthy living before we go into the schools, which makes sense, given all the media attention and advertising about the issue. The message is starting to get through to people.
271. However, we have begun to identify that the work now needs to focus more on attitudes, because knowledge does not change behaviour. Just think of how many people know that smoking is not good for them, yet still choose to smoke. We can put everything in place, but it all comes down to an individual choosing healthy behaviour rather than unhealthy behaviour. We want our programme to develop to address that issue. Because we have carried out the evaluation, we can see that people’s knowledge is changing. We still need to run knowledge programmes, but we perhaps need to start targeting people’s attitudes, by carrying out more intensive work with smaller groups.
272. As an organisation, we obviously need to have the necessary resources in place to carry out that work, whether that involves funding or personnel. The schools will need resources to allow them to let children out of class for one hour a week for six weeks so that we can engage them in slightly more intensive work. Treasa will be able to go into detail about food choices.
273. Ms Rice: Through the health action programme, we promote the balance of good health, which shows the healthy plate, the five main food groups, portion sizes, and the foods that we should be eating each day. Fruit and vegetables and carbohydrates should make up the largest portions, as they are the two main food groups. We explain to the children and young people that, unfortunately, we should be eating the least amount from the saturated-fat food group, as those are the foods that are bad for us.
274. Children become aware of the choices. We tell them how much exercise they need to do to work off a whole pizza — around three hours of exercise. We talk about various snacks and show the equivalent number of sugar cubes in each one. It will surprise you all to know that a relatively small portion of jelly babies contains the equivalent of 60 sugar cubes. We always get a strong reaction when we tell people that — people do not realise that they contain so much sugar. Thus, the message that certain foods are bad for them is getting through to children and young people. We can see them hiding their wee cans of Coke and packets of crisps.
275. The Deputy Chairperson: Perhaps the Health Committee needs to hear that advice, too. [Laughter.] We were shocked there.
276. Ms Kerr: Another aspect worth mentioning is that Centra supports our health action work. We talked about connections with the food industry, and that has fed into the Committee’s inquiry. Centra is a key supporter of our programme, and that is an example of the food industry following up on our work. We talked about a motivational approach, and we give bikes and iPods to children as part of that work.
277. Ms Rice: There is also a fruit voucher scheme: kids who take part in the health action programme get a free fruit voucher, so they can get a free piece of fruit from their local Centra store, which gives them a wee bit of incentive to eat their five portions of fruit and vegetables every day.
278. Ms Kerr: The stores display healthy messages and run promotions and strategies, working alongside us and the schools. That triangle of connections has been very productive, and is an example of the links among the sectors.
279. Mr Gallagher: Thank you for that information. There seems to be some gain from the link with Centra, but do you think that that type of programme is effective? What else do children and young people buy when they are in a Centra store? Perhaps they go in to buy something else that you would not recommend at all. How can you say that that programme is working well to counter obesity and promote healthy eating?
280. Ms Rice: That is why we are trying to develop another programme that works on people’s attitudes, which would follow on from the knowledge-based programme.
281. Dr Hughes: We do not measure behaviour because the ‘Young Persons’ Behaviour and Attitudes Survey’ generally records the behaviours of young people. We hope that those types of surveys will highlight the change in behaviours further down the road. At this stage, the evaluation of our programme measures whether knowledge levels have changed. Because of that evaluation, we have been able to see that we need to move towards dealing with attitudes. We can then look specifically at how behaviour changes before and after that work, because it is the attitudes that matter.
282. Dr Deeny: Ladies, I thank you for your presentation, but you have destroyed my enjoyment of pizzas. [Laughter.] I did not realise how much work that your Big Bus creates for poor overstretched GPs. [Laughter.]
283. Ms S Ramsey: You are well paid.
284. Dr Deeny: As was mentioned during the previous evidence session, communication with the public is important. As a GP, the link between obesity and cancer is a new message. We have long known about other causes of cancer, so how we get that message out is very important. People should know that putting too much of certain foods in their mouths can lead to cancer.
285. Lifestyle and behaviour were mentioned, and that message should be promoted in the right way. For example, I heard a message on a local radio station this week — I understood the message, but I know that it will cause alarm and make some people anxious. I do not remember the exact words, but the general message was that alcoholic drink could cause breast cancer. The advert then proceeded to talk about safe limits of alcohol consumption. That message could be very alarming for people who drink moderately.
286. People present in my surgery with mental-health problems due to anxiety — people sometimes even become hypochondriacal. We do not want to make people obsessive about what they do. I do not want to live in a nanny state — I want to live in a country where people make informed choices. We cannot push messages down people’s throats or make them feel guilty about their actions — adults have a choice. Will you do what you can to ensure that your message educates and informs people, instead of alarming and terrifying them?
287. Ms Rice: We make sure that the people realise that the message is about moderation — we can have our pizzas and jelly babies, but it is important to have a healthier balance by eating plenty of fruit and vegetables and less unhealthy food.
288. Dr Deeny: Do you see where I am coming from? I can expect people who heard that radio message to come into my surgery on Monday and ask whether they have cancer, because they had a couple of drinks at the weekend. The message must be balanced.
289. Dr Hughes: We give counselling and complementary therapy services to cancer patients. One issue that arose in our evaluation of those services was that many patients who are diagnosed with cancer use self-blame as one of their coping strategies. The statistic that 80% of cancers are preventable means that many people automatically think that they could have prevented their cancer.
290. Just because someone has a certain lifestyle does not mean that they will get cancer — there is a link between the two, but, for example, some people who smoke do not get cancer. People who live certain lifestyles increase their chances of getting cancer.
291. Ms Kerr: The danger is labelling people. Some of the research states that obesity is caused by low self-esteem, so our programmes try to tackle that by looking at a wider way of connecting information. Therefore, if you are sending out wider lifestyle messages, which address eating and the dangers associated with obesity, they must tackle people’s motivations, find out their attitudes and inform them on how they can change those attitudes. That is the way to approach obesity —; regarding it as a problem or labelling people will isolate people.
292. In trials that we mentioned, some children will not change into their PE kit for boxercise classes, because they are overweight. In that instance, we should try to offer the programme in a way that offers an option, rather than making someone more distraught by highlighting them in what they feel is a negative manner.
293. Dr Hughes: Promoting self-efficacy is also important — the belief that the people are able to carry out the behaviours needed to make change. Enhancing the independent characteristics of the individual is important.
294. Mrs Hanna: Good afternoon; you are very welcome. That was a very good presentation; you kept to the point. The message that I took from it was that there was a need for more working together, and for better communication and co-ordination. One group of people may be involved in one piece of work, and it would help them to know about research and evaluations, particularly when it comes to introducing initiatives. Things are all over the place, and we are not working well together.
295. I was interested in what you said about people’s perception that they have a good diet. We all like to persuade ourselves of that, despite the pizzas and the Mars bars. It is about attitudes and motivation. When people are tired, they will reach for a quick fix; they do not want an apple. People need to eat an apple when they are not so hungry, because they know that it is good for them. We all try to do that, but we do not do it very well.
296. Dr Deeny talked about a nanny state; I am not sure what a nanny state is. I think that we have a very dependent state here, in which we depend on other people to keep us healthy. Although it is all about balanced information, all of us must take more responsibility for our health. If I am a bit overweight, or drink too many glasses of wine, I will have to put my hand up to that, but it is up to me to get more exercise and watch what I eat — as long as I am informed. The thing is, we are informed; you said that most young people know about the benefits of the five portions a day. However, the difference between knowing about that and acting on it every day is where we all fall down. It will be difficult to say no to the second chocolate biscuit, and change our attitudes to exercise, diet and self-control. Those are the stumbling blocks that we face.
297. You said that you had had some successes. Are you able to monitor people for a longer time in order to determine whether they are changing their lifestyle? Can you tell whether people have got into the habit of eating less rubbish and taking exercise every day?
298. Dr Hughes: That is the problem. The healthy living programme for adults is a six-week programme, but there is no long-term follow-up. Schools, for example, find it difficult to find the time to cover specific topics, and to get young people out of the classroom again in order to measure their progress. Knowledge does not change behaviour; it is down to a combination of personality, attitudes and individual components, which are more difficult to measure. A more intensive programme is required; that is what we are developing now.
299. Mrs Hanna: I appreciate that you do not have the staff capacity or the resources, but it would be good, when you begin that programme, to tell people that you will contact them six months later. That would inform your programme.
300. Dr Hughes: The attitudes programme that we are developing will have a six-week follow-up, which will be part of the programme that we will ask schools to sign up to. We will take half an hour before the programme starts in order to allow people to fill in the evaluation forms that will measure their behaviours, and again at the end of the programme and a few weeks later, in order to determine whether the messages have been maintained, even for a short while. Then, hopefully, from that pilot, we will be able to develop the programme further and go back a year later. That depends on what the schools can do.
301. Mrs Hanna: It should be available for all groups that are involved, from the Department down. It is about what is working. That is where we fall down. We have all these initiatives that are, sometimes, not very well evaluated, and we do not have the feedback about what works and what does not.
302. Ms Kerr: Now that this data has come to light, we hope to follow up on the heath checks in order to discover whether the programme has made a difference and allow us to gather some valuable information.
303. Dr Hughes: Part of the evaluation of the health checks involves asking people whether they learned new information from the session and whether they plan to change anything about their behaviour — diet, exercise, smoking, and so on. A lot of people say that they intend to change, but that is only an intention. Intentions do not change behaviour. We follow up by contacting them and establishing whether they have changed anything.
304. Ms Kerr: On Mrs Hanna’s point about adopting a more co-ordinated approach, we came across an example of that the other day while negotiating with the Northern Board about its funding of some of our smoking-cessation programmes. During our discussions and input, we talked about coming to address the Committee, and the subject of obesity arose. The board had not made the connection between obesity, lifestyle and the programmes that we have already put in place.
305. In a sense, that widened the conversation’s remit to include those connections — men’s health checks as well as children’s. The discussion became about connecting parents with the health checks, and connecting the child to the parent through some sort of managed programme that involved the parent as an audience, and that educated the parent to help the child to change behaviours.
306. Therefore, funding from one area is received by a trust and is then connected into a particular strategy. However, the obesity strategy connects with all other strategies. I am not saying that a trust should not decide where to channel funding, but it is important that it is aware of those strategy connections and of treatment targets.
307. Dr Hughes: I suppose the “Cook it!" programme is relevant, in that it is about cooking healthily on a budget. Young people with whom we work do not always have control over what they eat at home if their parents cook. If young people and their parents are being engaged at the same time, programmes such as “Cook it!" can be run.
308. Ms Rice: “Cook it!" focuses on a different food group each week. It may be fruit and veg one week and proteins the next. Each week, there is a wee bit of theory followed by a practical cookery session; therefore, they actually cook to a recipe each week, and then take home those recipes in order to make the meals for their families in the knowledge of what is healthy.
309. The Deputy Chairperson: No other members have indicated that they want to ask any questions. I thank the witnesses for coming along — you have been very informative. Thank you very much.
12 March 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
Mr Nigel Gould |
British Medical Association Northern Ireland |
310. The Deputy Chairperson (Mrs O’Neill): We will now receive evidence from the British Medical Association (BMA). I welcome Dr Theo Nugent, who is a member of the general practitioners’ committee; Dr Colin Hamilton, who is the chairperson of the BMA committee for public health medicine and community health; Mr Nigel Gould, who is deputy secretary of the BMA; and Mr Ivor Whitten — whom we all know very well — is the BMA Assembly and research officer.
311. Dr Colin Hamilton (British Medical Association Northern Ireland): On behalf of the British Medical Association Northern Ireland, I thank the Committee for the opportunity to give evidence today. Obesity is a significant public-health problem in most of the western world, and there are particularly high levels in Northern Ireland.
312. Obesity is caused by an imbalance between energy input and energy expenditure, which basically means that if someone eats something and does not use the energy from it, it tends to stick; there is nothing magic about the science. The question is how to get the general public to accept what we all know has to be done so that we can try to turn back the tide of obesity.
313. As a screening tool, obesity is measured by body mass index (BMI). A score of between 20 and 25 is considered normal, but there are people in the Province who have a body mass index of 60 or higher. There are not many people in that category, but anyone who scores over 40 would be considered morbidly obese, and many of the recommendations for dealing medically with obesity are for such people.
314. Obesity affects people of all ages, and there is a mission statement in our submission about dealing with children. That is where addressing obesity becomes important; it is not necessarily an individual issue, particularly since it starts in childhood; it is a family and wider societal issue. Therefore, many of our recommendations are not purely for those in the medical profession, like us, or those in the health services that the Committee monitors. The problem has to be dealt with on a wide basis and include education, the provision of opportunities for exercise and many other issues.
315. The BMA scientific committee in England has produced many reports, all of which can be made available for perusal to Committee members. Those reports address obesity at a variety of levels, such as childhood and adolescence.
316. My specialty is public health, so I will concentrate on the statistics. Since 1997, measurements have shown a 26% increase in adult obesity. That is a very significant increase; I cannot think of any other population index that has shown that sort of growth. Currently, 59% of adults and 26% of children in Northern Ireland are overweight or obese. Those children will probably grow up and develop to a higher percentage of adults because of the nature of obesity. It has been said that obesity alone is a population time bomb that will, perhaps, cause the generation that is growing up to have a shorter lifespan than their parents. Whether that does or does not happen is in our own hands to a large extent. There is nothing about this problem that is inevitable; much of it is to do with lifestyles and the environment in which people live.
317. Obesity causes 450 deaths a year in Northern Ireland at a cost of £500 million to the economy. The savings that are possible are mentioned in our written submission. I will not describe all the diseases that are associated with obesity; most members will know about those already and will have heard about them in other presentations. However, we know about the growth in heart disease and in type 2 diabetes, which is closely associated with obesity. There are many others, including some cancers.
318. What is it about the foods that we eat that are causing the problem? It is about fats and sugars; I do not claim to be an expert on physiological science, but if people’s diets concentrate on saturated fats and sugar, it is almost certain to result in obesity. If that is associated with lack of exercise, a cycle will build up. A problem with childhood obesity is that the next phase of life in the female population tends to be pregnancy. If a woman is obese by the time she becomes pregnant, a range of complications can occur that will affect the next generation. I will not go into all the potential medical effects; they are listed in our submission. At the end of this litany, the BMA believes that action must be taken to encourage people to make better dietary choices and to engage in a more active life. As I said at the beginning, this is not rocket science.
319. There has been a lot of coverage on the radio today about the suggestion of a tax on chocolate as an approach to the problem. The BMA does not believe that that is the way to go; to focus on one foodstuff does not seem to be very sensible. That proposal came from someone in Scotland; I would point out that a deep-fried pizza contains no chocolate and would be much worse than the occasional chocolate bar. To focus on individual foodstuffs on the basis of a parallel to smoking cigarettes is not the way to go. We all need to eat; none of us need to smoke, so there is a totally different dynamic at work.
320. The BMA will start to work with Northern Ireland’s new regional public health agency in a couple of weeks’ time, on 1 April. I do not want to speak for Dr Rooney or Dr Harper, but as we will be joining the new organisation soon, there is no question that obesity will be a top priority. Since this is not purely a health problem, however, there are other parts of the public service, including the Committee, that can concentrate on the issue. One is the interdepartmental public health committee, which has been in existence for many years and has achieved some good results. Obesity is an ideal subject for that committee to consider. The promotion of healthy eating habits in the school curriculum — I do not know whether schools still call it home economics — lends itself to education for life about what is healthy and what is not. That would be a matter for the Department of Education.
321. The provision of cycleways and walkways in new housing estates would, presumably, be a matter for the Housing Executive, Roads Service and other bodies about which members know more than I do. We envisage a multi-agency approach to tackling obesity, and we also want to encourage the private sector. It is important not to assume that education stops at school.
322. Over the past couple of years, the failure of some major supermarkets to adhere to a simple method of outlining whether the food that people buy from the shelves is healthy has been slightly disappointing. Those members who do the shopping will be aware of the simple red, amber and green traffic-light systems that anyone can understand. In some supermarkets, products are described as containing so many kilojoules of such and such per kilogramme. I cannot understand that, so how on earth anyone doing the shopping is meant to scan a product with that sort of overload of information and be able to buy healthy food, I do not know. Any pressure that could be brought to bear on private industry, particularly the food and retail food industries, would be extremely valuable, because people need not only to know what is healthy but to be able to access it.
323. I do not want to go into too much detail, because my colleague, as a GP, works more closely with the people affected. He will detail some aspects of dealing with the problem as it affects the population.
324. Dr Theo Nugent (British Medical Association Northern Ireland Northern Ireland): GPs are well placed to spot folks who appear either to have problems with obesity or to be heading in that direction. We are reasonably well placed to detect and manage some of the problems that arise, or the medical fallout, from obesity, such as osteoarthritis, raised blood pressure, heart disease and diabetes.
325. However, GPs are not terribly well placed to give people good advice on how to control their obesity. If, for example, a patient arrives at my surgery with a body mass index of over 30, that is a starting point and gives a rough estimate, or indication, of a weight problem. That individual might be tremendously fit and the extra weight might be all muscle, but, from my experience in east Tyrone, that is not always the case.
326. What does a GP do when patients seek help and to where does he refer them? More to the point, patients may have been motivated to seek help to produce a real change in their health profile years down the line, but where can GPs seek help based on evidence of a reasonable chance that patients will stick with the programme to which they sign up?
327. As Colin said, GPs are also faced with the broader issue of two or three generations of the same family presenting with similar health problems that stem from obesity. As GPs, face to face with patients and trying to help and advise them, where do we start? The main plea from GPs in the BMA is for an answer to that question. We know that the problem is increasing, and public-health colleagues are able to keep us well apprised of the demographic time bomb, but what can we do that will be effective in helping our patients to tackle the problem?
328. Dr C Hamilton: Members will see a few bullet points on pages 4 and 5 of our paper. In my panic to get through my presentation, I missed a couple of those, one of which concerns the role of employers. At lunchtime, I heard for the first time that the BMA has a good programme of yearly checks for its staff, including blood pressure, weight, and so forth. I am slightly envious of Mr Gould and Mr Whitten who are BMA staff, because the NHS is a poor employer in that respect, and, as one of
329. There are some good employers in the Province and others that are not so good. During a credit crunch, the temptation is probably to run down, rather than improve, such services. We would like to see employers being encouraged as well.
330. We have also suggested that the public health agency should research what works and what does not work, because that is a difficult area. Many people have been working hard in health action zones, and so forth, in communities. To date — and, in part, because of the four-board system — the best practices have not been spread throughout the Province. However, I think that that will happen quickly when we move to the new system. We have to find out what works.
331. It is not a counsel of despair. I know that I sounded pessimistic at the beginning of my presentation, but there are other parts of the world, such as Finland and parts of the United States, in which major results have been achieved. People have said that it is not easy to achieve a lifestyle change in Northern Ireland, but I argue against that. Our population is as ready for a lifestyle change as any other. In Finland, for instance, success was achieved because the wives and mothers were informed that, if they wanted their husbands and children to live longer, changes would have to be made. That has made a significant impact over the past 20 years or more.
332. Northern Ireland is not that different. Scotland is similar to here, and I know that there are programmes available there that are beginning to achieve results. Therefore, I am not as pessimistic as, perhaps, I sounded at the beginning.
333. The Deputy Chairperson: Thank you for your presentation. A research paper on how programmes in Norway have been taken forward, and their success, is being developed. I share your hopes for the role of the public health agency. We can see the importance of the role that it will play in tackling obesity, and, as part of the inquiry, we have invited representatives to attend the Committee after Easter.
334. Theo said that GPs are well placed to detect obesity. We have already heard about the lack of places or services, such as dieticians, to which individuals can be referred. Will you provide some information on follow-through services that are available and the problems that GPs are encountering? Detection is well and good, but it will be difficult to do anything about it if support and assistance are not available.
335. Dr Nugent: There is little problem when someone turns up with a fallout from his or her obesity, such as diabetes. There are services available to help them to deal with that. However, a colossal workload is required when an individual is referred with what the dietetic service term “simple obesity". That is, usually, a complicated obesity, and, to be fair, it does not test the motivation of the patient. I end up suggesting that they go to Weight Watchers. That is not a flippant comment; it tends to work. The Weight Watchers programme is based on healthy eating and the type of eating pattern that can be sustained lifelong. It does not recommend that individuals eat food that tastes like cardboard or that is made up in a milkshake, or any other gimmick.
336. I am also aware of exercise programmes. My practice does not have access to any, but I know a few practices that do. The consensus is that patients enjoy taking part in exercise programmes. They are motivated to go, and they ask to be signed up to them. They complete their 12-week programme, but I am not certain whether there is a longer-term follow-up. I do not know whether patients stick with it; they probably do not. However, it is worth trying. If those people do not try the exercise programmes, it reinforces the idea that leisure centres are only for the Lycra battalion who work on the treadmills for an hour or two at a time. They are for people who want to establish a healthy lifestyle.
337. There is a limit to where we can send people before they develop problems, and it is difficult for GPs to see how they can motivate individuals or encourage self-motivation in families. We are talking about families.
338. The Deputy Chairperson: Therefore, exercise should be available on prescription. When the Committee considered the issue of mental health as part of our inquiry into the prevention of suicide, GPs said that they suggested to people who were feeling down that they joined an exercise class but that those people could not afford to do so. We considered that joining a class would be beneficial. I know that exercise cannot be prescribed to everyone as it would be costly, but perhaps some aspects of that idea could be looked at.
339. Dr Nugent: It can be quite simple. The idea must be put into the public mindset that exercise does not have to be complicated. If people can do a 20-minute walk three or four times a week, that is brilliant. People should start with the simple stuff. Media programmes look for complicated answers to the problem and show intensive training regimes. That is all very well, but simple lifestyle changes can include, for example, cutting down on butter. That is not rocket science stuff to mystify the issue, but it makes it simple and relevant to the vast majority of people.
340. Dr Deeny: You more or less hit on what I was going to say. As a GP, it seems to me that, every time a societal problem arises, it is left to GPs to sort out. I could not agree more with Theo that GPs can deal with the consequences of obesity but that prevention is another matter.
341. Last week, the Committee heard evidence from departmental officials, and, as I said previously, too much emphasis is placed on diet as opposed to exercise. It is a two-way process, and it also includes parents and schools, the Department of Health, Social Services and Public Safety, the Department of Education and, perhaps, other Departments. I am aware of schools that place too much emphasis on academic achievement as opposed to exercise. Last week, departmental officials told the Committee that each school is given guidance that they should devote at least two hours a week to exercise but that they are not required to do so by the Department of Education.
342. I am sure that you will agree that that should be considered, because, when one drives through any large town, one can see that young people have become heavier. As I mentioned last week, I have come across girls who smoke to control their weight, and that is a shocking and frightening situation.
343. I have never been keen on the use of drugs to treat people who are overweight. I know that such drugs exist and that GPs sometimes have no choice but to prescribe them because a person’s health — or, indeed, life — may be at serious risk. However, those drugs create a mindset in which people think that all they have to do to lose weight is to take a drug.
344. I also agree with Theo’s point that people’s mindset about places such as leisure centres is that they are only for really fit people and for athletes, who seem to take over the treadmills for a long time. Those places should be for people who want to become healthy.
345. The Deputy Chairperson and the Chairperson have previously said that exercise is good for mental health. We know that endorphins make people feel good after exercise. It would be a good idea for GPs to select patients who could benefit from exercise programmes and to work alongside local government agencies or councils. In the long term, that would save the Health Service a lot of money. I would like to hear practical ideas about how that could be done. I know that that has been piloted in certain practices, but I would like to be able to prescribe some of my patients to take exercise, rather than writing out a prescription for drugs to try to curb their appetite.
346. Dr Nugent: The medication that supposedly controls obesity medicalises the condition and presents it purely as a medical problem for which there is a tablet. To an extent, human nature means that people will see obesity as not being their problem and that they simply need their tablets. My simplistic view is that such medication falls into two basic categories. The first type of medication stops people absorbing fat from their bloodstream, and it causes dreadful side effects in people who take the medication but do not follow a low-fat diet. The second type of medication is designed to do different things to the body, and it can do much nastier permanent damage to the circulation and elsewhere.
347. I agree that, in attempting to prescribe exercise and changing people’s mindsets, it is important to demystify leisure centres and turn them into places that are for people. Probably the original concept behind leisure centres was to have a community resource to which people could have access, and — I mean no harm to those who are addicted to exercise — it needs to be accessible to others. How do we go about that? I have found that word of mouth is a tremendous piece of machinery. If a programme were up and running where people could go along, where family groups could be encouraged to go, and it was no longer seen as a bit odd for families to exercise in a group in a low-key way — they do not have to be elite sports persons, and they do not have to be into one particular sport — it is bound to be an enormously powerful tool. It would also send out the right message.
348. I am happy that I am a GP in an era in which the old paternalistic mindset has long gone and that one of mutual respect exists. Without mutual respect, our profession could not function. That is also a useful tool. I hope that doctors are perceived by patients as being equal. Doctors have knowledge — and patients have different skills — but we are equals, and we are there simply as advisers and guides. However, there must be something out there that demystifies exercise.
349. Cycling is another classic form of exercise, as Colin said. When one wanders around Amsterdam, there is a fear of being clobbered by a bicycle every two seconds, because people forget that bicycles still exist. I cannot remember the last time that I saw an entire bicycle; they are usually chained frames attached to a lamp post because they have been vandalised.
350. It is simple, uncomplicated stuff: The BMA and GPs would welcome any move towards a public mindset of encouraging exercise at a simple level.
351. The Deputy Chairperson: Dungannon District Council took the decision recently to close the leisure centre so that it could be used solely by the XXL club, which some people might not even want to go to. When the local councils give evidence to the Committee, we can discuss further making leisure services more available and ask about the possibility of having private sessions in order to get people interested and moving without feeling intimidated.
352. Mr Gardiner: Dr Deeny has covered the issue of GPs, and GPs are the first port of call when a person has a problem. Dr Hamilton said that the hospitals were about the biggest offenders. Have you seen some hospital menus? If not, the Committee can ask for them, to see what is going wrong.
353. Dr C Hamilton: I have not seen any menus recently. I have paid attention to —
354. Mr Gardiner: You made a statement to the fact that they were the biggest offenders.
355. Dr C Hamilton: No; I said that they certainly were the biggest offenders as regards employment. Staff canteens always have a “healthy option" that I would not call healthy. We are suggesting that schools should no longer have only one healthy option, and that, for several days at least, there should be healthy food only so that pupils do not have the option of chips. In most staff canteens in Health Service hospitals, people will veer towards the chips and not the unfamiliar food, because they are consistent.
356. Mr Gardiner: Are you saying that healthy food is not based on five portions a day of fresh fruit and vegetables, and so forth?
357. Dr C Hamilton: Dieticians preach about five portions a day, and people need to have a certain amount of fruit and vegetables. However, that does not mean that people must spend their lives eating like a primate that eats only fruit. I will, occasionally, treat myself to fish and chips — about once a month — or chocolate once a week.
358. Mr Gardiner: Confession is good for the soul.
359. Dr C Hamilton: Absolutely. However, there are some people who eat nothing but fruit and vegetables, which is fine for them, but it is not really practical for most people’s lifestyles nowadays. However, a reasonable balance is required, and that is where education comes in. It is harder to teach a reasonable balance than an absolute.
360. Mr Gardiner: I thought that the BMA would have had an opportunity to look at the menus of the hospital authorities before it came to the Committee. Madam Deputy Chairperson, may I move that the Committee asks for different hospital menus to be provided in order to see what food is being served?
361. The Deputy Chairperson: We can do that.
362. Mr Gardiner: If the Committee can take any action, it will.
363. Mrs Hanna: Eating is pleasurable and fun, and we do not want to remove the fun entirely. However, as you said, people should enjoy fish and chips occasionally or, as I do, eat two or three chips from other people’s plates.
364. Although you are not specifically responsible for the problem, you are in an ideal position to know your patients’ backgrounds and the challenges that they face. Poverty and a lack of choice are the origins of much of the problem, and the figures continue to support that assertion. I understand how that happens, because less-well-off people cannot buy nice berries, and so on, from Marks and Spencer. Perhaps they do not have much choice, and the chippy is nearby.
365. Schools no longer teach much home economics. There is less emphasis on budget and managing a household than there was traditionally. Many people do not cook any more, do not know how to cook and do not eat meals at the table. There is a culture of TV dinners, and supermarkets are full of ready meals at bargain prices. Those ready meals are not fresh and contain many additives, and, as you said, one could not begin to analyse what is in those products.
366. People have huge challenges to overcome. Once somebody is overweight, it is difficult to lose weight, because, at that stage, eating is an addiction, and it is difficult to find motivation. Some sort of a partnership is required, and you said that you work with the health action zones. We must get closer to communities and try to encourage people to use leisure centres — which should be free of charge — for fun exercise classes for the entire family. Leisure centres could also put two healthy options on restaurant menus rather than one healthy and one unhealthy option. It can sometimes be difficult to make healthy food attractive, but it can be done.
367. Our approach must be based on practical solutions. We have analysed the situation, and we know the issues and the diseases that obesity is causing. We need to prevent obesity in people who are not overweight by offering better education and more exercise in school. We must practically support people who are overweight or obese in their communities and work with personnel in health action zones and other health groups. GPs should probably be part of that partnership, because they know the people, the background and the dangers.
368. Some sort of practical partnership will start to make a difference. That is easier said than done, but we have discussed the matter with some groups and will discuss it with many more. However, we need to be able to measure any difference. We should be able to return a year later to some groups in the community to see whether people are eating a healthier diet or whether they are feeling better. We could conduct some practical pilot schemes and measure the outcomes in order to determine what works and what does not work. Several groups need to work together practically on that matter.
369. Dr C Hamilton: Mrs Hanna makes some good points, a couple of which are reflected in our recommendations. I participated in a radio programme on U105 this morning. The caller on air before me was a father called Dave. He complained that he visited his local Spar in order to buy oranges for his child to take to school instead of sweets. He discovered that the price of oranges had increased hugely whereas the price of chocolate had decreased hugely. I understand his frustration. He tried to do something but the retail industry made it difficult for him.
370. Mrs Hanna mentioned ready meals. We all eat ready meals; they are a natural part of life. One thing that always bugs me is: why do beans with less salt and less sugar cost more? The same principle applies to other items. What is the justification for that? I do not know if the Committee will take evidence from the retail trade or the food industry, but it would be interesting to hear an answer to that question. Many food companies offer healthy alternatives, but why is there a premium on those healthy alternatives?
371. Mrs Hanna: The companies say that it is more work to remove the salt, in which case I suggest that they remove the salt from all products.
372. Dr C Hamilton: Precisely. Salt does not occur naturally in many basic foodstuffs. Therefore, it must be added somehow or other.
373. Dr Nugent: I also take your point that it is desperately important to look at outcomes and to see what actually works. Nothing is more demotivating than to launch a series of initiatives that roll on, year after year, and do not produce results. We cannot stand over them and have confidence in them; nor, indeed, can the public have confidence in them. That is an important point.
374. Mrs McGill: Having listened to today’s and last week’s evidence, I am beginning to think that, although this Committee is conducting the inquiry into obesity, perhaps the Committee for Education or the Committee for Culture, Arts and Leisure should be doing it. I have read Dr Domhnall MacAuley’s editorial, which is among our papers. You may not have seen it, but it is a good piece. The editorial is entitled: “Physical activity may be good for you but we are not the key players".
375. It finishes:
“Let us not be foolish enough to accept responsibility for a task we cannot deliver. There are many aspects of practice where we can make a difference. This is not one."
376. We are the Committee for Health, Social Services and Public Safety. You are the BMA. I have listened to what Theo said in response to our comments. I have also considered your submission. Much of it relates to what is, and what should be, happening in education.
377. Last week, I made the point to the departmental officials that I do not see the 26% of young people who are physically obese. That may be an indictment of what I see when I look at young people. There are many young people around the Building.
378. According to your paper, the figure for 2005, which is probably the most recent that is available, is 26%. We also have figures for 2003 and 2002. There does not seem to be an up-to-date figure for childhood obesity. That may be an issue. I do not dispute that there is a problem; however, is there any danger that the problem could be exaggerated in the first instance?
379. Dr C Hamilton: One of the problems of obesity, particularly in children, is that it is, to an extent, invisible. I am no expert on children. However, if a child is overweight compared with his or her peers, he or she is not going to be standing around on street corners or going places with the school team. That boy or girl is a lot more likely to be shut indoors and involved in solitary activities. That is part of, and reinforces, the problem. He or she will be using the computer as opposed to taking part in healthy sports, simply because he or she feels different and separated from other children.
380. Although that is a trite explanation for the issue that you have raised, there is a certain degree of truth in it. That problem can be tackled only through engagement with schools: it goes into areas that are beyond the Health Service, such as bullying, and so forth. That is a significant issue, which is why, when people get to the stage when they need to attend dietary clinics, psychologists are available. When people have spent years in that cycle, it can produce significant problems. However, is it one of compulsion; has the person learned the habit that food is his or her only comfort, and that has become that person’s lifestyle? It is not a purely physical problem; it has a mental overlay.
381. Mrs McGill: I understand that, but I want to know about the figure of 26%, which represents one quarter of young people. I know that these are 2005 figures, but still —
382. Dr C Hamilton: That figure does not mean that 26% of young people are morbidly obese, but rather overweight or obese. It is a question of thresholds. Like everything else — blood pressure or cholesterol — it is a continuum. If you find out what the figure was 50 years ago, you will discover that it was a lot less, and today’s figure is a lot less than in some other countries. I am afraid that we get used to the average in Northern Ireland.
383. Mrs McGill: I repeat: we need up-to-date figures rather than figures from 2003 or 2002.
384. Dr C Hamilton: I have no problem with that.
385. Mrs McGill: I think that those figures come from the Department.
386. I concur with what Carmel said about the situation in schools. There was a drive some time ago to have healthy eating in schools — Jamie Oliver’s campaign. To avoid eating a healthy lunch, the young people used to take lunches with them — crisps, and so on. As you have said, this is a major challenge.
387. Ms S Ramsey: I will not declare an interest here; I would have to declare an interest at every Health Committee meeting that I attend.
388. I wish to support Claire’s point, because this is not solely a health issue. Last week’s discussion with officials brought out that point. Has the BMA contacted other Departments on this issue? We say that it is not a health issue, but as a health professional organisation, the Committee compounds the problem when it adopts the issue. The BMA has a duty to talk to other Departments.
389. We need an update from the Department of Education. I have heard that there is a problem over the budget for extended schools. We aim to promote prevention, and we need to be proactive. As was said earlier, we need to get the message over at an early age. The prospect of extended schools was welcomed by everyone: it is not a health issue. However, we should try to get information on this issue because I am sure that this Committee would be genuinely concerned if the budget for extended schools were in jeopardy.
390. Dr C Hamilton: I agree completely with that. I am a governor of a couple of schools in Derry — one is primary, the other secondary. Both run the extended schools programme. They are excellent in teaching people to choose the healthy breakfast option, and so on. However, it is a vulnerable budget that may or may not be continued. We would like to encourage policies like this — policies that achieve results. This may not be a purely educational issue, but it certainly works for those who attend it. It must be encouraged.
391. The Deputy Chairperson: The Minister of Education does not want that budget jeopardised in any way. In this inquiry, we can urge the Department of Finance and Personnel to ensure that there is money for extended schools.
392. Mr McCallister: The Department of Health, Social Services and Public Safety has to pick up the cost of obesity, but its involvement comes too late. Other Departments should be involved beforehand. Probably, in an ideal world, all those other policies would be pursued, and obesity would not trouble GPs too much.
393. Your presentation is interesting in that the solutions to this problem are amazingly simple, but the problem is hugely complex. For Committee members, as policy-makers, it is difficult to take simple solutions and put them in place in every community.
394. Colleagues have raised interesting aspects. Carmel spoke of the huge inequalities in health. In the more deprived communities, not only are opportunities to exercise limited but healthier food options are also much more restricted. My background is in the agrifood sector, and I have visited the premises of food processors. I have seen the variations in quality, and the only factor that identifies the better-quality product is the price.
395. One can understand how easy it is for families on lower incomes to be drawn towards unhealthy food, and all of the problems that that brings, so it will be interesting to see how perfectly simple, everyday solutions to building a healthier lifestyle and diet — such as taking 20- to 30-walks or replacing the school car run with a walk to school — might be implemented. Simple solutions can address what has become a complex and costly societal problem.
396. Dr C Hamilton: Getting exercise need not be complicated; one does not have to go to the gym. Looking back 50 or 60 years, one discovers that obesity was not a working-class problem, but, rather, one of the middle and other classes — the people who had money to spend on food. Nowadays, the situation has totally reversed.
397. One reason for that is that much more exercise used to be taken during people’s normal day-to-day lives. For instance, there was not the same level of public transport; people tended to walk to the shops and carry their shopping home. It is not for me to tell people never to take a bus; however, one might suggest that they walk to the shops and, having finished their shopping, take a bus or a black taxi home. For many people, that would involve a 15- or 20-minute walk, and if such behaviour were to become the norm, in itself, it would achieve many of the results about which we have been talking.
398. One could easily suggest the same thing to middle-class people with four-by-fours. If someone lives a quarter of a mile from their children’s school, there is no need to ferry them there in the Chelsea tractor. I am not suggesting that people should send small children to school alone; they should walk with them, and establish the habit early. Walking is by far the best exercise; it is natural, one does not have to learn how to do it, and one can do it more or less anywhere.
399. Changing the types of food that people eat is a little more complicated, because many factors must be considered, such as pricing. Nevertheless, the simple foods that our ancestors ate — such as porridge — are perfect health foods. Nowadays, porridge has been replaced with sugary breakfast snacks, because they are fractionally easier to prepare in the morning. However, nearly everyone has a microwave, so it should not be difficult to make porridge instead of having cornflakes. Simple measures can work.
400. Mr Buchanan: There is no doubt that the increased level of obesity in today’s society is a worrying factor. Obviously, we all agree that prevention is better than cure, but, in order to prevent obesity, we must begin by getting our message through to very young people.
401. Although we talk a lot about taking a multi-agency approach, in my experience, it is difficult to co-ordinate such a united approach and to action it on the ground. Local councils provide leisure facilities and parks, but the problem is with connecting with people in order to encourage them to use those facilities. Similarly with schools; we can introduce all the programmes we want, but, once again, the problem lies with encouraging children to make use of them.
402. All those problems can be traced back to a lack of discipline in homes and families. Discipline in families, especially with respect to children, is the key to preventing obesity. Therefore, we must consider how best to connect with families in order to embed a culture of discipline, because no matter what sphere of life one cares to mention, the results of a lack of discipline at home are apparent throughout society. We must get back to that key component: discipline in the home.
403. What are we doing to educate families about the need to have that element of discipline in the home in order to prevent obesity? What has the BMA done to date? What meetings has it had with other Departments such as the Department of Education or the Department of Culture, Arts and Leisure about this problem?
404. Dr C Hamilton: Theo will answer on the primary care side, which includes family health issues.
405. The BMA is a national organisation, so much of our work and research has been undertaken nationally. Much of our scientific wing’s research has been done with English Departments, including some of the research and the booklets that we have already mentioned. I am not sure, Ivor, whether there has been any direct work with, for example, the Committee for Education. I do not think that we have received any invitations from that Committee.
406. Mr Ivor Whitten (British Medical Association Northern Ireland): No, we have not. Mr Buchanan made a valid point, which has been made before. What work is the BMA doing with other Committees if it is saying that the problem is societal and not purely medical? The BMA can take on that kind of work, although our members work at different levels with different Departments because of the existing co-ordination with the Department of Education at board level. Many of our members are already involved at that level. The BMA would, perhaps, wish to examine more strategic issues rather than day-to-day matters. However, I take the point; it is a cross-departmental issue, and it can affect the whole gamut of society in Northern Ireland. DETI and DEL are involved in creating employment and encouraging innovation.
407. As a BMA staff member, I can have a simple health check every year, which records my body mass index, my cholesterol and my blood sugar levels. I do not normally visit my GP except with my kids, and that private-sector health check immediately expands the cohort. Such a simple health check could easily pick up on busy working people who perhaps look after their kids or even their parents, or carers who look after everyone else but do not look after themselves. They are generally being missed because they do not present to their GP for a check-up. If check-ups are done in a simple manner through private-sector industries and organisations, that will immediately expand the cohort of people who are being tested and told that they should see their GP. Perhaps their BMI is a little higher than it should be, and they need to go to their GP just to be on the safe side. It encourages people to think about themselves and to ensure that, if something is picked up, they go to their GP. GPs can deal only with the people who present themselves. The responsibility to act goes across all Departments.
408. Food and nutrition are also important factors, with which DARD can become involved. Northern Ireland has excellent food standards; how can we improve nutrition throughout society? Healthy options in school meals were mentioned, but why cannot all food be healthy? We should try to make healthy food look a more attractive and easier option. It is easy to discuss those options, but incredibly difficult to implement them. The Committee is making a start, but the message must be spread further. It should co-ordinate its discussions with other Committees on how to make the issue cross-departmental.
409. We all have a responsibility, which we accept. It could be said that this Committee is making a start in its inquiry into obesity in Northern Ireland. Action to address obesity is currently very patchwork in that there are many pilots but very little co-ordination. The public health agency could be a major stakeholder, at least in a co-ordinating role, in ensuring that good pilots are rolled out across Northern Ireland and that they are properly monitored so that we can get as much information as possible. That is required, because we have very little information on how obesity is being tackled in Northern Ireland.
410. Dr C Hamilton: The important points about the role of the family should not go unheard.
411. Dr Nugent: Mr Buchanan, your point is very important. As a parent, until recently I thought that discipline was something that parents imposed on their children. Fortunately, my children are now at an age to disabuse me of that notion — I am now incorrect on most issues, and they are there to keep me right.
412. In my experience as a GP, most parents become bashful and annoyed about their smoking habits, not because members of their peer group are criticising them but because their kids come home from school and give them an earful about it. My youngest fellow is the only one of my three kids to do home economics at school, and it is amazing what he is aware of, what he knows and the issues on which he is prepared to pontificate. Obesity will never be one of his problems, because he is built like a racing snake, and he is the only one of my three children who will not get scurvy.
413. The education of kids, and boys in particular, is an interesting matter. Until recently, in many schools — although not all schools — home economics was almost a taboo subject. By giving boys more encouragement and access to that subject, they can gain an incredible amount of knowledge. That is also an important motivator for parents, because, when they are in Tesco, their children now question what they are buying. There are wider issues with regard to the economics of food pricing, but education and discipline from the kids upwards are the way to go.
414. The Deputy Chairperson: I could not agree more with you, because my kids are also like that. For example, yesterday was No Smoking Day, and my wee boy had my husband tortured all day by asking if he had smoked yet. Therefore, kids are important in tackling obesity.
415. Reference was made to Weight Watchers, but I do not want to pick on that programme in particular, because there are others such as Unislim. Do such programmes have a role to play in tackling obesity? I do not think that they are regulated. Do have any feelings on whether they should or could be regulated?
416. Dr Nugent: For a start, those programmes are accessible; they do not cost a packet, and they offer peer support. I also do not want to single out Weight Watchers, but it is the only programme in our area of which I am aware. There is a Weight Watchers “lite" in our area, which is typically for males who do not want to take part in a programme with a group of females of a certain age. Without being sexist or ageist, many males will not go to such groups, but they can access information online or in paper format, which gives them education about healthy eating with tasty food.
417. As an ordinary GP who works in an ordinary practice, that is the only thing that seems to make a difference: people sign up to a weight-loss programme and come back lighter, happier and, more to the point, are no longer eating food that is wildly expensive or that tastes of cardboard, as food from a zero-fat diet would. Those people are eating food that is spicy, tasty and interesting. I do not know about regulation, but the programmes seem to be well organised and well run.
418. The Deputy Chairperson: I thank you all for your contributions, which have been very helpful to members as we progress our inquiry. We will forward you a copy of our report when it is published.
26 March 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mr John McCallister
Ms Sue Ramsey
Witness:
Dr Michael Ryan |
Northern Health and Social Care Trust |
419. The Deputy Chairperson (Mrs O’Neill): I welcome Dr Michael Ryan from the Northern Health and Social Care Trust. Members will recall that we met Michael at one of our informal discussions. A copy of his submission and other relevant papers are in Members’ papers.420. Dr Ryan, thank you for sitting through our long business session. I invite you to lead off and members will ask questions when you have finished.
421. Dr Michael Ryan (Northern Health and Social Care Trust): Thank you very much for your invitation to come back to the Committee. I will talk to my written submission. I have also submitted supplementary information. I emphasise that I am speaking as clinician in the front line: I am not an academic clinician. I see patients who are at a very high risk of cardiovascular disease, particularly diabetes and high cholesterol. My motivation to get involved in this topic is due to the fact that 90% of the patients that I see are either overweight or obese, and there is no specific service for them to avail of.
422. Although the Department has made many efforts in the community, there is a significant shortfall in the care offered to patients — unless they are children, which is laudable — in the primary or secondary health-care arena. That is my motivation for coming here today.
423. There is no comprehensive, strategically planned, service for dealing with overweight and obese adults, in particular. There is also no seamless stream of care packages available for those who suffer from overweight and obesity. According to the World Health Organization, about 7% of all disease, about one third of all coronary heart disease and stroke, and almost 60% of hypertension disease are secondary to overweight and obesity.
424. As I mentioned, 90% of the patients I see for diabetes; about 80% who attend cardiac clinics; 70% who attend our gastrointestinal clinics, and about 60% who attend respiratory clinics have significant co-morbidity that is linked to weight and obesity. The difficulty is that there is no service for those patients. A large proportion of the population needs professional help.
425. I have appended a table to my submission that puts the issue of weight and obesity in context by ranking its health-risk factor against the risk factors of other conditions that have considerable resources invested in them. For example, smoking will roughly quadruple a male or female’s risk of diabetes, which accounts for approximately 12% of total health-care costs. Some patients who have hypertension — for which treatment is expensive — take three or four hypertension agents on a regular basis.
426. Abdominal obesity is on a par with those risk factors as regards the risk of cardiac disease. However, as a proportion of that risk, the resources put in to deal with the problem are miniscule. The problem is that, unlike other issues, there is no “plug-and-play" approach to tackling obesity. No tablets or agents, such as those used to control cholesterol or deal with hypertension respectively, can be used to tackle obesity. A fundamentally different approach is needed to tackle obesity than those that are being used to address conventional risk factors.
427. Secondly, much of the morbidity and premature mortality linked to hypertension, diabetes and cardiac disease is underpinned by the co-existence of overweight and obesity among those patients. At a whole range of clinics, obesity is the common denominator in a high proportion of patients’ conditions. My contention is that a vast range of clinical services is being “silted up" with patients who attend with obesity-related co-morbidity, but who have nowhere to go.
428. A doctor might pick up on the fact that a patient has diabetes, hypertension, a respiratory problem or heart disease and send him or her to a specialist in the respective field. However, the patient’s fundamental problem will not go away until the obesity issue is addressed, because it underpins the primary presenting complaint. In the current structure, adults with a weight-related problem are being squeezed into other clinics.
429. As I said, about 90% of the patients that attend my diabetes clinic have weight-related issues. It is well established that more than 90% of diabetes is caused by overweight — too many calories in, too few calories out.
430. Fundamentally, the current approach lacks cohesion and an overarching strategy. It fails to produce objective and quantifiable outcome measures, such as the assessment of value for money and clinical effectiveness. I suggest that the current approach is inadequate; we see the evidence for that in that the obesity and overweight epidemic is now described in the medical literature as having reached a crisis point.
431. I suggest that we adopt best practice: the Counterweight programme in Scotland, for example, has been shown to be very successful in primary care and we can use that as a model framework for an obesity service in the Province. The interesting outcome of that is that for every unit of weight lost, the drug costs — the treatment of hypertension, diabetes, heart failure and cardiac disease — drops by 6%. Therefore, there is a cost-effective aspect to this proposal.
432. The managed clinical network model of service delivery is now well established and has been shown to be an effective means of delivering targeted services for specific reasons. The approach to weight management at all levels of intervention should be supported by the managed clinical network. Much of the cost of such a programme is already embedded in the system because we are already dealing with the consequences of overweight and obesity on people’s health, but it is unrecognised and unquantified because there is no specific weight-related programme targeted at the problem. Considerable resources have already been invested in tackling weight-related problems but, as a practising clinician at the front line, I see no evidence of their effectiveness. A managed clinical network model, specifically for obesity, would be able to evaluate programmes of care and produce solid evidence or otherwise of cost-effectiveness and clinical effectiveness.
433. I have submitted some slides as evidence to back up some of what I am saying. I am conscious of time. On the first slide, to which I have already referred, you can see that eating fruit and vegetables reduces risk, particularly in women, and that exercise will halve the risk, particularly in women. Cholesterol is very important and very expensive to tackle, but its threat to health is on a par with overweight and obesity. Obesity is, literally, the elephant in the living room.
434. I hope that the slides complement what I have said. I apologise for the small size of the writing, but otherwise it would run to 10 pages.
435. Obesity is reckoned to cost the Health Service £120 million per annum in Northern Ireland. We are already expending resources on the consequences of obesity: I propose that we invest in preventing that outlay on patient care. The impact of obesity on an adolescent or a young adult is equivalent to that of smoking and there has been a tremendous effort put into smoking as regards awareness and prevention. There are smoking cessation clinics and smoking cessation nurses: we do not have the equivalent for obesity and yet it poses the same threat to health. As we gain from the use of cholesterol drugs and blood-pressure drugs, and as the death rates from cardiovascular disease fall, the death rate from diabetes increases. A report in January 2009 showed that 55 patients died from diabetes 10 years ago in Northern Ireland. The figures from last year show 188 patients having died from diabetes.
436. Diabetes is an inevitable consequence of weight gain: our submission contains slides showing obesity as a risk factor for type 2 diabetes in women and men. For those of you who are not familiar with body mass index (BMI), I will give an example. A person who is 5 ft 6 in tall and weighs nine and a half stone would have a body-mass index of 25, which is fine. A person who was 5 ft 6 in tall and weighed around 12 and a half stone would have a body-mass index of 30. I see patients who weigh twice that, as does every doctor in the Province. It is a useful benchmark to know when a person is clinically obese.
437. When people develop diabetes, they may say that they have a mild form of diabetes. That is like saying that you have a slight touch of pregnancy. It is a serious and significant health threat. We can see mortality and glucose as a continuum. I draw your attention to mortality, as it is such a “hard" end point, and there is no coming back from it.
438. The tragedy of the shortfall in healthcare provision is that much of the diabetes cases can be prevented. There are three trials to show that, within three years, intervention can prevent about 60% of diabetes from occurring. I present a summary of those trials in the submission. Exercise and weight control can prevent at least that amount of diabetes, which is costing the healthcare system dearly. Once a person is diagnosed with diabetes, his or her life expectancy is reduced by approximately 10 to 15 years.
439. If we invest in weight loss and obesity, there are a number of benefits that will arise from a 10% loss in body weight — those benefits are detailed in the slides. Again, I draw your attention to mortality, because it is so dear to my heart. One can see that obesity-related cancer deaths will drop by 40%. Some cancers, particularly in women, are linked; about half of certain cancers in post-menopausal women are related to obesity, according to a recent report.
440. There is no drug or combination of drug therapies that would achieve those gains across the board globally. The absence of such an approach to weight and obesity is a serious shortcoming in healthcare provision. The fact that there is not a “plug and play" technology makes it a difficult area, and one that doctors conventionally tend to avoid, because it requires a different approach; repeated intervention and support at psychological, social, or physical levels.
441. I have provided a hypothetical example in the submission, which details the years of life lost for someone aged 40, who is 5 ft 6 in tall and weighs 12 and a half stone, with a body-mass index of 30. At age 40 they would lose approximately seven years of life. There are very few medical illnesses that, globally, across the population, achieve that level of compromise in relation to life expectancy.
442. The impact of obesity and overweight is worse than all the cancers put together, on an epidemiological basis, and yet we can intervene, and it can be prevented if caught early enough. If there were a structured programme that would involve as many impact points as possible, we could prevent very significant premature mortality and morbidity in the population.
443. In summary, I support the proposal for significant investment; from my perspective as a practising clinician, the research has gone on long enough. There is very good evidence that weight can be controlled, that weight gain can be mitigated, and that the consequences of weight loss are well established. We have effective means of intervening, with motivational analysis, behavioural modification from the Scottish Counterweight programme to show that such intervention is cost effective. However, political will is needed to make it happen, and that is why I am here today. Thank you very much.
444. The Deputy Chairperson: Thank you for your presentation. It will be valuable to the Committee as it carries out its inquiry.
445. You talked about a managed clinical network, and the staff and training required for that. Will you give the Committee more information on the nature and extent of the specific training needed for staff to deliver such a programme, and how that programme would be delivered?
446. Dr Ryan: A managed clinical network is a well-established model of healthcare delivery, and there are several in the Province. Fundamentally, it is protected time for a range of interventions under a structured programme. It has terms of reference, a management board, specific goals, and an audit programme to quantify its outcomes.
447. I do not feel that training is the problem. For example, in my job plan I have no time to deal with obesity. The scale of the problem lies mainly in the community — in schools, play areas, secondary schools, universities, etc — and that would be a major plank of a network. The difficulty is that the effort that we are putting into schools is not part of a strategic system: we are not measuring the outcomes. For example, there are many community groups — such as WeightWatchers — and there are many facilities for exercise. We are not harnessing those resources in a structured and managed way.
448. I cannot say how much I would need specifically. Many trusts have a managed network for diabetes. The expertise probably exists already, and much of the effort and expenditure exists. However, it must be released specifically for obesity. I cannot quantify that at this stage. The cost of not doing it now will be much higher five years down the line.
449. Mr Gardiner: When I was reading your submission last night, the economy, the efficiency and the effectiveness jumped out at me, and you have referred to some of them. Do GPs need training in obesity? Can health visitors deliver information? How can we improve the system? You have talked about a programme, and getting it across to schools and various organisations. Please elaborate on that?
450. Dr Ryan: The problem as I see it — from my perspective as a clinician with nowhere to send my patients — is that knowledge is not the problem. We are all aware of the need for reducing calories, and we are all aware of the need to exercise. The difficulty is the patient’s relationship with calories and food. It is a complicated issue: it is fundamental to a patient’s sense of well-being. Some specific training is required, and the most effective strategy used in Scotland and Wales contains motivational analysis and behaviour modification techniques, which is a branch of psychology — it is not knowledge. Patients know that they should not eat cream buns or whatever it may be.
451. Mr Gardiner: I am not so sure that patients do know, and it would be better for them if their GPs told them so.
452. Dr Ryan: You are absolutely correct.
453. Mr Gardiner: Should someone in authority not get that message across?
454. Dr Ryan: Yes; but the message must be approved and standardised. GPs seem to be delivering a slightly different message depending on the biases, their expertise, or the level of interest that they or their staff have. Some of those messages are neither appropriate nor effective, and that is where the managed network approach comes in. There would be a single message, approved and evidence-based. It is not a group hug.
455. Weight and obesity are well-established causal factors, in the same way as blood pressure and cholesterol. We need to become more scientific and rigorous in how we deal with weight issues. Having a group hug is not acceptable; we can no longer depend on well-meaning individuals doing their best. There is evidence that there are effective strategies, and, for the health of our population, we must implement them with a sense of urgency. We all need to be retrained.
456. Mr Easton: It is good that you are enthusiastic. My feeling is that we force food retailers and producers to reduce the amount of fat, sugar and salt that goes into food, any measures that we put in place will not help much. I would appreciate hearing your comments on what we might do about that problem.
457. You touched on the subject of diabetic clinics. Do you think that a clinic should be developed specifically for obese people?
458. Finally, what is your opinion of the Norwegian nutrition policy and healthy-eating campaigns, which seem quite good?
459. Dr Ryan: My answer is yes to all of the above. We do need to engage with the food industry, but only up to a point, because it will be led by market forces. Educated people make different choices than uneducated people. In our efforts to improve the health of the community, although it is important to engage with the food industry concerning salt, fat and sugar, the question is what can we do with a 35-year-old person who weighs 26 stone and cannot walk because he or she is so heavy? The cost of dealing with the health problems associated with such a patient is enormous; whereas, the cost of dealing with that person’s diet and getting him or her back to work is relatively small.
460. Two weeks ago, I saw a patient in my clinic — I am the only clinician who accepts obesity referrals — who carried her tummy in a modified shopping trolley. That lady cannot work because of her weight: her mobility and her social interaction are compromised — she is 52 years old. We need specialist clinics and services for such people — their lives are blighted. Suggesting that we ignore the problem, or just treat people’s blood pressure, is not dealing with the fundamental morbidity of what is an enormous social and personal problem. We must tackle it at a social, educational and individual level.
461. There should be adult obesity clinics to specifically target patients who fall through the community-level and primary-care-level filters, because cases involving overweight or obese people are silting up the vast majority of clinics in hospitals and GP practices. We need somewhere for those patients to go, so that they can receive the expert treatment and intervention that they require. The cost of not doing that will eventually be much greater than the cost of doing it.
462. The Surgeon General of the United States commented that this is the first generation of Americans whose life expectancy is less than that of their parents, specifically because of the obesity problem. An obese teenager is likely to be a cardio-vascular invalid in his or her 40s. We must do something about that problem as a matter of urgency, and that tone is reflected in the literature, which describes a tsunami of obesity.
463. When I was training, type 2 diabetes was called “maturity-onset diabetes". Nowadays, I see 18 and 19-year-old people with that condition, and paediatricians are seeing it in the under 16s. That was unheard of. All I can say is that in my view, it is the single biggest health problem facing our community.
464. Dr Deeny: Thank you, Michael. I am sorry that I missed the start of your presentation. As a GP, I am very concerned about obesity. I have two quick questions about the problem. First, I have my doubts about the BMI. One of the measurements is a waist-to-hip ratio. Last week, we saw the wonderful victory in Cardiff. Many of the guys who played in that rugby team would certainly have a BMI that, according to the charts in a GP’s surgery, would be classed as obese, yet they are big, strong and physical guys. I wonder whether the BMI needs to be discounted and replaced with a better measure of obesity. Some of those rugby guys are 18 stone and are built like the side of a house — they could run through you.
465. Secondly, as a doctor, I too think that it is our duty to get the message out and make it clear that this is a major epidemic that will have serious health consequences for the next generation, and those that follow, if it is not addressed.
466. As I said before, I am worried that we are perhaps going to extremes in being too alarmist. I say that for two reasons. You mentioned that, for about half of certain cancers in post-menopausal women, there is a link between obesity and cancer, and that is what made me ask the question. I was delayed because I had a surgery this morning. I called with a patient who is worried about cancer. Unless a statement such as yours is made more accurate — explaining how great the link is, as opposed to simply saying that there is a link — we are in danger of worrying a significant section of the population who are already starting to worry about cancer, particularly if there is a family history of it.
467. I will give you another example, which I mentioned a few weeks ago. There is an advertisement on the radio and on television, which is perhaps another example of going a little bit too far and almost terrifying people to force them to live a certain way. The advertisement is to do with breast cancer and drinking, and there is no doubt that there is a link there. However, that advertisement worries me. It shows a lady drinking and the drink going down the oesophagus, which is fair enough. It then states that drinking within the normal limits can reduce the risk of cancer. To me, listening to that, it sends out the message that even drinking sensibly and normally is associated with a link to breast cancer. On the one hand, people are being told that if they stick to the normal weekly units of alcohol — 14 units for women, 21 units for men — that that can have beneficial effects on health. Now we are hearing that if you stick within those limits, it will not get rid of you chances of breast cancer, it will only reduce them.
468. I am talking as someone who has been in general practice for some years. For doctors, and all medical people, getting the message out there to the community, strong and clear, is of absolute importance. However, I fear that we are going to extremes and terrifying people. Perhaps sometimes we get the wrong message across. Can you quantify the link between post-menopausal women who are obese and cancer?
469. Dr Ryan: There was a recent editorial in the ‘British Medical Journal’ (BMJ) on that very topic, which stated that: “Among postmenopausal women in the UK, 5% of all cancers (about 6,000 annually) are attributable to being overweight or obese. For endometrial cancer and adenocarcinoma of the oesophagus...half of all cases in postmenopausal women are attributable to overweight and obesity."
470. I did not make that up. That is from the ‘BMJ’.
471. I accept that the BMI is an imperfect measure. I have been waiting for 20 years for the perfect measure. The difficulty is that meanwhile, patients are dying. We cannot wait for the perfect measure; however, I accept that the body mass index is not the ideal. You are quite right; it is a different kettle of fish if muscle weight is a contributory factor. However, at least it would sift out, on an epidemiological or population basis, those patients who might be targeted for lifestyle intervention.
472. In the literature on the issue, there is absolutely no doubt that the lighter that a person is — within reason — the longer he or she will live. I am convinced of that connection, and there is vast evidence to support it. Actuarial statistics from insurance companies will bear that out forcibly.
473. I have presented one or two of the best slides to show that even being moderately overweight will compromise life expectancy. I stand by that assertion. I accept that patients may not worry about losing two or three years from their lives, but that has the same effect on mortality of the whole population as all the cancers put together. To get the weight message into context, the Americans have a great phrase — “the soft stuff is the hard stuff". Blood pressure is a plug and play; someone takes the tablets, and it goes away. Cholesterol is also easy to address. However, obesity is a much more tenacious and difficult problem. I can understand why we do not have a simple solution to obesity, but that does not mean that we can afford to ignore the problem — the cost of ignoring the problem will be enormous.
474. Dr Deeny: I do not want to ignore the problem, but we must get across a message that is as accurate as possible. For example, I am concerned that the message about menopausal women will worry people more and affect their mental health. People who are obese and post-menopausal will read that message and think that they have a 50% chance of getting cancer. That is my concern.
475. Dr Ryan: Knowledge is power. In my clinical practice, I use that type of knowledge all the time — the more that a patient knows about his or her condition, the more he or she is empowered to deal with it. In no situation is that more important than in a lifestyle-related problem. If a lady is obese and concerned about her cancer risk, perhaps she will be motivated to do something about it. There are very few cancers that people can address by changing their lifestyles. If a lady loses 10% of her weight, she will reduce her risk of obesity-related cancers by 40%. That is the epidemiological return on weight loss, which is well worth it. There are some serious threats to health, and putting the minds of patients at ease is important. However, it is equally important to give patients the hard and cold facts, and the literature on the issue supports that.
476. Ms S Ramsey: I do not know whether I should thank you for your presentation. I am sitting here thinking that maybe I should just go home, go to bed and give up the ghost, because what I have heard is depressing. I agree that knowledge is power, but responsibility comes with that power.
477. In your presentation, you mentioned the importance of mindsets and attitudes in how we deal with the problem. Some people say that a sizeable percentage of those who suffer from obesity, some forms of cancer and diabetes come from socially deprived areas. That is an issue that we need to talk about. We also need to address the problem early, which means that we need to invest in schools.
478. Alex Easton said that food producers and manufacturers need to examine their ingredients, but we are not investing in school meals. A large percentage of the children who receive school meals come from socially deprived areas, and they are getting food that will create problems for them later in life. If we are going to be honest, we need to be brutally honest and admit that we — as a society and as the people who are supposed to be in charge — are feeding the problem; pardon the pun.
479. We also need to invest more in after-schools programmes, whether those are for recreation or study. The Assembly has debated the issue of whose responsibility it is to fund after-schools programmes. One Minister and Department are fighting with another Minister and Department, and the issue of neighbourhood renewal is getting lost because of that. Therefore, we need to be brutally honest about that.
480. Education is the key. We need to be honest about the advertisement and sponsorship of big events. A number of years ago, cigarette companies advertised at events, then it was the alcohol companies, and now it is either big fast-food companies or soft-drinks companies. We need to be clear about that.
481. Do you believe that other Departments and Ministers are playing an active role in trying to deal with and tackle this issue? A number of weeks ago, officials from the Department of Health, Social Services and Public Safety told us what they will do. However, we, as a Committee, have no control over the Department of Education, the Department for Social Development (DSD), or the Office of the First Minister and deputy First Minister (OFMDFM). I want you to be honest, because we need to tackle this issue as a collective problem. Do the Executive have a collective responsibility and mindset to deal with the issue of obesity?
482. Dr Ryan: That is a difficult question for me to answer. I do not know what is going on in the Executive. I am simply addressing the issue from my perspective as a practising clinician. I see more and more patients with a primary problem that I have no authority to help them with; I have no means to help them. Obesity is a problem that I should and could help them with if I had the time. In running a diabetes clinic, I have an obligation to my employer to see diabetes as the primary focus. Although I do address all the other issues as best I can, obesity is such an intractable and deep-rooted problem that it needs specific, targeted intervention.
483. Obesity is a health issue; an education issue; a social policy issue; and a public transport issue. I agree with you, I do not know who should pay for this. All I know is that there are consequences that have yet to be realised. The difficulty is that I do not see the evidence to suggest that the provision of school meals produces fitter, lighter, healthier, smarter children with a longer life expectancy.
484. My primary measurement is death. If I intervene to help patients, I must be satisfied that there is evidence to show that they will live longer. That is my only justification for adding chemicals to their mix or for instructing, advising or guiding them to change their lifestyle. My concern is that resources are being expended and that there is no overarching infrastructure to weigh those in the balance in order to ascertain whether they are producing value for money.
485. Ms S Ramsey: First, forget about the evidence about the value of schools meals. School meals are being provided, so we should ensure that those are of the highest standard. Secondly, I know loads of people who would love to be able to afford to buy free-range chicken. I use this example to show why people get caught in the trap. A free-range chicken can cost £8, £9 or £10; whereas a processed chicken costs approximately £2. Although we need to change the people’s attitude to food and lifestyle, we also need to ensure that they are able access healthier produce.
486. Dr Ryan: I agree, but I do not know of any evidence to show that free-range chickens are any more nutritionally beneficial than processed chickens.
487. Ms S Ramsey: We are led to believe that they are.
488. Dr Ryan: If I were selling free-range chickens, I would lead you to believe that, too.
489. Mr Buchanan: In your opening remarks, you mentioned the Counterweight programme in Scotland. How long has that been in operation, and how has it been evaluated? How much would it cost to set up a similar programme in Northern Ireland? Finally, how long would it take to roll out such a programme across all the health board areas?
490. Dr Ryan: The Counterweight programme in Scotland is primary-care based and provides specifically trained staff to deal with obesity. It is rigorously evaluated by the University of York and the University of Aberdeen. Counterweight has produced credible evidence of the cost-effectiveness of that type of programme.
491. To implement a similar programme region-wide would require a significant amount of priming money, but that would be recouped through a reduction in drug costs, reduced levels of diabetes, fewer hospital admissions, and so forth. I can only hazard a guess that to roll out such a programme across the Province may cost approximately £500,000 a year for the first two or three years.
492. The Deputy Chairperson: Dr Ryan, thank you for coming today. Your evidence has been most helpful to the Committee, and I will ensure that you receive a copy of the final report.
2 April 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Ms Claire McGill
Witnesses:
Ms Tracy Gibbs |
College of Occupational Therapists |
|
Ms Pauline Mulholland |
British Dietetic Association |
|
Ms Teresa Ross |
Chartered Society of Physiotherapy |
493. The Deputy Chairperson (Mrs O’Neill): I welcome Ms Pauline Mulholland, a board member of the British Dietetic Association (BDA); Ms Tracey Gibbs, chairperson of the College of Occupational Therapists (COT); and Ms Teresa Ross from the Chartered Society of Physiotherapy (CSP). I invite you to make your presentation, after which members will have an opportunity to ask questions.
494. Ms Pauline Mulholland (British Dietetic Association): I thank the Committee for giving us the opportunity to present allied health professionals’ views on tackling obesity.
495. The Committee’s inquiry is timely, given the new healthcare arrangements and organisations that came into being yesterday. It also gives allied health professionals the opportunity to make a more co-ordinated and robust contribution, not only to tackling obesity, but to addressing a range of related long-term conditions.
496. On behalf of the British Dietetic Association, I alert the Committee to the fact that dieticians are uniquely qualified health professionals, which is demonstrated in the way in which they assess, diagnose and treat individuals and the wider public with problems that are related to diet and nutrition. Dieticians make a singular contribution to the prevention and management of obesity at all levels.
497. At regional level, we feel that we can contribute by working with strategic groups in overseeing the development and implementation of a policy on obesity. To date, we have not had the opportunity to do such work; we are involved only at the lower levels of strategy development and would therefore welcome the opportunity to contribute at a higher level. On the subject of commissioning, we can contribute to the design of services to meet patients’ dietary and nutritional needs. We lead on the implementation of obesity and food-guidance policies in local trusts and in education. We support individual patients in the management of clinical obesity, and we also work with communities and voluntary groups on prevention. That is where local people can make the changes necessary that are to tackle the issue.
498. In our written submission we provided the Committee with a range of examples of preventative measures. We also provided to the Committee a recent British Dietetic Association leaflet outlining the contribution that dieticians can make. Some examples in Northern Ireland are the Cook It! programmes, which are run throughout the Province, the FRESH programme, which is for young adolescents with obesity in north and west Belfast, and Bank Your Smile, which is an oral health project in the west. Those initiatives are designed to deliver the Investing for Health strategy and the Fit Futures strategy in the Province.
499. The British Dietetic Association considers that the new Regional Agency for Public Health and Social Well-being provides the opportunity to evaluate such schemes across Northern Ireland and to decide which of them to commission to create the best outcomes for the public. For maximum impact, we would like those schemes to be embedded in core services across Northern Ireland.
500. We are engaged in joined-up working with many other agencies. That is because people other than dieticians have a role to play. We work with education providers, local councils and environmental health officers. We also work with local leisure centres and other bodies that provide physical activity programmes in support of tackling obesity. We established a range of schemes in schools, but given the fact that one meal a day is eaten at school, we must build on those. We must ask what happens with parents and children beyond the school hours.
501. One of our key roles is the management of clinical obesity, which is a challenge for individuals and professionals. People aspire to lose a significant amount of weight over a short period, and sometimes that puts them off accessing our services. We need to manage such expectations and promote the message that if individuals can be encouraged to lose 10% of their weight and to maintain that weight loss, they can achieve significant health benefits. The evidence shows that a 10% weight loss will reduce blood pressure and cholesterol, improve the control of blood sugar for people with diabetes, and reduce the death rates for a number of conditions. As a result, we may be able to reduce the number of drugs that such patients have to take, thereby reducing public expenditure.
502. The outcomes from intensive weight-management programmes across Northern Ireland have been well recorded, and we have several examples. Those outcomes are achieved through a combination of dietary advice, exercise and techniques to change behaviour. Thus we aim to alter an individual’s entire lifestyle and to maintain that change in the long term. We do so using supportive practical approaches, such as cookery demonstrations and supermarket tours. That is because people need to get not only advice, but the skills to put that advice into practice.
503. In order to deliver on the significant agenda of challenging obesity in Northern Ireland, we would like it to be recognised as a disease in its own right. We would also like a regional obesity framework to be established to support the delivery of the agenda across the Province. The Department of Health, Social Services and Public Safety and other Departments can lead by example by implementing schemes that teach people about healthy nutrition in the workplace, for instance. There are many examples of that type of scheme across the UK. Of particular note is a scheme in Wales, through which the Minister of Health and Social Care implemented a charter for vending in healthcare facilities. Our challenge is to extend that throughout the public sector in Northern Ireland, thereby improving individuals’ workplace choices.
504. Ms Tracey Gibbs (College of Occupational Therapists): Thank you very much. I am delighted to be able to speak to the Committee on behalf of the College of Occupational Therapists.
505. I will discuss a number of the key areas that we identified in our document. Obesity is a significant issue for the many different groups of people with which we work. That includes people of all age ranges in acute-hospital settings and in their community environments and people who suffer from chronic conditions and other co-morbidities that are often associated with obesity. Other groups of people with which we deal include those with mental-health problems and learning disabilities. We also work with wheelchair users, particularly children and younger people.
506. Occupational therapists (OTs) in Northern Ireland have identified an increased need for specialised bariatric equipment, and we outlined some implications of that need in our written submission. Bariatrics is the science of providing healthcare for our heavier population. On a day-to-day basis, that has major implications for transporting patients in hospital beds, the use of hoists and porters’ chairs, and for the use of seating in hospitals and in the patient’s home. Addressing the need for specialised equipment for that client group is a major challenge that faces therapists.
507. Although there is a lot of emphasis on the global epidemic of obesity, it is also important to consider the needs of the obese person. It must be ensured that they are treated with respect and dignity and that stigma and discrimination are avoided. A person who is overweight may feel socially isolated or excluded. Their role as a caregiver, as a spouse or as a child, for example, may be affected. As a result, occupational therapists consider the ability of the overweight person to look after themselves and their ability to function in their own environment. Very often, activities of daily life may be affected.
508. Occupational therapists feel that it is important to address this issue from a preventative, health-promoting perspective. It is also important to help people cope with the symptoms or results of their condition and to prevent further problems. Investment should be provided so that preventative programmes that incorporate health-promotion and lifestyle-management strategies can be delivered to address the broad spectrum of issues among all clients across all age ranges.
509. A co-ordinated, all-systems approach to tackling the issue is necessary. There should be a national service framework for the treatment of obesity. Meaningful activities could be used as intervention. For example, people should be encouraged to become involved in activities that they enjoy, such as gardening or dancing, so that their mind and interests can be engaged. Ultimately, exercise on prescription should be broadened to include activity on prescription.
510. It is important that the home and general environment is accessible to people who are overweight or obese so that their problems are not compounded by being housebound, which can lead to further inactivity. Community integration should be encouraged to increase self-esteem. People will be motivated to maintain and improve their functional independence. That is particularly important for schoolchildren; it must be ensured that their schools, respite facilities and day-care facilities have the appropriate environmental design.
511. Occupational therapists endorse the concept of inclusive environmental design that considers the needs of all users, including those with obesity. We can provide expert opinion for that client group on equipment, environmental housing design, caregivers’ needs, lifestyle management and mental-health issues.
512. Overall, we recognise the challenges of our increasing obese population in Northern Ireland. However, we feel that further investment is essential across all our allied health professions so that equity for all can be delivered.
513. Ms Teresa Ross (Chartered Society of Physiotherapy): I want to highlight the role that physiotherapy, along with the other allied health professions, plays in the management and prevention of obesity. The Clinical Resource Efficiency Support Team (CREST) guidelines point towards secondary care, but the management of obesity involves primary care and secondary care. It is a healthcare issue that concerns the whole population, not just one element of it.
514. Physiotherapists have the skills and expertise to assess and allow people to take part in exercise programmes and to undertake exercise prescription. Some of our work involves people with type 2 diabetes and people with musculoskeletal disorders, such as people with muscular sclerosis or neurological conditions that mean that they may be confined to a wheelchair. That means that one must look at other ways of allowing them to exercise, because they will not be able to go to a gym or take part in group exercise. Exercises must be modified to allow those people to have some kind of physical activity that will help to prevent secondary ill-health problems that can result from poor fitness levels. Such conditions include cardiovascular disease and stroke, and there are others.
515. From a physiotherapy point of view, exercise is important for a person’s well-being and self-esteem because the whole person is being treated. It is important to improve a person’s self-belief and self-esteem and allow them to have the confidence to take part in exercise. Exercise programmes have moved into leisure centres across the region. Those programmes are not just for people receiving primary care; they are for children and for those with an adult learning disability or a physical disability. People can go along and get introduced to exercise, take part, and then start doing those exercises themselves. However, some people are afraid to go into an environment where there are machines and equipment. The physiotherapist helps them to become accommodated safely into that environment, and our Over to You scheme allows people to take control of their own health and well-being. That is an important part of a physiotherapist’s role. Exercise is not something that physiotherapists can do to people; they must take control of it themselves.
516. Part of our job is to introduce patients to other environments. Obesity is a community issue and a population issue. It is not a health issue alone. It is a full-partnership issue; therefore, it is important to use all the partnerships that we can to help us to deal with obesity.
517. We must look at other ways of exercising. My colleagues mentioned dancing, walking, running, boccia and bowls. There are all kinds of exercises, and it is a matter of introducing people to them.
518. We take a person-centred approach. Although people may be referred with a sore back or a broken leg, ultimately, the whole person has to be managed. They may become inactive as a result of their condition, which may cause them to become overweight. That, in turn, may cause them to lose their self-esteem and their feelings of self-worth. It is important that behaviour be modified and that the person be built up in such care settings as successfully as possible.
519. Through the projects that we have run in primary and secondary prevention, we have found that the partnership that is involved is huge and that it must be developed. One cannot just treat the individual in question; everyone, including family, friends and neighbours must also become involved to allow for the peer support that people need to allow them to manage their problem.
520. Ms Gibbs mentioned manual handling. The Chartered Society of Physiotherapy leads a lot of the manual handling training for Health Service staff, including nurses, medics, allied health professionals and social workers. People are trained in how to manage obese patients safely, and that training then allows them to have the equipment and techniques in place.
521. Whenever obese patients are admitted to hospital, the theatres or X-ray departments may not be designed properly to deal with them. Physiotherapists advise on how to set up a department and manage the equipment and to have the necessary equipment in place or contracts available for bariatric patients to be well looked after.
522. The CREST guidelines of 2005 refer to the role of physiotherapy and the advice on exercise to enable people to manage obesity and to become fit. Of the people who present at physiotherapy departments, 20% do so for reasons other than being obese. However, that leaves us in a prime position to educate, train, advise and empower those people to look after their own lifestyles. Ultimately, a lot of the issue concerns a change in lifestyle and thinking.
523. A lot of schemes that have been run from a physiotherapy, allied health professional and multidisciplinary point of view have been funded by the Big Lottery Fund or by some other short-term grant. That has been a difficulty, because although the scheme may run for three years and be proven, it may then not get permanent funding. It is important that we influence that.
524. The incidence of falls is another factor that has an impact. I know that a lot of work is being done on falls, osteoporosis and other conditions. However, an obese person’s muscles become weaker — their muscle tone lessens and their balance reduces; therefore, the risk of falls or of osteoporosis from not doing weight-bearing exercises is increased. It is important that people’s lifestyles incorporate physical activity. That involves the entire community and every possible partner having an educational role.
525. Under the old arrangements, physical-activity forums considered the health and well-being of the population. They looked at deprivation and other issues and encouraged a multidisciplinary or multi-agency approach to the management of obesity. Allied health professionals are well placed to help and to influence that work in the future.
526. Ms Mulholland: In summary, we hope that the examples that we provided help the Committee to recognise the significant contribution that allied health professions can make to the prevention and management of obesity. We look forward to working with many groups and agencies to deliver on that significant task. Again, we thank the Committee for giving us the opportunity to present our evidence.
527. The Deputy Chairperson: Thank you very much Pauline, and thank you all for your contributions. The Committee recognises the key role that you play.
528. With the launch of the new Regional Agency for Public Health and Social Well-being yesterday, what do you consider to be the potential role that local commissioning groups (LCGs) and the agency itself can have in addressing health inequalities in general, but, in this case, obesity in particular? Obviously, that agency now has a key role in health prevention, promotion and education. Do you have any views on that?
529. Ms T Ross: We welcome as really important the involvement of the new authority, the LCGs and the membership of the local government agencies in the new structure. As a chair of the local health and social care group (LHSCG) in the Southern Trust, I know that the relationship with local councils and other local partnerships was key to our being able to commission services that helped meet population needs — it allowed us to make decisions on the most focused investment that would achieve the best impact on a population.
530. Therefore, the new agencies provide a positive forum for us to build upon. Their involvement in local communities will be a good influence, and the involvement of local council representatives will help to build a better future.
531. The Deputy Chairperson: There will be an increase in leisure opportunities, which comes back to that multi-agency approach.
532. Ms Mulholland: The point is to combine the best examples of what has worked across the region and to roll them out in the mainstream. At the same time, we must consider what has been tried and tested and what fits with a particular local community, because all communities are different. It is about what the people in those communities and voluntary groups think will work and what they are happy to engage with so that the desired outcomes can be achieved.
533. Ms T Ross: The other point to make about leisure opportunities is that it is really important that the rules, and an open approach, are standardised. Some of our examples show that a partnership with the providers of leisure facilities on issues of costs and other matters can be built more easily in some places than in others. A common approach would be good, because it would to allow for healthy activities to move into other arenas.
534. Mr Gardiner: Tracey, as a representative of occupational therapists, how do you deal with obese people who have a mental illness or a learning difficulty?
535. Ms Gibbs: That is certainly a challenge for those therapists who work in front line services. For example, patients with mental-health difficulties have usually been attending occupational-therapy services for a number of years, and it is important to engage them in a specific, tailored and therapeutic activity programme to gradually reintegrate them into the community. That is done by identifying their hobbies and interests, trying to regenerate their ability to become involved in leisure activities and, ultimately, participation in the recently established condition-management programmes, through which occupational therapists try to enable people to get back into work through vocational rehabilitation.
536. Therefore, we deal with such patients through a range of programmes that involve both individual and group work. Occupational therapists have been working with folk who have mental-health disorders and have been trying to overcome the issue of obesity and the problems that it causes.
537. In addition, from a learning-disability viewpoint, an increasing problem for occupational therapists is the use of equipment, and wheelchair sizes in particular reflect that. Our population is possibly getting more overweight — obese — which results in challenges in sourcing the most suitable wheelchair for a patient to ensure that it fits into his or her day-care centre, respite facility and home environment. Along with our physiotherapy and dietetic colleagues, we try to address the huge implications of obesity and to ensure that the home life, work life or school life of a patient is as manageable and independent as possible. That is achieved through individually tailored activity-based programmes, correct supply and prescription of equipment, close monitoring of a patient at home, and very close liaison with teachers, care givers and the whole carers’ network.
538. Mr Gardiner: What percentage of the patients that you treat have a mental illness or a learning difficulty?
539. Ms Gibbs: I work in an acute hospital and deal with physical disabilities, so I cannot give you the exact percentage offhand. However, I can source that information for you.
540. Ms Mulholland: Allied health professionals know that occupational therapy is the most recognised therapy for mental-health and adult disability. Therefore, a much higher proportion of occupational therapists work with clients who have mental-health problems.
541. The Deputy Chairperson: Can I clarify whether allied health professionals are represented on the obesity steering group?
542. Ms Mulholland: No, they are not. One of our recommendations is that allied health professionals should contribute to that group’s work. We are involved, but not directly; one of our colleagues managed to be nominated by her trust to one of the subcommittees and has introduced the idea that it is important to have dieticians represented on the group. We have managed to get a dietician on the food and nutrition subgroup; the British Dietetic Association was not invited to sit on the food and nutrition subgroup, even though such matters are our core business and we are the only professionals in the healthcare system who are regulated to act on those issues. We have a role to play on the obesity prevention steering group.
543. The Deputy Chairperson: I think that Committee members would agree with that point; I certainly do. As I said at the start of the meeting, you have a key role to play. That might feed into our recommendations.
544. Ms Mulholland: I plan to send a letter to the chairperson of the subgroup asking whether they would like us to contribute.
545. Dr Deeny: Ladies, I thank you for appearing before the Committee. As a doctor, I think that it is vital that you should be a representative of allied health professionals on the steering group. I should know this, but could you remind me of whether there will be two allied health professionals on each local commissioning group?
546. Ms Mulholland: As far as I know, there will be only one representative for a minimal amount of time — approximately one or two days a month.
547. Dr Deeny: I want to focus on the prevention of illness through exercise. Everybody is talking about that, and it is a multi-agency, cross-departmental issue. As a community physician and a GP, I want the education sector to be involved, and I am glad that councils are involved. Tracey mentioned environmental design. As an OT, what practical measures do you think could be taken to help facilitate people’s exercising in their own homes? How can we facilitate that environmental design in order to tackle the epidemic of obesity?
548. Last week, the Committee Clerk gave me a document that shows that GPs in the Belfast Health and Social Care Trust can prescribe leisure centre activity to patients. Although there was an arrangement in the west at one stage, GPs in the Western Board and other areas cannot prescribe in that way, and we must address that matter. Rather than wait until people get sick, if we are serious about real health promotion and disease prevention in the future, it is important that we establish a facility whereby GPs can use methods other than prescribing drugs in order to help people to lose weight.
549. As a GP, I want to be able to access patients whom I consider to be morbidly obese and whose health is threatened. Why should I be unable to prescribe physical activity as opposed to drugs, which are much more expensive? That is how we should progress. I was shocked by the document that the Committee Clerk gave me last week. I was pleasantly surprised to find that GPs in some parts of Northern Ireland refer patients to leisure centres. However, that does not happen in other parts.
550. Ms T Ross: I know that GPs in the Southern Trust prescribe exercise. They refer patients directly to leisure centres. Thereafter, the fitness instructor and the physiotherapist in a leisure centre work in partnership to assess the patient and set up an individual programme for them. The fitness instructor then takes control of the exercise programme. However, the fitness instructors require some training.
551. That would definitely be a positive way to progress and would allow the health system to target people who are at risk of ill health, as opposed to those who are actually ill. Therefore, it is important to develop the idea of prescribing exercise, and it should be rolled out.
552. Dr Deeny: The Committee Clerk has just handed me a document about the pre-fitness GP referral scheme. It is 12-week scheme that is similar to other UK schemes, and it operates in conjunction with the Eastern Health and Social Services Board’s Healthwise scheme. It is co-ordinated by the GP referral officer at a fitness centre. I think that such schemes are part of the future of healthcare and the prevention of illness.
553. Pauline is correct: such schemes will identify people who are perhaps a year or two away from a major health event or illness. Diabetes is already visible in young people in primary care. It used to be called maturity onset diabetes, but it can occur at any age, so it is now known as type 2 diabetes. Given that, such schemes must be a major part of our health strategy for the future, and we need to push access to them. We perhaps need to reach a point at which nurses can prescribe exercise, after having consulted with GPs and identified those patients that should be referred to leisure centres.
554. Ms Mulholland: That is one opportunity that the new Regional Agency for Public Health and Social Well-being will create. For example, how do we find out what is going on in different parts of the Province? Many schemes have been introduced in patches, and the Healthwise scheme in the Eastern Board area — where I am from — has been running for some time. I think that it was, perhaps, established on the back of Big Lottery funding. Several health-prevention schemes have received Big Lottery funding, but they did not receive the mainstream funding that would have enabled their benefits to be rolled out.
555. The Cook It! programmes, which promote healthy cooking, are one example of an environmental scheme. They are funded by the Big Lottery Fund across the Province and have received mainstream funding in two trust areas. However, in others trust areas, they have not received such funding. Therefore, some of our population has access to absolutely fabulous programmes that work and that have been evaluated, but those programmes do not exist in other areas. That inequity must be addressed, and the introduction of our new structures and way of doing business will provide an opportunity of which we must take advantage.
556. Ms Gibbs: With respect to environmental issues, our colleague Padraig O’Brien is working with the Housing Executive. However, occupational therapy needs more resources and more specialist knowledge of housing issues. In Northern Ireland, there is just one occupational therapist who is a clinical specialist in housing. Presently, he happens to work in the Northern Trust.
557. With such a person in place, specific research can be carried out in, for example, evidence-based practice, enabling us to prove which equipment is the most effective and efficient by trying out various devices in peoples’ homes. In different trusts, various waiting lists exist, and an assortment of equipment is being issued. Therefore, the range of equipment that is fit for purpose, research based and most efficiently costed must be streamlined.
558. Another way to move forward would be to have dedicated occupational therapists working specifically in housing. Other essential groups with which we must work and have closer links include housing authorities, the Housing Executive, the private sector, local schools and special schools. In addition, we must consider the whole area of risk management and become more environmentally efficient by devising practice standards in communities that ensure that any equipment that is to be recommended and prescribed is the best that we can deliver.
559. Dr Deeny: My question could apply equally to physiotherapists. There are not enough occupational therapists, who play a vital role in health and community care. Will you provide the Committee with statistics outlining how many OTs are in each of the five trust areas?
560. Ms Gibbs: Yes.
561. Dr Deeny: Could you also provide the Committee with the college’s estimate of how many OTs each trust should have? Most of us would agree that —
562. Ms Gibbs: There are 770 qualified professional occupational therapists in Northern Ireland, and the College of Occupational Therapists has 27,000 to 28,000 members. There are probably more than 200 occupational therapists in the Belfast Trust, approximately 120 in the Western Trust, and the remainder are dispersed among the other trusts. However, I can submit precise and up-to-date figures.
563. Dr Deeny: I would appreciate that. How many OTs does the college suggest that there should be in Northern Ireland?
564. Ms Gibbs: We have just submitted a response to workforce planning in the College of Occupational Therapists. The recommended numbers for each person in the population is much higher than the present numbers, but I can get the specific figures from our policy officer for Northern Ireland and forward them to you.
565. Mr Gallagher: I am glad to hear that there are so many OTs in the west of the Province; however, there appear to be few in places such as Fermanagh. That is an ongoing problem, but it is not for you to deal with today. Nevertheless, it will be interesting to see the figures when they come through.
566. You talked about the important role that dieticians must play. In addition, the British Dietetic Association mentions both the importance of having highly trained professionals and the need for support — including financial support — for them. Given that we must pay more attention to the problem of obesity, can you give us some idea of the position with respect to the population of Northern Ireland? Do you feel that we have enough well-trained professionals to work in that sphere?
567. Ms Mulholland: All the areas of work in which we are involved are regulated professions, and we are all regulated by the Health Professions Council.
568. Mr Gallagher: Does that include experts in diet?
569. Ms Mulholland: Yes, dieticians are regulated by the Health Professions Council. We are all graduates who have had to go through a training programme. We face challenges, in that others who are not regulated and trained in that way provide dietary messages that are not consistent with evidence-based practice. Being called a dietician is a protected title for all those who work in that area. Therefore, if you call yourself a dietician, you have to be regulated by Health Professions Council.
570. We recognise that there are limits to the number of dieticians in the Province. We are in a difficult position in healthcare, and we are all aware of the budgets. We recognise that we need more dieticians. We are working with the Department of Health’s service delivery unit to look at new access criteria with regard to waiting-list management. One criterion that we have set is that we would accept referrals from any health professional for a patient who has a body mass index that is greater than 30, which is clinically obese. The capacity is not there for us to deliver on that, so that is a challenge, and we would like to raise that issue with health commissioners and have that criterion accepted.
571. However, we have to be honest and say that dieticians are not the only ones who work in that way; our nursing and medical colleagues, GPs and practice nurses are all key and have their own messages to give. As a profession, we also work with commercial slimming companies. With regard to Dr Deeny’s point about exercise on prescription, there are examples in England of people’s being given access to weight loss on prescription. There needs to be a way to validate and ensure that commercial companies are reputable and that they follow evidence-based work.
572. To answer the question, we would honestly have to say that we do not have enough dieticians. We would want to have more highly specialised dieticians to look at prevention strategies. We can lead on those strategies and work with others to deliver them, because our expertise is in setting up the mechanisms. We work with community groups to deliver those strategies, and we do so very much on the clinical specialist side
573. One of our big challenges is that the majority of people who come to dieticians with clinical problems of obesity come with other medical conditions that need to be considered, such as diabetes and heart disease. The issue is not necessarily about just healthy eating; other dietary complications need to be managed.
574. The Deputy Chairperson: Your paper refers to the role of a consultant dietician and support workers.
575. Ms Mulholland: There are a number of consultant dieticians working on obesity in England. That is a new role, and those consultants are highly specialised. They exist for all the allied health professions. It is a growing area. However, we do not have any consultant dieticians leading on obesity in Northern Ireland. Their roles are split 50/50 between research and practice, and they are very much looking at undertaking research in the population and providing advice on strategy, development and clinical practice for all dieticians — potentially across the Province, if such a post existed.
576. On the other side of the scale — which fits in with the recommendations in the priorities for action to look at the distribution of unqualified healthcare workers to qualified colleagues — we have dietetic assistants, and the other professions have comparable assistants.
577. That is a new and growing role in dietetics in Northern Ireland, and the key things that dietetic assistants can do for we dieticians is to translate the messages that we give to patients into real-life actions for them and to support them to understand those messages. For example, we have looked at providing dietary advice on obesity to individuals or groups. A dietetic assistant could then take a group of patients to a supermarket and show them how to read labels, which they might have done in practice. They can take a product off the shelf — for example, margarines and spreads — and point out the differences between them.
578. Therefore, the point is to translate the message into practice, because so many messages are very confusing. When you go to the supermarket, you need to know which is the low-fat product and which has sugar and which does not. Are low-sugar biscuits OK? No, they are not, because the sugar has been taken out and fat has been added, making them worse than the standard product. That is the role of the dietetic assistant — they take those messages, translate them and make them live for individuals.
579. Mr Buchanan: Thank you for appearing before the Committee today. No doubt, if we want to tackle obesity, a multi-agency approach has to be taken in order to take it on and do something about it.
580. Throughout your presentation, you talked about the issues that are key to tackling obesity. Exercise and education are crucial, as are education and peer support for people who participate in some of those activities. How do you encourage people to participate in exercise, leisure, or in the programmes that you talked about that are being put in place? How do you encourage people who are in the obese category to participate in exercise to seek to reduce their weight and to make themselves healthier?
581. What work do you do with young people in schools or colleges to seek to get the message across that obesity is a serious problem and is something that everyone has to consider? How do you measure the results? I am sure that in your profession you deal regularly with many obese people. How do you measure the results of the programmes that you have in place to ensure that they are having an effect on the people with whom you are dealing?
582. Ms T Ross: From a physiotherapy point of view, we work across all the programmes of care, which means that we work with adults with learning disabilities, with children, with people who have physical disabilities, and with people in primary-care settings. Therefore, in all those fields, there is an opportunity to influence those people to take part in exercise.
583. For some people, it is about looking at what they can do in their own environment. A lot of it is to do with motivation, with trying to get people to change their mindsets and getting them interested in exercise, as well as trying to talk to them to find out what they like to do. We can prescribe exercise, but unless it links to people’s lifestyles, their family environments, or getting support from their families, they may not continue with it.
584. In mainstream schools, we have a programme for obese children, and the biggest success was when the parents, children and their siblings came to the programme together, took part in exercise and got advice on diet and exercise. It was a learning curve, and at the end of the 12 weeks — and even when we reviewed it a year later — they were sustaining the programme because they were supporting one another.
585. The change in the individual family’s self-esteem and confidence has been really evident with some of the schemes that we have run for adults with learning disabilities. There are issues around obesity and being overweight and accessing leisure and community groups and sporting teams. However, through physical-activity forums, we work in partnership with education providers, local football clubs, hockey clubs, and so on. Therefore, we are taking a community-based approach to the issue.
586. We assess people’s ability to take part in exercise or fitness regimes. We assess the risks that are involved and devise a programme that fits in with those and with their lifestyle. Therefore, it is important to know what someone is interested in and to find out where they can avail themselves of that activity. We can widen the whole partnership to include community development, local councils, and sports organisations. The impact that it has is very good.
587. We can weigh people, test their blood pressure and cholesterol and monitor all those things, but the greatest effect is on people’s confidence, well-being and self-esteem. If people go for a walk, join a walking club, go dancing, or even go out, their whole body image improves greatly and they feel so good that their ability to meet other people and to converse with them also improves. Therefore, such programmes have very beneficial effects on quality of life. People get all the health benefits from having their blood pressure, cholesterol and similar physical elements tested, but they also get improved quality of life and well-being, and their mental health improves. Therefore, the whole family unit and community benefit.
588. Ms Mulholland: There has been a huge campaign to improve nutrition in schools. Standards for the provision of food in schools have been set that have been implemented. One of the most recent developments has been the employment of a dietician in the Health Promotion Agency as a schools’ co-ordinator. Under the aegis of the new regional health agency, she will have a key role across the Province in evaluating how nutritional standards are implemented in schools. Nutrition advisers assess those standards regularly in schools to determine how they are progressing against their targeted tasks. They also give feedback and provide timescales for progress.
589. Ms Gibbs: When it come to measuring the effectiveness of our service, I should point out that occupational therapists cannot always pick up on patients in a physical setting until they present to an acute medical ward with, perhaps, a diabetes-related, arthritic or chest disorder. Those people come in with chronic conditions, and although they happen to be obese, we are unable to intervene — or to know anything about that client group — unless they are given a bed in a medical ward. Very often, we are dealing with compensation and addressing secondary problems. In future, hopefully, with more representation at departmental level and with more strategic guidance, we can employ ways to intervene at an earlier stage and work collaboratively to address the problem upstream rather than downstream, which lessens the effect of intervention.
590. The Deputy Chairperson: That concludes our question-and-answer session. Thank you for your presentation and your submissions to the Committee; they have been very helpful to our inquiry.
23 April 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Witnesses:
Ms Mairead Boohan |
Queen’s University Belfast |
591. The Deputy Chairperson (Mrs O’Neill): Our first evidence session is with Queen’s University Belfast as part of our inquiry into obesity. A submission has been circulated to members, as well as a suggested issues paper.
592. I welcome Professor Frank Kee, the director of the UKCRC Centre of Excellence for Public Health, Dr Michelle McKinley, the principal investigator at the Centre for Public Health; and Ms Mairead Boohan, the deputy director of the Centre for Medical Education. I invite you to make a brief presentation, after which members may have some questions.
593. Professor Frank Kee (Queen’s University Belfast): I have provided Committee members with copies of a PowerPoint presentation, to which I will speak. I want to highlight some areas that the Centre for Public Health is emphasising in its current research strategy on obesity. The strategy focuses on causes, interventions and the way in which we believe that future policy scenarios and their consequences should be monitored, and why we see opportunities opening up that give researchers such as us greater traction with policy-makers and practitioners in the future. I know that the Committee has already taken evidence from a range of bodies, and I appreciate that this problem stretches over the life course and concerns how we live and where we live.
594. Although our own behaviour and the behaviour of cells may ultimately be the final mediator of how fat we become, the challenge for us, as epidemiologists and public health specialists, is to distinguish those proximal causes from the distal causes and work out the best way to improve on prevention of the problem.
595. There is often a needless and contrived tension between two ways to approach this issue: either chasing the tail of the distribution of people who are worst off; or shifting the mean of the distribution. As public health specialists, we usually prefer to try to shift the mean of the entire distribution of risk in the population.
596. In our handout, I point out a strategy that the Department of Health in England launched on 11 February 2009 — ‘Putting Prevention First: Vascular Checks: Risk Assessment and Management Strategy’. The strategy outlines attempts to pick up those most at risk, and the Department of Health is trying to chase those with the heaviest body mass index (BMI).
597. The object is to find the people who are at highest risk and then act to mitigate that risk. That is one method. Before the Department of Health supported that policy, it did some detailed health-economic modelling to ensure that the effort would be justified. At the Northern Ireland Centre of Excellence for Public Health at Queen’s University, and in the UK Clinical Research Network (UKCRN), we are trying to build up the expertise to carry out that type of modelling.
598. I am sure that members have already heard about the Foresight report, which examines the problem of obesity at a societal level. In my PowerPoint presentation, I refer to the futility of isolated initiatives; one might say that that describes the recent document that was produced by the Department of Health. To chase only the people at the tail of the distribution, or other isolated initiatives, will not tackle the problem, and that is not the way that we approach our research into obesity.
599. We have to take account of elements that affect the mean of the distribution and those that affect the worst-off people. The nature of individual behaviours is one way to examine obesity; they are extremely important. Dr McKinley will give members a flavour of a couple of studies that are under way that examine individual behaviours, after which I will make a few comments about the broader societal research that we are undertaking.
600. Dr Michelle McKinley (Queen’s University Belfast): I thank the Committee for the opportunity to present this evidence. I work in the nutrition and metabolism group at Queen’s University, which is directed by Professor Ian Young. I will summarise some of the research that Professor Patrick Johnston mentioned in his letter of 13 March 2009 to the Committee.
601. The nutrition and metabolism group runs several dietary intervention studies, in which we ask people to change one aspect of their diet. We monitor the effect of that change on a variety of factors that are related to risk of disease. I will explain some examples that will give members an idea of the types of studies that we run.
602. The first study examines the effect that increasing the intake of fruit and vegetable has on insulin resistance in people who are overweight or obese. Being overweight is associated with insulin resistance, which means that the body does not respond well to the insulin that it produces. Insulin resistance, in turn, is associated with an increased risk of heart disease and diabetes. It follows that interventions, dietary or otherwise, that may prevent or retard insulin resistance may help to reduce future risk of heart disease and diabetes. That is the reason that we have embarked on this study to examine the effect of increased fruit and vegetable intake on that health-related outcome.
603. We are also interested in the effects of different weight-loss diets, not only on weight loss but on insulin resistance and other risk factors for cardiovascular disease. We recently completed a study that compared the metabolic effects of a low-fat diet with a low-carbohydrate diet in people who are overweight. In addition to that metabolic research, we have an interest in the study of the management of obesity. There are many strategies to help people to lose weight, but it is equally important to help people to maintain weight loss.
604. Maintaining weight loss is extremely challenging, and only some 20% of overweight individuals who lose weight will actually keep that weight off in the longer term. Therefore, given the relapsing nature of weight loss, there is a need to identify novel ways to help people to maintain their weight loss and to test those approaches using robust methodologies. Internet-based programmes offer potential because they are interactive, readily accessible, relatively low cost compared with other interventions, and there is potential for widespread dissemination in the population. We have access to a unique Web-based behaviour change programme, which has been shown to help people to increase their activity levels and to lose weight. We will now test whether that Internet-based technology also has a role to play in helping people to maintain their weight loss.
605. We are happy to provide further details of any of our research programmes if desired by the Committee.
606. Professor Kee: Dr McKinley outlined one dimension of the research. In the PowerPoint presentation, I illustrate where consensus is emerging on both sides of the Atlantic about research priorities. It is being said that we need to take a broader view of research priorities, examining the environmental and societal forces that act on all of us and which regulate our intake and our energy expenditure. Therefore, individuals cannot simply be seen in isolation.
607. A sociologist in America produced a lovely piece of work, which hit the headlines and appeared in all major newspapers on both sides of the Atlantic. It is known as the Framingham heart study, and it examined a large group of people’s social networks over 30 years. The study found that the people who became fattest also had friends becoming fatter at the same time, and it posited that there were social network effects on how we regulate our energy intake and expenditure. It also suggested novel ways in which public health specialists could tackle that problem, harnessing the power of social networks. It underlined the need for longitudinal studies in populations, because we would not have found that without longitudinal studies in Framingham. As Michelle said, public health specialists are now starting to use new vehicles such as the Internet to transmit public health messages, and some of our work will harness a novel approach such as that.
608. The Department of Health in London recently issued a new social marketing campaign document, which focuses on how people make decisions. It uses the exchange concept, and perhaps, in our research, we should think about how to reward healthy choices. An innovative research scheme, Points4Life, has been launched in Manchester. It is based on loyalty cards for supermarkets, and people will be rewarded with more points if they buy healthy options or if they take more exercise. We are building that concept into a new research project. Before the scheme was launched, consumer market research was carried out in Manchester to find out what the voters wanted, so Points4Life is exactly what the community wants. That is one novel method to change the way in which we make our decisions.
609. We have tried to incorporate that concept into a research proposal, which has been shortlisted by the National Prevention Research Initiative. The proposal will study the impact of the Connswater Community Greenway in east Belfast, which was awarded funding from the Big Lottery Fund last year, on physical activity behaviours in the local area. We will build the idea of a loyalty card into that project, whereby people who use the Greenway can be rewarded with redeemable points in local retail outlets. It is an exciting new avenue of research for us, and it is one way to get the private sector interested in transmitting public health messages. One message emerging from that recent social marketing document from the Department of Health is that we need more public-private partnerships, as well as academic partnerships, to tackle the problem. In public health, translational research is about making a difference.
610. People talk about a bench-to-bedside model of transitional laboratory research. We talk about “bench to trench" — what really makes a difference to communities — and we will make a difference to communities only if we harness the power of those communities. That is what we are trying to do in the Connswater project.
611. My PowerPoint presentation refers to what we must do to capitalise on the available research opportunities. I know that this is the Committee for Health, Social Services and Public Safety, but obesity is not the Department of Health, Social Services and Public Safety’s problem: it is a societal problem. We will need all 10 or 11 Departments working together, whether on transport or urban design solutions, which will help to make a difference, or in ensuring that the right data is available for future planning, including data from the ‘Northern Ireland Health and Social Wellbeing Survey’, which is currently being reviewed by the Northern Ireland Statistics and Research Agency. We must continue to ensure that physical examination is an element of that survey.
612. I hope that researchers from Queen’s University and the University of Ulster can talk effectively to all 10 or 11 Departments that have an interest in solving the obesity problem, whether that be the Department for Regional Development, the Department for Social Development or the Department of Culture, Arts and Leisure. All those Departments are interested in our Connswater Community Greenway proposal.
613. My final PowerPoint slide refers to the UKCRC Centre of Excellence for Public Health, of which I am the director, being a partnership among Queen’s University, the new Public Health Agency, the Department of Health, Social Services and Public Safety, the Institute of Public Health in Ireland, the Community Development and Health Network, which allows our research to be more grounded and embedded to meet the needs of communities, and W5, which helps us to transmit our messages about new ways of tackling the obesity problem directly to schools. As researchers, we hope to have increased traction with the communities and with the policymakers. In fact, we had a wonderful seminar at W5 with policymakers and practitioners who helped us to engage with several schools from across the Province about obesity and obesity control.
614. That is the research that we are carrying out at Queen’s University.
615. Ms Mairead Boohan (Queen’s University Belfast): I will cover the undergraduate curriculum, and I thank the Committee for giving us the opportunity to make this presentation, which will build on the information given by Professor Johnston in his submission. I will explain the structure and the way in which we deliver the undergraduate curriculum at Queen’s University.
616. The curriculum is delivered using an integrated-systems-based approach. That means that, in years 1 and 2 of the curriculum, students work through each of the body’s systems. For example, when students are learning about the digestive system, they do not learn about only the anatomy; they learn about the physiology of the system. They also learn some of the basic clinical and physical examination skills that the clinician will use when examining that system. Given that it is an integrated course, they also cover epidemiology. When students are learning about the gastrointestinal system, they will consider the incidence and prevalence of diseases and illnesses associated with that system. They will also cover behavioural science — in other words, how the behaviour of the individual, and cultural and social factors, impact on health.
617. As the students are working through each of the body systems in years 1 and 2, information about obesity is included and integrated as appropriate. The students learn about the metabolic controls of the body system. When considering obesity and nutrition, the metabolic control covers the calorific and food intake and energy expenditure. The students learn about “normal" calorific intake — in other words, normal food consumption and what the body needs to function effectively and the energy that is expended from the body. They also learn about what happens when an individual over-consumes and ultimately becomes obese, and what may happen when an individual under-consumes food and suffers from malnutrition.
618. As part of the behavioural sciences element, we consider the modifiable and non-modifiable factors that may contribute to obesity. Modifiable factors include an increase in exercise and changes in patterns of eating and in eating behaviour. Non-modifiable factors include genetic predisposition to obesity and the conditions that can result from obesity — for example, diabetes and hypertension.
619. In years 3, 4 and 5, students begin their clinical rotations. During clinical attachments, when appropriate, they come into contact with patients who suffer from conditions directly resulting from obesity, metabolic disorders such as diabetes, thyroid problems and other conditions associated with diabetes — for example, hypertension and coronary heart disease, which are currently major problems for our population. In their surgical rotations, students learn about the diagnosis, treatment and management of those conditions and complications that can arise from them. Pre- and post-surgery complications for obese patients have implications for Health Service delivery, including extended stays in hospital.
620. Through orthopaedic and rheumatology courses, students also learn other health consequences of obesity — for example, damage to limbs and joints such as the hips and knees, which may result in surgical problems.
621. In year 4, the paediatrics course identifies and discusses obesity in childhood, which is a major health problem. During that course, students also learn how to measure body mass index and how to identify whether somebody is obese. The obstetrics and gynaecology course explores health and fertility problems — for example, polycystic ovaries, which can result from obesity.
622. In the general practice course in year 4, students revisit the health and behavioural science elements of managing and treating obesity, during which there is, again, much focus on dealing with the management of obesity and on eating patterns at a population level and, importantly, at the level of the individual. Students learn that mass-population education campaigns are often unsuccessful in managing conditions such as obesity. Individuals and barriers to complying with healthy eating — for example, budget and family finances — must be considered.
623. That covers what all students will learn about obesity in the core curriculum. In addition, the students have the opportunity to select components that are delivered from years 1 to 3. Each semester, students are given a range of about 25 modules from which they select those that they want to study in that semester. In year 2, two modules are delivered, providing students with much additional information about obesity. I have copies of the study guide for the module ‘Childhood Obesity: Understanding and Managing a Growing Problem’, if Committee members wish to take a copy. It contains information on current problems about managing obesity in our society.
624. Year 2 students also take a module entitled ‘Medics in Primary Schools’, which involves 55 primary schools in the greater Belfast area. Over 10 weeks, pupils visit the school of medicine for one afternoon a week to study a range of topics including a healthy living environment and healthy eating. That module teaches students that, quite often, children do not have much input or say in their diet. What primary-school children consume is decided by family members or by the content of school meals.
625. That is an overview of what is covered in the core curriculum and the student-selected components.
626. The Deputy Chairperson: Thank you very much for your presentation. We all agree that this is not just a health issue; it has to be tackled across the board on a cross-departmental basis. Professor Kee, you sit on the obesity prevention steering group. The Committee has received evidence from other interested parties. Dr Jane Wilde emphasised the need for more research to inform policy. Do you feel that there is currently a gap? Plenty of research is being done, but perhaps it is not feeding through to policy. There is a research element to the obesity steering group, but is it a strong element?
627. Professor Kee: The obesity task force has a data and research subgroup, which has met on about three occasions. I think that it is planning an event at the end of the summer. In the broader research community, people have recognised that working directly with policy-makers and practitioners must be the way forward. That will be beneficial because communities will co-design the research questions and come up with the solutions. That approach has been adopted on both sides of the Atlantic.
628. That is why I made a reference to “bench to trench". As public health specialists, we are more interested in what is effective rather than what is efficacious. There is a distinction in our mind about what is effective and works in real life rather than what works in a laboratory. Ultimately, the community will help us to design the best solutions.
629. The Deputy Chairperson: I like what Dr McKinley said about there being plenty of strategies to lose weight, but the problem is maintaining that weight loss. That is always the biggest challenge for anybody whom I know who has a weight problem. Anything that moves towards that type of project must be welcomed.
630. Mr McCallister: Following on from the Deputy Chairperson’s point about assessing how that is put into practice, what involvement will you have with the new Public Health Agency? Your point about schoolchildren visiting the school of medicine is interesting. Were those visits effective? Should we consider rolling out such schemes? As a pilot scheme, it has worked very well.
631. As the Deputy Chairperson said, we are mostly concerned with delivering the policy on the ground. Your point concerned making it easy for people, whether that be walking to school or through a person’s lifestyle choices or the built environment. All those elements should come together. I am keen to assess how we can intervene earlier and educate people at a younger age.
632. Ms Boohan: I will pick up on your comment about schools. That student-selected component has been running since 2000, and it started with 10 schools. It is confined to the greater Belfast area for timetabling reasons. In 2001, we did an evaluation with the 10 schools that had participated in the previous year. It was carried out by colleagues from the graduate school of education. They interviewed the school pupils who had taken the module during the previous academic year. The module covers a range of issues, and the one area that the pupils recalled most clearly concerned diet, food and nutrition. They talked to the researchers about how, when they were in a supermarket, they were able to inform their parents that certain foods were not a healthy choice, perhaps because of a high salt content.
633. Although that was a small evaluation, it definitely seems to have had an impact, probably because the pupils saw the medical students as role models. Although the medical students are at university, they are relatively close in age to the pupils and can, perhaps, identify more closely with them than an older or more experienced person can.
634. Professor Kee: Your question had two parts, one of which asked about schools and schoolchildren. We ran a debate day in W5, when sixth-formers from eight or nine schools across the Province debated the “nanny state". The way in which they interpreted both sides of the argument was marvellous. The chief executive of an advertising agency, the Chief Medical Officer and Basil McCrea, who spoke from the perspective of an MLA and legislator, attended the event. The sixth-formers quizzed the representatives with some smart questions. As Mairead mentioned, our schoolchildren are tuned into what drives societal behaviour and how to react to that. We did not come up with any new solutions that they had not thought of themselves.
635. The second part of your question relates to the new Public Health Agency. My contract is partly with Queen’s and partly with the agency. As a multidisciplinary centre, we received an award from the Department for Employment and Learning in summer 2008 to enable us to take the first steps towards creating an obesity observatory similar to that funded by the Department of Health in England. That will help us to communicate more effectively to various bodies, including health bodies and local councils, our knowledge of what works and what does not work. That must be multi-sectoral and multidisciplinary. It is important for the new agency, and for academics, to build capacity that will help us to model the consequences of different policies.
636. Mr Easton: Your research considers the body’s mechanisms and how much fat and sugar that it needs. If we are to reduce obesity levels, we must force food manufacturers to include the correct levels of fat and sugar in food. They tend to use too much sugar, because it is nice and everyone likes it. Through your research, what levels do you believe are required for the body to function, and what amounts should be contained in foodstuffs? Our inquiry should determine those levels to ensure that Departments are aware of safe levels and know how to force food companies to adhere to those levels.
637. Obesity is linked to diabetes. My father is diabetic, and, although he will kill me for saying so, he was quite a big man when he was younger. Therefore, I recognise the correlation between diabetes and obesity. Will eradicating obesity eradicate diabetes, or will some people contract that disease regardless of whether or not they are obese?
638. Professor Kee: I will answer the second question and ask Dr McKinley to answer the first one. Eradicating obesity will not eradicate diabetes, because there are two common types. Type 1 is, generally, contracted during childhood or as a young adult and is not associated with obesity to a great extent. Older, heavier people are more prone to type 2 diabetes. We must tackle obesity, because that will help to remove the factors that drive the diabetes epidemic. The rates of type 2 diabetes are increasing more quickly than those of type 1. Therefore, we must concentrate on solving the obesity problem to forestall the epidemic of type 2 diabetes. Dr McKinley will answer your question about food standards and the Food Standards Agency, because she has worked on both sides of the fence.
639. Dr McKinley: The Food Standards Agency has a wide communication strategy on that issue. It previously conducted a major campaign to try to reduce levels of salt in various foods, and it is now considering levels of saturated fat in food. Fat is energy dense and may be one of many factors that contribute to the obesity problem. The Food Standards Agency is the source of information on current dietary recommendations. The Department of Health issues recommendations on healthy diets, and the Food Standards Agency provides practical advice and information, which is communicated to consumers in a number of ways, including food labels.
640. Traffic-light labelling was a Food Standards Agency initiative. Communication strategies such as this have been designed to help the consumer to make healthier choices, and research now focuses on whether those strategies are helping the consumer effectively or whether other approaches should be considered.
641. For example, our research on comparing a low-fat diet with a low-carbohydrate diet for weight loss considered, where people were losing around the same amount of weight on those diets, whether one had a beneficial effect on areas such as cholesterol and blood pressure over another type of diet. There is much suspicion over whether low-carbohydrate diets have detrimental effects on health. The study revealed no major differences between the two types of diet.
642. More work must be done to find out what exactly are the best dietary approaches to offer to people who are trying to lose weight and to find dietary approaches that will not have any detrimental effects on the health of that person in the longer term. More research must be done, but the low-fat, high-fibre approach is still the standard weight-loss diet that is recommended and supported by health professionals.
643. Mr Easton: Unless the food companies are forced to do the right things with food, not much of a difference will be made. The inquiry does not have the powers to enforce that. We need to force the food manufacturers to make a difference to people’s lives.
644. Mr McCallister: There is a great deal of dissatisfaction, not only on the nutrition side but on the sourcing of food, including the definition of “fresh". The food-labelling agenda is huge, right up to European level.
645. The Deputy Chairperson: We will explore that further when the Food Standards Agency and the Food and Drink Association come before the Committee.
646. Mrs Hanna: Good afternoon; you are very welcome. Thank you for your presentation. The research is important in giving us a better understanding.
647. As many people know, it is hard to lose weight. For people who are significantly overweight, it can be a huge challenge just to start a diet. You mentioned healthy choices and the Points4Life initiative.
648. Dr McKinley talked about colour coding. That is done by Marks and Spencer, for people who can afford to shop there, but it is not done by Tesco, where the cheapest products are perhaps high-fat products. That is terrible, because some people are unable to afford that choice.
649. Another issue is better understanding of nutrition. The teaching of home economics at school used to cover a bit of budgeting and cooking, when people used to cook more and ate around the table. Many people now use ready meals, which are probably not as nutritional. They probably have a higher fat content, because they are tastier with additives and more salt. There are challenges with that.
650. Metabolic control was mentioned. We all blame a slow metabolic rate if we are not losing weight. What do you mean by that? I think Mairead spoke about that. Frank mentioned nutrition and metabolism. What impact does that have on losing weight?
651. Professor Kee: The questions so far have mentioned nutrition. The studies that have compared populations that have seemed to have become fatter over time have shown that the total calorific average intake has not been the significant variable. The expenditure of energy has been the significant variable. I can identify that trend towards sedentary living over my lifespan. We must not lose sight of that.
652. Mrs Hanna: You also said that one should look at the people one has been keeping company with over 20 or 30 years.
653. Professor Kee: As well as that, we can all look back on our primary-school years. I do not remember a single child who was overweight in the primary school that I attended.
654. Mrs Hanna: We walked to school.
655. Professor Kee: We did. I remember walking a couple of miles to school.
656. Mrs Hanna: We skipped, and we played rounders. We did not have computers or Game Boys.
657. Dr McKinley: In relation to losing weight, nutritionists are sometimes very black and white about energy balance: to stay the same weight, energy in must match energy out. Both sides of the equation are important: dietary intake and physical activity. Much research is under way, and I am not an expert in the genetic aspect of obesity or in whether some people are more prone to it than others.
658. The example that I am thinking of is the study that compared two weight-loss diets with different compositions. We provided people with their food and controlled their calorie intake. Both groups lost approximately the same amount of weight. Overall, it seems that, when people have a reduced calorie intake, they lose weight. In our sample, there may have been some people who were slightly more resistant to weight loss.
659. I referred to the “metabolic effects". We are trying to understand whether some diets are better for long-term health than others. Is a low-fat diet safer, in the long term, for someone who is overweight as opposed to a more fashionable low-carbohydrate diet? There are numerous books on low-carbohydrate diets but, at present, we do not know enough about their effects on health. However, some people find it easier to lose weight on low-carbohydrate diets, so we cannot be dismissive. We need to do the research and find out whether it is safe for health professionals to recommend such diets to people who are struggling to lose weight, who have tried the low-fat/high-fibre approach and for whom that has not worked. We need to explore different dietary approaches to suit the individual. Everyone is different when it comes to weight loss.
660. You referred to cooking. There has been an erosion of cooking skills. However, initiatives have been taken in Northern Ireland. There is a Cook It! programme, about which the Committee will hear more from others presenting evidence. Efforts are being made to rejuvenate those skills at all levels in the population. That is where home economics comes in. Uniquely, in Northern Ireland, home economics is still on the curriculum, and that might be crucial. It might be the only place where some children learn cooking skills because they may not learn them at home.
661. Mrs Hanna: School meals have been mentioned previously and whether chips could be removed from school menus to make meals healthier. Games should also be encouraged in school. Not everyone plays games — Gaelic, netball or whatever — but we must try to make sport fun. If children get used to activity, they crave it, whereas if they never do sport, they are more inclined to sit around.
662. The Deputy Chairperson: We need a cross-departmental approach, because that issue must be tackled by the Department of Education.
663. Ms Boohan: Several years ago, it became apparent that some medical students were unaware of the nutritional content and value of many of the foods that they were consuming and that, ultimately, their patients would consume. As part of the year 1 behavioural sciences programme, we give students an article from a popular magazine providing dietary advice. We then give the students a number of patient scenarios: in one, an affluent, well-educated family will probably understand a lot about nutrition and, in another, there is a family that has a single income that is below the basic minimum wage. We get the students to work out reasons why the families described in each case scenario are able to comply with the dietary advice in the magazine.
664. During tutorials, students often comment that they did not realise that X amount of salt or hidden fats are contained in the convenience foods that they eat. Therefore, medical students are being educated about the foods that they consume as well as about the foods that their patients will consume.
665. The Deputy Chairperson: There are no further questions. I thank you all for your informative presentation. We will certainly forward you a copy of the report that we produce at the end of our inquiry. Thank you very much.
23 April 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Witnesses:
Ms Karen Smyth |
Northern Ireland Local Government Association |
|
Ms Katrina Morgan-Talbot |
Belfast City Council |
666. The Deputy Chairperson (Mrs O’Neill): The next item on the agenda is the evidence session with the Northern Ireland Local Government Association (NILGA). We have received submissions from NILGA as well as from several local councils.
667. I welcome Karen Smyth, who is head of policy at NILGA, and Katrina Morgan, who is leisure operations manager at Belfast City Council. I invite you to make your presentation, after which members may ask questions.
668. Ms Karen Smyth (Northern Ireland Local Government Association): Thank you, Chairperson, for inviting NILGA to give evidence to the Committee. We appreciate the opportunity. Unfortunately, I must apologise for the absence of elected members at the meeting. We would have liked to have brought along some of our elected members; however, several other meetings are taking place. The Committee will be aware that our members are busy with the review of public administration (RPA) and policy development panel meetings. Therefore, trying to get someone to attend has been problematic.
669. We intend to run through the NILGA submission that the Committee has already received. I will then bring Katrina Morgan in to discuss more fully the projects that Belfast City Council, in particular, is working on.
670. Preventive healthcare is a key issue for local government. It has a huge impact on communities; citizens’ well-being; and on the economy, which relies on people’s fitness for work. The integrated work of councils’ environmental health, community and leisure services officers currently provides demonstrable success at local level. It indicates that a more joined-up approach to the issue is key to a successful approach to tackle obesity. Local government is particularly well placed to tackle regional issues such as obesity at local level and to initiate projects that make a real difference to local communities.
671. We have found that the best and most successful projects are often implemented in partnership with other agencies, such as the education and health boards, which provide a link to schools, as well as the Fit Futures teams and health-promotion teams. Often, councils assume the role of enabler in much of that work. They have a civic-leadership duty to ensure that citizens maintain a healthy lifestyle.
672. Councils have played a full role in Investing for Health partnerships. A number of examples show how councils have taken the lead on well-being. For example, in the Newry and Mourne District Council area, the council’s facilitation of the well-being action partnership has been an exemplar of how a partnership approach can improve health.
673. The Chief Environmental Health Officers’ Group is to convene a nutrition subgroup to look at how environmental health officers can best become involved in tackling obesity in the general population and also to share ideas and initiatives that might be happening elsewhere in Northern Ireland, the rest of the UK and the Republic of Ireland. That subgroup will also include members from the Food Standards Agency Northern Ireland (FSANI), and we will be working in partnership with them.
674. Local government environmental health officers have been involved in promoting schemes. For example, in conjunction with food manufacturers, they have been promoting the Food Standards Agency’s traffic-light scheme. We are willing to work with the agency on further emerging initiatives, such as its campaigns on saturated fat and salt. Other projects of that nature include the implementation of the Chartered Institute of Environmental Health’s awards for healthier foods and special diets.
675. Members will also be aware that councils are the foremost providers of leisure facilities in Northern Ireland. Their leisure services offer a wide range of physical activity programmes and facilities that target the entire community, often according to age. They encourage citizens to engage in sport and other physical activities.
676. Ms Katrina Morgan (Belfast City Council): Good afternoon, folks. I will cite some examples of the successful programmes that Belfast City Council has run over the past year for various age groups. Choose n Move is a programme that is targeted at children between the ages of four and 16. It was designed by our health development unit and contains two key messages: eat more fruit and vegetables and become more active. The programme consists of 11 activities, and children are referred to it and are tracked through leisure centres, and parents can also obtain information from our Choose n Move website.
677. Moving up through the age groups, the FRESH project is targeted at children between the ages of 11 and 13. FRESH stands for food, relaxation, exercise, self-esteem and health. It is partly funded by the Eastern Health and Social Services Board, and it is delivered in partnership with the Belfast Health and Social Care Trust, Belfast Community Sports Development Network (BCSDN) and other councils, such as Lisburn City Council, Down District Council and North Down Borough Council.
678. Belfast City Council has three programmes in place, and they are based at Shankill leisure centre, Avoniel leisure centre, Ballymacarrett recreation centre/Andersonstown leisure centre. We like to target families, as well as kids. One of our programmes is called Fit Families, and it is run in conjunction with the Maureen Sheehan Centre, which is part of the Belfast Trust. It is a pilot project, which involves five families in west Belfast. The programme includes activity books, education, physical activity opportunities and weekly review meetings. We hope to have the first evaluation of that project by June 2009.
679. Other projects that are targeted at families include the parent, toddlers and children programme, which is delivered with the help of the Healthy Living Centre Regional Alliance. In total, we have rolled out 13 programmes that are being delivered through 50 different educational workshops; their evaluation is due in May 2009.
680. We consider some of our other programmes to be innovative. For example, two Kidzfit gyms are based in Belfast: one is at the Shankill leisure centre, in the north, and one at the Falls leisure centre in the west. Figures show that, so far this year, more than 2,000 kids have participated in those programmes, which involve activities specifically for kids. We are trying to branch out beyond leisure centres, and the Greater Shankill Sports Committee and the Shankill Junior Football Club have become involved.
681. Finally, the Healthwise programme runs in many council areas across the North. It is funded by the Eastern Health and Social Services Board and offers a free 12-week programme. Patients are referred to a leisure centre to participate in the programme, and that referral can be based on anything from weight or obesity problems to general health problems. The participants are evaluated at the end of the 12-week programme. Last year, more than 1,000 people participated in the programme through Belfast City Council. That is a little flavour of what Belfast City Council and some of its local partners do.
682. Ms Smyth: Members will be aware, and I have already referred to the fact, that NILGA works intensively on the review of public administration and local government reform. It is essential that local government grasps the opportunities, particularly those presented by the health and social care reforms. A local council plays a vital role as service provider, civic leader, partnership convener, community focus and advocate on health issues. We draw the Committee’s attention to the Lyons Review, which identified local government as a place-shaper and highlighted the need to take a wider view of health and wellbeing. In addition, a recent World Health Organization report refers to urban planning as a key aspect in the consideration of the wider elements of health provision.
683. Councils should be taking up opportunities in the new joint-working pilot schemes and local commissioning groups. In addition, following local government reform, community planning, the power of well-being and other powers will increase the ability of local government to influence the health of local communities.
684. We are keen to think differently and to innovate, focussing on outcomes and not on who does what, and we look forward to working with the new Public Health Agency at regional and local level on obesity issues. The new health structures will provide a greater role for local government through participation in the Public Health Agency and in local commissioning. The Minister has already invited expressions of interest from councils on the possibility of hosting joint pilot schemes to focus on addressing specific health and well-being inequalities. We will meet the Minister shortly to take that work forward.
685. The Minister’s letter indicated the possibility of collocating health and social care staff with local government staff to support councils in exercising their power in well-being and community planning and in inter-sectoral partnerships, and we will explore the way forward on that. Those staff could also assist in developing local health-improvement plans to reflect local needs with regard to issues such as obesity. We would also support the local commissioning group in developing commissioning plans to deal with Health Service provision and measures to prevent ill health. We want to develop and extend those arrangements post-2011.
686. NILGA makes a number of recommendations on taking forward work on obesity. It hopes that the ‘Fit Futures: Focus on Food, Activity and Young People’ report will be fully implemented. We believe that a comprehensive, cross-cutting, long-term Northern Ireland strategy to tackle obesity needs to be drafted and implemented as soon as possible, bringing together all major stakeholders. There should be a scoping exercise of existing good practice, to be shared with all relevant agencies and central and local government departments.
687. Central Government should fund the roll-out of known successful initiatives, such as the Cook it! programme, and develop a joined-up approach at regional level in order to ensure consistent messages on healthy eating. Cooking skills should be made a mandatory part of the school curriculum, and healthy food choices should be available in all schools. We want to continue to work in partnership with the Food Standards Agency and the food industry in order to improve the nutritional quality of the foods that are available for sale.
688. Healthy eating awards should be available to food-business operators in Northern Ireland, and social marketing tools should be used in a campaign directed at the parents of young children and at the general population to increase awareness of health-related issues that are caused by obesity, because the accessibility of young people to the wrong foods needs to be addressed at regional level. There should also be adequate opportunities for young people to participate in physical activity at school and in the wider community.
689. The Deputy Chairperson: Thank you for your presentations. Local government will play a key role in tackling obesity and a number of other issues. As we move forward with the RPA, the transfer of community planning powers to local councils will be crucial for tackling health inequalities, because, quite often, people from socially deprived areas are more likely to be obese or to have long-term illnesses. With regard to the way in which local government feeds into the cross-departmental obesity steering group, do NILGA representatives sit on that group?
690. Ms Smyth: As far as I know, there are links between that group and the Chief Environmental Health Officers’ Group. We have participated at officer level rather than at elected-member level, but I can check that.
691. The Deputy Chairperson: That is a key matter, because, every week since this inquiry began, we have been hearing about access to leisure services and about a lack of play facilities. Obviously, that is all part of the whole process.
692. Ms Smyth: Community planning will be crucial, and working things out in local area agreements in the community planning processes will be vital in sorting out the whole problem.
693. The Deputy Chairperson: Katrina, you spoke about people in the Healthwise programme being referred. Is that referral from a GP?
694. Ms Morgan-Talbot: Yes. It is commonly known as the GP referral programme, but, technically, it is called the Healthwise programme. An individual can be referred for anything, including obesity or obesity-related illnesses such as high blood pressure or heart disease. People do, therefore, pass through the programme, and it is open to all age groups.
695. The Deputy Chairperson: Does that happen only in Belfast City Council, or does it happen across the board?
696. Ms Morgan-Talbot: It happens in a majority of councils in Northern Ireland.
697. The Deputy Chairperson: This is the first time that I have heard of that programme. The Committee has previously teased out the issue of what a GP can do.
698. Ms Morgan-Talbot: We roll out the GP referral programme, and, in Belfast, we link up with GPs through the Eastern Health and Social Services Board. The GPs sign up to the programme, and there is a process through which individuals are referred and which involves indicators and suchlike. In the past, individuals have come into leisure centres to inquire about the programme. If their GP was not on the list, we would have gone back to our partners to try to encourage that GP to sign up to the programme and to come on board.
699. The Deputy Chairperson: OK. Is that programme free for the participants?
700. Ms Morgan-Talbot: Yes. It is a 12-week programme, and it is free for participants.
701. The Deputy Chairperson: That needs to be publicised to make more people more aware of it. That message is not currently out there.
702. Ms Morgan-Talbot: It is quite well known. Last year, more than 1,000 people participated in the programme, even though there was only enough funding for 800 people. However, we decided that, despite the fact that that funding ran out around November, we should continue to take people on the programme, because we did not want to stop it dead.
703. We find that the biggest hurdle for people is the fear factor of making that first appointment and coming to see us. People can be referred, but sometimes it takes about three months for them to visit us. Perhaps a little more awareness of the benefits of the programme would be helpful.
704. Mr McCallister: How many GPs are involved in the programme? Are all GPs aware of it?
705. The Deputy Chairperson: The Committee recently heard evidence from representatives of the British Medical Association (BMA) and they did not discuss the programme. That is why it seems to be new to us, and why I think that doctors are unaware that they can refer patients to it.
706. Ms Morgan-Talbot: OK. I can double check that information. I know that information on the Healthwise programme is normally sent out to local GPs, but I do not know whether that is enough to entice them into the programme. I will check what mechanisms exist for informing people.
707. Mr Gardner: Has that trial programme dealt solely with GPs in Belfast?
708. Ms Morgan-Talbot: No. Several other councils are involved —
709. Mr Gardner: I have not heard anything about it. I represent the Upper Bann constituency, which includes Lurgan, Portadown and Banbridge, and I am not aware of any activities in those areas.
710. Ms Smyth: I will contact the councils to find out which ones are participating, and I will inform the Committee.
711. The Deputy Chairperson: The Committee would appreciate that. A GP sits on this Committee, and he is unaware of the programme, because he has talked about what he would do —
712. Ms Smyth: That may have something to do with the board area in which he works.
713. The Deputy Chairperson: It would be good if you could provide that information to the Committee.
714. Mrs Hanna: Good afternoon, you are very welcome. It all sounds so simple: eat more fruit and vegetables, get out more and, maybe, eat a bit less, but that seems to be very hard to do. The councils, more than any other bodies, are closest to those on the ground. Not only that, the councils operate the leisure centres and the playgrounds, and we must utilise those facilities better.
715. Ms Morgan-Talbot: We should not concentrate only on the leisure centres; we should also examine the role that our parks can play. We must try to make the parks more user-friendly to entice people into them, rather than just keeping them as green spaces. We want to work in partnership with the parks.
716. For example, we engage with schools. We run a very successful cross-country championship, during which we carry out awareness sessions that deal with nutrition and various other things. We try to include families. We see family engagement as crucial, because if families can be encouraged to adopt a healthy lifestyle, the children will naturally fall in to sync.
717. Mrs Hanna: It seems that much research and analysis has been carried out, yet the solution is so simple. It seems that attempts to motivate people to become more active are not working. Do you agree?
718. Ms Morgan-Talbot: Motivation plays a huge role, but culture is also very important. For example, there are areas in Belfast that suffer socio-economically and have higher rates of children not attending school or not finishing qualifications. In those areas, the level of parental participation in fitness sessions is also lower. Therefore, it is key that we reach those hard-to-reach communities.
719. The World Health Organisation’s Commission on Social Determinants of Health recently published a report that suggested that urban planning was a key to improving health. We very much agree with those sentiments and want to utilise things such as cycle schemes as a way of encouraging people to become socially involved in exercise rather than just visiting a leisure centre. Indeed, Belfast City Council is carrying out a strategic review of leisure this year, and we see that review not just as a way to examine our stock, but as a way to examine methods of improving community engagement and getting people from the wider community into our parks. We will seek to do that by joining up with other partners, clubs, groups and societies in an attempt to promote leisure, whether in participation or as recreation.
720. Mrs Hanna: You referred to schemes at the Shankill and Falls leisure centres, have you measured any outcomes of those?
721. Ms Morgan-Talbot: It can be hard to actually sit down and determine how to measure the outcomes, but, through the local schools, we have found that the children who participated in the programmes — those who possibly would have skipped PE classes in the past — have found that they have become interested in, and actually look forward to, exercise. As a result, those kids will come in at weekends with their parents.
722. The council operates a means-tested benefit pricing policy in all our leisure centres to attract folk who are on low incomes or unemployed. It runs month by month, depending on which schemes we run. If we run a successful scheme in an area, we discover that many more families join leisure centres. They become involved, and leisure centre usage increases. However, actual health outcomes are harder to determine.
723. Mrs Hanna: Those results are very powerful. You are saying that the people who are taking part in your initiatives are becoming more active and more involved, and that is what we want. If the simpler things, such as those initiatives, are working and are helping children to be more active, we should be doing more of that. We keep thinking of other things that we need to do, but maybe it is better to keep doing the simple things.
724. Ms Morgan-Talbot: When programmes such as the FRESH project, which is an 18-week course that is aimed at 13-year-olds, come to an end, we find that many of the kids come back to the leisure centres. We try to get funding to bring them back with their youth clubs, for instance. We incorporate various elements — not just leisure, but nutrition advice and other things — to make the programme interesting, and to make people see that a leisure centre is more than just a swimming pool and a main hall.
725. Mrs Hanna: If something like that is working we should be using it. We already have the leisure centres, the parks and the playgrounds.
726. Ms Morgan-Talbot: I am not sure whether members are aware of the Active Communities investment programme, which is open to all councils and is funded by Sport NI. Belfast City Council has received funding to employ coaches to deliver key health benefits to communities. We hope to have 17 coaches in place by October. In order to do that, we have linked up with local government bodies and local groups that have identified their key aims and sport-development programmes for increasing participation among hard-to-reach groups in communities, such as people with disabilities, children, young mothers and older folk. It is a three-year programme that will reach out into the community. We often find that people do not want to leave their community, and they want to go to classes in their local community centre or church hall. It is crucial to empower people to get involved.
727. Mrs Hanna: Although I appreciate that it is sometimes difficult to measure outcomes, I would welcome a report on such schemes that says what Ms Morgan-Talbot has been saying — that such programmes make a difference. Participation can be measured to some extent.
728. Ms Morgan-Talbot: Yes, it can.
729. Mrs Hanna: We need to know whether people are becoming more active and going back to the leisure centres or participating more in schools. That is the natural way to get children to be more active, and if it is working, that is good.
730. Mr Gardiner: Do you have any direct link with Craigavon Borough Council? Lurgan Park, which is the largest park in Northern Ireland won the green flag award. The next largest park is Phoenix Park in Dublin.
731. Mrs Hanna: It must be big.
732. Mr Gardiner: It is. Well, you can do a one-mile walk around the lake, or a two-mile walk, if you want to get young people involved in exercise and keeping fit. There is fishing, and new stands have been put up for people who want to fish.
733. Ms Morgan-Talbot: I am not sure if we have any direct links. I know that —
734. Mr Gardiner: That is why I am pushing this. You represent NILGA, which covers all local council areas. Craigavon Borough Council is involved; it has to be a two-way process.
735. Ms Morgan-Talbot: That is great; thank you very much.
736. The Deputy Chairperson: Katrina is speaking from Belfast City Council’s perspective. Karen is the representative from NILGA.
737. Ms Smyth: When I was researching our report, I was inundated with examples of good practice from different council areas. It was my understanding that those examples had already been fed to the Committee, and I did not want to repeat information that members had already received. I will forward that to you.
738. Mr Gardiner: OK.
739. The Deputy Chairperson: NILGA recommended a scoping exercise on existing good practice; that is exactly what we are talking about. Have you done that work?
740. Ms Smyth: Yes. We have done a partial scoping exercise of what already exists. When we ask councils for information, we do not get 26 replies very often. The work is under way, and we could take that forward for the Committee if it wants us to do so.
741. The Deputy Chairperson: It would be very helpful to have that information.
742. Mrs McGill: I would expect there to be particular focus on neighbourhood renewal areas because of deprivation and, by extension, poor diet. How is that addressed by Belfast City Council?
743. Ms Morgan-Talbot: The council has a strategic neighbourhood action programme (SNAP), which has developed action plans for 11 or 12 areas. The action plans address key themes from the environment to health. Each individual area, through a specific working group and various partners, has identified key actions that we will deliver.
744. Mrs McGill: Do those actions link to exercise and issues around obesity in particular?
745. Ms Morgan-Talbot: Yes.
746. Mrs McGill: I think that that would be fundamental, given that there are links.
747. Ms Morgan-Talbot: The council’s leisure services division had an input into how it would help to deliver all the action plans. I cannot tell you, off the top of my head, whether those plans are directly related to obesity, but I would be very surprised if they did not link into it in some way. I can look into our plans and come back to the Committee.
748. The Deputy Chairperson: There are no other questions. Thank you very much for coming along and giving your presentations today.
30 April 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
Professor Eamonn McCartan |
Sport Northern Ireland |
749. The Deputy Chairperson (Mrs O’Neill): I welcome Professor Eamonn McCartan, the chief executive of Sport NI, and Mr John News, the participation manager of Sport NI.
750. Professor Eamonn McCartan (Sport Northern Ireland): It is an honour and a privilege to be invited to the Committee. It is the second time that we have attended. When we were last here, the subject matter was the Committee’s inquiry into the prevention of suicide and self-harm. Today’s subject is obesity, the tackling of which has an important role in society. John News is one of our senior managers, and, in collaboration with officials from the Department of Culture, Arts and Leisure (DCAL), officially has been responsible for Sport Matters, which is the strategy for sport and physical recreation in Northern Ireland. Members will know that the comprehensive definition of sport requires physical activity and physical recreation.
751. We hope that, as we become more experienced in presentations to the Committee, we will become more interactive. We have provided the Committee with a copy of our information, and one could build another Assembly with the amount of research on obesity that has been carried out around the world. I am content that you are familiar with the research findings and with the tsunami of obesity that has engulfed the developed world and the western world.
752. With your permission, I shall provide an overview of how we intend to make our presentation. The purpose of the presentation is to provide a brief introduction to the role of Sport Northern Ireland. You have all the research, and you know the basic energy equation. If a person takes in more energy than they expire, the energy has to stay somewhere, and, in the case of middle-aged men such as me, it generally goes on the tummy, and we get a little bit heavier. Nonetheless, it is a huge problem for an individual’s health and for the health of society. The problem must be tackled if we are to have fit and healthy individuals and, therefore, a fit and healthy society.
753. I wish to talk about how, and explore the ways in which, sport and physical activity can help. I ask you to park some of your traditional views on sport. There is a traditional framework for sport as it is seen on television, but sport is a much more expansive and expanded sector than simply competitive sport. One need only go to Shaw’s Bridge on a summer’s evening to see people walking for two or three miles out to the Drum Bridge and back. People walk through Barnett Demesne. There are various forms of physical activity, and it is that element of sport on which I shall focus.
754. Towards the end of the presentation, I shall repeat the evidence that you have already received from other people about how obesity levels are increasing in young people, middle-aged people and old people and how that impacts on their quality of life and on the cost of health provision, which eats into limited resources.
755. Central to the vision of sport for Northern Ireland is the aspiration to have fit and healthy people who are capable and competent and enjoying a high quality of life, therefore contributing to, and not being a burden on, society. It aims to promote a culture of lifelong enjoyment and success in sport and physical activity that contributes to a peaceful, fair and prosperous society.
756. We have several important strategic objectives. We aim to increase participation in sport, physical activity and physical recreation. We aim to improve performance in sport, and we aim to do so through a managerial style that is effective and efficient. Through sport and physical activity, we are trying to improve the quality of life of individuals in Northern Ireland so that they have a better physical and emotional quality of life and so that, as a better person, they are more capable of contributing to a healthier and more positive society in which individuals are fit, confident and competent people. Many factors contribute to that fit, competent and healthy individual, one of which is physical activity. I will hand over to my colleague to answer this question: why should Government act?
757. Mr John News (Sport Northern Ireland): The answer to that is contained in the quotations that we have highlighted in our written submission. The first is from the World Health Organization (WHO) in 1996, and the second is a more recent statement by England’s Chief Medical Officer in 2005. It is not our intention today, as Eamonn said, to go over all the evidence. We can see the evidence on the streets, in the schools and in the shopping centres. It is all around us; we can see that people are increasingly overweight or obese.
758. We believe, as the Committee does, that it is not just a problem for the Department of Health, Social Services and Public Safety. The fact that representatives from Sport NI are here today and that we are increasing our investment in physical activity programmes underscores our belief that we have a role to play in finding a solution. One of our concerns is that, if we do not act quickly, the problem will simply get bigger. That is why we are saying that Government must act now. The longer we delay, the more it will cost in future and the bigger the problem will be when we finally decide to act. We are working on the basis of the adage that prevention is better than cure.
759. The Committee’s time is limited, so we will not retrace the history of obesity in the public-sector policymaking processes. In our submission, we show how, even in the past six or seven years, the challenge of obesity for public-sector policymakers has become embedded in the process. It is about bringing the 2002 Investing for Health strategy up to date with the obesity prevention steering group, which the Department of Health, Social Services and Public Safety convened in 2008. There is a consensus among policymakers that we all must act.
760. The challenge, as we see it, is that partnership working will be crucial to that action and its implementation. Partnership is an easy word to articulate. It is easy for us to represent partnerships on organisational charts, but the real challenge is to make partnerships happen. It is about how people make decisions and investments that complement one another. That is the biggest challenge. It is not about convincing people of the need to act but making sure that we all act in concert towards the same set of objectives.
761. Eamonn mentioned Sport Matters, the draft strategy for sport and physical recreation. That document attempts to move away from strategy to implementation. The challenge is to take the actions off the paper and put them into practice. Sport NI suggests that there are two different settings for priority action. The first is about policy, and Eamonn will cover some of those points.
762. Professor McCartan: Undoubtedly, members, it is an a priori fact that obesity exists in the western world and here in Northern Ireland. All empirical evidence shows that it is on the rise. If we all accept that fact, it is time that we began to prioritise some actions. At a policy level, Sport NI advocates the formation of a clear, accountable, physical strategy by the Northern Ireland Executive, which would sign it off and set targets and tasks for Departments.
763. Mr News: We are conscious that we need to give the Committee examples. We do not want to leave members with words on a page. One in four children is overweight or obese. Although the inquiry into obesity is being held by the Committee for Health, Social Services and Public Safety, why, when we talk about translating departmental targets into action, do we not set targets for schools to reduce the percentage of children and young people who are overweight or obese? Schools can measure, monitor and act on that. We can suggest to them how to go about that.
764. It could be: two hours of PE for every child; two hours of extra-curricular physical activity for every child; ensuring that there is community access to school facilities in the evening; and GPs prescribing physical activity rather than expecting people to make that choice for themselves. The Government must work to ensure that there is a culture of physical activity and that it is accessible and a default position.
765. Professor McCartan: You will have heard that we argued that all Departments, in a cross-departmental fashion, should take responsibility for that. In doing so, we contest that that would promote not only a cultural change but a societal, structural and organisational change at a societal level and an individual level.
766. The policies and the evidence are there. Where in the world have other people got on with it? We are advocating that we in Northern Ireland get on with tackling the problem of obesity. There are policy examples from other countries, one of which is very close. The Scottish Government recognised that obesity in Scotland was rising at a disproportionately higher rate than the rest of the United Kingdom, so they developed a physical activity strategy on a cross-departmental basis and set aside £24 million over three years.
767. One of the big difficulties that we associate with partnerships is: who will take the lead? Quite often, people are content to sit around the table in partnership as long as nobody is leading. The Scottish Government said that they needed a leadership group, so they appointed sportscotland to work in an Active Schools network and to be responsible for increasing physical activity among young people in schools in Scotland. The Government held sportscotland responsible, gave it a level of resources and tasked it to undertake the work over three years.
768. There is the capacity in Northern Ireland. The problem is the same, but we now need to move from policy to practice and from policy to implementation. A lead group should be identified — whatever it may be — and it should take responsibility for addressing obesity in various categories — for example, young people, teenagers, people in their 20s, 30s and 40s, and so forth.
769. Mr News: If we are to address the problem, all those sectors must sing from the same hymn sheet. District councils have responsibility for the community planning process, and they have a power of well-being and a responsibility to ensure the health and well-being of ratepayers in district council areas. The education sector is developing area-based plans and considering synergies between the schools estate and access to the schools estate by local communities. The health sector is seeking to develop health-based plans.
770. Why cannot physical activity be a common theme that will run through each of those area plans? The last thing that we need is three sets of plans pulling in three separate directions. We need to ensure that sectors work together to organise physical activities to combat the rise in obesity. We must ensure that sports coaches can work in schools and that teachers understand what GP referral schemes are doing. Our health professionals must understand what is happening in the sports sector and the education sector. As Eamonn said, that means that we must have one organisation — a group of people — coming together to share that information and make the investment decisions together.
771. Professor McCartan: We are in a fortunate position in Northern Ireland, because Sport NI and others have developed programmes that clearly address the issue of obesity through the principle of increased physical activity. Obesity occurs when the energy taken in is in excess to the energy going out. Over the past few years, we have identified programmes to cater for various sectors. We have several target group areas, which include: activities in relation to play; people who drop out of participation in physical activity and physical recreation; the more traditional sedentary population; and, as I get older myself, older people. We have had considerable success in those target groups.
772. Mr News: Departments are sometimes averse to investing in high-risk projects. Sport Northern Ireland is a development agency, and we see it as part of our remit to take those risks and to invest in areas in which there has, perhaps, not been a track record of investment. Many of our investments in recent years have been evidence-inspired, because we can see that there is a problem, and we believe that we can make a difference.
773. More adults need to be involved in physical activity. However, the way to achieve that is to take a long-term view, so we need to make sure that children and young people have the skills and competencies to be able to be involved in sport and physical activity. Young people need to be physically active and to go on the family weekend cycle ride. Young people learn those skills in a family setting and in a school setting, where all children spend the first 16 years of their lives, and, importantly, in a preschool setting.
774. That is why we recognise the importance of play. Over the past four years, we have invested a significant amount of our resources in PlayBoard, and together we have involved 4,000 children and young people under the age of eight in the physical activity programmes. Much more importantly in our view with regard to sustainability, 332 play workers are now trained and competent in using physical activity programmes. That is the legacy.
775. Play workers are not the only people who have an influence on children and young people. The single most important influence on children is, perhaps, their role models and those they see around them. Those are their peers and their parents. That is why one of the dropout points that we identified in much of our research has been among post-natal mothers and young mothers in particular.
776. We invested in a project in the upper Springfield area of west Belfast and into parts of north Belfast in which, through 10 community centres, 100 young mothers aged 16 to 35 have been involved in post-natal physical activity programmes. Crèches are provided so that mothers and their children are not separated. Although one might think that those are just babies, toddlers also go along to those classes. They watch their mothers being active and enjoying physical activity and see that as a positive and enriching experience.
777. We have investments in Derry City Council in partnership with health action zones in the north-west, where we have engaged with more than 100 GP referrals. Rather than prescribing very expensive obesity drugs, the GP sector in the north-west is prescribing exercise in local leisure centres. We have produced several publications in recent years that highlight those developments in non-traditional settings.
778. Professor McCartan: The last time that we appeared before the Committee, we briefed you on the benefits of physical exercise and activity for mild depression. GP referrals can address some of the barriers that prevent people who are not particularly active, who are overweight and who have an issue with their body image from exercising. No one in their right mind who falls into that state wants to go to an aerobics class where they will stick out among people who are neat, trim and fit. Therefore, that one interaction with a GP, who sends patients to a sports hall or leisure centre where they are mentored, encouraged and can see direct progress, provides them with a pathway to health and fitness. We believe that that approach will become more widespread in the next five to 10 years.
779. We all know that we have leisure centres, and we all know that they are open and that people can go to them. However, that of itself is not the answer. People need a pathway, encouragement, direction and mentoring. That can be done, particularly for those social groups that cannot see the benefits of physical activity and exercise.
780. Mr News: There are projects for older people, which we describe as nifty-fifty projects. I must say that that uses the World Health Organization’s definition of older people rather than our own.
781. Professor McCartan: When John briefed me this morning, I reminded him that I am over 50 years of age. [Laughter.]
782. Mr News: I am treading on thin ice.
783. Rates of physical activity participation show a big drop-off among older people. One way to improve the quality of life of older people is to increase their social networks. We should give older people more opportunities to interact with their peers and prevent them from being alienated from society.
784. We have an investment with Craigavon Borough Council, which runs physical activity programmes across three leisure centres in Lurgan, Portadown and Craigavon. We have heard stories that that project has engaged older men and given them more opportunities to meet their peers. As a result, they have discussed other health problems such as prostate cancer and subjects that they would not otherwise have ever discussed in their social groupings. There are also opportunities for women to be involved in physical activity programmes, and there are 220 participants in the project in the Craigavon area.
785. The way forward is to make isolated examples of good practice more mainstream, and we must find a way to meet that challenge. How do we make examples of good practice the norm? How do we create the culture of enjoyment that is envisaged in the strategy?
786. Professor McCartan: It is a question of what we do next: how do we turn the evidence-inspired policy into practice? We want people to be more physically active as individuals, with their families, in school, in work and in communities; thereby, we will get an active and healthy society. The Committee should have cognisance of the need for the physical activity strategy to be promoted, developed, encouraged and implemented by a lead agency.
787. There is empirical evidence that obesity is on the rise and that it is a major cost to our health and our health provision. The UK Government’s Foresight programme predicts that nearly 60% of the UK population will be obese by 2050, and the direct cost of obesity is £10 billion a year. Only 32% of the UK population meet the Chief Medical Officer’s recommended levels of physical activity; therefore, almost 70% do not meet those levels.
788. Mr News: One in four children in Northern Ireland is overweight or obese. It is a startling figure that 70% of us are not physically active enough. There is talk of swine flu and pandemics, but more than 2,000 people in Northern Ireland will die this year as a result of physical inactivity.
789. Professor McCartan: There is resounding empirical scientific evidence that obesity is on the rise, and the variables that contribute to obesity are well known. The policy has been developed in places such as America, Scotland and Finland, and it could be developed quite speedily in Northern Ireland. The next trick is the move from policy to practical action. A delivery agency needs to provide single leadership. We cited the example of the Scottish Government granting £24 million over three years to sportscotland to address obesity in school. Such measures need to be implemented in Northern Ireland.
790. The Deputy Chairperson: Thank you for your presentation. You talked about a lead agency, and there is no doubt that sport improves the quality of life for everyone and that early intervention is vital in creating a culture of active participation in sport and leisure. You also talked about physical education and targeting young people in school, but physical education is often pushed to one side by an emphasis on literacy and numeracy strategies and other educational strategies. There is a great deal of work to be done on that issue. The Committee intends to discuss physical education with the Department of Education (DE) next week.
791. I know that Sport NI was to have been the lead organisation in rolling out the DCAL strategy for sport and physical recreation. The strategy was put out for consultation last year, but it has still not been implemented. What effect will the strategy have when it is finally introduced?
792. Professor McCartan: The strategy will have a significant effect in increasing participation in sport and in increasing the physical activity of our young people, although not only of our young people. Properly resourced and implemented, it will go some way to addressing obesity levels. However, it will not of itself address the problem of obesity, as resources will be spread among other issues. Responsibility for publishing the strategy lies with others, not with us.
793. The Deputy Chairperson: Do you know why it has been delayed?
794. Professor McCartan: That is a matter for the Committee.
795. Dr Deeny: I could not agree with the witnesses more. The Committee has discussed obesity many times; it is a societal problem. The danger with societal problems is that they become medicalised and are attributed to problems with health. I enjoyed your proactive and enthusiastic presentation. I am a GP. If we are serious about tackling obesity, we must increase our activity rates. I was interested to hear you talk about what you are doing in Derry city; I was aware of GPs prescribing exercise programmes for appropriate patients in Belfast but nowhere else. Therefore, it is good to hear that similar programmes are being carried out in Derry. I hope — indeed expect — that such GP prescription will be the future for all medical practices. That is what must be done.
796. I wanted to ask you about the extent of your involvement with the Northern Ireland Local Government Association (NILGA) and the various local authorities. I would like what is being done in Derry city to be replicated in Omagh or in Fermanagh and elsewhere in the North.
797. You said that some people are so conscious of their body image that they are reluctant to go into leisure centres. However, do you see a role for private health clubs, for example, in working with statutory bodies to address the problem of obesity?
798. Last week, on the radio and in the media, there was talk about the £8 million that has been spent over the past three years on drugs that doctors prescribed for those who are morbidly obese. We have to prescribe such drugs to people whose obesity places their lives in danger. I heard an individual on the radio say — quite disgracefully — that obesity drugs should not be funded at all, even though people’s lives are at risk.
799. However, prescribing drugs for obesity is a short-term solution; we need a long-sighted approach, which is where the prescribing of exercise comes in. I held a surgery this morning, although no one attended who was obese; they were all asking about swine flu. There are times when one would like to be able to prescribe exercise.
800. You talked about the lead group, which was interesting. A similar scheme has been established in Scotland. Who do you think should be the lead group? It will obviously have to be a group with a bit of clout that will be able to enforce certain measures. I am pretty certain that it is only a recommendation that schools should provide two hours of PE each week. I do not think that that is being carried out in many schools because they are placing too much emphasis on other subjects. That should become law, no matter what schools’ priorities may be as regards academic achievement. They must make sure that their population take exercise, particularly as they spend so much time in front of computers. It should not be simply recommended; it should be compulsory.
801. You are involved at council level, and you are very enthusiastic, so do think that you should be the lead group? Who should be given the money and the clout to say to councils and schools — with the backup of this Committee and the Department of Health, Social Services and Public Safety — that that is what should happen with our young people?
802. Professor McCartan: You made four or five points, and we will try to address them all. If we miss any, you can come back to us.
803. I will begin with the issue of physical activity in schools and the amount of time that is set aside for it. There has been a fundamental change in our lifestyles: we have moved from being an active society to a sedentary society. That is fairly obvious to us all. We used to do things manually, but we now have machines, cars and buses. We tend to be less active than we were previously.
804. We have one of two options: either to take in fewer calories or to do more exercise. In the past, we exercised by playing in the street and going for walks, runs, and so forth. That is becoming increasingly difficult for young people. Schools are one place in which safe, structured and innovative physical activity can be delivered. You are quite right to identify two hours of PE each week being a guideline. Some schools do it very well, and others do not do it very well at all. There is also best practice in England, where there is a two-plus-two strategy. That is yet to be implemented in our schools. Our younger children are not getting that opportunity to participate.
805. We want our younger children to be literate in maths and English, but there is no mention of their being physically literate in relation to their lifelong skills and competencies of keeping themselves healthy and fit for purpose. What we are trying to advocate — particularly in our schools — is the concept of physical literacy. Although games may be involved, it is not about competitive games; it is about developing young people’s physically literate skills of running, jumping, throwing, landing, rolling and participation in fun physical activities that will encourage them and demonstrate to them the benefits of physical activity and exercise.
806. That is an issue that we have to address with those who are in charge of education. In our opinion, we have to increase the level and opportunities for our young people in schools through physical education. We have to improve the quality of the delivery of physical education.
807. Mr News: You asked about working with district councils and NILGA. In the past two or three years, our relationship, and the way in which we work, with district councils has been strengthened. In the past 12 months, we have been conscious of the changes that are on the horizon in relation to the restructuring of local government and the move to 11 district councils.
808. In October 2008, Sport NI announced a major investment to increase participation in physical activity programmes. Over the next five years, £15 million will be invested in the Active Communities programme, the purpose of which is to reduce some of the health inequalities that are the result of low rates of participation. Active Communities is not about traditional games or sporting activities. District councils will be given money to develop the appropriate partnerships in those consortia areas.
809. We have asked each of the 11 consortia to submit implementation plans to us. We are receiving some innovative plans in which district councils are working alongside education and library boards to develop physical literacy skills, play programmes, nifty-fifty programmes, targeting sedentary populations, health action zones and neighbourhood renewal partnership areas across Northern Ireland. There are some sport-specific ideas, but we are also receiving more enquiries about physical activity leaders.
810. The settings are important; not everyone wants to go to a council-owned leisure centre, but neither can everyone afford to go to a private health club or leisure centre. The health inequalities across Northern Ireland show a definite correlation between socio-economic status and participation in sport and physical activity. We are trying to encourage people to use the rich natural environment. We want more people walking along the towpath in Belfast or using our parks and the Northern Ireland countryside. Although the traffic on the roads is increasing, we still have a rich network of country roads and minor roads on which people can walk or cycle. We are trying to encourage greater use of the Mournes and the Fermanagh lakelands for non-traditional activities.
811. Professor McCartan: The review of public administration will provide new structures in Northern Ireland, particularly for our local authorities and district councils. A central tenet of the review is community planning. Sport Northern Ireland can take the lead role in the development of a physical activity strategy in partnership with the district councils and their agents. In that way, we can establish the major objectives, key performance indicators and a level of accountability as has been experienced in Scotland.
812. The Deputy Chairperson: I remind members that we have only 15 minutes left in this evidence session, and four members want to ask questions. Please keep your questions and answers succinct.
813. Ms S Ramsey: I have a load of questions, but I will go through them quickly.
814. The good thing about the Committee’s inquiry is that we can make recommendations to other Departments and Ministers. Some of the issues that have been raised are cross-departmental in nature. I am not as confident on the issue of local councils as they sit at the moment. I agree that change will occur as a result of the restructuring of the councils, but quality is the cornerstone. The provision of play areas is a big issue in my area, so I am conscious that, although Sport NI is giving them £15 million, the councils are off the hook when it comes to providing play facilities in some areas.
815. I agree with you; your written and oral presentations send out a clear message that Departments have not had a joined-up approach to the issue. We can see that in the conflicts about the extended schools programme and whether it is the responsibility of the Department of Health, Social Services and Public Safety, the Department of Education or the Department for Social Development. Addressing the lack of play spaces and leisure facilities will cost money. The issue of planning is missing, and it must play a key role. It seems to be easy to get planning permission for a fast-food outlet, a pub or a club in disadvantaged areas. We must also challenge the fast-food mindset and easy access to such outlets.
816. We can tie some of those issues into the cutbacks in DCAL’s budget — money that is being taken away because of the 2012 Olympics. That has a negative impact on communities here. Your submission states that people have easy access to the wrong food; what does that statement mean in the context of advertising at sporting events? How do you judge which companies advertise at sporting events? Fast-food outlets advertise prominently at some of those events. By the way, your presentation was useful.
817. Professor McCartan: I will try to address all those issues; however, if I do not, let me know.
818. You asked about planning and fast food. Although this is anecdotal, I saw a report on the news last week in which a local authority closed down a kebab shop because of its proximity to a post-primary school. That seemed an eminently sensible move, because, although the school was trying to provide high-quality low-fat food, the children were buying the fast food.
819. Ms S Ramsey: Will you provide details about that?
820. Professor McCartan: The shop was closed down. I will obtain the details; I do not have that with me. Planning is important and is addressed in Sport Matters.
821. Mr News: Sport Matters recognises the need to plan an environment that is conducive to physical activity. In many modern buildings, an escalator is the first mode of transport that greets people. Architects who design buildings should place stairs at the forefront rather than the escalator.
822. On a more serious note, when planning permission is issued for new housing developments, the situation should be avoided in which ball games are not allowed on green spaces. Play facilities should be placed on those green spaces at the heart of the community, where parents know that their children can play safely. We should build cycle paths to allow people to cycle, rather than take the car, into the town centre. We must ensure that we have a public transport infrastructure, through which people can take a bus to the train station and carry their bike on the train. In the long term, those decisions will create a situation whereby society, by default, encourages a culture of physical activity.
823. Physical activity should not be considered a bolt-on; we must plan for such a society now, because it will be cheaper in the long run. If we bring that notion to the school setting, we need to ensure that, in planning our schools estate, school facilities are accessible to the community. We need to create an access point to the school — one that does not entail opening the whole facility — through which adults and children can use the school facilities. There are technical solutions to all those issues. However, we must step back and draw breath before we put pen to paper and realise our aims. We want to create one set of facilities on a shared estate that can be used by everybody and that encourages them to be more physically active.
824. Professor McCartan: The power of advertising is massive, particularly on young people. Ms Ramsey is correct; advertisers recognise the strength of sport and sporting events, and, therefore, they want to be associated with major events such as the FA Cup final, the All-Ireland Senior Football Championship final, the Heineken Cup, and so on.
825. The relationship among sponsors, advertisers, event organisers and governing bodies has been successful. For example, the Gaelic Athletic Association has a strong view on the advertising of alcohol and will move to alcohol-free sponsorship in the next couple of years. Sport NI has a direct relationship with the Belfast city marathon. Although Coca-Cola sponsors that event, all parties to it, including Belfast City Council, have encouraged the sponsor to use Deep RiverRock — which, as we know, is water — to promote the event, because we perceive the consumption of water to be more healthy than the over-consumption of fizzy drinks.
826. Sport will have to address that huge issue. The marketeers and advertisers see a direct connection between major sporting events and their target markets. They buy the events and the advertising, and they promote their products. Sport has become conscious of that, and it has become conscious of its own social responsibility. I hope that alternative ways will be found to do that in the years ahead.
827. There has been a reduction in lottery funding because of the 2012 Olympics, and that has affected funding for Sport Northern Ireland. The Northern Ireland Assembly has given £53 million for the creation of elite facilities. Although a reduction in funding is always sad, we are glad to have been given £53 million, which, we hope, will see much-needed facilities being built right around Northern Ireland to meet the sporting and local needs of the community.
828. Mr Gallagher: My points relate to physical education and the school curriculum, which we have touched on before. First, what is taught in PE lessons? It is not enough simply to provide football. When children leave school, about 10% or 15% of them will continue to play football. Children must be exposed to a range of activities in school so that, if they discover that they get enjoyment and satisfaction out of playing badminton, dancing, swimming or whatever, those experiences are provided at that stage.
829. Secondly, there is the issue of a minimum of two hours a week for PE. I agree that there should be an absolute minimum of two hours a week for physical activity for children because it will be an important aspect for the rest of their lives. There are 25 hours in the school week, and the Department of Education, or those who advise the Department, tell us that, at Key Stage 3, pupils must have access to 24 subject areas. Clearly, that has a negative effect on having two hours of physical education available for young people.
830. My views on that would take about three hours to explain, so I will condense them. It is nonsense to believe that we can educate children in 24 subjects over 25 hours a week. The end result is that they will have experienced a whole lot of everything but they will have learned very little about key areas. However, the report will be based on all our submissions and evidence sessions, which is why I return to those two areas — the minimum amount of time necessary for physical education and the quality of the physical education programme provided in schools.
831. Professor McCartan: Mr Gallagher’s comments are exceptionally consistent with our own. We believe that two issues must be addressed in relation to the quantity of physical education in schools. We are strong advocates for the provision of two hours during the curriculum time and two hours post-curriculum time. Above all, we are keen, and we are committed to the quality of physical education. It is incumbent on those who are tasked with, and have the privilege of, teaching physical education that they do so for all children, not just the talented. They must expose children to all the physically literate skills and competencies required not only to play sport but to carry out a worthwhile role in society. Dexterity and fitness are important for pupils who take up manual jobs.
832. Sport Northern Ireland strongly supports the concept that there must be an increase in the quantity of physical education. However, of itself, quantity will not be beneficial without an improvement in quality. We all know and can relay examples; for instance, my wife managed to avoid physical education for the bulk of her seven years at post-primary school. She proudly boasts that she did it only twice. [Laughter.] One must ask why that is the case. It can only be that sport was not presented to her in an attractive and inclusive manner. Therefore, if she did not like competitive games such as football or camogie, there were no alternatives. There is an absolute host of alternatives.
833. A prime example of how to succeed in a non-keen, non-competitive sport is Dawson Stelfox. He was a smallish build at school, and he did not play rugby, hockey or cricket. He merely went on to become the first Irishman to climb Mount Everest and the first British man to climb Everest by the east route. Sport is fortunate to have a range of physical activities that can attract and develop skills and competencies, wherever they lie, in individuals in our schools. Therefore, we support the provision of two hours of physical education every week.
834. Mr News: I will add to what Eamonn said in relation to two hours of PE. If we do not know how much PE every child receives, the adage that I heard recently applies: no data, no problem, no action. We must measure how much PE is taught in our schools. The evidence that we have seen recently leaves no doubt that, where the PE curriculum is delivered well, it is delivered exceptionally well. Primary-school teachers are some of the most resourceful people in this part of the world. Their integration of various subjects into a school day is one way in which we envisage achieving a culture of lifelong enjoyment of sport and physical activity.
835. Sport Northern Ireland recently did some work with education and library boards, during which a new resource called Activ8 was introduced, which members may have seen on television a few weeks ago. Activ8 gives teachers a resource that encourages children to be physically active for 60 minutes each day, in line with the Chief Medical Officer’s recommendations. However, it does so in a way that is part and parcel of the school day by providing examples of how to build sport and physical activity into numeracy lessons, how to encourage children to write about their weekend physical activity, thus helping the literacy curriculum, and how to encourage pupils to be aware of the world around them and to contribute as active citizens. There are innovative ways in which physical activity can be built into the curriculum. It does not have to be about two hours of ring-fenced PE each day. The key is 60 minutes’ physical activity every day, and two hours of physical education a week is part and parcel of that overall programme.
836. A challenge for us is to ensure that the message does not become too convoluted for those working in education, health or sports that they confuse 60 minutes, two hours, seven times a week, five times a week and five pieces of fruit a day. There must be a clear, simple, consistent message about how to make physical activity the default position.
837. Professor McCartan: What was your adage about a lack of data?
838. Mr News: No data, no problem, no action.
839. Mr Gardiner: Thank you very much for your presentation. Professor McCartan, you mentioned Craigavon, and I declare an interest as a member of Craigavon Borough Council. I was pleased that you did mention it, because the council has three leisure centres, and Banbridge — which is in my constituency — also has one. However, the real issue is not about the facilities themselves but in getting people to use them. For example, Craigavon has the only artificial ski slope in Northern Ireland, yet some people do not know that it exists. Craigavon also has some of the finest walks around the shores of Lough Neagh, and water skiing is available there and on the Craigavon lakes.
840. I want more of a concentration at school level. We must bring those children on and get them to use those facilities. What representation has Sport NI made to the schools to sell your wares or to tell them about some of the things that they can do to keep themselves active and fit?
841. Professor McCartan: Craigavon has a tremendous set of facilities: indoor, outdoor and natural. Furthermore, Craigavon was very fortunate to have an excellent sports development officer in the shape of John News, who developed a good sports development strategy before coming to Sport NI. I congratulate the work of Craigavon —
842. Mr Gardiner: He was properly trained then? [Laughter.]
843. Professor McCartan: He certainly received very good training.
844. Mr Gardiner: Lurgan Park, the largest park in Northern Ireland, also won a green flag award in 2008.
845. Professor McCartan: It did indeed.
846. The problem that you identified regarding the use of leisure centres is not one that is restricted to Craigavon but is experienced across Northern Ireland. For sports development to succeed, each district council must have a robust sports development strategy, and those strategies succeed best where they are people-focused rather than facility-focused. There is a need for facilities, but the “build and they will come" philosophy of sports development, which was prominent in the 1970s and 1980s, has now been replaced with a philosophy of “build and provide development officers, and they will come and multiply".
847. You also — quite rightly — touched on the issue of schools, with which there must be a crucial relationship. Indeed, we are trying to establish a strategy through Youth Sport where there is a relationship between schools, communities and sports clubs, and an iterative interaction with schools and clubs using community facilities. We encourage that, and, in our community planning under the RPA, we have asked the new authorities to take a slightly different approach. Our recommendation is that they continue to invest in facilities but that they also combine that with a strong and robust sports development plan, bringing the three key elements of school, community and club into an interface with them.
848. In that area, we have made representations to the Bain Review and the Department of Education with respect to facility provision. Our view is that there should be one public sporting estate as opposed to a local authority estate and an educational estate, because of the limited capital capacity. Sport NI contends that, if we can think smart, we can build a school facility that can be used by the school during the day and by the community in the evenings or at weekends.
849. I am originally from west Belfast, and one of the grammar schools there, in which I taught, has four grass pitches, a running track, a dust football pitch, a swimming pool and two handball courts, yet those facilities were closed during the summer, Christmas and Easter holidays. It would seem sensible that, if we are going to plan the development and use of our estate, we do so in the context of a holistic front and examine community and educational uses. In planning for the future, it is possible to plan facilities that can meet the needs of both, but that will require more investment in educational facilities, because the Department of Education currently builds facilities according to its green book. Although those facilities may be ideal for primary-school children or post-primary schoolchildren, they are not ideal for grown adults. Broadly speaking, an additional investment would be required to make them so, and we are trying to work with the Department of Education on that. Sport Northern Ireland has a significant level of capital funds available for over the next 10 years that, if combined with help from DE, could cater for the needs of schools and the community. That would stop the regrettable underuse of facilities that you correctly identified.
850. Mr Gardiner: You did not tell me how you will communicate with the schoolchildren to encourage them to become involved.
851. Mr News: Part of the Activ8 programme that was launched recently involved increasing the awareness, through publications, of primary schoolchildren and their parents of the Web-based resource, www.activeplacesni.net. Over the past few years, Sport NI has undertaken an extensive data-gathering exercise. To identify the exact location of all the recreation facilities, we contacted and worked with all district councils, private sports clubs, governing bodies of sport, private providers and the education sector. We have now mapped that information to a Web-based geographic information system (GIS). A child or parent can go to the website, type in their address or postcode, and the resource brings up a list of all the available facilities in their area. People being aware of where the facilities exist is at least a start. The next step is to assess the quality of the facilities.
852. We engage with schools by working closely with each of the education and library boards and the inter-board physical education panel to consider opportunities for engaging with children and young people. However, as we are aware that the PE curriculum must also be delivered, we are also assessing its quality. One of the actions identified in the draft strategy for sport relates to teacher education. I mentioned that some of the most resourceful people in this country are primary-school teachers. However, they leave their initial teacher training without the skills, competence and confidence needed to deliver PE training because they have not specialised in it. One of our fundamental tasks is to examine that initial teacher training. Teachers can take various bolt-on continuing professional development (CPD) courses to develop their skills, competence and confidence, thereby enabling them to build physical activity into the school day. While continuing to specialise in geography, mathematics, English or whatever their subject happens to be, we can provide ongoing remedial work. We must determine where the challenge lies and consider a review of initial teacher education.
853. That is how we engage with schools and support our colleagues. We invest in the five education and library boards to help them to support teachers, and we provide resources for teachers and schools.
854. Professor McCartan: On that point, we hope that, by 2012, 100,000 additional primary schoolchildren will be participating in sport through the Activ8 programme. If the Committee deems it worthwhile, we will leave the relevant information with you to consider.
855. The Deputy Chairperson: I am conscious that we are behind schedule, but two members still want to ask questions. Do you need to leave, or are you OK for time?
856. Professor McCartan: We are OK.
857. Mrs Hanna: I will be brief. Good afternoon, Eamonn and John. You are most welcome, and thank you for your presentation.
858. Much has been said about trying to prevent children from becoming overweight and good programmes. However, it seems to be a case of ensuring that the programmes are implemented. You talked about physical literacy and said that children are skipping, running and jumping. You also mentioned that it is important to make exercise fun, so that children want to continue with it when they get home from school.
859. You referred to the lack of leadership. We must figure out who should be tasked with delivering the programmes. The Committee will hear from educators next week, when we can put the same questions to them. You said that Scotland is slightly ahead of us. Has Scotland managed to task a specific person or group to take on that leadership role to ensure that physical activity takes place in all schools? It seems that much good work is being done and many good programmes exist but that they are not being rolled out in all schools. Who will intervene at the early stages to prevent obesity in young children? I know that we have to pick up the pieces in respect of some children, but we need to try to prevent it happening in young children.
860. Professor McCartan: When we were preparing for the evidence session, I reminded my colleagues about old-fashioned quality control. I used to teach business studies, and, in old-fashioned quality control, we went through the manufacturing process, looked at our product, and, if it was not up to standard, we threw it out. There was no prevention involved in the process, and there were no interventions along the way to put the problem right. Therefore, we advocate the early-years approach that you talk about, including skills for life, where we develop physical literacy — that is, running, throwing, jumping, landing, understanding the need to eat healthily, understanding the need to eat five pieces of fruit a day and to include fibre in their diet, as well as understanding the need to have sleep.
861. You said that it is crucial to have fun. People sometimes forget to have fun when they are participating in physical activity and leisure. People tend to repeat the things that they enjoy, which is why some of us eat too much or drink too much. Therefore, it is important to get the healthy lifestyle issue instilled into our young people, not just during their primary or post-primary years but for their whole lives. We need to develop a knowledge and understanding of the benefits of physical activity and not expose children at an early age to competitive team games. We are opposed to the exposure of very young children to competitive team games, because it quickly divides them into children who can play them and those who cannot, and the children who can play them will continue to play them for the rest of their playing lives, and those who cannot play them will be exiled to the side to stand in the cold and the wet. We are very much opposed to that.
862. Leadership is required, but, in Northern Ireland, we tend to work in partnership. As John said earlier: no data, no problem, no action. An issue that arises with partnership is the lack of action, because everyone is involved, yet no one is involved. Therefore, I like the idea of getting an organisation to be held responsible for taking the lead, albeit it will work with other partners in execution and implementation, but, ultimately, it will be held responsible. In Sport Northern Ireland, we are willing to take on that responsibility. If there is someone better to do that job, that is fine, but we are willing to take it on and to be held responsible in the same way as sportscotland is in Scotland.
863. Mrs Hanna: Is it working in Scotland?
864. Mr News: It has worked in Scotland as a catalyst for action. Sportscotland put the resources into schools, and the money came from the health budget. As a result of that action in schools, principals have seen a step change in the attitudes of parents and pupils. Some years ago, Tessa Jowell talked about tackling the “poverty of aspiration", and principals have reported that pupils and parents in the communities that they serve now want something better, and they are making more proactive choices.
865. There was an earlier question about planning and fast-food outlets. The Active Schools programme is about adopting a whole-school approach. It is not simply about saying that we have to ensure that every child must have two hours of physical activity or physical education. It looks at the diet and nutrition of school meals and the roads infrastructure around schools. There is an exclusion zone for cars around schools at drop-off times in the morning and at pick-up times in the afternoon. Bike sheds have been installed, and all the broken windows have been fixed. Representatives went to local councils and said that they did not want any fast-food outlets licensed within 200 yards of the school gates. They said that they wanted to make water available free of charge to all their pupils, and they distributed water bottles to them.
866. Therefore, it was a whole-school approach. It was about changing lifestyles, and it has delivered dividends. That happened because there was leadership, resources were invested, someone was made accountable, but the accountability was for others to act as well. Therefore, the school, the local council and health and social services board had to take action. It was about joining that up and saying that that organisation — in this case, sportscotland — was accountable for the success.
867. Mrs McGill: I have listened to everyone’s contributions and responses. Although schools and education play an exceptionally important role in tackling obesity, there is more to it than that. All the blame cannot be levelled at the door of schools.
868. I was looking at the priorities for action and the implementation plan in your submission. I repeat — and I have a reason for saying this — what happens in schools and the role played by the Department of Education is critical. Sport NI also has a vital role to play. You suggest that every child should get an additional two hours of, presumably after-school, extra-curricular sport and physical activity. How will that be achieved in rural areas such as mine? I would like you to be able tell us that Sport NI will step in to assist in some way. Perhaps it will, and, if so, I would welcome its contribution.
869. You also suggest that all newly qualified teachers should have the necessary training to deliver physical activity programmes in schools. How would that work? You have made that a priority for action and implementation. Have you spoken to the Department of Education? If you consider it to be a key priority, I would have thought that you would have dealt with it before the Committee began its inquiry into obesity.
870. I apologise for not being brief, but I ask that your answers be brief.
871. Professor McCartan: I shall try my best to answer the member’s questions as briefly as possible. We have spoken to the Department of Education with respect to teacher training, and it has accepted, and will implement, our proposal.
872. Mrs McGill: Will that apply to all primary and post-primary teachers? What did you recommend?
873. Mr News: In the draft Northern Ireland strategy for sport and physical recreation, there is a table entitled “Key Steps to Success". Those implementation suggestions are eight out of 100 key steps to success, so you are absolutely right to say that schools are not the only answer. However, those key steps to success have come about as a result of positive engagement with all Departments, particularly the Department of Education.
874. The Department of Education and the education sector recognise that reviewing initial teacher education is a key issue in delivering the high-level target of halting the rise in obesity in Northern Ireland by 2013. Therefore, they are signed up to implementing that proposal. The next challenge is to make it happen. For instance, when will the Department of Education undertake the review of initial teacher education? Several hours a year are already set aside in teachers’ initial teacher training to educate them about physical activity and physical education. We should step back and consider what teachers are actually trained to do in those hours. It may be that the content of that training must be changed, or we might have to increase — from six hours to eight hours per annum — the amount of training that teachers receive in physical education. It is about what we do and how we do it, and the Department of Education is signed up to that.
875. Professor McCartan: The policy and principle have been agreed, but the implementation has yet to be worked out. All new teachers will receive that initial training.
876. I will try to answer the second point about Active Schools. We all have to work smart to get the biggest bang for our buck. There are four sectors that we must address if we —
877. Mrs McGill: I am sorry, Chairperson. I was asking whether Sport NI would have a role in promoting the two hours of extra-curricular sport and physical activity that it mentions as one of its implementation priorities. I am not sure whether the following priority, which is to establish a network of Active Schools, is the same thing.
878. Mr News: The short answer is yes. Many of the investments that we have made over the past number of years in governing bodies of sports, community and voluntary organisations and district councils have been about trying to put a network of people in place to help to deliver that two hours of extra-curricular activity and make use of the £15 million that was earmarked for the Active Communities programme. That programme is not about delivering the PE curriculum; we are clearly focused on the opportunities for one million participants that can be delivered through that programme over the next five years. Approximately 100,000 people will be involved in that extra-curricular programme: some of that number will be children and young people; and some will come from the other under-represented groups that we mentioned earlier — older people, women, people with disabilities and people who live in rural areas.
879. The Deputy Chairperson: Thank you very much, gentlemen. The session has been very informative and will help our inquiry to move forward.
880. Professor McCartan: Thank you. I wish the inquiry well.
14 May 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
Ms Gerry Bleakney |
Public Health Agency |
881. The Deputy Chairperson (Mrs O’Neill): We now move to the inquiry into obesity. Today’s witnesses are from the new Public Health Agency: Dr Eddie Rooney is the chief executive, Dr Carolyn Harper is the director of public health, and Ms Gerry Bleakney is a health promotion commissioner.
882. Dr Eddie Rooney (Public Health Agency): I will give some context of where we are as an agency, because it may have a bearing on how much we can tell the Committee. The Public Health Agency has been in existence for six weeks. The agency has inherited many strands, but it is still putting its own stamp on priorities and how those will sit in its business plan. That work has become a little more difficult over the past couple of weeks because we did not quite expect that element of health protection — swine flu — to take such a high profile so early. Nevertheless, we are trying to move on as quickly as we can to establish the agency’s priorities. We will hold our second board meeting next week to try to progress that as quickly as we can.
883. There is no doubt that tackling obesity will be one of those high priorities because it is a priority for the Department and the Executive, and we know that it is a vital health issue, particularly in our area of health, which assesses prevention and wider public health. It is not an easy issue to tackle because it is so embedded in our lifestyles. It has taken many years to reach our current position.
884. My colleagues Carolyn and Gerry will very briefly take us through the presentation. One issue that they will address is how far we have moved towards becoming a sedentary population over the past 50 years. We will not be able to turn the tide quickly. However, much has been learned. We know that we must plan, and we must demonstrate to the Committee that we are on top of the task and the level of attention that we are giving to it.
885. At the outset, it is clear to us is that the issue will not be solved by the Public Health Agency or the health sector. It is at the core of cross-departmental and inter-sectoral working. That will inform how we approach partnerships with other organisations and bodies. That will not happen through strategies. For too many years, we have been involved in different aspects of nutrition and physical activity. I chaired the Fit Futures steering group, and I emphasised its cross-sectoral nature.
886. We must link strategic words with community action. One advantage of having an agency such as the Public Health Agency is that we can straddle that link. The agency is an implementation body, and we realise that we must work at ground level to have an impact. That will guide our approach as we start to develop our own planning system and our actions in relation to obesity.
887. We will take members through some key parts of the strategy. We are very happy to take as many questions as members can come up with. Our responses will be on the basis of it being very early days for us. We do not have a blueprint that demonstrates our solution, but formulating that is a priority.
888. Dr Carolyn Harper (Public Health Agency): Members have received much information from other presentations, so I do not want to spend too long on that. I will then highlight some programmes and interventions in Northern Ireland and indicate the direction in which we think our own actions and those of others need to go.
889. It struck us that, when daily activity levels of the current population are compared with those of the population 50 years ago, it equates to running one marathon each week. That is a lot of activity and a lot of calories being burnt.
890. The key facts are: 60% of adults and one in five primary 1 children — four- and five-year olds — is overweight or obese. There is increasing evidence that the impact of obesity is similar to that of smoking more than 10 cigarettes a day. Therefore, it is not simply an aesthetic issue; it is a genuine health issue, and there are some health conditions for which the risk is increased among those who are overweight or obese.
891. There is also a significant impact on our health services. I need to draw your attention to a correction to one figure in paragraph 3 of our paper. The paper states that the current cost to the Health Service of anti-obesity drugs is £0·5 million a year; the cost is, in fact, £0·5 million a quarter, with a total figure of £2 million a year. Overall costs to the economy have been estimated at some £500 million a year, much of which relates to lost working days.
892. Action is focused on different settings and target groups. The Health Promoting Homes initiative is intended to get the entire family involved in changing behaviour and understanding the need to do that. The Healthy Steps for Life programme tries to embed some of those good habits in children at an early age. Eddie mentioned the need for community involvement, real engagement and ownership. There are schemes that are targeted at communities to own and take a lead on the issue. The workplace is another key setting.
893. FRESH is a weight-management programme for 11- and 12-year-olds. For children in their early years, there are programmes that are targeted at playschools, nursery groups, childminders and those who interact daily with young children. Nutritional standards have been introduced for school meals, and we are trying to address where children spend their days, both in school and at home.
894. Our approach is to prioritise obesity prevention and to own it at both central Government and local government level. It is a genuine issue that needs to be tackled with co-ordinated action across all Departments and with central Government action reflected at local government and within local communities and neighbourhoods. Obesity prevention needs to be brought down to neighbourhood level. A key task over the next few months will be to strengthen our existing relationships with local government, councils and other partners in education, transport, planning, and so on, and to translate that central direction into action on the ground.
895. On the matter of working with communities, I have highlighted the approach in France with the Ensemble, Prévenons l’Obésité des Enfants (EPODE) programme, of which you may have heard. It is concerned with planning the environment to promote walking and cycling. Parks, leisure facilities, and so on, have their part to play in tackling obesity. That emphasises the importance of cross-Government working.
896. Families are a priority. Parents influence what their children eat, and children influence their parents. Our approach is to give practical skills and knowledge of what a normal diet is and to address the shift towards fast food and larger portion sizes, which, subtly and latently, have become normal behaviours and patterns. It is about reframing and helping people to understand what a healthy, normal diet is.
897. Although some interventions are in place, it is essential that we are able to extend their scale and sustainability. Evidence has shown that 3,000 four- to five-year-olds and 4,500 11- to 12-year-olds already require interventions because their habits and behaviours are creating weight problems for them.
898. We cannot tackle obesity through single, small-scale interventions. Given the limitations of available funding, that approach has had to be taken. However, we want to take a dual approach. First, we want to draw in additional funding, and, secondly, we want to connect the existing services and programmes not only in the health and social care service but in transport and education to get the most of that resource. We want to take a fresh look at how we connect people to all available services.
899. Another key issue concerns measuring the impact of programmes and knowing what does and does not work. That will require an additional focus and some specific attention. Without that, we will simply continue to hope for the best rather than tackle the issue in a cohesive way.
900. We need to learn from effective practice elsewhere. Evidence has begun to emerge from some areas about what does work. We need to think that evidence through, accept it at a Northern Ireland, cross-Government level and then make sure that it is implemented at a local level. Finally, it is important that we bring that evidence base to others so that we can inform policies.
901. Our paper lists some immediate priorities that I will not go through. However, I want to draw out some concluding points. As a society, we cannot treat ourselves out of this situation by prescribing drugs or performing operations; rather, we must focus on prioritising prevention.
902. A key lesson to be learned from other areas where there has been some success in tackling obesity is that it is about communities and neighbourhoods. People must recognise and accept that they own obesity and that is not done onto them by health and social care professionals. They need to accept that obesity is much more fundamental than an aesthetic issue; it is a health issue of which they have to take ownership for their sake and the sake of their families. Those are the key points.
903. The Deputy Chairperson: The Public Health Agency has a key role to play not only in tackling obesity but in addressing many others issues such as prevention and getting that message out early through education.
904. You referred to the good evaluation of the EPODE programme in France and said that the programme resulted in overweight boys experiencing a 50% decrease in obesity, which is a good statistic. How big is that programme? Was it very costly to implement? Could it be easily adapted for a pilot scheme here?
905. Ms Gerry Bleakney (Public Health Agency): That is one programme that is being trialled, and those are preliminary results. Some health professionals from England are in France to evaluate the programme fully. The preliminary results look very promising; however, we will have to wait for the full results.
906. As regards evaluation, many health improvement initiatives that have been used over the years have not been as good as they should have been. We need a gold-standard-type agreement on the sorts of issues that we should be building into evaluations, and then we can move towards achieving that across the UK. The Institute of Public Health in Ireland, the all-Ireland obesity observatory, the Public Health Agency and others will work together to achieve that for the country.
907. Mr Easton: During the inquiry, I have harped on about a particular point that I will also make to you. The work that the agency does is all well and good, but it is really designed only to try to keep a lid on matters.
908. No matter what we come up with in the inquiry, the situation can be resolved only by getting everyone to exercise and, more importantly, to force the food industry to limit the fats, sugars and salts in their produce. Until we do that, other measures will only keep a lid on the problem. I know that you cannot force the food industry to act, but what action are you advising the Department to take? Can we force the food industry to put the right ingredients in their foods, because that is the way to tackle obesity?
909. Dr Rooney: In many ways, you have hit the nub of the issue. If you think of all the issues that we tackle as mathematical equations, obesity should be one of the easier ones to solve: restrict what and how much people eat and get them to exercise. Those two measures will solve the problem.
910. However, it is difficult to tackle obesity, because there are so many players and interests, and because we are trying to turn the clock back on 50 years in which we have been going in a very different direction. It is also difficult to tackle the problem because we are dealing with fundamental aspects of our culture and what makes people tick. Even some of the basic aspects of tackling obesity that look simple turn out to be complex. For example, early investigations pointed out the importance of early years and early intervention. In the research that formed part of the Fit Futures initiative, which included kids as young as two and a half years of age, the basic messages were understood, such as the difference between good and bad. The role of enjoyable activity as part of a solution was also well understood, but it is not necessarily matched by the way in which society works. One cannot deal with children if one does not deal with parents and carers at the same time.
911. We are trying to turn the tide on many historical practices and behaviours at the same time as dealing with the issue at its source, which is not easy. The problem is multifactorial: for example, people’s rights are highly valued, but where they bring people into clear areas of risk, we have to turn the tide. That points to community-based approaches, which is why we are interested in examining some of the evaluation work and international research. There are lights in the tunnel; the holistic approach seems to be showing some benefits in countries such as New Zealand and Finland among others.
912. Research is a key element of the agency’s work, and we need to sharpen up our research on what measures work here and make sure that we do everything to publicise them. We are dealing with several interests and factors, many of which we do not have direct control over but still have to influence.
913. Mr Easton: We all know the health message, and I am fit at the moment, because I am knocking on doors and canvassing for the European election. However, I am in the habit of eating what is put in front of me; I do not look at food packaging and will probably die 10 years younger as a result. That is why legislation on food packaging is required; I need help to eat the right food, because it is too convenient for me to eat the wrong foods. That is why I encourage you to force the Minister to do something about that.
914. The Deputy Chairperson: We must all be very healthy, because we are all out knocking on doors.
915. Dr Deeny: As a GP, I want to be able to prescribe exercise regimes for patients where appropriate and play a role in preventative medicine as opposed to drug treatment. That is part of the future and does occur in some areas in the east of Northern Ireland.
916. The EPODE programme mentions boys, but are there any results for girls? As I have mentioned before, I am a little worried about obesity in girls: two young girls admitted to me in front of their parents that they smoke to suppress their appetites, which is a worrying development. I do not know whether girls get as much exercise or are as proactive as boys. Why does the EPODE programme make specific reference to boys?
917. An astounding number of people do not eat fruit or say that they do not like fruit. The same people will say that they feel guilty that they are not eating the recommended five portions every day. They are even unsure about what constitutes five portions, so will you quantify exactly what is meant by five portions? Some people think that it means eating five meals, but the five portions could be contained in two meals.
918. Ms Bleakney: Primary care and secondary care are able to make referrals. Referral schemes have been operational across Northern Ireland; there is a scheme in the eastern area and part-schemes in the southern and northern areas. As a new agency, we need to draw on what has been best practice and what has produced good results. We will try to share that information to ensure that there is an equitable provision of good practice across the region and that as many people as possible are granted access to good practice.
919. I have been heavily involved with the referral scheme in the east, but the evidence base to support it is questionable. We had already committed to the scheme when the National Institute for Health and Clinical Excellence (NICE) guidance came out, and it was then suggested that it should be run only as part of a well-researched approach. Clients from general practice, primary care and secondary care give good reports about the scheme in the east, and we think that it is working. We will continue to assess the scheme because it is an expensive intervention. It is also a potentially very cost-effective intervention given the health outcomes that it creates.
920. EPODE is a community intervention that includes boys and girls. Our paper reports the boys’ figure simply because it is the most striking; I could not give you the corresponding figure for girls off the top of my head. EPODE is a holistic project that is taken forward by the mayor of the local town or city. It develops community spirit and engagement around social action for change. EPODE is about physical activity and healthy eating rather than obesity, although its outcomes influence obesity.
921. The five-a-day message has been around for quite some time, but we need to do some more work on public awareness. There has been a difficulty in Ireland in that, although potatoes are still part of many people’s staple diet, they do not count as one of the five a day. The former Health Promotion Agency has used some very good material to raise awareness. How many grapes are in a portion of fruit? We can all visualise apples, oranges and bananas, but what constitutes a portion of kiwi or another more unusual fruit? We need to work on the public awareness of some aspects of the five-a-day message.
922. Mr Gardiner: Have you briefed families and agencies that take children into their care? What is your role in ensuring that those children, boys and girls, are properly cared for?
923. Dr Rooney: We are in the process of developing priorities and identifying target groups in the health and public health agenda. Families with children in care will be one of those groups. We will be able to provide you with more information over the next couple of months as we formulate our strategies. It will be a priority for the agency across the public health area.
924. Mr Gardiner: Do you think that that will be up and running in a couple of months? Will people be briefed, know what they are expected to do and what information to pass on?
925. Dr Rooney: We will certainly do our very best to ensure that that is the case. The agency is an action agency, and we will follow through on all development areas down to community group level. However, it is still early days.
926. Ms Bleakney: Much work has already been done for looked-after children in residential care or children who are placed with foster carers. Much has been done to make nutrition education and support available to those carers. We have identified the development of clear nutritional standards for residential care and children’s homes as a potential area of work. There are clear nutritional standards for education in schools, but there have been issues about children in residential homes. The main emphasis is on having as few children in residential homes as possible. However, we have a corporate parenting responsibility, and nutrition and physical activity are two key elements of that. Therefore, there is a plan to work on that within the next year.
927. Mr Gardiner: It is the family home that I am thinking about. When children are placed in care, what follow-up is there? Do you check whether that is being implemented to protect that child from going down the route to obesity?
928. Dr Rooney: We will certainly take that issue on board.
929. Mrs Hanna: I agree with Alex about food labelling. Often, the bargains are the rubbish food with the least food value and the most additives. There is an issue about our fondness for food and how it is used as comfort or reward. When my children were small, the thinking was that, if parents did not give their children anything sweet, they would never like sweet foods. Whether we like it or not, however, children seem to like sweet foods instinctively. It is about the culture. However, as the Public Health Agency, your message has to be about all of us taking ownership and responsibility for our own health, albeit with as much support as possible. You said that this issue covers many Departments and that much of what can be done for children is in the area of prevention, starting, for example, with antenatal classes, parents, preschool, and, if necessary, healthy breakfasts in schools. Much of that is happening. However, a lead person or agency is needed to ensure that it is happening and that its progress is monitored. Everybody is doing bits and pieces, but, unless someone is given absolute responsibility for progress, it will never come together.
930. Years ago, one of my children was involved in a piece of research. All I can remember is a man named Dr Sean Strain, and that it was carried out by the University of Ulster and Queen’s University. For a week, we had to keep a diary of everything that my daughter ate. We were not to be “good" for that week; we were to be honest. They did cardiovascular tests, and she loved being on the exercise machine. I did not hear about any outcomes, but it was a major piece of research at the time. I wonder if you know anything about it. You said that not enough research is being undertaken. It comes down to having one person in charge with the authority to involve all other areas and to monitor what is happening.
931. Dr Rooney: To have effective ownership, people need to know what to do, believe that it is right and know how to do it. We need to provide support on all three issues. We have gained a lot, and, although I would never try to turn the clock back on technology, we have also lost a lot. I have seen, particularly at community level, the loss of some basic skills. Programmes such as Cook It! try to reinstate those lost life skills. It is up to us to take that leadership role. However, it is a collective leadership; it is up to the agency to play its part, and it is up to many other people to play their parts. We have to break down the message and understand it from the perspective of people living in the community, as opposed to the message descending from on high. That will be a challenge for us. It is a thread running through the whole public health agenda. It cannot be done remotely. It must be done in communities and working with them. The agency must be able to demonstrate that it can work in that environment, and we are actively pursuing that.
932. When that barrier is broken, we have a real chance. There is a need for animation in communities and a real desire to do something. However, people struggle with how it can be achieved, and extra support is needed to make it happen. We must fill that challenging gap.
933. Mrs Hanna: I agree with you that it is about leadership. Everyone has to give leadership, but if there are no specifically dedicated people who have responsibility, it can be difficult to quantify the progress. That is what it is about. If we could see that we were improving, we could build on that.
934. The Deputy Chairperson: As there are no more questions, I thank you very much for your presentation.
21 May 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Claire McGill
Witnesses:
Mrs Maria Jennings |
Food Standards Agency Northern Ireland |
935. The Deputy Chairperson (Mrs O’Neill): I welcome Maria Jennings, deputy director of the Food Standards Agency (FSA), and Andrea Marnoch, head of the agency’s dietary health unit. You are both very welcome. I invite you to make a presentation, after which members may want to ask questions.
936. Mrs Maria Jennings (Food Standards Agency Northern Ireland): Good afternoon, Madam Chairperson and members of the Committee. Thank you very much for inviting us to give evidence. You have received the agency’s formal written submission. In the time that is available, Andrea and I will try to give you a flavour of some of the work that we are doing with the food industry and to raise consumer awareness of dietary health issues.
937. The Committee has met me previously. The Food Standards Agency is a UK-wide Government Department. It is our responsibility is to ensure that all food is safe to eat, and we also aim to protect consumers’ interests where food issues are concerned. Our local office in Belfast ensures that the agency’s principles and objectives are suitable for the needs of all consumers in Northern Ireland. We have a vision, which is that there must be safe food and healthy eating for all. For the purposes of the obesity inquiry, Andrea and I will concentrate on how the agency works to achieve the element of the vision that concerns healthy eating for all.
938. I am sure that you are all aware of the little chart that shows the eatwell plate. All our messaging is based on that plate, which is used widely by healthcare and education professionals. That chart illustrates that is a question of trying to get the balance right. We want people to get one third of their food intake from the fruit and vegetable part of the plate and about one third from the fibre part of the plate, which consists of bread, rice, pasta, and so forth. The final third should come from proteins such as meat, fish, eggs and beans, and milk and dairy products. Members will be glad to see that there is also a small segment for foods that are high in saturated fat and sugar. Our message is that healthy eating is all about balance; we are not in the game of demonising foods.
939. The agency set a number of high-level dietary health targets in its 2005-2010 strategic plan. Those include reducing the population’s intake of salt and saturated fat and encouraging improvements in nutrition labelling to help consumers make healthier choices.
940. Our work has three key strands. First, influencing food products to ensure that healthier options are made available to people so that they can make their own choices; secondly, influencing people so that they are aware that the healthy choice is the easier choice; and thirdly, influencing the environment, particularly the food environment, so that some of the barriers to making healthy choices are removed. I am sure that members will have heard about those barriers.
941. Andrea will give more detailed examples of how we influence food products and help people to make healthier choices.
942. Mrs Andrea Marnoch (Food Standards Agency Northern Ireland): As Maria said, the agency works with food businesses and their trade associations to support and encourage a reduction in the levels of saturated fats and added sugars in the foods that they prepare. For the past 18 months, the agency has been working on an energy intake reduction programme. I will discuss that programme and the effects of saturated fat on the diet. We know that on average, people eat far more saturated fat than is recommended, and rising levels of obesity suggest that energy intakes exceed energy requirements.
943. Following the success of the FSA’s work on salt reduction, the agency developed a programme of initiatives to try to reduce the level of saturated fat from its current level of 13·3% of energy intake to the recommended level of 11%. We focus on four areas of action: raising consumer awareness; promoting healthier choices; considering reformulating mainstream products to reduce their levels of saturated fat and sugar; and reducing portion sizes.
944. The agency launched a consumer campaign in February this year that targeted women between 25 and 60 years old and who are from social classes C1, C2 and D. That campaign was based on qualitative research that the agency carried out that suggested that the consumption of saturated fat was higher in that demographic.
945. The campaign was about raising awareness of the health effects of saturated fat and giving consumers simple tips on how to reduce such fat in their diets. Examples included cutting fat off meat and grilling rather than frying and grating instead of slicing cheese. I hoped that we would have feedback from that campaign for the Committee today; however, it is still early days, and the data are still being accumulated. Early indications suggest that consumer responses to the campaign have been positive and that they have understood the key messages.
946. The agency has identified the key food groups that contribute to levels of saturated fat and added sugar intakes, and it is working with the food industry on reductions in those food groups. The focus for that work is dairy products, meat and meat products, biscuits, cakes and pastry, snacks, confectionery, soft drinks and retail sectors.
947. I will give examples of how that work is progressing. Premier Foods, whose brands include Mr Kipling, Ambrosia and Sharwood’s, has reduced the saturated fat in its Mr Kipling ‘Delightful’ range by 50%. McCain Foods has reduced the saturated fat in its potato products by more than 70%, and since 2006, Marks and Spencer has removed 70% of saturated fat from a range of crisps and 30% from a range of sandwiches. Therefore, that demonstrates that a lot of work is being done in that area.
948. The agency is working with the food industry to identify opportunities to reduce the size of single-serve portions of, for example, soft drinks and sweet and savoury snacks. How we address portion sizes with the population and the food industry will be a big part of our work over the next 12 to 18 months. A large part of that work will include examining with the retail sector how they could realign in-store promotions so that healthier options are promoted. At the minute, in-store promotions can encourage the increased consumption of energy-dense, salty foods.
949. Mrs Jennings: That leads me neatly to front-of-pack signpost labelling; it deserves a special mention. The agency has been working for a long time to provide a simple signpost on the front of food packaging that will let consumers know exactly what is in a pack.
950. We started that work because consumers told us clearly that that was what they wanted. There was no front-of-pack labelling when the work commenced about four years ago. After extensive consumer research, the agency produced a simple scheme that is based on traffic lights — red, amber and green — for the four main nutrients, that is, fat, saturated fat, salt and sugar.
951. A number of retailers and manufacturers, including several in Northern Ireland, have adopted the agency’s scheme. During the same period, a number of similar schemes appeared. Consumer and health groups started to ask for one simple and easily understood scheme that could be applied to all foods.
952. The agency, in partnership with the Department of Health, Social Services and Public Safety (DHSSPS), commissioned a comprehensive independent survey that looked at all the current schemes. It took almost 18 months to complete that work, and the findings have just been published. Not surprisingly to us, the study found that a single, consistent front-of-pack labelling scheme would be most helpful to consumers. Overall, the evidence shows that the strongest label is that which combines the words “high", “medium" and “low" with the traffic light colours red, amber and green, and with the percentage guideline daily amounts (GDA), with levels of nutrients expressed as a portion of the product.
953. The full report on signpost labelling is available on our website. The agency and the Department of Health will consider the report’s findings and agree on the next steps. A public consultation will then take place, so the Committee might wish to hear from us again on this issue.
954. I will highlight briefly the work that we are doing on catering premises. People are eating outside the home more than ever before. What used to be a treat is now becoming the norm. Therefore, it has become more important for pubs, cafes and restaurants to provide nutritional information on their menus. Our work in catering premises is aimed at giving consumers the information that they need so that they can make healthier choices. Again, consumers told us that they want to see such information when they eat out. In Northern Ireland, we are working closely with environmental health officers to take work on that forward.
955. Several major national catering chains are taking part voluntarily in a pilot programme to provide calorie labelling for their customers. We have also secured healthy eating commitments from six of the UK’s largest high street restaurant chains. The work that is being done with Burger King provides a good example of how that company has started to reduce the salt, fat and sugar in its dishes. It has also started to provide a range of healthier options using healthier cooking methods, and it gives nutritional information on its menus.
956. We are planning to extend that work to workplace catering, and we are keen to discuss with the other Departments how we could improve catering in the public sector in Northern Ireland.
957. Mrs Marnoch: I will talk about how we influence the environment and some of the partnership activity in Northern Ireland that we are involved in that may be of interest to the Committee.
958. The agency has been involved in the school meals steering group, which led to the development of nutritional standards for school lunches. Those standards have been rolled out. We have also been involved with the new food policy that will be launched in schools as part of a whole food in schools policy. We have entered into a partnership agreement with the Council for the Curriculum, Examinations and Assessment (CCEA) in Northern Ireland in setting up a teachers’ panel to help support the dissemination in the primary and post-primary sector of a number of educational resources that focus on nutrition.
959. We have also started work with the Department of Culture, Arts and Leisure (DCAL) as part of work on the Olympics and the 2012 strategy in Northern Ireland. Over the course of the next 12 to 18 months, we hope to bring forward a joint package of measures on physical activity and eating well for young people in Northern Ireland. We have also worked with the Department for Social Development (DSD) on the development of the magazine ‘The Good Life’, which targets households in Northern Ireland with vulnerable people over the age of 65, and we support the Department’s promoting social inclusion (PSI) work on homelessness.
960. As Mrs Jennings said, we work closely with district councils on what we do with the food industry and local caterers. We launched a grant scheme early last year on the saturated fat campaign, and several initiatives are going on across the Province that will support the work in that area.
961. Finally, the Food Standards Agency is an evidence-based organisation, and all our policy work is based on sound evidence. I will touch briefly on the two main surveys that are relevant to the Committee’s work. In the UK, the diet and nutritional status of the general population is monitored through the national diet and nutrition survey, which until last year, had been rolled out across the rest of the UK but not in Northern Ireland. However, for the first time the survey is in Northern Ireland, and we have completed the first year of fieldwork. It is funded jointly by the Food Standards Agency, the Department of Health, Social Services and Public Safety and Safefood. It is an important survey, because it will tell us for the first time whether what we are doing is having an impact on the nutritional status of the population in Northern Ireland.
962. The national diet and nutrition survey collects detailed information on food consumption through four-day food diaries and through checking nutrient intakes and nutritional status, which is done through blood sampling. Information is also collected using physical measurements, which means that there is a physical activity questionnaire for all ages, and through actograph measurements, which are taken over the course of seven days for children aged four to 10. It also collects information on the socio-economic, demographic and lifestyle indicators of the households that are involved. We hope to report back in the next 12 to 18 months about what it will mean for Northern Ireland in comparison with the rest of the UK.
963. The low income diet and nutrition survey (LIDNS) was carried out between 2003 and 2005, and its results were published in 2007. Its aim was to study material deprivation in the diets of the bottom 15% of the population. The fieldwork included 400 households in Northern Ireland, and that enabled us to make inter-country comparisons with Scotland, Wales and England for the first time. In many respects, the areas of concern about the food that people eat that that survey pinpointed were similar to those identified already in the general population. However, compared with the general population, the low-income population was less likely to consume wholemeal bread and tended to consume more non-diet soft drinks, more processed meats, more whole milk and more table sugar. Consumption of fruit and vegetables fell well below the recommended level of five portions a day, and consumption of oily fish was very low.
964. In Northern Ireland, we work in partnership with Northern Ireland Statistics and Research Agency (NISRA) to support the fieldwork of these surveys.
965. Mrs Jennings: I reassure the Committee that we will continue our work in Northern Ireland. We have been delivering on the relevant objectives that were identified in ‘Fit Futures: Focus on Food, Activity and Young People’, and we have a seat on the obesity prevention steering group, about which you heard. I chair its food and nutrition subgroup, which is tasked with putting a framework in place for us to take forward work in Northern Ireland.
966. The agency is also consulting on its strategic plan for 2010-2015. We would like the Committee to visit our offices so that we can outline some of our priorities for the future.
967. The Deputy Chairperson: Thank you for the presentation and for the invitation, which we will take you up on.
968. The signposting, labelling and traffic-light system is very handy. People are always in a rush in supermarkets, and they do not have time to study labels. Therefore, something like the traffic-light system, which is a positive move, will help.
969. Andrea said that one of the agency’s strategic targets is to reduce the intake of salt and saturated fat. You gave good examples of companies such as McCain Foods and others that have worked with you. How do you engage locally with the food and drink industry across the North? Are supermarkets reluctant in any way to get involved and work from positive examples?
970. Mrs Jennings: I am sure that you know that the larger supermarkets control a lot of the movement of food around the UK. At a national level, we can influence the production of food and getting it on shelves. We are involved with some of the local supermarkets and independent retailers in Northern Ireland to try to influence them and what they provide for consumers.
971. The biggest impact will be felt with large manufacturers at a national level. Northern Ireland is a food producer, and it exports a lot of food, so we work closely with the red meat industry, for example. We work with the Meat Exporters’ Association and the Northern Ireland Food and Drink Association (NIFDA) to try to take forward a lot of the work in Northern Ireland.
972. We are building on the partnerships that we have in trying to encourage some of the manufacturers and retailers in Northern Ireland to start to mirror some of the work that has been going on in the rest of the UK.
973. Mrs Marnoch: It is worth adding that 11 companies in Northern Ireland have adopted the signposting scheme.
974. Mrs Jennings: We have been pleasantly surprised that a lot of the food companies in Northern Ireland have taken the high moral ground, are very interested in the health agenda and are moving towards taking up signposting labelling.
975. Dr Deeny: The traffic-light signposting seems to make a lot more sense for the public. However, who in God’s name would have time to read the GDA? For example, an item may contain 12% of the daily recommended intake of sugar, but one would need to be a mathematical genius to work out that, having eaten the item, one could eat a further 88% of sugar and a further 81% of fat that day. Other elements will only confuse people, and no one will pay any attention to them.
976. The traffic-light system seems to be ideal. It mentions low saturates, and there used to be much talk of polyunsaturates. Is that still a big thing? Do the public need to know about saturated fat and polyunsaturated fat?
977. My second question is of interest to me as a GP. Does your organisation have an input into making advice on healthy eating available in health centres? As I said last week, there is still a lot of confusion out there. For example, in my surgery, we have a lot of worthwhile leaflets that we give to patients about how to lower cholesterol. We also give out diabetic sheets, which provide information on how to lower sugar levels. Those leaflets are very helpful, and if patients have those problems, they will often try to tackle them. However, I would like to see a leaflet that tells people who do not have those problems what they should eat.
978. Last week, I mentioned that we need to eat five portions of fruit and vegetables a day, but people do not know whether that means that they should have meals and have fruit with every meal or whether it means something else. If leaflets were produced and placed in health centres and leisure centres, for example, people could pick them up, and they would find out exactly how to get their five portions of fruit and vegetables every day. It is just confusing. I was wondering about your input into that. It would be very worthwhile to have such information. Many people, myself included, do not eat enough fruit, and some people do not eat any fruit at all. How can we encourage our young people to get to like fruit in schools, for example?
979. Mrs Jennings: The overall amount of fat that people eat, particularly saturated fat, is the issue. There was a whole discussion about trans fats and the amount of trans fats that people eat, but the issue is to drive down the overall amount of saturated fat that people are eating and to increase the levels of polyunsatured fats that they consume.
980. Mrs Marnoch: The magazine ‘The Good Life’, to which I referred earlier, targets people in Northern Ireland who are aged over 65. It has been distributed to all health centres in Northern Ireland, and whenever we produce publications, we send them to health centres. However, I know what you are saying about people having a role in providing information and advice. Historically, it has tended to be dieticians and possibly trusts who have supported giving advice and information at a local level.
981. Mrs Jennings: It is right for dieticians to give one-to-one consultations and specific advice on people’s diets. We are in the game of providing those overarching messages that you are saying are quite confusing. In England, lot of money is going into a big marketing campaign called Change for Life, and in Northern Ireland, we need to push for an integrated, single form of messaging that is simple enough for the public to understand. We will be pushing for that in the obesity prevention steering group.
982. Mrs Marnoch: There have been a lot of positive developments in schools in the past few years, particularly through new nutritional standards in school lunches. That has changed fundamentally the food choices that are available in schools. The curriculum has a lot of positive messages that are joined up with the healthy eating messages to reinforce that. However, schoolchildren are a very difficult group to reach, and their intake of fruit and vegetables is very low. A study carried out by Queen’s University shows that that has a particularly negative impact on the bone density of pubescent girls. Therefore, we carried out research a few years ago with Queen’s University and the University of Ulster, and we launched a survival guide for first-year students, because they were the most vulnerable group. A lot of emphasis was put on their fruit and vegetable intake, and we worked with the caterers on site and with students in halls of residence to try to reinforce some of those messages through that resource and through catering. It is always going to be a challenge with that age group, but the environment has changed significantly, so the message can be supported.
983. Mrs Jennings: With the whole school approach — and I am sure that you will be hearing from the Department of Education about that — there are a number of schemes in schools, such as the better break schemes. Schools are doing brilliant work with trying to encourage children to eat healthier food.
984. Mrs Marnoch: The Big Banana project is being launched. Actually we have five of them, so I suppose we could say that a bunch of bananas is being launched. We are going to roll that project out across primary schools from September.
985. The Big Banana has games about nutrition and food hygiene, and it has food-safety messages for children in primary schools. It has a mixture of board games and card games, and we are looking forward to getting it out to people and then seeing what the response will be.
986. Dr Deeny: What about putting leaflets in health centres to explain to people who do not have conditions such as diabetes how they should get their five portions of fruit and vegetables a day? Many adults do not know how to go about that; they need practical advice.
987. Mrs Marnoch: We would be keen to discuss that with the Public Health Agency. The Department of Health, Social Services and Public Safety would have tended to have led on the five-a-day campaign. However, we will reinforce that point in all our messages.
988. Mrs Hanna: I assumed that five-a-day meant an apple, an orange, a banana and a few carrots and peas. I take a simple approach, but perhaps it is not as simple as that. Some of the questions have been half answered already, but it is good to hear that we are going to have one signposting scheme. We need to know what average amounts are; it is a bit like buying tomatoes, because they are sold singly, in trays or in 1 kg packs, and it is impossible to figure out which are the cheapest.
989. You talked about food processors that are working with you, such as the makers of the Mr Kipling brand. However, those companies seem to reduce salt and fat only in their light and diet ranges. I know that they will say that the public want the products that contain salt and fat, but it would be better if you could persuade the food processing companies to make gradual reductions in all their product ranges.
990. How much influence do you have? You told us what was happening across the water, but are you part of an organisation that has more power? The answer lies somewhere between forcing people to change what they are doing by way of legislation and influencing change. It is a question of how far you can go. It is a carrot-and-stick situation; with a bit of encouragement, some will go further, but others will not move at all. We need everyone to make changes, and not just in the light or diet ranges; those are for the people who are looking already at the traffic lights and thinking about their diet. However, most people are not doing that, and the light food ranges are often dearer, even though they supposedly contain less salt and fat. We must make things simpler for everyone so that all processed food is a bit healthier.
991. Mrs Jennings: There is no doubt that you are right. Through our own surveys, we know that products that are marked “light" or “healthy eating" do not attract the general population, and people steer away from them. We are trying to get the food processing companies to make improvements to the standard, routine products by reformulating them and taking salt and saturated fat out of them.
992. We are working with a full range of manufacturers in a sector. For example, if we are working with all the major manufacturers of potato crisps, we establish a norm for that industry and set a target below that norm. That target has to be met over time, because it takes their customers time to change their tastes. If you took half of the salt out of a packet of crisps, no one would buy them, which defeats the purpose of the exercise. Those targets, and the commitments that have been made by all those industry groups, have been published on our website. The industry groups are now publicly accountable for the achievement of those targets over the specified period.
993. Mrs Hanna: Are you saying that they have to achieve those targets?
994. Mrs Jennings: Yes. It is about getting the industry to take collective responsibility so that individual companies are not left behind.
995. Mrs Hanna: I can understand that they want to sell their products. I like salt in my crisps, and I need to be weaned off it gradually. That is what a lot of people do at home when they are using salt with their dinner, but eventually, they will not have it on the table anymore.
996. I want to ask you about what is happening in school and hospital canteens. I know that a lot of work is going on in those places. How much influence can you have in that area?
997. Mrs Marnoch: A school meal nutritional group was set up a few years ago. It was established to develop food-based nutritional standards for school lunches. That started in 2003, and it was piloted in approximately 100 primary and post-primary schools in Northern Ireland. The standards have been reviewed and, subsequently, developed, and new nutritional standards are being rolled out in schools now.
998. In the past six or seven years, there have been developments around school lunches. Added to that are healthy breaks and out-of-school-hours clubs that provide food according to agreed standards that have been developed against a whole-school food policy.
999. Mrs Hanna: I have watched television programmes featuring the likes of Jamie Oliver and have read articles on the subject, but in spite of what has been achieved by those, problems arise because chips are available with everything. A gradual move to low-fat chips will help to change diets. It is obvious that people will choose chips instead of an apple or baked potato, for instance.
1000. Mrs Jennings: Schools are a real success story; the improvement in the food provided in schools is one of the biggest successes of the Fit Futures strategy. Daily menus are devised in blocks of three or four weeks. That planning is aimed at giving children a balance in their diet, as it ensures that children receive one third of their recommended daily nutrition from their school meals in that period. School caterers have set up standardised recipes. They have been trained in nutrition and have been working extremely hard; it is a success story.
1001. Mrs Hanna: We need to get children to take school meals instead of eating a Mars bar and crisps.
1002. Mrs Jennings: That is correct. Mrs Hanna also mentioned legislation. It is important to note that we are constrained because, as members will know, all the legislation that is relevant to our work comes from Europe. We have to be careful that we do not do anything to prejudice the way in which UK food products are sold. We import a lot of products from the rest of Europe, so we cannot introduce legislation that gold-plates what Europe is doing.
1003. Mr Easton: It is recommended that we eat five portions of fruit or vegetables a day. Is it sufficient to eat five apples a day, for instance? I eat only one portion each day, so I am bad.
1004. Mrs Marnoch: It is recommended that you eat a variety. According to the World Health Organisation, one should eat at least five portions of fruit or vegetables a day. Therefore it is recommended that you eat more than five.
1005. Mr Easton: Since we started this inquiry, I have harped on about the importance of getting the food industry to control the fats, sugar and salt that are put in our food. That is the only way to control obesity. Although everything else that is done is good, it is merely a sticking plaster. The Food Standards Agency can only force food producers a wee bit. Are you saying that the matter is controlled by Europe rather than by Westminster or here?
1006. Mrs Jennings: We cannot legislate on the matter here, so we cannot propose legislation stating, for instance, that a particular food sector has to reduce its salt input by 50%. However, we can work in partnership with the food industry. That partnership has been successful in driving down the amount of fat and salt that is in our diet.
1007. Mr Easton: Can Westminster do that?
1008. Mrs Jennings: The UK Government cannot introduce national legislation on this matter, because it would disadvantage UK food companies in relation to the rest of Europe. We would be setting a standard that would be much higher than that for food produced in the rest of Europe or the rest of the world.
1009. Mr Easton: This is an example of the European Parliament needing to get its act together, because we are all suffering.
1010. Mrs Jennings: A lot of European countries are in different places on this issue. We are pioneering some of the work, particularly around signpost labelling and front-of-pack nutritional labelling. We do a lot of work in Europe, and we lobby on behalf of UK consumers.
1011. Mrs Marnoch: To be fair to the food industry, there have been significant developments in the area. We have received commitments from six of the UK’s largest high street chains, including Burger King, KFC, Subway and McDonalds. They account for a huge percentage of the market share. Those companies are working towards reducing the levels of saturated fat and salt in foods. It is a voluntary arrangement at the moment, but they have publicly made those commitments; they are stated on the FSA website.
1012. Carmel, you asked earlier why those companies only introduce such changes in certain ranges. I do not come from a technical background, and when all of the reformulation work started it was fascinating to find out how those products are produced. In relation to saturated fat, what is really interesting is that once the huge processing plants and factories change the oil used for one product, that impacts on all of the others. Those companies use the same oil and fat for most of their product range, meaning that a change for one product impacts across the entire range.
1013. Mrs Hanna: Therefore, we need those companies to change to using a better oil.
1014. Mrs Jennings: I agree, although sometimes that is a very expensive process. The FSA has reduced the overall salt intake by the UK population from 9·6 grams in 2007 to 8·6 grams in 2008; that is a reduction of one gram. Our estimates indicate that that reduction prevents around 6,000 premature deaths in the UK and is worth £2·7 billion to our economy each year. The FSA knows that the food industry is moving to implement some of those changes.
1015. Mr Easton: If the FSA gets rid of all the salts could it get us out of a recession as a result of all the money that that would save the economy?
1016. Mrs Jennings: We all need to eat some salt.
1017. Dr Deeny: Are low salts beneficial?
1018. Mrs Jennings: Low salt is the potassium equivalent of sodium chloride, and there are other issues surrounding potassium, as the Committee will know. It is also a much more expensive option, and the FSA would certainly not advocate swapping sodium chloride with potassium chloride.
1019. Mrs McGill: Thank you for the briefing. On the issue of schools, the west is definitely leading the way, particularly those schools in the Strabane District Council area. The council recently received a report on the work that has been done to promote healthy eating in schools in the area, and it seems to be a very good and effective project. Therefore, be assured that that message is getting through to the schools in the Strabane District Council area. I am familiar with a number of schools and sit on the board of governors for a couple of them, and I know that they are very energised by the project, which they have been involved with for a couple of years. I congratulate those schools and the FSA on that success.
1020. In your submission, you refer to the ‘Low Income Diet and Nutrition Survey’. That survey involved 400 households in Northern Ireland, was carried out between 2003 and 2005 and was published in 2007. Do you consider that research to be up to date?
1021. Mrs Jennings: All such research is extremely expensive to conduct. Following that survey, FSA put its allocated funding into the ‘National Diet and Nutrition Survey’, which takes the general population into account. However, there is no doubt that the low-income groupings will need to be looked at again. It is important to keep all surveys as up to date as possible.
1022. Mrs Marnoch: As Maria has said, the FSA is involved in a rolling programme and is committed to year-on-year monitoring. That involves 200 households in Northern Ireland being surveyed each year, meaning that we are getting data that is as up to date as possible.
1023. The national survey allows us to focus on particular subgroups. Next year, we hope to look at infants and young children, including those aged between 4 months and 18 months, as that age group is not currently included in the ‘National Diet and Nutrition Survey’. It also allows us to look at older people or other subsets of the population, depending on what the policy priorities are.
1024. Mrs McGill: It is important that the survey is based on up-to-date research and results. Is the Food Advisory Committee part of the Food Standards Agency? How many people sit on that committee? Am I correct in thinking that you have 43 staff?
1025. Mrs Jennings: We have 43 staff in our Belfast office. The Northern Ireland Food Advisory Committee comprises members of the general public. The chairperson is a member of the national board of the Food Standards Agency and, depending on the time of year, the Northern Ireland Food Advisory Committee has eight or nine other members. The committee members sit for a term of three years, which can be renewed for another three years. It is sometimes difficult to find members for that committee, and we will recruit for another couple of members in the summer. Therefore, you should encourage people to submit an application.
1026. I must jump to the defence of the other district councils in Northern Ireland, as it is not only Strabane District Council that works well. They work extremely well collectively, and there is a system for grouping them, which works according to whether they are based in the north, south, east, west or Belfast. The Northern Ireland food liaison group, which is the group of principal food officers in Northern Ireland, will take examples of good practice from all the district councils and apply those across the North. I hope that the work in Strabane will be captured and rolled out at a Northern Ireland level.
1027. The Deputy Chairperson: Thank you for your presentation and for answering members’ questions.
21 May 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Claire McGill
Witnesses:
Mr Andrew Dougal |
Northern Ireland Chest Heart and Stroke Association |
|
Mr Iain Foster |
Diabetes UK Northern Ireland |
|
Ms Victoria Taylor |
British Heart Foundation |
1028. The Deputy Chairperson (Mrs O’Neill): We will now move on to the next set of witnesses. I welcome Andrew Dougal from the Northern Ireland Chest Heart and Stroke Association (NICHSA), Iain Foster from Diabetes UK Northern Ireland and Victoria Taylor from the British Heart Foundation (BHF). I invite each of you to make a presentation, after which members will ask questions.
1029. Mr Andrew Dougal (Northern Ireland Chest Heart and Stroke Association): The obesity epidemic threatens to reduce the advances in health that have been made since the Second World War. For the first time in our history, young people may not live for as long as their parents. More than 60% of Northern Ireland’s population is overweight or obese, which greatly increases their risk of heart disease and stroke.
1030. For more than 60 years, the Northern Ireland Chest Heart and Stroke Association has campaigned for healthy lifestyles to prevent people suffering from those illnesses. We urge the Assembly to ensure that there is more effective cross-departmental efforts and resources to tackle that disaster. In particular, we make a plea for the Department of Education to work in conjunction with the Department of Health, Social Services and Public Safety. In the past, that did not always happen.
1031. The private sector must play its part and work with the voluntary sector and the statutory sector. Statutory regulatory bodies must remember that their role is to protect the consumer rather than the industry. Although the Food Standards Agency concentrated on food safety in its early days, it is now responding to the need for information on nutrition. For many years, the Chest Heart and Stroke Association and other organisations campaigned for the establishment of that agency, and the legislation to do that was enacted eight years ago. The FSA must protect the consumer in the same way that Ofcom protects the consumer rather than the TV industry or the advertising industry.
1032. Over one third of all deaths in Northern Ireland are caused by heart disease and stroke. Stroke is the third biggest killer and the leading cause of disability in Northern Ireland. Of those who have a stroke, one third make a full recovery, one third die, and one third have a substantial disability that results in some level of dependence on others for the rest of their life.
1033. To give the Committee some idea of the costs involved; £102 million is spent on direct health and personal social services; £87 million is spent on informal care in Northern Ireland, particularly by the families of those who are in care institutions; and £65 million is lost in income because of mortality, morbidity and benefit payments. That means that, in total, the cost to Northern Ireland is over £250 million.
1034. The Northern Ireland Chest Heart and Stroke Association believes that 40% of strokes could be avoided through proper preventative measures. That is why we are asking for a primary prevention programme on stroke. We asked for a similar programme on heart disease in the Assembly in 1984, and we finally got one in 1986. In the last 20 years, the number of premature deaths from coronary heart disease in people under the age of 75 has declined by 71%, so it is worthwhile to have a prevention programme. It is time that we had one on stroke.
1035. Thankfully, we have the Northern Ireland stroke strategy, and the Assembly has voted to spend £14 million each year on combating stroke. We want to see that money well spent. We want to see it used in reducing stroke and in treating people much more effectively, particularly with clot-busting drugs that have been available in the United States for 10 or 11 years but are only now becoming available in Northern Ireland.
1036. Figures from January 2008 show that over 150,000 people in Northern Ireland are obese. According to the Foresight report of 2007 — which is a seminal report — it is estimated that if current trends continue, by 2050, nine out of ten adults and two out of three children across the United Kingdom will be overweight or obese.
1037. It is the view of NICHSA that over the last quarter of a century, public representatives have had a binding duty to do all that they can to protect the health of our young people. As far back as 8 June 1984 — 25 years ago — NICHSA held a one-day conference entitled ‘the healthier Ulster diet’, which was chaired by Professor Philip James, who now chairs the World Health Organization’s task force on obesity.
1038. Sound nutrition must not be solely for the middle classes. Health authorities, food producers and retailers must see it as their duty to ensure that everyone is empowered to have a healthier diet. In essence, it is important that we have leadership on this issue. There may be a need for a tsar who could take the issue on.
1039. The importance of school-based activities must be emphasised. It is essential that we ensure that healthy eating is part of a whole-school policy. We have been asking for that for 25 years, and we are pleased that the Food Standards Agency, the education and library boards and the Health Promotion Agency are now getting there. There have been major changes. That should be a requirement in every school, not only middle-class schools. Coronary heart disease and stroke is most rampant in the lower socio-economic groups, and that is where we have not been successful. We must focus more and more of our efforts on dealing with that.
1040. The point that Dr Deeny made about guideline daily amounts in the previous evidence session is very valid. I am not innumerate, but I find it difficult to understand them. I find the traffic light system to be very positive, as is using the terms “low", “medium" and “high" to describe the various contents of food.
1041. Sixteen major companies have deviated from the traffic-light system recommended by the Food Standards Agency before it had the opportunity to launch that campaign. That has caused huge public confusion. Those companies, which I am not going to name today, have done no good for the health of their customers. They have failed to empower their customers. We would like to see all companies sticking to one simple system that people understand.
1042. Stroke is the largest single cause of disability in our community. Preventing stroke can be of huge benefit to the people of Northern Ireland, the Health Service and our economy.
1043. Ms Victoria Taylor (British Heart Foundation): Good afternoon. Thank you for inviting us to speak to the Committee. As a dietician, obesity is an issue that is close to my heart and one that I spend a lot of time working on. The British Heart Foundation is keen to see improvements in obesity levels, as obesity is, in itself, an independent risk factor for heart disease, but it can also be seen as an accumulator, in that it has an effect on other risk factors including diabetes and hypertension, which is also linked to stroke.
1044. The INTERHEART study estimates that 63% of heart attacks in western Europe were due to central obesity. Another factor that we need to consider is whether people are apple shaped or pear shaped; the apple shape being more inclined to central obesity, which has a greater link to heart disease. People who are apple shaped, or have more central obesity, are twice as likely to have a heart attack as those who are not.
1045. The reasons for action have been set out in the Foresight report, which contains stark and sobering predictions of what will happen by 2050. Based on changes to BMI alone, the report predicts that heart disease will increase by 20% by 2050. That will have not only human costs, but economic costs, through the treatment of those who have heart conditions. We are pleased that death rates from heart disease have fallen since the 1970s. Although the fall is partly due to reductions in risk factors, such as smoking, the decrease is also due to better treatments; people with chronic diseases are living longer with long-term medication.
1046. The question of how to solve the problem is very difficult to answer. We are aware that there is no single solution; a joined-up approach is needed not only between Departments, but between the different sectors. The food industry was mentioned but, as a non-Government organisation, we are keen to work with the Government also. We are also aware of the need to raise problems that we see in food advertising.
1047. The focus of the British Heart Foundation is more on prevention than management. We want individuals to receive good advice, but we recognise the need for a supportive environment. The approach to obesity should be a combination of diet and physical activity, which are the two sides of the energy-balance equation, as well as behaviours.
1048. As a whole, the population is getting bigger, but there are groups of the population who find it more difficult to select and prepare a healthy diet, which is partly based on income. Therefore, as we have already heard, it is vital to make healthy choices the easier choices.
1049. Before I talk about our recommendations to the Assembly, I will point out what the BHF is doing. We are keen to support work that is ongoing, and hopefully our educational resources will help individuals and front line staff to do that work. We are also very proud of our social marketing campaigns. The Food 4 Thought campaign, which looks at what children should do to combat obesity and targets 11- to 14-year olds through schools, has been taken up by schools in Northern Ireland — 128 signed up the most recent campaign. This year, the campaign also takes an innovative look at the consequences of the choices that children make.
1050. The two most pressing policy calls concern advertising to children before the 9.00 pm watershed, rather than just during children’s programmes, and front-of-pack food labelling. We are strongly in favour of the traffic-light system, so we welcome the support expressed for it this afternoon.
1051. A joined-up approach is vital; we need to see all Departments working together. The approach to physical activity and planning policies may involve Departments that would not obviously lend themselves to the obesity problem; however, the problem is not the responsibility of only the Department of Health. We are looking forward to the publication of the service framework for cardiovascular health and well-being. It is also important that we have good monitoring and evaluation of the Fit Futures strategy so that its goals are achieved and we can know whether it has been successful.
1052. Although those goals cannot necessarily be achieved directly by the Northern Ireland Assembly, we would welcome its support for halting the advertising of junk food to children before the 9.00 pm watershed and also for ensuring that there is a single system of front-of-pack food labelling that is clear and that people will understand.
1053. Mr Iain Foster (Diabetes UK Northern Ireland): I am Iain Foster from Diabetes UK. Six years ago, I was diagnosed with type 2 diabetes. Therefore, I have a personal and a professional interest in the issue.
1054. I understand that the Committee’s inquiry has been ongoing for some time. You have heard a range of evidence. I do not need to rehearse the statistics; the evidence is very clear. Dr Michael Ryan from the Northern Health and Social Care Trust gave fairly comprehensive evidence on the medical side of diabetes. I would challenge one or two of his statistics, although only on minor details; I will not quibble over them.
1055. Essentially, I want the Committee to bear in mind, particularly with regard to obesity and diabetes, the importance of getting beyond the misconception that diabetes is a mild condition. It is not mild; it is a chronic condition that has no cure. Type 1 diabetes will take up to 20 years off a person’s life expectancy. Type 2 diabetes will take up to 10 years off a person’s life expectancy. You can imagine the impact that that has on a person and his or her family, as well as the impact on the Health Service.
1056. At current levels, over £1 million is spent each day in Northern Ireland to treat 65,000 people who have been diagnosed with the condition. Current prevalence models predict that that will rise to over 80,000 people during the next five to 10 years. The Health Service cannot sustain that level of care. Diabetes is a complex condition; patients must see a range of health professionals and take a range of medication. It is intensive and cost heavy. Therefore, it is in the interests of individuals, communities and the Health Service to stop the increase in the number of people who develop diabetes.
1057. With regard to obesity, it is important to remember that there two types of diabetes; type 1 and type 2. Type 1 is genetic and tends to develop in younger people. It has no connection whatsoever to weight issues. At times, even as a diabetes charity, we can be slightly guilty of raising the profile of diabetes in a simple way to get the message across. Yet it is important that we do not have the simplistic model that all diabetes is weight-related, particularly because people who are diagnosed with type 1 diabetes are mainly children. We have a lot of anecdotal evidence of children being bullied and stigmatised because of their diabetes. Type 1 diabetes is not weight-related, and it is important to make the distinction between the two types.
1058. Even type 2 diabetes is not exclusively caused by excess weight or obesity. The causes of type 2 diabetes are still not fully known. Much research is still being done. Weight contributes to around 80% of cases of type 2 diabetes. The other 20% of people who have type 2 diabetes have no weight issues whatsoever. We are aware of people who are heavily obese but have never developed type 2 diabetes. Therefore, it is a complex picture and it is important not to become too simplistic about it.
1059. As regards current treatments of diabetes and obesity, it is clear that society and the Health Service have failed. There is no issue about that. That is not an attack on the Department of Health. The amount of money that it invests in diabetes care is quite clear; however, statistics show that there has been a steady increase in the incidence of diabetes. Logically, therefore, it would seem that the cause of that increase is beyond the remit of the Health Service. There are wider factors that are very much to do with lifestyle that the Health Service currently cannot control. Obesity and the health complications that it causes are a lifestyle issue.
1060. Until now, the Health Service has treated the complications and consequences of obesity using a medical model; it has not viewed obesity as a lifestyle disease. Skills, investment and knowledge relating to people’s lifestyle choices are at a basic level throughout the Health Service. Lifestyle is not a technical, medical issue. Many healthcare professionals feel uncomfortable tackling other people about their lifestyle choices. Many of those issues are outside the Health Service’s control and, to be honest, are probably beyond politicians’ control.
1061. Therefore, I understand that it is a difficult challenge for you as politicians to try to affect that situation. It is a complex situation and no single piece of legislation will achieve the desired result. As it is beyond your control, you will, obviously, not have experience of it and you may feel uncomfortable addressing it.
1062. Unless we start to regard obesity as a lifestyle disease, we will not stop its increase. Levels of obesity will continue to rise, and its consequences will be phenomenal and much worse than other issues that receive far more resources and applied intelligence. Obesity as a lifestyle disease has received little investment or attention. It is important to consider someone’s wider lifestyle and all the factors that feed into it.
1063. We do that by changing people’s attitudes, and that is a challenge in a similar way that dealing with drink-driving, wearing seat belts and smoking in public places were big challenges. However, changing people’s attitudes to lifestyle choices presents an even bigger challenge. Strong legislation played a role in shifting people’s attitudes to smoking and drink-driving, and politicians must face that fact when thinking about obesity.
1064. Until now, all efforts to tackle obesity have concentrated on information, advice, and awareness. By and large, that message has been received. People might not know about daily allowances and other technical details, but most have a reasonable idea of what is or is not healthy. Even having a good knowledge, however, does not affect some people’s behaviour positively. Therefore, there must be an additional trigger or lever to change people’s behaviour. I am quite sure that legislation is required. In the past, people have taken a hands-off approach and have been scared of having nanny-state accusations made against them. To shift the wider cultural sense of what is acceptable and signal what direction should be taken requires stronger political leadership from the Health Service and other areas of Government on legislation, the food industry, education and leisure activities. Without that, the trend in obesity will continue, and the Health Service will face the consequences and possibly start to crack under the strain.
1065. I stress that leadership, the recognition of obesity as a lifestyle disease, and legislation are required. Obesity is a complicated issue, because it does not require a single piece of legislation or affect only one section of society; it covers a many elements of modern life. I advise you not to underestimate the challenge. One thing is certain: if we do not attempt to tackle obesity, the future will be very bleak for us all. I could go on, but I am conscious of time.
1066. The Deputy Chairperson: There is little that you said with which the Committee does not agree. We all recognise that obesity must be tackled across all Departments. To pick up on a couple of key points, Victoria, you said that healthier choices must be the easier choices. That is a simple point, and we can work on it.
1067. Iain made a point about having to regard obesity as a lifestyle disease, and I agree that it must be examined in that context. You also discussed the need to challenge attitudes, and smoking has long been described as the single greatest cause of preventable premature death. Much effort went into bringing about a cultural shift, and smoking is now socially unacceptable.
1068. You told us today, and we heard in previous evidence sessions, that the obesity epidemic is a massive threat to public health. One submission stated that for the first time in our history, parents will outlive their children. You also said that 145,000 people are obese and that the prediction is that nine out of 10 adults and two out of three children will be obese or overweight by 2050. Are you saying that it is time for obesity to be recognised as the number one public-health issue facing society and that it should be tackled accordingly, in much the same way that smoking was dealt with in the past?
1069. Mr I Foster: Absolutely. Unless obesity is tackled, we will not make progress. Obesity requires the level of leadership and investment that would be given to the number one public-health issue. There are always competing demands for resources, time, energy and so forth, but obesity must be put at the top of the agenda. A significant amount of complications, even beyond the diabetes epidemic, result from obesity, and it places restrictions on people’s quality of life and their life expectancy. People may live longer, but only if they are supported by extremely expensive Health Service resources that would, as a consequence, be denied to other areas of need.
1070. We do not often talk about it, but, in a sense, public spending is a competition. Health is important, but should we spend less on education, on the environment or on other issues? Ultimately, we have to, because society makes choices about where the budget goes. Obesity will increasingly demand more public resources. Smoking and drinking may be damaging to public health, but they are nothing compared with what obesity will do to our population over the next 10 or 20 years. It has to be top of the agenda, and we have to have very strong political leadership.
1071. Mr Dougal: Let us hope that the politicians will have the moral courage to act swiftly on this issue. It took almost 40 years for resolute action to be taken on smoking. As far back as 1965, the Health Minister, Sir Kenneth Robinson, and Tony Benn banned the advertising of cigarettes on television, but almost 40 years passed before there was a total ban on the advertising and promotion of tobacco products. That indicates weak and irresolute government.
1072. Some 25 years ago, when we in the Northern Ireland Chest Heart and Stroke advocated that nutrition was linked to heart disease, people thought we were not quite sane. Now that link is proven, and people know that there is a connection between nutrition and cardiovascular disease. Government should act now to empower people to make sensible choices. They will not be able to do so unless there is effective, simplified and comprehensible nutritional labelling on the front of the pack — it should not be written in tiny figures on the side panel, making it difficult for some people to read.
1073. It is important that people understand that they should get that opportunity. I know that the single European market has created difficulties. This is an issue at European level; I know that 800 amendments have been tabled to a Bill that is proceeding through the European Parliament. However, that is not to say that moral pressure should not be put on food manufacturers and retailers here to have an effective voluntary system through which they can indicate that they care for their customers’ health and wish to give them choice. If that were to happen, we would like to see Government put their shoulders to the wheel and make sure that something is done. If we cannot do that by statutory means, we should do it through moral obligation.
1074. Mr I Foster: The evidence is very strong. We need to restate and clarify it, and we need consensus, but the evidence exists. However, we must ask what we are going to do about it.
1075. It is almost like a battle. We have a child in one hand, with its life before it, full of avenues that it may go down, and we are up against a lifetime of habit and the example that parents and society give. We are also facing the food industry, the advertising industry, transport, technological advances and sport, which is now mostly a spectator event. People do not participate in sport; they watch it on television. These days, the most popular leisure activity is probably shopping. Consumerism is one of the huge forces that focus on the individual. To combat all that, we must encourage people to make healthy lifestyle choices. It is an unfair struggle, and it is almost impossible.
1076. If we were to sit back, take a hands-off approach and talk around the edges, we would lose the battle. There must be more focus and more dedicated action to counterbalance all those other forces. Therefore, legislation is necessary.
1077. Ms Taylor: Given that the Foresight figures are predictions, it is not too late to change things. It should also be remembered that in 2050, nine out of 10 adults will be obese. Those adults are today’s children, so we need to work with them now.
1078. Dr Deeny: We held a very interesting conference here on obesity on Tuesday. Many top people — professors, researchers and clinicians — from different countries attended. You mentioned one of them, Dr Michael Ryan, who is a paediatrician. There is no doubt that the message is coming through, and we need to get awareness of the issue in the media. The public are not aware that this is an epidemic. The epidemic is not coming; it has started already. The clinicians’ frustration is palpable, and they want something done about it as soon as possible.
1079. You talked about the knock-on effects of obesity, including diabetes, ischaemic heart disease, renovascular disease, stroke, and hypertension. Often, the precursor to those conditions is obesity. The cost of the situation to public health, productivity and the economy will be enormous.
1080. You mentioned a stroke strategy. You are right; it is not before time that that strategy has been introduced. Moreover, heart disease and other illnesses are dealt with much better now. It is great to see that in my professional career. Do we need an obesity strategy? As we all know, it is a societal problem, but the health sector will have to take the lead again.
1081. Some people at Tuesday’s conference believed — and you are right about this, Victoria — that all Departments must be involved in a joined-up way. However, the Department of Health, Social Services and Public Safety will have to drive any strategy and will have to ensure that other Departments participate. DHSSPS will have to pick up the consequences of the illnesses that arise from the obesity epidemic. Do we need a tsar to lead our strategy? Should we give one individual the responsibility to pull together all Departments and the authority to ensure that the issue is placed at the top of the agenda? As we can now see in primary care, the problem is worsening.
1082. The medical journals and at least one newspaper covered a story this week in which some eminent medical researchers said that everybody over the age of 60, regardless of whether they have high blood pressure, should take a pill to reduce their blood pressure. That is not the right way to tackle that issue. Indeed, it is similar to the concept of a polypill. Giving people a polypill is like closing the stable door after the horse has bolted; it does not deal with the situation, but treats the outcomes of obesity, for example, rather than preventing the problem. However, some people are pushing that idea.
1083. I am sure that the multinational drug companies are keen to introduce a polypill. All those companies are trying to create the first pill that controls blood pressure, blood sugar levels and cholesterol. It could earn a company billions of pounds. What is your view on that matter?
1084. Do we need someone to take the lead on the obesity strategy in Northern Ireland? We need to take the issue seriously and, through the media, get the message across to the public, who probably do not realise how serious the obesity problem has become.
1085. Mr Dougal: The first research from the States into obesity in children was published here in 2001 or 2002. Seven years have elapsed, and we have not advanced that much. A tsar is essential. Professor Roger Boyle, who is the heart tsar in England and who subsequently took the lead on stroke services, has been highly effective. Northern Ireland led the field in the development of stroke services and stroke units. However, after Roger was appointed to lead the stroke strategy, England overtook us. We need a personality and a focus to provide the leadership that has not existed in Northern Ireland. Roger Boyle and others in England have done a great deal to advance the battle against heart disease and stroke.
1086. My chairman, Professor Varma, and I are not keen on the idea of everybody over the age of 55 taking a tablet for blood pressure. Only people with elevated blood pressure should take such medication. I have heard Sir Richard Doll from Oxford talk about the polypill. I think that the idea of having such a pill has many flaws. Last week, an epidemiologist from Liverpool said that reducing the population’s cholesterol measurement by 1 mmol/l will save many lives. However, we still take the view that a population approach could benefit people hugely. People who are diagnosed with diseases need tablets, but the whole population should not be on tablets.
1087. Mr McCallister: You are all very welcome. The discussion has been interesting so far. The difference between the discussion on obesity and that on smoking is that there is no debate about the science or the lobby behind this argument. We need to prevent obesity rather than tackle it once it has happened. I listened to the discussion, and I agree that we need to consider how to plan communities and develop new towns and villages and the schools therein. For example, we must encourage more families to walk to school and to build that into their routine, and we should support the ongoing work in that field.
1088. Education through schools has been mentioned, and a joined-up approach should be taken to training our teachers. Supermarkets and others in the industry will respond more quickly to a market-led exercise when their customers start telling them what they want. We must get back to what we described previously as honest food; the issue is to know where the food is from and what is in it. There is a huge job of work to be done in promoting that agenda, because it is critical to address the inequalities that have been discussed.
1089. I have a background in the food industry, and I have visited some of the businesses concerned and have seen what goes into cheaper products. That is one of the key reasons for our having such health inequalities and a reason that people in certain communities will have their life expectancy reduced by 10 years or more. I agree with what you say, and your input into the inquiry will be invaluable in helping us to take the matter forward. I hope that the Public Health Agency will set about becoming a tsar-type figure and start to address the issues. How do you see that moving forward? Have you had any interaction with the new agency, or are you hoping to do so?
1090. Mr I Foster: It is early days for the Public Health Agency. We have taken a step forward from where we were previously, but the Health Promotion Agency should be able to learn lessons and learn from mistakes that have been made in the past and take the matter forward. The matter must be given more of a priority, and the agency should have a greater budget. We must also ensure that it has a closer connection with other parts of the Health Service, that is, the other bodies, commissioning groups and regional bodies. If that were to happen, there would be more communication and interplay. Hopefully, that will improve things. However, it is not the final answer, and it will not solve the problem. Additional things need to be done.
1091. The Public Health Agency was conceived and developed in the context of the wider review of public administration (RPA) for the Health Service. It was not constructed to solve the obesity crisis. It may be one useful mechanism to take us forward in that direction, but far more remains to be done across Government. Essentially, the issue is about budget; it is about other Departments signing up to a strategy and perhaps allocating some of their resources to see the benefits that becoming involved in such a strategy would bring and how their self-interest as an Education Department, a transport section or an Environment Department could be served. If they were to become involved, they may be able to tick some of the boxes of their target cultures and decide whether they could allocate money to the Department of Health, Social Services and Public Safety or to a new organisation that could take on some of the issues.
1092. It is a challenge, and a range of practical day-to-day things could be done. Education was mentioned, and I remember doing home economics when I was at school. However, my son has just left the education system, and he has no idea how to cook. His education did not include any of that. His concept of cooking is using a microwave. Perhaps I have failed as a parent in that regard, but, on a practical level, he does not know what honest food is.
1093. There are pros and cons with having a tsar to deal with the matter. Nevertheless, it should be explored.
1094. Ms Taylor: I am not able to say to what extent we are working with the Public Health Agency at the moment, but as I said, we would welcome working with any of the Government agencies. That is an effective way of working.
1095. To go back to the comment about honest food, it would be great if consumers were demanding that supermarkets supplied them with more healthy options. We want to know how informed the consumers’ choices are, what informs them, and how the marketing of junk food with its high fat, salt and sugar compares with the healthier options. We need to address the extent of the advertising of such food and level the playing field. At the moment, we cannot compete in the same way, and our messages are sometimes drowned out by those about the less-healthy options.
1096. Sport has been discussed, and I was glad that how we plan communities and make families active was mentioned. It is important to remember that overweight or obese children are much less likely to participate in sport and that we must encourage physical activity in our daily lives.
1097. Mr Dougal: We will be working with the Public Health Agency, and that work must be led by epidemiologists who are heavily involved in research on the matter. Our campaign to prevent heart disease began in 1984, which was a time when many thought that heart disease could not be prevented. That campaign was led by world-renowned epidemiologist Professor Alan Evans. Given that, the work of the new agency on obesity must be informed by epidemiologists’ research.
1098. Mrs Hanna: The seminar on Tuesday was excellent, and the point was made strongly that a lot of good research exists that must be used — in fact, a lot of time and money is spent on research. I made the point that a person or an organisation must take ownership of the situation or take a lead in dealing with it. I am not dying about the terms “tsar" or “commissioner". A lot is happening, but that work is not being brought together, and unless somebody is tasked with taking control, nothing will happen.
1099. The Committee has just taken evidence from the Food Standards Agency. I asked its representatives about the legislation, because it certainly modifies behaviour. Iain Foster mentioned — and I was aware of this — that even when we know what we should be eating, we do not eat it. That is true, and we must all put our hands up and admit to eating a chocolate bar when we know that we should not. However, there remains a deprivation gap for people who do not have enough money to make choices. Some of us can buy nice fruit or other food in Marks and Spencer, but others do not have those choices. There is also the fact that schools no longer teach home economics, and it is quicker and cheaper to buy carry-out burgers.
1100. Given that not enough is happening, we must adopt a carrot-and-stick approach that is more about the stick. Legislation must be used. Do all the witnesses agree that obesity is the number one priority and that it is almost like a time bomb? People often do not change their behaviour until they get a frightener — as people here say — and fall ill or are forced to change. The many statistics that are available indicate that obesity contributes to other illnesses, including heart disease, stroke and diabetes.
1101. People are dying younger. Unless we address obesity, we will be reminded of the awful idea that some parents will outlive their children. We do not want to overly frighten people, but warnings must be balanced.
1102. A great deal of support is necessary. We must lead, and the Committee and the Public Health Agency must take that lead. The agency was represented at the seminar on Tuesday, where it was accepted that dealing with obesity involved more than just the Department of Health, Social Services and Public Safety. It was acknowledged that the pieces must be picked up by the DHSSPS and that it is probable that someone from that Department will take the lead. However, I believe that the responsibility should rest with the Public Health Agency.
1103. A lot is happening, and some of that work was brought together at the seminar on Tuesday. The Committee has taken a lot of evidence, but it is now time for what may be called a brainstorm to move the process on. Some of what is done about tackling obesity must be based on what the Committee heard from the Food Standards Agency. Pressure must be put on food producers and manufacturers to do the right thing. That may not be possible immediately, but there should be a timescale for weaning us off fat and salt. Moral pressure must also be exerted, but it takes more than that to change people. At the same time, complications in European legislation must be teased out. I am merely thinking aloud about what must be done and what support and advice is needed to make progress on the situation.
1104. To return to my question, I would like to know whether we all agree that obesity, which feeds into all our other priorities such as diabetes, stroke, heart disease and cancer, is the number one priority. There can be no better time than now to take action, given that the Committee is in the middle of its inquiry. However, support and input from other people will also be required.
1105. Mr I Foster: In itself, the inquiry will create a lot of societal challenges. For example, what will happen to the inquiry’s findings? How will they be pursued? Will the ensuing report just be added to all the other documents that have been produced on the subject? I know that you are concerned about the number of commissions in Northern Ireland; we have had enough commissions and quangos, and we do not want any more. We need to see action, and that will depend on how the Government use the limited finance and influence that they have to the maximum benefit. They must be a bit more creative and not approach the matter in the same bureaucratic and inward-looking way that they have approached other matters in the past.
1106. Andrew Dougal and I sit on the Department’s obesity prevention steering group, and although it is still early days for it, neither of us is overly excited or optimistic about it making one dot of a difference to most people’s lives. The challenge, therefore, is to determine how aspirations can be translated into actions by investing in programmes that might produce societal changes. However, we must be realistic and not set one- or two-year targets; we are talking about a 10- or 20-year process. As we have seen in the past, when the Government talk about a 10- or 20-year process, it can be code for saying that they do not need to worry about the matter at hand. The real test will be the shift in how the Government respond.
1107. Mr Dougal: We must act speedily. Research has been available for seven or eight years, we have the obesity prevention steering group, and the World Health Organisation has produced a report on the matter, as has the Department of Health in England. Let us get on and do things.
1108. We must also remember that although we have had success in preventing heart disease and stroke, that was achieved in the higher socio-economic groups. Therefore, although I agree with the total-population approach, there may be a need to focus on the more deprived groups in society to ensure that those people are empowered to change their lifestyles. Many of those people feel that their lives are so awful that there is no point in changing their lifestyles. Therefore, we must get the message across that if those people quit smoking and change their diets, there can be benefits for them, such as avoiding coronary heart disease, strokes, cancers and diabetes. Those are the important points to make, and we must home in on those people and empower general practitioners and those who work in primary care to provide the support in the community that is necessary to allow those people to believe that the health that they enjoy and their lives can be improved greatly.
1109. The Deputy Chairperson: Thank you for coming along. Your evidence has been informative, and you made a number of points that we hope to look at more closely and incorporate into our response.
28 May 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witness:
Dr Una Lynch |
Queen’s University Belfast |
1110. The Deputy Chairperson (Mrs O’Neill): The witness for this evidence session is Dr Una Lynch from Queen’s University Belfast. By way of introduction, Dr Lynch is a qualified nurse, midwife and health visitor. Dr Lynch has an MSc in community health from Trinity College Dublin, and, in 2007, she graduated with a doctorate in governance from the School of Law at Queen’s University Belfast.
1111. Dr Lynch has worked in public health practice, and education policy and research, across the island of Ireland. In 2000, she was seconded to the World Health Organization (WHO) in Copenhagen to work on a ministerial conference on public health nursing. In 2005-06, a leading lights lecturers into industry award from Queen’s University enabled her to travel to Cuba to study the country’s health system.
1112. Dr Lynch, we are privileged to have you here today to talk to us as part of our inquiry into obesity. I invite you to make your presentation, after which members may have questions.
1113. Dr Una Lynch (Queen’s University Belfast): Good afternoon, and thank you very much for inviting me to address the Committee. The evidence that I will present this afternoon is based on my research of the Cuban health system. I spent four and a half months in Cuba researching the country’s health system.
1114. I welcome the leadership that has been shown by the Committee in holding an inquiry into the obesity epidemic, which is symptomatic of the deficits in the existing model of healthcare provision in Northern Ireland. The inquiry, therefore, provides an excellent opportunity to act as a vehicle to address those deficits and to create a health service that is truly fit for purpose. We have much to learn from the Cubans on that subject. Obesity is rapidly emerging as the main public health issue in Northern Ireland and throughout the developed world. However, the burden of obesity and its associated problems, such as diabetes and heart disease, are disproportionately borne by the poorer sectors of society.
1115. My paper and presentation stress the importance of primary healthcare, active citizenship and community participation in delivering effective public policy generally and in addressing the issue of obesity in particular. I am conscious that some — perhaps all — members of the Committee have not yet had the opportunity to visit Cuba. Therefore, I spoke to the Committee Clerk, and he kindly agreed that I could table a second paper, which is a pictorial guide to my presentation, and I will refer to that too.
1116. The first photograph is a typical image of Cuba: the seafront in Havana. The quotation that is superimposed on the photograph is from an extremely interesting character, Professor Francisco Ochoa. He was one of the first doctors to qualify after the triumph of the revolution in 1959. He qualified in the same year and has subsequently become one of the leaders in public health throughout Latin America. He is featured in ‘The Lancet’ and has won awards from the Pan American Health Organization. I felt that it was fitting to start with his reflection:
1117. I will leap now from the seafront in Havana to the House of Commons. A report of the House of Commons Health Committee on health inequalities was published in March 2009. It states:
“In 2006 a girl born in Kensington and Chelsea has a life expectancy of 87·8 years, more than ten years higher than Glasgow City, the area in the UK with the lowest figure (77·1 years)."
1118. The reality is more shocking, because Belfast Healthy Cities published a report in 2008, ‘Divided by Health: A City Profile’, which revealed that the life expectancy for boys born in west Belfast is 71 years, which is 17 years less than girls born in Kensington and Chelsea. That is a startling fact and reflects the inequalities among citizens in different parts of the UK. It is an indictment of our capacity to realise William Beveridge’s vision of the National Health Service.
1119. Cuba, I believe, provides us with inspiration and hope, and makes us realise that, with all the resources that we have at our disposal in Northern Ireland, we can do so much better. Cuba has a very poor economy. Despite its economic situation, however, Cuba has managed to achieve quantitative health indicators such as infant mortality and life expectancy that are comparable with all the high-income countries.
1120. The infant mortality rate in Cuba and in Northern Ireland is five: five babies in every 1,000 born live will die in their first year. We do not want any babies to die in the first year of life, but that is a reality. In the developing world — in Zambia, for example — for every 1,000 live births, 102 children will not see the end of their first year.
1121. Cuba has achieved those results despite a pitiful economy. It is spending 7% to 8% of its gross domestic product on healthcare, which is a similar proportion to the UK and Ireland. However, because of differences in economy, the UK is actually spending seven times as much, the Republic of Ireland eight times as much and the United States of America 18 times as much as Cuba on healthcare. Something interesting is going on in Cuba, and we can learn from that.
1122. Modern health systems are dominated by diagnosis and treatment of disease, with prevention and public health relegated to a back seat. That was highlighted in the 2008 World Health Report. Cuba, by placing primary care as a driver for its health system, has managed to turn that traditional paradigm on its head. Even Cuba’s most strident critics will admit that it does health very well. For Cubans, it is fair to say that health has become emblematic of the success of the revolution. Cuba makes that happen through a powerful Ministry of Public Health, which governs the entire health system.
1123. I will now return to the photographs in the ‘Hello!’ magazine-style guide presentation, as it were. I will focus on the second photograph, which is captioned “family doctor/family nurse". In 1984, the Cubans, having visited initiatives throughout the world and considered different health systems, were hugely impressed by the British model of general practice. That year, they decided that general practice was where it was at, and they were going to build a system around general practice and primary care.
1124. Twenty-five years later, they have established a system that supports primary care. They do not have the notion of primary and secondary care. They have a health system that is built around primary care, to which the family doctor and family nurse are crucial. They work and live in the communities and, depending on population density, work with between 1,000 and 3,000 people.
1125. The third photograph was taken in a family doctor’s practice, but it could have been taken at any practice in Cuba. If one walks off the street into any family doctor’s practice, one sees, in the waiting room, the needs analysis of the area, which shows the population profile, the age/sex distribution, the breakdown of conditions affecting that population and the uptake of vaccination and screening. Sometimes, the charts do not look pretty, because the resources at the practices’ disposal are not equivalent to ours; sometimes, they will be hand drawn, but they are all displayed in waiting areas.
1126. However, even more excitingly than that, the family doctor/family nurse practice is governed by a local health committee, which brings together representatives from all the key stakeholders, including the local women’s groups, and so forth. Every six months, they sit down and draw up an action plan — not a strategy or a glossy document. They examine the needs of the population, the environmental factors and the social issues to see how they can plan together. The beauty of that system is that it feeds up from that small level to municipal level and, finally, to national level, which has enabled the Cubans to develop a system that is constantly evolving.
1127. The next page contains three photographs of primary-school children in Cuba. In 1959, education and health were the two priorities for the new Government after the revolution. If one wants the public to participate, the public must be educated and have confidence. Confidence comes from education, and education is prioritised all through a Cuban’s lifespan. Primary-school, secondary-school and university education is free.
1128. I have included a photograph that has a relevance to obesity. The Cubans are interested in education not only from an academic point of view but in preparing children for life. At the beginning of each academic year, Cuban schoolchildren are measured, weighed and undergo a fitness assessment, which examines how far they can run and how high they can jump. That is then reassessed at the end of the year. The school is being measured not only on its academic performance but on how its children’s physical and fitness levels are progressing.
1129. The next selection of photographs show círculos de abuelos — grandparents’ circles. Health promotion, prevention and public health covers the lifespan of a Cuban, and it is not focused on children only. Anyone who visits Cuba and goes out early in the morning — from 8.00 am to 8.30 am — will see groups of older people doing gentle exercises in the parks and plazas. The lady in the photograph with her back to the camera has come from the equivalent of the Cuban sports council. Someone from that institution will visit those groups about two days a week to keep the group motivated and ensure that exercises are done properly and safely. Another photograph shows a lady standing side on: she is the peer leader. These are peer-led initiatives that are run by the community and taken by the community. Another lovely thing is the fact that, because the family doctors and nurses work locally in the community, they can drop into those sessions and chat with people. They may check blood pressure and blood sugar levels, and generally keep an eye on the population with whom they work so that health issues and contact with patients is not always carried out in a medicalised environment.
1130. I am stressing a focus on primary care, on needs analysis that enables people to target resources on those areas that are most needed, which realises the vision of equity, and on education, which enables the community to participate and be active players.
1131. I started with a quotation from an interview that I conducted with a Cuban, Professor Francisco Ochoa. I will end with another quotation, which is a challenge to all of us. My research question was about public health and why the Cubans are so successful. The quotation is from Professor Silvia Martínez, another highly esteemed medical doctor in Latin America. She challenged my question and said that a low infant mortality rate is not a success. The fiercest critics of Cuba are the Cubans themselves, because they are continually striving to do better. Bearing in mind the difference between girls born in Kensington and Chelsea and boys born in west Belfast, Professor Martínez said:
“To maintain the infant mortality rate is a social responsibility. Responsibility like Beveridge says: responsibility. A child of one year has a right to this. I imagine that there should not be anything lacking that will guarantee its protection: if you work for this you are fulfilling your duties, nothing more."
1132. The Deputy Chairperson: I enjoyed reading your paper and am interested to learn more. The paper clearly outlines the successes of the Cuban Government. We need to examine more closely the fact that, given the current economic climate in Cuba, it achieves better health outcomes than some developed countries. I particularly like the design of your submission and the concept of the umbrella, which shows how public health is the backbone of, and the dominant ministry in, Cuba and how it plays a key role in determining the work of all other Departments.
1133. Time and time again, the Committee has discussed the need for cross-sectoral working and how one Department should take the lead on the issue, provide information and filter it to other Departments. The new Public Health Agency was established last month. The Committee argued strongly for the establishment of that body, because we thought that it should play a key role in tackling public health, which might have been lost on a board that deals with general daily health needs.
1134. One of your recommendations mentions that the systematic needs assessment successfully underpins policies and strategies in Cuba and that its Government often consider that matter. The concept of placing information on the wall of doctors’ surgeries will probably alert people to the fact that they are more prone to, for example, heart disease because of the area in which they live. All those ideas are welcome. The challenge is how to gather information here and what to do with it. Do we do well here? Do we have effective needs analysis here? Have we gathered information, and do we use it properly?
1135. Dr Lynch: Thank you for your comments. I am glad that you have taken the paper’s contents on board; you have reflected the information accurately. I also hope that the Public Health Agency puts public health at the forefront.
1136. We collect information very well here, and we collect any amount of it: we have information overload. However, we share that information poorly, and we are incredibly bad at using information that we have collected from the population to consult with the community in order to decide priorities and responses. The Cuban system is sophisticated but, at the same time, simple. The Government make issues simple and accessible to the population in order to make them workable. They recognise that the local community understands best.
1137. Infrastructures are in place here, and the existing system does not need to be tweaked much. As a health visitor, I noticed a headline in the ‘The Guardian’ in 2004 — it may have passed members by — that described 1994 as the “year the tots grew out". A researcher from the University of Manchester, who was not from a health background, considered the health visitors’ percentile charts. Every health visitor who visits a family checks babies’ weight, height and head circumference. The researcher examined the composite information and concluded that three-year-olds started to show a trend towards obesity in 1994.
1138. I am unsure why we cannot share that information. Rather than collect information on individuals, we need to collect that information and, thereafter, consider real public health practice. Our system tends to focus on the individual, which is why debates tend to be around hospital beds; one person fits in one hospital bed. We must consider the issues in a community context. We need to create more life pictures.
1139. We have excellent resources. The Northern Ireland Statistics and Research Agency (NISRA) website proves that we have good access to resources. However, those resources are not filtered down. Every citizen has a right to know the risks of living in a particular area. For example, a person has a right to know that his or her life expectancy is 17 years less in a particular area. How can we change that situation and provide people with that information? People have a right to information. We tend to use language such as “service user engagement". We should change that type of phrase, because it suggests that a person uses a service rather than being part of that service.
1140. Cuba uses that information to ensure that the public feel part of the system. The public are creating the system; they are real stakeholders. In Cuba, they do not use the language of “stakeholders" or “user". They focus on citizens.
1141. We have the information, but it will take a change in mindset, which it is possible to achieve. It will take no additional money; it will be cost-effective if we just ensure that people living in areas are familiar with the situation.
1142. Mr Gardiner: Thank you very much, Dr Lynch, for the presentation and for the photographs that you provided. It immediately struck me that there are more females trying to keep fit than males. The men in the photographs are like beanpoles. Is there a reason for that?
1143. In Northern Ireland, we pride ourselves on the Health Service that we offer to our community and citizens. However, Cuba seems to be more active on obesity than we are. Can we pinpoint our problems? What should we put into action?
1144. Dr Lynch: The dominance of the women was not noticeable to me, but perhaps that is my bias. There is a very slim older man in the photograph. When that photograph was taken, there was an exercise wherein older people stand balanced on one foot in order to improve balance and co-ordination. The gentleman in question sat that one out. I thought that he was not putting in as much effort as the women, as it transpired that he was 95 years of age. It is very powerful to see this system in action, in which someone in his 90s is actively involved. It is still not too late to focus on prevention.
1145. Mr Gardiner: It speaks well.
1146. Dr Lynch: It does, but get down there to see it in action.
1147. In preparing for this session, I revisited some of the literature, and I commend to you an article by Sharon Friel, Mickey Chopra and David Satcher, “Unequal Weight: Equity Oriented Policy Responses to the Global Obesity Epidemic", in the ‘British Medical Journal’ in 2007. The authors highlight the fact that obesity is a multifactorial problem:
“Missing in most obesity prevention strategies is the recognition that obesity — and its unequal distribution — is the consequence of a complex system that is shaped by how society organises its affairs."
1148. That recognition is also missing in Northern Ireland. For example, I met some young parents in Sandy Row as I was on my way to Queen’s University from the Europa bus station. I asked them about parks and facilities. Down there, one often sees cars parked on both sides of the street and children out on little bicycles. The place is not really conducive to children’s play. The parents told me that the nearest park, which is not Botanic Gardens, is not a place in which parents want their children to play.
1149. If we are serious about a policy that is conducive to health in every sense, including to the prevention of obesity, we need to look at safe areas that enable children to be active and to play safely. It is not just about health; it is about linking up education so that people can make informed decisions. It is all very well having information printed, but people do not understand what is meant. Education, play facilities and transport are all interlinked. Every Department can assist with this.
1150. Mr Gardiner: In many schools, and particularly in primary schools, exercise is being introduced more and more, at least compared with the situation over the past 10 years.
1151. Dr Lynch: You are right. There was a policy that was working against that. Schools are playing their role, but children also spend a lot of time outside school. There is a move in many schools to open up their facilities, and that is very welcome. However, there is much to be said for creating safe spaces for children to ride their bicycles and to use roller skates and skateboards so that they can exercise more.
1152. Mr Gardiner: I agree that there is room for improvement, but you definitely practise what you preach.
1153. Dr Deeny: You are more than welcome, Una. I would love to go to Cuba to see how primary care works there. At long last, we are starting to see that health promotion and disease prevention are the way forward for a much healthier population. There is far too much short-sightedness in the Health Service here. We wait until someone gets a disease and then we treat it, but, if health promotion and disease prevention were taken on, we would save loads of money. As a GP, I am very interested in that. For well over 20 years, I have seen protocols and strategies, and I am fed up to the teeth with them. It is, as you said, information overload. It is good to hear about Cuba’s action plans.
1154. You mentioned that community involvement, through a local health committee or something similar, runs primary care in Cuba. How exactly does that happen?
1155. More and more healthcare provision is moving into the community. As healthcare professionals, our concern is whether we will have the financial and personnel resources to meet that challenge in the future. I hope that we will. Is primary care in Cuba provided with the finances and the personnel? It seems to be, so perhaps that is an easy question.
1156. My final question is the big one. How can the Department of Health, Social Services and Public Safety, and the Minister, be convinced that the future lies in focusing on primary care rather than in having a divide between primary and secondary care, which I have seen for years?
1157. Dr Lynch: I thought that those were all big questions. I am very happy for you to head to Cuba. I can set that up to be done cost-effectively. I could set up accommodation for you in the school of public health, and it would not cost much. The system in Cuba is an inspiration to anyone who works, or is interested, in public health, and it shows us that we can make a difference.
1158. I shall start by explaining the governance structures. The community health committee comprises the family doctor, the family nurse, representatives from the local schools, grocers, bakers, people who are responsible for transport, and so on, and local elected representatives. Every six months, the committee plots out its action. That health committee also has a governance role relating to what happens in the practice, and we also have lessons to learn from that.
1159. To give an example: I worked with a GP in Havana, and, towards the end of the placement, I took her out to lunch. She had been on holiday, so she should have been relaxed, but she seemed anxious. She told me that she was anxious because she had to appear before the health committee. A child from her patch with whom she had been working had been born at 36 weeks. By any stretch of the imagination, a birth at 36 weeks is not a big problem, but it is officially classified as being an early birth, and the baby is classified as having a low birth weight. The baby was absolutely fine, but it is standard practice that a health committee gets together to revisit the pregnancy to see whether anything could have been done during the pregnancy that had not been done and whether something could be learned from it. That was not done in a defensive way or as part of a blame culture but to ensure that it did not happen again.
1160. That is only one example of how the committee works. Everyone works together; it is not only the doctor’s responsibility but that of other people in the local community. People are employed at municipal level to oversee the functioning of those health committees and the taking forward of action plans.
1161. I shall give another example of how that needs analysis works and how it is responsive. The demographic challenge that Cuba faces is similar to ours in that we have exactly the same life expectancy, although Cuba has a slightly larger percentage of older people. The challenges are the same; as the population gets older, more people will have diabetes and heart disease. For that to be managed effectively, people need to be seen early and in primary care.
1162. The next stage up from the family doctor/family nurse is the polyclinic. Unlike our polyclinics, those in Cuba function 24 hours a day, seven days a week. They are serviced by GPs, who feed into it. I was in Cuba for three months, and, eight weeks after leaving, I came back for a further six weeks. In that space of time, the Cubans had been feeding their profiling data up to a national level.
1163. In Cuba, rates of car ownership are low, and older people face challenges using public transport. Consequently, they are unlikely to use public transport. Similarly, older people are more likely to need specialist medical services. Therefore, cardiologists are sent to the polyclinics. Depending on needs profiles in the area, cardiologists might be there for one to five days a week. The same arrangement applies to endocrinologists, and so on.
1164. Interestingly, in 1984, Cuban doctors did not want to work in primary care; it was not considered an exciting part of medicine. Today, primary care is where it is at, and all doctors want to get into it. It is not about money; in Cuba, people are not generally motivated by money, and doctors there are not offered financial incentives. Initially, the Cuban Government used access to housing to encourage doctors and nurses to work in primary care. Nowadays, family doctoring and nursing are recognised as the exciting areas of healthcare.
1165. Healthcare professionals in Cuba do not use the words “primary" or “secondary" care, and, if we wish to get rid of that split in the Health Service, we need to devise a system that concentrates exclusively on serving the public. It is irrelevant where care is delivered. It should be focused on the needs of the population. Therefore, your point is well made; we need to get rid of the division between primary and secondary care. It should not be about a competition for budgets and who gets what. Rather, it should be about how to best serve the needs of the population.
1166. With respect to resources —
1167. Dr Deeny: The Department and the Minister seem to be focusing on primary care.
1168. Dr Lynch: Everyone here on the hill depends on public support, but members of the public do not talk about primary or secondary care; they just know that the system is not working. If people were better informed about the burden of risk on certain communities, there might be greater accountability. As Fidel Castro said: “el maldito dinero" — that awful thing, money. Do not let money get in the way. We must decide where we want to go and what we want to achieve, and then work towards those goals. The difference between Cuba and here is that, having decided where we want to go, we tend not to get there for this, that or the other reason, whereas the Cubans decide where they need to go based on their citizens’ needs, and do what is necessary to get there. If we set clear goals, things will fall into place. It is not always about money.
1169. Mr McCallister: That was an excellent and interesting presentation, and I would be happy to join Kieran in Cuba.
1170. One of the striking, and alarming, facts to come out of your presentation is the 17-year difference in life expectancy between two parts of the country. I wish to tease out some of the points that you raised. The new Public Health Agency, which the Deputy Chairperson mentioned, provides an opportunity to focus on some of the points that you raised. Moreover, during the inquiry, we have come to realise that many of the things that need to be done do not involve rocket science; it is just a matter of doing much better in some of the areas that you highlighted, such as community planning.
1171. Kieran referred to local health committees, and it seems to me that we are getting stuck in our attempts to deliver services on the ground. Regardless of whether councils or the Assembly are responsible, we must remain focused on the agenda of decentralising care and delivering services locally. On average, how many people do local health committees serve? How local is local?
1172. Dr Lynch: I am delighted by the growing list of people who are going to visit Cuba, because they will be made very welcome. Cubans are the last people to blow about what they do; however, once people come to visit, they are open and generous in sharing information with them.
1173. The family doctors and family nurses work with populations of between 1,000 and 3,000, and there are local health committees at that level. The family doctor/family nurse practices feed into basic work groups, which bring together between 10 and 15 practices, and those feed into another group. It is a matter of acquiring information about the local population at a low enough level. We get caught up in whose responsibility it is rather than getting down to the grass roots and creating family practices and other facilities in housing estates.
1174. A great relationship and trust is established between patients and general practitioners and nurses. We have a very sophisticated system that involves district nurses, health visitors, midwives and social workers. Northern Ireland’s capacity for an integrated system is a strength that other parts of the UK have not had, and we can create something that feeds in at policy level. It is important that we start with the really vulnerable populations. There are already good models and initiatives such as the health action zones and Sure Start.
1175. I did a wonderful interview with Francisco Ochoa, and he said that the Cuban system has evolved, which is why, in my submission, I used the metaphor of a repaired umbrella that is continually evolving. There is a notion that it is difficult to make changes within socialism, but healthcare in Cuba has evolved. Francisco laughed and said that he had travelled the world and seen pilots, particularly in Europe, that have gone on for 20 years. We are good at initiating small-scale measures such as health action zones and Sure Start, but we need to take measures on a larger scale. If the political will is there, anything can happen.
1176. Mr Gallagher: Your very good presentation makes it clear that we can learn important lessons from the Cuban system. I am sure that you will agree that there are different circumstances in the two countries. Indeed, you talked about the disposition of the Cuban people and how they have a different lifestyle to people here. They are more relaxed and comfortable with themselves, which is probably a relevant factor. The climates are also very different; people in Cuba can spend many more hours outdoors in most seasons, and that helps them to have more active lifestyles.
1177. Given that Cuba is an island and the political circumstances in that part of the world, I assume that Cuba is fairly self-sufficient in food production. I am sure that the Cuban climate helps the growing of a great variety of fruit and vegetables. Can you comment on Cuban people’s diet and how it contributes to how long they live?
1178. Dr Lynch: One does not go down to Cuba for the food, because the food is terrible. Cubans eat lots of fried food. They have lived through difficult times, particularly with the collapse of eastern Europe in the 1990s. Cuba was isolated not only geographically but politically. It went through the same situation then as we are going through now.
1179. You made a point about fruit and vegetables. Cuba has a warm climate, but its location in the hurricane belt means that its production is challenged. The hurricane season is between May and November, and Cuba has developed great practices to manage that. It has been able to keep mortality rates low. In fact, its production of fruit and vegetable is not great.
1180. In his interview, Francesco Ochoa said that Cubans’ diet is appalling. There is a notion that they are never satisfied and that they continually want to do better. Cubans love pork — a bit like we love our bacon. Therefore, they consume a lot of pork and fried food. It is certainly true that they do not consume much processed food. However, their diet per se is not particularly good.
1181. Cubans take plenty of exercise, partly because of transport problems. However, the Government create interest in, and an appetite for, sport among children. Baseball is Cuba’s national passion, and anyone who is interested in sport likes baseball. Participation in sport is considered to be a citizen’s right, so entrance to baseball games is free. Compare that with rugby or GAA. In Cuba, entrance to games is a right, which encourages interest in sport.
1182. Participation in dance is also encouraged. It is not considered to be a pastime for elite children, and all children can take part in dance. For example, Cubans are encouraged to go along to the national theatre and attend the ballet. I paid around $40 to watch a performance. One US dollar is worth around 21 Cuban pesos. Cubans pay five pesos to watch the national ballet or to visit the theatre. Therefore, the culture promotes exercise from childhood onwards. It promotes dance as a form of exercise, and sport.
1183. The Cuban diet is not great, and the Government are working to improve it. Television programmes educate people about food and teach them how to cook. If you visit Cuba, it is not for the food.
1184. Mr Gallagher: Do Cubans eat largely home-produced food?
1185. Dr Lynch: They do, largely. However, much of their food, particularly chicken, is imported from the United States.
1186. Ms S Ramsey: I welcome Dr Lynch to the Committee. Her presentation was great. I have been to Cuba, and I agree that dance is one of the country’s major pastimes for people of all ages. No matter where you are in Cuba, you can turn around and see people dancing in the streets.
1187. Mr McCallister: Did you participate, Sue?
1188. Ms S Ramsey: I did indeed.
1189. A key lesson is that we should not be afraid to look at other countries and to learn from best practice elsewhere. The inquiry has meant that, although we are the Committee for Health, Social Services and Public Safety, we have been in touch with various Departments because we know that obesity is not only a health issue. That will be reflected in our recommendations. The health budget is a sizeable portion of the overall Budget. A key aim of the inquiry is to show that obesity is not always a health issue: it is also about prevention and exercise.
1190. I want to take a holistic approach to the issue and not simply focus on health. We operate in the context of the outworkings of the review of public administration, devolution and local Ministers, the majority of whom live, work and socialise in the constituencies that they represent; that is good. You mentioned the health action zones, and I have seen the positive work that they have done on specific issues. However, in certain constituencies, it is piecemeal. We must consider that issue.
1191. The Deputy Chairperson made a point about a specific needs analysis for the North and its health boards, which can be extended to the border counties and throughout the island. We must also consider that issue. I have used this example before: in some constituencies, there has been an increase in asthma. It is accepted that the planting of more trees can have a positive impact on reducing the instances of asthma. The Department for Social Development has planted trees in various constituencies to address that. Although asthma is a health issue, the Department for Social Development had the authority and the money to deal with it. It just takes small tweaks here and there.
1192. I agree with you about the Investing for Health strategy. Kieran Deeny made a valid point. I was a member of the Committee for Health, Social Services and Public Safety when the ‘Investing for Health’ report was brought forward by Bairbre de Brún. I agree with you that it was visionary. It was probably the first time that all the Departments got together with the Executive and considered investment in health. It was not just a health issue. Do you believe that other Departments still play their part in the Investing for Health strategy? Do you believe that, with the establishment of the Public Health Agency, public health and prevention will take centre stage or will it remain a poor cousin?
1193. Money has been mentioned a few times. Do you think that we need to overhaul the boards’ funding formula? We must get away from the piecemeal approach. Do you think that there is a need for the Department of Health, Social Services and Public Safety to overhaul it?
1194. Department of Education officials gave evidence some weeks ago, and we had two Departments fighting over which would fund after-school projects and breakfast clubs. It is all very well for the Executive, Ministers and Committees to be visionary, that mindset still prevails among civil servants. Their approach is one of “we can only go so far" and “it is not my responsibility" instead of a collective approach.
1195. Your presentation was top class, and I recommend going to Cuba to witness its healthcare system at first hand.
1196. Dr Lynch: It will be only when the Departments work together and have some joined-up thinking that a difference will be made.
1197. The Assembly is a fledging Administration, and we are only getting on our feet. I do not for a moment advocate that the current membership should still be here in 50 years, but the Cubans have had 50 years of continuous Government, and that shows that much can be achieved through joined-up thinking and working together.
1198. From 2002, devolution has been synonymous with public health. The new Public Health Agency is most welcome because it puts public health on the agenda. It is early days: some things could be tweaked and worked out, but I am optimistic about how it will work. Your example of tree planting is exactly the sort of thing that does not cost much in resources but is sustainable for the future. It is a simple act that, done today, prevents expenditure in the long term. It is not always about money. Unfortunately, in Northern Ireland, money is always at the front of health issues. Some healthy discussion would help. There is a debate about the number of MLAs, but the number of MLAs could be a real strength if we take on board the notion of MLAs sitting on local health committees. Those committees would be spread out across Northern Ireland, and MLAs would bring their voices right into Stormont.
1199. That would make a genuine connection from the grass roots to Stormont, and that is the link that is missing. We tend to talk in grandiose language and produce beautiful documents. Last night, I spoke to Dot Kirby, who is a former BBC Northern Ireland health correspondent. She said that one could always judge the importance of a report by the weight of the paper and the colour quality of the photographs. Perhaps there should be an embargo on coloured documents and strategies, and we could focus on actions and on what people see on the ground. We could save much money on that and spend it in small ways to make a difference.
1200. As for funding, healthcare is not necessarily about money. We all need to take a long hard look at ourselves and think about how we can do better with our resources. More money would be welcome and would mean that we could do an awful lot more, but we are already much wealthier in every sense: we have a highly educated country; we are a small country; we have a great environment. We have scope to do so much.
1201. There is a short-sighted notion that it takes the market to sort out the health system. I went to Cuba with that notion. We have an ageing population, and the risk of older people developing cataracts will increase. Cuba has the capacity to meet the needs of more than its own population. When I was in Cuba, an apartment block was being used to treat people who were flying in from Venezuela every day to the misíon milagro — the miracle mission — where cataracts are treated and people are given back their sight.
1202. People arrived from Venezuela, were taken by bus to the apartment block, went by escalator to the top floor and gave a blood sample. They then went back down and settled into their rooms. Later that day, they went back up and were seen by a general physician, an ophthalmologist and an anaesthetist. If they were deemed fit for surgery, off they went and had their cataract treated and returned to Venezuela a few days later.
1203. That is happening in a developing world country that is able to plan strategically by using information. We are closing hospitals here. Northern Ireland could be a centre for health tourism. We could sustain hospitals in rural areas and build up an infrastructure if there were a wee bit of imagination. We are bringing in teams from elsewhere to treat cataracts in Northern Ireland. Therefore, it is not always about money; it is about using what we have.
1204. Mrs Hanna: Good afternoon, Una. You are very welcome. We have a great opportunity through this obesity inquiry and the establishment of the new Public Health Agency. The timing is right to try to make a difference.
1205. I was fascinated to hear about a different culture, and we are all fascinated by Cuba. I have not been there, but I have read about it. It is interesting that, despite the fact that Cubans have far less money, they have equal or better health outcomes. You said that health workers are charged with looking after the health of others. You spoke about 24-hour clinics and specialists going to the people. We have had debates about that here, but we have not done anything about it. Equipment is often unused from 5.00 pm and over the weekends, yet we have long waiting lists.
1206. You talked about the Cuban diet and the fact that they do not use processed food. However, we are told that exercise really makes a difference. It is not that people are eating so much more but that we have sedentary lifestyles, and people are not burning calories.
1207. We do some positive things in the community. We plant trees, and we are considering more playgrounds and parks. Does Cuba experience antisocial behaviour as we do? If a tree is planted here, it almost needs a 6 ft wire fence with lights on the top to stop people from pulling it down. As for attitudes to health, we are inclined to depend more on the Health Service. We have all seen the “I need a prescription" and the “doctor, doctor" advertisements.
1208. How do we encourage or empower people to take more responsibility for their own health? Is the situation any different in Cuba? There is also the issue of tackling and challenging lifestyles — for example, smoking and drinking. I appreciate that there is a better chance of scoring hits with prevention and early intervention. However, it is harder to pick up the pieces, and, in the Health Service, we are inclined to pick up the pieces all the time. So much money goes on picking up the pieces that it is a vicious circle.
1209. We do not seem to be able to prevent or to intervene early because we spend so much time picking up the pieces. However, a start has been made with children, and Sure Start is an example of good practice. However, pilots can go on for ever. We do not evaluate pilots, and good pilots are not mainstreamed. It does not matter whether they are good, bad or indifferent. They are not judged on their merits, but some of them last and some of them are dropped, even if they are good. That is where we fall down. The culture should be about getting down to the grass roots to try to make a difference. There is a huge difference between the haves and the have-nots. That is an issue for the Committee. How do we encourage people and communities to take more responsibility and work with health professionals to consider their own health?
1210. Dr Lynch: That means that you are on the list to go to Cuba. If you go, you will see it in action. It is about rights and responsibilities. No matter where one goes in Cuba, one will see notices giving information about rights and responsibilities; it is double-edged. People can realise those responsibilities only if they are given education.
1211. You mentioned vandalism; I will quote another Latin American, Paolo Freire, whose work advocates practices similar to those in Cuba. His view is that people talk by their actions; actions are often more expressive than words. When people are destructive, it usually means that they do not feel included. People feel excluded and alienated from society. In Cuba, work is done to create that engagement and bring people in. In socialism, there is a strong notion about the pursuit of the perfect human being; socialism recognises that everyone is intrinsically good. In Cuba, all citizens are valued, whoever they are, and engagement is promoted. The work that is done with people with disabilities is amazing, and carers of people with a disability are prioritised.
1212. I will provide Committee members with a copy of a ‘British Medical Journal’ article that highlights the challenge of trying to address the obesity agenda when faced with market forces that promote processed foods that are empty of nutritional value but very high in calorific value. If one goes to Cuba, one can see the exchange. It is about citizens engaging with the health professionals. The health professionals do not have all the knowledge; we all have different pieces of knowledge, and we are in it together.
1213. Mrs Hanna: Are the differences between Northern Ireland and Cuba down to the ethos of socialism and the different culture?
1214. Dr Lynch: In Cuba, medicine and nursing are considered as vocations, and humility is valued; perhaps the greatest insult that one can give to Cubans is to call them ostentatious or arrogant. They pride themselves on humility.
1215. Mrs McGill: Thank you for your briefing, Dr Lynch. In your paper, you mention equity; it is written on the umbrella diagram. Is there equal access to all services throughout Cuba? I am from the west, and we have had several debates about the provision there. Tommy and Kieran will be aware of that. You also mentioned hospitals in rural communities. I will not go over all the argument again, but I am interested in whether there is equal access to services in Cuba. Although Cuba focuses on primary care, that clearly is not the case here, and we rely not so much on prevention as on dealing with problems when they arise.
1216. In the area that I represent, for example, the out-of-hours provision is changing, and we are concerned about that. That service will move from Strabane — a small rural town — to Derry. People feel that the services there have been reduced. I am not clear, Dr Lynch, about how that can be addressed.
1217. It was interesting to hear that the Cuban diet relies so heavily on fried foods and contains little fresh fruit and vegetables. As for exercise, if we had Cuban weather, people might be more encouraged to go out and exercise in the morning, and so on.
1218. At the start of your presentation, you used the word “epidemic" when referring to obesity. If the health system in Cuba were transposed here, would it end the obesity epidemic?
1219. Dr Lynch: The Cubans would be the first to say that their health system is particular to Cuba. The health system that evolves in each country is reflective of its context, and Cuba has a particular political context and structures. One could not simply take the Cuban model exactly as it is and bring it into Northern Ireland. However, key elements of that model, such as the focus on primary care, equity, needs assessment and community participation, could be central to our system. The health system in Cuba has evolved over 50 years. It would, therefore, be difficult simply to introduce it here.
1220. Mrs McGill: As far as the Committee’s inquiry into obesity is concerned, is Cuba, therefore, not a particularly good example of what can be done to address the problem?
1221. Dr Lynch: It is in a sense, and that brings me on to the second part of my answer. Cuba has managed to create its current health system because it has a strong political will to ensure and safeguard the health of the population. It has a Ministry of Public Health that is not one of the lowly Ministries. It is a powerful Ministry that influences the action of the Ministries of employment, economy, foreign affairs, and so forth. Everything is influenced by the Ministry of Public Health. It does not merely receive the crumbs from the table but influences the actions of every other Ministry. That is crucial. If we are serious about public health, it is not simply a matter of improving the health system; it involves all the wider social determinants of health.
1222. In answer to your question about the situation in the west, I may come across as a real fan of Cuba. However, before travelling there, I was suspicious of the socialist ethos and wondered whether I would be shown only the best aspects of the health system. I spent some time in Havana before travelling around the country. We know about Guantanamo because of the military base there, but it is a huge province in Cuba. It is the country’s most rural and isolated province, and I was curious about how well the health system worked there. It all worked well in Havana, but how would it work out in the sticks?
1223. It was simply amazing to see a family doctor/family nurse practice that was exactly the same as one in Havana, even down to the paint. The shortages in Cuba mean that the same green/blue paint is used on walls everywhere. The practices with GPs and nurses are exactly the same; all have health profiles on the wall.
1224. I interviewed the director of public health in Guantanamo, because it blew my mind how a country with the resources of Cuba was able to achieve that parity. I asked him about clinical governance, because we argue about doctors having to see a certain number of cases to remain clinically competent, and so forth. I asked him how he ensured the clinical competence of practitioners. I wish that I had brought a video camera at that point, because he looked at me as though I had two heads. That is when I realised that our system is focused on profit and the market.
1225. He told me that the citizens in Guantanamo have the same rights as the citizens in Havana and other parts of Cuba. Therefore, the surgeon or doctor must, of course, be competent, so their duties were rotated to ensure that they retained their level of competency. Geographically, Cuba is a much bigger country than ours, but there are ways in which systems can be put in place to ensure that the citizens, irrespective of where they live, are not subject to bias.
1226. The Cuban example is a challenge. They do not look two or three years ahead; they have a vision for five, 10, 15 or 20 years into the future. The Cubans argue that to close down a service in a certain area and to remove its capacity and infrastructure will result in an urban migratory shift, which itself creates problems and depletes capacity. Consequently, there is a bias towards an ageing population and other related factors. The Cubans take a holistic view; it is difficult to do it justice in an hour’s discussion. I recommend that the Committee go to Cuba and see the system upfront, because it challenges the notion that there is only one way to do something.
1227. The Deputy Chairperson: I take your point about rotating doctors in order to maintain their competences. Trusts have had to close hospitals in rural areas because the doctors say that they cannot maintain and update their skills. The simple answer to that would be to rotate them among the other hospitals in the trust area. That seems like the logical thing to do, even at GP level.
1228. Dr Lynch: It goes back to the mindset of what the system is there for. Is its purpose to protect public health, or is it to make life comfortable for the people who work in it? If we mean to put citizens’ public health first, we must create systems that support that. The solutions can be found if there is a political will to make something happen.
1229. The Cuban people make incredible demands on their health service and have huge expectations. The Cuban Government are very pragmatic; when we asked them why they set certain priorities, they told us that, if they did not do things in a certain way, they would lose the support of the people, and the revolution would not continue. It is all about political will.
1230. Mrs Hanna: Are you saying that we need a Castro? [Laughter.]
1231. The Deputy Chairperson: That concludes our questions. Thank you for coming along; it has been a very interesting presentation, and it will help our inquiry.
11 June 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mrs Carmel Hanna
Mr John McCallister
Witness:
Mr Michael Bell |
Northern Ireland Food and Drink Association |
1232. The Deputy Chairperson (Mrs O’Neill): Our first evidence session is with the Northern Ireland Food and Drink Association. Members have copies of the submissions from the Food Standards Agency, Safefood, the Food and Drink Association, as well as a briefing paper from the Assembly Research Services. I welcome Michael Bell, the executive director of the Northern Ireland Food and Drink Association. He will give a brief presentation, after which members can put questions to him.
1233. Mr Michael Bell (Northern Ireland Food and Drink Association): I will start by telling the Committee who I am and why I am here. I have been involved in the local food and drink industry for 25 years. I was involved in manufacturing for 12 years and have been representing the industry for some 14 years. I am also a chartered food scientist. After putting Northern Ireland food and drink into context, I will address the questions posed by the Committee.
1234. How important is Northern Ireland food and drink to Northern Ireland? It is the biggest industry, bar none. In 2007, our turnover was £2,724 million — that is, £2·7 billion. We employ 18,400 people directly, a further 25,000 farmers depend on manufacturing, and 10,000 people work in haulage, hygiene, cold storage and other services. Some 20,000 people work in food retailing in the Province. In total, approximately 80,000 jobs are dependent on the agrifood sector in Northern Ireland, making it far and away the biggest part of the economy. Of the £2·7 billion turnover, 65% is exported, of which 41% goes to GB and the rest to the Republic of Ireland or the EU.
1235. That is the good news. The not-so-good news is that the industry’s profit margin is, at 2·8%, very low. I am happy to give the Committee copies of the statistics. All the statistics that I quote come from the Department of Agriculture and Rural Development, and they can be accessed from its website.
1236. To underline the importance of the industry, 19% of total manufacturing sales in Northern Ireland come from food and drink. It accounts for 15·8% of external sales and approximately 24% of all manufacturing employment. One of my member companies employs more people than Shorts. It tends to be overlooked because it has always been there as a background industry. However, I want to stress that it is extremely significant. The industry is a big supplier to GB.
1237. What is the role of the Northern Ireland Food and Drink Association in the industry? Our vision is of a sustainable, strong, growing cluster of local quality food and drink enterprises. The association will build an internationally competitive industry that will create wealth for our society stakeholders.
1238. If I have read the Committee material correctly, the obesity agenda is the focus for today, and the association engages with that agenda in several ways. Our members are increasingly engaged in providing nutritional labelling on packaging. Virtually all our members’ products at the retail channel display either the Food Standards Agency (FSA) traffic-light system or the guideline daily amount (GDA) system. To date, that is less developed at the food service channel. However, the association is active at the local food service channel through its subsidiary company, Taste of Ulster; I brought some materials for the Committee on that.
1239. Members of the FSA and I sit on a food subgroup of the Department of Health, Social Services and Public Safety. The subgroup is preparing a paper on obesity for the Minister, and that is due in early 2010. Our members are also engaged in the reformulation of products in an attempt to reduce sugar, fat and salt as per FSA and Westminster guidelines.
1240. However, having said that the association is engaged in those activities, I must make one or two things clear. No one has more of a vested interest in healthy, happy consumers who live for a long time and eat many of our members’ products than the Northern Ireland Food and Drink Association. The Government appear to have missed that point, so we have been consistently making it to them. There are no bigger stakeholders in this matter than our members and our industry. Without healthy consumers, we would have no industry.
1241. The complexity of the issue is worth mentioning. There is a shared responsibility for the obesity agenda, which is complex and multifaceted, and a co-ordinated approach is required to prevent and address the problem effectively. Responsibility for addressing the problem must be shared by Government, sectors, professions, communities and individuals, and, in order to get anywhere, we need integration and harmonisation among those stakeholders. Furthermore, a commitment to taking action based on evidence rather than opinion is vital in making progress.
1242. My final two points are important. First, in light of the economic position in which we find ourselves, work on the obesity agenda must achieve the maximum impact and outcomes for the minimum cost; we must achieve value for money. Secondly, local needs must be addressed.
1243. I was struck by a statement from our colleagues in the Scottish Parliament, in which a Minister said that, although Scotland produces some of the best food and drink in the world, it has the worst diet and health. I do not agree with the first part of that comment, but I am struck by the fact that the Government there are trying to address both matters simultaneously.
1244. I have more material that should be useful to the Committee, so, if you are happy, I will download some of it for you. I am happy to answer questions.
1245. Sir Liam Donaldson, the Department of Health’s Chief Medical Officer, stated that the core issue is that only 6% of people understand the risks of being overweight. Obesity is seen as a vanity rather than a health issue, and we must change that mindset.
1246. In late 2008, the Cabinet Office, to which the association gave evidence, published a paper on the food industry, ‘Food Matters: Towards a Strategy for the 21st Century’, which states:
“The Government’s vision for the food system is one that is more sustainable — economically, socially and environmentally. The future strategic policy objectives for food should be to secure: fair prices, choice, access to food and food security through open and competitive markets; continuous improvement in the safety of food; a further transition to healthier diets; and a more environmentally sustainable food chain."
1247. Our industry believes that Northern Ireland is uniquely situated to make great strides on the environmental agenda and, indeed, on the health agenda. However, we need commitment from the Assembly.
1248. There is a presumption that much of the obesity agenda can be addressed by the food and drink industry in isolation from other stakeholders. That ignores the energy output agenda. To illustrate the energy output agenda, I will quote some statistics from ‘The Times’:
“On average British children spend five hours and 18 minutes watching television, playing computer games or online each day. The total of 2,000 hours a year compares with 900 hours in class and 1,270 hours with their parents."
1249. The elephant in the room is that children are becoming incredibly sedentary. I am happy to pause there. As I said, I have a significant amount of material on which to draw.
1250. The Deputy Chairperson: Thank you, Michael. I neglected to apologise at the start of the meeting for having to rearrange your visit to the Committee; you were due to come along three weeks ago.
1251. I will pick up on a few points. You said that the association’s members are actively engaged in the labelling system, whether traffic light or GDA levels. Are all your members involved in that?
1252. Mr Bell: To answer that question, it must be understood how food is distributed from our members to the public. Approximately 60% of the food goes through food retail — that is, the shops that we all use. An estimated 40% is distributed through food service — restaurants — which do not have a point-of-sale, nutritional-labelling system. Therefore, 40% of the food distributed by our members through that channel is not labelled, because the portion size is beyond the manufacturers’ control. It is supplied to a restaurant as an intermediate and is portioned as that establishment sees fit.
1253. In respect of food retail, the answer varies. Manufacturers may sell goods bearing their own label, in which case they have complete control of labelling, and, as required by law, that virtually always carries nutritional information. Beyond that, those manufacturers are moving towards GDA or FSA-style labelling. However, a significant proportion is sold as retailer-own product by major supermarkets under their own label. In that case, the supermarkets, not the manufacturers, control how the labelling is presented. I hope that that is clear.
1254. The Deputy Chairperson: Yes, that is fair enough.
1255. Mr Bell: There are different channels. My members can control some matters, but there are quite a few that they cannot.
1256. The Deputy Chairperson: You stated that the public presumed that obesity can be tackled by the food and drink industry alone. The Committee recognised early in the inquiry that that is not the case and that tackling obesity is also about people becoming active. The relationship between consuming too many calories and weight gain is accepted, but there is less recognition of the link between alcohol intake and calories. Is the drinks industry doing anything to raise awareness of that issue?
1257. Mr Bell: I cannot represent the drinks industry per se. My association does not have alcoholic drinks firms as members; they are represented by a separate organisation. However, I can comment that alcohol is a significant calorific contributor in, and rising component of, the diet. In response to the FSA draft plan that is out to consultation, my association has stated that it is illogical for the FSA to discuss sugar, fat, salt and calories but make no mention whatsoever of alcohol or of fibre, which remains critical to the debate because fibre has a dramatic affect on how much sugar, fat and salt is absorbed and retained.
1258. Mr McCallister: I register an interest. I am a shareholder in a milk-processing company, which may be a member of the Northern Ireland Food and Drink Association.
1259. Some of the evidence that the Committee has received suggests that calorie intake has not increased dramatically over the past 20 years in comparison with weight gain in the population. Therefore, the Committee accepts that a sedentary lifestyle plays a key role in obesity, which leaves just about everybody with a part to play. Evidence suggests that the FSA tends to target sugars, fats and salt for food labelling. Although it is fine to reduce those ingredients in some products, how can people be encouraged to eat a balanced diet, bearing in mind that we need a certain amount of everything for a balanced diet? Does the food industry have a problem with the FSA’s approach to food, especially to salt?
1260. Mr Bell: The science of nutrition is young and evolving. In my working life, nutritional messages have been stated, withdrawn a few years later and a different position adopted. That has turned the public off new nutritional messages.
1261. The FSA and the Government are committed to their 6 g a day of salt. As a scientist, however, it is wrong to say that 6 g of salt a day is the right amount for everyone. Body mass, diet and metabolism rate all have an effect, as does whether one burns 2,000 calories or 4,000 calories a day. However, the message that society in general needs to reduce its salt intake is correct, and the Government chose to use that mechanic to address the issue.
1262. The problem that association members and I have is best illustrated by a specific incident. In 1987, when I was technical director of a large and well-known Belfast bakery that has since ceased trading — the brand name lives on, so I will not name it — we were asked by the Government, in the original Committee on the Medical Aspects of Food and Nutrition Policy (COMA) report, to reduce salt in the product. The industry dropped salt from 2·2% to approximately 1·8% in finished products, and sales immediately nosedived.
1263. At the same time, the Government were telling people to eat more bread, particularly wholemeal bread to increase fibre intake. Salt plays a major part in making wholemeal bread palatable, because it is quite insipid without salt. As a result of sales nosediving, the industry returned to the previous salt levels.
1264. Furthermore, trying to adjust the formulation of individual products, apart from the accusation of nannyism from the state, flies in the face of what our European colleagues are doing. Every chef in the land will talk about Parma ham or prosciutto, and hold them up as super-products and include them in their dishes. They contain more than 4% salt, which is twice as salty as any product in our market. Therefore, we are not standing back and considering balanced diet and exercise. Instead, we are focusing on reformulating all the food in the supermarkets and thinking that that will address the issue. It might, but probably not in my lifetime.
1265. Evidence for that comes from what has been learned about smoking. I do not know whether there are any smokers in the room who read what is printed on cigarette packets — before they are taken out of public view in shops, which is the next Government proposal. To print on a product, in huge black letters, that it will kill you had minimal effect on particular social groups. In fact, consumption is still increasing. That tells me that the public are beginning to become immune to messages, and the principle that the public’s behaviour will be changed by putting ever more information on the product is flawed.
1266. Mr McCallister: We want to give people the message that their diet should be balanced and contain a little bit of everything. Someone who eats a lot of Parma ham would have an enormous salt intake, but no one would suggest that a diet should consist entirely of Parma ham. I sometimes worry that, if the FSA targets one aspect of the diet, it might get a result for the overall population but not the desired balance.
1267. Mr Bell: The association expressed its concerns about that to the FSA. I encourage the Committee to read the London Department of Health’s short paper, ‘Economic Costs of Obesity and the Case for Government Intervention’. In that article, Barry McCormick logically argues that emphasis needs to be put on children. Once poor eating patterns have been learned, they are extremely difficult to correct. It is difficult to correct the poor life skills education that some youngsters have received. My 25-year-old niece now has perfect teeth because she was encouraged to eat more fruit and vegetables and screened from having too much sugar.
1268. Mr Easton: I agree with your suggestion that an overall approach should be taken. My stepdaughter spends all her time on a computer, which does my head in. She goes out with her friends but does not do any exercise, and that is probably not good for her longer-term health. You mentioned the effect that alcohol can have on weight, which I had not thought about. Indeed, it might be helpful if we got more information about how alcohol affects weight.
1269. Many people are so set in their ways that they may be incapable of changing their diets. I have been honest enough to say that, although I know about the traffic-light system, I go into the supermarket and buy anything that looks good. I am lucky that I am skinny, but one does not know what is going on inside the body; a heart attack, for example, may be just down the road.
1270. We talk about a multi-agency and multifaceted approach, but I get the impression that people will not listen unless they are forced to cut down on the fat, sugar and salt in their diets. Regardless of the traffic-light system, the majority of people will buy a product unless there has been a major health scare about it. We have an awful lot of work to do to change attitudes. I do not know how we will to do that, because we have given so many different messages.
1271. You mentioned that there was a reduction in the sale of bread that had been made healthier. Would serious cuts in the amounts of fat, sugar and salt in foods have drastic effects on food companies, leading to job losses, and so on?
1272. Mr Bell: I am afraid that the answer to that question is very complex. I represent about 140 companies that produce a combined total of some 2,000 products. Every one of those products is different and has a different level of sugar, fat, salt, some that is added and some that is not added. For example, butter is 80% fat, and spring water is 0% fat. However, water is toxic in overdose. Last year, a radio station in California ran a competition entitled “hold your wee for a Wii". A lady died after drinking five gallons of water in an attempt to win a Nintendo Wii.
1273. Everything is toxic if taken to an extreme. The central theme is balance. Correcting the ingredients of the members of the association’s products is like squeezing a balloon. If the balloon is constricted so that, in the retail channel, one can buy only products that are low in sugar, fat, salt and, therefore, somewhat bland, people will eat more carry-outs or make alternative meals at home, adding more salt.
1274. A behavioural pattern in Northern Ireland that amazes me is that people season food with salt and pepper before they taste it. I have observed that everywhere. Many carry-out and restaurant meals have a sugar, fat and salt loading that is worse than anything from a supermarket.
1275. I am sorry that that has not answered your question directly, but it would take a long time to unpack the issue because it would involve examining the issue sector by sector. The recession has had a significant effect on food-purchasing patterns and consumer behaviour. Although the overall turnover in the industry is significantly recession-proof, I will give one statistic to illustrate the point. Butter sales, year on year, have risen by 15%; for a while, the industry scratched its head and wondered why butter sales would increase during a recession. The answer is that people are making their own sandwiches at home. People who make their own sandwiches invariably use more butter than is used in commercially made sandwiches, which have a nutritional declaration that manufacturers are committed to meet and not exceed.
1276. Dr Deeny: You mentioned schools earlier; does your association have any input in schools? It is important not only to have input and output exercises but to have an input into what schoolchildren eat and drink — soft drinks, for example. A few years ago, I had an issue with my kids because they were drinking Coke until it was coming out their ears.
1277. Does your association have a responsibility to draw the dangers of some of those foods to people’s attention, or do you represent only the businesses that produce them? I hope that I have picked you up incorrectly, but it concerns me that you mentioned the advertising of cigarettes and said that, although there are warnings on the packets, they are more or less dismissed. That is not grounds for saying that warnings should not be given. Advertising has a powerful influence on what people eat. Does your association not have a responsibility to ensure that advertising is responsible and informative?
1278. Mr Bell: The answer to your last question is yes. Advertising by local food and drink manufacturers is relatively low-key and small-scale. That goes with the size of the industry. You are probably referring to major multinational companies with significant advertising capacity. Those multinationals can speak for themselves, and there are such companies based in the Province. It is laudable that soft drinks companies associate their products with calorie burn, as are the resources that they have put into promoting calorie burn and balanced diets.
1279. Some of the approaches that have been taken involve trying to win over the public by negative rather than positive messaging. The FSA used images of sick bags and slugs to try to change consumer behaviour at various points in the food industry. That imagery turns people off instead of encouraging them to carry the message forward.
1280. The obesity epidemic affecting the next generation will be won and lost in schools. It is an epidemic, and some of the worst statistics in the world come from these islands. I am struck by an experiment on snacking that a Welsh set of schools has been conducting for over 20 years. Fruit, vegetables and water were provided to a set of schools, and the subjects were tracked into their early adult life. The results showed a significant difference between them and a controlled population. That provides strong evidence that more intervention must be made at school level.
1281. Dr Deeny: Where does your organisation stand on the point that someone must keep a hold on businesses that are in the food industry only to make money? John referred to foods that have very high levels of saturated fats, salt and sugar. Someone must hold the industry to account so that the place is not coming down with foods that kids and adults see advertised on television and which will, in the long term, affect their health.
1282. Mr Bell: The paper to which I referred earlier mentions products that have a downside. That applies to almost everything that contains alcohol. If any product that is sold in an off-licence is taken to excess, it will take a male past the recommended maximum of 21 units of alcohol in a week. Alcohol has a significant downside, and it could have a further downside because it could lead to health problems, antisocial behaviour, and so on. The same argument can be made on tobacco. The sale of tobacco brings an economic advantage to the Government, and there is a list of downsides to it. The view has been taken that the downsides outweigh the upsides.
1283. The consumer’s right to choose food must be preserved, because very few products can definitively be said to be damaging. I have been challenged previously by people who have said that our members produce food that is unhealthy or bad. Not one of our members produces a bad food product. There are bad diets and bad consumption patterns, where people eat a particular product to excess, and it is not part of a balanced diet, but our members can provide only the information and the best-quality product possible. The dairy sector, for example, is a significant and high-quality industry, but to eat nothing but butter as a significant part of one’s diet for a significant amount of time would be damaging.
1284. The Deputy Chairperson: That brings the session to a close. Michael, I thank you for attending; it has been very helpful to the Committee.
1285. Mr Bell: Thank you. I shall leave some books for members, and I hope that you will visit some of the local Taste of Ulster establishments and sample the local food.
11 June 2009
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mrs Carmel Hanna
Mr John McCallister
Witnesses:
Ms Jill Fitzgerald |
Department of Education |
1286. The Deputy Chairperson (Mrs O’Neill): I welcome Louise Warde Hunter, Alan McMullan and Jill Fitzgerald, of the Department of Education, to the Health Committee. I invite you to make a presentation; the members may have some questions afterwards.
1287. Ms Louise Warde Hunter (Department of Education): There is much that I would like to say, but I appreciate that the Committee is short of time. Would a 15-minute presentation be reasonable?
1288. The Deputy Chairperson: We allow up to an hour for each evidence session; that includes your presentation and members’ questions.
1289. Ms Warde Hunter: Let me know if I am too long-winded on any area, so that I can move on to another. I want to do it in whatever way suits you best.
1290. Thank you for asking us to give evidence as part of your inquiry into obesity. We share the Committee’s concern at the rise of obesity and especially childhood obesity, which is the main locus of the Department of Education. The Department welcomes the inquiry and we hope that we can play our part in the shared drive to stop and ultimately reverse the trend. Alan McMullan is a former policy leader on school meals and the school food policy, which will be launched in September. Jill Fitzgerald is health and physical well-being co-ordinator for the Department. My background is early years, and I am new to this area. Forgive me if I read from my script.
1291. We understand that health-related policies span the whole of the Department, from what is taught in school to the design of schools, from school-based weighting and the measuring of programmes to the medical needs of individual children. We have a good broad knowledge of policies that contribute to obesity prevention. We will do our best to answer your questions. If there are questions that, between the three of us, we cannot tackle, we will take that away and give you formal written replies.
1292. You have seen the supplementary paper that was issued lately and which summarised the Department of Education’s vision and priorities. I want to make the connections between what we are trying to do and obesity.
1293. The Department of Education’s vision is to ensure that every learner fulfils his or her potential at each stage of development. In order to help us achieve that, our emphasis must be on learning and providing the highest quality of education for every child in a way that helps them transcend the barriers that they might experience in life. We are trying to raise standards for all and close the gap between the highest and the lowest attainments. However, there are also other important areas: how we develop the education workforce, improve the learning environment and transform education administration. Over the next 10 minutes, I will try to demonstrate to the Committee how all those points are linked to health and well-being and, in particular, to the issue of young people and obesity.
1294. Basic skills such as literacy and numeracy are essential to good physical and mental health. Last year, 47% of young people did not achieve a grade C or above in English and maths, and therefore our focus on raising standards is clearly important. In the revised curriculum, young people are not considered solely with reference to the qualifications that they acquire at age 16 or 18; we think of their holistic needs. They must be equipped to play their part in society, to be economically active and to participate as citizens. We must also equip them with an understanding of how to make healthy choices and adopt healthy lifestyles. We do that in the curriculum primarily, though not exclusively, through personal development. That includes making physical education compulsory until age 16 and home economics compulsory until age 14 for all students — that includes boys and boys’ schools.
1295. We recognise that the gap between the highest and lowest attainment of qualifications is even greater among socially disadvantaged pupils. I am sure that the Committee is familiar with that; I will not rehearse that. We know that low attainment can have an effect not only on young people’s employment or further education prospects, but on their future health and that of any family that they might have. We want to demonstrate that we are not just in the business of equipping young people to get qualifications, but equipping them in a much broader educational sense for all the issues that they will face in life.
1296. I want to highlight the extended-schools programme. It has a number of key aims around reducing underachievement and improving the life chances of children and young people from disadvantaged communities in tandem with the concept of fostering health, well-being and social inclusion. The extended-schools programme plays a significant role in promoting healthy lifestyles. Last year, approximately 700 extended-schools programmes were run in 450 schools in Northern Ireland, linked to the healthy lifestyles concept through breakfast clubs, after-school schemes and youth sport and leisure activities.
1297. We also work on pupils’ emotional health and well-being. Nowadays we talk more and more about resilience. Young people who experience poor emotional well-being, for whatever reason, and who have not developed the ability to deal with life’s challenges, cannot possibly fulfil their learning potential. To support that, we have introduced counselling in post-primary schools as a priority. We know that in times of stress, some people react by overeating. For many young people, that can spiral into eating disorders. Emotional well-being is fundamentally connected to physical well-being, and overeating is one issue that we can begin to address through school counselling.
1298. The education workforce is vital to securing and improving the education outcomes that young people need. It is about having the right people on the ground to address the issues that are pertinent to the Committee’s inquiry. The Department’s curriculum advice and support service provides physical literacy co-ordinators to the education and library boards as well as running programmes such as curriculum support in primary schools. All those programmes require professionals to understand and be equipped for delivery in schools. That is connected to what we need our teachers to do and how we need to relate to other school staff.
1299. We recognise that the review of public administration has identified the need for radical reform of education. Rather like the health sector, we have tried to reshape the Department of Education to place greater emphasis on policy formulation, the strategy for the management of education, monitoring of workforces and systems, and performance. We must look at how we are using public money in a way that supports our key stakeholders — children and young people, and their parents.
1300. In our written submission we have given details of a full programme of work by the Department that is specifically about obesity prevention. I would not dream of teaching my granny how to suck eggs but, as we know, it is about the imbalance between energy in and energy out, which results in undesirable weight gain among young people. There are two areas that I want to concentrate on. The first is about “energy in", which is to do with food in schools, and the second is about “energy out", which deals with physical activity.
1301. The Department’s most recent work on food in schools began in 2000. Rather than give members chapter and verse in a laborious way, I will say that the process has evolved through testing the development of a policy and consulting on it, working with nutritionists on healthier menus for school canteens, and working with dietitians. We started off in 2000 and had a public consultation throughout 2001-02. At that point we recognised that we were not turning a small skiff around — it was more like turning a tanker around — and that a more evolutionary and gradual approach to the issue would work best. That has been borne out by the experience across the water, where, post-Jamie Oliver, the snap decision on school menus meant that there was a huge fall-off in the numbers of pupils taking school meals. The revolution meant that young people were not taking as many school meals, and we had the spectacle of the tabloids reporting on mothers feeding their kids burgers through the school gates. That is not what we want to see happening in Northern Ireland. In a way, that is a justification of the more evolutionary approach that we have taken.
1302. Following that consultation, the Department of Education decided to publish nutritional standards in a booklet entitled ‘Catering for Healthier Lifestyles’. The Department also engaged with its partner bodies — the education and library boards and the Health Promotion Agency and Food Standards Agency — on a pilot project that aimed to implement the sorts of standards that had been developed.
1303. In 2004, around 100 schools were identified to pilot the new nutritional standards. That pilot lasted for a year. It was designed to establish pupils’ attitudes to change and how to manage the change across the remaining 1,150 schools. The idea was to test out the new standards. The pilot was fairly successful. The majority of schools and pupils responded very positively, and a number of key conclusions were drawn. The drop-off in the uptake of meals at a time of change was a feature that was noted even then. It was also noted that pupils began to return to the meals service in schools as time passed. The numbers began to rise, though not to the original level. If it was not “chips with everything", then young people were clearly voting with their feet and perhaps identifying other ways. Other features were that pupils did not like oily fish and certain types of vegetable were not popular. However, from the pilot, the Department and its partner bodies were able to develop a strategy that gave pupils time to become accustomed to new menus in an incremental approach.
1304. Interim standards were introduced to remove less healthy food from menus in a series of stages; to adopt preparation and cooking methods, such as puréeing, that disguised certain vegetables — as a parent at one time of three small children, I recognise such ruses; and to roll it out to manageable tranches of schools to try to get buy-in. It was a more gradual and gentle way of enabling young people to develop their tastes and to access the healthier option.
1305. The Department’s preparations for the first tranche of schools coincided with the Jamie Oliver work, at which point the Treasury came in. As a result of the Treasury’s initiative, Northern Ireland got an additional £3 million to support the increase in the quality of school meals. That funding was aimed at getting high-quality ingredients, investing in equipment, training catering staff, and supporting the communication and marketing plan targeted at our young people. Some national minimum targets were also set for the food element. I am happy to come back to that and to take any questions on it.
1306. We ended up with a rolling programme for the implementation of the new nutritional standards. It began in 2005 and ran to 2007, when all schools under the control of boards had implemented the new nutritional standards. Figures show that, in 2005, before the programme was introduced, the uptake of meals was 52%. That fell slightly and, by the end of 2007, it was about 51%. In October 2008, the meals census suggested that it had dropped by a further 0·5%. Therefore, there was an impact, but it was not the massive drop-off that perhaps other jurisdictions experienced.
1307. Since then, the Department has asked the Educational and Training Inspectorate to look at how schools are performing in this area. The Inspectorate has employed two nutritional associate inspectors to carry out that function. The results have largely been very positive in the first tranche of schools to have been inspected.
1308. As the development and roll-out have progressed, it has become clear that competing sources of food in schools were reducing the impact of the new nutritional standards. Therefore, in order to embed the gains made from the implementation of the standards, the Department has developed what it calls a “whole school" approach to nutrition. That involves addressing a number of issues that impact on childhood nutrition and the food choices that children make in schools. Those include the type of foods that are provided in school meals and the other food that is provided in schools through vending machines, tuck shops, break-time snacks and drinks, breakfast clubs and food brought into schools in packed lunches and snacks. I can bear that one out — I know from personal experience that we are not allowed nuts, due to the risk of anaphylactic shock, but we are also not allowed sweet biscuits or drinks. Other issues addressed included access to food en route to school and at lunchtime, and the quality of the dining environment. There are a range of other issues that span around that, but I just wanted to highlight the ones that children and parents experience most.
1309. The vehicle for achieving the objective of a whole school approach is, as I signalled earlier, the proposed policy that the Department now has on food in schools. The public consultation on that policy is planned to start in September. A final postscript to the bid on food in schools is that, in conjunction with developments relating to the food in schools policy, the Department, along with the Public Health Agency, the Health Department and the University of Ulster, is conducting research into a marketing and promotion campaign designed to support the drive against obesity. The aim of that strategy is to raise awareness of nutrition-based health-related issues and help children and parents make the connection between their present diet and the future consequences for their health.
1310. At yesterday’s meeting of the Education Committee, I mentioned that the Department in re-brigading itself — that is, changing how it is internally structured — is, with the advent of the families and communities directorate that I am responsible for, trying to place a much greater emphasis on its relationship with parents. Therefore, the Department recognises the importance of communication and of gaining the hearts and minds not just of children and young people, but also, critically, those who are looking after them at home, and those who are supporting and influencing them in the community background.
1311. At the other end of the spectrum — the “energy out" end of the equation — there are lots of opportunities for young people to be physically active before, during and after school. For example, there is getting to and from school, which provides an opportunity for children to walk or cycle when it is safe to do so. Indeed, the rural safe routes to schools initiative is a very good example of how a number of different Departments and agencies worked with 18 rural primary schools to put in place school travel plans that allow more children to cycle or walk to school.
1312. During the school day there are also opportunities at lunch and break times for children to run about and be active. Lots of primary schools have playground markings that encourage traditional playground games such as hopscotch, and there is an encouragement for children to get active. However, I think that the big, key role for schools is in teaching children the necessary skills to allow them to be physically active, both during the school day and in their chosen after-school or outside activities. Fundamentally, that is done through the delivery of physical education (PE) in the curriculum.
1313. PE is a separate area of learning in the curriculum, which is compulsory across all key stages. At least two hours of PE per week is recommended, but how schools take that recommendation onboard may vary. However, two hours of quality provision is what the Department, advised by experts, has assessed is required. It allows for the developmental brigading of skills and the gaining of knowledge and understanding in the range of activity areas that make up the PE curriculum.
1314. To meet the recommended two hours, there are developing opportunities through the connected learning associated with the revised curriculum. For example, the Council for Curriculum Examination and Assessment has produced ‘Ideas for Connected Learning’ to assist teachers across the different areas of learning. Examples of how activities in PE can actually be used to connect with the rest of the curriculum have been quite important, and those sorts of resources have also been provided to teachers.
1315. The Department has also addressed what we call physical literacy through the fundamental movement skills programme, which provides teachers with continuing professional development on the planning, teaching, learning and assessment of basic physical skills that form the building blocks for children’s active and enjoyable engagement in the activities in the PE curriculum. The PE curriculum also includes opportunities for pupils to develop knowledge, understanding and skills in athletics, dance, games, gymnastics, swimming and outdoors education.
1316. As the Committee knows, the Minister of Education was an active sportswoman earlier in her career, and she has been passionate about sport in schools and about young people being active. Having recognised the importance of developing children’s physical literacy, in the 2007-08 school year she introduced a physical literacy sport programme for the youngest primary-school students. It focused on Foundation Stage and Key Stage 1 — P1, P2 and P3. GAA and Irish Football Association coaches are working alongside teachers in some 550 primary schools to help develop the physical literacy of the young people who are taking part. Approximately 13,000 primary-school students take part in the programme each week. The programme is targeted at areas of greatest disadvantage.
1317. Teachers have also been receiving more support from the boards to help them deliver the physical literacy programme on skills for young people, and extra-curricular physical activities are provided to offer children and young people the opportunity to develop their skills in new contexts. That is sometimes about competing with other schools. However, it is important that the majority of children and young people are given the chance to demonstrate positive attitudes to increased opportunities to take part in sport and physical activities. Some of the latest research is saying that girls, in particular, fade out from taking part in PE and physical activity, and there are issues around that and what it can lead to. It is connected to issues relating to weight gain and self-esteem. That brings us back to the connection between physical well-being and emotional and mental well-being.
1318. I apologise if I have been long-winded, but I hope that I have given you some insight into how seriously the Department of Education is taking its role in obesity prevention. We are striving to do a number of things. The focus on healthy lifestyle choices, including the importance of healthy eating and physical activities, is about equipping young people with the capacity to go forward.
1319. Earlier, I mentioned the relationship between the Department and parents. I do not doubt that the development and management of the food in schools policy in the autumn will be an important learning point for us. Schools are taking a lot of positive steps to ensure that children are presented with healthy eating choices when they are at school, and with increased opportunities for quality physical activity.
1320. As head of youth policy, I am not sure how strongly the food in schools policy is being carried into youth settings. If we are doing so well on the notion of healthy choices in school tuck shops, we will need to think about joining up the dots for young people. It should not just be happening between 9.00 am and 3.00 pm; it should also be happening in any youth settings that they have. I will take that up with colleagues in the Department.
1321. The Deputy Chairperson: Thank you for your interesting and comprehensive presentation. I know that you are in charge of the early-years strategy, which we hope to see coming forward soon. Are there obesity targets in that? Education is key in giving young people the information to help them make informed choices when they get older. Early intervention will set their habits. Is there anything in particular in that?
1322. Ms Warde Hunter: I will have to double-check. I have seen so many iterations of my own strategy that I cannot remember what is in it. Early years and the play-based curricula that operate in preschool and P1 and P2 through the foundation curriculum are strongly based on play, including active outdoor play. If we are to have these healthy eating options through the food in schools policy, that will clearly apply in nursery settings as well. As you will know, voluntary playgroups do not have a long enough day in which to afford children a meal. Perhaps it is less of an issue there, but it will not be a diminution of their commitment to provide the healthy options — fruit and toast — as a mid-morning snack. Thank you for your comment; I will take that back and revisit the strategy from that angle to ensure that, if we do not have a clear expression on that, that we will try to express the physical well-being aspect more clearly.
1323. The Deputy Chairperson: The Department recommends that each child should have two hours of PE each week. That has been raised with the Committee on a few occasions, and Sport NI was also very vocal on the issue. Does physical education form part of the teacher-training programme?
1324. Ms Warde Hunter: I do not know if that is part of the initial teacher training. I imagine that there might be an element of it.
1325. Ms Jill Fitzgerald (Department of Education): I cannot give you the exact detail, but there is coverage for primary-school, non-specialist teachers. Specialist PE teachers will receive PE training, and non-specialists who go into the primary-school arena will have an element of PE training.
1326. The Deputy Chairperson: How is that monitored? Some schools may offer two hours or sometimes more, and other schools may not be meeting that two-hour target. Is that target monitored by the Education and Training Inspectorate?
1327. Ms Warde Hunter: The inspectorate certainly takes account of that target when it is carrying out inspections. That is the point that I was making about the target being set out in the guidelines that the Department has adopted in relation to the curriculum; it gives schools the autonomy as to how to conduct the curriculum. We are not being prescriptive; we are not saying, for example, that all post-primary schools have to teach French on a Tuesday. That is not the philosophy that we have had about the curriculum, and it is not what schools or teachers want. You are quite right. Our position is that these are guidelines, and an inspection could ask how those guidelines are being followed and whether it is appearing in the school development plan.
1328. Dr Deeny: I have raised this a few times: is it not the case that schools should have to do this? Sport NI told the Committee about the two-plus-two strategy in England: that is two hours of PE within the curriculum, and two hours outside it. I see it happening in general practice. You mentioned girls who fade out of doing sports. That starts a vicious cycle, because they start to put on weight, and then they do not want to take part in sport. I think that, rather than recommendations and simple guidance, it should be part of a school’s week. I am aware of schools that allow those pupils who are not very good at sport to fall by the wayside. That is what I have been told. Schools do not insist on every child having two hours of physical activity each week. I think that two hours is not enough. Can you not enforce this for the sake of our kids’ health?
1329. Two girls at my practice have told me that they are smoking because it keeps their weight down. I thought, mother of God, is that what they are doing? They have fallen out of the system. One person has told me that there is no interest in sport, so they go for a walk down the town. What is going on here? All schools like to do well in sports, whether it is between schools or on a larger scale, but a large section of our young population are falling by the wayside and not getting the physical activity that they should do.
1330. There is a duty not only on the Health Department and Health Committee, but on the Department of Education, to ensure that schools see physical education as important for development, and that it should be prioritised. I see that in primary care, with girls in particular. Boys seem to keep exercising, but you are correct that girls, as they get older, seem to drift away from exercise. That is a worrying development.
1331. Ms Warde Hunter: I reiterate that the Department takes an overarching approach to the delivery of the curriculum; as PE is part of the curriculum, the Department has not done anything more than issue guidelines. It is about consistency with the overall approach.
1332. Ms Fitzgerald: The scenario here is different to that in England where two hours of PE a week has been made compulsory. We are in a scenario where no subject is compulsory for any given time. Therefore, although a subject is compulsory in the curriculum — as PE is — the Department is not in a position to say how much time it should be allotted. To do it for PE would make it different from all other subjects and constrain schools in their teaching of the curriculum.
1333. Dr Deeny: There is a difference: unlike other subjects, PE has a very positive effect on people’s health. You could make a difference.
1334. Ms Fitzgerald: Personal development is also a subject that makes a difference to lifestyles, in terms of drugs and alcohol and self-esteem. PE is very important, which is why it is included in the inspections.
1335. Ms Warde Hunter: There are clearly strong feelings on the issue. I would be happy to take the concerns of Dr Deeny and the wider Committee, if it endorses them, back to the Minister so that she can consider them. It is important for us to conduct that message back.
1336. Mr Buchanan: Thank you for the presentation. I apologise for missing part of it, but what I did hear was very good.
1337. A change of mindset in children, going on into their parents and families, is required. There is a mindset where people are not geared up to do physical exercise, which must be completely changed. The provision of sport in schools also has to be looked at. There are folk who excel at sport; it is something that is built into them and they are energised about it. However, there is another section of the school who have no interest in sport. Maybe the provision of sport in schools should be divided into two sections; one for those who are energetic and want to get at it and one for those who slide back a bit. Perhaps there could be a more creative sports programme which would encourage the other section to get involved a bit more in sport and healthy programmes. I am sure that it is not beyond the wisdom of someone to sit down and look at how to get a more creative sports programme to encourage those other folk who do not like sport to take part.
1338. I agree that education has a big part to play in that. In your submission, there are some references to healthy eating programmes in schools. How are the various aspects of the Healthy Schools scheme being co-ordinated? How are the effects of that programme being measured and evaluated in individual schools and in board areas? Is there any evidence that the scheme is benefiting children?
1339. Mr Alan McMullan (Department of Education): I am primarily looking at the measures to change the type of food that is served in schools. Our principal measure of that is the uptake of school meals. We looked closely at the uptake of school meals when the nutritional standards, which aim to get a more healthy background, were introduced. We took a gradual approach to introducing those measures, and uptake decreased only slightly overall. The decrease has been bigger in secondary schools, where we feel that individual eating habits are already well formed and are, therefore, extremely difficult to change at that stage. In primary schools, the figures show a very slight increase.
1340. Through our food in schools policy, we aim to ensure that primary-school children get the healthy food that they need, so that when they go to secondary school they carry on the good eating habits that they have learned. We expect to see uptake increase even further in a few years’ time.
1341. Mr McCallister: My questions will probably overlap some of the other questions that have been asked already. Initially, are you aiming to introduce pupils to, and teach them about, good food, rather than going to the other extremes of banning tuck shops and removing vending machines?
1342. Mr McMullan: We needed to make a fairly big step change, so we went after the main meal of the day, which, in some cases, is the only proper meal that pupils get. Having introduced nutritional standards for all school meals in 2007, we are now extending the food in schools policy to all other food. We have the legislative base to impose nutritional standards on the main meal of the day, but we do not have any legislative power over other food in schools. Therefore, we are trying to improve what is in vending machines and packed lunches by educating pupils and parents.1343. The food in schools policy will bring forward proposals for legislation that will affect other food in schools and give us the power to totally ban things. That said, 70% of the schools that were visited already had a food in schools policy in place; clearly, schools are taking the message on board.
1344. Our nutritional associates are out there inspecting schools; if they see any breaches, they try to cajole the school into changing the food that is sold in vending machines. Instead of taking the big bang approach, we encourage replacing one row of food in vending machines with other healthier alternatives every couple of weeks, so that there is a gradual process and pupils are brought along with that.
1345. Mr McCallister: I accept Kieran’s and Tom’s points about pupils who mitch PE and pupils who do not. It is almost like preaching to the converted with that more elite group. Are there any figures to show whether the percentage of kids participating in PE has improved over the past number of years? Is there any evidence that we have at least begun to turn the corner and increase or stabilise the numbers participating? Are any records kept on that?
1346. Ms Warde Hunter: I do not know the answer to that, but I will go away and find out.
1347. Ms Fitzgerald: I can hazard a guess. All children should be participating in PE, and it is the teacher’s duty to deliver PE to all the children in his or her care. All children have different abilities, and it is the teacher’s duty to assess those in order to help pupils progress. Teachers must bear in mind that girls will disengage from PE earlier and that some children might have disabilities. It is for the teacher to assess that and ensure that a pupil’s participation matches his or her ability, which will encourage interest.
1348. Mr McCallister: Your answer is no different to an answer that would have been given 10 years ago. Would the standard response 10 or 20 years ago have been that all children should have engaged in some form of exercise?
1349. Ms Warde Hunter: Through the curriculum? What you are asking is whether, given the guidelines for two hours’ exercise, there is a baseline through which we can identify that 50% of schools provide one hour a day, 25% offer an hour and a half and 25% offer another amount. I put my hands up; we are not gathering the data in that way — not recently anyway. If the Committee supports such an approach, it may be possible to gather statistical information on the implementation of guidelines and the uptake of such activity. That could supplement the work of the inspectors, who visit individual schools or area bases. It is a guideline approach, notwithstanding what Kieran said earlier.
1350. Mr McCallister: We have nothing against which to measure results. Your answer sounds similar to one that would have been given when I was at school: that children should do a certain amount of PE a week. However, that has obviously not happened, and, 20-odd years later, kids are becoming obese and, hence, the Committee has undertaken this inquiry.
1351. Are the 18 schools that are involved in the safer routes to school programme making any headway? I am aware of the success of that pilot project. Will the Department roll that scheme out to more schools?
1352. Ms Warde Hunter: Sorry; I do not know the answer to that question. As I said to the Chairperson at the beginning of the meeting, I have recently adopted this role. Therefore, sadly, I am not the fount of all knowledge yet. I will take that question back to the Department and provide a written answer.
1353. Ms Fitzgerald: The Department was a partner in that scheme, which was driven by Sustrans and the Department for Regional Development.
1354. The Deputy Chairperson: I met a couple of members of the Scottish Health and Sport Committee when they came here. They undertook an inquiry into the uptake of PE in schools and found that about one third of schools actually provided the required two hours of PE. Do you have any indication of whether we perform better or worse than that?
1355. Ms Warde Hunter: I do not know.
1356. The Deputy Chairperson: That is OK.
1357. Ms Warde Hunter: I am sorry; I am not good with statistics today.
1358. Mr Gallagher: We could not be better than Scotland, because today it is all about extending and expanding the curriculum and ticking boxes. It is not the fault of the witnesses, who provided a good presentation. However, in many cases, we do not know what physical education children do in school. Some kids, because of their health or their genes or whatever, might not be up to two hours’ PE a week. Therefore, I understand why the Department does not have a regulation that requires everybody to do a minimum of two hours’ PE a week. At the same time, part of the path that we have to take to address the obesity problem is to find out exactly how much PE children are doing in school. There seems to be a gap in that area, and the Department seems unable to keep accurate records on how schools teach PE.
1359. The other problem is that schools, because of all the curriculum pressures, are juggling responsibilities. They find it difficult to accommodate PE because it is getting pushed aside. We must bring some sense to how the curriculum is delivered nowadays, rather than telling schools that they must deliver all of it.
1360. In the present circumstances, it is simply not possible for schools to deliver the entire curriculum in a way that benefits children. Therefore, instead of making teachers, kids and everyone dizzy trying to jump through hoops, we need to take a more balanced approach. Certainly, it is important that the curriculum offers choice; however, it must fit into the school’s timetable alongside PE. I am sure that a way can be devised for schools to record the time that is spent on PE or for someone else to record it for the Department.
1361. Entitlement to free milk is a pertinent issue in schools because of milk’s importance in the diet, especially for growing children. Do all schools that have pupils who are entitled to free milk provide that entitlement? Does the Department do any checks on how free milk is administered?
1362. Mr McMullan: Certainly, there is an EU milk scheme. As far as I am aware, it is a voluntary scheme in schools. It is for schools to decide whether to take it up. I am not sure how many schools are involved in the scheme. I am sorry that I cannot answer your question.
1363. Ms Warde Hunter: We can certainly take it back to the Department to try to get a response.
1364. Mr Gallagher: It would be helpful to the inquiry if we had that data.
1365. Ms Warde Hunter: I appreciate members’ concern about balance and the Department’s apparent lack of clarity about the audit trail on the two hours of PE. If I can get a better answer on that issue, I will certainly bring it to you. I do not want to leave the member with the impression that we do not know what is going on in schools, so I want to read you the following paragraph about the minimum content for PE in schools.
1366. Schools are required to deliver athletics, dance, games and gymnastics at Foundation Stage and Key Stage 1. At Key Stages 2 and 3, those areas — apart from dance at Key Stage 3, for whatever reason — and swimming must be delivered. Therefore, teaching children to swim is statutory. At Key Stage 4, pupils may study PE at GCSE level or equivalent. They must have the opportunity to plan and participate in a regular, frequent and balanced programme of PE that, among other things, helps to develop and sustain a healthy and active lifestyle.
1367. The point is that we definitely know the progression of the curriculum, the importance of physical literacy and so forth. We know what activity children and young people should do at different stages. Kieran asked how we know whether that activity is being done for a minimum of two hours. I will try to get clarity on that point and bring it back to members.
1368. The Deputy Chairperson: Thank you very much for coming along and making your presentation.
1369. Ms Warde Hunter: Thank you very much indeed.
18 June 2009
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Mr Alex Easton
Mr Sam Gardiner
Mrs Claire McGill
Witnesses:
Ms Clara Swinson |
Department of Health |
1370. The Chairperson (Mrs I Robinson): We now come to the penultimate oral evidence session of the Committee’s inquiry into obesity. Members will recall that the Committee had planned to travel to London to meet the Department of Health and to examine how the obesity strategy is implemented at a local level by visiting a primary care trust, but, unfortunately, that was not possible. We are particularly grateful to Clara Swinson, deputy director of the cross-Government obesity unit in England, for accepting the invitation to come to the Assembly today to brief us on developments in England, and I welcome her to the Committee.
1371. Members have a briefing paper from the Department of Health, a copy of the executive summary of the ‘Healthy Weight, Healthy Lives’ strategy and a briefing paper from Research Services. Ms Swinson will make a brief presentation, and that will be followed by members’ questions. Before you begin, Ms Swinson, I apologise for the length of time that you had to wait, but the matter that we were discussing has to be dealt with before summer recess.
1372. Ms Clara Swinson (Department of Health): Thank you; it is good to be here. I am the deputy director at the Department of Health with responsibility for the cross-Government obesity unit, which is responsible for obesity policy for central Government in England. I will set out the approach to obesity in England, and then I will, of course, be happy to take your questions.
1373. Just like other nations, we have a growing obesity and overweight challenge. In England, about 60% of adults and 30% of children are overweight or obese. The Foresight expert review, launched in 2007, said that that figure would rise if nothing was done. The experts predicted various stages up until 2050, by which time the majority of adults would be obese and only 10% would be a healthy weight.
1374. Obesity has a significant impact on individual health, the Health Service and the cost to society and the economy. The Government are, therefore, committed to tackling obesity in line with the best available evidence, which comes from the Foresight review. In 2007, we set ourselves a public service agreement, which are the central Government targets in England, with an overall ambition to ensure that everyone is able to reach a healthy weight. Starting with children, the target by 2020 is to have flattened and then reduced levels of childhood obesity to their 2000 levels.
1375. With that ambitious ambition, our strategy is based on the areas that are identified in the Foresight report, which looks at both individual action and the wider environment because of the obesogenic and passive-obesity issues. It also looks at the role of Government, but certainly does not believe that Government can solve the problem alone, and at the role of society. The strategy also recognises that we need to try some things out, see how effective they are and learn as we go on, not to wait until we have a perfect evidence base.
1376. The strategy, a summary of which has been provided for the Committee, first of all sets out for the individual what we are doing to help people to make healthier choices. A large part of that is the Change4Life movement and social marketing campaign, which was launched earlier this year. That will be extended to younger people with the launch of Start4Life in the autumn for children from 0 to 12 months old. That will be extended to adults next year.
1377. We are looking to increase the information that is available to consumers through, for instance, nutritional labelling on products in supermarkets and stores, and labelling in non-retail settings such as fast-food restaurants. We also have a national child-measurement programme which weighs and measures all children in reception year and at age 11. That information can now be routinely fed back to parents.
1378. That is what we are doing to help the individual to make a healthier choice. The second strand is very much about ensuring that the environment supports those choices and makes the healthier choice the easier choice. A lot of work has been done on children in early years and in the school environment; there are strict standards on food that is available in schools, increased focus on physical education (PE) and sport, and, from the early years, encouragement for breastfeeding and healthy habits.
1379. On the “energy in" side of the equation, our healthy food code puts in one place the various things that we want industry to do, and consumers, too. Those range from labelling to portion size and product reformulation. I will not go through them all, but there are a whole set of issues around “energy in". On the “energy out" side — we give each side equal weight — our aim is to help people to build physical activity back into their daily lives, focusing on programmes for individual walking and cycling. The programme also involves working with town planners on future development, and we have a Healthy Towns programme which is in its second year.
1380. For adults, we are thinking about the role of the employer in encouraging healthy choices and about what employers in both the private and public sectors can do in respect of that. That is a brief overview of what we are doing about the environment.
1381. Obviously, we need to provide services to those who are at risk and to those who are overweight and obese already. In England, we have the National Institute for Health and Clinical Excellence guidelines and primary care trusts (PCTs). We allocate money — £69 million this year — to PCTs for them to translate as they see fit into the weight-management services that they need to provide for their local communities. We do some work centrally to help them to make the case and to commission high-quality services.
1382. Finally, we look at the whole delivery system. There is a role for central Government. I spend a lot of time cross-Government working with my colleagues in other Government Departments. We report to a ministerial committee that has 10 or 12 Departments represented on it. There is a lot of work for local government in schools and the wider public sector. There is a large task of building a coalition of the willing with commercial and voluntary sectors so that everyone plays their part in creating a society where we can all reach a healthy weight.
1383. We are doing a lot to increase our knowledge. As I said at the start, we do not have a perfect evidence base, and, therefore, we still work with the advisers who were involved with the Foresight report. We have a national obesity observatory. We evaluate what we do. We are committed to producing an annual report that sets out what we have done each year and that also looks at what we have learnt in that year so that we can amend policy as required.
1384. I hope that that gives a helpful overview. We are by no means there yet. It has been years in the making and it will take years to tackle the problem fully. However, I believe that we have a comprehensive strategy, with some exciting bits of work under way. The Government are certainly taking a leading role, but we know that Government alone cannot change the situation.
1385. The Chairperson: Thank you very much, Clara, for that very interesting presentation. Given their usage of computers and so on today, children become couch potatoes and do not get a lot of exercise. Do you work closely with local authorities to deliver free entry to their recreational facilities for children to use the football pitches and other equipment in those areas?
1386. Ms Swinson: Yes; you are quite right that changes over time have made us more sedentary. We have two messages for children: 60 active minutes and activity in school. For local authorities it is very much about making sure that their open spaces and what can be done for free are attractive and that people know about them. As regards other recreational spaces, one particular initiative is the free swimming that is available in many areas of England now for the under-16 and over-60 age groups. As you said, we need to build regular activities into children’s lives from an early age.
1387. Mrs O’Neill: We also recognise that the problem is not going to be fixed overnight and that it is a societal thing. Any changes will be seen over the longer term.
1388. We had the Department of Education along last week and we were talking about PE in schools and about how some schools deliver two hours of physical education each week but others do not. The direction from the Department is that schools should provide two hours. We discussed whether that should be made a mandatory minimum requirement for schools. Are there any targets or mandatory obligations on schools to provide more PE? Obviously, if children and young people are provided with encouragement to take part in physical activity at an early age, they are more likely to carry that on into adult life.
1389. I would also like more information on the healthy community challenge fund referred to in the paper to the Committee.
1390. Ms Swinson: Yes, schools should provide two hours a week of PE, and about 90% of children now receive that. Many schools offer an additional three hours of activity that need not be standard PE or sport but that could be offered to children through after-school clubs, at lunchtime, or throughout the day rather than just in PE lessons. That is what is happening in schools.
1391. The healthy community challenge fund, which we abbreviate to Healthy Towns, is a fund of £30 million over three years. We looked at some successes achieved in towns in France through the Epode project and developed the idea for England. Evidence shows that, although no society as a whole has tackled obesity, there has been some success on a community level when people really got together and worked across agencies.
1392. Therefore, we set out what we wanted to achieve but did not specify to areas what they had to do. Instead, we asked for proposals. Some of the proposals focused on food and others on activity. They all had to involve both local authorities and primary care trusts, but the proposals varied depending on whether they focused on infrastructure or prevention.
1393. We were seeking seven or eight applications but received more than 160. We went through a process that led to the selection of nine towns — one in each region of England. The programme was also match-funded; the aim was not to tell people what to do, but to let them know that money put forward for their proposal would be matched by central Government. We have now signed off on all the Healthy Towns project plans and they have been granted their second year of funding.
1394. At a national level, we are also conducting an evaluation of the nine Healthy Towns. By the very nature of what we asked for, their projects were very varied. Therefore, in another year or two we will have the results of their first year or 18 months in operation.
1395. Mr Gardiner: I am chairman of the boards of governors of two primary schools that have breakfast clubs to encourage healthy eating. Rather than bring in sweet stuff to eat, the children are dropped off at 8.00 am and they have breakfast at school. We are not doing away with flowers or things like that, but our children plant apple trees, carrots, parsnips, beetroot and the like, and the children are taking an amazing interest in a healthier lifestyle. The schools also provide water coolers and containers with which the children can get water at any time during school hours. Therefore, we are on that track and trying to overcome this problem that we are facing by cutting down on sweet stuff.
1396. Ms Swinson: Many groups in our society need to reconnect with basic knowledge about food such as vegetables and basic cooking skills that have been lost over the past few decades. That should be encouraged when people are young.
1397. Mr Gardiner: Are we on the right track, then?
1398. Ms Swinson: Yes.
1399. The Chairperson: In the absence of any other questions, I thank Ms Swinson for coming all the way from London and wish her a safe journey back to the mainland.
18 June 2009
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Sam Gardiner
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
Dr Naresh Chada |
Department of Health, Social Services and Public Safety |
1400. The Chairperson (Mrs I Robinson): This final evidence session of the inquiry is with officials from the Department of Health, Social Services and Public Safety. Members have been supplied with the Department’s submission to the inquiry and a briefing paper from the Assembly Research Services.
1401. I welcome Mr Rob Phipps, Ms Christine Jendoubi and Dr Naresh Chada. I invite you to make a brief presentation, after which members may ask questions. We will allow up to one hour for the evidence session.
1402. Mr Rob Phipps (Department of Health, Social Services and Public Safety): We are pleased to be back at the inquiry’s conclusion. We have been following its progress with interest, and, through reading the Hansard reports, we have noted some of the comments and points raised.
1403. When we first gave evidence to the Committee on 5 March 2009, Andrew Elliott outlined the Department’s position on the issue and stressed its commitment to addressing obesity across the life course. I wish to update the Committee on the work that has been, and is being, carried out on the issue of prevention. I will hand out copies of a newsletter to members; in fact, you are the first people to see it. It will be distributed to everyone who deals with the issue of obesity at local and regional levels and elsewhere.
1404. At the last evidence session, we spoke about our intention to develop a 10-year strategic framework to address obesity across the life course. In our original submission, we annexed a logic model. The 10-year framework will be outcome-focused and outcome-based. It will take a thematic approach to the life course. For example, not only will it target young people, children, adults and older people but it will subdivide maternal matters into antenatal and post-natal issues. We can then consider other outcomes such as obesity in the workplace. The framework lends itself to a matrix-type approach, because it not only considers obesity in younger people or older people but it is also settings-based.
1405. The short-term outcomes, which will probably take two to three years to achieve, have the potential to address many of the issues that have already been brought to the Committee’s attention, such as nutritional standards, levels of participation in physical activity by young people and older people, and the role and support of the food industry. All those issues can be covered within that outcome-focused approach.
1406. Our steering group is cross-departmental, and the final framework must be cross-sectoral and cross-departmental. At present, four advisory groups are working on that to develop the outcomes, which they will complete by the end of September 2009. An email address has been provided in the newsletter for people to send in their thoughts and to make comments. Between October 2009 and January 2010, we will develop the framework. That will involve discussion and negotiation with other sectors and, in particular, the Departments. It is important that there is buy-in across the entire sector.
1407. The big question is: how do we measure the success of those outcomes? How do we measure the difference that they are making and the impact that they are having? A data research group is currently working on that. It is examining the evaluation of good practice, as well as the types of surveillance systems that are in place.
1408. Assessing progress and impact, and measuring the difference that is being made, is a big challenge. That will be built into the process, and we will have indicators that will demonstrate the difference that is being made. That is absolutely essential. A group is working on that, and we hope to finish that process by January 2010. People will feed their ideas and thoughts into the initial consultation, and it will then go out for full public consultation in February, March or April 2010. We will take on board the comments that we know we will receive, and we will then redraft the strategic framework. It sounds rather frightening, but we hope to launch the strategy by June 2010. That may seem a long way off, but there is much work involved to get it right.
1409. That is where we are. I hope that the newsletter gives you more background to the process.
1410. The Chairperson: It is very helpful. Thank you very much.
1411. Mrs O’Neill: Early intervention is crucial, and the new Public Health Agency has a key role to play in tackling the epidemic. Do you see the agency having a role?
1412. Mr Phipps: The Public Health Agency is part of the process. The agency is represented on all the groups that I mentioned, including the steering group. It is already inputting to the development process, but it has an essential role in delivery and implementation. I am sure that members will appreciate that the agency is in the process of getting its structures in place, but we are keen to work closely with it, because it will be a key partner in the delivery of the framework.
1413. Mrs O’Neill: In relation to primary care, an incentive was introduced for GPs to identify patients over 16 years of age old who have a body mass index over a certain level. Does that not place more focus on treating obesity as opposed to adopting a more preventative approach? Is there an incentive to work with GPs so that they can help their patients to be more active or to refer them to use council leisure facilities, for example?
1414. Ms Christine Jendoubi (Department of Health, Social Services and Public Safety): It is opportunistic. We do not have anything in place for GPs to go out and hunt down fat patients. However, when such patients present, GPs are paid to offer them a resource pack that provides them with dietary advice as well as advice on smoking. However, one must remember that patients are free to turn down offers of treatment. GPs will refer patients to smoking cessation clinics, give them advice, carry out routine blood pressure monitoring and thyroid function tests. They will keep a register of obese patients and follow them up annually to measure their weight, test blood lipids and glucose. GPs will refer them to physical activity resources or programmes, but they are not universal.
1415. I have read about practices in England that will prescribe patients a physical activity course in their local leisure centre. A GP can prescribe anything that a pharmacist can dispense, but, obviously, a pharmacist cannot dispense swimming lessons. However, it is entirely possible that arrangements can be made with leisure centres so that the cost of physical activity courses can be redeemed from the former Central Services Agency, or the Business Services Organisation, as it is now known. I do not know it for a fact, but I imagine that that is the general idea behind the Grove Wellbeing Centre, where the swimming pool is on site. That type of cross-governmental approach should be encouraged. That is the purpose of those types of dual amenities.
1416. Mrs O’Neill: Community planning will be vital, and that will provide the opportunity for the different agencies to get together to look after the population that they serve.
1417. Mr Phipps: In the early 1990s, the former Northern Board had a voucher scheme; GPs gave out vouchers to people whom they felt would benefit from them. Community planning will kick in in a couple of years’ time, and it will give a role to the agencies and the local councils. Local councils will be important, and leisure centres, in particular, will have a crucial role to play.
1418. The Scottish weight-management programme Counterweight involves a patient’s GP and family. We are aware of those schemes; a representative from Counterweight made a presentation to the obesity prevention steering group. That programme is popular in Scotland. Further discussion is required for many of those issues, and there is potential to make suggestions.
1419. The Chairperson: Some councils do that already. Castlereagh Borough Council has a set-up in which people can use the leisure facilities to improve the quality of their health. As you say, local authorities will play an important role in the future with the redrawing of local government boundaries.
1420. Mr Easton: You are doing good work. I am not knocking you, but much of what you are doing, or what we are considering, is directed at people who already have a problem. Apart from the work that is being done in schools and exercise being recommended, what are you doing to try to ensure a healthier population? That is vital.
1421. I keep harping on about the muck that food companies put into food. If that does not change, there will always be a problem, regardless of what we do; it will be akin to treating the problem with a sticking plaster. Are all our food laws governed by Europe? Is that our major problem? Are you examining legislation that we could use to try to force food companies to moderate the doses of various ingredients that they use?
1422. There are four advisory groups examining four issues. Why do you need four groups? Is it merely to speed up the process?
1423. Dr Naresh Chada (Department of Health, Social Services and Public Safety): I agree that it is vital that we target people in the early years, and all the public health evidence bears that out. The structure of what we have been trying to do in Northern Ireland through Fit Futures and the further work that Rob Phipps outlined tend to corroborate that line of thinking.
1424. None of us is an expert on food legislation, so I am happy to get back to you on some of the details. I understand that the Food Standards Agency gave evidence to the Committee and informed you that most of the legislative issues relating to food and, particularly its content, are set by Europe and, to some extent, national legislation. Therefore, we are constrained about what we can do in Northern Ireland.
1425. Mr Phipps: There will always be an issue about food and nutrition. Dieticians and nutritionists always have issues about food and nutrition. Similarly, representatives from Sport NI and other colleagues will say that physical activity is also important. We acknowledge that, and we thought that the best way to ensure that we included that in the framework was to have experts from those two groups to raise those points. Mr Easton’s points may be discussed at the food and nutrition group, for instance.
1426. There is also an issue about consistent messages. Inconsistent or different messages going out at the same time, or at different times, annoy everyone. The education, prevention and public information advisory group is tasked with trying to achieve consistency. A point was made about the role of the Public Health Agency, public health campaigns and public campaigns. It is imperative to achieve consistency, and that advisory group has been tasked with that.
1427. The fourth group is concerned with data and research, which involves a roomful of researchers and statisticians who grapple with the big issue. The newsletter may state that. We also bring the chairpersons together. They are not independent to the extent to which they plough their own furrow, so we bring them together and have regular meetings, which is when the crossover occurs. That works well.
1428. Mr Gardiner: I ask for clarification because my mind is probably not functioning properly. The newsletter states that, in Northern Ireland, some 59% of adults have a weight problem, and 5% of children in primary 1 are obese, with 22% of children in primary 1 being overweight or obese. Does that mean that 17% of children are overweight?
1429. Mr Phipps: Yes, it does
1430. Mr Gardiner: That is not very clear.
1431. Mr Phipps: Thank you very much. The newsletter has not yet been circulated, so we can make that clearer.
1432. Mr Gardiner: Please do that because you are contradicting yourselves somewhat.
1433. Mr Buchanan: I welcome you to today’s meeting. I commend you for the ongoing work. This is a big issue that has come to the fore in Northern Ireland in recent years. Early-years intervention is vital. It is important to educate in the early years because prevention is always the best medicine. I assume that some of those groups work with schools, the education system and local authorities to establish incentives so that people are encouraged to try to tackle this serious problem. What plans are in place to treat overweight children and adults in the secondary sector?
1434. Ms Jendoubi: If they are older than 16 years of age, they will fall within the ambit of directed enhanced services (DES). There is always an opportunity for the surgical route, but we do not recommend that because people do not routinely go down that route. Many teenagers, particularly girls, want that route, which they see as being the easy way out. However, it is not a route that we routinely recommend because it is drastic.
1435. There are also normal dietetic services from the trusts. Youngsters will be referred when they present. If they go to their doctor with a problem, or if they turn up with any kind of health problem and their doctor feels that they have a weight issue, they will be offered a resource kit if they are old enough to avail themselves of it. They will be offered routine tests, and they will be followed up for weight measurement and routine monitoring as quickly as the doctor feels that they need to be. They will then be referred to a trust dietician for further advice.
1436. Mrs O’Neill: Are allied health professionals represented on the obesity prevention steering group?
1437. Mr Phipps: I would need to double-check that.
1438. Mrs O’Neill: A witness in Committee told us that allied health professionals were not involved, and they felt that they were not represented. They would have much to offer.
1439. Mr Phipps: Bear with me; I have the membership of the steering group, but I will have to go through my 3,000 documents. People say that various groups should be represented, and we say that that is great. We are inviting people. Just now, I cannot see a representative. However, I will take that point and ensure that there is an allied health professional by the next meeting.
1440. Dr Deeny: I am sorry that I was delayed.
1441. On the subject of exercise, I have worked in general practice for years now, and it is important to promote exercise. It is not only good for physical health and the prevention and tackling of obesity but for mental health. Some years ago, a couple from England who came into my area suffered a terrible tragedy and lost a family member through suicide. That couple has come on in leaps and bounds because they exercise frequently at the leisure centre. Their intake of drugs has gone down dramatically. I see that every day.
1442. In 2010, the cost of prescriptions will be reduced to zero. However, should it not be the case that, across Northern Ireland, GPs should pick appropriate motivated patients for exercise programmes? Motivation must be assessed for all types of conditions.
1443. Last week, representatives of the Department of Education were witnesses at the Committee. They told us that they would consider the Department’s guidance of two hours’ physical exercise for schools. I do not think that that is enough. Physical exercise should be compulsory, and it should be almost four hours a week. I suspect that some schools do not do physical exercise at all, and the focus is far too much on academic activity as opposed to exercise. For want of a better phrase, we are getting some obese Einsteins — children who are bright but not physically fit. Will the Department of Health, Social Services and Public Safety work with the Department of Education on that matter?
1444. With the advent of the new local commissioning groups (LCGs) — I must declare an interest because I am a member of the Western Local Commissioning Group — will GPs and elected councillors work together on commissioning groups and perhaps come up with exercise programmes to improve public health?
1445. Mr Phipps: The process that I described means that people can suggest such outcomes for the role of GPs and that of physical education in schools. Our physical activity group met yesterday, and the Department of Education was represented on it. They spoke about giving evidence to the Committee last week, so the number of hours of physical activity was a discussion point. We are keen to work on that area.
1446. I take the point about linkage with good mental health. One of my personal frustrations is that much of our work is about promoting self-esteem and good body image, which is excellent for mental health. It cuts across a range of lifestyle behaviours — alcohol, drugs and other issues. We are aware of those points. There is a potential for those to be built into the strategic framework, but we will then have to get the buy-in. There is certainly potential, and we are working closely with the Department of Education and the Department of Culture, Arts and Leisure on Fit Futures.
1447. Dr Chada: The point about local commissioning groups is extremely important. When the public health infrastructure matures at a local level, it will be important for local commissioning groups to work with partners such as local government and public health professionals. That will ensure a common approach so that people have access to exercise and leisure opportunities, thereby tackling the obesity issue. We need to examine that work carefully at a local level. Commissioners need to take that on board.
1448. Mr Phipps: It is a challenge; it is part of the regional vision, but it will be delivered locally. The framework will, I hope, enable that so that there is regional consistency. However, local bodies know their localities better than we do. The entire process is about that, and it can put in place those types of initiative. There must be consistency in what we are saying. One can go to area A and receive a certain message, and then go to area B and receive an entirely different message. People might say that we should get our act together. However, it is about how the issue of messages and information is managed. It is not unique to health issues. There is a range of issues, and it is about trying to manage a regional vision against local delivery.
1449. Dr Chada: What might be appropriate in an inner city might be completely different in a rural setting. We must consider all the initiatives to see how they can best be evaluated and in which setting they will be the most effective.
1450. Ms Jendoubi: We would expect local commissioning groups to turn their attention to that issue, and the fact that councillors and doctors are on local commissioning groups should make life much easier.
1451. When Barry Gardiner was Minister with responsibility for education, he had plans to increase the length of the school day and have two hours’ physical activity in the middle of each day. However, that did not go down terribly well with the teachers’ unions, and the plan was not pursued.
1452. The Chairperson: That concludes the oral evidence for the inquiry.
Appendix 3
Written Submissions
Obesity Inquiry Submissions
Organisation Page
Ofcom
OFMDFM Committee
Department of Employment & Learning
Conservation Volunteers Northern Ireland
Royal College of Psychiatrists
University of Ulster
Obesity Management Association
LighterLife (UK)
Northern Ireland Commissioner for Children and Young People (NICCY)
Centre for Obesity Research and Epidemiology
Banbridge District Council
Western Health & Social Services Board
North Eastern Education and Library Board
Dr Michael Ryan – The Northern Health and Social Care Trust
Fermanagh District Council
Health & Social Services Councils
Omagh District Concil
Department of Health, Social Services & Public Safety
Ards Borough Council
Action Cancer
Belfast City Council
Abbott
Southern Health and Social Service Board and Southern Investing for Health Partnership
South Eastern Health and Social Care Trust
Department of Culture, Arts and Leisure
Armagh City and District Council
Chartered Society of Physiotherapy Northern Ireland
Newry and Mourne District Council
Northern Ireland Environment Link
The British Dietetic Association
Belfast Health & Social Care Trust
Institute for Public Health in Ireland
Department for Regional Development
Public Health Alliance
British Heart Foundation Northern Ireland
Sustrans
College of Occupational Therapists
Ballymena Borough Council
Ajinomoto
Cambridge Health & Weight Plan
Western Education & Library Board
Department of Agriculture and Rural Development
PlayBoard
Northern Health & Social Services Board
Sport NI
Northern Ireland Cycling Forum
British Medical Association
Department of Finance and Personnel
Health Promotion Agency for Northern Ireland
Department of Social Development
Royal College of Nursing
Safefoods
Royal College of General Practioners
Department of Education
Southern Health and Social Care Trust
Western Health and Social Care Trust
NILGA
Queen’s University Belfast
Ulster Cancer Foundation
Food Standards Agency Northern Ireland
Diabetes UK
Dairy Council for Northern Ireland
NI Assembly Facilities Branch
Helping Hands Ltd
Dr Una Lynch
Public Health Authority
OFCOM
Introduction
1. This submission is in response to the Northern Ireland Assembly’s request for written evidence for its Inquiry into Obesity. It outlines the actions we have taken to limit children’s exposure to television advertising to food high in fat or salt or sugar (HFSS), on the basis of our findings that advertising (amongst other factors) had a modest, direct effect on children’s food choices and a larger but unquantifiable indirect effect on children’s food preferences, consumption and behaviour.
Background
2. Ofcom was established under the 2003 Communications Act. One of our duties is to secure a wide range of high quality television services. Related to this, we must report on the extent to which the public service broadcasters (PSBs) have fulfilled the purposes of public service television broadcasting, and to make recommendations with a view to maintaining and strengthening the quality of PSB in the future. Advertising is clearly an important part of the funding system both for commercial broadcasters who have public service obligations and others that also offer alternative choices of channel viewing to the BBC, which is, of course, funded by the licence fee.
3. Ofcom also has statutory responsibility for regulating television advertising in the UK. Ofcom delegated responsibility for regulating the content of television advertising to the Broadcast Committee on Advertising Practice - BCAP (an arms-length offshoot of the Advertising Standards Authority) in 2004. However, Ofcom retains responsibility for approving changes to the rules. The rules for non broadcast alcohol advertising are the sole responsibility of the ASA (see http://www.asa.org.uk/asa/codes/cap_code/ShowCode.htm?clause_id=2152).
4. Clearly, any changes to the arrangements for advertising need to be carefully thought through in terms of their direct impact on the public’s viewing experience, and their indirect impact on the choice and quality of viewing available to the public as a result of the implications for advertising revenue. In all its policy work, Ofcom carries out detailed research and undertakes impact assessments to ensure that any regulation is evidenced based and proportionate.
Research into Obesity and TV advertising
5. A growing body of research has generated concerns in government and society about rising childhood obesity levels and ill-health due to dietary imbalance, specifically the over-consumption of high fat, salt and sugar (HFSS) foods and the under-consumption of fresh foods, fruit and vegetables. Both the Department of Health (DH) and the Food Standards Agency (FSA) have identified television advertising as an area where action should be considered to restrict the promotion of HFSS foods to children.
6. In December 2003, the Secretary of State for Culture, Media and Sport, asked Ofcom to consider proposals for strengthening the rules on television advertising of food aimed at children.
7. In response, in early 2004, Ofcom conducted research into the role that television advertising plays in influencing children’s consumption of foods that are HFSS. In publishing its research report in July 2004, Ofcom concluded that advertising had a modest, direct effect on children’s food choices and a larger but unquantifiable indirect effect on children’s food preferences, consumption and behaviour. Ofcom therefore concluded that there was a case for proportionate and targeted action in terms of rules for broadcast advertising to address the issue of childhood health and obesity. However, Ofcom also noted that one of the conclusions from the independent research was that multiple factors account for childhood obesity. Television viewing/advertising is one among many influences on children’s food choices. These other factors include social, environmental and cultural factors, all of which interact in complex ways not yet well understood. In these circumstances Ofcom considered that a total ban on food advertising would be neither proportionate nor, in isolation, effective.
8. In November 2004, DH published a White Paper reiterating the Government’s view that there was ‘a strong case for action to restrict further the advertising and promotion to children of those foods and drinks that are high in fat, salt and sugar’ in both the broadcasting and non-broadcasting arenas. At the same time the FSA published a consultation on a scheme which would identify HFSS food and drink products by means of nutrient profiling. This model was intended to help Ofcom reach decisions on the restriction of television advertising for less healthy foods. In December 2005, the FSA completed their work on a nutrient profiling scheme and delivered it to Ofcom.
Consultation Process
9. In March 2006 Ofcom proceeded to consult on a range of different options for new restrictions on television advertising to children. Ofcom published a Statement and further Consultation in November 2006 which said that it had concluded that, in the context of its statutory duties, the aims of further regulation in relation to television advertising should be to balance the regulatory objectives set out below. In the light of the consultation responses and after considering all the available evidence, Ofcom extended the scope of the first regulatory objective to include all children under the age of 16, instead of children under the age of 10. We decided that the revised regulatory objectives were to:
- reduce significantly the exposure of children under 16 to HFSS advertising, as a means of reducing opportunities to persuade children to demand and consume HFSS products;
- enhance protection for both older and younger children as well as parents by appropriate revisions to advertising content standards, so as to reduce children’s emotional engagement with HFSS advertisements, and reduce the risk that children and parents may misinterpret product claims, and to reduce the potential for “pester power";
- avoid disproportionate impacts on the revenue of broadcasters;
- avoid intrusive regulation of advertising during adult airtime, given that adults are able to make informed decisions about advertising messages; and
- ensure that any measures that are put in place are appropriate and sufficiently timely to enable Government to observe changes to the nature and balance of food promotion by early 2007.
10. The November Statement identified Package 1 as its preferred option, but sought views on whether a modified version of this package (Modified Package 1) would better fulfil Ofcom’s regulatory objectives. Modified Package 1 was set out in detail in the November Statement.
Conclusions
11. After a detailed examination of all consultation responses and the available evidence, Ofcom decided that Modified Package 1 should be adopted. Accordingly, it was agreed that the following package of measures to restrict the scheduling of television advertising of food and drink products to children would be applied:
- scheduling restrictions would be confined to food and drink products that are assessed as HFSS as defined by the FSA’s nutrient profiling scheme;
- advertisements for HFSS products must not be shown in or around programmes specifically made for children (which includes pre-school children). This measure would remove all HFSS advertising from dedicated children’s channels;
- advertisements for HFSS products must not be shown in or around programmes of particular appeal to children under 16; and
- these restrictions would apply equally to programme sponsorship by HFSS food and drink products.
12. Ofcom also decided that, alongside these scheduling restrictions, revised content rules would apply to all food and drink advertising to children irrespective of when it is scheduled. The full content rules are set out in the annex. Key elements of the content rules include a prohibition on the use of licensed characters, celebrities, promotional offers and health claims in advertisements for HFSS products targeted at pre-school or primary school children.
Implementation
13. The revised BCAP content rules came into force for new campaigns with effect from the date of the Statement (February 2007). Any campaigns that were already on air or in planning had to comply with the new rules from 1 July 2007.
14. The scheduling restrictions came into force in two stages as follows for all channels except children’s channels:
- with effect from 1 April 2007, HFSS advertisements were not be permitted in or around programmes made for children (including pre-school children), or in or around programmes that are likely to be of particular appeal to children aged 4-9; and
- with effect from 1 January 2008, HFSS advertisements were not be permitted in or around programmes that were likely to be of particular appeal to children aged 4-15.
15. Children’s channels were allowed a graduated phase-in period, with full implementation required from 1 January 2009.
16. In accordance with the co-regulation arrangements put in place by Ofcom and its co-regulatory partners, responsibility for interpreting the rules rests with the Broadcast Committee on Advertising Practice (BCAP), while the ASA is responsible for securing compliance. All the new rules, both for scheduling and for content, will form part of and be included in the BCAP Television Advertising Standards Code.
17. The scheduling restrictions and revised content rules apply to all channels transmitted by UK broadcasters whether aimed at UK audiences or outside the UK.
18. In announcing the restrictions, Ofcom said that it would carry out a review in late 2008 to assess whether or not the restrictions were having the expected effects, in terms of:
a) the reduction in HFSS advertising seen by children;
b) use of advertising techniques considered to appeal to children in HFSS advertising; and
c) the impact on broadcasting revenues.
19. At the request of the Government, we brought forward the start of the review to July 2008.
Further Reviews
20. In conducting the 2008 review, Ofcom worked work closely with the Department of Health and the Food Standards Agency, both of which have also been conducting related reviews in this area.
21. In October 2008 the Department of Health published its report Changes in Food and Drink Advertising and Promotion To Children, which looked at the balance and nature of advertising for HFSS products across a range of media, including television, radio, press, outdoor and cinema advertising. The report found food and drink advertising attractive to children has fallen considerably on TV while increasing significantly in other areas.
22. The FSA has commissioned an independent panel to review the nutrient profiling model in the light of experience. The panel’s draft conclusions were to be reviewed by the Scientific Advisory Committee on Nutrition towards the end of 2008, with a view to recommendations being made to the FSA Board in early 2009. If the FSA decides that changes should be made to the nutrient profiling model, Ofcom would need to consider whether corresponding changes should be made to the model used to identify products that are subject to advertising restrictions.
2008 Ofcom Review Findings
23. Ofcom concluded a review in December 2008 assessing how the restrictions are working. It is important to note that Ofcom did not look to see whether the rules are having effects on child obesity – it would not be realistic to expect short term changes in obesity, and in any case, television advertising is only one of a large number of factors that affect obesity. Rather, Ofcom looked at whether the restrictions are working as intended. The findings revealed that :
- scheduling restrictions have reduced the number of HFSS product advertising impacts (i.e. each occasion when a viewer sees an advert) among children aged 4-15 years by 34% between 2005 and 2007-8
- younger children (4-9 year olds) saw 39% less HFSS advertising; older children (10–15 year olds) saw 28% less HFSS advertising between 2005 and 2007/8;
- overall, children saw 41% less advertising on the main commercial channels (ITV, Channel 4, Five, and in Wales S4C1) and 27% less advertising on digital commercial channels;
- children saw 63% less HFSS advertising during children’s airtime (including both children’s channels and children’s slots on other channels);
- children saw 35% less HFSS advertising in adult airtime on the main commercial channels, but 7% more on digital commercial channels. The biggest increases occurred on the main commercial channels’ spin-off services[1], whose share of HFSS child impacts grew from 4% to 16%; and
- overall children saw 29% less HFSS advertising between 18:00 and 21:00.
24. Separate analysis carried out by Ofcom suggests that only about 40% of all food and drink advertising seen by children was for HFSS products likely to appeal to them. The remainder was either for non-HFSS products, or HFSS products such as spreads, cooking oil and drinks mixers.
25. Ofcom estimated that the advertising restrictions, once fully implemented, would reduce child HFSS impacts (the number of times an HFSS advert is seen by a child aged 4-15) by some 41% of the 2005 level (the last year for which we had comprehensive revenue and viewing data at the time).
Changes in the use of advertising techniques seen by children
26. Surveys carried out by Ofcom’s co-regulator the Advertising Standards Authority (ASA) show that broadcasters are complying with the HFSS content rules.
27. Children saw fewer food and drink advertisements using techniques considered to be of appeal specifically to children in 2007/8 than in 2005[2]. In particular:
- children saw less advertising featuring licensed characters (-69%), brand equity characters (- 36%), other characters (- 4%), promotions (- 36%) and health claims (- 18%). Children saw more advertising featuring celebrities (22%), but the growth all took place in adult airtime, and included advertisements featuring celebrities mainly of appeal to adults (e.g. Ian Botham and William Shatner);
- in children’s airtime, advertising impacts for children arising from all of these techniques declined and, with the exception of ‘other characters’ and ‘celebrities’, also declined in adult airtime; and
- further changes are likely when HFSS advertising is removed from children’s channels.
- Overall, our analysis suggests that children are exposed to significantly less advertising using techniques considered to be of appeal to children.
- In relation to brand advertising and sponsorship, there is no evidence which supports the view that advertisers are using these techniques to circumvent the restrictions on HFSS advertising, although the paucity of data makes definitive conclusions impossible.
Impact on broadcasters
28. In restricting the advertising that broadcasters could carry, Ofcom sought to avoid a disproportionate impact on the revenues of broadcasters, and to avoid intrusive regulation of advertising during adult airtime, on the grounds that adults are able to make informed decisions about advertising messages. Ofcom estimated that the restrictions would affect the advertising revenue earned by broadcasters, although some would be able to mitigate that loss to a greater or lesser extent.
29. The review found that restrictions on food and drink advertising have not been the most significant factor affecting broadcasters in the period under review. In particular, on the basis of data supplied by broadcasters:
- children’s channels saw a significant decline in food and drink advertising revenue. However data provided by broadcasters indicates that total advertising revenue on children’s channels has nevertheless increased overall;
- main commercial channels (ITV1, GMTV, Channel 4 and Five) have seen a 6% decline in food and drink advertising revenue. They have also experienced a reduction in overall advertising revenues;
- most other digital commercial channels have been able to increase their revenue from food and drink advertising, so mitigating the effects of restrictions to a greater degree than we expected.
Future review
30. The final phase of restrictions will be implemented on 1 January 2009, when children’s channels will be required to remove all HFSS advertising from their schedules.
31. Under transitional arrangements, children’s channels have been allowed to include a progressively declining amount of HFSS advertising in their schedules between April 2007 and December 2008. Unlike other channels, they have no scope to move HFSS advertising out of children’s airtime to other parts of the schedule. The purpose of the transitional arrangements was to allow them time to seek alternative sources of revenue to mitigate the loss of revenue from HFSS advertising.
32. In 2007/8, children’s channels accounted for 17% of HFSS advertising seen by children. If none of this advertising was displaced to other channels, we could expect a further overall 11 percentage point reduction in impacts since 2005 on top of the 34% reduction that we estimate has occurred.
33. The actual outcome is likely to be influenced by a number of factors, including the requirements of the advertising restrictions, the evolution of scheduling and viewing patterns, the changing emphasis of advertising campaigns, and the extent to which HFSS advertising displaced from children’s channels re-appears in adult airtime on other channels. Other factors that may influence the outcome include the extent to which product reformulation (a long term process) contributes to changes in the balance of HFSS and non-HFSS products advertised on television, and possible changes to the nutrient profiling scheme stemming from the FSA’s 2008 review.
34. For these reasons, we need to look at actual data from 2009 in order to gauge the full effects of the restrictions. Accordingly, we intend to carry out a further review in early 2010, once we have full-year data from both 2008 and 2009. As with the current review, the focus will be on whether the advertising restrictions are having the anticipated effects, rather than attempting to identify the direct impact of the restrictions on child obesity levels.
Annex
BCAP Broadcasting Code rules - HFSS products
7.2 Food and Soft Drink Advertising and Children
Notes:
(1) The rules in 7.2 must be read in conjunction with the other rules in this Code, especially section 8.3, ‘Food and Dietary Supplements’. For rules on the scheduling of HFSS product advertisements, please see the BCAP Rules on the Scheduling of Television Advertisements. References to food apply also, where relevant, to beverages.
(2) The spirit, as well as the letter, of the rules in this section applies to all advertisements that promote, directly or indirectly, a food or soft drink product.
(3) These definitions apply in rule 7.2:
- Children - refers to persons below the age of 16.
- Advertisements targeted directly at pre-school or primary school children – advertisements that directly target pre-school or primary school children through their content as opposed to their scheduling. For rules on the scheduling of HFSS product advertisements, please see the BCAP Rules on the Scheduling of Television Advertisements.
- Licensed Characters - those characters that are borrowed equities and have no historical association with the product.
- Equity Brand Characters - those characters that have been created by the advertiser and have no separate identity outside their associated product or brand.
- HFSS products - those food or drink products that are assessed as high in fat, salt or sugar in accordance with the nutrient profiling scheme published by the Food Standards Agency (FSA) on 6 December 2005. Information on the FSA’s nutrient profiling scheme is available on the FSA website at:
http://www.food.gov.uk/healthiereating/advertisingtochildren/nutlab/
7.2.1 Diet and lifestyle.
Advertisements must avoid anything likely to encourage poor nutritional habits or an unhealthy lifestyle in children.
Notes:
(1) This rule does not preclude responsible advertising for any products including those that should be eaten only in moderation.
(2) In particular, advertisements should not encourage excessive consumption of any food or drink, frequent eating between meals or eating immediately before going to bed.
(3) It is important to avoid encouraging or condoning attitudes associated with poor diets, for example, a dislike of green vegetables.
(4) Portion sizes or quantities of food shown should be responsible and relevant to the scene depicted, especially if children are involved. No advertisement should suggest that a portion intended for more than one person is to be consumed by a single individual or an adult’s portion, by a small child.
(5) Advertisements for food should not suggest that an inactive or sedentary lifestyle is preferable to physical activity.
7.2.2 Pressure to purchase
Note: Please see also 7.3 (Pressure to purchase)
(a) Although children may be expected to exercise some preference over the food they eat or drink, advertisements must be prepared with a due sense of responsibility and should not directly advise or ask children to buy or to ask their parents or other adults to make enquiries or purchases.
Notes:
(1) This extends to behaviour shown: for example, a child should not be shown asking for a product or putting it into the parent’s trolley in the supermarket.
(2) Phrases such as “Ask Mummy to buy you" are not acceptable.
(b) Nothing in an advertisement may seem to encourage children to pester or make a nuisance of themselves.
(c) Advertisements must not imply that children will be inferior to others, disloyal or will have let someone down, if they or their family do not buy, consume or use a product or service.
(d) Advertisements must neither try to sell to children by appealing to emotions such as pity, fear, loyalty or self-confidence nor suggest that having the advertised product somehow confers superiority, for example making a child more confident, clever, popular, or successful.
(e) Advertisements addressed to children should avoid ‘high pressure’ and ‘hard sell’ techniques, i.e. urging children to buy or persuade others to buy. Neither the words used nor the tone of the advertisement should suggest that young viewers are being bullied, cajoled or otherwise put under pressure to acquire the advertised item.
(f) If an advertisement for a children’s product contains a price, the price must not be minimised by the use of words such as "only" or "just".
Note:
Products and prices should not be presented in a way that suggests children or their families can easily afford them.
7.2.3 Promotional offers
Promotional offers should be used with a due sense of responsibility. They may not be used in HFSS product advertisements targeted directly at preschool or primary school children.
(a) Advertisements featuring promotional offers linked to food products of interest to children must avoid creating a sense of urgency or encouraging the purchase of excessive quantities for irresponsible consumption.
(b) Advertisements should not seem to encourage children to eat or drink a product only to take advantage of a promotional offer: the product should be offered on its merits, with the offer as an added incentive. Advertisements featuring a promotional offer should ensure a significant presence for the product.
(c) Advertisements for collection-based promotions must not seem to urge children or their parents to buy excessive quantities of food. They should not directly encourage children only to collect promotional items or emphasise the number of items to be collected. If promotional offers can also be bought, that should be made clear. Closing dates for collection-based promotions should enable the whole set to be collected without having to buy excessive or irresponsible quantities of the product in a short time. There should be no suggestion of “Hurry and buy".
(d) If they feature large pack sizes or promotional offers, e.g. “3 for the price of 2", advertisements should not encourage children to eat more than they otherwise would.
(e) The notion of excessive or irresponsible consumption relates to the frequency of consumption as well as the amount consumed.
7.2.4 Use of characters and celebrities
Licensed characters and celebrities popular with children must be used with a due sense of responsibility. They may not be used in HFSS product advertisements targeted directly at pre-school or primary school children.
Notes:
(1) Advertisements must not, for example, suggest that consuming the advertised product will enable children to resemble an admired figure or role model or that by not doing so children will fail in loyalty or let someone down.
(2) This prohibition does not apply to advertiser-created equity brand characters (puppets, persons or characters), which may be used by advertisers to sell the products they were designed to sell.
(3) Persons such as professional actors or announcers who are not identified with characters in programmes appealing to children may be used as presenters.
(4) Celebrities and characters well-known to children may present factual and relevant generic statements about nutrition, safety, education, etc.
7.3 Pressure To Purchase
7.3.1 Direct exhortation
Advertisements must not directly advise or ask children to buy or to ask their parents or others to make enquiries or purchases.
7.3.2 Unfair pressure
Advertisements must not imply that children will be inferior to others, disloyal or will have let someone down, if they or their family do not use a particular product or service.
[1] Commercial spin off services are ITV2, ITV3, ITV4, Men and Motors, Channel 4+1, E4, More 4, Film Four, Fiver, Five US and +1 time shifted versions of the channels
[2] Our analysis mirrors the findings of the Department of Health report which used a different measure (advertising spend) to establish the reductions in children’s exposure. Both pieces of analysis show a fall in impacts for all techniques considered to appeal to children.
The Committee for the Office of the
First Minister and deputy First Minister
Inquiry into Obesity
On 28 January 2009, the Committee for the Office of the First Minister and deputy First Minister considered your invitation to submit written evidence in relation to your Committee’s Inquiry into Obesity.
The Committee for the Office of the First Minister and the deputy First Minister sought in its recent inquiry into Child Poverty to develop a detailed understanding of child poverty in Northern Ireland and to use this understanding as the basis for the development of constructive suggestions to assist the Executive, and indeed future administrations, in developing a robust strategy to eliminate child poverty.
The Committee sought written and oral evidence regarding child poverty, and received several responses that highlighted the findings of the ‘Health and Social Care Inequalities Monitoring System: Second Update Bulletin 2007’ linking child poverty and obesity. The bulletin states that 5·9% of children in deprived areas are obese compared to 4·9% in areas that are not described as deprived.
Witnesses from Playboard; Eastern Health and Social Services Board; Western Investing for Health Partnership; Western Health Action Zone; and Derry City Council addressed obesity in their responses to the Committee’s inquiry. Among these submissions are examples of good practice to tackle the problem via improved play opportunities and programmes to educate families about personal development; physical activity; diet, nutrition and oral health; and to improve knowledge and skills for healthy lifestyles.
As you will appreciate, the Committee received a great deal of information in the course of its inquiry. In its summary, the Committee subsumed the issue of obesity into its conclusion on measures to tackle long-term disadvantage:
“In the long-term, improving the health and well-being and educational outcomes of families in poverty has a critical role in helping to address the cycle of deprivation. The Committee recognises the successes that there have been over the past decade in improving overall educational outcomes and in increasing life expectancy and reducing levels of preventable illness. However, the gaps in educational and health outcomes between children living in poverty and children from more affluent backgrounds remain stubbornly unaffected. The Committee is convinced of the importance of early intervention and family based approaches in seeking to break the cycle of poverty and wishes to see the Executive establishing specific objectives to increase the level of investment across government in early years services and to increase the number of places provided within Sure Start. The Committee has also identified the need for legislation relating to the planning of children’s services to be reviewed to ensure that there is a truly joined-up approach to children’s services planning in Northern Ireland."
Recommendation 41 of the report was as follows:
“The Committee considers that more attention needs to be paid to identifying and targeting the population groups at most risk of poor educational or health outcomes with specific, evidence-based strategies that will deliver real improvements for such groups."
The Executive response to this focused on the OFMDFM-led multi-agency Promoting Social Inclusion workstream and the overall Lifetime Opportunities Strategy.
I hope that these references will signpost you to the evidence relevant to your inquiry and that the Child Poverty Report provides useful background information about the health and opportunity costs, including obesity, that result from child poverty.
Yours sincerely,
Mr Danny Kennedy
Chairperson, Committee for the Office of the First Minister
and deputy First Minister
Department for Employment and Learning
Contents
- Summary of the Department’s aim, strategic objectives and key areas of activity
- Summary of DEL key business areas
- The context of the Department’s work
- The relevance by business area of the Department’s work towards tackling obesity and an indication of the opportunities that DEL might have to identify and respond to the needs of individuals
1 Departmental Aim
- To promote learning and skills, to prepare people for work and to support the economy.
- Strategic Objectives
To promote economic, social and personal development through high quality learning , research and skills training: and
To help people into employment and promote good employment practices
2 Department’s key areas of activity
- Enhancing the provision of learning and skills, including entrepreneurship, enterprise, management and leadership.
- Increasing the level of research and development, creativity and innovation in the Northern Ireland Economy.
- Helping individuals to acquire jobs, including self employment, and improving the linkages between employment programmes and skills development; and
- the development and maintenance of the framework of employment rights and responsibilities.
3 Key Business Areas in DEL
Corporate Services: Minister’s Private Office/ Office of the Permanent Secretary/Central Management, Press Office, personnel, staff welfare, staff training, departmental records, [statistics / research and evaluation.]
Strategy and Employment Relations: Strategy and Equality covering compliance with S75 statutory duties and in particular the Department’s linkages with interdepartmental strategies; Employment and Industrial Relations, including responsibility for relevant legislation, and sponsorship of the Labour Relations Agency; the NI Certification Office; the administration of the Office of Industrial and Fair Employment Tribunals; the Industrial Court; and the Redundancy Payments Service; Migrant Workers Unit (facilitating the interdepartmental strategy); statistics/economists/research and evaluation.
Higher Education: Development of policy for the planning, funding and administration of higher education. Also, policy for student loans and awards, education maintenance allowances and for the payment of postgraduate awards.
Further Education: Development of policy for the planning, funding and administration of further education, including the reconfiguration of the Further Education Sector in line with the FE Means Business Review. Also responsible jointly with the Department of Education for the policy and curriculum for the 14-19 age group.
Skills and Industry : Responsibility for the NI Skills Strategy that sets out a vision for skills in Northern Ireland in 2015 and focuses on raising the skills levels of the workforce, enhancing the quality of those entering the workforce, and addressing the employability of those not in employment. This includes Careers Information, Advice and Guidance policy and delivery and the policy and administration of Training for Success, Apprenticeships, Bridge to Employment and Management Leadership programmes and also for sector development and the associated Sector Skills Councils.
Preparation for Work: Responsibility for the administration and delivery of the New Deal programmes; Steps to Work initiatives; the Disablement Advisory Service; Pathways to Work targeted at Incapacity Benefit recipients; Progress2Work (NI) to assist with overcoming major barriers to employment resulting from problems associated with homelessness and substance misuse, an offending background; and other community based employability initiatives such as LEMIS (Local Employment Intermediary Service) designed specifically to engage with unemployed and economically inactive people in Northern Ireland’s most disadvantaged areas, and help them equip themselves for work.
Employment Service (part of Preparation for Work Division): the delivery of the public employment service through frontline teams in the network of 35 Jobs & Benefit Offices and JobCentres. A pivotal function of the Service is its local engagement with employers and the availability of “online" vacancy filling services to assist business and jobseekers alike.
4 Context of DEL’s work
DEL’s Contribution to the Programme for Government is summarized as follows:
Priority: Growing a Dynamic, Innovative Economy
Actions: Increase by 300 the number of PhD research students at local universities by 2010
Introduce a new programme to increase the commercialisation of university and college research by 2010.
Goals: Increasing the employment rate from 70% to 75% by 2020
Ensuring by 2015 that 80% of the working age population is qualified to at least GCSE level or equivalent.
Increasing the number of adult learners achieving a qualification in literacy, numeracy and ICT skills by 90,000 by 2015.
Increasing by 25% the numbers of students, especially those from disadvantaged communities, at graduate and postgraduate level studying Science, Technology, Engineering and Mathematics (STEM subjects) by 2015.
Priority: Promote Tolerance, Inclusion and Health and Well-Being
Actions: Put in place by 2010 a careers advice service to meet the needs of people with disabilities.
In carrying out its business DEL will contribute to the following Public Service Agreements (PSAs):
- PRODUCTIVITY GROWTH - Improve Northern Ireland’s manufacturing and private services productivity
- SKILLS FOR PROSPERITY - Ensure our people have the right skills to deliver economic prosperity now and in the future and increase skills and career choices in STEM subjects – (DEL in lead)
- INCREASING EMPLOYMENT – Subject to economic conditions, increase employment levels and reduce economic inactivity by addressing the barriers to employment and providing effective careers advice at all levels – (DEL in lead)
- CHILDREN AND FAMILY - To ensure that children are cared for, live in safety, are protected from abuse, receive the support they need to achieve their full potential, become more independent and grow into well adjusted adults, taking their place in the community
- HELPING OUR CHILDREN AND YOUNG PEOPLE TO ACHIEVE THROUGH EDUCATION - Encourage all our children to realise their potential by improving access to formal and non formal education and provision tailored to the needs of disadvantaged children and young people.
- HOUSING, URBAN REGENERATION AND COMMUNITY DEVELOPMENT - Promote decent, energy efficient, affordable housing and regenerate disadvantaged areas and towns and city centres, and support community development to create environments which enhance quality of life and contribute to well-being
- INVESTING IN THE HEALTH AND EDUCATION ESTATES Take forward a programme of investment to provide a modern fit-for-purpose health and education estate in line with best practice and ensuring value for money
In the delivery of its programmes and services DEL has a range of contractual and other arrangements with delivery partners. These include Universities, Further Education Colleges, training organisations – both private sector and voluntary and community organisations, and other organisations providing specialist support for DEL customers.
DEL’s Role in tackling Obesity
The Department for Employment and Learning is an active member of the NI Physical Activity Implementation Group. This Group is taking forward the recommendations in the NI Physical Activity Strategy which aims to increase levels of health related physical activity particularly among those who exercise least. DEL’s direct influence in this regard is linked by its role and remit.
Further Education
The welfare of students in FE Colleges falls directly to the institutions involved.
FE Colleges are important institutions in which health can be promoted. Many students gain information about nutrition through their learning programmes. DEL has therefore issued guidelines on issues within the FE sector on physical activity, eating and health as well as drugs and substance abuse.
Most of the FE colleges have sporting/fitness facilities which are available for use by students. The Governing Bodies have ultimate responsibility for sport and facilities.
Within the FE sector, DEL funds a range of Physical Education and Sports Studies/Sciences across NI. Capital funding continues to be available for all curriculum areas, including sports facilities.
Higher Education
DEL supports innovation, research and development in universities including in the field of health. For example, the University of Ulster’s Sports Related Studies was placed in the top third of Sports-Related Studies in the UK in the recent Research Assessment Exercise. Among the research areas studied by the institute are:
- Adolescent lifestyle and health
- Health benefits of physical activity
In addition, our two universities are undertaking excellent work, in the field of diabetes, which it is widely recognized is often developed by people who are obese.
Queen’s University Belfast Diabetes Research Group
The Group is based on the Royal Victoria Hospital site of Queen’s University Belfast (QUB). There are active collaborations with local clinicians (diabetes), and with national and international groups.
The major work of the Group involves the vascular complications of diabetes and obesity, a major risk factor for the development of type 2 diabetes.
Of the successful projects recently awarded funding, through DEL’s ‘Strengthening the All-Island Research Base’; one is entitled ‘Diet, Obesity and Diabetes’. Its objective is to bring together the leading research groups throughout Ireland to provide a comprehensive all-island research centre to improve the primary and secondary prevention of obesity and diabetes. QUB will work in collaboration with the Institute of Public Health in Ireland and The National Research Centre for Diet, Obesity and Diabetes, University College Cork.
University of Ulster Diabetes Research Group
Since its formation in1989 the Group has built an extensive range of external networks being the founder of the European Association for the Study of Diabetes (EASD) Islet Study Group and playing a pivotal role in the establishment of the EU-funded Islet Research European and Latin-American Networks. The Group has also played a key role in diabetes research both nationally and internationally through senior positions in the British Diabetic Association/Diabetes UK, the EASD and establishing rich collaborations with numerous Centres of Excellence worldwide. The Group’s activities are expanding and the formation of a province-wide HPSS funded RRG in Diabetes and Endocrinology has strengthened local clinical collaborations.
Areas of research studied by the group include assessment of diet and lifestyle factors in gestational type 1 and type 2 diabetes. This research aims to assess what women with diabetes eat in relation to lifestyle and published dietary guidelines. A further element is assessing maternal diet and lifestyle factors in relation to gestational diabetes and pregnancy outcomes.
While DEL has links with teacher training colleges, the curriculum and supply of teachers is the responsibility of Department of Education.
However, regarding training for non-teacher coaches, SkillsActive (the Sector Skills Council for Active Leisure) is very much involved in determination of the skills needs in its sector in NI and works through a very robust network of employers and stakeholders. SkillsActive has a sector skills agreement for the industry which refers to coaching and identifies the needs of this sub-sector. They are continuing to seek employer and stakeholder views and work towards an action plan to address these needs.
With the exception of the Open University, all of the Higher Education Institutions in Northern Ireland have, or provide access to, dedicated sports facilities for staff and students to avail of. These include, for example, the Physical Education Centre (PEC) at Queen’s University and a range of leisure facilities at three of the University of Ulster’s campuses. UU also has boasts the Sports Institute for Northern Ireland at its Jordanstown campus and, in common with the other institutions, hosts a number of sports clubs and teams.
Sectoral Development
SkillsActive is the Sector Skills Council (SSC) responsible for upskilling the workforce in the sport and leisure sectors. DEL is providing funding support for projects including, Workforce Development Planning in Sport; Workforce Development Initiative; and Profile of the 2012 Active Leisure Workforce.
Skills for Care and Development is the SSC responsible for developing and training the social care and children’s services workforce. NI Social Care Council is the regulatory body for the Northern Ireland social care workforce. It is an independent public body, established to increase public protection by improving and regulating standards of training and practice for social care workers. This includes National Occupational Standards to Promote the Health and Physical Development of Children; elements include:
- Plan and implement physical activities and routines for children to meet their physical development needs.
- Plan and provide food and drink to meet the nutritional needs of children Promote children’s healthy physical development
DEL Staff
Many DEL staff have benefited from attending the NICS Sports Association (NICSSA) Healthworks events over the past number of years. The core 2 day programme includes advice on nutrition, alcohol consumption and exercise. The course is available to all staff through the Centre for Applied Learning. There are also options for shorter, more specific sessions which DEL managers tend to incorporate into team time or other events.
The Lifestyle and Physical Activity Assessment programme is operated by the Occupational Health Service (OHS) with places allocated to each Department. The programme includes a lifestyle evaluation and assessment of activity levels. A physiological assessment includes measurement of blood pressure, cholesterol, strength, flexibility, lung function and stamina. On completion of the test, general advice on improving lifestyle is given and each participant gets a personalised fitness printout.
In relation to DEL staff, as with other public sector organizations, catering policies
are reviewed to ensure that healthy food options are available on their premises.
DEL Commitment
The Committee will wish to be aware that the Department for Employment and Learning is committed fully to the aims and objectives of Fit Futures, the Investing for Health Strategy and the NI Physical Activity Strategy, all of which focus on the importance of tackling obesity. DEL will continue to engage with the work of the various Groups on which it sits and do all within scope of its core business to address this important and widespread issue.
Department for Employment and Learning
3 February 2009
Conservation Volunteers Northern Ireland
Conservation Volunteers Northern Ireland has been a registered charity involving all sections of the community for 25 years. We’re aiming for a better environment where people feel valued, included and involved. Every year Conservation Volunteers Northern Ireland, which is part of BTCV, connects with 29,800 people who make positive differences to their local communities and their environments. Our mission is to create a more sustainable future by inspiring people and improving places.
Conservation Volunteers’ values are integral to all our work. They have been developed through two decades of a ‘hands-on’ approach to conservation activities. During this time we have adapted to meet the changing needs of communities, we care about people, the communities in which they live and the quality of their lifestyles and living environment.
Conservation Volunteers Northern Ireland aims to create a better environment where people from all ages, abilities and cultures feel valued, included and involved. This is achieved through the delivery of projects under four broad themes: Health, Environments for All, Direct Action and Biodiversity.
Welcome for the Inquiry
Conservation Volunteers welcomes this Inquiry by the Health Committee into this important issue facing the whole of society. Rising obesity levels, especially in children, is a serious problem that also reflects some more general problems in society and will have major impacts on public health and medical care for many years to come.
Across the UK the equivalent of £886 per head of population is spent per year in providing what amounts to a national sickness service and we spend £1 per person per year on sports and physical activity which could actually prevent a lot of that sickness."
Obesity – Lifestyle and diet
It is recognised that the fundamental causes of obesity are lack of physical exercise and poor diet. A number of other factors are also being taken into consideration, such as increased consumption of high calorie energy dense foods, increased levels of TV watching, use of games consuls, advertising and promotion of unbalanced diet, availability of convenience food, cost of healthy food options, inadequate cooking skills, and transport and planning decisions. British Heart Foundation statistics 2004 show Northern Ireland individuals spend on average 157.1 minutes per day watching TV and DVD’s, 3.5 minutes gardening and 4.4 minutes walking.
Linking the natural environment and health
Conservation Volunteers believe that there is a direct connection between quality of living environment and quality of life. We recognise that disadvantaged communities generally experience poorest quality built and natural environments, as well as poor health, poor education and poor employment prospects. Improving one aspect of these issues is not the solution. Increasing physical activity alone is not the answer, objectives need to include learning on wider health issues e.g. mental health, diet and nutrition, community involvement and cohesion whilst demonstrating how easy and effective it is to increase your daily exercise levels and sustain these over a period of time.
There is mounting evidence of the links between direct contact with the natural environment and the positive benefits to individuals and community health. In society, as a whole, there is an increase in sedentary, virtual lifestyles which is having a dramatic increase in very real physical and mental health problems. Extensive research has shown that physical activity can be an effective method of improving psychological well-being, reducing clinical depression, risk of depression, anxiety and stress, and improving aspects of mental functioning such as planning, short-term memory and decision making. It has also been mooted that people have a biologically-based attraction to nature (‘biophilia’) and that being in and connecting to nature can itself provide mental health benefits (Mental Health Foundation 2007).
Conservation Volunteers Green Gym Project has developed a flexible needs based approach which tackles overlapping issues of sedentary lifestyles, poor diet and nutrition, mental ill health, social isolation, poor living environment, lack of environmental and health awareness. As the Green Gym creates the opportunity to increase physical activity without exercising in the conventional sense of the term, Conservation Volunteers encourage individuals to be healthier physically therefore happier mentally. Direct involvement in the Green Gym address additional issues of community empowerment and ownership.
Help individuals and communities to develop skills to make healthier lifestyle choices.
The quality of life in disadvantaged urban areas can be significantly improved though raising awareness about how to make healthier lifestyle choices, e.g. by providing hands-on experience of growing, cooking and eating fruit and vegetables and measuring dietary changes through participants food diaries. The Green Gym assists participants to take the first steps to increase physical activity levels whilst incorporating healthy eating and improved nutrition, and equip them with the knowledge and confidence to sustain these on a long-term basis.
Green Gym Community Fruit & Vegetable Gardens
The overall aim of this project is to establish and sustain affordable healthy eating in areas of long-term deprivation. Through the direct involvement of local people the project increases knowledge and develops skills across a range of areas, e.g. growing vegetables, cooking for health and nutritional information. Conservation Volunteers Fruit & Vegetable Green Gyms are delivered in Partnership with Belfast Health Trust Community Dietitic Services, providing a holistic approach to healthier lifestyles. The physical activity of developing the community gardens is complemented by health eating and nutrition sessions.
Conservation Volunteers have six years of experience of developing community fruit and vegetable gardens through our Green Gym Project. This project helps achieve objectives outlined in a number of Regional Diet & Nutritional Strategies:-
‘Fit Futures: Focus on Food, Activity and Young People’
‘We are What we Eat - Future Challenges’
The Eat Well Model, formally the Balance of Good Health Model is an integral part of this project where indoor information sessions will be delivered in conjunction with the practical garden development and growing. The Cook it Model is also incorporated with sessions covering how to cook fresh produce from your garden, food hygene and cooking on a budget. Conservation Volunteers will expand this holistic approach to healthy eating into the two identified project areas.
Monitoring of existing fruit and vegetable Green Gym projects shows an increase in number of pieces of fruit and vegetables eaten per day after six months of regular involvement. On project day one 0-16 year olds consumed 0.97 pieces per day and adults 0.7. These figures increased to 4.28 and 3.8 respectively by project day 15 (NI Green Gym 2007).
Integrated Solutions to Obesity
As highlighted across a number of Health Strategies tackling the current issues including obesity lies beyond the capacity of the Health Service alone. Joint up partnership working is required of affective approaches are to be implemented and successful.
Adopting an integrated approach to obesity, addressing several causal factors while promoting more sustainable lifestyles and food consumption, will have many benefits for public health and for the health service, as well as additional benefits to the community through enhanced provision of goods and services which will facilitate people to adapt to the changes facing us all in the 21st century.
Conservation Volunteers would like to thank you for this opportunity to comment on the raising issues of Obesity in Northern Ireland. If you require any further details or clarification of the comments please do not hesitate to contact us.
The Royal College of Psychiatrists
Mr Hugh Farren
Clerk to the Assembly Health Committee
Room 412
Parliament Buildings
Stormont
Belfast BT4 3XX
12 February 2009
Dear Mr Farren
Thank you for your invitation to provide evidence to the Assembly Health Committee’s inquiry into obesity. The Royal College of Psychiatrists commends the Health Committee for its work in this area.
People with mental illness and those with learning disabilities are more likely than the general population to be obese, to have physical health problems arising from this, and to have difficulty managing weight. We therefore welcome the Health Committee’s interest in including this group of people in considering an obesity strategy for Northern Ireland.
As a College, we are committed to helping the Assembly understand the issues involved in psychiatry in Northern Ireland, and hope the Committee will continue to call on us as appropriate.
Yours sincerely
Dr. Philip Mc Garry FRCPsych
Consultant Psychiatrist
NI Division Public Affairs Officer
The Royal College of Psychiatrists is the statutory body responsible for the supervision of the training and accreditation of psychiatrists in Britain and Ireland and for providing guidelines and advice regarding the treatment, care and prevention of mental and behavioural disorders.
The College has 294 members in Northern Ireland, as well as younger doctors in training. These doctors provide the backbone of the local psychiatric service, offering inpatient, day patient and outpatient treatment, as well as specialist care and consultation across a large range of settings.
The College welcomes the Assembly Health Committee’s inquiry to examine the current approach to tackling obesity, and is grateful for the opportunity to contribute to this.
Why consider people with mental illness and learning disability?
It is widely acknowledged that people with severe mental health problems and/or learning disability are more likely than the general population to be obese, and have a higher level of associated physical health problems.
This is an international trend, not unique to the United Kingdom, and is associated with a complexity of factors including medication, disadvantage and lifestyle. However, research in England and Wales quantifies the problem.
The Disability Rights Commission’s Closing the Gap report on healthcare inequalities experienced by people with mental health problems and learning disability in England and Wales (2006) found people with mental illness are much more likely than other people to be obese (33% of people with schizophrenia and 30% of those with bipolar were obese, compared to 21% of the remaining population), and to have significant related health risks and major health problems such as heart disease, hypertension, stroke and diabetes[1]. They are twice as likely to die from coronary heart disease as the general population[2].
Both people with mental illness and people with learning disability are likely to die younger than other people. People with serious mental health problems are also more likely than others to get illnesses such as strokes and coronary heart disease before 55. Once they have them they are less likely to survive for five years.
A review of international research[3] found that children and adolescents with major depressive disorder may be at increased risk for developing overweight; obese people seeking weight-loss treatment may have elevated rates of depressive and bipolar disorders; general obesity is associated with major depressive disorder in women; and abdominal obesity may be associated with depressive symptoms in men and women. However, it found that most overweight and obese persons in the community do not have mood disorders.
Obesity can be a particular issue in inpatient settings, particularly where patients are resident for a lengthy period, for example when they are detained. One forensic mental health trust in England found that it is not uncommon for patients to put on 30-40 kg while in hospital[4].
Why do people with mental health problems and learning disability carry more weight?
Many of the reasons that people with mental health problems and learning disability are obese are the same as for the general population: eating too much calorie-rich food and exercising too little.
However, the reasons for this can be complex.
- Social deprivation – obesity is a greater problem in areas of social deprivation, and people with mental illness are among the most socially excluded group. While it is possible to maintain a cheap, balanced diet, people may need education and encouragement to do this.
- Inactivity – people with mental illness tend to be more inactive than the general population due to both motivation and opportunity, and may need to be proactively engaged in activities. Inactivity can be a particular issue in inpatient settings.
- Medication factors – some psychotropic medications, in particular antipsychotics and mood stabilisers, increase hunger levels. Particular antipsychotics are well known to be linked to significant weight gain.
- Emotional eating – some people with mental health problems will over eat when emotionally distressed, or to deal with low self esteem. There is a strong correlation between obesity and depression (especially in women) and anxiety[5][6]. Over-eating and binging can be self-harming behaviours in some patients[7].
- Medical practitioners can sometimes be loathe to raise the issue of weight with a person who is already vulnerable, but should be prepared to sensitively address this and to check for associated physical health risks.
- Community dieticians often do not know how to cope with people with mental health problems, who may have fluctuations in motivation and difficulty managing medication side effects.
What could be done to address this?
All aspects of an obesity strategy are likely to apply to people with a mental health problem, but this group may be difficult to engage and require additional input and support.
People who use mental health services need to be educated about the physical health effects of food intake and obesity and encouraged to agree to positive changes to diet and exercise. Care planning should be used to support dietary modification, and encourage activity.
NICE Guidance on Obesity states that “Managers and health professionals in all primary care settings should ensure that preventing and managing obesity is a priority at both strategic and delivery levels. Dedicated resources should be allocated for action"[8]. It does not set out guidance specifically for managing obesity in people with mental illness.
However, NICE Guidance on Schizophrenia states that GPs and other primary healthcare professionals should monitor the physical health of people with schizophrenia. Physical health checks should be carried out at least annually and have results clearly documented by the primary care clinician and communicated to the mental health care coordinator and/or psychiatrist, and recorded in secondary care notes. Monitoring should include: weight gain and obesity (waist hip ratio or waist circumference); blood pressure; dietary intake; activity levels and exercise; blood levels of glucose; and lipids.
General practitioners may need to be proactive in helping people with mental illness manage their weight. This may be a sensitive issue, but should not be avoided. Mental health staff should also be proactive about addressing the issue, and where appropriate liaise with, and encourage contact with, the GP.
Diet can be problematic for people with severe mental illness. Health professionals should take this into account, and support and education should be provided to help people maintain a healthy diet. GPs should also ensure that advice on diet is given to people with severe mental illness, as included in the 2006 GP contract.
Mental health staff should be able to directly refer patients to community dieticians, and there should be a pool of dieticians trained to offer advice and support to people with mental illness. This could potentially be offered in community mental health settings.
People with severe mental illness may find shopping for food and cooking difficult, and should be provided with practical support to manage this. Mental health teams could take some responsibility for providing practical support to address these issues.
Keeping active is an important element of protecting the body from physical health problems, and can also be beneficial for mental health. GPs could consider prescribing exercise programmes for people with mental health problems who are becoming overweight. People with mental illness should be able to access leisure facilities at a concessionary rate.
In summary, the Royal College of Psychiatrists would encourage the Health Committee to consider how any obesity strategy will engage people with mental health problems, and how health practitioners can be supported to provide the necessary input.
Appendix 1
Key findings from the Disability Rights Commission
The rates of co-morbidity of severe mental illness and physical illness that are sometimes linked to obesity are higher than in the remaining population (unadjusted for differences in age distribution):
- Ischaemic heart disease is more common in people with schizophrenia (4%) and bipolar disorder (5%) compared to the remaining population (3%)
- Stroke is more common in people with schizophrenia (2%) and bipolar disorder (1.5%) compared to the remaining population (1%)
- Hypertension is more common in people with schizophrenia (12%) and bipolar disorder (15%) compared to the remaining population (10%)
- Diabetes is more common in people with schizophrenia (6%) and bipolar disorder (4%) compared to the remaining population (2%)
[1] Health Inequalities Experienced By People With Schizophrenia and Manic Depression: Analysis of General Practice Data in England and Wales, Report for the Disability Rights Commission (2005), Q Research, available at http://83.137.212.42/sitearchive/DRC/library/health_investigation/research_and_evidence.html (accessed February 2009)
[2] Department of Health. Choosing health: supporting the physical health needs of people with severe mental illness. August 2006
[3] McElroy SL et al, Are mood disorders and obesity related? A review for the mental health professional. Journal of Clinical Psychiatry, 2004 May;65(5):634-51
[4] West London Mental Health Trust (2006), Draft Obesity Management Strategy, available at www.rcpsych.ac.uk/pdf/Draft_Obesity_Strategy_June_2007_West_London_MHT.pdf (accessed February 2009)
[5] McElroy SL et al, Are mood disorders and obesity related? A review for the mental health professional. Journal of Clinical Psychiatry, 2004 May;65(5):634-51
[6] Simon GE et al, Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006 Jul;63(7):824-30
[7] West London Mental Health Trust (2006), Draft Obesity Management Strategy
[8] NICE. Obesity. Clinical guideline 43. December 2006
University of Ulster
Committee for Health and Social Care and Public Safety: Inquiry on Obesity
Thank you for asking the University of Ulster to comment on this very important public health issue. The University has a range of internationally renowned researchers in this field. In particular, I include the Northern Ireland Centre for Diet and Health (NICHE) where a number of important studies have been undertaken into the causes, effects and prevention of obesity. In addition, researchers in our School of Nursing have been funded to investigate the phenomenon of obesity in people with learning disability. Furthermore, staff in our School of Sports Studies have researched the effects of exercise on combating obesity. You could bring it to the Committee’s attention that the research quality of each of these disciplines was rated internationally excellent or world leading in the most recent Research Assessment Exercise. This is a measure of the expertise available in Ulster and if required, I am sure these colleagues would be pleased to provide you with further information. There follows our comments on the three terms of reference drawn up by the HSSPS Committee:
Introduction
Obesity is increasing at an alarming rate and estimated predictions suggest the numbers of adults and children who are overweight or obese shall increase dramatically, with over half the population in many developed countries being obese by the year 2050. The outcomes to health that can result from being obese include atherosclerosis, heart disease, diabetes, respiratory problems and a number of cancers. Problems are not restricted to physical illness with reports highlighting how obese children can face emotional issues such as low self esteem, poor expectations for their future and feelings of isolation because they are marginalised and stigmatised for being fat.
Diet, physical activity and behaviour modification have been integral to most health promotion intervention programmes that attempt to tackle obesity. But, to date no country in the world has been able to achieve sustained reversal of overweight and obesity trends.
1. Assess the scope and appropriateness of the current approach to tackling obesity and the promotion of lifestyle change
This is very difficult to determine for 2 main reasons:
1) Currently in NI there are so many different approaches: “Healthy Breaks", “Get a life get active" and “Eat well to keep well" to name just a few. The problem may well be that the public get a mixed message.
2) The approaches that have been undertaken have not been rigorously analyzed and so any useful information has been lost.
The most important factor when trying to achieving successful changes within a whole population is a uniform approach from all agencies. This will require one over arching body directing the strategy.
The Fit Futures undertook a consultation and reported in 2007 their priority approaches are:
Policies and strategies to tackle obesity should take adequate account of the importance of the role of parents and families in establishing and supporting good nutrition and active living, particularly during the first few years of a child’s life. One of the key messages to emerge from the Fit Futures consultation process is that parents have primary responsibility for ensuring the health and well-being of their children, but that action needs to be taken to support parents to fulfill this role effectively.
The development of the basic knowledge and skills necessary to encourage and support children and young people to be active and eat healthily, among those supporting and working on a daily basis with children and young people, was also identified as an important way of enabling children to make healthy choices. Policies and programmes also need to recognise the complexity of obesity and that a long-term commitment will be required if current trends are to be halted and then reversed.
Obesity is not restricted to one sector of society and a population approach to obesity prevention should be adopted. However, particular attention should be paid to the needs of children and young people on low income or with a disability as they face additional barriers to healthy eating and active living. Activity levels in girls are also a particular concern. In addition, policies and programmes to tackle obesity in children should recognise that the most effective solutions are likely to be positive and focus on promoting and developing the self-esteem of young people and that there is significant benefit to be gained from making the healthy option the fun option. Above all, the Fit Futures taskforce recognises that policies and strategies to tackle obesity must take account of the available evidence in relation to what works and what doesn’t work when it comes to obesity prevention.
(http://www.dhsspsni.gov.uk/showconsultations?txtid=22125)
However, on area that is often passed over is psychology, in a mini review Malterud and Tonstand, (2009) outlined that Individual vulnerability and neurobiological mechanisms that may lead to weight gain must be taken into consideration, when developing strategies for health promotion. Prevention of weight gain is very holistic in its nature and must take on board, socio demographic, cultural and genetic characteristics. Also, when promoting interventions or strategies to overcome weight gain/obesity it’s important to avoid body weight control into a question of morality and social identity.
2. Examine the availability of weight management or other intervention services to tackle obesity and related ill-health
Some of the obvious strategies have been by using drug intervention; however, these are limited to obese individuals and the weight loss is minimal. An intervention looking at drugs (i.e. tesofensine 0.25mg, 0.5 or 1.0mg) which inhibit presynaptic uptake of NA, dopamine and serotonin appear to double the weight loss in obese patients compared to currently approved drugs (Astrup et al., 2008)
Some interventions have looked at eating behaviours related to obesity and it’s association with job stress (Nishitani, et al., 2009). It has been argued that obesity treatments should include therapeutic strategies that decreases body related worrying and sad mood, particularly for the overweight/obese who are high in negative affect (i.e. sad mood state).
Growing evidence suggests that obesity is not just linked to a weight problem but also neurocognitive outcomes. Positive affectively in obesity treatment is, therefore, discussed (Cserjesi et al., 2009). Results provide support for current cognitive-behavioural models of binge eating and have implications for treating binge eating and intervention efforts with children (i.e. 8-13 year olds). Also there is a discussion review on the need for practitioners and health care professionals to become involved in the evaluation studies that build on the limited base of current evidence (Wofford, 2008) (I forwarded this ref last week to the obesity group so you should have a copy).
A recent study in Barcelona highlights the need to consider socio-economic indicators when implementing strategies to improve public health; however, they don’t really relate this to obesity as such (Cano-Serral, 2009).
It is clear that the increasing concern about obesity trends (an consequences) have led to many initiatives (e.g. to improve nutritional quality of food in NI schools/promotion of health promoting schools) to try to tackle the problem. While such initiatives are to be welcomed evidence on the effectiveness of such interventions ranges from thin to non-existent (or impossible). In any case, given that obesity is a complex and multifaceted disorder such initiatives in isolation are unlikely to have significant impact unless part of a multi-sectoral joined up policy on obesity. The latter will be key to any successful strategy for tackling obesity.
Note: to date no country has such a joined up, comprehensive approach to obesity.
Currently there exist no official guidelines for prevention and management of obesity.
3. Consider what further action is required, taking account, as appropriate, of the potential to learn from experience elsewhere
We think this paper may be quite relevant to help address this question James F. Sallis, (2009).
Top five promising methods that can be used in research now:
1. Policy change evaluations that assess (1) implementation, (2) enforcement, (3) community acceptance, and (4) impact over time on rates of obesity or obesogenic nutrition behaviors;
2. Surveillance research to track changes in food-industry activities with the potential to influence nutrition behaviors (e.g., packaged portion sizes, reduced-calorie options) would allow researchers to (1) identify opportunities for natural experiments, (2) examine the influence of industry activities on nutrition behaviors and obesity, and (3) determine how industry activities shift in response to policy changes;
3. Observational multilevel studies, including research designed to examine interactions between individuals and food environments (e.g., what individual factors increase susceptibility to obesogenic food environments);
4. Studies designed to examine (or quantify) the influence of multiple environmental domains and their interactions on rates of obesity (or obesogenic nutrition behaviors);
5. Cross-disciplinary and transdisciplinary collaborations that incorporate complementary methodologies (e.g., qualitative and quantitative approaches).
Top five research priorities:
1. Conduct research in minority and low-income populations, such as the evaluation of policies to reduce/eliminate disparities in access to food (e.g., tax incentives for stores in low-income neighborhoods);
2. Develop standardized measures of food environment and nutrition policies (for various types of environments and contexts) to improve the comparability of findings across studies);
3. Examine motivations for food choices, including tensions between internal and external (environmental) factors on behavior;
4. Conduct research relating to home and family food environments;
5. Conduct research guided by systems theory.
All of which could be implemented although modified here.
Key issues for the future
- Plan with a long term horizon. Obesity is a side-effect of our own “success" and there will be no quick fixes to this problem. (Realistically it is most unlikely that we will arrest, let alone reverse the current NI trends in obesity for the foreseeable future). There should be no more one-off (knee-jerk) programmes – systematic changes that are sustained and sustainable are key;
- Maintain a high profile;
- Information campaigns on their own are unlikely to have large impacts;
- Optimal response may be to use incentives (monetary and otherwise) or other strategies to make it cheaper and easier to be thin, not fat;
- Technology is part of the problem but also part of the solution (e.g. food reformulation);
- Most of the factors that influence the population prevalence of obesity lie well beyond the capacity of the individual, the family or even the Health Sector to modify. Hence the need for a trans-sectoral approach – essential to have the inputs and support of all public and private sector stakeholders who have the potential to influence lifestyle and body weight;
- Needs to be adequately resourced!!! (and resources shared).
Specifically with regard to the public sector
- Identify where public agency objectives intersect;
- Promote “conjoined" approach in public sector;
- Joint policy development and implementation;
- Local planning of health agendas needs to take explicit account of obesity;
- Steps to redress social class inequalities in health – and the social class gradient in obesity.
What needs to be done?
- Research: what works? Assemble an evidence base;
- Need to apply the “Precautionary Principle – do the interventions and fully evaluate them to ensure that the investment benefits those concerned;
- Need to find ways to better support parents and families. Prevention of childhood obesity is paramount but there is a dearth of evidence on effective strategies to prevent obesity in younger (pre-school children);
- Rigorous evaluation of the probable link between obesity and food insecurity could help to identify interventions and policies that could reduce both the social gradient and prevalence of obesity;
- Few professionals (e.g. health, education) are well trained in obesity prevention and management;
- Early intervention on weight gain (specific attention to high risk groups e.g. children with one/two obese parents).
Finally the way food marketing contributes to childhood obesity is of importance, Harris, 2008, describes various mechanisms which may be implemented in order to change the current situation (Harris, 2008).
In the School of Sports Studies and the Sport & Exercise Sciences Research Institute we are involved in a range of studies relating to physical activity and health. Many of these have implications for both obesity prevention and management- although neither of these have been primary outcome measures.
For example our group has recently shown the beneficial effects of acute (single bout) and chronic (12 week training program) moderate intensity aerobic exercise on various cardiovascular, metabolic and physical indices of health in a group of obese subjects suffering from impaired glucose tolerance (IGT) or ‘pre-diabetes’.
This research was recently presented at the American College of Sports Medicine Annual Conference 2009 in Seattle, USA. 2 abstracts have been published in Medicine and Science Sports and Exercise Vol 41 no.5 May 2009 supplement : McClean et al pp S26 and McNeilly et al pp S511
We also have a range of publications on the role of exercise in altering health parameters in a range of populations which have a slightly more tangential relevance to obesity prevention - if you would like our Research Institute Director, Eric Wallace to forward these- please let us know
Obesity Management Association
This report is presented in response to the invitation by the Committee for Health, Social Services and Public Safety to submit evidence to assist the Committee to carry out an inquiry into obesity.
Executive Summary
- Obesity treatment costs will continue to escalate each year – expected to reach £46billion by 2050.
- Obesity is a medical disease not a “Social Illness".
- Focusing solely on fat intake fails to recognise the impact of salt, sugar and alcohol which are major contributory factors.
- Overweight people will become obese, by which time the challenge to provide effective treatment has multiplied.
- By ignoring the socio-economic profiles of those most at risk contributes to the problem.
- Busy lifestyles, poor education, depression, stress, low esteem, lack of family unity are all contributory factors.
- NHS has been unable to deliver either short or long-term solutions because it does not have either the manpower or budget to deal with this crisis.
- 80% of OMA clinic patients surveyed had passed through the NHS which failed them. Identifiable needs of this patient group include:
- A positive response
- Help and solutions
- Understanding of and access to all treatments available
- Time to be treated – with the doctor or nurse
- Assistance to achieve consistent weight loss
- Reliance on Exercise, Diet, Education, Healthy Eating and Lifestyle Change as an initial treatment is a failed policy for the majority of obese patients as it chooses to ignore the individual patient’s clinical condition.
- Early medical intervention is essential rather than a last option.
- Long term and in certain cases lifetime medical treatment will ensure increased control of the problem and reduction in the obese population.
- NHS needs the Private Sector to assist with the burden.
- Average cost to the NHS per patient of a single visit to the doctors and drug treatment for one week is £37.75 which is five times the cost when compared to the private sector which is £7.50 per patient visit.
- NAO figures state the cost of treatment for overweight diabetics to be £4 billion and is projected to reach £14billion.
- BMI as a benchmark is outdated and restrictive – it does not allow all health factors to be taken into account.
- Treatment of obese and overweight children requires a different approach. There is a spectrum disorder – at one end there is the supportive family that takes positive action, at the other end one has little or no action to support the child. In the worst cases, overweight and obesity are accepted as the “norm".
Assessment of the Scope and Appropriateness of Current Approaches to the Prevention of Obesity and the Promotion of Lifestyle Changes
Until very recently obesity had been considered to be a lifestyle disease, but after a review by the United Kingdom Government’s National Audit Office, the accent changed and obesity is now regarded as a serious life threatening disease - the consequences of which cost the Government in excess of £6billion per year to treat, and this amount is rising. (This is the estimated cost to NHS in England and Wales only as both Scotland and Northern Ireland have independent health services).
These consequences include diabetes, high blood pressure, heart disease and cancer. They take up medical staff time, hospital beds, medicines and worry for patients and their families. In addition to the £6billion treatment costs, there is also a loss of earnings for the families and the value of lost workdays which collectively could add a further £1+billion to the eventual cost.
Historic and current policies to deliver long-term solutions for the treatment of obesity do not work.
The UK Government’s current anti-obesity policies focus on well meaning but ineffective practices which depend on the positive and continuous commitments from the patient;
- Dieting
- Healthy eating
- Exercise
- Education
- Lifestyle Changes
- Medical intervention as a last resort
These have failed to stop the crisis, and therefore a different approach is required.
The outcome is there is a major group of people who are overweight and obese due to poor diets, lack of exercise and an unwillingness to change their lifestyles and eating habits.
The socio-economic profile of the highest population group of obesity patients are C3 – D and E, namely low income households, poorly educated, low personal esteem who lack motivation and are dependent on the State.
The results of OMA’s 2007 survey of patients through its clinics confirm the above, and a genuine reluctance to engage with their General Practitioners. We believe this is largely due to time constraints and pressure on General Practitioners.
OMA recognises there are a group of patients across all socio-economic groups whose personal physiology results in them being obese.
The UK Government’s approach is to educate centrally using television press, outdoor and direct mail advertising supported with PR and to pass treatment responsibilities to Primary Care Trusts, so in practice there are hundreds of different ideas and ambitions without a common theme. [refer to the appendix on the latest programme introduced by the Scottish Government which confirms this positions].
Advertising by the Government puts the accent on obesity and becoming ill, however advertising that if you become slim, you become fit and happy tends to work better – especially with children. Surprisingly none incorporate the use of private clinics which can offer lower cost in patient treatments thereby releasing pressure and demands on the NHS.
The current treatments of obesity in the UK NHS have the classic central Government philosophy;
- One size fits all – you are not an individual you are a statistic.
- Guilt or social responsibility for being obese – it’s your own fault.
- You can change through – diets, exercise, education and lifestyle change – where is the help and support?
- Medical – clinical intervention when it is too late to do anything else.
Child Obesity
The loss of school playing fields and fear of children being abused causes many children to stay at home and undertake no exercise, which increases obesity. However, all football clubs should be encouraged to give exercise (and fun) to very large numbers of children and O.M.A. would be prepared to organise this.
The traditional home economic teaching in school would help children of poorer families to understand what is healthy and necessary, such as the five-a-day advertisement which has been successful. Add to this how to eat healthily within your budget would address the financial question.
In this vein, the use of Irish celebrity chefs heading up good kids and family food/diet campaigns locally and shown on national television can focus the mind of children and youths. This can be very cost effective and it is reality television, which is now popular with this audience.
The National Institute of Clinical Excellence (NICE) issued guidance regarding the treatment of children, but this excluded the use of medicines in the under-18 age group.
Dr Jeffrey Fine, OMA Board Member and Harley Street specialist in the treatment of overweight and obese patients has also produced guidelines on the treatment of obesity in children – an extract from his report follows;
Intervention Strategies
The treatment of obese and overweight children requires a different approach to that of adult treatment programmes.
Unfortunately many doctors consider this to be a “glandular problem" and simply check height and weight and conclude because of their age they lay down fat more easily – with respect this is a myth Obesity results from excess of food intake over output, one must of course exclude rare causes. Constitutional facts are not a cause.
Similarly, obese infants and toddlers do not always end up being obese adults “the bonny baby" belief is another myth.
The older the child the more likely the problem is to persist. This is a spectrum disorder. At one end a supportive family will take action to address the issues, sadly at the other end the behaviour problems by uninterested family obesity is the norm, and therefore little or no action is taken to rectify the problems.
The G.P. is well placed to manage the problem, compared to hospital doctors who are unable to establish any long-term relationship or solution.
B.M.I. (Body Mass Index) –is the normal measurement process to determine obesity; in addition Doctors should incorporate an additional and simple objective measure of waist/hip ratio when evaluating the patient’s condition and treatment.
Obesity in Children is Endemic in urban society, which results in the need to change national diet.
Experience shows the best results involve family members who must monitor and support the child in the treatment programme.
The National Obesity Forum is against the use of medicines except as a very last resort.
European Union law states that patients cannot be treated with drugs until their body mass index (BMI) is 30kg/m2 unless there are other reasons such as diabetes, high blood pressure or high cholesterol when treatment can start at BMI 27. As obese patients are showing the consequences of obesity they should be started on treatment at BMI 27, not 30, and the Primary Care Trust should make a special effort to treat this group urgently.
Professor M. Lean, Human Nutrition Faculty of Medicine at the University of Glasgow, stated in the BMJ 2008; 337:2408 that only drugs, diet, exercise and bariatric surgery aid will lead to permanent weight loss.
O.M.A. believes that in certain cases medicines should be included in the first line of treatment, together with diet and exercise programmes. It also believes that obesity can be overcome on a Doctor to patient basis with regular appointments and excellent close supervision of the patient.
Examination of the availability of weight management and other intervention services to take obesity-related ill health and to consider further action.
General Practitioners are normally the first clinical professionals to diagnose obese patients. As obesity affects 25% of the population and budgets are constantly squeezed, they are often reluctant to begin treatment of their patients with drugs. Instead they give the patients diet sheets, tell them to exercise, think about lifestyle changes, educate themselves and invariably none of these recommendations work.
O.M.A. believes the scope of the current UK Government approach is limited because:
- It depends upon the patient to make lifestyle changes which he / she does not wish and in many cases is unable to implement.
- Obesity is at its highest levels occurs within the socio-economic groups c3 – DE.
- Special diets are too expensive for the average family household.
- Exercise is not an option for many patients.
- Non-invasive clinical intervention (drug treatments) is left until a patient has a reached a BMI 30 level, by which time the patient become clinically obese and to achieve a natural BMI of say 23 is not only difficult but in most cases impossible.
- Clinical treatments should start earlier – by the time a patient has a BMI of 30, it is no longer a case of prevention – but weight management and control.
- Patient motivation is ignored. Motivation is essential in all weight management programmes – in order to keep patients motivated they require achievable goals which produce acceptable results.
- There are no clinical treatments for children.
- Places for obese children to exercise in groups are not readily available.
- Philosophy varies from Primary Care Trust to Primary Care Trust.
- Infrequent supervision of adult treatment does not allow proper engagement with, or management of, any worthwhile or sustainable weight management programme to keep the patient encouraged.
- Central Government anti-obesity - Health campaigns are useful but not effective.
- Reliance on food manufacturers and commercial fitness centres will not resolve the issue of ever increasing obesity patients.
- Work with OMA registered clinics.
Consider what further action is required
We understand the UK Government now recognises and accepts the NHS unable to deal with the size of the problem due to lack of services and increasing co-morbidity costs.
A programme of pro-active and preventative action is required which includes;
- Treat patients as individuals not statistics.
- Earlier medical intervention to be considered.
- Challenge both clinical and drug therapy guidelines.
- NHS Doctors to be encouraged to refer overweight/obese patients to Private Clinics.
- Treat Child obesity within the family.
- Explain and demonstrate healthy eating.
- Encourage societal participation in exercise.
- Not in all cases – earlier medical intervention within a controlled clinical environment should be adopted as parallel programmes between the NHS and private health sectors.
- Establish external groups from all sectors treating obesity to prepare a series of detailed recommendations to the Northern Ireland Assembly.
Appendix
Statement by the Scottish Government on its actions in dealing with its Obesity priority
What is the nature and extent of the Scottish Government’s action on this priority?
The Scottish Government has a twin approach to tackling unhealthy weight through an integrated implementation of our national Physical Activity Strategy ‘Let’s Make Scotland More Active’ and ‘Eating for Health: A Diet Action Plan for Scotland’. Additional measures in schools will be secured through the Schools (Nutrition and Health Promotion) Act 2007. We plan to publish an action programme covering healthy eating, physical activity and healthy weight in spring 2008. This will build on, rather than replace, existing delivery of the Physical Activity Strategy and Diet Action Plan. The strategic spending review 2007 has committed an additional £40 million over the next three years to delivering in these three interlinked policy areas.
LighterLife (UK) Ltd
Introduction
LighterLife welcomes the opportunity to submit written evidence to the Assembly Health Committee inquiry into obesity. We acknowledge that the factors that lead to obesity are multiple (as outlined by Foresight in Tackling Obesities: Future Choices, 2007). However, our comments will focus on the sector in which we are operating – that of community-based adult weight management services and in particular the use of very low calorie and low calorie diets.
LighterLife – Who we are
LighterLife, founded in 1996, is a successful weight loss and weight management company. As well as the CEO and the Board of Directors, LighterLife benefits from the clinical input of an independent Medical Advisory Board. Our Chief Medical Officer is Professor Iain Broom, consultant in clinical biochemistry and metabolic science at Grampian University Hospitals NHS Trust.
LighterLife central office is based in Harlow in Essex. We have a network of over 280 EdExcel-accredited weight-management counsellors who operate across all four countries of the UK and the Republic of Ireland. Weight-management counsellors run single sex groups which typically have up to 12 patients. We have worked with over 100,000 patients.
Our programmes – What we do
The LighterLife Programme
The LighterLife Programme has been developed with two main components:
- Nutritionally complete Foodpacks which are used in place of conventional food; and
- Techniques from cognitive behavioural therapy (CBT) and transactional analysis (TA) delivered by Edexcel-accredited weight management counsellors
using a Very Low Calorie Diet (VLCD) for people who are obese (a typical VLCD patient comes to us with a BMI of 37).
The LighterLife Programme complies with COMA and NICE guidance. Alongside the Foodpacks, LighterLife provides behavioural therapy (cognitive behavioural therapy and transactional analysis techniques) specifically developed for the treatment of overweight and obesity to address the issues behind patients’ eating and levels of physical activity and the strategies they can put in place to prevent them putting on weight in the future.
The therapeutic package and the materials that accompany it are an important part of the LighterLife Programme – and are supported by evidence that patients are more likely to lose weight and maintain that weight loss if they do so as part of a group and have support.
LighterLife Lite
In November 2008, we introduced LighterLife Lite, a Low Calorie Diet (LCD) for patients who have a BMI from 25 to 29.9. This uses the same approach as the VLCD, except that instead of four Foodpacks, patients have three nutritionally balanced Foodpacks and one conventional meal a day.
What are the issues?
The key issues in tackling obesity
Obesity has become a major public health epidemic. In Northern Ireland 60% of adults have a weight problem and as many as 1 in 5 are obese. Prevalence of obesity is increasing at such a rate that on current trends it will surpass smoking as the greatest cause of premature loss of life. Obesity is associated and linked to many physical and psychological health problems, including coronary heart disease, diabetes, kidney failure, osteoarthritis, back pain, cancer and hypertension. Psychologically, people who are overweight or obese have lower self-esteem, higher levels of depression and increased rates of isolation.
Despite this, the response remains patchy and there is no coherent approach to tackling the causes of overweight and obesity and preventing the rise in overweight and obesity in order to reduce the number of people who are overweight and obese.
There is a need to have a good and clear understanding of the geographic prevalence of overweight and obesity and to understand its causes. Once these are established, it is important to ensure that action to tackle obesity is targeted at all ages, all communities and coordinated across all sectors.
We know that:
- it would be impossible for those who are overweight and obese to devote the amount of time they would need to physical activity to reduce their weight to the level they need to – without also undertaking a significant change in eating patterns
- overweight and obesity increase with age
- the number of obese men is fast approaching the number of obese women
- obesity and morbid obesity are particularly common in lower socio-economic groups, particularly among women
- all female minority ethnic groups have levels of central obesity above that of the general female population.
The health service response to date – what is working well
We welcome the way in which Governments have made a commitment to tackle the causes of overweight and obesity and to help those who are overweight and obese to lose weight.
We are encouraged by moves that some parts of the health sector have made to work with the commercial sector and to use its expertise. However, we believe that there is scope to develop this relationship further and to increase the number of private sector providers working in partnership with the NHS.
The evidence base and policy framework identifies that solutions need to be multi-pronged and need to focus on:
- The environment and economic and social factors;
- The encouragement of a healthy lifestyle incorporating healthy eating and physical activity (primary prevention);
- The focus on interventions to address the needs of those who are overweight and obese (secondary prevention).
The traditional weight reduction pathway identifies four levels of intervention:
1. Primary prevention;
2. Commercial weight management services in the community;
3. Specialist obesity services in hospital; and
4. Morbid obesity services in hospital.
Primary prevention has been at the front of practitioners’ minds and there does not appear to have developed a clear patient pathway for those for whom general advice on healthy eating and physical activity are not working.
As primary care practitioners and patients become more aware of the risks associated with obesity, there is a need to ensure that they have the expertise they need to deliver primary prevention and at the same time to recognise that it may not work for all target groups. In these cases, there is a need to identify what options in secondary prevention are available.
The health service response to date – what can be improved
Whilst there has been an increase in activity in relation to primary prevention, drug therapies and bariatrics, there is an opportunity further to develop work on the use of the commercial weight management services in the community, particularly in relation to patients who are obese. There is scope to be more receptive to different approaches in any review Northern Ireland is making of its overweight and obesity services.
At a national level, there is a need to acknowledge the part community based interventions can play in combating overweight and obesity. This may be encouraged through the:
- provision of suitable information to patients directly
- production of specific guidance on different interventions (including LCDs and VLCDs)
- production of specific guidance on which services to purchase and how to tender for them
- introduction of local targets to reduce the levels of overweight and obesity prevalence in adults
- guidance on local budget setting in order to ensure that overweight and obesity services are purchased.
What the health service needs to do next (DHSSPS and Health Boards)
Given the extent of the problem and the predicted costs to the health service (and the rest of society) which will result from inaction, there is a need for the health service to expand its service provision and to revisit the traditional weight reduction pathway. Despite the development of pharmacological and surgical treatments, dietetic treatment is still the basic therapeutic tool against obesity (Ayyad, Andersen 2000).
The current weight reduction pathway implies that the boundary between service provision in the community and in hospital is drawn at the stage when a person moves from being overweight to obese. In other words, health care purchasers are being asked to:
- provide services or to buy commercial weight management services in the community for people who are overweight; and
- provide services or to buy commercial weight management services in hospitals and not in the community for patients who are obese.
There is a need to revisit this, not least because of the numbers of people who are overweight and obese and the costs of providing interventions for all of them in clinical settings. We do not think that it would be possible to provide weight management services to everyone who is obese and could benefit in a hospital setting (whether in the private or public sectors or both). There is also a need to recognise that VLCDs and LCDs are effective tools in weight reduction.
LighterLife believes that there is a strong case for ensuring that guidance provided by the Health Boards is comprehensive and looks at a wide range of ways in which overweight and obese patients can be treated in the community by a range of providers.
As noted in ‘Our Programmes’ (above) LighterLife is a leading provider of overweight and obesity management services in the community. The LighterLife Programme is clinically supervised and combines a VLCD with techniques from cognitive behavioural therapy (CBT) and transactional analysis (TA).
VLCDs enable patients who are overweight and obese to lose weight in a way that is safe and effective. It is recognised that for obese patients the rate of weight loss can be rapid at the outset (on average women lose 1 stone per month and men 1.5 stones). This initial weight loss can be an important motivator for patients to continue to lose weight. Over the longer term VLCDs offer a sustainable weight loss of, on average, 0.5 – 1kg per week.
The Route to Management Programme which follows the weight loss phase enables patients to successfully manage their weight in the future. Both our VLCD and recently launched LCD offer patients the opportunity to address the issues surrounding their overeating in the absence of all (or in the case of LighterLife Lite, most) conventional foods.
Working with the commercial sector – training needs
It is important to provide clear guidance and training for health professionals on how they can work with the commercial sector and how this needs to be considered as a necessary addition to current service provision.
This guidance needs to identify the range of providers and ensure that they are considered in the creation of:
- a patient pathway; and
- a new weight reduction pathway.
It also needs to take account of the growing number of overweight and obese adults and the growing number and variety of weight management services (including VLCDs and LCDs) and the need to tailor approaches both in hospital and community settings that are going to be effective.
Need for more research to demonstrate the effectiveness of different interventions – a national need
The research in the field of obesity is vast. However, there is little research to identify the pros and cons of different community-based weight-management programmes and their success relative to that of, say, drug therapies and bariatrics in the medium to long term. This and associated areas (including training needs) are covered in detail in the NICE guidance (2006).
Conclusion
We are encouraged by this inquiry and the scope to identify a plan of action which will tackle the obesity epidemic. We believe that in order for this to be as effective as possible, there is a need for agencies in the public sector to work together and to coordinate action.
There is also a need to ensure that the mechanisms are developed for the local delivery of services across agencies, including the health sector, and that those managing the delivery of services have the expertise needed to identify the most suitable intervention for particular patients.
In the health sector specifically, there is a need at a national level, to recognise the variety of programmes available in the commercial sector and to acknowledge the contribution they can make.
The Northern Ireland Commissioner
for Children and Young People
1.0 Introduction
The Office of Commissioner for Children and Young People (NICCY) was created in accordance with The Commissioner for Children and Young People (Northern Ireland) Order (2003) to safeguard and promote the rights and best interests of children and young people in Northern Ireland.[1]
Under Articles 7(2)(3) of this legislation, NICCY has a mandate to keep under review the adequacy and effectiveness of law, practice and services relating to the rights and best interests of children and young people by relevant authorities. The remit of our Office is children and young people from birth up to18 years, or 21 years of age if the young person is disabled or in the care of Social Services.
In determining how to carry out her functions, the Commissioner’s paramount consideration is the rights of the child and NICCY is required to base all its work on the United Nations Convention on the Rights of the Child (UNCRC).[2]
2.0 Assess the scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change
As highlighted by the Chief Medical Officer[3] in his annual report in 2007, “one in four girls and one in six boys in primary one are overweight or obese".
According to a press statement[4] from the Minister of Health “Figures from 2006/07 show that approximately 22% of Northern Ireland’s Primary school children are classed as overweight and obese".
The increasing number of children and young people in Northern Ireland who are obese illustrates that current approach to the prevention of obesity is not effective.
2.1 Barriers identified in the Review of Children Rights
‘Children’s Rights: Rhetoric or Reality, A review of Children’s Rights in Northern Ireland’[5] by NICCY launched on 17 February 2009 highlights just some of the difficulties that children and their parents face when attempting to lead healthy lives, these include;
- The cost of providing a healthy diet;
- Impact of marketing unhealthy food on children’s preferences and food choices;
- Inadequate education around healthy lifestyles, which impacts on children’s preferences and choices
- Barriers in access to play and leisure activities and facilities;
These factors all have an impact on a parent’s ability to provide their child with a healthy diet and promote an active lifestyle. The review highlights that many of the initiatives such as healthy schools pilots and sure start healthy start vouchers are discrete initiatives and are not available in all schools or communities. While these initiatives are having a positive impact on some communities they need to be available across all of Northern Ireland.
2.2 Ten year strategy for children and young people
The ten year strategy for children and young people ‘Our children and young people - our pledge’ makes direct reference to the increasing rates of child hood obesity. This strategy contains a target to halt the increase of childhood obesity by 2010; the driver for change on this target is the Fit Futures Implementation Plan. Given that this target needs to be met by next year, the committee will need to closely monitor the implementation of Fit Futures to ensure that the appropriate actions are put into place.
2.3 Fit Futures Implementation Plan
A draft plan was put out to public consultation at the start of 2007, however to date no information is available on the Department of Health, Social Services and Public Safety (DHSSPS) website as to the status of the implementation plan. Many of the actions outlined in this draft implementation plan have a direct impact on the health of children, including play and recreation, early years, advertising and promotion of food to children and healthy schools. If these actions are fully implemented it will have a positive effect on the health and wellbeing of children, in particular the levels of child hood obesity.
It is essential that DHSSPS prioritise the actions from this implementation plan; it needs to be monitored and evaluated to ensure that it is having a positive impact on the levels of childhood obesity.
3.0 Examine the availability of weight management or other intervention services to tackle obesity related ill health
In his annual report the Chief Medical Officer made reference to a programme ‘Fit Families’ developed by the Northern Investing for Health Partnership. This programme works with families to improve diets and physical activity. However this programme is only available in the Northern Board. Investing for Health Partnerships are carrying out excellent work in the community, but where an evaluation shows the positive impacts of a programme such as this, efforts should be made to replicate the programme across Northern Ireland.
In ‘Children’s Rights: Rhetoric or Reality, A review of Children’s Rights in Northern Ireland’ children and young people in some schools told us about ‘walk to school’ initiatives which aimed to get children and their parents walking to school as an alternative to car or bus journeys. These initiatives should be promoted and supported by DE and further developed so that all schools promote walking and cycling to school.
The implementation of the Department of Education (DE) guidance ‘New nutritional standards for school lunches and other food in schools’ is welcomed as it will have a positive impact on children receiving school meals, in particular on children who are in receipt of free school meals.
4.0 Consider what further action is required, taking account, as appropriate, of the potential to learn from experiences elsewhere
While NICCY appreciates that the remit of the Committee is Health, Social Services and Public Safety, we believe that many strategies from other government departments have a significant impact on obesity and therefore recommendations of this inquiry will be the responsibility of other departments. It is essential that the committee clearly notify other departments of their responsibilities, and liaises with them in tackling this important issue.
As highlighted in the Fit Futures report the focus of tackling obesity needs to be on early years, when attitudes towards food and physical activity are formed. The report highlighted that without significant intervention over 1 in 4 (27%) 4.5 to 5.5 yr olds will be overweight or obese by 2010[6] therefore we recommend that action needs to be focused on educating children and young people, and supporting their parents to enable them to live healthy lifestyles.
4.1 Play
While we recognise that the provision of play and leisure is not within the remit of the HSSPS Committee, it is central to tackling childhood obesity. A report from the Northern Ireland Audit Office[7] illustrates that children are not as physically active as they should be, with activity declining with age. Inherent to the ability of children to live active lifestyles is their access to play and leisure and activities.
The NICCY review of children’s rights shows that children and young people face multiple barriers when attempting to lead healthy life styles through active play. In particular they can not find safe, affordable, accessible and age appropriate play and leisure activities. This is having a profound impact on the ability of children and young people to stay active and healthy.
The Northern Ireland Play Policy was approved by the Northern Ireland Executive in December 2008. The next step involves the development of two implementation plans, one for 0 -11year olds and one for 12 - 18year olds. OFMDFM must develop and implement these plans as soon as possible, allocating appropriate funding to ensure that the actions can be implemented.
Research completed by NICCY to be published later this year shows that out of 21 councils who responded to their questionnaire, only ten Councils had a play policy. This research recommends that all Councils should develop a play policy, as part of their statutory duty to develop and maintain play and recreation facilities. In advance of the changes to Local Councils through the Review of Public Administrations, the Department of the Environment should be working cooperatively with OFMDFM to prepare the new larger Councils to meet their duties relating to the delivery of play and recreation.
The draft Northern Ireland Strategy for Sport and Physical Recreation was published by the Department of Culture, Arts and Leisure (DCAL) last year for consultation. This draft strategy contains targets to increase the participation of children and young people in sport and recreational activities. This strategy is comprehensive and if implemented in full would provide increased opportunities for children and young people to participate in quality sport and physical recreation across a range of settings but mainly through schools and community based activities. As highlighted in our response to the consultation on this draft strategy, the costs of sport and recreation may be a barrier to the participation of some children; this was not adequately addressed in the strategy. In order for children and young people to participate fully in sport, it must be both accessible and affordable.
The draft strategy was subject to consultation in late 2007 and to date it has not been finalised nor has it been implemented. DCAL must allocate appropriate funding to the all actions to ensure the full strategy can be implemented in full.
4.3 Impact of poverty on obesity
In their report to the UN Committee on the Rights of the Child, the four UK Children’s Commissioners highlighted the impact poverty has on the increasing rates of childhood obesity.
“Improving the diet of children born into poorer families is more difficult due to inadequate income and restricted access to healthy food. We are also concerned about the growth in marketing to children, explicitly encouraging the consumption of unhealthy food products. In areas of socio-economic deprivation, opportunities to exercise are more likely to be limited; for example, there may be nowhere safe to play, no facilities for physical activities outside school, and a shortage of money to participate in such activities.[8]
The Institute of Public Health in Ireland report ‘Tackling Food Poverty: Lessons from the Decent Food for All Intervention’ details the impact that food poverty has on obesity[9]. This report from IPH shows that children living in poor household are more likely to adopt unhealthy behaviours in early life; this is due to poor information and skills; poor access to physical activities and poor finances.
Lifetime Opportunities, the Government’s anti poverty and social inclusion strategy is the policy framework to reduce poverty. In addition to this the Committee for First Minister and deputy First Minister carried out an Inquiry into Child Poverty in Northern Ireland. The actions from both reports need to be implemented without delay to ensure that parents on low incomes have adequate support to help them provide their children with a healthy diet and lifestyle.
However, the committee needs also to recognise that, while poverty impacts on children’s nutrition and health, it doesn’t always result in obesity, other evidence shows that food poverty can result in children being smaller in weight.
4.4 School Transport
In 2005, NICCY commissioned research into the views of children and young people, parents and carers and other interested parties on issues affecting safe travel to school. We launched a report ‘Safer Journey to Schools’[10] into the findings of this research in 2006. This recommended that the Department of Education reviews the current statutory walking distances for home to school transport, to identify the impact that changes could have on school transport provision.
The research made a number of recommendations to reduce car based journeys, including;
- Implementation of more safer routes to school initiatives and school safety zones
- Schools should map routes which children take to and from school to identify possible problems that they might encounter
- Safer routes projects should include a variety of traffic calming measures
- Prohibiting parking at school gates to address traffic congestion
- Schools should develop travel plans for pupils which includes traffic calming measures and walking to school initiatives
In order to reduce car based journeys to school, investment is needed to further develop and improve walking and cycle routes to make this a more attractive and safer alternative.
A part of increasing walking/cycling to school will require the Department of Education to ensure that road safety continues to be included in the curriculum of both primary and secondary schools, with an assessment of the impact of this awareness programme in schools.
5.0 Conclusion
As statistics in section 2.0 highlight Obesity is clearly a significant health issue for children in Northern Ireland. While the Department for HSSPS must take a lead in implementing measures to tackle childhood obesity, other departments have an important role in implementing other strategies and policies that have an impact on the ability of children and young people to lead healthy and active lifestyles.
A number of discrete initiatives have been introduced across Northern Ireland to tackle childhood obesity; these initiatives have been developed by Investing for Health Partnerships, Health Promotion Agencies and individual Health and Social Care Trusts, however they are specific to one geographical area and usually funded on a short term basis. The initiatives which are having a positive impact on the rate of childhood obesity need to be supported by a comprehensive policy framework.
The Implementation of Fit Futures is central to tackling childhood obesity. DHSSPS need to make appropriate funding available to ensure all the actions of Fit Futures are fully implemented.
[1] Further information on the role and remit of the commissioner can be accessed at www.niccy.org
[2] The following articles of the UNCRC have a particular relevance to this inquiry:
Article 17- the right of children to access information and materials from a range of sources, especially those aimed at the promotion of their physical health and wellbeing
Article 24- the right to highest standard of health care, this includes education on and are supported in child health and nutrition
Article 27- the right of the child to adequate standards of living, with a onus on the state to provide measures to assist parents materially and through support programmes, particularly with regard to nutrition.
Article 31- the right of the child to rest and leisure and to engage in play and recreation activities.
[3] http://www.dhsspsni.gov.uk/cmo-annual-report-2007.pdf (access at 3rd February 2009)
[4] http://www.northernireland.gov.uk/news/news-dhssps/news-dhssps-131108 obesity_time_bomb.htm
[5] Copies of this report can be sent to committee members on or after 17th February 2009 on request.
[6] Department of Health, Social Services and Public Safety (2007d) Fit Futures: Focus on Food, Activity and Young People: Response from the Ministerial Group on Public Health including Consultation on Fit Futures Implementation Plan 2007.Belfast: DHSSPS
[7] http://www.niauditoffice.gov.uk/pubs/obesity/8100_Obesity_Diabetes.pdf (accessed at 3rd February 2009)
[8] UK Commissioners report to the UN Committee on the Rights of the Child
[9] http://www.publichealth.ie/files/file/Tackling_Food_Poverty_lessons_from_the_DFfA_intervention.pdf
[10] Research can be accessed at www.niccy.org
Centre for Obesity
Research and Epidemiology
In the Western world today, individuals who are underweight are vastly outnumbered by those who are overweight and obese. Almost one quarter of adults in the UK1, 2 and a third in the USA3 are obese and there is consistent evidence that the obese will continue to gain weight over time if not offered intervention.4 Obesity is a major public health risk, presenting a burden of obesity-related disease5, impaired quality of life6 and implications for medical care expenditure.7
The dual metabolic challenge of unlimited access to palatable food and greatly diminished physical activity both have a key role to play in explaining such disappointing statistics. The solution is necessarily multi-dimensional, and individuals exhibit different susceptibility according to genetic variation in control mechanisms which affect eating behaviour. Individuals are also variable in their capacity to respond to treatment by altering their behaviour.
Obesity is one of the most important and preventable causes of morbidity and mortality facing primary care today. However, the obese attend General Practice frequently8 and have additional prescribing compared to age and sex matched normal weight controls.9 Primary care prescribing costs increase steadily from £50.71 for men, £62.59 for women at BMI 20 kg/m2 to £198.66 for men, and £160.73 for women at BMI 40kg/m2 10
While the burden of obesity on NHS resource is well documented, there is a need to focus on what can be achieved from realistic weight loss from health and NHS resource perspectives. Consideration must turn to cost avoidance. Patients, General Practitioners and healthcare providers have held over-ambitious expectations for weight management which go beyond what is achievable, affordable or medically valuable. Research has demonstrated enormous medical gains11,12,13 and significant cost-avoidance from modest, and achievable, weight loss (5-10%) and more from long term avoidance of weight gain. Such expectations need to be addressed and refocused.
Despite clinical guidelines for obesity management14, 15 and related disease16, there is little evidence that obesity can be managed successfully in a primary care setting. Many weight management solutions offered to primary care lack evaluation and others have proven unsuccessful. Isolated weight management training events for primary care practitioners have been unable to demonstrate patient weight loss.17
Costs rise disproportionately with the disease progression10, and strategies which offer a modest reduction in body weight, may offer a more favourable health economic profile. The strategy which stands the greatest chance of success needs to be evidence based, culturally sensitive and locally delivered. It must address the range of levels of obesity, but focus on the majority of obese people, for whom a modest weight reduction can offer not only realistic targets, but tangible health benefits.
The Counterweight Programme was set up in 1999 to evaluate a structured model based on established weight management interventions using theoretical and evidence-based approaches, and to assess the feasibility of primary care as an appropriate setting.18 It is a novel approach which draws on theory and evidence relating to changing behaviours of health professionals and patients.19
Counterweight is based on a model of continuous improvement with closed-loop audit enabling on-going programme evaluation and refinement. An initial evaluation phase was conducted 2000-2005, demonstrating that if practice nurses are provided with training on a structured programme18, are mentored within clinical practice19 and results are continuously audited, they can achieve and maintain clinically beneficial weight loss in their obese patients.20 Mean weight loss in patients who attended the Counterweight Programme was 3.0 kg and 2.3 kg at one and two years, respectively. Weight loss of this nature results in multiple clinical benefits and loss of 5-10% has been previously shown to reduce progression to diabetes by up to 58% over 4yrs.11, 12
Counterweight Health economic analysis demonstrated that the cost of delivering the programme across the UK would be approximately £60 per patient entered and that prescribing costs should theoretically reduce by £6.35 per male patient and £3.50 per female patient over the first year alone (assuming the population has similar baseline BMI as in Counterweight (BMI 37 kg/m2)).10
Weight management advisers (WMA), all registered dietitians (or clinical nutritionists) facilitate programme implementation. They offer expertise in obesity management and provided protocols and training materials for staff. One hour of training is provided for GPs and a 12-hour training programme is provided for practice nurses (PN). Mentoring in practice is provided until practice nurses reach competency and confidence is achieved. The PN role is to deliver patient education through discussion about weight management, communication of information, and the transfer of “behaviour change" skills during weight management sessions.
The Counterweight intervention focuses on adults aged 18–75 years with a BMI over 30 kg/m2 or 28 kg/m2 with associated co-morbidity. The nurse-led intervention is delivered within a group or one-to-one setting in a general practice. The programme has also been implemented at a small level in a community and pharmacy setting. Intervention consists of six sessions over three months followed by quarterly follow-up to 12 months with annual review recommended thereafter.
Lifestyle interventions are a goal-setting approach, a structured prescribed eating plan or a group programme, all based on creating a 500 kcal daily energy deficit.
Goal setting involves the PN and patient working together to mutually agree goals for dietary and lifestyle change. Practice nurses are coached in the skills of negotiating goals to change lifestyle, as collaborative goal setting has been found to be more effective in weight management than health professional selected goals. The prescribed eating plan (PEP) is an individualised food portion plan with approximately 30% energy from fat.
The group programme is based on six one hour sessions run bi-weekly for a three month period. Sessions include discussions on weight loss targets, healthy eating, shopping, cooking, eating out, physical activity and relapse prevention. Each group aims to recruit 10-15 participants and sessions are based around the principles of adult learning, designed to encourage group interaction and active learning. Session plans, and teaching materials are provided to practices and the WMA typically facilitates the first patient group over three months with the PN observing. Following this the PN is encouraged to take responsibility for facilitating the group.
After 12 weeks of lifestyle intervention pharmacotherapy is considered where appropriate. The Counterweight model follows evidence-based guidelines and prescribing is usually led by local protocol.
In 2006, Counterweight was commissioned by the Scottish Government as the weight management option for the Keep Well Programme, an anticipatory care programme for the prevention of cardiovascular disease in areas of high deprivation in Scotland. In 2008 the programme was expanded and offered to each health board by the government. In England, the Counterweight Programme is commissioned by individual primary care trusts and the programme has undergone a smaller but steady expansion.
The Counterweight team have developed significant expertise in expanding the programme into new regions. The team offers support with practical facilitation of local implementation plan for Counterweight, identification of the preferred model of delivery according to local needs, protocols for data collection and ongoing programme evaluation, joint working with local stakeholders, and training of a local dietitian (Counterweight buddy) to continue expanding the programme in each area after the initial implementation phase.
An effective obesity strategy requires many interdependent strands, preventing the overweight becoming obese, and preventing disease progression in those who already are obese. Such a strategy needs to be evidence-based, delivering a service for patients which will dovetail with other public health campaigns and initiatives, and target resources where they have been shown to make a real difference. The Counterweight programme is currently the only primary care programme demonstrating clinically valuable weight change outcomes.20
The Counterweight Project Team includes eight leading obesity UK NHS physicians, as well as a team of 14 registered dietitians/nutritionists with more than 10 years experience in the field. Outcomes from the Counterweight programme have been published in peer review journals and presented internationally. Implementation of the Counterweight Programme in Northern Ireland will require funding for the Counterweight team, evaluation costs, local incentives for general practice and some commitment from dietitians, but offers a workable solution for the management of obesity, which is realistic, evidence-based, and effective in a similar setting.
References
1. Department of Health. Health Survey for England 2004.London: Health and Social Care Information Centre, 2005
2. Scottish Health Survey – 2003 results. See http://www.scotland.gov.uk/publications/2005/11/25145024/50251
3. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295:1549–55
4. Heitman BL, Garby L. Patterns of long-term weight changes in overweight developing Danish men and women aged between 30 and 60 years. Int J Obes Relat Metab Disord 1999;23:1074–8.
5. Must A, Spadano J, Coakley E, Field A, Colditz G, Dietz W. The disease burden associated with obesity. JAMA.1999;282:1523-1529.
6. Lean ME, Han TS, Seidell JC. Impairment of health and quality of life using new US federal guidelines for the identification of obesity. Arch Intern Med. 1999; 159: 837-843.
7. National Audit Office: Tackling Obesity in England. Report by the Controller and Auditor General. London. 2001
8. Counterweight Project Team. The influence of body mass index on number of visits to general practitioners in the UK. Obes Res. 2005; 13: 1442-1449.
9. Counterweight Project Team. Impact of obesity on drug prescribing in primary care. British J Gen Pract. 2005; 55: 743-749.
10. The Counterweight Project Team. Influence of body mass index on prescribing costs and potential cost savings of a weight management programme in primary care. J Health Serv Res Policy 2008; 13 No 3: 158-166.
11. Diabetes Prevention Programme Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. NEJM. 2002; 346: 393-403.
12. Tuomilehto J, Lindstrom J, Eriksson J, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. NEJM. 2001; 344: 1343-1349.
13. National Heart, Lung and Blood Institute. The Practical Guide. Identification, Evaluation and Treatment of Overweight and Obesity in Adults. Nat Inst Health; USA.1998.
14. HTA 2004 Broom J, Avenell A, Aucott L, Brown TJ, Poobalan A, Stearns S, Smith WCS, Jung R, Campbell MK, Malek M, Grant AM. Systematic Review of the Long Term Outcomes of the Treatments for Obesity and Implication for Health Improvement and the Economic Consequences for the National Health Service (2004).
15. Health Development Agency. The management of obesity and overweight: an analysis of reviews of diet, physical activity and behavioural approaches. H.D.A. 2003.
16. Joint British Societies’ Second Report (JBS2): Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005; 91: (Suppl V): v1-v52.
17. Moore H, Summerbell CD, Greenwood DC, et al. Improving the management of obesity in primary care: cluster randomised trial. BMJ. 2003; 327: 1085-1088.
18. Counterweight Project Team. A new evidence-based model for weight management in primary care: The Counterweight Programme. J Hum Nutr & Dietet 2004; 17: 191-208.
19. Counterweight Project Team. Empowering primary care to tackle the obesity epidemic: The Counterweight Programme. Eur J Clin Nutr 2005; 59 (1): S93-101.
20. Counterweight Project Team. Evaluation of the Counterweight Programme for obesity management in primary care: a starting point for continuous improvement. Br J Gen Pract 2008; 58: 548-554.
Banbridge District Council
The followings outlines the steps that Banbridge District Council is taking in relation to the issue of obesity and its prevention.
Work with Food Businesses
EHOs have been involved in promoting the Food Standards Agency’s ‘traffic light scheme’ in food manufacturers in this area and are willing to work with them on other emerging initiatives such as their saturated fat and salt campaigns.
Appointment of Dietitian Specialist
A Dietitian Specialist has been employed with Southern Group Environmental Health Committee (SGEHC) for the period April 2008 - end March 2011, to work with Council EHOs and local food businesses on improving the nutritional quality of food sold from catering outlets. This does not include premises where nutritional standards already exist, for example schools, nursing homes, etc. The initiative is known as CHOICE (Choosing Healthier Options in Catering Establishments).
Between April 2008 and March 2011 the Dietitian Specialist will also be working alongside a Community Project Officer, who will be working on a community based initiative to improve the diet and nutrition among communities in the Southern group area. Both of these positions have been part funded by the SHSSB.
Community Nutrition Project
2 of our Environmental Health Officers have completed a Diploma in Nutrition, part funded by FSANI. This will assist them in delivery of the CHOICE initiative in this area and also enhance involvement in other forthcoming initiatives which the FSANI are keen to develop e.g. ‘Grubs Up’. Council may also provide nutrition training for local food business operators.
The Overweight and Obesity Prevention Group
The Principal EHO (Food Control/ Infectious Diseases/ Health Promotion) at SGEHC is a member of the SHSSB Overweight and Obesity Prevention Group. This group concentrates on initiatives to follow up on the Fit Futures report.
Investing for Health Joint Appointments
In 2003 joint appointments of three Investing for Health Officers were made in the Southern Group area, jointly funded by the District Councils and SHSSB. Part of their remit within the Southern Investing for Health Partnership is to tackle obesity as per the original Investing for Health Strategy.
Joint appointments of Health Improvement Workers
In 2009 three Health Improvement Workers will be appointed to work across the five Southern Group Councils and one of their key health improvement objectives is nutrition and the promotion of healthy eating in areas of social deprivation.
SHSSB Cook It programme Steering Group
SGEHC were involved in the steering group and hope to be involved with the new proposed Community Cooking programmes currently being set up by the SHSSB.
CEHOG Nutrition Sub-group
The Northern Ireland Food Liaison Group, a subgroup of the Chief Environmental Health Officers’ Group, is to convene a nutrition subgroup to look at how best EHOs can become involved in tackling the obesity issue in the general population and also to share ideas and initiatives that may be happening elsewhere in NI and the rest of the UK, etc. This group will also have membership from FSANI.
Recommendations for the future
- The Fit Futures report should be fully implemented.
- A NI strategy to tackle adult obesity should be drafted and implemented a soon as possible.
- A scoping exercise of existing good practice should be shared with all relevant agencies and central and local Government Departments.
- Central Government should fund the expansion of successful initiatives such as the ‘Cook It’ programme.
- Cooking skills should be made a mandatory part of the School curriculum.
- The FSANI should continue to work in partnership with the food industry and EHOs to improve nutritional quality of foods available for sale.
- Healthy Eating awards should be available to food business operators in NI.
- Social marketing tools should be used in a marketing campaign among parents of young children and the general population to increase awareness on health related issues caused by obesity.
- Accessibility by young people to the ‘wrong’ foods should be addressed at a regional level involving a number of partners, including the food industry.
Western Health and
Social Services Board
There are a number of key strategic documents that directly impact on the battle of obesity. They are the Investing for Health Strategy, Physical Activity Strategy and Fit Futures. In addition, you will be aware that there were plans to have a Diet & Nutrition Strategy and also a Life Changes Strategy to focus on obesity in adults. There are a number of other strategies that are led by other agencies and departments, which also contribute to opportunities to tackle the rise of obesity. These include strategies around sport, recreation and leisure and tourism, as well as regional development in respect of cycleways, walking paths and community safety.
In order to take a more strategic approach in the West, the Board has established the Western Obesity Prevention Group, which includes representatives from the five Councils, DOE Planning, Health & Social Care and the Community and Voluntary Sector. This group reviews activities within the West, but also feeds directly into the work that is being taken forward at a regional level through the group being led by the Chief Medical Officer.
A significant amount of work has been done in terms of developing priorities, based on research and consultation with stakeholders. The key areas that this Board is moving forward are:
- Developing joined-up public health and policy;
- Providing real choice;
- Supporting healthy early years;
- Creating healthy schools;
- Encouraging the development of healthy communities;
- Building the evidence-base.
It is acknowledged that there is a need for better collaboration around issues such as health policy, food policy and physical activity policy, to ensure that there is clarification in terms of the messages we are trying to get out to the wider population. Within this there is a particular key role for Local Authorities to take a leadership role in collaboration with professionals from Health & Social Care. This work is well placed to move forward within the Investing for Health Partnerships, which are already in place and are taking forward a range of initiatives.
There is a challenge in providing opportunities and access to real choice, particularly for those from disadvantaged communities, with a particular emphasis on children. There are initiatives in place addressing lifestyle and environmental issues and ensuring that information being fed out through the media is understood by the wider population. There is a wider issue around the role of the local food industry, and in particular around nutritional labelling, which still needs further work.
Early intervention is vital and this can be taken forward from breastfeeding through to education establishments. There are real opportunities where we can create healthier schools, but it is important that within the schools’ development plan, there is a clear mandatory requirement that schools must have in place the theme of improving health within the school setting.
Schools are not the only setting to be considered. In terms of promoting healthy communities, we need to see how we can reach out to more disadvantaged communities and those at risk of obesity, including people with disabilities, to ensure those individuals who are at risk of obesity are supported.
There is an ongoing challenge in terms of developing the evidence-base. One of the biggest difficulties is ensuring that the programmes available are quality assured and based on good evidence in terms of intervention. The gap in the evidence base has resulted in a range of initiatives from the Private Sector in terms of tackling obesity, which may not necessarily be approved by health professionals.
There are a number of key stakeholders that are vital. They are:
- Parents and Families;
- Health Care Social Services;
- Teachers and Childcare Workers;
- Employers & Board of Governors;
- Local Authorities;
- Ministerial Group in Public Health.
In order to make any sort of impact, it is important that the resources, which are very restricted, are targeted at those most at risk. Certainly in terms of adulthood obesity, the Western Obesity Taskforce has focused on those with a BMI between 25-30, i.e. those who are deemed to be overweight and at risk of becoming obese, so we can make a change to prevent further people from becoming obese.
In terms of the action plan, I have attached for your information, the Fit Futures Action Plan for the Western Board area, which highlights the significant range of initiatives that we are currently leading on. I have also enclosed details of how we would propose to take these initiatives forward. However it is worth highlighting a number of those projects that have proven very successful. Initiatives such as:
- Health Promoting Homes - the award-winning programme which targets families from disadvantaged communities, and to date over 450 families have benefited from the programme.
- Field to Fork – a joint initiative with the Education & Library Board to educate children in Primary Schools where food comes from and its link to environmental sustainability as well as good diet and nutritional food.
- Creation of a Community Diet & Nutrition Team – a follow-on from the successful Cook It! Programme. The Western Board has established a Community Diet & Nutrition Team, which will roll out initiatives such as Cook It! but also feed into a broad range of initiatives around tackling the rise in obesity in disadvantaged communities.
- Breastfeeding Support – the Board has commissioned significant investment in promoting breastfeeding in collaboration with the Trust and the Community & Voluntary Sector to support mothers to opt for breastfeeding and to ensure that they place breastfeeding at the core of healthy diet and nutrition for their children.
In relation to the availability of weight management and other intervention services to tackle obesity related to ill-health, it is acknowledged that there is increasing dietetic capacity within a community and secondary care service but the demand is continually growing. There are drug options, which have limited effect when diet fails – such as Orlistat or Sibutramine. There is a lack of funding around bariatric services for patients in Northern Ireland who have persistent obesity when lifestyle and other drugs fail. Bariatric surgery has been shown to reverse diabetes and reduce mortality and there is an issue about equity to services which are available in other parts of the UK – this adds to the inequalities in health that we experience. It is acknowledged that while many patients can be managed in a community obesity clinic setting, there is a need for investment in specialist services in secondary care. We acknowledge that physicians in diabetes and endocrinology are appropriate specialists to manage such a service. However, they are already overwhelmed by the demand, as the diabetes epidemic has put additional pressure on the services that they are facing.
In terms of further action required, there is a need for further development of the All-Ireland Obesity Observatory, in terms of ensuring that we can get a better
understanding of what initiatives are being taken forward and have greater collaboration between those identifying core issues and those delivering appropriate services.
There is also a clear need to ensure we have a better evidence-base of what interventions actually do work which reflect the setting and target audience for which they are being designed. There is a necessity to ensure that there is the appropriate investment required, both in early intervention and prevention, as well as in treatment services.
There is a need for a better understanding in terms of the role that other agencies can take forward work that would contribute to reducing the burden of obesity and its subsequent ill-healths. There is a key role here for the Ministerial Group in Public Health to drive this greater collaboration that will support initiatives that are tackling the issue.
North Eastern Education
and Library Board
Current approach to tackling obesity and the promotion of lifestyle change
Curriculum:
The Curriculum Advice and Support Service of NEELB works with schools to support the implementation of the Northern Ireland Curriculum which includes statutory elements such as Home Economics, Personal Development and Mutual Understanding (PDMU) and Physical Education:
- Home Economics at Key Stage 3 enables pupils to explore their health in a practical context, enhancing their potential to live a healthy lifestyle and make responsible choices about their diet and food.
- An understanding of the benefits of a healthy lifestyle including healthy eating is part of PDMU in Key Stages 1 and 2 and of Personal Development at Key Stage 3. Pupils are encouraged to develop healthy attitudes and behaviours in relation to eating and food.
- Physical Education is statutory for all pupils from Key Stage 1 to Key Stage 4. Physical Education has a role to play in providing pupils with regular, frequent and appropriate physical activity opportunities, information and guidance and by encouraging and empowering pupils to make informed and responsible choices about the role of physical activity in their lives.
There are specialist subject officers available within NEELB CASS to provide specific and relevant advice, resources and training for teachers and schools in all of the above areas.
Partnerships:
- NEELB is a member of the Northern Investing for Health Partnership contributing to the actions of the Health Improvement Plan. Staff from the Curriculum Advice and Support Service sit as members on the Obesity Prevention Sub Group and the Northern Partnership for Physical Activity.
- The Northern Health and Social Services Board provided NEELB with a one-off payment of £46,000 to operate a grant funding scheme to support initiatives related to Fit Futures, including secondment of a co-ordinator to oversee the work. Post primary schools had the opportunity to apply for a grant to support relevant initiatives in March 2007 and the Northern Investing for Health Partnership (NIfHP) Obesity Prevention sub-group recommended that a dietitian be seconded to NEELB to work exclusively with schools from Nov 07 – Oct 08. Additional funds were provided to extend the dietetic secondment for an additional year from Nov 08 – Oct 09. This secondment opportunity is to support the NIfHP’s Obesity Prevention and Food and Nutrition work and to assist in the implementation of the Fit Futures Implementation Plan. The main aims of the initiative are to help develop whole school approaches to tackling obesity in children and young people and to develop robust food and activity policies aimed to sustain positive changes for health and well being.
The dietitian’s remit includes:
- Working with the NEELB Curriculum Advice and Support Service in liaison with local and regional players such as NHSCT Health Promotion Officer for Schools, School Catering Service, including the Nutritional Standards Coordinator, NHSCT Oral Health Promotion Service, School Nurses, Councils and other dietetic staff working with schools.
- Providing advice, resources and training on healthy eating for pupils, teachers and parents.
- Contributing to the professional development of school catering staff.
- An interim report of progress can be found attached (Appendix 1)
- In 2004 the Northern Neighbourhoods Health Action Zone Fresh Fruit in Schools Scheme Steering Group successfully bid for funding through the then New Opportunities fund’s (now the Big Lottery Fund) Coronary Heart Disease, Stroke and Cancer Programme. The NEELB was represented on the Steering Group by the Health Promoting Schools Coordinator, the Assistant Adviser for Personal Development and Home Economics and the Catering Service Manager. The bid proposed that a project would be carried out in the Northern Health and Social Services Board (NHSSB) area, to enable primary schools to develop Healthy Breaks Policies within their schools. The project was titled the “Healthy Breaks initiative" and was designed to build on the Northern Neighbourhoods Health Action Zone’s Fresh Fruit in Schools Scheme. The aim of Healthy Breaks was:
“To improve the health and life chances of children who are most at risk from Coronary Heart Disease, Cancer and Stroke in later years by encouraging children from disadvantaged areas to adopt and sustain healthy eating patterns at school, home and in the community and to create environments to facilitate this".
Big Lottery Fund allocation of £300,000 enabled the Healthy Breaks Initiative to target 28 Primary Schools in the NHSSB area. Funding enabled the initiative to run for three years ending in December 2007.
- The NEELB, in partnership with South East Antrim Life Education (SEALE), Northern Investing for Health Partnership, Antrim and Newtownabbey Borough Councils, currently delivers a healthy living programme using a mobile unit (Life Education Centre) and trained educator to Primary Schools in the Council areas. The programme is geared to meet the requirements of the various age groups and using the high tech unit along with visual aids, explain the dangers of smoking, drugs obesity and the need for healthy eating. The programme is delivered to each class in the school, enabling children to participate in activities to examine the effect of their lifestyle and their attitudes towards obesity, drugs, alcohol and tobacco along with substance abuse. In addition, the educator meets with the parents to explain how they can improve the health of their children by changing their lifestyle and by working with teachers, provide a healthy environment for the children.
Physical Activity:
- NEELB appointed a Physical Literacy Coordinator (Primary) in January 2007 to support the delivery and dissemination of the Fundamental Movement Skills (FMS) Programme. Outcomes have been as follows:
- Since April 2008…95 teachers have been trained in Fundamental Movement Skills to promote understanding and delivery of high quality Physical Education/Physical Activity in the school/home and recreationally.
- 15 schools have had intensive support from the Physical Literacy Coordinator i.e. 1 day per week for 1 term. Children were encouraged through a programme of Physical Activity/ Health Awareness and Healthy Eating by The Physical Literacy Coordinator.
- The NEELB produced and developed a Home/School Physical Activity pack (Fit for Fun – “The Way Forward") to encourage children to play more at school and at home and also to educate and encourage Parents to join in with the activities. The activity pack is a resource targeted primarily at Foundation Stage teachers, pupils and parents. £12,000 funding from the Northern Partnership for Physical Activity will be provided to roll the pack out to schools during 2008-9. 250 Primary Schools in NEELB will receive the pack with the total number of homes anticipated to be contacted over the next three years through the distribution of the resource approx 33,000. Primary 1 teachers will receive the packs to distribute to all the parents/carers of Primary 1 children. The resource will enable the Teachers already trained in Fundamental Movement Skills by the NEELB between 2005 and 2008 to consolidate and develop and enhance the quality of physical activity of the children on five different levels:-
- Within the Physical Education Curriculum
- Within Play-Based Learning
- In the playground during recreation (break-time/ lunch-time)
- Linked to “homework" type activities
- At home with Parents/carers/siblings
- The NEELB has made use of a dance project officer to deliver a 6 week programme of aerobic work out to increase activity levels among Primary 7 children and educate them on the use of Dance to keep fit. To date, 9 schools have received the Dance programme over a 6 week block.
Extended Schools:
Now into its third year of implementation, the NEELB currently have 59 Extended Schools funded by DE. The majority of schools are operating activities and services within the Extended Schools Programme that contribute to the ‘Being Healthy’ High Level Outcome. During the year 2006-7, 105 activities and services were recorded as impacting on ‘Being Healthy’ and in 2007-8 this increased to 145. Activities include e.g. breakfast clubs, sports activities/clubs, cookery classes, healthy eating demonstrations. In 2007-8, 22% of extended schools reported an identifiable improvement in pupil health and fitness and 92% reported that the Programme was ‘very good/good’ at fostering health and well being and social inclusion.
Health Promoting Schools
The NEELB had 53 schools in the Health Promoting Schools Pilot from 2002 – 2006 with the majority implementing Healthy Eating and Physical Activity initiatives. Since 2006, NEELB has continued to provide support, training and resources, where possible, to the existing schools with the additional funding provided by the Health Promotion Agency (£10,000 in 2006-7; £20,000 in 2007-8).
NEELB School Catering Service
The Education Catering Service of NEELB has, for many years, been involved with Health Professionals across all sectors with the aim of improving the health and well being of pupils attending controlled and maintained schools within the Board’s Area:
- In conjunction with Health Promotion Agency and Department of Education the Education & Library Boards were involved with the production of Catering for Healthier Lifestyles Document in 2001. Between March 2004 and March 2005 a trial was conducted across a range of schools, ten of which were in NEELB. A programme was then set out to roll it out across all schools.
- DE made available to the meals service funding to assist in a range of crucial areas to ensure guidelines could be met. It encompasses areas such as food, training, equipment, marketing and the employment of Nutritional Standards Co-ordinators. The Co-ordinators main task was, in conjunction with Catering Managers, to implement and monitor nutritional standards.
- To support this important work further, revised nutritional standards were introduced in September 2007. These standards formed part of DE’s contribution to the cross-departmental Investing for Health and Fit Futures initiatives. The purpose of these initiatives is to improve the health of children in NI through nutrition and physical fitness strategies in line with the strategic goals of the Children and Young People’s Funding Package.
- The Nutritional Standards Co-ordinators have developed training courses to raise awareness on healthy eating for schools, to include Catering Staff, Supervisory Assistants, PTA’S, Board of Governors and most importantly the pupils.
- In NEELB 800 managerial and operational staff have received nutritional training in accredited nutritional courses. Key staff have also been trained in special diets which include weight reduction as determined by health professionals.
- A group has been set up to market the service to all key stakeholders.
- The funding made available has assisted in the quality of food on offer and ensures that a wide range of fresh foods can be included. Bread, milk and fresh fruits are offered within the meal charge encouraging pupils away from less healthy items. Menus have been developed to reduce fat, sugar and salt. Equipment has been purchased to assist in the healthier style of food production.
- The Department of Education inspection programme includes the monitoring of school meals and reports the good progress that is being made to improving the health of children.
- The Catering Service believes that through its work with all appropriate agencies that as the pupils progress through school, they will learn about nutrition which will continue into the food choices they make in the future.
- We work closely with schools to ensure those entitled to a free meal avail of it.
Dr Michael Ryan
Northern Health and Social Care Trust
The ‘Fit Futures’ strategy (2006) rightly focuses on activity and young people. The ‘Fit Futures’ taskforce identified six strategic priorities which included the development of joined-up public health policies and the building of an evidence base. Services for young adults and the middle aged depend very much on the individual interests of the person themselves, and their primary and secondary care services. The lack of a comprehensive, strategically planned service for the overweight and obese adult is a major shortcoming of the current healthcare system.
The CREST report (2005) produced guidelines for the management of obesity in secondary care but has not resulted in the attraction of significant resources for the implementation of its recommendations.
The epidemic of obesity is well established and is not showing any signs of abating, particularly among the young. Currently, more that half our adult population is either overweight or obese. Their World Health Report 2002 estimated that over 7% of all disease burden in developed countries was caused by overweight, and that around a third of coronary heart disease and stroke, and almost 60% of hypertensive disease in developed countries was due to overweight. It is estimated that around 45% of patients diagnosed with cardiovascular disease in the UK are overweight. At least 75% of obese people will have one or more co-morbidity e.g. 80% of diabetics are overweight or obese.
Achieving weight loss is pivotal in reducing total cardiovascular risk. A modest weight loss of around 10% can result in a 20-25% fall in mortality, 30-40% fall in disease related deaths, a 50% reduction in the development of diabetes as well as a 40-50% fall in obesity related cancers. Figure 1 illustrates graphically the role of obesity in cardiac risk relative to conventional risk factors.
Obesity is also a significant risk factor for cancer. Among postmenopausal women, about 5% of all cancers (approximately 6000 cases annually) are attributable to being overweight or obese. For endometrial cancer and adenocarcinoma of the oesophagus about half of all cases in postmenopausal women are attributable to overweight or obesity.
Obesity and overweight are recognised priorities for action at both local and national NHS levels. There is incontrovertible evidence that weight reduction, however achieved, is effective in reducing morbidity and prolonging life. A large proportion of our population needs professional help with weight related health issues.
Current Approach
Current NHS services for a wide range of clinical conditions, particularly diabetes, cardiovascular, and respiratory services, are being stretched by the high prevalence of co-morbidity associated with excess weight. Up to 80% of patients attending diabetic clinics are overweight or obese. Weight loss can result in meaningful improvements in quality of life and duration of event-free survival.
Current clinical services, designed to address specific clinical conditions, such as diabetes, cannot adequately address the special needs of the obese patient. Clinical services are becoming effectively ‘silted up’ with patients whose primary cause for attendance is ‘overshadowed’ by the co-morbidity of excess weight. Addressing the obesity can be more beneficial, in terms of health gain for the patient, than dealing with the ‘primary’ cause of attendance. These wider implications of overweight in terms of consumption of healthcare resources remain unknown.
Currently considerable resources are expended in ‘squeezing’ obesity and weight management into time set aside for other activities. This approach has significant limitations;
1. it consumes considerable but unquantified resources
2. there is no consistent approach to weight management
3. it does not produce quantifiable output such as kilograms of weight lost or reductions in the development of diabetes or other complications
4. as weight loss is often not the primary concern of the encounter, the special needs of the obese patient may be effectively addressed.
The lack of quantifiable outcomes and coherent strategic approach leads to lack of clinical and managerial credibility. This lack of credibility and confidence makes it difficult to establish properly funded and managed programs of care despite the evidence of cost-effectiveness in the literature.
Fundamentally, the current approach lacks cohesion and an overarching strategy and fails to produce objective and quantifiable outcome measures such as assessment of value for money and clinical effectiveness.
Description of the existing service
There is currently no specific service or co-ordinating management structure for obese adults to collate practice and audit progress against measurable targets. Most overweight or obese individuals are presenting to cardiac, diabetes, and a range of other services in the community as well as in primary and secondary care, with issues that are often, in whole or in part, secondary to their weight (hypertension, diabetes, mobility issues, depression).
These patients are currently ‘managed’ as follows;
1. Seen in a range of other clinics whose services are designed for purely medical conditions.
2. The clinics operate with fixed slots for patient encounters which is often not optimal to deal with lifestyle issues.
3. Review is often by healthcare professionals whose primary interest may not be obesity such as diabetologists, cardiologists, dietitians etc.
4. Patients are reviewed at relatively long time intervals which is not appropriate for achieving weight loss and lifestyle change.
5. Standard clinical and biochemical parameters of cardiovascular risk are measured and treatments adjusted to achieve targets not directly related to weight (such as blood pressure and cholesterol).
Such a service provision model is not appropriate to adequately address the obesity issue.
Within the current financial year, NHSSB has part-funded a 2 year ‘Motivate’ project based on the successful Scottish Counterweight Programme. This has been part funded from the Condition Management Programme, part of a wider initiative to enable individuals on Capacity Benefit to return to work. We would envisage integrating this type of initiative to our Long-term Conditions programme in the Trust, and with a project developed by the European Centre for Connected Health.
The Northern Investing for Health Partnership (NIfHP) has in place an Obesity Prevention Sub Group to facilitate, oversee and drive forward relevant actions within the Health Improvement Plan (HIP) and related strategies, including Fit Futures. The group has been in place since the end of 2005 and has a broad range of professional and organisational representation.
The group advises the NHSSB (as lead and accountable body of the partnership) on the allocation of Fit Futures and food and nutrition funding. The group links with the Northern Partnership on Physical Activity (NPPA).
Initiatives taken forward through the group have included a wide variety of approaches and sectors. All initiatives have been evaluated. Full details are available on request. Some examples are , family focused programmes to support families with obese children, weight management training for primary care professionals, healthy cooking training for commercial food suppliers, support for community nutrition and activity programmes, a healthy eating programme for ethnic minorities, and awareness raising workshops for schools thorough ELB.
The NIfHP also funds four Trust based posts in support of obesity prevention; two breastfeeding posts and two prevention focussed dietetic posts (these two posts are due for review over the coming months).
The NHSSB and Northern Health and Social Care Trust are working together to put in place a team, based in the Trust, to co-ordinate and drive forward obesity prevention in the NHSCT/NIfHP area. This team will be in place within the next number of months.
The current investment in weight management lacks overall cohesion, strategic planning, and a strong evidence base. The total quantity of resource expenditure, particularly in the community and ‘indirect’ clinical care remains unquantified by is undoubtedly significant. The current ‘system’ consists of a wide range of ‘interventions’ championed by enthusiastic and well meaning individuals but the lack of overall co-ordination renders many of the programs difficult to evaluate. The lack of an overarching structure with the authority and resources to implement best practice across the province is a major shortcoming.
Proposals for further action
Weight management by conventional means (dietetic advice and clinical encouragement) is difficult, but research now shows that best results are obtained through the use of intensive, structured, intervention programmes, delivered by specifically trained individuals in an appropriate setting. The Finnish Study and the Diabetes Prevention Programme are two published examples of how a structured approach can lead to successful outcomes. A reduction of about 57 % in progression of ‘at risk individuals’ to type II diabetes was achieved with a 7 % weight loss over a 6 month period. The ‘counterweight program’ in Scotland has proven successful in primary care and this proposal aims draw on the experience of this program for the community, schools, primary prevention, and secondary care. Furthermore, in terms of drug costs, each unit reduction in body-mass index achieved by ‘counterweight’ resulted in a 6% decline in drug costs.
The prevalence of BMI <25 (normal-weight) is set to half, and BMI > 30 (obese) set to double over the next 10 years. The effectiveness of combinations of lifestyle intervention and pharmacological therapy in achieving weight loss and quality-of-life improvement is well established.
The ‘conventional’ approach to weight management and lifestyle change has not resulted in universally convincing, significant and demonstrable benefits to public or individual health. Despite considerable resources being consumed, both known and hidden, on weight management endeavours, the benefits of the current approach remain uncertain. The inexorable increase in overweight and obesity in the younger population particularly, would suggest that the conventional model of service provision is ineffective and required urgent review.
I propose that a structure be developed to direct and monitor resource expenditure along the lines of a managed clinical network (MCN). Such an MCN should be obesity-specific and have appropriate terms of reference to address weight-related issues across the spectrum of NHS involvement.
The proposed MCN service program will complement the existing service in the following ways;
1. The entire weight management program should be co-ordinated and managed using an MCN model to ensure optimal value for money, clinical effectiveness and quantifiable outcomes.
2. Overweight and obese individuals from the community, primary and secondary care could be treated in a single, seamless stream, based on the clinical risk associated with weight using interventions approved by the MCN.
3. The MCN will focus on weight management as an entity in itself that merits specific intervention using appropriately skilled personnel and evidence based strategies applied in the most appropriate environment across the entire spectrum of intervention.
4. The approach to weight management at all levels of intervention that are supported by the MCN, and that utilise public resources, should be explicitly evidence-based with auditable targets and outcomes.
5. The MCN would be responsible for the production of such audits .
6. The programme will be delivered following the principles of the recently published NICE guidelines on Behaviour Change.
7. The MCN will provide ‘hard data’ on effectiveness of intervention in terms of weight loss, cost, progression of associated co-morbidities, and patient wellbeing.
8. Specific funding should be identified to establish an MCN for obesity in each Trust with a strategic management board at regional level.
Much of the cost of such a program is likely to be already ‘embedded’ in the system as a wide range of community, primary and secondary care resource is diverted from its primary purpose to address the additional morbidity secondary to co-existing overweight and obesity. The initiation of a specific prevention and therapeutic program for obesity is likely to enhance the efficiency of a range of existing services as well as prevent additional morbidity.
The MCN could, as part of its remit, review the cost-effectiveness of its own program. Current evidence suggests that, with appropriate costing information and using best evidence-based practices, weight management can itself be a cost-effective intervention.
The program will operate as per standard clinical lines in accordance with the Declaration of Helsinki and Good Clinical Practice. Clinical Governance will be ensured by the Family Practitioner Unit.
How does this fit in with local priorities
The Department of Health is committed to developing services for overweight and obesity and considerable resources have already been invested in this problem. The scale of the problem is such that these resources are overstretched, particularly in primary and secondary care, and cannot adequately address the needs for both prevention and intensive intervention.
Current efforts at weight management consume considerable resources but often do not deliver measurable outcomes. The proposed MCN will integrate and upgrade existing services through a structured approach which will promote evidence-based interventions and deliver quantifiable output.
The MCN-directed program will be required to be delivered by qualified staff with training in behaviour change skills (to include motivational interviewing and cognitive behaviour skills).
There is a great deal of interest, effort, resources, and goodwill being directed at this problem. The lack of strategic overview, evidence-based implementation, and quantifiable outcome, compromises credibility. Service management is often reluctant to allocate resources to weight control programs when the existing investment is so poorly accountable and has produced such poor evidence of effective outcomes in general.
I maintain that the MCN-based approach can address many of the deficiencies of the current system and allay concerns regarding the appropriateness of further investment in weight management programs. Furthermore, the embedding of audit and accountability in the MCN structure and terms of reference will deliver confidence in relation to the value for money for such investment.
Local priorities, whatever the specific details, are always about evidence of cost effectiveness and value for money. The current system does not deliver on either score, or at least, there is no solid evidence that it does.
While considerable additional resources will need to be invested to establish the proposed overarching structure for weight management which will span community, primary and secondary care activities, the continuation of the current disparate and ad-hoc approach is unlikely to deliver in the future what it has failed to deliver in the past.
Michael Ryan
Consultant Chemical Pathologist
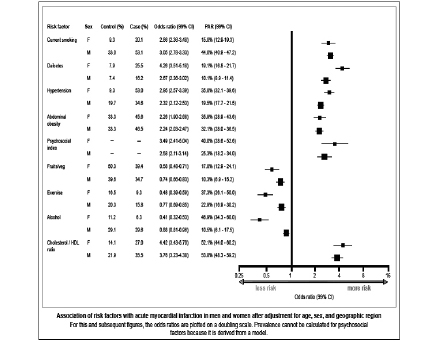
Figure 1. Presents the risk due to abdominal obesity and physical inactivity in relation to other ‘conventional’ risk factors such as blood pressure. Bearing in mind that these conventional risk factors such as blood pressure, cholesterol, diabetes and psychosocial index are also affected by obesity, the true impact of obesity is clear yet the resources directed at obesity are not commensurate with its important role in cardiovascular risk.
Fermanagh District Council
1. Current Obesity Trends (Western Region)
We recognise that obesity is increasing particularly among children and understand that in the WHSSB region 20-30% of early years school children are already overweight. Current statistics also show that 26,899 adults in the WHSCT area have a BMI of 30 or above while 3627 have a BMI in excess of 40. Furthermore, almost 10% of the Western area population are obese based on the present population of 293,000 (WHSCT 2008).
2. Current Actions to tackle Obesity
Currently there are a range of different initiatives, programmes and projects devised by HSSB’s, Councils and others attempting to combat the increase in obesity. However these are mainly identified and promoted on a local basis and are often developed in isolation.
There are a number of organisations seeking to address obesity and these include the HSSB’s, ELB’s, Local Authorities, Social Care Trusts,
- 2 –
Investing for Health Partnerships etc. However a co-ordinated approach is needed.
Some projects are working very successfully e.g. the GP Referral Scheme which could be replicated on a province wide basis.
3. What action is needed
A joined-up province wide approach is needed with an audit of the current programmes to determine those most successful and worth rolling out across the country.
There needs to be a strategic approach developed which identifies the local agency, the partnership organisations, the programmes to be developed and the financial resources available and needed. A partnership approach needs to be taken.
4. Some suggestions:-
a) Tackling Obesity in Children
- Continue the school swimming programme (a partnership between WELB and the Councils).
- Support P.E. in schools particularly small rural schools with no dedicated P.E. teachers.
- Encourage use of schools premises and facilities out of school hours. Pitches, halls, etc.
- Encourage access to the countryside, through the provision of walking routes, cycling routes, events etc.
- Enable sporting activities and competitions for children through schools, clubs and Leisure Centres.
- Continue to provide locally accessible leisure centres and facilities.
b) Tackling Obesity in Adults
- Continue the GP Referral programmes and roll these out Province wide.
- Encourage access to the countryside (as above).
- Enable activities such as walking festivals, cycling activities etc.
- Continue to provide locally accessible leisure centres and facilities.
The Councils already deliver some of the activities above but could play an increasing role as part of a partnership approach and with the necessary finance available.
Health and Social Services
Councils for Northern Ireland
1. The Health & Social Services Councils (HSSCs) were set up by Government in 1991 to represent the views and opinions of the public. This written evidence therefore reflects that perspective.
2. The current obesity ‘epidemic’ is likely to put pressure on health and social care services for the foreseeable future regardless of the impact of current programmes. The experiences of patients/clients using weight management programmes need to figure in any future strategy.
Scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change.
3. The HSSCs would make the following comments. These are drawn from a variety of sources including the HSSC’s overview of service delivery and specific activities such as two consultation events organised by the HSSCs on the Service Framework for Cardiovascular Wellbeing and attended by over 70 community activists.
4. Weight management/healthy lifestyle initiatives require a cross departmental approach. The DHSSPS cannot provide the full range of measures required. This means that a social model and response to obesity is required rather than a pure health model. In particular, a joined up approach with the Department of Education is essential. With the policy lead for Early Years moving to DE in April 2009, there is an opportunity to revisit work currently being done.
5. Current approaches involve a range of interventions including drug therapy, genetic testing, surgical treatment and diet/lifestyle advice. Which treatment is provided may depend on level of obesity, associated health risks, etc. Obesity is sometimes seen as the patient’s own fault. With practitioners not always trained in weight management, programmes can be undertaken without appropriate support. The lack of adequate support is likely to mean that the treatment is less likely to succeed and therefore reinforces negative perceptions that the treatment is not worthwhile.
6. For the bulk of the public, the first experience of promotion of weight management will be through community based initiatives which are becoming more common. The HSSCs welcome the broad range of HSC initiatives aimed at the promotion of healthy lifestyle change ranging from healthy eating in playgroups to inclusion of targets in the CVD Service Framework. The difficulty is how best to ensure a joined up approach and assess which initiatives work best. Feedback from the public often references confusion about the vast range of messages on healthy eating/weight management directed at them. The messages delivered to the public need to be empowering not confusing.
7. Whilst the HSSCs support a performance target approach which allows baselines to be developed and improvement measured against this, the danger is that it can become a tick box exercise that does not impact on the quality of the patient/client experience. Our indications are that the public is becoming increasingly sceptical about the current target culture in the HSC as not necessarily delivering an improved service. The collection of data can seem to become an expensive end in itself with potential for duplication of tasks being carried out by administrators remote from practice.
8. Multi-agency approaches such as Investing for Health have proved a useful way of focussing attention on ‘healthy choices’ in relation to lifestyle. However, this project based approach potentially has limited local impact without impacting on an overall strategy. It is not clear whether such investment is delivering value for money or contributing to evidence based future service delivery. Through Investing for Health linkages with Local Authorities have been strengthened. There appears to be a particular role for local government in relation to obesity through leisure, sports development, etc. With recent proposals in regard to community planning, it may be that there is an enhanced role for local authorities in bringing together key players.
9. Examine the availability of weight management or other intervention services to tackle obesity related ill health
10. As with every aspect of health and social care, the HSSC believe that a patient/client focussed service will deliver the best results. The HSC must engage with its service users to determine what best meets their needs and can deliver results.
11. The role of primary care services is of key importance to service users. This raises issues of access to GP services including their role, surgery opening hours, additional services. Our anecdotal evidence shows a considerable public interest in an MOT approach to healthy lifestyles/weight management whereby practice nurses could offer one-to-one/family advice and support. GPs also need to be supported in delivering advice effectively without ‘lecturing’ or de-motivating the patient. There may be a training requirement for primary care staff in relation to assessment for appropriate weight management programmes and associated support with associated costs.
12. The current perspective of the re-configured HSC Trusts is to view health promotion and community development as two sides of the same coin and to utilise community development as a tool for health promotion. This obviously makes good sense and provides a joined up approach to meeting community needs. However, this has to be done in a way that is a genuine partnership with communities and service users. If the end result is yet another tick box exercise on behalf of the Trusts, the result will be disengagement of local community activists to the detriment of the social capital of communities.
13. Good community development practice should begin with communities reflecting on their needs and experiences. It recognises that people’s health is determined by their social, economic and environmental experience, as well as by individual factors. Given the nature of the obesity epidemic, it is not uncommon to ‘blame’ the individual for their weight problem. It is also a reality that the individual has to be engaged in the weight reduction programme if it is to be successful. A patient client centred approach to weight management is required if this engagement is to take place. A successful response to obesity must reflect this reality.
14. Access to funding for small local initiatives is as relevant for weight management initiatives as other health related matters. Feedback from community groups has indicated to us that access to funding for exercise groups (in particular for the over 50s) is a barrier to a broader range of community health promotion activities. However, the HSSCs are very aware of the need to ensure that such activities offer value for money and are evidence based with outcomes that can contribute to the overarching strategy rather than ad hoc local activities.
15. Consider what further action is required taking account as appropriate of the potential to learn from experience elsewhere.
16. It is important that the post-RPA organisations are able to add value to this work. The role of the Regional Board will be important in the commissioning of a joined up strategy whilst local commissioning groups need to develop the ability to ensure that this regional approach is able to respond to particular local needs. The role of the Well-being Agency is likely to be key delivering against this agenda and should enable co-ordination of a clear evidence based health promotion strategy. The relationship between the Agency and the Regional Board will be important in delivering joined up services.
17 The ‘obesity epidemic’ is a common problem throughout the western world. There will be numerous opportunities to explore methodologies that are seen as successful in other countries. We do feel however that whatever strategies are adopted will not be fully effective unless they are patient centred and culturally appropriate to Northern Ireland and its increasingly diverse population.
18. Conclusion
The HSSCs welcome the opportunity to contribute to this important review believing that the outcome will be important for individuals and communities in Northern Ireland as well as for the future of Health & Social Care Services.
Omagh District Council
Omagh District Council is represented on the Western Area Obesity Taskforce Executive Committee. The Committee’s role is to oversee, coordinate and drive forward the strategic implementation of initiatives that will address the prevention of obesity in the population of the West including the Fit Futures Strategy.
The primary functions of the Group are:
- To provide advice and strategic direction on all relevant issues relating to obesity prevention, including the development of an approach to tackle obesity in the adult population
- To influence the work and strategic direction of the regional obesity prevention taskforce
- To facilitate and oversee the implementation of the recommendations and various actions within Fit Futures as they impact on the WHSSB area.
- To review the evidence base for interventions and examine issues around quality assurance, engagement and dissemination of best practice.
- To identify key stakeholders in the West and secure their buy-in to addressing the issues
- To assist in the effective implementation and monitoring of Fit Futures.
- To monitor progress against targets and produce a report on progress on implementation for the Ministerial Group on Public Health or as determined by any other Government Department.
The Group will also carry out a number of performance management duties
- To develop appropriate data collection arrangements in order to allow for monitoring of progress.
- To develop a mechanism for regular reporting to the steering group by relevant organisations.
- To identify barriers to progress, and subsequently feedback relevant issues and possible solutions to the regional steering group and other relevant organisations.
- To publicise progress were appropriate.
Omagh District Council actively engages with the public and commercial sector to improve diet and health.
The Leisure Services Department offer a wide range of physical activity programmes. The Council has upgraded Leisure facilities recently with the opening of a £2.5 million fitness suite. The department also operates a multi sport programme offering sport coaching in the community which has an indirect effect on obesity especially amongst children.
The Council has hosted the Senior Citizen Consortium for a number of years and offers a physical activity session every Thursday for the over fifties.
Omagh District Council in partnership with the DoE has also developed urban walks for people to avail of in Omagh town centre and encourage the public to use these as a means of physical activity.
As part of the ODC Sport, Leisure and Recreation Strategy, members of the public are actively encouraged to engage in sport and physical activities at their own level. At present the Leisure Services Department are in the process of introducing the condition management programme in partnership with the Western Health and Social Services Care Trust where clients on benefits will be referred to the Omagh Leisure Complex to take part in a 12-15wk exercise programme with a view to increasing their physical and mental state and assist in their return to the workplace.
The Omagh Sports Forum recently held a Sports Nutrition seminar which was free of charge, it is anticipated that more of these seminars will be organised in the future.
Recently twenty four boys and girls were presented with plaques to recognise their achievement in a cross-community sporting project. The eight to eleven year-olds participated in a variety of sporting activities including volleyball, mini-cricket, team building games and outdoor pursuit activities over a four-week period.
Funded by Omagh District Council’s Community Relations Programme the project aimed to help the children build relationships based on trust and mutual respect whilst encouraging them to engage in physical activity. This project built on the successful “One Small Step" project organised last year where children from the three Council owned Community Centres came together to learn about each other cultures through the sports hockey, gaelic football, rugby and camogie.
The ‘Grassroots Programme’ has been established in partnership with ODC and the Irish Football Association to encourage more people to take up football, and stay in the game longer.
The Council has developed the Strule riverside walkway and cycle path within the town centre in association with Sustrans (UK’s Leading Sustainable Transport Charity). This path will connect communities to each other and the places they need to go every day to work, school and retail outlets.
Omagh District Council Environmental Health Department (EHD) is delighted to have been the first council in Northern Ireland to offer the Chartered Institute of Environmental Health Level 2 Award in ‘Healthier Food and Special Diets’ to caterers operating within the district. Significant interest in the course was generated, and it is anticipated that another course will be run by the Council later in the year. Caterers from a variety of settings attended the course including those working in childcare facilities, nursing and residential homes, work canteens, hotels and restaurants.
This accredited nutrition qualification provides candidates with information they need to prepare nutritious food, develop healthy recipes and cater to a variety of dietary requirements. It is anticipated that the caterers on receiving the nutrition qualification will be in the position to offer more nutritious and healthier options to their customers who are increasingly aware of the health effects of a poor diet.
Environmental Health Officers offer nutrition advice to caterers when conducting inspections within catering establishments. Nutrition advice is issued to all childminders on registering their business with the EHD.
The Western Group Environmental Health Service is represented on the Western Health and Social Care Trust Nutrition and Oral Health Group who work in partnership to support the promotion of nutrition and oral health in the Western Health and Social Care Trust Area by:
- Providing a link to the Western Board ‘Fit Futures’ Steering group and oral health promoters group
- Providing a link to the Health Promotion Department and Lifeskills sub groups
- Identifying, supporting and overseeing projects to support the Fit Futures and Oral Health promoters group
- Monitoring trends in nutrition and oral health across the board area
- Reviewing the effectiveness of health promotion interventions aimed at improving oral and nutritional health
- Identifying and addressing areas of further support and development
- Promoting consistent evidence based messages
- Contributing to the implementation of the Trust and other strategic action and intervention plans for the promotion of nutrition and oral health
- Working in partnership with other agencies
The Health Promotion Group within Omagh Council provides the following services to their staff:
- Regular check up with nursing staff
- Free fruit days
- Reduced membership in Omagh Leisure Complex
- Westfield Health Care package
- Walking Challenges
- Golf Challenges
- Weigh-in competitions
It is evident from the above briefing note that Omagh District Council works in partnership with a range of organisations to address the issue of obesity both in terms of food and nutrition and exercise and activity provision.
In addition the Council engages with their staff in cascading information, advice and guidance on all aspects of healthy lifestyles which also addresses obesity.
Department for Health,
Social Services and Public Safety
1.0 Introduction
1.1 The prevalence of obesity has increased dramatically over the past few decades throughout the UK and in many other Western countries. Staying a healthy weight, eating sensibly and keeping active can improve health and reduce the risk of diseases associated with being overweight, such as coronary heart disease, osteoporosis, cancer and type two diabetes.
1.2 The obesity related conditions outlined above reduce life expectancy, undermine quality of life, and impose huge burdens on families, carers and health services. Investing resources in addressing obesity should provide value for money for Government at all levels. If levels of obesity continue to rise unabated it is very likely that the related costs will grow significantly over the next few decades.
Obesity Definition
1.3 Obesity is a condition where weight gain has got to the point that it poses a serious threat to health. Obesity is usually measured by Body Mass Index (BMI), which is a function of person’s height and weight. In adults having a BMI of 25-30 is classified as being overweight and having a BMI of 30 or more is classified as obese. For children special reference curves have been designed to calculate BMI as the height and weight of children varies with age and gender.
1.4 However, BMI should only be considered as an approximate guide to overweight and obesity because it may not correspond to the same level of fat in different individuals. For example, differences in distribution of fat around the body, higher or lower than average amounts of muscle, and ethnic differences may mean that people with the same BMI have different levels of fat, and this may affect the associated health risks.
Impact of Obesity
1.5 Research has indicated that being obese may increase the risk of the following health conditions:
- heart disease and stroke;
- type 2 diabetes
- some cancers, including post menopausal breast cancer;
- hypertension;
- gall bladder disease;
- osteoarthritis;
- sleep apnoea;
- breathing problems;
1.6 Evidence also indicates that obesity:
- can reduce life expectancy by approximately lower back pain; and
- complications in pregnancy.
- 9 years; and
- can impact on emotional/psychological well-being and self-esteem, especially among young people.
Prevalence of Obesity in Northern Ireland
Adults
1.7 The 2005 Northern Ireland Health and Social Wellbeing Survey (HSWB) found that overall 59% of all adults measured were either overweight (35%) or obese (24%). The 2005 Survey also reported that 64% of adult males and 54% of adult females were either overweight or obese (compared to 63% and 50% for men and women respectively in the 1997 survey). By comparison the Scottish Health Survey 2003 also recorded Scotland at 24%. The National Audit Office in their report: Tackling Obesity in England, recorded adult obesity prevalence in England at 23% and
Children & Young People
1.8 The position is also particularly worrying among our children and young people. Data from the NI Child Health System indicate that in 1997/98, based on measurements carried out during the primary one health appraisal, approx 4% of children aged around 5 were found to be obese with 17% classified as being overweight or obese. In 2004/05 more than 5% of children were obese with 22% classified as being overweight or obese. Using this data it has been projected that without significant intervention just over 7% of children aged around 5 will be obese and almost 27% will be overweight or obese by 2010.
1.9 The following graph sets out the percentage of children in Northern Ireland aged 4 ½ to 5 ½ classified as either overweight or obese, using the international approach, from 1997-98 to 2005-06.
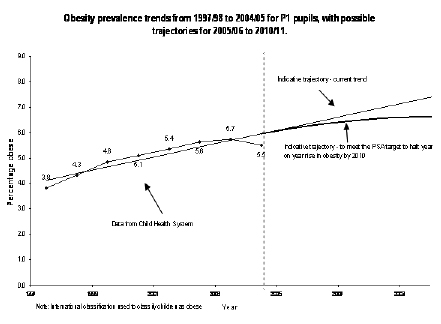
Aetiology of Obesity
1.10 Obesity occurs when an individual takes in more energy through the food and drink they consume than they expend through natural bodily processes and physical activity. The direct cause of obesity is, therefore, an energy imbalance. However, it doesn’t take much to tip the balance. It has been estimated that an average adult whose daily energy intake is just 60 calories more than their energy output will become obese within ten years.
1.11 It is less clear, however, which factors contribute most to tipping the energy balance. In terms of the intake side of the equation, people don’t appear to be taking in more calories, but our current diet contains too much fat and sugar. Eating high fat, energy dense foods can create an overeating effect and contribute to obesity. It is also recognised that evolving eating patterns has a key role to play, for example, there is more snacking and greater dependence on prepared foods.
1.12 In relation to energy use, people today are undoubtedly less active than previous generations and low levels of activity contribute to obesity. The National Audit Office has previously estimated that the extra physical activity involved in daily living 50 years ago, compared with today was equivalent to running a marathon a week.
Obesogenic Environment
1.13 It may seem simplistic that an individual is solely responsible for their weight gain, however research has shown that a very complex range of factors is involved – from biology, through to the built environment, to the advertising people are exposed to everyday. It is therefore unclear the extent to which many individuals are able to make genuine choices.
1.14 Increasingly it has been acknowledged that the causes of obesity are associated with a wide range of inter-related factors, from the physical, socio-economic and cultural environment, which act to promote calorie intake and discourage physical activity. These factors are referred to collectively as the “Obesogenic" environment.
1.15 Several hypotheses have been put forward to explain the increase intake of energy, including:
- increased portion sizes;
- increased energy density of food;
- increased availability of ‘fast foods’; and
- over-advertisement of energy dense foods.
1.16 There are also a range of hypotheses to explain environments that are less conducive to energy expenditure, including:
- mechanisation of tasks which previously required manual labour;
- concerns over the safety of children and an increased perception of risk leading to reductions in outdoor play and physically strenuous games;
- labour-saving devices; and
- sedentary entertainment.
Cost of Obesity
1.17 Across the UK obesity rates have tripled over the last twenty years. A House of Commons Health Committee Report (2003-04) estimates the cost of obesity at £3.7bn per year. Alternatively, the Foresight Report on Obesity estimated that the NHS costs attributable to overweight and obesity projected to double to £10 billion per year by 2050. The wider costs to society and business are estimated to reach £49.9 billion per year (at today’s prices).
1.18 It has been estimated that in Northern Ireland obesity is resulting in 260,000 working days lost each year and is costing the economy approximately £500 million.
1.19 The Northern Ireland Clinical Resource Efficiency Support Team (CREST) on managing obesity also estimated that just stopping the year-on-year increase in levels of obesity would save the Department £210 million over the next twenty years (June 2005).
1.20 The recent Northern Ireland Audit Office report refers to a number of the consequences of obesity and diabetes. It reports that the treatment of those suffering from diabetes is reckoned to cost the health services across the UK around £1 million every hour.
2.0 Obesity Prevention Policy
Policy Background
2.1 The Northern Ireland Assembly’s Programme for Government identified working for a healthier people as one of five overarching priorities. Investing for Health (IfH), published in March 2002, is Northern Ireland’s Public Health Strategy, and it sets out how these commitments are to be met. The strategy outlines the approach to improving health and wellbeing, reducing health inequalities and also provides a framework for efforts to achieve this commitment.
2.2 Even before the publication of IfH, the Department of Health, Social Services, and Public Safety had recognised the relationship between a healthy diet, physical activity and good health, especially in respect of Coronary Heart Disease. For example these issues were key elements in the “Change of Heart" programme that operated in the 1980s and 1990s. Subsequently work was undertaken to develop separate food and nutrition and physical activity strategies. However, more recently there has been a greater acceptance of the need to develop an integrated approach to obesity.
2.3 The Ministerial Group on Public Health (MGPH), which oversees the ongoing policy development and implementation of IfH, became particularly concerned about the quickly rising levels of obesity in Northern Ireland – especially among children and young people. Therefore in 2004 MGPH established the Fit Futures Taskforce to examine options for preventing overweight and obesity in children and young people, and to make recommendations for integrated, cross-Departmental Action to MGPH.
Development of Fit Futures
2.4 To take forward this work, the Fit Futures Taskforce initiated wide-ranging research and engagement processes. To develop the evidence base for the recommendations the research aspect included:
- developing a local research and information baseline;
- conducting a review of the international evidence base; and
- carrying out comparative research, including looking at approaches in other countries.
2.5 In addition, a number of consultation and engagement events and workshops were held with key stakeholders, including young people and their parents. At the same time literature and desk reviews were commissioned which looked at the current evidence base relating to prevention and good practice. A particular focus was placed on looking at effective policies and programmes that were currently in operation.
Summary of the Fit Futures Report
2.6 The final report of the Fit Futures Taskforce was published in 2006; it identified a number of priority approaches and made over 70 recommendations for action.
2.7 The Key Principals of Fit Futures are set out below:
- providing leadership and leading by example;
- building on existing good practice;
- adopting an holistic and long-term approach;
- focussing on environmental and lifestyle factors;
- taking account of key motivating factors;
- being positive and encouraging to help young people develop a sense of self esteem and self worth;
- adopting a population approach;
- reflecting the importance of early years and the significant role of parents and carers;
- ensuring Schools fulfil a key role;
- recognising the importance of basic knowledge and skills in the community; and
- being evidence based.
2.8 One of the key points made by the report was the recognition that, given the obesogenic environment, the Department of Health, Social Services and Public Safety (DHSSPS) could not effectively address this issue on its own. It therefore contained a joint target, between DHSSPS, the Department of Education (DE), and the Department of Culture, Arts and Leisure (DCAL), “to halt the rise in obesity in children by 2010".
Fit Futures Implementation Plan
2.9 Based on the responses to the Fit Futures report, an Implementation Plan was developed and published for consultation in February 2007. This consultation process was used to inform further policy development on this issue. Following the consultation period full consideration was given to comments received and to the emerging policy environment.
2.10 Shortly after the publication of the implementation plan, strategic and policy developments from elsewhere reinforced the need to develop a whole population approach to the issue. This was particularly informed by the “Foresight" report (see paragraphs 2.16-2.19) which was launched in October 2007.
2.11 Reflecting on these developments, the Department decided to integrate Fit Futures into the development of a broad strategic framework to address obesity across the life course. Therefore, while this implementation report was not formally published by the Department, progress has been, and continues to be, made to deliver on its recommendations and actions at both the regional and local level.
2.12 Although the strategic emphasis is currently on developing an integrated obesity framework, the Department does recognise the need to incorporate elements relating to physical activity and food and nutrition. At this stage, therefore, the Department is not planning to develop separate strategies for these areas, but it will ensure that they are fully incorporated into the overarching framework, and that relevant outcomes and outputs are developed in relation to physical activity and food and nutrition. Meanwhile, the Department has established a process to oversee the delivery of Fit Futures and develop a life course approach to preventing obesity (see Section 3).
Funding
2.13 DHSSPS allocated £832,000 to the implementation of Fit Futures in 08/09. In addition, a further £550,000 and £300,000 has been allocated for work around promoting physical activity and improving food and nutrition respectively.
Local Delivery
2.14 Much of the funding set out in paragraph 2.13 has been allocated to the local Health and Social Services Boards to deliver local actions, activities and programmes aimed at meeting the needs of their local populations and helping to prevent obesity.
2.15 As part of Fit Futures, the Investing for Health Partnerships in each Board area were tasked under a Priorities for Action target to develop and deliver local integrated Fit Futures Plans. This work continues to be taken forward at a local level.
Obesity Policy Developments
2.16 In 2005, the Westminster Government commissioned Foresight to carry out a systematic review of obesity. Foresight reported its findings ‘Tackling Obesities: Future Choices’ Project in October 2007 – and this has informed local policy development and the Department’s decision to undertake a life course approach to preventing obesity.
2.17 Foresight is the Westminster Government’s science futures think tank based in the Government Office for Science. The aim of the programme is to build on the scientific evidence base to provide challenging visions of the future to help inform government strategies, policies and priorities.
2.18 The UK wide project looked at how to respond sustainably to the prevalence of obesity in the UK over the next 40 years, and its key findings include:
- most adults in the UK are already overweight. Modern living ensures every generation is heavier than the last – `Passive Obesity’;
- by 2050 60% of men and 50% of women could be clinically obese. Without action, obesity-related diseases will cost an extra £45.5 billion per year;
- the obesity epidemic cannot be prevented by individual action alone and demands a societal approach;
- tackling obesity requires far greater change than anything tried so far, and at multiple levels: personal, family, community and national; and
- preventing obesity is a societal challenge, similar to climate change. It requires partnership between government, science, business and civil society.
2.19 A copy of the ‘Tackling Obesities: Future Choices’ Foresight Project is available on Foresight’s website at: http://www.foresight.gov.uk/.
England
2.20 England published their cross-Government Strategy, “Healthy Weight, Healthy Lives" in January 2008 and can be found at; www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_082378.
Scotland
2.21 In June 2008 Scotland published an action programme covering healthy eating, physical activity and healthy weight called Healthy Eating, Active Living: An action plan to improve diet, increase physical activity and tackle obesity (2008-2011) which can be found at www.scotland.gov.uk/Publications/2008/06/20155902/0.
2.22 This builds on, rather than replaces, the existing delivery of the Physical Activity Strategy and Diet Action Plan. The strategic spending review 2007 has committed an additional £40 million over the next three years to delivering in these three interlinked policy areas.
Wales
2.23 On 29 June 2006 the Food and Fitness Implementation Plan for Children and Young People was launched by the Welsh Assembly. This can be found at http://wales.gov.uk/topics/health/improvement/food/food-fitness/plan/?lang=en.
2.24 A new Welsh Assembly Government-funded programme designed to help overweight and obese children manage their weight and become fitter, healthier and happier was rolled out across Wales from 20 January 2009. The £1.4 million scheme will target around 2,000 children aged between 7-13 years old and their families over the next three years.
Wider Europe
2.25 These developments also informed our thinking on this issue, along with a range of other policy developments across a range of European countries (A paper by WHO Europe entitles “Nutrition, Physical Activity and Prevention of Obesity: Recent Policy Developments in the WHO European Region" – provides a very useful summary of these developments and can be found at www.euro.who.int/Document/NUT/Instanbul_conf_ebd07.pdf.
3.0 Developing a Life Course Approach
Obesity Prevention Steering Group
3.1 To oversee the progress against the Fit Futures recommendations, and lead the development of an overarching policy to prevent obesity across the life course, the Department established the cross-sectoral Obesity Prevention Steering Group (OPSG) in February 2008. In recognition of the emerging policy consensus that acknowledges that obesity is an issue the DHSSPS cannot effectively address on its own, the OPSG also contains a strong representation from other local Government Departments, particularly DE, DCAL, Department of Regional Development (DRD), Department of Social Development (DSD), and Department of Agriculture and Rural Development (DARD). The membership of the steering group and its Terms of Reference are set out at Annex A.
Advisory Groups
3.2 In recognition of the wide range of areas and issues that form the obesity context, four policy advisory sub-groups have been established to support the work of the OPSG. This approach also acknowledges the particular role that food and nutrition and physical activity must play in addressing obesity. These groups, which have similar terms of reference to the OPSG, are:
- the Food and Nutrition Advisory Group;
- the Promoting Physical Activity Advisory Group;
- the Education, Prevention and Public Information Advisory Group; and
- the Data and Research Advisory Group.
3.3 As an initial step, each Advisory Group, whose membership is set out in Annex B, considered the appropriateness of their terms of reference and sought to identify additional members who would be essential in taking forward this work.
3.4 Following initial discussion the Advisory Groups considered the progress to date against the outcomes in Fit Futures, and set out any future plans to address these. Subsequently the groups have been considering the ongoing appropriateness of these actions aimed at addressing childhood obesity and have begun to revise them in order to form the early years, and children and young people sections of an overarching obesity prevention framework. This will ensure that the good work taken forward under Fit Futures is not lost within the life course approach and will instead be used to inform and lead the development of this policy.
Obesity Strategic Framework
3.5 The next step is for the OPSG, and the Advisory Groups, to look forward and decide what outcomes they would like to see achieved in the next 5 and 10 years. This forward looking piece of work will allow the development of a range of short, medium, and long term outcomes and actions using the logic model approach (see Annex D for further information).
3.6 It is anticipated that this development process will take place over the next financial year. However, this work will not prevent action on this issue in the interim. Work will continue on delivering on the revised Fit Futures recommendations, and on programmes aimed at preventing obesity in the adult population.
North/South/East/West
3.7 It is clear that this is an issue that is facing much of western society and not just Northern Ireland. In particular, we are keen to learn from and build on the work taken forward within the other UK jurisdictions. To this end, an informal four nation, Information sharing sub-group has been established. This has allowed us to build relationships and knowledge in this area, and learn from good practice and research undertaken elsewhere.
3.8 We also recognise that this is an issue facing Ireland, and we continue to build our relationship with our colleagues there. Outcomes from this cooperation include an all-Island obesity conference held in Belfast on 13-14 November 2008, the running of the “Little Steps, Go a Long Way“ campaign developed by Safefood across the island, and the establishment of an all-island Obesity Observatory.
3.9 It is anticipated that the links that have been developed will be used to inform the development process. It will also provide the opportunity, where appropriate, to take forward work on a joined up consistent basic and potentially allow us to gain again from economy of scale.
4.0 Obesity Treatment
Primary Care
4.1 Primary Care has an important role in the identification, assessment and management of obesity. Obesity Management is integral to the management of other conditions such as coronary heart disease, stroke, atrial fibrillation and diabetes.
Investments in primary care
4.2 The 2004 General Medical Services contract brought significant investment in General Medical Services (GMS) in Northern Ireland. The size, scale and scope of the investment in primary care, together with the incentives for practices to improve the quality and outcomes in treating acute and chronic health problems, facilitated the concentration of General Practitioners and their staff on the delivery of high quality primary care. GMS funding flows via three main funding streams, Global Sum, Enhanced Services and the quality of care to patients across a range of common chronic diseases through the Quality and Outcomes Framework (QOF).
Quality and Outcomes Framework (QOF)
4.3 QOF is a fundamental part of the GMS Contract; it remunerates GP practices for providing good quality care to their patients and it helps to fund work to improve further the quality of care provided.
4.4 Clinical standards is one of the four main components of the quality framework. Since April 2006, the QOF has included an indicator for practices to set up a register of patients aged 16 and over who have a Body Mass Index (BMI) equal to or greater than 30kg/m2. The extension of the existing QOF indictor on obesity was to encourage practices, by way of an incentive, to provide interventions, that would, based upon the best available evidence and recommendations by the National Institute for Clinical Excellence (NICE), reduce the prevalence and severity of conditions linked to obesity.
Directed Enhanced Service (DES)
4.5 Further, by way of a Directed Enhanced Service (DES), since 2006, additional funding approximately £800k has been provided to build on the capacity of practices to play an important role in the service provision for early detection and provision of necessary follow-up of patients who have a BMI of 30kg/m2 who are likely to develop morbidity such as diabetes mellitus. The service is directed at helping those patients with obesity with or without other co-morbidities.
4.6 In relation to this DES practices are required to develop a written protocol for such patients, that includes:
- the frequency of repeat weight measurement, testing for blood lipids and glucose;
- if the service is available, the physical activity referral process;
- criteria for anti-obesity drug treatment;
- description of the contents of the practice resource kit available to such patients; and
- description of the follow-up protocols for such patients, including routine blood pressure monitoring and thyroid function tests;
- undertakes to offer, for those patients who smoke, referral to local specialist smoking cessation services and provide all relevant information to motivated patients;
- undertakes to offer and record an annual follow-up treatment plan for those patients identified with lipid or glucose abnormalities, e.g. impaired glucose tolerance; and
- a requirement that the contractor (practice) develop a practice resource kit for, and provides such a kit to motivated patients with a BMI greater than 30 who are likely to develop morbidity such as diabetes mellitus;
4.7 In addition, there is a requirement for practices to ensure that any health care professional who is involved in the management and treatment of patients has the necessary experience, skills and training with regard to the identification and treatment of patients with a BMI greater than 30 who are likely to develop morbidity such as diabetes mellitus, and training needs in relation to those areas outlined are regularly reviewed.
4.8 Full details of the service description relating to this DES can be found at: http://www.dhsspsni.gov.uk/index/hss/gp_contracts/gp_contract_directions.htm.
Current status in Northern Ireland
4.9 All the practices in Northern Ireland have participated in the QOF since its introduction in April 2004. In relation to co-morbidities areas the achievement points were in the range of 99% to 99.8%. The 2007/08 QOF achievement figures by practices in Northern Ireland illustrate the commitment of GPS quality patient care. Furthermore Practices achieved the maximum points available in relation to the DES relating to obesity
4.10 The Department has continued to offer incentives to primary care practitioners to enhance and develop their services through the QOF and the DES initiatives. In 2009, the treatment of mild to moderate depression was included as a DES. Whilst this DES is not directly linked to the treatment of obesity it is generally recognised, although not in all cases, that there are psychological consequences of obesity such as lower self esteem or social isolation. By assessing patients who suffer from mild to moderate depression it may be possible to establish that their depression is linked to low self esteem as a result of obesity and appropriate intervention may be offered to address both conditions.
4.11 Although there is no data currently available to demonstrate the cost effectiveness of primary care interventions as a result of the incentives provided through the QOF and the DES initiatives, evidence suggests that even a modest weight loss of 5-10 % of body weight in an obese person can result in health and well-being benefits and thus should result in cost savings in health care.
4.12 Finally, the Department continues to look for opportunities within the GMS contract to address obesity issues. However, as the contract is UK wide areas identified will have to be agreed across the 4 UK Health Departments before they can be implemented.
Secondary Care
4.13 However, it is recognised that the problem of obesity cannot be addressed through primary care management alone. While services may be mainly primary care-based they interface with secondary care in many ways. The growing epidemic of obesity has practical implications for hospital services in terms of transport, accommodation and equipment to manage increasingly heavy patients as well as the increasing pressure on services due to the adverse impact that being overweight/obese has on people’s health.
4.14 Patients with significant weight management/obesity issues which may be directly or indirectly linked to their condition are seen and treated in almost every service within secondary care. These include diabetes, cardiology, respiratory (e.g. sleep apnoea), rheumatology, cancer care, surgery, maternity, infertility and mental health. Historically it has been the presenting condition that is treated and managed, although obesity issues may be one of a number of contributing factors in the development of the disease/condition.
4.15 Health and Social Care Trusts are taking steps to address the challenges presented for secondary care services by the growing numbers of patients who are significantly overweight or obese. For example:
- education programmes for diabetes which inform people about diet, nutrition and exercise as part of lifestyle advice and self management of their condition, are held in both primary and secondary care settings;
- patients for whom surgery is planned will receive general advice in relation to good diet, BMI at day surgery pre-assessment and referral to dietician if appropriate. Pre-operative assessment will include advice on weight loss as part of the patient’s pathway to recovery; and,
- weight management advice is offered to patients who may have established cardiovascular risk or are waiting for cardiac surgery. Patients may also be referred to initiatives which provide physical activity support.
4.16 Nutrition and Dietetic Services can provide proactive services for patients with weight management or obesity issues across the range of secondary care hospital based services. Referrals of inpatients are normally made at the consultant’s discretion and the dietetic service can provide advice and guidance with diet and lifestyle. Outpatient referrals may also be made to dietetics in relation to patients with co-morbidities such as diabetes, cardiology, cardiac rehabilitation programmes, surgery and general medicine.
4.17 It is recognised, however, that specialist supporting dietetic services need to be further developed to meet current and anticipated future demands. There will need to be additional staff, primarily dieticians and nurses, and training/specialist knowledge enhanced in secondary care. All this will require investment, and will need to be considered in light of other competing priorities for health and social care funding.
Bariatric Surgery
4.18 The management of obesity can be challenging, and patients for whom a dietary approach has been unsuccessful, surgery (usually referred to as bariatric surgery) may be considered. Bariatric surgery is the term used to describe a range of surgical procedures which are carried out to modify the gastrointestinal tract to reduce the intake and/or absorption of food. There are two main types of bariatric surgery:
- Restrictive – where the size of the stomach is restricted so the person feels full with less food. Restrictive procedures include gastroplasty and gastric banding;
- Malabsorptive – where parts of the gastrointestinal tract are bypassed to limit the absorption of food. Malabsorptive procedures include jejunoileal bypass, gastric bypass and biliopancreatic diversion.
4.19 Surgical management is complex and involves not just the surgical operation but extensive care and support from a range of professionals both before surgery and on an ongoing basis after the operation. A patient will need multidisciplinary team assessment to consider if there are underlying medical conditions which need treatment; exclude serous psychological problems which could result in poor outcomes; and confirm they understand the benefits and risks of the surgery, as well as their ability to adhere to the long-term dietary changes needed if surgery is to be successful. Dietary management after surgery may require specialised support to avoid serious complications.
NICE Guidelines
4.20 On 22 October 2008, the Department issued a circular endorsing a National Institute for Health and Clinical Excellence (NICE) clinical guideline on obesity as applicable to Northern Ireland. NICE clinical guidelines are not mandatory and are endorsed as developmental standards. The HSC is expected to take account of the guidelines in their future planning and delivery of services to patients who are obese or overweight; however in determining their priorities for service development, commissioners must take into account local circumstances, the strategic objectives established for the HSC and competing demands and pressures for a wide range of health and social care services generally.
4.21 The NICE guideline recommends that bariatric surgery to aid weight loss should be available to patients meeting certain body mass index (BMI) criteria. Commissioners have estimated that there are more than 50,000 people in NI who could be eligible using these criteria. Although NICE estimates that only 2-4% of these people would come forward for surgery, this is by no means certain. The cost of treating only 2% of the eligible population and providing the necessary life-long follow-up would be in the order of £20 million. If more people come forward, the cost would rise pro-rata.
4.22 A comprehensive bariatric surgery service is not available in Northern Ireland at present. To date arrangements have been put in place for over 120 patients from Northern Ireland to have bariatric surgery in specialist units in England. Lifelong follow up is being arranged locally. £1.5 million has been set aside for the provision of bariatric surgery in the 2008/09 financial year.
4.23 Commissioners are considering options for the commissioning of a bariatric service, including appropriate pre- and post-operative care and ongoing dietary support. The current position is that they are developing a plan to enable patients who stand to benefit most from bariatric surgery to access it. It is anticipated that these arrangements will be put in place for the 2009-10 financial year.
5.0 Summary
5.1 The prevalence of obesity in Northern Ireland presents a major challenge, not just for medicine and public health but for governance and decision making. The deceptively simple issue of encouraging physical activity and modifying dietary habits, in reality, raises complex social and economic questions about the need to perhaps reshape public policy in food production, food manufacturing, healthcare, retail, education, culture and trade.
5.2 There are many and varied contributors to the obesity problem and these are societal as well as individual responsibilities. This idea suggests that understanding and tackling the obesogenic environment is necessary to complement school and family-based interventions.
5.3 There are opportunities for Northern Ireland to take a leading role in this worldwide problem by developing and implementing a cross-cutting, comprehensive, long-term strategy that brings together multiple stakeholders. The Department through its development of an Obesity Prevention Strategic Framework is determined to take on this challenge. The Department also has to face the challenge of treating those who present to the health service. These are not issues that will be solved overnight but will take a structured approach over time.
Annexes
Annex A – Terms of Reference and Membership of the Obesity Prevention Taskforce Steering Group
Annex B – Membership of Advisory Groups
Annex C – Links to Key Documents and Information
Annex D – Logic Model
Annex A
Obesity Prevention Steering Group Terms of Reference
Chair: Professor Ian Young QUB
Role: The Obesity Prevention Steering Group will oversee, co-ordinate and drive forward the implementation of Fit Futures, and to agree the way forward to prevent obesity in the adult population. The Steering Group will provide relevant advice but will not be directly responsible for the allocation of funding.
Secretariat: DHSSPS Health Development Policy Branch
Primary Functions
- To facilitate and oversee the implementation of the recommendations and various actions within Fit Futures.
- To drive forward the implementation of Fit Futures by providing strong and visible leadership.
- To provide advice and strategic direction on all relevant issues relating to obesity, including the development of an approach to tackle obesity in the adult population.
- To consider the need for additional resources to assist effective implementation and monitoring of Fit Futures.
- To monitor progress against targets and produce a report on progress on implementation for the Ministerial Group on Public Health at the end of year one.
Performance Management Arrangements
- To develop appropriate data collection arrangements in order to allow for monitoring of progress.
- To develop a mechanism for regular reporting to the steering group by relevant organisations.
Annex A
- To identify barriers to progress, and subsequently feedback relevant issues and possible solutions to MGPH and other relevant organisations.
- To publicise progress were appropriate.
Membership:
Membership of the Obesity Prevention Steering Group will be drawn from as wide a range of organisations as possible, including the statutory sector and voluntary/community organisations.
Those steering group members representing the statutory sector must:
- work at a senior level in their organisation and be able to report on progress;
- have overall responsibility for this area within their organisation; and
- have access to the most senior levels in their organisations.
Those steering group members representing the voluntary/community sector must:
- be able to demonstrate an intimate knowledge of community based obesity prevention initiatives; and
- be able to offer considered opinion on a broad range of obesity related matters; and
be able to provide feedback on the work of the steering to the wider community network.
Annex A
Advisory Groups and Reporting Structure
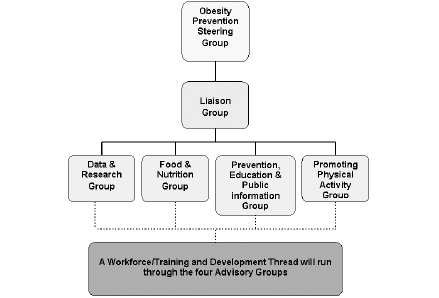
Annex A
Membership of Obesity Prevention Steering Group and Advisory Groups
OBESITY PREVENTION STEERING GROUP MEMBERSHIP
Prof. Ian Young – Queens University Belfast (CHAIR)
Andrew Dougal – NICHSA
Andrew Elliott – DHSSPS
Andy Bready – DRD
Angela McComb – HPA
Anne Madden – NICHSA
Brendan Bonner – WHSSB
Ciaran Mee – DCAL
Claire Wright – DHSSPS
Dr Michael McBride – DHSSPS
Dr Naresh Chada – DHSSPS
Gary Maxwell – DHSSPS
Gerry Bleakney – EHSSB
Hilary Johnston – NHSSB
Iain Foster – Diabetes UK
Ian McClure – DHSSPS
Jacqueline O’Loughlin – Playboard
John News – Sport NI
Lynn Donnelly – SHSSB
Lynne Smart – SHSCT
Maria Jennings – FSANI
Marian Faughnan – Safefood Ireland
Martina McNulty – NILGA
Mary O’Neill – NHSCT
Maura O’Neill – WHSCT
Nick Harkness – Sport NI
Prof. Barbara Livingstone – University of Ulster, Data
Rob Phipps – DHSSPS
Sam Knox – SGEHC
Sharon Lawlor – D.Ed
Siobhan Fitzpatrick – Early Years (NIPPA)
Sonia Montgomery – WHSCT
Annex B
ADVISORY GROUP MEMBERSHIP
Food & Nutrition
Maria Jennings (Chair) - Food Standards Agency
Alan McMullan - DE
Andrea Marnoch - Food Standards Agency
Andrew Dougal - NICHSA
Angela McComb - Health Promotion Agency
Cliodhna Foley Nolan (or rep) - Safefood
Gerry Bleakney - EHSSB
Caroline Kerr - Playboard
Judi McGaffin - WHSSB
Glynis Henderson - CCEA
Martina McNulty - Southern Group Environmental Health
Mandy Gilmore - Southern Trust
Maura O’Neill - Western Trust
Rob Phipps - DHSSPS
Ian McClure - DHSSPS
Claire Wright (Secretariat) - DHSSPS
Physical Activity
Nick Harkness (Chair) - SportNI
John News - SportNI
Brendan Bonner - WHSSB
Gillian McClay - Playboard
Jill Fitzgerald - DE
Kim Kensett - EHSSB
Ciaran Mee - DCAL
Neil McGivern - SEELB
Andy Bready - DRD
Nicola Browne - Health Promotion Agency
Jack Palmer - DCAL
Sabrina Lynn - Southern Trust
Valerie Richmond - Limavady Council
Rob Phipps - DHSSPS
Ian McClure - DHSSPS
Gary Maxwell - DHSSPS
Claire Wright (Secretariat) - DHSSPS
Data & Research
Prof Barbara Livingstone (Chair) - UU
Frank Kee - QUB
Ruth Balmer - FSA
Annex B
Gillian Gilmore - HPA
Nicola Armstrong - Research & Development Office
Hilary Johnston - NHSSB
Helen McClure - DE
Marita Hennessey - Safefood
Kevin Balanda - Institute of Public Health for Ireland
Dr Christine McMaster - EHSSB
Kieron Moore - DHSSPS
Bill Stewart - DHSSPS
Rob Phipps - DHSSPS
Gary Maxwell - DHSSPS
Claire Wright (Secretariat) - DHSSPS
Prevention, Education & Public Information
Siobhan Fitzpatrick (Chair) - Early Years (formerly NIPPA)
Denise Boulter - DHSSPS (Nursing)
Anne Madden - NICHSA
Sharon Gilmore - FSA
Andrew Castles - Safefood
Andy Bready - DRD
Jill Fitzgerald - DE
Rob Phipps - DHSSPS
Ian McClure - DHSSPS
Claire Wright (Secretariat) - DHSSPS
Annex C
Links to key Documents and Information
Foresight Tackling Obesities: Future Choices:
http://www.foresight.gov.uk/
Healthy Weight, Healthy Lives:
www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_082378
Little Steps – go a long way:
www.littlesteps.eu/site/contact
Fit Futures:
www.dhsspsni.gov.uk/ifh-fitfutures.pdf
Fit Futures Implementation Plan:
www.dhsspsni.gov.uk/fit-futures-implementation-plan.pdf
Northern Ireland Audit Office report on Obesity and Type Two diabetes:
www.niauditoffice.gov.uk/pubs/onereport.asp?
Investing for Health (IfH), published in March 2002:
www.dhsspsni.gov.uk/show_publications?txtid=10415
WHO: “Nutrition, Physical Activity and Prevention of Obesity: Recent Policy Developments in the WHO European Region":
www.euro.who.int/Document/NUT/Instanbul_conf_ebd01.pdf
GP Contracts:
www.dhsspsni.gov.uk/index/hss/gp_contracts/gp_contract_directions.htm
National Institute for Health and Clinical Excellence (NICE) clinical guideline:
www.nice.org.uk/Guidance/CG43
House of Commons Health Committee Report (2003-04):
www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4098721.pdf
National Physical Activity Strategy ‘Let’s Make Scotland More Active’ www.sctoland.gov.uk/Publications/2003/02/16324/17896
Scotland’s White Paper on Nutrition, Overweight and Obesity May 2007 www.scotland.gov.uk/Topics/Government/International-Relations/Europe/EuropeanStrategy/EU-Priorities/PriorityNutrition
Annex C
Health Eating, Active Living: An action plan to improve diet, increase physical activity and tackle obesity (2008-2011) www.scotland.gov.uk/Publications/2008/06/20155902/0
Food and Fitness Implementation Plan for Children and Young People
Welsh Assembly:
http://wales.gov.uk/topics/health/improvement/food/food-fitness/plan/?lang=en
Annex D
Logic Model
In its simplest form, the logic model analyzes work into four categories or steps: inputs, activities, outputs, and outcomes. These represent the logical flow from:
1. inputs (resources such as money, employees, and equipment) to
2. work activities, programs or processes, to
3. the immediate outputs of the work that are delivered to customers, to
4. outcomes or results that are the long-term consequences of delivering outputs.
The basic logic model typically is displayed in a diagram such as this:
INPUTS --> ACTIVITIES OR PROCESSES --> OUTPUTS --> OUTCOMES
This can also be expressed thus:
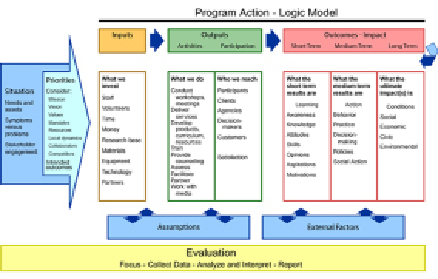
Logic models have been developed elsewhere in respect of addressing obesity. They facilitate a focus on outcomes, but also enable an integrated approach (cross-sectoral) to be developed.
Additional Information from Department for Health,
Social Services and Public Safety
Apologies for the delay in replying to your query, at present there is no recurrent funding for bariatric surgery in Northern Ireland. The HSC Board does not routinely commission bariatric surgery although they may consider applications for funding where exceptional clinical circumstances are present.
The replies to your three questions are as follows:
1. Approximately 80 patients had surgery outside NI in 2008/09 year. The background to these cases was that non-recurrent funding was made available in 2005 to permit a number of bariatric procedures to be carried out at the Royal Group of Hospitals to clear the then waiting list of twelve. Subsequently, a number of consultants accepted referrals of patients for consideration of bariatric surgery, in anticipation that a local bariatric service might be introduced. A moratorium was imposed on such referrals in October 2007, but by then over 100 patients had been given an expectation of treatment. The legacy Health Boards made arrangements for a one-off initiative to offer these patients assessment and treatment in England which completed during the 2008/09 year. Of this cohort, 80 proceeded to surgery.
For 2009/10 year the legacy Health Boards agreed to fund a short term bariatric services pilot with a budget of £1.5m and a target of providing treatment in England during the year for between 100 and 150 patients. This is ongoing and it is not clear at this time how many people will be treated by the end of the pilot as some may actually need more than one surgical procedure.
2. No. The Department has no plans at this time to provide this surgery in Northern Ireland. The Department is awaiting an evaluation of the pilot exercise which will not end until March 2010. Any future proposals for a bariatric surgery service will have to find funding at that time.
3. It is estimated that there are more than 50,000 people in NI who could be eligible for bariatric surgery using NICE Criteria. Although NICE estimate that only 2 - 4% of the eligible population would come forward for surgery, this is by no means certain. The cost of treating 2% of the eligible population (i.e 1,000 patients) and providing the necessary long term follow up would be in the order of £10m. If more than 2% came forward the resource would rise on a pro rata basis. This estimate is based on current NICE guidance for patients with BMIs of > than 35 with co morbidities or patients with BMI’s > than 40 without.
The Pilot in Northern Ireland is currently offered within a more restricted referral criteria. The patient must have a BMI of > than 50 with co morbidities or > than 60 without co morbidities. These criteria were selected on the basis that they were considered to target the group of patients who would be most likely to have the best health improvement as a result of substantial weight loss.
The 2005 Health and Well Being Survey estimated that at that time there were almost 13,500 people in Northern Ireland with a BMI of > than 50. Figures are not readily available for those with a BMI > than 60. We do not have any guidance or a methodology to assess how many of those with BMIs > than 50 would come forward and be considered clinically appropriate for surgery.
Secondary Care Directorate
Ards Borough Council
Environmental Health Service
With the assistance of funding from Fit Futures, the Environmental Health Service is piloting a schools programme looking at ‘Safe and Healthy Lunchboxes’. The programme is aimed at teaching Key Stage 3 pupils about a balanced diet, the ‘eat well’ plate and how to adapt this to their lunchboxes. The programme provides pupils with the knowledge and understanding to make healthier choices for their lunches. It is hoped that, following the pilot, the programme will be offered to all secondary schools within the Borough.
Leisure Services
The Council has three leisure centres as well as a range of outdoor recreation grounds throughout the Borough. The leisure centres have a wide range of facilities to suit the whole family, from small children to the over 60s. These facilities allow all residents of the Borough access to physical activity along with assistance from fully qualified fitness instructors. Within the leisure centres, specialist programmes to tackle obesity are also run. These include:
- FRESH Programme – Currently in the second part of the pilot, the 12 week programme tackles childhood obesity by assisting children to maintain their weight through an educational programme containing two activity sessions each week. School nurses identify overweight or obese children for the programme. The programme is funded by Fit Futures.
- Healthwise Scheme – This scheme is run in conjunction with the South Eastern Health and Social Care Trust and allows participating GPs, nutritionists, physiotherapists and specialist nurses to prescribe exercise to patients they think will benefit from supervised physical activity. Leisure Centre staff are trained to advise individuals on conditions such as high blood pressure, diabetes and obesity and provide them with suitable exercise programmes. The scheme receives approximately 350 referrals each year with 30% of those having obesity issues.
- Momentum – Momentum Gym staff provide ongoing help, advice and motivation as well as assisting to set a programme of exercises designed to help each individual reach their goals, including weight loss.
- Momentum Healthy Eating Plan – This is available to all members to assist them to keep track of what they eat, change their diet, lose weight and provide help and advice on what they should be eating. The package includes a daily food diary for 6 weeks, a Glycemic Index food list, recipes and tips on healthy eating. Measurements and body fat analysis are taken in the first and last weeks of the programme, along with weekly weigh-ins. Momentum staff can also provide advice on weekly diets and make suggestions for improvement.
- Multi Skills - The Multi Skills Club is aimed at children between 5-9 years. The club is not sport specific but develops basic movement and sports skills with the aim of encouraging children to get more active.
Action Cancer
Body weight is controlled by the physiological balance between energy intake as food and drink and energy expenditure in activities of daily living such as work and leisure. When the balance is not maintained, the result is gaining weight. Obesity is defined as an excess of body fat as measured by body mass index (BMI) ratio in adults, but is also now being used to classify many of our children too. There is concern regarding the populations increasing weight and escalating levels of obesity because of the increasingly recognised connections between obesity and other health issues, such as heart disease, liver disease and cancer. Cancer Research UK (CRUK) has highlighted that the majority of individuals do not realise that obesity is the second biggest risk factor for developing some types of cancer.
Adults
In 1997 it was estimated that in Northern Ireland almost half of all men and more than one third of women are overweight, while one fifth of men and one quarter of women were classed as obese. More recently, however, the 2005/6 NI Health and Wellbeing Survey (NIHWS) highlighted that a similar proportion of men (24%) and women (23%) were obese. In addition, men were more likely (64%) than women (54%) to be overweight in some way. The change in these figures, over a relatively short period of time, is an indication of the growing problem.
Children
Obesity in children is becoming one of the most common childhood health problems in Europe and has the greatest impact for future negative health consequences. With current estimations indicating that 20% of boys and 18% of girls Northern Ireland’s primary school children are classed as overweight and obese, this has serious implications for the future health of our communities (Yarnell, JWG, McCrum EE, Paterson CC, Skidmore P, Shields MD, McMahon J and Evans AE (2001) Prevalence and awareness of excess weight In 13 and 14 year olds in Northern Ireland using recent international guidelines. Acta Paediatrica, 90, 1435-1439).
Contributing factors
Many factors have been identified as contributing to weight gain, including but not limited to:
- Increasingly sedentary lifestyles
Only 30% of all people in NI take above the recommended level of physical activity of at least 30 minutes per day on five days a week. In addition, 23% of people said that they were not regularly active in the previous six months and did not intend to be so in the next six months (NIHWS).
- Changes in eating patterns
The Department for Environment Food and Rural Affairs (DEFRA, 2006) report that the amount of energy derived from fat (37.7%) is still above the recommended level of 35%. Energy from saturated fatty acids (14.8%) is, also, still above the recommended 11%. Increased snacking on foods rich in fat and sugar and increased dependence on convenience foods, such as takeaways, can have large quantities of hidden fat and therefore are a very high source of calories. In addition, when examining the purchases of fruit and vegetables throughout the UK, quantities purchased for the household were lowest in NI.
- Social Class
There is some evidence to suggest that there is a correlation between poverty and obesity. People on lower income have higher propensity for fast food diets and food with little nutritional value. Additionally, people with little disposable income are less motivated to engage in regular exercise due to the high costs associated with gyms or sports clubs (Inequalities and Unfair Access Issues Emerging from the DHSSPS (2004) “Equality and Inequalities in Health and Social Care: A Statistical Overview" Report).
When examining the information, however, an interesting point to note is the energy intake from all food and drink was 1.8% lower than the previous year, continuing a long-term gradual decline (DEFRA, 2006). This begs the question, if energy intake from food and drink is declining, why is obesity still increasing? Is this an indication that the major contributing factor to obesity is a sedentary lifestyle?
In addition to the above findings, some work carried out on Action Cancer’s Big Bus mobile unit (which travels across Northern Ireland) highlights some specific information in relation to the lifestyle of those in our communities. The Big Bus provides people access to health checks (where an individual can have their blood pressure, BMI and cholesterol checked). Since September 2006, 4640 people have accessed this service. Of the 4640, 3885 requested their blood pressure be checked and because their BP was above normal 56% were referred to their GP. With regards to BMI, 2768 chose to find out their BMI. The average BMI of this group was 28 (minimum 17, maximum 53) above the healthy level of 25. Finally, of the 2509 that had their cholesterol checked, 27% were referred to their GP for increased cholesterol.
With regard to other health behaviours, all those accessing the health check service are asked about their lifestyle. A total of 75% reported that they think their diet is healthy, yet only 51% report that they eat five portions of fruit and vegetables each day, 52% report eating oily fish at least once a week, 59% avoid adding salt to their food and 51% avoid sugary foods. In addition to the eating patterns of our users, 84% report that they exercise less than twice a week and only 6% report exercising over 5 times a week.
The discrepancies between the individuals actual diet and their perceived diet require further investigation, however, they could indicate an additional factor for growing obesity levels, i.e. individuals may believe they are being healthy when in fact they are not.
Dealing with the problem
Increasing obesity levels is a global epidemic and as such various strategies, recommendations and initiatives (focusing on prevention, identification, assessment and treatment) are being implemented by governments worldwide. Preventing weight gain can reduce the risk of many cancers and it is recommended that healthy eating and physical activity habits are established early in life to prevent unhealthy weight gain and obesity. Those who are already overweight or obese are advised to avoid additional weight gain, and to lose weight through a low-calorie diet and exercise. Even a weight loss of only 5 to 10 percent of total weight can provide health benefits (Vainio H, Bianchini F. IARC handbooks of cancer prevention. Volume 6: Weight control and physical activity. Lyon, France: IARC Press, 2002). Within Northern Ireland, a number of strategies are the basis of many programs that aim to tackle the obesity problem. For the health promotion work of Action Cancer the Investing for Health strategy forms the basis of program objectives.
Investing for Health strategy (IFH)
The main objectives of IFH are to:
(1) Stop the increase in the levels of obesity in men and women.
(2) Increase the levels of physical activity and address the issue of sedentary behaviour
(3) Promote the benefits of a balanced healthy and affordable diet.
At Action Cancer numerous programmes have been developed for work with young people and adults. All focus on improving health behaviours associated with the development of cancers, including healthy eating and exercise:
- Health Action
The aim of Health Action is to raise awareness of what you can do to reduce your risk of getting cancer as adults. It is a unique programme that successfully increases the knowledge levels of Key Stage 3 and Key Stage 4 pupils. It is important to know that if you take care of yourself now when you’re young; it’s one of the best choices you can make for leading a healthier, happier and longer life.
The programme content focuses on healthy eating, exercise, sun safety, smoking, alcohol and early detection, with an optional exercise session, either boxercise or dancercise. The topics covered address the following areas in Northern Ireland Curriculum:
- Key Stage 3 & 4 Learning for Life and Work (Home Economics-Healthy Eating; Personal Development – Self Awareness & Personal Health
- Key Stage 3 & GCSE (Single) Science (Living organisms – Nutrition – Diet/Living organisms-Respiration - Smoking and Health)
- Key Stage 3 & GCSE Home Economics (Diet and Health)
- Key Stage 3 & 4 Physical Education (Health Related Physical Activity)
CCEA have endorsed this programme and encourage schools to make use of such a valuable resource.
- Cook IT Programme
This is a community-based nutrition education programme designed to promote healthy eating on a budget. It aims to raise awareness of the Balance of Good Health and what constitutes a healthy diet. This 6 week course provides an insight into the Balance of Good Health and basic hygiene, and the 5 main food groups. It is a participatory programme combining theory and practice, with group members making and sharing a meal together week 2 to 6.
Other programmes include the Healthy Living and Cancer Awareness programmes, both of which are informal education programmes focusing on increasing knowledge levels of lifestyle behaviours that are linked to increased cancer risk, which also include aspects of healthy lifestyles.
What is working well
Since the health promotion team work in the area of promoting healthy living, with a focus on cancer prevention, we have a great deal of experience with the practicalities of following strategies and initiatives set out by government. Currently, within the area of health promotion, there are a number of aspects we think work well:
- Educating individuals from a young age, is reinforcing healthy messages which they can take into their adulthood, helping develop healthy habits to reduce their risk of developing cancer when they are older.
- The use of a variety of delivery methods within all of our programmes; this assists in the learning process for both adults and young people (Group work, visual aids, DVDs).
- Reaching large numbers of young people right across Northern Ireland through our Health Action programme, therefore the key messages are being highlighted on a province wide basis.
- Media coverage highlights our programmes, which in turn helps to engage the public in healthy lifestyle choices.
- Provision of government strategy ensures consistent aims and objectives across independent organisations, e.g. schools and community organisations
What’s not working well
Again, because we work in the area of health promotion, we are also aware of the problems we face when trying to reach the aims an objectives of set strategies and initiatives. In our experience we find:
- Knowledge alone doesn’t change behaviour
- Individuals can get confused by the mixed messages coming from the media about what is healthy and what is not.
- Schools only have specific times allocated to bring in external groups
- There is a lack of provision of healthy alternatives
- Children have less control over what’s cooked at home
- Recruitment for adult programmes can be difficult
- Numbers on 6 week programmes (or long-term programmes) can drift of towards last few weeks, therefore clients are missing out on key messages.
- Difficulty ensuring areas with the most need are targeted.
- Young people may not be willing to try new foods.
- In schools, the size of groups can sometimes be too big, therefore not enough time is spent on each topic.
- In schools, sometimes teachers tend to have a lack of discipline over the pupils and therefore the young people can tend to get distracted and again miss out on key messages.
- Young girls tend not to want to partake in exercise or seem keen on doing exercise.
- Increased working hours leading to a reliance on convenience products.
Recommendations
- If adults believe their diet is healthy they are unlikely to change this behaviour. The figures from Action Cancer’s health checks indicate that a discrepancy occurs between perceived healthy diet and actual healthy diet. This discrepancy needs further exploration.
- The issue of increasing obesity levels is a complicated issue with numerous contributing factors. Tackling the issue will require a holistic, strategic approach, focusing on multi-dimensional change.
- Both prevention and treatment need to be included in any strategies.
- Strategies should have clear goals as well as clear descriptions of the methods used to achieve the goals.
- Clarification of healthy eating should not predominantly come from the advertising of specific products.
- Strategies need to ensure individuals have the resources available to them when they decide to change their behaviour.
- Government must work with organisations within the communities who deal with the issue on a daily basis.
• Schools programmes should focus on smaller groups to ensure effective information provision. Government needs to support schools and teachers by providing resources to allow this.
Belfast City Council
Belfast City Council welcomes this opportunity to comment on the draft terms of reference for the Committee’s inquiry. In general, the Council supports the examination of the current strategic approach to tackling obesity and its impact on health and well-being and would welcome further opportunity at later stages in the inquiry to input into the recommendations and offer an operational perspective on future implementation and management arrangements.
Throughout the memoranda the following documents are referenced;-
(i) Investing for Health reports from 2006 and 2007 – “Fit Futures – Focus on Food, Activity and Young People";
(ii) Northern Ireland Audit Office report from 14 January 2009 – “Obesity and Type 2 Diabetes in Northern Ireland"
Background
On a global basis, physical inactivity, unhealthy eating and being overweight are important preventable causes of chronic disease and illness. The social and economic costs of obesity are enormous and have the potential to increase significantly over the coming years.
The increasing levels of obesity in Belfast, as in the rest of Northern Ireland are of concern to the Council. The need to address obesity through addressing lifestyle factors such as physical activity and eating habits is well established and has been the subject of intense focus by a number of government Departments in the recent past;-
- the Department of Health, Social Services and Public Safety;
- the Department of Culture, Arts and Leisure
- the Department of Education and Learning
In line with the policy and programme agenda which has been emerging since the 1990s the Council has taken significant steps to reflect policy aims in its physical activity strategies and service provision. More recently, as the evidence base for childhood obesity has become clearer, the Council has implemented programmes to try to impact childhood obesity following the publication of the “Fit Futures" taskforce recommendations.
The “Fit Futures" recommendations also provide guidance on the development of a long-term life course strategic framework to address obesity across the whole of the Northern Ireland population which the Council is keen to play a developing role in.
Belfast City Council: Current Role and Opportunity
Belfast City Council’s overall purpose is to improve quality of life now and for future generations. One of the greatest quality of life issues in the city is health and wellbeing in that there continues to be a significant difference between the health and life expectancy of those living in deprived areas and those living in more affluent areas.
Obesity represents one element of this ‘health gap’ which is not something which can be addressed by the Departments or the Health Service alone as its causes relate to many other social, economic and environmental factors such as employment, education, housing, social inclusion, safe, clean and attractive neighbourhoods, access to leisure and open spaces etc, as well as people’s lifestyles.
The City Council has a key role to play in leading in the development of a healthier City and has made this an underpinning priority under the Supporting People and Communities theme of its 2009-2011 Corporate Plan.
In terms of delivery, the Council currently provides a wide range of services within communities which impact or have the capacity to impact on people’s health and wellbeing and obesity levels. These include leisure services, community services, environmental health, good relations, community safety, city development, parks and open spaces, services for children and young people and older people, economic development, regeneration, culture and arts, etc.
The Council also has the democratic legitimacy to play a role in ensuring that health improvement objectives such as tackling obesity are addressed in a co-ordinated way across the City by the many service providers involved.
There is currently a significant opportunity for the Council to play a greater role in making a difference to obesity levels through the evolving RPA and the current reorganisation of health and social care structures in Northern Ireland. The new health structures will also see a greater role for local government through participation in the new Regional Agency for Public Health and Social Wellbeing (RAPHSW) and in local commissioning. For example, four local elected representatives will sit on the Belfast Local Commissioning Group for health from April 2009, making decisions about budgets, contracts and service finance.
The Council also has an increasing role in liaising with Government in relation to the health and wellbeing of communities. This role can involve giving advice, lobbying in relation to policy and responding to consultations. Recent examples have included debates on suicide, alcohol abuse, poverty etc.
On 16 December 2008, Minister McGimpsey invited expressions of interest from District Councils on the possibility of hosting joint Regional Agency for Public Health and Social Well-being (RAPHSW) / Council pilots which would focus on addressing specific health and well-being inequalities. The Minister’s letter also indicated the possibility of co-locating health and social care staff with local government staff to support Councils in their future power of well-being and community planning role and inter- sectoral partnerships.
These staff could also assist in developing local health improvement plans, programmes and projects to reflect local community need (such as obesity) and would also support the Local Commissioning Group in developing commissioning plans which not only deal with health service provision but also measures to prevent ill health. These arrangements could be developed further and extended post 2011.
Belfast City Council is keen to participate in this pilot and sees this as a real opportunity for more effective joined up working including work on obesity. The Council is also currently undertaking a Strategic Review of Leisure in the city which has health and quality of life outcomes as a key driver. This review will inform how the Council will provide and “partner to provide" for a broad range of leisure and physical activity outcomes for the next 20-30 years.
The Council wishes to act now as failure to adequately address the rise in obesity will affect not only individuals and their families, and the wider community, but also local and regional government through higher health care costs and reduced productivity. In Northern Ireland the cost attributable to lack of physical activity includes over 2,100 deaths per annum, equivalent to over 18,000 life years lost and 1.2 million working days lost each year.
Belfast City Council feels strongly that despite the increased focus afforded by government, obesity is becoming more prevalent and the current strategy and target to “by March 2010, halt the rise in obesity" does not yet appear to be delivering significant outcomes.
The Council would recommend including the following elements within the terms of reference in order to deliver a robust and integrated inquiry into Obesity:
(i) The level of resources dedicated to the issue and an examination of an integrated financial management approach to prevention, intervention and further action by all statutory agencies involved;
(ii) Participation and partnership working to effectively address obesity through prevention, weight management or intervention programmes and education;
(iii) Examination of the current statutory powers of the relevant agencies working with obesity related issues and possible extension thereof;
(iv) The feasibility of the application of international best practice at a local level and where the relevant roles and responsibilities should lie;
(v) Aiming for health equity in all policy and statutory planning.
The 2005/06 NI Health & Social Well-being Survey reported that 27% of children between the ages of 2 and 10 years were classified as overweight or obese.
It reported that 64% of adult males and 54% of adult females were overweight or obese. In addition it reported that Obesity is most prominent amongst the middle aged - almost one third (29%) of those aged 45-54 were obese compared with 13% of those aged 16-24 years.
Being overweight or obese reduces life expectancy by 9 years and it significantly increases the risk of developing coronary heart disease and cancer.
Belfast City Council is very well positioned to assume a more significant role in combating obesity given the related remit of the services it currently provides such as;-
- activity programmes in our leisure centres and community centres;
- GP and pharmacy referrals to our fitness programmes under the “Healthwise" initiative;
- a focus on food safety and nutrition through our Environmental Health Service;
- generating economic and social development through funding and programmes of support e.g. Neighbourhood Renewal & PEACE funds to deliver healthier communities and places to live
- the priority we have given to Health and Well-Being outcomes in our corporate plan
- our ongoing work in education and participation across all our services
1. Prevention of Obesity and the promotion of lifestyle change
There are a number of current programmes of work to halt the rise in obesity which is being implemented and these initiatives in the area of prevention are very obvious, such as being physically active and reducing calorie intake. But clearly, as trends in recent years demonstrate, taking these simple steps is easier said than done.
- Studies consistently show that most children are no longer as physically active as they should be, and that activity declines further with age
- Effective prevention is difficult to achieve because the factors that shape people’s health are complex and intertwined
- A new draft Strategy and Action Plan was prepared and a series of targets set for 2010; this process was, however, then subsumed within the development of Fit Futures.
- More recently, the Northern Ireland Assembly’s Programme for Government identified working for a healthier people as one of five overarching priorities. This included commitments to increase physical activity and to provide opportunities for more active lifestyles by developing cycle and pedestrian networks, and to promote the benefits of sport.
The Council would reiterate the relevance of the six priorities for action outlined by the “Fit Futures" taskforce;-
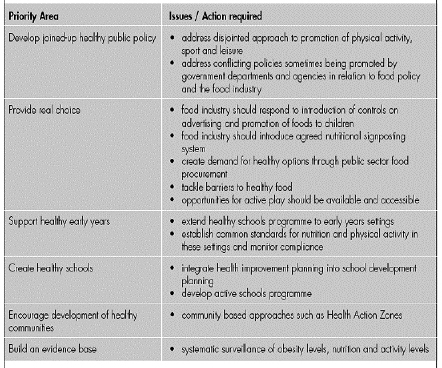
Investing for Health and Fit Futures provided a coherent structure and common branding for a wide range of health promotion programmes. They were set up as the whole-of-government initiative to coordinate action on obesity. So far, the Ministerial Group on Public Health which has responsibility for implementing and monitoring Investing for Health has focused on pulling existing initiatives into a consistent framework and encouraging cross-agency coordination.
The Department of Health, Social Services and Public Safety has now put in place an Obesity Prevention Steering Group. The Council understands (from the recent NIAO report ) that this cross- sectoral group, with representation from practitioners, policy makers and researchers, will be developing a Strategic Framework for addressing obesity across the life course, following closely the recommendations in the Foresight Report which demonstrated the complexity of the issue.
As part of this approach, four Policy Advisory Groups have been established –
these cover physical activity, food and nutrition, education and prevention, and data and research. This will facilitate an informed, research-led integrated approach to addressing obesity and associated conditions.
There is a real need for rigorous and robust research in the field of prevention during an individual’s life course and in particular preventing childhood obesity and promoting early year intervention. A full evidence base to enable the most effective decision making to be made is required. There are few local studies on prevention; much of the research which has been carried out is inadequate to allow for specific recommendations to be made.
2. The availability of weight management or other intervention services to tackle obesity related ill-health
The Council currently operates a range of weight management; nutrition guidance and interventionist strategies which would benefit from full exploration in an obesity inquiry. The examples are:
- Healthwise programme in partnership with EHB: targets adults and older people who are referred to the programme to tackle being overweight and obese.
- FRESH programme: follows on from the Fit futures’ initiative is a partnership approach which targets young people who are severely obese by providing a series of 12 sessions to enable them to bring about active lifestyle changes and improvements in health. (FRESH – Food; Relaxation; Exercise; Self esteem; Health)
- Health and Environmental Services Department have been working with businesses to improve the nutritional composition of foods on offer. This has included giving advice and assistance in the preparation of healthier foods and in food labelling so that the consumer has the necessary information to make healthier choices. Councils also use their food sampling programmes to advise on nutritional composition.
- Development Services provide economic and social development support and funding to generate safer and healthier communities in particular where there are high levels of deprivation (Neighbourhood renewal & Peace Funds).
- There is the potential for greater partnership working with Health and Social Service’s Dietetic staff in providing advice and assistance to businesses if this work is effectively planned, resourced and evaluated.
The Council would emphasise the following points in terms of a more strategic approach to weight management or intervention services…
Any interventions carried out must be properly evaluated to add to the evidence base. A consistent approach to research gathering across the region would be effective in providing a sound scientific base on which to recommend an effective approach to deliver healthier people and communities.
The Council is in a unique position to provide support, guidance and an enforcement role simultaneously in order to prevent; manage and overcome obesity through co-ordinated and community led action.
The Council would welcome as an outcome of the inquiry process - a co-ordinated and agreed referral process for intervention programmes.
Since the establishment of the Fit Futures taskforce there has been a significant allocation of resources to preventative approaches and to building necessary capacity in those working with children, young people and their families. The importance of early interventions and preventative approaches has been specifically recognised in the 10-Year Strategy for Children and Young People.
Comprehensive performance reporting will need to include meaningful measures for each type of prevention initiative. Whilst the PSA target which was aimed at halting the rise in obesity by March 2010 was defined and published, it only provides a good, high-level target and could be expanded in breadth, for example, to focus on gender differences, children and socio-economic groupings.
At the same time, there is a continuing need to consolidate and better co-ordinate current activities in relation to tackling obesity - e.g. Fit Futures identified gaps in the information on obesity risk factors, particularly at the local level that would help planning. The Council would support this view that there is a glaring need to build the evidence for effective intervention and to ensure that it informs the design and delivery of primary prevention programmes.
This will require a surveillance system to provide strategic and timely support to the implementation and review of reforms under these policies and provide robust capacity to measure achievements against agreed physical activity and healthy eating targets.
Under this heading the Council would advocate that the scope of the exercise should include:
- A threefold approach to focus on prevention at an individual, family and community level.
- In addition the assessment needs to focus on health, environment, wellbeing, nutrition and all other social determinants individually and collectively to ensure an effective scoping exercise.
- Co-ordinated intervention at all levels is required using all available forms – education, training, development of learning, co-ordinated promotion and marketing of the same message from all agencies involved to develop informal social control over the choices being made to integrate an active lifestyle and healthy diet to nurture their wellbeing.
- The council reinforces the need to look at the inextricable link between levels of activity and diet to obesity as, “ most evidence suggests that the main reason for the rising prevalence of obesity is a combination of less active lifestyles and changes in eating patterns"
- There is an opportunity to affirm the council’s role as guardian of the health and wellbeing of its citizens given the remit of its main departments; Parks and Leisure department; Health and Environmental Services and Development and building on their existing roles.
The 2009 Health and Social Wellbeing Survey will provide a more up to date regional assessment of progress towards halting the rise in obesity. Nevertheless the need to measure and assess progress on a regular basis in order to inform implementation and target the funds available for research and action at both regional and local level remains.
3. The potential to learn from experience elsewhere
The Council recommends that the inquiry look closely at the local best practice being delivered as a foundation on which to build a comprehensive and consistent approach to tackling being overweight and obesity.
Parental involvement is a primary driver to affect change and future action is essential in this area to address all aspects i.e. play development, education; nutrition; active lifestyle; weight management and prevention.
Education and awareness is required for all sections of the community and all agencies should adopt a ‘one message approach’ agreed by all partners who have a duty of care to reduce overweight and obesity. Schools, community, libraries and leisure centres are key places for the message to be delivered.
It is the development of basic knowledge and skills necessary to encourage and support people to be active and eat healthily that a strategic approach needs to include – the issue of obesity is a complex one which requires a long term commitment if current trends are to be halted and then reversed.
The Fit Futures taskforce considered not just what should be done, but also how it should be done to have most effect. It recommended that that policies and strategies to tackle obesity should take adequate account of the importance of the role of parents and families in establishing and supporting good nutrition and active living, particularly during the first few years of a child’s life.
Parents have primary responsibility for ensuring the health and well-being of their children, but action needs to be taken to support parents to fulfil this role effectively.
Some lessons in terms of implementation and scale of approach required may be learned from the approach taken by the Australian state of Victoria which examined Obesity as part of National Reform Agenda "Victoria’s plan to address the growing impact of obesity and Type 2 diabetes" - Council of
Australian Governments, April 2007. This agenda significantly strengthened the work of the Victorian Health Promotion Foundation (VHPF) and the non-government organisations with a health focus. Some of the programmes in
Victoria is as follows:
(i) The Go for your life programme is committed to developing healthier communities by promoting physical activity, healthy eating and the structural and environmental changes needed to enable this, including improved walking and cycling trails in regional communities. A variety of strategies are used to prevent obesity including whole-of-community approaches to increase physical activity and healthy eating among children, families and older Victorians.
(ii) Under Municipal Public Health Plans, there is a legislative requirement, unique to Victoria, for all 78 local councils to prepare municipal public health plans, reflecting the pro-active approach to public health promoted by the World Health Organization. Additionally, some local councils are involved in targeted diabetes prevention work through the Primary Care Partnerships (local networks of primary care services). Collaborative approaches have been adopted to improve consumer food choices.
(iii) The Food for Life programme is a joint initiative of relevant government departments to explore opportunities to assist in the manufacture and distribution of healthy foods and improve consumer demand. The Food for All programme is a joint initiative of VHPF and local councils to improve food access, particularly fruit and vegetables, of people living in disadvantaged communities.
Abbott
Abbott is a global, broad-based healthcare company devoted to the discovery, development, manufacture and marketing of pharmaceuticals and medical products, including nutritionals, devices and diagnostics. We have a continuing focus and interest in pharmacotherapy to tackle obesity and weight management services.
We are pleased to respond to this consultation. As the Department for Health, Social Services and Public Safety’s (DHSSPS) ambitious Public Service Agreement (PSA) target now imminent for delivery[1] the Committee’s inquiry is both important and timely.
We hope that the Committee’s recommendations will be translated into policy that supports efforts from a range of stakeholders to stem the rise in obesity across all parts of the population in Northern Ireland. We are keen to work with the Health Committee, the DHSSPS and wider stakeholders in support of this.
Assess the scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change
1. Policy-makers have rightly recognised the need to take urgent action to halt, and ideally reverse, the increase in the prevalence of obesity. Tackling obesity in both adults and children is critical. Latest data from the Northern Ireland Audit Office states that 60% of adults have a weight problem and as many as one in five are obese. Figures from 2006/07 show that approximately 22% of Northern Ireland’s primary school children are classed as overweight or obese.[2]
2. Obesity is associated with a number of chronic diseases including type 2 diabetes, hypertension, coronary health disease and stroke, metabolic syndrome, osteoarthritis and cancer. Being overweight or obese significantly increases the risk of mortality at any age and there is a nine-year reduction in life expectancy for obese patients.[3] Approximately 8.7% of UK deaths are attributable to excess weight.3 [4] The Ministerial Group on Public Health has identified that halting the rise in obesity could save the DHSSPS at least £200 million over the next 20 years.[5]
3. With such a significant impact on the health of the nation and the public purse, the need for an ambitious PSA target is clear. The recent NIAO 2009 report recommends that the PSA target “needs to be expanded, for example, to focus on gender differences, children and socio-economic groupings." Although additional strategies may be needed to target key groups such as children or particular ethnic minorities, Abbott believes that the right approach for the overarching PSA is to maintain its focus on addressing obesity across all ages. We are urging the administrations of the other UK nations to set similarly ambitious but appropriate targets.
4. The NIAO report also identifies the need to “build the evidence for effective obesity intervention strategies and to ensure that this informs the design and delivery of primary prevention." Currently, the main source of evidence-based guidance to primary care is that produced by NICE in its clinical guideline: CG43 Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children.[6] This guidance has been endorsed for implementation by the Chief Medical Officer for Northern Ireland, Dr Michael McBride.[7]
5. The NICE clinical care pathway can be summarised as:
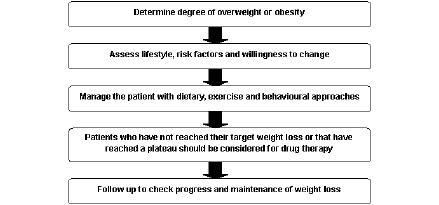
Adapted from NICE Obesity Guidance, 2006
6. The NICE guidance highlights the dearth of evidence relating to the impact of lifestyle interventions in the area of obesity, noting that there is “little evidence specifically on the cost effectiveness of non-pharmacological interventions (diet, physical activity and behavioural treatment) in the treatment of obesity".6
7. However, NICE accepts the evidence on the cost and clinical effectiveness of pharmacotherapy, stating that “drug treatment should be considered for patients who have not reached their target weight loss or have reached a plateau on dietary, activity and behavioural changes alone."
8. The guideline therefore advocates a holistic approach to weight management, acknowledging the role for appropriate pharmacotherapy support alongside lifestyle change. Indeed, drug therapy and lifestyle modification in combination are demonstrably more effective than either measure used alone.[8]
9. Abbott believes that any obesity strategy should recognise the important contribution that pharmacotherapy can make in enabling people to both start and sustain weight loss. Health professionals should be aware of the interventions that exist, and the evidence behind them, and be provided with training to enable them to support patients who are looking to lose weight.
Examine the availability of weight management or other intervention services to tackle obesity related ill health
10. There are many potential models for delivering weight management services. Services may be secondary care-led, linked to a diabetes or cardiovascular disease clinic for example, or led in primary care by GPs and practice nurses. Potential service models include: Directed Enhanced Services; Local Enhanced Services; community weight management programmes; GPs with a special interest in obesity.
11. Whichever service model is chosen, the service must able to offer evidence-based guidance and support. Abbott is currently developing a toolkit as a practical resource for anyone wanting to commission or provide obesity-management services for their local health economy. The toolkit draws together recent policy and clinical guidance and outlines a four-step approach to aid the development of local obesity services:
- Assessing local need and agreeing local goals
- Developing a local service strategy
- Securing the service
- Monitoring and evaluation
We would be happy to provide a copy of the toolkit to the Committee.
12. Increasingly, people are looking to the internet to find sources of support to help them manage their weight. In 2002 as part of our commitment to improving public health, Abbott set up a non-promotional patient support programme to aid weight-loss. The programme, Change For Life, is accessible to patients, the public and health professionals, and incorporates lifestyle advice and healthy eating recipes, along with other motivational support tools. The programme has been very successful, with over 25,000 subscribers to date.
13. We are happy to share our expertise in this area and are keen to work with the DHSSPS should they consider developing online support tools in this area.
Consider what further action is required, taking account, as appropriate, of the potential to learn from experience elsewhere
14. Abbott believes that tackling obesity effectively requires a holistic, multi-agency approach. It must combine not only prevention of obesity in those whose weight is currently under control, but also treatment of those whose weight is giving cause for concern – using lifestyle interventions with pharmacotherapy for those patients where it may be appropriate.
15. We believe that the DHSSPS should consider using existing levers to generate policy change. One such would be incentivising GPs to improve the identification and management of obesity under the Quality and Outcomes Framework (QOF), which has been shown to have a positive impact on clinical practice. In the area of chronic kidney disease (CKD) for example, QOF points were allocated in the 2006 settlement. In 2007-8, 96.8% of the points available for identification and management of CKD were achieved by GP practices, reflecting a renewed focus on the condition.[9]
16. Currently, eight points are available to GP practices which can “produce a register of patients aged 16 and over with a BMI greater than or equal to 30 in the previous 15 months."[10] No points are available for providing advice to patients on weight management. This compares to 33 points available in the QOF for capturing data on smoking status, plus a further 35 points available if patients’ notes record that they have been provided with smoking cessation advice or referred to a specialist service. This means that 11 times as many points as are available for management of smoking as are available for tackling obesity. This is despite recent estimates that put the cost of obesity to the NHS in 2007 at some £4.2billion a year[11], compared to healthcare costs of smoking of £2.7billion a year.[12]
17. Abbott believes that the allocating QOF points to obesity management, as has happened with smoking cessation, would be an effective way of incentivising better weight management in primary care and improving patient outcomes.
Once again, thank you for the opportunity to respond to this consultation. Please do not hesitate to contact us if you require further detail on the points we raised above. In the first instance please contact by email on Len.Gooblar@abbott.com.
Yours sincerely
Len Gooblar
Government Affairs Manager
[1] Building a Better Future: Northern Ireland Executive Programme for Government 2008-11. Annex 1: PSA Framework
[2] Obesity and Type 2 Diabetes in Northern Ireland 2009. Northern Ireland Audit Office. NIA 73/09-09 Press Release, 14 January. Available at http://www.niauditoffice.gov.uk/pubs/onepress.asp?arc=False&id=210&dm=0&dy=0
[3] House of Commons Health Committee. Obesity. Third Report of Session 2003-4 Volume 1. London: The Stationery Office Ltd; 27 May 2004
[4] National Audit Office. Tackling Obesity in England. NAO, London, 2001. Available from: http://www.nao.org.uk/publications/0001/tackling_obesity_in_england.aspx. Accessed January 2009
[5] Fit Futures: Focus on Food, Activity and Young People. Response from the Ministerial Group on Public Health. January 2007
[6] CG43 Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children. NICE, December 2006. Available at: http://www.nice.org.uk/Guidance/CG43
[7] Circular HSC (SQSD) (NICE) 58/08 CG 43. DHSSPS, 22 October 2008
[8] Wadden TA, Berkowitz, RI et al
[9] National QOF tables 2007-08 – clinical domain. Available at : http://www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-and-performance/the-quality-and-outcomes-framework/qof-2007/08/data-tables. Accessed February 2009.
[10] GMS Statement of Financial Entitlements. NI – 3rd Edition. Available at:
http://www.dhsspsni.gov.uk/qof_context#source. Accessed January 2009.
[11] Foresight Report: Tackling obesities – future choices. Project report, second edition. Government Office for Science, 2007.
[12] Beyond Smoking Kills: Protecting Children, Tackling Inequalities. ASH, October 2008
Southern Health and Social
Service Board and Southern
Investing for Health Partnership.
1.0 Context including current approaches to tackling obesity and the promotion of lifestyle change in the Southern Area
1.1 The Southern Health and Social Services Board (SHSSB), has since its establishment in 1973, worked to improve the health and wellbeing of the residents of the Southern area of N Ireland, as defined by the five districts of Armagh, Banbridge, Dungannon and South Tyrone and Newry and Mourne.
1.2 The importance of nutrition as a determinant of health has long been recognised and promoted by SHSSB. It published its first Nutrition Policy in 1985, incorporating this as a quality standard in all contracts with its then Providers. Following publication of a number of Regional Strategies in the 1990’s focusing on Healthy Eating, Physical Activity and Breastfeeding and the Investing for Health Strategy in 2002, the Board recognised that multi-sector approaches would be required to address these key issues. It established a number of multi-agency Steering Groups to work collaboratively across the Southern area to implement the recommendations of these strategies. These groups produced and implemented annual Action Plans identifying multi-sector approaches to addressing the recommendations in each strategy. They also carefully followed trends in lifestyle behaviours in the resident population and targeted interventions at specific target groups, including disadvantaged and marginalised communities and localities. In particular, a recent CAWT (Co-operation and Working Together) report focusing on Diabetes, highlighted the significance of increasing weight in the rising tide of early onset Type 11 Diabetes in the Border population. It reinforced the need for concerted, collaborative action to deal with the consequences of more people developing Type 11 diabetes and to prevent people from developing it in the first place.
1.3 In response to the rising trends of overweight and obesity in both the adult and more alarmingly in childhood populations, SHSSB directly and more recently through its collaboration with the Southern Investing for Health Partnership (SIHP), has re-focused efforts to tackle this major public health issue. A summary of the trends in the rates of overweight and obesity in both the adult and childhood populations in the Southern area over past years is included at Appendix 1.
2.0 Weight management and associated interventions to tackle obesity related ill health
2.1 SHSSB has and continues to commission a range of services to tackle this issue in both the adult and childhood populations. SIHP also has funded a range of interventions to promote positive lifestyle changes in all population groups and in particular with marginalised groups and individuals that have identified overweight and obesity as an issue for them. These include:-
2.2 Monitoring of BMI (Body Mass Index) in the Year 1 and more recently Year 8 student population. Funding has been provided since 2007 to support arrangements for collection and recording of BMI measurements of all Year 8 pupils through the School Nursing Service within SHSCT. To date 89% of Year 8 pupils have had their weight recorded and this indicates that 11% of children weighed fell into the obese category and 1% in the underweight category.
2.3 Provision of support for those children identified through the monitoring process as being obese or at particular risk. Currently a multidisciplinary healthy lifestyle programme for children identified as needing the service and who are suitably motivated and their families is being piloted across the southern area. Each parent and child attends a weekly 2 hour session over an eight week period where they participate in an exercise programme, receive advice on nutrition and participate in group sessions which concentrate on promoting self esteem and self confidence to encourage behavioural change.
2.4 Testing new approaches to working with obese young people. A pilot programme with Armagh City & District Council for children with BMI outside normal range aimed to introduce a variety of physical activities to a small number of clinically obese children referred by the Community Paediatrician in Craigavon Hospital. Activities ranged from light circuit classes, fitness suite usage, cycling, orienteering, tennis and walking. The children, their siblings, friends and parents were encouraged to take part in the programme.
2.5 The Dietetic service within the Southern HSC Trust has been commissioned to develop a “Nutrition in the Workforce" policy to promote healthy eating and physical activity in the workplace. This will target hospital staff and clients within the Acute Sector and also the local workforce and will be underpinned by a weight management programme aimed at Health Sector staff. This will augment the Healthy Eating Policy for patients, which is currently being updated.
2.6 A new training programme targeting Day Nursery staff in the community has been commissioned from the Southern HSC Trust Dietetic department. This recognises that healthy life-styles must commence from early childhood. In addition the “Family Toolkit" which promotes healthy eating in the under 5’s is being extensively used in the community and supported by the “Dig it and Eat it" project in local schools.
2.7 However, both SHSSB and SIHP recognise that they will never “treat" their way out of the current levels of overweight and obesity in both the general and childhood population and that a longer term prevention strategy to halt and these reverse the current trends is required. 28% of adult females and 27% of adult men are obese in the Southern area (8% and 10% respectively above the Priorities for Action target) and correspondingly 27% of men and 26% of women in the Southern area are sedentary, i.e. they have undertaken no physical activity lasting 20 minutes in the previous week. These two facts are not un-related.
2.8 In 2006, the Department of Health, Social Services and Public Safety published “Fit Futures: Focus on Food, Activity and Young People". SHSSB and SIHP agreed to collaborate on the implementation of this strategy area and a new multi-agency Fit Futures Steering Group, chaired by SIHP was established. Focusing specifically on the target group of young people, this Group complements the work of the Physical Activity Strategy Implementation Group Chaired by SHSSB. Together, the two Groups provide a unique opportunity to tackle the major contributing determinants of overweight and obesity i.e. nutrition and physical activity, across the Southern area in a collaborative but focused and complementary way.
2.9 The Fit Futures Steering Group has developed an integrated Obesity Action Plan tackling Overweight and obesity in Children. This Plan (available www.southernifh.com in the Publications section) identifies 65 specific interventions currently in place in the Southern area to address this issue.
2.10 The Physical Activity Strategy Implementation Group was established by SHSSB in the late 90’s to oversee the implementation of the regional physical activity strategy. Commissioning decisions are informed by the work of the Group which is chaired by a Board Officer. The focus is very much centred on community approaches which promote physical activity. This helps to create a supportive environment for tackling childhood obesity. To date 180 volunteers have been trained to lead over 60 walking groups in the southern area. A free “Cycle Lending Scheme" established a number of years ago has been extended to include tandems and children’s bicycles. Officers from District Councils are trained to promote and lead the cycling groups. Other initiatives include positive playgrounds, Step-o-meter challenge, Street Dance programme, Trim trails, Community Challenge, 50+ Clubs, Mugga programmes, summer Physical Activity Schemes and “Fit 4 You" programme which focuses on disability. The Action Plan for the Group is available on request and SHSSB has funded a Physical Activity Co-ordinator post to support the work.
2.11 The Annual SIHP Small Grant Programme 2008 – 09 focused on overweight and obesity with 36 Community Groups funded to promote healthy eating and physical activity at local level. Details of these can be found at www.southernifh.com Small Grant Programme.
2.12 In addition SHSSB and SIHP have commissioned a number of significant strategic interventions, which it is anticipated, will have long term positive outcomes. These include:-
2.13 The development of “Nutrition in the Workplace: A Toolkit for Action and Guiding Principles".
This resource provides a framework to create workplace environments which facilitate healthy choices and increased awareness of a balanced dietary intake for adults. By promoting good practice in the workplace, it is anticipated that individuals will take the positive learning from this setting and transfer it to their own home and family situations. The Toolkit was awarded the British Dietetic Association’s Elizabeth Washington Award in June 2008, a national recognition of excellence.
2.14 Publication of Analysis of School Lunch Menus in the Southern Area of Northern Ireland: A comparison with food-based and reference nutrient standards". November 2008
This work has highlighted that a sample of school lunch menus in the Southern area, whilst meeting the majority of current food based standards, do not meet all reference nutrient standards as used in the rest of the UK.
2.15 Development and Implementation of “Healthy Steps for Life" Programme
In March 2008, SIHP agreed to invest significant funding to develop a new approach to tackle overweight and obesity in the Southern area. The “Healthy Steps for Life" programme focuses on promoting healthy eating and physical activity in children under 5 years of age and is currently developing a range of approaches and interventions.
3.0 Intervention services
3.1 People who are obese are initially provided with advice through primary care services. They can access specialist drug treatments and dietetics advice through this route. NI has high rates of prescriptions of drug treatments for obesity. There is little evidence that attendance at specialist secondary care obesity clinics is more effective in achieving weight loss than interventions in primary care. However, such clinics may have a role in assessing patients who may be eligible for surgical intervention. As NI does not have a surgical treatment programme, there is no specialist obesity clinic in NI at present.
3.2 In October 2008, the CMO issued a Circular on Obesity to Boards and Trusts in NI. The guidance, which was from the National Institute for Health and Clinical Excellence (NICE), recommended that bariatric surgery to aid weight loss should be available to patients meeting certain body mass index (BMI) criteria. As with other DHSSPS guidelines, it was recognised that implementation is subject to resource availability and that Boards need to balance a range of demands and competing priorities.
3.3 It is estimated that there are more than 50,000 people in NI who could be eligible for bariatric surgery using NICE criteria. This number is expected to rise at a further 5% each year. Although NICE estimate that only 2-4% of these people would come forward for surgery, this is by no means certain. The cost of treating only 2% of the eligible NI population (i.e. 1,000 patients) and providing the necessary long-term follow-up could be in the order of £10 - £15 million.
3.4 NICE recognised that commissioners would need to build this service over a number of years and that they would have to manage demand in some way. It was envisaged that at the end of 5 years, the NI population should require funding for around 130 procedures a year. This is significantly at odds with the potential numbers of eligible people in the population.
3.5 In GB, many PCTs do commission bariatric surgery but, for financial reasons, a significant proportion have raised the BMI criteria for eligibility substantially above those recommended by NICE.
3.6 Quality aspects of bariatric surgical services
A multidisciplinary team assessment is necessary to ensure patient suitability for surgery and the long-term lifestyle changes it requires. In addition, surgeons need to be able to offer a full range of techniques, including laparoscopic surgery, and undertake a minimum volume of procedures to achieve and maintain skills. Appropriate follow up services, including the input of dieticians and specialist physicians, need to be in place. At present not all of these skills are available within NI.
3.7 Implications for commissioners in NI
The costs of implementing NICE guidance in NI are not affordable in the current Comprehensive Spending Review period. Boards recognise that there may be a small number of patients for whom bariatric surgery may be justified on the grounds that their level of risk, and hence likelihood of benefit, is substantially greater than the average group of patients meeting NICE criteria. A pragmatic approach is to assume that the clinical benefits of this surgery are likely to be greatest for those patients with the highest BMIs, particularly those who also have significant obesity-related co-morbidities. This is in keeping with the approach adopted by some GB commissioners. An example of a raised threshold would be to expect that patients being put forward as meriting surgery should have (i) a BMI of =60 without significant obesity-related comorbidities or a BMI of =50 if they have a serious obesity-related co-morbidity. Even with this higher threshold, there are almost 13,500 people in NI whose BMI is =50. Setting a higher BMI threshold for surgery would therefore still result in uncertainty as to the likely numbers of people who would wish to be referred for assessment and treatment.
3.8 It is not possible to operate one’s way out of an epidemic. However, the Health and Social Care (HSC) sector should seek to develop a process to fund bariatric surgery and associated assessment, treatment and follow-up, for patients who meet certain criteria, which may be higher than the NICE guidance. Until funding can be identified, commissioners may consider requests for bariatric surgery on an exceptional basis. This is a complex issue, with significant financial implications and there is no quick solution.
3.9 In light of the potential numbers of patients in NI who would meet NICE criteria, the current funding position, and the financial consequences of providing treatment for all those who might present, it has been agreed by Boards that, within the current CSR period, bariatric surgery cannot be commissioned routinely for patients meeting the NICE-recommended BMI criteria.
4.0 Future Work
4.1 The foundation has been laid within the Southern area to develop and implement a strategic approach to tackling overweight and obesity, now recognised as a significant public health issue. However, SHSSB and SIHP recognise that they can only do so much and must be supported by a regional, national and international policy frameworks and action, including:-
- Joined up approaches at national and regional level to promote healthy eating for both adults and children
- Policy shifts to create health promoting environments through positive planning and legislation
- Action to ensure all young people have the opportunity to engage in sufficient and sustained physical activity
- Resources to ensure young people have access to healthy nutritious meals and snacks in the education setting
- Support for family based interventions which specifically target sedentary behaviour
Appendix 1
Levels of Overweight/Obesity in Adults and Children
Adults
Proportion of SHSSB population (aged 16+ years) who are overweight or obese, 1997 and 2005/06
Source: NI Health and Social Wellbeing Survey, 1997 and 2005/06
As the data is obtained from a survey and so does not cover the full population, it is not acceptable to present the data at a lower geography than HSSB
Overweight: BMI between 25 and 30 kg/m2.
Obese: BMI greater than 30 kg/m2.
Children
Proportion of SHSSB children in Primary 1 who are overweight or obese, 2002/03 – 2006/07
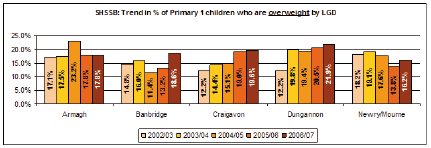
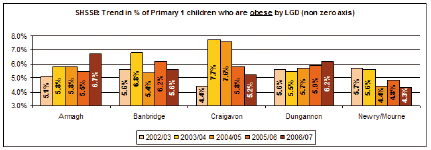
Proportion of SHSSB children in Primary 1 who are overweight or obese, 2006/07
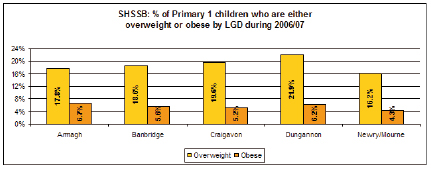
Year refers to school year (Sept-June)
Figures above are categorised using International Obesity Task Force measures
The information provided is at primary school level, i.e. children screened are those who attend a school within the SHSSB area and therefore some children screened may actually reside outside the Board area
Source: SHSSB Child Health System
South Eastern Health & Social Care Trust
The South Eastern Trust welcomes the Inquiry into Obesity being conducted by the Committee and appreciates the invitation to submit memoranda. The Trust provides a number of services, on behalf of commissioners, aimed at reducing obesity in the South Eastern area. Specifically, the Trust:
- Manages a Fit Futures Community of Interest in the South Eastern Trust area. This Community of Interest brings together a range of voluntary, statutory and community sector representatives to agree actions in terms of improving child physical activity levels and nutrition. In addition, the Community of Interest jointly agrees and distributes funding to specific grass roots schemes that will encourage and facilitate children to engage in healthy lifestyle choices in terms of diet and physical activity. We believe that this co-ordinated locality approach has been very effective in terms of ensuring co-ordination between the many agencies involved.
- Manages an Adult Nutrition and Physical Activity Community of Interest across the South Eastern Trust area. This group undertakes the same type of role as that described for Fit Futures but focuses instead on the adult population including older people and people with a disability.
- Contribute and support community led physical activity and nutrition initiatives. We believe that local communities have a key role to play in addressing obesity and as a Trust; we are keen to support local communities when they take ownership for the level of physical activity and diet in their local community.
- Through the Community Health Development Workers that the Trust employs, we support a range of ‘grass-roots’ activity with local groups aimed at tackling obesity. For instance, we have worked with local schools in a variety of areas, particularly deprived communities, to ensure healthy snacks are available and to help educate children as to what is and what isn’t healthy. The workers have supported other innovative schemes, such as the purchase and distribution of a mixed bag of vegetables to isolated adults and families by local communities.
- The Trust runs a ‘Leap Forward’ physical activity programme for staff which enables staff members to get involved in physical activity on a weekly basis on-site.
- As part of our Trust Health Improvement Plan, working groups have been established to improve the nutritional value of both hospital and residential food routines.
- We offer Weigh to Health and Cook It programmes to community and staff groups on an ongoing basis through a variety of trained staff.
- The Trust manages a LAPS worker who promotes and co-ordinates physical activity programmes for adults with a disability. This client group is at particular risk of obesity and this worker is playing an important role in mitigating this risk.
We believe that the Trust can plan an important role in helping to tackle obesity due to its local presence, especially in areas of deprivation. Moreover, through the health visitors and school nurses that the Trust employs, we have a unique insight into where support is most needed. We believe that this targeted approach, combined with personal support, is more effective than broad, media type campaigns. Moreover, we would suggest that:
1. Obesity should be understood in a wider context than simply a lifestyle choice concerning nutrition or physical activity. Obesity is often combined with issues of mental health, self esteem, isolation, family support and emotional wellbeing. The root causes of obesity are often complex requiring a more in-depth solution. As an example of this, the Trust currently employs an emotional wellbeing worker in the Ballymote area of Downpatrick. This worker has recently developed two initiatives with the local community which are tackling these wider issues:
a. A ‘walk and talk’ weekly activity has been established in the local community whereby isolated, unfit local residents participate in a gentle walk together at the end of which there is an informal talk on an emotional wellbeing issue. This activity accomplishing three things. Firstly, it provides physical activity with the associated health benefits. Secondly, it provides social interaction and support for people who would otherwise be isolated and thirdly, it provides education in terms of emotional wellbeing, an issue that can often lie at the heart of obesity.
b. The creation of a boccia league in Downpatrick. This league has proved hugely successful in re-introducing physical activity into people’s lives, as we as providing social interaction and support, for those who would not be able to conduct more high intensity forms of physical activity. When thinking of obesity, small, initial steps which are ‘fun’ are often the most important.
2. As with many things related to health development, the earlier healthy habits are established the better. To this end, the Trust, through the Sure Start programme that it delivers, seeks to introduce healthy lifestyle choices at an early age, as well as through engaging with schools and the delivery of Fit Futures.
3. In terms of adult obesity, we have experienced some very positive results from staff engaged in the Leap Forward physical activity programme at work, including reduced back pain, significant weight loss and improved wellbeing. This programme involves running a range of physical activity classes after work for staff. The learning from this programme has been that:
a. Convenience is very important to physical activity and the closer to work the better. In addition, if activities can be organised either before or after work there will be better outcomes. Local council run health centres can be very important in this regard. In addition, the cycle to work initiative, whereby staff members are encouraged to buy their own bike to cycle to work, is a very positive step.
b. If a group of staff can be encouraged to attend activities together, on a recurrent basis, this will help individuals to stay motivated and committed, as will a variety in terms of the activities offered.
We hope that the information supplied in the memoranda is of use to the Committee when undertaking its Inquiry into Obesity.
The Department of
Culture, Arts and Leisure
The Department of Culture, Arts and Leisure (DCAL) is responsible for the central administration and promotion of sport in Northern Ireland. DCAL is also responsible for setting the public policy frameworks and priorities for sport within Northern Ireland.
In discharging these responsibilities the Department works through Sport Northern Ireland (SNI). SNI is a Non-Departmental Public body within DCAL and is statutorily responsible for the development of sport in Northern Ireland, including the distribution of funding.
Strategy for Sport and Physical Recreation
Over the past 2-3 years DCAL, in partnership with SNI, has been developing a new 10 year Strategy for Sport and Physical Recreation in Northern Ireland. The aim is to provide a high level template for the development of sport and physical recreation in Northern Ireland which reflects the aspirations and priorities of all sports stakeholders. The new Strategy is also expected to inform the direction of future investment.
Since this initiative was launched, DCAL has consulted extensively with DHSSPS and other Government Departments and stakeholders on key issues to be considered within a new Sports Strategy. These discussions and other on-going work has uncovered significant evidence of the contribution that regular and sustained participation in sport, as a form of physical activity, can make to improving public health including reducing incidences of obesity. However, the available evidence also suggests that participation rates in sport in Northern Ireland are amongst the lowest in the UK and falling. In 1996/97, for example, the proportion of adults who participated in sport over the previous 12 months was 60% compared to 49% in 2007/08.
In 2007/08, the then, Minister for Sport, Edwin Poots MLA, published for 3-month consultation a draft 10 year Strategy for Sport and Physical Recreation in Northern Ireland. This document proposed a new 10 year vision for sport and physical recreation in Northern Ireland of “a culture of lifelong enjoyment and success in sport". It also recommended that Government should commit to taking action to develop sport and physical recreation and suggested a series of specific Government commitments to sport over the next 10 years.
The draft Strategy further set out 24 high level targets, to be achieved over the 10 year period, for sport and physical recreation. These included 11 targets aimed at improving participation rates in sport and physical recreation in Northern Ireland and further targets designed to improve the quality of and access to sports facilities at community level. Amongst the targets were specific objectives focusing on children and young people, adults, women, people with a disability and socio-economically disadvantaged groups. The draft also recommended that future measurement rates for participation in sport and physical recreation should be cognisant of the recommendations of the Chief Medical officers in the UK in relation to healthy physical activity. The document emphasised that successful delivery would require commitment and resources from all stakeholders (Central Government, district councils, SNI, sports governing bodies, clubs, the commercial and voluntary sectors). It went on to set out proposals for implementing the Strategy that embraced all relevant stakeholders.
It should be noted that the draft estimated at the time that the funding the shortfall facing stakeholders to fully deliver all targets at c.£20m per annum over 10 years. The document also emphasised that levels of public funding will be subject to the normal budgetary and business planning processes, including other competing priorities, and the ability of all stakeholders to contribute.
Current Position
Following completion of the consultation exercise in January 2008, a final version of the Strategy for Sport and Physical Recreation was submitted to the Northern Ireland Executive in December 2008 for consideration at a future meeting. In the interim, and under the current CSR settlement, DCAL secured £129.5m up to 2010/11 to help implement all aspects of the Strategy and sports policy in DCAL. This funding will be delivered via SNI. SNI has already developed, and is supporting, a number of complementary community sport programmes aimed at increasing levels and frequency of participation in sport as a contribution to tackling obesity and improving overall the health and well being of the NI population. The CSR settlement for sport has also helped to reduce the previous estimated funding shortfall to fully implement the Strategy from c.£20m per annum to c.£13m per annum.
As well as these developments, DCAL has developed a number of Public Service Agreement (PSA) targets, based around the Sports Strategy and to be achieved by 2011. These include a target to halt the decline in adult participation in sport and physical recreation by 2011, to have 125,000 children participating in sport and physical recreation by 2011 and to have a minimum of 10 new or upgraded sports facilities that will not only support the player/athlete development in Olympic/Paralympic sports, but will also be available for community and school use.
To monitor progress, SNI, with DCAL’s assistance, has put together a 4 year research strategy to improve baseline information on sports related issues including participation and to enable effective monitoring and measurement of progress on Sports Strategy targets. As part of this SNI, with DCAL’s support, has already commissioned a large scale bespoke survey on levels of adult participation in sport and physical recreation in Northern Ireland. DCAL and SNI are also working in collaboration with DE on the development of further surveys examining other issues including children’s participation. Both DCAL and SNI continue to be represented on DHSSPS’s Obesity Prevention Steering Group which was set up last year in response to the Fit Future’s Task Force Report published in 2006.
Armagh City and District Council
1.0 Context including current approaches to tackling obesity and the promotion of lifestyle changes in the Southern Area.
The vision of Armagh City and District Council is that it will be “an inclusive, progressive, outward looking area with a vibrant and diverse economy offering a high quality of life, within an attractive physical environment".
The Council have identified Four Corporate goals to help them achieve this Vision:
- Investing in our Community
- Growing our Economy
- Caring for our Environment
- Improving our Health and Wellbeing
2.0 Council initiatives which impact on obesity issues
There are principally two departments within the Council whose work directly impacts on obesity: the Leisure Services Department and the Environmental Health Department. The initiatives currently in progress in each department are outlined below:
2.1 Leisure Services
“Working for a healthier tomorrow, today" is the vision for the Recreation and Leisure Department within the Council.
The Leisure Service Industry is changing at Local Authority to become a Well-being service. This change is brought about by the staggering health statistics particularly around obesity and cardiac care and also due to the increased public knowledge in the benefits of health.
As result, Armagh City and District Council have adopted the role of “enabler" and hope to provide services which are both preventative and promotional through the provision of a specialist range of quality services / programmes and instruction / advice, suitable for all ages, gender, race and abilities.
In addition, relationships have been forged with other agencies, especially within the Statutory Sector for example the Southern Investing for Health Partnership and the Southern Health and Social Services Board in relation to the prospect of future development of services and infrastructure that will benefit the resident of the District long after the Review of Public Administration in 2011.
Armagh City and District Council supports the two overarching goals of the Investing for Health Strategy:
- To improve the health of our people by increasing the length of their lives and increasing the number of years they spend free from disease, illness and disability
- To reduce inequalities in health between geographic areas, socio economic and minority groups
In 2003 joint appointments of three Investing for Health Officers were appointed in the Southern Group area, jointly funded by the District Councils and SHSSB. Part of their remit within the Southern investing for Health Partnership is to tackle obesity as per the original Investing for Health Strategy.
The department has been incredibly successful in attracting external funding through partnership work and this trend will continue.
In working in partnership, ACDC seek to work with those partners with a genuine interest and commitment in the target area and will especially continue to work will the Health and Education Service which are already in transition due to RPA.
Weight management and associated interventions to tackle obesity related ill-health
Armagh City and District Council is committed to developing and supporting a range of programmes that address the issue of obesity.
The Exercise for Health Programme facilitates conditions such as obesity, cardiac rehabilitation, respiratory disorders, musculo –skeletal disorders and Diabetes Mellitus to name a few. Clients must be referred to the Programme by their GP, Practice Nurse, Consultant, Dietician or Physiotherapist. The Exercise for Health Programme is monitored by a steering group made up of representatives from Armagh City and District Council and the Southern Health and Social Care Trust as well as two General Practitioner’s, a Cardio Physiotherapist, Dietitians and former clients.
The Get Set and Go programme is an eight week structured exercise session for young people, delivered in conjunction with the Dietetic Department of Armagh and Dungannon Trust, through a referral process similar to that used in the Exercise for Health programme. The ‘Get Set… GO!’ Programme’ acts as a catalyst towards combating child obesity within the Armagh area, where currently 18.5% of Primary 1 children are overweight, and over 6% are obese. There is a strong belief that Primary prevention will avoid further health problems in later adult years.
The Council has also promoted a ‘Fit Kidz’ programme in schools offering incentives to pupils who chose the healthier options from the schools canteens. The healthy eating and sport scheme, promoted healthy eating while at the same time encouraging exercise. The Council worked in partnership with the school to introduce an incentive and reward scheme whereby points were allocated to healthy food and ‘cashed in’ for vouchers entitling them to free swims at the local leisure centre.
Representatives from ACDC work in Partnership with those from the Southern Health and Social Care Trust to deliver a series of Walk Leader Training to members of different community groups across the District. This training focuses on the health benefits of Walking specifically in relation to obesity. In conjunction with this Council representatives work in Partnership with the Chest Heart and Stroke Association to create a number of Highway to Health routes across the district. This is a simple innovative scheme which aims to encourage people of all ages to walk for leisure and good health. There are currently seven Highway to Health routes developed. Similarly, a number of Cycle leaders have been trained through partnership work with the Southern Area Physical Activity group.
A number of Community and Workplace Health Challenges to encourage healthier eating and physical activity have also been delivered throughout the City and District over the past number of years.
Armagh City and District Council is represented on the Multi-agency Fit Futures Steering Group, chaired by the Southern Investing for Health Partnership. This group has developed an integrated Obesity Action Plan tackling Overweight and Obesity in Children. It is through this group that the Council have been able to secure funding to support a number of programmes to address obesity. The Council also aid the delivery of the Promoting Healthy Eating in Schools programme through the joint appointment of the Investing for Health Officer.
Armagh City and District Council has worked in partnership with representatives from the Southern Health and Social Care Trust to develop a healthy Eating Policy in line with the Corporate Plan and the council’s commitment to improve the health and wellbeing of the people it serves.
The Council is committed to enabling people to make healthier choices as outlined in the Public Health Strategy for Northern Ireland ‘Investing for Health’, and in the Department of Health, Social Services and Public Safety’s long term strategy, ‘A Healthier Future’. These strategies recognise the importance of good nutrition and in particular the importance of promoting healthy eating in the workplace setting, where adults spend significant amounts of time.
Through Sports Development we have actively sought funding from Awards for All to help increase participation in sport and physical recreation amongst women and girls in rural areas.
Active communities is an investment programme that recognises the importance of, and seeks to contribute to, the participation targets outlined in the NI Strategy for Sport & Physical Recreation to by 2018 deliver at least 6 percentage points increase in women’s participation rates in sport and physical recreation (from the 2012 baseline).
2.2 Environmental Health Department:
Work with Food Businesses
In general EHOs have been involved in promoting for example the FSA’s traffic light scheme in food manufacturers in this area and are willing to work with them on other emerging initiatives such as their saturated fat and salt campaigns.
Appointment of Dietitian Specialist
A Dietitian Specialist has been employed from April 2008- end March 2011 to work with EHO’s and local food businesses to improve the Nutritional quality of food sold from catering outlets. This does not include premises where nutritional standards already exist, for example schools, nursing homes, etc. This initiative is known as CHOICE (Choosing Healthier Options in Catering Establishments).
In April 2008- end March 2011 the Dietitian Specialist will also be working along side a Community Project Officer who will be working on a community based initiative to improve the diet and nutrition among communities in the Southern group area. Both of these positions have been part funded by the SHSSB.
Community Nutrition Project
A number of Environmental Health Officers from all five constituent Councils of the Southern Group area have completed a Diploma in Nutrition, part funded by FSANI. This will assist them deliver the CHOICE initiative in this area and also get involved in other forthcoming initiatives that the FSANI are keen to develop e.g. Grubs Up. Further information is available from FSANI on their proposals. Councils may also decide to provide Nutrition training for local food business operators.
The Overweight and Obesity Prevention Group
The Principal EHO (Food Control/ Infectious Diseases/ Health Promotion) at Southern Group Environmental Health Committee(SGEHC) is a member of the Southern Health and Social Services Board (SHSSB) Overweight and Obesity Prevention Group. This group concentrates on initiatives to follow up on the Fit Futures report.
More detail is available from Lyn Donnelly, the Southern Investing for Health Manager who chairs the group.
Joint appointments of Health Improvement Workers
In 2009 three Health Improvement Workers will be appointed to work across the five Councils in the Southern area. One of their key health improvement objectives is Nutrition and the promotion of healthy eating in areas of social deprivation.
SHSSB Cook It programme Steering Group
SGEHC were involved in the steering group and hope to be involved with the new proposed Community Cooking programmes currently being set up by the SHSSB.
Representation on NI Fit Futures Groups
Officers from the SGEHC are representing Councils across NI on the Obesity Prevention Steering Group and its Nutrition subgroup.
CEHOG Nutrition Sub-group
The Northern Ireland Food Liaison Group- a CEHOG subgroup is to convene a Nutrition subgroup to look at how best EHOs can become involved in tackling the obesity issue in the general population and also to share ideas and initiatives that may be happening elsewhere in NI and the rest of the UK, etc. This group will also have membership from FSANI.
Future Work
Working in partnership with a number of key agencies has provided the foundation to develop and implement a strategic approach to tackling overweight and obesity, now identified as a serious public health issue.
Armagh City and District will continue to work to ensure there are adequate opportunities for young people to engage in physical activity. They will continue to promote the benefits of healthy eating by implementing the Healthy Eating Policy throughout Council facilities and work in partnership with key agencies to ensure consistent messages on healthy eating and physical activity in a number of key settings, schools, community and resource centres.
Chartered Society of
Physiotherapy Northern Ireland
Background
The CSP is the professional, educational and trade union body for the UK’s 47,000 chartered physiotherapists, physiotherapy students and assistants. Physiotherapy is the third largest healthcare profession after medicine and nursing/midwifery. CSP members work primarily in the health service, but also in the independent sector, education, research and industry. Over 98 per cent of all registered physiotherapists are members of the CSP.
The CSP commends the Health Committee for its inquiry into obesity and the recognition of the growing obesity problem in Northern Ireland and of the impact of obesity on the health care system. The prevalence of overweight and obese individuals has increased substantially over the past decade and is set to further increase in the future if measures are not taken now to prevent this. As stated in the DHSSPSNI Healthier Futures regional strategy
“Rising levels of obesity and lower levels of physical activity will increasingly contribute to the burden of disease. Obesity is a contributory factor to a number of conditions such as stroke and cardiovascular disease. Obese men are more than 33% more likely to die from cancer and obese women are more than 50% more likely to die from breast cancer".
(Healthier Futures, DHSSPSNI 2004)
The CSP fully supports the aspiration to obesity prevention expressed in the DHSSPSNI “Fit Futures" document, which states that:
“In the Fit Future, children and young people, of all ages and from all sections of our society, will be motivated and supported to access a range of readily available, quality, enjoyable opportunities to be active and eat healthily."
(Fit Futures Focus on Food Activity & Young People, DHSSPSNI 2005)
In addition the CSP supports the six strategic priorities areas outlined in the Fit Futures strategy in relation to: -
- Developing Joined-Up, Healthy Public Policy
- Providing Real Choice
- Supporting Healthy Early Years
- Creating Healthy Schools
- Encouraging the Development of Healthy Communities
- Building the Evidence Base
However, it is unclear at this point in time what progress has been made by the Ministerial Group for Public Health in implementing the recommendations for priority action contained in the Fit Futures strategy. The CSP would ask the Health Committee to clarify with the Department of Health, Social Services & Public Safety what progress has been made to date in relation to the recommendations contained in the Fit Futures strategy and how those recommendations are being taken forward by the Ministerial Group for Public Health.
The Role of Physiotherapy
The role of physiotherapy in the management and prevention of obesity is considerable. Physiotherapy has a crucial role to play in the provision of exercise programs to at-risk groups in the community as well as in treating many of the secondary health problems associated with obesity. Some of the health problems for which there is evidence of efficacy and cost effectiveness for physiotherapy management are:
? Musculoskeletal conditions
? Type 2 diabetes
? Respiratory problems
? In the Community
The considerable economic burden of obesity is set to progress rapidly. While not the only solution to this problem, the effective utilisation of the health workforce is critical to the fight against obesity. This submission clearly identifies the contribution physiotherapists can make in addressing this problem.
Musculoskeletal conditions
Physical activity is important for the maintenance of healthy weight and for decreasing overall morbidity from a number of conditions including obesity, cardiovascular disease and diabetes. Chronic musculoskeletal conditions are strongly linked with a high Basal Metabolic Index (BMI) (WHO, 2003) and the incidence of musculoskeletal conditions is increased by lifestyle factors, which lead to increased obesity and sedentary routines (Woolf & Pfleger, 2003). The type of musculoskeletal conditions experienced by overweight and obese individuals is variable. However one of the most common conditions is arthritis, which is thought to be due to increased loading on the joints (Felson et al, 2007).
Muscle weakness, pain, and joint stiffness associated with arthritis can often limit the choices of physical activity (American College of Sports Medicine, 2000 & 2001). Because physiotherapists are highly skilled in exercise prescription, they can play a key role in the design, delivery and implementation of exercise programs for the management of these disorders. Physiotherapists are able to design appropriate modifications to exercise programs so that the benefit of increased physical activity is achieved without aggravating any co-existing musculoskeletal problems caused by arthritis. Appropriate exercise plays a vital role in prevention and early intervention. The treatment of arthritis and musculoskeletal conditions is a core function of physiotherapy practice.
Type 2 diabetes
Obesity and physical inactivity are key contributors to the development of Type 2 diabetes (AIHW, 2002). Known risk factors for Type 2 diabetes include high blood pressure and inappropriate dietary intake (Shaw & Chisholm, 2003). Exercise can play an important role in preventing or delaying the onset of Type 2 diabetes because of its ability to improve blood sugar metabolism, reduce body fat, increase muscle mass and improve cardiovascular fitness (Aas et al., 2005; McAuley et al., 2003).
Physiotherapists have the broad clinical knowledge and skills necessary to manage patients with diabetes. Common co-existing medical conditions for people with diabetes include heart disease, obesity, high blood pressure and stroke. Physiotherapists are able to take into consideration these conditions and tailor treatment (including exercise programs) to the client’s individual needs. Physiotherapists frequently design exercise programs to reduce sedentary behaviours and increase physical activity. With optimal design, these programs may contribute to the reduction of body fat levels and improve glucose metabolism – both of which are important in the treatment of diabetes (particularly Type 2) - as well as for general health and fitness.
Respiratory Conditions
Respiratory conditions such as asthma, sleep apnoea and chronic obstructive pulmonary disease are also positively correlated with obesity (WHO, 2003). Research undertaken by Sulit et al. (2005) found that children with a BMI in the 95th percentile are significantly more likely to suffer asthma and wheezing. In addition, they found that sleep-disordered breathing (SDB) in children is related to obesity and wheezing in children.
Training in healthy subjects improves cardiorespiratory performance and improves musculoskeletal function. If evaluated at a time when they are symptom free, people with asthma respond to exercise in the same physiological way as healthy subjects (Satta, 2000). However, many patients with asthma often avoid physical activity.
One reason for the sedentary lifestyle may be exercise-induced asthma (EIA). The mechanism for EIA is not fully understood, however it seems to be related to the increase in pulmonary ventilation that occurs in response to heavy exercise (Tan & Spector, 1998). It is estimated that 80 per cent of people with asthma experience varying degrees of EIA (National Asthma Council of Australia, 2002).
Prevention of EIA by modification of the exercise environment and optimal pharmacological management is essential in the physical training of people with asthma (Satta, 2000). Physiotherapists have a thorough knowledge of exercise prescription and respiratory pathophysiology and therefore play a significant role in the development and monitoring of exercise programs for people with asthma.
In the Community
Physiotherapy is an holistic approach to addressing physical dysfunction in order to enhance the health and well being of adults and children. The CSP contends that promoting physical activity is one important strategy to address the current problem of obesity. Physiotherapists are well trained to assess the cardiopulmonary, musculoskeletal, and physical functions of children and adults who are obese and to work with such groups and their carers in prescribing appropriate physical fitness, strength, and motor skill programs to meet their health needs. Physical activity is critical to the maintenance of healthy weight. Physiotherapists are expert in addressing physical dysfunction and thus assisting individuals with barriers (e.g. obesity) to participation in physical activity.
With obesity a significant and escalating problem in modern society, and the Government’s increasing emphasis on physical activity as a major part of the solution, physiotherapists are in an ideal position to help people make informed decisions on how to lead healthy lifestyles and enjoy maximum quality of life. Physiotherapists are taking on an increasing role in developing and tailoring exercise sessions to manage weight, for example, running classes for those who have specific medical problems and supervising more generic classes run by exercise instructors.
As part of its commitment the CSP has established a 5-year integrated program of work to enable the profession and other stakeholders to realise the significant contribution it can make to enable the health and wellbeing of society through physical activity. The project is called Move for Health and aims to work in parallel with other international initiatives (WHO, WCPT) targeted at physiotherapists and physical activity issues. Move for Health is in its early stages of development and so will be meeting with members throughout 2008 to gain a thorough understanding and appreciation of the profession’s perceptions between the role and responsibility of physiotherapists and physical activity.
One of the core components of the Move for Health project will be to create strategic alliances with other health promoting organisations in order to raise the profile of what physiotherapy can offer individuals to maintain health and wellbeing through physical activity.
In conclusion the Health Committee should urge the government to take advantage of the knowledge, skills and experience that health professionals such as physiotherapists have as part of its overall approach to encouraging and enabling physical activity and in working across government departments to explore collectively how we can effectively tackle the problem of obesity.
References
Aas AM, Bergstad I, Thorsby PM, Johannesen O et al. (2005) An intensified lifestyle intervention programme may be superior to insulin treatment in poorly controlled Type 2 diabetic patients on oral hypoglycaemic agents: Results of a feasibility study. Diabetic Medicine 22, 316–322.
American College of Sports Medicine (2001) ACSM’s Resource Manual: For Guidelines for Exercise Testing and Prescription (4th Ed). Lippincott, Williams and Wilkins.
Australian Institute for Health and Welfare: Australian Centre for Asthma Monitoring (2005) Asthma in Australia 2005. AIHW Asthma Series 2. AIHW cat. no. ACM 6. Canberra: AIHW. Felson DT, Niu J, Clancy M, Sack B, Aliabadi P, Zhang Y (2007) Effect of Recreational Physical Activities on the Development of Knee Osteoarthritis in Older Adults of Different Weights: The Framingham Study. Arthritis & Rheumatism (Arthritis Care & Research) 57(1), 6–12.
McAuley KA, Murphy E, McLay RT, Chisholm A et al (2003) Implementation of a successful lifestyle intervention programme for New Zealand Maori to reduce the risk of type 2 diabetes and cardiovascular disease. Asia Pacific Journal of Clinical Nutrition 12, 423–426.
Satta A (2000) Exercise training in asthma. Journal of Sports Medicine and Physical Fitness 40, 277–283.
Shaw JE and Chisholm DJ (2003) Epidemiology and prevention of type 2 diabetes and the metabolic syndrome. Medical Journal of Australia 179, 379–383.
Sulit LG, Storfer-Isser A, Rosen CL, Kirchner HL, Redline S (2005) Associations of Obesity, Sleep-disordered Breathing, and Wheezing in Children. Am J Respir Crit Care Med 171, 659–664.
Tan RA and Spector SL (1998) Exercise-induced asthma. Sports Medicine 25, 1–6.
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bulletin of the World Health Organization 81, 646–656.
World Health Organisation (2003) Obesity and Overweight: Global Strategy on Diet, Physical Activity and Health, WHO, Geneva.
Newry and Mourne District Council
1.0 Background including current approaches to tackling obesity and the promotion of lifestyle change with particular reference to the contribution of Newry and Mourne District Council.
1.1 Newry and Mourne District Council has a strong commitment to the promotion of the wellbeing of the people of the District both through the provision of services, support to the community/voluntary sector and through the Council’s civic leadership at a local level.
Central to the Council’s vision for the wellbeing of its population is a commitment to work in partnership, as we believe to make a significant difference it is essential to build trust, cooperation and an openness to partnership approaches. This has been demonstrated by the Council’s facilitation of the Wellbeing Action Partnership, a multisectoral partnership of Public, Community and Voluntary organisations that have come together to see how we can contribute to improving people’s health through addressing the factors, which cause ill health.
Newry and Mourne Council has played a full role within the Southern Investing for Health Partnership (SIHP), since the partnership’s inception. Since 2004, the Council has jointly employed an Investing for Health Officer, in partnership with SIHP and the Wellbeing Action Partnership, with a remit to embed the Investing for Health ethos within the core business of the Council and to promote a focus on the determinants of health (such as healthy lifestyles) within the local community. In its leadership role, the Council is in the process of adopting a policy promoting healthy eating at all Council events and functions.
1.2 The Council is the foremost provider of leisure facilities in the area, operating 2 leisure centres, 2 swimming pools, 33 playing fields, 5 tennis courts, 5 bowling greens and one running track. In addition, the Council has provided substantial assistance to sporting organisations in the area towards the provision of their facilities. The Council’s dedicated team of leisure staff work closely with the community to provide a full range of sports activities and classes. In addition, the Sports Development Team play a major role in the organisation of many special events such as the Newry City Marathon and the Schools Cross Country Event.
1.3 Newry and Mourne Council places a particular emphasis on supporting sport and leisure activities for people with disabilities, a group who can be particularly vulnerable to weight management difficulties. The Council employs a dedicated Disability Liaison Officer with a remit to oversee the clubs and classes, which we provide for people with disabilities. The Liaison Officer works closely with the Sportability committee, a group representing a range of disability groups to ensure that as broad a range of activities as possible is provided. The Council recently worked with the local Health and Social Services Trust and the Wellbeing Action Partnership to provide a hoist to enable people with severe disabilities to access the standard trampoline facilities at Newry Sports Centre.
1.4 The Council also runs and maintains nineteen community centres, which are widely used for recreation and leisure activities. The Investing for Health Officer has also developed a partnership with the Health Trust and local community networks to organise a highly successful Community Challenge, focusing the attention of local groups on the promotion of physical activity and healthy eating. The 2008 challenge also provided an opportunity for the integration of groups of individuals with learning difficulties to participate with others on this issue.
1.5 As an employer, the Council sees the wellbeing of its approximately 550 employees as a priority and has developed a number of programmes to promote health and thus reducing sickness absence. Included among these programmes is the promotion of the use of the Council’s leisure centres and swimming pools by staff and Councillors through reduced rates and free access. The Council’s staff canteens provide a range of healthy options and are constantly working to improve the selection available to staff. A weight management support group has also been set up for staff to encourage each other to reach and maintain a healthy weight.
1.6 Through its Environmental Health Department, the Council is working with other employers to improve workplace nutrition standards throughout the area.
2.0 Weight management and associated interventions to tackle obesity related ill health
2.1 The Council recognises that the current levels of obesity and overweight cannot be reduced by medical intervention alone and that a broader, prevention strategy is required. Current figures for the Southern Area show that 28% of adult females and 27% of adult men are obese and that 27% of men and 26% of women have undertaken no physical activity lasting 20 minutes or more in the previous week. As demonstrated above, the Council is making a substantial contribution to encouraging the adoption of healthier lifestyles.
2.2 However, the Council also believes it can, in partnership with others, contribute to weight management in those who are overweight or obese. For example, the Council’s Leisure Services Department has worked with the dietetics and physiotherapy departments of Daisy Hill Hospital on the Over to You exercise referral programmes for both adults and young people. However, such programmes, particularly those aimed at young people can be expensive as they require substantial commitment of both Council and Trust staff.
2.3 It is interesting to note from the measurement programme for all 5-year-old children, that the levels of obesity and overweight of both boys and girls in this age group, within the Newry and Mourne Area, are reducing. This result, which appears to be in contrast, to the wider Northern Ireland results should be investigated to determine the causes of this reduction and if it can be replicated in other areas.
3.0 Future Work
3.1 The foundation has been laid, particularly within the Southern Area, to develop and implement a strategic approach to tackling overweight and obesity. Poor dietary habits and decreasing physical activity have become ingrained in the population and it will take a long-term approach involving many organisations to make any substantial changes in this culture. The current media profile of this issue provides an opportunity to refocus people’s attitudes. However, the present economic situation provides a significant threat, in that people will chose less nutritious options, which they perceive as cheaper.
3.2 The introduction of community planning in 2011 will provide opportunities for Councils to come together with other organisations to undertake the sort of work, which can make a difference on this issue. This will require a commitment from all agencies to participate fully and share resources and knowledge if the potential is to be realised.
3.3 In the meantime, the Council believes it is important to move forward on action to address the matter to include:
- The development of joined up approaches at regional level to ensure consistent messages on healthy eating.
- There must be adequate opportunities for young people, and particularly girls, to participate in physical activity both within the school setting and in the wider community.
- It is essential to ensure that a broader range of healthier food choices are available in schools, workplaces etc and, particularly where young people are involved, unhealthy options are kept to an absolute minimum.
In conclusion, the Council believes obesity is an important issue, which must be placed on the agenda for much of the Public and Community Sector. Local interventions can make a significant contribution to this issue but these must be balanced by a strong regional commitment which supports, including with funding, these local level approaches.
Northern Ireland Environment Link
Northern Ireland Environment Link (NIEL) is the networking and forum body for non-statutory organisations concerned with the environment of Northern Ireland. Its 53 Full Members represent over 90,000 individuals, 262 subsidiary groups, have an annual turnover of £70 million and manage over 314,000 acres of land. Members are involved in environmental issues of all types and at all levels from the local community to the global environment.
1. Welcome for the Inquiry
NIEL welcomes the Inquiry by the Health Committee into this important issue facing society. Rising obesity levels, especially in children, is a serious problem that also reflects some more general problems in society and will have major impacts on public health and medical care for many years to come. This issue presents the opportunity to deliver joined up government by delivering the targets of other departments as a means of achieving the primary aim of reducing obesity and in so doing to improve the health and quality of life for a high proportion of Northern Ireland’s people. It will also have major impacts on reducing the cost of health care delivery.
2. Linking Environmental Quality and Health Benefits.
The link between a pleasant environment and enhanced human health is now strongly established. There is a great deal of evidence to support the synergistic benefits of engaging in physical activities whilst being directly exposed to nature. Research conducted by the University of Essex[1] suggests that exercise in pleasant rural settings reduces blood pressure, increases self esteem and improves mood to a greater extent than exercise in rural unpleasant, urban pleasant and urban unpleasant environments. The Woodland Trust has also collated evidence linking activity in wooded areas with enhanced wellbeing www.woodland-trust.org.uk/wcc/index.htm. There are a number of schemes which are designed around this principle, for example the Conservation Volunteers Northern Ireland organise a Green Gym and St. Malachy’s Primary School in Belfast use there wildlife garden as part of their PE activities, but there are many other environmental organisations that are providing activities in exceptional areas that are not currently recognised as contributing to the sense of wellbeing, and the physical fitness, of participants.
Organisations that are encouraging activity in young people or adults, and are doing so in areas which have acknowledged added benefits, should be supported financially and demonstrably by health professionals. There is a need to change the ‘Medical Model’ which GPs follow to include recreation as a valid therapy/prescription. To facilitate this, greater credence should be given to preventative medicine and the promotion of physical exercise within the health profession, and more most be done to promote this same message to the public.
3. Integrated Working across Departments is Required
As part of the Comprehensive Spending Review, Departments present their priorities to DFP. NIEL believes the focus should be on outcomes and all Departments should be working on how they can contribute to the PSA targets rather than trying to interpret what they do now in terms of the PSA targets. Linking health and environmental messages is an example of sustainable development which should be developed and properly funded with the benefits recognised across Departments.
Recent government documents including the Fit For Futures report fully recognised and stressed the link between poverty, poor diet and obesity. The department with responsibility for targeting social need and the anti-poverty strategy therefore needs to be fully involved in the development and implementation of plans and programmes designed to tackle obesity issues. The Department should be addressing this issue by involving all government departments.
4. Obesity and Lifestyle
It is clear that one of the main causes of obesity in both adults and young people is our sedentary lifestyle. The lack of exercise also contributes to the high levels of cardiovascular disease in NI and treating this is a major cost for the health service, as well as exacting a high social cost for those suffering and their families and carers. A comprehensive programme addressing the various contributing factors to obesity and cardiovascular illness could reap great benefits in terms of general public health as well as decreasing costs to the health service through treatment. There are also associated benefits in terms of making lifestyles more sustainable in terms of transport, energy use and making Northern Ireland more fit for a low carbon future. Programmes such as those by the Health Promotion Agency, which promote more active lifestyles have both environmental and health benefits.
5. Obesity and Diet
The second major contributor to obesity is our current diet, centred for many people around processed and convenience foods. Promoting a healthier diet, concentrating on fresh fruit and vegetables and decreasing the proportion of meat and dairy products as well as processed foods and sugars will have significant impacts on levels of obesity and a number of diseases related to it, such as cardiovascular disease, diabetes and allergies. Again, a coordinated programme encouraging people to improve their diets and buy locally produced fresh foods can have very positive impacts on both health and sustainability. Integrated programmes with other departments, including Agriculture and Environment, promoting these issues can appeal to people from a variety of aspects and have many benefits.
6. Integrated Solutions to Obesity
To summarise, adopting an integrated approach to obesity, addressing several causal factors while promoting more sustainable lifestyles and food consumption, will have many benefits for public health and for the health service, as well as additional benefits to the community through enhanced provision of goods and services which will facilitate people to adapt to the changes facing us all in the 21st century.
We thank you for the opportunity to make these comments. We hope that you find them helpful and that they will be incorporated in your recommendations. If you would like to discuss them further please do contact us.
[1] Pretty et al 2005. ‘A Countryside for Health and Wellbeing: the physical and mental health benefits of green exercise’.
British Dietetic Association
The Northern Ireland Board of the British Dietetic Association brings together representatives of the dietetic profession in Northern Ireland. We are the strategic leading body for the profession in Northern Ireland.
We would like to thank you for the opportunity to respond to this Northern Ireland Assembly inquiry into obesity.
With rising levels of obesity, the associated health risks and the cost to the NHS and the economy, it is something that needs to be dealt with as a matter of urgency. Addressing this however, is a huge challenge that requires a pan-governmental approach. Dietitians have an essential role leading in its prevention and treatment at governmental, DHSS, Board, Trust and local community levels.
Dietitians have much to contribute influencing strategic planning and working in partnership with other health professionals and a wide range of stakeholders including voluntary/community groups, education, local councils, local supermarkets, The Food Standards Agency, the Health Promotion Agency etc.
Registered dietitians (RDs) are the only qualified health professionals that assess, diagnose and treat diet and nutrition problems at an individual and wider public health level. Uniquely, dietitians use the most up to date public health and scientific research on food, health and disease, which they translate into practical guidance to enable people to make appropriate lifestyle and food choices. This will be illustrated for obesity with examples below.
Dietitians have a unique contribution to make to the prevention and management of obesity at all levels including:
- Regional - e.g. DHSSPSNI Obesity Prevention Steering Group, Health Promotion Agency, Food Standards Agency, etc.
- Commissioning and regulation – assessing needs to inform design of services and contribute to delivery and monitoring.
- Organisational policy – e.g. implementation of NICE Obesity guidelines, FSA guidelines on food served to adults in major institutions.
Please find below information relating to the Committees particular areas of inquiry:
Assess the scope and appropriateness of the current approach to the prevention of obesity & the promotion of lifestyle change.
Dietitians in Northern Ireland are involved in a large number of nutrition programmes and initiatives that have been developed and delivered in partnership with a variety of other agencies. A recently produced leaflet, ‘Dietitians: Working to improve public health through nutrition’ (enclosed) outlines the contribution of those who specialise in this field and the contribution they make to delivering current NI strategies, e.g. ‘Investing for Health’ and ‘Fit Futures, Focus on Food, Activity and Young People’.
Funding for these initiatives however, is often short term and non-recurrent. Further support including mainstream/long term funding to allow successful, validated pilot programmes to be sustainable and to promote life-long changes which are of benefit to peoples’ eating and lifestyle patterns are required.
A comprehensive and coherent approach to prevention is necessary to ensure that all opportunities to intervene are taken; for example promotion of maternal nutrition, breastfeeding, opportunities for physical activity. Many interventions that aim to prevent obesity are school directed despite evidence that preschool years are really important in establishing appropriate eating habits. There is a need for dedicated programmes aimed at families with young people.
It is also important that opportunities are maximised, for example, the free fruit in schools scheme provided free fruit for young children at primary school but there was little reinforcing of the messages through additional work with children and parents. Where the latter approach has been included elsewhere evaluation demonstrates increased fruit intake within and outside school.
Examine the availability of weight management or other interventions to tackle obesity-related ill-health.
There is evidence to support the use of a variety of dietary treatment approaches to weight loss (NICE 2006). It is recognised that weight loss occurs initially and is then followed by weight stabilisation (NICE, 2006). The degree of weight loss seen, while clinically significant, may not meet the expectations of the client or referrer. Careful consideration is required when goal-setting with the client and behaviour changes should be maintained in the long term, via realistic, achievable goals, preferably set by the clients themselves (DOMUK, 2007).
In most Trusts in NI inpatients referred to the dietetic service receive dietary treatment during admission. However, in many areas, current resources do not enable outpatient support post discharge.
Recent capacity and demand analysis calculations for the Service Delivery Unit AHP waiting list initiative demonstrates that only limited dietetic time is available for weight management of outpatients. This represents historic capacity and is in no way capable of addressing the obesity epidemic. Dietitians currently treat people with obesity within general clinic settings. Rarely have dedicated specialist clinical obesity services been commissioned.
In relation to the SDU AHP waiting list initiative, the new draft dietetic access criteria suggest that adults with BMI > 30 who demonstrate readiness to change, will be eligible to be referred to dietetic services. The anticipated demand that this will generate for dietetic services is concerning unless additional service capacity is commissioned.
While obesity forms part of the dietary management of diabetes, heart disease, cancer, etc. current resources do not allow evidence based obesity management as would be determined by NICE Obesity Guidelines 2006.
Dietitian led pilots of Intensive Weight Management Services, supported by the drug industry and some using anti-obesity drugs, have been extremely successful. Patient outcomes met and indeed exceeded weight loss targets in research and the Royal College of Physicians guidance at that time using a combination of dietary treatment, behaviour change techniques and exercise programmes. Many of these services were stood down due to the inability to secure recurrent funding. The specialist services recommended in 2005 in the CREST ‘Guidelines for the Management of Obesity in Secondary Care’ have never been commissioned.
It is also important to recognise that accepted dietary and lifestyle approaches to weight loss and maintenance are difficult and require commitment, time and skills. Many people have been raised in homes where food was not home-cooked, and attended schools where cookery and practical skills were not taught. In these cases, even if they are willing to change, they will be unable to do so unless empowered with the required skills and capabilities (Maryon-Davis, 2005). Practical approaches, such as cookery sessions, supermarket tours, and food label reading advice may help to bridge this gap and make sustained change possible. Dietetic Support Workers have a key role to assist in achieving this.
Behaviour change training and group facilitation skills should be considered essential for healthcare professionals, in order that any opportunities to intervene are maximised.
Consider what further action is required, taking account of the potential to learn from experience elsewhere.
The Review of Public Administration in NI provides an opportunity for new organisations to work in partnership to tackle obesity. The challenge for all parties working in prevention and management of obesity is how to provide sustained support to individuals and the likely impact this may have upon scarce resources.
Obesity should be recognised as a disease in its own right with appropriate streams of funding to deliver evidence based clinical management for all ages, in all setting and across all programmes of care.
‘Healthy Weight Healthy lives’ (Department of Health, January 2008) promises to support the commissioning of more weight management services in England by providing extra funding. A similar strategy for obesity management is required for NI supported by an Obesity Framework. This requires cross-governmental strategies involving health, education, transport, planning and local councils etc. Tough strategic decisions, similar to those being taken for smoking, from the NI Assembly / DHSSPSNI need to be implemented. 23 % of the population smoke and 100% eat.
We need to achieve a suitable balance between preventing and managing obesity and individual choice. We need to challenge the public in relation to balancing their right to eat what they choose and their responsibility for their own obesity related ill health.
DHSSPSNI and other NI departments should lead by example and look to their own public authority facilities in the first instance to promote healthy food options and limit promotion of less healthy options. FSA guidance is available for suitable food standards in public sector. This can be supported by practical guidance for implementation, e.g. SHSSB, Nutrition in the workplace: A Toolkit for Action, Guiding Principles.
Initiatives like those in relation to vending machines in Wales should be considered, not only for DHSSPSNI, but also across all of the public sector.
In the same way that sustained change is needed by individuals to achieve and maintain weight loss, a sustained approach by Government and other funding agents is needed to allow work done on the ground to be continued and evaluated over time. The publication of ‘Choosing Health’ (Department of Health, 2004) has meant that longer term funding has been available in the NHS and many potentially useful community-based initiatives have occurred as a result.
England has led the way with the appointment of Consultant Dietitians in Obesity. The current work of dietitians in Northern Ireland needs to be further supported and strengthened to include leadership from highly expert dietitians who can concentrate on this area and support all Health Care Professionals to play their part. Equally the role of Dietetic Support workers in prevention and management of obesity needs to be further developed.
The Northern Ireland Board of The British Dietetic Association recognise that obesity is a complex issue and dietitians have a unique contribution to make. In this response we have outlined a number of ideas which are not exhaustive. We would like to request a meeting to take the opportunity to discuss this inquiry in more detail with the Health Committee.
References
Clinical Resource Efficiency Support Team (2005) Guidelines for the Management of Obesity in Secondary Care.
Cross-Government Obesity Unit, Department of Health and Department of Children, Schools and Families, January 2008, Healthy Weight, Healthy Lives: A cross-government strategy for England.
Department of Health (2004) Choosing Health, Making Healthier Choices Easier. White Paper. Department of Health: London.
Dietitians in Obesity Management UK (2007) The Nature of the Dietetic Intervention: is it time for a radical rethink? England: DOMUK.
Department of Health, Social Services and Public Safety, March 2002, Investing for Health.
Fit Futures Focus on Food Activity and Young People, January 2006.
Maryon-Davis A (2005) Weight management in primary care: how can it be made more effective? Proc. Nutr. Soc. 64 (1): 97-103.
National Institute of Health and Clinical Excellence (2006) Obesity: the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. England: NICE.
Royal College of Physicians (1998) Clinical management of overweight and obese patients. London: RCP.
Belfast Health and Social Care Trust
It is an accepted fact that a majority of medications prescribed for psychiatric conditions are responsible for weight gain and can lead to the development of obesity in patients.1 This is particularly the case with the use of antipsychotic, mood stabilisation and anti-depressant medication.2 Individuals with long term enduring mental illness can self regulate symptoms such as low self esteem, anxiety and problems with body image by comfort eating .This situation maybe further exacerbated by other associated symptoms of their condition such as lethargy and low motivation to change patterns of behaviours. Hence people with mental illness are predisposed to the development of obesity by the nature of their illness; the situation is however made worse by the fact that the medication prescribed for the treatment of their condition does in fact further increase their likelihood of developing obesity.
Crest Guidelines 2005 highlight the serious obesity related co morbidities such as heart and peripheral heart disease, diabetes, hypertension, cancer and problems with the loco motor system. The Crest Guidelines highlight the fact that even a 10% reduction in weight can induce up to a 50% reduction in obesity related cancer deaths, up to a 50% reduction in the development of diabetes as well as having a significant positive impact on lowering blood pressure cholesterol levels.
With obesity a significant and escalating problem in modern society, and the Government’s increasing emphasis on physical activity as a major part of the solution, physiotherapists are in an ideal position to help people make informed decisions on how to lead healthy lifestyles and enjoy maximum quality of life.
The promotion of physical activity in management of mental health is well established .Physical activity can enhance mood increase socialisation as well as contributing to weight reduction and the associated positive impact on the individual’s physical health. The role physiotherapy has been to date very underutilized within mental health and with the appropriate resources could demonstrate the effectiveness of the use of core physiotherapeutic skills in the management of mental health problems with particular reference to the management of obesity.
Statutory providers should take advantage of the knowledge, skills and experience that health professionals such as physiotherapists have as part of its overall approach to encouraging and enabling physical activity in the challenge to decrease the growing problem of obesity in contemporary society.
Physiotherapists working in mental health have in depth knowledge of the mind body relationship and have an understanding of the physical manifestations of mental health problems. This is fundamental in the formation of a good therapeutic relationship with the client and can empower the client to make the required changes to achieving improvement in their mental and physical health. Physiotherapists are very experienced in developing and tailoring exercise sessions to manage weight, for example, running classes such as cardiac and pulmonary rehabilitation sessions for those who have specific co morbidities and supervising more generic classes such as pool exercise, relaxation and core stability run by exercise instructors. Physical fitness in people with mental health problems and learning disabilities is considerably worse when compared to controls of similar age. People with schizophrenia have been found to have poor levels of physical fitness compared to the general population.3 Hospital based patients with depression also have lower levels of physical fitness compared to non-hospitalised groups. For these potentially higher risk patients, the knowledge of exercise physiology, underpinning clinical knowledge and appropriate clinical assessment skills place the Physiotherapist in an ideal position to ensure safe, individually targeted and effective exercise programmes are implemented for a wide range of acute as well as community settings.
Anxiety and depression are two of the most common presentations of mental illness. Socioeconomic factors can contribute to mental health, poor diet; lack of exercise, the absence meaningful activity and the effects of medication can lead to a predisposition to overeating and the development of obesity. Exercise can also reduce trait anxiety and is comparable in effect to other forms of psychotherapy used to treat anxiety .Exercise for people with schizophrenia can improve social interest, the energising effects from the exercise, can lead to improved behaviour, lowering of depressive symptoms and increased self-esteem .
Physiotherapists have the skills to access individuals with obesity problems by developing good therapeutic relationships, once formed the treatment aims shifts to improving body awareness by physical interventions such as massage, acupressure and Tai Chi. Once an improvement in body awareness has been achieved the individual is better placed to engage in supervised one to one exercise programmes. This may develop into group based activity with the ultimate goal being for the individual to acquire the motivation to self regulate their own physical activity and body weight. The knowledge and skill could also be effective in the prevention of obesity .Physiotherapists are best informed to educate and develop the individual’s exercise potential which in turn would have a positive impact on lifestyle change.
There is a growing acknowledgement that body awareness is very important in allowing clients to feel ownership of their physical self, a situation that may have become distorted due to the their psychological problems. The physiotherapist can offer acknowledgement of the mind body relationship by skilled and targeted physical interventions ranging from manual therapy techniques to relaxation, acupuncture and specialised exercise programmes. All of these help to improve the body image satisfaction. Once the individual has achieved this, they are in a much better position to take control of their body are more receptive to make changes to help improve their condition. One author highlights the benefits of the active involvement of physiotherapists within the multidisciplinary team in the mental health setting e.g. eating disorders The application of physical treatments were also found to be appropriate in a condition that is largely regarded as a psychiatric/psychological problem. In particular, physiotherapy was perceived as a useful application in the management of distorted body image.5
New ways of working in Psychiatry 2005,2007 advocates a review of working practices to ensure improved person centred ,needs led and cost effective services. In order to achieve this, there must be a more flexible and effective use of existing resources and expertise. Complementary therapies have in recent years been granted funding in some mental health services. It is acknowledged that such therapies have made a worthwhile contribution. However it could be argued that allied health professionals such as physiotherapists have not been given the opportunity to realise the full potential and effectiveness of their skills and knowledge in the treatment of mental health conditions and existing co morbid conditions such as obesity.
References
1. Virk et al 2004 Psychiatric medication induced obesity: an aetiological
Review Obesity reviews Volume 5 Issue3 167-170
2. Schartz et al 2004 Psychiatric medication induced obesity: Treatment options Obesity Reviews Volume 5 issue 4 233-238
3. Donaghy ,Durard 2000 A report on the Clinical effectiveness of physiotherapy in mental Health Chartered Society of Physiotherapy London
4. Donaghy, Durard 2000 A report on the Clinical effectiveness of physiotherapy in mental Health Chartered Society of Physiotherapy London
5 . Rosen 1995 assessment and treatment of Body Image Disturbance Eating Disorders and Obesity
Guildford press New York
6 . Broadbridge 1998
International Journal of Therapy and Rehabilitation, Volume 4 Issue 6, 01 Jun 1998, pp 284 - 290
The Institute of
Public Health in Ireland
Introduction
The Institute of Public Health (IPH) aims to improve health on the island of Ireland by working to combat health inequalities and influence public policies in favour of health. The Institute promotes cooperation between Northern Ireland and the Republic of Ireland in research, training and policy advice.
IPH congratulates the Health Committee on selecting obesity as its subject for inquiry and welcomes the inquiry’s focus on the scope and new possibilities for obesity prevention. IPH thanks the Committee for the opportunity to contribute our views and experience.
Summary
- The UK Foresight report offers an in-depth understanding of the nature and complexity of obesity, its causes and approaches to address them. IPH believes this report provides an excellent basis for a strategic framework to guide a sustainable and effective response to obesity in Northern Ireland.
- As well as developing a longer term strategy, urgent and shorter term action is needed to coordinate current activities and ensure focus on the most vulnerable groups. This is particularly important during the recession when the cost of healthy food may act as a real barrier to healthy eating. A strong strategic approach should link to other key government policies on poverty, social inclusion and sustainable development.
- Most of the actions which are needed to prevent obesity fall outside the health sector. A cross government and wider societal response extending well beyond the health sector is required to halt the rise in obesity and its harmful consequences. New forms of incentives should be explored to ensure the strong and effective cross departmental support which is essential to reduce the barriers which are hampering effectiveness.
- The Executive’s PSA target to halt the rise in obesity is welcome. Intermediate outcomes and targets should also be set to measure progress and identify gaps in knowledge.
- The recent NIAO report calls for action to strengthen knowledge and evidence, build relevant information systems and link science, policy and action. IPH strongly supports this call.
- There is a strong case for working with other jurisdictions including other parts of the UK, Ireland and Europe. This should be done in a systematic and transparent way, and used to identify areas of cooperation and learning.
1. Extent and impact of obesity
1.1 In 2007 an extensive UK Foresight Report pointed out that nearly 60% of UK population could be obese by 2050, with substantial health and economic implications. A similar picture exists in Northern Ireland with an increasing proportion of the population overweight and obese, and resultant significant costs to individuals and society. The case for action has been well spelt out in several government reports including Fit Futures and the recent Northern Ireland Audit Office report. Obesity is an important risk factor for a wide range of serious conditions including heart disease, cancer, hypertension and diabetes. IPH forecasts that over the period 2005 to 2015 there will be 26% increase in the proportion of people with Type 2 diabetes if current trends continued. The loss of productivity and the costs of care and treatment of obesity and related conditions have serious effects on the economy and threaten to engulf the health service. Obesity is estimated to cause 450 deaths per year, £14.2 million in lost productivity and £90 million cost to health and social care.
2. Why is obesity increasing?
2.1 Reasons for the rise in obesity have been widely analysed and debated. Society has radically altered with major changes in work patterns, transport, food production and food sales. As the recent UK Foresight study puts it “The pace of the technological revolution is outstripping human evolution and for an increasing number of people weight gain is the inevitable – and largely involuntary - consequence of exposure to a modern lifestyle. This transition has been at least three decades in the making……the causes of obesity are embedded in an extremely complex biological system set within an equally complex societal framework".
3. Strengthening the strategic response
3.1 Important initiatives have been set up and led by DHSSPS including the 2005 cross departmental strategy Fit Futures: Focus on Food, Activity and Young People which assessed levels of obesity in young people and described actions that should be put in place, and the 2007 implementation plan which also outlined an extensive range of proposed actions and responsible agencies.
3.2 The recently formed Obesity Prevention Steering Group (OPSG) will oversee implementation of Fit Futures and develop a new strategy for obesity prevention across the life course. Groups have been set up on data and research, nutrition and food, physical activity and education, and each of these groups has agreed terms of reference.
3.3 We suggest that regular reporting through e-bulletins compiling the actions of and outcomes of each of these groups would keep the issue on the political agenda and public agenda and inform professional in the field thus encouraging cooperation and avoiding duplication or the feeling that not enough is being done. It would also allow for transparency of funding decisions.
3.4 Many current local initiatives are highly innovative and based on strong intersectoral partnerships but research and experience suggest their effectiveness is often hampered because they are not supported by a wider strategic approach. A task for the OPSG is to ensure coherence between regional and local work.
3.5 There are now a huge range of initiatives aimed at promoting healthy eating and physical activity, and many organisations in Northern Ireland and across the island have responsibilities in these areas. Clear agreement is needed on who is responsible for what, with assigned responsibility and accountability to develop, disseminate and support implementation.
3.6 We concur with the published reports and support the approach that is being taken. However we also have a number of suggestions which we believe need to be considered.
4. What else is needed?
4.1 The recent Northern Ireland Audit Office report noted and welcomed the DHSSPS developments but stated clearly that more needed to be done.
4.2 IPH feels that as well as a strategic population based response, action is needed in the short and medium term to prevent the substantial and immediate harm being wrought to individuals and society.
4.3 There is a need to identify the groups that disproportionately carry the burden of obesity and respond by providing appropriate services and support to those who have most need. The Public Health Alliance report on food poverty identifies this as a priority.
4.4 Obesity is more prevalent in people who are poor, and there is a strong socioeconomic gradient in obesity. The proposed Northern Ireland obesity strategy should consider the findings of the recent report of the Commission on the Social Determinants of Health (CSDH) which sets out how nations should respond to the appalling health gap within and between societies, and ensure that the new strategy is closely linked to government strategies to tackle poverty and social exclusion.
4.5 It is currently difficult to grasp what is going on and identify what is working well. Coordination should be a priority for the new Public Health Agency which could lead a more systematic and coordinated approach, support the work of primary care teams and reduce current fragmentation and duplication. The emerging role of local government in community planning and the strengthening of its role in public health provides opportunities for local action.
4.6 Good local work by many professionals has been hampered by weak legislation on food labelling and promotion of high fat products to adults and children. During the recession it is more important than ever to ensure healthy food is affordable, and that local action is effective.
4.7 IPH suggests identifying good practice by the development of a toolkit of (accredited) community-based interventions for tackling poor diet, inadequate physical activity and obesity in various settings.
4.8 The setting of a PSA target to halt the rise of obesity by 2010 is welcome but intermediate outcomes are also vital to complement this high-level target and establish if progress is being made. Adequate knowledge may not exist to define appropriate and measurable targets and IPH suggests that as gaps in our knowledge become apparent, research should be commissioned and information systems developed so these gaps can be filled.
5. Cross government action
5.1 A systems approach, defining obesity as a societal and economic issue, requires cross party support and the commitment of the NI Executive and wider society. The Foresight report outlines the importance of strong leadership and accountability.
5.2 We note the programme for government sets a PSA target “to halt the rise in obesity by 2010". Any plan to achieve this target requires cross government support and action by sectors responsible for food and agriculture, transport, planning, education and finance. IPH would welcome the Health Committee’s role in advocating for cross party support to ensure action across government and the wider business sector. Without this IPH believes that it will not be possible to halt the rise in obesity.
5.3 Most of the upstream work that is needed will be by non health departments and their agencies and the mechanisms for ensuring that this happens need to be robust and clear. IPH suggests that the Health Committee considers the setting of joint PSA targets agreed between government departments with shared accountability for delivery.
5.4 Responsibility for cross departmental work lies with the cross department Ministerial Group on Public Health (MGPH). IPH suggests a stronger approach involving all Minsters in this important social and economic threat. Transparency of meetings with minutes and decisions published on the web and regular reports on progress would inform and encourage wider social action.
5.5 Northern Ireland’s broad based and cross government strategy Investing for Health (IfH) recommended that all government policies should consider their impact on health. IPH has produced guidelines on health impact assessment (HIA) and many policy-makers and practitioners have been trained in the HIA. The Health Committee could play a very significant role by insisting that all government policies were assessed in terms of their health impact, with particular reference to the impact on health inequalities and the obesogenic environment.
5.6 IPH has produced reports which outline the impact on health of the built environment, transport and education and these offer guidance for government departments and other agencies on ways in which policies could be more supportive of good health.
5.7 As the recession impacts on the finances available to public services, it is essential that an effective public health approach is taken and that vital cross sectoral work and “upstream work" is supported.
6. Beyond the health sector
6.1 International analysis demonstrates that effective action requires the full commitment of sectors beyond the health sector as numerous policies and actions beyond the health sector are highly influential in determining what we eat and how active we are. The importance of working with and gaining full commitment from sectors including education, food, built environment, leisure and transport is crucial. To illustrate this we use examples relating to the food industry, and the built environment.
6.2 A recent IPH evaluation of the Decent Food for All (DFfA) intervention in the Armagh and Dungannon Health Action Zone highlighted the very significant role played by the large multiple, discounter/freezer and affiliated independent stores like Tesco, Sainsbury, Spar and Centra. It is essential that the food industry acts responsibly on issues such as the composition of food products, sourcing and pricing of food products, simpler, consistent food labelling across the island and controls on food marketing in the media and in-store promotions - particularly those aimed at children, as well as the location and content of retail food outlets.
6.3 We believe that an urgent response is needed by the food sector including well designed and binding rules to provide clear and prominent nutrition facts and information and restrict fraudulent claims. We think that voluntary codes of practice are unlikely to achieve the depth and strength of change that is required to protect health. There is a particular worry that the recession will impact on the ability of people’s ability to afford healthy food resulting in greater intake of high fat, high calorie food.
6.4 An important way of encouraging physical activity is through changing our built environment. For example recent guidance from the National Institute for Clinical and Health Evidence (NICE) states everyone concerned with the “artificial environment" and those planning the use of natural environments should be maximising the potential for physical activity. All planning applications should give priority to people’s exercise. Transport planners should give priority to pedestrians and cyclists by widening pavements, and introducing more cycle lanes. www. nice.org.uk/ PH008
7. Strengthening evidence-informed policy and practice
7.1 The Foresight report noted that “Integrating science and policy in a model of continuous quality improvement is critical" to the success of our efforts to tackle inequalities.
7.2 Creating better links between research, policy and practice is a key objective of the new UKCRC Centre of Excellence in Public Health (a partnership between Queen’s University, IPH, the Community Development and Health Network and W5). The Centre is carrying out high level research in areas including food choices, economic incentives, land use and social policy. Researchers in these areas (and other key researchers in Northern Ireland) can aid the Health Committee and ensure that relevant research is used to inform policy and practice. IPH suggests that the Health Committee conduct a round table involving local researchers to consider what can be learnt to assist an effective response in Northern Ireland.
7.3 Guidelines from the National Institute for Clinical and Health Evidence (NICE) are applied as appropriate in Northern Ireland. We need to look at developing better strategies to implement these guidelines in practice and ensure we achieve the expected benefits.
7.4 An obesity observatory was established in late 2008 by the English Department of Health to strengthen evidence-based policy and practice. IPH has been exploring the utility of establishing an obesity observatory to support implementation of the obesity strategy by widening access to data, evidence and good practice, developing the evidence base, helping to implement good policy and practice, and monitor obesity, its determinants and consequences.
8. Working with UK, Ireland, and Europe
8.1 Many of the factors that affect our diet such as the production, marketing and distribution of food either operate at national, all island, European and global level. It is vital that we cooperate with national and international organisations and make good use of international experience. We must also recognise the fundamental role of the Common Agricultural Policy (CAP), EU competition regulations and advertising rules in influencing our food policies, sometimes in ways which are harmful to health.
8.2 As trends demonstrate obesity develops slowly within individuals and communities and a long term sustained approach spanning several generations is needed to prevent the alarming health and economic effects of obesity.
The Department for
Regional Development
1. The Department for Regional Development is keen to play its part in the collective effort to tackle the threat to health and well-being that is posed by obesity. Obesity causes around 450 deaths each year in the North and evidence shows that it:-
a. reduces life expectancy by approximately 9 years;
b. increases the risk of the North’s biggest killers, coronary heart disease and cancer;
c. increases the risk of developing Type 2 diabetes; and
d. can impact on emotional/psychological well-being and self-esteem, especially among young people.
2. Given that as many as one in five adults and nearly one in ten children between the ages of two to ten in the North are classified as obese, the scale of the problem is clearly significant.
3. Taking regular exercise is known to be an effective method of reducing the rate of cardiovascular disease and research shows that 30 minutes of physical activity each day could significantly improve people’s health.
4. The Department has developed strategies over recent years and put operational initiatives in place to encourage a change in travel behaviour, away from the use of the private car towards more sustainable and healthier means of travel, such as walking and cycling.
Shaping Our Future: Regional Development Strategy for Northern Ireland 2025
5. In 2001 the Department’s Regional Development Strategy recognised the importance of the need to change the local travel culture and at the same time contribute to more active and healthier lifestyles. In particular, the Strategy recognised the need to revive the healthy habits of walking and cycling, for short journeys, by people of all ages. In addition, all planning policy introduced, after the adoption of the Regional Development Strategy, has made walking and cycling an integral part of the planning process for new development.
Regional Transportation Strategy for Northern Ireland 2002 2012
6. In 2002 the Regional Transportation Strategy recognised the importance of walking and cycling as sustainable, healthy and socially accessible forms of transport. The Strategy doubled the proposed levels of funding for walking and cycling infrastructure, as well as raising the awareness of the benefits of such activities. The associated local Transport Plans, which support the Strategy, include walking and cycling blueprints for all our major towns and cities. These aim to establish extensive walking and cycling networks, which will be well used, are safe and enjoyable, and give access to all who wish to pursue a healthier lifestyle.
Northern Ireland Cycling Strategy
7. In 1998 the Department established a Cycle Forum to help develop a cycling strategy for the North, in co llaboration with a range of partners. The Cycling Strategy, published in 2000, identified a number of measures to improve conditions for cyclists and promote a pro cycling culture locally. The Strategy formed the basis for the support and recognition given to cycling in the Regional Transportation Strategy and the subsequent Transport Plans.
Northern Ireland Walking Strategy
8. In 2003 the Department published a Walking Strategy with the assistance of the Walking Forum. It contained a series of 80 actions to improve facilities for pedestrians. Measures were subsequently incorporated into the walking blueprints in the Transport Plans for our urban areas, to support walking as a travel mode.
Road Safety and Speed Limits
9. Road safety is a key priority for the Department and we have always been conscious of the need to manage traffic speeds, particularly in the vicinity of schools as a major contributor, to encouraging sustainable travel to and from school.
10. The Department’s Roads Service continues to roll out a programme of signs, road lining, and in certain areas, reduced speed limits have been introduced at schools, to make motorists aware of the presence of children walking and cycling to school. As part of this programme, Roads Service has initiated a trial of part time speed limits at two schools near Coleraine and Ballymoney. This 20mph speed limit is only in force at the start and finish of the school day, at the period of highest risk to children walking and cycling to school. Early indications are that the pilot schemes have been successful in reducing speed and there has been a broad welcome from the schools and communities involved.
11. The concept of the 20 mph speed limits at schools forms part of a wider consultation on the setting of speed limits generally, which the Department launched in January 2009. Comments received, as part of the consultation, will help formulate the final policy on the setting of speed limits.
Travelwise Safer Routes to Schools Initiative
12. In 2004 the Department launched the Travelwise initiative to raise awareness of sustainable travel options and to demonstrate to businesses, commuters and schools that they could all play their part in meeting the challenge of developing healthier lifestyles.
13. Since 2004, the Travelwise Safer Routes to Schools team has been tackling the issue of “the school run" by promoting more walking, cycling and greater use of public transport, as well as car sharing for the journey to and from school.
14. The Safer Routes to Schools programme includes:-
- curriculum based education resources;
- promotional materials;
- improved signage and route markings;
- cycle shelters and lockers;
- walking and cycling initiatives;
- road safety training;
- development of School Travel Plans and School Safety Zones; and
- improved infrastructure within the school grounds and on the public roads.
15. The Department has already made a significant difference through the Safer Routes to Schools initiative and since its introduction in 2004 has worked with 151 schools, involving over 45,000 pupils and their parents and has committed over £2.3 million to the initiative.
16. In 2008 during Walk to School Week, 200 schools registered for activity events, and over 41,000 pupils and their parents took part. In a survey carried out to evaluate the Safer Routes to Schools scheme in 2007/08, 50% of the schools which took part confirmed that they observed more children walking and cycling to school.
Inter-Departmental Activity
17. Through the DRD-constituted School Travel Advisory Group (STAG), officials work with the Departments of Education, Environment, Health, Social Services and Public Safety and other partners, such as Translink and Sustrans, the Sustainable Travel charity, to co ordinate the approach and optimise combined organisational efforts, to promote sustainable, safe and healthy school travel.
18. Whether through the Department of the Environment’s Road Safety Education Programme, or the Department of Education’s improvement of facilities within the school estate, or Department for Health, Social Services and Public Safety (DHSS&PS) jointly developed fitness awareness education campaign, the benefits of a multi-agency approach are recognised as significantly affecting and contributing to the numbers walking and cycling to school. Children taking part in physical activity, which in turn encourages parents, teachers and others to participate as part of the daily routine, is very much a target for STAG.
19. The Department is committed to playing its part within the structures established by the DHSS&PS to address the problems presented by obesity and take forward the Fit Futures Action Plan. The Department considers it important for the Travelwise team to continue to contribute to the work of the Obesity Prevention Steering Group and its advisory Sub Groups, including the Promoting Physical Activity Group (PPAG).
20. PPAG has invited specific organisations, one being Sustrans, to develop proposals for the purposes of specifically providing a possible 5 year programme, across the North known, as the “Active School Travel Proposal for Local Schools". This records a multi agency approach to promoting and funding a Sustainable School Travel Initiative, to over 200 schools per year. The PPAG will shortly seek to co ordinate a multi agency funding bid to the Assembly for approval.
Conclusion
21. The Department is committed to making its contribution towards tackling obesity, primarily through its Travelwise campaign, to promote alternatives to the private car and encourage the adoption of healthier travel options such as walking and cycling.
22. The Department is also supportive of the multi-disciplinary, inter-agency approach to developing a comprehensive strategic response to obesity and will continue to play an active part in the work of the Obesity Prevention Steering Group and its sub groups.
Public Health Alliance
Obesity is a growing and significant public health threat within our population. It is a complex issue which will require integrated cross-cutting solutions and involve much more than interventions and services aimed at addressing lifestyle and behaviours.
As with most major public health challenges the root causes and ultimately solutions will lie largely outside the health service. In 2007 the Public Health Alliance supported by the University of Ulster; the Institute of Public Health (in Ireland) and the Chartered Institute of Environmental Health concluded a two year research project which examined the scope and extent of food poverty in Northern Ireland. I enclose copies of the both the executive summary and the full report as the basis for and background to our submission.
Whilst clearly food poverty is in itself a wholly different challenge, nonetheless there is strong evidence to indicate that people living in food poverty almost always have a diet which predisposes them to the risk obesity.
Perhaps more importantly many of the findings and recommendations from this report have significant implications and linkages with future efforts to tackle obesity. You may wish to note the recently established Obesity Prevention Strategic Group is considering the findings from this report as part of their deliberations.
PHA would very much like the opportunity to discuss this issue in more detail with the Committee and would be happy to present evidence on it if deemed appropriate.
British Heart Foundation
Northern Ireland
Introduction
1. The British Heart Foundation Northern Ireland
1.1 The British Heart Foundation Northern Ireland (BHF Northern Ireland) is the UK’s heart charity, dedicated to saving lives by investing in pioneering research, supporting and caring for heart patients and their families, campaigning for change and providing vital information to help people care for their own heart health.
1.2 BHF engagement in public health is broad-ranging, and we fund a number of organisations including the BHF Centre for Physical Activity and Health at the University of Loughborough and the BHF Health Promotion Research Group at the University of Oxford. We are also active members of the European Heart Network.
2. Heart and circulatory disease
2.1 Heart and circulatory disease is Northern Ireland’s biggest killer – responsible for more than one in three deaths each year[1]. Of the 14,532 deaths in Northern Ireland in 2006, 4,879 of them were from heart and circulatory diseases.
3. Obesity
3.1 Obesity is a major risk factor for heart disease. The INTERHEART study estimated that 63% of heart attacks in Western Europe are caused by abdominal obesity.[2]
3.2 As in the rest of the UK, obesity levels in Northern Ireland are high, and represent a substantial public health risk. Figures published in January 2008 show that over 144,945 people in Northern Ireland are obese[3]. The Health and Wellbeing Survey 2005-06 found that a quarter of men and 23% of women in Northern Ireland were obese, an overall increase in adult obesity of 26% since 1997.[4]
3.3 Across the UK it is estimated that if current trends continue, by 2050 overweight or obesity will affect nine out of ten adults and two out of three children[5].
4. Key recommendations
- The Fit Futures strategy must be accompanied by adequate resources and systems to monitor and evaluate success
- The Service Framework for Cardiovascular Health and Wellbeing must be financially supported and fully implemented
- All government departments and agencies must work together and take a joined up approach as part of a long term strategy to reverse obesity
- The Northern Ireland Assembly should champion central government level prevention measures including a 9pm watershed ban on advertising of unhealthy food to children on television
- The Northern Ireland Assembly should oversee urban planning policies which promote physical activity
- The Northern Ireland Assembly should dedicate at least as much energy on encouraging participation in physical activity as for competitive sports
- The Northern Ireland Assembly should ensure that all public health policy seeks to address health inequalities
5. Views on tackling obesity
5.1 BHF Northern Ireland welcomes the health committee’s call for evidence on tackling obesity.
5.2 BHF Northern Ireland believes that it is crucial to tackle the increasing incidence of lifestyle related disease by helping individuals to make healthier choices regarding diet and exercise; by supporting people with the creation of an environment which enables positive choices about health; and by ensuring that people already living with obesity are given the best help possible to change their lives.
6. General points
6.1 BHF Northern Ireland recognises that tackling obesity has been a Department of Health, Social Services and Public Safety (DHSSPS) priority for some time, and that more recently the Assembly’s Programme for Government has identified working for healthier people as one of the five key priorities. Tackling obesity and associated ill health will also help to reduce health inequalities in Northern Ireland.
6.2 Investing for Health highlights how crucial it is to engage with the population, so that people become more active in protecting and improving their own health.
6.3 BHF Northern Ireland agrees that providing people with the skills and information they need to improve their own lifestyles is important. However, legislative measures to create a health enabling environment are also required from the UK Government and Northern Ireland Assembly. These should include:
- Action to support the introduction of a 9pm watershed ban on the advertising of unhealthy foods
- The mandatory introduction of a front of pack labelling system based on Multiple Traffic Light principles
- Local planning policies which protect green space and promote active travel.
6.4 In order to deliver Fit Futures, BHF Northern Ireland considers the following to be essential:
- The Public Service Agreement target to halt the rise in obesity by March 2010 should be revised
- Funding must be available to deliver the Fit Futures priorities in the long term as obesity will not be reversed in the short term.
- Systems must be in place to monitor obesity levels and evaluate successful initiatives so that they can be rolled out across Northern Ireland.
- All government departments and agencies must be working together in a joined up fashion
7. Food marketing to children
7.1 Poor diet is playing a major role in the growth in obesity[6]. Evidence confirms that television adverts have an impact on food choices and that there is an association between the proportion of overweight children and the number of food advertisements shown each hour during children’s television.[7] The Hastings Review[8] found that food promotion affects preferences not only at brand level (e.g. persuading people to choose one burger restaurant over another) but also, more importantly, at category level (e.g. persuading people to eat more burgers instead of fruit).
7.2 BHF Northern Ireland believes that children need to be protected from aggressive marketing of foods high in fat, saturated fat, salt and sugar (HFSS) and we have been a leading voice in the call for a ban on such advertisements on television before 9pm.
7.3 Although Ofcom have put in place regulations which restrict HFSS adverts during dedicated children’s programming, millions of children are still exposed to such adverts during pre-watershed family programmes such as the X Factor or Coronation Street.
7.4 Additionally, BHF has published two campaign reports which highlight alternative, non-broadcast methods of marketing which food companies are now using to target children and their parents throughout the UK. How parents are being misled: a campaign report on children’s food marketing[9] highlighted how companies are playing parents concerns to actively market unhealthy children’s food. Protecting children from unhealthy food marketing outlined proposals for a regulatory system to limit the marketing of unhealthy foods to children in all settings.
7.5 Children using the Internet can also be subject to a variety of sophisticated marketing techniques. With the current largely self regulatory system in place it is near impossible to limit their exposure to company websites which use child-friendly characters and graphics, games, competitions and downloads to promote unhealthy foods and encourage brand loyalty.
7.6 Examples include:
http://www.knittedbynanas.com/
http://www.aglassandahalffullproductions.com/
http://www.irn-bru.co.uk/
7.7 These examples are illustrative and intended to provides examples of the kinds of tactics used. They are not a comprehensive review of all such material.
7.8 BHF Northern Ireland would like the Northern Ireland Assembly to:
- Adopt a position of favouring a mandatory ban on pre watershed advertising of HFSS foods to children on television, and strict regulation of non-broadcast marketing methods.
8. Food labelling
8.1 BHF Northern Ireland believes that a clear front of pack labelling system will help consumers to make healthier choices. We have been calling for a model that is underpinned by the use of the Food Standards Agency’s multiple traffic light colour coding.
8.2 GDAs in addition to traffic light colours would allow those who wish to make a more detailed analysis of nutritional content to do so, whilst allowing everyone to benefit from the at a glance colour interpretations.
8.3 A combination of traffic light colour labelling and GDA information was the favoured option by consumers who contributed to qualitative research carried out in September 2006 to inform the BHF’s position on signpost labelling. When presented with an example of colour coded GDAs, one consumer noted, “that’s just what we were asking for; something with the traffic light colours but the % RDA (recommended daily allowance) too".
8.4 There is further evidence to support a combined approach. For example, before launching the Multiple Traffic Light scheme, the FSA carried out large scale qualitative and quantitative research[10], which involved interviews with over 2,500 consumers to test their ability to use a number of labelling models, including MTL, monochrome GDA (MGDA) and colour-coded GDA (CGDA). Generally the Multiple Traffic Light model was the best overall performer, enabling consumers to correctly identify the healthiest food options on most occasions. However, the CGDA model also performed well, and both outperformed the model without colour coding.
8.5 BHF‘s How parents are being misled report identified a standard system of food labelling as a key way to help parents navigate confusing nutritional messages about foods, so that they can easily see which foods are not as healthy as the marketing messages claim they are.
8.6 BHF Northern Ireland would like the Northern Ireland Assembly to:
- Adopt a position in favour of mandatory front of pack labelling based on the principles of the Multiple Traffic Light Model. This should be incorporated into the upcoming Food and Nutrition Strategy and Action Plan.
9. Physical activity
9.1 Increasing levels of physical activity is an important part of reversing current trends in obesity.
9.2 BHF Northern Ireland believes that all aspects of the environment can be harnessed to promote physical activity including streets and routes that are attractive to cyclists and pedestrians, well designed green spaces and parks and new buildings and schools which are managed to increase opportunities for physical activity. This will require concerted joined-up action across government.
9.3 In England, the BHF recently welcomed the Be Active Be Healthy strategy which includes a commitment to ensure that the forthcoming national planning policy review will help to tackle obesity and support healthy communities. The new strategy also includes a breakdown for each Primary Care Trust in England of the financial costs of physical inactivity. This research was undertaken by the BHF Health Promotion Group at Oxford University and should act as a lever to increase investment in physical activity at the local level.
9.4 The BHF is also a member of the Take Action on Active Travel coalition calling for a population-wide shift from sedentary travel to walking and cycling across the UK. Proposals include a ‘health check’ on every transport and land use decision, investing 10% of transport budgets in walking and cycling and introducing 20mph speed limits for streets used by children and close to schools and other public buildings.
9.5 The BHF National Centre for Physical Activity and Health has published research confirming that there are a number of barriers to physical activity for children and young people including embarrassment and self-consciousness about their bodies and competence. For example, girls and young women are less likely to participate in physical education classes at school. It is therefore important that children and young people are given a range of opportunities to participate in physical activity encompassing free play as well as organised sports. BHF Northern Ireland calls for government and schools to expend at least as much resource on encouraging participation as they do on promoting competitive sports[11].
9.6 BHF Northern Ireland supports recent guidance from the National Institute of Health and Clinical Excellence (NICE) which contains a number of recommendations including introducing a new 5 year campaign to promote physical activity, developed in consultation with children. The guidance also proposes co-ordinated local strategies to increase physical activity measured through regular evaluation, identification of a senior council member as a champion for children’s physical activity and making school facilities available to children and families outside the school day so they can take part in physical activity[12].
9.7 BHF Northern Ireland believes that the Northern Ireland Assembly should:
- Oversee urban planning policies which promote physical activity. We believe that the Northern Ireland Assembly might usefully replicate the approach of the Be Active Be Healthy strategy in determining the financial costs of physical inactivity according to each Health & Social Services Board.
- The Northern Ireland Assembly should dedicate at least as much energy on encouraging participation in physical activity as for competitive sports
10. Workplace health
10.1 The workplace offers significant potential as a setting to promote healthy lifestyles to the adult working population. This is well recognised in the UK but to date under-utilised.
10.2 The BHF jointly funded the Well@Work workplace health initiative which looked at ways of improving diet, increasing physical activity and determining which changes in and around the workplace can effect positive differences in employees’ health and achieve and lasting improvement to their lifestyles. The two year initiative comprised nine regional projects in England and encompassed 32 workplaces representing different sized organisations and sectors.
10.3 Several projects achieved modest increases in employees’ healthy behaviours. However, a crucial finding in the evaluation was that one-off projects did not sustain behaviour change in the absence of strong management involvement and supportive environments within the workplace (including the necessary facilities and amenities for active travel and healthy eating).
10.4 BHF Northern Ireland believes that the Northern Ireland Assembly should:
- Review and update the Workplace Health Strategy to ensure that workplaces are helping to support health and wellbeing.
11. Northern Ireland Structure & Policy
11.1 BHF Northern Ireland supports the DHSSPS’s policy commitment to improve the health and well-being of the people of Northern Ireland. Additionally, we support the development of a range of service frameworks which aim to set out explicit standards for health and social care that are evidence based and capable of being measured, and specifically the emphasis within all the frameworks on health and well-being.
11.2 BHF Northern Ireland believes the issue of obesity can only be addressed when the vision as outlined within policy is properly taken forward within operational plans, strategies and frameworks throughout all Health and Social Care structures in Northern Ireland. As outlined within our response to the Service Framework for Cardiovascular Health and Well-being we stressed our concern that the standards did not sufficiently address the connection between cardiovascular disease and inequalities such as social deprivation.
11.3 In reference to structures, we would emphasise the need not only for a joined up approach to public health throughout all health structures, but better interdepartmental working as well as closer working with the voluntary sector.
11.4 BHF Northern Ireland believes the vision is there to improve health outcomes through the new structures. We would stress that the relationship of the Regional Agency for Public Health and Social Well-being (RAPHSW) with the Regional Health & Social Care Board (RHSCB) and its Local Commissioning Groups (LCGs) is crucial in commissioning and the redesigning of services.
11.5 For policy objectives to become a reality, BHF Northern Ireland believes that the Northern Ireland Assembly should:
- Ensure that the Service Framework for Cardiovascular Health and Wellbeing is financially supported and fully implemented
- Ensure that all public health policy is subject to constant monitoring and evaluation
- Ensure that all health policy properly address health inequalities
- Encourage greater partnership working in the areas of early identification, primary and secondary prevention between the Health and Social Care and the voluntary sector in Northern Ireland
[1] www.heartstats.org
[2] Yusuf S et al on behalf of the INTERHEART Study Investigators (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study), The Lancet; 364: 937-952
[3] Data source: Payment Calculation and Analysis System (PCAS) as at 31 March 2008, taking account of locally resolved adjustments up to 30 June 2008
[4] NISRA Health and Social Wellbeing Survey 2005-06
[5] McPherson et al for Foresight (2007); Tackling obesities: future choices – project report, Government Office for Science
[6] The Strategy Unit (2008); Food matters: towards a strategy for the 21st century. The Cabinet Office.
[7] Changing children’s food preferences, Halford & Boyland.
[8] Hastings et al. (2003) Review prepared for the Food Standards Agency. Centre for Social Marketing: The University of Strathclyde
[9] How parents are being misled: a campaign report on children’s food marketing, British Heart Foundation, 2008
[10] Food Standards Agency, Qualitative Signpost Labelling Refinement Research, November 2005, 1
[11] http://www.bhf.org.uk/heartwise/index.asp?secID=1517&secondlevel=1521&thirdlevel=1526&artID=6949
[12] http://www.nice.org.uk/Guidance/PH17/Guidance/pdf/English
Sustrans
Sustrans is the UK’s leading sustainable transport charity.
Our vision is a world in which people choose to travel in ways that benefit their health and the environment. We work on practical, innovative solutions to the transport challenges facing us all. Sustrans is the charity behind the award winning National Cycle Network, Safe Routes to Schools, Bike It, TravelSmart, Active Travel, Connect2 and Liveable Neighbourhoods, all projects that are changing our world one mile at a time.
Preamble
“The top five policy responses assessed as having the greatest average impact on levels of obesity [include]: - increasing walkability / cyclability of the built environment….."
Foresight Tackling Obesities report, Government Office for Science 2007
Sustrans is pleased to be able to offer a contribution to the work of the Committee in considering obesity in Northern Ireland and how to address it. We have thirty years’ experience of practical promotion of walking and cycling through projects like the National Cycle Network and Safe Routes to Schools. In England, Scotland and Wales we have worked closely for almost a decade with Government health departments, the National Health Service and public health bodies to advance understanding of the role of active travel in healthy living, inform policy making and establish effective programmes in this area.
We hope this brief submission will be of use to the committee and are happy to expand or clarify on any details you may require.
Obesity and sedentary living
In recent years, across the developed world, the scale and cost of obesity and its implacable rising trend have come into sharp relief. The UK Government’s Foresight programme in 2007 showed that nearly 60% of the UK population could be obese by 2050. This would cause a seven-fold increase in the direct healthcare costs of overweight and obesity, with the wider costs to society and business reaching £49.9 billion (at today’s prices).
In Northern Ireland the cost attributable to lack of physical activity includes over 2,100 deaths per annum, equivalent to over 18,000 life years lost, and 1.2 million working days lost each year. The cost of physical activity and obesity to the NI Economy in 2010 is likely to exceed £500m.[1]
The Health and Social Wellbeing Survey 2005-06 found that a quarter of all men and 23% of women in Northern Ireland were obese. The survey findings also show that this represents an overall increase of 26% in adult obesity since 1997.[2] Analysis provided to the Clinical Resource Efficiency Support Team (CREST) group on the management of obesity[3] estimated that just stopping the year on year increase in levels of obesity would, over the next twenty years, save the Department of Health, Social Services and Public Safety £210 million.
There is clear consensus on the scale of the problem posed by obesity generally, and sedentary lifestyles particularly, and on the urgent need to tackle the problem. Approaches to tackling obesity focus on diet and nutrition (“energy in") and on active lifestyles (“energy out"). Sustrans recognises the importance of addressing both, but our comments are restricted to the area in which we work, the latter.
Importance of active travel in healthy lifestyles
Historic approaches to the promotion of physical activity have often sought to promote “exercise", “fitness" and sport, but a moment’s thought should clarify that these are not likely to be appealing to most inactive or overweight individuals. As the Chief Medical Officer for England has put it, “for most people, the easiest and most acceptable forms of physical activity are those that can be incorporated into everyday life. Examples include walking or cycling instead of travelling by car".[4]
In Northern Ireland, the Regional Development Strategy and Regional Transport Strategy now both recognise that action is required to increase levels of walking and cycling. At the consultation stage of Fit Futures a number of stakeholders highlighted the contribution that the achievement of current targets to quadruple cycling trips, and to increase by 10% the average distance walked per person, would make to obesity prevention.[5]
Addressing the obesogenic environment
The pivotal role of active travel in promoting activity among currently inactive people is now widely recognised, and we do not propose to dwell on it here. The issue today, in European societies at least, is how most effectively to promote active living, and how to bring about significant and sustained increase in the number of people choosing to travel in ways that benefit their health. For Sustrans, the key factor, but one which is unfortunately sometimes overlooked in discussion of policy and interventions on active living, is that the environment is the central determinant in people’s individual choices. Over recent decades we have allowed the environment within which we live to become dissuasive of physical activity, for example due to the dominance of our streets by motor traffic. This is now commonly called the “obesogenic environment" (this applies also to areas such as food retailing, which we do not address). In order to raise physical activity levels, we need to make the environment more conducive to active living, and this includes transforming the streets to be more walking and cycling friendly – just as Foresight recommended in our opening quote.
In a paper co-authored with public health, social medicine and physical activity specialists in 2003, Sustrans proposed that “modification of social, economic, and environmental factors may yield greater health dividends than individual lifestyle approaches. Indeed such interventions may be necessary before individual lifestyle approaches can be effective."[6] We hold to this view, and believe it is widely shared by experts.
For example, in its guidance on the promotion of physical activity and active living, the World Health Organisation recommends that “urban planners .…. need to integrate health and active living considerations fully into their work… … transport officials can provide a balanced transport system that enables residents to walk or cycle to shops, school and work."[7]
Guidance from National Institute for Health and Clinical Excellence
In our view, a key document from within the UK is the guidance published in 2007 by the National Institute for Health and Clinical Excellence (NICE) on physical activity and the environment. NICE acknowledged the crucial role of the environment in supporting or deterring physical activity, and in a typically thorough evidence review looked at over 94,000 published papers. The strongest evidence base NICE could find came from active travel – walking and cycling – and as a result the majority of the recommendations in their guidance relate to intervention in this area.[8] The box below illustrates the type of measures recommended by NICE, but we urge the Committee to consider the recommendations in their entirety, at http://www.nice.org.uk/Guidance/PH8/QuickRefGuide/pdf/English
This central focus on walking and cycling as physical activity is sustained in other guidance from NICE, and the Committee might also find it interesting to look at a checklist for local authority Overview and Scrutiny Committees, published by the Centre for Public Scrutiny, designed to assist elected authority members inquiring into the work done by their officers to promote active living. It prompts members to check on very similar points to those listed in the box. The checklist can be downloaded from http://www.cfps.org.uk/publications/item.php?itemid=88
NICE guidance puts walking and cycling centre stage in active living
NICE recommendations include:
- local facilities and services easily accessible on foot and by bicycle
- re-allocate road space from car to active travel
- restrict motor vehicle access (for example, by closing or narrowing roads to reduce capacity)
- road-user charging schemes
- traffic-calming to restrict vehicle speeds
- safe routes to schools
- provide a comprehensive network of routes for walking, cycling
Source: Promoting and creating built or natural environments that encourage and support physical activity, NICE, 2007
Effective implementation
We believe that policy in Northern Ireland is moving the right way. Fit Futures is offering a vision of joined-up policy on physical activity. It tells us that “Government departments and agencies should establish a common vision for physical activity and its role in delivering government objectives. This vision should include agreed targets to increase participation in quality physical activity, including sport and leisure, active play and active travel and to improve levels of physical skills among children and young people, and should inform planned strategies and programmes on sport, active travel, physical activity and play." However, until recently, there has been little done to actually implement Fit Futures and despite good initiatives by the Health Promotion Agency and the Physical Activity Coordinators the most recent NI Physical Activity Strategy was back in 1998-2002. It is therefore welcome and of the upmost importance, that the DHSSPS is producing an Obesity Strategy for Northern Ireland which we assume will outline actions needed to encourage active travel.
We are, however, concerned about the regular policy references to sport. It is most important that policy makers recognise sport as only a minority slice in the pie of physical activity, and not the most likely to appeal to currently inactive and/or overweight individuals.[9] The major concentration, as we have illustrated, should be on active travel as a healthy component of people’s everyday lives.
And above all, we urge the most explicit commitment to address the environment. If government at all levels does not establish planning, transport, regeneration and economic policies which put active living, and specifically walking and cycling, centre stage, then obesity can be expected to continue its advance. This means significant revision will be required of investment priorities, especially in transport. However, at least on the transport side, it does not necessarily mean more investment – economic appraisal to date of walking and cycling investment shows it to be very much better value than traditional spending on motor transport.[10]
A role for Sustrans’ programmes
Sustrans has a thirty year history of effective practical programmes promoting walking and cycling, and a decade working with physical activity specialists. In England, we are working in ever-closer partnership with the health sector, and the National Health Service is increasingly turning to our programmes as health promotion commissioning. These include:
- Active School Travel – Bike It and Safe Routes to Schools
Bike It works intensively with schools to increase levels of cycling to school and establish a pro-cycling culture. A typical work programme includes assemblies and classroom work, assistance with school travel plans and healthy schools work, securing the installation of cycle storage and cycle training, after school cycle skills sessions, and a series of family-friendly school travel events and rides. In 2007 we surveyed 11,000 children, and found that although 47% of pupils would like to cycle to school, only 3% were doing so.
In four years of operation Bike It has rapidly expanded to 40 staff addressing almost 500 schools in England and Wales, and around 70,000 children benefited from Bike It during the 2008 - 9 academic year. A survey of 50 Bike It schools in Summer 2007 showed that everyday cycling had more than trebled from 3% to 10% of journeys, once a week (or more) cycling had increased from 10% to 27%, and 25% of pupils had started cycling for the first time. Bike It also raises the numbers receiving cycling training, number of secure cycle storage places, levels of bike ownership, and preference for cycling.
The Rural Safe Routes to Schools programme in Northern Ireland saw Sustrans working with 18 rural primary schools. Following a range of interventions such as walking buses, cycle training and physical interventions such as cycle tracks, new pedestrian crossings and cycle sheds, travel behaviour changed amongst the pupils and parents. Those pupils usually being driven to school dropped from 65% to 49% and those walking to school rose from 20% to 33% and cycling rose from 5% to 7%.
Commenting on the Rural Safe Routes to School project, Dr Michael McBride the Chef Medical officer for Northern Ireland says
“In Northern Ireland, currently around one in four girls and one in six boys in Primary One are overweight or obese. Many of these children are not as physically active as they should be, they do not have a healthy balanced diet and this can contribute to an unhealthy lifestyle. By increasing the amount of physical activity in children now we can work towards improving the health and well being of the child through their whole life course.
I therefore support the work of Sustrans in promoting walking and cycling to school as a means of increasing the opportunity for children to take part in physical activity and which in turn encourages parents, guardians and teachers to participate."
- TravelSmart
TravelSmart is the UK’s leading travel behaviour change programme. It works with households to offer tailor-made information and support, allowing people to walk, cycle and use public transport more often. This delivers measurable reductions in car use, by enabling people to switch just a few day-to-day trips to more sustainable and active forms of travel – when and where it suits them best. In the UK, a total of around 315,000 households have been targeted in 21 pilot and large-scale projects conducted since 2001. Our current programme includes programmes in Exeter, Watford and Lowestoft, each targeting 25,000 households over the next three years.
TravelSmart is evaluated using before and after surveys across the whole target population (including those choosing not to participate in the marketing intervention), and adjusted to take account of background changes in behaviour measured across a separate control area. Projects have achieved relative reductions in car driver trips of 6% to 14%, with increases of 5% to 45% in walking and 14% to 75% in cycling. Recent evaluations have shown increases in exposure to active travel of 7 to 28 minutes per week on average across the whole target population. Total annual savings in car kilometres of 427km to 1,699km per household also generate significant reductions in CO2 emissions from a sector that is under-performing in relation to national climate change targets.
- The National Cycle Network and other infrastructure interventions
The National Cycle Network has been developed, UK-wide, since 1995, by Sustrans in partnership with local authorities, community groups, business, the NHS and others. Following an initial “strategic routes" phase (1995-2000) the concentration has been on creating ever-denser local networks linked to the strategic routes – for example through the hugely popular Connect2 local projects. These focus on the urban and peri-urban settings where most people live and there is most potential for a shift to walking and cycling. In 2006 the Network won the World Health Organisation’s Combating Obesity Award for its role in enabling people to be physically active every day.
The National Cycle Network is the biggest single generator of walking and cycling journeys throughout the UK, and usage is intensively monitored. In 2007 there were 354 million trips on the Network, roughly 50:50 walking and cycling. Usage on existing routes continues to grow at about 5% per annum, and growth is also generated by expansion of the Network itself. In Northern Ireland 75% of all users confirmed the National Cycle Network has helped them increase the amount of physical activity and 40% said that the routes had helped them increase levels of physical activity by a large amount. The Network is becoming a catalyst for increasing cycling with 48% of cyclists saying they are cycling more than a year before and 43% of cyclists intending to cycle more in the year to come.[11] Our monitoring indicates that on a UK wide basis usage level represents a saving of 70 million trips by car per annum, reducing congestion and road danger, and saving an estimated 329,000 tonnes of CO2.
Joining up policy
We would stress that the implementation of the approach we recommend, and the roll-out of programmes such as ours, also offer collateral benefits in other policy areas: interventions promoting active travel help with delivery of government objectives in the fields of climate change emissions reduction, energy security, road safety and quality of life.
The last word
Visions are easier to come by than delivery, but we would like to give the last word to the Department of Health in England, and their colleagues in other government departments, for the following from the English cross governmental obesity strategy: we could learn a lot from them as we work towards an Obesity Strategy for Northern Ireland.
“Our vision [is of] Government, business, local communities and other organisations … creating urban and rural environments where walking and cycling [are] the norm"
Healthy Weight, Healthy Lives: a cross-government strategy for England
[1] Investing for Health, DHSSPS, 2002
[2] NISRA Health and Social Wellbeing Survey 2005-06
[3] CREST, 2005 Guidelines for the management of obesity in Secondary Care
[4] At least five a week; the Chief Medical Officer’s report on physical activity, Department of Health, 2004
[5] Department of Health, Social Services & Public Safety, 2006 Fit Future: Focus on Food, Activity and Young People
[6] Lawlor et al, Journal of Epidemiology and Community Health 2003;57:96–101
[7] Promoting physical activity and active living in urban environments, World Health Organisation, 2006
[8]National Institute for Health and Clinical Excellence. Promoting and creating built or natural environments that encourage and support physical activity. London. NICE 2007
[9]Active travel as physical activity promotion, Sustrans, 2004
[10]http://www.sustrans.org.uk/default.asp?sID=1164381904000
[11] The National Cycle Network in Northern Ireland Route Monitoring Report 2004, Sustrans/Irish Field Surveys
http://www.sustrans.org.uk/webfiles/Ireland/NI_Route_User_Monitoring_Report_2004.pdf
The College of
Occupational Therapists
The College of Occupational Therapists is the professional body for occupational therapists and represents over 28,000 occupational therapists, support workers and students from across the United Kingdom, 770 of whom are in Northern Ireland. Occupational therapists work in the NHS, Local Authority social care services, housing, schools, prisons, voluntary and independent sectors, and vocational and employment rehabilitation services.
Occupational therapists are regulated by the Health Professions Council, and work with people of all ages with a wide range of occupational problems resulting from physical, mental, social or developmental difficulties.
The philosophy of occupational therapy is founded on the concept that occupation is essential to human existence and good health and wellbeing. Occupation includes all the things that people do or participate in. For example, caring for themselves and others, working, learning, playing and interacting with others. Being deprived of or having limited access to occupation can affect physical and psychological health
The College of Occupational Therapists welcomes the opportunity to contribute to the inquiry being carried out by the Assembly Health Committee to examine the current strategic approach to tackling obesity and it’s impact on health and well-being.
Assess the scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change.
The College of Occupational Therapists recognises and supports the role occupational therapists can play in promoting the health and wellbeing of their service users. With worldwide concern about obesity and it’s impact the College believes occupational therapists have a significant role to play.
The Northern Ireland Health and Social Wellbeing survey 2005-06 found that overall, 59% of adults measured were either overweight (35%) or obese (24%). A similar proportion of men (25%) and women (23%) were obese. Obesity was most prominent amongst the middle aged.1 "On a global basis, physical inactivity, unhealthy eating and being overweight are important preventable causes of chronic diseases such as Type 2 diabetes." 2
Whilst the profession fully supports the objectives of the prevention of obesity and the promotion of lifestyle change, we would like to note there is an ongoing requirement for the care management of people with obesity as a long-term condition, which can also often accompany other morbidities. Occupational therapists act as care managers for people with a range of conditions. They are also well placed to work with overweight or obese people both in a preventative health promoting way e.g. healthy eating as well as “supporting people to cope with the symptoms or results of their condition, or in preventing further problems."3
The fact that obesity is a significant issue for many people with a mental health problem or a learning disability is one we would like to highlight. “People who use mental health services, in particular those with a diagnosis of schizophrenia or bipolar disorder, are at increased risk for a range of physical illnesses and conditions, including coronary heart disease, diabetes, infections, respiratory disease and greater levels of obesity." 4 One of the issues and concerns
for people with a learning disability mentioned in the Equal Lives report is – “there are significantly higher levels of obesity." 5
The conclusions of the research study “Obesity and metabolic syndrome in a psychiatric rehabilitation service." Tirupati S; Chua LE, were that, "The rates of obesity and metabolic syndrome in patients with chronic severe mental disorders on antipsychotic drug treatment were 2 to 3 times that in the general population. A majority of them were untreated. Detection, monitoring and appropriate treatment of obesity and metabolic disorders should be a component of an assertive care management program to reduce morbidity and mortality and improve rehabilitation outcomes." 6
Occupational therapists are known as one of the five key workers in mental health services and have much to offer this client group.
In her presentation “The Role of the Occupational Therapist in Tackling Obesity",7 occupational therapist, Helen Uttley gives an overview of the holistic way an occupational therapist can work with a learning-disabled client group.
The Disability Rights Commission in one of a series of 10 documents giving detailed recommendations on the priorities within the Disability Agenda, Tackling health Inequalities, Creating an alternative future, February 2007 highlights some of the issues for Britain, “To tackle obesity among people with learning disabilities and / or severe mental health problems nationally, for example, would have greater impact than to do so for the whole of Birmingham and Coventry combined. National programmes to tackle health inequalities would not ignore whole cities like Birmingham or Coventry – yet disabled people are often ignored in national health improvement programmes."8
Another group who we would like to draw attention to are wheelchair users. There are over 24,000 wheelchair users in Northern Ireland and the management of weight gain for this group is of concern to occupational therapists. It should also be noted that the management of weight gain forms one strand of the process, when assessing for the provision of a wheelchair.
The occupational therapist makes an important contribution to the long term management of obesity in terms of maintaining mobility, promoting independence in personal care activities and ensuring access to essential facilities in the home
Occupational Therapists in Northern Ireland are identifying an increasing need for specialised bariatric equipment i.e. toilet aids, commodes, chairs, perching stools, extra width showers, chairs and wheelchairs etc. There is also the need for hoists and pressure cushions that can accommodate the obese/morbidly obese.9
There are also considerations in regards to increased storage and manoeuvring space for the home, hospital or nursing home etc. The increased space standards required to manoeuvre and store this equipment can have a subsequent impact on the size of housing adaptations.
These trends are creating new health and safety considerations, increase the costs of equipment and adaptations and require additional staff time to research and source new products and invest in enhanced education, advice and training of carers. The impact on personal carers is also of concern due to the potential of increased risk of injury.
In addition equipment and adaptations may need to be reviewed due to a subsequent increase in weight, as over time a person may exceed safe weight limits for essential equipment such as stair lifts. This again has resource implications e.g. staff and equipment costs.
Examine the availability of weight management or other intervention services to tackle weight related ill health
A person who is overweight may feel socially isolated or excluded, their role as a parent, caregiver spouse, child etc may be impacted. Their occupational performance, functional ability and mobility may be affected. Obesity can impinge on the occupational roles of a person’s life such as self-care, productivity, work, education and leisure. Occupational therapists analyse strengths and look at barriers to recovery and assist people to build up their strengths, which in turn promotes social inclusion, encourages self-determination and builds confidence to enable recovery.
Whilst there is a lot of emphasis on the ‘global epidemic’ of obesity, it is also important to consider the needs of the obese person, ensuring they are treated with dignity and respect avoiding stigma and discrimination.
Occupational therapists would endorse the concept of inclusive environmental design, which would consider the needs of all users including those with obesity. It is important that the home environment is accessible to people who are overweight or obese, so that their problems are not further compounded by being housebound which can lead to further inactivity. It is also important that the general environment is accessible thus supporting community integration, self-esteem and the motivation to maintain or improve mobility.
Occupational therapists are often involved in the recommendation of supervised play areas for children with disabilities and would stress the importance of the need for activity and play for children and young people across all abilities as this is one of their ‘occupations’, which is important for their good health and wellbeing.
Jessica Heslop in her research aimed to explore the role of occupational therapy with people who have bariatric needs. She points out that evidence within the literature review she carried out “with regards to education does suggest that there can be a decrease in the stigma and discrimination towards people with bariatric needs by educating the staff about accepting obesity as an actual condition rather than as ‘gluttony’.10
She also questioned why there is not a National Service Framework for the treatment of obesity? “There are plenty of publications to advise the public and health professionals on how to suggest a healthier lifestyle, but not how to accommodate the people with bariatric needs when they require the services that are supposed to be available to them."10
Heslop introduced and explored the use of the ‘Lifestyle performance Model’ (Velde and Fidler 2002) 11 as a means of working with people with bariatric needs to improve their quality of life.10 Occupational therapy practice is based on client centred care and this model was “presented as a way of representing a more holistic view of a person’s needs and wishes, which also emphasised the huge influence an environment; including people as well as the physical environment, has on peoples’ abilities."
Heslop also said, “Within the literature review there was substantial evidence to show that interventions purely focussed on weight loss were predominantly unsuccessful." The evidence she writes “highlighted that interventions which provided meaningful activities, which could then incorporate exercise more sensitively, were more successful."10
Her main conclusion included an explanation into how the core skills of occupational therapists can facilitate education for the multidisciplinary team and the person. The role of occupation was explored as a way of facilitating an improved lifestyle and therefore an increase in a person’s quality of life.
Consider what further action is required, taking account as appropriate, of the potential to learn from experience elsewhere.
The Lifestyle Redesign Programme®12 developed for older people by occupational therapist Florence Clark and colleagues at the University of Southern California in the mid 1990’s was part of the evidence base for the public health intervention guidance developed by the National Institute for Health and Clinical Excellence (NICE) 13
The feasibility of translating this programme into a UK context was explored by Gail Mountain and Claire Craig at Sheffeild Hallam University from 2004-2006 and led to the development of the programme Lifestyle Matters ( Craig and Mountain 2007)14 The College of Occupational Therapists guidance, Health Promotion in Occupational Therapy suggests.. “There are further questions regarding the benefits of this form of approach for other user groups which warrant exploration; for example the US group have applied the Lifestyle Redesign concept to people with pressure sores, to people with problems with weight control and to stressed executives."3
Occupational therapists are working on developing evidence based tools to calculate spatial requirements of people with obesity and associated mobility equipment. The profession is currently evaluating a software package called Idapt - an interactive design and planning tool for occupational therapists in this regard.
We endorse the six priorities for action identified in Fit Futures15 however would like to stress the need for developing joined-up healthy public policy. Clear interdepartmental and interagency arrangements for communication, collaboration and reporting must be established, to ensure that there is an efficient and well co-ordinated approach. Health promotion should be incorporated within care provision whenever possible and integrated throughout all areas of development of policy. The joined up approach needs to be at the departmental level at the development of policy and strategy so that the delivery is cohesive and co coordinated across statutory community and voluntary bodies. There need to be systems, which collaborate and provide a comprehensive approach and “opportunities for health promotion need to be identified when considering care pathways, service developments or the evaluation and re-organisation of current services."3
More statistical data defining the extent of the issue of obesity in Northern Ireland is needed and how specific groups are being targeted in terms of addressing their needs such as for example, people with mental health problems, learning or physical disabilities or those with physical or sensory impairments.
The College of Occupational Therapists supports a bold whole systems approach as indicated as critical in Foresight - Tackling Obesities: Future Choices- Summary of Key Messages “- from production and promotion of healthy diets to redesigning the built environment to promote walking, together with wider cultural changes to shift societal values around food and activity."15 We feel it is important that cross-departmental work looks at common issues and how they can be addressed in a coordinated cohesive way. Multidisciplinary working is also extremely important to ensure that effective working is taking place For example an occupational therapist and dietician could work with someone with mental health problems who is overweight or obese. They both could complement each other’s roles in terms of meeting the needs of the client.
Whilst interventions for those with obesity will have to be reactive and treatment orientated the move towards health promotion intervention and activity that is preventative and proactive is important.
It will be important to work with families and communities to make healthy lifestyle choices to ensure child diet and activity patterns developed from an early age will be beneficial to health and so can be continued and replicated into adulthood.
It should be ensured that all groups in society in Northern Ireland should be included in the development of programmes targeting their particular needs in regard to obesity in Northern Ireland in an inclusive and comprehensive way.
References:
1 Northern Ireland Statistics and Research Agency (NISRA) (2006) Northern Ireland Health and Social Well-being Survey 2005-06, Belfast, Central Survey Unit,
2 Report by the Comptroller and Auditor General (2009) Obesity and Type 2 Diabetes in Northern Ireland: Belfast, Northern Ireland Audit Office
3 College of Occupational Therapists (COT) (2008) Health Promotion in occupational therapy: guidance, London, COT.
4 Department of Health Choosing Health (August 2006) Supporting the physical needs of people with severe mental illness - commissioning framework, London, Department of Health.
5 Review of Mental Health and Learning Disability (Northern Ireland) (2005) Equal Lives: Review of Policy and Services for People with a Learning Disability in Northern Ireland. Belfast Review of Mental Health and Learning Disability (Northern Ireland)
6 Tirupati S; and Le, Chua (2007) Obesity and metabolic syndrome in a psychiatric rehabilitation service, Australian & New Zealand Journal of Psychiatry Jul; 41(7): pp606-10.
7 Stafford, South Staffordshire and Shropshire Health Care NHS Foundation Trust Presentation -The Role of the Occupational Therapist in Tackling Obesity
http://www.southstaffshealthcare.nhs.uk/services/ahp_ot/projects/obesity.pdf
8 The Disability Rights Commission, “Tackling health Inequalities, Creating an alternative future, February 2007 (One of a series of 10 documents giving detailed recommendations on the priorities within the Disability Agenda)
9 Disabled Living Foundation (2006) Choosing Equipment for the Heavier Person, Disabled Living Foundation
Available at: www.dlf.org.uk/factsheets <http://www.dlf.org.uk/factsheets/pdf/Choosing_Equipment_for_the_Heavier_Person.pdf>
10 Heslop, Jessica (2008): A critical review into the role of occupational therapy in promoting the quality of life for people with bariatric needs. Unpublished thesis, York St John University. 2008, York
11 Velde, B., and Fidler, G. (2002). Lifestyle performance: A model for engaging the power of occupation, NJ, Thorofare, SLACK, Inc.
12 Clark F, Azen SP, Zemke R Jackson J, Carlson M, Mandel D, Hay J, Josephson K, Cherry B, Hessel C, Palmer J, Lipson L (1997) Occupational therapy for independent-living older adults: a randomised controlled trial. Journal of American Medical Association, 278(16), pp.1321-1326.
13 National Institute for Health and Clinical Excellence (NICE) (October 2008) Mental Wellbeing and Older People. Guidance for Occupational therapy and physical activity interventions to promote the mental wellbeing of older people in primary care and residential care. <http://www.nice.org.uk/PH016#documents>)
14 Craig C, Mountain G (2007) Lifestyle matters: maintaining the health and wellbeing of older people. Bicester, Speechmark Publishers.
15 Department of Health Social Services and Public Safety (2006) Northern Ireland Investing for Health: Fit Futures: Focus on food, activity and young people, Report to the Ministerial Group on Public Health, Belfast: Department of Health Social Services and Public Safety Northern Ireland http://www.dhsspsni.gov.uk/ifh-fitfutures.pdf
16 (2007) Foresight: Tacking Obesities: Future Choices - Summary of Key Messages. Government Office for Science. London. Department for Innovation Universities and Skills
Ballymena Borough Council
Introduction
Ballymena Borough Council welcomes the opportunity afforded to present our concerns and opinions to the Committee.
The rapid increase in the number of obese people in the UK is a major challenge, it is estimated that if this trend is unchecked over half of the population could be obese by 2050. The economic implications of this are substantial. The NHS costs attributable to overweight and obesity are projected to double to £10 billion per year by 2050 and the wider costs to society and business are estimated to reach £49.9 billion per year (at today’s prices).
One school of thought would suggest that obesity is due entirely to personal lifestyle and diet choices. Another however is that people today generally do not have less willpower nor do they eat more than previous generations and that it is important to look beyond the obvious and to accept that society has radically altered over the last 5 decades, with major changes in work patterns, transport, food production and sales. It is thought that these changes have exposed a common underlying biological tendency to both put on weight and retain it. Being overweight or obese increases the risk of a wide range of chronic diseases including diabetes (Type 2), cancer, cardio vascular disease etc. It can also impact upon public health through its impairment of the individual’s well-being, quality of life and ability to earn.
Local Context
Body Mass Index (BMI) is routinely used to measure for obesity. BMI equals weight (Kg) divided by height (m2), obesity is considered to be a BMI of 30 and upward.
In Northern Ireland research has shown that 60% of adults have a weight problem and as many as 1 in 5 are obese. Figures from 2006/7 show that approximately 22% of Northern Ireland’s primary school children are classed as overweight and obese.
The Health and Well-being Survey 2005/6 (Public Health Information and Research Branch) shows that in the NHSSB area 37% of adults are overweight and 26% are obese, levels, which are 2% above the Northern Ireland average. This research also shows that 23.1% of children in the NHSSB area are classed as overweight & obese. Northern Investing for Health Partnership, Health & Well-being Statistics show that in 2006/7 the average prevalence for obese patients aged 16 + in Northern Ireland was 79.9 per thousand, and in the NHSSB area was 91.0 per thousand. Closer examination of the survey results shows that 8 GP Practices in the Ballymena area exceed the NHSSB average and a further 5 exceed the NI average (results range from 117.8 to 80.7 per thousand patients) i.e. 13 of the top 57 GP practices fall within the borough of Ballymena.
These statistics highlight the worrying level of obesity throughout Northern Ireland and particularly in our own council area. This is an issue, which Ballymena Borough Council would welcome the opportunity to become more practically involved in.
Current Situation
Obesity is an area of concern which affects the entire age range of the population and is therefore unlikely to be satisfactorily addressed through one catch all strategy, and will necessitate differing approaches to tackle the issue. However there appears to be no cohesive strategy available at present for guidance for those with an interest in this issue.
In August 2004 a cross-departmental taskforce was established by the Ministerial Group on Public Health to examine the options in relation to preventing the rise of overweight and obesity and to make recommendations to MGPH on priorities for action. This led to the drafting of the strategy Fit Futures: Focus on Food, Activity and Young People, which included:
- Establishing a healthy schools policy for toddlers and children
- Facilitating an annual business and nutrition forum
- Establishing a Fit Futures Programme Board led by DHSSPS, Department of Education and Department of Culture Arts and Leisure
- Web-based resources on nutrition and physical activity
- Trebling the number of pupils participating in safe routes to school.
This strategy remains in draft format although many of the key priorities contained within it are being addressed by various organisations through their own agendas e.g. the Food Standards Agency, Department of Regional Development and the Northern Investing for Health Partnership, which has introduced a Fit Futures Action Plan.
This lack of strategic direction has led to a very “piecemeal" approach to the issue of obesity and although attempts have been made to ensure a multi agency approach there is a tendency for partners to withdraw into their “professional silos" running stand alone schemes. These schemes due to their fragmented nature appear to have little measurable impact as the obesity levels continue to rise.
Ballymena Borough Council therefore welcomes the creation of the Public Health Agency and hopes that this will provide a focus; cross-departmental leadership and influence for future work in the health improvement sector.
The Way Forward
The UK Government’s Foresight Programme was asked to examine the issue of increasing obesity and the subsequent report states;
It will take several decades to reverse the factors that are driving current obesity trends. Currently no country in the world has a comprehensive long-term strategy to deal with the challenges posed by obesity. There is an urgent need for action to halt the rapid increase and to develop a sustainable response."
It is the opinion of Ballymena Borough Council that a comprehensive cross-cutting long-term strategy is required that brings together all the major stakeholders e.g. primary health care providers, public health professionals, food industry representatives, local authorities, communities etc.
As previously stated it appears that currently the majority of initiatives take the form of intervention rather than prevention. Ballymena Borough Council feels that there is an important distinction between prevention and the intervention/treatment available from Primary Health Care providers. Once gained, excess weight is difficult to lose. It is therefore the opinion of the Council that the emphasis upon prevention is crucial although it is acknowledged that there are already significant numbers of overweight/obese people who require treatment and that these numbers will continue to rise regardless of short-term measures.
When discussing prevention and intervention measures it is vital to also consider the impact of the forthcoming budget cuts being imposed upon the Primary Care Trusts and the knock on effect that these cuts will have on the provision of frontline services. Ballymena Borough Council is of the opinion that these cuts will significantly affect the availability of many such services hence the need for effective prevention measures to decrease future demand upon reduced services becomes even more vital.
Ballymena Borough Council feels that as the hub of local communities district councils are best placed and have the skills necessary to deliver prevention based initiatives. It is important to remember that obesity can not be considered as an isolated issue, it is inextricably linked with other areas such as food and nutrition, food poverty, physical activity, alcohol consumption and even community safety as the perception of danger is often given as a reason for not taking exercise in local parks etc.
Interventions based on improved nutrition and increased physical activity can be effective for some individuals, but tackling the obesity problem for the total population will require interventions that target the environment as well, for example food policy and marketing and the transport infrastructure. Hence it is the opinion of Ballymena Borough Council that the ideal forum for addressing such wide-ranging topics would be through the process of community planning and the associated power of well-being, roles to be assigned to the new Councils through the current RPA.
The National Institute for Health and Clinical Excellence (NICE) guidelines on obesity acknowledge the enhanced role for local authorities, schools and other public agencies, and private and voluntary sector providers in developing opportunities for people to secure better health. Although there is no simple solution the most effective strategies for prevention and management of obesity share similar approaches and cannot be viewed in isolation from the environment in which people live. This further supports the Council contention that prevention measures could best be tackled on a local level through the auspices of community planning
The ongoing RPA provides an excellent opportunity for Councils to take a lead role in the development and implementation of multi agency community based initiatives in many spheres including this and Ballymena Borough Council would willingly seize the opportunity.
Ajinomoto
Ajinomoto is a global leader in the manufacture and marketing of amino acids, nucleotides, and amino acid-based ingredients including the low-calorie sweetener aspartame.
Ajinomoto welcomes the opportunity to contribute to the Health, Social Services and Public Safety Committee’s inquiry into obesity. Please find below our comments, particularly in regard to the first question of the scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change. Our suggestion is for a simple, cheap and effective approach that can make a real difference in the number of calories which people consume. We hope that you will find these comments helpful.
Background
- According to the Foresight report Tackling Obesity: Future Choices,[1] on current trends, levels of obesity and overweight in the UK will rise to 60% in men, 50% in women, and 25% in children by 2050. According to the Northern Ireland Health Promotion Agency, already in Northern Ireland 59% of adults and 26% of children are overweight or obese.[2]
- As is widely recognised, obesity is a risk factor associated with a number of serious health conditions, including cardiovascular disease, diabetes and cancer.
- Children are especially at risk of diet-related ill health and obesity-related illnesses.
- The challenge posed by obesity to the health services in Northern Ireland, as in the rest of the UK, is enormous, not least in financial terms. The Health Promotion Agency estimated that each year it causes 450 deaths and costs the Northern Irish economy about £500 million.
The contribution of sugar to levels of obesity
While there are a number of causes of obesity, it was recognised in the Cabinet Office Strategy Unit’s Interim Paper on Food[3] that:
- The diet of the average British adult contains too much added sugar; and
- The largest single source of added sugar in the average child’s diet, especially amongst children from a lower income background, is soft drinks.
In order to improve people’s health, especially amongst children, and tackle the rising levels of obesity of the whole of the UK population, the sugar content of the average consumer’s diet should be reduced.
To help achieve this, the Northern Ireland Executive should educate consumers about the benefits and calorie savings that can be achieved by choosing low- and no-sugar beverages and encourage people to opt for low-calorie or sugar-free options, whenever available, including for their children.
This would be a simple, clear message that is easy to understand and would support the Executive in achieving its objectives in terms of reversing the growing number of obese and overweight people in the UK.
Scientific evidence supporting the role of low-calorie sweeteners
Considerable evidence exists on the merits of using low-calorie sweeteners in reducing overall energy intake, including:
- De la Hunty, S. Gibson and M. Ashwell, “A review of the effectiveness of aspartame in helping with weight control", British Nutrition Foundation Nutrition Bulletin (2006)
- F Bellisle and A Drewnowski, “Review: Intense sweeteners, energy intake and the control of body weight", European Journal of Clinical Nutrition (2007)
A number of studies and reviews have all concluded that there are no safety issues with regards to the use of aspartame, including:
- The panel on food additives, flavourings, processing aids and materials in contact with food (AFC) of the European Food Safety Authority (EFSA) evaluation on the long-term study on the carcinogenicity of aspartame conducted by the European Ramazzini Foundation in Bologna, Italy, May 2006
- The Panel concluded on the basis of all the evidence currently available, that there is no need to further review the safety of aspartame nor to revise the previously established Acceptable Daily Intake (ADI) for aspartame (40 mg/kg body weight)
- Magnuson, B. A., Burdock, G. A., Doull, J., Kroes, R. M., Marsh, G. M., Pariza, M.W., Spencer, P.S., Waddell, W. J., Walker R., Williams, G.M., “Aspartame: A safety evaluation based on current use levels, regulations, and toxicological and epidemiological studies", Critical Reviews in Toxicology, 2007
- Toxicology research concluding that the levels of aspartame consumed by humans are safe
Children’s hydration
Adequate hydration is an important factor for everyone but, in particular, to maintain high levels of alertness and cognition amongst schoolchildren. However, in order to ensure regular consumption of liquids and maintain healthy levels of hydration, choice and variety of drinks are known to be important considerations for all consumers, especially for the young.
Currently the only drinks allowed to be provided in schools in Northern Ireland are plain water, milk, pure fruit juices, yoghurt or milk drinks (with less than 5% added sugar), drinks made from combinations of the above (eg smoothies), low-calorie hot chocolate, tea and coffee.
Some of the possible hydration options pose their own difficulties. While pure water is an obvious healthy low-calorie option, it is, however, unreasonable to expect children to make this their drink of choice throughout the day. Similarly, although milk and fruit juice are good, healthy options, it should be remembered that these drinks may contain as many calories as a full sugar soft drink and therefore should only be consumed in moderation. Indeed, research has also linked excessive consumption of natural fruit juice to obesity (Dennison et al., 1997; Malik et al., 2006). This has also been acknowledged by the Scottish Government in their report Growing up in Scotland: Sweep 3 Food and Activity Report.
A table showing the calorific values of several popular soft drinks can be found on page 4.
In order to provide an achievable selection of beverages that will provide adequate hydration without excess calorie consumption, we believe that low-calorie sweetened beverages should be considered as contributing to a healthy diet.
Consumer Preferences
Some organisations, such as the School Food Trust, have argued low-calorie sweeteners are counter-productive because they encourage a preference for a sweet taste. However, we would like to point out that that there is no evidence that drinking products containing low-calorie sweeteners develops or maintains a preference for sweet tasting drinks or foods, a fact that was acknowledged by Paul Goggins MP, Parliamentary-Under Secretary of State (now Minister of State) for Northern Ireland in a letter to Committee Chair Iris Robinson, in 2006.
It is also wrong to argue that consumers would prefer not to consume artificial sweeteners such as aspartame, as the year-on-year growth in sales of sugar-free and reduced-sugar drinks demonstrates that consumers increasingly prefer low-calorie options. This is a positive example of consumers making healthy choices for themselves, and something which should be encouraged.
Research by Ajinomoto shows that consumers do not have an issue with artificial sweeteners such as aspartame; consumers are much more concerned about ingredients that make them fat and unhealthy, than about low-calorie sweeteners.
Encouraging consumers to opt for a healthier choice is simpler and more effective than engineering a nation-wide change in consumer tastes and limiting consumer choice.
Conclusion
Low-calorie sweeteners, such as aspartame, can play an important and helpful role in reducing the overall calorific content of people’s diets and in reducing the overall obesity levels in the UK, thus improving public health and reducing demands on public health services.
The single most effective move that Government could take to improve public health, at no extra cost and with no need for regulation, is to issue clear and consistent messages that consumers who want to choose a sweetened beverage, should consider choosing a low-calorie option.
Annex 1: Caloric Values of popular drinks
| Coca-Cola (330ml can) | 139 |
| Coca-Cola Zero (330ml can) | 1 |
| Diet Coke (330ml can) | 1 |
| Ribena Blackcurrant (330ml bottle) | 142 |
| Really Light Ribena (330ml bottle) | 13 |
| Ribena 100% Pure Juices Blackcurrant Blend (250ml bottle) | 133 |
| Red Bull (250ml can) | 113 |
| Red Bull Sugar-Free (250ml can) | 8 |
Annex 2: Typical Caloric Values (250ml servings)
| Milk | Semi-skimmed | 122 |
| Skimmed | 86 | |
| Reduced lactose | 113 | |
| Semi-skimmed goat’s | 113 | |
| Fruit juice | Apple | 116 |
| Cranberry | 139 | |
| Orange | 108 | |
| Tomato | 51 | |
| Vegetable juice | Mixed vegetable | 40 |
| Carrot | 58 | |
| Soya, rice & oat drinks | Soya drink | 115 |
| Oat drink | 88 | |
| Fermented milk | Kefir | 150 |
| Flavoured milk | Banana | 175 |
| Strawberry | 185 | |
| Tea & coffee | Tea with semi-skimmed milk | 18 |
| Coffee with semi-skimmed milk | 24 | |
| Added teaspoon of sugar | 16 | |
| Hot Chocolate | Maximum permissible | 50 |
[1] http://www.foresight.gov.uk/OurWork/ActiveProjects/Obesity/Obesity.asp
[2] http://www.healthpromotionagency.org.uk/work/Publicrelations/PressReleases/all_island_obesity_conference_2008.html
[3] http://www.cabinetoffice.gov.uk/media/cabinetoffice/strategy/assets/food/food_analysis.pdf
Cambridge Health and Weight Plan
Background
According to the Northern Ireland Health Promotion Agency, currently in Northern Ireland 59% of adults and 26% of children are overweight or obese.[1] These adults have an increased risk of a number of serious health conditions, including cancer, diabetes cardiovascular disease and osteoarthritis, as well as an overall shorter life expectancy.
Obesity poses an enormous challenge to Northern Ireland, not only in health terms but also in financial terms, due to the costs of treating obesity and the fact that those with serious medical conditions are less able to work and be economically active. The Health Promotion Agency has estimated that each year in Northern Ireland, obesity causes 450 deaths and costs the economy about £500 million.
About Cambridge Health and Weight Plan
Cambridge Health and Weight Plan (CHWP) was established in 1984, and offers a variety of weight management options, including a Very Low Calorie Diet (VLCD) programme and a Low Calorie Diet (LCD) programme, for those who are overweight and clinically obese. Flexible programme options are offered between 415 kcal/day and 1500 kcal/day, all using a nutritionally balanced formula food as the foundation.
Cambridge Health and Weight plan welcomes the opportunity to contribute to the Health, Social Services and Public Safety Committee’s inquiry into obesity. Please find our comments below.
The Current Approach in Northern Ireland
Most recent efforts to tackle obesity in Northern Ireland have focused on the area of prevention. There has also been a focus on children, in an attempt to stop the next generation becoming obese, rather than concentrating on adults that are currently obese. Fit Futures, the Northern Irish strategy to tackle obesity in children, identified general priorities such as developing joined up healthy public policy, providing real choice in terms of food, and supporting healthy early years, schools and communities.
However, for some sectors of the population, such general efforts to encourage people to improve their diet and exercise levels have not proved effective, and a more interventionist approach is required. This is particularly the case for severely obese adults, for whom reaching a healthy weight can seem a daunting task.
What are VLCDs and what benefits do they offer?
We believe that commercial weight management organisations, such as CHWP, can play an important role in supporting health services in tackling the growing obesity problem. Several primary and secondary care environments in England already use the VLCD programmes, which are also available within the wider community as a referral option.
VLCDs are formula food diet programmes which provide between 400-800 kcals per day and come in the form of shakes, soups and bars, designed to replace more traditional meals to give effective weight loss at predictable rate. These products contain carefully formulated amounts of energy, protein, carbohydrate, fat, fibre and all essential micro-nutrients. VLCD products are nutritionally balanced, containing at least 100% RDA per day of listed vitamins and minerals, to ensure that those on a VLCD get the nutrients they need.
VLCDs are aimed primarily at those with severe weight problems (typically a Body Mass Index in excess of 30 kg/m2) and provide an opportunity to help them make changes in their diet which allow them to adopt healthier lifestyles in the long-term. For people who are severely overweight, the fact that VLCDs offer faster weight loss then most alternative diets can also motivate people during the early stages of the diet.
Re-education towards longer term healthy eating habits, behavioural change and feedback to health professionals as appropriate to each individual are common to all programmes, helping people to sustain a healthy weight in the long-term.
During their time on the diet, participants are supported by a specially trained counsellor, who advises them on which programme is most appropriate for them and how to use it properly. These counsellors provide both individual and group support and motivation during the weight loss process, with the aim of changing long-term behavior towards eating in order to ensure that the weight loss is sustainable. This support carries on once the target weight has been reached.
Before commencing a Cambridge programme, participants must notify their GP, and the counsellors also monitor the amount of weight lost and general health of the clients during their time on the diet.
It should be noted that VLCDs are acknowledged as an option in the NICE guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children.[2] In fact, NICE guidelines on prevention and management of obesity suggest that there is evidence that a multi-component commercial group programmes may be more effective than self-help. This fact was also acknowledged by Lord Warner, then Minister of State for the UK Department of Health, in October 2006.[3]
VLCDs are also a more cost effective treatment for obesity than other treatments which are available. For example, a twelve week ‘package of care’ providing a Cambridge VLCD programme including all product and counsellor services is currently priced at £450. Twelve weeks of drug treatment would cost £638 (based on one initial 17.2 minute GP consultation (£52)[4] and one 11.7 minute follow-up with the GP at 3 months (£36), plus 5 fortnightly 30 minute consultations with a practice nurse (5 x £14 = £70) plus an average drug treatment cost, sibutramine or orlistat of £40 per week (12 x £40 = £480). Weight loss after 12 weeks of VLCD (12kg)[5] would be expected to be greater than weight loss after 12 weeks of drug treatment (5-6kg)[6], thus expressed as cost per kg of weight loss a VLCD programme costs less than half the cost (£450/12 = £37.50/kg) of drug treatment (£638/6 = £106/kg), and need not draw on NHS staff time resources.
It should also be noted that when obesity is treated by surgery or drugs, NICE still recommends that this treatment is followed up by cognitive behavior therapy in order to ensure the long-term sustainability of the weight loss, which is an additional cost on top of the primary treatment. With VLCD programmes such as Cambridge, this is an integral part of the treatment, providing further cost effectiveness.
Suggestions for future action
CHWP believes that it would be beneficial if the Northern Irish population had access to more information on weight management programmes in general. In addition, health professionals, such as GPs and pharmacists, should also have more comprehensive information about all the various weight management programmes available. This would ensure that people can make informed choices when choosing the most appropriate weight loss option for them.
To this end, the Northern Ireland Health, Social Services and Public Safety Department, should consider developing:
- General guidance documents for health professionals, which provides accurate and comprehensive information on the different options available for weight management, including VLCDs.
- An overall comprehensive obesity strategy to tackle the rise in obesity in Northern Irish adults, including detailed information on care pathways and treatment options. For such a strategy to be effective, it should not just focus on prevention, but also offer specific suggestions for treatment options for those adults already experiencing weight problems.
- More information for those trying to lose weight, including an NHS Choices style website for Northern Ireland, where people with weight issues can find impartial and accurate factual information about the different options available to them, as well information as how they can access particular weight management services in their local area.
Conclusion
The commercial weight management sector can play a useful role in helping to tackle the obesity crisis in Northern Ireland. However, for this to work successfully, the health services in Northern Ireland need to be aware of the variety of options available to them to help overweight and obese people achieve a healthy weight, and ensure that both medical practitioners and the general public are also aware of these options. The focus needs to be on specific interventions that can help people achieve a healthy weight.
[1] http://www.healthpromotionagency.org.uk/work/Publicrelations/PressReleases/all_island_obesity_conference_2008.html
[2] http://www.nice.org.uk/nicemedia/pdf/CG43NICEGuideline.pdf
[3] http://www.publications.parliament.uk/pa/ld199697/ldhansrd/pdvn/lds06/text/61009w0013.htm#0610054001114
[4] Unit Costs of Health and Social Care 2008 compiled by Lesley Curtis, Personal and Social Services Research Unit, University of Kent
[5] Weight-loss outcomes: a systematic review and a meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up Franz MJ etal JADA 2007; 107: 1755-1767
[6] Ibid.
Western Education & Library Board
The Board has a track record of partnership working across a range of health initiatives involving representatives from key divisions in our service such as, Transport, Curriculum Advisory and Support Services, Youth, School Meals and Children and Young People’s Services. Our Property Services and Procurement Services also work closely with schools to ensure quality provision for sports facilities, catering/dining halls and outdoor play areas.
Many of our schools now have a cashless system for school meals which supports healthy choices for children. The system also provides for sound data collection and analysis of eating patterns, nutritional intake and seasonal changes in food choices. In addition it ensures those on free school meals are not stigmatised since all pupils have the same swipe card. Those on free school meals have the allowance credited to their account automatically.
The Youth Service ensures health promotion is to the forefront of their curriculum in youth settings encourage young people to engage in sporting events, games, outdoor pursuits and summer schemes. The WELB makes good use of its centre at Gortatoile in County Fermanagh where young people can access one day or residential facilities. A dedicated team there supports team building exercises, abseiling, canoeing and other outdoor activities.
For the past 14 years the Western Education & Library Board (WELB), Western Health & Social Services Board (WHSSB) and the Western Environmental Health Group (WEHG), of the five local councils, have taken the lead in providing a Health Promoting School Award to all schools in our area who choose to participate. Each year 50 -70 schools take part in the scheme which provides support in evaluating how they are addressing health promotion in their school and identifying what further steps they need to take. Schools then set out their targets and representatives from the partnership visit the schools to carry out an assessment. Schools are then categorised into levels of bronze, silver or gold and receive awards at a ceremony towards the end of the school year. An assessment report is issued to school which forms part of their base-lining data for the following year.
The scheme is currently being revamped to bring it more into line with the Northern Ireland Curriculum and the Health Promotion Self Evaluation Toolkit designed by the five Education & Library Boards (ELBs), and the Health Promotion Agency (HPA). The revised version of the award scheme will go out to schools in September 2009.
The Board has been able to provide a number of physical activity programmes on a cross border basis through SEUPB funding. These border counties initiatives have afforded young people a vast range of opportunities they might not have otherwise been able to access. We are conscious of the rural setting in which many of our young people reside and the difficulties they experience due to lack of transport after school or at weekends. Every effort has been made to engage with other providers such as sporting clubs, local councils as well as voluntary and community groups, so Board officers are aware of local provision and can encourage schools to add their support.
Whilst the attached report highlights some of the current provision the WELB has in place, it must be recognised that we encourage a holistic approach within schools/youth settings to the promotion of a healthy lifestyle. Specific initiatives have a place but schools and clubs need to audit and self evaluate how they support healthy lifestyles and what steps they can take in conjunction with external providers to enhance current provision. This will require careful action planning with time bound targets and monitoring and evaluation processes built in from the start. It will also require schools to analyse available quantitative and qualitative data in order to identify those groups of young people needing particular support or interventions in addition to any standard provision. Such a focus requires close working relationships with families and the wider community including Councils and Neighbourhood Renewal Groups, since the root causes of obesity cannot be tackled by the school/club alone.
| Physical Education and Obesity | Western Education & Library Board | ||
| Description | Funding | Age group (beneficiaries) | Details |
| Fundamental Movement skills | 5 – 10 years | This course, run across Northern Ireland, enables teachers to identify and improve children’s movement patterns. This includes 22 basic skills like running, jumping, throwing and catching. Being proficient in these skills, children can participate confidently in play, dance, games etc thus contributing to enjoyment and life long participation in physical activity. | |
| Gymnastics | 4 – 11 years | This course provides opportunities for teachers to explore how gymnastics can develop children’s creative abilities. Provide teachers with confidence to allow pupils to create, practice and perform movements they have created themselves. | |
| Dance | 4 – 11 years | This course provides opportunities for teachers to explore how dance can provide learning experiences which will help young people enjoy rhythm and movement, work with others, make decisions and problem solve when developing their ideas | |
| First Aid/Dental Trauma | 4 – 18 years | This is an emergency first aid sports course for primary and Post Primary teachers. | |
| Youth Sport | WELB , VEC & Peace 11 funding | 4- 18 years | Creating after school sporting opportunities for all children. This project gives young people different sporting experiences other than there traditional school sports. Quality coaches hold six week programmes in schools giving children experience in many different sports. |
| Summer Schools | WELB | 4 - 18 years | During the summer holidays schools hold programmes for children in the school setting many of which are health promoting and sporting programmes. |
| Youth Service | WELB | 8 - 18 years | Youth club provision includes many health and recreational physical activities. |
| Outdoor Pursuits Centres | WELB | 8 - 18 years | These residential centres give children a chance to experience challenging outdoor activities as well as team building opportunities that builds character for life |
| Training for Pupils | WELB & Youth Sport Trust |
Training for groups of pupils in skills development | |
| Top Link | 15 - 18 years | This is a leadership programme aimed at senior pupils in Post Primary schools. These pupils develop and utilise leadership skills by organising and running a sport or dance festival for local primary schools. It provides an opportunity for personal development through a national programme with recognition and support for existing work and further opportunities in this area. | |
| PE in Schools | Physical Activity is taught in every school and Board officers support the continuous professional development of teachers. | ||
| Extended Schools Programme | DENI | 4 - 18 years | Some 140 school in the WELB are classified as Extended Schools by the Department of Education. Most of their action plans include elements of physical activity and healthy eating such as breakfast clubs, sporting events, after school games and activities. Parents are also encouraged to partake in physical activity programmes. Cooking programmes are provided for parents in many schools. Numerous summer schools and weekend activities are also run. Playground markings have been updated and training for supervisors has enhanced physical activity. |
| Heart Start First Aid | British Heart Foundation & WELB | 4 – 18 years | Groups of teachers are trained in First Aid on a rolling programme each term in conjunction with the British Heart Foundation |
| Home Economics in the Curriculum | WELB/DENI/ CCEA/UU | 11 -18 years | Home Economics is now a core subject in the N Ireland Curriculum. The WELB officer supports all post primary schools in meeting this requirement. Facilities in ‘all-boys’ schools are now being provided to ensure they can implement the programme and teachers are receiving additional training in conjunction with the University of Ulster. |
| Partnerships | HPA/WHSSB | 4 – 18 years | The WELB works in partnership with many organisations such as the Western Health Board/ the Trust and the Health Promotion Agency in drawing up support materials and piloting approaches to promoting Heath. e.g. The Self Evaluation Tool for a Healthy School. |
| Personal Development in the Curriculum | WELB/DENI/ CCEA | 4 – 18 years | Personal Development is a core element of the N Ireland Curriculum under Learning for Life and Work. This are focuses on personal health and promoting healthy life styles. WELB officers support the professional development of teachers in this field. |
Department of Agriculture
and Rural Development
The Forest Service is currently preparing a strategy to develop the recreational and social use of its forests. The draft strategy, which has been subject to a 12 week public consultation, recognises a number of opportunities relating to health and well-being that are relevant to the obesity inquiry. These include:
- Promotion of forests for health and wellbeing;
- Promotion of forests for organised sporting events;
- Partnerships with health and outdoor education providers;
- Facilitation of Woodland Schools in partnership with education bodies; and
- Environmental learning opportunities on forest trails.
An example of the type of initiative that might be possible is the Highway to Health trail in Belvoir park Forest (originally developed in conjunction with the then Knockbracken Health Trust).
There is considerable evidence from other forestry organisations in Britain and in the south, of the health benefits provided by outdoor activities. For example, Forestry Commission Scotland published in 2007, a strategy entitled Woods for Health, which focuses on making local woodland accessible to welcome and help people build healthy activity into their daily lives. The document highlights evidence that physical activity can be a preventative measure against obesity, heart disease, some types of cancer, stroke, and Type II diabetes, leading to better health and savings on treatment costs. A similar initiative would be possible here, if the necessary resource and commitment from health partners could be secured.
The draft Strategy indicates that Forest Service will seek ways to promote the contribution of forests to health, including partnership working and social marketing. It acknowledges that Forest Service is not resourced or skilled to identify and fully realise the potential health opportunities, but commits Forest Service to develop partnership arrangements with health organisations, such as the Health Promotion Agency. The aim is that through this process, opportunities can be identified and resourced. Resourcing any resulting initiatives will be vital.
As well as this, I firmly believe that promoting the consumption of natural farm products, including milk, could form part of a wider drive to encourage healthier diets. The nourishing, fresh food which our agri-food industry can provide can support such a drive and this, in turn, would also help secure the future sustainability of our local food producers.
PlayBoard
Northern Health and
Social Services Board
1. Assess the scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change:
The Northern Health & Social Services Board has in place an Obesity Prevention Sub Group facilitated by the NIFHP, and a Northern Partnership for Physical Activity facilitated by the Northern Trust both of which oversee the delivery of related strategies and priorities including Fit Futures, food and nutrition issues and physical activity.
Initiatives taken forward through the groups have included a wide variety of approaches and sectors. All initiatives have been evaluated. Full details are available on request. Some examples are:
- Family focused programmes to support the management of diet and lifestyle with obese children run in partnership with the Trust and local Councils;
- Volunteer Leader training and the development of walking groups;
- Support for community nutrition and activity programmes,
- Healthy eating programme for ethnic minorities through the local Further Education College;
- Awareness raising workshops and playground markings schemes for schools across NEELB.
- Community based physical activity programmes targeting young people in Health Action Zones and disadvantaged areas.
The NHSSB funds a Co-ordinator for Physical Activity and the NIfHP also funds four Trust based posts in support of obesity prevention; two breastfeeding posts and two prevention focussed dietetic posts (these two posts are due for review over the coming months).
The NHSSB and Northern Health and Social Care Trust are working together to put in place a team, based in the Trust, to co-ordinate and drive forward obesity prevention in the NHSCT/NIfHP area. This team will be in place within the next number of months.
In addition to the above nursing services, particularly health visiting and school nursing make an important contribution to this area including :
- Antenatal contact, information leaflets and advice on benefits of breast-feeding in
- Promotion of healthy start – giving children best possible nutritional start in life
- Promotion and support for breastfeeding
- Breast feeding support groups
- Weaning advice and support – baby weaning clubs
- Healthy start information
- Weighing and measurement of weight/height and appropriate advice
- Advice about infant/toddler feeding and healthy eating for families
- Family health needs assessment and support with health related problems/ diet/exercise
- Health promotion activities such as "Munch Bunch Programme"
- Working with education to promote healthy lifestyles educational sessions
- Puberty talks in year 7 with focus on healthy diet and physical activity
- Implementation of weight measurement programme in year 9
Work in this area in particular needs to be resourced and developed further with potential for profiling in schools/health appraisals/health promotional activities/cook it programmes etc.
The Regional review of the Child Health Promotion Programme currently being undertaken across the Province in line with National Programme, will give additional emphasis and strengthen the need to promote diet, physical activity and reduce obesity at every contact by Health Professional and in particular health visiting and school nursing.
2. Examine the availability of weight management or other intervention services to tackle related ill health:-
Children
Within the Northern Trust there is a weight management clinic in the Antrim area for children. There are issues relating to capacity, resourcing and equity of access within the Trust. This programme is supported by health visiting staff in follow up home visiting to offer advice and support and maintain motivation for those attending the programmes. This is however unfunded and will be reviewed as part of comprehensive spending reviews/ review of health visiting school nursing
There is significant lack of weight management programmes/support etc across the Trust for those children being picked up through the school weight measurement programme.
Adults
Supervised weight loss programmes and bariatric surgery, where general weight loss advice and support is ineffective it may be appropriate to consider a more intensive intervention such a supervised weight loss programme or Bariatric surgery.
Supervised weight loss programmes are very common as private/commercial enterprises but it would not be affordable to fund such programmes through health and social care revenue. However, for a specifically targeted group of people who are morbidly obese (generally BMI greater than 40) and have associated physical complications such as hypertension of diabetes, funding some such programmes may be cost effective in terms of reducing spending on drugs, outpatient and inpatient care. An example is the Counterweight programme: a primary-care led obesity management programme which has been evaluated over the last six years across the UK and is being piloted in a modified form in the NHSSB area. In evaluation studies Counterweight has achieved a weight loss of over 5% in 43% of programme participants in 12 months. This was associated with a reduction in medication costs greater that the cost of the programme itself.
Some patients with very high BMIs may be recommended as benefiting from bariatric surgery. This is the generic term for surgery to the stomach and/or intestine designed to reduce weight through structural modification of the gastrointestinal tract. Recent NICE guidelines identified bariatric surgery as appropriate in a selected group of patients with significant obesity with or without associated complications. The development of a bariatric surgery service for Northern Ireland is currently under consideration. It is estimated that there are more than 50,000 people in Northern Ireland who could be eligible for bariatric surgery using the NICE criteria. The cost of treating only 2% of the eligible population (i.e. 1,000 patients) and providing the necessary long-term follow-up would be in the order of £10 million. This highlights the issues of affordability of such a service and the potential impacts of less intensive initiatives in preventing individuals reaching the stage where bariatric surgery is deemed to be the only option.
Regardless of the outcome of the debate regarding management of the most severely obese people, it is clear that all existing and proposed services must be networked ensuring that each individual receives the level of support and treatment appropriate to their circumstances.
3. Further action required and potential to learn from experience elsewhere
We welcome the creation of the Public Health Agency which will create unprecented focus and leadership for health improvement and preventative care and facilitate the re-energising of the Ministerial Group for Public Health to ensure cross Government leadership and influence. We also look forward to the development of the new strategic direction incorporating physical activity, food and nutrition and obesity priorities into one Strategy/Plan for all of the population.
We believe there is vast scope and energy for taking further action to tackle rising levels of obesity and endorse the findings and recommendation of the recent Foresight Report, Tackling Obesities: Future Choices undertaken on behalf of the Government Office for Science.
This report highlights that obesity is a complex, multifaceted condition that has no easy or obvious solution. The report points out that the attention often given to the most extreme cases of obesity has masked the fact that we as a nation are slowly getting fatter and there is a danger of obesity becoming the norm.
The report also highlights the importance of looking beyond an unhealthy weight being the result of individual choice on diet, exercise and lifestyle and the need to tackle the obesogenic environment in which a range of factors in our physical, socio-economic and cultural environment act to promote calorie intake and discourage physical activity. This is endorsed by the World Health Organisation.
The evidence relating to obesity is limited and focused primarily towards causes rather than prevention. Even the interventions which have looked most successful haven’t been delivered at a scale that offers a clear option for Public Health Strategies. The most promising are community based interventions focussing on diet and physical activity in children and have been used as the basis for a programme involving over 130 towns in France, Belgium and Spain. The early data available is encouraging but full report won’t be available for several years (EPODE).
The evidence to date indicates a number of parts in the life course where there may be specific opportunities to influence behaviour:
Critical periods of metabolic plasticity (e.g. early life, pregnancy, menopause).
Times linked to spontaneous changes in behaviour (e.g. leaving home, becoming a parent).
Periods of significant shifts in attitude (e.g. peer group influences, diagnosis of ill health).
In 2007 the launch of the CEMACH report on “Saving Mother’s lives" took place which indicated that maternal obesity is now a major and growing risk factor for maternal death and more than half of the women who died were either overweight or obese and more than 15% were extremely obese. The report provided 10 key recommendations for policy makers, service commissioners and providers and healthcare professionals.
Two of the recommendations are:
- Preconception care - better counselling and support to be provided for women, especially those with pre-existing serious medical or mental health problems such as epilepsy, diabetes<http://www.medicalnewstoday.com/info/diabetes/whatisdiabetes.php> and obesity (BMI > 30).
- Guidelines for development - guidelines in the care of women who are obese, have sepsis during pregnancy and, pain and bleeding during early pregnancy should be produced.
CEMACH is planning to undertake a national enquiry into obesity in pregnancy as a result of its concerns about the impact on outcomes for both mother and baby. Healthy mothers have healthier pregnancies and healthier babies. The fact that more than half of the women who died were obese or overweight, and that preventable causes of cardiac disease were the leading cause of death shows that strong public health messages are needed both before and during pregnancy.
Breast feeding and early growth patterns provide the only clear evidence to support the critical period of development associated with long term consequences (Barker, D.J.P. 2007).
There is some evidence to show that behaviour in early childhood is significant and it is known that obesity in a parent increases the risk of childhood obesity (Reilly et al 1999).
In older adults effective interventions associated with modest weight loss have been shown to reduce the healthcare costs arising form associated chronic disease such as diabetes.
Evidence from research on social marketing suggests that it is unlikely that public information campaigns that urge people to avoid certain foods and exercise more frequently will be enough to adequately address the problem (Maio et al 2007). Interventions which inform as well as shift motivation and provide the necessary skills are more likely to lead to behaviour change (Fisher, J.D. and Fisher, W.A. 1992).
Interventions based on improved nutrition and increased physical activity can be effective for some individuals, but tackling the obesity problem for the total population will require interventions that target the environment as well, for example food policy and marketing and the transport infrastructure.
The low usage of sports facilities and formal exercise programmes, particularly by people of lower socioeconomic status, highlights the need to consider alternative ways to increase physical activity.
The National Institute for Health and Clinical Excellence (NICE) guidelines on obesity acknowledge the hazy divisions between the prevention and management of obesity and the need to ensure substantial changes to produce the reductions in preventable diseases such as obesity in order to lead to the required reductions in future healthcare costs.
The guidelines acknowledge the enhanced role for schools, local authorities and other public agencies, and private and voluntary sector providers in developing opportunities for people to secure better health.
The NICE guidelines include the following recommendations which we endorse and believe that given appropriate cross Government funding and leadership they could be put into effect through existing and emerging local partnership arrangements:
- Local authorities should work with local partners, such as industry and voluntary organisations, to create and manage more safe spaces for incidental and planned physical activity, addressing as a priority any concerns about safety, crime, inclusion and transport;
- Early years settings should minimise sedentary activities and implement the recommended guidance on food procurement and healthy catering;
- Schools should assess the whole school environment and ensure that the ethos of all school policies helps children and young people to maintain a healthy weight. This includes policies relating to building layout and recreational spaces, catering, food and drink brought into school, the taught curriculum and school travel plans;
- Workplaces should provide opportunities for staff to eat a healthy diet and be physically active;
In addition NICE has provided guidance on related areas including physical activity within primary care and with children in schools.
We believe all actions and policies should take account of health inequalities, in particular in relation to food poverty, which can be defined as an inability to access an affordable ‘healthy’ diet. Many low cost foods, particularly ready meals’ have high calorific value and are high in fat, sugar and salt. The prevalence of take away outlets is higher in many socially deprived areas. These factors emphasis the role for government, both regionally and locally, and for organisations such as the Food Standard Agency.
Sport NI


The Independent Members of the
Northern Ireland Cycling Forum
1. The independent members of the Northern Ireland Cycling Forum Board welcome the opportunity to contribute to the Health Committee’s Inquiry.
2. The NI Cycling Forum Board oversees the implementation of the NI Cycling Strategy. Membership of the Forum comprises staff from the Department of Regional Development, Government Agencies, Local Councils and non-governmental cycling organizations, Sustrans, CTC and the NI Cycling Initiative.
3. The Forum’s independent members hold posts on the Forum on a voluntary, unpaid basis.
4. We welcome an opportunity to meet the committee should the committee consider it advantageous.
The Problem
5. The Northern Ireland Health Survey 1997 shows 56% of adults as overweight 37% or obese 19%.
6. 10 years later in 2007 the NI Health Survey shows 59% of adults measured were either overweight 35% or obese 24%
7. An increase of more than 25% in adult obesity levels over 10 years.
8. The Young Hearts study of 12 and 15 year olds living in NI reported in 2005 a 25% increase of adolescent overweight and obesity in over 10 years
9. Spending by DHSSPS on anti obesity drugs started in 2000 and cost £474,000 that year. By 2007 spending had risen to £3,325,743[1]. This was 400% more than the yearly figure spent on cycling by the Department of Regional Development
10. The Health Committee has already noted obesity costs the local economy £500 million a year
11. Belfast is the most car dependent city in Europe[2]. In a recent Assembly debate the Minister for Regional development is quoted" This morning, while travelling to Belfast, I sat for more than two hours in a traffic jam, so I am aware of the frustrations and difficulties involved in getting into and out of the city amid the congestion"[3].
12. It is children who carry the heaviest burden of this dependence on the motor car with NI having the 2nd worst child pedestrian and child cyclist casualty rates out of 24 developed countries.[4] Fear of traffic discourages active travel[5].
Healthy Eating
13. We look to other expert informed opinion on the issues of healthy eating, access, availability and affordability of healthy food
Integrated Daily Physical Activity – Contributing to the Solution
14. Fit Futures, Focus on Food, Activity and Young People published by DHSSPS in 2005 explains the causes, and the actions required to reduce childhood obesity. The report notes the World Health Organisation believes we live in an obesogenic environment in which a range of factors in our physical, socioeconomic and cultural environment act to promote calorie intake and discourage physical activity[6]
15. A Healthier Future 2005 -2025 published by DHSSPS envisages by 2025 people from all backgrounds in NI will view a healthy diet and physical activity as normal
16. The Institute of Public Health in Ireland demonstrated the relevance of social determinants to public health and the importance of vehicle speed management, traffic calming and other traffic management approaches in the promotion of active travel[7] .
17. Comparative European and North American country studies show lower levels of obesity where there are high levels of active travel[8]
18. Speed management has long been recognised[9] as a key promoter of safer active travel. One of the planned actions noted in the NI Cycling Strategy published in 2000 by the Department for Regional Development was a commitment to introduce appropriate measures to reduce traffic speed. Unfortunately the department did not publish a consultative document on speed management until 2009
19. Through answers to written questions the Minister for Regional Development has stated Roads Service receives many requests for traffic calming schemes and demand greatly exceeds the capacity to supply these measures[10].
20. The Transport and Engineering Unit of Roads Service is bringing forward a number of initiatives to encourage active and sustainable transport but these initiatives are overwhelmed by the Executive’s other road priorities.
21. Cycling and Health published by Cycling England[11] asserts that it is vital for the health of England – and the health of the planet - that health and transport professionals focus on positive actions to encourage cycling, especially where a cycle journey will replace a car journey. Transport and health authorities need to recognise the potential of cycling to improve many aspects of public health and place it at the heart of a healthy transport system devising safe cycling policies and promoting the use of cycling – by children and adults alike on a daily basis
22. Cycling can help people be more active. A regular cyclist enjoys a level of fitness of someone ten years younger, and has a life expectancy of two years above the average.
23. The House of Commons Parliamentary Health Select Committee’s report on obesity (May 2004), states: “If the Government were to achieve its target of trebling cycling in the period 2000-2010 … that might achieve more in the fight against obesity than any individual measure we recommend within this report."
24. To effectively and economically tackle obesity active travel must be prioritized CTC[12] recommends
25. Reducing people’s fear of road danger – by tackling speeding and other forms of dangerous driving, and by giving cyclists visible priority on the roads; and
26. Promoting more and better cycle training – to give people the confidence and skills to cycle for their day-to-day travel (e.g. for school, work and other journeys).
27. Cycle training has been found to be exceptionally effective in increasing the frequency with which people cycle, the length of the journeys they are prepared to cycle and their willingness to cycle in all seasons[13]
28. The CTC in submissions to other Obesity Inquiries elsewhere show that the benefits of cycling far outweigh the risks. Life years gained due to the health and fitness benefits of cycling outweigh the life-years lost through injuries by a factor of around 20:1[14]. As cycling rates increase cycling casualty rates fall[15].
29. Sustrans submission to this current inquiry shows promotion of physical activity through integrated daily activity rather than sport is the easiest and most acceptable form of physical activity for most people
30. Other European Countries have harsher climates and more difficult topography than NI yet can achieve much higher levels of cycling and active travel. . In NI 63% of all journeys are less than 5 miles[16] (a 30 minute bike ride). 97% of rural dwellers in NI live within 5 miles of a rural settlement and services[17]
31. Evidence from elsewhere suggests cost effective intervention in the prevention and treatment of obesity is based on increasing integrated daily activity rather than expensive medical and pharmacological interventions
32. Increasing daily activity can be achieved economically and effectively by a number of measures which prioritizes walking and cycling and reduces car journeys especially those of 5 miles are less
[1] Central Services Agency
Pharmacological treatment should be considered only after dietary, exercise and behavioural approaches have been started and evaluated. Nice Guidelines December 2006
[2] Smyth A W 2001 Contemporary Lifestyles and the implications for sustainable development, Cities,18.2 pp 103 -113
[3] NI Assembly 10th Nov 2008
[4] Ending the Scandal of Complacency House of Commons Select Committee on Transport shows NI with 2nd worst child pedestrian and cyclist rates out of 24 developed countries
[5] Research paper published by Department of Transport
[6] Obesity: preventing and managing the global epidemic. Report on WHO consultation 2001
[7] Institute of Public Health in Ireland Health Impacts of Transport March 2005
[8] An example is BassettDR and others: Walking,,Cycling and Obesity Rates in Europe, North America and Australia. Journal of Physical Activity and Health 2008,5,795 -814
[9] Vaa,The beneficial effect of speed limit reduction Oslo 1997s
[10] AQW 1359/07 is a typical answer.
[11] http://www.cyclingengland.co.uk/site/wp-content/uploads/2009/01/cycling_and_health_full_report.pdf
[12] CTC the national cyclists’ organisation CTC has over 70,000 members and supporters in the UK, including both recreational and utility cyclists
[13] Cycle Training works Page 8
[14] Hillman, M. Cycling and the promotion of health. PTRC 20th Summer Annual Meeting, Proceedings of Seminar B, pp 25-36, 1992.
[15] Evidence available from CTC and Sustrans
[16] Travel Survey for NI 2005-2007 Dept for Regional Development
[17] Rural Settlement Patterns and Access to development land: Developing the Evidence base, Environmental Planning Dept QUB 2008
The British Medical Association
Introduction
1. The British Medical Association
1.1. The British Medical Association, or BMA, is the professional organisation and trade union for doctors in the UK. The BMA in Northern Ireland, or BMA(NI), supports almost 5,000 members from every branch of the medical profession in Northern Ireland. It is the voice of the medical profession - putting across to politicians, the public and the press the profession’s collective views on a wide range of subjects including public health, medical ethics and the state of the NHS.
1.2. The BMA represents consultants, general practitioners, staff and associate specialists, junior doctors, public health doctors and medical academics, and medical students. The BMA has a committee to work on behalf of the interests of each of these branches of practice with a Council to represent all the branches of practice in a single entity.
1.3. The BMA is the only recognised trade union for doctors able to negotiate on their behalf with government in relation to contracts and terms and conditions.
1.4. As well as this function, the BMA produces a wide range of policies from public health issues to medical ethics, and from the state of the health service to doctors’ contracts. The BMA also produces a wide range of publications on health issues including the British Medical Journal.
1.5. The BMA is a voluntary professional association of doctors, speaks for doctors at home and abroad, provides services for its members, is an independent trade union, is a scientific and educational body, is a publisher, and is a limited company, funded largely by its membership fees.
1.6. The BMA believes in a health service that is free at the point of delivery; is centrally planned; is adequately funded; provides equality of access regardless of locality or income; is exclusively based on clinical priority; provides an equal standard of care; ensures equality of health outcome; does not discriminate in terms of race, age, disability or religion.
Inquiry into obesity
2. Summary
2.1. The BMA(NI) welcomes the Health, Social Services and Public Safety Statutory Committee inquiry into obesity.
2.2. The BMA has published a number of reports that take a holistic approach to health in young people including obesity. These include “Growing up in Britain: ensuring a healthy future for our children" (BMA 1999), “Adolescent Health" (BMA, 2003), “Preventing Childhood Obesity" (BMA, 2005), and “Child and Adolescent Mental Health" (BMA, 2006).
2.3. The BMA(NI) is concerned about childhood health and nutrition. Placing the needs of children at the centre of our thinking is vital, as this period is a crucial stage in development. Childhood obesity rates in the UK are soaring and a child’s dietary behaviour is likely to continue into adulthood.
2.4. In Northern Ireland 59% of adults and 26% of children are overweight or obese.[1]
2.5. Obesity is estimated to be causing around 450 deaths each year in Northern Ireland with a cost of around £500 million to the economy.[2]
2.6. The four most common health problems associated with obesity are heart disease, type 2 diabetes, hypertension and osteoarthritis. Obesity also increases the risk of a number of cancers such as colon and prostate cancer by up to 33%.[3]
2.7. The BMA recommended in its report “Preventing Childhood Obesity"[4] that there should be nutrition-based standards for schools meals, the removal of unhealthy foods from vending machines, improved food education in schools and the banning of marketing to children of unhealthy foods.
2.8. The BMA(NI) also
2.8.1. believes it is not only important to try to tackle the present obesity issue but also to be proactive in promoting better health choices for the future and believes this is a cross-departmental responsibility.
2.8.2. believes that cooking should be a compulsory part of the school curriculum, with special emphasis on how to provide healthy meals on a restricted budget.
2.8.3. believes that funding should be increased to improve access to sport and recreation facilities within schools and communities.
2.8.4. believes that accurate food labelling and clear information is imperative to encourage the public to make informed choices about their diet.
2.8.5. calls for funding to establish and sustain training programmes for those who are involved in the care of children with obesity.
2.8.6. believes that there should be a sustained and consistent public education campaign to improve parents’ and children’s understanding of the benefits of healthy living.
3. Background information
3.1. Childhood health and nutrition are of great concern to the British Medical Association. Placing the needs of children at the centre of our thinking is vital, as behavioural patterns established in childhood will continue into adulthood.
3.2. The four most common health problems associated with obesity are heart disease, type 2 diabetes, hypertension and osteoarthritis.
3.3. Obesity increases the likelihood of developing cancers such as breast, colon, endometrial, oesophageal, kidney and prostate cancer by up to 33%.[5]
3.4. The availability of ‘fast food’ is of great concern as these products contain high levels of fat and sugar and have a high energy density. Fast food is often a replacement for healthier food options, thus reducing the quality of the overall diet. The risk of being obese increases with the frequency of consumption of such fast food.[6]
3.5. In women, obesity increases the risk of subfertility. It also increases complications for pregnant women[7], such as,
- Congenital malformations and first trimester spontaneous abortion - Obesity has been associated with an increased risk of foetal congenital malformations and first trimester spontaneous abortion.
- Gestational diabetes - A multicentre cohort study found a 2.6-fold increased risk of gestational diabetes for obese women, and a fourfold increased risk for morbidly obese women.
- Hypertensive disorders of pregnancy - A cohort study found an increased likelihood of chronic hypertension and pre-eclampsia complicating pregnancy.
- Macrosomia - Obesity confers an increased risk of macrosomia (birth weight 4000 g) and large for gestational age fetuses.
- Stillbirth - A recent meta-analysis found an approximately twofold increased odds of stillbirth associated with obesity.
- Prolonged labour - Obesity is associated with prolonged labour giving birth at term and with poor uterine contractility in women who are giving birth for the first time.
- Caesarean birth and associated anaesthetic and surgical complications - A recent meta-analysis found that obese women have an increased risk of unplanned caesarean birth (as high as 50% in some studies), caesarean birth carries additional risks of higher rates of anaesthetic complications and perioperative infections among obese women
3.6. Worldwide over 22 million children under five are severely overweight.[8] In the UK there are around 1 million obese children under 16 years of age.[9] These soaring rates in obesity have lead to an increase in childhood type II diabetes and will lead to more future cases of heart disease, osteoarthritis and cancer.
3.7. Since 1997, there has been a 26% increase in adult obesity In Northern Ireland.
3.8. In Northern Ireland, 59% of the adult population and 26% of children are either overweight or obese.[10]
3.9. Tackling obesity could save the health service in Northern Ireland £8.4 million, reduce sickness absence by 170,000 days and add an extra ten years of life onto an individual’s life span.[11]
3.10. Obesity is estimated to cause around 450 deaths each year in Northern Ireland with a cost to the economy of around £500 million.[12]
3.11. The first Northern Ireland Physical Activity Strategy, “Be Active – Be Healthy" 1996-2002, was published in March 1996. The overall aim of the Strategy was to increase levels of health-related physical activity particularly among those who exercise least.
3.12. In 2002 the Department for Health Social Services and Public Safety published a strategy document called “Investing for Health". This document contains the framework for action to improve health and well-being and reduce health inequalities which is based on partnership working amongst Departments, public bodies, local communities, voluntary bodies, District Councils and the social partners.
3.13. In 2004 the DHSSPS published a consultation document entitled “A Five Year Physical Activity Strategy and Action Plan".
3.14. In 2006 the Department for Health Social Services and Public Safety published a report to the Ministerial Group on Public Health called “Fit Futures: Focus on Food, Activity and Young People".
3.15. In 2007 the Ministerial Group on Public Health published its response along with a consultation on the implementation of “Fit Futures: Focus on Food, Activity and Young People".
3.16. The DHSSPS, along with a number of stakeholders, have over the past number of years produced a number of nutrition and physical activity strategies.
3.17. There is currently a Long Term Condition Directed Enhanced Service (DES) in Primary Care for general practitioners.[13] This DES incorporates the identification of and provision of support and advice for patients with a Body Mass Index (BMI) of 30 or more. A BMI of 18.5 to 24.9 is considered normal, a BMI of 25 to 29.5 is considered overweight, a BMI of 30 to 40 is obese and anything above 40 is considered morbidly obese.
3.18. In the 2007/2008 Quality and Outcomes Framework 100% of available points for the implementation of the obesity part of this DES were achieved in Northern Ireland.[14]
3.19. The National Institute for Health and Clinical Excellence (NICE) has published new guidance on promoting physical activity for children and young people, called “Promoting physical activity, active play and sport for pre-school and school-age children and young people in family, pre-school, school and community settings".[15] The guidance is aimed at everyone who has a direct or indirect responsibility for promoting physical activity for children and young people, including those working in: The NHS, education, local authorities and the wider public, private, voluntary and community sectors. The guidance may also be of interest to parents and other carers.
3.20. The BMA released its report “Preventing Childhood Obesity" in 2005. Its recommendations call for nutrition-based standards for schools meals, the removal of unhealthy foods from vending machines, improved food education in schools and the banning of advertising and marketing to children of unhealthy foods.
3.21. Other BMA reports include “Growing up in Britain: Ensuring a healthy future for our children" (1999), which considered the nutritional needs of children aged 0 to 5 years; “Eating disorders, body image and the media" (2000), which considered the role the media can play in shaping young people’s attitudes to eating and body shape; and “Adolescent health" (2003), which reviewed nutrition, exercise and obesity in adolescents.
4. Conclusion
4.1. The BMA(NI) is responding to the Health Committee enquiry as it feels very strongly that it has a role and a responsibility to represent medical professionals’ views from the frontline on how obesity can be addressed including early intervention and prevention and hopes the Committee finds the recommendations useful.
4.2. The BMA(NI) recognises that obesity is a social phenomenon and all Departments need to work together to tackle this issue.
5. Recommendations
5.1. Food education and the acquisition of related practical skills should be compulsory in schools.
5.2. There should also be special emphasis on how to provide healthy meals on a low income. In order to do this effectively, teachers should receive training on what constitutes a good, balanced diet and how to prepare food. Investment in facilities and effective curriculum development are needed.
5.3. Primary and nursery schools should provide milk free of charge to children in their care.
5.4. All manufacturers should be legally obliged to reduce salt, sugar and fat in pre-prepared meals to an agreed level within a defined time frame. School food contractors should be encouraged to use different approaches to food preparation more frequently, such as boiling, grilling and baking, to reduce fat levels.
5.5. There should be increased access to subsidised sporting facilities for both children and their parents. Ready access for those from lower socio-economic groups is particularly important.
5.6. ‘Exercise on prescription’ (for example, reduced cost/free access to local authority sports centres) should be promoted within primary care.
5.7. Choice in the style of exercise offered to children is desirable, as not all children want to play competitive or mixed sports. The needs of disabled children should also be reflected in the choice available.
5.8. School and municipal playing fields should be protected and promoted.
5.9. There should be a ban on the advertising of unhealthy foodstuffs, including inappropriate sponsorship programmes, targeted at school children.
5.10. Celebrities and children’s television characters should only endorse healthy products that meet nutritional criteria laid down by the Food Standards Agency (FSA). The media has a role to play in encouraging improvements in children’s diet and exercise.
5.11. Supermarkets should consider price promotions for healthy food instead of chocolates, sweets and crisps.
5.12. The BMA believes that accurate food labelling and clear information is imperative to encourage the public to make informed choices about their diet. Nutritional labelling must be clear, simple and easy to understand. Health claims made on food must also be addressed. Both nutritional and content claims on labels, and functional claims on packaging and in advertising, must be accurate and verifiable.
5.13. The BMA strongly advocates that nutritional labelling and health claims should be regulated. Regulations must apply to all traders, suppliers, manufacturers, caterers, agencies, retailers and importers of foods. They must be adequately policed and monitored by a board such as the Food Standards Agency.
5.14. There needs to be funding to establish and sustain training programmes for those who are involved in the care of children with obesity. This includes specialist school nurses, health visitors and GPs.
5.15. This should be complemented by resources to allow children from any region within the UK to gain access to specialist regional obesity services.
5.16. There needs to be clearer guidance and advice as to the most effective ways of losing weight and maintaining weight loss.
5.17. There should be UK-wide surveillance of factors that lead to childhood obesity, developed by the public health observatories.
5.18. There is very little evidence about the effectiveness of interventions and therefore research is needed on the effectiveness of weight management and treatment programmes, the longitudinal impact of obesity on individuals and society, the impact of physical activity (by type) on obesity and co-morbidities, and the relationship between environmental factors and obesity prevalence.
5.19. An audit of the number of departmental strategies related to reducing obesity and its impact on health should happen along with an evaluation of the outcomes of these strategies.
[1] Northern Ireland Statistics and Research Agency (2007), “Health and Social Wellbeing Survey 2005/06", Belfast, NISRA
[2] Department of Health, Social Services and Public Safety (2002), “Investing for Health", Belfast, DHSSPS
[3] Obesity Focussed (2008), “Obesity and Cancer Statistics: Complex Issues" [online], available from: http://www.obesityfocused.com/articles/obesity-and-cancer/index.php [accessed 18 February 2009]
[4] British Medical Association (2005), “Preventing Childhood Obesity", London, BMA
[5] Obesity Focussed (2008), “Obesity and Cancer Statistics: Complex Issues" [online], available from: http://www.obesityfocused.com/articles/obesity-and-cancer/index.php [accessed 18 February 2009]
[6] Shroder, H, Fito, M and Covas, M I (2007), “Association of fast food consumption with energy intake, diet quality, body mass index, and the risk of obesity in a representative Mediterranean population", British Journal of Nutrition, 98, pp 1274-1280
[7] Stotland N E (2008), “Obesity and pregnancy", British Medical Journal, 337, a2450
[8] WHO (2006), “Obesity and overweight fact sheet"[online] available at http://www.who.int/dietphysicalactivity/publications/facts/obesity/en/ [accessed 09 February 2009].
[9] O’Connor, L (ed.) (2004), “Children, young people and health related decisions: a review of the research literature and discussion of the implications for health education of children and young people." Roehampton, University of Surrey & Educari.
[10] Northern Ireland Statistics and Research Agency (2007), “Health and Social Wellbeing Survey 2005/06", Belfast, NISRA
[11] DHSSPS Economics Branch (2003), “Unhealthy Living Model 2nd Edition", Belfast, DHSSPS
[12] Department of Health, Social Services and Public Safety (2002), “Investing for Health", Belfast, DHSSPS
[13] Department of Health Social Services and Public Safety (2008), “The Primary Medical Services (Directed Enhanced Services) Directions (NI) 2008 – NI Service specifications", Belfast, DHSSPS
[14] DHSSPS (2008), “Quality & outcomes framework statistics for Northern Ireland 2007/08", Belfast, DHSSPS
[15] National Institute for Health and Clinical Excellence(2009), “Promoting physical activity, active play and sport for pre-school and school-age children and young people in family, pre-school, school and community settings", London, NICE
Department of Finance and Personnel
Thank you for your letter of 16th January outlining the Terms of Reference for the Committee’s Inquiry into Obesity and seeking written submissions.
I wish the Committee well with their work on what is a significant public health issue. I am supportive of the strategy of prevention not only because it can reduce treatment costs but also because of the wider economic and societal benefits.
Nevertheless, I would stress that any funding required to implement future recommendations from the inquiry will need to be secured from the existing departmental budgets.
I hope this is helpful.
Nigel Dodds OBE
MP MLA
Health Promotion Agency
for Northern Ireland
Introduction
The Health Promotion Agency for Northern Ireland (HPA) is pleased to have the opportunity to respond to the Committee for Health, Social Services and Public Safety’s Inquiry into Obesity.
The Health Promotion Agency for Northern Ireland (HPA) is the major regional provider of health promotion services and plays a leading role in policy development and the provision of advice on health promotion issues. The HPA is committed to working with many statutory, voluntary and private bodies and with national and international health promotion organisations. By working with others we aim to shift the emphasis of modern health services towards prevention, protection and education, to reduce the need for treatment or rehabilitation and improve overall quality of life.
Priority areas of work include nutrition, physical activity, smoking, drug and alcohol misuse, mental health and sexual health. We are committed to reducing the incidence of coronary heart disease and cancers which are Northern Ireland’s biggest killers.
The work of the HPA includes:
- Policy development and advice
- Research, information and analysis
- Public and professional information (campaigns and publications)
- Training and professional development
The comments from the HPA are outlined in response to the Committee’s three areas of particular interest.
The scope and appropriateness of the current approach to the prevention of obesity and the promotion of lifestyle change.
The HPA is an active member of the Obesity Prevention Steering Group and all its sub-groups on Food and Nutrition, Physical Activity, Communication and Research and Information.
In addition to its involvement in these key groups, the Health Promotion Agency fulfils its statutory obligations through its programmes of work on nutrition and physical activity, which aim to meet the targets, objectives and actions detailed in key documents, including the Investing for Health Strategy and Fit Futures Report.
Examples of this work include those outlined below.
Nutrition matters for the early years
The HPA has developed guidance on feeding the under fives for use in all day care settings, including day nurseries, play groups and by childminders. The guidance has been provided to all day care facilities and in addition staff from these facilities have been offered the opportunity to attend local training seminars, which have been conducted in partnership with staff from Health and Social Care Trusts. The document includes a menu checklist which is used routinely by Social Services staff in their initial and routine inspection of childcare facilities.
Food in schools
The HPA has been working in partnership with the Department of Education and the Education and Library Boards for several years to develop and implement nutritional standards for school meals and other food in schools. This has led to the appointment of a Food in Schools Coordinator, who is based in the HPA and jointly funded by DE and DHSSPS.
Cook it!
This is a regional community based nutrition education programme which aims to increase nutritional knowledge and understanding and enhance cooking skills. The programme is supported at regional level by the HPA and is delivered locally within Health and Social Care Trusts. Trained Cook it! tutors deliver the six-week Cook it! programme at local community level.
Thorough evaluation of the programme across Northern Ireland highlighted increased nutritional knowledge and dietary changes as a result of participation in the programme , well as other benefits, including weight loss, increased physical activity and the pursuit of further education and employment opportunities.
The Cook it! programme is currently being adapted for use with people with learning difficulties.
Nutrition training for professionals
The HPA is an accredited centre for the delivery of training for the Royal Society of Public Health nutrition courses. Five courses leading to the Diploma in Nutrition and Health have been completed for Environmental Health Officers and senior school meals caterers. The course equips delegates with a good understanding of basic nutrition enabling them to train caterers in basic nutrition and provide advice and support. This is considered to be a very valuable area of work because of the increasing number of meals and snacks which are purchased and eaten away from home.
Websites and printed resources for the public
The HPA has developed a number of websites for use by the public, two of which are of particularly relevant to this inquiry: www.getalifgetactive.com and a new website, www.enjoyhealthyeating.info which will be launched in March. Both sites provide up-to-date scientifically based information to enable all age groups to be more active and eat more healthily in order to achieve and maintain a healthy weight. These are complemented by a range of printed resources including Small changes: big benefits, Enjoy healthy eating, Get a life, get active and Get a life, get active…go walking.
Public information campaigns
The HPA has developed a number of public information campaigns on physical activity, for example, Every step is a forward step, Go walking. Go biking and No excuses. The support materials have included information on both activity and nutrition to tackle both side of the energy balance equation.
A new campaign is under development, which will specifically target children and their parents. The campaign will be launched later in 2009.
Get active in the community
This scheme, which is in its eleventh year, offers small grants of £500 to community and voluntary groups to encourage those in their local community to be more active, particularly those who are sedentary.
The availability of weight management or other intervention services to tackle obesity related ill health
Weight management clinics are not offered consistently across Northern Ireland and access to these varies markedly. A consistency of approach is essential, to ensure that access to weight management clinics and programmes for children and their families is the same, regardless of area of residence. Consideration should also be given to those involved in the delivery of these clinics, as it is essential to ensure that such programmes are organized and delivered by professionals who have appropriate training in this specialist area.
The use of family-centred approaches should be considered, in which the cooking and eating habits and activity levels of the entire family are addressed.
A number of commercial initiatives have been developed in recent years, employing a wide range of approaches to weight loss. Consideration should be given to the standardisation or licensing of such initiatives to ensure that appropriate methods of weight loss are employed and that vulnerable groups, including children are not inappropriately advised.
Further action required, taking account, as appropriate, of the potential to learn from experience elsewhere
Current funding streams for the implementation of the Fit Futures plan has led to the provision of small grants to organisations and groups at local level. Whilst this approach has been beneficial in encouraging innovation, there is at present no centrally held knowledge or database of these local projects, including their aim and objectives, methodologies and results of evaluations. As the Obesity Prevention Steering Group and it sub-groups become established, it will be important to consider these issues, in order to promote the sharing of information and avoid duplication of effort.
Local Commissioning Groups should be informed about local interventions and the need for regional approaches.
The Foresight Report Tackling obesities: future choices provides a detailed analysis of obesity and the opportunities for its management. In order to avoid duplication of effort, the information contained within this report should be used to inform the development of future approaches in Northern Ireland. We would also recommend that it is appropriate to buy into the Change for life campaign in England and benefit both from the considerable expertise which has been invested in the campaign development and the ‘economy of scale’ which would result. Some advertising for the campaign is already viewed by the public in Northern Ireland, through some television channels and other routes.
It is acknowledged that once overweight and obesity are established, weight loss is difficult to achieve and even more difficult to maintain. It is recommended, therefore that the prevention of overweight and obesity are given increased priority, particularly within the following areas.
Early years settings
The work conducted by Foresight highlights that the early years should be a key
Focus for preventative work. Current initiatives such as Surestart and Homestart offer great potential for working with families with young children, particularly those from disadvantaged circumstances. To date the focus given to nutrition by these organisations has been ad hoc. We recommend that there should be an increased emphasis given to good nutrition within the Surestart and Homestart programmes, including the development, implementation and evaluation of a regional programme with local support and training for Surestart and Homestart provided by Registered Dietitians.
In addition, the work on Nutrition matters for the early years identified above with childcare providers should be strengthened and further developed.
Schools
The current work outlined above should be continued and strengthened, with the continued funding of essential posts to support this work, including the Associate Inspectors within the Department of Education, a Regional Food in Schools Coordinator (at present based within the HPA) and the local Nutritional Standards Coordinators (based within the Education and Library Boards).
Primary care
As indicated above, weight management clinics are not offered consistently across Northern Ireland and access to these varies markedly. It is essential to ensure that access to weight management clinics and programmes for children and their families is the same, regardless of area of residence. It is also essential to ensure that such programmes are organized and delivered by professionals who have appropriate training in this specialist area.
Public sector catering
The public sector has an important opportunity to act as a role model through the implementation of nutrition policies within al Government facilities, hospitals etc, leading to changes in procurement practices and the provision of a wide variety of healthy food choices through catering outlets and vending machines.
Department for Social Development
The Department’s Neighbourhood Renewal Strategy supports some health programmes throughout Northern Ireland. Details are as follows.
Southern Regional Development Office:
Southern Regional Development Office funds some health programmes which include an element relating to healthy eating - Cook It etc, and some sports related programmes, provision of Multi Use Games Areas, playing fields, etc all of which would have links to encouraging and supporting healthy lifestyle choices.
Northern and Western Regional Development Office:
RDO Western Division NR currently fund a health programme in all NRAs. Although neither of the programmes have specific targets around obesity they all have an overall programme focus on healthy lifestyles, healthy eating and weight management. Colleagues in WHSSB and WHSCT have in the past preferred not to badge as obesity programmes due to difficulties this would present in advertising and securing uptake from Neighbourhood Renewal Area residents.
The overall funding package for each area is detailed below:
Dungannon 09.07 to 03.10 £13,115.22
Coalisland 09.07 to 03.10 £31,001.15
Omagh 10.08 to 06.09 £33,895.00
Enniskillen 09.08 to 06.09 £58,564.00
North West Development Office (NWDO):
NWDO fund the following 2 projects through Neighbourhood Renewal that address obesity:
- Derry City Council - Active Citizenship - Through Sport Programme - provide sporting services to tackle obesity.
- Old Library Trust - Healthy Living Centre - The Centre provides tailored programmes aimed at tackling the prevalence of obesity.
Belfast Regeneration Office
Belfast Regeneration Office has used Neighbourhood Renewal Funding to support a wide range of community-based projects located in disadvantaged areas of the city.
Whilst a number of the projects supported are health-related, none of these is specifically designed to address the issue of obesity, at least not in isolation.
Broader health programmes, funded through the Neighbourhood Renewal Programme and delivered by community-based organisations do however include health promotion initiatives and actions to encourage greater physical activity and healthier eating choices. Some specific programmes also cover weight management issues.
Typically, Shankill Women’s Centre runs a ‘weigh to health’ programme, but this is only one of a number of classes/courses that they offer. Other Women’s Projects and some broad-based programmes operated out of funded community facilities run similar schemes.
The other link the Department has with obesity related issues is in the area of Social Security benefits. Since October 2008 new medical codes were introduced, one of which was a specific code for obesity. Reports show that from that date there are 52 Disability Living Allowance (DLA) claims and 64 Incapacity Benefit (IB) claims where obesity is recorded as their main disabling condition. Figures also show that 15 of the DLA claims and 22 of the IB claims come from Neighbourhood Renewal Areas.
Royal College of
Nursing Northern Ireland
Introduction
1 RCN Northern Ireland welcomes this opportunity to submit written evidence to the Committee in relation to its Inquiry into obesity. We hope that our comments will prove helpful to the Committee in its consideration of this issue.
2 RCN Northern Ireland is aware that the Committee is already well-informed about the incidence and extent of obesity in Northern Ireland, underlying causes, determinants, impact upon health, and economic costs. It is not our intention, therefore, to repeat this familiar statistical evidence. Nor do we seek to address the important cross-sectoral measures that need to be taken in respect of education, partnership with the food industry and promoting healthy lifestyles that are central to tackling the issue. Instead, our submission focuses primarily upon the contribution that nurses and nursing can make to addressing obesity.
Executive summary
3 The key points that RCN Northern Ireland would wish to draw to the attention of the Committee are as follows:
- A number of targets and strategies are already in place to address obesity and associated issues in Northern Ireland. The Committee may wish to assess progress in relation to these targets and strategies before determining a new course of action.
- Nursing has a major role to play in addressing obesity and the broader public health agenda in Northern Ireland.
- Nurse-led community health projects have a proven positive impact upon the health and social care of communities in Northern Ireland, including specifically in relation to obesity.
- Early intervention, particularly through school and other specialist community public health nurses, is central to tackling obesity.
- A major workforce development plan is essential to ensure that we have the right numbers of appropriately qualified health and social care practitioners in place to help tackle obesity.
- The nursing input to the new health and social organisations is inadequate to ensure that this nursing contribution to the public health agenda is effectively secured.
Obesity as a health priority
4 In its strategy document A healthier future: a twenty year vision for health and well-being in Northern Ireland 2005-2025, the DHSSPS acknowledges that “rising levels of obesity and lower levels of physical activity will increasingly contribute to the burden of disease. Obesity is a contributory factor to a number of conditions, such as stroke and cardiovascular disease. Obese men are more than 33% more likely to die from cancer and obese women are more than 50% more likely to die from breast cancer." The strategy commits the DHSSPS to “… seek to reverse the current increase in the level of obesity in men and women so that by 2025 the proportion of men who are obese is less than 15% and the proportion of women who are obese is less than 17%. (In 1997 17% of men and 20% of women were obese)." In relation to children, the DHSSPS also seeks to stop “… the increase in levels of obesity in children by 2010 and reducing it by 50% by 2025".
5 RCN Northern Ireland supports this direction of travel and suggests that the Committee may wish to explore with the DHSSPS whether these targets are still extant, whether in retrospect it believes them to be sufficiently ambitious, what specific measures it has implemented in pursuit of the targets, and what progress has been made to date in achieving them.
The role of nursing in tackling obesity
6 The positive impact that innovative community nursing can exert on levels of obesity in Northern Ireland is demonstrated by an award-winning project established by the former Homefirst Community Trust (and now managed by the Northern Health and Social Care Trust) at Glenfield estate in Carrickfergus. The project features a nurse-led walk-in clinic, shaped by and focused on the needs of the community in an area of social deprivation and delivered through a nurse practitioner-led service providing first contact care, health promotion and elements of chronic disease management with strong public health principles. Central to the clinic’s success has been an award-winning weight management programme and monthly health promotion sessions.
7 The success of the programme can be gauged by the fact that, during its first year of operation, 65% of clients lost weight over a course of weekly sessions that attracted between 25 and 50 clients. An average 58% weight loss was recorded during this first year. The nurse practitioner-led service has increased patient choice and access to services and is a model that should be replicated in other areas of health and social care need across Northern Ireland. The clinic’s establishment and initial development was driven by nurse practitioner Ivy Bradley, who, on the basis of her work in establishing the project, was highly commended by the Nursing Times at its UK awards in 2006 and was a finalist in the RCN Northern Ireland Nurse of the Year Awards the same year.
8 RCN Northern Ireland believes that the early intervention of specialist community public health nurses and particularly school nurses is essential to addressing childhood obesity and therefore tackling the problem at an early stage. Our manifesto for the 2007 Northern Ireland Assembly elections noted that: “… increasing the numbers of school and community nurses is essential if we are to tackle the rise in obesity amongst children and young people". RCN Chief Executive & General Secretary Dr Peter Carter recently stated: “If we are going to get children on the right track, if we are going to end this growing obesity problem, [trusts] need to recruit the right numbers of school nurses who can identify unhealthy children from an early age and intervene accordingly". This view is supported by guidance published by the National Institute for Health and Clinical Excellence, which emphasises the need to “… assess the whole school environment and ensure that the ethos of all school policies helps children and young people to maintain a healthy weight, eat a healthy diet and be physically active, in line with existing standards and guidance".
9 In Northern Ireland, the number of school nurses currently employed by the Health and Social Care service is inadequate to secure this vision. According to the Northern Ireland Health and Personal Social Services Workforce Census published by the DHSSPS, as at 31 March 2007 there were 119 nurses by headcount in the whole of Northern Ireland. Only 23 of these worked full-time, giving a whole time equivalent figure of 88. Department of Education data confirms that the total pre-school and school population in Northern Ireland for 2007-2008 was 326,114. This means that each school nurse theoretically covers 41,581 children and young people. School nurses have a key role as gatekeeper to the health and social care service for many children and young people, enabling issues such as obesity to be tackled effectively at an early stage. Clearly, however, this role can only be secured if there is a significant investment in securing the right numbers of school nurses, an investment that would be repaid many times over by future savings in the cost of obesity-related ill health in Northern Ireland.
10 With regard to the adult population, the same points can be made. DHSSPS workforce statistics do not effectively delineate the broad range of specialist community nurses working within the Health and Social Care Service and so it is difficult to make an equivalent comparison. However, it is unlikely that the ratio is significantly higher. The Chief Nursing Officer for Northern Ireland recently stated that: “Health is a fundamental human right. All citizens should have equal rights to health, fair and equitable access to health services and health information according to their needs. The nursing contribution comes through joined-up teamwork, supporting health in early years and through schools and community development". RCN Northern Ireland endorses this vision but believes it will not be secured without a workforce development programme that delivers the right numbers of appropriately-qualified community nurses working in the health and social care service and empowered to tackle major public health issues such as obesity by working in partnership with other professions and with communities.
11 All nurses are in direct contact with patients, clients and communities. The nursing workforce in Northern Ireland embodies a huge potential for the effective dissemination of health promotion messages related to obesity, in addition to screening and brief interventions. Nurse practitioners, practice nurses and treatment room nurses in particular are in a prime position to run obesity or weight management clinics as well as to assess, screen and provide one-to-one advice to individuals. Health visitors maintain contact with families with pre-school children in their own homes, providing an opportunity for individual support and advice to mothers that can impact positively on other family members. Health visitors are also often involved with Surestart programmes; many deliver positive parenting sessions, health promotion classes to community groups and other public health initiatives with people of different ages, all with the potential to provide health promotion, intervention and support on obesity.
12 There is a need to raise awareness amongst all nurses in relation to obesity, and to achieve consistency across the five Health and Social Care Trusts and communities throughout Northern Ireland in terms of assessment, screening, brief intervention, referral and follow-up. Obesity awareness should be incorporated within all pre-registration nursing programmes of education and reinforced through continuing professional development activity, not just for community nurses but also for those practising in traditional acute settings.
Health and social care reform in Northern Ireland
13 The new health and social care system that will be established in Northern Ireland from 1 April 2009 is founded upon the Minister’s intention to place the public health agenda at the heart of the system, focusing the service on the promotion of good health, tackling health inequalities and addressing the underlying causes of ill-health. RCN Northern Ireland entirely supports this direction of travel, which builds upon and intensifies the trends identified in A healthier future: a twenty year vision for health and well-being in Northern Ireland 2005-2025. We believe that obesity is an excellent example of the type of public health issue that the new system should be able to address and upon the achievement of which it will justifiably be judged.
14 RCN Northern Ireland remains concerned, however, that the structures of the new health and social care organisations will not enable the nursing contribution to the public health agenda to be secured and that this will affect the capacity of the new organisations to realise the Minister’s priorities with regard to issues such as obesity. Specifically, the Regional Agency for Public Health and Social Well-being will include just two tier 3 posts reporting to the Director of Nursing and Allied Health Professions. Only one of these posts is likely to be a nursing post and the post-holder will be responsible for the entire safety, quality and patient/client experience agenda within the Regional Agency. In our response to the recent DHSSPS consultation on these proposed structures, RCN Northern advocated the creation of three tier 3 posts reporting to the Director of Nursing and Allied Health Professions. One of these proposed posts, Assistant Director for Public Involvement and the Patient/Client Experience, would be responsible inter alia for the provision of nursing advice, participation in the community development and health agenda, and in the design of service improvement programmes for public health.
15 Within the new structures, the designated tier 3 lead for health and social well-being improvement (which will presumably encompass the obesity agenda) reports to the Director of Public Health Medicine. The DHSSPS has not yet indicated how this post and the other tier 3 posts reporting to the Director of Public Health Medicine will relate to the nursing tier three posts. This is another matter of concern to RCN Northern Ireland. Health promotion, health improvement and the wider public health agenda are not exclusively medical functions. The DHSSPS must specify how it will ensure that the contribution of nursing and the other non-medical health and social care professions to issues such as obesity and the broader public health agenda can be secured.
Conclusion and further information
16 RCN Northern Ireland reiterates our gratitude to the Committee for inviting this submission and we hope that our comments will prove helpful. We would be pleased to supply any further information that the Committee may require and to discuss these issues in greater depth with the Committee, should it wish to do so.
Safefoods
Safefood is a significant player in the nutrition field on the island of Ireland (IOI). Our Corporate Plan activities cover research, surveillance and communication, and key to this is fostering an all-island approach. The North South Ministerial Committee (NSMC) have approved these activities and at the November 2007 NSMC sectoral meeting it was identified that one of our high level objectives was “TO PROMOTE A ‘JOINED-UP’ APPROACH TO FOOD SAFETY AND NUTRITION STRATEGIES ACROSS THE ISLAND OF IRELAND".
Obesity is the major focus of safefood’s nutrition related activities. Given its unique position as a North-South Body safefood is actively involved in the obesity implementation groups in Northern Ireland (NI) and Republic of Ireland (ROI). It is a member of the Department of Health, Social Services and Public Safety (DHSSPS) Obesity Prevention Steering Group in NI and the Department of Health and Children (DOHC) Intersectoral Group in ROI.
To support the Health Committees inquiry safefood wish to provide the following information and comments
1. A summary of safefood activities in the area of obesity is provided in appendix 1.
2. The NSMC sanctioned the establishment of an All-island Obesity Action Forum by safefood in 2008. The first inaugural meeting of this forum took place in December 2008 and range of stakeholders from government, community, academia and industry were invited to attend. The aim of the forum is to support the obesity policies in both Northern Ireland (NI) and Republic of Ireland (ROI) by bringing together stakeholders to identify and promote collaboration in common areas of action across jurisdictions, to facilitate the exchange of best practice and promote networking on the island of island. Two workshops are being currently planned for May and September 2009. Each workshop will address a common area north and south. The areas under current discussion are communication, research and catering.
3. Food poverty in NI needs to be a focus - it is well recognised that food poverty is associated with higher rates of overweight and obesity and poorer dietary habits. safefood funded the Public Health Alliance to conduct research into the extent of food poverty in NI. This research was launched in 2007. However, a concerted action by key stakeholders in NI is required to drive this issue forward. The Food Standards Agency (FSA) and safefood have arranged to host an exploratory meeting with stakeholders on 23rd April 2009.
4. As is evident in DHSSPS Obesity Prevention Steering Group much is being done in the area of tackling overweight and obesity and much public money is being spent. However there remains scope for greater collaboration and co-ordination.
5. The life course approach to tackling obesity is required in addition to the current focus on children. Early intervention treatment as well as established obesity treatment must be addressed, requiring a primary care intervention strategy.
Appendix 1
Summary of key nutrition activities carried out by safefood 2004-present.
| Activity | Description | Status |
| All-island approach | ||
| All-island Obesity Action Forum | Aim to support the obesity policies in both Northern Ireland (NI) and Republic of Ireland (ROI) by bringing together stakeholders to identify and promote collaboration in common areas of action across jurisdictions, to facilitate the exchange of best practice and promote networking on the island of island. | Biannual workshops will be held in 2009 and 2010. Each will focus on a common area of action in both jurisdictions. |
| Nutrition Exchange Programme | A funding programme to support nutritionists and dietitians in IoI to collaborate and share best practice | A pilot programme was run and evaluated in 2006/7. A revised programme was launched in September 2007. To date 53 people have participated. |
| Food Poverty | safefood and FSA NI funded the development and evaluation of a community based project the ‘Decent Food for All’ programme in the Armagh Dungannon Health Action Zone. It aimed to tackle poverty by increasing food awareness and improving physical and financial access to safe healthy food. It incorporated community education, healthy lifestyle choices, regeneration of local communities and markets, and sustainability. safefood are co-funders of Healthy Food for All which is a multi-agency all-island initiative seeking to promote access, availability and affordability of healthy food for low-income groups on the island of Ireland. It brings together NGO, community groups and government agencies and departments on the island of Ireland. Healthy Food for All and safefood are establishing a Demonstration Programme on Community Food Initiatives and are looking for funding applications from eligible groups and organisations. The purpose is to establish a Demonstration Programme of Community Food Initiatives on the island of Ireland. Community Food Initiatives are projects that improve the availability and accessibility of healthy food for low-income groups at a local level, using a community development approach. | The learning from this project has been shared with many key stakeholders through project site visits for community groups and through a research dissemination workshops on an all-island basis This network has been established for 3 years. safefood and FSA NI have agreed that there is need for a more concerted effort among NI stakeholders. A meeting of stakeholder is planned for 23rd April 2009 to drive the issue forward in NI. Between five and seven initiatives will be funded over a three-year period staring 2009. Each initiative will receive annual funding over a period of three years to set up, manage and sustain a project. Funding will be up to a maximum of €75,000 (£60,000) provided on an incremental basis over the three year period. |
| Food and Nutrition Forum | A platform for collaboration on nutrition, facilitating the sharing of experiences across jurisdictions and between sectors. safefood acted as secretariat | Met regularly in 2005 and 2006. The Forum has now been developed into the all-island Obesity Action Forum |
| Dietetic Directory | The establishment and development of a database of activities in the field of dietetics in IoI to support collaboration and cooperation | The database currently has information from 75% dietetic departments on IoI. To be evaluated in 2009. |
| Pilot initiatives | Support for pilot health promotion initiatives that have the potential for roll out across IoI. Initiatives funded include X-pert diabetes programme and pre-school healthy eating polices. | Hit on Health Project – this project developed an initiative that provided and highlighted healthy food options in the catering sector. Rolled out further in ROI. Project is available to NI if required. Currently supporting Western Health and Social Services in piloting a budgeting and healthy eating programme called Food Values |
| All-island workshops | Salt workshop 2006 Dietary Habits Conference May 2007. Both in collaboration with FSA NI and Food Safety Authority of Ireland | Completed. Evaluated through participant satisfaction questionnaires. |
| Promotions | ||
| Salt Campaign | Phase 1 – Awareness that a high salt diet is bad for health. Included radio, billboards and press. Phase 2 – A workplace campaign aimed at adults to reduce salt intake – included radio, press and print material. Phase 3 – Continue with a workplace salt campaign | Run initially in May 2005 and repeated in November 2005 Run in May 2006. Rolled out in collaboration with the Irish Heart Foundation and the Chest Heart and Stroke Northern Ireland. The target audience was businesses with at least 100 employees or more. Two hundred thirty nine (239) businesses took part across the island of Ireland with 197 in the Republic of Ireland and 42 in Northern Ireland. Evaluated internally. Currently in development for roll out in Q3 2009. |
| Treats Campaign | Phase 1 – awareness that children are eating too many fatty and sugary treat foods are that these foods are often nutritionally poor – included TV, poster and print media. Phase 2 – provide practical advice on reducing high fat and sugary snack foods in children’s diet – children’s treat chart and parents’ information booklet disseminated through disadvantaged schools. | Launched November 2005. Evaluated using safetrak. Launched February 2007. Evaluation currently underway. 21,000 leaflets distributed In NI |
| Superfoods | Promote the consumption of fruits and vegetables, wholegrains and leaner meats. Phase 1 – parents of young children (2-8 years) through radio, press, supermarket trolley handles, website and bus rears. Phase 2 – parents and children targeted. Used TV, radio, press, supermarket trolley handles, website. Phase 3 – parents and children targeted directly in the supermarket at point of purchase. Initiative supported by TV, radio and press. | Evaluation- safetrak and Omnibus research Launched November 2006. Launched June 2007. Launched September 2007. |
| Little Steps | This campaign is notable in that it was developed by safefood in partnership with the Health Service Executive (HSE) and in collaboration with the Health Promotion Agency, Northern Ireland. Aim: The campaign is called “Little Steps go a long way" and aims to support parents/guardians as positive role models for their children for healthy eating and physical activity. | The campaign elements include TV, radio, website, PR, direct marketing and outdoor advertising. The campaign was launched in June 2008 and will be developed further over the next 3-5 years. |
| Weight Loss for Adults | safefood develop a website to provide practical and evidence based advice to adults on the island of Ireland on achieving weight loss. safefood is currently developing a workplace weight loss initiative targeted at the road haulage industry on the island of Ireland. The initiative with use social marketing techniques to engage with this target group. The initiative will focus on a combination of healthy eating and physical activity. A pilot is scheduled to take place in May. | The website is www.weigh2live.eu, was launched in May 2008 and will be developed on an ongoing basis to support health professionals and the general public. Under development |
| Education Resources | How we measure up –Deciphering Food Labelling. - aims to give post primary students a better understanding of food labels and how to use them to make healthy and safe food choices. It was developed in conjunction with the Council for the Curriculum, Examinations and Assessment (CCEA). Safefood developed a curriculum based resource called Taste Buds that is supported by research to show it is an effective tool. Taste Buds aims to help children aged 8-10 years enjoy learning about the origins and production of food and the importance of eating a balanced diet and being active. ‘safefood for life’ resource for post primary schools. The safefood for life programme is a certified food safety programme that is being delivered in post primary schools across the island of Ireland. The programme aims to help students develop important food safety skills and allows them to sit an online food hygiene examination at the end of the course. On completion of the online examination successful students will meet the minimum training requirements to work in the food industry. | It was sent out in a regular dispatch of material to the heads of Home Economics by the CCEA in 2005. This project was originally developed by a research team led by University of Ulster. Currently working with Farm2Fork resource in Western Health and Social Services Trust to develop resource for NI to prevent duplication of resources. To date in NI Total number of schools registered for safefood for Life– 77 Total number of schools who sat exams- 33 Total number of exams (i.e. students who sat the online exam) – 546 |
| Research | ||
| Research programme 2001 onwards | Supported the completion and dissemination of nutrition related projects. Key projects included were (1) Hit on Health Project (2) Communicating the healthy eating message (3) Novel Strategies for Food Risk Communication (4) Standard of healthy living on the island of island. (5) Food Poverty In Northern Ireland (6) Ongoing consumer research | (1) Project completed in 2005. Has been rolled out in a larger area. Disseminated through academic and dietetic networks. (2) The CD-Rom developed has been enhanced to include food production material. Currently working with Farm2Fork resource in WHSST to develop resource for NI. (3) Project results were disseminated through report and a workshop in October 2005 (4) Project results were disseminated through report and a workshop in April 2007 (5) Project completed and disseminated through final report and workshop in November 2007. (6) safefood conduct consumer research on an ongoing basis including omnibus surveys and qualitative research |
| Needs assessment for provision of nutrition information on safefood’s website | A needs assessment has been completed by a University College Cork research internship | The findings were applied and safefood’s website was revised and relaunched in December 2008. |
| Surveillance | ||
| National Children’s Survey | Detailed analysis of dietary habits of children aged 5-12 years | Project completed in 2008 |
| Salt Intakes | Estimate of salt intake using urinary salt excretion in adults in RoI. Provide comparable data to that available in NI. | Project due for completion in 2009 |
| National Diet and Nutrition Survey – Northern Ireland | Support the expansion of the project to include Northern Ireland with Food Standards Agency and DHSSPS. | Funding and planning agreed for a 3 year period. Fieldwork commenced in 2008 |
Royal College of General Practitioners
Physical activity may be good for you but we are not the key players
Let’s get real. General practice cannot cure the cycle of creeping inactivity, bulging waistbands and obesity. This is a medical problem with a potentially huge healthcare burden but, it does not have a medical solution. We need to be clear about what we can do, because it is easier to pass responsibility to the medical profession, and primary care in particular, than face up to the implications of making a serious commitment to those changes necessary to reduce overall calorie intake and increase the population’s physical activity. Physical inactivity is a social problem. It is a function of our computerised, mechanised and immobilised society. We are a low activity convenience society fed by high calorie convenience foods. The primitive hunting and gathering instincts are focused more on the struggle in the shopping centre, than on any physical activity. Doctors cannot solve this problem.
General practice is the care of the individual. Our attempts at health promotion in primary prevention have had remarkably little success. Cardio vascular risk-factor reduction looked to have potential, and the problems we addressed were important and relevant. But, the impact was minimal. Even well-funded nurse-led innovative projects like OXC heck had modest impact with major resources.
Such findings were in keeping with the major systematic review of randomised controlled trials, which suggested that risk factor interventions had a limited role and that other government-led interventions could be more effective.
And, if we wish to improve diet and physical activity levels, there are important lessons to be learned from our interventions in smoking.
Evidence from high quality observational, cross-sectional and cohort studies is clear. Physical activity is good for you, and obesity is associated with inactivity. But, that does not mean that interventions to increase activity will be successful in reducing obesity. Efforts to increase physical activity through primary care have had limited success. A number of studies have shown that it is possible to create programmes to increase physical activity (including exercise prescription), address barriers, record advice given, and intention to increase activity — but most are process studies and few have longterm outcomes.
The most recent systematic review (Cochrane) on efforts to increase physical activity has shown that interventions to increase physical activity are, at best, moderately effective. Similarly, methods to reduce obesity include efforts to change overall lifestyle with specific interventions advising combinations of diet and exercise. Lifestyle interventions have shown only small amounts of weight loss of marginal clinical relevance and while we have little evidence of what works in preventing and treating obesity, research does show us what doesn’t.
GPs themselves have a realistic view of what is possible. GPs believe that obesity is the responsibility of the patient and do not consider obesity management to be within their professional domain. Patients think otherwise. They tend to blame an internal control problem and would like a professional-based solution, but doctors favour a patient-led approach.
There is an Olympic dimension. The 2012 Olympics focuses greater emphasis on the benefits of sport and exercise. Indeed, the Royal College of General Practitioners has been pivotal in creating the new Faculty of Sports and Exercise Medicine and establishing specialist training. We could easily be swept along by this groundswell of enthusiasm and commitment to sport and there is a danger that well-meaning leaders of our profession might agree to the unrealistic inclusion of obesity management through exercise promotion in the Quality and Outcomes Framework. This is a public health issue.
The barriers to physical activity are not issues limited to personal health care. They are predominantly environmental, social, and societal. The solutions are multidisciplinary and cross-departmental. Providing bicycle lanes, making showering facilities available in the workplace, funding crèches at the leisure centres, reversing the erosion of sporting activity in schools and the sale of public sporting amenities are not health issues, but have health implications related to physical activity. Making it a primary care problem is the easy option, directing the public gaze away from the need for more integrated and much more expensive social and environmental factors. Let us not be foolish enough to accept responsibility for a task we cannot deliver. There are many aspects of practice where we can make a difference. This is not one.
References
1. Coulter A, Fowler G, Fuller A, et al. Effectiveness of health checks conducted by nurses in primary care: final results of the Oxcheck study. BMJ 1995; 310: 1099–1104.
2. Ebrahim S, Smith GD. Systematic review of randomised controlled trial of multiple risk factor interventions for preventing coronary heart disease BMJ 1997; 314: 1666.
3. Yach D,McKee M, Lopez AD, Novotny T. Improving diet and physical activity: 12 lessons from controlling tobacco smoking. BMJ 2005; 330: 898–900.
4. Hillsdon M, Foster C, Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst Rev 2005, 1: CD003180.
5. Jain A. Treating obesity in individuals and populations. BMJ 2005; 331: 1387–1390.
6. Epstein L, Ogden J. A qualitative study of GPs views of treating obesity. Br J Gen Pract 2005; 55(519): 750–754.
7. Ogden J, Bandara I, Cohen H, et al. General practitioners’ and patients’ models of obesity: whose problem is it? Patient Educ Couns 2001; 44(3): 227–233.
Department of Education
The Department of Education (DE) welcomes the Committee for Health, Social Services and Public Safety’s (DHSSPS) inquiry into obesity and the recognition that the issue goes beyond the DHSSPS and requires a concerted effort by a range of departments and organizations.
1. Within DE we recognize the vital role that education has in equipping our children and young people for life. The education system in general has always been to the forefront in encouraging healthy lifestyles and providing children and young people with the foundations on which to build for active and healthy lives in the future.
2. DE has worked closely with the Fit Futures taskforce in the past and continues to participate in the Obesity Prevention Steering Group and all its advisory groups.
3. The principle priority for action for DE coming from the Fit Futures report is Creating Healthy Schools. There are a number of initiatives already underway in DE, which support the recommendations of the Fit Futures report and which provide the basis of a developing healthy schools policy.
4. Whilst the issue of obesity is traditionally viewed as an imbalance between diet and physical activity, the healthy school policy should not confine itself to the healthy eating and physical activity elements alone rather the policy should address the four strands of a healthy school – healthy eating, physical activity, personal development and emotional wellbeing. It is envisaged also that the policy will take a whole school approach and include early years’ provision and youth services.
5. The building block for this policy has already been put in place by the inclusion within the Education (School Development Plans) Regulations (NI) 2005 of a requirement that school development plans must include an assessment of the arrangements for the promotion of the health and wellbeing of staff and pupils. All schools are required to produce these plans every three years. All schools should, therefore, have commenced a process to develop and implement a healthy school programme as part of its school development planning process.
Early Years
6. The transfer of Early Years to DE now means that DE has policy responsibility for settings such as child minders, day nurseries, playgroups, parent and toddler groups, Sure Start projects and crèches. These settings are all registered and inspected by the Social Services Inspectorate in connection with the requirements of these Children (NI) Order 1995.
7. Provision is made within the registration and inspection requirements for nutritional standards that should be demonstrated. In this regard, a policy entitled ‘Nutrition in the Early Years’ is used as guidance for the settings.
8. The draft care standards for Early Years are in development by DHSSPS, although they are already being used as good practice. They include significant reference to the need for settings to show that ‘good health of children is promoted and safeguarded’ and the specified indicators of this are that the food should be healthy.
9. A further standard denotes that ‘Children are provided regularly with adequate quantities of food and drink, which is of good quality and in line with healthy eating and oral health guidelines’. It is an essential criterion that settings should demonstrate their compliance with the Health Promotion Agency’s ‘Healthy Eating-Nutritional Guidelines for Early Years settings’.
10. Sure Start also offers many programmes extolling the virtues of healthy eating to parents and young children, an example being the Cook it programme and the Family Health programmes offered to families in Sure Start catchment areas.
11. Physical activity and play are an integral element of development in the early years and fundamental to a healthy and happy childhood.
Schools
Food in Schools
12. Since 2002 DE has been working to implement New Nutritional Standards for School Meals, as a key ‘Investing for Health’ goal for Departments was to tackle the problem of obesity.
13. In September 2005 additional funding, rising to £3.2 million in 2008/2009, was made available to improve school meals in the north of Ireland. The funding is being provided to increase the food content value of schools meals to a minimum of 50p in nursery, primary and special schools and 60p in post primary schools. The implementation of these standards has been supported by a cross-departmental School Meals Nutritional Standards Steering Group.
14. Good progress has been made to improve food in schools with the completion from September 2007 of the New Nutritional Standards Initiative across schools in all Board areas. The Education and Library Boards (ELBs) have also recruited Nutritional Coordinators whose responsibility is to develop staff training programmes and to ensure the implementation of the new food-based standards. The coordinators also ensure that staff within schools receive appropriate training and that this is accredited where possible.
15. Since 2006/07 the Education and Training Inspectorate (ETI) have been examining schools’ general approaches to promoting healthy eating. Two Nutritional Associates have been recruited to work with ETI in a sample of inspections to evaluate the nutritional quality of school meals and wider healthy eating programmes.
16. DE is also working with DHSSPS to use initiatives developed by the health sector to contribute effectively to the continued delivery of the new food in schools standards and associated objectives. To date they have carried out 217 inspections and found that most schools are making good or very good progress towards meeting the nutritional standards and the general approaches to promoting healthy eating. In some schools this practice is outstanding.
17. There is evidence that if we are to encourage children and young people regularly to consume healthier options, there must be a whole school approach. Work is already well underway to deliver this approach to schools in the north of Ireland. It has been proposed that the New Nutritional Standards initiative be extended to include all sources of food in schools such as tuck shops and vending machines. DE consulted on the issue of providing only healthy choices in these areas, and received agreement from consultees that vending etc, should be included in the standards. The proposal was discussed and supported by the Assembly’s Education Committee in November 2008.
The Revised Curriculum
18. The revised curriculum includes a Personal Development and Mutual Understanding strand for primary pupils and a Learning for Life and Work strand for post-primary pupils which allow pupils to explore issues such as the benefits of healthy eating and physical activity, the consequences of poor dietary choices, ways of achieving a healthy diet, the influences on their physical and emotional health and ways of developing their self-esteem.
19. The flexibility of the revised curriculum allows for links to be made between curriculum areas such as supporting healthy living through, for example, Home Economics, a statutory requirement at Key Stage 3 which should provide pupils with opportunities to explore ways to achieve a healthy diet in terms of food and Personal Development which should provide opportunities to address obesity.
20. Physical Education (PE) is a compulsory part of the statutory revised curriculum for all pupils in Years 1-12. While it is a matter for schools to determine how much time is devoted to PE, DE guidance recommends they provide at least two hours per week.
Primary Sports Programme
21. In November 2007, the Minister for Education launched the Curriculum Sports Programme for primary schools, the aim of which is to develop the physical literacy skills of our youngest pupils, raise pupils’ confidence, self-esteem and motivation to learn, and support a healthy lifestyle by encouraging ongoing participation in physical activity.
22. School participation in the programme is voluntary with priority given to schools whose pupils would benefit most from the opportunity to take part in curriculum-linked physical activity.
23. A total of some 60 coaches from the GAA and the IFA have been working in schools and to date nearly 550 primary schools have benefitted from the Programme.
Active Schools
24. In response to the Fit Futures report, DE has committed to working with DHSSPS and DCAL to establish an active schools partnership to develop plans to deliver an increase in levels of physical education and after school sport and physical activity.
25. The active schools programme flowing from this should support schools to access opportunities for quality physical activity, including active play, active travel, physical education and sport during and after school and to make linkages with facilities, groups and clubs in the community that encourage and support physical activity.
Extended Schools Policy
26. In 2006, DE launched its Extended Schools (ES) policy. The health and well being of children and young people is at the heart of the extended schools programme and it has much in common with the health promoting school. They share common objectives in relation to health, safety and children’s development as well as the recognition of the importance of involving parents and the wider community in the work of the school and in particular in areas of disadvantage. There are currently around 450 schools that receive funding under the ES policy. From the 2007/08 reports submitted by schools participating in the ES programme 87% have programmes in place that contribute towards making their school a healthy school.
27. Some £10 million was been earmarked to support ES activities at the most deprived and disadvantaged schools for each of the 06/07, 07/08 and 08/09 financial years. ES can be hubs of their local community offering a range of programmes before, during and beyond the traditional school day including fostering the health, well-being and social inclusion of children and young people.
28. An increasing number of schools have developed, with the support of partner organizations, wider food in schools initiatives such as breakfast clubs and cooking clubs. The ES programme provides opportunities to further develop such initiatives. DE recognises the importance of ensuring that such initiatives contribute effectively to the delivery of food in schools objectives.
29. Sport and leisure activities are specifically identified as being services in which schools can invest funding provided through the ES programme. It is anticipated that the programme will therefore contribute to increasing levels of physical activity within those ES who have identified a need in this area.
The Travelwise Safer Routes to Schools (SRS) initiative
30. The Travelwise Safer Routes to Schools (SRS) initiative was launched in April 2007 and ended in September 2008. It was led by the Department for Regional Development (DRD) in partnership with the DE. The initiative aimed to tackle the school run by encouraging young people to walk, cycle and use public transport in their journey to and from school. DE was responsible for any necessary infrastructure within school grounds such as cycle shelters, cycle paths and lockers. DRD Roads Service was responsible for the provision of any infrastructure improvements to the highway such as traffic calming measures and cycle lanes. The scheme was managed by SUSTRANS and 18 primary schools in rural areas took part.
Youth Service
31. Youth work plays an important role in encouraging children and young people to live a healthy lifestyle.
32. Through the delivery of the Youth Work Curriculum, youth workers adopt a holistic approach to matters relating to the health and well-being of young people, focussing on a number of key areas including Self Esteem, Physical and Mental Health and Risky Behaviour. Youth workers aim to educate young people by imparting knowledge about key issues relating to their health and well being as well as helping them to develop the skills they need to act on that knowledge and lead more healthy lives.
33. Full time and part time staff within the youth service are provided with ongoing in-service training programmes which address a number of health related issues including obesity. Ongoing links with a range of specialist agencies such as the Health Promotion Agency help to inform and supplement this training. Though partnership arrangements with the Health and Social Care Trusts, further training is provided to better equip youth workers to support young people’s emotional and mental well being. These training programmes help to ensure that staff throughout the youth sector is well-equipped to support and advise young people to make healthy choices.
Departmental guidance
34. In youth clubs/units, the engagement with the young person is voluntary; they come to centres to enjoy themselves in a safe environment. Compliance with healthy eating policy is a matter for each club/unit. I wrote to all youth settings in 2008 encouraging them to provide a range of healthy options in terms of what’s on offer in tuck shops and vending machines etc. The youth service responded positively to this request.
35. Youth workers are also able to access further advice and guidance on healthy eating via the DE’s website, and also from the Education and Library Boards and the Health Promotion and Food Standards Agencies to support them in assisting young people with maintaining a healthy lifestyle through improved nutrition.
Health education programmes
36. Through the youth work curriculum, health education programmes dealing with issues such as obesity, drugs, alcohol and the benefits of exercise are provided for young people at youth clubs and organisations. Programmes in relation to diet, healthy eating and cooking are also provided, often in partnership with Health Trusts. These programmes enable young people to further develop their understanding of issues such as healthy eating, food hygiene and the importance and benefits of regular exercise. They promote a healthy attitude to food and eating and ensure that young people have the necessary knowledge and skills to choose and maintain a healthy diet.
Physical activity programmes
37. Youth clubs/units and outdoor education centres provide ongoing programmes which include physical activities such as sports, hill walking, orienteering and sailing. In this way, the youth service gives young people the opportunity to participate in healthy physical activity and to develop healthy pastimes and leisure pursuits. Coaching in a range of sporting activities is also available, which can further develop young people’s skills in their chosen sport and can help to encourage them to continue with that sport into adulthood. The youth service is responsible for the statutory outdoor education centres, these centres offer exemplars of best practice including involvement in healthy activities and the range of healthy meals they offer.
Additonal Information -
Department of Education
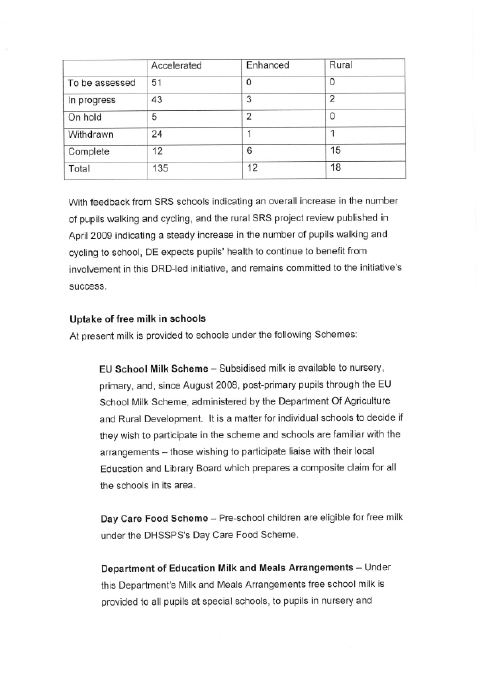
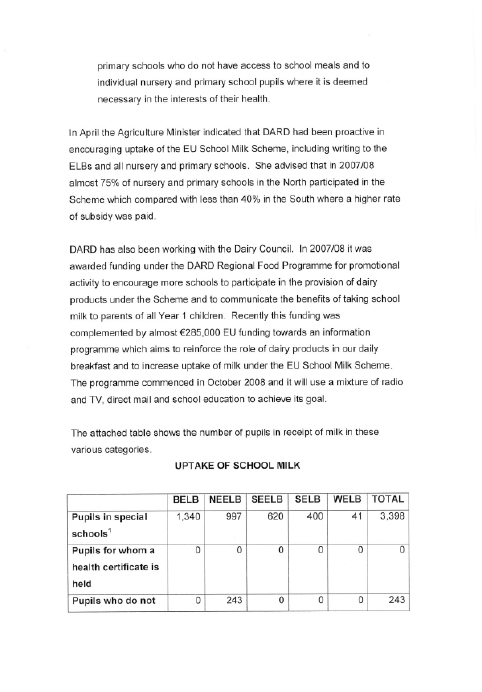
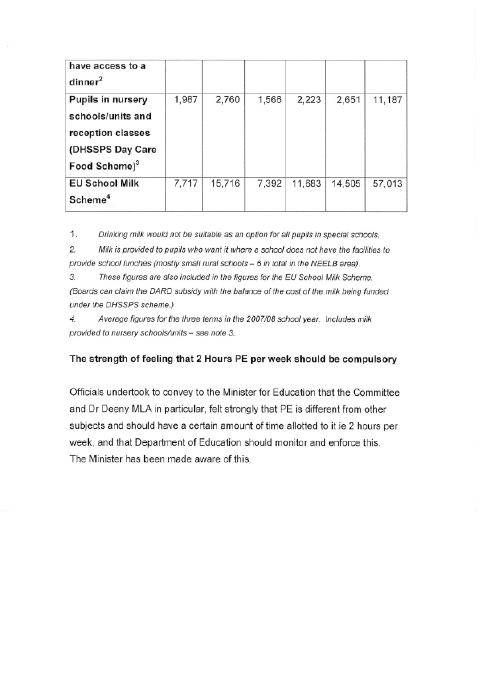
Further Submission from
the Department of Education
Summary Paper from Department of Education
The Committee has received the Department of Education’s response of 23 February 2009 to the Committee’s Inquiry into Obesity. The purpose of this short paper is to outline the current priorities in the Department of Education, the long established links between health and education and the Department’s approach to all aspects of health and wellbeing which, along with the more targeted initiatives, contribute to obesity prevention in children and young people.
The Department of Education’s vision is “to ensure that every learner fulfils his or her potential at each stage of development". In the period immediately ahead, the focus for this Department will be on the following key actions:
- Raising standards for all
- Closing the gap between the highest and lowest attainment
- Developing the Education workforce
- Improving the learning environment
- Transforming education administration
If children and young people are to be motivated by education, they must have access to a broad and balanced curriculum that has at its heart a clear focus on literacy and numeracy and that reflects their interests, is relevant to their needs and to the needs of society and our economy. Roll-out of the revised curriculum, will better prepare young people for all aspects of life and work and have a greater emphasis on developing the skills they need.
The key priority of the Department of Education is to raise educational standards for all young people, hence an emphasis on literacy and numeracy and academic excellence. Nevertheless, within the education sector we have long acknowledged the close links between health and education. In order to raise standards we need children to experience good levels of emotional and physical health & wellbeing in order to concentrate and learn. In short, healthy children learn better. By the same token, a good education can impact positively not only on a young person’s immediate and longer term job prospects and life chances, but also on their future health and that of their family.
Knowledge along with the personal and social skills provided through education can better equip children and adults to interpret and use information and services to maintain and improve their own health and make healthy lifestyle choices, thereby countering health risks such as obesity.
The Department acknowledges the important role it has in educating our children and young people about healthy lifestyles and choices which can impact on health issues such as obesity. The written evidence already supplied to the Committee outlines the steps taken so far by the Department of Education to meet the PSA target it shares with DHSS&PS and DCAL to help stop the rise in childhood obesity by 2010. It has participated enthusiastically in the Fit Futures Taskforce, of which the chairperson was a DE official. It has implemented many of the recommendations of the report, especially in the areas of Food in Schools, the revised curriculum, the Primary Sports Programme and Extended Schools. The Food in Schools policy which recently cleared the Executive, will issue in May 2009 for public consultation. Work is ongoing in both the schools and youth sectors.
The measures to counter obesity are not simply confined to the healthy eating and physical activity agenda. They go beyond that to look at personal development and emotional health and wellbeing, tackling real life issues like bullying and relationships with the aim of building self esteem and resilience. It is a whole child, whole school approach to counter social and personal impacts.
The promotion of pupils’ emotional health and wellbeing has been identified as a priority for action at Ministerial level. The Department began work in September 2007 in partnership with all key statutory, voluntary and community sector stakeholders and interested parties including the Department of Health, Social Services and Public Safety and the then Health Promotion Agency to develop a ‘Pupils’ Emotional Health and Wellbeing Programme’. Work is continuing with an aim to complete by Autumn 2009.
Since September 2007, professional counselling services have been available for young people in post primary schools. Research is underway to determine the need for, and audit of, counselling and other therapeutic interventions so as to begin extending appropriate support into the primary and special sectors.
Schools facilitate many initiatives eg health assessment and weighing and measuring programmes and the Department works with DHSSPS on a range of strategies which impact on the health of young people.
The Southern Health
and Social Care Trust
Introduction
One of the key goals within the Investing for Health strategy is to:
“stop the increase in the levels of obesity in men and women so that by 2010, the proportion of men who are obese is less than 17% and of women to less than 20%." (DHSSPS, 2002)
More specifically, the government target set out within Priorities for Action 2008/09 states that the rise in obesity should be halted by 2010.
According to figures from 2005, 28% of adult females and 27% of adult men in the Southern Area are obese, representing an increase since 1997. A key challenge in addressing this rise, and one of the corner stones to the success in doing so, is to continue to empower people in the community, particularly those most at risk of poor health and diet patterns, to eat more healthily, to take more regular exercise, and to provide an environment for healthy living in the home and in the community.
In seeking to meet this challenge head on, the Southern Health and Social Care Trust has developed a health improvement plan which sets out its key strategic direction and provides operational objectives for the prevention of obesity and the promotion of lifestyle change in its population. Implementation of this health improvement plan involves multi-disciplinary approaches to service development and delivery within the Trust, with engagement from the Promoting Wellbeing Team, Dietetics, Health Visiting, and Physiotherapy. This internal partnership approach is further developed across other sectors and settings to ensure that there is an integrated approach to the prevention of obesity across the Trust area.
2. Current approaches to the prevention of obesity and the promotion of lifestyle change in the Southern Trust area
The following is a summary of key activities and initiatives which have been implemented or supported by the Southern Trust over the last number of years to prevent obesity and promote lifestyle change.
2.1 Programmes which focus on nutrition for health
Community Cooking Skills
Building on the success of Cook It, a community nutrition education programme, which had run in the Southern Trust area 2004-2008, the Trust has developed a model for the delivery of a community cooking skills programme to incorporate a range of approaches to healthy eating and nutrition in the community and the home.
Between 2004 and 2008, the Cook It project team trained over 50 volunteers and professionals working within the community to provide over 70 six-week nutrition education programmes to community groups across all regions of the Trust, and particularly the most vulnerable, including school-aged mothers, Travellers, young people moving on to independent living and people with physical and learning disabilities.
In total, over 600 people participated directly in Cook It courses. It is further estimated that this represents a total number of beneficiaries in excess of 2000 people, many of whom are children and young people whose parents have participated in Cook It and have brought their learning and skills back into the home.
The newly developed ‘Community Cooking Skills’ programme will incorporate the Cook It methodology as one of a range of approaches to supporting those in the community, particularly those on a low income, to cook and eat more healthily on a budget. Other methods and resources which will support this overall approach include:
- Cooking Skills DVD – this resource will provide a step-by-step guide to cooking low income and nutritionally balanced meals to a range of community organizations and families throughout the area of the Southern Trust;
- Cooking Skills programmes and resources for parents including weaning recipes;
- Adaptation of resource materials and recipes to suit the needs of people with low literacy, those with a learning disability, Travellers and BME groups;
- Targeting of programmes to specific groups e.g. looked after children, foster carers, and people with mental health problems.
Promotion and Support of Breastfeeding
Breastfeeding is recognized as the healthiest start in life with health and wellbeing benefits for both mother and baby. The Southern Trust has committed to achieving UNICEF Baby Friendly status across the Trust area. A Trust breast feeding policy has been developed and a Baby Friendly Steering Group established with action plans in development.
Weaning with Family Meals
This easy-to-follow recipe booklet uses family foods and shows how they can be used and adapted for feeding infants. The “Weaning with Family Meals" recipe booklet was also customized to the food preferences of the Portuguese community and has been translated into Portuguese and printed for use with families in the area.
Healthy Families Tool Kit
This resource, which was launched in December 2008, is aimed at supporting professional and community workers engaging with families to help them to adopt healthy eating and physical activity choices. The resource has been developed in line with the NICE Guidelines for prevention and management of Obesity. It comprises guiding principles on healthy eating, physical activity and behaviour change and practical resources for use with families to help them assess their activity and eating patterns and make changes. To date 34 professionals including health visitors and school nurses have been trained in the delivery of this resource and it is being integrated into family practice across the Southern Trust.
Nutrition in the Workplace toolkit
This toolkit provides a practical approach to healthy eating. In particular it focuses on the workplace as a setting to implement healthy eating guidance and practice.
It was developed jointly by Southern Trust, SHSSB and SIfH and is currently being distributed to workplaces throughout the Southern area. The resource recently won the British Dietetic Association’s Elizabeth Washington Award for 2008.
School Nutrition Action Groups (SNAG Toolkit)
A toolkit has been developed for schools that gives then practical advice and suggestion on how to set up and run a successful SNAG, as well as ideas on nutrition initiatives that they can implement within their own school. It is based on shared learning from the Big Lottery funded “Food in Schools" project which finished in March 2007.
Healthy Lunchbox Leaflets
This leaflet gives advice to children and parents on what to include in their lunchbox. 10,000 leaflets have been distributed to all schools within SHSCT.
Dig it and Eat it
Dig it and Eat it is a programme developed by the Conservation Volunteers NI to involve people in growing fruit and vegetables as a means of learning about food and nutrition and participating in physical activity. Investing for Health funding was secured to support the piloting of a Dig it and Eat it programme in 3 primary schools within the SHSCT area. Topics included an introduction to the Eat Well Plate, Healthy Lunch Boxes and the 5-a-day message including fruit tasting/smoothie making.
Health Promoting Homes programme
Health Promoting Homes is a programme focusing on tackling the obesity issue within the home setting and is run in South Armagh Sure Start. It consists of three modules run over six months - Personal Development, Nutrition, and Physical Activity. The Oral Health Dietitian facilitates two sessions at the end of the Nutrition module: - one session on nutrition & oral health and one session on children’s diets.
Training on “Nutrition matters for the early years" document
Dietitians have provided nutrition training sessions for child minders at pre-registration and post-registration courses and at Support Groups. This has proved very successful with very positive feedback.
2.2 Programmes which focus on Physical Activity for health
Walking for Health
Over 300 people throughout the Southern Area have been trained and supported to lead walks. Walking groups have been established across all localities and there are people from a broad range of age groups and abilities that participate in walks on a regular basis as a direct result of the support and infrastructure that has been developed and grown throughout the area.
Key outputs/outcomes to date
- An audit of registered and active walk leaders and groups has taken place – currently there are 250 walk leaders and 64 active walking groups participating in the network.
- A total of 6 Volunteer Walk Leader Training programmes have taken place between April 2008 and February 2009. As a result 99 new walk leaders have been trained.
- An additional 4 VWL Trainers were identified and trained to deliver the Walk Leader programme.
- 3 new walk leader forums have been established in the Armagh/Dungannon, Craigavon/Banbridge and Newry/Mourne areas.
- A Southern Area Walking Group directory is currently being compiled and will be made available through partner websites.
- The 2009 Walk Leader Festival held in Parkanaur Manor House and Forest Park was attended by 90 people.
Southern Area Cycling for Health
The Cycling Leader initiative was started in 2007. The purpose of this initiative is to provide an opportunity for those who do not have access to bicycles to take part in guided cycles with trained leaders. A total of 30 bicycles were purchased and stored in secure units or ‘pods’ (10 in each) in Loughgall, Portadown and Newry, with the support of the local council. The initiative was officially launched in March 2008 at which point 22 leaders had been trained.
Key outputs/outcomes to date:
- 4 Additional Cycle Leader courses were held training a total of 22 cycle leaders from a range of statutory and community settings.
- A cycle leader register has been established and updated.
- Leaders and participants are all insured and insurance information will be produced for leaders and included within training materials and participant packs. This will be renewed on an annual basis.
- In 2008 a study was carried out investigating the potential to further develop the Cycle for Health scheme for children & young people. As a result of the recommendations 18 bicycles have been purchased for use with the 13-17 age groups. 6 bicycles will be placed held at each of the 3 sites
Community and Workplace Health Challenge
The workplace health challenge has centred on the “step-o-meter" challenge for the past 5 years and it is planned to hold another such event in the early spring of 2009. Opportunities for community health challenges are currently being explored in each of the localities across the Southern area.
Key outcomes/outputs to date:
- A community and workplace health challenge focusing on physical activity and healthy eating ran with 180 people/36 groups participating. Another is planned for May ‘09.
- A workplace challenge was held for staff in the Craigavon Area Hospital. A total of 30 people took part in 6 teams. It is envisaged that in 2009 these teams will feed into an area wide health challenge.
- The annual Step Challenge targeting workplaces, day centres and primary care is planned - it is expected that up 500 people (50 teams) will take part across the Trust area.
Staff Leisure Centre Schemes
The SHSCT Health and Wellbeing group is currently negotiating the roll out of this programme for all staff across the trust. Currently staff can access a scheme across all council areas except Newry and Mourne. This is a work in progress.
Health for U Programme for Migrant Workers
This multilingual/visual resource is currently being developed in partnership with the Ulster Cancer Foundation and will be piloted with 80 staff in Avondale Foods in March 2009.
Children’s Play Programmes
Key outputs/outcomes to date:
- A series of physical activity challenges with young people took place in the early summer of 2008. Over 150 young people from schools and youth groups across the area participated in competitions that were run on the Trim Trails facility in Loughgall Country Park.
- 60 young people participated in a fun “World Cup Football" in the summer of 2008. In addition to the sporting element of this initiative, participants also took part in workshops that addressed wider health issues such as healthy eating and smoking issues.
- 6 young adults from youth clubs across the Southern area are currently participating in a pilot training scheme on Street Dance leadership. This programme, run in partnership with SELB Youth Service, will develop the knowledge of participants on the benefits of physical activity and impart the skills needed to deliver a dance programme in their respective youth settings.
- Plans are currently underway to develop an OCN Level 2 Accredited Street Dance programme in partnership with the Maiden Voyage Dance Company. It is envisaged that the training will be piloted with a number of community, voluntary, education, health and council sites with the aim of increasing the opportunities for young people to participate in dance.
- 6 schools across the Southern Area have participated in playground training which was delivered by Playboard. This brings the number of schools that have taken part in this training to 12. An evaluation report on the impact of this training is currently being compiled.
- 2 Tops Activity tutors have been identified to support the delivery of Tops Activity within Rural Youth Clubs. Training was delivered to 24 youth workers representing 12 youth clubs with the aim of increasing physical activity levels through the provision of alternative activities and games. An evaluation is planned.
Older People, Disability and Care settings, including 50+
There continues to be a significant focus for supporting those who work with older people in a range of settings to undertake training and development to enhance their practice in the promotion of physical activity and movement with client groups.
Key outputs/outcomes to date:
- An evaluation and review is currently underway of the impact of training to date to support physical activity in older people and those with limited mobility.
- A database has been compiled of all those who have been trained to deliver the above programmes since 2004.
- A total of 4 Level 1 Chair-based exercise training programmes have taken place this year. As a result, 57 leaders from a range of settings are equipped with the skills and knowledge to deliver chair based activity sessions to over 1400 older people.
- 36 leaders have been trained in Creative Dance and Movement.
- 2 Boccia Leader training courses have been delivered creating an additional 22 leaders from a range of settings.
- 60 people representing 6 ‘50+ clubs’ across the southern area have participated in 50+ Clubs competition. An evaluation has been completed and further links with Age Concern Initiatives are being explored.
3. Availability of weight management or other intervention services to tackle obesity related ill health
A range of weight measurement programmes and other services are offered across the Southern Trust area by professionals including Dietitians, Health Visitors, School Nurses and Physiotherapists:
BMI Measurement
The Trust’s school nursing service is currently in its second year of Body Mass Index (BMI) measurement of all year 8 children in the Southern Trust. To date, 89% of pupils have had their weight recorded – early indications are that approximately 11% of children weighed are classed as obese.
In response to these findings, 5 weight management programmes will be delivered by the dietetic and school nursing service in the Southern Trust and, subject to a positive evaluation, these will be rolled out next year.
These programmes will be offered to children identified with a raised BMI. Following best practice, it will combine the key elements of family involvement, practical education in nutrition, increasing physical activity and behavioural change.
The planned programmes will embrace a proactive holistic multidisciplinary approach run by a Dietitian, school nurse and fitness instructors. Each child and parent will attend weekly sessions over a period of 8 weeks at a suitable community venue in each locality, each of which will include exercise, nutrition education and motivational interviewing/group work techniques for behaviour change.
School nurses also respond to individual requests for support for children and parents where obesity has been raised as a health issue.
Paediatric ‘Over to You’
‘Over to You’ is a healthy eating and exercise programme, based on group sessions run over 7 weeks for parents and children. It includes weekly exercise sessions followed by a nutrition activity which includes topics such as the Eat Well Plate, portion control, lunchboxes, snacks, a supermarket tour for the parents and dental health.
Exercise Referral
The exercise referral schemes offered throughout the Southern Area have been developed to provide physical activity for sedentary individuals to prevent or treat a range of health conditions known to be associated with physical inactivity. Within the Southern Area there are three models for physical activity referral which have been developed in response to local need, delivered in partnership with local councils and/or Trust staff.
Key outputs/outcomes to date:
- 4 key staff within local GP referral schemes received refresher training in exercise referral, ensuring that the skills and knowledge of staff are up to date and that the quality of the service can be maintained.
- 4 staff received training in Wright Foundation Exercise Referral Level 3 to support the developments of the scheme in their area.
- 5 key staff from the local Councils received training in Top Activity to support the delivery of a range pf alternative activities targeted at children and young identified as overweight and obese.
3. Further Action
The Trust is committed to monitoring the impact of the initiatives outlined above and to consolidate the strategic and operational partnerships that exist to ensure a cross-sectoral and multi-disciplinary approach to the issue of obesity prevention.
In addition, the Trust is actively pursuing the development of new schemes and approaches to obesity prevention and the promotion of healthy lifestyles:
REACH
The Trust has led the development of a partnership application to the Big Lottery Fund with a project known as Regenerating Environments and Communities’ Health (REACH).
The REACH project is aimed at:
- Building the capacity of harder to reach groups, to improve their physical health and well being.
- Increasing the use of urban and rural environment to improve health and wellbeing.
A key element of the REACH programme is the development of community lifestyle programmes.
Cross-Border Obesity Prevention and Management Programme
In association with CAWT (Co-operation and Working Together), the Southern Trust is a key participant in the development and delivery of a new cross-order obesity prevention programme.
Western Health and Social Care Trust
The Western Trust provides the following evidence for the Health Care Committee in relation to ‘Enquiry into Obesity’.
Obesity in both children and adults is an increasing problem and the Trust is committed to playing its part in tackling it. The Trust has convened a multi-agency partnership executive group, the Western Area Obesity Taskforce, under the umbrella of Fit Futures Strategy to give strategic direction to tackling the issue. It links with the regional obesity taskforce. Obesity is an agreed theme to be addressed in 2009/10, which is to include Fit Futures and the new Life Course strategy. Additional investment has been identified and action plans are being developed for implementation in 2009/10 onwards.
Scope of the Current Approach
The Western Trust leads on a large number of programmes and initiatives in partnership with a variety of other agencies. Appendix 1 gives an overview of the interventions delivered by the Trust in partnership with the community, voluntary and other statutory sectors, eg education. However the need still exists to ensure a more co-ordinated approach, assessing the impact of interventions at a local and regional level and a robust method of collection and analysis of information to ensure we are making a real difference to the health and wellbeing of the population.
Focused intervention from within the Trust’s Nutrition and Dietetics service supports a range of activities targeted towards specific patient groups e.g. people with coeliac disease or diabetes, cardiac and pulmonary rehabilitation groups. Other activities are targeted towards children e.g. mother and toddler groups, schools and summer schemes.
Funding for these initiatives however, is often short term and non-recurring. In order for evidence-based programmes to continue, further support is needed including mainstream/long term funding to allow successful, validated pilot programmes to be sustained and to promote life-long changes which are of benefit to people’s eating and lifestyle patterns. It is also important that opportunities are maximised for learning from other models for example “Food 4 Life" where evaluation demonstrates impact on the health and wellbeing both of targeted groups and the wider population.
Examine the Availability of Weight Management or Other Interventions to Tackle Obesity-related Ill-health.
The Trust is currently piloting a ‘Body Balance’ weight management programme in the primary care setting. This programme will be evaluated (in association with the University of Ulster) and if successful, the resource would then be available to roll out throughout the Trust area. The Trust is working with community groups and providing them with the training to enable them to deliver weight management programmes locally.
The Trust is also working with our main commissioner, the Western Board, to examine the possibility of commissioning a weight management programme to be delivered through pharmacies. The Nutrition and Dietetic Service will assist in the review of the suitability of this programme.
Throughout the Western Trust there is a clinical service available to obese patients. Work is ongoing on a regional basis to standardise access criteria and care pathways and it is anticipated that referrals will only be accepted for individuals with a Body Mass Index (BMI) >30. This highlights that a gap may exist for individuals who are overweight (ie BMI 25-30) and the Trust recognises they also have needs.
Appendix 1 also provides the detail of the interventions being led by the Trust’s Health Promotion Department.
Consider what Further Action is Required, taking account of the potential to learn from experience elsewhere.
With the new structures of the Obesity Taskforce at the DHSSPS, the associated sub-groups, and public pressure, there is an opportunity to maximise working in partnership to tackle obesity. This requires cross-departmental strategies involving health, education, transport, planning and local councils to make a real difference. The development of an action plan with key partners on obesity prevention and early management for children and adults at a regional level with direction for the implementation on a local basis across all areas is required to ensure quality and consistency of delivery.
The challenge for all parties working in prevention and management of obesity is how to provide sustained support and the likely impact this may have upon scarce resources. A strategic approach similar to that taken for smoking would be useful.
Physicians from across specialties including General Medicine, Endocrinology and Diabetology have highlighted the need to address the issue of obesity through a multidisciplinary approach, with clinics established to diagnose, treat and support patients with access to a regional bariatric service for specialist surgical intervention. Such interventions would include gastric banding or gastric bypass.
There is a need to challenge the public in relation to balancing their right to eat what they choose and their responsibility for their own obesity-related ill health. The mainstreaming of evidence based interventions such as models already successful in the UK and US (Food 4 Life) targeted on a regional basis would ensure quality assured implementation. Enabling change would involve the investment in a core number of programmes targeting the family approach to obesity prevention and management through various mediums with more community and voluntary involvement.
The Trust welcomes the opportunity to respond to the Health Committee’s inquiry into obesity and will continue to support the development and implementation of the approach to halt the rise in obesity.
Appendix 1
Under each of the following areas is a brief description of current work in the Western Trust led by the Health Promotion Department aiming to tackle the rise in obesity
BMI Measurement
- BMI measurement will continue to be offered to all children in year 8 by schools nursing and a pilot programme will be developed to support those children identified as being obese or at particular risk.
School and community Based Initiatives to Support Physical Activity, Healthy Eating, Self-esteem / Well-being
- Munch Box Challenge, which is a Healthy Lunch Box Initiative, aimed at improving nutrition and oral health in children within the school environment. At present it is running within 150 primary schools.
- Healthy Breaks initiative aims to promote healthy snacking habits in children from a young age.
- 321 Award Programme, a scheme for all pre school and all special schools throughout WHSCT which It aims to improve oral health and nutrition through the provision of tooth brushing programmes, schools based education and healthy snacks.
- The Healthy Habits Challenge aims to promote healthy lifestyles through the implementation of a fun 4 week challenge combining physical activity, oral health and nutrition. The toolkit is currently being developed and will be distributed to all 45-post primary schools in the WHSCT area. The programme is being discussed with school nurses with a view to it being rolled out with all year 8s in 09/10.
- The Healthy Walking Bus aims to promote the importance of a healthy, active lifestyle for primary school children. The health behaviours of the children taking part will be targeted in four ways to support a healthy lifestyle – walking to school to increase activity levels, practicing road safety messages, eating more fruit and vegetables and drinking more water, and taking care of their teeth. The toolkit is being developed and will be distributed to all 189 primary schools in WHSCT.
- Breakfast clubs which aim to encourage children to adopt healthier eating patterns and oral health habits through eating a healthy breakfast and brushing teeth before class.
- Bone Fun Day. This has been developed and implemented with post primary schools throughout the WHSCT for approximately five years. It aims to encourage young people to improve eating habits and physical activity levels to build healthy bones.
- Health Promoting School Award, This award aims to challenge nurseries, special schools, primary schools and post primary schools within the WHSCT to develop their full potential as health promoting settings. The award aims to encourage a whole school approach to lead healthier lifestyles involving teachers, parents, staff and pupils.
- Physical activity programmes including hip hop body shock delivered to local young people in their communities.
Resource Development
- Obesity leaflet which was produced by HPD to incorporate information on healthy diet and physical activity.
- Snack leaflet which was produced by HPD to incorporate information on healthy snacks.
- A closer look at the oral cavity. This resource has been developed for use with Year 8-10 in post primary schools and currently being piloted with six schools.
- The Catch Pack, a healthy eating resource has been distributed to all primary schools and special schools to assist in the delivery of consistent healthy eating information.
Delivery of Breastfeeding Strategy
- Breastfeeding policy/Leaflet. All mothers have the right to receive clear and impartial information to enable them to make a fully informed choice as to how they feed and care for their babies. The policy is for contact with parents, infants and young people. A leaflet has also been developed to be given to new mothers to assist in the continuation of breastfeeding.
- Breastfeeding Education pack for Post Primary Schools. This resource aims to raise awareness of breastfeeding among young teenagers and promote positive attitudes towards breastfeeding. The resource is in file format for use by teaching staff.
- Breastfeeding support group pocket cards to aid in the maintenance of breastfeeding rates.
- Breastfeeding awareness campaign yearly to raise awareness of breastfeeding within the WHSCT.
- Breastfeeding newsletter as part of communication strategy.
Support for full range of Professions in Tackling Obesity
- Community Health Educatiors training, This 2 day training course aims to equip community workers with a health education role to effectively deliver consistent oral health and nutrition messages within their area or work.
- Promoting Oral Health Pack, a Tool kit for health visitors and health professionals working with children andthose with special needs. It aims to equip health professional to deliver consistent oral health and nutrition messages to parents and carers.
- Feeding Policy for the first five years. This policy, which is primarily for the use of health professionals, provides evidence-based information on healthy nutrition for pregnant women, infants, young children and the wider family.
- Food and Nutrition Policy/Leaflet. This policy provides guidelines on the provision of healthy food choices for staff, clients and patients. A leaflet has also been developed for use by staff, patients and clients.
- The Body balance weight management programme is a multi-component intervention that will be delivered by practice nurses on 2 pilot sites in the Trust area in 0910. The pack will target overweight/obese clients and patient outcomes will be compared to those of a control group who have received nutrition advice only from nurses. The proposal is currently being discussed with the Family practitioner services unit of WHSSB and the University of Ulster and dates for training all 150 nurses have been agreed.
- The Body balance weight management programme will furthermore be rolled out to pharmacies in an approach to ensure consistent message delivery of messages.
- Discussions are underway on the Healthy Towns concept in councils in the western area.
- GP exercise referral schemes. Three successful schemes running in the western area. In first 14months the Limavady scheme had 166 referrals to the scheme.
- Lifeskills initiative. A cross-cutting approach to develop a programme to help equip children and young people with the necessary skills to reach their full potential and make healthy choices. Evaluation of first phase complete.
Targeting Resources on Children with a disability and Children Leaving Care and Training, to Support Delivery of Evidence Based Initiatives
- Adult Training Centre oral health and nutrition programme which aims to improve awareness of oral health and healthy eating, facilitating a positive change in the attitudes and behaviour of staff working with adults with learning disabilities, who attend day care and adult training centres in the WHSCT area.
- Oral Health and Nutrition Training for carers in Nursing and Residential homes. The Health Promotion Department co-ordinates this training that is offered to care workers in all nursing and residential homes across the WHSCT Area. The training covers all aspects of the oral cavity in the older client and includes nutrition, dysphasia and dental hygine.
- Games for all targeting teachers and youth leaders to run physical activity sessions aimed at children with disabilities
Support for Community Food Team
- Delivery of Cook it! training to Trust staff and community and voluntary groups in a bid to improve skills and knowledge in health eating.
- Food Values. A programme supported by Safe food addresses shopping on a budget will be piloted this year in the west further roll-out and capacity building based on evaluations.
CAWT Obesity Initiative
- In addition a new cross border initiative funded by INTERREG IV facilitated by CAWT will be implemented in 2009/10 with a focus on obesity prevention and supporting those who are already obese. The work will be focused on obesity prevention targeting families and children with a management element for those children already overweight/obese.
Partnership Work with Western IFH Partnership
- Health Promoting Homes - delivers an innovative, integrated approach to tackling the rise of overweight and obesity. To date over 450 families have completed the programme, focussed within the Top 10% deprived communities in the WHSSB area. Plans are in place to develop sectoral approaches to the programme targeting specific population groups for example farmers and men. The programme includes 8-week modules on nutrition, physical activity and self-esteem.
- Active Families Programme - This programme is in process of development and will pilot over the 2008-2010 financial years. The programme is developing an accredited training programme which will take a role modelling approach within a family setting to tackling self-esteem and alcohol abuse through physical activity. The programme will be delivered in disadvantaged communities and to communities of interest.
- Play - The Play Strategies focus on developing creative and innovative ways to integrate play and physical activity within existing natural and built environments. Significant progress has been made with a number of the Councils, however progress remains to be made with the remaining Councils
- Food Poverty - Engagement with the Education and Library Board in the development of an educational resource (Field to Fork) enabling children to focus on healthy, nutritional food and learn about the Eatwell Plate. This resource has been rolled out across 194 Primary Schools in the Western area. Further work remains to bring this educational resource to Secondary School level and negotiations at a Regional level to mainstream across Northern Ireland.
NILGA
Introduction
NILGA, the Northern Ireland Local Government Association, is the representative body for district councils in Northern Ireland. NILGA represents and promotes the interests of local authorities and is supported by all the main political parties. Preventative healthcare is a key issue for local government due to the huge impact it can have on local communities and well-being. NILGA is pleased to be able to have an opportunity to comment on the Assembly Health Social Services and Public Safety Committee Inquiry into Obesity and we trust that our comments will be taken into account when developing an assembly position on the matter. For further information regarding this response, please contact Karen Smyth, Head of Policy at NILGA on (028) 9079 8972 or at k.smyth@nilga.org
Summary
This response is designed to show how local government is currently working to tackle obesity as an issue, and how it intends to take this work forward in the future. NILGA also makes recommendations as to practical measures which could be taken by service providers to improve work in this area. The integrated work of council environmental health, community and leisure services offices is currently providing demonstrable success at local level, and would indicate that a more joined-up approach to this issue will be key to a successful approach to tackling obesity. NILGA is aware that the Committee will have already received a myriad of examples of good practice from councils, so this response will concentrate on general principles, using brief examples where appropriate.
Current Work: General
Councils working on regional issues at local level
Local government is particularly well placed to tackle regional issues such as obesity, at a local level and to initiate projects that make a real difference to local communities. For example Belfast City Council has done work on healthy Chinese takeaway projects, Kids Gyms and the Choose n Move programme for Youth, and Ards Borough Council has engaged in ‘Healthy Lunchbox’ programme for children.
The best and most successful of these projects are often implemented in partnership with other agencies, such as the Education and Health Boards, providing a link to schools, the Fit Futures teams and Health promotion teams Councils have the role of ‘enabler’ in much of this work, and have a civic leadership duty to ensure their citizens maintain a healthy lifestyle.
Our councils have played a full role within the Investing for Health Partnerships, and there are a number of examples where councils have taken the lead on well-being eg in Newry and Mourne DC area, the council facilitation of the Wellbeing Action Partnership has been an exemplar of how a partnership approach can improve health.
CEHOG Nutrition Sub-group
The Northern Ireland Food Liaison Group - a subgroup of the Chief Environmental Health Officers Group is to convene a Nutrition subgroup to look at how best EHOs can become involved in tackling the obesity issue in the general population and also to share ideas and initiatives that may be happening elsewhere in NI and the rest of the UK, etc. This group will also membership from FSANI.
District Councils providing fitness opportunities
Councils are the foremost provider of leisure facilities in Northern Ireland and leisure services departments offer a wide range of physical activity programmes and facilities, targeting the entire community often on an age-related basis, and actively encouraging their citizens to engage in sport and physical activities. Newry and Mourne Council in particular, places emphasis on working with the disabled, a group which can be vulnerable to weight management issues.
Councils have worked in partnership with other agencies such as DOE and Sustrans to provide pleasant walking and cycling environments in urban and rural localities. Council led or sponsored sports activities such as the Milk Cup and the ‘Grassroots project’ have encouraged more involvement in football and other sports.
Councils are also keen to engage their staff in health promotion activities with many offering discounted or free access to fitness facilities and organising fitness challenges and sporting activities.
District Councils working with food businesses
In general Environmental Health Officers have been involved in promoting, for example, the FSA’s traffic light scheme with food manufacturers and are willing to work with FSA on other emerging initiatives such as their saturated fat and salt campaigns. Other projects of this nature include implementation of the Charterd Institute of Environmental Health Awards in “Healthier Food and Special Diets"
Post-RPA Working
NILGA would be of the view that there is a need for local government to grasp the opportunities presented by the health and social care reforms. There are vital roles for local councils as service provider, civic leader, partnership convenor, community focus and advocate on health issues.
The Lyons review identifies local government as a ‘place shaper’ alongside a need to take a wider view of health and well-being.
Councils will be taking up opportunities within the new joint working pilots and local government commissioning groups. Also, post-local government reform, community planning, the power of well-being and other powers will increase the ability of local government to influence the health of their local communities.
Local government is keen to think differently and innovate, focussing on the outcomes, not on who does what, and looks forward to working with the new Public Health Agency on issues related to obesity, both at regional and local level.
The new health structures will also see a greater role for local government through participation in the new Regional Agency for Public Health and Social Wellbeing (RAPHSW) and in local commissioning.
On 16 December 2008, Minister McGimpsey invited expressions of interest from District Councils on the possibility of hosting joint Regional Agency for Public Health and Social Well-being (RAPHSW) / Council pilots which would focus on addressing specific health and well-being inequalities. The Minister’s letter also indicated the possibility of co-locating health and social care staff with local government staff to support Councils in their future power of well-being and community planning role and inter- sectoral partnerships.
These staff could also assist in developing local health improvement plans, programmes and projects to reflect local community need (such as obesity) and would also support the Local Commissioning Group in developing commissioning plans which not only deal with health service provision but also measures to prevent ill health. These arrangements could be developed further and extended post 2011.
NILGA believes that councils are keen to participate in this pilot and sees this as a real opportunity for more effective joined up working including work on obesity.
Recommendations for the Future
NILGA would make the following recommendations with regard to taking work on Obesity forward:
1. A strong regional commitment is required on obesity, which needs to be adequately funded. As part of this, the Fit Futures report should be fully implemented.
2. A comprehensive, cross-cutting long-term NI strategy to tackle obesity should be drafted and implemented as soon as possible, bringing together all the major stakeholders.
3. A scoping exercise of existing good practice should be shared with all relevant agencies and central and local Government Departments.
4. Central Government should fund the roll-out of known successful initiatives such as the Cook It programme, and should develop a joined up approach at regional level to ensure consistent messages on healthy eating.
5. Cooking skills should be made a mandatory part of the School curriculum, and healthy choices available in all schools, with unhealthy choices kept to a minimum.
6. The FSANI should continue to work in partnership with the food industry and EHOs to improve nutritional quality of foods available for sale.
7. Healthy Eating awards should be available to food business operators in NI.
8. Social marketing tools should be used in a marketing campaign among parents of young children and the general population to increase awareness on health related issues caused by obesity.
9. Accessibility by young people to the ‘wrong’ foods should be addressed at a regional level involving a number of partners- especially the food industry
10. There must be adequate opportunities for young people to participate in physical activity both within the school setting and in the wider community
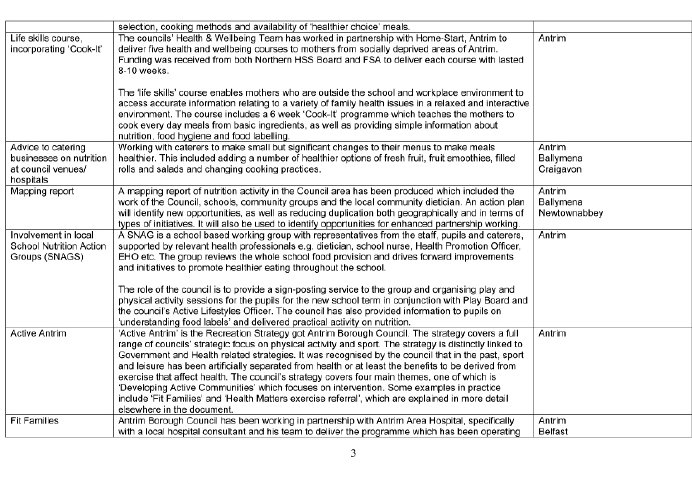
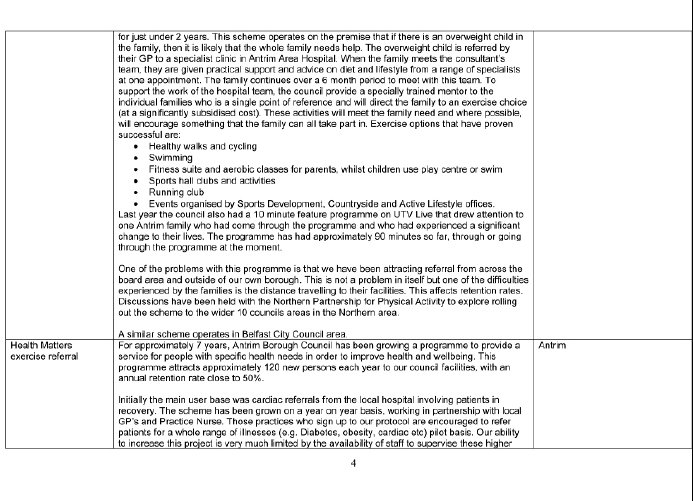
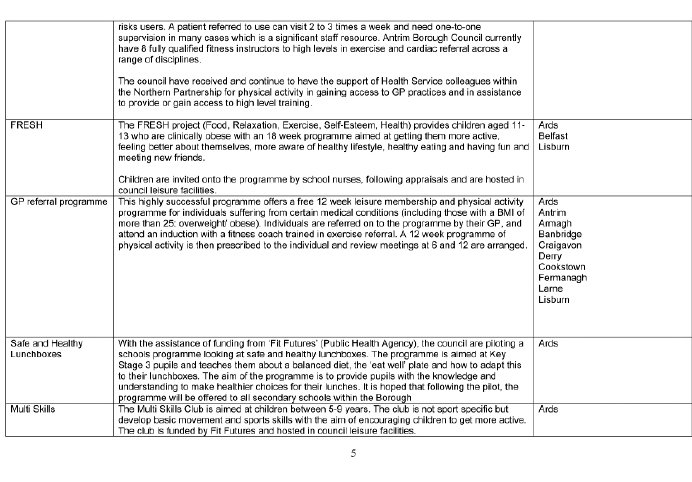
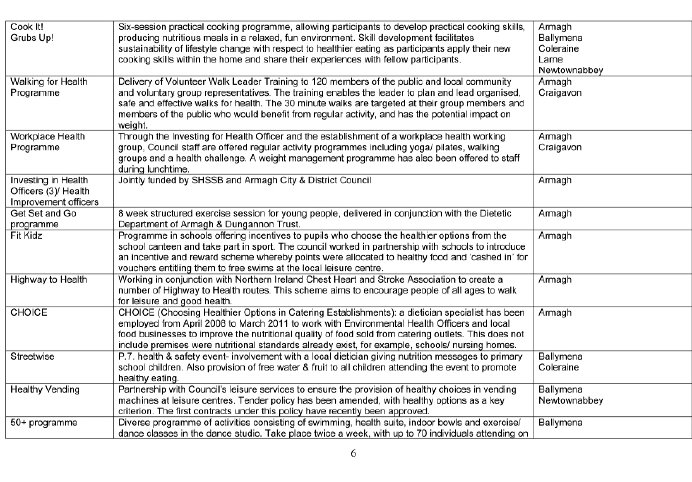
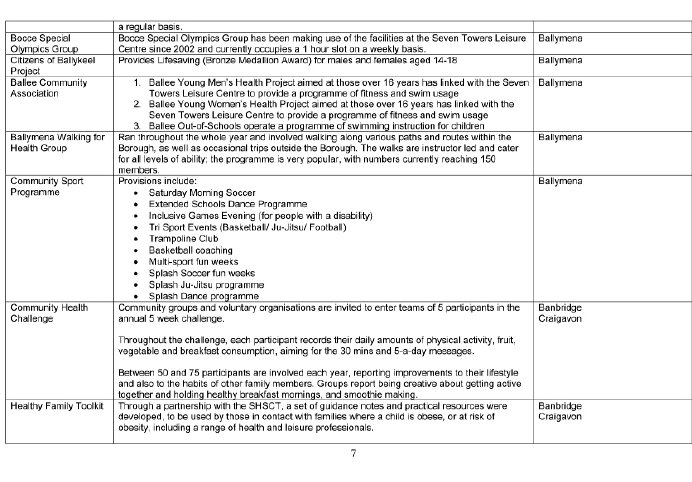
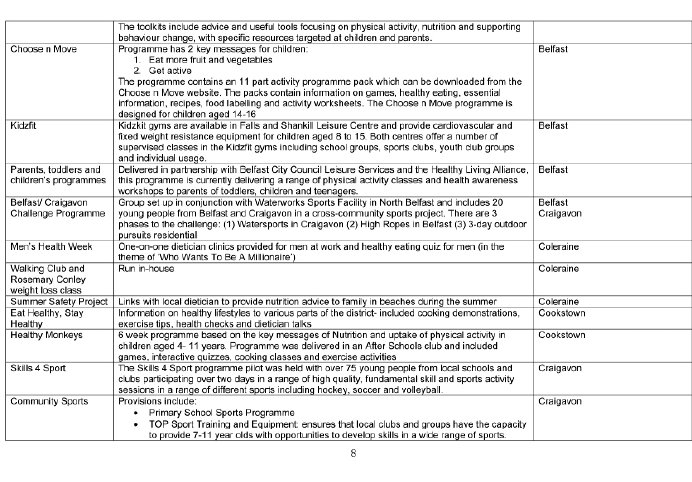
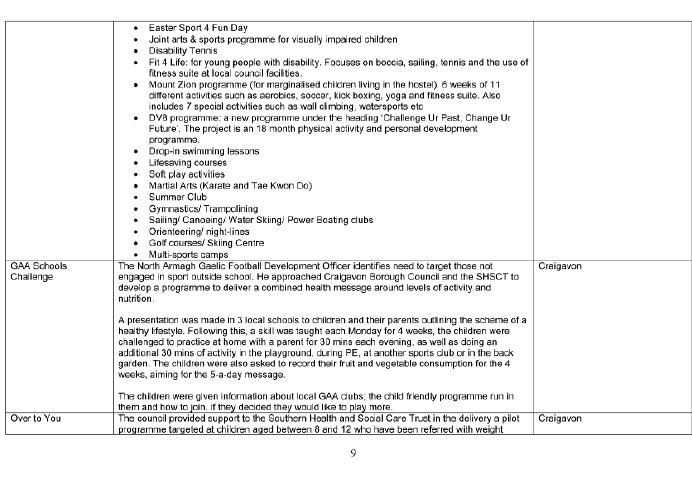
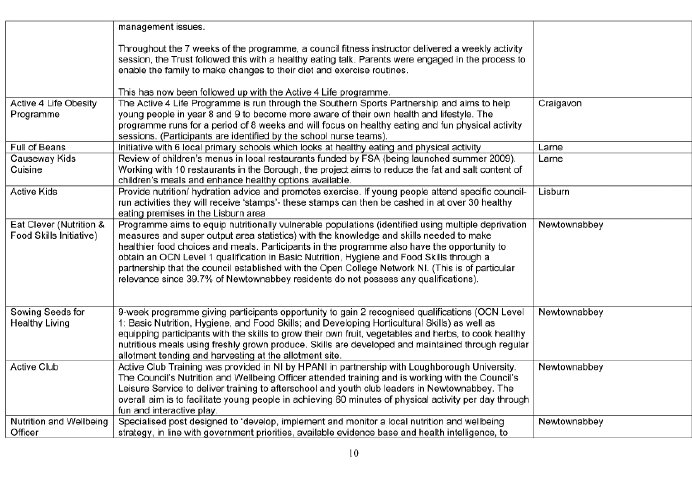
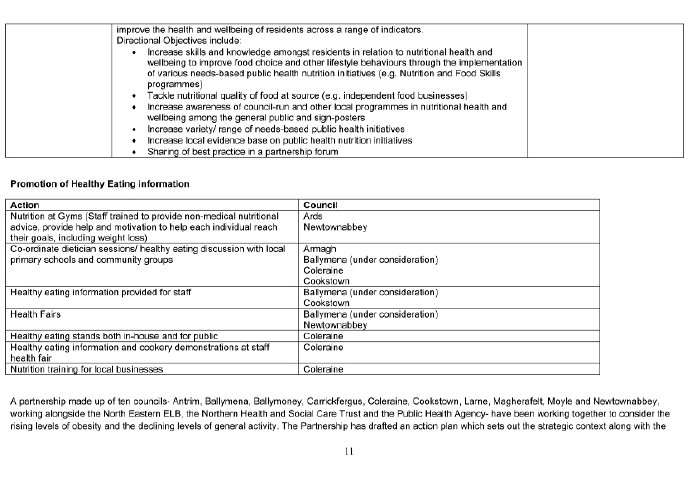
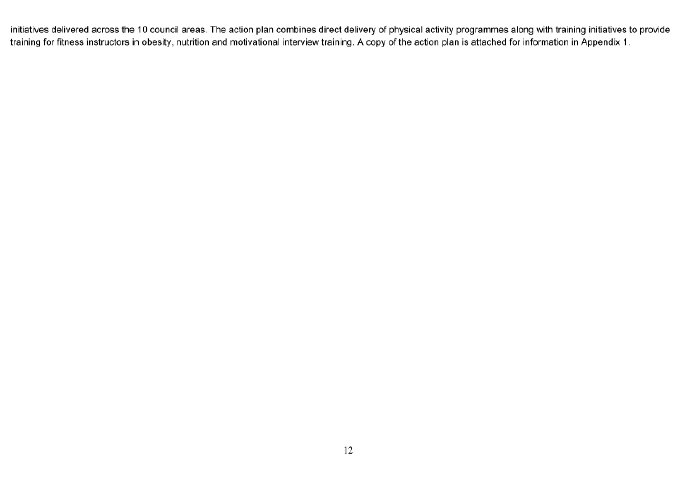
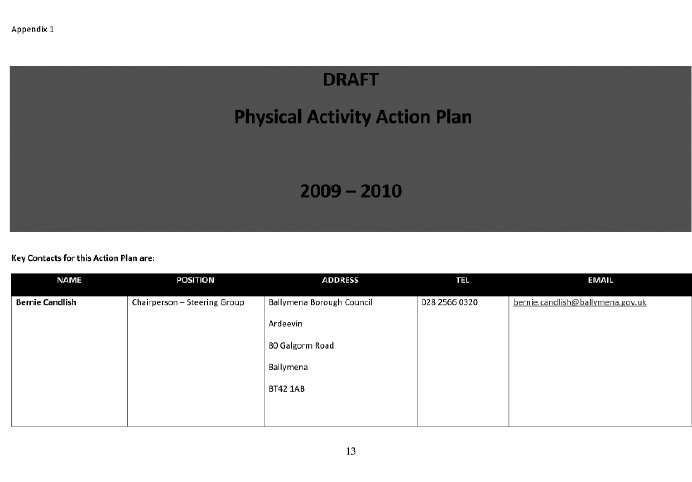
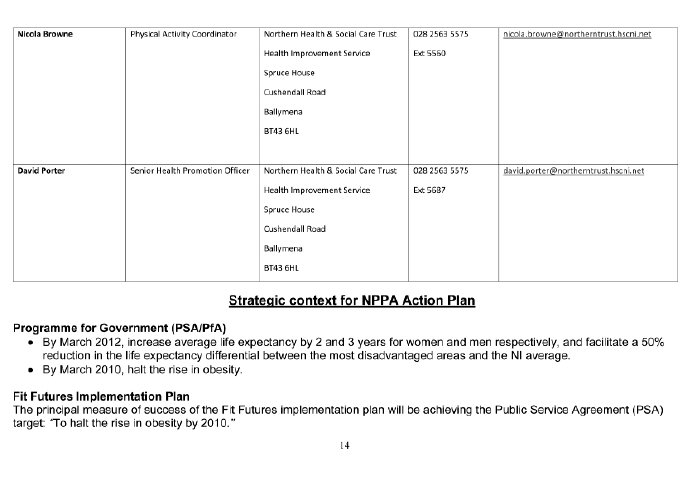
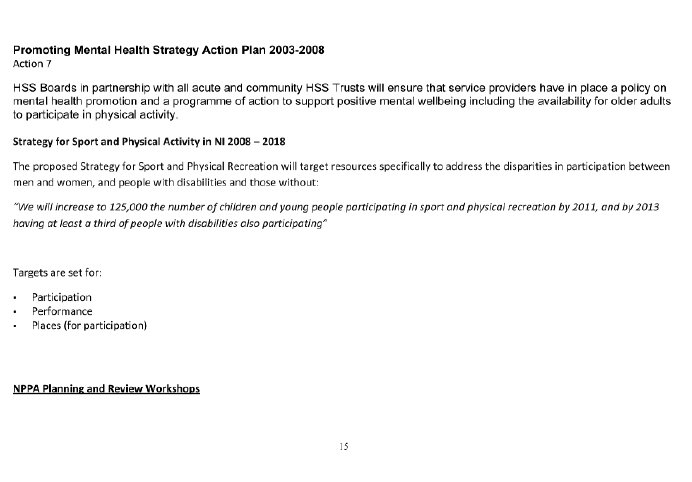
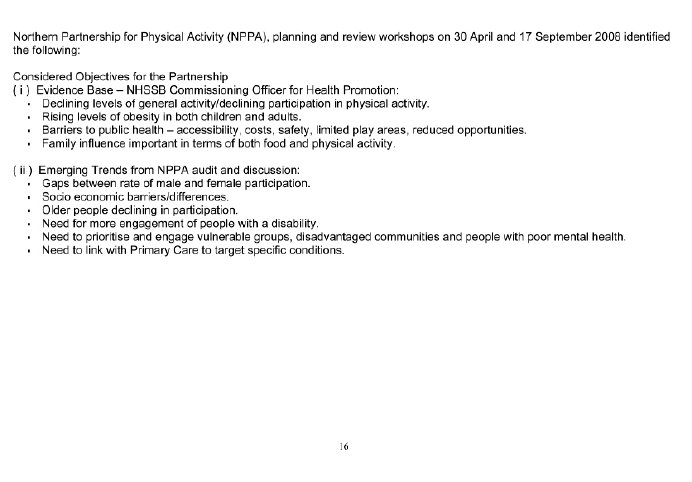
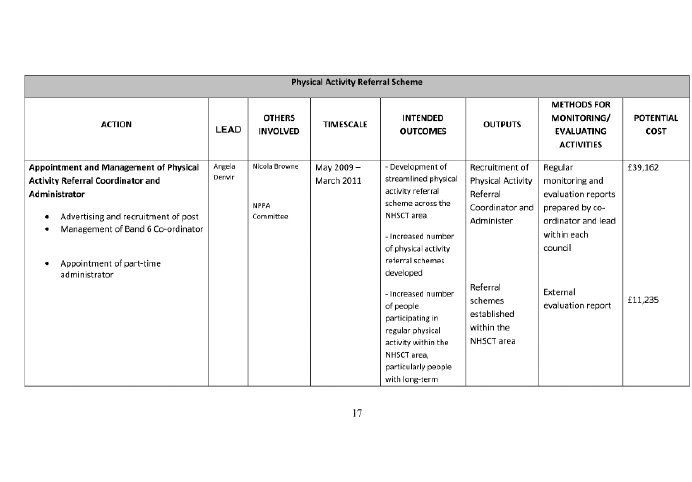
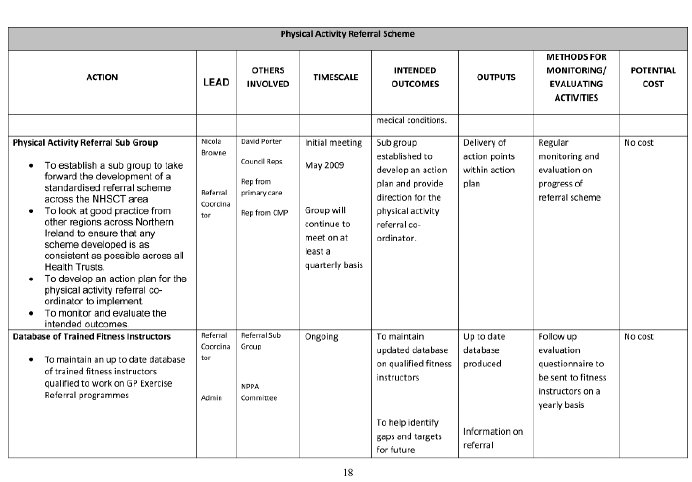
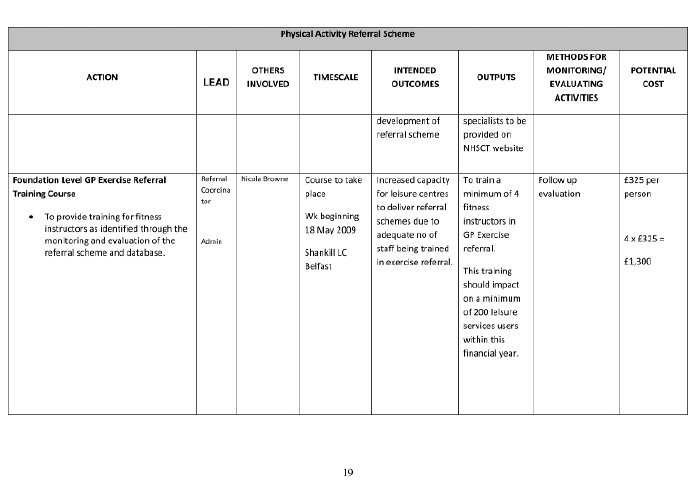
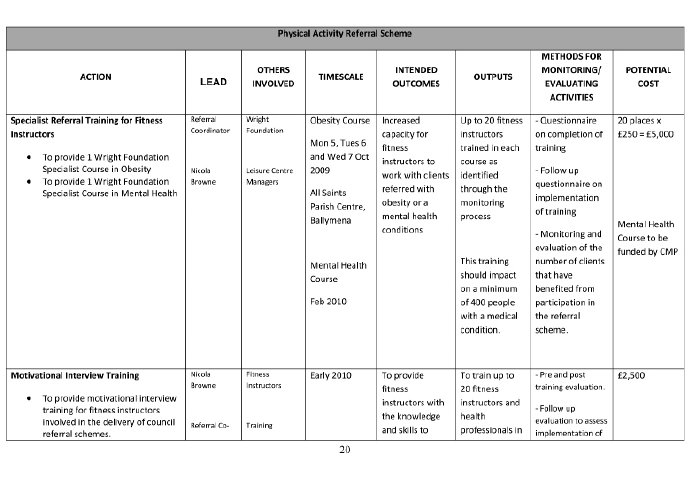
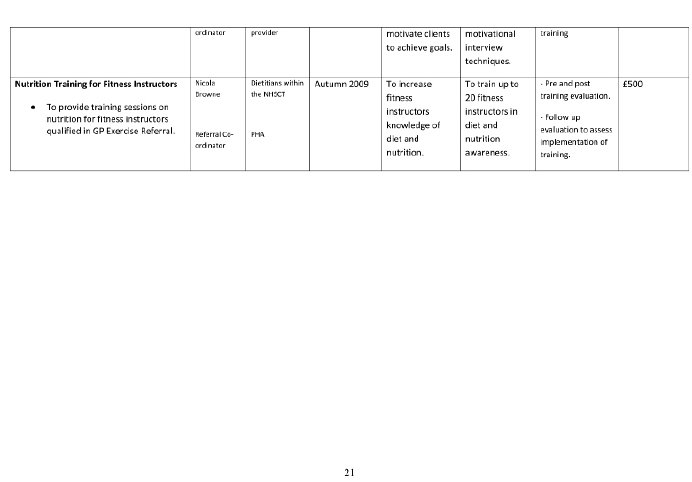
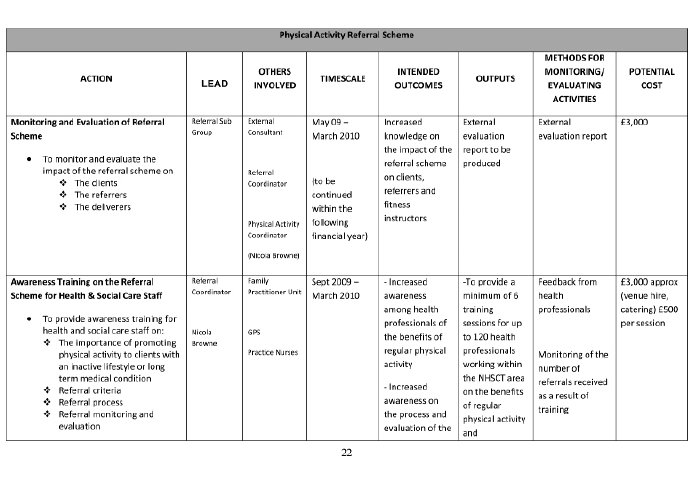
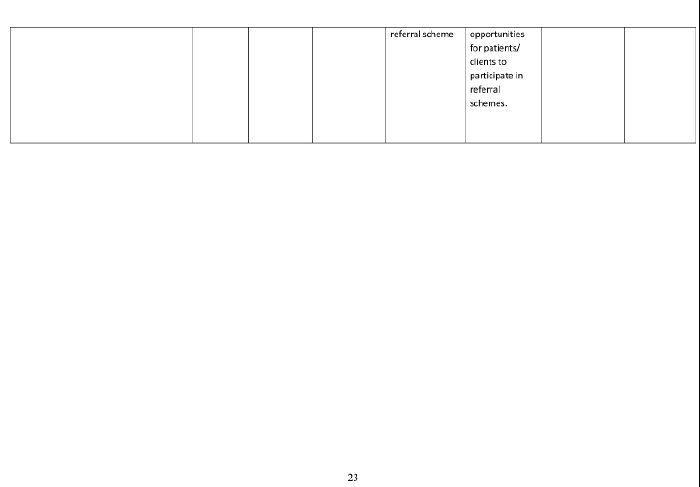
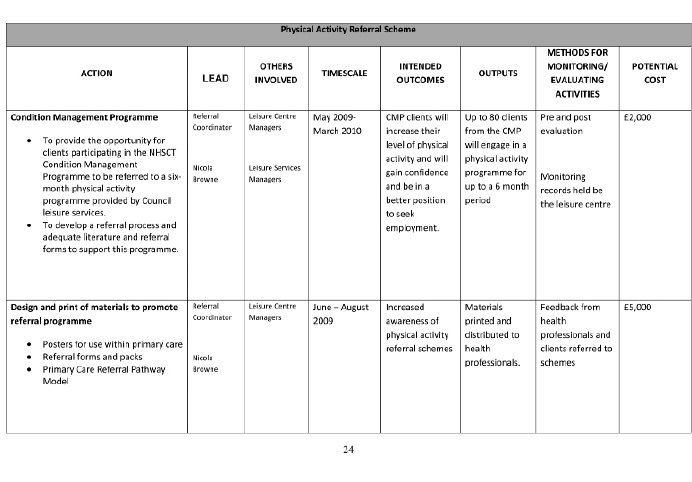
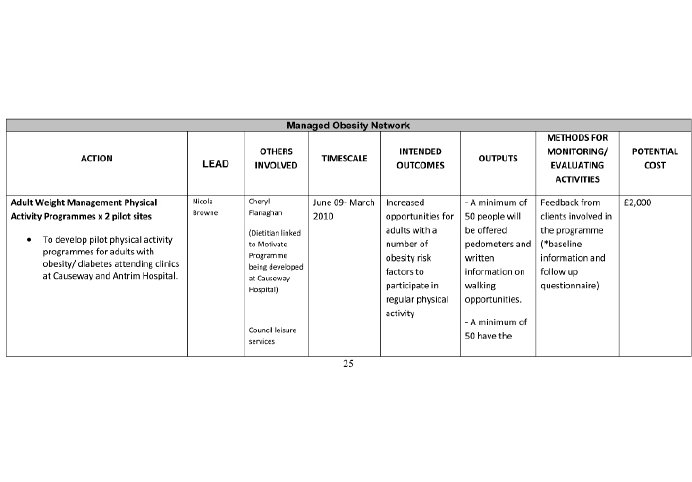
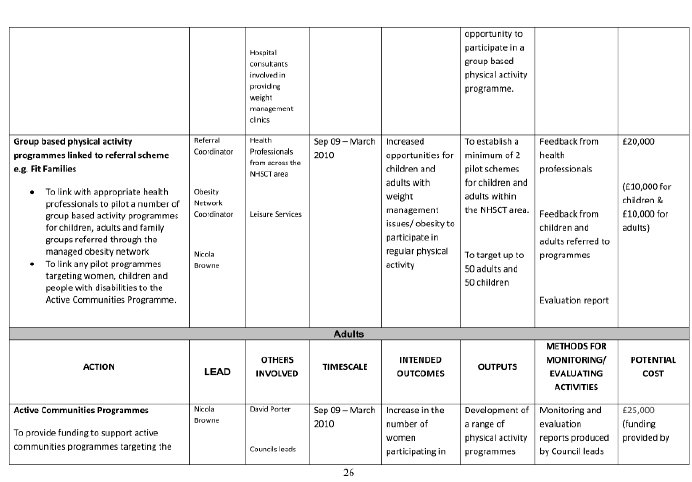
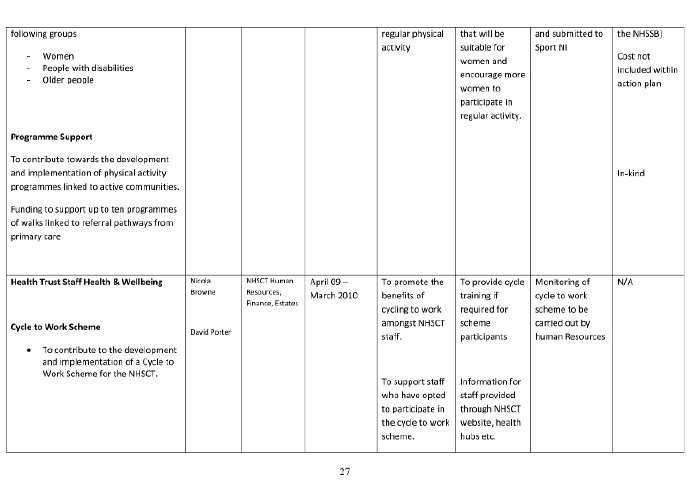
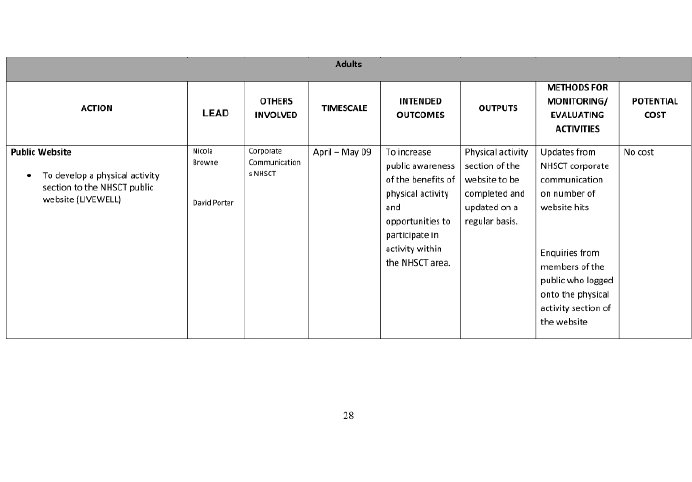
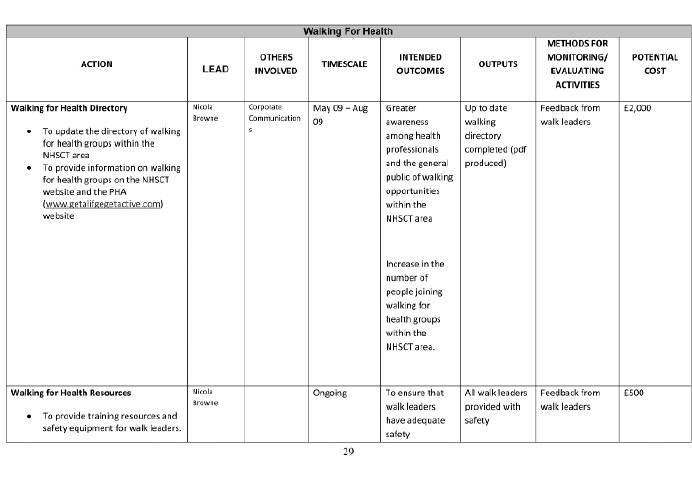
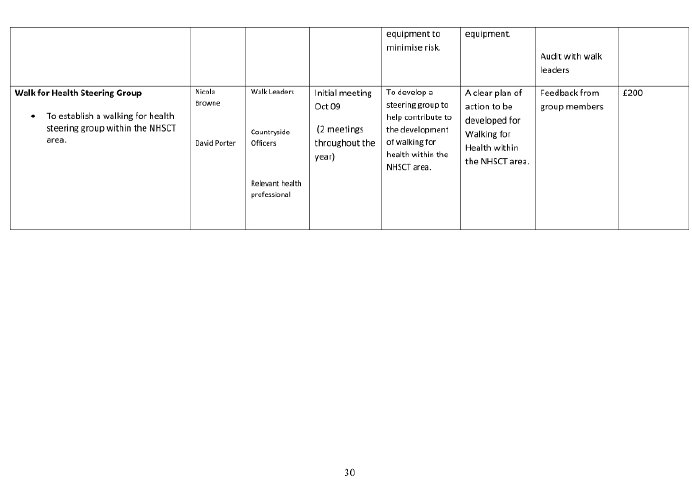
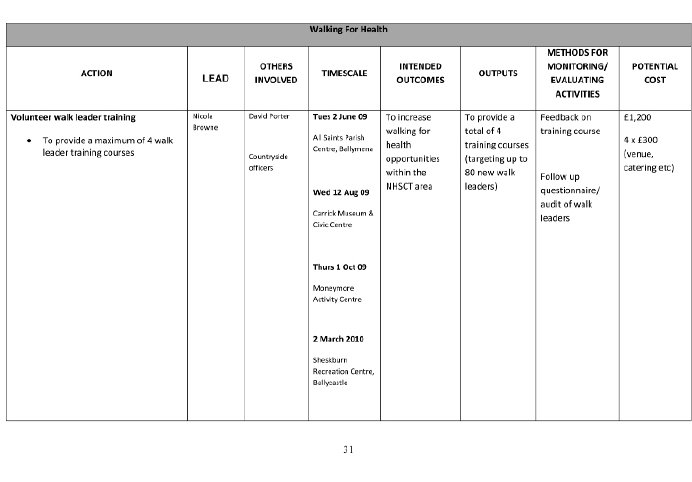
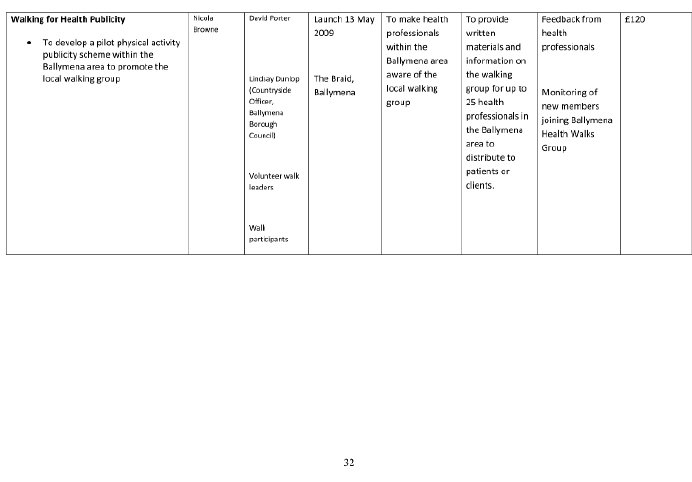
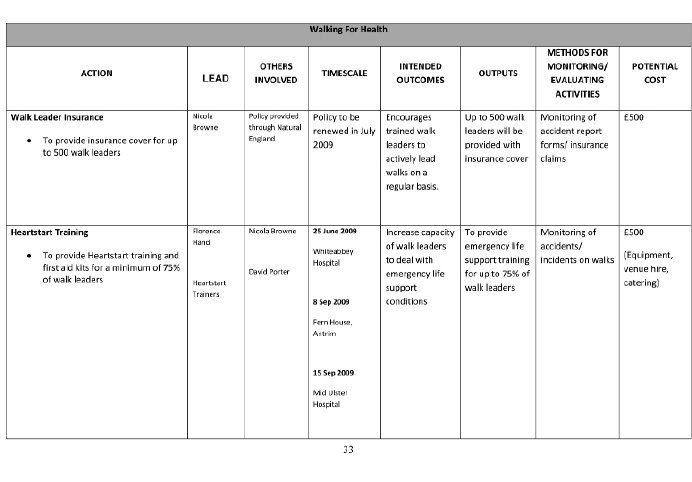
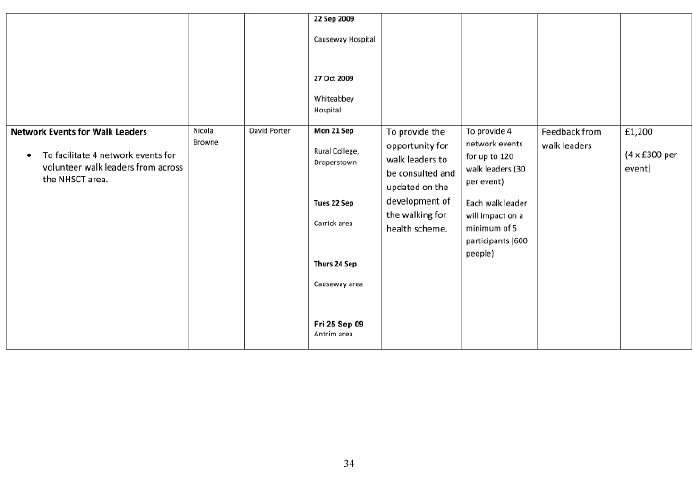
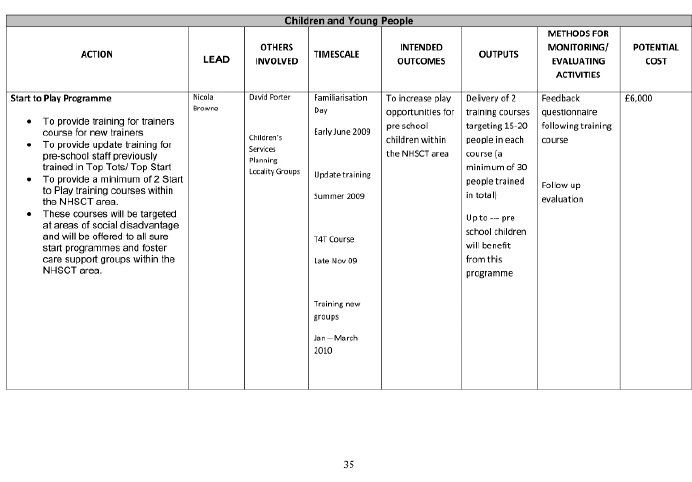
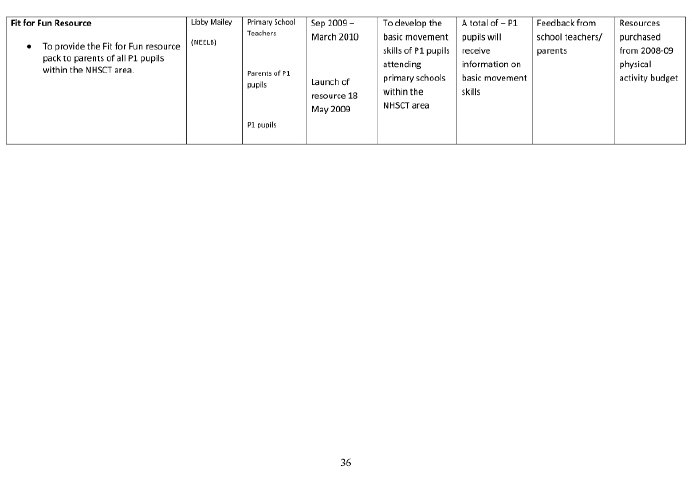

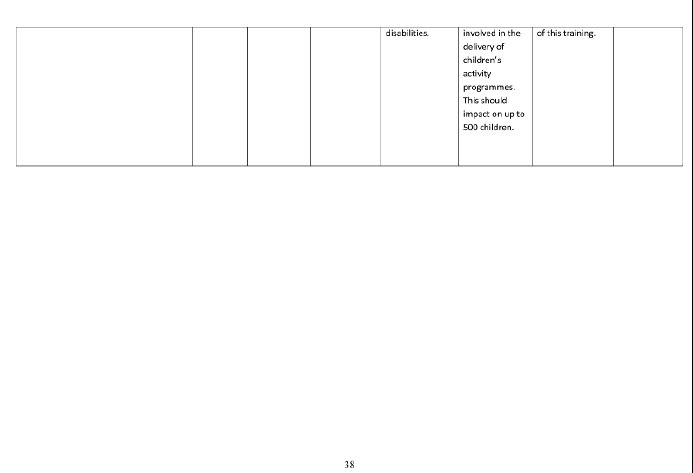
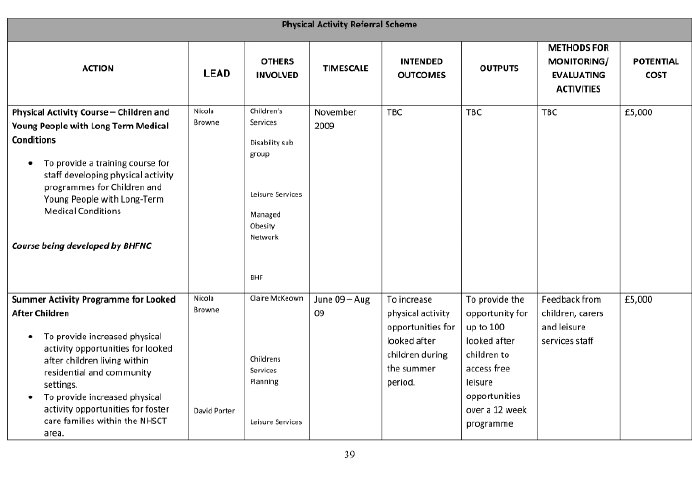
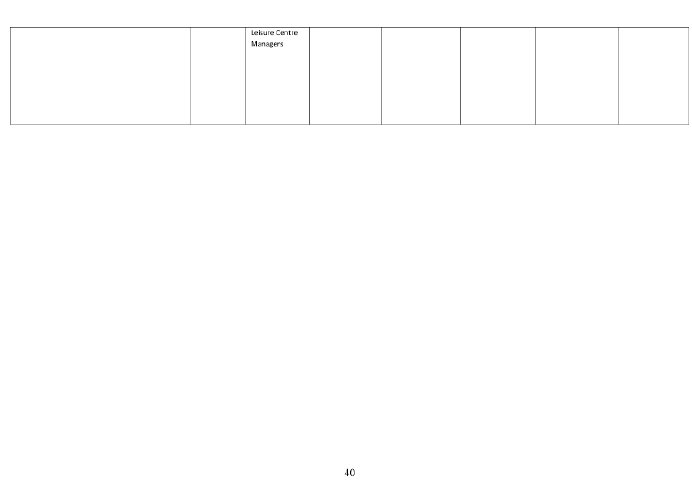
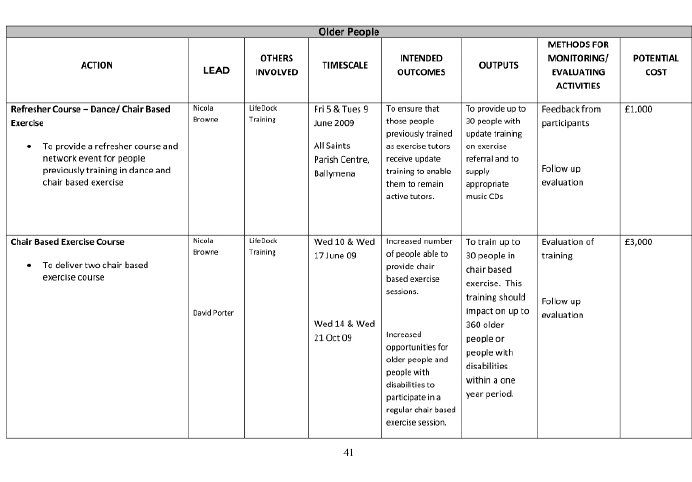
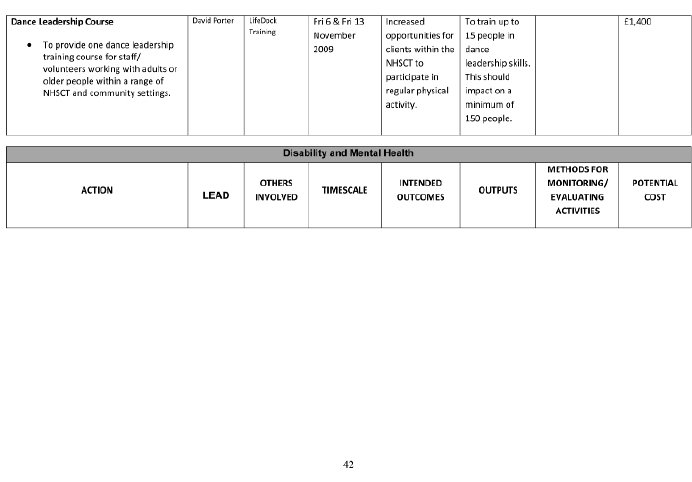
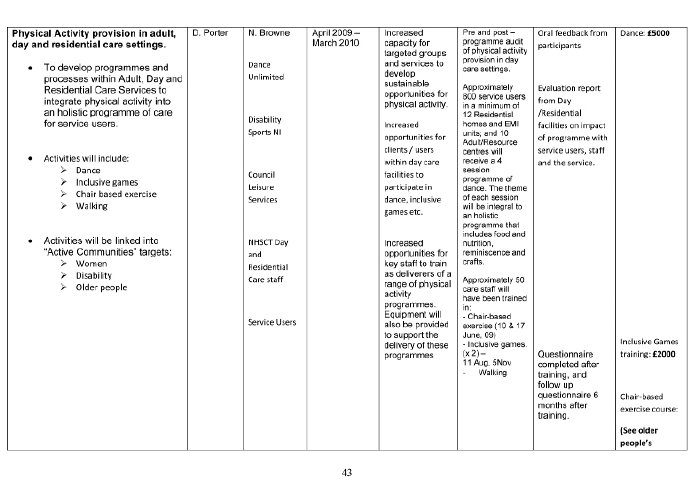
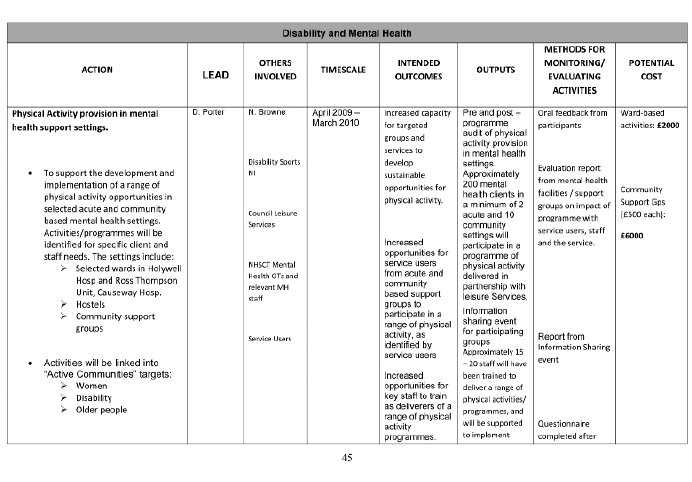
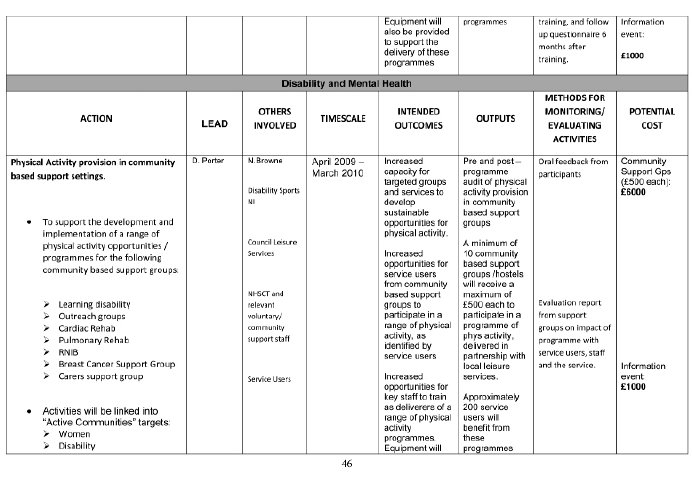
Queen’s University Belfast
Obesity is now a major problem for society and tackling its impact at the earliest stage, both in prevention, education and treatment, is very important. Within the School of Medicine, Dentistry and Biomedical Sciences we have recently begun new initiatives related to tackling the issues of Obesity from both an educational and research point of view. I will outline these programmes under the headings of Education and Research programmes below:
Education programme
Education in regards to Obesity has been incorporated and recently revamped throughout the undergraduate medical curriculum. The topic is embedded throughout the educational programme across Years 1-5 and is addressed as appropriate during both systems-based teaching and clinical teaching.
During Years 1 and 2 students follow an integrated systems-based course, the main focus of which is the study of the normal structure and function of the human body, learning about metabolism and physiology. The education around Obesity is delivered in the context of normal nutritional and dietary requirements. The topics covered include physiological principles underpinning normal metabolic controls and the factors that determine energy requirements. Other topics include genetically inherited conditions resulting in obesity, energy intake and expenditure and the calorific value of various foods and consequences of under- and over-eating.
The students are taught the importance of body mass index (BMI) and also learn how to measure BMI and other anthropometrical indices. Within the Epidemiology and Public Health components of the course we explore the recent increasing prevalence of Obesity in the population and the changes in illness patterns including the increased incidence of diabetes and other illnesses that are associated with this disease. As part of these educational programmes we also look at issues related to the overall societal impact of Obesity and the cost implications. Within the Behavioural Sciences element of the curriculum we focus on the current trends and behaviours in relationship to eating and exercise patterns. The importance of addressing unhealthy dietary lifestyle choices from the perspective of the individual rather than at a population level is particularly emphasised. Nevertheless, we begin with the overall population dynamic of these lifestyle choices. As part of this, students are also introduced to the psychological and social factors determining food preferences and choices. Throughout Years 1 and 2 students are referred to the following publications on Obesity:
- The Nation’s Health 34 (9), 2004. American Public Health Association
- Royal College of Physicians of London. Storing up Problems. The medical case for a slimmer Nation. Report of a Working Party 2004.
- National Taskforce on Obesity. Department of Health and Children, Republic of Ireland 2004.
- Department of Health. Annual report of the Chief Medical Officer 2002, London.
During educational Years 3, 4 and 5 the curriculum focuses primarily on the acquisition of clinical skills and the application of scientific knowledge to clinical practice. The educational programmes during this part of the course are again integrated throughout the programme. During medical rotations students learn about the impact of obesity on the clinical incidence and management of diabetes and other inherited and non-inherited metabolic disorders. The relationship between coronary heart disease and cardiovascular illnesses, stroke, etc. are all addressed during this programme. During clinical rotation students learn about the health complications associated with Obesity, including surgical complications, extended hospital admissions and longer recovery times following procedures. The management of fertility problems associated with Obesity are also covered during the Obstetrics and Gynaecology course as well as the association between some gynaecological problems, for example, polycystic ovary syndrome and obesity.
During the Paediatrics course we focus on the increasing incidence of childhood obesity and the childhood epidemic of diabetes and explore the social and cultural factors underpinning this. Genetic factors linked to obesity are also addressed and again students learn about the importance of measuring BMI and other indices of body weight in children. As part of the General Practice course students have an opportunity to revisit the issue of Obesity in the context of the general population and the role of Health Promotion programmes in influencing behaviour change in society. Various models of behaviour change are also explored. During 2nd and 3rd Year there are a number of Student Selected Components such as “Childhood Obesity. Understanding and Managing a Growing Problem" which includes an overview of recent relevant research on Obesity; Genetic and Lifestyle Factors contributing to childhood obesity; Diabetes – Type 1 in Childhood; and Nutrition in Society.
Therefore, as you will see from this brief outline, the overall topic of Obesity and its impact both at an individual and societal level, is covered very comprehensively in the undergraduate medical curriculum.
Research
Given the major, recent epidemic in both Obesity and Childhood Diabetes, the area of Nutrition and Public Health has become a major focus for the School of Medicine, Dentistry and Biomedical Sciences. As part of this new School, one of the new Research Centres that has been developed is the Centre for Public Health at Queen’s University Belfast under the leadership of Professor Ian Young. The Centre houses a number of very important research programmes, including the Centre for Excellence for Public Health which focuses on Nutrition and Physical Activity, and is one of the five Centres of Excellence across the UK funded by the UK Clinical Research Collaboration (UKCRC). Several work streams within the Centre for Public Health have a focus on health impacts of Obesity and they include programmes on Nutrition, Physical Activity, Chronic Disease, Dietary and Physical Activity interventions. In addition, there are a number of other significant
research funding initiatives that have recently been awarded to the Centre for Public Health. These include the award from the HSSPS R&D Office and the Food Standards Agency for projects looking at the effects of Obesity on insulin resistance and the potential for reducing this through increasing the dietary consumption of fruit and vegetables. In addition, there also has been the recent DEL-funded All-Island Initiative in Diet, Obesity and Diabetes, as a partnership between researchers within the Centre for Public Health, the Institute of Public Health in Ireland and the National Research Centre for Diet, Obesity and Diabetes at University College, Cork. Investment within the Centre for Public Health as a result of this initiative will include the appointment of two senior academics and four other research staff who will further expand and develop the current programme of research in Diabetes and Obesity. In addition, the Wellcome Trust NI Clinical Research Facility, which will open 2011, will have Nutrition and Obesity as one of the three major areas of focus where novel interventions, as well as understanding of disease programmes, will be accelerated.
In addition to these research programmes a number of senior medical colleagues from the Centre for Public Health, as well as the Centre for Cancer Research and Cell Biology, liaise closely with local government bodies as well as nationally in relationship to Obesity. Professor Ian Young, the Director of the Centre for Public Health, chairs the Obesity Prevention Steering Group within the Health Development Policy Branch of DHSSPS, and Professor Frank Kee, a member of the Centre for Public Health, is a member of its research subgroup.
Enclosed you will find an outline of the programme of research funded by the Food Standards Agency and the R&D Office and also the All-Island research programme on Diet, Obesity and Diabetes led by Professors Ian Young and Frank Kee.
Ulster Cancer Foundation
The Ulster Cancer Foundation is a local charity that helps to save lives and enhance the quality of life of everyone affected by cancer through care services, research, prevention, public campaigns and advocacy.
Cancer Prevention Department
The principle aim of the Cancer Prevention Department (CPD) is reduce the risk of developing cancer and promote its early diagnosis. UCF’S CPD uses the best current available evidence to direct the focus of our public information, training, resource development and awareness raising campaigns and programmes. These initiatives target many key groups in various settings and where possible, are implemented in partnership with appropriate statutory, voluntary, community and private sector organisations. Our programmes complement Government Strategies and are evaluated to measure impact and ensure their quality.
Background to overweight, obesity and cancer
During the past two decades the prevalence of overweight and obesity has been increasing throughout the world (National Cancer Institute, website). Experts have concluded that the chief causes of obesity are a sedentary lifestyle and the over consumption of high calorie foods (Vainio & Bianchini, 2002).
In the UK, about 13,000 people every year could avoid getting cancer if they maintained a healthy body weight (Bergstrom et al, 2001). This number is only going to increase in the future since more cancers are being linked to obesity, and the number of people who are overweight is increasing (Cancer Research UK, 2009).
It has also been estimated that more that 12 million adults in England alone will be obese by 2010, while 25% of children who live in a home with obese parents will become obese themselves (Department of Health, 2006).
Research has found that the evidence linking overweight, obesity and cancer is now even stronger than it was in the mid-1990s, with evidence showing that the more fat you carry on your body the greater your risk of developing cancer (The Lancet, 2008, World Cancer Research Fund (WCRF), 2007).
Recent evidence shows a convincing link between overweight, obesity and many of the most common cancers, including bowel, oesophagus, pancreas, kidney, endometrium (womb) and breast (post-menopausal) The Lancet, 2008, WCRF, 2007). A probable link has also been found with some of the lesser known cancers, such as gallbladder cancer (The Lancet, 2008, WCRF, 2007).
WHO states that overweight and obesity are the most important avoidable known causes of cancer after tobacco (WHO/FAO 2003), while the World Cancer Research Fund state that maintaining a healthy weight is one of the most important things that you can do to reduce your risk of cancer.
Scientists believe that there are several reasons for this link between overweight, obesity and cancer. One example is the relationship between excess fat and the hormone balance in the body (WCRF, 2007). Research has shown that these fat cells release hormone, e.g. oestrogen, which can increase the risk of cancers, e.g. breast cancer (WCRF, 2007).
Scientists estimate that by making changes to food we eat, increasing the amount of physical activity we do, and maintaining a healthy weight, about one third of all cancers could be prevented (WCRF, 2007).
Experts also stress the importance of encouraging people to establish habits of healthy eating and physical activity early in life to prevent overweight and obesity (National Cancer Institute, 2009).
Ulster Cancer Foundation Programmes in response to obesity in N Ireland
UCF have responded to the growing obesity epidemic in Northern Ireland through the development of programmes highlighting the links between diet and physical activity and health.
The following initiatives, numbered programmes 1 – 8, are promoted and delivered by UCF professional staff:
- Programme 1
Physical Activity and Cancer Engage – (PACE)
UCF physical activity based course. Duration 12 weeks.
Aim
To engage sedentary individuals in undertaking Physical Activity.
Outcome
Participants are made aware of the major health benefits of appropriate physical activity and identify barriers to their participation. Individuals identify a personal goal and plan of action. Participants learn the basic concepts of motivation and seek to identify their key motivation for engaging in physical activity, ongoing support mechanisms are agreed including buddying and weekly messaging. The Innerscan Body Composition Monitor is used to obtain each individual’s measurements. A stretch and warm-up exercise programme is demonstrated and the importance of physical activity safety explained. Week 1 – Benefits and barriers to physical activity, individual measurements taken, goal setting and motivational psychology discussed.
Weeks 2-5 - Participants are followed up weekly and supported via phone or messaging systems. Week 6 - Measurements are retaken, progress is then discussed and a brief outline of healthy eating covered. Week 7-11 - Participants are followed up on and supported via phone or messaging systems. Week 12 - Measurements are taken, results interpreted, participant awards given and ongoing lifestyle goals agreed.
- Programme 2
Quit2Fit
Aim
This project aims to help smokers to quit whilst managing their weight.
Many smokers associate giving up smoking with weight gain and are therefore not willing to try. We want to emphasise that this is not the case and with help and support, stopping smoking doesn’t mean gaining weight.
Objectives
1. To help people to stop smoking
2. To support those smokers trying to quit to maintain/lose weight.
3. To build upon community capacity throughout Belfast
4. To create a cross community support group/groups for people across Belfast for people trying to quit smoking whilst maintaining/losing weight.
- Programme 3
Fit Factor
Aim
To increase awareness of the link between positive lifestyle choices and overall health and wellbeing to school aged children.
Objectives
1. To target all P3, P4 and P5 (remove this) classes in NI with health promotion messages which will improve self esteem and promote positive behaviour change.
2. To promote accessibility of affordable fruit and vegetables to all families in NI.
3. To work alongside teachers to deliver a relevant, curriculum based programme.
Additional information
Over 250 schools – 10,000 pupils – registered for Fit Factor and received a Teachers’ Toolkit with modules on healthy eating, physical activity, self-expression and creativity. The final stage of this programme was to produce a creative project and submit it to the Fit Factor competition in the hope of winning up to £5000 to spend on sports equipment for the school.
- Programme 4
Starring Genevieve
Aims
1. To increase children’s knowledge of healthy eating.
2. To improve children’s attitudes towards healthy and unhealthy foods
3. To assist teachers’ and classroom assistants’ educate children on the importance of eating a healthy diet.
Additional information
Currently over 1000 children have benefited from the Starring Genevieve school visits, while every school in Northern Ireland has received the Starring Genevieve story book.
Background info to development of Starring Genevieve
The Government document ‘Fit Futures’ (2005) highlighted healthy eating in children as a key public health goal. In response to this a ‘Community of Interest’ group was established for the Belfast Health and Social Care Trust. This group consisted of a range of individuals including teachers, parents, school catering staff, dieticians, Surestart staff and health promotion staff. The group was keen to take forward the recommendations from Fit Futures.
The Ulster Cancer Foundation representative on this group took on the remit to develop a healthy eating resource for Primary One children. With continuous support and guidance from the ‘Community of Interest’ group, the Ulster Cancer Foundation representative developed the Starring Genevieve teaching pack. This pack consists of: a large (A3) story book (each school will receive one copy), a small (A5) story book (each school five copies) and the website. The website will include a parent page, a teacher page and educational activities for the children. The storybook has been endorsed by Council for the Curriculum Examinations and Assessment. As the main element of this teaching pack is the read-a-long story book with large colourful pictures it is also suitable for children with mild-moderate learning disabilities and also those with sight and hearing problems.
Starring Genevieve was developed to help teachers incorporate the issue of healthy eating into the new curriculum. It can be taught mainly under ‘Personal Health and Mutual Understanding’ but also other sections of the curriculum. An integral part of the new curriculum is that Information Technology be included in schools. The website was designed with this is mind.
- Programme 5
Health Fairs
Health Fairs offer an excellent opportunity to engage with individuals in an informal manner to raise awareness of cancer prevention and early detection messages.
A range of cancer risk issues and screening concerns can be addressed. Our displays and interactive equipment is used to deliver personalised feedback on risk factors and lifestyle choices to participants.
The use of interactive equipment to supply participants with personal data relating to their health status has proven extremely popular and is recognised as an effective tool in prompting behavioural change and supporting healthier lifestyle choices. Interactive and visual resources include:
InnerScan Body Composition Monitor
The InnerScan monitor offers in-dept body composition information by displaying weight, body fat percentage and total body fat percentage. It provides adults with information about visceral fat rating, muscle mass, physique rating, basal metabolic rate (BMI), metabolic age, and more.
Obesity Model
The obesity model is a great way to show the effects of obesity, the body cross-section shows the accumulation of fat around hips on a pear shaped and apple shaped body. The model also illustrates the effects of subcutaneous and intra-abdominal fat on the colon, ureter, small intestine and other internal structures.
Clogged Artery Model
This model’s realistic look and feel graphically demonstrates what happens inside a clogged artery when it fills up and blocks with layers of plaque.
Fat Chunk
This unique Biolike substance gives individuals the feel of real fat and viewers a realistic picture of what fat looks like inside the body.
APRIL Software
After photographing an individual, the image of their face can be drastically changed using the APRIL age progression software programme. The effects obesity can all be graphically illustrated on the individuals face and by adding on the years the effect can be all the more startling to observe, the soft-wear also allows for the effects of smoking and sun exposure to be added. Smoking cessation, care in the sun and dietary information and advice can then be offered to anyone shocked into considering some lifestyle changes as a result.
References:
National Cancer Institute
Obesity and Cancer: Questions and Answers
http://www.cancer.gov/cancertopics/factsheet/risk/obesity
World Cancer Research Fund
Recommendations for Cancer Prevention
http://www.wcrf-uk.org/PDFs/RecommendationsBooklet.pdf
Vainio H, Bianchini F. IARC handbooks of cancer prevention. Volume 6: Weight control and physical activity. Lyon, France: IARC Press, 2002
Bergstrom, A., et al Overweight as an avoidable cause of cancer in Europe. Int J Cancer, 2001, 91, p421-430
Cancer Research UK
Body weight and cancer: the evidence
http://info.cancerresearchuk.org/healthyliving/obesityandweight/howdoweknow/
Department of Health. Forecasting obesity to 2010 (2006)
Egger et al (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. The Lancet, Volume 371, Issue 9612, Pages 569 - 578, 16 February 2008
The Food Standards
Agency Northern Ireland
Introduction
1. The Food Standards Agency (FSA) is a non-Ministerial Government Department with UK wide responsibility for food safety and protecting other consumer interests in relation to food. Its remit is set out in the Food Standards Act 1999. The work of the FSA is overseen by an independent Board appointed through open competition and accountable through Health Ministers to Westminster Parliament and Devolved Administrations. The FSA’s office in Northern Ireland (FSANI) was set up in April 2000 and is accountable both to Parliament and the Northern Ireland Assembly.
2. FSANI comprises the Director, and 43 staff, plus the Northern Ireland Food Advisory Committee (NIFAC). The Chair of NIFAC is also a member of the FSA Board.
3. The FSA’s vision is “safe food and healthy eating for all" and it works closely with health and education departments and directorates across the UK. In particular, responsibility for nutrition policy is shared between the Agency and health departments.
4. This paper describes the Agency’s nutrition policy programme in broad terms. It also provides more detailed information on the individual initiatives that will have an impact on obesity and which the Committee may be interested in.
Eating for Health
5. The Agency has set out a number of strategic targets include reducing population salt and saturated fat intake, contributing to achieving a balance between calorie intake and energy output and encouraging improved nutrition labelling to help consumers make healthier choices.
6. There are three clusters of activity which seek to:
- Influence people’s knowledge and skills
- Encourage businesses to improve the nutritional composition of foods
- Foster an environment which promotes healthier choices
To ensure its nutrition policies are based on the best available evidence, the Agency allocates significant resources to supporting development of independent expert advice, evaluating the impact of its policies and generating and interpreting dietary research and survey data.
Table 1
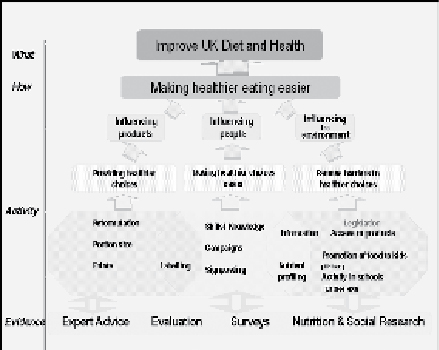
Table 1, above, illustrates how the Agency has established an integrated nutrition policy programme with the aims of providing healthier choices for consumers, making healthier choices easier and removing barriers to healthier choices. This can be broadly captured under Influencing Products, Influencing People and Influencing the Environment.
Influencing Products
The Agency is working with food businesses and their trade associations to support and encourage reductions in the levels of saturated fat and added sugar in the foods they produce. In addition, the FSA is encouraging food businesses to make available to customers a wider range of smaller portion sizes and healthy options to help support their efforts to balance the calories they consume with their dietary needs.
Saturated Fat & Energy Intake Reduction Programme
7. Currently people are eating far more saturated fat, on average, than is recommended, and rising levels of obesity indicate that energy intakes currently exceed energy requirements. Following the success of the FSA’s salt reduction work, the Agency has developed a programme of initiatives to reduce the level of saturated fat from 13.3% to 11% of energy intake and help consumers balance the calories in their diet with their needs. There are four areas of action: -
- Raising consumer awareness
- Promoting healthier choices
- Reformulation of mainstream products to reduce saturated fat and added sugar levels and
- Reducing portion size
8. The Agency launched a consumer campaign in February 2009 targeting women 25-60 years old from classes C1,C2 and D. The campaign aimed to raise awareness about the health issues if saturated fats are over consumed and provide simple tips to help consumers to cut down. The campaign has been developed to ensure that consumers following the advice would not have higher food costs.
9. On reformulation, the Agency has identified the key contributing food groups to saturated fat and added sugar intakes and is working with the food industry on reductions in these food groups. The focus for this work is with the dairy, meat and meat products, biscuits, cakes and pastry, snacks, confectionery, soft drinks and retail sectors. This builds on the good work that many sectors and individual food companies have already done.
10. To contribute to the programmes described above the Agency is working with the food industry to identify opportunities to reduce the size of single serve portions, for example of soft drinks and sweet and savoury snacks. It is also considering how best to provide consumer advice on appropriate portion size. An academic workshop has concluded that the evidence base on portion size and weight gain justifies these actions. Re-alignment of in-store promotions which could encourage increased consumption of energy dense, salty foods to promotion of healthier foods also has a part to play.
Influencing People
Campaigns
11. The Agency has a key role in ensuring that people have the information they need to make choices and in helping them to decide what changes they need to make to their diet and to put these into practice. We do this in a number of ways. For example, our saturated fat campaign in February this year focussed on the health implications of a diet high in saturated fat and the simple, positive steps people can take to reduce the amount we eat.
Front of pack food labelling
12. The development of a simple front of pack (FoP) nutrition labelling system by the FSA has been prompted by consumer demand for prominent, reliable, easy to use information. The Agency published recommendations for voluntary FoP nutrition labelling of food in March 2006. These are based upon extensive and robust consumer research carried out over 18 months and involving more than 2600 UK consumers.
13. The Agency’s recommendations take the form of a set of principles that businesses who wish to provide FoP nutrition information may follow. These recommend that businesses provide numerical information on fat, saturated fat, sugars and salt levels per portion of the product and use a red, amber or green colour code to indicate whether the level is high, medium or low, in accordance with criteria agreed by the Agency. Additional information on calories and/or the percentage of a Guideline Daily Amount (GDA) can also be provided. The recommendations apply to selected processed foods[1] where consumer research has indicated that the information would be most helpful to consumers.
14. Eight retailers (representing a market share of more than 40%) and 26 manufacturers, including 11 in NI, have adopted a FoP nutrition labelling scheme based on the Agency’s recommendations, and 23 consumer and public health groups support this approach. Evidence from adopters indicates high levels of consumer approval for this approach, shifts in sales towards healthier products and that the traffic light approach provides a powerful incentive to companies to reformulate their products to reduce levels of the nutrients highlighted on FoP.
15. An alternative FoP approach based on GDA information, without use of traffic light colours, has been adopted by other retailers and manufacturers (GDA schemes). Users of these approaches report high levels of customer awareness and that this labelling is acting as a stimulus to product development and reformulation.
16. As a result of voluntary action by many food businesses UK consumers have access to simplified FoP information on a very wide range of products. When it made its FoP recommendations the Agency decided to examine the effectiveness of alternative approaches. As a consequence it is funding an independent study to evaluate the impact of the three main FoP nutrition signpost labelling approaches used in the UK on purchasing behaviour and consumer knowledge. Results from this work are expected to be published in May 2009. A public consultation will be carried out during the summer of 2009, based on the findings of this survey.
The provision of information to customers in catering establishments
17. Provision of nutrition information in pubs and restaurants, cafés and on takeaway food has become increasingly important as the proportion of food eaten out has increased. Households in the lowest quintile of household income obtain only around half as much of their energy intake from eating out, compared to the highest income quintile[2].
18. This work will be an important part of the Agency’s strategy to help consumers make healthier choices. Recent qualitative research carried out for the Agency found consumers want to see clear and easy-to-use information when they are choosing what to eat. The FSA wants to see more consistent nutrition information for consumers at the point they make a decision about what they eat out of the home and is currently piloting calorie labelling at point of sale. A number of companies are acting as early adopters to voluntarily introduce calorie labelling, which will see calorie information provided on menus and other materials available at the point consumers choose what to eat.
19. Healthy eating commitments have been published from six of the UK’s largest high street restaurant chains, including KFC, Subway, McDonalds and Burger King. The types of action that these voluntary commitments promote include reformulating dishes to reduce the amounts of saturated fat, salt and sugar, menu planning to introduce a wider range of healthier options, using healthier cooking methods and providing customers with more nutritional information to help them make healthier choices. In addition, the Agency has focused on a number of different sectors involving the largest companies in the workplace catering, quick service restaurant, pub dining, casual dining, and coffee and sandwich shop sectors. This approach allows any catering company to make commitments appropriate to its operation, type and size.
Influencing the Environment
Working in partnership we will continue to collaborate with other Departments and public bodies in Northern Ireland to achieve shared objectives and remove barriers to healthier choices.
Evidence Base and FSA Nutrition Research
20. Underpinning all of the above is a commitment to ensuring that policy is grounded in evidence. The Agency is an evidence based organisation and uses research to inform policy development across a range of nutrition programmes and initiatives. In the UK, the diet and nutritional status of the general population is monitored by the National Diet and Nutrition Survey programme (NDNS). This survey is, for the first time, running in Northern Ireland and is jointly funded by FSANI, DHSSPS and safefood. The NDNS collects detailed information on food consumption, nutrient intake, physical measurements, nutritional status, and socio-economic, demographic and lifestyle indicators.
21. Surveys carried out between 1992 and 2001 in Great Britain indicated differences between households based on household receipt of benefits, social class and household income. The Agency therefore commissioned a Low Income Diet and Nutrition Survey (LIDNS) to provide robust, nationally representative, baseline information on the dietary habits and nutritional status of the low income (materially deprived) population.[3] The survey was carried out in 2003-05 and the survey report was published in 2007 (‘Low Income Diet and Nutrition Survey’, TSO, 2007). The aim was to study the diets of the bottom 15% of the population in terms of material deprivation. The fieldwork included 400 households in Northern Ireland.
22. In many respects the areas of concern identified by LIDNS in the low income population were similar to those already identified in the general population, although some were more marked in LIDNS. Compared with the general population, the low income population was less likely to consume wholemeal bread, and tended to consume more non-diet soft drinks, more processed meats, more whole milk and more table sugar. Consumption of fruit and vegetables fell well below the recommended five portions a day in adults and children. (Men 2.4 portions per day on average, women 2.5 portions, boys 1.6 portions, girls 2.0 portions.) Consumption of oily fish was very low.
Conclusion
23. The Agency’s nutrition programme includes a range of initiatives which tackle concerns about diet related diseases such as cancer and cardiovascular disease. These diseases are also co-morbidities associated with type II diabetes and obesity, which are both of increasing concern across the UK.
24. This work is being progressed in England in partnership with the Department of Health, through the Healthy Food Code of Practice set out in the Healthy Weight Healthy Lives Strategy document. The Agency is confident that through the deliberations of the Obesity Prevention Steering Group and its sub-groups, that Northern Ireland will have an equivalent strategy within the next 12 – 18 months which reflects the breadth of work needed to effectively address the complexities of tackling obesity.
[1] (1) Sandwiches, wraps, filled baguettes and similar products; (2) Prepared or ready meals, whether hot or cold; (3) Burgers, sausages; (4) Pies, pasties and quiches; (5) Breaded or coated or formed meat, meat alternative, poultry, fish and similar products including those in sauces; (6) Pizzas; (7) Breakfast cereals
[2] Expenditure on Food Survey 2002/3
[3] The term ‘low income’ is used here to reflect not just low levels of income but also wider aspects of material deprivation.
Diabetes UK
1: Key Issues
Obesity represents a major public health challenge to Northern Ireland and results in reduced mortality and increased morbidity rates for people affected. It is estimated that obesity leads to the deaths of over 2,500 people per year in Northern Ireland at current levels.
The treatment of obesity and its complications costs the Northern Ireland Health Service several million pounds every day. The cost of treating diabetes and it complications currently cost the Northern Ireland Health Service over £1 million per day. Obesity levels continue to rise across the world and in Northern Ireland 2006 figures showed that 25% of all men and 23% of women were obese.
Being overweight or obese increases your risk of developing Type 2 diabetes at any stage of your life. It is therefore obvious that any action taken to reduce obesity levels will also reduce the incidences of Type 2 diabetes.
The 2009 Northern Ireland Audit Office Report Obesity and Type 2 Diabetes in Northern Ireland stated:
“Taken together physical inactivity and unhealthy eating are important preventable causes of chronic disease and their impact is increasing. The rise in Type 2 diabetes is one example of a chronic disease that is closely connected to these risk factors"
Obesity and diabetes are complex conditions the 2007 Foresight Report – Tackling Obesities: Future Choices summarised the complexity in the following way:
“Obesity is the consequence of the interplay between a wide variety of variables and determinants related to individual biology, eating behaviours and physical activity, set within a social, cultural and environmental landscape"
The mainstream Western Health Service has been based on the identification and treatment of disease and not the prevention of illness or the promotion of good health. This medical model has dominated the medical profession and has focused attention on the laboratory rather than the community and the test tube rather than the individual.
This medical model has produced a perceived dichotomy between disease and illness: disease being the domain of the heath professional and illness the domain of patients, families and increasingly, social scientists (Thirlaway & Upton 2009).
The core issue in relation to defeating obesity is the understanding that it is a lifestyle disease with its main causes and determinants being behavioural and social. It should be no surprise therefore that attempts to treat obesity based on the medical model have failed to have any significant impact.
For any programme or intervention to be effective in stopping the rise in obesity and eventually reversing the trend it needs to be based on the acceptance of obesity as a lifestyle disease involving the behaviour choices made by people within the context and influence of social and cultural factors.
A wide range of agencies have promoted a healthy eating, healthy lifestyle message to the public over the past two decades. Although not universal, the knowledge of what generally constitutes a healthy lifestyle is widespread. However this knowledge has not changed or improved people’s behaviour.
Parallels can be drawn with the issues of smoking or drink-driving, in the sense that for a long time there was widespread public knowledge that both smoking and drink-driving were extremely harmful and yet this knowledge did not change people’s behaviour.
People’s behaviour began to change when there was a cultural shift making this behaviour socially unacceptable. Strong legalisation was also required to achieve this change. Only when the general public changed their perception of what was normal and acceptable did people’s behaviour began to change in a meaningful way.
Tackling obesity represents a far greater challenge in changing people’s behaviour. Changing what society and individuals feel is acceptable in relation to the many factors which contribute to obesity is a major undertaking. But unless we are successful in this undertaking we will all suffer the most severe consequences both individually and collectively.
Up to now health promotion has focused on public information, trying to increase knowledge of healthy lifestyle choices. There has been no desire to restricted peoples access to unhealthy food, drink or lifestyle activities because of the fear of ‘nanny state’ accusations. However it is unlikely that health promotion alone will change current lifestyle culture enough to stop the rise in obesity levels.
Part of the necessary shift in how the public view their own health and lifestyle is the development of a sense of value and control. People need to value and appreciate their health as something they have responsibility for and control over. This means moving away from the view that healthcare is controlled by healthcare professionals towards the position where people believe and act in a way which produces healthy lifestyle choices.
It should be the role of government and the Health Service to invest in supporting the development of people’s self-efficacy skills and confidence. Only by adapting such an approach will we achieve the required shift and improvement in people’s health and well being.
This shift is a complex process and requires careful strategic planning, investment and needs to be managed alongside the provision of the existing Health Service. This process cannot be successful under the current funding levels and the public expectations of the Health Service. Financial and policy support from wider government and society is required.
2: Obesity and Diabetes
The causes of diabetes especially Type 2 are complex and no fully understood but it is clear that being overweight or obese significantly increases the likelihood of a person developing the condition.
However not every case of Type 2 diabetes is caused solely by a person being overweight or obese. There are a range of risk factors which contribute to the development of Type 2 diabetes. Other risk factors beside weight include family history, genetic make up, ethnic background, age, stress levels and other medical conditions. It is thought that obesity is a factor in up to 80% of Type 2 diabetes cases.
Diabetes is a major public health issue across the UK as the number of people affected increases dramatically. The number of people living with diabetes has steadily increased in recent years and the prevalence models predict a major increase in the coming years. Since 1996 the number diagnosed with the condition has increased from 1.4 million to 2.5 million. This number is set to continue to rise at an alarming rate as our population ages and becomes more obese. There also remain up to half a million people who have the condition but are not yet aware of it.
Diabetes mellitus is a condition in which the amount of glucose (sugar) in the blood is too high because the body cannot use it properly. Glucose comes from the digestion of starchy foods. Insulin is vital for life. It is a hormone produced by the pancreas that helps the glucose to enter the cells where it is used as fuel by the body.
Type 1 Diabetes develops if the body stops producing insulin. It usually appears before the age of 40 and is treated by insulin injections and diet. Regular physical activity is recommended.
Type 2 Diabetes develops when the body’s insulin output is reduced or when the insulin that is produced does not work properly (known as insulin resistance). This type of diabetes usually appears in people over the age of 40, though often appears before the age of 40 in South Asian and African-Caribbean people. It is treated by diet and physical activity, or by diet, physical activity and tablets, or by diet, physical activity and insulin injections.
3: Diabetes in Northern Ireland
There are currently over 65,000 people diagnosed with diabetes in Northern Ireland and a further 12,500 people who are undiagnosed. There were nearly 4,000 new cases diagnosed in 2007-08 and currently over ten new cases are diagnosed every day. There was a 7% increase in the number of adults living with diabetes in Northern Ireland in 2007; this increase is expected to be nearly 10% for 2008. 10% of all deaths are diabetes related and £1 million per day is spent on diabetes care that is over 10% of the Northern Ireland Health Budget.
Forecast models from The Institute of Public Health in Ireland predict that the number of people living with diabetes in Northern Ireland will increase to over 80,000 by 2015-20
4: The Impact of Diabetes
Diabetes is a progressive condition and is associated with serious chronic ill health, disability and premature mortality. Diabetes will affect a person’s health from their head to their feet and all their internal organs. Long-term complications include heart disease, stroke, blindness, kidney disease, impotence, depression, nerve damage, eating disorders and amputations.
Evidence demonstrates that many of these long-term effects can be avoided with early and effective treatment.
Diabetes is a complex life long condition which affects individuals in different ways. It is a progressive condition which changes and responds to people’s changing live style and age. As a result the treatment of diabetes is complex and varies from individual to individual.
The DHSSPS draft Service Framework for Cardiovascular Health and Well Being, includes the following summary of diabetes:
Diabetes is a life-long condition that can impact upon almost every aspect of life – lifestyle, relationships, work, income, health, wellbeing and life expectancy.
The potential impact of diabetes includes –
- Reduced life expectancy. In Type 1 diabetes, life expectancy may be reduced by as much as 20 years and by as much as 10 years in Type 2 diabetes.
- Five time higher mortality rates from coronary heart disease
- Three times higher risk of stroke
- Additional risks in pregnancy, with higher rates of congenital malformations and higher perinatal mortality rates
- Diabetes is the leading cause of renal failure, accounting for one in four people starting renal replacement therapy
- The second most common cause of lower limb amputation
- The leading cause of blindness in people of working age.
Effective management of diabetes increases life expectancy and reduces the risk of complications developing.
High quality diabetes care requires not only the co-ordination and co-operation of the range of professionals who make up the multidisciplinary team but also self-management. The empowerment and involvement of the individual with diabetes is crucial.
5: Current Approach to Treating Diabetes
There is currently no Northern Ireland wide strategy or plan or clear approach to the prevention of diabetes or for the treatment and support of people living with diabetes. This is in sharp contrast to England, Scotland and Wales were National Service Frameworks exist for diabetes.
Diabetes UK has campaigned for the introduction of a Diabetes Service Framework into Northern Ireland over the past two years and can supply the committee with further details of the need and the benefits of such a framework.
In 2003 CREST (Clinical Resource Efficiency Support Team) published a joint report with Diabetes UK – A Blueprint for Diabetes Care in Northern Ireland in the 21st Century. The report was produced by a working group of over 50 people and represented a unique consensus of the entire diabetes community in Northern Ireland including Healthcare Professional, Health Service Management and people living with diabetes. The report proposed a clear way forward for the modernisation of diabetes services in Northern Ireland closely based on the National Diabetes Framework being delivered in Scotland at the time.
Unfortunately the 2003 CREST Report has never been implemented in Northern Ireland
In 2007/08 a Regional Diabetic Retinopathy Screening Programme was funded by the DHSSPS and roll-out began in 2008.
In 2008 the Regional Medical Audit Group (RMAG) commissioned report – Regional Audit of Structured Diabetes Education in Northern Ireland was published. The audit was conducted and written by the Belfast Health and Social Care Trust, the University of Ulster and Diabetes UK Northern Ireland. The audit showed that less then 20% of people with diabetes in Northern Ireland had been offered any type of patient education.
One of the reports recommendations stated:
“The provision of structured diabetes education is a vital component of high quality diabetes care. This intervention should be afforded the same value and rigour as any other patient intervention. Funding for provision of structured diabetes education across Northern Ireland needs to escalate significantly in order to meet NICE guidance and recommendations."
The Northern Ireland Audit Office report was very clear in one of its conclusion:
“While we acknowledge that addressing the problem of obesity has been a Departmental priority since the mid 1990’s, the full impact of its primary prevention strategies on reducing the burden of Type 2 diabetes has still to be realised"
The DHSSPS is about to publish a new Services Framework for Cardiovascular Health and Well Being. The CV Framework contains 44 standards including three relating to diabetes care. The standards for diabetes are:
1: All people with diabetes should have an accurate diagnosis made
2: All patients with diabetes should have access to structured education programmes and emotional and psychological support. Services incorporating these elements will encourage partnership in decision making, support individuals in managing their diabetes and help them to adopt and maintain a healthy lifestyle.
3: All patients with diabetes should have access to, at a minimum, an annual review to a defined standard by an appropriately trained multidisciplinary team.
The three diabetes standards in the CV Framework is a wholly inadequate response to the challenge of tackling diabetes in Northern Ireland. Diabetes UK has produced a briefing paper outlining our criticism of the CV Framework in relation to the prevention, care and treatment of diabetes.
The Northern Ireland Audit Office report contains a summary of other DHSSPS initiatives to tackle obesity.
Diabetes UK has run a number of very effective public awareness campaigns over recent years such as the Measure Up campaign and the Silent Assassin campaign.
6: Recommendations
The Health Service is currently very effective at treating the complications of diabetes but is failing to prevent the growth in the condition or the development of its associated complications. There is a clear need for a sea change in the approach to the prevention and treatment of diabetes in Northern Ireland. There are a number of specific actions which the DHSSPS could take to support this shift:
- The introduction of a Diabetes Service Framework into Northern Ireland
- Targeted screening of at risk groups using evidence based risk assessment
- Targeted action to stop the rise in Type 2 Diabetes
- The creation of Diabetes Managed Clinical Networks in every Trust Area
- Ensure every person with diabetes is offered quality patient education
- Ensure people with diabetes are offered Weight Management support
- Ensure people with diabetes are offered psychological & emotional support
- Ensure diabetes HCP’s and trained in lifestyle intervention techniques
- Develop the expertise of HCP’s in the field of lifestyle disease management
There is a strong evidence base to show that lifestyle and therapeutic interventions with people who are at high risk of developing Type 2 diabetes – because they are overweight, obese or have impaired glucose tolerance- are effective in preventing or at least delaying the onset of diabetes.
In summary the most important intervention which will have the biggest impact on the quality of life and people living with diabetes and ease the burden on the Health Service would be improved support for people with diabetes so they can achieve effective self management. This will improve their health outcomes, reduce their use of Health Service resources and prevent the development of complications. This could be achieved by improved access to patient education programmes for people living with diabetes and the introduction of a Diabetes Service Framework into Northern Ireland fulfilling NICE standards.
The Northern Ireland Audit Office a report makes a number of suggestions in relation to target setting and the performance measurement of future policies.
Tackling Obesity in general:
Great benefit would be gained if the DHSSPS, the local universities and the wider health community invested in developing a deeper knowledge and expertise in the field of lifestyle disease management. A useful introduction to this area is The Psychology of Lifestyle, Promoting Healthy Behaviour. Thirlaway & Upton 2009. Routledge. ISBN 0-415-41662-0. The University of Wales Institute, Cardiff.
A number of other areas of action would help support the campaign against the rising levels of obesity in Northern Ireland:
- Whole government approach – ineffective to leave to DHSSPS alone
- Develop a more lifestyle disease based approach
- Increased use of the psychology of lifestyle disease management and self-efficacy techniques in supporting people
- Develop and refine the public health message
- Increase effectiveness of interventions targeted at young people and parents
- Wider recognition given to the role played by popular cultural, the food industry, methods of transport and leisure time choices
- Increased pressure/partnership with the food industry in relation to food production, labelling and advertising
- Measures to support making a Work/Life Balance a reality for more people
- Effective Promotion of cooking skills throughout the school curriculum
- The need for improved monitoring of the obesity situation and production of quality information and statistics
7: Diabetes UK
Diabetes UK is the largest patient organisation in Europe with a membership of nearly 200,000 people. We have 400 Local Support Groups and invest over £8m every year into diabetes research.
We champion the rights of people with diabetes and campaign to ensure they receive the highest possible standard of healthcare. We also work in partnership with the Healthcare Professionals who support people living with diabetes.
In Northern Ireland we have over 3,500 active members and supporters. We provide a range of local information and support services for people including;
- Information & Advice for people with diabetes, their families and carers
- An Advocacy Service
- 20 local Support and Parents Groups
- Support and education events for local Healthcare Professionals
- Children’s Care Events and residential care holiday events
- Public awareness campaigns
- Lobbying government and Health Trusts to improve diabetes care
- Research grants to Queens University Belfast and University of Ulster
- Local Fundraising activities
Diabetes UK Northern Ireland is self funding and receives no financial support from government or the Health Service.
Dairy Council for Northern Ireland
Summary
- There is increasing evidence that dairy foods may have a positive role in weight control (in both children and adults).
- A large number of studies have now reported that individuals with a high intake of dairy products are less likely to be overweight or obese than those who consume few dairy foods.
- Research also suggests that dairy foods might make it easier to lose weight. A series of studies has found that including three to four servings of low-fat dairy foods a day as part of a calorie-controlled diet helps people to lose more weight than cutting calories alone on a low-dairy diet.
- It has been suggested that the calcium in dairy may be partly responsible for these beneficial effects. A number of studies have reported that adults and children who have a high-calcium diet tend to be slimmer than those who eat few calcium-rich foods, to gain less weight overtime and to lose more weight on reducing diets.
- Calcium may work by binding fat in the intestine and increasing its excretion from the body. Alternatively, some work suggests that calcium may alter the way fat cells function and help the body break down and burn fat.
- Other compounds in dairy foods may also play a part as the weight-loss effects of dairy are greater than for the equivalent calcium supplement. One possibility is dairy’s protein which may have a positive effect on satiety and feelings of fullness.
- It is important to note that further research is needed to understand fully the relationship between dairy consumption and weight. Nevertheless, this emerging role for dairy foods is another good reason for adults and children to ensure they have sufficient dairy in their diets.
There is increasing evidence that dairy foods may have a positive role in weight control in both children and adults.
A large number of studies have now reported that adults who consume more calcium and dairy foods weigh less and/or have less body fat than those who consume little or no dairy. For example, researchers analysing data from the National Health and Nutrition Examination Survey (a programme of studies designed to assess the health and nutritional status of adults and children in the United States) found that in men and women, increased calcium intake was associated with lower body fat (1). Similarly, using data from adults in the Quebec Family Study, researchers reported that a higher calcium intake was significantly associated with lower body weight and fat in women and found a similar trend in men; dairy foods provided about 60% of the calcium in the study subjects’ diets (2).
Similar relationships have been noted in children such that a higher intake of dairy foods has been associated with a lower percentage of body fat. For example, in children followed from ages two to eight years old, a higher dietary calcium intake from calcium-rich foods such as milk, cheese and yogurt was associated with a lower percentage body fat (3). In another study, which investigated the effect of eating dairy foods in early childhood on the changes in body fat from five to 13 years of age, children who consumed the least dairy gained most fat during childhood (4).
Although such observational studies can not confirm a cause-and-effect relationship between dairy and weight, they have been valuable in identifying associations and guiding researchers to investigate the connection further. For instance, it has been postulated that including low-fat dairy foods in a weight-reducing diet may make it easier to lose weight. There is evidence from intervention studies to support this. For example, in a 24-week study of 32 obese adults, those who consumed three servings of milk, yogurt or cheese a day while on a balanced, reduced-calorie diet, lost significantly more weight and fat than those who consumed little or no dairy (5). Participants on the high-dairy diet (1200 - 1300 mg/day calcium) lost 70% more body weight and 64% more body fat than those on the low-dairy diet. Further research has suggested that the ability of dairy / and or calcium to augment weight loss on reducing diets may be most evident in those whose diets are low in dairy / calcium in the first instance (6). Similarly, simply adding dairy / calcium to an already adequate diet does not automatically result in weight loss, particularly in normal weight subjects (7). It is important to note however, that in such interventions nor does supplementation with dairy foods result in weight gain.
Researchers have conducted cellular, animal and human studies to better understand the specific mechanisms responsible for dairy’s impact on body weight and fat. While more research is needed it has been suggested that the calcium in dairy may play an important part in these beneficial effects. Calcium may work by binding fat in the intestine and increasing its excretion from the body and so decreasing fat (and therefore calorie) absorption (8). Dairy calcium may be much more effective in this respect than other forms of calcium (9). Alternatively, some work suggests that calcium may alter the way fat cells function and help the body break down and burn fat (1). Calcium-driven effects on appetite have also been postulated (6). Other compounds in dairy foods may also play a part as the effects of dairy are greater than for the equivalent calcium supplement. One possibility is dairy’s protein which may have a positive effect on satiety and feelings of fullness.
It is important to note that further research is needed to understand fully the relationship between dairy consumption and weight. Nevertheless, this emerging role for dairy foods is another good reason for adults and children to ensure they have sufficient dairy in their diets; for certain groups of the population in Northern Ireland - young women and teenage girls in particular - this is not currently the case. Certainly, from the available evidence it seems likely that for those trying to maintain a healthy weight and particularly for those trying to lose weight, a low dairy intake may be counterproductive.
References
(1) Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB Journal 2000; 14:1132–1138.
(2) Jacqmain M, Doucet E, Despres JP, Bouchard C, Tremblay A. Calcium intake, body composition, and lipoprotein-lipid concentrations in adults. American Journal of Clinical Nutrition 2003; 77:1448-1452.
(3) Carruth BR and Skinner JD, The role of dietary calcium and other nutrients in moderating body fat in preschool children. International Journal of Obesity 2001; 2: 559-566.
(4) Moore LL, Bradlee ML, Goa D, Singer MR. Low dairy intake in early childhood predicts excess body fat gain. Obesity 2006; 14: 1010-1018.
(5) Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obesity Research 2004; 12(4): 582-590.
(6) Major GC, Alarie FP, Doré J, Tremblay A. Calcium plus vitamin D supplementation and fat mass loss in female very low-calcium consumers: potential link with a calcium-specific appetite control. British Journal of Nutrition 2009; 101: 659-663.
(7) Gunther CW, Legowski PA, Lyle RM, McCabe GP, Eagan MS, Peacock M, Teegarden D. Dairy products do not lead to alterations in body weight and fat mass in young women in a one year intervention. American Journal of Clinical Nutrition 2005; 81(4): 751-6.
(8) Boon N, Hul GB, Stegen JH, et al. An intervention study of the effects of calcium intake on faecal fat excretion, energy metabolism and adipose tissue mRNA expression of lipid-metabolism related proteins. International Journal of Obesity 2007; 31: 1704-1712.
(9) Lorenzen JK, Nielsen S, Holst JJ, Tetens I, Rehfeld J, Astrup A. Effect of dairy calcium or supplementary calcium on postprandial fat metabolism, appetite, and subsequent energy intake. American Journal of Clinical Nutrition 2007; 85: 678–87.
Dairy Council for Northern Ireland Activities
A fundamental part of the Dairy Council for Northern Ireland’s remit is to communicate the benefits of including dairy products in a balanced diet and to provide factual information to allow individuals to make informed choices about which dairy products they consume. The Dairy Council is, therefore, very much involved with the education of both children and parents on food and nutrition issues, and encouraging consumers to eat a healthy, balanced diet is a central part of the Dairy Council’s work. The Dairy Council promotes milk and dairy products only within the context of a balanced diet (based on current government guidelines for healthy eating) and does not advocate excess consumption of any dairy food, to children or any other group. The dairy industry produces a wide range of dairy products including low-fat and reduced-fat options and we strive to make consumers aware of this.
We are involved with food and nutrition education in a number of key areas:
Schools
The Dairy Council provides a wide range of nutrition education resources to both primary and post-primary schools. In addition, we are involved in a number of other educational activities.
In primary schools, the Dairy Council offers the ‘Food & Fitness’ programme. Food & Fitness is intended to support the efforts being made by schools to encourage healthy eating and enable children to make informed choices about food and exercise. The programme has been running for five years and each year reaches over 20,000 pupils in over 300 primary schools. It focuses on helping children at Key Stage 2 learn about a balanced lifestyle; the importance of a healthy diet and physical activity. The programme consists of a 40 minute interactive presentation including colourful props and a Food & Fitness rap all designed to stimulate and engage the children. In addition, teachers are provided with teaching packs and notes to enable them to provide additional lessons on the theme of balance, and each pupil is provided with a leaflet to take home to their parents which summarises the key messages.
The Dairy Council is also very much involved in practical food education in schools and considers the development of cooking skills to be a vital tool to enable children to adopt healthier eating habits. The Dairy Council’s ‘Young Cook of the Year’ competition has been running in post primary schools for over 15 years, and is open to pupils in Key Stage 3, Key Stage 4, and Special Education. It serves to encourage and support pupils’ practical work as well as raising the profile of practical food education. The brief for the competition each year is developed in conjunction with the Council for Curriculum, Examinations and Assessment (CCEA) and has a healthy eating theme. The Dairy Council has also produced a recipe resource for post-primary schools to compliment the new Home Economics curriculum and the increased opportunities for practical work therein which addresses nutrition, healthy eating and practical skills development.
The Dairy Council strongly supports the concept of a ‘whole-school’ approach to food and nutrition, whereby teaching of good nutrition in the classroom is matched by the provision of healthy food in the rest of the school environment, for example at break-times and school lunches. To this end, we have been involved in a number of initiatives including healthy snacking schemes (e.g. Boost Better Breaks) and encouraging awareness and uptake of the EU subsidised School Milk Scheme. With regard to the latter, a publication entitled ‘Milk and More’ has been developed which is distributed to the parents of all new pupils starting primary school. The resource not only highlights the nutritional benefits for children of semi-skimmed mid-morning milk but of the importance of eating well throughout the school day.
Families
The Dairy Council considers education and support for parents to be an important part of improving eating habits. We believe that unless the family as a whole can be encouraged to adopt a healthier lifestyle, children are not likely to change their behaviour or continue with any improved behaviour. The Dairy Council is involved with parents in a number of ways. For example, parents (and other family members such as grandparents) are given the opportunity to join the Dairy Council’s Parent’s Club. Members receive the ‘Good 4 You’ magazine two or three times a year which provides a wide range of information, advice and ideas on healthy eating and healthy lifestyle, including encouraging physical activity.
Health professionals
In addition to work within schools and with parents, the Dairy Council works with a number of health professional organisations involved with children and parents. These include health visitors, practice and school nurses, dietitians and dental health professionals. We supply a wide range of education resources and also provide an information service to help health professionals keep up-to-date with the latest nutrition research. This includes organising conferences and meetings. Recent themes for Dairy Council Conferences include Childhood Obesity, Young People’s Nutrition and Health, Women’s Nutrition, and Nutrition for Older People all of which include a focus on helping to facilitate dietary behaviour change.
Co-operation with other organisations
It is clear that to stand any chance of slowing the accelerating obesity epidemic a multi-sectoral approach is required. As outlined above, the Dairy Council already works with a wide variety of health, nutrition and education organisations and also with government departments and agencies. We look forward to continuing and extending such co-operation in future.
Promotion of physical activity
The Dairy Council considers that increasing physical activity is an important part of obesity prevention. Where possible, we therefore endeavour to highlight the benefits of physical activity, as well as a healthy diet, in our activities and resources directed at children and their parents. In addition, our involvement with the international youth soccer tournament, the Milk Cup, affords the opportunity to promote a healthy, active lifestyle to young people and their families across Northern Ireland.
Northern Ireland Assembly
Facilities Branch
This paper has been prepared by Facilities Branch in consultation with Eurest to assist the Committee for Health, Social Services & Public Safety with their inquiry into obesity. It details the actions and initiatives currently in place within the Northern Ireland Assembly, in partnership with the catering provider Eurest, to promote healthy eating in the workplace. It also outlines those measures that are either in operation, or have been proposed for future implementation, to encourage greater levels of exercise by individuals.
1. Introduction
A person is obese when he/she carries too much body fat for their height and sex, defined as a Body Mass Index (BMI) of 30 or greater. Obesity can develop when you eat more calories than you burn off over a period of time. The rate at which you burn off calories from food and drink is known as your metabolic rate. People who are very active generally have a higher metabolic rate than those who are inactive because they burn off calories faster through energetic activity. Crucially, if the amount of calories provided by your daily food intake is more than the calories you burn off, the body stores the extra energy as fat.
Fast foods, high calorie snacks and large portions all mean it is easy to take in more energy than we need. As a result, obesity has now become one of the most serious medical problems of the Western World. According to figures from the National Audit Office, being obese can take up to nine years off your lifespan. Medical problems typically caused by obesity include depression, high blood pressure, heart disease and diabetes.
Obesity and associated problems develop gradually as a result of poor diet and lifestyle choices and, to some extent, your genes. It is therefore widely agreed that the best way to prevent becoming obese is by eating healthy food and exercising on a regular basis.
2. Promoting Healthy Eating
The current Support Services Contract is held by Eurest (a member of Compass Group, PLC), who provide all catering within the Northern Ireland Assembly, namely the Blue Flax Restaurant, Press Bar, Members’ Bar, Members’ Dining Room, Brassiere, Committees and Events. From the outset of the contract, it was made clear to the supplier that healthy eating would be of high importance in the provision of the service. This commitment was demonstrated by the following comments in the contract specification:
“The Contractor shall promote healthy eating and shall encourage a reduction in salt, sugar and fats, and an increase in foods high in dietary fibre" (p.58).
To ensure that healthy eating remains a priority, Facilities Branch liaise with Eurest on a regular basis, and since the commencement of the contract in March 2007, several innovative catering options that provide healthy eating have been introduced, to accompany those healthy options previously offered.
2.1 Balanced Choices
In recognition of growing public awareness surrounding the importance of healthier eating, alongside increasing concerns over the rise in obesity, the Compass Group has developed a programme of activities, supported by specialist training, under the banner of ‘Balanced Choices’. The ‘Balanced Choices’ concept was introduced by Eurest to Parliament Buildings during November 2007. Menu compilation is by strict guidance using nutritionally specified ingredients. Due to the popularity of the concept, it was agreed to implement it as a daily feature, giving Secretariat staff the ability to make informed choices that meet their own dietary and lifestyle requirements. (See Appendix 1: Sample Menus).
By working with and targeting their suppliers and manufacturers to ensure the ingredients they use and the products they serve deliver optimum nutritional benefits, Eurest focus on:
- The reduction of sodium salt
- A reduction in fats (particularly trans and saturated fats)
- A reduction in added sugars
- Encouraging fibre rich foods
- The availability of fresh fruit (whole and prepared for convenience)
2.2 Breakfast Service
Eurest currently offers a wide range of breakfast items. Whilst they continue to market the traditional fry option in the Blue Flax Restaurant, their chefs (under the instruction of Executive Chef Barry Emerson) take added care to ensure that the cooking methods deployed during food preparation reduce the fat content of the cooked breakfast:
| Item(s) | Cooking Method | Nutritional Relevance |
| Tomatoes | Grilled | No added salt or oil |
| Soda & potato bread | Grilled | Lightly brushed with sunflower oil |
| Sausages & bacon | Grilled | No added oils |
| Baked beans | Saucepan | Added fibre to the diet |
| Eggs | Shallow Fried | Poached/scrambled eggs cooked to order |
| Mushrooms | Poached | Water and little oil |
As an alternative, the provision of a ‘breakfast health shelf’ allows the customer to choose from four freshly prepared fruits and two yogurts (one natural and one flavoured). A porridge bar was also introduced to the Blue Flax Restaurant two years ago as a rich nutritional breakfast option. Oats are packed with Vitamin E and the range of toppers provided offer additional fruit and nuts to increase nutritional value. In addition, the presence of beta-glucan in porridge helps reduce blood cholesterol levels and regulates the absorption of glucose. A further range of sugar free cereals, including muesli, are available daily and served with semi-skimmed milk. Breakfast juices (apple, orange and/or cranberry) are also available daily in an unsweetened form.
2.3 Lunch Service
Emphasis is on freshness to ensure products are served with a high vitamin and mineral content. The team of chefs use salt sparingly during the cooking process and utilise the following range of methods to ensure foods are cooked using little or no oil:
Shallow frying Grilling Poaching Dry roasting Boiling
Two fresh soups are prepared daily using fresh local ingredients. Soups are made without oil, lightly seasoned using Lo salt and are not finished with cream. Servings of soup are 10fl oz and therefore form one part of the ‘five a day’ recommendation. Soups are served with home baked rolls which contain added fibre and herbs to aid digestion.
During July 2008, Eurest introduced their ‘Wild Greens’ concept, which focuses on the provision of light salad and protein based produce. Again, due to high customer demand and popularity, Eurest have retained this offer as a daily option within their catering outlets. June 2009 saw the introduction of a new range of Wild Green dishes by Eurest.
The salad bar itself consists of 10 different salad choices. Nine of these items are made using only fresh ingredients. Dressings are offered separately, allowing the customer to choose low fat or mayonnaise based. The sandwich bar’s choice of breads and rolls has also increased to include high fibre and seed based products. Spreads are low calorie.
Fresh vegetables, cooked ‘al dente’ to increase their fibre content, are available daily for customers to choose from. Pulses are served daily in the form of baked beans and processed peas. Baked potatoes are also featured everyday and are often served with tuna or beans to offer a high fibre option. Mashed potatoes are made using no cream or butter and are lightly seasoned.
A full range of health and diet drinks are available from the chilled cabinet. All milk served in the dispensers is semi-skimmed. A choice of cartons is available in either semi-skimmed or full fat. Lo salt is available at the cutlery stations for all users.
A variety of whole fresh fruit is available on a daily basis, with a minimum of five choices featured. Fruit pots are also offered, incorporating a varied selection of mixed fresh fruit. Fruit platters are provided for Committees on a regular basis and are very well received.
2.4 Promotional Material
At the entrance to the Blue Flax Restaurant, a range of nutritional leaflets are available for customers wishing to obtain nutritional guidance. Menus are available to peruse on the Assembly intranet site (AssISt) on a daily basis. Table talkers periodically feature cooking and well being information for employees to read. All information has been well received.
2.5 Tariffs
Prior to considering a proposal for a catering tariff increase in March 2008, and following on from feedback received from the Catering Focus Group, Facilities Branch requested that Eurest factor in a freeze or reduction of tariffs for several healthy eating options. Facilities then assessed the proposals and negotiated further. Fruit items (e.g. apples, bananas, oranges, pears, pineapple pots and grape pots) saw a reduction of between 8.80% and 9.20%. Two salad boxes saw a reduction of 9.10% and 9.30%. Other items held at 2007 prices included milk (1/2 pint, pint and glass), baked potatoes and smoothies.
2.6 Confectionary and Font Water
Whilst still available for purchase within the Blue Flax Restaurant, confectionary is no longer located at the till points, in an attempt to discourage the impulse purchase of unhealthy food. Font water is supplied for consumption throughout Parliament Buildings.
3. Encouraging Greater Levels Of Exercise
There is currently a Workplace Travel Plan in place for the Northern Ireland Assembly. It was produced by Atkins Transport Planning Belfast in November 2008 for the entire Stormont Estate, with the aim of encouraging smarter and more sustainable travel. A staff survey formed the foundation of the Travel Plan. A total of 1,625 survey responses were received out of approximately 2,880 staff working within the Stormont Estate Area, representing a return rate of 56%. The response rate was 92% within the NI Assembly.
3.1 Access to the site by walking and cycling
There are good quality footways in the areas surrounding the Northern Ireland Assembly, on Stoney Road, Massey Avenue and Upper Newtownards Road. Pedestrians can access the Stormont Estate from all three roads, with an additional pedestrian access on Upper Newtownards Road, at Dundonald House and Annexes. High quality footways provide links to all existing buildings and annexes within the Estate.
The Comber Greenway is a 7 mile traffic free section of the National Cycle Network Route 99 running along the old Belfast to Comber railway line, parallel to the Newtownards Road. The route encompasses Comber, Dundonald, Ballyhackamore, Holywood Arches and Dee Street. There are, however, no other cycle routes within the surrounding Estate Area.
3.2 Promoting walking and cycling
At the heart of the Plan are two achievable but challenging objectives focused on the promotion of walking and cycling throughout the Stormont Estate:
- Increase walking from 1.4% (22 respondents) to 2.5% (Nov 2009) and 3.5% (July 2010). Approximately 170 staff currently live within 1.5 miles of the Estate area.
- Increase cycle modal share from 0.7% (11 respondents) to 2% (Nov 2009) and 4% (July 2010). Approximately 580 staff currently live within 4 miles of the Estate area;
Walking and cycling provide health benefits, such as reducing the risk of heart disease and strokes. It therefore follows that one of the main benefits of developing and implementing the Travel Plan will be the opportunity to encourage more active lifestyles for employees.
3.3 Primary Initiatives
- The provision of 150 cycle parking spaces at key locations throughout the Stormont Estate. There is currently a bike shed located at the Lower East Assembly Car Park;
- To inform staff of the existing shower facilities in Parliament Buildings (on 3 floors);
- The provision of lockers within each main building;
- The Stormont Estate Area Travel Plan Steering Group is currently considering the implications of employers providing interest free loans for staff to buy a bicycle and cycling equipment. A ‘Salary Sacrifice Scheme’ was introduced by HM Treasury some years ago offering staff the opportunity to purchase a bicycle, nominally for use in the journey to and from work, free of all taxes and duties. A further reduction is made to the individual’s national insurance contributions and income tax. The total financial impact of this means the full retail price of the bicycle is reduced by at least 40%. It is already in operation in the private sector and in parts of the public sector.
- The Travel Plan co-ordinator (Patricia McConnell, with Pat Neeson as the Assembly’s representative to the Steering Group) will distribute personal alarms to staff who feel they would like to have one with them. Pedometers will also be purchased to use as promotional tools and will serve to highlight the health benefits of walking to work;
- The Northern Ireland Assembly took part in the ‘Bike to Work Day 2009’ during Travelwise NI Bike Week by promoting cycling to work during that week;
- The promotion of a bicycle mileage allowance during Bike Week and through The Bike User Group (BUG).
3.4 Complimentary Initiatives
- The Travel Plan co-ordinator will contact local cycle shops to negotiate discounts for staff buying cycles or equipment locally;
- The availability of pool bicycles located around the Estate will also be promoted;
- The Travel Plan co-ordinator will set up a Bike User Group (BUG). BUG will arrange training days for employees where, for example, national standards cycle trainers can provide on road training to adults;
- Employees and visitors will also be made aware of the ‘Bike It with Translink’ initiative which allows people to cycle as part of their journey to work by bus or train or for business purposes. All bicycles will be carried free of charge on trains (dedicated space permitting) and buses, if the bus has a boot and space available (there are no restrictions for folding bikes). However, bicycles are only permitted after 09:30am.
4. Conclusion
There are currently a number of actions and initiatives in place within the Northern Ireland Assembly to both help promote healthy eating and encourage greater levels of exercise. In partnership with Eurest, Facilities Branch ensures the provision of ‘Balanced Choices’ menus, nutritional information and healthy options throughout the catering outlets within Parliament Buildings. Facilities and Eurest have demonstrated that they are receptive to proposals put forward by its customer base and take every opportunity to promote healthy eating. With regards to the promotion of exercise for individuals, Facilities Branch is involved heavily in the implementation of the Assembly’s Workplace Travel Plan, which is an ongoing strategy. Properties Directorate will shortly appoint a Sustainability Manager who will continue to encourage the uptake of walking and cycling as preferred modes of transport to and from the workplace.
Appendix 1: Sample Menus
The following menus were utilised during the week commencing Monday 15th June 2009.
(i) Balanced Choice Menu Option
(ii) Balanced Choice Vegetables
(iii) Balanced Choice Information
(iv) Blue Flax Lunch Healthy Options
Soup 1 – Chicken & asparagus
| Chicken – very good source of protein – 4oz provides 68% of daily value for protein. |
| Low in fat |
| Asparagus – excellent source of Vitamins A, C & K |
Soup 2 – Lentil
| Lentil – very good source of cholesterol lowering fibre – virtually fat free |
Balanced choice – Olive & lemon chicken
| Chicken – very good source of protein – 4oz provides 68% of daily value for protein. Low in fat |
| Olives – good source of Vitamin E |
| Lemon – Excellent source of Vitamin C. Contains compounds that have anti cancer & antioxidant properties |
(v) Vegetable/Potato Menu
Vegetables
Leek Provencale 61p
Roast celeriac 51p
Baked beans 42p
Peas 42p
Potatoes
Creamy mash 51p
Baked potatoes £1.03
Sauté potatoes 61p
Large freshly cut chips £1.08
Small freshly cut chips £0.60
Rice 61p
Helping Hand Ltd
The situation in context
It has been well recognised for a generation that obesity is one of the most, if not the most, pressing health issues facing Western populations. Clear associations exist between levels of obesity and those of coronary heart disease, hypertension, strt is important to tackle obesity across the life-course, there are good reasons to focus attention on obesity in childhood:
- Obesity “tracks" well from childhood into adulthood and at least half of obese school-age children become obese adults.
- Long-term changes in health-related behaviours are more likely to be achieved within younger population groups.
- A focus on young people allows intervention to be aimed at a wider family group for each individual, and also wider peer groups, particularly through schools, offering a broader potential reach for any given intervention.
National data from England in 2004 showed that among 2-10 year olds 16% of boys and 12% of girls were obese (BMI = 95th centile) and among 11-15 year olds 24% of boys and 26% of girls were obese.
Local data suggest that at present within Northern Ireland, approximately 1 in 4 school age children are either overweight or obese. These figures are startling, but increase year on year, and may well represent an underestimate due to the limitations of data collection.
Prevention and Intervention
Much time and debate has been given to the relative merits of prevention and intervention in childhood obesity, but this is not a straightforward choice. Without doubt, public health measures (including legislation) are required in order to shift population trends in diet and physical activity. However, the genie is already out of the bottle, and effective interventions are urgently required for obese individuals now- there is a significant “right skew" to obesity-related morbidity, i.e. the most significantly obese will generate far greater amounts of illness (and cost to the NHS) than those at relatively lower levels of fatness.
Doing nothing is simply not an option - health economists in England estimate that the direct cost to the NHS attributable to obesity (in England alone) in 2007 was £4.2billion, projected to rise to £6.3billion by 2015. It is therefore imperative that public health measures go hand in hand with interventions to help the most significantly obese young people across the Province avoid developing an adult lifetime of obesity-related illness.
It makes eminent sense within Northern Ireland for both policy-makers and professionals to draw on and where possible improve on existing best practice.
Proposed solution
Helping Hand proposes the delivery of 5 pilot programmes of intervention, aligned to the 5 Trust areas and aimed at post primary children throughout Northern Ireland. Attendees will be directed to the programme through an agreed referral programme.
The venues will be schools dormant in the summer months with excellent indoor and outdoor sporting facilities to deliver the physical activity part of the programme and modern home economics classrooms where the diet and lifestyle education programme can be delivered. In 2009 alone Helping Hand Ltd will hire 20 schools throughout Northern Ireland for week long schemes through the government funded Fostering Achievement Scheme- with the positive relationships existing between Helping Hand and the schools we have already provisionally secured a school in each of the 5 Trust areas who are keen to be involved in the proposed weight management programme.
Obesity research has been hampered by a relatively poor evidence base, but it is increasingly clear that whilst weight management by conventional means (dietetic advice and clinical encouragement) is difficult, best results are obtained through the use of intensive, structured, intervention programmes, delivered by specifically trained individuals in an appropriate setting. Good examples of such programmes in the UK include:
- The Counterweight Program in Scotland, which has proven successful in long-term weight reduction in adults in primary care.
- The Carnegie Weight Management Programme, based at Leeds Metropolitan University, which has produced encouraging results in children, both in a residential and non-residential setting, within summer scheme programmes.
Background
Helping Hand has significant experience in the design and delivery of structured programmes to address individual and group needs and have built a team of skilled professionals who are leading in their professional fields.
We have a wide range of networks that will support the roll out of these programmes throughout NI and have provisionally secured suitable venues to roll out pilot programmes in each of the 5 Trust areas. Helping Hand is funding a study visit for all the members of the proposed delivery team to Carnegie Weight Management to be undertaken in July 2009 as a result of our networking and partnership approach with leaders in this field.
Our non residential intervention programmes will run through the course of the summer break to ensure no interference with attendees’ academic commitments. Our programmes will focus on the core components of:
- Diet- This aspect of the programme will promote all the kinds of food that you would find at home but will teach participants the types and amounts of foods they should eat. Attendees will follow a meal plan designed by our qualified dietitian at home and bring in a packed lunch every-day in accordance with this guidance. The attendees will also use home economics classrooms equipped with cookers/sinks etc. to allow them to learn more about healthy eating and food preparation.
- Physical activity- This will all be in the form of fun based games in a supportive environment. The aim of this aspect of the programme is to make physical activity fun and build confidence through participation.
- Lifestyle- These sessions are the key to continuing to manage weight after the initial intervention programme and ensure that attendees make better future choices about what food they eat. Our approach promotes good planning, continual monitoring and family involvement.
- Social interaction- The programme will give everyone the chance to meet new friends and people who they may not otherwise meet. There will be many social activities planned to support these programmes and ensure that it is a valuable and life changing opportunity for all who participate.
Each attendee will undertake a structured programme of intervention that will follow a timetable of activity and education in classroom and non classroom environments, delivered by our regional teams of professionals. Timetables will be designed to ensure balance of focus as well as results, to ultimately ensure that attendees have a positive experience and realise the benefits and see the effects of the time and effort invested. Education and application of learning over a 3-4 week period at each of the regional venues will be supported by rigorous monitoring and evaluation of results to demonstrate the tangible benefits of this approach and the success that can be delivered through specifically designed programmes of intervention.
Track record
As a business we have an excellent track record of success of delivering effective support strategies to the government. We currently provide education and tuition services to children in foster care, and hold the current contract for the provision of these services until 2012.We deliver regional programmes of study at Easter and Summer schemes as well as one to one tuition throughout the academic year, through the Fostering Achievement scheme. In 2009 alone we are delivering 20 week long programmes throughout Northern Ireland. We also provide a range of professional services to a private client base.
The Delivery Team
The programmes will be designed in consultation with our multi disciplinary team of health and education professionals, comprising of:
Project Manager - Simon McKee BA (Hons), PGCE, ACE Director, Helping Hand Ltd.
Simon is a fully qualified Physical Education teacher with over 16 years teaching experience and has been Managing Director of Helping Hand since inception in 2006. He has a keen interest in child health and education issues. Simon has a proven track record of delivery in the implementation of a range of educational schemes, delivered throughout the Province.
Paediatrics- Dr David Watkins MBChB MD MRCP(UK) FRCPCH DipSEM(GB&I)Consultant Paediatrician, Northern HSC Trust & Honorary Clinical Lecturer in Child Health, QUB
As a general paediatrician with a keen interest in sport (and physical activity among the wider community) Dr. Watkins has developed an interest in childhood obesity over several years. His postgraduate research at QUB involved leading a team examining trends in the development of risk factors for coronary heart disease, including diet, fatness, blood pressure, habitual physical activity and aerobic fitness among 2000 children aged 12 and 15 throughout NI.
Key publications from this project include the following:
- Ten-year trends for fatness in Northern Irish adolescents: the N.I. Young Hearts Project – repeat cross-sectional study (DC Watkins, LJ Murray, CAG Boreham, G Cran, IS Young, C McGartland, PJ Robson, JM Savage). Int J Obesity 2005; 29: 579-585.
- Ten-year blood pressure trends in adolescents: analyses of cross sectional surveys in the Northern Ireland Young Hearts Project (DC Watkins, P McCarron, LJ Murray, GW Cran, CAG Boreham, PJ Robson, C McGartland, G Davey Smith, JM Savage). BMJ 2004; 329: 139-141.
Since taking up his current consultant post, Dr. Watkins has set up and led the Province’s first dedicated NHS multi-disciplinary children’s weight management clinic, offering children and their families support from dietetics, specialist health visitors, and a mentored family physical activity programme, the Fit Families Scheme, through an innovative partnership with Antrim Borough Council. Dr. Watkins is currently involved in a multi-agency group setting up a Managed Clinical Network for Obesity within the Northern Trust.
Dietetics- Sharon Madigan, PhD, MSc., Registered Dietitian
Sharon graduated with a primary degree in Biological Sciences in 1991 and an MSc degree in Biomedical Sciences / Human Nutrition 1993 and obtained her professional qualification in Dietetics in 1995.In 2005 Sharon completed her doctoral studies within the Faculty of Life and Health Sciences at the University of Ulster. Sharon’s PHD thesis was “The development, delivery and evaluation of a pragmatic nutritional educational intervention for primary care health professionals".
Since 1996 Sharon has worked in a senior capacity in Community Dietetics as a clinician delivering dietetics services to community based GP clinics where the majority of the patients (adults and children) were over-weight or obese and may also have had some co-existing medical or surgical issues (Diabetes, Cardiovascular disease Cancer etc).
Previous to starting work in clinical dietetics Sharon was employed as a Research Assistant at the Centre for Diet and Health at the University of Ulster. Here she gained invaluable experience in the area of the collection of food consumption data, laboratory techniques, data analysis, report writing, conference presentations and the preparation of research publications for peer review.
Sharon was the principle investigator on a research project which developed and evaluated a nutrition education program within primary care. Research topics included a needs assessment with health care professionals and service users, patients and carers; developed a training programme and project evaluation. She also designed and developed resources, which also meet the needs of the health care professionals and has been involved in guideline development in Northern Ireland, working with the Clinical Resource Efficiency Support Team (CREST).
Health promotion experience includes education and resource development in the area of infant and child nutrition, healthy eating guidelines, Diabetes, Cardiovascular disease, dietary issues for ethic groups, supporting other health professionals and the general public in the area of diet and nutrition. Sharon has also acted as a contact for the media / public to answer questions on issues such as food labelling, diet and disease, novel foods and dietary supplements.
Physical Activity and Education- Neal Kennedy BA (Hons), PCGE, Dip Ind. Studies
Neal Kennedy is Head of Physical Education at one of the leading grammar schools in Northern Ireland. He qualified in Physical Education from the University of Ulster in 2001 with a BSc (Hons) in Sport Exercise & Leisure Studies with a Diploma in Industrial Studies (Distinction). As part of his training he has undertaken modules in Health Related Physical Education and Exercise Physiology.
Neal delivers GCSE and A level PE courses that serve to highlight the importance of physical activity for young people and consider important topics such as diet, fitness and exercise and guidelines for a healthy lifestyle.
Neal also holds the Northern Ireland Institute of Coaching Gym Fitness Instructors Award and has extensive experience of delivering Summer Schemes throughout regions in Northern Ireland.
Helping Hand would like to thank the Committee for Health, Social Services and Public Safety for the opportunity to submit this proposal and their invitation to an informal meeting.
Mr. S. McKee
Managing Director Helping Hand Ltd (M) 0044 (0)7798 870 815
Dr Una Lynch
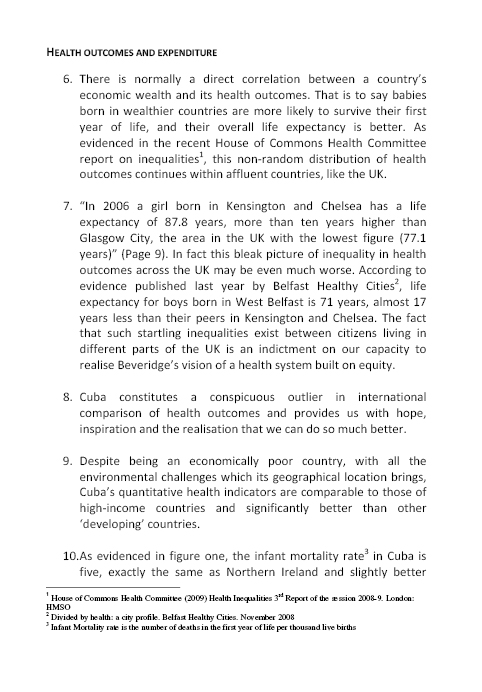
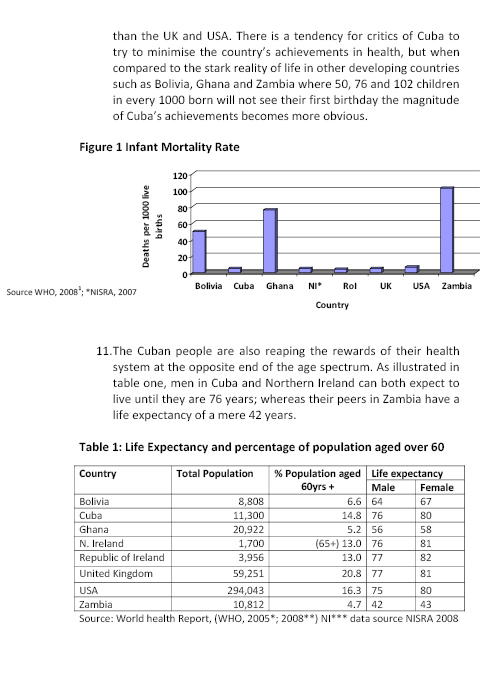
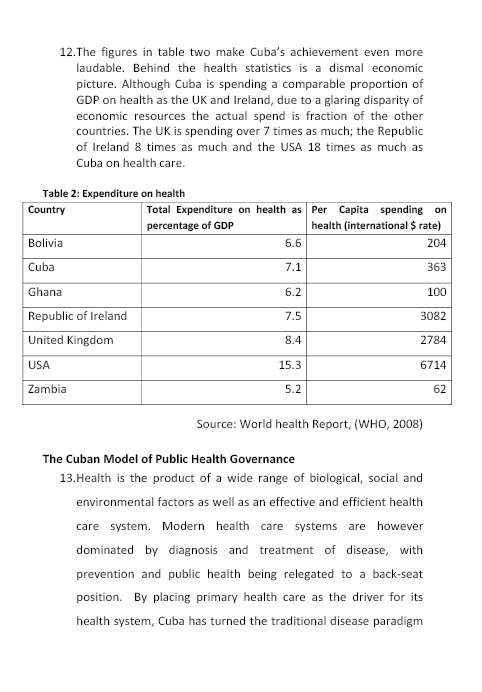
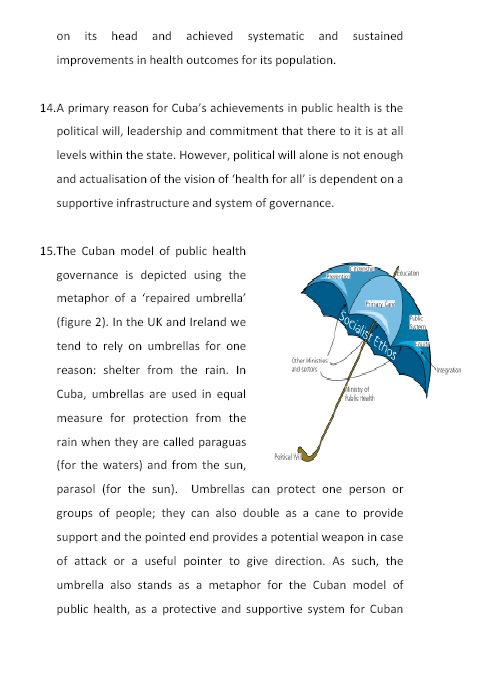
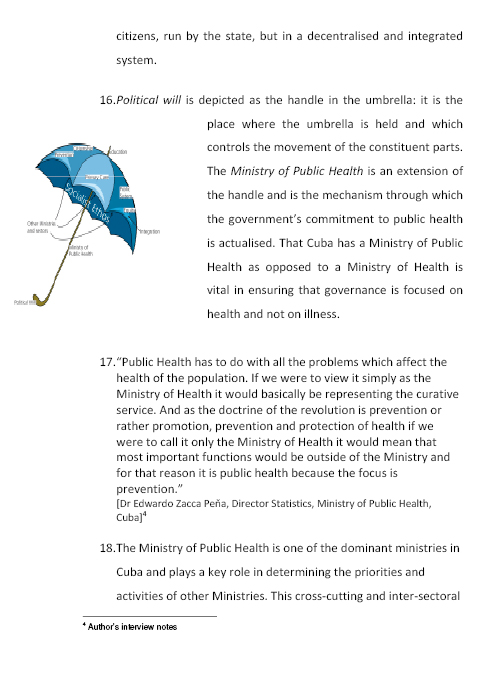
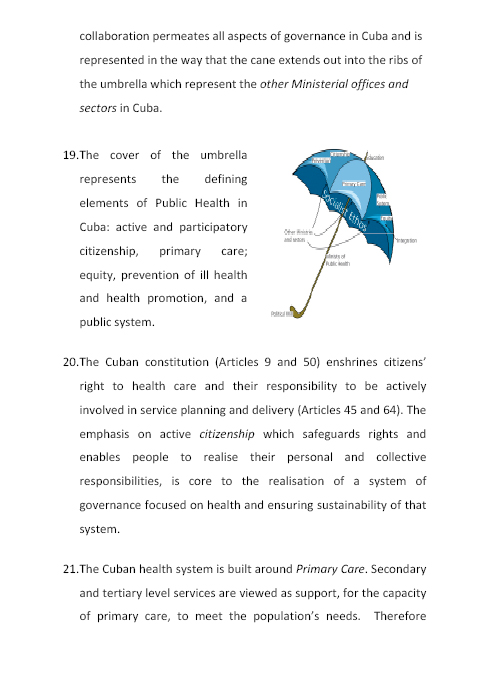
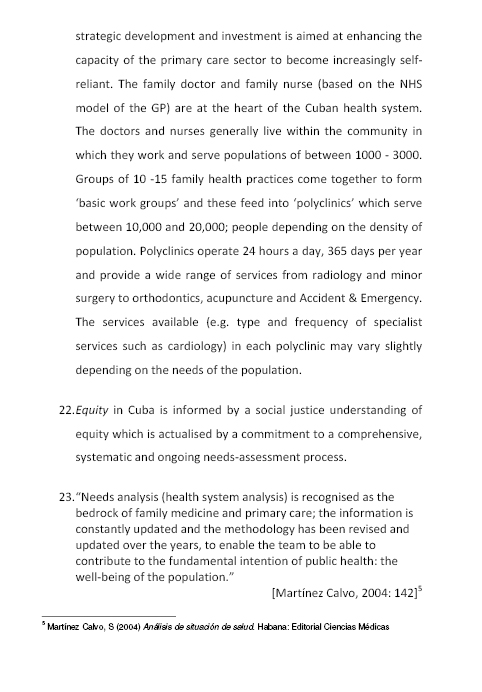
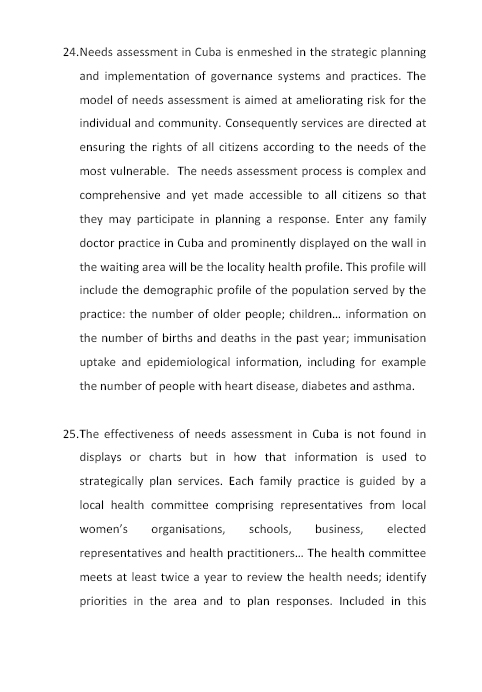
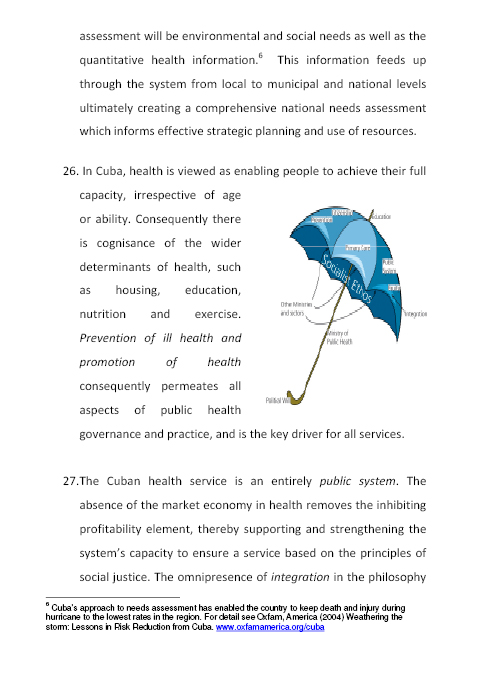
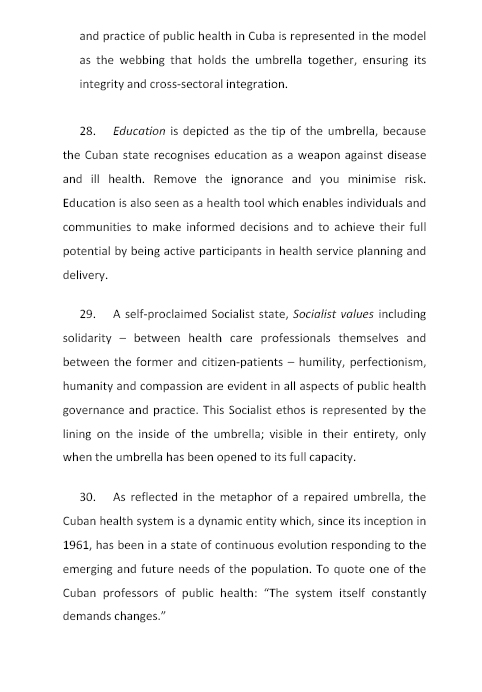
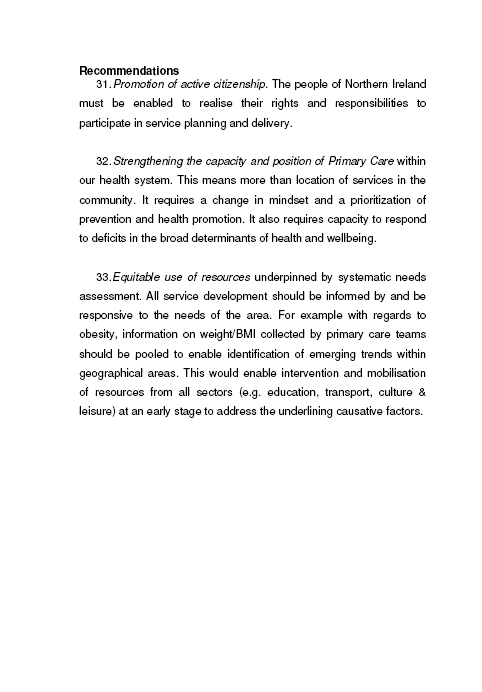
Public Health Agency
1. Introduction
In their submissions to the Committee, a number of organisations have described the obesity problem in some detail. This submission therefore summarises some key facts, describes current actions to tackle the problem, and outlines the planned approach of the Public Health Agency.
2. Background
- Obesity is measured by Body Mass Index (BMI), calculated from a person’s height and weight. People with a BMI above 30 are considered obese.
- Obesity occurs when you eat and drink more energy (calories) than you use. Physical, socio-economic, cultural and environmental factors contribute to a situation where too many people consume more calories than they use.
- People today are less active than previous generations. Some estimates put the difference in daily activity levels now compared to 50 years ago as being equivalent to running one marathon per week.
3. Key Facts
- UK obesity rates have doubled over the last twenty years and will take time to reduce.
- In NI, almost 60% of adults are overweight (35%) or obese (24%). Similar rates are seen in Great Britain.
- Among children in NI, around 1 in 5 is overweight and 1 in 20 is obese. Childhood obesity is a strong predictor of obesity in adulthood.
- Obesity in a parent increases the risk of childhood obesity by 10%.
- Anti-obesity drugs cost the health and social care system around £0.5m per year. Around 50,000 people in NI could be eligible for surgical treatment of obesity if NICE guidelines were applied in full, at an estimated cost of £750m.
Key Point: It is not possible to treat our way out of the obesity epidemic. Instead, we have to focus investment on prevention.
4. Cost of Obesity to Individuals
- The health risks to an individual increase sharply when their BMI is over 30. Recent studies suggest that the risk of premature death in people with obesity is similar to that seen in people who smoke more than 10 cigarettes/day[1].
- Obesity is not therefore an aesthetic issue – it shortens life and increases the risk of a range of conditions:
- heart disease, high blood pressure and stroke;
- type 2 diabetes
- some cancers, including post menopausal breast cancer;
- osteoarthritis and back pain;
- sleep apnoea;
- complications in surgery and pregnancy.
5. Cost of Obesity to the Economy
- UK Wide: Estimated at £3.7bn per year currently, but nearly 60% of the UK population could be obese by 2050 which would cost £45.5 billion (at today’s prices).
- Northern Ireland loses 260,000 working days each year and obesity is costing our economy approximately £500 million.
Key Point: Stopping the year-on-year increase in levels of obesity would save the DHSSPS £210 million over the next twenty years
6. Strategic Context – NI
- A number of strategies contribute to preventing obesity:
- Investing for Health Strategy (2002) focuses on determinants;
- “Fit Futures Taskforce" (2004) focuses on children and young people;
- Health Promotion Strategies on Breastfeeding, Nutrition, Physical Activity promote activity and good nutrition.
- In addition, the DHSSPS leads the Obesity Prevention Steering Group and has set a target to halt the rise in obesity by March 2010.
- DHSSPS allocated £832,000 to implement Fit Futures in 08/09. A further £550,000 and £300,000 has been allocated to promote physical activity and improve nutrition respectively.
Strategic Context – Rest of UK
- England: “Healthy Weight, Healthy Lives" January 2008
- Scotland: “Healthy Eating, Active Living" June 2008
- Wales: “Food and Fitness Implementation Plan" for Children and Young People 2006
7. Action in N Ireland
The following are a few examples from the several hundred initiatives which are taking place regionally. All are in line with the NICE guidance and Foresight recommendations.
- Health Promoting Homes in the western area is an award winning initiative that involves a 26 week training and support programme delivered by the community sector. To date, 430 families have benefited from the programme.
- Healthy Steps for Life Programme in the southern area focuses on promoting healthy eating and active lifestyles for under 5’s, targeting parents and carers, child minders, playgroups nurseries and other child care providers.
- Community and Workplace Challenges allow community and workplace teams to compete in health promoting challenges e.g. 6 – 8 weeks of regular walking measured by pedometers. They get points for each of these and the winning team gets an overall prize at an award event. These are extremely popular and there is great competition between and within the teams for the various prizes that are on offer.
- FRESH is an holistic weight management programme which has been developed for year 8/9 pupils in the eastern area with a BMI above the 98th centile. This is a 12 week programme of physical activity, nutrition and behavioural change activities delivered twice weekly. A further 6 weeks of physical activity sessions are delivered when the first 12 weeks are completed. A FRESH graduate programme is also developed with the aim of sustaining positive behaviour change and social support for the young people. The Cook – It programme is also offered to parents and young people. Similar programmes run across the region.
- Environmental Health Professionals from health and local government in the northern area have produced guidelines which have been issued to all Environmental Health Officers with a remit for food to enable them to promote good nutrition to local catering businesses, with a particular focus on the provision of meals to young consumers.
- Nutrition Matters for the Early Years provides information on healthy eating, physical activity and dental health for child care providers in day nurseries, play groups and childminders and is being implemented across Northern Ireland. It is also now offered to foster carers.
- Compulsory nutritional standards for school meals and other food in schools (including breakfasts, tuck shops, vending machines and after schools activities) are being implemented in all nursery, primary, post primary and special schools. Nutrition Associates have been appointed within the Education and Training Inspectorate to assess schools’ compliance with the nutritional standards as part of the General Inspection programme within schools. A new publication, Top Marks, has been developed to support the work on food in schools and provides a guide to establishing breakfast clubs, healthy snacks schemes, healthier vending as well as information on implementing the compulsory nutritional standards. A website providing information on healthy eating, easily prepared recipes and an on-line quiz that provides feedback on current eating patterns has been established (www.enjoyhealthyeating.info). Registered Dietitians have been appointed to help schools across NI implement healthy eating initiatives.
All of these actions have been, or are in the process of being, evaluated and are proving to be successful in enabling people to make positive lifestyle changes in relation to obesity.
8. Approach of the Public Health Agency
Given the cost to individuals and our society, tackling the problem of obesity will be one of the Public Health Agency’s key priorities over the coming years.
Based on our own experience through Investing for Health partnerships and other initiatives to promote health and wellbeing, and the evidence from the Foresight Report, WHO, European Commission, NICE and others, we will develop our approach around the following principles:
- Prioritise obesity prevention across all government programmes – health and social care alone cannot solve this problem. It requires coordinated concerted action at central and local government level and additional investment for many years to come. The Public Health Agency is establishing new joint working arrangements with Councils and local government officers and will have teams in place through 2009. Working closely with education, planning, sports, and other sectors, those teams will develop coordinated action and investment to reduce obesity in their area;
- Planning for ‘fit’ communities – in France, the EPODE programme resulted in a 50% decrease in the percentage of overweight boys. We will work with local government to plan an environment that promotes ‘walkability’ and cyclability’ through safe, attractive parks and leisure facilities; provides easy access to healthy food choices and limits availability of less healthy choices;
- Involving the community and voluntary sector to provide a range of programmes in local communities, for example, sports and other clubs that get young people out and active and away from TV and other sedentary activities. Local communities know the types of programmes that people will attend and we will involve them as co-designers and providers of those programmes at neighbourhood level;
- Involving the whole family in changing behaviour – parents, particularly mothers, have a major influence on what the family eats. We will prioritise programmes that provide practical advice and skills in preparing healthy inexpensive meals to help change the home environment;
- Early years intervention – the foundations for a healthier life are created in the first 5-6 years. A number of programmes already target the early years and aim to build life skills among families with young children. We will prioritise investment to expand these programmes and will consider including children who are overweight or obese and their parents as a target group;
- Extending the scale and sustainability of programmes, particularly those provided by the community and voluntary sector. With limited funding and much of it non-recurrent, many programmes are too small scale and too short-term to have a lasting effect. Around 3100 4-5 years olds and 4500 11-12 year olds in NI are overweight or obese; existing programmes deal with only a small percentage of these children. We will seek additional recurrent investment to enable many more programmes to be delivered direct to people at a community/neighbourhood level;
- Connecting existing programmes and facilities – cross-referral between statutory and community or voluntary programmes makes best use of the total resource that exists, and minimises duplication of services. It requires good knowledge among all staff at a very local level of the services available and cross-referral as a routine way of working. We will work with Trusts, community, voluntary and other providers to ensure their staff know the connections they can make between services in their local areas;
- Measuring the impact of programmes – the impact of individual programmes must be measured more robustly than has happened to date. Additional funding will be required to support additional measurement, but without measurement, we cannot identify the projects that should continue or increase, and those where investment should stop. We will press government departments for additional funding to support measurement;
- Learning from effective practice elsewhere – while evidence of preventing obesity at a population level is limited, examples of effective interventions at a local level do exist. We will continue to identify those examples and apply here, the factors that made them successful;
- We will inform government policy on obesity – Evidence of effective policies in other countries is beginning to emerge. For example, Norway has used food subsidies, target pricing and clear labelling to encourage people to choose healthy rather than unhealthy options. We will work with government departments here to develop policies appropriate to NI.
Our immediate priority areas will include:
- Ensuring a care pathway is developed for use by the School Nursing Service across all HSC Trusts to point children to the right programmes;
- Developing a portfolio of evidence based holistic, family-based weight management programmes and prioritising funding towards those;
- Mainstreaming the Cook It! programme across the region;
- Developing a standard evaluation framework to support high quality, consistent evaluation of weight management interventions;
- Working with the Institute of Public Health (IPH), the Centre of Excellence for Public Health at Queen’s University Belfast, and others on obesity in Northern Ireland;
- Ensuring an appropriate balance in resources between obesity prevention and treatment to ensure short-term targets are met whilst also looking to longer-term objectives;
- Ensuring adequate research and development programmes are taken forward locally;
- Working with DHSSPS to develop the Life Course Obesity Prevention Strategy;
- Developing a social marketing approach to change how people relate to and understand obesity, tailoring the messages in a way that the target audiences will respond.
Conclusion
Previous generations were threatened by lack of nutritious food and diseases related to malnutrition. This generation, in particular, is the first to face the very real threats associated with obesity. While the factors that cause obesity are complex, the evidence on what works is increasing. The challenge for government and all agencies in NI, is to learn from and apply that evidence through coordinated action at community/neighbourhood level right across NI. The Public Health Agency will play its full role in leading and supporting that work in partnership with all other sectors.
[1] Neovius M, Sundstrom J, Rasmussen F. BMJ 2009;338:b496
Appendix 4
Other Evidence Considered by the Committee
Table of Contents
Submission Page Number
Response from Belfast Trust 587
Response from Northern Trust 601
Response from Southern Trust 611
Sport NI Presentation 637
Obesity Research Paper 1 643
Obesity Research Paper 2 Catch Program 677
Obesity Research Paper 3 Norwegian Program 682
Obesity Research Paper 4 English Obesity Strategy 687
Fire Service Letter 693
Response from Belfast Trust
about Hospital Menus
Patricia McCann
Public Liaison Services
Belfast Health and Social Care Trust
1st Floor, Nore Villa
Knockbracken Healthcare Park
Saintfield Road
Belfast BT8 8BH
T: (028) 9096 0058
F: (028) 9056 5553
E: patriciaz.mccann@belfasttrust.hscni.net
Our Ref: DC/1132/0809
9 April 2009
Ms Michelle O’Neill MLA
Deputy Chairperson
Committee for Health, Social Service and Public Safety
Room 412
Parliament Buildings
BELFAST
BT4 3XX
Dear Ms O’Neill
Inquiry Into Obesity - Meals served to Hospital Patients
Your letter of 20 March 2009 to Mr William McKee, Chief Executive of Belfast Trust has been passed to Public Liaison for response.
Please find enclosed base sample menus used in the Belfast Trusts Royal Hospital and in Knockbracken Wards covering a one week period.
Can I please ask you to submit any future requests for information to either the postal address above or to our generic e-mail address publicliaison@belfasttrust.hscni.net and we will ensure that your request is dealt with promptly.
I hope you will find this helpful. If I can be of any further help please let me know.
Yours sincerely
Patricia McCann
Public Liaison Services
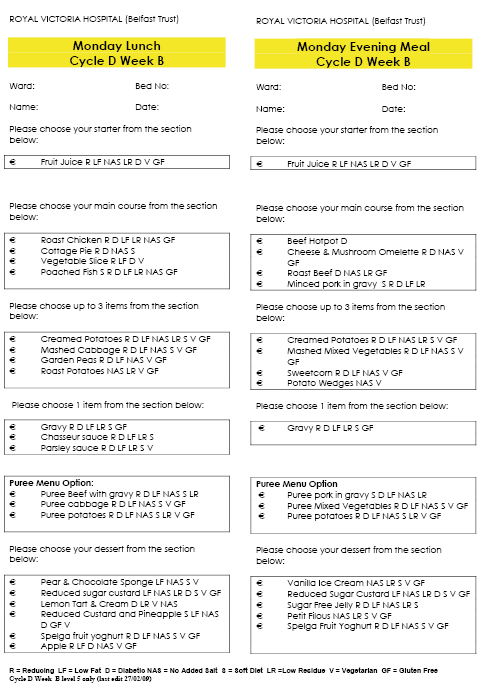
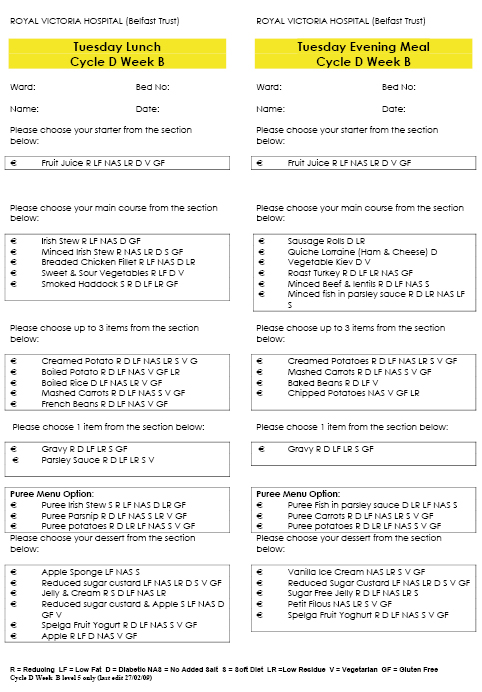
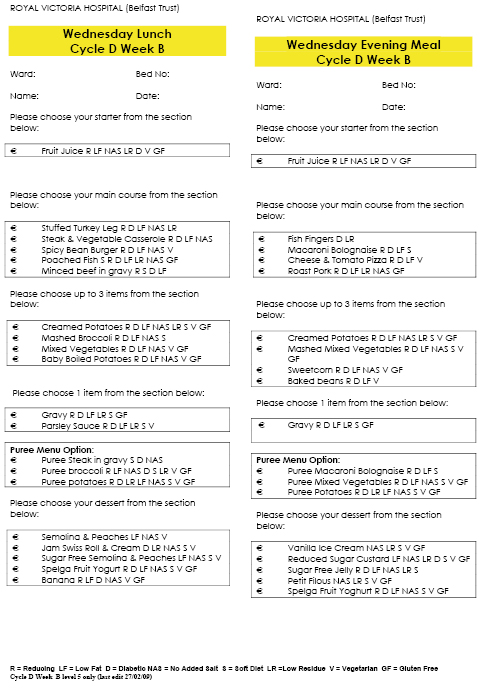
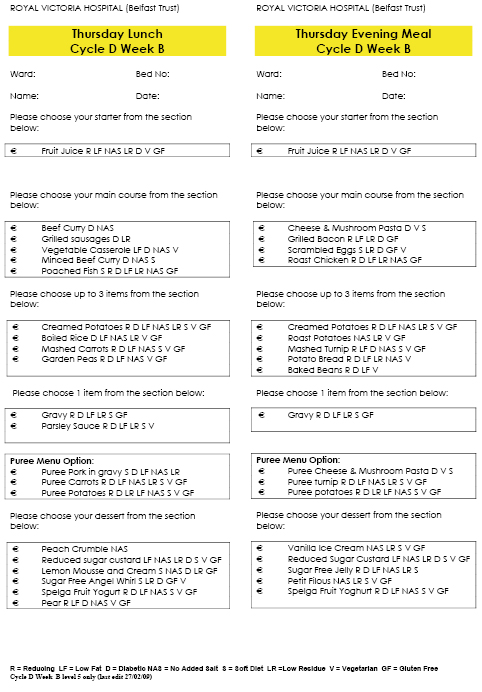
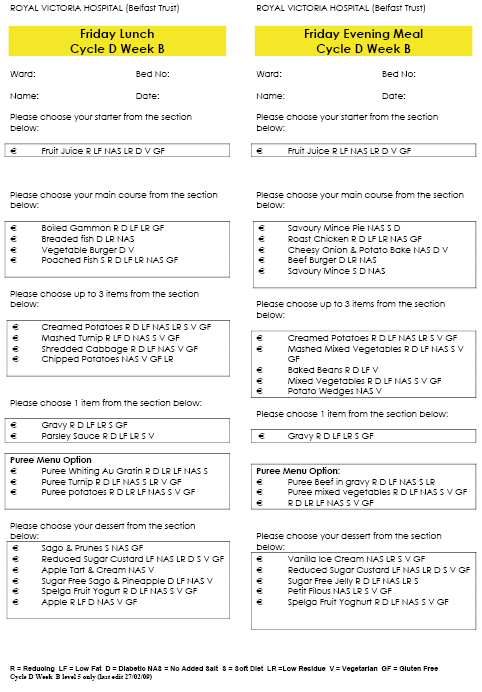
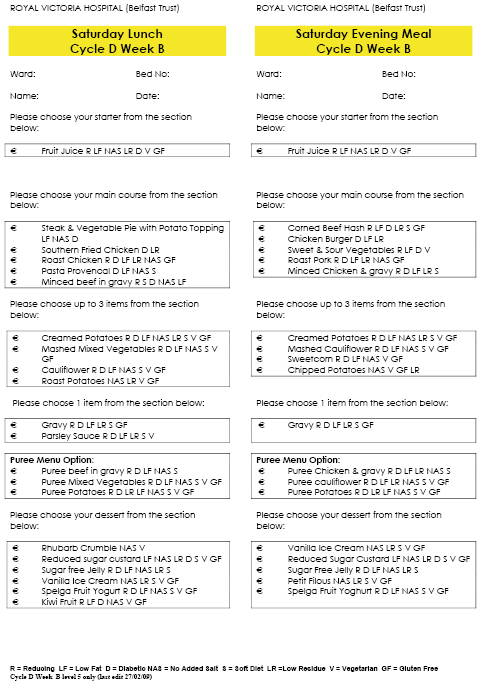
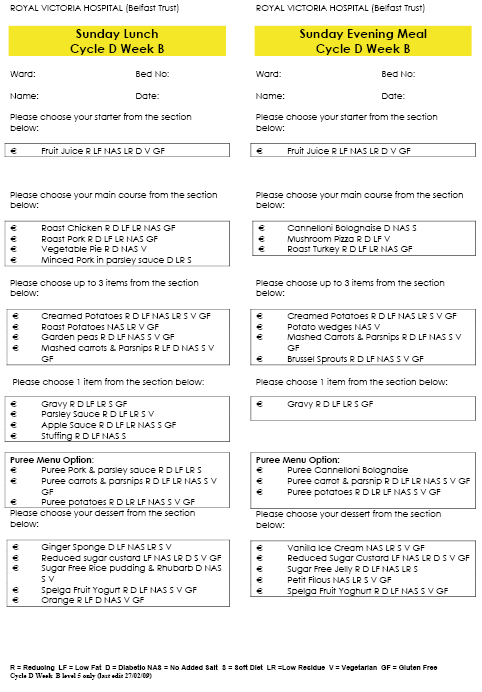
Response from Belfast Trust
about Hospital Menus
Cycle D Week A Knockbracken Wards
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Lunches | ||||||
| Home-made Veg Soup | Leek Soup | Chicken Soup | Asparagus Soup | Home-made Veg Soup | Minestrone Soup | Chicken & Sweetcorn Soup |
| Gammon & Pineapple | Loin of Pork | Southern Fried Chicken | Sausages Bacon | Chicken & Chasseur Sauce | Roast Pork & Apple Sauce | Roast Beef |
| Chicken Curry & Boiled Rice | Steak & Vegetable Pie | Beef Goulash | Minced Steak Pie | Breaded Salmon / Fried Fish | Chicken Pie | Gammon & Pineapple |
| Cheese & Mushroom Omelette | Vegetable Burger | Vegetarian Quiche | Vegetable Spring Roll & Savoury Rice | Pasta Provencale | Cheese & Potato Bake | Baked Bean Hotpot |
| Minced Ham & Parsley Sauce & Mashed Carrot & Parsnip | Minced Steak & Veg & Mashed Mixed Veg | Minced Beef Goulash & Mashed Turnip | Savoury Mince, Mashed Carrot | Minced Whiting, & Mashed Turnip | Minced Chicken & Parsley Sauce Mashed Carrot | Minced Ham & Parsley Sauce & Mashed Cauliflower |
| Puree Ham & Parsley Sauce, Carrot & Parsnip & Potatoes | Puree Steak & Veg, Mixed Veg & Potatoes | Puree Beef Goulash, Turnip & Potatoes | Puree Beef, Carrots & Potatoes | Puree Whiting, Turnip & Potatoes | Puree Chicken & Parsley Sauce, Carrot & Potatoes | Puree Ham, Cauliflower & Potatoes |
| Poached Whiting | Poached Whiting | Poached Whiting | Poached Whiting | Poached Whiting | ||
| Roast Beef Salad | Corned Beef Salad | Tongue Salad | Chicken Salad | Roast Pork Salad | Roast Beef Salad | Mushroom & Mature Cheddar Quiche Salad |
| Mixed Veg | Diced Turnip | Baked Beans | Shredded Cabbage | Sliced Green Beans | Garden Peas | |
| Sliced Green Beans | Garden Peas | Brussel Sprouts | Carrot & Parsnip | Diced Turnip | Sliced Carrots | Cauliflower |
| Carrot & Parsnip | Sliced Green Beans | Roast Potatoes | ||||
| Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes |
| Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes |
| Rhubarb Tart & Custard | Pear & Chocolate Sponge & Custard | Wholemeal Peach Crumble & Custard | Apple Sponge & Custard | Raspberry Mousse | Pineapple Sponge & Custard | Dutch Apple Crumble & Custard |
| Fruit Jelly & Ice-Cream Jelly & Ice-Cream |
Sago & Pineapple | Strawberry Blancmange & Fruit Cocktail | Fruit Jelly & Cream Jelly & Cream |
Lemon Tart & Custard | Rice Pudding & Raisins | Ice Cream & Chocolate Sauce |
| Sugar Free Jelly | Sugar Free Sago & Pineapple | Sugar Free Strawberry Blancmange & Fruit Cocktail | Sugar Free Custard & Apple | Sugar Free Custard & Peaches | Sugar Free Rice Pudding & Raisins | Sugar Free Chocolate Sauce |
| Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt |
| Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt |
| Apple | Orange | Pear | Banana | Apple | Orange | Pear |
Cycle D Week A Knockbracken Wards
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Teas | ||||||
| Beef burger | Tuna & Pasta Bake | Plain Omelette | Whiting Au Gratin | Sausage Roll | Southern Fried Chicken | Fried Fish |
| Chicken & Broccoli Pie | Chicken Salad | Cottage Pie | Chicken Maryland | Braised Liver | Pasta Bolognese | Corned Beef Hash |
| Vegetarian Sausages | Cheese & Onion Pastie | Boiled Gammon | Vegetable Slice | Vegetable Kiev | Vegetable Burger | Spicy Bean Burger |
| Minced Chicken & Gravy & Mashed Broccoli | Mashed Carrot | Mashed Mixed Veg | Minced Whiting Au Gratin & Mashed Carrot & Parsnip | Minced Liver & Mashed Cabbage | Mashed Mixed Veg | Mashed Turnip |
| Puree Chicken & Gravy, Broccoli & Potatoes | Puree Tuna & Pasta Bake, Carrot & Potatoes | Puree Beef, Mixed Veg & Potatoes | Puree Whiting, Carrot & Parsnip & Potatoes | Puree Liver, Cabbage & Potatoes | Puree Pasta Bolognese, Mixed Veg & Potatoes | Puree Corned Beef Hash, Turnip & Potatoes |
| Grilled Bacon | Roast Beef | Loin of Pork | Roast Beef | Bacon | Roast Chicken | |
| Ham, Cheese & Tomato or Tuna & Onion Sandwich | Egg & Onion, Chicken or Corned Beef Sandwich | Salmon, Turkey or Salad Sandwich | Roast Beef, Egg Mayonnaise or Tuna & Onion Sandwich | Chicken, Salad or Cheese Sandwich | Ham, Egg & Onion or Turkey Sandwich | Egg & Onion, Salad or Corned Beef Sandwich |
| Garden Peas | Tomato | Peas & Sweetcorn | Mixed Vegetables | Sweetcorn | Tomato | Baked Beans |
| Baked Beans | Baked Beans | Potato Salad | Coleslaw | Peas | ||
| Tomato | Spicy Slices | |||||
| Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Croquette Potatoes | Creamed Potatoes | Creamed Potatoes |
| Chipped Potatoes | Boiled Potatoes | Potato Wedges | Spicy Slices | Boiled Potatoes | Chipped Potatoes | |
| SUPPER SNACK | ||||||
| Sago | Strawberry Blancmange | Custard | Custard | Rice Pudding & Raisins | Chocolate Blancmange | Custard |
| Sugar Free Sago | Sugar Free Straw-berry Blancmange | Sugar Free Custard | Sugar Free Custard | Sugar Free Rice Pudding & Raisins | Sugar Free Chocolate Blancmange | Sugar Free Custard |
| Pancakes | Carrot Cake | Fruit Bannock | Jam Doughnuts | Veda | Jam Swiss Roll | Shortbread |
| Banana | Pear | Apple | Orange | Pear | Banana | Apple |
| Breakfast | ||||||
| Porridge | Porridge | Porridge | Porridge | Porridge | Porridge | Porridge |
| Sausages | ||||||
| Bacon | ||||||
| Scrambled Eggs |
Cycle D Week B Knockbracken Wards
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Teas | ||||||
| Beef Hotpot | Minced Beef & Lentils | Fish Fingers | Cheese & Mushroom Pasta | Savoury Mince Pie | Corned Beef Hash | Canneloni Bolognese |
| Chicken Salad | Sausage Rolls Quiche Lorraine (Ham & Cheese) | Macaroni Bolognese | Bacon & Potato Bread | Roast Chicken | Chicken Burger | Ham Salad |
| Cheese & Mushroom Omelette | Vegetable Kiev | Cheese & Tomato Pizza | Cheesy Onion & Potato Bake | Sweet & Sour Vegetables & Boiled Rice | Mushroom Pizza | |
| Minced Pork & Gravy & Mashed Mixed Veg | Minced Fish & Parsley Sauce & Mashed Carrots | Mashed Mixed Veg | Mashed Turnip | Savoury Mince & Mashed Mixed Veg | Minced Chicken & Gravy & Mashed Cauliflower | Mashed Carrot & Parsnip |
| Puree Pork & Gravy, Mixed Vegetables & Potatoes | Puree Fish, Carrots & Potatoes | Puree Macaroni Bolognese, Mixed Vegetables & Potatoes | Puree Cheese & M/room Pasta, Turnip & Potatoes | Puree Beef, Mixed Veg & Potatoes | Puree Chicken & Gravy, Cauliflower & Potatoes | Puree Canneloni Bolognese, Carrot & Parsnip & Potatoes |
| Roast Beef | Roast Turkey | Roast Pork | Roast Chicken | Beef Burger | Loin of Pork | Roast Turkey |
| Corned Beef, Ham or Egg Mayonnaise Sandwich | Ham, Cheese or Egg & Tomato Sandwich | Cheese, Salmon & Salad Sandwich | Tuna & Onion, Egg & Onion or Turkey Sandwich | Tuna & Onion, Ham or Salmon Sandwich | Corned Beef, Egg & Onion or Chicken Sandwich | Cheese, Turkey or Ham Sandwich |
| Mixed Vegetables | Tomato | Garden Peas | Spaghetti | Mixed Vegetables | Tomato | Carrots |
| Garden Peas | Baked Beans | Sweetcorn | Tomato | Coleslaw | Garden Peas | Tomato |
| Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes |
| Chips | Boiled Potatoes | Chipped Potatoes | Spicy Slices | Chipped Potatoes | Chipped Potatoes | Potato Wedges |
| Supper Snack | ||||||
| Custard | Semolina Pudding | Lemon Mousse | Sago Pudding | Jelly | Rice Pudding | Custard |
| Sugar Free Custard | Sugar Free Semolina | Sugar Free Angel Whirl | Sugar Free Sago | Sugar Free Jelly | Sugar Free Rice | Sugar Free Custard |
| Chocolate Chip Cake | Veda | Pancake | Shortbread | Jam Doughnuts | Jam Swiss Roll | Fruit Bannock |
| Pear | Apple | Orange | Banana | Pear | Apple | Banana |
| Breakfast | ||||||
| Porridge | Porridge | Porridge | Porridge | Porridge | Porridge | Porridge |
| Sausages | ||||||
| Bacon | ||||||
| Scrambled Egg |
Cycle D Week C Knockbracken Wards
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Teas | ||||||
| Home-made Veg Soup | Asparagus Soup | Minestrone Soup | Leek Soup | Home-made Veg Soup | Minestrone Soup | Chicken & Sweetcorn Soup |
| Stuffed Turkey Leg | Braised Liver | Roast Beef & Yorkshire Pudding | Boiled Gammon & Parsley Sauce | Cottage Pie | Roast Beef | Italian Braised Steak |
| Irish Stew | Chicken Casserole | Chicken & Pasta Bake | Brown Stew | Fried Fish | Roast Chicken | Roast Lamb |
| Mushroom & Mature Cheddar Quiche | Vegetarian Sausages | Cauliflower Cheese | Vegetable Slice | Cheese & Mushroom Omelette | Vegetarian Spring Roll | Cheese & Onion Pastie |
| Minced Irish Stew & Mashed Turnip | Minced Liver & Mashed Carrots | Minced Chicken & Pasta Bake & Mashed Mixed Veg | Minced Ham & P. Sauce & Mashed Cauliflower | Mashed Carrots | Minced Chicken & Parsley Sauce & Mashed Cabbage | Minced Lamb & Beef & Mashed Turnip |
| Puree Irish Stew, Turnip & Potatoes | Puree Liver, Carrots & Potatoes | Puree Chicken & Pasta Bake, Mixed Veg & Potatoes | Puree Ham & P Sauce, Cauliflower & Potatoes | Puree Beef, Carrots & Potatoes | Puree Chicken & Parsley Sauce, Cabbage & Potatoes | Puree Lamb & Beef, Turnip & Potatoes |
| Poached Whiting | Poached Whiting | Poached Whiting | Poached Whiting | Poached Whiting | ||
| Cheese Salad | Roast Pork Salad | Tuna Salad | Tongue Salad | Chicken Salad | Smoked Mackerel Salad | Ham Salad |
| Diced Turnip | Sliced Carrots | Shredded Cabbage | Sliced Green Beans | Garden Peas | Sliced Green Beans | Brussel Sprouts |
| Sliced Green Beans | Garden Peas | Mixed Vegetables | Cauliflower | Carrot & Parsnip | Shredded Cabbage | Carrots |
| Mushy Peas | ||||||
| Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes |
| Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes | Boiled Potatoes |
| Dutch Apple Crumble & Custard | Rhubarb Tart & Cream | Sultana Sponge & Custard | Rice & Fruit Cocktail / Puree Fruit Cocktail | Wholemeal Pineapple Crumble & Custard | Apple Sponge & Custard | Canadian Tart & Custard |
| Semolina & Pineapple | Jam Swiss Roll & Custard | Jelly & Pears/ Ice-Cream | Lemon Tart & Cream | Strawberry Mousse & Cream | Chocolate Blancmange & Pears / Ice Cream | Chocolate Swiss Roll & Cream |
| Sugar Free Semolina & Pineapple | Sugar Free Custard & Fruit Cocktail | Sugar Free Jelly & Pears | Sugar Free Rice & Fruit Cocktail | Sugar Free Custard & Pineapple | Sugar Free Chocolate Blancmange & Pears | Sugar Free Angel Whirl |
| Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt | Fruit Yogurt |
| Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt | Mullerlight Yogurt |
| Apple | Pear | Banana | Orange | Apple | Banana | Orange |
Cycle D Week C Knockbracken Wards
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Teas | ||||||
| Grilled Bacon, Scrambled Egg & Soda Bread | Boiled Gammon | Sausage Roll | Chicken Maryland & Pineapple | Cornish Pastie | Minced Steak Pie | Steak Grill |
| Roast Beef | Roast Beef Salad | Roast Chicken | Chilli Con Carne & Boiled Rice | Roast Loin of Pork & Apple sauce | Stuffed Sausage | Roast Chicken |
| Breaded Salmon Fillet | Cheese & Onion Pastie | Baked Bean Hotpot | Vegetarian Sausage | Macaroni Cheese | Vegetable Tikka & Rice | Vegetable Chilli & Boiled Rice |
| Minced Chicken & Gravy & Mashed Carrots | Minced Ham &Parsley Sauce & Mashed Turnip | Minced Pork & Gravy & Mashed Cabbage | Mashed Carrots | Mashed Broccoli | Savoury Mince & Mashed Mixed Veg | Minced Pork & Parsley Sauce, Mashed Carrots |
| Puree Chicken & Gravy, Carrots & Potatoes | Puree Ham, Turnip & Potatoes | Puree Pork & Gravy, Cabbage & Potatoes | Puree Beef, Carrots & Potatoes | Puree Macaroni Cheese, Broccoli & Potatoes | Puree Steak, Mixed Veg & Potatoes | Puree Pork & Parsley Sauce, Carrots & Potatoes |
| Beef Burger | Roast Chicken | Roast Turkey | Boiled Gammon | |||
| Egg & Onion, Chicken or Salad Sandwich | Corned Beef, Egg & Onion or Chicken Sandwich | Ham, Tuna & Onion or Salad Sandwich | Roast Beef, Chicken or Egg Mayonnaise Sandwich | Tuna & Onion, Cheese & Tomato or Turkey Sandwich | Egg Onion, Ham or Salad Sandwich | Corned Beef, Salmon or Cheese Sandwich |
| Tomato | Sweetcorn | Carrots | Baked Beans | Spaghetti | Garden Peas | |
| Peas | Garden Peas | Spaghetti | Coleslaw | Carrots | Mixed Veg | Baked Beans |
| Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes | Creamed Potatoes |
| Chips | Potato Wedges | Spicy Slices | Boiled Potatoes | Boiled Potatoes | Croquette Potatoes | |
| Chipped Potatoes | Chipped Potatoes | |||||
| Supper Snack | ||||||
| Custard | Jelly | Rice Pudding | Strawberry Mousse | Chocolate Blancmange | Custard | Jelly |
| Sugar Free Custard | Sugar Free Jelly | Sugar Free Rice Pudding | Sugar Free Custard | Sugar Free Chocolate Blancmange | Sugar Free Angel Whirl | Sugar Free Jelly |
| Veda | Carrot Cake | Pancake | Chocolate Chip Cake | Shortbread | Fruit Cake | Fruit Bannock |
| Orange | Banana | Apple | Pear | Orange | Apple | Pear |
| Breakfast | ||||||
| Porridge | Porridge | Porridge | Porridge | Porridge | Porridge | Porridge |
| Sausages | ||||||
| Bacon | ||||||
| Scrambled Eggs |
Response from Northern Trust
about Hospital Menus
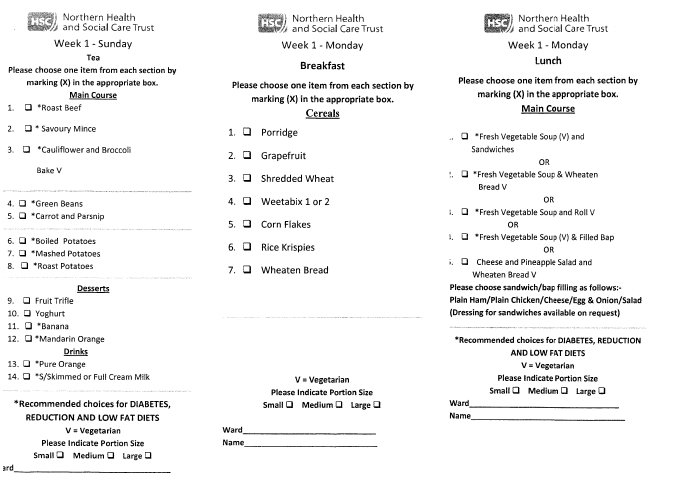
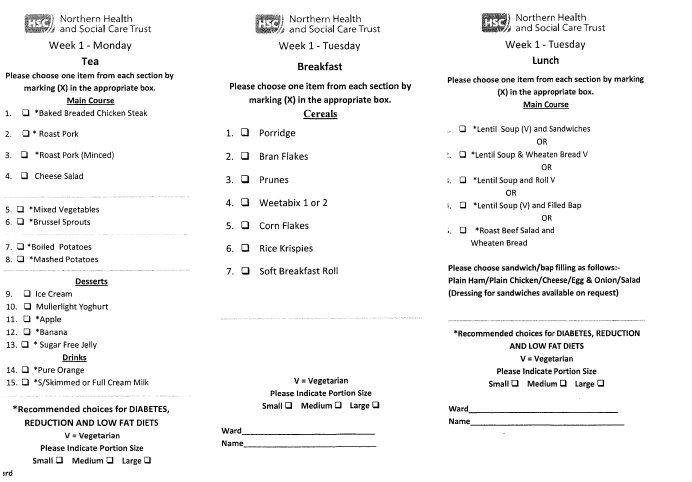
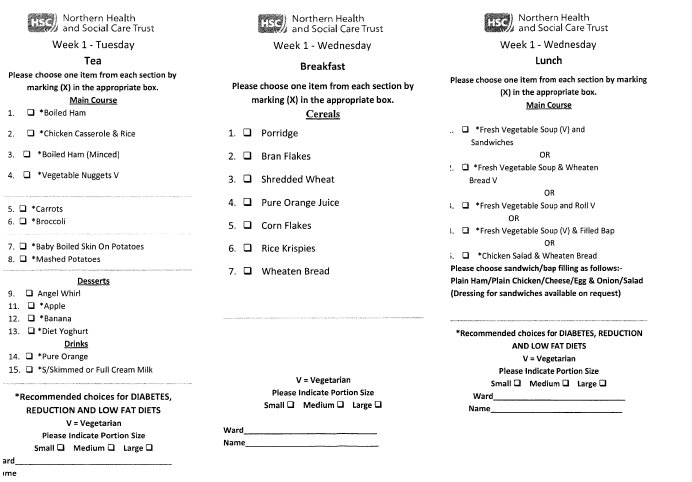
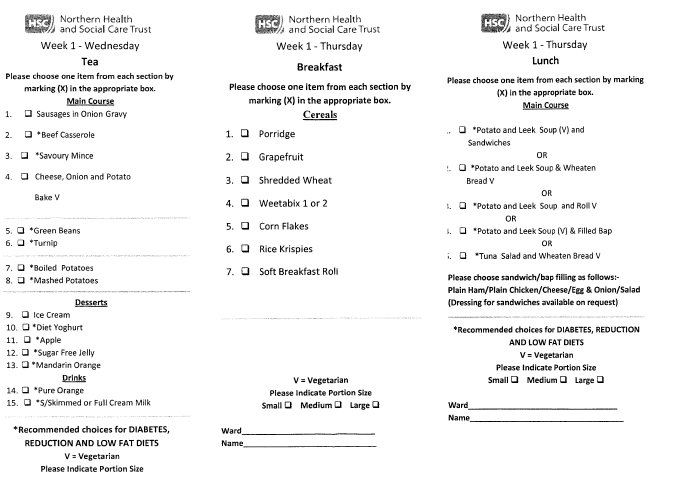
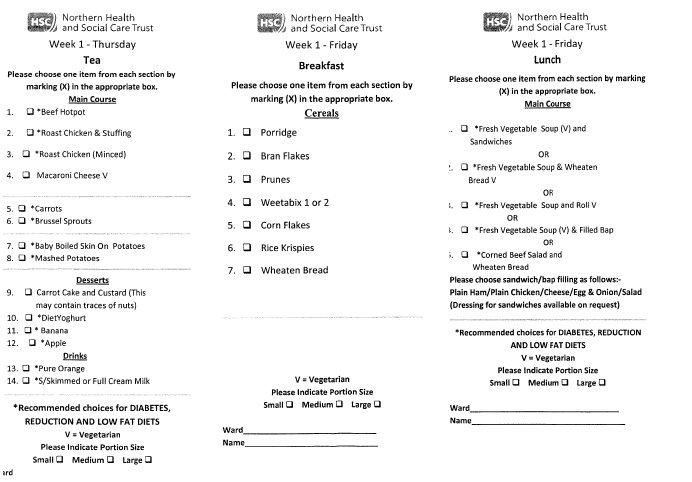
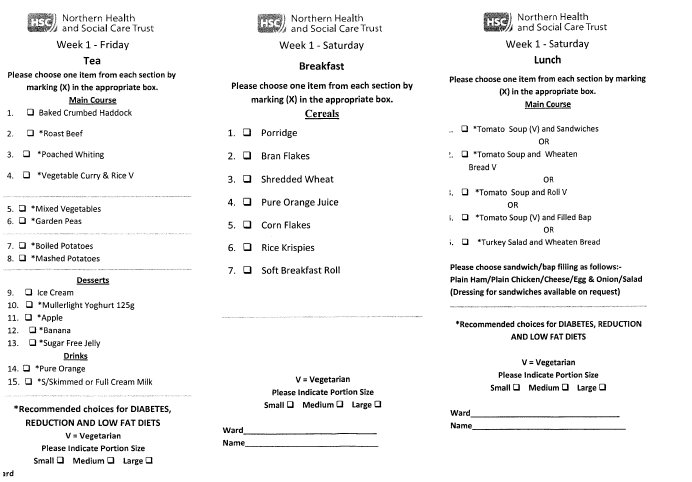
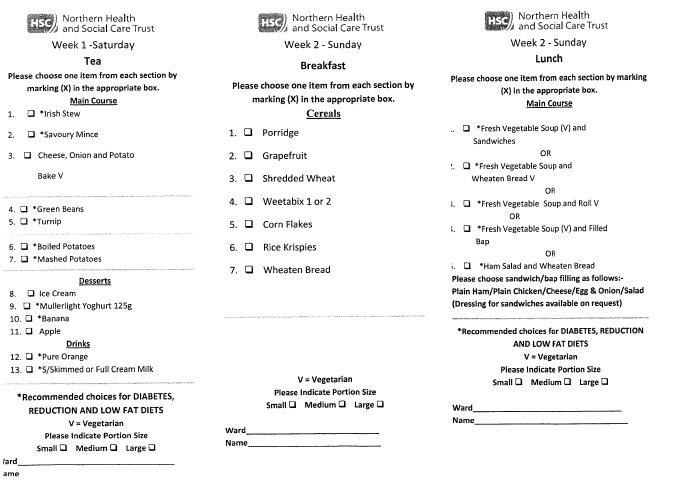
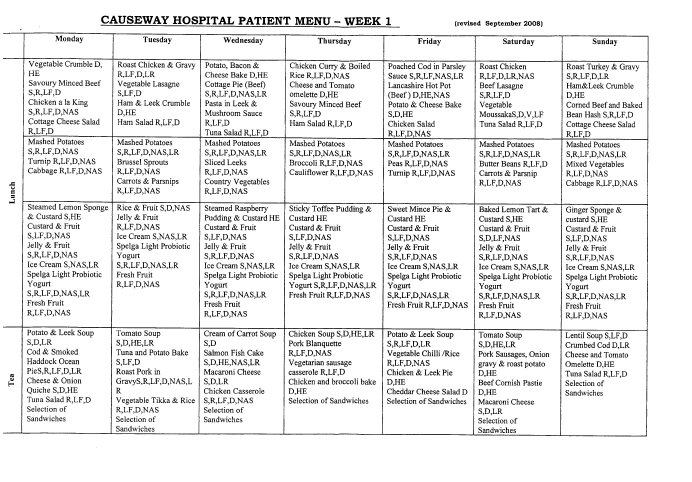
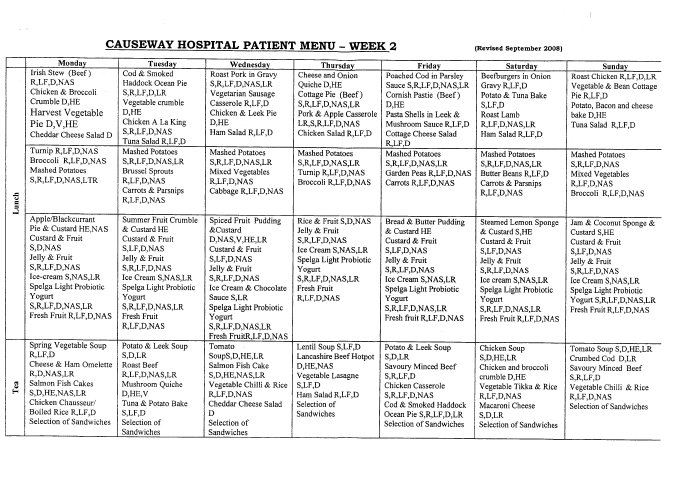
Response from Southern Health and
Social Care Trust about Hospital Menus
Michelle O’Neill MLA
Deputy Chairperson
Committee for Health, Social Services and Public safety
Room 412
Parliament Buildings
BELFAST
BT4 3XX
8th April 2009
Dear Mrs O’Neill
I refer to your query of 20th March 2009 received on 27th March 2009 regarding samples of hospital menus.
I attached same for your perusal; any queries do not hesitate to contact me.
Yours sincerely
Mrs Anita Carroll
Assistant Director – Acute Services
Functional Support Services
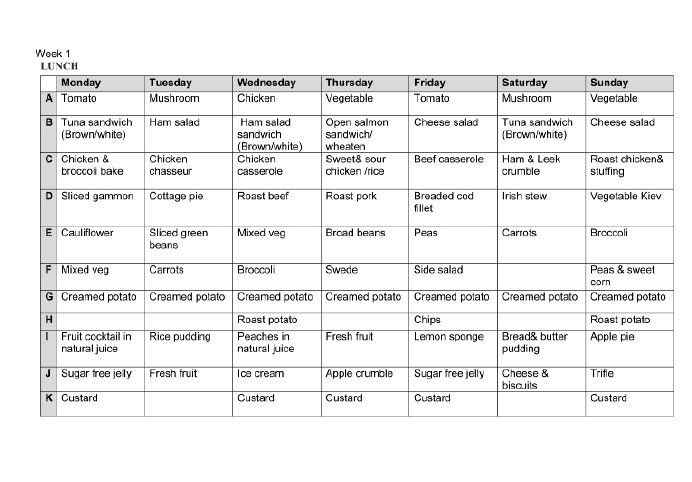
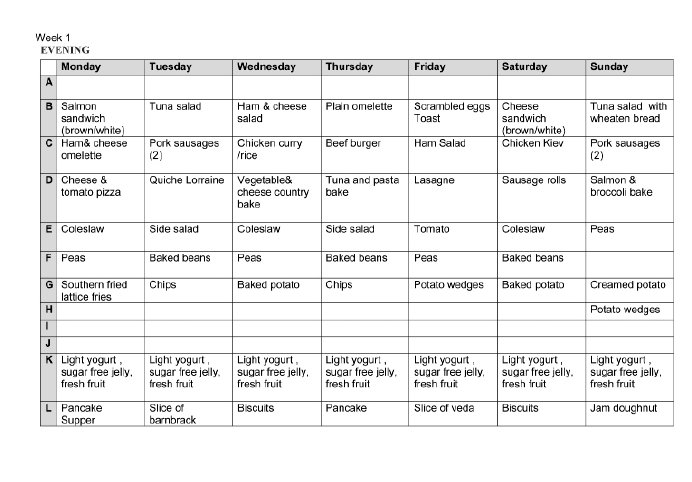
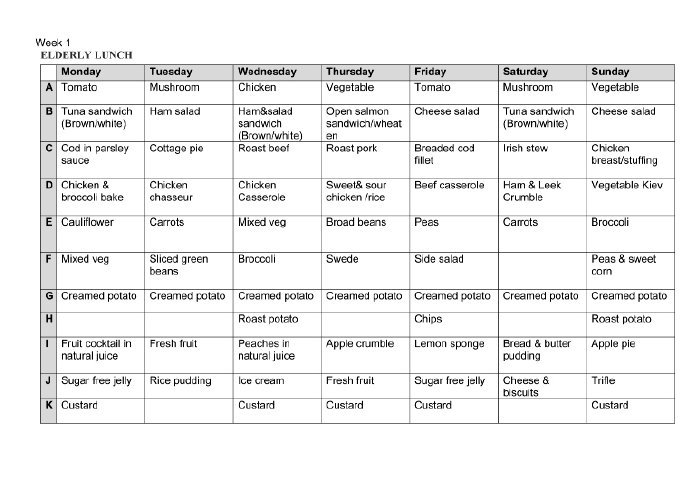
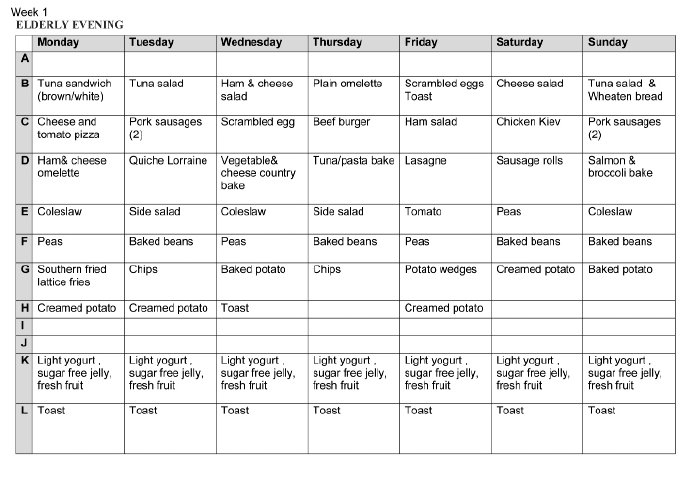
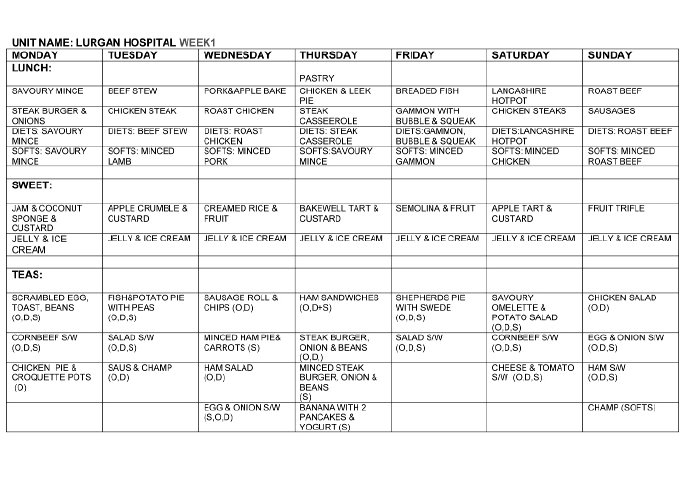
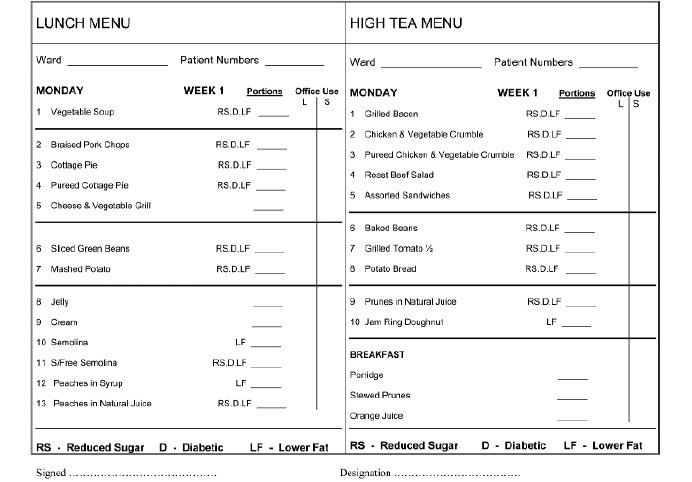
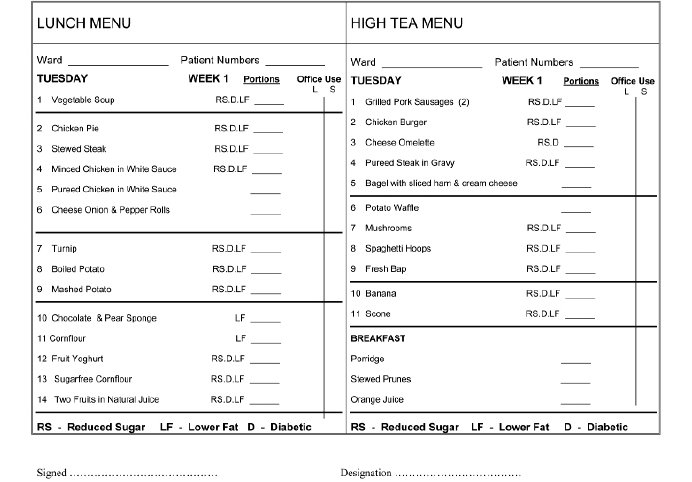
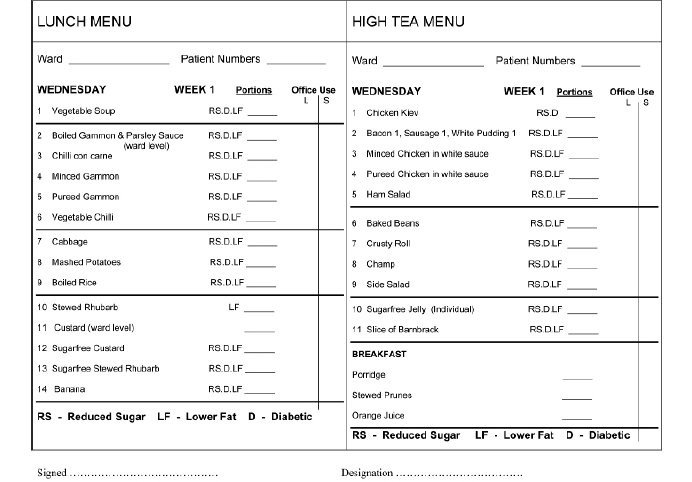
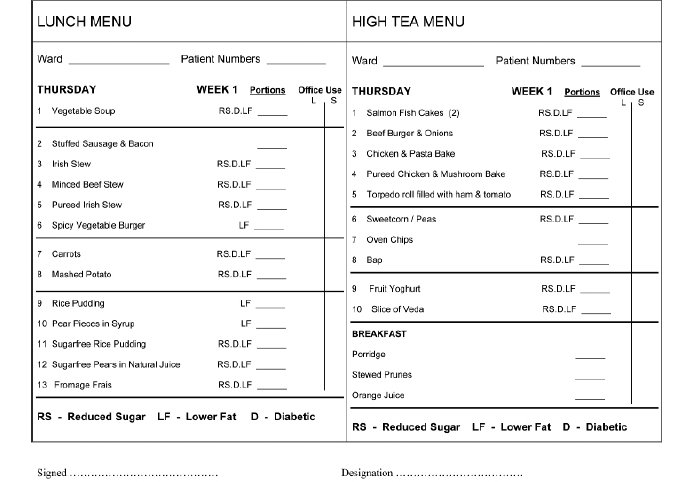
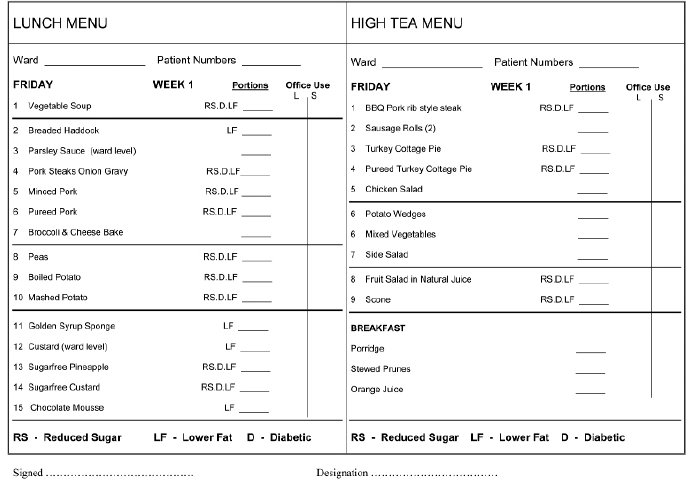
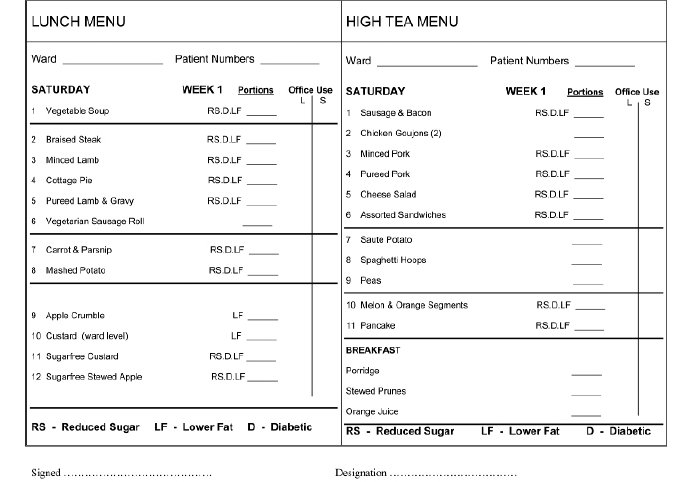
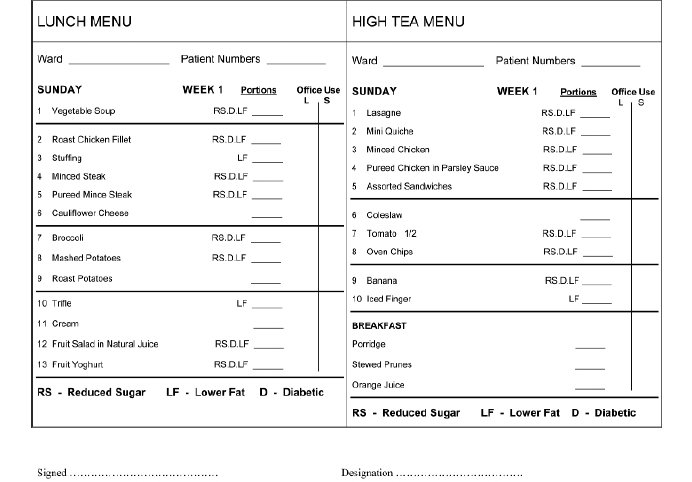
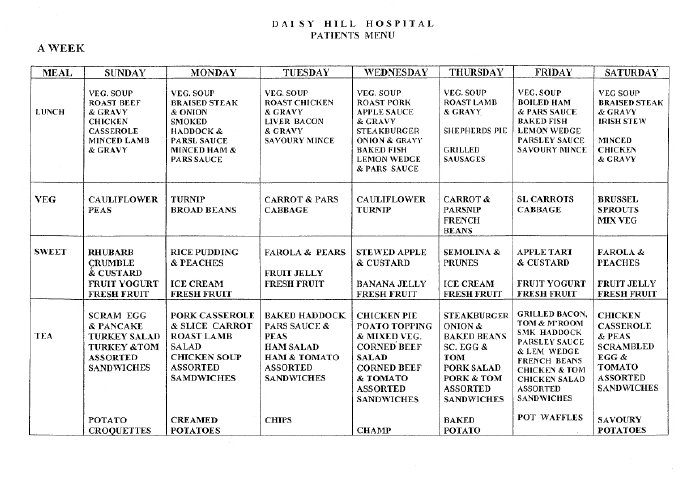
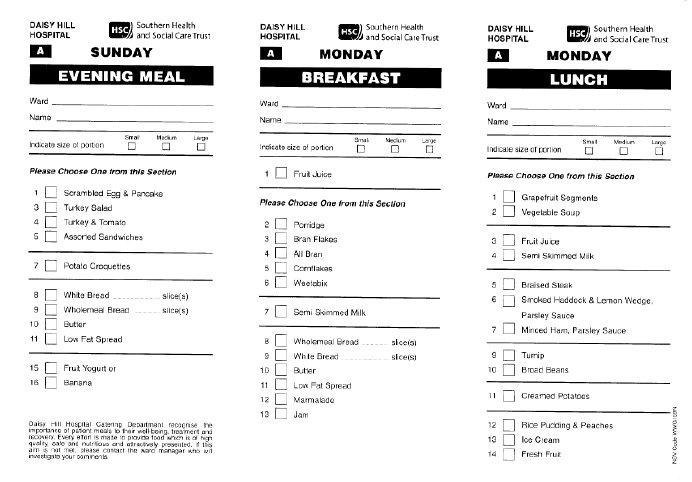
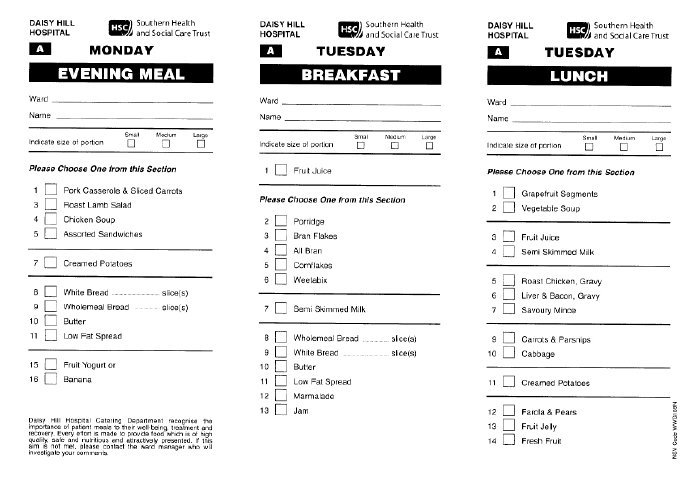


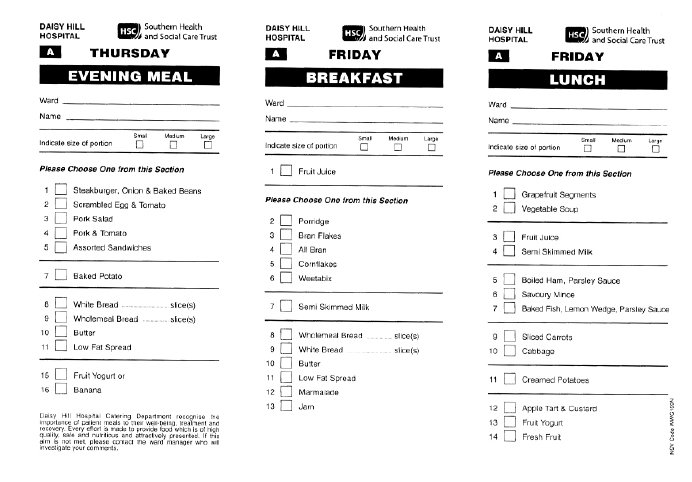
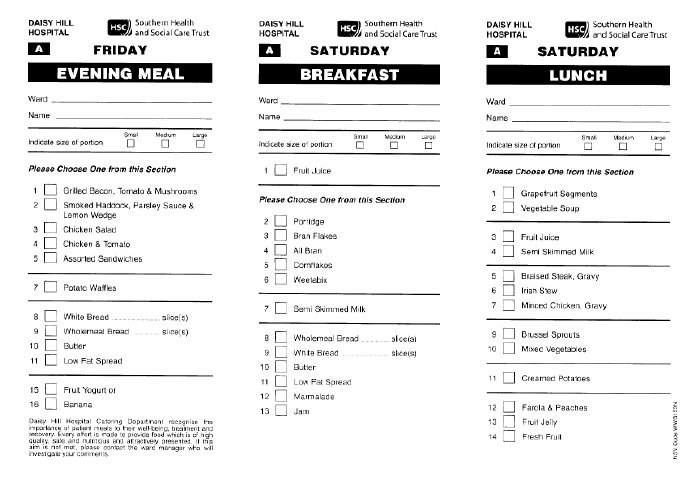
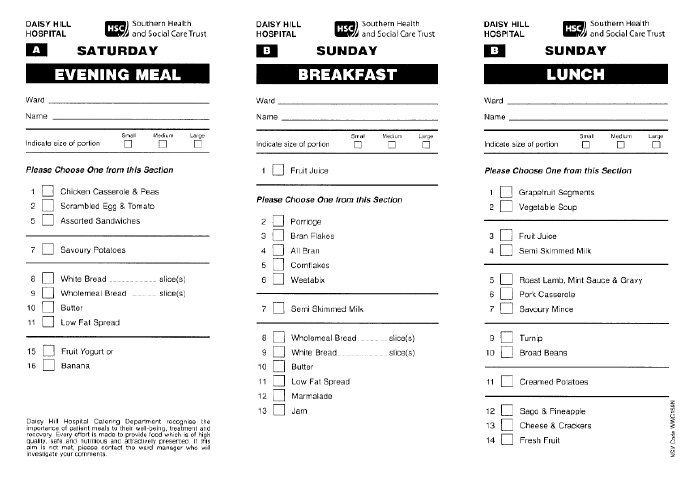
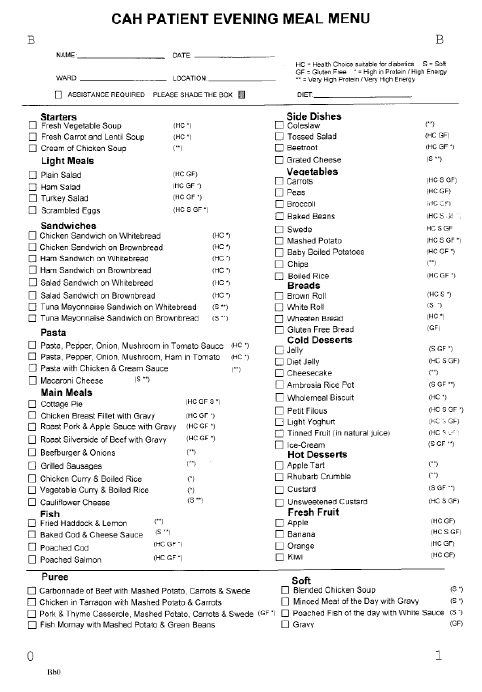
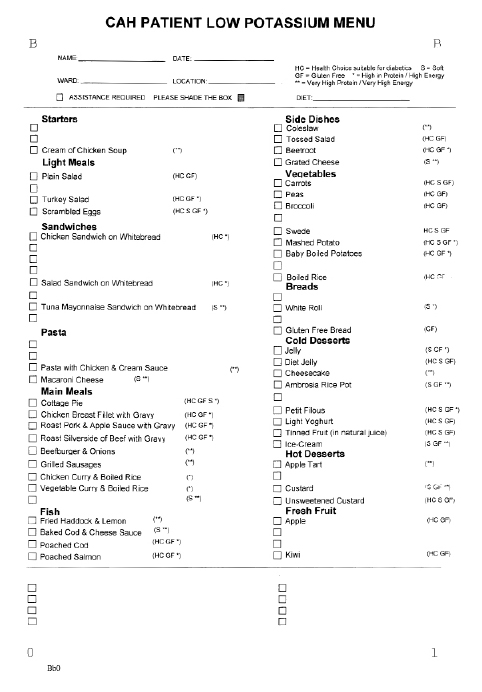
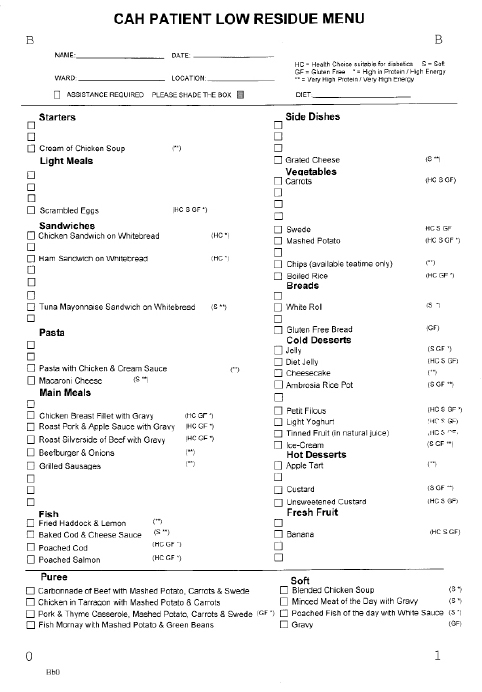
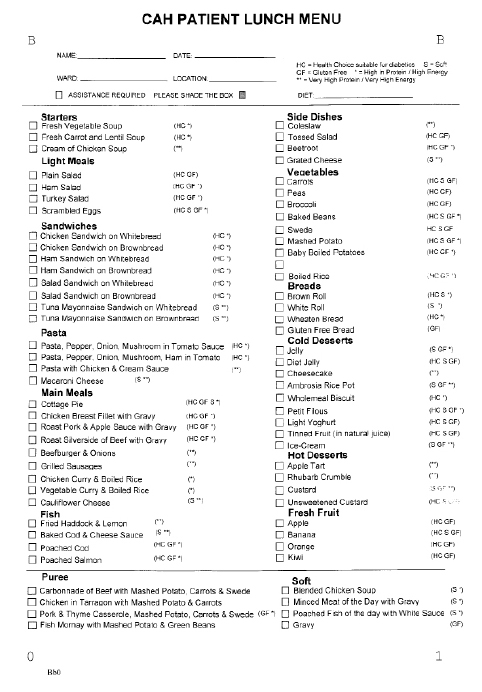
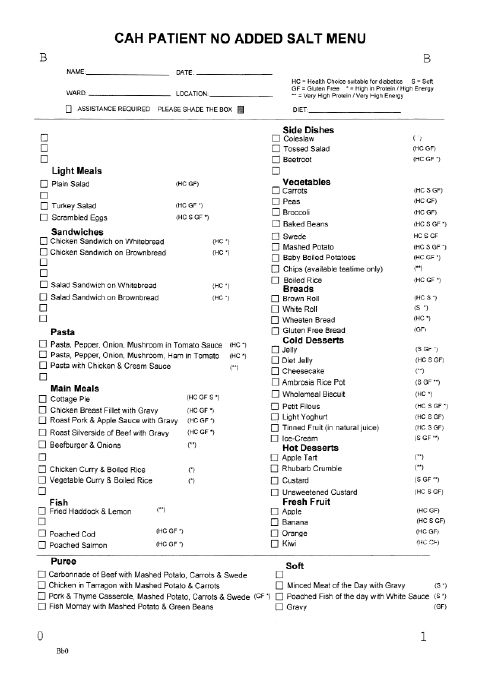
Tabled-presentation from Sport NI
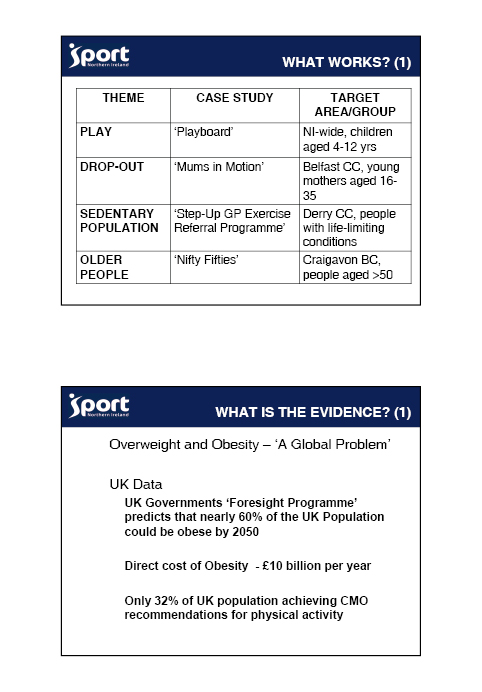
_fmt.jpeg)
Research Paper 20th of February 2009
Obesity Inquiry Research Paper
This research paper provides an introduction to the issue of obesity and its increasing prevalence throughout the population in Northern Ireland.
The paper identifies the extent overweight and obesity levels in Northern Ireland and the policy response from the DHSSPS in tackling this challenging public health issue. The paper also highlights the key causes and risk factors associated with obesity and provides a comparative overview of a number of interventions and treatments currently employed in the UK and internationally.
Library Research Papers are compiled for the benefit of Members of The Assembly and their personal staff. Authors are available to discuss the contents of these papers with Members and their staff but cannot advise members of the general public.
Contents
1. Introduction – Obesity – A Global ‘Epidemic’ 646
2. Obesity Prevalence 648
2.1 Measuring Obesity – Body Mass Index (BMI) 648
2.2. United Kingdom and the Republic of Ireland 649
3. Causes and Risk Factor of Obesity 649
3.1 Overview of the Causes of Obesity – Energy Imbalance 649
3.2 Biological Causes and Risk Factors 650
3.2.1 Genetics and Genomics 650
3.2.2 Hormonal and neural pathways and feedback loops 652
3.3 Impact of Early Life and Growth Patterns 652
3.4 Behaviour 653
3.5 The Living Environment – Obesogenic Environment 655
3.6 Health Inequalities 656
4. Obesity in Northern Ireland 656
4.1 Levels of Obesity 656
4.2 Impact of obesity in Northern Ireland – Health and Economic Costs 658
4.3 Developing a strategic policy response to obesity in Northern Ireland 659
4.3.1 Progressing Fit Futures – Developing a coherent policy framework 659
4.3.2 NIAO Report on Obesity and Type 2 Diabetes 660
4.3.3 Adopting a Life Course to tackle obesity 661
5. Intervention and Treatments for Obesity 661
5.1 Intervention - Introduction and General Approaches 661
5.2 Interventions for individuals – Primary Care 664
5.3 Interventions for Individual – Secondary Care (Bariatric Surgery) 665
5.4 Community Interventions – Good Practice Examples 666
5.4.1 Northern Ireland 666
5.4.2 Other UK Examples 667
5.4.3 International Examples 669
6. ‘Building A Sustainable Response’ (Foresight Report (2007)) 669
Appendix 1 671
Appendix 2 675
1. Introduction - Obesity – A Global ‘Epidemic’
Overweight and obesity can be defined ‘as abnormal or excessive fat accumulation that may impair health’.[1] The obesity issue has generated considerable debate fuelled by concerns of the World Health Organisation (WHO) and governments around the world that obesity prevalence has reached epidemic levels. A number of observers contest the general consensus of rising obesity levels by arguing that the ‘myth of obesity’ is perpetuated by the state seeking to exert a ‘big brother’ influence over the personal lives of its citizenry.[2] The majority view, based on extensive government and independent research is that obesity represents one of the most complex public health issues confronting governments in the decades ahead.
In recent decades, there has been a significant increase in overweight and obesity prevalence rates in many countries around the world. According to the WHO, ‘excess body weight poses one of the most serious public health challenges of the 21st century.’[3] The WHO’s latest projections indicate that globally in 2005 there were approximately 1.6 billion adults (15 years and over) overweight and at least 400 million obese. In Europe, the WHO contends that the rapidly increasing prevalence of obesity will include 150 million adults and 15 million children by 2010.[4]
Even in the developing world there is evidence that levels of overweight and obesity are increasingly affecting population health, many of who already suffer from the affects of malnutrition. A 1999 United Nation (UN) study discovered obesity in many developing regions and growing rapidly, even in countries where hunger exists. In China, the number of overweight people jumped from less than 10 per cent to 15 per cent in just three years. In Brazil and Colombia the figure at the turn of the century was round 40 per cent, while even in sub-Saharan Africa, where the majority of the world’s hungry live, obesity levels are increasing, especially among urban women. In addition to these figures, the study also revealed that there was a correlation between rising income and increasing obesity prevalence throughout these developing regions.
Another interesting finding within the UN report was the connection between obesity and micronutrient deficiency. Despite the rise in levels of overweight as well as those suffering from starvation, the study argued that both groups were being deprived of important micronutrients like vitamins and minerals. According to a Senior Officer in the UN’s Food and Agriculture Organisation, ‘The thinking used to be that if people get enough energy in their diets, the micronutrients will take care of themselves…But increasingly people are eating larger quantities of cheap food that fill the stomach but still leave the body without those micronutrients’.[5]
Figure 1: The growing epidemic of obesity[6]
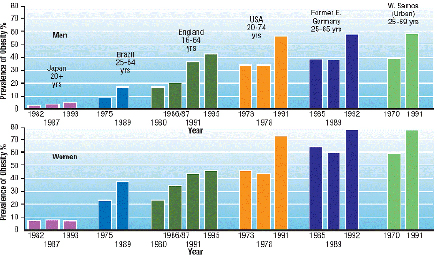
Another interesting finding within the UN report was the connection between obesity and micronutrient deficiency. Despite the rise in levels of overweight as well as those suffering from starvation, the study argued that both groups were being deprived of important micronutrients like vitamins and minerals. According to a Senior Officer in the UN’s Food and Agriculture Organisation, ‘The thinking used to be that if people get enough energy in their diets, the micronutrients will take care of themselves…But increasingly people are eating larger quantities of cheap food that fill the stomach but still leave the body without those micronutrients’.[7]
A major part of the explanation for the WHO’s forecast in relation to the long-term challenge presented by obesity is the widespread and embedded nature of the condition within many modern western societies. While acknowledgement of the acuteness and prevalence of obesity is a relatively recent development, the transition of modern societies characterised by increasing obesity levels has been occurring over the last three decades. Research commissioned by the UK Government’s Foresight programme examining ways of tackling obesity, revealed that, ‘the causes of obesity are embedded in an extremely complex biological system, set within an equally complex societal framework [and] will take several decades to reverse those factors driving current obesity trends.’[8]
A recurrent conclusion within the substantial body of research undertaken into obesity is that while effectively tackling the condition may seem straightforward i.e. reduce energy-dense food and drink consumption and engage in more regular physical activity, the reality is rather different. The primary factor contributing to the complexity of obesity is that ‘energy imbalance’ is determined by a ‘complex multifaceted system of determinants or causes’. Part of this complexity is the need to effectively tackle the societal impact of the rapid pace of technological revolution that began in the previous century and continues to contribute significantly to the development of an increasingly ‘obesogenic environment’. The incremental movement towards these environments comprise a whole range of social, cultural and infrastructural conditions which compromise an individual’s ability to adopt a healthier lifestyle.
Effective intervention in tackling the growing problem of obesity and overweight has become a priority at the centre of public health strategies around the world. A major part of the explanation for this lies in the significant consequences on health and the economy generated by increasing obesity prevalence rates across the population. Firstly, the direct medical consequences of obesity are well known and include coronary hearth disease, a number of cancers including breast and colon cancer, as well as a number of orthopaedic conditions. Secondly, policymakers are increasingly concerned that the growing obesity problem will place a substantial financial burden on their respective health finances. This is particularly pertinent within the four universal, tax-funded health systems of the NHS. According to the 2007 Foresight report (Butland et al) in the UK ‘by 2050, 60 per cent of males and 50 per cent of females could be obese, adding £5.5 billion to the annual cost of the NHS, with wider costs to society and business estimated at £49.9 billion.’[9]
2. Obesity Prevalence
2.1 Measuring Obesity – Body Mass Index (BMI)
One of the key mechanisms routinely employed in the measurement of obesity prevalence around the world is the Body Mass Index (BMI). BMI is a simple index of weight-for-height (weight in kilograms divided by the square of the height in metres) and is recognised by the WHO as the most useful mechanism in providing a population-level measurement of overweight and obesity. It is important to note, however, that it is also widely recognised that there are certain limitations associated with BMI. The WHO has advised that figures derived from the BMI should be employed as a rough guide as they may not accurately reflect the same degree of fatness in different individuals.[10] These limitations are particularly apparent in the measurement of childhood overweight and obesity as height and weight continue to change as children grow. Recent research has advocated the measurement of waist circumference as being more closely associated with mortality and morbidity than BMI.[11]
Figure 2: Body Mass Index Classifications[12]
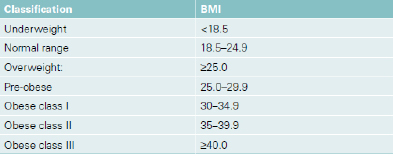
2.2 United Kingdom and the Republic of Ireland
Obesity is defined as someone within a BMI of 30 or over. According to the WHO Europe Regional Database, in the UK, 62.3 per cent of adults (aged 16 years and over) are overweight with a BMI of 25 and over, with 24.4 per cent of these adults obese. Meanwhile, in the Republic of Ireland, the 2007 Survey of Lifestyle, Attitudes and Nutrition in Ireland (SLAN) reported that 39 per cent of the adult population were overweight and 25 per cent were obese. Following a similar trend in the UK, overweight and obesity levels in the Republic of Ireland have continued to rise or remained the same over the period of the previous two surveys in 1998 and 2002. Obesity levels based on self-reported data have increased over the period of the three surveys, from 11 per cent in 1998 to 15 per cent in 2002 and levelled off at 14 per cent in 2007. Overweight levels have increased between 1998 (31 per cent) and 2002 (33 per cent) and increased again in 2007 (36 per cent).[13] While these figures do not include measured BMI of individuals and are reliant on self-reported data through completion of questionnaires, the data indicates there has been a significant rise in the prevalence of overweight and obesity in the Republic of Ireland in the last decade.
It is important to note the difficulties associated with collating accurate data across the different jurisdictions. In her review of the comparative analysis of anti-obesity policies in operation throughout the devolved regions, Musingarimi highlights a number of points which currently undermine the comparative analysis of the prevalence rates across the UK. Firstly, she points to the fact that in the UK data on health (including overweight and obesity) are collected separately in the devolved regions and currently there is no single UK-level obesity surveillance survey undertaken. Secondly, following on from the point made earlier relating to prevalence rates in the Republic of Ireland, there are reliability issues around the methodologies employed in data collection. For example, data for England and Scotland use actual measurements of height and weight while in Wales and Northern Ireland, less-reliable self-administered questionnaires – which are known to result in underestimation of prevalence are employed.[14]
3. Causes and Risk Factors of Obesity
3.1 Overview of the Causes of Obesity - Energy Imbalance
Historically, obesity had been thought to be only a simple matter of an imbalance of the equation between energy intake and energy expenditure. However, research has now indicated that many factors involved in why an individual may become obese including genetic, physiological and behavioural factors.
Energy is consumed in the diet through protein, carbohydrate and fat and excess calories are subsequently converted and stored as triglycerides[15] in adipose tissue (body fat). Over time, consumption of excess calories, without an increase in energy expenditure, will cause excess body fat to be stored which may lead to obesity. Energy expenditure is composed of basal metabolic rate, the thermic effect of food and physical activity (including both activity-related thermogenesis[16] [volitional exercise] and non-activity related exercise thermogenesis [all other activity not related to ‘sporting-like’ exercise]). It has been estimated that spontaneous minor activity performed during the day accounts for 20 per cent of the differences of energy expenditure between individuals in a 24 hour period.[17]
Although the specific causes of obesity at an individual level are varied it is accepted that, ‘At the heart of obesity lies a homeostatic biological system that struggles to maintain energy balance to keep the body at a constant weight. This system is not well-adapted to a fast-changing world, where the pace of technological progress has outstripped human evolution’.[18] It is also now accepted that ‘changes in the external environment have revealed this underlying tendency to gain weight in more of the population…the technological revolution of the 20th Century has left in its wake an ‘obesogenic environment’ that serves to expose the biological vulnerability of human beings’.[19]
The following sections of this paper discuss key causes and risk factors of obesity in more detail, including:
- Biological causes and risk factors, including genetics and hormonal and neural pathways;
- Impact of early life and growth patterns;
- Behaviour with respect to eating and physical exercise;
- The living environment – obesogenic environment; and
- Health Inequalities.
3.2 Biological Causes and Risk Factors
Food is a fundamental biological necessity, so the body has evolved that the ‘hunger drive is very powerful…by contrast, there is limited sensitivity to abundance. The feelings of having had enough (satiety clues) are weak and easily overridden by external factors such as the sight of food and how it tastes’.[20] Evidence from research ‘argues against any difference in basic physiology between the slim and obese, or any mechanism that somehow protects lean individuals from weight gain by the stimulation of specific metabolic pathways when faced with an energy excess’.[21]
3.2.1 Genetics and Genomics
It is believed that any explanation of the obesity epidemic must include the role of genetics as well as the role played by the environment,
One commonly quoted genetic explanation for the rapid rise in obesity is the mismatch between today’s environment and ‘energy-thrifty genes’…according to the ‘thrifty-genotype’ hypothesis, the same genes that helped our ancestors survive occasional famines are now being challenged by environments in which food is plentiful year round…the thrifty genotype is just part of a wider spectrum of ways in which genes can favour fat accumulation in a given environment.[22]
Genomics is the study of the entire human genome and involves studying individual genes as well as the interactions of multiple genes with each other and with the environment. Research highlights that considering the obesity epidemic from a genomics perspective, has the potential to improve the effectiveness of prevention and intervention strategies. However, it is not yet possible to allow for a personalised obesity intervention based on genetic predisposition.[23]
Only 1 per cent – 5 per cent of obesity cases can be explained by a single gene mutation,[24] however, common obesity (which effects most people with obesity) ‘is a complex disorder with contributions from multiple genes and gene variants…the search for specific genes…provides a foundation for understanding the effect of environmental and lifestyle factors’.[25] Evidence suggests that genetic factors are involved in all aspects of weight regulation, including appetite, eating behaviour, taste, satiety, thermogenesis[26] and motivation to exercise. More than 400 genes or markers have now been associated with obesity and some of the more commonly discussed genes and their characteristics are listed in the table below:
Examples of Genes Involved in Obesity and Their Associated Phenotypes[27]
| Gene | Associated Phenotype (Characteristic) |
| Leptin | Satiation, metabolism |
| Melanocortin | Feeding behaviour, binge eating |
| Ghrelin | Appetite stimulation |
| Neuromedin ß | Feeding behaviour, satiety |
| PROP | Taste preference |
| PPAR | Fat metabolism |
| Mitochondrial uncoupling proteins | Energy expenditure |
| Melanocortin and MC4R | Energy expenditure |
Some recent genetic findings include:
- The impact of the FTO allele,[28] described as ‘the most clear genetic link yet to obesity in the general population’ people carrying one copy of the FTO allele have a 30 per cent increased risk of being obese compared to a person with no copies. A person carrying two copies of the allele has a 70 per cent increased risk of being obese, being on average 3Kg heavier than a similar person with no copies of the allele, ‘among white Europeans, approximately one is six people carries both copies of the allele’[29];
- In 2008, in a genetic study of more than 90,000 people, researchers identified six new genetic variants that are associated with increased Body Mass Index. Five of the genes ‘are known to be active in the brain, suggesting that many genetic variants implicated in obesity might affect behaviour, rather than the chemical processes of energy or fat metabolism’[30]; and
- In January 2009, scientists published the results of a ten year study which looked at the genetic makeup of obese children under six and morbidly obese adults, most of whom had been obese since childhood or adolescence, and compared this with age matched people of normal weight. The study revealed three new genetic variations linked to the risk of severe obesity.[31] Further research is needed to establish whether or not these gene variants are acting independently or together to increase risk of obesity.[32]
3.2.2 Hormonal and neural pathways and feedback loops
Numerous circulating peptides and steroids (produced in the body by fat cells, the gastrointestinal tract and the endocrine pancreas) influence appetite through their actions on the hypothalamus,[33] the brain stem and the autonomic nervous system[34]. Analysis of the function of genes involved with obesity has identified important hormonal and neural pathways and feedback loops, especially for the hormone leptin and for the melanocortin system. Researchers are currently investigating anti-obesity therapies based on these naturally occurring hormones and neurotransmitters. It is believed that control of appetite and the hormonal and neural systems underpinning this control will be key to weight control strategies.[35]
These hormonal and neural pathways provide the more immediate links between emotional cues to eat, food ingestion, and absorption, including the stimulation of gut hormones and the release of insulin. Longer-term control of energy is provided by feedback loops which come in part from fat (adipose) tissue itself. Leptin is a good example of one of the molecules involved in the control of energy intake and appetite control. It is now believed that falling levels of leptin stimulates hunger and food seeking behaviour to increase food intake when body weight is low. ‘Some constitutionally lean individuals may have a finely tuned appetite control system that precisely matches energy intake to meet energy needs. Other individuals may have a poorly tuned control system in which food intake is persistently above energy needs, making them more susceptible to obesity’.[36]
The melanocortin system is believed to be the best characterised neuronal pathway involved in the regulation of energy homeostasis. It is likely to be involved in integrating long-term adipostatic signals from leptin and insulin, received by the hypothalamus, with acute signals regulating hunger and satiety, primarily received by the brain stem.[37]
3.3 Impact of Early Life and Growth Patterns
It is accepted that the pattern of growth during early life is one determinant of the future risk of obesity. ‘A baby’s growth rate in the womb and beyond is in part determined by parental factors, especially with regard to the mother’s diet and what and how she feeds her baby’.[38] In common with other research around the world, which has demonstrated that undernutrition and stunting of growth in early life promote adult obesity, a recent discovery of a collection of over 8500 child growth records in Helsinki, Finland has shown that the pattern of growth that leads to obesity-related disease actually begins with low birthweight and small body size during infancy,
A sample of 2003 people in the Helsinki cohort, selected at random…show that small body size at birth, low BMI at 2 years and increase in BMI between 2 and 11 years are linked to the development of insulin resistance, a known risk factor for coronary heart disease and type 2 diabetes.[39]
The period soon after birth is believed to be a time of ‘metabolic plasticity’ and while there is less evidence of a link between actual birth weight and obesity, it is weight gain in early life that appears to be the critical issue. Breast-fed babies show slower growth rates than formula-fed babies and this may contribute to the reduced risk of obesity later in life. It appears that low birth weight babies may be susceptible to a catch-up rapid weight gain while other babies may experience this as a direct result of their diet. Weaning practices have also been implicated in a risk of later obesity. Despite the need for more research, work to date suggests that ‘early life is a critical period for health development’.[40]
Research work is ongoing within the UK to identify genetic, dietary and other factors that act during fetal and infant life, with the aim of identifying the factors of early infant diet and growth that predict childhood obesity and to develop and test interventions to avoid excessive infant weight gain and childhood obesity.[41]
A study involving over 8000 children aged 7, has highlighted eight key factors associated with an increased risk of childhood obesity at the age of 7.[42] The factors included those outlined above:
- Birth weight;
- Size in early life, measured at 8 and 18 months;
- Rapid weight gain in the first year of life;
- Rapid catch-up growth between birth and two years of age; and
- Early development of body fatness in pre-school years i.e. before the age at which body fat should be increasing (at the age of 5-6).
- The following additional factors were also identified:
- Obesity in one or more parents;
- More than eight hours spent watching TV a week at the age of three; and
- A short amount of sleep – less than 10.5 hours a night at the age of three.
3.4 Behaviour
Energy balance is influenced by two main behaviours, eating behaviour (shaped by drive to eat and opportunity to eat) and physical activity (shaped by individual metabolic predisposition and the environment of the individual). When considering the role of behaviour in obesity, ‘organisational behaviours play a substantial but often unconsidered role in cuing the behaviours of individuals. For example, it is organisations that make decisions about the range of snacks in the workplace, the availability and content of vending machines, and whether employees receive incentives to use cars but no incentives to use bicycles.[43]
The influence of family behaviour on children is important as children are more likely to be obese if one or more of their parents are obese. This is not just genetic but the home environment and the attitudes and behaviours of parents and family members also contribute to this increased risk for children.[44]
It has been recognised that,
...observational studies of human behaviour in this area are hampered by the lack of robust, objective measures of dietary intake and physical activity and by behavioural and attitudinal measures in large populations". However, “it is now widely accepted that there are subtle shifts in both diet and physical activity that influence obesity trends, and at a population level, may be below the limits of detection of current methodologies.[45]
It remains difficult to accurately measure dietary intake outside a laboratory setting. However combining data from various kinds of research, a number of dietary risk factors have been indicated:[46]
- Foods with a high energy density (especially snack foods consumed to supplement rather than replace meals);
- Diets high in fat and low in fibre; and
- Consumption of sugar-rich drinks.
Behavioural research has indicated that changes in the food environment, (e.g. increased variety; advertising; low cost for processed, energy dense foods; increased eating and snacking outside the home) have stimulated food intake beyond that required the match energy expenditure and people’s weight has increased as a consequence. Behavioural researchers propose that there is a need to ‘model and test food environments that are hypothesized to result in better weight control’ and that ‘industry will need to engage with a health agenda that promotes less, rather than more, consumption’.[47] Some research has focused on very specific aspects of eating behaviour, for example, speed of eating. A study in Japan looked at the eating habits of 3,000 people. Compared with those who said they did not eat quickly, fast-eating men were 84 per cent more likely to be overweight, and women were just over twice as likely. It has been suggested that such fast eating behaviour could interfere with the gastric feedback signalling system in the body which tells your brain to stop eating as your stomach swells with food.[48]
Acknowledging a recognised decline in overall physical activity, the World Health Organisation defines physical activity as ‘all movements in everyday life, including work, recreation, exercise and sporting activities’. For adults, it is generally accepted that there have been systematic reductions in energy expenditure due to there being fewer manual jobs, increases in car ownership and the use of labour saving devices both at home and at work. Measuring physical activity outside of the workplace is difficult as focus has been on ‘overt exercise’. This type of exercise seems to account for,
a very small proportion of total energy expenditure and is likely to play only a minor role in preventing obesity, although positive benefits on wider disease risk should not be ignored…attention has therefore focused on the importance of energy expended during routine daily activities as a contributor to overall energy expenditure.[49]
Although there is evidence of reduction in children walking and cycling to school and decreased outdoor play due, in part, to parental fears of safety, the impact of changes on physical activity in children is “less clear".[50] It is recommended that children and young people have at least 60 minutes of at least moderate intensity physical activity each day and at least twice a week this should include activities to improve bone health, muscle strength and flexibility.[51]
The influence of the appropriate knowledge and skills on individual behaviour is also an issue. Being able to interpret and understand food labels can help people to make healthy choices, particularly with the increase of ready prepared foods in the diet. Research has also identified that inadequate cooking skills are a barrier to health eating in young people.[52]
3.5 The Living Environment – Obesogenic Environment
The environment in which we live has been described as being ’obesogenic’. The definition of obesogenic is “the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations"[53]. It is now generally accepted that environmental factors, including the built and food environments and technological developments can influence the availability and consumption of different foods and also influence the levels of physical activity taken by populations. In general,
the advancement of technology has tended to engineer physical effort out of the environment in the past few decades. This trend is widely apparent in the UK, in a built environment that decreases and disincentivises the need to walk, and in the decline of manual occupations.[54]
Research has suggested a number of environmental factors that increase people’s tendency to undertake physical activity. These factors, often lacking in suburban neighbourhoods, have all been cited as encouraging walking or cycling:[55]
- Increased residential densities;
- Neighbourhood design features, such as historic structures;
- Land-use mix, in particular local shops, services and schools within primary residential neighbourhoods;
- The presence and quality of pavements and footpaths;
- Enjoyable scenery;
- Perceptions of safety; and
- The presence of others.
Food environments include availability and accessibility to food, and food advertising and marketing. The workplace and particularly school environments have received much interest, for example, in the UK the television chef Jamie Oliver’s campaign on school dinners resulted in ‘dramatic government intervention and the banning of specific foods from school menus.[56]
It is proposed that the food environment and the built environment are closely related and that ‘there is a need to consider these important obesity related factors together’[57] and that further work is required ‘to examine how aspects of the built environment or building design influences people’s food habits e.g. the proximity of shops to schools or the location of vending machines’.[58]
In the North East of England an obesogenic network (north east obesogenic environment network, NEOeN) has been established to initiate integrated working partnerships within research, practice and the wider community. It regards tackling the obesogenic environment as looking at planning, design, transport, physical activity, food, culture and policy. The objective of NEOeN is to provide a networking facility across practice, academia and communities and it believes through cross sectoral partnerships there is the potential to impact on the rising obesity rates in the North East of England.[59]
3.6 Health Inequalities
With regard to socioeconomic inequalities, patterns of obesity in the UK are seen to be in line with other high income countries. As rates of obesity have increased they have increased most among adults and children from poorer backgrounds, however the widening of obesity inequalities is more evident among women than men[60].
The emerging socioeconomic gradient of obesity in children is of particular concern as both overweight and obese children have increased risk of obesity in adult life and weight management interventions among children and young adults are of limited effectiveness…weight gain among parents may be amplifying the growth of childhood obesity through the generation of a repeating cycle.[61]
A number of reports indicate that age and gender have an impact on activity levels. ‘For boys, activity levels remain the same until aged fifteen, but activity levels in girls decline significantly after the age of nine. After age fifteen, levels of physical activity decline for both sexes’.[62]
Inequalities in obesity also vary by ethnic group. Asian children are more likely to be obese than white children and rates are higher among Black African, Black Caribbean and Pakistani women than in the general female population of the UK. Rates of adult obesity are lower than in the general population of the UK for men from ethnic minority groups with the exception of Black Caribbean and Irish men.[63]
There is evidence to suggest that obesity may be more prevalent among people with disabilities, however it should be noted that disability can be a cause of obesity,
Higher rates of obesity have been found in adults, especially women, with mild to moderate learning disabilities that live in the community than in the general population…disability can impact…in a number of ways, including: different requirements in relation to energy intake, feeding difficulties, strong food preferences or by impacting on the ability to shop and cook….knowledge and understanding of health information can also present a barrier to healthy eating for people with a learning disability.[64]
4. Obesity in Northern Ireland
4.1 Levels of Obesity
On 13th November 2008 at the opening of the All-Island Conference on Obesity (‘Obesity: weighing up the evidence’), Health Minister Michael McGimpsey stated that,
There is no doubt that the obesity time bomb in Northern Ireland is ticking louder than ever. Our level of obesity, especially amongst our children is incredibly worrying…We will continue to work closely across jurisdictions, to share experience and expertise in order to make the best possible inroads into this shared problem.[65]
The Minister’s comments illustrate the fact that in recent years there has been a significant increase in levels of obesity and overweight among children and young people in Northern Ireland. At the same conference, Health Promotion Agency chief executive, Dr. Brian Gaffney citing figures from Northern Ireland’s 2002 public health strategy Investing for Health stated that an estimated 450 deaths a year are attributable to obesity and that obesity costs the local economy approximately £500 million per year.
Figure 3: Percentage of children aged 41/2 to 51/2 in Northern Ireland classified as being overweight or obese[66]
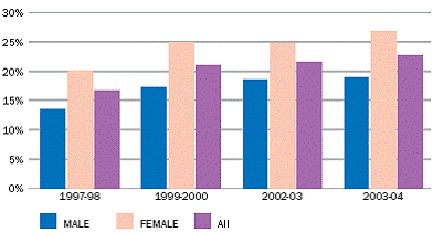
According to the Child Health System (managed by the Health and Social Services Boards) in 2003-04, one in four girls and one in five boys in Northern Ireland were found to be overweight or obese in Primary One. The percentage of children classified as obese in Primary One has increased year on year since 1997. According to the DHSSPS, more recent data shows that the level of obesity in Primary One has declined slightly since 2003-04 from 5.7 per cent of the age group to 5.1 per cent which is still comparatively high. Moreover, the Young Hearts study of 12 to 15 year olds living in Northern Ireland reported that levels of overweight and obesity increased in the decade 1990-2000.[67] Meanwhile, data from the Northern Ireland 2005-2006 Health and Social Wellbeing Survey revealed that 59 per cent of adults were overweight. In relation to obesity levels 25 per cent of men and 23 per cent of women were obese.[68]
Table 1: Proportion of Adults overweight and obese in each Health and Social Services Board (HSSB) by gender[69]
| Overweight | Obese | |||||
| HSSB | All | Male | Female | All | Male | Female |
| Eastern | 32 % | 36 % | 29 % | 21 % | 21 % | 21 % |
| Northern | 37 % | 38 % | 35 % | 26 % | 27 % | 24 % |
| Southern | 35 % | 41 % | 29 % | 28 % | 27 % | 28 % |
| Western | 36 % | 44 % | 28 % | 23 % | 26 % | 21 % |
4.2 Impact of obesity in Northern Ireland – Health and Economic costs
The rising proportion of overweight and obese children, young people and adults in Northern Ireland demonstrates the scale of the problem. Over the past three decades, the population has steadily become accustomed to living in an obesogenic environment which encourages excessive food consumption while simultaneously decreasing opportunities for engaging in regular physical activity. Similar to the consequences in other parts of the UK and in the Republic of Ireland, there are significant implications associated with increasing obesity prevalence relating to population health and the direct and indirect economic costs.
According to Investing for Health, the cost attributable to a lack of physical activity includes over 2,100 deaths per annum equivalent to over 18,000 life years lost and 1.2 million working days lost each year.[70] Meanwhile, in his presentation to the HSSPS Committee, Dr Michael Ryan, Consultant Chemical Pathologist based within the Northern Health and Social Services Board stated that, approximately 750,000 people in Northern Ireland are either overweight or obese, with around 20 per cent of adolescents comprising this figure. Critically, he stated that due to the all-pervasive nature of the obesity problem (the majority of patients attending diabetic, cardiac, angina, vascular, respiratory and morbidity clinics have obesity as a significant underlying pathology) demands placed on the health service associated with treating the condition mean that obesity is effectively ‘clogging up’ a wide range of clinical services at community, primary and secondary care levels. Dr Ryan also argued that, ‘current attempts to address lifestyle change lack coordination into a central and manageable strategy [and]…because of a lack of services specifically targeted at obesity, the clinical and cost-effectiveness of other interventions is seriously compromised.’[71]
In the same presentation Dr Ryan alluded to the fact that there are significant cost implications for health systems in treating obesity and those diseases which are often associated with this condition. He referred to Scotland where around £170 million is spent per year in the treatment of obesity.[72] In terms of the financial impact of obesity in Northern Ireland, there is clearly a significant cost on the health service as well as wider society and the economy. It is estimated that between 30,000 and 50,000 people in Northern Ireland have diabetes and that this will double over the next decade. Treatment and care of diabetes accounts for around 5 per cent of health expenditure and a total of 20 per cent of hospital in-patient resources.[73]
By way of comparison it is worth considering the escalating costs of treating obesity within the largest health system in the UK – the English NHS. According to a Kings Fund report, the cost of treating obesity was approximately £47.5 million in 2002, a significant rise on the 1998 figure of £9.5 million which was largely attributable to rising drug costs. Additionally, the costs of treating diseases caused by obesity (such as coronary heart disease and type 2 diabetes) were estimated at between £945 million and £1,075 million in 2002. By 2007, the cost of prescriptions for all diabetes-related drugs had increased to more than £594 million, up 7 per cent on the previous year.[74]
The authors of the report make an important point in relation to the long-term financial burden of obesity on the NHS. They argue that, ‘if action is not taken, the financial cost to the NHS will grow and, according to Wanless [in his 2004 report][75] could make the NHS itself unsustainable. This is why investing in effective behaviour change interventions is more important than ever’.[76]
4.3 Developing a strategic policy response to obesity in Northern Ireland
Unlike England but similar to Scotland, Wales and the Republic of Ireland, there is currently no comprehensive obesity strategy being implemented in Northern Ireland. At present, of all the devolved regions, only England has a population-wide obesity specific strategy. While no population-wide strategies tackling obesity are currently being implemented, obesity is recognised as a priority in a number of key public health documents within the devolved jurisdictions. Additionally, interventions to address obesity have been incorporated in diet and nutrition and/or physical activity policy or strategy documents.[77]
4.3.1 Progressing Fit Futures - Developing a coherent policy framework
In response to the increasing levels of obesity, particularly among children and young people in Northern Ireland, a cross-departmental taskforce was established in August 2004 by the Ministerial Group on Public Health (MGPH). The culmination of the Taskforce’s work to examine ways to reduce the prevalence of obesity among children and adolescents in Northern Ireland was the publication of Fit Futures – Focus on Food, Activity and Young People in December 2005. Fit Futures built on the previous 2002 commitment by the DHSSPS outlined within Investing for Health to stop the increase in the levels of obesity in men and women by 2010.[78] Currently, the central target driving the anti-obesity strategic agenda in Northern Ireland is that contained within the Public Service Agreement (PSA) 8 outlined with the Executive’s Programme for Government 2008-2011. PSA 8 aims to ‘promote health and address health inequalities’ and in doing has established a target:
- By 2011, halt the rise in obesity.
Significantly, within Fit Futures, the Taskforce identified 6 priority areas (see below) which they recommended that ‘because of the health and financial consequences of inaction should be implemented as a matter of priority.’[79] These 6 priorities for action are detailed below:
Develop joined-up healthy public policy
- address disjointed approach to promotion of physical activity, sport and leisure;
- address conflicting policies sometimes being promoted by government departments and agencies in relation to food policy and the food industry
Provide real choice
- food industry should respond to introduction of controls on advertising and promotion of foods to children;
- food industry should introduce agreed nutritional signposting system;
- create demand for healthy options through public sector food procurement;
- tackle barriers to healthy food;
- opportunities for active play should be available and accessible
Support healthy early years
- extend healthy schools programme to early years settings;
- establish common standards for nutrition and physical activity in these settings and monitor compliance;
Create healthy schools
- integrate health improvement planning into school development planning;
- develop active schools programme
Encourage development of healthy communities
- community based approaches such as Health Action Zones
Build on evidence base
- systematic surveillance of obesity levels, nutrition and activity levels[80]
An implementation plan for Fit Futures was issued for consultation in early 2007 which set out a range of key tasks and target dates under the 6 priority areas. In February 2008, a DHSSPS-led Obesity Prevention Steering Group (OPSG) was established to oversee implementation and significantly to work on the development of an adult obesity strategy. This cross-sectoral group contains representation from practitioners, policy makers and researchers and has responsibility for monitoring the implementation of the 70 recommendations in Fit Futures.
Building on the focus on childhood obesity in Fit Futures, the OPSG is leading the development of a life course approach to obesity treatment and prevention. A key component is the establishment of four policy Advisory Groups with each group designated a key area – physical activity, food and nutrition, education and prevention, and data and research. According to the NIAO, this work will facilitate an informed, research-led integrated approach to address obesity and associated conditions.[81]
According to the authors of the Fit Futures report, stakeholders strongly suggested that the recommendations should be operationalised through building on existing structures and programmes. Moreover, one of the key messages that emerged from the Fit Futures process was the need to support a much more joined-up, coordinated approach to address the underlying causes of overweight and obesity. Subsequently, a number of different initiatives were coordinated and implemented through the HSSB-based Investing for Health Partnerships that have mainly focused on the school environment to raise awareness around the issue of obesity and promoting better nutrition and regular physical activity.
4.3.2 NIAO Report on Obesity and Type 2 Diabetes (2009)
Despite progressing the Fit Futures recommendations, the DHSSPS’s obesity policy agenda has received criticism from the Northern Ireland Audit Office (NIAO) in their recent report into the prevalence of Obesity and Type 2 Diabetes in Northern Ireland. According to the report,
Fit Futures called for measures to ensure that an effective evidence base on obesity risk factors was developed. However after three years, progress on this recommendation has been slow. In our view, the Department has to be at the forefront, of efforts to define and implement a regional surveillance strategy for obesity and its links with chronic disease, in particular Type 2 diabetes. It is important that the Department takes timely action to introduce a health monitoring survey to better understand the eating habits, physical activity and related biomedical health indicators of the population of Northern Ireland.[82]
In addition to these comments, the NIAO report also put forward a number of other recommendations to ensure the successful development of a more coherent policy framework in tackling obesity and Type 2 Diabetes:
- Include and deliver programmes demonstrated by research to be effective;
- Provide enough resources to deliver programmed with real impact and sufficient coverage of the region;
- Ensure effort and investment can be sustained enough to get results;
- Set specific objectives and targets relating to health eating for target population groups;
- Provide ongoing measures of success;
- Have the flexibility to reallocate or increase resources in response to emerging evidence on performance and the target outcomes; and
- Ensure that the governance arrangements covering the whole-of-government nature of its approach to obesity and diabetes are capable of driving effective outcomes.[83]
4.3.3 Adopting a Life Course Approach to tackle obesity
A key task for the Obesity Prevention Steering Group has been to extend the child-centred focus of Fit Futures to the development of a whole-population obesity strategy. An important dimension of this work has been the adoption of a ‘life course’ approach to tackle obesity.
According to Musingarimi, ‘the ‘life course’ approach to tackling overweight and obesity views the action and behaviour of individuals in the context of the continuum of their lives from birth to death, and transition through various life stages and transition points.’ In recent years, the majority of strategic approaches employed in tackling obesity levels have focused on children and young people mainly within the school environment. Recent research conducted by the UK Government’s Foresight project identifying approaches to tackle obesity, has advocated the employment of a life course approach as it recognises the important factor of age in preventing and treating obesity. An important observation relating to the development of a strategic approach to tackling obesity is that ‘the generational nature of obesity means thinking about a different strategy for different generations as options change. This also means thinking about long-term goals such as how to integrate health more into food culture, values and habits – which would take some time.’[84]
5. Interventions and Treatments for Obesity
5.1 Interventions – Introduction and General approaches
It is envisaged that implementing solutions for obesity is likely to require ‘unprecedented change [with the] involvement of partners outside traditional health sectors’. It is also likely that ‘interventions to prevent obesity will have to take place when the evidence is neither complete nor perfect. Instead, the evidence base needs to develop alongside the delivery of novel interventions, informed by the available evidence and strengthened by expert advice.[85]
The evidence to date indicates stages in life where there are natural opportunities to influence behaviour to prevent obesity. These stages include periods of ‘metabolic plasticity’ (e.g. early life and pregnancy); times linked to major change (e.g. leaving home, becoming a parent); and times when there are major attitude changes (e.g. peer group influence). ‘Breast feeding and early growth patterns provide the only period in which there is clear evidence to support the concept of a critical period of development associated with long-term consequences’[86].
Children are often considered ‘the priority population for intervention strategies because, firstly, weight loss in adulthood is difficult and there are a greater number of potential interventions for children than for adults. Schools are a natural setting for influencing the food and physical activity environments of children. Other settings such as preschool institutions and after-school care services will have similar opportunities for action’.[87]
The Northern Ireland Fit Futures taskforce has identified a number of general approaches that ‘should be taken into account when developing new policies and initiatives to tackle obesity and when refining existing policies and programmes’ as follows:[88]
- The importance of parents and families and making a good start – ‘with parents have a major impact on their child’s eating and physical activity patterns’;
- Supporting the development of basic skills – ‘children, young people and their parents need to have the knowledge and understanding of why healthy eating and active living are important. They also need to be able to differentiate between healthy and less healthy choices and they need the basic skills and confidence to select and adopt healthy choices’;
- Making a long-term commitment – ‘participants in Fit Futures were strongly of the view that to prevent levels of overweight and obesity from continuing to rise a sustained, co-ordinated effort would be required from throughout the public, private, voluntary and community sector’;
- Leading by example – ‘the role of government procurement in creating a demand for healthy options was highlighted as an important area for action’, e.g. meals in schools and hospitals and contents of vending machines in leisure centres, schools and hospitals;
- Adopting a population approach but responding to need – it is important that ‘policies and strategies should utilise approaches that enable access to all relevant population groups’;
- Being positive and promoting self-esteem – ‘a positive approach to obesity prevention is in line with current policies to promote good mental and emotional health and well-being’;
- Being evidence based – ‘the absence of a comprehensive evidence base should not prevent action now, but rather highlights the need for more rigorous evaluation of new policies and programmes in the future’.
In 2006, The National Institute for Health and Clinical Excellence (NICE) published a clinical guideline on obesity. The following key priorities for implementation of the guidance are directly extracted from the guideline and illustrate the main areas and situations where NICE propose that certain interventions are most beneficial[89]:
Key priorities for implementation
The prevention and management of obesity should be a priority for all, because of the considerable health benefits of maintaining a healthy weight and the health risks associated with overweight and obesity.
Public health
NHS - Managers and health professionals in all primary care settings should ensure that preventing and managing obesity is a priority, at both strategic and delivery levels. Dedicated resources should be allocated for action.
Local authorities and partners - Local authorities should work with local partners, such as industry and voluntary organisations, to create and manage more safe spaces for incidental and planned physical activity, addressing as a priority any concerns about safety, crime and inclusion, by, for example, providing facilities and schemes such as cycling and walking routes, cycle parking, area maps and safe play areas; making streets cleaner and safer; ensuring buildings and spaces are designed to encourage people to be more physically active; and considering in particular people who require tailored information and support.
Early years settings - Nurseries and other childcare facilities should minimise sedentary activities during play time, and provide regular opportunities for enjoyable active play and structured physical activity sessions; and implement Department for Education and Skills, Food Standards Agency and Caroline Walker Trust1 guidance on food procurement and healthy catering.
Schools - Head teachers and chairs of governors, in collaboration with parents and pupils, should assess the whole school environment and ensure that the ethos of all school policies helps children and young people to maintain a healthy weight, eat a healthy diet and be physically active, in line with existing standards and guidance.
Workplaces - Workplaces should provide opportunities for staff to eat a healthy diet and be physically active, through, for example, active and continuous promotion of healthy choices in restaurants, hospitality, vending machines and shops for staff and clients; and a supportive physical environment, such as improvements to stairwells and providing showers and secure cycle parking.
Self-help, commercial and community settings – Primary care organizations and local authorities should recommend to patients, or consider endorsing self-help, commercial and community weight management programmes.
Clinical care
Children and adults - Multicomponent interventions are the treatment of choice to include behaviour change strategies to increase physical activity levels or decrease inactivity, improve eating behaviour and the quality of the person’s diet and reduce energy intake.
Children - Interventions for childhood overweight and obesity should address lifestyle within the family and in social settings. Body Mass Index (BMI) (adjusted for age and gender) is recommended as a practical estimate of overweight in children and young people, but needs to be interpreted with caution because it is not a direct measure of adiposity. Referral to an appropriate specialist should be considered for children who are overweight or obese and have significant comorbidity or complex needs (for example, learning or educational difficulties).
Adults - The decision to start drug treatment, and the choice of drug, should be made after discussing with the patient the potential benefits and limitations. When drug treatment is prescribed, arrangements should be made for appropriate health professionals to offer information, support and counselling on additional diet, physical activity and behavioural strategies. Information about patient support programmes should also be provided.
Bariatric surgery is recommended as a treatment option for adults with obesity if all of the [NICE] criteria are fulfilled. Bariatric surgery is also recommended as a first-line option (instead of lifestyle interventions or drug treatment) for adults with a BMI of more than 50 kg/m2 in whom surgical intervention is considered appropriate.
5.2 Interventions for Individuals – Primary Care
An evidence-based Care Pathway for the management of overweight and obesity in primary care was published by the NHS in 2006.[90] For adults, the priority of intervention in primary care is reducing risk factors for the patient ‘rather than to return them to an ‘ideal’ or healthy weight range’.[91] This acknowledges the fact that small weight losses do produce health benefits, however that more significant changes result after a loss of 5-10 per cent of body weight. The aim is also to prevent further weight gain in patients with lower degrees of overweight. To achieve these aims, first-line primary care management is to help a patient with specific advice to:[92]
- reduce calorie intake;
- increase physical activity and reduce sedentary behaviours; and
- increase self-awareness about day-to-day behaviours that affect calorie intake and activity levels and combine advice in diet and physical activity with behavioural strategies e.g. avoidance of stimuli to overeating, such as not walking past the fish and chip shop, no longer keeping crisps in the house.
This primary care emphasis on reducing risk factors for the patient is highlighted by some researchers who propose that ‘in view of the limited success rates of all weight-loss strategies to date…where previous dieting attempts have failed, better outcomes and health improvements will arise from advocating weight stability goals. This means the promotion of weight maintenance (to ensure any reduction in weight is maintained) and weight constancy (where steps are taken to maintain existing weight without attempting weight loss)’.[93]
Anti-obesity drug therapy is considered as an addition, rather than an alternative to, lifestyle intervention. Both Orlistat and Sibutramine are currently in use in the UK for obesity treatment in accordance with NICE guidelines for prescribing the drugs:[94]
- Orlistat inhibits the action of pancreatic lipase enzymes in the gastrointestinal system and must be used in conjunction with a low fat eating plan as failure to do so results in gastrointestinal side effects such as diarrhoea;
- Sibutramine is a satiety enhancer which ‘works on the central nervous system by altering the chemical messages that control how a person feels and thinks about food’.
Regarding drug therapy, researchers have noted that, none of the available agents has the capacity to spontaneously change the body weight set-point without any specific dietary restriction…however [they can help in] achieving and maintaining effective weight reduction, although not all individuals are good responders to anti-obesity drug therapy…Discovery of new pharmacological alternatives, leading to greater efficacy in the promotion of weight reduction without affecting safety, is still the main objective for the treatment of obesity.[95]
The Counterweight programme is a good practice example of a primary care weight management programme. It is described as ‘the only fully evaluated, evidence based weight management programme within the UK – possibly worldwide’[96]. The model is based on Weight Management Advisers (dieticians specialising in obesity management), working in Primary Care Trusts training and supporting healthcare staff to put the programme into action. Lifestyle intervention is the first-line approach (with individuals or groups) and second-line interventions may include anti-obesity drugs, referral to a dietician, psychologist or secondary care service. Local dieticians are involved to take over once the model is implemented and it is anticipated that each trained practice could treat 50 patients a year.[97]
The NHS Care Pathway notes that, ‘if a person does not respond to first-line management’, they are considered for referral to ‘specialists such as dieticians, psychologists, physiotherapists and/or specialist weight management clinics. Surgery is generally considered for obesity only after all other interventions have been exhausted’.[98]
One good practice example of a Primary Care Specialist Obesity Service, established to treat people with morbid obesity within a primary care setting, is that established by Birmingham East and North PCT. The aim of the level 3 service is to provide more intensive specialist support, than would generally be possible in a primary care setting, from a multi-professional team. The patients of this service are those who have failed to control their weight at the level 2 service (community/primary care weight management service) and to provide a gateway to level 4 services (secondary care morbid obesity service).[99]
5.3 Interventions for Individuals – Secondary Care (Bariatric Surgery)
Bariatric surgery has increased ‘more than five-fold within 5 years in most developed countries. In parallel evidence is accumulating that surgically induced weight loss provides a survival benefit for morbidly obese patients. In two recent cohort studies…bariatric surgery compared with conservative management reduced long –term mortality in morbidly obese patients’.[100] These cohort studies were carried out in Sweden and the U.S. and they ‘separately found that obese people who underwent drastic surgery had a 30 percent to 40 percent lower risk of dying seven to 10 years later compared to those who did not have such operations’.[101]
It is one medical view that such surgery should be offered to overweight people as a form of disease prevention and not just carried out on the morbidly obese and that, ‘at least ten time as many people who currently have gastric bypass operations on the NHS already qualify for one under the Government’s own guidelines[102].
Bariatric procedures can be divided into those that reduce food intake (gastric restrictions) and those that reduce food uptake from the digestive tract (malabsorption). The two most common procedures worldwide are the adjustable gastric banding and Roux-en-Y gastric bypass, ‘both approaches have strong support among bariatric surgeons’, however ‘it is important that knowledge and skills are concentrated in bariatric surgery centres. Mortality in high-volume centres is lower than in low-volume centres’.[103]
In the UK there are guidelines for adults from NICE about who should be considered for bariatric surgery (surgery is not generally recommended for young people but may be considered in exceptional circumstances):[104]
- BMI is greater than or equal to 40 or 35-40 Kg/m2 with other significant disease e.g. type 2 diabetes, that could be improved by weight loss, and:
- All appropriate non-surgical measures have failed to achieve or maintain adequate clinically beneficial weight loss for at least 6 months;
- They are receiving or will receive intensive specialist management;
- They are generally fit for anaesthesia and surgery;
- They commit to the need for long-term follow-up;
- As a first-line option if BMI is more than 50 Kg/m2 and surgical intervention is considered appropriate.
5.4 Community Interventions – Good Practice Examples
5.4.1 Northern Ireland
The following are some examples of good practice and are taken from Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, (2005).
Western Investing for Health Partnership – Health Promoting Homes
The initiative was established to tackle obesity in children and in families in areas of disadvantage in Strabane and Castlederg. It offered participants ‘an integrated programme to support personal development, including the development of knowledge and practical skills on issues such as breastfeeding, nutrition and oral health and physical activity’.[105]
Craigavon Borough Council – Physical Activity
With the support of partners from the sport and health sectors, Craigavon Borough Council is encouraging participation in physical activity by those not usually involved. For example, a school-based dance and physical activity programme for teenage girls called ‘Teenage Kicks’ has been delivered to over 1000 girls in local schools; over-50’s clubs at local leisure centres; “Rusty Rackets" tennis programme; and a training scheme to accredit ‘walk’ leaders.[106]
Cherish Sure Start Project – Irvinestown
The Big Cook Little Cook programme, facilitated by a Cook It! Tutor involves a number of 2-hour sessions over a 4-week period on healthy eating and food hygiene for parents and children to do together. The aim is to ‘help both parents and children to make informed choices’.[107]
Decent Food for All – Armagh and Dungannon Health Action Zone
This is a 3-year partnership project, funded by safefood, the Food Safety Promotion Board and the food Standards Agency which aims to ‘encourage and support local communities, families and individuals to achieve a balanced, safe diet by providing practical, community-based and focused help and advice on food issues and nutrition’. It is delivered within 12 target wards across Armagh and Dungannon.[108]
Active Communities
In 2005 the Sports Council for NI, in partnership with the Big Lottery fund, launched a community sport programme targeting the 25 per cent of Northern Ireland’s most deprived electoral wards and groups, including older people and people with disabilities. A Community Sports Development Officer is to plan and deliver a range of activities that meet local needs, especially of disadvantaged groups.[109]
5.4.2 Other UK Examples
Change4Life
Change4Life is a Department of Health initiative and is described as ‘a society-wide movement that aims to prevent people from becoming overweight by encouraging them to eat better and move more’. Its advertising campaign began in January 2009 and talks about ‘fat in the body’ rather than fat bodies in order to make clear the links between fat and preventable illness. It also ‘pins the blame on modern life, which affects all of us, rather than pointing the finger at parents’.[110] Individual families are encouraged to join Change4Life via the website to receive information, games, tools, tips, a welcome pack and updates about what I happening in local communities. The suggestions for families are centred around the following areas:[111]
- Up and about (“why kids shouldn’t veg out and how to get them out and about");
- 5 A Day (making 5 portions of fruit and veg a day easy);
- Meal time (the importance of 3 regular meals);
- 60 active minutes (children should be active for 60 minutes per day);
- Snack check (reducing unhealthy snacking)
- Me size meals (the right sized portions for children’s ages);
- Cut back fat (easy ways to lower fat in the family diet); and
- Sugar swaps (ways to help children eat less sugar).
As part of the Change4Life campaign, nine towns/areas in England (Dudley, Halifax, Sheffield, Tower Hamlets (London), Thetford (Norfolk), Middlesbrough, Manchester, Tewkesbury and Portsmouth) are sharing in £30m to become ‘healthy towns’. The areas will all match the government funding to develop a range of schemes related to healthy living. For example, in Manchester Points4Life is a loyalty scheme to reward people with free activities or healthy food when they take exercise. Other initiatives include ‘cut-price promotions on fruit and vegetables and breakfast clubs in deprived areas’.[112]
MEND (Mind, Exercise, Nutrition…Do It!)
MEND is an organisation dedicated to reducing global childhood overweight and obesity levels. The MEND programme was developed at the Great Ormond Street Hospital for Children and the University College London Institute of Child Health. Together with its partners (public, private, voluntary and academic). MEND offers local healthy living programs to families.
There is a MEND programme for 7-13 year olds who are overweight (It runs twice a week after school in two-hour sessions over 10 weeks. The 20 MEND Programme sessions include an hour’s interactive workshop for children and parents, and an hour’s exercise for the children whilst the parents have an adult discussion) and a Mini-MEND programme for 2-4 year olds, whatever their weight (Mini-MEND’s ten weekly 90 minute sessions combine parent-toddler active play, parent discussion groups and children’s crèche-style creative play activities. They take place during the daytime at community venues such as leisure centres and Sure Start Children’s Centres)[113]. MEND are also aiming to develop effective and research-based obesity prevention and treatment programmes, training and resources.
WATCH IT
WATCH IT is an NHS Community Programme for children and teenagers in Leeds having difficulty with their weight. It is a year long intervention made up of bronze, silver and gold awards which are completed in succession. The WATCH IT trainers work with the family and are specially trained in nutrition and physical activity and have access to dieticians, sports experts, psychologists and children’s nurses to ensure the best advice. They meet with the families involved individually to assist with making the changes in nutrition and activity required.[114]
Carnegie Camps
Carnegie International Camp (as part of the non-profit organisation Carnegie Weight Management) was devised at Leeds Metropolitan University in 1999 as ‘Britain’s first residential weight loss summer camp for overweight and obese children’. It has continued to grow in a variety of ways in terms of both staff numbers and services offered. In addition to the summer camps there are now Carnegie Day Camps that run from 1-7 weeks in the summer and Carnegie Clubs, a community programme that runs all year. Young people and family members attend the 12-week programme for several hours a week to learn the ‘basics of healthy lifestyles and have the opportunity to try new activities to bring the fun back into exercise’.[115]
Commercial programmes
There are numerous commercial weight loss programmes in operation world-wide. The effectiveness of four of the main programmes available to adults in the UK, Dr Atkins new diet revolution, Slim-Fast Plan, Weight Watchers pure points programme and Rosemary Conley’s eat yourself slim diet and fitness plan, were evaluated in a ‘six month multicentre randomised unblended controlled trial’. All the diets resulted in significant loss of body fat and weight over six months compared with the control group. The average weight loss was 5.9Kg and average fat loss was 4.4 Kg over six months. The trial concluded that, ‘clinically useful weight loss and fat loss can b achieved in adults who are motivated to follow commercial diets for a substantial period. Given the limited resources for weight management in the NHS, healthcare practitioners should discuss with their patients programmes known to be effective’.[116]
5.4.3 International Examples
Reviews of evidence from other countries suggest that specific actions can be useful but ‘without overall coherence in policy and clear political drivers, they are most unlikely to deliver the required level of change....interventions in school settings suggest that a ‘whole-school’ approach (meal services, vending, class teaching, physical education, out-of-school activities) is more likely to be successful than one targeting individual children’.[117] Some specific international good practice examples of community and school interventions are described in Appendix 1 from Australia, Canada, China, France, New Zealand, Norway, Sweden and the U.S.
6. ‘Building a Sustainable Response’ (Foresight Report (2007))
In October 2007, the Foresight Tackling Obesities: Future Choices Project published a report advocating the development of a coherent and comprehensive approach to confronting the obesity problem in the UK. Based within the UK Government Office for Science the central aim of the obesity project is ‘to produce a long-term vision of how we can deliver a sustainable response to obesity in the UK over the next 40 years.’[118]
The UK-wide project has strongly influenced the development of obesity strategies including the publication of Healthy Weight, Healthy Lives: A Cross- Government Strategy for England in January 2008. The report put forward a number of key recommendations including the identification of a set of ‘core principles’ that are crucial in the configuration of a coherent and comprehensive response to tackling obesity.[119] These are:
1. A system-wide approach, redefining the nation’s health as a societal and economic issue
2. Higher priority for the prevention of health problems, with clearer leadership, accountability, strategy and management structures
3. Engagement of stakeholders within and outside Government
4. Long-term, sustained interventions
5. Ongoing evaluation and a focus on continuous improvement[120]
In addition to these core principles the Foresight report makes a number of other important observations and recommendations which it contends are critical to understanding the complexities of obesity and in developing a successful long-term strategy.
- Obesity arises primarily from a systematic shift in the wider environment, with corresponding effects on group and individual behaviour, against the backdrop of an obesity system where biological drivers favour weight gain. A sustainable response would create a scenario in which social and individual priorities favour healthy behaviours and where underlying biological mechanisms to control body weight are continually reinforced. A key feature of this response is that it places the concept of energy balance at the heart of a broad range of determinants of health.[121]
- Taken together, the evidence presented in this report provides a powerful challenge to the commonly held assumption that an individual’s weight is a matter solely of personal responsibility or indeed individual choice. Rather, the evidence supports the concept of ‘passive obesity’ (where obesity is encouraged by wider environmental conditions, irrespective of volition). As society has changed over the last three decades energy expenditure physical activity has declined. Today, the majority of people in the UK are sedentary when at work and at home. Most are car owners. Patterns of food consumption have also changed markedly. Eating habits have become more unstructured, and low-cost, energy-dense ‘food and drink on the go’ is widely consumed. For a multitude of reasons, healthy lifestyles may be less available to those on low incomes. [122]
- As a general rule, people do not ‘choose’ to be obese. Their obesity is mainly driven by a range of factors beyond their immediate control that in practice constrain individual choice. The commercial success of the weight loss market is testament to the belief invested in the power of individuals to control their own weight. However, the concomitant rise in obesity and the frequent weight regain common those who have dieted successfully is evidence of the failure of a response built solely on this approach. Strategies based on personal motivation and individual responsibility alone do not provide an adequate response to the obesity problem.[123]
- To be successful, a comprehensive long-term strategy to tackle obesity must act in two complementary ways to achieve and maintain a healthy population weight distribution. First, an environment that supports and facilitates healthy choices must be actively established and maintained. Second, individuals need to be encouraged to desire, seek and make different choices, recognising that they make decisions as part of families or groups that individual behaviour is ‘cued’ by the behaviours of others, including organisation behaviours and other wider influences.[124]
- The strategy needs to be planned and co-ordinated effectively by Government and must involve multiple stakeholders. The role of non-governmental organisations – businesses, employers and voluntary organisations – is also critical and in some cases may be the dominant influence. National strategic action must be coherent, with local strategies that reflect local conditions, needs and aspirations. In particular, the role of local bodies such as local government and local health authorities must be clearly defined and linked to sufficient resources and the necessary skills to implement effective responses.[125]
Appendix 1 – International Good Practice Examples
Australia
Victoria
Be Active, Eat Well is a community-wide campaign in the town of Colac, Victoria Australia. The program is funded by the state government of Victoria. Colac is home to ‘some of Australia’s poorest families who played an active role in designing and implementing the Be Active, Eat Well campaign…Key strategies include transforming canteen menus, introducing daily fruit, reducing television watching, and increasing activities after school’.[126] In the first three years of the campaign, children in Colac had significantly lower weight and smaller waist size compared with children in a nearby control area. In addition the program improved children’s health regardless of their socioeconomic status.[127] Due to its success, in 2007, a further six new community ‘Go for your life’ initiatives to combat obesity have been funded in Victoria focusing on children, families and older Victorians.
New South Wales
In 2007, the New South Wales Government launched ‘Australia’s largest ever obesity trial’ involving 4000 children up to the age of 15, randomly selected from 70 schools and childcare centres in the Hunter and New England region. Their height, weight and waist circumference measurements will be recorded for three years to assess the effectiveness of anti-obesity programs in the region.[128] The intervention components of the program include, for example, training for childcare staff regarding healthy menus, lunchboxes and physical activity; working with schools to integrate the concept of energy balance into the school curriculum; educational programs for parents of pre-school children; and working with community health services, early childhood health nurses, dieticians and GPs to offer specialist advice and support to monitor children at high risk of developing a weight problem.[129]
Canada – Quebec Program
In Quebec $400 million in new funding was provided in 2006 jointly by the government and a philanthropist[130] to address childhood obesity. It is planned that the money will go to ‘school boards, community groups, municipalities and other organisations that submit programs designed to improve healthy living habits, particularly among people under 25.[131] The money is in a ‘special fund’ to ensure it cannot be spent on other things and the ‘funds also include money to fund research into obesity, stricter regulations on dietary aids and a companion awareness programme aimed at adults and sedentary office workers.’[132]
China – Beijing
‘Happy 10’ is a pilot intervention in Beijing schools and it was designed especially for the urban school setting by the Chinese Centre for Disease Control and it is based on the ‘Take 10’ model developed in the US (see US section below). ‘Happy 10’ incorporates 10 minutes of physical activity into third and fourth grade classrooms twice a day. It is a card game, with each card describing an activity which can be led by a teacher or a child. ‘The ten-minute period is carefully calculated into one- or two- minute increments during which students pick up the card which determines what activity the class will do; engage in a timed sequence of light, moderate, and moderate-high activity; cool down while learning a health message; and reward themselves with a sticker placed on the classroom wall’.[133]
France – EPODE (Ensemble Prevenons L’Obesite des Enfants)
The EPODE operation is a community initiative built on a pilot study with the Fleurbaix Laventie Town Health Study, which was subsequently rolled out to ten towns in ten different regions in France. The objective is to curb the progression of childhood obesity by way of a five year plan. Two levels of intervention are involved[134]:
- Primary prevention which involves the entire community; and
- Secondary prevention involving the community and medical sector.
The action for schools includes educational tools for teachers, a transformed recess including more physical activity and improved school catering with themed learning spaces in schools to teach children how to cook with fruit and vegetables and provide tasting workshops.
For the entire community an annual Nutrition and Physical Exercise week will represent a focal point in the town calendar. The program contains many other community initiatives coordinated by a project leader in each town.
New Zealand
Two particular multi-component interventions are based in the family setting as follows:
- ‘Food with Attitude’ (FWA) and ‘Young and Active’ – FWA is a year long programme run by Auckland’s Community Child Health and Disability Service. It involves monthly visits to the child (aged 5-12) (at school or at home) following an initial visit by a Public Health Nurse and dietician with the child and his family at home. The family sign a contract to give the child lots of encouragement and help with healthy eating and exercise. Success is measured by changes in behaviour, self-esteem and achievement of individual goals. As an add-on, Sport Auckland has been funded to work with FWA children to develop exercise activities[135].
- Kids in Action (KIA)[136] is a family-based childhood obesity program, especially targeting Pacific people in the Counties Manukau District Health Board (Auckland) area. Referrals are received from schools and healthcare providers. The program involves a paediatrician, a nurse and a dietician and exercise instructors who work with the whole family. The children set goals for themselves and are awarded prizes. KIA includes:
- Paediatric assessment;
- Dietary advice;
- Weekly exercise session; and
- Family group conferences to develop strategies for the family.
Norway – Nordland
In 2004, the county of Nordland started a comprehensive school programme to provide pupils in all its 210 primary schools with at least 60 minutes of physical activity during every school day. By 2006, 144 schools had prepared activity programmes. The activity programmes were based on the schools own resources and combined physical education, outdoor education for various subjects, provision of more motivating playgrounds and walking and cycling to school.[137]
Sweden – Ostergotland
In 2005, all primary care units in Ostergoterland took part in prescribing physical activity. 3344 patients received such prescriptions, corresponding to 1.6 per cent of all the people visiting primary care units that year. After 12 months 49 per cent of the patients had followed the prescription, while an additional 21 per cent were regularly active in a different way from that prescribed.[138]
United States
NPAO
The Nutrition, Physical Activity and Obesity Program (NPAO) is a cooperative agreement between the Centres for Disease Control (CDC) and Prevention’s Division of Nutrition, Physical Activity and Obesity and 23 state health departments. The program goal is to prevent and control obesity and other chronic diseases through healthy eating and physical activity.[139] Two of the specific examples within this state program are as follows:
- Colorado Worksite Resource Kit – provides employers with resources to launch worksite wellness initiatives. The Kit outlines for employers how to plan, assess and successfully implement nutrition and physical activity interventions. The Kit is meant to complement a comprehensive approach to worksite health promotion; and
- Moses Lake, Washington State – Healthy Communities Moses Lake – encourages good nutrition and physical activity throughout the community via policy change, e.g. widening pavements and creating an interconnected system of paths for pedestrians and cyclists; a community garden project; supportive environments for breastfeeding.
Take 10
The ISLI (International Life Sciences Institute) formed its Physical Activity and Nutrition (PAN) program in Atlanta in1996. As part of PAN it developed Take 10, a classroom based physical activity program school children. Take 10 is a curriculum tool created by teachers and it integrates academic learning (in language, arts, maths, social studies, science and health) with movement in 10-minute physical activity sessions to reduce sedentary behaviour during the school day.[140]
CATCH
The CATCH program (Coordinated Approach to Child Health) is in over 7000 schools in the US and has been evaluated in over 80 peer reviewed publications. It brings schools, families and communities together to teach children how to be healthy for their lifetime. Healthy behaviours are reinforced through a coordinated approach in the classroom, in the cafeteria, in physical education and at home:[141]
- Classroom – Go for Health Series is the classroom health education curriculum that teaches children healthy behaviours;
- Physical Education – high energy, non-elimination activities;
- Cafeteria – Eat Smart component makes breakfast and lunch opportunities to learn, practice and adopt healthy eating;
- Home – CATCH Family component to make the home environment an extension to CATCH by getting parents and extended family involved; and
- Community – CATCH Kids Club designed for after school and summer schemes.
Boston Partnership between Schools and Business
Boston school and health officials have teamed up with local convenience stores near city middle schools to promote healthier drinks to students. To support an advertising campaign the stores have agreed to display health beverages such as pure fruit juice, water and milk prominently. The initiative will also track children’s beverage purchases over the course of the pilot scheme.[142]
Healthy Hawaii Initiative
The Healthy Hawaii Initiative is described as the only long-term, state-wide program to implement a social ecological approach to reduce obesity, increase physical activity, and improve nutrition. It is a collaboration between the state department of health, state department of education, and the University of Hawaii and the goal is to increase the years of healthy life for all people of Hawaii and reduce existing health disparities among ethnic groups in Hawaii in particular through nutrition and physical activity promotion. Interventions are targeted at the individual, social, and environmental level and use a variety of channels. The interventions are divided into four main delivery channels: 1) community-based interventions, 2) school-based interventions, 3) public education, and 4) professional education. Behavioural data results have shown positive trends, for example, leisure time with no physical activity in adults decreased by 7.2 per cent from 25.5 per cent in 1999 to 18.3 per cent in 2003. Over the same time period, the percentage of adults eating five or more servings of fruit/vegetables a day also increased by 5.2 per cent from 22.4 per cent to 27.6 per cent. The rate of overweight and obese adults decreased by 0.2 per cent, whereas in the rest of the U.S., the median of overweight and obese increased by 3.0 per cent.[143]
Appendix 2
Table 2: Criteria checklist for an effective obesity strategy[144]
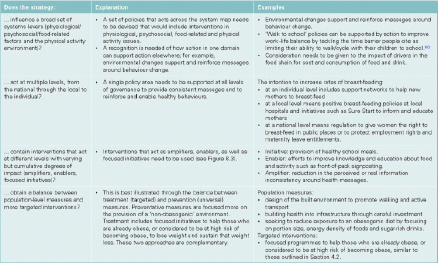
Table 3: Criteria checklist for an effective obesity strategy (Cont…)[145]
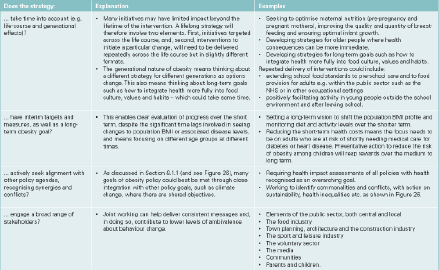
Table 4: Criteria checklist for an effective obesity strategy (Cont…)[146]
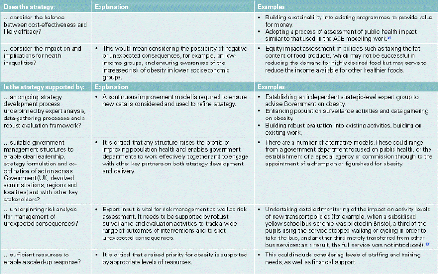
February 2008
[1] World Health Organisation (WHO (2006) Fact Sheet, September.
[2] See Basham, P and Luik, J. (2006) ‘Four big, fat myths’, Daily Telegraph.
[3] World Health Organisation (2007) The challenge of obesity in the WHO European Region and the strategies for response, World Health Organisation: 1.
[4] World Health Organisation (2007) The challenge of obesity in the WHO European Region and the strategies for response, World Health Organisation: 1.
[5] UN Report figures cited in an article published on the International Obesity Taskforce website entitled, ‘The developing world’s new burden: obesity’, January 2002 – the article can be accessed electronically at: http://www.iotf.org/popout.asp?linkto=http://www.fao.org/FOCUS/E/obesity/obes1.htm
[6] International Obesity Task Force (IOTF) and European Association for the Study of Obesity (EASO) (2002) Obesity in Europe – the case for action, London cited in National Taskforce on Obesity (RoI) (2005) Obesity – The Policy Challenges – The Report of the National Taskforce on Obesity 2005, National Taskforce on Obesity (RoI): 18.
[7] UN Report figures cited in an article published on the International Obesity Taskforce website entitled, ‘The developing world’s new burden: obesity’, January 2002 – the article can be accessed electronically at: http://www.iotf.org/popout.asp?linkto=http://www.fao.org/FOCUS/E/obesity/obes1.htm
[8] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 5.
[9] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 5.
[10] World Health Organisation (WHO) (2006) Fact Sheet, September.
[11] Price et al (2006) ‘Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index is associated with a greater risk of death’, Am J Clin Nutr, 84 (2): 449-460 cited in P. Musingarimi (2008) Obesity in the UK: A Review and Comparative Analysis of Policies within the Devolved Regions, International Longevity Centre: 8.
[12] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 150.
[13] Department of Health and Children (2007) Survey of Lifestyle, Attitudes and Nutrition in Ireland – Main Report, Department of Health and Children: 100-101.
[14] Musingarimi, P. (2008) Obesity in the UK: A Review and Comparative Analysis of Policies within the Devolved Regions, international Longevity Centre: 8-11.
[15] Triglycerides consist of three individual fatty acids bound together in a single large molecule; an energy source forming much of the fat stored by the body
[16] Thermogenesis - the production of heat in the body by physiological processes
[17] Wilborn, C. et. al. (2005), Obesity: Prevalence, Theories, Medical Consequences, Management, and Research Directions, Journal of the International Society of Sports Nutrition, 2(2): 4-31
[18] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3, page 48
[19] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Executive Summary, page 8
[20] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3, page 46
[21] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3, page 46
[22] Obesity and Genetics: A Public Health Perspective, CDC, Office of Public Health Genomics, www.cdc.gov/genomics/training/perspectives/files/obesedit.htm
[23] Zlot, A. et. al. (2007), Addressing the Obesity Epidemic: A Genomics Perspective, Preevnting Chronic Disease, 4(2), A31, http://ukpmc.ac.uk/articlerender.cgi?artid=1029831
[24] Mutation - any alteration in the inherited nucleic acid sequence of the genotype of an organism.
[25] Zlot, A. et. al. (2007), Addressing the Obesity Epidemic: A Genomics Perspective, Preevnting Chronic Disease, 4(2), A31 http://ukpmc.ac.uk/articlerender.cgi?artid=1029831
[26] Thermogenesis - the production of heat in the body by physiological processes
[27] Zlot, A. et. al. (2007), Addressing the Obesity Epidemic: A Genomics Perspective, Preventing Chronic Disease, 4(2), A31 http://ukpmc.ac.uk/articlerender.cgi?artid=1029831
[28] Allele - Any of the possible forms in which a gene for a specific trait can occur
[29] Major Genetic Study Identifies Clearest Link Yet to Obesity Risk, Wellcome Trust, Press Releases, 13 April 2007, http://www.wellcome.ac.uk/News/Media-office/Press-releases/2007/WTX036897.htm
[30] Brain genes associated with obesity, 15th December 2008, www.mrc-epid.cam.ac.uk/News/NewsArchive/Obesity_&_Brain.htm
[31] A variant near the PTER gene, a variant found in the NPC1 gene, and a variant near the MAF gene, which controls the production if the hormones insulin and glucagon
[32] Childhood obesity risk increased by newly-discovered genetic mutations, Imperial College London, News Release, 18th January 2009
[33] Hypothalamus - The part of the brain in vertebrates that lies below the thalamus and cerebrum. It controls the autonomic nervous system and the secretion of hormones by the pituitary gland.
[34] Coll, A. P. et. al. (2007) The Hormonal Control of Food Intake, Cell, 129(2), 251-262, Abstract, http://www.cell.com/abstract/S0092-8674(07)00447-3
[35] Understanding the hormonal control of appetite may be key to effective anti-obesity treatments, Wellcome Trust, News and Features, 12th February 2007, www.wellcome.ac.uk/News/2007/News/WTD026336.htm
[36] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3, page 44
[37] Cone, D. (2005), Anatomy and regulation of the central melanocortin system, Nature Neuroscience, 8, 571-578, Abstract, www.nature.com/neuro/journal/v8/n5/abs/nn1455.htm
[38] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.2, page 47
[39] Barker, D.J.P. (2006), Obesity and early life, Obesity Reviews, 8 (suppl. 1), 45-49
[40] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.2, page 47
[41] Ong, K., Determinants of fetal growth and childhood obesity, MRC Epidemiology Unit, www.mrc-epid.cam.ac.uk/Research/Growth/
[42] Eight factors for childhood obesity, www.dailymail.co.uk/health/article-349378/Eight-factors-childhood-obesity.html
[43] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.3.2, page 50
[44] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 29
[45] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.3, page 48
[46] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.3.1, page 49
[47] Wardle, J. (2007), Eating behaviour and obesity, Obesity Reviews, 8 (Suppl. 1), 73-75
[48] Speed of eating ‘key to obesity’, BBC News Channel, 22 October, 2008, http://news.bbc.co.uk/1/hu/health/7681458.stm
[49] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.3.1, page 49
[50] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.3.1, page 48
[51] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 25
[52] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 29
[53] Swinburn, B. et. al. (2002), Preventative strategies against weight gain and obesity, Obesity Reviews, 3(4), 289-301
[54] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.4, page 52
[55] Lake, A. and Townshend, T. (2006), Obesogenic environments: exploring the built and food environments, The Journal of the Royal Society for the Promotion of Health, 126(6), 262-267
[56] Lake, A. and Townshend, T. (2006), Obesogenic environments: exploring the built and food environments, The Journal of the Royal Society for the Promotion of Health, 126(6), 262-267
[57] Lake, A. and Townshend, T. (2006), Obesogenic environments: exploring the built and food environments, The Journal of the Royal Society for the Promotion of Health, 126(6), 262-267
[58] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3.4.3, page 54
[59] www.neoen.org.uk
[60] Law, C. et. al. (2007), Obesity and health inequalities, Obesity Reviews, 8 (Suppl. 1), 19-22
[61] The changing social pattern of obesity, Public Health Research Consortium, Short Report 4, January 2008
[62] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 32
[63] Law, C. et. al. (2007), Obesity and health inequalities, Obesity Reviews, 8 (Suppl. 1), 19-22
[64] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 35
[65] DHSSPS (2008) ‘Obesity time bomb is ticking louder than ever – north and south’, Press release.
[66] DHSSPS (2005) Fit Futures – Focus on Food, Activity and Young People, DHSSPS: 6.
[67] International Journal of Obesity (2005) Ten year trends for fatness in Northern Irish adolescents: the Young Hearts Projects, repeat cross-sectional study, 29: 579-585 – cited in NIAO (2007) The Performance of the Health Service in Northern Ireland, NIAO: 14.
[68] NISRA (2006) Northern Ireland Health and Social Wellbeing Survey 2005-2006 – Topline Results – Adult Obesity – document available electronically at: http://www.csu.nisra.gov.uk/adult per cent20obesity.pdf
[69] Statistics from the Health and Wellbeing Survey 2005-06 compiled by the Public Health Information and Research Branch.
[70] DHSSPS (2002) Investing for Health, DHSSPS.
[71] Presentation to the HSSPS Committee by Dr Michael Ryan, Miss Cheryl Flanagan and Mrs Donna Hanna, 29th September 2008.
[72] Presentation to the HSSPS Committee by Dr Michael Ryan, Miss Cheryl Flanagan and Mrs Donna Hanna, 29th September 2008.
[73] DHSSPS (2005) Fit Futures – Focus on Food,, Activity and Young People, DHSSPS: 46.
[74] Boyce, T., Robertson, R. and Dixon, A. (2008) Commissioning and Behaviour Change – Kicking Bad Habits final report, Kings Fund: 1.
[75] Wanless, D. (2004) Securing Good Health for the Whole Population – Final Report, HM Treasury.
[76] Boyce, T., Robertson, R. and Dixon, A. (2008) Commissioning and Behaviour Change – Kicking Bad Habits final report, Kings Fund: 1.
[77] Musingarimi, P. (2008) Obesity in the UK: A Review and Comparative Analysis of Policies within the Devolved Regions, international Longevity Centre: 13.
[78] DHSSPS (2002) Investing for Health, DHSSPS: 61.
[79] DHSSPS (2005) Fit Futures – Focus on Food,, Activity and Young People, DHSSPS: 11.
[80] Northern Ireland Audit Office (NIAO) (2008) The Performance of the Northern Ireland health service, NIAO, October.
[81] Northern Ireland Audit Office (NIAO) (2009) Obesity and Type 2 Disorders in Northern Ireland, NIAO: 20.
[82] Northern Ireland Audit Office (2009) Obesity and Type 2 Diabetes in Northern Ireland, NIAO: 22-23.
[83] Northern Ireland Audit Office (2009) Obesity and Type 2 Diabetes in Northern Ireland, NIAO: 21-22.
[84] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 134.
[85] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 4.1, page 62
[86] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 4.1.1, page 62
[87] Dehghan, M. at. Al. (2005), Childhood obesity, prevalence and prevention, Nutrition Journal, 4, 24, www.nutritionj.com/content/4/1/24
[88] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, Priority Approaches, pages 59 - 73
[89] NICE Clinical Guideline 43, Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children, Dec. 2006, www.nice.org.uk/CG043, pages 8-11
[90] www.library.nhs.uk/SpecialistLibrarySearch/Download.aspx?resID=270413
[91] NHS, Care pathway for the management of overweight and obesity, May 2006, www.library.nhs.uk/SpecialistLibrarySearch/Download.aspx?resID=270413 page 6
[92] NHS, Care pathway for the management of overweight and obesity, May 2006, www.library.nhs.uk/SpecialistLibrarySearch/Download.aspx?resID=270413 pages 7-9
[93] Pryke, R. and Docherty, A. (2008), Obesity in primary care: evidence for advising weight constancy rather than weight loss in unsuccessful dieters, British Journal of General Practice, 58(547), 112-117
[94] NHS, Care pathway for the management of overweight and obesity, May 2006, www.library.nhs.uk/SpecialistLibrarySearch/Download.aspx?resID=270413 page 10
[95] Scheen, A.J. (2008), The future of obesity: new drugs versus lifestyle interventions, Expert Opinion, Investigating Drugs, 17(3), 263-267.
[96] www.counterweight.org
[97] www.counterweight.org/PCTInfo.html
[98] NHS, Care pathway for the management of overweight and obesity, May 2006, www.library.nhs.uk/SpecialistLibrarySearch/Download.aspx?resID=270413 page 11.
[99] http://domuk.org/wp-content/uploads/2008/05/ben-pct-primary-care-specialist-obesity-service-march-08.ppt
[100] Korenkov, M. and Sauerland S. (2007), Clinical Update: bariatric surgery, The Lancet, 370, 1988-1990
[101] Benefits of weight-loss surgery, National Obestity Forum, www.nationalobesityforum.org.uk/obesity-news-centre-mainmenu-183/research-reports-mainmenu-186/326-benefits-of-weight-loss-surgery.html
[102] Surgery is ‘only means to healthy weight loss’ The Independent, 9 Sept. 2008, http://www.independent.co.uk/life-style/health-and-wellbeing/health-news/surgery-is-only-means-to-healthy-weight-loss-923481.html
[103] Korenkov, M. and Sauerland S. (2007), Clinical Update: bariatric surgery, The Lancet, 370, 1988-1990
[104] www.patient.co.uk/showdoc/40025123
[105] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 77
[106] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 81
[107] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 98
[108] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 118
[109] Fit Futures: Focus on Food, Activity and Young People, Report to the Ministerial Group on Public Health (Northern Ireland), DHSSPS, Dec. 2005, page 119
[110] www.dh.gov.uk/en/News/Currentcampaigns/Change4life/index.htm
[111] www.nhs.uk/change4life/Pages/make.aspx
[112] Nine ‘healthy towns’ get £30m pot, BBC News Channel, 10th November 2008, http://news.bbc.co.uk/1/hi/health/7719304.stm
[113] www.mendprogramme.org
[114] www.watchit.nhs.uk/?about.different
[115] http://carnegieweightmanagement.com/programmes/
[116] Truby, H. et. al. (2006), Randomised controlled trial of four commercial weight loss programmes in the UK: initial findings from the BBC ‘diet trials’, BMJ, http://www.bmj.com/cgi/content/abstract/332/7553/1309
[117] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science, Section 3, page 73
[118] See Tackling Obesities: Future Choices Project website at: http://www.foresight.gov.uk/OurWork/ActiveProjects/Obesity/Obesity.asp
[119] Also see the tables in Appendix 2 for the Foresight Report’s ‘Criteria checklist for an effective obesity strategy’
[120] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 128.
[121] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 120.
[122] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 122
[123] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 122
[124] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 122
[125] Butland, B. et al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 122.
[126] www.procor.org/community/community_show.htm?doc_id=702368
[127] Fat fighting scheme works for rich and poor, Sunday Age (Melbourne, Australia), July 27, 2008
[128] NSW Govt to launch obesity prevention trial, ABC Premium News (Australia), Feb. 17th 2007
[129] Australia’s biggest obesity trial launched, http://www.health.nsw.gov.au/news/2007/20070219_01.html
[130] Andre Chagnon, provided half of the $400 million from is charitable foundation, the Fondation Lucie et Andre Chagnon
[131] Couillard kicks off anti-obesity campaign, The Gazette (Montreal), October 24, 2006
[132] Ex-cable guy to fund Quebec’s obesity fight, The Toronto Star, Oct 24, 2006
[133] Happy 10 Pilot Intervention, Beijing, China, www.procor.org/community/community_show.htm?doc_id=680570
[134] EPODE, http://www.epode.fr/pdf/communiques/lancement_en.pdf
[135] www.arphs.govt.nz/Publications_reports/archive/child_obesity/childhood_obesity.pdf, pages 53-54
[136] www.arphs.govt.nz/Publications_reports/archive/child_obesity/childhood_obesity.pdf, page 55
[137] Physical activity and health in Europe, Evidence for Action, WHO Europe (2006), Edited by Cavill, N. et. al., page 22
[138] Physical activity and health in Europe, Evidence for Action, WHO Europe (2006), Edited by Cavill, N. et. al., page 18
[139] www.cdc.gov/nccdphp/dnpa/obesity/state_programs/about_us.htm
[140] www.take10.net
[141] www.catchinfo.org/whatis.asp
[142] www.procor.org/community/community_show.htm?doc_id=680552
[143] www.healthyhawaii.com/about_hhi/about_start_living_healthy/about_the_healthy_hawaii_initiative.htm
[144] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 133-135.
[145] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 133-135.
[146] Butland, B. et al (2007) ‘Tackling Obesities: Future Choices – Project Report’, 2nd edition, Government Office for Science: 133-135.
NI Assembly Research Paper
The CATCH Program (Coordinated Approach to Child Health)
A US. Obesity-Related Initiative for School Children
1. Origin of the CATCH Program – The CATCH Main Research Trial
The CATCH Program was originally known as the Child and Adolescent Trial for Cardiovascular Health. It was a multi-component, multi-year coordinated school health promotion program for elementary school children designed to decrease fat, saturated fat and salt in children’s diets, increase physical activity and prevent tobacco use. This original controlled clinical trial was evaluated between 1991 and 1994 in 96 schools (56 intervention schools and 40 control schools) in the four states of California, Louisiana, Minnesota and Texas. It was the largest school-based health promotion study ever funded in the US[1] and included “school environmental modifications related to food consumption, physical activity, and tobacco use. CATCH cafeterias were instructed to serve foods lower in fat, saturated fat and sodium; the physical education teachers were instructed to ….increase moderate to vigorous physical activity for at least 50% of class time; and school-wide policies were implemented to establish non-tobacco use"[2].
Study results showed that as a result of CATCH, “students in the intervention schools significantly increased time spent in moderate to vigorous physical activity within physical education classes (from 40% to 50%) and considerably decreased their consumption of fat in school meals (from 39% to 32%)"[3].
Five years after the main trial ended a study showed that the school-based CATCH program could be sustained and identified the factors of staff training, a program champion, adequate administrative support and adequate resources as being essential for maintaining the program successfully over time[4]. A 3-year follow-up study between 1995 and 1998 of 73% of the original CATCH participants found that they had “maintained a diet considerably lower in fat and saturated fat and participated in more vigorous physical activities in grades six through eight than did students in control groups"[5].
In 1999 CATCH was renamed Coordinated Approach to Child Health to reflect the shift from research trial to proven, sustainable schools program.
2. The CATCH Program (Coordinated Approach to Child Health)
2.1 Introduction
The present CATCH Program is built on the foundation of the original research trial and in 2006 received the Innovation in Prevention Award from the US Department of Health and Human Services’ National Prevention Summit. Currently CATCH is implemented in over 7000 schools and is marketed through Flaghouse Inc. who publish and distribute the program to schools and community organisations in the US and Canada[6].
Subsequent to the success of the original research trial, and with support from the CDC[7], the University of Texas (Houston) Prevention Research Centre has “endeavored to disseminate, implement and institutionalize the CATCH Program in schools". Specific CATCH Staff were employed to do so and such staff “became motivated to educate policymakers in Texas, which resulted in the development and passage of Senate Bill 19 in 2001 mandating that all elementary schools have a coordinated school health program by 2007"[8]. With the University of Texas (Houston) as the driving force of CATCH, Texan schools form the central hub of the Program and one third of all Texan elementary schools have adopted CATCH. Schools in Illinois, Maine, Florida, Georgia, North Dakota, North Carolina, and New Mexico, however, now also use the Program.
“CATCH is proving to be sustainable and feasible in a wide variety of settings. The program provides hands-on training and is designed to minimize the burden on teachers. Dissemination is well under way, and interest continues to grow"[9].
2.2 CATCH – Overview of the Program
This information is extracted from the main CATCH website[10].
The CATCH Program brings schools, families, and communities together to teach children how to be healthy for a lifetime. CATCH is effective because healthy behaviours are reinforced through a coordinated approach in the five areas of the Classroom, the Cafeteria, Physical Education, at Home, and After School.
In the Classroom - The CATCH Go for Health Series is a classroom health education curriculum that teaches children to identify, practice, and adopt healthy eating and physical activity habits. Hands-on activities encourage changes in behavior that support healthful eating and physical activity patterns-primary risk factors of heart disease, osteoporosis, high blood pressure, and obesity.
In Physical Education - CATCH PE combines high energy, non-elimination activities with teaching strategies that keep kids moving and having fun. CATCH PE significantly increases physical activity levels of students during PE class, and provides for a variety of experiences for students of all abilities.
In the Cafeteria - The CATCH Program considers school cafeterias an extension of the classroom. Through the Eat Smart component, breakfast and lunch become opportunities for children to learn, practice, and adopt healthy eating habits. School Food Service personnel prepare healthier meals and help coordinate healthy messages with the rest of the school.
At Home - The CATCH Family component is designed to get students, parents, and extended family members involved in practicing and adopting healthy eating and physical activity at home. By doing so, the home environment becomes an extension of the CATCH Program at school.
In the Community - Implemented in community-based programs across North America, CATCH Kids Club, has been designed for after-school and summer-school settings. Developed from the CATCH Program, healthy messages are reinforced beyond the school day via physical activity and nutrition education sessions.
2.3 The Five Component Areas – Further Detail
The information in this section is extracted and summarised from the Texas CATCH website[11].
2.3.1 The Classroom
The CATCH Go for Health Series is the classroom health education curriculum that teaches children to identify and adopt healthy eating and physical activity habits, with children learning the facts about healthy living every day as “lessons blend health topics with performance standards of core academic subjects such as graphing, understanding informational text, quantitative reasoning and formulating testable hypotheses" [12].
The Go for Health Series is based on Social Learning Theory “which targets changes in specific environmental, personality and behavioural factors that influence children’s health behaviour. A sequential storyline throughout the curricula revolves around a group of cartoon characters, Hearty Heart and Friends"[13].
The Curriculum materials for teachers ensure minimal preparation time and contain detailed descriptions of lesson procedures. Lessons can stand-alone or may be used to supplement other core content areas such as mathematics or language. Teaching guides contain ready-to-use materials such as reproducible hand-outs and transparency masters.
2.3.2 Physical Education
CATCH PE is an age appropriate physical education program which develops health related fitness, skill competency, and cognitive understanding about the importance of physical activity. CATCH PE kits for schools provide instruction via a variety of learning experiences, which address the wide-range of student ability in physical education class. The content enhances, not just sports skills, but also movement skills, physical fitness, social development, and aims to promote lifelong physical activity. The aim of CATCH PE is to provide[14]:
- movement which targets individual fitness and skill levels of all learners;
- Increased moderate-to-vigorous physical activity in physical education class;
- Adequate amounts of physical activity now and throughout life;
- Maximise time on task and learning opportunities; and
- Engage students in fun and motivating activities.
2.3.3 The Cafeteria[15]
The CATCH Eat Smart school cafeteria is described as a hands-on learning environment. At mealtime, children learn and practice healthy eating habits. The CATCH classroom and physical education lessons “come to life" as children experience first hand the concepts of “GO, SLOW and WHOA" foods. The foods on the school menu are marked as GO, SLOW or WHOA. For example, fruits and vegetables are GO foods, if fat is added to them they become SLOW foods and if they are fried they are WHOA foods. The concept is that GO, SLOW and WHOA foods can be eaten every day but the main foods in the diet should be GO foods.
Overall CATCH Eat Smart:
- Provides children with tasty meals that are lower in fat and saturated fat;
- Maintains required levels of essential nutrients and student participation;
- Coordinates healthy nutrition messages with other areas of the school; and
- Guides the entire school towards creating a healthy school environment.
The CATCH Eat Smart School Nutrition Program Guide is a tool for child nutrition service providers. The guide provides menu planning and food preparation suggestions. Suggestions are provided on how to gradually modify recipes to lower the fat, saturated fat, and sodium. The importance of program promotion is discussed and promotional methods are included. Nutritional fact sheets and supplemental activities which support the CATCH Classroom program help coordinate the cafeteria health message school-wide.
2.3.4 Family Component[16]
The CATCH Family component is designed to get students, parents and extended family members involved in practicing and adopting healthy eating and physical activity behaviors at home. The home environment becomes an extension of the CATCH Program at school and by creating this strong link between teachers and parents enhances the chances that the lessons learned at school will become a permanent part of a child’s life.
The CATCH ‘Home Team’ in the school:
- Provides multiple opportunities for parents and family member to visit the school and actively participate in CATCH activities;
- Serves as an educational program that motivates parents to change their own behaviours;
- Influences environmental change in the home that reflects the change in environment in the school; and
- Get families involved as much and as often as possible.
An integral component of the CATCH curriculum is parental involvement through homework assignments the children complete with their parents or an adult at home or away from school. Specific assignments are embedded in the lessons of each year’s classroom curriculum. Upon completion of each assignment, children earn points that are monitored by the classroom teacher. Extra points are earned when a parent or adult participates in the assignment. Parental involvement is also through participation in activities at school. CATCH Family Fun Nights provide a fun atmosphere for parents, community members, school personnel and children to come together and celebrate healthy living principles with CATCH oriented physically active games, snacks and children’s performances. CATCH schools are encouraged to plan and conduct a Family Fun Night each year.
2.3.5 In the Community – CATCH Kids Club[17]
The CATCH Kids Club (CKC) is a physical activity and nutrition education program designed for elementary school aged children in an after-school/summer setting. CKC is composed of nutrition education materials (including snack activities) and a physical activity component. The CKC program offers an easy-to-use format that both children and staff enjoy and is ready to implement in the after-school and summer settings.
During 1999-2000, the CKC underwent pilot testing and formative evaluation in 16 after-school sites in Texas. The results showed that CATCH Kids Club is inclusive (everybody plays), and it has been demonstrated to increase children’s physical activity and their nutrition knowledge and intentions. The education component aims to equip children with the knowledge, skills, self-efficacy, and intentions to make healthy dietary and physical activity decisions.
3. Lessons Learned From The CATCH Program
A recent review of the CATCH program has indicated the following lessons learned from the development and dissemination of the program[18]:
- The inclusion of teachers, school food service employees, school administrative staff, pupils and parents, during the development of the CATCH program has ensured the acceptability of the program;
- Successful dissemination of the CATCH program has required professional program staff who contact decision-makers, present the program at meetings, conduct training for schools and ensure quality control of the program;
- Within schools the supportive involvement of a school principal or other senior administrator is crucial;
- The effective training of interdisciplinary teams within schools (i.e. classroom and physical education teachers and food service staff) is important for success; and
- To gain support of teachers, the prepared CATCH lessons are aligned with applicable education standards and are provided with sufficient training for teachers.
[1] Funded by the National Heart, Lung and Blood Institute
[2] CATCH Texas, Science of CATCH, www.sph.uth.tmc.edu/catch/about_science.htm
[3] Franks, A.L. et. al. (2007), School-based Programs: Lessons Learned from CATCH, Planet Health, and Not-on-Tobacco, Preventing Chronic Disease 4(2), A33
[4] CATCH Texas, Science of CATCH, www.sph.uth.tmc.edu/catch/about_science.htm
[5] Franks, A.L. et. al. (2007), School-based Programs: Lessons Learned from CATCH, Planet Health, and Not-on-Tobacco, Preventing Chronic Disease 4(2), A33
[6] Spreading CATCH – Coordinated Approach to Child Health through America, www.changemakers.net/node/1124
[7]Centers for Disease Control and Prevention (US)
[8] CATCH for Improved Physical Activity and Diet in Elementary School Children: Effective and Successfully Disseminated, CDC, Prevention Research Centers (2007), http://www.cdc.gov/PRC/selected-interventions/adoptable-interventions/catch-improved-physical-activity-diet-elementary-school.htm
[9] CATCH for Improved Physical Activity and Diet in Elementary School Children: Effective and Successfully Disseminated, CDC, Prevention Research Centers (2007), http://www.cdc.gov/PRC/selected-interventions/adoptable-interventions/catch-improved-physical-activity-diet-elementary-school.htm
[10] What is CATCH? www.catchinfo.org/whatis.asp?
[11] http://www.sph.uth.tmc.edu/catch/
[12] CATCH Classroom Curriculum, www.sph.uth.tmc.edu/catch/curriculum_go_for_health.htm
[13] CATCH Classroom Curriculum, www.sph.uth.tmc.edu/catch/curriculum_go_for_health.htm
[14] CATCH Physical Education, www.sph.uth.tmc.edu/catch/curriculum_pe.htm
[15] CATCH Eat Smart Cafeteria, www.sph.uth.tmc.edu/catch/curriculum_eat_smart.htm
[16] CATCH Family Component, www.sph.uth.tmc.edu/catch/curriculum_home_team.htm
[17] CATCH Community Component, www.sph.uth.tmc.edu/catch/KidsClub.htm
[18] Franks, A.L. et. al. (2007), School-based Programs: Lessons Learned from CATCH, Planet Health, and Not-on-Tobacco, Preventing Chronic Disease 4(2), A33
NI Assembly Research Paper
Norwegian Nutrition Policy and Nutrition Campaigns (March 2009)
1. Introduction
The promotion of nutrition policy in any country is based on “a belief in State involvement to solve what is considered to be a social problem". However this involvement is complicated by “the liberal aim of sustaining the autonomy of the individual"[1]. This dilemma will influence the role that a state ultimately plays and to what extent information, fiscal and legal measures are applied. With reference to the traditional Scandinavian ‘social democratic’ solution, based on the belief of obtaining social welfare through market regulation, “decisions are commonly made as negotiated solutions between the state and organised interests"[2]. With respect to nutrition, there appears to be agreement within the Scandinavian region that efforts should be widespread so, in spite of conflicts with the agricultural sector, nutritional advice and its relevance for public policy has always been high.
Norwegian nutritional policy and nutrition campaigns have received considerable interest over the years, for several main reasons. Firstly Norway was among the first industrialised country to respond to the call from the World Food Conference in 1974 to produce a nutrition policy[3] and its policy is therefore the oldest and best established of the Scandinavian countries. Secondly, the distinguishing feature of its nutrition policy has been its “structural orientation, i.e. towards production and market regulation, as opposed to individual, information-based strategies"[4]. Such policy was possible because of “distinctive Norwegian political traditions, with a heavily regulated agricultural sector, combined with a welfare policy tradition emphasising influence on other sectors"[5].
2. Changes in the Norwegian Diet
Norwegian nutrition policy has focused extensively on fat reduction and this is where the results have been most positive. Over the past 25-30 years the proportion of fat in the Norwegian diet has decreased from 40% in 1975 to 34% in 2000 (however, the proportion of saturated fat has remained fairly constant). This decrease has been compensated by an increase in the amount of bread and other grain products and of sugar in the diet. The consumption of vegetables has increased by 52% form 1975 to 2000, while fruit consumption has increased marginally and that of potatoes has decreased[6].
The impact these changes have had on health is undecided. It is known that the incidence of coronary heart disease (between the ages of 0 – 79 years) has decreased by 30-40% from 1970 to 1992 (however, it is understood that Finland and Sweden saw larger decreases of 50-60% during this period), but “body weight has increased considerably in this period (men up to 9.1Kg) followed by an increase in type II diabetes"[7].
3. Norwegian Nutrition Policy - Time-line and Brief Details of Main Nutrition Policies and Initiatives (1960’s to present day)
3.1 1960s and 1970s
After World War II, the Nordic countries experienced a sharp increase in the incidence of cardiovascular disease and in 1968 Nordic experts agreed on a redefinition of nutrition recommendations that recognised the association between fat consumption and cardiovascular disease. This “challenged the …extensive subsidies to the dairy industry…From a status as essential foods, full-fat milk and butter were turned into a nutritional problem"[8]. Within the setting of controversy between nutrition recommendations and agricultural interests the nutrition recommendations were formulated in the 1976 first white paper from the Ministry of Agriculture, ‘Report on Norwegian Nutrition and Food Policy’, with goals of fat reduction included but moderated. It was noted as a political success but the policy was quite ambivalent as it tried to “match the needs of improved health through food behaviour changes with those of the (dairy dominated) agricultural sector"[9]. This first white paper was “closely linked with policies of agricultural self-sufficiency and regional development"[10]. The policy goals were divided in to four broad categories as follows[11]:
- Health – encourage healthy dietary habits, with the specific objective of decreasing fat consumption from 42% to 35% of total calorie intake, and a decrease in the ratio of saturated to polyunsaturated fats in the diet from 3.5:1 to 2:1 by reducing consumption of whole milk and margarine. The aim was an increase in the consumption of complex carbohydrates, fish and skimmed milk;
- Global Aid – to help stabilise world food supply in accordance with the recommendations of the World Food Conference (Rome, 1974) and decrease reliance on imported food which could be diverted to developing countries;
- Food Production – Promote consumption of domestically produced food and strengthen national food self-sufficiency; and
- Rural Economy – Strengthen the rural economy and halt decline in the number of small farms by making farming more profitable.
These goals were to “be achieved through a variety of implementation strategies to change the process of food production and distribution, and to provide consumers with information and incentives to choose a health-enhancing diet"[12]. One of the most visible measures was the “dramatic increase between 1973 and 1980 in the consumer price subsidies on domestically produced food as well as direct support to farmers to expand the total agricultural area"[13].
3.2 1980s
In 1981 there was a new white paper from the Ministry of Health and Social Affairs, in which the link between nutrition and health was emphasised and placed nutritional problems on the political agenda. The policy stressed “that the alterations in diet should take place by voluntary changes in food habits" and that it was “a public and community responsibility to ensure that circumstances are optimized to enable people to choose a nutritionally favourable diet"[14]. A wide range of measures were used to improve the diet including legal, economic, organisational and educational. There was a definite shift “toward implementation strategies emphasizing health education and individual responsibility for change"[15]. Nutrition, at this time, was regarded as an issue of knowledge and behaviour rather than a problem of food supply.
In the 1980s’ the National Nutrition Council of Norway (established in the 1940s) also moved its agenda towards health by removing industry representatives and keeping only experts within the fields of nutrition and medicine. It also became the National Council for Nutrition and Physical Exercise, thus combining another field of health promotion[16]. However this National Council for Nutrition and Physical Exercise has now been replaced by an expert advisory board on nutrition that, along with similar boards, has secretarial functions placed within the Health Authority[17].
In 1982 the ‘Everyday Food’ Nutrition Campaign was launched. The following information regarding the campaign is extracted from Blythe, C.R. (1984) The Norwegian nutrition campaign: setting goals and assessing results[18]. The dietary goals of the campaign were presented as a series of small changes in the daily meal routine, for example, spreading butter thinly, using low fat varieties of traditional dairy products. Prohibitions were avoided and a major theme was sensible eating during the week meant you could, more or less, eat what you liked at the weekends. Educational material for young children developed this idea of ‘everyday food’ and food to enjoy at weekends in books entitled “Best Friends and Saturday Friends".
The campaign was launched with a press conference, television and radio items and articles in the press. Posters were displayed in streets and on public transport. Fact sheets, school books, wall charts and games were produced. The centre piece was the widely advertised book Everyday Food.
The campaign placed a strong emphasis on involving people at local levels including worker’s organisations, works canteens, institutional caterers, women’s organisations, libraries and small food shops – all were encouraged to hold discussion groups, redesign menus, display posters and stock brochures.
3.3 1990s
In the early 1990s the third white paper, Challenges in Health Promotion and Prevention Strategies, was published by the Ministry of Health and Social Affairs and again the link between nutrition and health was emphasised. Policy became much more concerned with the prevention of diseases other than just cardiovascular disease, such as cancer, and promoted the consumption of fruit and vegetables. However, “far from being incorporated into a general health promotion agenda…nutrition policy seems to have retained a considerable part of its characteristic approach. Even now, indirect influence on the food market by negotiating with and influencing other sectors and actors is exercised with explicit ambitions…expressed as ‘healthy food should be easy to get’"[19]
In 1990-94, the Norwegian National Association for Public Health together with the National Nutrition Council and other voluntary and professional organisations, implemented a nation-wide campaign called ‘Spis med glede’ (Enjoy Eating). The campaign specifically targeted the retail sector, school children and the elderly. It focused on the enjoyment of food and highlighted positive messages focusing on the foods people should consume more of. Activities included ‘action weeks’ for bread, cereal, fish, fruit and vegetables, meat, milk and poultry, which included TV spots, brochures, in-shop demonstrations and exhibitions. The goals of the campaign were to[20]:
- Stimulate local activities which could change diet and exercise habits;
- Find key groups to disseminate information on diet and health;
- Stimulate collaboration between authorities, voluntary organisations, industry and the media in activities related to improving food habits;
- Increase understanding of the cultural and social meanings of food; and
- Target the retail sector to establish collaboration among food suppliers, wholesalers, retail chains and organisations
3.4 Current Policy and Problems
The most recent Norwegian Action Plan on Nutrition (2007-2011) ‘Recipe for a Healthier Diet’[21] has been developed through the collaboration of 12 Ministries. The plan contains specific measures to promote health and prevent illness by changing eating habits in line with nutrition recommendations. Reducing social inequalities in diet is a main goal. The measures emphasise contributions that make it easier to make healthy choices, facilitate healthy meals in kindergarten, schools and among the elderly, and increase knowledge about food, diet and nutrition. The Action Plan is a follow-up of White paper No. 16 (2002–2003) – Recipe for a healthier Norway, and signals a stronger focus on disease prevention work, physical activity and diet. The plan is linked with the Nordic Plan of Action for Better Health and Quality of Life through Diet and Physical Activity, adopted July 2006, and the Action Plan on Physical Activity (2005–2009) Working together for physical activity.
Norway has in recent years seen a new food-related problem in the increase of sugar consumption, especially among young people. In this instance nutritional policy proponents appear to be “directing attention towards individual responsibility …as a question of personal discipline", as “the institutional ‘landscapes’ of milk, fruits and vegetables do not fit for sugar, and the issue seems to evade an understanding of sugar as a social problem"[22].
Also now on the Norwegian agenda is school catering. There are no public school meals in Norway and children bring lunch from home. They can subscribe to milk and in some schools to the delivery of fruit. Through the Action Plan on Physical Activity (2005-2009) schools are considered a key setting for health-promoting interventions and models for school meals and daily physical activity at school are being tested. There are presently ongoing discussions around including one hour of daily physical activity as a national requirement and providing free school meals[23].
4. Concluding Comments
The Norwegian nutrition policy to date has been based on the premise that it is both feasible and worthwhile to declare through political decisions how the population should eat and regulate food supply accordingly and to alter the policy as nutritional advice is updated.
Historically the Norwegian policy is distinguished by its ‘structural’ orientation towards production and market regulation as opposed to individual, information-based strategies. However, over the past 10-15 years the focus has moved away from agriculture towards the health sector and schools and the present policy is more of a combination of the traditional ‘indirect’ measures and a health policy. “It is still an open question how this policy can handle the new emerging problems of increasing sugar consumption, overweight etc"[24].
With respect to lessons for Northern Ireland, it is not yet clear whether current Norwegian nutrition policy will manage to stem the rise of obesity in Norway. Although not yet at the level of that in the UK, the growing obesity epidemic “has arrived in Norway" as “in 1984 the obesity rates were eight percent for men and nine percent for women [and] the figures from 2000-2003 show a rate of 19 percent for men and 16 percent for women"[25].
Norway’s historically successful nutrition policy was first developed in the 1970’s as a direct response to the rising levels of cardiovascular disease and the result was a shift in the national diet to one including firstly less fat and subsequently more fruit and vegetables. However, as stated above it is only in recent years that the nutrition policy has moved towards a health promotion agenda and is yet to be determined if it will succeed in tackling the newest dietary problems in Norway of increased sugar consumption and rising levels of obesity.
Despite not being designed specifically to tackle obesity, there may be aspects of the successful Norwegian nutrition campaigns of the 1980s (Everyday Food Campaign) and the 1990s (Spis med glede) which are transferable to a Northern Ireland context. Both campaigns focused on very positive messages rather than prohibitions, took a wide cross-sectoral collaborative approach, which involved the retail sector and industry, and had a strong emphasis on involving people at local levels.
[1] Kjaernes, U (2003), Food and nutrition policies of the Nordic countries: how they have been developed and what evidence substantiates the development of these policies?, Proceedings of the Nutrition Society, 62, 563-570, page 563
[2] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, An Institutional Approach
[3] Roos, G. et. al. (2002), Dietary Interventions in Finland, Norway and Sweden: nutrition policies and strategies, Journal of Human Nutr. Dietet., 15, 99-110, page 102
[4] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Abstract
[5] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Abstract
[6] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Introduction
[7] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Introduction
[8] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Post-war nutrition policy: the problem of fat
[9] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Post-war nutrition policy: the problem of fat
[10] Roos, G. et. al. (2002), Dietary Interventions in Finland, Norway and Sweden: nutrition policies and strategies, Journal of Human Nutr. Dietet., 15, 99-110, page 102
[11] Klepp, K-I and Forster, J.L. (1985), The Norwegian Nutrition and Food Policy, Journal of Public Health Policy, 6(4), 447-463, page 449
[12] Klepp, K-I and Forster, J.L. (1985), The Norwegian Nutrition and Food Policy, Journal of Public Health Policy, 6(4), 447-463, page 450
[13] Klepp, K-I and Forster, J.L. (1985), The Norwegian Nutrition and Food Policy, Journal of Public Health Policy, 6(4), 447-463, page 450
[14] Roos, G. et. al. (2002), Dietary Interventions in Finland, Norway and Sweden: nutrition policies and strategies, Journal of Human Nutr. Dietet., 15, 99-110, page 102
[15] Klepp, K-I and Forster, J.L. (1985), The Norwegian Nutrition and Food Policy, Journal of Public Health Policy, 6(4), 447-463, page 450
[17] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Post-war nutrition policy: the problem of fat, New Conditions – a new policy?
[18] Proceedings of the Nutrition Society (1984), 43, 239-241
[19] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, New Conditions – a new policy?
[20] Roos, G. et. al. (2002), Dietary Interventions in Finland, Norway and Sweden: nutrition policies and strategies, Journal of Human Nutr. Dietet., 15, 99-110, page 104
[21] http://www.regjeringen.no/upload/HOD/Dokumenter_FHA/SEM/Kostholdsplanen/IS-0238_kortversjon_eng.pdf
[22] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, New Conditions – a new policy?
[23] http://www.euro.who.int/eehc/implementation/20071218_28
[24] Kjaernes, U. (2003), Experiences with the Norwegian nutrition policy, Appetite, 41, 251-257, Final Comments
[25] One in Five Too Fat, Aftenposten, 04/01/07 www.aftenposten.no/english/local/article1588576.ece
NI Assembly Research Paper
Briefing paper relating to the English obesity strategy Healthy Weight, Healthy Lives (HWHL) published by the Department of Health in January 2008.
1. Background
Like other jurisdictions within the United Kingdom and the Republic of Ireland, the population in England has experienced a significant rise in levels of overweight and obesity over the last decade or so. According to the Health Survey for England 2007, between 1993 and 2007 there was ‘a marked increase in the proportion of adults who were obese.’ The proportion categorized as obese (BMI 30 or over) increased from 13 per cent of men in 1993 to 24 per cent in 2007 and from 16 per cent of women in 1993 to 24 per cent in 2007.[1] According to the Department of Health, obesity is responsible for approximately 9,000 deaths a year in England and is an important risk factor for a number of chronic diseases, including heart disease, stroke, some cancers and type II diabetes.[2]
Figure 1: Obesity prevalence trends (in England) from 1993-2005 adults, and children aged 2-15[3]
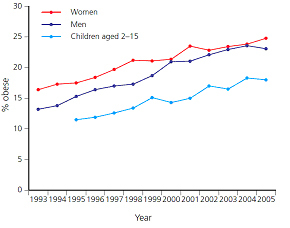
Given its significant population size and the wider projection contained within the 2007 Foresight report[4] that over half the UK population could be obese by 2050, there has been a concerted effort in recent years to tackle obesity in England. Currently only England is implementing a comprehensive, population-based strategy dedicated to tackling obesity throughout the life course. Published jointly by the Department of Health (DoH) and the Department for Children, Schools and Families (DCSF) in January 2008, Healthy Weight, Healthy Lives: a Cross-Government Strategy for England contains a number of ambitious targets to reduce levels of overweight and obesity. For example, one of the main targets identified within Healthy Weight, Healthy Lives, is that by 2020 the rising trend in obesity will have been reversed back to 2000 levels.[5]
2. Healthy Weight, Healthy Lives (2008)
Responding to the growing levels of overweight and obesity within the English population and building on the work of the Foresight programme, the UK Government launched a comprehensive, population-based obesity strategy in January 2008. An indication of the UK Government’s commitment to tackling rising levels of overweight and obesity in England is reflected in the decision to commit £372 million to support the various initiatives and programmes outlined within Health Weight, Healthy Lives over the period 2008-2011. This funding is over and above the £1.3 billion investment in school food, sport and play, and the £140 million additional funding for Cycling England allocated for 2008-2011.[6]
There is a focus within the English strategy on targeting the concerning rise in obesity among children and young people to counteract the ‘conveyor-belt’ in which excess weight in childhood continues into adulthood. The strategy highlights a study conducted in the United States which found that 55 per cent of obese 6-9 year olds and 79 per cent of obese 10-14 years remained significantly overweight or obese into adulthood.[7]
Healthy Weight, Healthy Lives builds on a number of key pieces of work around the obesity issue conducted by the Department of Health and other UK Government departments in recent years.[8] It should also be noted that prior to the publication of the English national obesity strategy, a number of Primary Care Trusts (PCT) had already drafted local action plans to tackle the growing obesity problem. The launch of Healthy Weight, Healthy Lives followed the implementation of a number PCT-led strategies which informed a ‘bottom-up’ approach to the strategic direction of obesity policy in England.
2.1 Key Areas of the Strategy
The central ambition of Health Weight, Healthy Lives is for England to be ‘the first major country to reverse the rising tide of obesity and overweight in the population by ensuring that all individuals are able to maintain a healthy weight.’ Underpinning this overriding target are five key areas to tackle obesity throughout the life course which were highlighted within the 2007 Foresight report. These are:
1. Promoting children’s health - early prevention of weight problems to avoid the ‘conveyor belt’ effect into adulthood;
2. Promoting healthier food choices – reducing the consumption of foods that are high in fat, sugar, salt, and increasing the consumption of fruit and vegetables;
3. Building physical activity into our lives – getting people moving as a normal part of their day;
4. Creating incentives for better health – increasing the understanding and value people place on the long-term impact of decisions;
5. Personalised advice and support – complementing preventative care with treatment for those who already have weight problems.[9]
2.2 ‘Cross-Government’ Implementation
A key feature of Healthy Weight, Healthy Lives which is congruent with an important recommendation that emerged from the Foresight report is the need for effective cross-Government implementation of the national obesity strategy. According to the Foresight report’s criteria checklist for an effective obesity strategy it is imperative to ensure, ‘suitable government managerial structures [are in place] to enable clear leadership, strategy formulation and co-ordination action across Government.’ Moreover, the report goes on to state that,
It is critical that any structure raises the profile of improving population health and enables government departments to work effectively together and to engage with other key partners on both strategy development and delivery.[10]
2.2.1 Cabinet Committee on Health and Well-being and Cross-Government Obesity Unit[11]
With the aim of providing leadership across the UK Government departments, a new Cabinet Committee on Health and Well-being was established. The remit of the committee includes tackling obesity and promoting healthy weight and, significantly, the membership includes all of the lead departments.
Meanwhile, reporting to the new Cabinet Committee is a new cross-Government Obesity Unity based in the Department of Health but led jointly with the Department for Children, Schools and Families. The Unit that includes staff and resources from across Government has a number of key responsibilities including:
- taking forward the commitment outlined in the Healthy Weight, Healthy Lives strategy;
- producing an annual report;
- leading across Government in developing further proposals as necessary to fulfill the ambition to reverse the rising tide of obesity and overweight;
- acting as the focal point for knowledge on healthy weight in Government;
- managing relationships between Government, industry and other stakeholders;
- building the evidence base on tackling obesity.
It is important to note that the Obesity Unit is supported in carrying out its responsibilities by an Expert Advisory Group of academics (building on the Foresight science advisers) and by a Delivery Reference Group. This group is composed of experienced representatives from across the delivery chain and across the country.
In continuing to support the development and evaluation of Healthy Weight, Healthy Lives, the Expert Advisory Group convened a horizon-scanning workshop in February 2009 with a wider group of public health (including obesity) experts. Participants in the different workshops included Dr Bryony Butland (one of the co-authors of the 2007 Foresight report) and Clara Swinson from the Department of Health’s Obesity Policy Team. Discussions during the event covered a range of issues including the impact of the current economic recession on population health and the development of Healthy Weight, Healthy Lives.[12]
3. ‘Delivering Change’ - Healthy Weight, Healthy Lives ‘One Year On’
In April 2009, the DoH and DCSF published the first annual progress report on the implementation of the national obesity strategy in England. Healthy Weight, Healthy Lives: One Year On highlights the extent to which the original key themes of the English obesity strategy have been taken forward in the government’s efforts to support individuals and families to achieve and maintain a health weight. The following section provides an overview of a selection of key programmes and initiatives identified within the main areas of the report.
3.1 Helping People Make Healthier Choices
While Healthy Weight, Healthy Lives represents a population-based strategy employing a life course approach to tackling obesity, young children and adolescents remain the primary target group to effect changes in their dietary choices and levels of physical activity. Two important programmes launched in the past year have sought to improve the availability of accurate information, the monitoring of children’s health and the promotion of positive attitudes and behaviours toward healthier diets and exercise.
3.1.1 Change4Life
Change4Life is a groundbreaking £75 million social marketing campaign designed to help us all eat better, move more and live longer.[13] Based on extensive academic and consumer research, the national advertising campaign provides a number of important insights into attitudes and behaviours related to obesity, diet and exercise. For example, the programme is intended to provide parents with a clear understanding of the links between poor diet and sedentary lifestyles and preventable illnesses. Its central aim is to create a social movement to support changes in attitude and behaviour related to diet and exercise.
The first phase of the campaign was primarily aimed at families with younger and pre-teen children whose current behaviour suggests that their children are the most at risk of weight gain. Forthcoming phases of the campaign aim to personalize the issue for parents, explaining how they can help prevent their children gaining excess weight. Meanwhile, throughout 2009-10, the DoH plans to extend Change4Life to other ‘at risk’ groups including very young children and those ethnic minority communities where levels of childhood obesity are particularly high, while continuing work with families. There is also an intention to launch Change4Life for at-risk groups of adults.[14]
3.1.2 National Child Measurement Programme
Of all the devolved regions, England has the most comprehensive data available.[15] Two key sources for collecting and collating this information is the Health Survey for England and the National Child Measurement Programme (NCMP). The NCMP which has experienced a number of important changes in recent years to enhance effectiveness is designed to improve awareness among parents of their child’s weight and provide support and advice where a child’s weight is a matter of concern. All parents of children aged 4 to 5 years old and 10 to 11 years of age receive feedback from Primary Care Trusts (PCT) and the data is accompanied by information to help parents interpret their child’s weight. Information on healthy living and signposting to follow-up services are provided as necessary. The vast majority of primary schools in England are now participating in the NCMP and around 50 per cent of PCTs routinely feed back results to parents, with all other PCTs providing results on request.[16]
3.2 Creating an environment that promotes healthy lifestyles
Drawing on the areas identified within the Foresight report that directly contribute to the ‘obesogenic’ environment, One Year On highlights a number of programmes currently being implemented that are designed to promote healthier weight in children, provide a supportive built environment and incentivise the adoption of healthier lifestyles.
3.2.1 Healthy Community Challenge Fund (HCCF)
Building on the emerging evidence contained within the Foresight report and elsewhere that making significant changes to the built environment can assist in effectively tackling obesity as well as climate change, the UK Government established the Healthy Community Challenge Fund (HCCF). The HCCF has provided funding to a small number of local areas throughout England including designated Healthy Towns. Since the establishment of the pilot scheme in November 2008 nine local towns/areas in England (Dudley, Halifax, Sheffield, Tower Hamlets (London), Thetford (Norfolk), Middlesbrough, Manchester, Tewkesbury and Portsmouth) are sharing in the £30 million investment which will be match-funded between 2008-2011.
In each of the nine local areas/towns their ideas on how to make activity and healthier food choices easier for local communities are being continually tested and evaluated. It is intended that maximum benefit will be derived from the schemes introduced within the nine areas and that learning is shared among a developing Healthy Town Network.[17]
3.2.2 Incentives for healthier lifestyles
One of the schemes introduced in Manchester as one of the designated Healthy Towns is called ‘Points4Life’. The loyalty scheme currently being piloted is designed to drive behaviourial change through rewarding individuals for making healthier choices around their diet and activity levels. Points are being awarded for those individuals making positive choices and these are redeemable against healthy goods and services from a range of public and private sector sources.[18]
3.3 Strengthening Delivery – ‘National Support for Local Delivery’
According to One Year On,
Government cannot and should not act alone to tackle obesity – all sectors of society have a part to play. The success of Healthy Weight, Healthy Lives depends on the commitment and effective relationships between different partners; central and local government; strategic health authorities, primary care trusts and primary care practitioners; schools and regional public health groups; and private and third sector organizations. We must all work in coalition, if we are to reduce the levels of obesity in our population.[19]
To ensure effective delivery of the national obesity strategy in England, One Year On identifies a number of key developments that have been implemented by Government to promote collaboration and joined-up working at the national level with key local delivery partners, including PCTs. These have included:
- setting a clear and national ambition for promoting healthy weight and including child obesity in the Child Health Public Service Agreement (PSA) to improve the health of all children and young people.
- allocating £69 million within the NHS allocations for 2009-10 to support PCTs as part of the overall allocation of £372 million for promoting the achievement and maintenance of healthy weight over the period 2008/09-2010/11;
- placing child obesity in the NHS Operating Framework as Tier Two national priority for local delivery meaning that all PCTs are required to set plans around child obesity prevalence for the period 2008/09-2010/11;
- putting in place a Child Obesity National Support Team (NST), which has played a pivotal role in supporting local areas.[20]
3.3.1 The Obesity Improvement Programme
Through its continuing work in local areas throughout England the NST has identified a number of significant gaps in understanding and capability and has recommended the expansion of support for local areas and partners to enable more effective delivery of programmes. In response, the cross–Government Obesity Unit has decided to establish a new Obesity Improvement Programme by mid-2009. The programme will provide more information, tools, training and innovation to strengthen local capabilities to prevent and treat overweight and obesity. As part of the Programme, a new website linked with the National Obesity Observatory will be launched providing a comprehensive listing of best practice and will provide a forum for sharing information and data.[21]
[1] The NHS Information Centre (2008) Health Survey for England 2007, The NHS Information Centre: 5.
[2] Department of Health (2007) Health Risk and Costs of Obesity, Department of Health we
[3] Department of Health (2008) Healthy Weight, Healthy Lives: a Cross-Government Strategy for England, Department of Health: 1.
[4] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 5. According to this report by 2015, 36 per cent of males and 28 per cent of females will be obese. By 2025, these figures are estimated to rise 47 per cent and 26 per cent respectively. By 2050, 60 per cent of males and 50 per cent of females could be obese (Page 5).
[5] Department of Health (2008) Health Weight, Healthy Lives; a Cross- a Cross-Government strategy, Department of Health: iii.
[6] Department of Health (2008) Health Weight, Healthy Lives; a Cross- a Cross-Government strategy, Department of Health: 28.
[7] Department of Health (2008) Health Weight, Healthy Lives; a Cross- a Cross-Government strategy, Department of Health: 1.
[8] See Department of Health (2004) Choosing Health – Making healthy choices easier, Department of Health; and Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science.
[9] Department of Health (2008) Health Weight, Healthy Lives; a Cross- a Cross-Government strategy, Department of Health: 5.
[10] Butland, B. et. Al. (2007) Obesities: Future Choices – Project Report, Second Edition, Foresight, Government Office for Science: 135.
[11] Information in this section is taken from: Department of Health (2008) Health Weight, Healthy Lives; a Cross- a Cross-Government strategy, Department of Health: 29.
[12] See Curry, A. and Ballantyne, J. (2009) ‘Department of Health Obesity Horizon Scanning Workshop’, The Futures Company. Available electronically at: http://www.dh.gov.uk/en/Publichealth/Healthimprovement/Obesity/HealthyWeight/DH_097478?IdcService=GET_FILE&dID=190140&Rendition=Web
[13] Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 11.
[14] Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 11-12.
[15] P. Musingarimi (2008) Obesity in the UK: A Review and Comparative Analysis of Policies within the Devolved Regions, International Longevity Centre: 8.
[16] Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 12.
[17] For more information on the various ‘case studies’ associated with the nine Healthy Town see Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 32-34.
[18] Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 37.
[19]Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 45.
[20] Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 46.
[21] Department of Health (2009) Health Weight, Healthy Lives; One Year On, Department of Health: 49.
Response from Fire Service
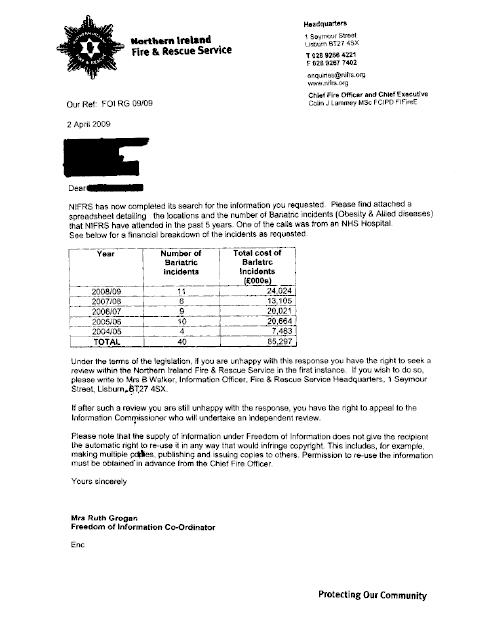
Appendix 5
Minutes of Research
Event held on 19th May 2009
Research event to inform the
Committee for Health, Social Services
and Public Safety’s Inquiry into Obesity
19 May 2009
Parliament Buildings
Although the event was attended by the Office of the Official Report (HANSARD), the transcript is verbatim and has NOT been subjected to the standard official-reporting process. Gaps in the transcript are due to that section of the meeting’s not being electronically recorded.
Members in attendance:
Dr Kieran Deeny
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Participants:
Dr Jane Wilde |
Institute of Public Health in Ireland (Chairperson) |
|
Professor Iain Broom |
Robert Gordon University, Aberdeen |
|
Professor Paul Gately |
Leeds Metropolitan University |
|
Professor Bernie Hannigan |
Department of Health, Social Services and Public Safety |
|
Dr Carolyn Harper |
Public Health Agency |
|
Dr Patricia Heavey |
University College Dublin |
|
Professor Frank Kee |
Queen’s University Belfast |
|
Professor Barbara Livingstone |
University of Ulster |
|
Mr Gary McFarlane |
Chartered Institute of Environmental Health Northern Ireland |
|
Professor Ivan Perry |
University College Cork |
|
Mr Mark Rollins |
Causeway Hospital |
|
Ms Hazel Ross |
Robert Gordon University, Aberdeen |
|
Dr Michael Ryan |
Northern Health and Social Care Trust |
Additional attendees:
Mr Hugh Farren |
Committee Clerk, Committee for Health, Social Services and Public Safety |
|
Mr Neil Foster |
Northern Ireland Assembly Research |
Electronic recording commences here.
1. Dr Patricia Heavey (University College Dublin): My name is Patricia Heavey. I am from the National Nutrition Surveillance Centre in University College Dublin, and I have recently taken up post as manager.
2. Professor Paul Gately (Leeds Metropolitan University): My name is Paul Gately, and I am Professor of Exercise and Obesity at Leeds Metropolitan University. I head up an academic unit called Carnegie weight management.
3. Ms Hazel Ross (Robert Gordon University): My name is Hazel Ross. I am a reader in nutrition at the Robert Gordon University in Aberdeen. I co-ordinate the Counterweight programme and manage a team of 14 dieticians who work across Scotland and England implementing the programme.
4. Professor Iain Broom (Robert Gordon University): I am Iain Broom, director of the Centre for Obesity Research and Epidemiology in Aberdeen. I am also the chairman of the Counterweight programme, and professor of metabolic medicine at Aberdeen.
5. Professor Bernie Hannigan (Department of Health, Social Services and Public Safety): My name is Bernie Hannigan. I am the director of R&D for health and social care in Northern Ireland, and chief scientific adviser to the Department.
6. Mr Gary McFarlane (Chartered Institute of Environmental Health Northern Ireland): I am Gary McFarlane; I should say that I have two hats. I am director of the Chartered Institute of Environmental Health in Northern Ireland, and I am also the co-chair of the Public Health Alliance for the island of Ireland. In the latter role, I was previously involved in research into poverty in Northern Ireland, the link between that and obesity.
7. With my former hat on, we are currently involved and working with colleagues Martin Carragher and Tim Lyon at City University London looking at some of the built environment issues around obesity.
8. Dr Carolyn Harper (Public Health Agency): I am Dr Carolyn Harper, director of public health at the Public Health Agency.
9. Mr Mark Rollins (Causeway Hospital): I am Mark Rollins, consultant paediatrician. I represent paediatricians’ views in Northern Ireland on childhood obesity, and I have undertaken some interventional projects in childhood obesity. On behalf of my paediatric colleagues, we need help.
10. Dr Michael Ryan (Northern Health and Social Care Trust): I am Michael Ryan; I am a consultant in the Northern Trust, lead in diabetes in Causeway Hospital, and we need help as well.
11. Dr Wilde: Thank you very much. We also have a number of people including researchers; would you like to introduce yourselves so that people know who you are and the important role that you have had in setting this up?
12. Dr Janice Thompson (Northern Ireland Assembly): I am Janice Thompson, researcher for the Health and Social Services Committee.
13. Mr Neil Foster (Northern Ireland Assembly): I am Neil Foster; I have worked with Janice in support of the Health Committee.
14. Dr Wilde: Thank you very much indeed. Turning to the programme, if you take a look at the programme and see how we set it out. This morning, we will have the presentations from each of the researchers, and we have broken up the sessions so that there will be two presentations and then some discussion, then two presentations and some discussion. I am very much looking forward to questions and answers.
15. Although the presentations have been prepared, we have asked the researchers to stick to 10 minutes each with the idea that it will really be about the debate, the dialogue that we have after that. That is what, hopefully, will take us into the discussion after lunch, where we will try to respond to some of the key questions that the Health Committee has already identified as important in relation to obesity. We will very much be focusing on the learning bit of the terms of reference of the Committee. Is everyone clear enough about the programme? Just ask away if you are not clear.
16. Welcome Dr Deeny. We have just gone around and introduced ourselves. Some of the biographies are in the pack. Dr Deeny is a member of the Health Committee. MLAs will come in and out depending on the day that they are having. Beside you are some of the key stakeholders.
17. In terms, then, of the discussion, we will take some discussion after the pair of talks, and then we will have more discussion after lunch. There is tea and coffee available. If you want a cup, just get up and help yourselves. In terms of the actual presentations, we do want to sort of keep to the outcomes rather than the methodology of the research. That is really, I think, what most people around the room are really interested in. As I said, proceedings will be recorded, and the transcript will be available for inclusion in the Committee’s inquiry report. Could I also ask you if you could turn your mobiles off? The problem is they interfere with the transcribing, if that is OK.
18. Our aim, as a group, is to come up with some practical recommendations to put to the Committee. When it has had a look at those, it will decide whether they will go into the report. The Committee report itself will be debated in the Northern Ireland Assembly and will go to the Health Minister to consider. So, we have a very big opportunity, I think, to actually influence what is put into the report and, hopefully, influence what happens in policy and in research in Northern Ireland.
19. Our aim is to be finished completely at 3.00 pm. There is also going to be a tour of the Assembly available for anybody who would like to. That is really the end of the information bit, except to say thanks again. I am really delighted that you have been able to come.
20. Now we will turn to the presentations. I am going to ask Frank to start us off. I am keeping to the time of 10 minutes for each presentation, as I said. Otherwise, we are going to get a little behind, so I will tell the presenters when it is about nine minutes, and I expect you to try and get to the end. Thanks.
21. Professor Kee: Thank you very much, Jane. I did not realise my first slide was up there. I was not being cheeky by putting up something that came from OFMDFM here. Since our centre got under way, some of the most heartening conversations that I have had have been with the policy innovation unit in OFMDFM.
22. Dr Wilde: I just meant to say earlier that some of the acronyms may not be well understood by everyone, so maybe just —
23. Professor Kee: The Office of the First Minister and deputy First Minister has a policy innovation unit. James McEldowney, who heads up that unit, gave me this slide. The key point that I wanted to emphasise was that, in managing this epidemic of obesity, we are going to need increasingly joined-up policies that are evidence-based. These policies have to be subject to review and evaluation. Again, perhaps I was being a little bit cheeky by maybe verging slightly off the brief because, maybe, you wanted hard and fast results from past studies, but I actually wanted to give some learnings about a current project proposal — lessons that I have learned and that the partners have learned in coming together about partnership working and getting everybody on the same page.
24. We responded to a National Prevention Research Initiative (NPRI) research call last summer. The National Prevention Research Initiative issued a call for research on primary prevention around behaviours. We wanted to put something in to respond to that call. Coincidentally, simultaneous to that call being issued, the Connswater Community Greenway won its £25 million Big Lottery Fund award to create green space in east Belfast. Among the key objectives of that Big Lottery Fund award was to improve physical-activity behaviours in the resident population.
25. Given the remit of our centre of excellence, which is not only to produce good research but also knowledge mobilisation and knowledge brokerage to work with a wide range of stakeholders, we immediately got in touch with the East Belfast Partnership and then tried to identify all the relevant stakeholders who should be involved in a project like this. Too often, perhaps, in the past, my experience has been, in working with different Government Departments and different agencies, this rather depressing experience here.
26. One model of us working with our partners is having the embedded researcher either in the policy setting or the policymaker embedded in the research setting. That does not go far enough for these new centres of excellence that the research councils have funded. Really, the model that we want to work to is knowledge co-production and knowledge generation together. And so when I was trying to pull the right team together to submit a bid to the NPRI, it was finding out who was doing what in this area across the statutory and non-statutory sector.
27. I want to first of all start with what a consensus panel in the US have said are the top priorities for obesity research. I knew that I was going to have to refer to something like this when we were putting the NPRI proposal together. The top priority there was the better evaluation of natural experiments. It does not only appear in consensus panels in the US, but from the National Institute for Clinical Excellence (NICE) in their recent guidance and recommendations for future research. Smarter, better use of natural experiments, and if there is not a bigger natural experiment about to happen in east Belfast that might affect physical activity and obesity, we do not have to look much further than the Connswater Community Greenway. I thought that was a really good hook to hang this proposal on.
28. They won their award in February 2008, and we had to submit a proposal last September, but I had to find all the right people to get together to prepare this proposal. We were interested in finding out whether the creation of the green space and the new amenities would increase the proportion of the target population achieving physical activity targets, whether it would reduce inequalities in achieving those targets and whether the actual initiative — because they were very community-minded when they put the proposal to the Big Lottery Fund award together — working together in a partnership, would enhance the social capital, but also whether the entire project, in terms of health, would be cost-effective.
29. Broadly speaking, if you look at the literature on the evaluation of natural experiments, you will get many, many different answers, different slants; but we wanted both a quantitative and qualitative evaluation of what was going to happen. Before-and-after survey; I said partnership. Well, you cannot just study that one area. It was again very fortuitous that DCAL were sponsoring Sport NI to do a Province-wide survey of physical activity in 2009 and again planned for 2013, roughly sandwiching the construction of the Greenway in east Belfast. So, readily available control population right across the Province. That was very, very fortuitous. So we have a regional comparison. We are going to be working, because we had meetings with them and they were on the project team, with the East Belfast Community Development Agency, which is embedded within the East Belfast Partnership. Various process evaluation measures will be undertaken, on which I will elaborate in a moment, and the economic evaluation is a key part.
30. This document came out in February, in the Department of Health in England, and they were referring to the necessity for partnerships, not only between the statutory and non-statutory sectors but with the business community as well. In Manchester, they are rolling out a very innovative programme of loyalty card schemes to support, for example, more purchases of fruit and vegetables, like you get extra loyalty card points if it is a Tesco card or a Sainsbury’s card.
31. Around about the time we were putting the bid together, we came in touch with the medical adviser of Natural England. He introduced me to the concept of a physical activity loyalty scheme whereby residents in east Belfast could have a swipe card, and if we planned to put sensors round the new amenities, if you swiped your card around the sensors it records how far you have walked using the green amenity. How many loyalty card points you will get depends on how far you walked. This was the subject of NICE consumer research with residents from deprived housing estates in Manchester. In terms of what they wanted to see loyalty card points attracting or being earned from, the use of green spaces was very high up in the priority.
32. That is what we are doing. We are planning to put these sensors around the Greenway, and people will swipe their card as they use the Greenway. What is clever, though, is that it will record how much you have earned in terms of your physical activity points and record it on your own personal web page. It will say how far you have walked, but we want to go beyond that and link that web page to a raft of motivational websites that we know are out there and on which some of our researchers are working. We know about the power of social networking, and there was a NICE paper in the ‘New England Journal of Medicine’ a couple of years ago about the social network effects on obesity.
33. We want to harness that power in linking it to our physical activity loyalty scheme. We will advertise events on the Greenway, we will put them in touch with motivational sites to help them plan their own physical activity. We are not really forging new ground in that respect, but the idea of the loyalty card scheme will be novel. We also want to capture the residents’ views of their physical environment.
34. When I got the project team together, I knew that the physical environment crossed many different Government Departments and agencies. I had to get Belfast City Council interested, I had to get DSD, who are interested in urban regeneration, DRD, who are interested in transport, DOE, who are interested in planning, and, happily for me, they all sent representatives to the research group. It was very, very important to have the contributions of all those people, but if I have a message there, I mean, of course, we have academic partners from a range of disciplines — nutrition, public health, economics, the built environment and architecture — but this would not, and I suppose you are looking for a punch line here, it has been shortlisted to the final stage at the MRC, but it would not have got to that stage were it not for all of these statutory and non-statutory partners getting on the same page. Really, that is what I have learned. I think that we have harnessed a lot of good will and genuine expertise that could come from those various bodies. The message that I wanted to leave was that we need information; we need information at a community level.
35. Of course, we are doing our own surveys as part of this focused research. One of the major sources of information in the future, looking forward beyond the lifetime of the Greenway project, will be the health and well-being survey. We are going to need good BMI and obesity data from that. However, we need to integrate the expertise that all those other Government Departments have, particularly in regard to geographic information systems (GIS) because I understand now that there is a GIS expertise consortium that operates across Government Departments. I have not yet managed to find out who is in charge of that — but I would like to harness those GIS skills. I will leave it at that.
36. The learning for me in preparing this bid has been in getting a shared commitment to a research agenda in the public sector that embraces the non-statutory sector as well.
37. Dr Wilde: Thanks very much indeed, Frank. We will come back, I think, to several of those points.
38. I am going to keep going with Paul Gately’s presentation now, but mark down questions that you specifically want to ask of Frank, or points that you want to make. Thanks very much for keeping to the time, Frank.
39. Professor Gately: Thank you very much. Good morning, everyone.
40. I am very grateful for the opportunity to share some of the work that I have been conducting in Leeds for 10 years at the university, and which I conducted for a further 10 years during my PhD and early academic career.
41. One of the things that I wanted to talk about is the strong relationship that we have at a regional level with the Yorkshire and the Humber Strategic Health Authority. We have done a lot of work with them around their Healthy Ambitions strategy, which is a regional approach to tackling obesity.
42. Through working in, and delivering, a large number of interventions over the last 20 years, dealing with 4,500 children, we have learned an awful lot. Some of the key things that we have learned are really around the implementation, not necessarily the key tactics — that is, the nutritional information that is necessary or the physical activity — but it is about how you put those things into practice. Those are some of the key challenges that we have found in our implementation, particularly around looking at prevention, treatment or a combination of the two, and is there a joined-up and live strategy? Some of the primary care trusts that we are talking to in England are very happy about the fact that they have an obesity strategy, but they are not very happy about the fact that it is just gathering dust on a shelf. It is not a live document that is driving their activities.
43. Some of the questions that we ask are about the knowledge to deliver locally owned and sustainable models, so while we have a number of primary care providers in the context of dietetics, physical activity, and so on and so forth, actually how joined up are they? You may have a multi-disciplinary team, but the key question is: are they actually delivering a multi-disciplinary intervention?
44. The next level is how we start to utilise the capacity of those key people that are there. NICE outlines two levels of training; generic and specific. We have designed two types of training programmes for that and we are trying to address some key factors. The first is that we know that there are 4·5 million children in the UK that are overweight or obese. We also know that 70% of parents identify their overweight child as having normal weight and 30% of parents with obese children define their child as just right. We published a study last year showing that a 74% of healthcare professionals underestimate an overweight child and 50% underestimate an obese child. There is a major issue about identification.
45. One of the questions that I often get asked by the media is how someone can let their child get to such a weight. My answer is a question: where is the stop in the system? There is clearly a need for such recognition. There is also a lot of work necessary: academics often make the research, design and develop of interventions sound very complicated, and often they are difficult, but with the right partnerships they can be done very well. That is why our academic role is critical within the university.
46. Finally, we have taken some positive steps in a critical area, albeit, it is very challenging to work in marketing and communication on these issues. If, for example, 70% of parents do not know that their children are overweight, we need to send them clear messages; and we need those messages to be sensitive and appropriate so that we engage people rather than turn them off.
47. There is no single solution with respect to delivery: Lots of different solutions need to be used, and obesity is such a serious issue that we need to use them. They need to be locally relevant and flexible to the range and needs that there are in the different communities we are providing for, and I question some of the interventions that just out of a box. How locally relevant are they and, therefore, how well can they be delivered?
48. I will give you a bit of history about our work. We started off with delivering intervention programmes but then really started to realise there were major gaps in the ability and capacity of the local providers — local authorities — to deliver effective interventions. Many people question the impact of behavioural interventions. Primarily, that is due to poor-quality interventions being delivered rather than behavioural interventions not working.
49. Finally, one of the biggest challenges we think exists stems from the fact that the media want to engage in the debate about overweight and obesity, but not necessarily in a way that is helpful. What programmes such as Gillian McKeith’s ‘You Are What You Eat’, and ‘Supersize Superskinny’, tend to do is switch off 90% of the population. Because people feel that they are not as extreme as the cases in the programmes, they do not think that they have a problem.
50. Many of my academic colleagues will run a mile when they are asked by the media to talk; some do not, but many do. They are nervous about being misrepresented. Part of the role that we have taken is to link that in with our wider communications strategy and interventions.
51. Another key feature of what we have done is to say that not every overweight or obese child is the same. There are lots of different ways of classifying overweight and obese children, and that is not the point I am trying to make. I am saying that needs are different. We have designed a number of different types of intervention, up to our more intensive intervention, which is a residential-type intervention for the more extreme cases. When there are children who are severely obese, 5% weight loss is just not enough.
52. In the UK, there are 140,000 children who are three standard deviations from the norm. Some people define them as statistical anomalies, but 140,000 is quite a big set of anomalies. That is why we are designing a more intensive model for that group.
53. Then, there are two kinds of community-type interventions. We are saying that we know that the school day is very busy and that we cannot continue to implement new strategies in schools. So, when are children free? They are free after school, at weekends and during holidays, and we have tried to fill those gaps. Many children are engaged in sport, have opportunities during holidays and after school: overweight and obese children do not have those same opportunities.
54. Finally, we have a website that provides a whole range of social-networking functionality to support the children and families. We have a parent site and child site that are security-protected members’ sites and are supported on a regular basis.
55. What this pathway does for obese children is to provide residential intervention followed by some form of local community intervention. For overweight children one can access the moderate intensity programme. It is trying to provide a whole range of solutions.
56. I am not going to spend too much time on this, but we have a strong evidence base — 25 peer-reviewed published articles on our work — that when we look at some of the key variables and outcomes that we are trying to achieve, we address all of them with published evidence and research. There are issues around some of the wider preventative and whole-school approaches, because the evidence base is just so poor, and I think that that is one of the key things that we need to move forward and appreciate. We have a lot of that evidence.
57. Most of our work started at the delivery level, but then we started to realise that we need to help PCTs and local authorities in the implementation using things such as surveys and helping them as regards partnerships. One of the things that we have done with a lot of the PCTs that we have worked with is they seem to be so stretched in terms of their communications. We were talking earlier about one of the current challenges regarding flu and swine flu, and one of the issues is about communication. How do we communicate appropriate messages? PCTs are often swamped with these sorts of challenges, so we have worked with them, utilising our PR and marketing skills, to help them do that, and then we offer a whole range of training options for PCTs. Further along, we have worked with some PCTs that have said to us:
“Actually, after a conversation with you, we have got none of this in place, and our strategy just looks like nice guidance, but it is not relevant to our local community. Can you help us to ask some of the really challenging questions to make sure that we design an appropriate strategy?"
58. I do not want to spend too much time on the outcomes, because I have brought a whole range of sample papers for people to read. I just want to go through a couple of case studies. We have got a couple of large-scale projects that I want to outline. There is a £3·5 million project with Rotherham PCT, which has really taken the initiative forward. We are working with them to deliver support for 2,000 children’s families. That will involve the residential programme and the community-orientated programme. We are also training their local providers and local generic health and children’s services community. That will allow us to ensure throughput.
59. I keep getting asked by the Department of Heath about the capacity to deal with all cases of obesity: I think that capacity is a red herring. The real issue is how to get the children to be aware that they need to access services. It is not about the fact that we need to be able to deliver services. Of course, we need to deliver services, but we can deliver lots of them without the children, and we need the children to deliver the effective services. So the health promotion component is critical with capability and capacity building.
60. The first cohort of 40 children who went through the residential camp was followed up by a community programme delivered locally by the PCT. There was quite a significant reduction over that period of time. We were fortunate to have Lord Darzi and David Nicholson visit the programme, and David Nicholson identified it as the best investment in public health that he had seen.
61. We were also approached by NHS Blackpool, which gave us a very challenging scenario of working with six families. They were saying that it was all well and good working with middle-class families, but what about those who are hard to reach. They gave us six families with a whole range of problems: drug and alcohol abuse; child-protection issues; prostitution; poverty, and mental health. They also sent two police officers with us just to look after us. So, you can imagine that my team were quite nervous.
62. The outcome was extremely positive, because we did a residential programme with the families that moved into a community intervention. What was critical was that the partner organisation that we worked with; the family intervention unit, which is located in the local police department, said to us that what was fascinating about it was that health for them is at the bottom of the agenda, because when one is dealing with drug and alcohol abuse, child protection and prostitution, health is not a big agenda item. What they found was that these families, through the intervention, moved health to the top of their agenda, because of the fact that it allowed them to put in place a whole range of issues, such as routine, positive behaviours and so on and so forth. That had a very positive outcome on those families.
63. The final point is about a regional roll-out. We have started to look at that. Again, the Department of Health asked us about a capacity issue. I think that there is an opportunity here, knowing that colleagues from Northern Ireland, and Ireland in general, have some great expertise in the universities and provider services with which I have had dialogue.
64. One thing that we are doing to deliver across the UK is selecting partner academic institutions in each of the regional health authorities. We already have two partnership agreements with the north-east and London. They will do a lot of the research, training and delivery. That allows us to gain greater reach very quickly, yet deliver a whole range of effective services with them.
65. If one takes quality-care-for-all as a vision, much of the work that we are doing is delivering on each of the core pillars of that strategy.
66. Dr Wilde: Thank you, Paul. We will come back to those points, and we can look again at some of the slides. There are copies of most of the presentations in the information packs. Thank you, Frank and Paul, for keeping to time. We now have 10 minutes in which to pick up some specific points relating to the presentations. The discussion will be totally open, so fire away.
67. Dr Harper: Frank mentioned that the loyalty card idea was based on research that was carried out with disadvantaged communities. What was the strength of that evidence and some of the messages coming out? I am asking this just to be sure that that approach has, in itself, an evidence base behind it.
68. Professor Kee: Dr William Bird, medical director of Natural England, had been very influential in giving the slant to the Department of Health. Research on healthy towns was commissioned, and towns across England and Wales could submit proposals for an injection of, I believe, £4 million to £6 million in each town.
69. Manchester formed a partnership between NHS Manchester and Manchester City Council, and they responded to the healthy towns’ initiative. I was fortunate in being sent a copy of their bid. I could not quote chapter and verse of the economic literature that they cited on the use of loyalty cards, but it was cited thoroughly. There is a body of literature on the use of financial incentives for behavioural change. The best way to put it is that it is mixed: it shows some effects in some areas, but not across the board by any means. However, they quoted from marketing and economic research on how people use loyalty cards.
70. There was a series of focus groups of 300 to 400 people from sink housing estates in Manchester and it was explored with them what they thought the use of a loyalty card such as that to support physical activity. In the Manchester scheme, which is called ‘Points for Life’, people could also use their loyalty cards to get extra points when they bought fresh fruit and vegetables. They are, I believe, also contemplating putting sensors across the environment so that one can swipe a card and get credited with extra loyalty points.
71. One of the slides showed the results of that market research. They were asking how people would like to earn and spend the points. Using natural green spaces came above using gymnasiums, which was interesting. Those were people in sink estates, so they would like to use natural green spaces to get out in the open and fresh air. As regards what they would like the points redeemed for, a range of options was included. As it was Manchester, options included discounts on Manchester United football team products.
72. They are thinking creatively and imaginatively about how they will reward people who earn the points for physical activity. I was quite convinced by the efforts that they had taken to find out the views of the people of Manchester and how the scheme might work. I can share with you that market research that they sent me. I do not think that it is confidential.
73. Dr Wilde: We will hold that point on incentives. I think that several other people might want to say something about different incentives.
74. Professor Hannigan: I have a couple of things to say. First, I commend Frank Kee on the community involvement in the research because it is something that Northern Ireland has been very slow in taking up. Nowadays, it is not appropriate just to involve communities as subjects of research. Communities need to be involved as active participants in the research at all stages of its development.
75. Paul Gately talked about getting to the hard-to-reach families, and Frank Kee talked about a number of things being delivered through the web. Hard-to-reach folk do not have access to broadband and the Internet and I wondered how you would deal with them so that they felt equally included.
76. In Northern Ireland, access to broadband is the responsibility of DETI. Professor Kee is talking about finding out the right contacts in the various Departments. When England came up with its obesity strategy, representatives of every relevant Department were brought together with the chief scientist and the director general for research and development in one room. Why can that not happen here? The Department of the Environment, Department of Agriculture and Rural Development, Department for Regional Development, Department of Enterprise, Trade and Investment, Department for Employment and Learning — almost every Department — need to participate in the obesity agenda.
77. Professor Kee: If you recall, Dr Wilde, we outlined this study to the cross-departmental ministerial group on public health. It is such a huge agenda that you sometimes struggle to find the right person to talk to, and usually it is about talking to someone, and then someone else, or a friend of a friend, and finding out who has it in their job description and who could make a contribution. I got there eventually, but Professor Hannigan is suggesting that having some sort of joint commitment to this joined-up working might make it easier.
78. We are not going to rely solely on the Internet for giving feedback. I do not know what the ownership of mobile phones is in schools, but it is extremely high, and one can send the feedback by an SMS to a mobile phone, and that is what we are intending to do.
79. Professor Gately: In the context of that issue, for us it is one of many communication activities that we have. We use SMS messaging to our wider audience as well. Because children can access the Internet through school, we take them through the process of logging on to our site and using it as part of their training. One programme involves using the web a lot more. We have a lot of activities involving children accessing information about local services, as regards the physical activity and guidance on healthy eating that is available in their local community. Interestingly, out of the six families that we had, five of them had and used the net at home. The numbers are obviously increasing. We found that children are much more comfortable using the net and that parents are much more comfortable speaking on the phone. There are different levels of communication in the different groups.
80. Can I tell you, chapter and verse, about what different types of demographics need in terms of communication now? One of the interesting elements about this is that there is a lot of natural learning to have with the implementation of intervention, and that is partly what we are trying to do with our work as well. We also take very much an action-research approach.
81. Dr Deeny: This meeting is very welcome today, and it will be very important for the Committee’s inquiry into obesity. But, wearing my GP hat, I have a question for Professor Kee. GPs have the opportunity of being in the front line and seeing obesity quite often. Where is the GPs role in prevention? I have mentioned quite often at Committee that GPs should have access to prescribing activity, for example, to the appropriate patients.
82. I also have a question for Professor Gately. Another major problem in general practice is that we have people who are hard to reach. You talked about the Internet. Could you link those two? For example, that young people could get a series of exercises that could be prescribed by their GPs and that GPs could prescribe them. At the end of the day, a major part of our report will involve prevention and exercise, which is a major part of the whole thing.
83. Professor Kee: You will be pleased to know that I went to see the lead GP for East Belfast, Dr Samuel John Kyle in the Holywood Arches Health Centre, when we were putting this together. When we were thinking about how to dispense the cards, we wanted the involvement of the GPs and practice nurses. They will see the hard-to-reach, the people who are overweight, the diabetics and whatnot. They will be consulting with their problems. We want to use that as an outlet for the cards and also as an opportunity to promote the use of the outside.
84. GPs have been involved in exercise-prescription in Belfast. I have not worked in Belfast: I have worked in the Northern Board in the past, but I know that those exercise-prescription schemes have been evaluated in partnership with the city council. I think there has been variable success.
85. Professor Gately: It is a really important point. That is what I was trying to say. What is the journey for children through the process? I am particularly interested in children: it is my area of work.
86. The first problem, from a GPs perspective, is that very few of these children present for health issues to GPs. That is a major problem. That, as a journey, is limited at that initial point. The second thing is that much of our wider communications strategy is trying to capture children from within the community to then access or be made aware of the services. Then we go through a process of helping them through, and the health authority through, a referral by their GP. It streamlines the process and makes it simpler. Many families see it as a health issue, with health outcomes, but the people who are going to solve it are not GPs. A whole range of other service providers are going to do that. That is why communication is absolutely critical.
87. The final piece of the jigsaw, as regards GPs, is what incentive there is for them to make the throughput of children coming into interventions work effectively. Many PCTs that we talk to say that they are not going to deliver it through GPs, because GPs do not have the time and are not incentivised to do it. It is not relevant to what they are doing and we need other, wider, strategies. We are always trying to engage with GP colleagues to refer children to our programmes.
88. Professor Livingstone: I will make a brief observation, and it more or less supports what Paul is saying as regards primary care. Obviously, that is pivotal in the whole area of obesity. Generally, GPs do not see their work as being in the area of prevention: so, there are a few barriers to break down.
89. Mr Rollins: As a paediatrician, my view is that GPs are seeing children with obesity and are referring them to paediatricians in the hope that we are going to say that the child is not obese and has some sort of other problem. Unfortunately, they are all obese. To be fair to the GPs and ourselves, what are we going to do? We do not have the programmes. Kieran needs different programmes to be available and to be able to engage with the families and say: what would you like to do, and are you prepared to do it. Many children come to us at age 16 saying that their parents told them that they had puppy fat. They say: look at me now — some puppy fat.
90. Getting back to basics, there are 400,000 children in Northern Ireland, 100,000 of whom are currently overweigh and obese. Some 60% to 70% of children are going to be obese as adults. That is a fact. With adolescents, we are up to 70% or 80%. In Northern Ireland, we have no intervention programmes at all. We are starting from a complete base. My worry is that we may decide we need more evidence such as: what is best for the locality? It is too late. I have had you over here a couple of times. What do you think we should do if we are going to tackle this problem now, or do you think we need more evidence from the locality? Of course, we need evidence all the time, but where do we start? Who should we be engaging with?
91. Professor Gately: That is the sum-up of the day. You are not starting from a baseline position. There are lots of people who are knowledgeable about this. Lots of practitioners could be drawn in. As I have outlined, one thing that we have found in the PCTs that we have worked with is that strategic positioning at the start of identifying the pathway is important. Where do GPs fit in? Where do paediatricians fit in? Where do dieticians fit in? Open up the landscape and start to state each person’s role, responsibility, and what you are trying to achieve?
92. How do we then define a whole range of services that are relevant for these children from both a health perspective and the children’s services perspective, and children’s services more broadly in terms of education? I think that once you have the strategy, it is then a matter of some simple training for some key professionals who already know a large majority. They just need to be given two things: first, some more technical knowledge and; secondly, some broader confidence.
93. One of the big issues that we face in engaging with our colleagues in education and children’s services is that they have a couple of issues. First, if they tell a child that he or she is overweight and obese, they are going to get lamped by the parents. Secondly, if they are going to turn the kids the other way, they may suddenly have a population of anorexic children. The evidence base does not support those things. It is a matter of confidence. It is about raising awareness, giving people the competencies, and then having a suite of different services being offered that children, families and indeed the associated GP who is going to direct those children to those appropriate services.
94. The pieces are already there: what you have is the opportunity to take on board the lessons learned by many others. Some of the work that we have done allows you to do that. There is a whole range of other people along this side of the room who are effectively doing this at different levels who would be well-engaged.
95. We are working with Roehampton University, which has very strong skills in education and is leading in new research in that area through our partnership. That is great for us, it is great for them, and it ticks all the necessary boxes so that everyone wins and everyone feels as though they are contributing to something much bigger. At the same time, we are all gaining capacity and reach very quickly.
96. Dr Ryan: I support Mark from the coal face, if you will forgive the phrase. Ninety per cent of my patients are overweight or obese. Eighty per cent of our cardiac patients, 70% of our respiratory and gastro patients are overweight or obese. We need something now: we cannot wait. When children reach 16 or 17 are they going to fall off the edge?
97. We need a programme that reaches every case. We do not just want to prevent obesity; we want to prevent the diabetes and premature deaths, for example, that accompany it. There is very good evidence that, for example, that the DPP programme can prevent about 60% of people from developing diabetes. Those are interventions that are available, in theory, if we had the resources: waiting for another five years for more research is just too late.
98. Dr Wilde: I do not want to underplay the frustration that people feel. I want make sure that we come back to that and discuss how research can help.
99. Dr Ryan: I have a patient that I use as an illustration to the Health Committee. She pushes her abdomen in a wheelchair in front of her. There is nowhere for this patient to go. She is 42 years old and her life is ruined. This is not an acceptable system. We are failing these patients.
100. Professor Perry: I have a brief comment. Obviously, we are talking about a very challenging and complex problem, and we need interventions at all levels. Part of the response has to be about going back to the point about the determinants of health and well-being and trying to tackle some of those; not that that, of itself, will solve the problem.
101. I will tell you briefly about a small piece of research that we did. We looked at the promotion of physical activity in two relatively deprived inner-city communities, one in Cork and one in Dublin.
102. Electronic recording paused
103. Professor Livingstone: Electronic recording recommenced.
104. The study period started at 9.00 am on day one and ended at 9.00 am on day five. In between days one to four, the subjects were fully residential, ate all their meals in the metabolic suite. They were not aware we were surreptitiously measuring everything they ate. These visual analogue scales (VAS) are simply appetite scales. I will come to these in a minute, because they are very important, and they offer a number of salutary lessons.
105. Basically, the subjects alternated between standard portion sizes and large portion sizes, and I will not go into the exact background to the study. They had a very attractive menu of foods. Right then, we are talking about limited by choice, a range of breakfast foods, sandwiches, soups for lunch, four dinner choices, four dessert choices and a range of snacks. Each subject had their own dedicated lockable fridge and dry cupboard for storing dry snacks. The thing to note is when the volunteers made their selection of foods in the first study period, they got exactly the same foods in the second study period. The only thing is that we altered the portion size.
106. Just in case you think we are talking here about large portion sizes, in-your-face large portion sizes. Folks, each and every one of us are facing these scenarios every day. We are not appreciative how just subtly our portion sizes are increasing, and we are going with it. This is the orange juice portion, Cornflakes. The subjects were not actually aware — none of them — of the purpose of the study, and they did not realise that we were altering the portion sizes. These are scenarios each and every one of us is facing, and that is a chicken curry.
107. Very quickly, the results. There were 43 subjects who took part in the study. I want to draw your attention to the fact that over half of the males were overweight, and about one third of the females were overweight. Nobody was obese; the rest were of normal weight. I have a whole host of results here to show you, but this is one summary bar graph slide. It shows the overall calorie intake over the four-day period on the standard portion-size condition and the large portion-size condition for males and females. Over the four days, the males increased their food intake on the large portion size by 17%. They managed to consume 2,500 calories more over those four days.
108. As regards the females, they in fact increased their energy intake by 10,000 calories; a 10% increase in energy intake. The next slide shows overweight changes. On the standard portion size, we saw no change in body weight. Would you believe that, on the large portion-size condition, the men gained on average 0·9 kg and the women gained 0·6 kg?
109. This is probably one of the most interesting slides of the whole lot, because we asked the subjects to assess their own appetite sensations during the study. Before eating, on the large portion-size conditions, subjects reported feeling less hungry, more full, having less desire to eat, and they said they could eat a smaller amount. That is before eating. However, nevertheless, they consume more food when it is presented to them, and they did not report feeling any fuller afterwards. That is a huge issue in obesity work. I think that most people, virtually all of us, have lost touch with our appetites and hunger signals, and, basically, if food is there, we will eat it.
110. In the study, which has limitations — it is a residential study, but, nevertheless, it would be very difficult to do it in free-living conditions — increased food portion sizes did result in significant and sustained increase in food intake. Sustained is important, because over the four days, on the large portion-size condition, you might think that, after a couple of days, people get fed up eating large portions. They did not; they just carried on eating them. They were not aware that they were actually eating larger portions. There is no doubt that the portion-size issue is one very important factor in our food environment in relation to the obesity epidemic that we will have to tackle.
111. The kind of work that we do serves to remind us that, although, obviously, I totally agree with everything that we have been doing so far on the need to have all the joined-up thinking and all the rest about obesity, how the hell do we persuade people to get their head out of the trough and get their butt off a seat, because that is the bottom line. Thank you very much.
112. Dr Wilde: Thank you. We have a bit of discussion time now; we will keep it fairly short. Thank you, Iain, Hazel and Barbara.
113. Mr Rollins: Iain and Hazel, the great selling value of your programme is not only the quality and the cost of it, but sustainability. That has been the key, because a lot of us do these pilot programmes, and, when they get to a year, people say that a year is the key, but it is not. All of our projects tail off, but you have been able to do it. You would be topping and tailing this. What are you going to try to do between the second, third and fourth year onwards? Is it giving more time to individuals for discussion, or is it to bring in the motivational experts, which is a buzzword now? How do you foresee trying to improve that sustainability, other than leaving it up to the individuals?
114. Ms H Ross: One of the learnings in terms of the application that Paul mentioned both in the PCTs in England and in the health boards in Scotland, once we have been commissioned to work, there is quite a lot of joined-up working in terms of where are things at anyway, and planning, how Counterweight is going to be fitted into the obesity framework pathway, or healthy living pathway. In Scotland, we have been commissioned in chunks of funding for two years, and, in England, it is one year. It takes about eight months talking to actually get geared up. That is not at our end, but, if you push too fast, you have not got the buy-in from all different Departments, from dieticians and the various Departments, and it takes longer to do the start-up.
115. There are some learnings in terms of Government liaison with the health boards in Scotland. The health boards have said that they would have liked more direction from Government about how they saw those slotting together, so that there are things that we could, maybe, go back to explore later.
116. Relating to sustainability as well, apart from a delayed start in every area, it appears Counterweight works really well once we get in, but it takes longer to get started. The funding of the buddy dieticians has been a temporary thing in Scotland, and it has caused issues where it relates this programme being a pilot for so long. Some health boards who, in our eyes, are very forward thinking are saying this is our huge opportunity during the two or three years we have got Counterweight. In some of our health boards, they are saying that all of our community-based dieticians can do a little bit of Counterweight as part of their job. They will do the mop up and ongoing support after we do all of the intensive training.
117. In areas where they are feeling like the Government has dumped the programme on them, they are saying, “Well, after these two years, if we are not going to get any more funding for buddy dieticians, we will just stop doing Counterweight." I think it just opened discussion about the different pros and cons of how programmes can be brought into different areas. We have got a model that we have found to be very sustainable in a lot of areas, but it needs to be so carefully handled to work well, and I think there is quite a lot about the longer-term vision of pathways and strategies that it needs to be built into. Some of our ongoing work is building on the sustainability with the structures, pathways and negotiation.
118. The next bit is testing Counterweight in different settings. We have only just started evaluating Counterweight in the community, in pharmacies. I did not mention that we are also doing workplaces. Counterweight is happening in BP. That is because it sits within one of our health board areas. There is wider evaluation where it is important to check we are getting the same level of evidence that we did when our nurses were delivering Counterweight. Clearly, our nurses have a huge amount of clinical expertise in managing all of the weight-related complications. A general healthcare assistant does not come from the same background.
119. We are expanding on our delivery and practical application of getting the programme positioned. We are testing it in wider areas. We are also developing more expertise in being able to get the evaluation, getting the data, in electronic form, where it can be very easily evaluated, because the Scottish Government were going to develop an evaluation that was much broader than Counterweight as part of the Keep Well programme, which is to do with deprivation. The national evaluation did not work. After two years, they said, “Work out your own evaluation." We have just put it into test in the last year, and we have now managed to get a system where dumps of anonymous data can come from practices and be amalgamated so we can come up with the evidence.
120. We have done different things. I do not know if that answers your question. Is there anything that is missing?
121. Mr Rollins: Well, it is just the sustainability. Do you feel that, by giving more time and more dietetic involvement, or is it the behaviour approach — you must have thought?
122. Professor Broom: In terms of sustainability within the individual, is that what you are talking about, rather than the practice?
123. Mr Rollins: A bit of both, yes: of the individual.
124. Professor Broom: There is quite a lot put into relapse management as far as the training of the clinical staff is concerned. One of the learnings that we brought from the research to the development phase is that the nurses themselves asked for that relapse-management training to be brought upfront. We would leave it very much up to the practices to decide when and if they want to bring patients back. Patients are free to return to the weight-loss programme and have further mentoring, if you like, by the practice nurses.
125. The problem, of course, is workforce moving on and having to retrain in the practice. That is why it is essential that, in each primary care trust or health board area, there is continual funding from the health board or PCT to maintain an individual trained in weight management. You cannot just take a dietician and shove her in and say, “You will deal with weight management." We had to train all of the dieticians. Hazel will tell you they went through a fairly intensive programme.
126. Ms H Ross: There is one other point, though, that you have mentioned that is really important to do with sustainability, which has become a bit of a burning issue across the UK and has been touched on earlier, and it is to do with the GP contract and where obesity sits. Ultimately, we recruit practices by getting the most enthusiastic ones to come on board, and we have never yet gone into an area where practices have not wanted to do it.
127. In some health board areas, we have got blocks of practices coming on board and a health board that is asking why it does not offer Counterweight in other settings to balance. The big crux is that the GPs are saying that they are being paid more to just look at diabetes or just look at the other medical disease areas and that weight itself is not bringing in the points.
128. At the moment, within the Keep Well programmes in Scotland, there was funding for incentives to get people through the programme, and, where there was funding for incentives, it massively affected the amount of time that practices could offer to bring people through the programme. The practices were paid in blocks as patients progressed through those appointments. One of our PCTs in Essex, England, just commissioned 20 practices, and its initial waft of communication with practices was getting a cool response. All of a sudden, the GP heading up the obesity strategy found £20,000 or £30,000 for prioritisation of obesity, and he put in some incentives.
129. Now there are practices queuing up at the door to do it, because they are saying now we can just argue that this is a priority. I think there is a bit of a debate about the fact that we have a programme that works, but the clinician that we are training has to be paid, and they are either a nurse or a healthcare assistant. The nurses are there anyway, but they are not maybe doing as much structured work with weight anyway, and the healthcare assistants were never there anyway in some of our areas and brought in new people.
130. Dr Deeny: Some of my questions have been answered, Hazel. First, I have a mindset problem — I have loads of mindset problems — with portion sizes. I was brought up with the notion that it is a sin to leave good food. I see my kids, who are all into sport, and they can leave food; however, I would nearly eat it for them, because some of us have a mindset problem. That is why I have to work on the portions that I eat. As a GP, I am very interested in the Counterweight programme. I looked at the figures that you mentioned; £12 a year for Counterweight per patient.
131. Professor Broom: It is £60.
132. Dr Deeny: How much is it for five years?
133. Professor Broom: The cost of treating a patient for one year — the programme lasts one year — is £60.
134. Dr Deeny: Well, if you take 50 patients per practice that is £3,000 a year per practice. That is not a big amount of money, when you think of the drugs that we are providing. I was saying to Mark earlier that I do not like writing prescriptions for drugs, particularly central nervous system (CNS) drugs.
135. Professor Broom: What I did not show is the drug detail that we looked at is that you can actually cost recover almost 50% of the cost of delivering Counterweight by a reduction in drug costs. That may not be in practices, but that is the overall cost to the Health Service.
136. Dr Deeny: Many of us do not like writing prescriptions for drugs, particularly those that work on the CNS. There have been concerns in the US about various side effects and stuff like that. I agree that this is an issue for central Government and that GPs throughout the whole of the UK and Ireland should be thinking very seriously about building that into our practices. We should have obesity clinics just as we have diabetic clinics.
137. Professor Broom: Sixty per cent of the top 10 drugs in the UK are delivered to the obese population. So, the 25% who are obese are taking 60% of the top 10 drugs.
138. Dr Deeny: We need to build into GPs right across so that they are incentivised. That is where the cost goes in. Obesity, as you know, has now been introduced to the outcomes framework, so it is made of interest. We have the staff to do that. If you are talking about 50 patients over a whole year, it would not be that much. Does the Health Department in Scotland support that?
139. Ms H Ross: We are funded in Scotland and work in every health board. Just to add to what you said, the health-economic costing includes the cost of the nurses’ time, and, in most scenarios, new nurses are not employed; they are just rejigged. Instead of just weighing people for ever and saying to them to eat less, they do Counterweight. So, often, new costs are not spent. From the health-economic costing, they did put it in as if it were new money.
140. Dr Wilde: We need to keep moving, but you have questions, Ivan and Bernie. After that, we will move on to the next subject.
141. Professor Perry: That is the first time that I have seen the data, and I want to highlight how impressive the economic analyses are. Someone with whom I worked in health economics once made the point that the first rule in health economics is that you never save money, you only decrease the rate of spending. Therefore, the fact that you are estimating savings is hugely significant. Nurse time is a scarce resource, as we all know, and you obliquely referred to the feasibility of less highly skilled workers being trained.
142. Professor Broom: Lanarkshire elected not to deliver Counterweight within primary care. However, the data was linked back to a primary care centre. Counterweight was delivered by trained healthcare assistants as opposed to practice nurses. They are much cheaper than practice nurses, but, in effect, we were getting better weight-loss data from Lanarkshire than from the rest of phase one of Keep Well in Scotland. We were getting 5 kg of weight loss in Lanarkshire as opposed to 3 kg elsewhere.
143. Ms H Ross: That is because they only did Counterweight and became very good at it. There are practice-employed healthcare assistants too, and they do equally as well as nurses.
144. Professor Hannigan: What do we know, objectively, about the effectiveness of the various initiatives for teaching people how calorific their food is? My personal view is that a lot of it is just branding and that it is a publicity stunt by various supermarkets.
145. Professor Livingstone: What do you mean?
146. Professor Hannigan: Do you know the way that there are traffic lights on food labels?
147. Professor Livingstone: Yes.
148. Professor Hannigan: Or, in other ways, there are people who are reasonably numerate or who can find the box in English on the back of the package.
149. Professor Livingstone: You are wondering who has time in the supermarket to look at that?
150. Professor Hannigan: Exactly. How receptive are people in being able to translate what is on the packets into how it will affect them?
151. Professor Livingstone: That is the gap; I do not think that people fully appreciate that. As regards nutrition principles, dietary principles and dietary guidelines, if you ask most people, they can tell you that they eat five a day. They can talk about carbohydrates, saturated fat and all the rest of it, but accurately applying nutritional labelling into their choice of food, I am not certain, but I have my suspicions that people are not very effective. It is the old adage that people eat food, they do not eat nutrients.
152. Dr Wilde: Does anyone care to make a one-line comment on the evidence on food-labelling interventions?
153. Professor Perry: A natural experiment is about to unfold in the US, where legislation at federal level will require fast-food chains to indicate calories, and so forth, and that will be interesting.
154. Professor Hannigan: Do we know whether more people understand the amount of calories they were eating as a result of labelling?
155. Professor Gately: No; the research on menu-board labelling that is just out from New York State shows that it does not switch people’s behaviours in any way, shape or form.
156. Ms H Ross: Our experience is that you have to get down to behaviour. People are doing such extreme things in terms of their eating patterns. If they could understand their own behaviour, they might just eat one packet less. It might be very unscientific, but they might just say, “I feel better about myself, so I am not going to eat a whole packet of biscuits. I will eat something else instead."
157. Professor Livingstone: There are all kinds of subtle things going on. The crockery that people use is getting bigger, and, as a result, the portion size is growing.
158. Dr Wilde: I have heard that. We have time for only two more comments.
159. Professor Broom: As far as food labelling is concerned, you can label food as much as you like, but, if it does not taste as well as you would expect, you will not stick with it.
160. Mr G McFarlane: I have two points to make. First, behaviour is different from understanding in relation to labelling. Secondly, certainly in some of the work in which I have been involved, the labelling initiatives and schemes are improving, but there is scope for more improvement.
161. Dr Wilde: OK. I am just going to move on to the next bit, but we can come back to the issue of labelling and the evidence for and against it. Thanks very much indeed, Iain, Hazel and Barbara.
162. Professor Ivan Perry: Going back, and it dovetails very much with what Professor Livingstone said, we all know that there is an obesity epidemic in children worldwide. The importance of this work, as with all public health surveys, is that it gives us a sense of the magnitude of the problem and, hopefully, an appropriate sense of urgency.
163. Our work has looked at trends in the height and weight of children from the south of Ireland, where we have data from 1948 to 2002. Doctor Bernard Cousins, who co-ordinated the work in 1948, is still alive and was delighted to get a copy of the published paper on this work.
164. The data is based on a study of more than 19,000 children. It was a North/South oral health survey that was carried out by our colleagues in the dentistry school in Cork. When we realised that they were doing this, we asked them if they would consider measuring height and weight. Our colleagues in the dental profession were happy to do that. So, we have data from North and South. I will present data only from the South today, because we had the trend data from the South.
165. In the interests of time, I will not labour what has been happening. A lot has changed since 1948, and I will not labour that fact. The salient point is that McDonald brothers opened their first self-service hamburger restaurant. In 1948, as we all know, there was a significantly different environment than there is now. When we are thinking about obesity, there is no getting away from the fundamental environmental determinants. As we will see, the environment has changed adversely and, perhaps, sharply in recent years, but I do not think that we should accept that the changes are necessarily irreversible.
166. The other element, over the period, is the growth of the Irish economy. The figures on the slide are not GDP per capita — I wish they were — they are simply GDP. We have had the Celtic tiger phenomenon; but now, I suppose, that has been transformed into a Celtic kitten. There have been other studies of trends in height and weight, but, perhaps, not that many over 60 years, and not that many in a country that did not really have a post-war boom. So, we did not benefit from Marshall aid, and so on. It was only in the past few decades that the economy in the South took off. We have data on height and weight from the 1940s, 1970s and from the early 2000s. I do not need to labour the effects of growth in the economy and in changes of lifestyle, food choice and portion size and so on that went with that.
167. In 1948, a national nutritional survey was carried out. The height and weight of just under 15,000 children in the Republic of Ireland was measured between 1946 and 1948. Then we had data from the 1970s. That work was led by Hilary Hoey and colleagues, and, in fact, our current growth standards in the South are based on that work. In 2002, we had the data from the North/South oral health study that I have just described. Again, there were roughly 17,500 children in the South of the original 19,000 children. So, they were relatively large sample sizes.
168. Essentially what we are finding — and its not surprising although it is relatively stark — is that the data on height is the good news end of the story. As countries develop, as economies develop with improvement in basic nutrition and sanitation, you get significant trends in growth, and these drive the increases in life expectancy that we have seen in all developed countries over the last century. So, we are seeing at every age, small but highly significant increases in height going from 1948 to 1970 and, indeed, continuing from 1970 to 2002. That is just comparing boys at age 14. An average 14-year-old boy was 145 cm in 1948, and that had increased to almost 170 cm in 2002. So, they are very welcome increases in height.
169. Obviously, one expects a parallel increase in weight; but we are finding, as you will expect, weight increase is substantially disproportionate to the increase in height. Again, it is worth emphasising that this is a population-level phenomenon. At every age from four to 14, children are taller and heavier. So, it starts in the cradle. When you look again, the figures for 14-year-olds are particularly stark. I have got a soon-to-be 14-year-old myself at home at the moment, and it is interesting to compare that the average 14-year-old boy was 37 kg, which is about five and a half stone, in 1948. By 2002, that had increased to just below 61 kg, which is nine and a half stone. So, that is a four-stone increase in weight. That just puts it in terms we can all identify with.
170. There are similar trends for girls, and trends that we were seeing at all ages. Although there was some increase in weight between the 1940s and the 1970s, perhaps slightly more took place later: there is some evidence of acceleration between the 1970s and 2002. So, when we translate this — and obviously the appropriateness of BMI as a measure in childhood is debated — the data on BMI emphasise the extent to which the increase in weight has been disproportionate to the increase in height.
171. We know what is driving this, and Barbara Livingstone has summarised it very powerfully and, indeed, has provided very elegant laboratory data supporting what is happening to our children as regards large portion sizes and the decreasing opportunities for physical activity. This is just looking at trends in Ireland over two decades as regards mode of travel to school. As one expects, from 1981 to 2002, the proportion of kids travelling on foot is falling and the proportion of kids travelling by car is increasing year-on-year. Again, this is not an immutable law of nature. These are the sorts of simple environmental issues that we can potentially do something about. However, it requires multi-sectoral and Government-led initiatives.
172. The data provides pretty stark and compelling evidence of the evolution of the obesity epidemic in childhood and, as we know, this will contribute to epidemics of triple type-2 diabetes and also heart disease and cancer, with the expected impacts on health.
173. Dr Wilde: Thank you, Ivan. We will carry on straight to Patricia Heavey.
174. Dr Patricia Heavey: Good afternoon. My name is Patricia Heavey and I am here from the National Nutrition Surveillance Centre (NNSC) at UCD. I have officially started in this job yesterday. [Laughter.]
175. I will give you a brief overview of the NNSC. It is run by Professor Cecily Kelleher. She could not be here today; and, as I said, I am the manager for the NNSC. One of the first activities that I want to talk about that we have recently been involved in, and this is following on from the data that Ivan has just presented, is the outcomes from the National Taskforce on Obesity. In May 2005, the report of the National Taskforce on Obesity, ‘Obesity: The Policy Challenges’ was published. The aim was to provide the policy framework for addressing the high prevalence and rising levels of overweight and obesity, in particular, childhood obesity that was being produced and we could see was happening in Ireland. The report provided 93 recommendations for actions aimed at six sectors. There are five aimed at high-level Government, 22 at the education sector, 13 at the social and community sector, 24 at the health sector, nine at food commodities, production and supply and 20 for the physical environment.
176. The NNSC was commissioned by the Health Service Executive in 2007 to review the progress and address these recommendations in this report. The NNSC identified about 100 key stakeholders and letters were sent asking them to complete a postal and electronic questionnaire. That was followed by three reminder letters and questionnaires, and organisations were also asked to outline any new initiatives that met the NTO recommendations.
177. A draft report was produced last year and was compiled by the NNSC. It was used recently by the report of the Inter-sectoral Group on the Implementation of the Recommendations of the National Taskforce and it was published in April 2009.
178. Our review fed into that report, and it was shown that significant progress had been made in 30 recommendations; partial implementation had occurred on 29; there was action progressing on 26; while no progress was reported on eight of the recommendations. When that was broken down, one can see that different sectors approached had different progress reports to date. In high-level Government, there was significant progress seen on two of the recommendations, and partial implementation on two. As one goes further down, one mostly sees partial implementation or action progressing in the majority of the recommendations as opposed to significant progress.
179. Obviously there is a lot of work involved. Several working groups have resulted from the report, and a lot of them will be reporting later in the year on the recommendations and how those have been implemented.
180. I will return to the NNSC and what it actually does. The centre is required by the Department of Health and Children to provide an independent source of information and advice and is responsible for the collection and collation of variable data relating to nutrition and health. There is also an advisory board to oversee the running of the centre, with external membership from the health promotion unit of the Department of Health and Children.
181. The centre’s aims are to provide accurate, reliable and timely information in an accessible form at short notice; to monitor trends in health status correlated with all aspects of the food chain and advise on these findings for health planners; and to provide a source of information and research expertise, particularly in nutrition epidemiology and surveillance methodology to those wishing to mount specific projects such as micro-surveys.
182. Here are some of the projects that we are involved with that have been set out for 2009. There are several investigations, particularly into grey literature. The first one is looking at the grey literature on existing data of growth monitoring of children in Ireland. We are looking at a review of the national guidelines for community-based practitioners on the prevention and management of childhood overweight and obesity; family-based approaches to treating childhood obesity; and a review of national and international research relating to obesity. We are finding that there is a lot of work going on at ground level, but we need to collate it and bring it all together and look at those grey areas.
183. One of the surveillance studies that we have been involved in recently has been the Lifeways cross-generational study. That is a unique cohort study that started in 2001 and was designed to capture Irish longitudinal data by recruiting three generations of the same family. Data was collected in 2001 on the mother and the baby, and we have now been able to follow up on height and weight measurements etc on these children, and we have now got a nice set of data on these children. These are hopefully going to be fed into the national database on growth measurements, which has been a recommendation of the National Taskforce on Obesity.
184. Another project that we are also involved in is the WHO childhood obesity surveillance project. The Department of Health and Children and the Health Service Executive (HSE) commissioned the NNSC to carry out this work in the Republic in 2008. That ties in with the recommendations made in the report of the National Taskforce on Obesity. We carried out the surveillance project last year, between April and July, and we collected data on 2,400 seven-year-olds. The report is being produced at the moment. From that, we have seen that we are still seeing high levels of obesity and overweight. With girls, that is significantly higher in seven-year-old girls; 28% of girls are overweight or obese compared with 18% of boys who are overweight or obese. Again, that will be published in the next couple of months.
185. Finally, I just want to mention a project that we are working in partnership with the Institute of Public Health and the Health Research Board (HRB) Centre for Diet, Diabetes and Obesity. That project is being co-ordinated by Ivan Perry. The NNRC will produce internationally competitive research that will provide the evidence base for public policy, health promotion and clinical practice and the prevention and management of obesity, diabetes and related metabolic disorders. That is an overview of the work that we are carrying out.
186. Dr Wilde: Thank you very much, Trish. We have time for discussion on any questions on the last two, or any other, issues that you want to raise at this stage. I am delighted that John McCallister MLA, a member of the Health Committee, has joined us for this session. You are very welcome.
187. Mr McCallister: Thank you.
188. Dr Wilde: We are having presentations with follow-up discussions; so the floor is open for any questions or points that anybody wants to make.
189. Professor Kee: Thank you for a very enjoyable presentation, Ivan. Simple though the data are, you spoke convincingly of the sometimes subtle and not-so-subtle cultural changes that have occurred over that long span. My plea is that we do not create a false dichotomy in that we must invest in treatment programmes to the exclusion of other things. We must do things hand in hand; we have to tackle the broader determinants and we have to have treatment programmes in place. So, it is not a false dichotomy; we have to do both. I know that you worked in London for a while, and that you remember Geoffrey Rose saying that we have to shift the mean figure as well as tackling those in the tail of the distribution. We must not content ourselves with putting the ambulances at the bottom of the cliff; we have to have fencing at the top.
190. Dr Wilde: That is a very important point, in view of our discussions.
191. Mr G McFarlane: Trisha, I do not wish to put you on the spot, because I appreciate what you said about me. However, of the 93 recommendations, which is a lot, it strikes me that there was no reported significant progress made with the food commodity sector. I know that that is going to be an ongoing challenge, and it taps into some of Barbara’s comments. Do you know why that is the case?
192. Dr Heavey: A lot of the recommendations were not quite expected. Perhaps they were expecting a bit more. The recommendations in that sector are in progress, but I think that a lot of the time they are waiting for information, especially with regards to food labelling and such things. That is why there has not been as much progress, and a lot of the time it is not enforced as such. They are recommendations, so whether you will see those recommendations taking place is another thing.
193. There are several working groups in that area, and it did appear that a lot of work was being done. But when one broke it down, there had not been many changes at the ground level or at industry level. It was very much directed at —
194. Mr G McFarlane: The reason I ask is because I have particular interest in this. I almost have a hypothesis on it. It seems to me that the food industry, potentially, has a huge contribution to make to tackling obesity, and I am not sure that we are using the conduits into that industry to best effect at the moment. It is about engineering change and implementing some of it.
195. Professor Perry: We have been involved with colleagues in the Food Safety Authority of Ireland in looking at dietary salt, and there has been a lot of detailed engagement with the food sector on that matter. Progress is very slow and painstaking, but when one sits down with them, they are willing to meet you part of the way. We need a carrot-and-stick approach, because we need to incentivise the less-engaged elements of the sector.
196. Dr Wilde: I welcome Carmel Hanna, who is a member of the Health Committee.
197. Mr Rollins: I thank Ivan for warning us about what is happening in the South of Ireland. We are aware that kids are getting taller and fatter, and your BMI charts are changing because of that. You have this evidence now. My colleagues who try to kick off some interventional projects in the South cannot sustain anything.
198. Funding is a huge issue. I do not want to get into the realms of public sector money in the South, but can you tell us your frustrations from taking this forward now? You talked about projects. You have the evidence. The evidence is there. You are going to get further information. All the kids are getting fatter. What is the next step, and can you give us an indication from the Government in the South about whether they are taking this seriously or is this going to be at the bottom of the list?
199. Professor Perry: There is frustration in the lack of urgency. I come from an academic perspective and I am not directly involved in service planning. But at Government level, my colleagues who are working on the cardiovascular strategy are trying to link the obesity agenda with the green agenda — what you might call global fattening alongside global warming. There are common issues driving both of those, particularly in relation to cheap fossil fuels and transport.
200. Those are not things that will produce overnight solutions, but it is likely that, in the next decade or so, as the global warming agenda kicks off, Governments will have to address it. We need to be ready to ensure that the health agenda, particularly obesity, is a further reason that there would be joined-up thinking between the Department of the Environment and the Department of Health, Social Services and Public Safety.
201. Professor Livingstone: I wish to return to the issue that Gary raised about the food industry. It is instrumental in all of this; there is no doubt about that. The industry is moving a slowly, and I support what Dr Heavey said about nutrition and labelling. It is slow to act because the EU has yet to deliver.
202. I do not like the attitude of the food industry being the villain of the piece. It may well be, but we all have to work together in the sector, and the Food Standards Agency has been working with the food industry and has, for example, reduced the levels of salt in processed food quite significantly. There is a lot of room for reformulation; there is a lot of room for working in collaboration, and I think that taking a negative stance will not help anyone with this issue.
203. Mr G McFarlane: I was not taking a negative stance. What I meant was that we need to realise that the food industry is about making money —
204. Professor Livingstone: Yes. I am a shareholder in a food company and I have no issue with that. I also appreciate that the food industry can and will take action. It is not going to lose out because consumers are looking for healthier food. It is under pressure to produce healthier food and, therefore, shares will go down. I think that the food industry is protecting it. I am not protecting the food industry, but I think that we have to work side by side with it, and it is making strides.
205. Dr Wilde: It is perfectly reasonable for us to have some dilemmas and a bit of controversy. It would be completely sad if we were to put all of the dilemmas under the table, so I think that it is good to have one of those raised.
206. Mr McCallister: I am a shareholder in a food company as well —
207. Professor Livingstone: I am glad that you have said that, otherwise it would be reported in the papers tomorrow. [Laughter.]
208. Mr McCallister: I also had a background in agriculture before coming into this role. I was interested as a follow on from the points that I was making between linking some of this in with the environmental agenda. I take Professor Livingstone’s point that food companies will respond to the market, so there is very much a link between the two and how you work that together. We have been involved in a campaign a party political level on honest food labelling, from where the food comes from, and building on that.
209. I do not think that the EU has failed to grasp the nettle on this one. However, we need to see much more action there. There is an opportunity for us to build on some of that, and drive a public health agenda and pressurise the food industry to play its part. We should use the environmental argument as well.
210. Dr Wilde: I think that that is very important. I am just using my chairman’s privilege to say that we in the institute do have a public health agenda for the European elections. I will put a copy out. That makes the point that it is time for a healthier Europe.
211. Professor Kee: First, picking up on the point that Mr McCallister made, the EU also has promulgated a policy of health in all policies. The EU wants to put health on the table of all Government Departments, and it is very important that all Government Departments address that issue.
212. I want to make one other point, and it is about cross-departmental investment in solving this problem. We know that there is an intricate two-way relationship between economic growth and public health. Public health drives economic growth and economic growth can, in the right circumstances, drive health. There has been massive investment in some aspects of infrastructure for health research and discovery, and I guess, across both universities, about £50 million has been put into facilities largely in the biotech side of health research. However, the engine of public health discovery is something that we saw on the slides — longitudinal studies and cohorts following up for long periods of time. That is the infrastructure that public health research requires, and that is the engine of discovery. We would not have known lots of different things about heart disease risks, obesity and smoking were it not for studies such as those conducted at Framingham, Rotterdam, or wherever. When we are talking about where investment has to go into public health research, we should bear that in mind.
213. Professor Broom: Just to add to Ivan’s Celtic tiger, if you actually look at the developed world and look at those countries that have freed up their economies dramatically — the United States, the United Kingdom and Australia — and compared them with France and Norway, the levels of obesity are certainly different. So, the free-market economy actually drives obesity as well, apart from driving the global-warming issues.
214. Professor Gately: I just wanted to make a point, really around Professor Perry’s data, which in many ways is fascinating and really helpful. Because one of the problems that we face in the context of some of the activities that are currently underway and being considered around prevention are around most of the concepts — most people are actually looking at children under the age of five at the moment as a key target group.
215. And, in some ways, I have slight problems with that as a group, because the recognition of those children as overweight and obese by themselves, by their parents, by healthcare professionals is very, very difficult, particularly given what Professor Perry’s data is showing; that we are talking about, over a 50-year period, a 2-kg change in a four-year-old male and a 1·6-kg change in a four-year-old female. Whereas, for a 14-year-old over that period of time, we are talking about a 23 kg change and we are talking a 19 kg change for girls.
216. Some of the problems with looking at a young age that are likely to see a very small changes is that you are not going to be able to detect the impact of interventions at such a young age. And therefore, it then makes the economic case, which, I think you guys have put forward very, very well, around children and around where investment should be extremely difficult. And we have done some crude economic analysis of our interventions, and it shows up that for every £1 invested, we see an annual £1.10 return on a child that would be three standard deviations from the norm, because they are going to be the most expensive ones. They are the cases Michael Ryan was talking about. But we can only see them presented to us as young children or adolescents, not very young children.
217. In terms of thinking through where might the strategies be, I would step back and try and observe the landscape, and rather than jump in at under-fives, which is what a lot of people are trying to do at the moment, I would step back and say; OK; they are an important age group, we see that some of the preventative work is working. Rather than to keep focusing on that age group and designing new interventions, let us actually see, further down the line, where most action is necessary, because the NCMP data, which was out last week from England, very clearly shows that whilst we have seen a plateauing in BMI, we are also seeing the more obese children becoming more obese quicker.
218. So, I think it is really, really useful data that I think could maybe help shape where the targets might be. Because, you know, Michael made a very clear appoint about targets for adults, and I think there are some good interventions. We have got some good intervention outcomes for children and adolescents, but the young children data is very, very poor, and we know less than 50% of obese five-year-olds will be obese adults is what the evidence base shows clearly.
219. Mr McFarlane: I just wanted to sort of reinforce and pick up on the point that Professor Perry made about the links between, in particular, the environmental sustainability of the climate-change agenda. I mean, I would really like to, maybe, explore that this afternoon, because there are inextricable links between obesity, particularly in terms of prevention, in fact they are completely and inextricably linked. And I think we would be missing a trick if we did not use what is, frankly, in a global sense, a more pressing crisis to actually drive, if you like, more effective intervention. So, there is a great deal of complementarity there. I mean, it is no coincidence that the most obese nation in the world is also the most carbon intensive, in other words, America.
220. Professor Broom: Just to follow up on Professor Gately’s comments, I would take slight issue with him in that I think behaviour trends are actually set in the under-fives. You may not see the problems early. The weight changes are dramatic, but the behaviour is set. One of our biggest problems I think we have is our current risk-averse society; the kids are not allowed to play freely. They have structured play at nursery school.
221. They should be out and about. They should be climbing trees, falling and breaking their collarbones or whatever. They are not allowed to do that now. They are in-built to be totally static and they have structured play. It is the fault of our risk-averse society.
222. Professor Hannigan: Ivan, did you say that for the 2002 study that you had North/South data?
223. Professor Perry: Yes.
224. Professor Hannigan: Ok, so, obviously, here we did not have the Celtic Tiger, although people’s lives improved over the period. Were there any differences in the data between kids North and South?
225. Professor Perry: I have the North/South paper here.
226. Professor Hannigan: All right, maybe we could have a look at that at lunchtime.
227. Professor Perry: We did not have the trends over time in the North. When we compared cross-sectionally, one thing we found that was slightly surprising was that children in the South were marginally taller, but there were no significant differences in weight. The sampling strategies were broadly similar in both; they were both school-based surveys. The response rate was marginally lower in the North than in the South, so we have to be maybe a bit cautious in making comparisons. There were no striking differences.
228. Professor Hannigan: So, therefore, equating the change to such a large extent to the different economic climate in the Republic perhaps is not the whole story.
229. Professor Perry: I think that is right. I suppose what has really been happening in all societies has been a gradual improvement in living standards and the relative cost of food has been falling and so on. I suppose it was just that slightly sharper upturn in the South.
230. Professor Hannigan: Finally, a lot of people have mentioned the economic value of investment in these schemes. If we think about and quoted frequently the recent Wellcome Trust study that showed that for every pound invested in cardiovascular disease research your return on investment from health gains and economic gains is 37p per year in perpetuity. That is a massive economic and health benefit from investment in cardiovascular research.
231. Professor Perry: Is that a recent publication?
232. Professor Hannigan: It was published in November 2008 and is on the Wellcome Trust website. It is called ‘Medical Research: What’s it worth?’
233. Professor Gately: I just wanted to clarify my point around behavioural interventions, because I am looking at it from two perspectives. One is prevention and one is treatment. I think there is a shift and a very strong drive across a lot of the PCTs we are talking to in England about treating obesity in children under five. I think there is risk with that. I think you are absolutely right from a preventative strategy and shaping some of those key behaviours is absolutely critical. I think that is where investment should continue, and I think we have seen some of the outcomes of that in some of the NCMP data. In terms of direct interventions for those young children, we do not know what the outcomes of those interventions are going to be, which is why I was making that point. I totally agree with you.
234. Dr Ryan: Again, I would make an appeal for action. I feel that the intervention and the urgency of action needs to be commensurate with the risk. My concern about a lot of the discussion this morning is the lack of sense of urgency in terms of the threat to the welfare of our population. When you are obese, say for a 40-year-old woman, being obese will take four years off your life at least. That is worse than all the cancers put together, and we need some kind of commensurate response in terms of establishing obesity and getting recognition of it as the major threat to our health that it is. The younger that people become obese, the more it will crimp not just their life expectancies, but the quality of their lives. The scale of our response has to be commensurate with the scale of the risk.
235. Professor Hannigan: As a follow-up to that, the Medical Research Council (MRC) recently released figures that quantify the risks to lives of obesity. I cannot remember the number, but it is a significant detriment to one’s lifespan. It is not quite as bad as smoking, but it is significant nonetheless.
236. Dr Harper: On the positive side, I would say that there is an increasing recognition of the need for urgency in this area, and the fact that the Health Committee is having this inquiry is one indicator of that. Certainly, within the public health agency, the whole area of the prevention and treatment of obesity will be a top priority for us.
237. I think that some of the debate reflects the need for a clear … We have heard the joined-up phrase, and we need that, but at action level. Seeing how both the preventative elements and the treatment elements fit together and the wider determinants work fits together as well. Particularly, the very young age group and the message is there. It is building the skills and the knowledge that will see them and their families through life. Equally, at the other end, we have got to have that high cost, high intervention element to it as well. I have got a lot out of this debate so far, and I am looking forward to the discussion this afternoon as well.
238. Mrs Hanna: My apologies for being late, but I was at another Committee meeting. I hope to pick up any papers that you may have to help inform me. I am a very practical person. I am always trying to get stuck in to see what we can do. I do think that it is very much part of the public-health agenda. I think that a big part of it is to try and encourage people to take more responsibility for their own health. We know that that is a huge issue, particularly in the less-well-off areas, and there is a widening gap between the haves and the have-nots. People do not have the choices that we have to go to Marks and Spencer for their nice fruit.
239. What practical programme do we have there? Maybe the breakfast into school, also bringing fun into play at school, to show children that when they go home they can go out to play and have games — as Professor Broom said.
240. A lot of it is also about some one group or person taking ownership, leadership and co-ordinating. It is all over the place. There is a lot of good work being done. There are good pilots, but the good ones are not being picked up, as often happens. We have to one group or one person who has got to lead on this and pick up from everywhere.
241. I heard Dr Ryan talk. A lot of it is about trying to motivate people. We all know what it is like if the chocolate is sitting there and we want to eat it. People who are doing it all the time are becoming more and more overweight. How do you break that cycle? A lot more thought has to be put into that.
242. It is working with people, particularly less-well-off people, because that is where we have most of the challenged lifestyles. [Inaudible] They are the people who maybe are not counting their units, or whatever. We need to get in there and really work with those people to try and change, and to be as supportive as possible, with good practical programmes.
243. I am a midwife as well, and I think you get in at the antenatal stage. You have got to get in with good nutrition programmes and activities, because a lot of our parents now … I know that when I had my first baby, I was at sea — although I had been a midwife. However, for someone who has not had good parenting skills from his or her parents, they do not know. We see people with babies, and they do not even know about keeping a baby warm or how to give gentle chastisement to a toddler. A lot is about early intervention.
244. I heard what you said about having to look at what happens down the road, but I am a great believer in prevention and early intervention. They pay dividends. One needs to be as practical as possible and to be focused on the work on the ground with the people who have these challenges. They have very little money, they have the children who are all over the place; they do not have time to cook, so it is much easier to go to the shop at the corner or the supermarket to pick up a burger — a burger full of rubbish.
245. Mr McCallister: I will be brief. I want to follow on from your point about the difference between early prevention and intervening almost at medical level.
246. I think we have become a very risk-averse society. You used the example of falling out of a tree. Thankfully, I did not do that when I was growing up; although I was up plenty of trees, right enough. The difference between, even you take something simple like walking to school; a good healthy thing. Rural schools’ groups and Sustrans have been trying to get more of that sort of thing. The very simple thing of the school run and you are back even into huge environmental issue and the risk involved in that.
247. Dr Wilde: There are so many different things. We have had a really good morning. I just want to thank the researchers so much for making the presentations, but also everybody else for joining in so well. It was really good. I know that Iain has a quick comment on what Carmel said. What we will do after that is break, have lunch. There is plenty of time for discussion. The Committee Clerk will tell us where we need to go at lunchtime. We want to start again at 1.40 pm so we do get this discussion honed up for the afternoon. So, Iain, you just wanted to make a quick comment, did you not?
248. Professor Broom: Just to pick up on Carmel’s point about deprivation. Data that we did not show from the Counterweight programme actually demonstrated that it was more effective in deprived areas than in non-deprived areas. We got bigger drops in weight; much bigger drops in blood pressure; much greater improvements in glycaemia; and overall better improvements in the lipid profile. That was data that we have not shown, but it is in the papers.
249. Dr Wilde: And there are papers and examples. It is also recorded, Carmel, so that is fine. Thank you all very much.
Electronic recording paused.
Afternoon Session
-Electronic recording recommenced.
250. Dr Wilde: Members might come and go, but as long as we leave a couple of chairs at the end of the table. It is good to see you back with us, Kieran.
251. Our task for the afternoon session is to look at some of the areas of questioning that have already been developed as part of the inquiry and which have been put together by the research team to help us in our discussions.
252. The questions have been divided into four areas. We will go through all the areas, but I suggest that we try to focus on one area at a time. That does not mean that we cannot drift into other areas, but if we could concentrate on them one at a time, particularly looking, at this stage in our discussion, for points that we would like the Health Committee to consider when it is in session and as part of its report.
253. As well as putting forward points from this morning, any other points that you think are important in relation to those areas would be very much welcomed by the Committee. We have a good hour for our discussion, and I will take 15 minutes on each area and try, at the end of each 15-minute period, to try to summarise some of the key points.
254. I suspect that, in some of the areas, possibly like the last one, there might be fewer people here who have a particular interest in that area than others. That does not mean that that area is less important. It means just that we do not have the people, so we might spend less time on that area. Therefore, we will give it a go in that timed way, allowing for just a little bit of overplay on the timing if necessary.
255. Before we get into the discussion, please feel free to say whether there are there any other general points before, such as handling matters in a different way or making a point from this morning. I am conscious of something about which I had a brief discussion, which is that, if you feel dissent emerging in your own mind, please do say. I think that we can cope. We had a really good morning. It is OK to have controversial and dissenting voices. I am going to an event tomorrow in Dublin called Space for Dissent, and I am really looking forward to that. Heaven knows what the meeting will be like. [Laughter.] We are civil dissenters.
256. Dr Deeny: I missed a bit of the end of the session this morning. I was having a discussion with Gary over lunch, and the current economic climate has an impact on this matter. I was talking to a gentleman last night who has had to give up his job as a bricklayer and is now working seven days a week and 70 hours a week as a taxi driver. That has impacted on his life in a major way to bring in money for his family. He was a bricklayer for about 20 years.
257. We are talking about this, and it is good to be talking, it is very important, about how this whole economic problem, globally and here as well, is going to have an impact on all of us — for example, on how people eat. I do not think that we will be able to arrange set times for family dinners and suchlike.
258. Professor Gately: I think that most of the data would suggest that deprivation is a strong influence on levels of overweight and obesity. The National Child Measurement Programme (NCMP) has shown that, within levels of deprivation, obesity is going up in the higher levels, whereas, in the lower levels of deprivation, the BMI plateau shows reductions. So we are achieving some change. However, not with deprivation, and that would be associated with the poor economic climate.
259. Dr Wilde: I would like to hold that point and to discuss it now. That issue is, in a sense, part of number one anyway. As you said, the economic climate but also the particular point about how research can help policy and practice, particularly in relation to the people who are already, and increasingly will, suffer the worst effects of obesity. Therefore, I think that it is worth spending some time thinking a bit about that.
260. Dr Ryan: Is that not a potential area for high-level Government policy, where you can manipulate, so to speak, the choice of foods through a pricing strategy? Secondly, certainly in our area, one sees local greengrocers and fruit shops closing down to be replaced by a fast-food joint. Those are, in a way, Government policy issues that would send a significant message. If we can produce cigarette boxes that say “smoking kills", surely we can do something about belly-buster burger joints that sell treble burgers. There is a place in America that sells “triple bypass burgers".
261. Mr G McFarlane: I was going to say something else, but since that point has been raised, I do not know whether the Committee is aware that Martin Carragher has just concluded a study in Tower Hamlets, which is looking at the relationship between fast-food outlets and proximity to schools and the actual dietary patterns of school kids. Surprise, surprise, there is a straightforward correlation. One of the outcomes, which we support, is a look at the planning system and changes to planning policy that — at the risk of sounding nanny state-ish — restrict the number of fast-food outlets that are allowed to be near schools. Jane, I know that this is into built environment stuff, but, just as the point was made, I thought it worth pointing this out. The planning system and changes to it are a part of this jigsaw.
262. The point I was going to make was the direct relationship between income and predisposition to obesity, which I absolutely agree with you about. Certainly, within the limitations of the study we did on food poverty in Northern Ireland, it was very clear through the focus groups that that actually took place. The participants were saying: we know what we need to eat, we know what we should be eating, but there are limiting factors, cost — access, whether it be price or physical access — being the main one. The economic climate being as it is is only going to increase that. That is the problem.
263. Professor Hannigan: The first question is a very specific one, about the research community assisting in evaluations. This may refer a wee bit to some of the others.
264. Towards the end of last year, we launched a framework called ‘Commissioning Research’. The idea is that we were beginning to bridge the research-to-policy gap that exists big time in Northern Ireland. Because of our changes, becoming part of the Public Health Agency and loss of staff and various things, we have not really managed to get that going. What we can provide in R&D is a bridge to enable dialogue to happen with the community, the Government, the policymakers and then commission research that can be short term, long term, very focused, et cetera, as appropriate. As I mentioned to you at lunchtime, we have done that in relation to suicide. In a couple of weeks, I hope, we will provide the funding for projects on areas of self-harm that were agreed with the Department. We can do the same thing in other areas. Obviously, there are funding constraints. We have not a clue how much money we will have, but the mechanism for doing that exists.
265. Dr Wilde: Thank you, Bernie. It is helpful to have that.
266. Professor Livingstone: I am intrigued by the statement: how can the research community assist in the development of an effective measure of evaluation? Are you talking about the development of the tools for evaluation, or how is it about the research community doing or helping in the evaluation?
267. One of the major gaps in this part of the world is that we do not have really good surveillance on monitoring data, and you cannot really evaluate anything until you have that in place. As regards the evaluation, I totally support the fact that we do need to evaluate what is going on out there at the present time and, to be honest — I have just been talking to a number of people at this meeting — there are a lot of short-term projects that have been initiated and which have probably been completed but have been forgotten about. To my mind, that is inexcusable and a waste of public money. From the start, evaluation should be built in and ongoing. We need to find some way of building up some website, portal or whatever of what is on out there, properly evaluated, what works, what represents good practice and what other people can lift.
268. As regards tools for evaluation, the National Obesity Observatory had some excellent tools, and I do not think we should reinvent the wheel. I have just been into the New Zealand website for obesity prevention, and they have an excellent evaluation system. We need to put in place an evaluation structure. We need to evaluate what is out there and identify what is good practice and what is failing, because it is just as important to convey that properly.
269. Dr Wilde: I know that Frank wanted to come in on that, but I have got Gary, Ivan, Frank, and then it would be good to hear from some of the people from England, Scotland and Ireland — well, you know what I mean.
270. Mr G McFarlane: This kind of follows on from Barbara’s point; I read the question to mean assisting and evaluating obesity-related interventions. I have read the obesity-related interventions, rightly or wrongly, as being more about implementation and delivery of projects and initiatives that are trying directly to address the obesity issue than — and I am just clarifying this before I make my comment — about the policy that supports them. I think that it is important to make that distinction; they are different animals for me.
271. That being as it may, the single word that came to mind to answer the question was “offer". In other words, the question is how can the research community assist in the development of effective methods? Offer to do it. Particularly in sectors outside central Government, there is an issue around capacity, and I am thinking particularly about the local government sector here in Northern Ireland, where they would welcome the support and assistance of the research community in doing that. Although I take on Barbara’s point about tools that are already out there, it may just be about signposting, directing people or lending some support, but “offer" is the single word that came to mind.
272. Dr Wilde: Thanks, Gary. I welcome Claire McGill, who is a member of the Health Committee. We had presentations this morning, Claire, from the different researchers with us, and, this afternoon, we are really looking at some of the key questions that the Health Committee has acknowledged are important in terms of our research.
273. Professor Perry: In terms of natural experiments, I hoped that the Committee would take a very broad view of that and include evaluating actual policy experiments. In terms of tobacco and alcohol, we have evidence that certain policies work, particularly in relation to taxation and advertising. There is a certain kind of evidence base where people will argue that food is in a different category, which it is, but, nonetheless, there will be significant overlaps between food policy, tobacco and alcohol that should not be ignored.
274. The other issue that comes up is that, once you begin to think about policy initiatives for tax and bans on advertising, someone used the term “nanny state". That term always comes up, and, when you hear that term, you can be pretty sure that there is a vested interest out there. It is easy for us who are not in politics to say that the political system has to accept that, at a certain point and level, there is a battle to be fought. Not all of the food sector will be supportive. There is a lot of propaganda. The starkest propaganda out there is, for instance, that there is no such thing as poor food, only poor diets. There is a lot of food out there that you would not serve to primates in captivity, not to mention our children. That is a political issue.
275. Dr Wilde: Thanks, Ivan. Next is Frank, then Michael, and after that, Mark and Carolyn.
276. Professor Kee: Barbara articulated the desire for a repository of good practice and evaluation tools. That is one of the work packages within an award given to our centre, to Ivan and to the Institute of Public Health to take the first steps to create an obesity observatory for Ireland that would act as a repository of good practice and evaluation tools. Hopefully there will be progress on behalf of us being appointed to begin that work.
277. Secondly, I could not agree more with Barbara’s point about surveillance data. We need surveys that are fit for purpose, and for the last two iterations of the health and well-being survey we have not had measures of BMI. We must ensure that we have physical measurements in future health and well-being surveys in Northern Ireland.
278. Thirdly, Ivan talked about policy analysis and the evaluation of policy. In poor old Mexico, which is feeling the brunt of things at the moment, the health ministry has been at the forefront of a variety of policy experiments — not in infectious diseases, I have to say, but in terms of addressing the social determinants of poor health. A lot of what they do is methodologically within the framework of what the MRC calls complex intervention step-wedge designs. Our legislators and statutory sector can think about the way policies are rolled out. They could well be done in a variety of ways which gives us a greater evaluation dividend.
279. Dr Ryan: I am sorry to put a damper on the party here again, but there have been natural experiments over the last two generations showing that lifestyle change has resulted in a major threat to the life expectancy of this generation. This is the first generation in history in which the parents will outlive the children. Actuarial data shows that for every kilogram a person is overweight, an insurance company takes approximately a year off their life expectancy. Those guys deal in hard cash: they are betting money on people dying sooner because of weight. How many natural experiments do we have to wait to happen before we really get serious about doing something? I am sorry to harp on about the same message. I see the patients every week, as many of us do. There is nowhere for them to go; there are no resources for us to help them; and as for collecting data — we have been collecting data for 40 years.
280. Professor Livingstone: I take your point, but I do not think what we have been saying opposes what you are saying. There is an imperative to do something. I also think that alongside that, we should be gathering evidence about what is working otherwise there will be a lot more natural experiments and we will have more waste of resources.
281. Dr Ryan: In an environment of limited resources, where are our priorities? Hard decisions need to be made. Are we going to continue to observe or are we going to try to intervene? This meeting is evidence that the awareness issue has been addressed to a point. We now need an intervention strategy.
282. Mr Rollins: To go back to Barbara’s point: we are still all over the place. Lots of studies and pilot projects have been going on for years in Northern Ireland, and there are more taking place all the time. We have to gather them together and find out what works. For example, I was involved in an intervention study based on a fitness scheme to slim down obese children. The trouble is that we did that scheme in April 2006. We stopped it because it worked; we all lost weight, improved lifestyle sustainability for a year, but it is another one just thrown into the mix. We have to pull everything together. We cannot wait for the gold standard.
283. Frank talked about BMI. Some of my child professional colleagues do not want to measure those kids, and I have problems with that, because parents will come to me and say, “yes, I will get my kid measured; you will tell me that his BMI is high, so what are you going to do about it?" If I do not have some programme for dealing with that then —
284. We know the problem in Ireland. There is no point in just getting actual numbers. Yes, we will continually get those numbers, but we have to do something. We have to collate everything. There is great stuff going on in schools and in sports, but we are all over the place and we need to pull it all together. It is all out there. We have got the experience from England and Scotland. Let us see what is going on here.
285. Professor Livingstone: You have given schools as an example. A lot has gone on in Northern Ireland schools. It would be a model for the rest of the country such as the introduction of key skills in cooking and standards for school meals. Is that going to work, or is it just something —
286. Dr Wilde: I am sorry to interrupt, but there are loads of people with their hands up. It is not to take away from what you are saying, but everybody must get a chance. I will come back to you, but Carolyn, Iain and Paul are on the list. I have to do it like this; otherwise not everybody will get a chance.
287. Professor Livingstone: I apologise. It is quite wrong to —
288. Dr Harper: I do not know that there is all that much disagreement between us. We all agree that there is a need for urgency and joined-up action. There are areas in which there is evidence, and there are areas in which the evidence is not exactly clear, so we have to do both. We have to develop a coherent action plan that is not just about health but about the whole inter-sectoral response. We have to get those actions to ground level, but researchers have to be an integral part of developing the actions and evaluating them as they happen. Otherwise, we will not be any clearer six months, a year, or two years from now as to whether we should continue to invest money in those particular areas.
289. Equally, on the policy side, researchers, and the results from the actions on the ground, should inform further policy on pricing, differential taxation, et cetera. This is back to the coherent joined-up action plan that we need for Northern Ireland. One thing in our favour is our size, geographically, in the sense that if any area can do it, we and the South probably can, with the establishment of the Public Health Agency as a regional organisation and with the, in some ways, scope and remit to work across Northern Ireland and pull some of those actions together into a coherent plan. That should also be very much informed and evaluated by the research community.
290. Professor Broom: To follow on from what Barbara was saying; there is a huge amount of money spent on small projects throughout the UK. None of those projects is ever evaluated. Most are in the area of health promotion, and there is no evaluation whatsoever. It amounts to £20,000 here, £30,000 there, £2,000 in the next place. It all adds up to multi-million pounds. It is not directed; it does not really go anywhere. One gets a report, but not a proper evaluation. There is no research behind it. To my mind, it is a complete and utter waste of money.
291. The money would be far better put into programmes that are known and shown to work. We have programmes that work; we have programmes that work as regards childhood obesity. Again, if one looks at prevention and treatment, then the prevention of obesity has to be aimed at our children. We already have 25% of our adult population obese, but there is no treatment strategy for them, although there are strategies that work. It takes funding to make sure that one will reduce the BMI of a population by one or two units, because that is what we are aiming for — to take the mean BMI of a population down by one to two units. That will reduce the health risks drastically and be extremely cost effective in terms of our health economy.
292. That is one thing. The other thing to pick up from what Michael said about having to remember that if 50% of our shape is genetic then our shape is built according to our genes. Some people are going to be fatter and some are going to be thinner. The big problem that we have is that there has been a huge change in the environment over the last 30 or 40 years, most of which is down to automation and to the fact that people do not have time to cook properly. Not only that, they have actually lost cooking skills, as Barbara said. One of the problems is that home economics, which was taught in schools in my day, when kids were actually taught how to cook, is no longer taught. That, fortunately, is changing.
293. Most of our 20- or 30-year-olds do not have the cooking skills of our mothers and grandparents. Food is not that expensive: it is cheaper now than it ever was. What is expensive is pre-prepared foods. Fast foods are expensive in relation to the nutrition you get from them. We need to educate the population to not use pre-prepared foods. That is a big problem for the food industry, because that is where most of its money comes from.
294. To pick up on a point about satiety, the food industry does not tell the general population that pre-prepared foods must have a longer shelf life, and so preservatives are added to them. A lot of those preservatives have direct actions on the brain: they increase appetite and suppress satiety, so that we tend to eat more. If we just ate natural food, without preservatives, we would not be in the situation that we are in.
295. Dr Wilde: That has given us plenty to think about.
296. Professor Gately: We work with a range of different primary care trusts in England, and we find that some are very interested in setting up and delivering an intervention that is sustainable and that self-perpetuates future development. It is delightful to work with people like that, because they understand that you need to scope the problem, identify the key practitioners, deliver a good quality intervention, evaluate it, and feed that information back into the system to move forward. That comes with a much bigger price tag. Then there are other PCTs who only want to spend a small amount of money. You talk about whether you have the right people and the right systems. The answers are yes, we only want one thing, which is the delivery of an intervention. We have key performance indicators that we want to deliver against, and that is what we want you to do. We do not tender for the work of some of those PCTs, because it is not in our interests to do so. However, we tender for some of the work, because, politically, it is important to us, and it allows us to gain some evidence about why that model does not work. That is what we are finding.
297. Those who want to evaluate aligned to action are developing programmes. Rotherham is a very good example. The head of public health now spends very little time in Rotherham, because she travels around the UK talking about their strategy. Lord Darzi and David Nicholson came to see her. She talks not only about the work with us, but about a broader strategy in adults as well. One PCT invested £5·5 million. That is the most significant investment in obesity in terms of interventions that I have come across, but they are reaping the rewards of doing a complete programme. That is absolutely critical.
298. One thing I would say about practice and research is that, as Carolyn has pointed out, we are often saying the same thing, which is that the language is missing at some point. The public health specialists we are working with are saying to us “key performance indicators" and we are saying “variables". However, they can be the same if they are organised effectively, but you just do not get them to join up together. That is why we have a lot of interventions that are small scale and collect no real data for the future. Therefore, it is much bigger, as everyone said, activities around action and research and evaluation around it.
299. To build on that, I will broaden out one of the strategies that I referred to earlier. That has been to work more closely at regional level across the UK to get wider capacity and delivery of service provision. We are partnering with different academic institutions. It is a win-win situation, because we can disseminate a model much easier and young people at university are going through training programmes in nutrition, dietetics, psychology, physical activity, education, and are now getting opportunities to deliver. Therefore, enthusiastic young people who are on the same level as children and young people are then delivering those programmes to families. The university benefits because it is delivering training in the local community to primary care trusts, and it is generating revenue. It also benefits from a range of academics who can contribute in their own little ways. Some of them want to do specialist research, and others want to do broader generic research. We are seeing real enthusiasm around this now, which will help us to gain capacity. I have listened to my colleagues in Ireland, and I think that there are key experts around who can help it to work, as long as the language comes together and the action and the research is done together.
300. There is a very strong opportunity, because, as Barbara said, a lot of the protocols for the research are already there. We know that some of them are weak but they are what we have got.
301. Professor Kee: I want to make a meta-point dealing with capacity in Northern Ireland, not necessarily the research capacity directly. Again, if I just give you the exemplar of that Connswater Big Lottery Fund award, the Department of Finance and Personnel (DFP) had to do an appraisal of the Big Lottery Fund application. There is a great shortage of health economics expertise in Northern Ireland. I was just looking at that DFP appraisal of the Connswater bid, and it was done in many ways just to serve a DFP appraisal purpose; it did not have the health and economic perspective and had the fixed DFP rules.
302. I heard a lot about how cost effective some of those interventions may or may not be, but we need to look at public sector investments through the health lens and challenge DFP economists to take a slightly different tack whenever they are making big public-sector investment.
303. Mrs McGill: I apologise for not being here earlier, I was in the Chamber. The discussions are very interesting and I will come to Frank’s point in a minute. I was thinking that one could transpose this debate and discussion and place it in some other scenario and one would end up with almost the same situation.
304. I do not know how Kieran feels about this, but, as a member of the Health Committee, I have not yet heard what I might do about this matter. As regards Frank’s final point, I agree that it is difficult to know what lens DFP or any Government Department have to use when considering projects. DFP is the Department of Finance and Personnel, but I suppose if the issue concerns health, there should be a health focus, so I take that point.
305. Dr Deeny: I am just looking at the two questions on how to research and thinking to myself that I cannot answer either of them. [Laughter.]
306. Dr Wilde: Ok, well let us see. Nobody has been silenced so far. Have a look at the second question and see what thoughts it might inspire in you.
307. Professor Hannigan: As regards incentives to adopt healthier lifestyles; in December 2008, there was a UK-wide meeting facilitated by the MRC to set out what are called national ambitions to try to use research to lessen the burden of illness across the UK. In prioritising what could be done, obesity was discussed, and it was said that one of the problems is that we do not know, and there is no research to tell us, how best to change people’s behaviours. Therefore, it is too difficult to tackle and it is unlikely that it is going to be supported at the same level as other interventions.
308. I will be at a meeting this Thursday to see what is on the agenda as far as national ambitions are concerned, but research into how to change people’s behaviour has not been shown to come up with anything that really works.
309. Professor Perry: Research does not tell us how to alter behaviour because a lot of that research is predicated on a model that attaches too much importance to personal agency. Across the spectrum of public health, we overemphasise personal agency. There is a significant group of people who are convinced that if we could get into the schools and educate the children, and that could talk to the parents and change people’s knowledge. Of course, we have several decades of research that shows that no matter how much effort you put into doing that, it does not work, unfortunately.
310. In terms of evaluating natural experiments, there potential for a tremendous natural experiment, North/South, in that somebody said that if it was not possible to make a dent in the obesity problem here in the North, given the population size — which is, obviously, a economically-developed, well-educated population, and so on — and with very clear instructions, it will be difficult to do it in most places in the world. It is tremendously exciting, given that you now have a single public-health structure here in the North, to develop a series of initiatives at policy and environmental level, and then have a control in the South, where, sadly, it is unlikely that we will have any major developments in the next while. You can never be certain, but I think that we are a bit behind the North in terms of public-health leadership. It is fascinating to see what would happen if the North could really go for this at a public-health level and then we could make those comparisons with the South.
311. Dr Deeny: I am thinking that — and I do not know which side of the table has the researchers — it is great to have all the experts here today. The first question is how you can influence the policymakers. If each of you were given one or two sentences to speak in front of 108 Members of the Assembly or, indeed, the Health Committee, what would you tell us to do to tackle the epidemic of obesity?
312. Dr Wilde: Well, there is your challenge: the elevator challenge. You have practiced this for years, folks. [Laughter.]
313. Professor Livingstone: Money. That is my answer.
314. Dr Wilde: OK. Barbara is going to go first. [Laughter.]
315. Kieran is making a serious point. Let us go round the table and give us a good answer. That would be really helpful. Thanks, Barbara.
316. Professor Livingstone: It will certainly require huge investment, not just lip service. I appreciate all the limitations on the budget these days. You have to decide where your priorities lie. That is important to us who vote for you. If you think that obesity is a priority, then I think you must help us to put — we are talking about joined-up thinking, and I could not agree with you more — all the relevant agencies and bodies together. You must kick ass, get together and then start moving forward. That would be my opinion.
317. Ms H Ross: Claire was not here this morning, but Iain, Paul and I gave presentations on a childhood programme and a programme for adults.
318. Speaking specifically for our programme, and we have been running it for nearly 10 years, we have substantial evidence that it works. There is an opportunity to do what Scotland has done and fund a programme that works. What we are seeing in England is that the Government are saying, “Well, there is still limited evidence, so we will tell PCTs to follow evidence-based interventions." So, some PCTs use Counterweight, but it costs more to use Counterweight because we do not do a cheap and nasty training course: we follow our clinicians, train them, support them, and evaluate them. It costs more, like Paul’s programme.
319. Most PCTs in England send their clinicians on training courses to hear about evidence-based interventions, but it is not really evidence-based by the time it hits where the patients are. I think that we have two case studies in England. One could do what Scotland has done with its programme by finding something that works. If one knows what that part of the strategy is, one can join lots of bits on. Or, one can do what England has done and say that there is still not enough evidence, so we will say to do evidence-based interventions, but one will end up with more chaos. That is my reckoning.
320. Professor Perry: I have a two-minute pitch. As politicians, you must protect the taxpayer from the catastrophic exposure that will come from doing nothing. There is an economic incentive in large sections of the economy for us all to eat more. As policymakers, we are not here to represent the farming, food or any other sector that is clamouring for our votes. Ultimately, we are here to protect the health of the population, which will require us to take on the dairy and other sectors. That is probably not an easy thing to do, but it is part of the challenge.
321. Professor Kee: In clinical medicine, doctors sometimes talk about the teaching moment: for example, a person who has had a coronary might just give up smoking after that teaching moment. What would be the teaching moment for legislators should you have two minutes in front of them? Last year, in British Columbia, the Exchequer there produced a report that showed that it would be bankrupt by 2025 and all its money would be in the healthcare sector because of problems like obesity. There would be no money left for any other sector: education, defence, or whatever. That could be a teaching moment.
322. Let me mention another one. I heard about a simple intervention that was very effective; it was to put up better signage at stairwells to get people to use them. The signs did not just say “Please use the stairs"; they used a phrase that was something like “Can you spare a minute to save an extra two years of life?" The message was that, if you habitually take the stairs, which takes several minutes per day, you add to your life expectancy. In trying to create a teaching moment, you must make it personal to the legislators and tell them that they have the opportunity to make a difference.
323. Professor Broom: To follow up on what Frank said, in the future the UK will be spending its entire current NHS budget on treating type-2 diabetes. If we carry on as we are going, it will not be able to treat anything else. I would also like to back up Barbara by saying that we need resources. If we spent even half as much on obesity as we spend on an anti-smoking campaign, we might get somewhere. We need proper advertising. There is lots of advertising on television about stopping smoking, but there is only a 7% success rate. That is not a huge success rate, but the number of smokers is gradually coming down. We can do better with obesity; we can give you a 30% success rate.
324. Professor Gately: My comment is that we should act, invest and lead. The action is absolutely necessary for all the reasons that my colleagues mentioned. Not acting means that future generations will suffer the economic and health consequences and will have a poorer quality of life; it is as simple as that. I deal with children who weigh between 20 stones and 30 stones. There are lots of those kids out there. Their lives are effectively ruined before they become adults; it is as simple as that. If we do not act now, those numbers will continue to increase.
325. Investment is absolutely critical, and it must be in quality and in programmes that show outcomes but also show a commitment to development and research in the future.
326. Aligned with that is that there is an element of success breeding success. When we first started in our area of work, we were absolutely ridiculed by the media on a number of different fronts, but when we showed the strong outcomes, I had health professionals coming back to me a year or two later. They said that they were among those people who had questioned what we were doing but they said that we had actually done it, we had gathered the evidence and fed it back to them and had shown strong outcomes.
327. That is the investment, but with a commitment. That is also linked into the leadership. Healthy Weight, Healthy Lives, which is a Government strategy, is an excellent strategy, but there is a gross limitation in the action plan associated with it. There is nice talk about leadership, but unless there is true leadership, we might as well not even start.
328. Mr McFarlane: Just to pick up on the theme that has been running here, I think that there needs to be commitment — and all of this is going to take resourcing — but within that, we need to recognise that the system which we are operating in is not necessarily designed to best fit that. In other words, what I am saying is that obesity is clearly a Department of Health issue, but it has fundamental things that will contribute to it that lie in other Departments; neighbourhood renewal, sustainable development. The system in the Civil Service actually does not lend itself to that kind of collaboration. I would urge the Health Committee to be courageous in terms of seeing that other Departments can help you realise some of the goals here, but recognise what you are dealing with.
329. I also think that, to come back to the question … I absolutely take Hazel Ross’s point about evidence. You can say we need more evidence or you can say we can talk about this until the cows come home, until the disaster befalls us and it is too late, which goes back to the point that you were making about action, and I absolutely agree with that. The question is around how you can mobilise and support local communities. I think there is an opportunity coming in Northern Ireland for the research community to actually really get to grips with that through the community planning process. We do not know what that is going to look like yet, quite frankly, and I think that there is a real opportunity there. There is a schism and a gulf between policy development and implementation, and I think the research community can really help to bridge that. We need to start listening to what communities are telling us they need, and not imposing on them what we think they need.
330. Dr Wilde: The first bit of what Gary said is moving us to this idea. As well as the points that have been made in relation to Dr Deeny’s challenge about the points that you really would want to make to politician, Gary has moved us to this idea of what else needs to happen in the wider obesogenic community — issues like what kind of design of communities do we need to challenge that stops the children getting to the point where their lives are being ruined or where they require surgery or whatever. If we could just move to the second bullet point in question 2 and just think a little bit about not only how the research community can involve local communities in tackling the effects of an obesogenic environment, but also how can research help in relation to the kind of built environments that we are creating within Northern Ireland, ie question 4. That is such a crucial part of the creation of the obesity epidemic. Perhaps, around the table, we do not have researchers, apart from Frank Kee’s point about the design of the Connswater work, but I would like to hear something from you about that for the Committee.
331. Mr Rollins: I am still not convinced that the MLAs really understand the problem. We talk about a quarter of children in Northern Ireland — 100,000 kids. I have seen a 13-year-old who weighs 21 stone, and I am wasting my time talking to the local leisure centre manager that I am happy for her father to supervise her on the treadmill. I am thinking, what am I wasting my time on? I am not convinced. It is a huge problem out there; there are bad enough genes as it is for all the other things. I do not know what we should do, or whether we should use shock tactics. Before we can get into this, I do not see that the public really realise the huge problem we have.
332. Dr Wilde: Maybe, just to respond to that, part of the day was really about creating dialogue. Dr Deeny has asked you a question. Are you returning to Kieran and other members of the Health Committee to say, do you really —
333. Mr Rollins: As Kieran says, there are a lot of issues currently in Northern Ireland, but where does obesity fall in. I do not think that we are convincing, and we need to convince to help the Health Committee and what we can do to try and highlight the problem further. We are no different to everybody else, but this is Northern Ireland or the South of Ireland or together.
334. Dr Deeny: Just one point. Paul Gately mentioned the word, and it has been discussed in our Health Committee but it has by some of the members, about all the research has proven beyond a doubt that this is — and I agree with Mark Rollins here — to suggest that politicians are not in touch with reality, and that is not the first time that has been said.
335. Mrs McGill: You should not generalise.
336. Dr Deeny: It is not just Department of Health, it is societal; it is the whole issue of obesity. Certainly, it is like a lot of things, it falls on health to deal with the results of what is a societal problem. What I am wondering about — and you talk about leadership — should we appoint in Northern Ireland a leader who will co-ordinate all these Departments. If, for example, I have mentioned a few times about education, and we are talking to them in a couple of weeks, but I know that there is guidance that every school should give two hours per week in Northern Ireland for activity. It is only guidance, and I know that some schools do not do it; they are more wrapped up in achieving academic qualifications. We said this a couple of weeks back, we do not want our population going off with all these A levels and A stars, but being very unhealthy and obese. We should be saying — we need somebody maybe to co-ordinate all these Departments and give that person a very important role; but also responsibility that if they see all this research that is coming forward and all the evidence that is proving that we are fat and approaching a health disaster —
337. Professor Broom: I am not sure where this two hours has come from, because, when I was a kid, we had five hours a week compulsory physical education. Why have we lost that five hours? Where the devil have they gone to? We should get it back again.
338. Dr Deeny: I sense the frustration, and being a clinician as well, where I sense at this part of this side of the table where you want to see action and want to see things being done. It is frustrating. Again, I do not like writing drugs for obesity when I think maybe I could be doing something else. Whereas if we had somebody who has that responsibility and has that role and seeks that all of this research and evidence that we have is put into action and as soon as possible. Do you think is that an idea? An individual named and employed as such, rather than everybody trying to pull the same way but nobody —
339. Professor Hannigan: If we re-interpret the community to mean also GPs and other primary care practitioners within the community, because we did discuss earlier the fact that, potentially, helpful interventions are not being delivered because GPs are not being paid for it, does not suggest that they are fully engaged with the seriousness of what is facing us. But to take an extreme, not necessarily a personal view, but if we have said for alcohol and tobacco you cannot sell them to under 18s, and if we are saying the potential effect of obesity is greater than the detrimental effects of alcohol, why don’t we say you cannot sell x foods to under 18s?
340. Professor Perry: I would be inclined to agree that, in a sense, you will need a level. That sounds extreme, and you might not agree, but that is the idea. It is policy at that level of seriousness that will possibly be needed, maybe not through banning, but through taxation. If you look at how cheap it is for kids to buy these games — for the Wii, the PlayStation and so on — and there is fiscal policy there, and then there is the whole kind of advertising. Legislation or something can be done about that. People will say that we cannot do anything locally because it is all at EU level and so on, so I am not underestimating the complexities.
341. We will, in time, move towards measures like that. I often make the analogy with being asked to turn off our lights at home to protect the climate from global warming. Personally, I think that being advised to turn off the lights is almost comical. We need systems-level investment in nuclear power to reduce our reliance on fossil fuel. In the same way, we need serious, systems-level responses, not sort of little tokens that make us feel better but achieve little.
342. Professor Gately: I am just picking up on the points from Dr Deeny and Mr McFarlane. The way I look it is that it is a relatively new issue and we, therefore, need a relatively new solution. What, in many ways, we try to do is to utilise the capacity that is out there at the moment. So, I often, and this is going to be much more implemented across England in the forthcoming year, is the use of multidisciplinary teams for interventions.
343. Now, I would love to do a research study that compares a multidisciplinary programme against a multidisciplinary team, because most often when I work with multidisciplinary teams they are not delivering a multidisciplinary programme, it is a number of independent people all doing different things, but it is not joined up with the person at the heart. And so often we are trying to fit this issue into a box that does not necessarily exist, and I think we need to seriously think about that and how we are going to do it.
344. I think that Gary McFarlane’s point is really well made, and I often talk about this. The outcomes of obesity are health-related, but the inputs have very little to do with health, which is why I see that my clinical colleagues are very frustrated with something that they have absolutely very little to do with that they are dealing with. One of the things that I find, interestingly, I think, why health picked this up as an issue is they are very competent at picking issues and working through a process and documenting that process; that is why health does very well, whereas, in some ways, education does not do that sort of process as well. And education, and other Departments, could have a much stronger impact on the input, and that is why I think that, arguably, you move obesity out and make obesity an issue to be deal with in its own right, deal with it in its own way, with a new solution, let us say, whatever that might be, whatever structure that might be.
345. But, the key thing behind it is that there is no point putting an obesity czar in with no ability to lead, or invest or action, because you are just shifting the responsibility somewhere else. It comes back to a commitment action, and I think it does probably need a new solution.
346. Dr Harper: One thing that would certainly make the public health agencies role easier is that, from my point of view, the ideal is with the Executive own this as an issue, so that across the Executive there is then, you have got the, and you are using the accountability lines for individual Ministers and their Departments, so that they are able to deliver — whether it is the Department of Education, DETI, DEL or any of the others — their element of it and are held to account by the Executive. Equally, the Executive are then taking decisions about prioritising the prevention or reduction of obesity as an outcome.
347. If that is happening at a co-ordinated, central-government level, then, at a local government level you have got the Public Health Agency as a regional organisation that can bring some of that co-ordination in terms of what is needed and drawing people together, but you have also, then, got our relationship with local government and what local government will be doing around community planning. So, you are trying to in both some regional consistency, but also, then, that local flavour of action on the ground, again, cross-sectoral. You have then got that tie-up between the central-government action and local-government action, and the local government able to take it down then into the neighbourhoods and the communities that need it, so you have got that total blend. That would be my ideal, if I had a choice.
348. Dr Wilde: OK, it is 2.45 pm, and what I said was that we would try and have a discussion until about 2.45 pm before we drew this to a close. I just want you to have a quick look at the questions again. We have got into question 4 a little bit, particularly in the last bit of the discussion. We have not talked very much about surveyance, although that point has been made several times.
349. Could I just ask you spend a minute looking at the sheet with the questions to see if there is anything else that leaps out at you that has not been said by anyone during the course of the debates that we have had.
350. Dr Harper: I suppose there is just one point from my perspective: while the statistics are frightening in terms of the trends and the direction that it is going in, at the same time about 40% of the adult population is currently not overweight. There is something about learning from those people in terms of what they do and how they manage their energy balance as well. If some of the research communities could study those individuals as well as the other side of that.
351. Professor Harper: The other point would be things that we do in other areas that do not have a huge obvious obesity — [inaudible.] — for themselves. I always come back to say investing in preschool education and so on, and giving kids the kind of intensity of an educational start in life that reduces their risk in life of all sorts of health problems; alcohol and substance abuse and smoking. Increasingly, the evidence is coming forward that kids do better in terms of obesity in that kind of emotional and educational support in the first decade. It is a very obvious point, but we are never tackling obesity by itself; there is the alcohol and the smoking and mental health and so on.
352. Dr Wilde: In terms of general points, everybody has had a really good chance to say what they wanted to say. Do you think it would be possible for us, in the last 10 minutes, to pick up and decide and agree about seven points that we would really like to put to the Health Committee before I start trying to do something that maybe impossible, do you think this is possible? I can only do it if you help me so I need to know do you think it is possible that we could do that. Would anybody like to dissent from that? So we are going to give it a bash.
353. From the very brief notes that I have taken on some of the points that I have made, I will try and pick out about 10 or 11 points and then if you think that one of them is not sufficiently important, so we are really going now for the big points, metapoints if you like, that we would like to put to the Health Committee in relation to what has come out in this discussion between researchers and stakeholders with some input from MLAs.
354. The first point that I think has come out strongly is the idea of making quite sure that there is a joining up, a partnership if you like, between the research community, stakeholders, communities, and where appropriate, politicians and policy makers. That has been a constant theme that people have said.
355. A second point that has been repeatedly made is that it is important that in Northern Ireland, where we believe so much is going on, that there is a real attempt to try and co-ordinate what is happening in a really firm and clear way, and that without basing our interventions on some kind of evidence, that it is basically not ethical to continue to develop interventions when we do not know whether they work or not. Sorry, I have not said that very elegantly, but I hope you understand the point that I am getting to which has been made several times.
356. Thirdly, and I think we are very lucky to have had the folks from outside Northern Ireland, that we should not be reinventing the wheel and when there is evidence of something that is good, please could we pick it up and decide this is what we are going to run in Northern Ireland and not feel that we have to reinvent everything from the start. We have had some very good examples and some clear examples of things that work, so could we make sure that those are picked up and taken on.
357. The next point relates to cross-government work, and there is a very great call from everybody around the table to ask the Health Committee to help in making sure that obesity is seen as a real priority for Northern Ireland, for the Executive; it is not just a matter for the Heath Committee or the Health Service.
358. I know that that is something that has been said many times, and it has been said to the Health Committee. However, it is something that the Health Committee can take a leadership role on in a much greater way than any of us can as researchers, stakeholders or policymakers. The idea of obesity being a really big issue that is causing, and will cause, mammoth difficulties is only going to be solved if the Executive pick it up, make it a priority and consequently provide investment.
359. There is an issue outside Northern Ireland, at European level for example, where a lot of what happens is influential and very important in terms of many health issues but particularly obesity. Although it has not been mentioned, I think that we should be asking our MEPs to make obesity and health a much greater concern. It is OK to be the farmers’ friend, but what about being the friend of the people of Northern Ireland as well? That is another major point.
360. The next point that was made is that it is important that we challenge the people who are not obesity friendly. While on some occasions that means that we can work with the food sector, there are going to be occasions on which they have to be challenged. The point about challenging other interests and vested interests wherever they come from is important. We need surveyance systems, and I take the point about frustration and getting onto action. However, we will not know what is working unless we have decent surveyance systems, so it is important to keep that going and to ensure that the surveyance is fit for purpose.
361. I may have said something like this before, but another point is to make sure that when we adopt programmes that work, that we do it in a comprehensive way; others have described that too, particularly Paul Gately, Iain Broom and Hazel Ross. We are not just looking for short interventions; we are looking for systems interventions that are related to a decent research-and-development function as part of that; I think that Carolyn Harper described that as well.
362. Talking about the Executive picking up major issues, I think that one of the key issues is the pricing issue. Obviously, it is only when the Government take obesity seriously, and when there are proper policies that relate to obesity at Government, economic, financial and pricing level, that we are going to see really good change.
363. OK; that is some of the points that have come across to me. Have I left out any of the big points that were raised? Please just say if I have. I am sorry that we do not have a flipchart, because that would make it a lot easier.
364. Dr Deeny: This point is directed more towards Carolyn Harper or her new department or agency. The role of the media is something that has not been mentioned today. The media has played a very strong role in alcohol and tobacco, for example. Awareness of the obesity and its consequences has been mentioned by a number of people. I do not think that the public are nearly as well aware of the serious nature of the matter as they should be.
365. Dr Wilde: I think that that is something that Paul Gately mentioned, and maybe he would like to say more about it. Thanks Kieran.
366. Professor Gately: That is one of the areas that we have been trying to do some research on. We started to get much more engaged in the media by having a whole range of families in our interventions asking the most ridiculous questions that they had read in ‘Cosmopolitan’ or seen in a TV programme. We spend a lot of our time re-educating those people from the popular media that has negatively influenced them. That is a fundamental challenge, and we have looked at it. We have tried to get some research money to look into TV shows that we would argue do present positive and sound messages as opposed to some of these TV shows that do not; it is very difficult to do that.
367. We also went to the Department of Culture, Media and Sport (DCMS) and asked if it would be interested in asking the question. It said that it is the Department of Health’s responsibility to look after obesity. When I asked the Department of Health, it said that that is not really on its agenda. The media have a massive role to play. The problem is the context of investment.
368. Last year, with colleagues in Yorkshire and the Humber, we looked at an investment as part of the Change4Life strategy for a TV programme, ‘Influencing Families’, based on very sound evidence-based information. We were trying to look at a public-private partnership in that we would get the TV company to invest in it in terms of what they would normally pay for a TV show but then get the Department of Health to invest the rest of the money to make sure that it was evidence-based and sound.
369. All the longer-term components of the entertainment aspect, which cost more money and which TV people do not want to do because they want to get it quick and dirty and cheaper, whereas that NHS investment can do it. But then we fell foul of Ofcom regulations. It is just a real minefield of challenge, but not challenge that I do not think we can overcome.
370. I think that it is a key tactic of a strategy to engage with the media. When I was at the Ulster Paediatric Society symposium with Mark Rollins, we did some radio interviews. I think it is all part of how do you engage a wider public and practitioners in action, because the media is extremely powerful and if we use it the right way we can get a lot out of it. It is free as well. It comes cheap; if you give it something that is interesting, it is pretty cheap to achieve your objectives.
371. Ms Hanna: I think that it is right that it is a priority for the Executive, but it is like never-never land to be perfectly honest about it if you go on to the list of the Programme for Government. Unless some body or there is some champion there who is going to collate and who is going to get the evidence-based. Whatever we need to make sure that we move it on to actions, it has to be either a group. I do not think it is the new public health body, but I do think you have to be part of it. I do not think you have to take the whole ownership of it, but there has to a dedicated person or group. I do not think it is going anywhere if it does not. Certainly, it has to be in their priorities, but if you just depend on it going into the Executive nothing happens.
372. As a politician, I am being honest. [Laughter.]
373. Mr G McFarlane: It actually follows on directly from what Carmel has just said and to come back to the point that you made in your summing-up, Jane. First of all, I think that there is maybe value in the Health Committee seeing this as two different sides of the same coin. The treatment part is very much the Health Department and the health services’ issue. It is an urgent issue, and our colleagues down here have made that very clear all day and I agree with them and support them. But on the upstream preventative side, I absolutely agree that you need a champion.
374. I am not convinced that, if it goes into the Executive, it will go anywhere. Sustainable development went to OFMDFM out of the Department of the Environment and it is nowhere. That is just an example of what happens. I would urge you to be smart about the way in which that champion takes it forward, which is what I was trying to articulate, albeit maybe not very well. If you create a heading that is obesity is the number one and we need to make it a priority above all other priorities, it becomes another silo potentially in a range of competing priorities, all of which have merit.
375. I offer the climate change analogy notwithstanding our Minister and not wanting to get into that as an example, but to look for ways in which actually obesity can complement other cross-cutting agendas and be very smart about how you do that. Climate change is a great example of where actually the two are completely inextricably linked and actually entirely complementary. There are others. Champion yes, but the way in which you take that forward is the new approach, not this is the issue and everybody must come here but this is the issue how do we embed it in other key strategic policy areas?
376. Dr Harper: It is good to have the advice about the Executive. In the absence of that, certainly as a public health agency, this issue will be one of our top priorities and we will be looking very much to get action on the ground to address it.
377. Building on Gary’s point, if we tackle it as an obesity issue, it becomes all the negative connotations of that. Through the agency and through the other work that we will be doing, we will be doing a lot of interventions in communities and building on the back of those and piggybacking on those. Much of this is about giving people some life skills about nutrition and food preparation and understanding some of the issues around portion size and calorie content in food, and so on. So, building on some of those other things that we will be doing in the agency anyway as much as we can and working then, as I said, with the other sectors at council and local government level to take forward some of those other initiatives over and above that.
378. Mrs Hanna: Chair, I should have said that, within Government, I think it is so obviously cross-departmental from the Department of Education, to the Department of the Environment, to the Department for Regional Development. It cannot just sit in the Department of Health, because there is just too much. Certainly, if we do anything in the Health Committee, as I have said to my colleagues, it has to be a cross-departmental group.
379. Mr Rollins: But it is where the drive comes from. I am conscious today that important players are not here, such as the Department of Education and the Department of Culture, Arts and Leisure. They have tremendous expertise, but they are not going to drive it. The drive has to come from the Department of Health, whether you like it or not, in co-operating with those members. They have the expertise. There are tremendous obesity-related skills going on, but somebody needs to pull it together, because we are just drifting in circles.
380. Paul is worrying about the English tsar; in Northern Ireland, we need somewhere to head this up. We need to know exactly what is going on. There are projects going on, and none of us here knows what is going on. They would be crying out to tell us about them today. We need to know what is going on and then drive it forward. The Department of Education is not going to do it on its own, and the Department of Culture, Arts and Leisure is not going to do it. It has to come from the Department of Health.
381. Dr Wilde: I totally agree with what Mark is saying. I do think that, with something like swine flu, it is pretty clear who is doing what: everybody has got a role; it is a major issue; Carolyn knows what is happening; there is a trust meeting; three breakfast meetings a week; and everybody is getting organised. And obesity? Fine. So I think that we have a lot to learn from how we cope with communicable disease. Claire, you had a point a little while ago. Then I will pass to Kieran to close it on the grounds that everybody has had a really decent chance to have a say. OK, Claire?
382. Mrs McGill: I was just going to formally dissent from Carmel’s comments about the Executive. [Laughter.]
383. Dr Wilde: Oh no, the Health Committee has started disagreeing with each other.
384. Mrs McGill: It is just a joke.
385. Mrs Hanna: It is coincidental that it is the DUP and Sinn Féin.
386. Mrs McGill: I am Sinn Féin. Joking aside, I think it was Gary who mentioned neighbourhood renewal and in terms of working together. Certainly, the Executive have a role. Neighbourhood renewal is particularly cross-departmental. Neighbourhood renewal was supposed to deliver — for those people who are maybe not familiar with it — all of this in disadvantaged areas, where evidence would appear to show that obesity and overweightness — if that is a word — is a problem in those areas. So the neighbourhood renewal thing did not really have the joined-upness that it should have, in my view.
387. Maybe the Executive will, or will not, resolve these issues. I am not even sure that the Executive is the place for this. There are competing challenges and priorities, and when we all sit round the table and say that everybody should do whatever, sometimes it gets more difficult the bigger the whole thing gets. So, while probably the Executive will do what they can, and we will speak to our own individual Ministers — and we have all got Ministers in the Executive — certainly the profile could be raised.
388. Dr Wilde: Iain and Paul just want to say something.
389. Professor Broom: It is quite fortuitous, because you just hit the nail on the head, Claire. I was about to say that I drew up a programme for the Scottish Executive based on deprivation, because they had already made up their mind that, from a public health point of view, they were going to, effectively, target moneys in disease prevention in deprived areas. The data from the Counterweight programme clearly demonstrated that it was most effective in deprived areas.
390. Therefore, the money came with the Keep Well programme. The weight management part of the Keep Well programme did exceptionally well and was well ahead of the rest of the programme. Therefore, it was actually hived off from Keep Well and is now a completely separately funded programme by the Scottish Government. They ring-fenced £40 million from their total health budget. The English budget was £400 million, which is roughly about right — 10% of the population. That £40 million was ring-fenced for obesity strategic work, of which 10% was delivered to the Counterweight programme. Therefore, the Counterweight programme receives £4 million of funding from the Scottish Government to run it throughout the whole of Scotland.
391. Professor Gately: I know that it is not a discussion for now, but it is really to try to understand what are the key drivers, because we are talking about an issue that is the most common disease in our children, yet no public health services, educational services, social services or children’s services cater for that group.
392. I do not want to finish on a downer, because we have had such a positive day. However, I think that the message of Every Child Matters is absolutely right, but you do not matter if you are an obese child.
393. Dr Wilde: Perhaps that is a good note to finish on. I thank the people who helped to get this session together and to thank the Health Committee for encouraging us to have the session. Thank you very much.
394. Dr Deeny: It is my duty to close the session. I have found today to be very beneficial. As a doctor, I know that obesity is an epidemic. We mentioned swine flu and the great work that the Department is doing to deal with it. I do not wish to end on a negative note, but obesity kills, and thousands of people will die prematurely. Therefore, it is a very serious issue, and it is good that everyone here is singing off the same hymn sheet. We all know what we are facing here, and it is about getting that message out right through society. The media can play a very important role in that.
395. I have been in general practice for nearly 25 years, and I can see the changes in young folk. GPs now have to record smoking status, and, in the past two years, two young girls have told me that they smoke because it keeps their weight down. That is unbelievable. One of the girls said that she was very happy with her body and that she will stop smoking when she is 30. She is only 15 now, and I told her that it will be very hard to get off the cigarettes when she has been smoking 15 years. Therefore, those are the sort of issues and knock-on effects of obesity. People just think of obesity as being overweight, but they do not realise what else is involved.
396. This has been very helpful, and maybe it is the beginning of something. The Health Committee must really think about this issue very seriously. The Committee’s first inquiry into the prevention of suicide was a very important issue as well, and it was very much a family problem. Now we are conducting an inquiry into obesity, and, the more you look into it, the more you realise just how serious it is. Therefore, your contributions have been more than useful.
397. I will finish off by thanking everyone who has taken part in this very worthwhile event. It will feed into the Committee’s inquiry, and we hope that we will have practical benefits in the battle against obesity. I thank Dr Jane Wilde, in particular, for developing the original idea and for chairing the proceedings. I also thank the researchers who have given up their time to share the outcome of their research with us. I thank all the stakeholders who have come along and shared their experience with us and took part in the discussions. I thank the members of the Health Committee who called in at various times and have taken part in the discussions. I also thank Assembly Research staff and our Clerk, Hugh Farren, who is always top class when it comes to organising things. He wrote that for me by the way. He did not write that bit. [Laughter.] I have put that in.
398. A lot of work has gone into today’s event. I want to thank the Committee team for arranging it and Hansard for recording it. The Health Committee will take on board everything that has been said. I hope that you get a chance to read our report. Hopefully, it will give a kick-start to addressing the major challenge of obesity and its serious health consequences for this part of the world, working alongside those of you who have come from different parts.
399. Lastly, I wish everyone here a safe and pleasant journey home.


Professor Gately’s Powerpoint Presentatiion:
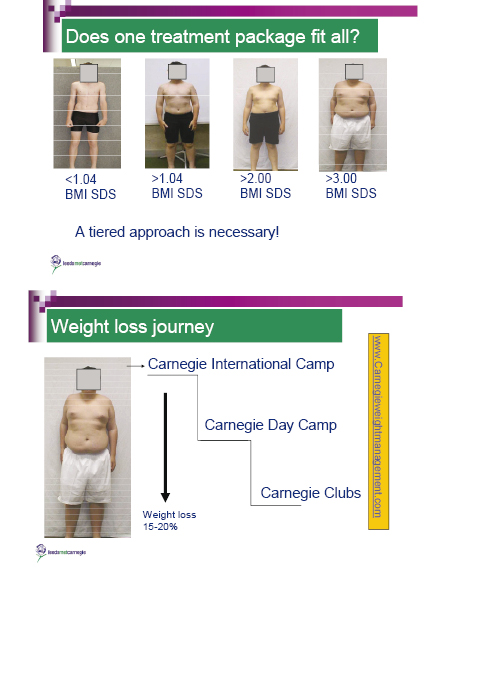
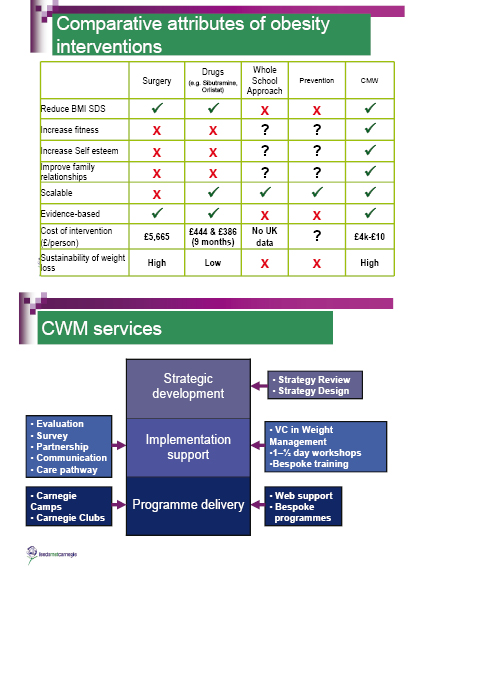
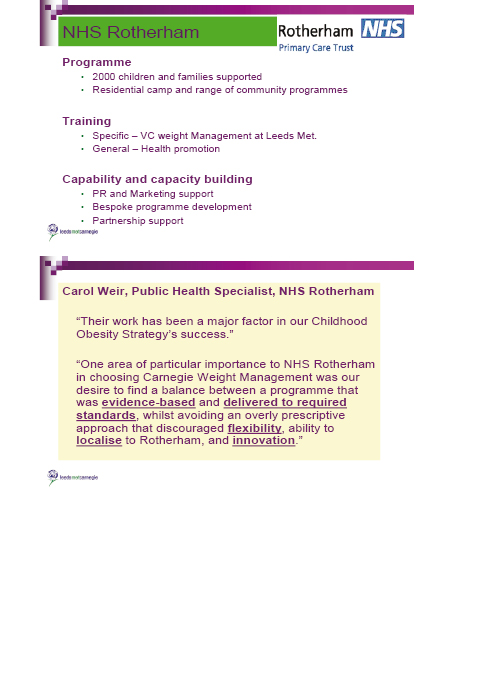
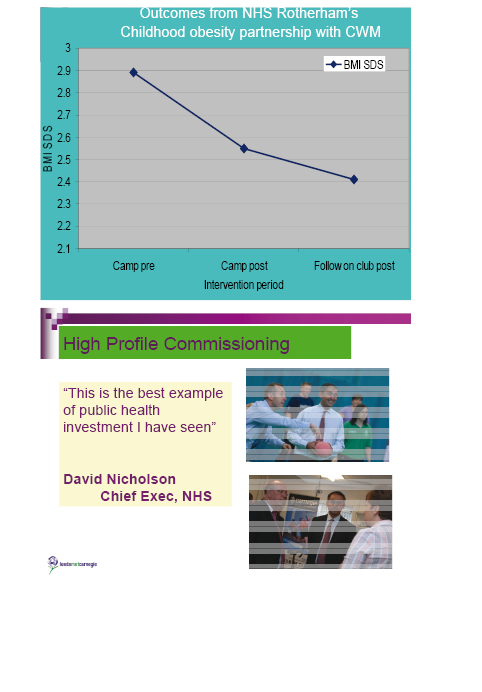
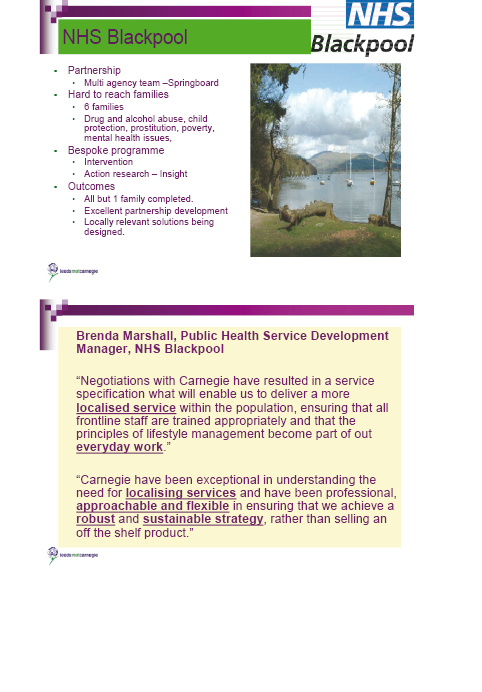
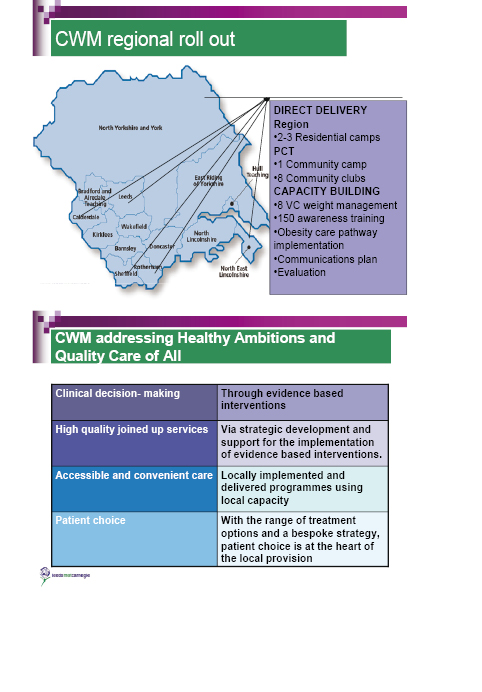

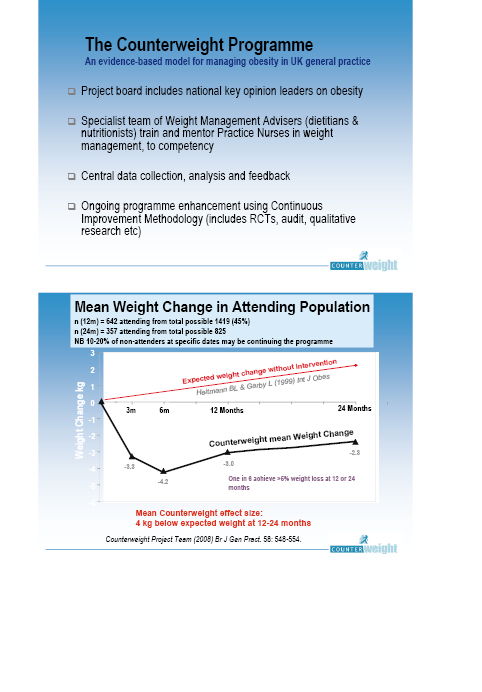

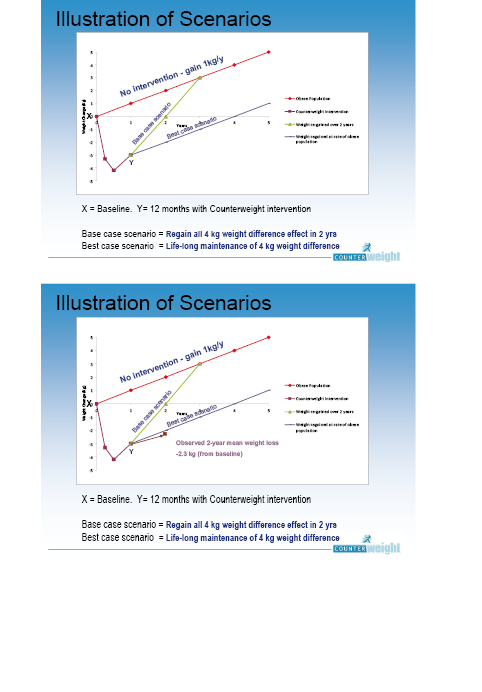
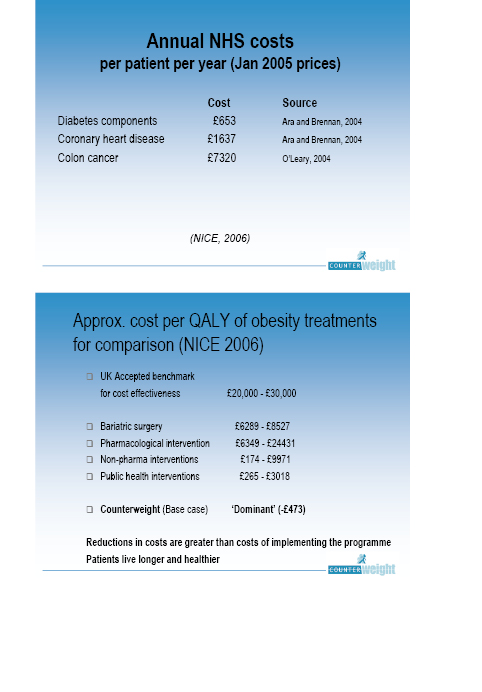




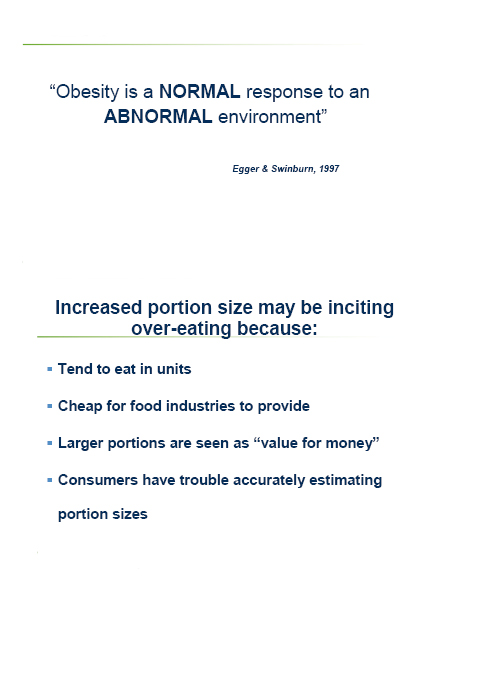

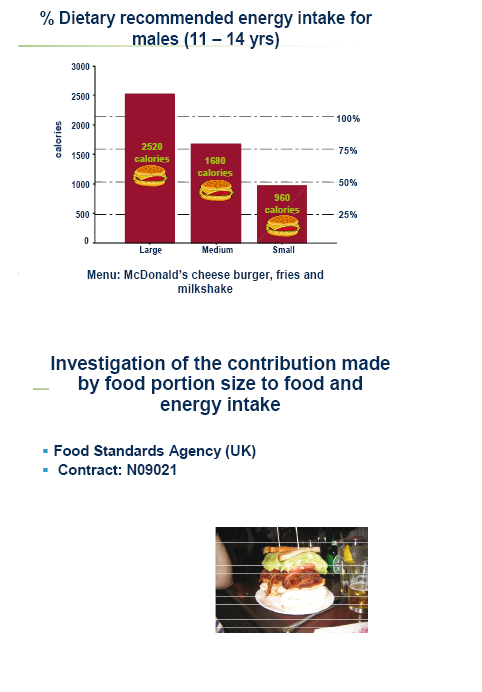
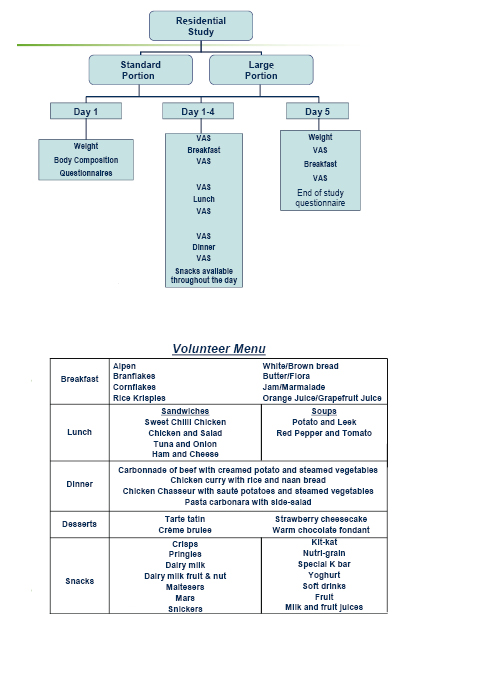
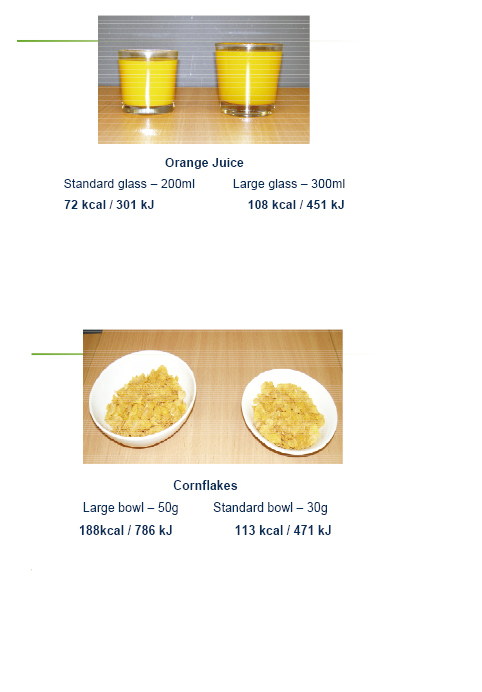
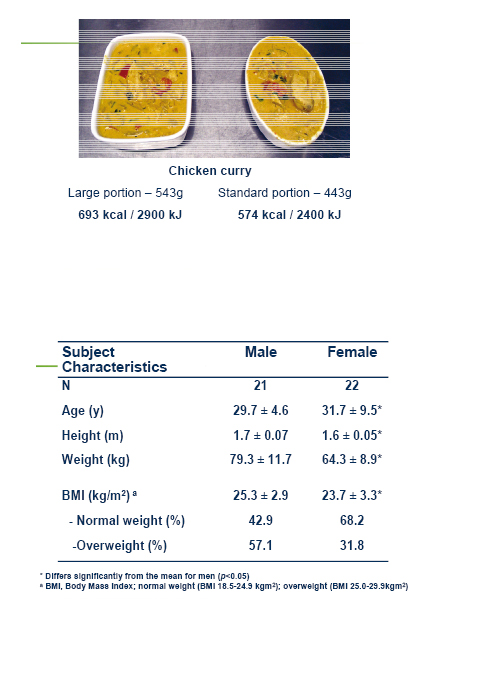
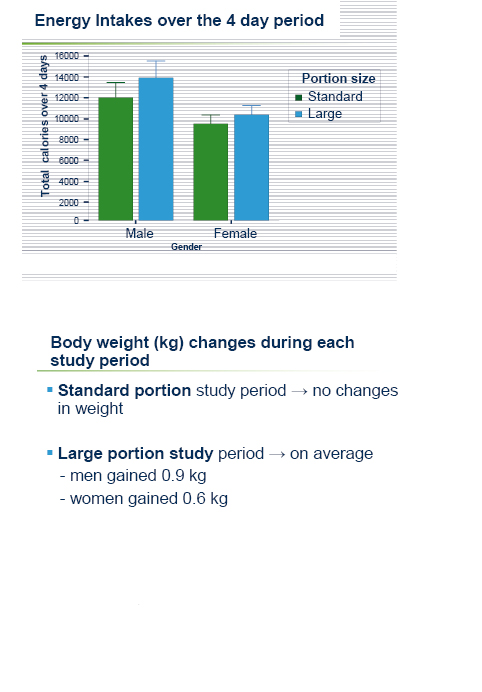

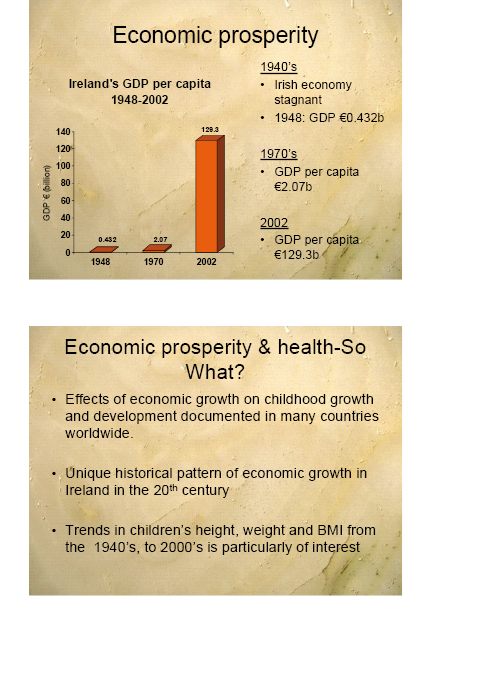
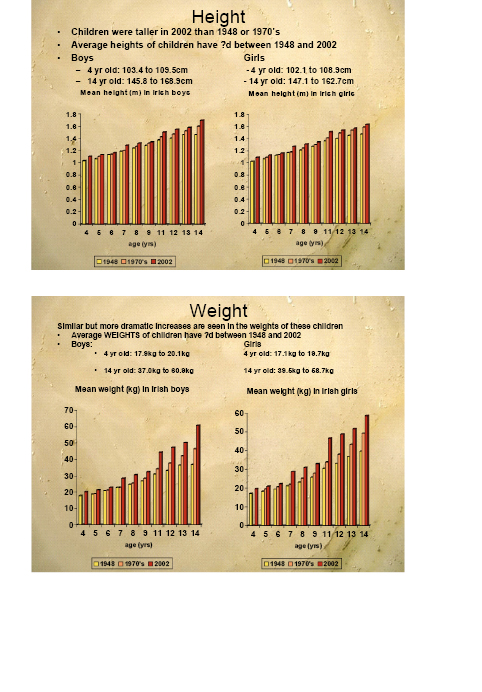
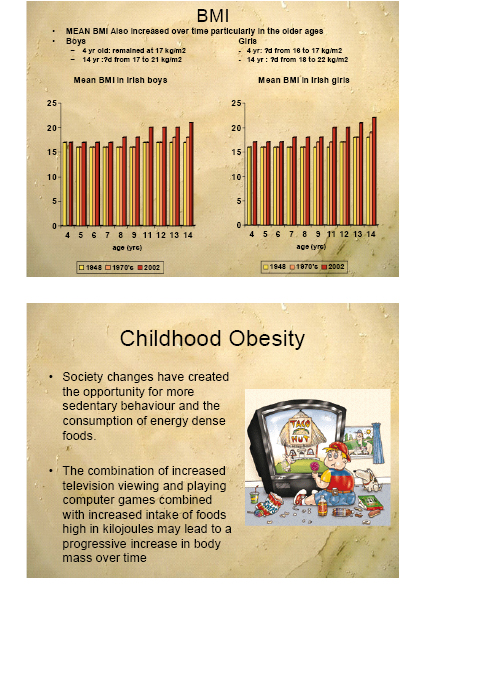
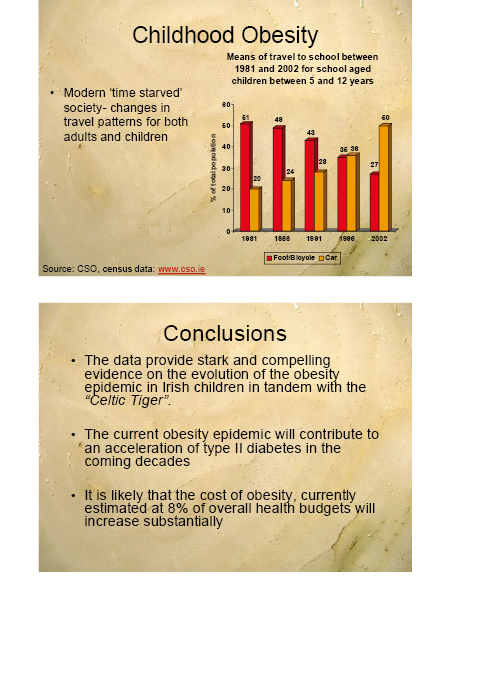
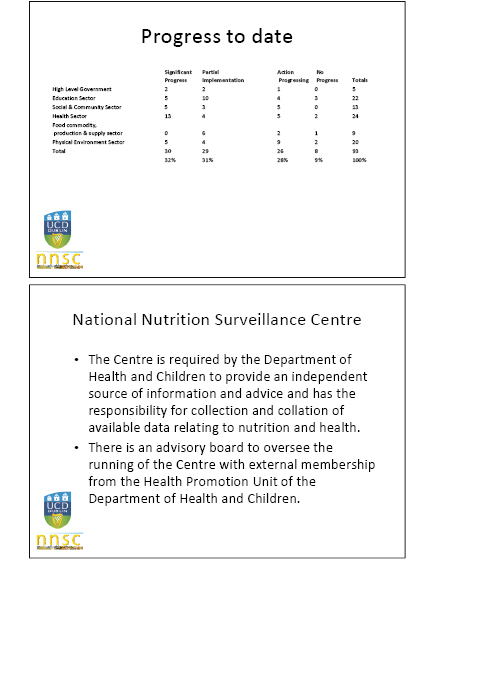

Appendix 6
List of Witnesses who gave Evidence to the Committee
Witnesses who gave Evidence to the Committee Regarding the Inquiry into Obesity
26/02/09 |
Dr Jane Wilde |
Institute of Public Health in Ireland |
|
05/03/09 |
Dr Naresh Chada |
Department of Health, Social Services and Public Safety |
|
05/03/09 |
Dr Caroline Hughes |
Action Cancer |
|
12/03/09 |
Mr Nigel Gould |
British Medical Association Northern Ireland |
|
26/03/09 |
Dr Michael Ryan |
Northern Health and Social Care Trust |
|
02/04/09 |
Ms Tracy Gibbs |
College of Occupational Therapists |
|
Ms Pauline Mulholland |
British Dietetic Association |
||
Ms Teresa Ross |
Chartered Society of Physiotherapy |
||
23/04/09 |
Ms Mairead Boohan |
Queen’s University Belfast |
|
23/04/09 |
Ms Karen Smyth |
Northern Ireland Local Government Association |
|
Ms Katrina Morgan-Talbot |
Belfast City Council |
||
30/04/09 |
Professor Eamonn McCartan |
Sport Northern Ireland |
|
14/05/09 |
Ms Gerry Bleakney |
Public Health Agency |
|
21/05/09 |
Mrs Maria Jennings |
Food Standards Agency Northern Ireland |
|
21/05/09 |
Mr Andrew Dougal |
Northern Ireland Chest Heart and Stroke Association |
|
Mr Iain Foster |
Diabetes UK Northern Ireland |
||
Ms Victoria Taylor |
British Heart Foundation |
||
28/05/19 |
Dr Una Lynch |
Queen’s University Belfast |
|
11/06/09 |
Ms Jill Fitzgerald |
Department of Education |
|
11/06/09 |
Mr Michael Bell |
Northern Ireland Food and Drink Association |
|
18/06/09 |
Ms Clara Swinson |
Department of Health (London) |
|
18/06/09 |
Dr Naresh Chada |
Department of Health, Social Services and Public Safety |